A Practical Guide To Meaningful Use: Federal Register, 75 (144), Wednesday, July 28, 2010, Pp. 44589-44654
Diunggah oleh
dnice408Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
A Practical Guide To Meaningful Use: Federal Register, 75 (144), Wednesday, July 28, 2010, Pp. 44589-44654
Diunggah oleh
dnice408Hak Cipta:
Format Tersedia
A Practical Guide to Meaningful Use
Meaningful Use is a daunting issue confronting health systems today. Concerns about meeting its requirements have taken the forefront in shaping the decisions that are being made now by hospitals, physicians and other healthcare organizations that will have far-reaching implications. It is clear that the correct decisions must be made now; what is not clear is exactly what all the requirements will be. Until now, Meaningful Use requirements have been a moving target, and they still are to some extent, although the Final Rule document published by CMS [Centers for Medicare and Medicaid Services] on July 28, 20101, has provided a wealth of information. In addition, the Certification Criteria Final Rule was released by ONCHIT2 [Office of the National Coordinator for Health Information Technology] at the same time, adding yet more information. Yet all of the information included in these two documents, while crucial, is nevertheless buried in over 1000 pages; the Herculean task of reading the documents through completely and extracting useful information has led most hospital administrators and IT Directors to rely on the many outlines and guides that have been published since the Final Rules have come out. While these outlines are undeniably helpful in extracting the major points contained in the Final Rules documents, they still are just that; outlines. These one size fits all summaries do not begin to address the individual issues and concerns that each organization will find itself facing. Every organization is unique and brings its own concerns and challenges to the table. Each has its own culture, infrastructure and operating budget, within which they must interpret and carry out the Meaningful Use requirements. The challenge? How to obtain the information that applies directly to ones own organization in a format that is succinct and understandable.
Department of Health and Human Services, Centers for Medicare & Medicaid Services, 42 CFR Parts 412, 413, 422, and 495; Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Final Rule, Federal Register, 75(144), Wednesday, July 28, 2010, pp. 44313-44588. http://edocket.access.gpo.gov/2010/pdf/2010-17207.pdf 2 Department of Health and Human Services, Office of the Secretary, 45 CFR Part 170; Health Information Technology: Initial Set of Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology; Final Rule, Federal Register, 75(144), Wednesday, July 28, 2010, pp. 44589-44654. http://edocket.access.gpo.gov/2010/pdf/201017210.pdf
What is Meaningful Use and why should we be concerned about it? The CMS Final Rule states that an eligible provider (EP) and an eligible hospital (EH) shall be considered a meaningful EHR user for an EHR reporting period if they meet the following three requirements; i.e., they must: 1. Demonstrate use of certified EHR technology in a meaningful manner; 2. Demonstrate to the satisfaction of the Secretary (of CMS) that certified EHR technology is connected in a manner that provides for the electronic exchange of health information to improve the quality of health care, such as promoting care coordination; and 3. Using certified EHR technology, submit to the Secretary, in a form and manner specified by the Secretary, information on clinical quality measures and other measures specified by the Secretary.3 The Final Rule states that unless these three objectives are met, organizations and providers will not be considered for funds described in the HITECH Act 4 during the specified reporting period. An important corollary to this is that CMS has broken-down the achievement of these goals into three Stages, each of which has a list of specific goals which must be met. Organizations must be aware that while preparing to meet Stage 1 goals they must also be looking ahead to position themselves for the next stages and to carefully consider the choices available from their vendor with this in mind. Organizations must also consider during which reporting period and at what Stage they will choose to begin the process: some organizations may already be prepared to meet most Stage 2 requirements (which are due to be released at the end of 2011); to be eligible for payment during Stage 1 the criteria must only be satisfied for any continuous 90-day period during the reporting year. In addition, those hospitals or providers who do not begin the process until 2012 may still be eligible to receive the maximum amount of funding available if they continue to meet all requirements. Although the requirements initially proposed by CMS might have seemed unattainable for many organizations, after considering the many comments received during the Public Review period, CMS has lowered the bar considerably; whereas the initial requirements appeared inflexible, CMS has now revised them into a set of core criteria which are relatively static, and an additional set of objectives that may be chosen from a list, or menu, from which providers may choose the 5 that appear most relevant to their specialty or status.
