Plastic Surgery: Understanding Abdominoplasty and Liposuction
Diunggah oleh
doctorbanDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Plastic Surgery: Understanding Abdominoplasty and Liposuction
Diunggah oleh
doctorbanHak Cipta:
Format Tersedia
Plastic Surgery: Understanding Abdominoplasty and Liposuction 3.
0
JUDITH M. LOGAN, RN, BSN, CNOR, MBA, MAJ, ANC, USA; GEORGE BROUGHTON II, MD, PHD, COL, MC, USA
lastic surgery is becoming increasingly popular as women and men decide to modify their bodies to positively affect their body image. According to a 2005 statistical study by the American Society for Aesthetic Plastic Surgery (ASAPS), nearly 11.5 million surgical and nonsurgical cosmetic procedures were performed in the United States.1 Forty-eight percent of these procedures were performed in office-type facilities, 28% were performed in free-standing surgical centers, and only 24% were performed in hospitals.1 Abdominoplasty and liposuction were the two most popular invasive plastic surgery procedures performed in 2004.1 People decide to have these procedures for a variety of reasons: for body contouring after a significant weight loss from dieting or gastric bypass surgery, to improve their shape after childbirth, or to enhance or modify different areas of their bodies. The demand for increased privacy, convenience, and efficiency has precipitated an upsurge of outpatient procedures, from 10% of all surgical procedures in 1979 to 80% in 2006.1 To ensure patient safety, outpatient facilities performing plastic surgery should be accredited by the American Association of Ambulatory Surgery Facilities, the
Accreditation Association for Ambulatory Health Care, the Joint Commission, or a state-recognized entity such as the Institute for Medical Quality, or they should be Medicare certified under Title XVIII.1 Byrd et al2 showed that outpatient plastic surgery can be safe. In their case review of 5,316 consecutive procedures, they found a complication rate of less than 1%.2 According to Keyes et al,3 outpatient complication rates range between 0.33% to 0.7%, and the occurrence of death is approximately 0.002%. Many, if not most, of the office-based plastic surgery injuries arise from physicians practicing outside their medical training.4 Recognizing safety as a top priority, the American Society of Plastic Surgeons (ASPS) Board of Directors convened the Task Force on Patient
ABSTRACT
REQUESTS FOR PLASTIC SURGERY procedures that alter ones body image are on the rise. To ensure the best possible outcome, patients who request a combined procedure (eg, abdominoplasty and liposuction) must meet certain criteria to be eligible for surgery. It is critically important for patients to understand that these surgeries are not weightreduction procedures, and they must be prepared to make lifestyle changes to ensure long-lasting results. THESE PROCEDURES are performed in a variety of facilities (eg, surgeons offices, surgery centers, hospitals). PERIOPERATIVE NURSES must have a basic knowledge and understanding of abdominoplasty and liposuction and the special requirements and potential complications involved with these procedures. AORN J 88 (October 2008) 587-600. AORN, Inc, 2008.
indicates that continuing education contact hours are available for this activity. Earn the contact hours by reading this article and taking the examination on pages 601602 and then completing the answer sheet and learner evaluation on pages 603604. You also may access this article online at http://www.aornjournal.org.
AORN, Inc, 2008
OCTOBER 2008, VOL 88, NO 4 AORN JOURNAL 587
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
Many multiparous women complain of an abdominal bulge that just wont go away with diet and exercise. This postpartum bulge is from poor abdominal muscle tone caused by the failure of the body to repair the separation of the right and left rectus abdominis muscle after pregnancy.
Safety in Office-based Surgery Facilities in 2002.5-7 The task force has published statements and advisories to help assist physicians in clinical decision-making,5 emphasizing patient safety as the foremost concern in the practice of plastic surgery.
