Renal Function Tests
Diunggah oleh
Dr. Ashish JawarkarJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Renal Function Tests
Diunggah oleh
Dr. Ashish JawarkarHak Cipta:
Format Tersedia
1
Renal Function Tests
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
Notes on Clinical Pathology Renal function tests By Dr. Ashish Jawarkar Consultant Pathologist Vadodara
OVERVIEW 1. Indications 2. Classification a. Tests for glomerular function i. Clearance tests 1. Inulin clearance 2. creatinine clearance 3. cystatin c clearance 4. urea clearance ii. Blood biochemistry 1. BUN 2. Sr. Creatinine 3. BUN/Sr. Creatinine ratio 4. Urine proteins b. Tests for tubular function i. Tests for proximal tubular function 1. Glycosuria, aminoaciduria, LMW proteinuria 2. Urinary concentration of Na+ 3. Functional excretion of Na+ ii. Tests for distal tubular function 1. Specific gravity 2. Urine osmolality 3. Water deprivation test 4. Water loading ADH suppression test 5. Ammonium chloride loading test 3. Each test in detail
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
* Indications for RFT 1. To identify early renal impairment in patients at risk, such as i. Diabetes mellitus ii. Hypertension iii. SLE iv. UTI v. UT obstruction vi. Older age To diagnose certain renal disorders to asses response to treatment in renal disorders to adjust dosage of chemotherapeutic drugs To plan renal replacement therapy in advanced renal diseases
2. 3. 4. 5.
* Classification
Tests for glomerular function 1. For GFR clearance tests, indirect clearance 2. Blood biochemistry S. Creatinine, Bl Urea, BUN/S Creat ratio, Proteinuria (Albuminuria and microalbuminuria)
Tests for tubular function For Proximal Tubules For distal tubules i. Glycosuria, i. Specific gravity and Phosphaturia, osmolality Uricosuria, ii. water deprivation test aminoaciduria, LMW iii. water loading test Proteinuria iv. Ammonium chloride ii. Urinary excretion of test sodium iii. fractional sodium excretion
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
*Tests to measure GFR GLOMERULAR FILTERATION RATE: Definition: Rate at which a substance is cleared from the plasma in unit time by the glomeruli (in ml/min) Rationale: i. ii. iii. iv. v. vi. vii. Best for assessing excretory renal function Varies according to age/sex/body surface area (BSA) Also depends on renal blood flow and pressure Normal GFR = 120ml/min/1.73m2 GFR declines with age after 40 @1ml/min/year due to progressive glomerular arteriosclerosis Fall in GFR leads to accumulation of waste products GFR <15ml/min indicates uremia GFR <60ml/min/1.73m2 indicates >50% loss of renal function
Classification of chronic kidney diseases based on GFR: Stage Stage I Stage II Stage III Stage IV Stage V Disease Kidney disease with Kidney disease with Kidney disease with Kidney disease with Renal Failure GFR Normal GFR Mild decreased GFR Moderate dec GFR Severe dec GFR Value (ml/min/1.73m2) >90 60-89 30-59 15-29 <15
TESTS TO MEASURE GFR:
Direct assessment (Clearance Tests)
Indirect assessment from Sr. Creatinine
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
(i) CLEARANCE TESTS: Volume of plasma that is completely cleared of that substance per minute
C = UV/P
C = clearance (ml/min), U=Concentration of substance in urine (mg/dl), V=Volume of urine per min (ml/min), P=concentration of substance in plasma (mg/dl) Ideal agent for clearance studies: No ideal agent has been found, however the agent used should fulfill most of the following criteria: i. Should not bind to plasma proteins ii. should be freely filtered across glomeruli iii. should not be reabsorbed iv. should not be metabolized by kidney v. should be excreted only through the kidney Agents used: Exogenous i. ii. iii. iv. Inulin radiolabelled EDTA Radiolabelled 125I thiocynate 99 Tc-DTPA i. ii. iii. Endogenous Creatinine Urea Cystatin C
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
(A) Inulin Clearance test:
Rationale: 1. Gold Standard for measurement of GFR 2. Neither secreted nor absorbed and is completely filtered by glomeruli Method: 1. Bolus dose is administered followed by constant i.v. infusion for maintaining constant plasma levels 2. Timed urine samples are collected and blood samples are obtained at mid points of urine collection Disadvantage: Rarely used in practice because 1. Time consuming 2. Expensive 3. Need to maintain steady plasma levels
Normal Values: Inulin clearance
Males : 125 ml/min/1.73 m2 Females: 110 ml/min/1.73 m2
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
(B) Creatinine Clearance Test
Rationale: 1. Most commonly used for measuring GFR 2. Produced constantly from creatine in muscles 3. completely filtered by glomeruli, not reabsorbed, but is secreted in a small amount there is overestimation of GFR by 10% 4. Can help in finding out the number of nephrons damaged by disease process Method: 1. 24 hour urine sample is preferred 2. First voided sample is discarded 3. Subsequently all urine passed is collected in containers 4. Next morning voided sample is collected and all containers are sent to laboratory 5. A blood sample is obtained at midpoint of urine collection 6. Cimetidine which blocks renal secretionocan be used to prevent overestimation 7. Final calculation is by the formula UV/P, with adjustment of 10% for secretion
As we can see from the graph, as the creatinine clearance decreases, the remaining nephrons in the kidney decrease Also the dotted line shows that the serum creatinine begins to rise only after 50% of the nephrons are damaged, i.e. serum creatinine though useful is a less sensitive indicator of renal function.