3 4
See (1), pps 44326-44327. Health Information Technology for Economic and Clinical Health Act
Copyright, 2010 Healthcare Performance Group, Inc. All Rights Reserved.
Finally, the rules for quality reporting have also been simplified: now providers must only report data on three core quality measures for 2011 and 2012 (alternate measures are available for those providers to which these three measures do not apply), and three additional measures which may be chosen from a menu of 38 measures; in 2011 providers need only attest to the ability to document or transmit data on these measuresin subsequent years they will be required to actually submit the data results through the use of their certified EHR technology. Thus, many organizations that may have considered these Stimulus funds out of reach are now able to reconsider their options and begin to realign their strategic goals. Where do I begin? 1. Engage a knowledgeable member of your organization, or a Consultant working for your organization, who has read/can read the Final Rule on Meaningful Use from CMS and the Certification Criteria Final Rule from ONCHIT in their entirety, and understands clearly how each rule applies to your organizations particular situation. 2. Determine where your organization would best fit into the process: Which reporting period will you aim for? Will you begin in Stage 1, or can your organization meet Stage 2 criteria and save the time of achieving the objectives twice? 3. Consider the requirements for the next Stage(s) while preparing for the initial Stage; although rules have not yet been released, CMS has clearly indicated its intentions for the next Stage(s) in many of its responses to comments. 4. Choose the Objectives that your organization will seek to meet based on the core set and those from the menu set based on the organizations specific current state characteristics, strengths, and areas of specialty. 5. Understand what your vendors plans are for certification, and whether an upgrade will be needed or desired prior to beginning the process. Understand that the three Certifying Organizations have just recently been announced; therefore vendors have not been able to plan ahead with certainty as to what functionality would be necessary. So, you may encounter some hesitancy in vendor responses, and this is understandable, given the circumstances. 6. Work closely with your vendor through the testing and attestation process, and as biennial updates are released by CMS. How do we do it? Attesting to Meaningful Use will take a significant investment by the health system; it is not an IT or Quality Project but a housewide, enterprise wide initiative. The more one digs into the processes and objectives, the more details will rise to the surface and require careful examination. Failure to pay attention to them can be a lot like pulling a loose thread on a sweaterbe careful or it will unravel.
Copyright, 2010 Healthcare Performance Group, Inc. All Rights Reserved.
Given the critical, detailed nature of the objectives, we recommend a clinically driven, detailed process. Below we have provided an example of one objective; first, we define and completely understand the specific objective; second, we recommend following a proven clinical process to lead to adoption and attestation of the chosen objective. Example of a Meaningful Use Objective: 1. Choose an Objective to focus on: e.g., drug-drug, drug-allergy interaction checking, which is in the core set5. 2. Read the associated pages, including all commentary and responses, in the Final Rule document to understand clearly what this measure entails; i.e., does it include radiographic contrast media? Are food allergies included? Can we disable alerts due to alert-fatigue? Are any exclusions available for this objective? 3. Be certain that the EHR product provides this functionality, that it is enabled throughout the entire system, and that the EHR has access to at least one formulary for the entire reporting period. 4. Consider how this objective may be modified in future Stages and plan accordingly. 5. Attest to CMS, by the means specified by the Secretary, of the above. Clinical Adoption Process Steps Applied to Above Example (Drug-drug, drug-allergy interaction checking) We have chosen this approach because it is proven in the clinical treatment process and is well understood. This provides a repeatable framework that eliminates the trap of assumptions (rather than facts) and provides measurements and documentation of each objective. 1. Initial Interview/History: Find out how interaction checking is being done now Find out from your vendor which software version will be certified How well does the present method(s) work: What problems have there been in the past, system failures, sentinel events, and where did the process break down
See (1), pps 44334-44336.
Copyright, 2010 Healthcare Performance Group, Inc. All Rights Reserved.