ABDOMINOPLASTY
The first known report of an abdominal dermolipectomy was made in 1890 by Demars and Marx.8 Nine years later at the Johns Hopkins Hospital in Baltimore, Maryland, Kelly reported a transverse abdominal lipectomy.8 Making a transverse incision, he resected a panniculus weighing 7,450 g and measuring 90 cm by 31 cm by 7 cm. Kelly proposed performing the surgery for cosmetic reasons in 1910.8 In 1916, Babcock advocated wide undermining of abdominal wall skin and even corrected abdominal wall laxity with a buried silver chain.8 It was not until 1939 that Thorek first described a procedure called plastic adipectomy that preserved the umbilicus.8 In 1967, the first description for plicating (ie, folding and tightening) the rectus abdominis fascia was made.9 That same year, Pitanguy10 published his landmark paper outlining the modern principles of abdominoplasty: inconspicuous lower abdominal scar;
ample subcutaneous undermining extending to the costal margins; transverse umbilicalplasty; muscular aponeurotic reinforcement (ie, plication); and compressive postoperative dressings. Many different incision shapes and locations have been described, but it was not until 1973 that the so-called bikini line incision was described by Grazer.11 The location and shape of the abdominoplasty incision has been influenced by fashion. When the Saint-Tropez bikini with a very low waistline became fashionable, the abdominoplasty incision was almost horizontal so it could remain hidden, but when the French-line bikini with a very high leg cut became popular, the incision was changed to curve laterally to follow along the inguinal crease.9 With the popularity of liposuction, Matarasso developed a classification of abdominal contour surgery based on the patients anatomy using a spectrum of treatments from liposuction alone to combinations of liposuction and abdominoplasty.9 There are several variations of the abdominoplasty procedurecommonly called a tummy tuckdepending on the clinical situation. Table 1 lists different procedures commonly confused with an abdominoplasty and highlights the differences. A working definition for abdominoplasty is the excision of excess and lax abdominal wall skin and adipose tissue, usually the skin between 2 cm above the pubic symphysis to just above the umbilicus; plication of the rectus abdominis fascia; and creation of new umbilicus (ie, neoumbilicus). The surgeon does not actually create a new umbilicus; rather, the existing belly button is brought up through a new hole created in the skin that has been pulled down over it. Many multiparous women complain of an abdominal bulge that just wont go away with diet and exercise. This postpartum bulge is from poor abdominal muscle tone caused by the failure of the body to repair the separation of the right and left rectus abdominis muscle after pregnancy. The medical term for this separation is diastasis recti. Women with multiple pregnancies, pregnancies that occur close together, and
588 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
TABLE 1
Different Types of Abdominoplasty Procedures1-3
Procedure
Abdominoplasty (ie, tummy tuck)
Description
Surgical removal of excess abdominal skin and adipose tissue, usually from just above of the umbilicus to 2 cm above the pubis symphysis; repair of diastasis recti, and creation of a neoumbilicus. The patient must be placed in the reflexed position to close the skin. Surgical removal of limited excess abdominal skin and adipose tissue, confined centrally and below the umbilicus, and plication of rectus abdominis fascia. The umbilicus is floated (ie, is not detached from its surrounding abdominal skin). The patient may be placed in limited reflexed position for skin closure. Surgical removal of excess abdominal skin and adipose tissue (ie, pannus) only. The patient is not placed in the reflexed position for skin closure. Surgical removal of the pannus, usually from just above the umbilicus to 2 cm above the pubis symphysis, and the creation of a neoumbilicus. There is no plication of rectus fascia and the patient is placed in the reflexed position for skin closure. Surgical removal of the pannus and excess back skin and adipose tissuea single continuous incision is made circumferentially around the patient. A neoumbilicus is created, and plication of the rectus fascia may or may not be performed. The patients back is done first with the patient in the prone position after which the patient is turned supine for removal of the pannus. The patient is placed in limited reflexed position to minimize strain on the back wound closure.
Typical patient
Multiparous female
Miniabdominoplasty (ie, minitummy tuck)
The soccer mom (ie, a fit, well-toned woman with excess abdominal skin limited to the hypogastrium and diastasis recti) Male or female after moderate to massive weight loss Male or female after moderate to massive weight loss
Panniculectomy
Extended panniculectomy
Circumferential abdominoplasty (ie, belt lipectomy, lower body lift)
Male or female patients after massive weight loss, typically after gastric bypass surgery
Definitions Diastasis recti: separation of the right and left rectus abdominis muscles. Neoumbilicus: a new opening created through the newly pulled down abdominal skin to allow the umbilicus to pass through. Plication: pleating or folding and sewing of the rectus abdominis fascia. Reflexed position: the reclining position with additional flexion at the hips (ie, jack-knife position). 1. LaTrenta G. Abdominoplasty. In: Rees TD, LaTrenta G, eds. Aesthetic Plastic Surgery, Vol 2. 2nd ed. Philadelphia, PA: WB Saunders Co; 1994:1126-1178. 2. Pitanguy I. [Abdominal plastic surgery]. Hospital (Rio J). 1967;71(6):1541-1556. 3. Grazer FM. Abdominoplasty. Plast Reconstr Surg. 1973;51(6):617-623.