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
Disadvantages: 1. small amounts of creatinine secreted by renal tubules can increase even further in advanced renal failure 2. Creatinine level is affected by intake of meat and muscle mass 3. collection of urine is incomplete often 4. Creatinine levels are affected by drugs such as cimetidine, probenecid and trimethoprim that block tubular secretion
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
(C) Cystatin C clearance test
Rationale: 1. It is a protease produced by all nucleated cells of the body at a constant rate 2. It is not bound to proteins, freely filtered by glomeruli and not absorbed Advantages over Creatinine: 1. More sensitive and specific 2. Not affected by sex/diet/muscle mass
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
10
(D) Urea clearance test
Rationale: 1. Urea is freely filtered by the glomeruli but about 40% is reabsorbed 2. Thus it underestimates GFR and is not a sensitive marker
Importance of clearance tests:
As we saw in creatinine clearance graph, BUN and Sr. creatinine are not sensitive indicators of early renal impairment For serum creatinine to rise from 0.5mg/dl (normal) to 1.0 mg/dl, nearly 50% of the renal mass should have been damaged
Clearance tests are more helpful in this scenario of detection of early renal impairment
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
11
(II) Indirect estimation of clearance from serum creatinine value
Creatinine clearance
(140 age in years) x Body weight in kg ( 72 x serum creatinine in mg/dl)
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
12
*Blood Biochemisty
(a) Blood Urea Nitrogen (BUN)
Earlier methods measured only nitrogen content of blood urea. 28 gms nitrogen is present in a gram mole of urea and molecular weight of urea is 60 . So urea: nitrogen = 60:28. ie BUN can be converted to urea by multiplying by 2.14 Newer methods directly measure blood urea. Production of Urea: Proteins
Amino acids
Synthesis of tissue proteins
Energy
Ammonia
Urea Cycle
Urea
Excretion in urine Rationale: 1. Completely filtered by glomeruli and 30-40 % is reabsorbed 2. State of hydration affects estimation 3. Affected by non renal factors such as - high protein diet - upper g.i. hemorrhage 4. Less sensitive considerable destruction of renal parenchyma has to occur before urea is elevated
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
13
Methods: 1. Direct method (Di acetyl monoxamine method) Urea + DAM High temp, strong acid, oxidizing agent Yellow diazine derivative
Intesity of color is measured
2. Indirect method (Urease Bertholet reaction) 37 C Urea Urease Ammonia Phenol Alkaline hypochlorite Iodophenol
Intensity of color is measured
Normal levels: Normal Adults 7-18 mg/dl Adults > 60 years 8-21 mg/dl
Causes of increased BUN: Azotemia increase in level of BUN/urea Uremia clinical syndrome resulting from azotemia Pre renal shock CHF dehydration high protein diet, trauma, burns, g.i. hemorrhage Renal Impairment of renal function Post renal Obstruction of urinary tract
1. 2. 3. 4.
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
14
(b) Serum Creatinine
Production of Creatinine: Creatinine is a nitrogenous waste product formed in muscle from creatine phosphate. Rationale: 1. Creatinine is produced from muscles at a constant rate 2. Production is proportional to muscle mass and body weight 3. Its not reabsorbed, secreted in a small amount 4. It is not sensitive (see graph)
The dotted line shows that the serum creatinine begins to rise only after 50% of the nephrons are damaged, i.e. serum creatinine though useful is a less sensitive indicator of renal function.