2. Assessment/ Physical Exam: Read the Final Rule and become an expert on what it says about this Objective, then apply that info to your own system to determine what changes must be made Interview Pharmacy, RNs, Physician end-users, IT dept, etc., re: proposed changes in functionality Perform observational analyses of present user workflows Determine which reporting period and which Stage to begin working toward Compare State and Local requirements to CMS Meaningful Use requirements Perform stop-start-continue workflow analyses with users
3. Technical Assessment/Diagnostic Testing: What can the present system do; do we need to upgrade, and when Must other functionality be enabled/modified in order to enable this functionality Is a Formulary available to the System, can the functionality be enabled throughout system Consider how changes in this functionality will affect other areas/functioning of system Begin Testing and Attestation process
4. Discuss Data/Diagnosis: Evaluate results of testing and determine what is needed to modify the system to put full interaction-checking into use, if anything Continue testing and modification until functionality is achieved
5. Action Plan/Treatment Plan: Consider how this requirement will be modified/expanded in future Stages Upgrade system, if needed Train all users and end-users Successful attestation to CMS
6. Follow Up/Return Visit: Begin developing future functionality to move forward into next Stages of Meaningful Use. Evaluate effects on users and their reactions/response to new functionality
Copyright, 2010 Healthcare Performance Group, Inc. All Rights Reserved.
Wrapping Up Meaningful Use objectives are daunting, as will be the government-driven process; but it is a financial and competitive necessity for every health system in the US. The goal of improved patient care through quality driven processes should ultimately lead to better outcomes at lower costs but there will be many barriers to success. The most successful organizations will confront those challenges head-on by embracing the detailed analyses and other hard work needed to meet the requirements and ultimately emerge as stronger healthcare providers.
Corporate Headquarters Healthcare Performance Group, Inc. 23419 West 215 Street Spring Hill, KS 66083
th
Ph: 888-681-9501 Fax: 316-462-5900 info@HPGresources.com HPGresources.com
Copyright, 2010 Healthcare Performance Group, Inc. All Rights Reserved.
Anda mungkin juga menyukai
- Chapter 1 Capstone Case: New Century Wellness GroupDokumen4 halamanChapter 1 Capstone Case: New Century Wellness GroupJC100% (7)
- Analyzing Business Case and Feasibility of EMR SystemDokumen3 halamanAnalyzing Business Case and Feasibility of EMR Systemchandini50% (4)
- Android Attendance Management SystemDokumen54 halamanAndroid Attendance Management Systemskpetks75% (12)
- Telehealth Planning Guide for Program SuccessDokumen6 halamanTelehealth Planning Guide for Program SuccessHemprasad BadgujarBelum ada peringkat
- EHR Implementation Goals and Objectives GuidelinesDokumen12 halamanEHR Implementation Goals and Objectives GuidelinesrhvenkatBelum ada peringkat
- Enlc 553 Strategic Business ProposalDokumen18 halamanEnlc 553 Strategic Business Proposalapi-459703752Belum ada peringkat
- UservManual PDFDokumen62 halamanUservManual PDFanon_343750376100% (1)
- Health Analytics PWCDokumen40 halamanHealth Analytics PWCsandeep_prasad17Belum ada peringkat