older woman are most at risk for separation of the abdominis muscle. Many of these women also have areas of localized fat (ie, lipodsytrophy) along their flanks which is difficult to eliminate with exercise but is ideal for liposuction. Many surgeons will include liposuction with the abdominoplasty surgery to improve
the postoperative cosmetic result. ABDOMINOPLASTY PATIENT SELECTION. Proper patient selection and education are paramount factors to ensure long-term success of the procedure. Patients opting for abdominoplasty must have realistic expectations and should be committed to implementing some healthy lifestyle changes
AORN JOURNAL
589
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
that include eating a well-balanced diet and exercising regularly.12 The ideal candidate for an abdominoplasty procedure is a person who is of ideal weight with deflated excess abdominal skin, is a nonsmoker, is in good physical and mental condition, and has support for assistance at home postoperatively. Women desiring abdominoplasty also should be finished having children and have a reliable birth control method. Contraindications to abdominoplasty include severe comorbid conditions (eg, heart disease, diabetes, irritable bowel syndrome, presence of an ostomy, bleeding dyscrasias); future plans for pregnancy; morbid obesity (ie, body mass index greater than 40); unrealistic patient expectations; and lack of home support postoperatively. A history of thromboembolic disease or prior surgical scars to the right, left, or bilateral upper quadrant are considered relative contraindications. The decision to operate on a patient with upper quadrant scars is dependent on the size and age of the scar THE PROCEDURE. Preoperatively, the surgeon marks the planned incision lines with a permanent marker while the patient is standing (Figure 1). This should always be performed in a private setting, and the patient should be completely disrobed. If the surgeon is male, a female nurse or technician may be asked to step into the room to be a chaperone and provide emotional support for the patient who is in a most unflattering position. After the surgeon has marked the planned incision lines, the preoperative nurse administers IV antibiotics within one hour before the surgical incision is made. Some surgeons also may order an anti-inflammatory steroid (eg, dexamethasone) to be administered approximately one hour before surgery, particularly if liposuction is planned. Before the patient arrives in the OR suite, the circulating nurse should rotate the OR bed 180 degrees and ensure that the bed can bend into the reflexed position (ie, lounge chair position with the hips flexed) or jack-knife position. The circulating nurse coordinates with
Figure 1 Typical markings for an abdominoplasty; the circular areas marked with an X represent areas to be treated with liposuction.
the anesthesia care provider before transporting the patient to the OR. On arrival in the OR, the patient moves onto the bed in the supine position. Before induction of anesthesia, the circulating nurse places sequential compression devices on the patients lower legs and turns on the machine as a measure to prevent deep vein thrombosis (DVT).7,13 The nurse may place a pillow under the patients knees to prevent lower back strain. After induction of anesthesia, the circulating nurse inserts an indwelling urinary catheter. The nurse ensures that all pressure points are well padded and that the patients arms are padded and secured to the arm boards at less than 90 degrees. Some surgeons pretreat the planned incision lines with a local anesthetic containing epinephrine (eg, 1% lidocaine with 1:100,000 epinephrine) before the circulating nurse performs the surgical skin prep. The nurse performs the prep carefully in an effort not to remove any of the markings that the surgeon placed on the patient preoperatively. The type of prep solution used is based on the surgeons preference.
590 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
Each surgeon performs an abdominoplasty in a slightly different way. The first step is skin excision around the umbilicus and skeletonizing the stalk to the fascia. Next, the surgeon makes the lower abdominal incision down to the fascia and dissects cephalad to create an abdominal skin flap. The costal margins are the lateral margins, and the xiphoid process is the cephalad margin. The surgeon repairs the diastasis recti by plicating the abdominal aponeurosis in the midline using a permanent suture. The anesthesia care provider repositions the bed to place the patient in the reflexed position and the surgeon pulls the excess skin caudally and trims it as needed. Usually two flat silicone drains are placed in the hair-bearing area of the mons to drain any postoperative coagulum; however, some surgeons advocate using progressive tension sutures (ie, sewing the underside of the abdominal skin flap to anchor it to the underlying fascia) to close the dead space, thereby eliminating the need for drains.14 The surgeon delivers the umbilicus through a stab hole made in the abdominal flap to create a neoumbilicus. The surgeon then closes the wound in layers. Depending on the patients body habitus, the surgeon may perform liposuction of the abdominal flap or flanks and possibly other anatomic areas. The timing and method by which liposuction is completed is entirely determined by the surgeons predilection. Most surgeons place an abdominal binder around the patient with padding, usually bulky cotton roll or a silicone-gel adhesive foam pad. The foam pad is likely to be used if liposuction was performed as well. After positioning the patient roller under the patients back but not under the buttocks, the circulating nurse, anesthesia care provider, scrub person, and surgeon transfer the patient to the hospital bed, not a gurney or stretcher, that the circulating nurse has prepositioned into the same angle of reflex as the OR bed. The purpose of transferring the patient directly into the hospital bed is to minimize the number of opportunities for patient injury, which are most likely to occur during transfers. The urinary catheter usually remains in place. Postoperatively, the patient will be prohibited
The first step in the abdominoplasty procedure is to excise around the patients umbilicus and skeletonize the stalk to the fascia. Next, the surgeon makes the lower abdominal incision down to the fascia and dissects cephalad to create an abdominal skin flap.
from standing straight or lying flat. Failing to comply with this could result in catastrophic wound dehiscence and possible disruption of the muscular aponeurotic plication. It is very important that all nurses caring for the patient be made aware of this important restriction. Often, nurses post a sign above the patients bed and make notes in the patients chart to prevent a late-night flattening to take vital signs.