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
15
Methods: 1. Jaffes method Creatinine + Picric acid Alkaline reagent Colored product
Spectrophotometer Picric acid also reacts with glucose, protein and fructose, hence actual level is 0.2 to 0.4 mg /dl lower 2. Enzymetic method
Creatinine enzymes
H2O2 + phenol + dye
Colored product
spectrophotometer Normal Range: Serum Creatinine
Males 0.7 to 1.3 mg/dl Females 0.6 to 1.1 mg/dl
Causes of: Increased serum creatinine 1. Azotemia 2. dietary meat 3. Acromegaly, gigantism Decreased serum creatinine 1. Pregnancy (hemodilution) 2. Old age (decreased muscle mass)
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
16
(c) BUN/Serum creatinine ratio
Normal: BUN:Sr. Creatinine Causes of 12:1 to 20:1
Ratio >20:1 INCREASED BUN WITH NORMAL CREATININE 1. 2. 3. 4. High protein diet Increased protein catabolism G.I. Hemorrhage Dehydration decreased renal perfusion (Pre renal azotemia)
Ratio <12:1 INCREASED CREATININE WITH NORMAL BUN 1. Starvation 2. Low protein diet 3. severe liver disease In these three conditions, there is increased creatine breakdown in muscles to synthesize proteins increased creatinine BUN is normal
In these conditions there is increased protein break down increased BUN Muscle creatine is not broken down hence no increase in serum creatinine INCREASED BUN AND INCREASED CREATININE BUT INCREASE IN BUN IS MORE 1. Post renal azotemia (obstruction) In this condition there is obstruction to urine flow which pushes urea back into circulation - increase in BUN is more than that of creatinine
INCREASED BUN AND CREATININE BUT INCREASE IN CREATININE IS MORE 1. Acute tubular necrosis
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
17
(iv) Proteinuria
Rationale: 1. Normally a very small amount of albumin is excreted in urine. 2. Earlest evidence of glomerumlar damage in diabetes mellitus is occurrence of microalbuminuria (albuminuria in range of 30 to 300 mg/24 hrs) 3. Albuminuria >300mg/24 hour is termed clinical or overt proteinuria and indicates significant glomerular damage. For details see notes on urine analysis Protein in urine
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
18
*Tests to assess proximal tubular function:
(i) Glycosuria, aminoaciduria, LMW proteinuria
Rationale: 1. Proximal tubules reabsorb 99% of glomerular filterate. 2. Substances such as glucose, aminoacids and LMW proteins are reabsorbed by PCT. 3. Hence measurine these substances in urine gives us an idea about the function of PCT, if PCT are non functioning (or these substances are in excess) they will appear in urine. 1. Glycosuria i. ii. in renal glycosuria, glucose is excreted in urine when blood levels are normal due to lesion in tubules Glycosuria can also occur in Fanconi syndrome
2. Generalised aminoaciduria i. many aminoacids are excreted in urine due to proximal tubular dysfunction 3. Tubular proteinuria (Low molecular weight proteinuria) i. substances such as beta 2 microglobulin, retinol binding protein, lysozyme and alpha 1 microglobulin are completely reabsorbed by tubules ii. Detected by urine protein electrophoresis.