- Wgu 2013commDokumen48 halamanWgu 2013commdnice408Belum ada peringkat
- Recommendations Focus Criteria On Value and Achievability - Meaningful Use MeasuresDokumen5 halamanRecommendations Focus Criteria On Value and Achievability - Meaningful Use MeasuresDavid HarlowBelum ada peringkat
- HL7 Meaningful Use - White PaperDokumen5 halamanHL7 Meaningful Use - White Paperarijit00Belum ada peringkat
- Ehr Selection: Fall 2009 Idn Summit Peer-To-Peer Learning Exchange Research ReportsDokumen9 halamanEhr Selection: Fall 2009 Idn Summit Peer-To-Peer Learning Exchange Research Reportsraduben5403Belum ada peringkat
- The Future of Revenue Cycle: Preparing For Near-Term ChangeDokumen30 halamanThe Future of Revenue Cycle: Preparing For Near-Term Changecala708391Belum ada peringkat
- Textbook of Urgent Care Management: Chapter 23, Choosing the Electronic Health RecordDari EverandTextbook of Urgent Care Management: Chapter 23, Choosing the Electronic Health RecordBelum ada peringkat
- B.1 Learning Objectives: System Life Cycle: at The End of The Lesson, The Student Should Be Able ToDokumen73 halamanB.1 Learning Objectives: System Life Cycle: at The End of The Lesson, The Student Should Be Able ToPark Yoon AeBelum ada peringkat
- Module 11 - Assignment-Her MuDokumen2 halamanModule 11 - Assignment-Her Muapi-509979172Belum ada peringkat
- Meaningful Use Risks - Internal Audit Assessment and ResponseDokumen32 halamanMeaningful Use Risks - Internal Audit Assessment and ResponseSpit FireBelum ada peringkat
- Opinion: Healthcare's Next Big HIT?Dokumen2 halamanOpinion: Healthcare's Next Big HIT?Milagros Karina Calapuja QuispeBelum ada peringkat
- Selection of A Patient Safety StrategyDokumen5 halamanSelection of A Patient Safety StrategyEdwin J OcasioBelum ada peringkat
- Pilot TestingDokumen11 halamanPilot TestinggasibuteaBelum ada peringkat
- CPOE/EHR ImplementationDokumen21 halamanCPOE/EHR Implementationjunaid_alauddin5634Belum ada peringkat
- Planning An EMR ImplemetationDokumen5 halamanPlanning An EMR ImplemetationShruti CholaBelum ada peringkat
- Health Information Systems Acquisition and ImplementationDokumen10 halamanHealth Information Systems Acquisition and ImplementationKenson KipchumbaBelum ada peringkat
- Health and Human ServicesDokumen57 halamanHealth and Human Servicesperry spiropoulosBelum ada peringkat
- HL7 News 20120105Dokumen44 halamanHL7 News 20120105antaskBelum ada peringkat
- EHRs and Meaningful Use: A Guide to Stage 1 & 2 RequirementsDokumen4 halamanEHRs and Meaningful Use: A Guide to Stage 1 & 2 RequirementsNkeletseng MakakaBelum ada peringkat
- Power Point On MU 7-29-10Dokumen24 halamanPower Point On MU 7-29-10dboundsBelum ada peringkat
- Long-Term and Post-Acute Care (LTPAC) Roundtable Summary Report of FindingsDokumen23 halamanLong-Term and Post-Acute Care (LTPAC) Roundtable Summary Report of FindingsONC for Health Information TechnologyBelum ada peringkat
- Steven Mitchell Report 8 Lis 4776 Advanced Health InformaticsDokumen7 halamanSteven Mitchell Report 8 Lis 4776 Advanced Health InformaticsSteven Napoleon MitchellBelum ada peringkat
- 1 18654 8-Tips For EHR Adoption.Dokumen20 halaman1 18654 8-Tips For EHR Adoption.AndreeaMare1984Belum ada peringkat
- B.4.6. Implementation PhasesDokumen2 halamanB.4.6. Implementation Phasesmaga2000Belum ada peringkat
- ComforceHealth ComplianceDokumen14 halamanComforceHealth ComplianceVintiBelum ada peringkat