LIPOSUCTION
In 1921, Dujarrier documented the first use of a cannula to remove fat for cosmetic reasons. Dujarrier used a uterine curette to remove adipose tissue from the knees of a well-known ballerina. The attempt proved disastrous, resulting in amputation of the leg because of injury to the vascular supply.9 Interest in lipectomy resurfaced in the 1960s. Schrudde removed localized collections of fat by using a sharp curette placed through a small incision and then applying a secondary suction to remove the resultant tissue remnants.15,16 Kesselring and Meyer17 added a higher negative pressure to this method of sharp curettage and reported good to excellent results with this method. Not everyone had the same results; a high incidence of skin necrosis and seroma formation were reported
AORN JOURNAL
591
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
Patients with excessive stria (ie, stretch marks) are poor candidates for liposuction because their skin is not capable of retracting and remolding over the new underlying contour; instead, the skin becomes deflated and hangs from the patients body.
with similar techniques.15,16 A blunt cannula attached to a vacuum pump was the next major advance in lipectomy.18,19 Until this time, suction-assisted lipectomy was commonly performed in Europe but generally was regarded poorly in the United States. The ASPS commissioned a small group of surgeons to visit Europe in the 1980s and observe this newer simultaneous technique of cutting and sucking. They returned with a cautiously optimistic report. Significant refinements continue to be made. Hetter20,21 emphasized the importance of an adequate vacuum pump and aspirator. Teimourian et al22 stressed the use of smaller cannulas with various tips to minimize the incidence of secondary contour irregularities. Klein23-25 introduced the technique of suction-assisted lipectomy (SAL), which minimizes the fluid and electrolyte losses as well as the operative and postoperative blood loss and morbidity associated with the technique. Public outcry for a body contouring procedure that could be performed with minimal scarring was growing, and public demand made SAL the most common plastic procedure performed in the 1980s through today.7,26 LIPOSUCTION PATIENT SELECTION. Liposuction should be considered foremost as a surgical procedure to enhance body contouring and not as a surgical modality for weight loss.27
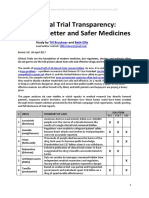
Patient selection criteria are similar to the criteria used for abdominoplasty. Liposuction patients must be especially committed to lifestyle changes (eg, eating a proper diet, exercising regularly) to achieve long-term results.28 Patients with excessive stria (ie, stretch marks) are poor candidates for liposuction because their skin is not capable of retracting and remolding over the new underlying contour. Instead, the skin will become deflated and hang from the body. Patients who have experienced massive weight loss may undergo liposuction of their arms and legs as one step in their overall surgical plan (ie, deflating the skin makes subsequent brachialplasty or medial thigh lift easier and safer). To be a good candidate for this surgery, patients also must be committed to the surgeons postoperative plan (eg, wearing compression garments as instructed, massaging the treated areas). TYPES OF LIPOSUCTION PROCEDURES. There are two kinds of liposuction procedures: SAL and ultrasound-assisted liposuction (UAL). These procedures are performed with the use of blunt, hollow metal cannulas that are connected to a suction machine. The surgeon moves the cannula back and forth along an axial plane in a fan pattern, parallel to the skin surface to bluntly dissect and aspirate cores of fat in a honeycomb pattern. WETTING SOLUTION. The concern for a large fluidvolume shift and blood loss after lipectomy warrants pretreating the area with a wetting solution (eg, a combination of 50 mL 1% lidocaine plain with 1 mg of epinephrine 1:1,000) in 1 L sodium chloride or lactated Ringers to make a 1:1,000,000 concentration. Table 2 shows the different formulas of wetting solution. The different techniques in the volume of wetting solution used are summarized in Table 3. The circulating nurse documents in the patients chart the amounts and areas injected with the wetting solution as well as the amount aspirated (Figure 2). Whether the solution is warmed is dependent on what type of liposuction is being performed: warm or room temperature solution is used for SAL and cool solution is used for UAL.