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
19
(ii) Urinary concentration of sodium:
Rationale: 1. Used to differentiate between pre renal azotemia and acute tubular necrosis 2. In pre renal azotemia, tubular function is preserved, i.e. reabsorption of sodium is preserved 3. In acute tubular necrosis, tubular function is not preserved, ie. Sodium is not reabsorbed. Values: 1. Pre renal azotemia: Urinary Na+ < 20 mEq/L 2. Acute tubular necrosis: Urinary Na+ > 20 mEq/L
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
20
(iii) Functional excretion of Na (FNa )
Rationale: Measurement of urinary sodium is affected by urine volume (mEq/L)
Hence to avoid this we can measure the exact quantity of Na+ reabsorbed as a fraction of amount of Na+ filtered to amount excreted
As with above test, this test is used to differentiate between pre and renal azotemia Method: F Na+ = Urine Na+ Plasma Na+ x x Plasma Creatinine Urine Creatinine x 100
Values: 1. Pre renal azotemia - <1% 2. ATN - >3%
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
21
*Tests that assess distal tubular function
(i) Specific Gravity
Rationale: 1. It is the ratio of density of substance to density of fresh water at 4C (39F) 2. At this temperature density of water is greatest and equals 1gm/dl 3. It means that a substance with specific gravity >1(@4C) will sink and <1(@4C) will float. Factors affecting specific gravity: 1. State of hydration 2. Tubule concentrating ability 3. Number and nature of dissolved particles HMW solutes like proteins and glucose affect specific gravity Methods: See notes on urine examination Causes: Increased specific gravity 1. Proteinuria 2. Glycosuria (diabetes mellitus) 3. Nephrotic syndrome 4. urinary tract obstruction with preserved concentrating ability 5. decreased renal perfusion with preserved concentrating ability Normal Value: Specific gravity 1.003 to 1.030 Decreased specific gravity 1. Diabetes insipedus 2. CRF with decreased concentrating ability 3. increased water intake Fixed specific gravity (@1.010) Chronic renal failure
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
22
(ii) Urine Osmolality
Rationale: 1. Osmolality measures the number of dissolved particles in a solution. 2. It is most sensitive and most commonly employed method to find out urinary concentrating ability Method: When solute dissolves in a solvent it leads to 1. Lowering of freezing point 2. increase in boiling point 3. decrease in vapour pressure 4. increase in oncotic pressure
These properties are used while measuring osmolality by a osmometer
Method:
0.1 M sucrose
Final level indicates osmolality
Semipermeable Membrane
as water enters The tube, its level rises
Water
Simple osmometer
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
23
Factors affecting osmolality: 1. depends only on number of dissolved particles 2. it doesnot depend on nature or molecular weight of dissolved particles like specific gravity does Normal: Urine osmolality (24 hour)
500 - 800 mOsm/kg of water With restricted fluid intake - >800 mOsm/kg of water
Application: (Urine : plasma osmolality ratio is calculated, used to differentiate pre renal and renal azotemia) Decreased urine:plasma osmolality ratio (either urine osmolality is decreased or plasma osmolality is increased) Seen in Acute tubular necrosis (decreased concentrating ability) Increased urine:plasma osmolality ratio (either urine osmolality is increased or plasma osmolality is decreased) Pre renal azotemia preserved concentrating ability
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
24
(iii) Water deprivation test for urine osmolality and specific gravity
Rationale: Measures concentrating ability of kidney with fluid restriction Method: Measurement of urine osmolality and specific gravity
Restriction of water intake for a specified period of time
Measurement of urine osmolality and specific gravity and comparison with earlier values
Rise in specific gravity and urine osmolality (>800 mOsm/kg of water, >1.025)
No rise in specific gravity and osmolality
Urinary concentrating ability maintained Or false positive result*
Administer desmopressin
Rise in sp. Gravity
No rise
Central DI (diabetes insipedus)
Nephrogenic DI
* false positive result is obtained in case of low salt, low protein diet or major electrolyte disturbances
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
25
(iv) Water loading ADH suppression test
Rationale: Measures ability of kidney to dilute urine after water loading Method: Over night fast
Drink 20 ml/kg of water in 15-20 min
Collect urine at hourly interval for next 4 hours
1. 2. 3. 4.