- Outsourcing Technology In the Healthcare Industry: In Depth Research to Protect the Security, Technology, and Profitability of Your BusinessDari EverandOutsourcing Technology In the Healthcare Industry: In Depth Research to Protect the Security, Technology, and Profitability of Your BusinessBelum ada peringkat
- ONC Notice of Proposed Ruling Making Stage 2 Certification Rule Fact SheetDokumen3 halamanONC Notice of Proposed Ruling Making Stage 2 Certification Rule Fact SheetEmilioCruzFernandezBelum ada peringkat
- EHRA InteroperabilityRoadmap 20090310 v3Dokumen40 halamanEHRA InteroperabilityRoadmap 20090310 v3Anonymous JE7uJR100% (1)
- Comp9 Unit6c Audio TranscriptDokumen12 halamanComp9 Unit6c Audio TranscriptP D SpencerBelum ada peringkat
- Credentialing SpecialistDokumen11 halamanCredentialing SpecialistMichael Variacion100% (1)
- Midterm: Healthcare: Students Name Institutional Affiliation Midterm: Healthcare Instructors Name Due DateDokumen6 halamanMidterm: Healthcare: Students Name Institutional Affiliation Midterm: Healthcare Instructors Name Due DateG BushBelum ada peringkat
- Health Information TechnologyDokumen15 halamanHealth Information Technologybilly momanyiBelum ada peringkat
- Aspects of Quality Management PlanDokumen16 halamanAspects of Quality Management PlanJohnBelum ada peringkat
- Hit Research ProjectDokumen20 halamanHit Research ProjectDavid JuarezBelum ada peringkat
- Chapter 7 Ehr EmrDokumen8 halamanChapter 7 Ehr EmrIT OsparBelum ada peringkat
- Microsoft Massachusetts HIX-IES System Review 021314Dokumen22 halamanMicrosoft Massachusetts HIX-IES System Review 021314Shira SchoenbergBelum ada peringkat
- Constant Readiness Handout PDFDokumen21 halamanConstant Readiness Handout PDFMaria Francesca MapaBelum ada peringkat
- Articulo 1 Jamia UsabilidadDokumen7 halamanArticulo 1 Jamia UsabilidadTatianaBelum ada peringkat
- Electronic Health Record Management SystemDokumen13 halamanElectronic Health Record Management SystemMaisha AnzumBelum ada peringkat
- The Role of Information Technology in Pharmacy Practice Is Dynamic and Not Likely To Lose Relevance in The Coming Years (AutoRecovered)Dokumen6 halamanThe Role of Information Technology in Pharmacy Practice Is Dynamic and Not Likely To Lose Relevance in The Coming Years (AutoRecovered)masresha teferaBelum ada peringkat
- Henry Nnorom. Electronic Health Records (2021SU) Summer 2021Dokumen4 halamanHenry Nnorom. Electronic Health Records (2021SU) Summer 2021henry nnoromBelum ada peringkat
- HCD WP 2012 ValueBasedPurchasingWhatHospitalsAndHealthSystemsNeedDokumen8 halamanHCD WP 2012 ValueBasedPurchasingWhatHospitalsAndHealthSystemsNeedPatBickleyBelum ada peringkat
- Running Head: FINAL EXAMDokumen7 halamanRunning Head: FINAL EXAMapi-307874398Belum ada peringkat
- Information Technology Will Save Health Care: Institute of MedicineDokumen7 halamanInformation Technology Will Save Health Care: Institute of MedicineKelvin Kurt B. AgwilangBelum ada peringkat
- General Medicaid RulesDokumen4 halamanGeneral Medicaid RulesRam KumarBelum ada peringkat
- White Paper - Utilization Management Through The Lens of Value-Based CareDokumen7 halamanWhite Paper - Utilization Management Through The Lens of Value-Based CarevamseeBelum ada peringkat
- Corporate Compliance Programs Plans-2Dokumen7 halamanCorporate Compliance Programs Plans-2WilliamArugaBelum ada peringkat
- Predetermined Change Control Plans - Guiding PrinciplesDokumen2 halamanPredetermined Change Control Plans - Guiding PrinciplesBhanu Prasad SBelum ada peringkat