592 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
TABLE 2
TABLE 3
1
Wetting Solution Formulas
Ingredient Fodors formula
Lactated Ringers solution (LR) Aspirates < 2,000 mL epinephrine 1:500 Aspirates 2,000 mL to 4,000 mL epinephrine 1:1,000 Aspirates > 4,000 mL epinephrine 1:1,500
Wetting Solution Techniques1
Technique
Dry Wet
Amount
1,000 mL 1 mL 1 mL
Description
No wetting solution is used 200 mL to 300 mL of wetting solution is infiltrated in each treated area 1 mL of wetting solution is infiltrated for every expected 1 mL of aspirate Wetting solution is infiltrated until adequate skin turgor is achieved, usually a ratio of 2 mL to 3 mL of wetting solution for every expected 1 mL of aspirate
Superwet 1 mL Tumescent
Hundstadts formula
LR* 1% lidocaine Epinephrine 1:1,000 1,000 mL* 50 mL 1 mL
Kleins formula
LR 1% lidocaine Epinephrine 1:1,000 8.4% bicarbonate 1,000 mL 50 mL 1 mL 12.5 mL
1. Rohrich RJ, Beran SJ, Kenkel JM. UltrasoundAssisted Liposuction. St Louis, MO: Quality Medical Publishing, Inc; 1998.
The University of Texas Southwestern Medical Center formula
LR** 1% lidocaine Aspirates < 5,000 mL 1% lidocaine Aspirates > 5,000 mL 1% lidocaine Epinephrine 1:1,000 1,000 mL 50 mL 30 mL 15 mL 1 mL
* Temperature of LR for ultrasound-assisted liposuction (UAL) should be between 38 C to 40 C (100.4 F to 104 F). ** Temperature of LR for UAL should be 21 C (69.8 F). 1. Rohrich RJ, Beran SJ, Kenkel JM. UltrasoundAssisted Liposuction. St Louis, MO: Quality Medical Publishing, Inc; 1998.
Although currently there is little scientific data identifying the maximal safe volumes of wetting solution to use,29 there is no doubt that complication risks increase with increasing lipoaspirate volume and with treatment of multiple anatomic locations.30 The ASPS Committee on Patient Safety Practice advisory on liposuction defines large-volume liposuction as using more than 5 L of lipoaspirate during one
surgical procedure.7,31 Using large volumes of aspirate induces substantial fluid alterations.7 The tumescent technique of infiltrating 2 mL to 3 mL of wetting solution for every 1 mL of anticipated lipoaspirate leaves behind 50% to 70% of the infiltrated volume, which can potentially result in fluid overload.6,7,32 Using more than 70 mL/kg of wetting solution infiltration is more likely to cause fluid overload. The complications of an estimated 70% of subcutaneous infiltrate becoming intravascular27 presents as increased blood pressure, jugular vein distension, and bounding pulses;7 cough, dyspnea, and lung crackles;33 and pulmonary edema.7,34,35 It is important that the surgeon knows the total lipoaspirate (ie, fluid plus fat removed) and volume of wetting solution used. Some surgeons believe that patients requiring large-volume liposuction should undergo the procedure in a hospital setting because the potential complications of this technique require extended observation and potential diuresis.7 Hypothermia also can be a confounding issue; it is absolutely imperative that warmed wetting solution be used for SAL. Warmed
AORN JOURNAL
593
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
Figure 2 Intraoperative liposuction data sheet. Reprinted with permission from Landstuhl Regional Medical Center, Landstuhl, Germany.
594 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
wetting solutions are avoided during UAL, however, to prevent burning. Cold solutions are used instead because of the excess heat generated during UAL. When UAL is going to be used for large-volume liposuction, the cold wetting solution should be infiltrated in stages to minimize prolonged contact with the body. The surgeon depends on the circulating nurse and scrub person for accurate fluid management and measurements to guide the patients postoperative care and safe discharge determination.7 SUPERWET TECHNIQUE. The superwet technique infiltrates 1 mL of wetting solution for every expected 1 mL of aspirate. This technique is favored by some surgeons to minimize the amount of wetting solution. LIPOSUCTION ANESTHETICS. Anesthetic agents added to liposuction wetting solutions provide the benefit of postoperative analgesia. These agents, however, must be used with caution. Bupivacaine is poorly reversed, is rapidly absorbed, and has a long half-life.36 Toxic effects include cardiac arrhythmias, seizures, respiratory depression, and coma, and bupivacaine can be lethal if injected intravascularly.7 Lidocaine, unlike bupivacaine, is more easily reversed, and up to 7 mg/kg can be injected with epinephrine into subcutaneous fat.37,38 Nevertheless, lidocaine toxicity has been associated with liposuction-related deaths.39 Toxicity presents with dizziness, agitation, lethargy, tinnitus, metallic taste, perioral paresthesias, and slurred speech.7 Lidocaine plasma levels peak at 10 to 12 hours after infiltration of wetting solution.40 To decrease risk of lidocaine toxicity, the ASPS task force recommends smaller concentrations of lidocaine in the wetting solution, using the superwet technique rather than the tumescent technique, and not using lidocaine with general or regional anesthesia.7 The task force further recommends that surgeons avoid epinephrine use in patients with conditions such as severe hypertension, cardiac disease, or peripheral vascular disease.7 Epinephrine dosing should be kept at less than 0.07 mg/kg,7 although higher doses have been reported to be safe.28
Lidocaine, unlike bupivacaine, is more easily reversed, and up to 7 mg/kg can be injected with epinephrine into subcutaneous fat; but, lidocaine toxicity, characterized by agitation, lethargy, slurred speech, tinnitus, and metallic taste, has been associated with liposuction-related deaths.