Measure Specific gravity urine volume osmolality (serum and urine) plasma levels of ADH
Scenario 1 1. >90% of fluid load excreted in 4 hours 2. specific gravity <1.003 after 4 hours 3. Urine osmolality <100 mOsm/kg after 4 hrs 4. ADH level decreased with decreased osmolality
Scenario 2 1. <80% excreted 2. >1.003 3. >100 mOsm/kg 4. ADH fails to decrease
Normal diluting ability of kidney
Renal function impairment OR False negative*
* False negative seen in 1. dehydration 2. cirrhosis 3. Malabsorption 4. adrenocortical insufficiency 5. congestive heart failure
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
26
(v) Ammonium chloride loading test
Rationale: After all the causes of metabolic acidosis have been ruled out
Renal tubular acidosis is the most likely diagnosis This test is done to confirm or rule out renal tubular acidosis
After overnight fast, urine pH should be <5.4
If results are inconclusive , we administer ammonium chloride which increases urinary pH and remeasure
Method: Measure baseline urinary pH and plasma HCO3- levels
Overnight fast and collect urine for next 6-8 hours
Scenario 1 1. Urine pH <5.4 2. plasma HCO3- Normal /high
Scenario 2 1. Urine pH > 5.4 2. Plasma HCO3- low
Scenario 3 Inconclusive results
Normal renal Acidifying ability
Type I renal tubular acidosis
Give NH4Cl orally
Collect urine samples Over next 6-8 hrs
If pH <5.4, acidifying Ability maintained
Notes on renal function tests By Dr. Ashish Jawarkar Contact: pathologybasics@gmail.com Website: pathologybasics.wix.com/notes
Anda mungkin juga menyukai
- Renal Function TestsDokumen28 halamanRenal Function TestsAbeer Ahmed100% (1)
- NPNDokumen46 halamanNPNGerald John PazBelum ada peringkat
- Urinalysis and Body Fluids for Cls & MltDari EverandUrinalysis and Body Fluids for Cls & MltBelum ada peringkat
- Hematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesDari EverandHematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesPenilaian: 5 dari 5 bintang5/5 (2)
- Hepatorenal Syndrome: Causes, Tests, and Treatment OptionsDari EverandHepatorenal Syndrome: Causes, Tests, and Treatment OptionsPenilaian: 4.5 dari 5 bintang4.5/5 (2)
- Renal PhysiologyDokumen54 halamanRenal Physiologyfrabzi100% (5)
- Plasma ProteinDokumen46 halamanPlasma ProteinM.PRASAD NAIDUBelum ada peringkat
- Plasma Proteins Lecture: Functions and AlterationsDokumen12 halamanPlasma Proteins Lecture: Functions and AlterationsAmine Gobran100% (2)
- Acid Base BalanceDokumen35 halamanAcid Base BalanceDhanasvi Dessai100% (1)
- DLC PracticalDokumen6 halamanDLC PracticalAngoruz Gohain BaruahBelum ada peringkat
- Carbohydrate Metabolism: By:-Dr - Priyanka Sharma 1 Year MDS Dept. of Public Health DentistryDokumen93 halamanCarbohydrate Metabolism: By:-Dr - Priyanka Sharma 1 Year MDS Dept. of Public Health DentistrySimham Venu0% (1)
- Liver Function TestDokumen50 halamanLiver Function TestJhannBelum ada peringkat
- Blood and Body FluidsDokumen24 halamanBlood and Body FluidsQasim NaeemBelum ada peringkat
- Kidney Function TestDokumen21 halamanKidney Function TestVinoantonyBelum ada peringkat
- Respiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandRespiratory Alkalosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Lab 9++10 Pathological UrinlysisDokumen38 halamanLab 9++10 Pathological UrinlysisSai SreedharBelum ada peringkat
- EnzymesDokumen229 halamanEnzymesJimwell AxalanBelum ada peringkat
- Acid Base ImbalanceDokumen50 halamanAcid Base ImbalanceDian Pratiwi BurnamaBelum ada peringkat
- 1 Body FluidsDokumen9 halaman1 Body FluidsSenthereng MoaisiBelum ada peringkat
- Enzymes Patterns in Different DiseasesDokumen47 halamanEnzymes Patterns in Different DiseasesMustafa KhandgawiBelum ada peringkat
- Clinical Lab TechnqDokumen67 halamanClinical Lab TechnqRatnamala SarmaBelum ada peringkat