- Medicaid Medical Record DocumentationDokumen3 halamanMedicaid Medical Record DocumentationRam KumarBelum ada peringkat
- Contract Research Duties of Sponsor and CRODokumen3 halamanContract Research Duties of Sponsor and CROwisetry72100% (1)
- Chapter 01Dokumen5 halamanChapter 01Hassan IqbalBelum ada peringkat
- HCD WP 2012 HowaBusinessIntelligenceRoadmapSavesDokumen7 halamanHCD WP 2012 HowaBusinessIntelligenceRoadmapSavesPatBickleyBelum ada peringkat
- Quality Management ModelDokumen11 halamanQuality Management Modelselinasimpson1901Belum ada peringkat
- Hype Cycle For Healthcare ProviderDokumen36 halamanHype Cycle For Healthcare Providershenero1Belum ada peringkat
- Textbook of Urgent Care Management: Chapter 37, Setting Up a Health-Care Compliance ProgamDari EverandTextbook of Urgent Care Management: Chapter 37, Setting Up a Health-Care Compliance ProgamBelum ada peringkat
- The Best Handgun Caliber For Your Concealed Carry WeaponDokumen6 halamanThe Best Handgun Caliber For Your Concealed Carry Weapondnice408Belum ada peringkat
- HL7Dokumen2 halamanHL7dnice408Belum ada peringkat
- Workplace GeneralBrochure USA FGW5600 SECDokumen0 halamanWorkplace GeneralBrochure USA FGW5600 SECdnice408Belum ada peringkat
- 3 Svmhs Nurse ADokumen8 halaman3 Svmhs Nurse Adram408Belum ada peringkat
- Claro Qye SiDokumen1 halamanClaro Qye Sidnice408Belum ada peringkat
- Claro Qye SiDokumen1 halamanClaro Qye Sidnice408Belum ada peringkat
- SFSDFSDF SD SDF SDF S DF SD FDokumen1 halamanSFSDFSDF SD SDF SDF S DF SD Fdnice408Belum ada peringkat
- Approved Printer MatrixDokumen4 halamanApproved Printer Matrixdnice408Belum ada peringkat
- Meaningful Use - Medicaid PDFDokumen6 halamanMeaningful Use - Medicaid PDFdnice408Belum ada peringkat
- Meaningful Use Ophthalmology Workflow ChartDokumen1 halamanMeaningful Use Ophthalmology Workflow Chartdnice408Belum ada peringkat
- EHRIP Eligible Professionals Tip Sheet PDFDokumen4 halamanEHRIP Eligible Professionals Tip Sheet PDFdnice408Belum ada peringkat
- Incentive Payments For Meaningful Use' of Your Electronic Health RecordDokumen22 halamanIncentive Payments For Meaningful Use' of Your Electronic Health Recorddnice408Belum ada peringkat
- MedPAC June Report To CongressDokumen259 halamanMedPAC June Report To CongressFrances CorreaBelum ada peringkat
- Design Quality ImqiproveDokumen53 halamanDesign Quality Imqiprovednice408Belum ada peringkat
- Full Text 01Dokumen108 halamanFull Text 01dnice408Belum ada peringkat
- Loss Control TipsDokumen6 halamanLoss Control Tipsdnice408Belum ada peringkat
- QA Monograph For AhahDokumen90 halamanQA Monograph For Ahahdnice408Belum ada peringkat
- Full Text 01Dokumen108 halamanFull Text 01dnice408Belum ada peringkat
- Why Is This Document HereDokumen9 halamanWhy Is This Document Herednice408Belum ada peringkat
- Student Ppe Checklist 2012Dokumen5 halamanStudent Ppe Checklist 2012dnice408Belum ada peringkat
- Why Is This Document HereDokumen9 halamanWhy Is This Document Herednice408Belum ada peringkat
- 2012 Holiday ScheduleDokumen1 halaman2012 Holiday Schedulednice408Belum ada peringkat
- Inspirational QuotesDokumen44 halamanInspirational Quotesdnice408Belum ada peringkat
- Salary RangeDokumen25 halamanSalary Rangednice408Belum ada peringkat
- 2012 Holiday ScheduleDokumen1 halaman2012 Holiday Schedulednice408Belum ada peringkat
- Learn Square Roots & Plot on Number LineDokumen11 halamanLearn Square Roots & Plot on Number LineADAM CRISOLOGOBelum ada peringkat