THE PROCEDURE. Most surgeons order preoperative IV antibiotics and an anti-inflammatory steroid (eg, dexamethasone). Ideally, the preoperative nurse should ensure that the steroid is completely infused one hour before the surgical incision is made. The circulating nurse places sequential compression devices on the patient before induction of general anesthesia or takes other antithrombotic measures in accordance with practice guidelines.7,13 After the patient is anesthetized, the circulating nurse pads any pressure areas and inserts an indwelling urinary catheter if the procedure is expected to last longer than three hours. The catheter is removed at the end of the procedure unless large volume liposuction was performed, in which case, the catheter usually is left in for postoperative fluid monitoring. The circulating nurse then performs the surgical skin prep, taking care not to remove the surgeons preoperative markings. These markings guide the surgeon by highlighting areas to be treated and areas to avoid. If some of the treated areas are on the flanks approaching the back, the circulating nurse may require assistance in rolling the patient from side to side to prep the back and flanks. Usually, the surgeon rolls the patient to one side while the circulating nurse preps that side and then the scrub
AORN JOURNAL
595
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
person lays a drape under the patient. The process is repeated for the opposite side. Some surgeons prefer to have the patient prepped circumferentially while the patient is standing next to the OR bed. Then the patient lies on the bed where sterile drapes are already prepositioned, after which the scrub person drapes the patient and the anesthesia care provider induces anesthesia. Depending on the liposuction technique to be used, the surgeon infiltrates the treated areas with a wetting solution. If volumes greater than 5 L of fat are expected to be aspirated, only 15 mL of 1% lidocaine per liter of wetting solution should be used.41 The surgeon introduces the wetting solution via small stab incisions, which also are used for the liposuction cannulas. The circulating nurse records the volumes and locations of the wetting solu-
tion. The surgeon waits approximately seven to 10 minutes after injection of the wetting solution before beginning treatment. If UAL is being performed, the surgeon inserts a blunt trocar that serves as a dilator for the UAL cannula and protects the patients skin stab incisions against thermal injury from the UAL cannula. The surgeon also protects the skin by inserting the cannula through a sheath or by laying a wet towel under the cannula to prevent thermal injury from accidental contact with the UAL cannula. These precautions are not necessary for SAL. The actual technique used to aspirate fat and the stop signals for ending the liposuction in a treated area are different for SAL and UAL. Table 4 highlights these differences. When UAL is being used, the circulating nurse records the treatment time. Most UAL
TABLE 4
Differences in Suction-Assisted Lipectomy (SAL) and Ultrasound-Assisted Liposuction (UAL) Techniques1
Characteristic
Stroke characteristics of the cannula Access incisions Cross tunneling/ criss-crossing strokes Skin protection at access incisions Sequence of liposuction End points/time to stop Nondominant hand position
SAL
Forceful Approximately 3 mm in size and multiple incisions Yes No Deep to superficial Final contour/pinch test Grasping and firm palpation*
UAL
Slow, rhythmic stroke (ie, 50% of the SAL rate) Longer (ie, 5 mm to 7mm) in size but fewer incisions No Yes Superficial to deep Loss of resistance/blood in aspirate Parallel and gentle palpation
* Grasping and firm palpation refers to grabbing the skin to create a roll and sliding the cannula through that roll to aspirate the fat; this is only performed during SAL. In UAL, the nondominant hand is placed on top of the skin with open palm pressing down gently and the UAL cannula slides under the hand. 1. Rohrich RJ, Beran SJ, Kenkel JM. Ultrasound-Assisted Liposuction. St Louis, MO: Quality Medical Publishing, Inc; 1998.