- Q. List Different Functions of The Kidney: (A) Homeostatic FunctionDokumen42 halamanQ. List Different Functions of The Kidney: (A) Homeostatic Functionramadan100% (4)
- LDHDokumen32 halamanLDHBrijesh Mukherjee100% (2)
- Renal DisordersDokumen77 halamanRenal Disorderslorelee_espaldon100% (1)
- Lecture Notes Analytical Biochemistry: Chapter - 1 Spectrophotometry and ColorimetryDokumen35 halamanLecture Notes Analytical Biochemistry: Chapter - 1 Spectrophotometry and ColorimetryHarpreet Singh100% (3)
- Physiology of DiabetesDokumen52 halamanPhysiology of DiabetesPhysiology by Dr RaghuveerBelum ada peringkat
- Fluid Resuscitation and Organ Perfusion EvaluationDokumen66 halamanFluid Resuscitation and Organ Perfusion EvaluationDewiRatnasariBelum ada peringkat
- Diabetic Emergencies Case StudiesDokumen32 halamanDiabetic Emergencies Case StudiesLamria Maloni Siahaan0% (1)
- Sickle Cell Disease: A Case Study of a 16-Month-Old Baby GirlDokumen52 halamanSickle Cell Disease: A Case Study of a 16-Month-Old Baby GirlhudaBelum ada peringkat
- KROK 1 EXPLANATIONS MicrobiologyDokumen18 halamanKROK 1 EXPLANATIONS MicrobiologyAkpene Racheal100% (1)
- LipidsDokumen13 halamanLipidsalianaBelum ada peringkat
- Lecture 1 Cell Injury Adpation and DeathDokumen39 halamanLecture 1 Cell Injury Adpation and Deathyat yat szeBelum ada peringkat
- Cardiac MarkersDokumen23 halamanCardiac MarkersAsmaaYLBelum ada peringkat
- Urine Screening of Metabolic DisordersDokumen24 halamanUrine Screening of Metabolic DisordersMark Arlo Hernandez SegundoBelum ada peringkat
- Metab DisordersDokumen36 halamanMetab DisordersDaena TimtimanBelum ada peringkat
- Physiology Cardiovascular Physiology NotesDokumen13 halamanPhysiology Cardiovascular Physiology Noteshedayatamin44Belum ada peringkat
- Microscopic ExaminationDokumen72 halamanMicroscopic ExaminationbubblyeivinejBelum ada peringkat
- Haematology Case Studies with Blood Cell Morphology and PathophysiologyDari EverandHaematology Case Studies with Blood Cell Morphology and PathophysiologyPenilaian: 5 dari 5 bintang5/5 (4)
- Study of Living Organism Chemistry (BiochemistryDokumen72 halamanStudy of Living Organism Chemistry (BiochemistryNatasha Jean100% (1)
- Titration of Amino AcidsDokumen40 halamanTitration of Amino AcidsBryan Janier100% (1)
- Kidney Function Test-1Dokumen11 halamanKidney Function Test-1jahansha kurramBelum ada peringkat
- Ni Nyoman Ayu Dewi Dept. of Biochemistry, Faculty of Medicine Udayana University Ayu - Dewi@unud - Ac.idDokumen37 halamanNi Nyoman Ayu Dewi Dept. of Biochemistry, Faculty of Medicine Udayana University Ayu - Dewi@unud - Ac.idWida Utami100% (1)
- Senior Medical Laboratory Technician: Passbooks Study GuideDari EverandSenior Medical Laboratory Technician: Passbooks Study GuideBelum ada peringkat
- Bioc416 PDFDokumen53 halamanBioc416 PDFrJ100% (2)
- Digestion & Absorption of CarbohydratesDokumen14 halamanDigestion & Absorption of CarbohydratesKuzhandai VeluBelum ada peringkat
- Clinical Biochemistry PDFDokumen105 halamanClinical Biochemistry PDFJepri Purwanto67% (3)
- Avi's Notes Clinical BiochemistryDokumen171 halamanAvi's Notes Clinical BiochemistryErfaneh FN100% (1)
- Packed Cell Volume (PCV) TestDokumen3 halamanPacked Cell Volume (PCV) TestchineduBelum ada peringkat
- Introduction To HematologyDokumen23 halamanIntroduction To HematologyReba PhiliposeBelum ada peringkat
- Biochemistry One LinersDokumen11 halamanBiochemistry One Linerssandeep MahapatraBelum ada peringkat
- Urine Formation: Reabsorption and Secretion, and Water ConservationDokumen5 halamanUrine Formation: Reabsorption and Secretion, and Water ConservationAshraf Moby100% (1)
- Introduction To HematologyDokumen95 halamanIntroduction To HematologyAhmad Farhan Hassan0% (1)