- CCEE SWD Basic Levers ToolDokumen28 halamanCCEE SWD Basic Levers ToolDivina Margarita Gómez AlvarengaBelum ada peringkat
- No.6 Role-Of-Child-Health-NurseDokumen8 halamanNo.6 Role-Of-Child-Health-NursePawan BatthBelum ada peringkat
- The Wafer-God and the Bloody History of the VaticanDokumen58 halamanThe Wafer-God and the Bloody History of the VaticanMin Hotep Tzaddik BeyBelum ada peringkat
- 3.2 Probability DistributionDokumen38 halaman3.2 Probability Distributionyouservezeropurpose113Belum ada peringkat
- Legal Research MethodsDokumen10 halamanLegal Research MethodsCol Amit KumarBelum ada peringkat
- Denodo Job RoleDokumen2 halamanDenodo Job Role059 Monisha BaskarBelum ada peringkat
- Hotel and Restaurant at Blue Nile FallsDokumen26 halamanHotel and Restaurant at Blue Nile Fallsbig johnBelum ada peringkat
- Practical LPM-122Dokumen31 halamanPractical LPM-122anon_251667476Belum ada peringkat
- The Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsDokumen10 halamanThe Impact of Information Technology and Innovation To Improve Business Performance Through Marketing Capabilities in Online Businesses by Young GenerationsLanta KhairunisaBelum ada peringkat
- Mama Leone's Profitability AnalysisDokumen6 halamanMama Leone's Profitability AnalysisLuc TranBelum ada peringkat
- Basic Calculus: Performance TaskDokumen6 halamanBasic Calculus: Performance TasksammyBelum ada peringkat
- Grade 10 - Mock Test - English - Feb - 2023Dokumen12 halamanGrade 10 - Mock Test - English - Feb - 2023rohanBelum ada peringkat
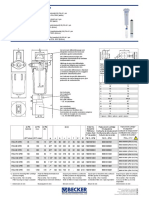
- Medical filter performance specificationsDokumen1 halamanMedical filter performance specificationsPT.Intidaya Dinamika SejatiBelum ada peringkat
- IT SyllabusDokumen3 halamanIT SyllabusNeilKumarBelum ada peringkat
- Linguistics: Chapter 1 - 10Dokumen41 halamanLinguistics: Chapter 1 - 10Ahmad A. JawadBelum ada peringkat
- Published Filer List 06072019 Sorted by CodeDokumen198 halamanPublished Filer List 06072019 Sorted by Codeherveduprince1Belum ada peringkat
- Sheqxel Bbs Participation Dashboard TemplateDokumen39 halamanSheqxel Bbs Participation Dashboard TemplateMuhammad Adytio DarmawanBelum ada peringkat
- ASD Manual and AISC LRFD Manual For Bolt Diameters Up To 6 Inches (150Dokumen1 halamanASD Manual and AISC LRFD Manual For Bolt Diameters Up To 6 Inches (150rabzihBelum ada peringkat
- Samsung 55 Inch LCD LED 8000 User ManualDokumen290 halamanSamsung 55 Inch LCD LED 8000 User ManuallakedipperBelum ada peringkat
- Donny UfoaksesDokumen27 halamanDonny UfoaksesKang Bowo D'wizardBelum ada peringkat
- Believer - Imagine Dragons - CIFRA CLUBDokumen9 halamanBeliever - Imagine Dragons - CIFRA CLUBSilvio Augusto Comercial 01Belum ada peringkat
- Research Paper On Organ DonationDokumen8 halamanResearch Paper On Organ Donationsheeliya whiteBelum ada peringkat
- IEC-60721-3-3-2019 (Enviromental Conditions)Dokumen12 halamanIEC-60721-3-3-2019 (Enviromental Conditions)Electrical DistributionBelum ada peringkat
- Compare and Contrast High School and College EssayDokumen6 halamanCompare and Contrast High School and College Essayafibkyielxfbab100% (1)
- Marijuana Grow Basics - Jorge CervantesDokumen389 halamanMarijuana Grow Basics - Jorge CervantesHugo Herrera100% (1)
- T23 Field Weld Guidelines Rev 01Dokumen4 halamanT23 Field Weld Guidelines Rev 01tek_surinderBelum ada peringkat
- Ne 01 20 09 2018Dokumen436 halamanNe 01 20 09 2018VaradrajBelum ada peringkat