596 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
machines display the treatment time and should ing liposuction unless liposuction was perbe reset when the surgeon moves to a different formed in conjunction with another procedure area. If the surgeon returns to a previously treat- that warrants admission or more than 5 L of ed area, the circulating nurse adds the additionlipoaspirate was obtained.7 Some surgeons al treatment time to the previous time. The cirmay opt to admit select patients for overnight culating nurse also records the UAL generator observation if more than 3.5 L of fat was aspiunit number and settings. Recording treatment rated. If the patient had large-volume liposuctime is not necessary for SAL. tion, the postanesthesia care unit nurse obBecause the wetting solution used in UAL is serves the patient for signs of pulmonary chilled, the surgeon infiltrates the wetting soluedema or intravascular fluid shifts by monitortion by anatomic area, usually completing treat- ing the patients blood pressure, pulse, and ment in bilateral structures as a single pair to urine output. If drains were placed, the surminimize the patients prolonged exposure to geon usually removes them in 24 to 48 hours. the chilled wetting solution. The circulating The patient usually changes his or her own nurse records the volumes aspirated and locadressing within a week. The discharge nurse intions for each treated site. structs the patient to remove the After the liposuction is comcompression garment and the pleted, many surgeons squeeze foam in the presence of a family and milk out any excess wetmember or friend. As a precauting solution. The surgeon then tionary measure, the nurse inAfter the liposuction closes the surgical incisions; structs the patient to sit for five preference determines the to 10 minutes after the dressing but before closure of manner in which the surgeon is removed and before showercloses the wounds. Drains usuing to avoid light-headedness the surgical incisions, ally are not necessary after and to have someone present UAL or SAL, but if large volwhen showering after removal many surgeons squeeze umes of lipoaspirate were reof the garment in the event moved or large areas were aglight-headedness occurs. Paand milk out any excess gressively treated, the surgeon tients can shower after the commay decide to place a drain. pressive garment is removed, wetting solution. The surgeon and scrub but should avoid tub bathing person place dressings covfor two weeks after surgery. ered with a silicone-gel adheThe patient wears the garsive foam pad on top of the ment continuously except treated areas. A silicone pad when showering for two is not placed over the buttocks, posterior flank, weeks and then at night for an additional two or back because the pad will cause friction weeks. Patients who have undergone abdomiburns and blisters. The surgeon places an abnal contouring wear an abdominal binder. dominal pad over these pressure areas to help Many patients wear the compressive garments compress the area. The circulating nurse and for prolonged periods for support while exercisanesthesia care provider assist the surgeon ing and to help decrease the edema in the exand scrub person in placing a compressive tremities that may persist for several months.41 garment on the patient. The compressive garPatients return for follow-up visits two, three, ment should have side zippers to make getand six weeks after surgery and then at three ting into and out of the garment easier for the and six months. During postoperative visits, the patient. There are a variety of compressive surgeon or nurse carefully assess all treated garments available for use on different areas areas to rule out infection or seromas.41 depending on the surgeons preference. Patients should expect POSTOPERATIVE CARE. The patient generally will maximal swelling from three to five days not be admitted to the hospital after undergopostoperatively,
AORN JOURNAL
597
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
bruising to resolve in seven to 10 days, and most of the edema to resolve in three to four weeks. Hardness and induration, however, can persist for at least six to eight weeks. The final result can be assessed in three to four months when the induration and edema have resolved.41 SATISFACTION. Liposuction alone is the most common cosmetic procedure performed. A self-assessment survey was mailed to 600 patients in Dallas, Texas, to examine patients attitudes and postoperative opinions, lifestyle changes, weight gain changes, and satisfaction with their liposuction procedure.12 The results revealed that the majority (ie, 80%) of the patients surveyed were satisfied with the results. Fifty-three percent of the respondents thought their appearance was either excellent or very good, and 33% responded that their appearance was good. Despite postoperative pain, some fat return, and occasional weight gain, 79.7% would have the procedure again and 86% would recommend liposuction to family members or friends. The importance of preoperative counseling and a mutual understanding of expectations between the patient and surgeon cannot be underestimated.12