- 1 Introduction and Cell AdaptationDokumen142 halaman1 Introduction and Cell AdaptationyuyanwongBelum ada peringkat
- ABO Blood Group System PDFDokumen112 halamanABO Blood Group System PDFFaye Millado100% (2)
- Clinical Pathology ReviewDokumen11 halamanClinical Pathology Reviewrob hBelum ada peringkat
- Pre-Exam Preparation and Specimen Collection GuideDokumen62 halamanPre-Exam Preparation and Specimen Collection GuideDianne JoyBelum ada peringkat
- Biochemistry of Cardiovascular SystemDokumen113 halamanBiochemistry of Cardiovascular SystemNindy75% (4)
- Acid Base Handout RevisedDokumen3 halamanAcid Base Handout RevisedKaren HutchinsonBelum ada peringkat
- Abnormal UrineDokumen28 halamanAbnormal UrinemujeebBelum ada peringkat
- Robbins Chapter 1 Cell As A Unit of Health and DiseaseDokumen46 halamanRobbins Chapter 1 Cell As A Unit of Health and DiseaseDr. Ashish Jawarkar0% (1)
- External Examination at AutopsyDokumen87 halamanExternal Examination at AutopsyDr. Ashish JawarkarBelum ada peringkat
- Anti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDokumen41 halamanAnti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarBelum ada peringkat
- Systemic Microbiology: BacteriologyDokumen42 halamanSystemic Microbiology: BacteriologyDr. Ashish JawarkarBelum ada peringkat
- AmyloidosisDokumen26 halamanAmyloidosisDr. Ashish JawarkarBelum ada peringkat
- Semen Analysis (WHO 2010)Dokumen14 halamanSemen Analysis (WHO 2010)Dr. Ashish Jawarkar100% (1)
- Control of Aerosol Transmitted DiseasesDokumen45 halamanControl of Aerosol Transmitted DiseasesDr. Ashish JawarkarBelum ada peringkat
- MycobacteriaDokumen62 halamanMycobacteriaDr. Ashish JawarkarBelum ada peringkat
- StreptococciDokumen91 halamanStreptococciDr. Ashish JawarkarBelum ada peringkat
- Control of Microbial Growth: Dr. Ashish Jawarkar Pathologist Parul Sevashram HospitalDokumen38 halamanControl of Microbial Growth: Dr. Ashish Jawarkar Pathologist Parul Sevashram HospitalDr. Ashish JawarkarBelum ada peringkat
- Needle Sticks Sharps Injuries: FactsDokumen31 halamanNeedle Sticks Sharps Injuries: FactsDr. Ashish Jawarkar67% (3)
- Blood and Its ComponentsDokumen72 halamanBlood and Its ComponentsDr. Ashish JawarkarBelum ada peringkat
- Biomedical Waste ManagementDokumen57 halamanBiomedical Waste ManagementDr. Ashish JawarkarBelum ada peringkat
- Sickle Cell AnemiaDokumen13 halamanSickle Cell AnemiaDr. Ashish JawarkarBelum ada peringkat
- Laboratory Approach To Bleeding DisordersDokumen33 halamanLaboratory Approach To Bleeding DisordersDr. Ashish JawarkarBelum ada peringkat
- Sputum ExaminationDokumen9 halamanSputum ExaminationDr. Ashish JawarkarBelum ada peringkat
- Laboratory Approach To AnemiasDokumen23 halamanLaboratory Approach To AnemiasDr. Ashish JawarkarBelum ada peringkat
- Nosocomial InfectionDokumen31 halamanNosocomial InfectionDr. Ashish Jawarkar0% (1)
- Thyroid Function TestsDokumen21 halamanThyroid Function TestsDr. Ashish JawarkarBelum ada peringkat
- Infections and ImmunityDokumen35 halamanInfections and ImmunityDr. Ashish JawarkarBelum ada peringkat
- Microbiology Quiz 2Dokumen52 halamanMicrobiology Quiz 2Dr. Ashish JawarkarBelum ada peringkat
- Liver Function TestsDokumen28 halamanLiver Function TestsDr. Ashish Jawarkar100% (2)
- Microscopy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDokumen21 halamanMicroscopy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarBelum ada peringkat
- Pregnancy TestsDokumen9 halamanPregnancy TestsDr. Ashish JawarkarBelum ada peringkat
- Microbiology Quiz 1Dokumen47 halamanMicrobiology Quiz 1Dr. Ashish JawarkarBelum ada peringkat
- Bacteria: Morphology and ClassificationDokumen44 halamanBacteria: Morphology and ClassificationDr. Ashish JawarkarBelum ada peringkat
- Sterilization and DisinfectionDokumen68 halamanSterilization and DisinfectionDr. Ashish Jawarkar100% (1)
- Basics of Microscopy and StainingDokumen29 halamanBasics of Microscopy and StainingDr. Ashish JawarkarBelum ada peringkat
- Culture Methods and Culture MediaDokumen48 halamanCulture Methods and Culture MediaDr. Ashish JawarkarBelum ada peringkat
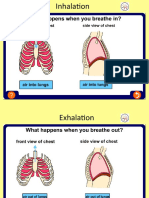
- Asthma Inhale and ExhaleDokumen14 halamanAsthma Inhale and ExhaleNguyen Nhu VinhBelum ada peringkat
- Chronology of Human Dentition & Tooth Numbering SystemDokumen54 halamanChronology of Human Dentition & Tooth Numbering Systemdr parveen bathla100% (4)
- Listening d1Dokumen4 halamanListening d1Ebin PauloseBelum ada peringkat
- 1 SMDokumen6 halaman1 SMmaryano 0015Belum ada peringkat
- Shaukat Khanum Memorial Cancer Hospital & Research CentreDokumen2 halamanShaukat Khanum Memorial Cancer Hospital & Research CentreUsama AjmalBelum ada peringkat
- Adverse Reaction Blood BankDokumen10 halamanAdverse Reaction Blood BankyourfamilydoctorBelum ada peringkat
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDokumen1 halamanCertificate For COVID-19 Vaccination: Beneficiary DetailsAshok KumarBelum ada peringkat
- Nursing Care PlanDokumen2 halamanNursing Care PlanJewelyn Bronda100% (2)
- Risk Prediction Model for Heart Failure in DiabetesDokumen20 halamanRisk Prediction Model for Heart Failure in DiabetesjamesboendBelum ada peringkat
- MBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dokumen1 halamanMBBS - General Medicine Reg Id: KMC - 142105 RX ID: 406824261Dipam HalderBelum ada peringkat
- Wild Foods For Wise Women by Susun WeedDokumen6 halamanWild Foods For Wise Women by Susun Weedclaricecaps100% (1)
- ABpsych NewpppDokumen15 halamanABpsych NewpppMarbie Aliyah B. PagadorBelum ada peringkat
- BuratDokumen5 halamanBuratFreya AvellanoBelum ada peringkat
- !the H Book For 5th Year OSCE - Part 1Dokumen147 halaman!the H Book For 5th Year OSCE - Part 1farzzana100% (1)
- Career Map - DoctorDokumen7 halamanCareer Map - DoctorAdityaBelum ada peringkat
- Ozone - A Wide Spectrum Healer by Gary Null PHDDokumen20 halamanOzone - A Wide Spectrum Healer by Gary Null PHDangelakimba100% (4)
- Demodex CanisDokumen19 halamanDemodex Canisapi-337841627Belum ada peringkat
- ODC Nursing FormsDokumen5 halamanODC Nursing Formsgyds_17Belum ada peringkat
- 2a. Atspph ScaleDokumen2 halaman2a. Atspph Scaleyani0707Belum ada peringkat
- Dialysis Inspection Tool 2014Dokumen11 halamanDialysis Inspection Tool 2014Maek100% (1)
- Overweight, Hypertension and Heart Disease ClassificationsDokumen4 halamanOverweight, Hypertension and Heart Disease Classificationsjagadish chandra prasadBelum ada peringkat
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisDokumen6 halamanSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedBelum ada peringkat
- How Food Handlers Can Spread IllnessDokumen2 halamanHow Food Handlers Can Spread IllnessSavitri Maharani BudimanBelum ada peringkat
- Vital Signs ChecklistDokumen21 halamanVital Signs ChecklistJapsay Francisco GranadaBelum ada peringkat
- Nicola Zammitt, - Alastair O'Brien - Essentials of Kumar & Clark's Clinical Medicine-Elsevier (2017) PDFDokumen927 halamanNicola Zammitt, - Alastair O'Brien - Essentials of Kumar & Clark's Clinical Medicine-Elsevier (2017) PDFJamie Baczewski100% (8)
- Biosure RGDokumen2 halamanBiosure RGJuan Martinez Del AngelBelum ada peringkat
- Greater Political ParticipationDokumen12 halamanGreater Political ParticipationBe-COOL State Of MindBelum ada peringkat
- FNDRC Vol 2 AppendicesDokumen43 halamanFNDRC Vol 2 AppendicesJohn Michael Macabenta100% (1)
- MOH, DHA and HAAD recalls from 2017 WhatsApp groupDokumen32 halamanMOH, DHA and HAAD recalls from 2017 WhatsApp groupshahzadBelum ada peringkat
- Skills Math WorksheetDokumen4 halamanSkills Math WorksheetBrennan MaguireBelum ada peringkat