enced a pulmonary embolism and 6.8% experienced DVT.7 The most common method of deep vein prophylaxis practiced during plastic surgery is the use of sequential compression devices alone.7 This method has been shown to reduce the incidence of DVT by 60%. Lowmolecular-weight heparin decreases the incidence by 78%. Subcutaneous heparin administered twice daily reduces the incidence of deep vein thrombosis by 69% and fatal pulmonary embolism by 96%.7
CONCLUSION
The combined procedure of abdominoplasty and liposuction has been gaining popularity. Many women and men are finding that this type of procedure allows them to regain their preferred body image. Plastic surgery is not for everyone, however. Those who elect to have this procedure must be willing and able to comply with dietary and exercise habits and be willing to adhere to follow-up recommendations. It is beneficial for patients to have a good family support system in place to assist with postoperative care and long-term lifestyle changes. With any type of surgical procedure, patients need to weigh the risks and benefits and seek out the knowledge and references of the surgeon who will perform the procedure, as well as learn the reputation of the facility where it will be performed. The surgeon should obtain a detailed informed consent, which identifies the risks this procedure could entail. Perioperative nurses must be knowledgeable about the different types of procedures, the types of wetting solutions, and how to properly set up the OR bed for positioning. Incorporating a plastic surgery team (eg, circulating nurse, scrub person, RN first assistant, physicians assistant) increases the efficiency of these procedures and lessens the time the patient will be under anesthesia. Ultimately, patient safety and outcome satisfaction are the goals of the OR team. Editors note: The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
COMPLICATIONS
From 1999 to 2000, a series of sensational articles were published in the lay media emphasizing the hazards of office-based surgery.42 Since then, 31 state medical boards or legislatures have drafted, or are in the process of drafting, regulations restricting office procedures. The most common serious complication from these procedures is DVT.43-45 This could lead to catastrophic complications of postthrombic syndrome, pulmonary embolism, and death that is well documented in the general surgery and orthopedic surgery literature. Deep vein thrombosis most commonly develops in the deep veins of the calf muscle. Postthrombotic syndrome is a consequence of venous stasis and venous hypertension caused by damaged venous valves that no longer regulate the unidirectional flow of venous blood out of the legs and back to the heart. According to one survey of patients who underwent liposuction, only 1% reported having experi-
598 AORN JOURNAL
Logan Broughton
OCTOBER 2008, VOL 88, NO 4
REFERENCES 1. Horton JB, Reece EM, Broughton G 2nd, et al. Patient safety in the office-based setting. Plast Reconstr Surg. 2006;117(4):61e-80e. 2. Byrd HS, Barton FE, Orenstein HH, et al. Safety and efficacy in an accredited outpatient plastic surgery facility: a review of 5316 consecutive cases. Plast Reconstr Surg. 2003;112(2):636-641. 3. Keyes GR, Singer R, Iverson RE, et al. Analysis of outpatient surgery center safety using an internet-based quality improvement and peer review program. Plast Reconstr Surg. 2004;113(6):1760-1770. 4. Scharnberg K. For some, cost of cosmetic surgery is personal health. Chicago Tribune. May 7, 2004:1. 5. Iverson RE. Patient safety in office-based surgery facilities: I. Procedures in the office-based surgery setting. Plast Reconstr Surg. 2002;110(5): 1337-1342. 6. Iverson RE, Lynch DJ. Patient safety in officebased surgery facilities: II. Patient selection. Plast Reconstr Surg. 2002;110(7):1785-1790. 7. Iverson RE, Lynch DJ. Practice advisory on liposuction. Plast Reconstr Surg. 2004;113(5):1478-1490. 8. La Trenta G. Abdominoplasty. In: Rees TD, La Trenta G, eds. Aesthetic Plastic Surgery, Vol 2. 2nd ed. Philadelphia, PA: WB Saunders Co; 1994: 1126-1178. 9. Gabriel A, Gupta SC, Freeman BG. Body contouring, abdominoplasty. eMedicine. http://www .emedicine.com/plastic/TOPIC12.HTM. Accessed August 11, 2008. 10. Pitanguy I. [Abdominal plastic surgery]. Hospital (Rio J). 1967;71(6):1541-1556. 11. Grazer FM. Abdominoplasty. Plast Reconstr Surg. 1973;51(6):617-623. 12. Broughton G 2nd, Horton B, Lipschitz A, et al. Lifestyle outcomes, satisfaction, and attitudes of patients after liposuction: a Dallas experience. Plast Reconstr Surg. 2006;117(6):1738-1749. 13. Broughton G 2nd, Rios JL, Rohrich RJ, Brown SA. Deep venous thrombosis prophylaxis practice and treatment strategies among plastic surgeons: survey results. Plast Reconstr Surg. 2007;119(1):157-174. 14. Pollock T, Pollock H. Progressive tension sutures in abdominoplasty. Clin Plast Surg. 2004;31 (4):583-589, vi. 15. Fuerst ML. Suction-assisted lipectomy attracting interest. JAMA. 1983;249(22):3004-3005. 16. Gargan TJ, Courtiss EH. The risks of suction lipectomy. their prevention and treatment. Clin Plast Surg. 1984;11(3):457-463. 17. Kesselring UK, Meyer R. A suction curette for removal of excessive local deposits of subcutaneous fat. Plast Reconstr Surg. 1978;62(2):305-306. 18. Fournier PF, Otteni FM. Lipodissection in body sculpturing: the dry procedure. Plast Reconstr Surg. 1983;72(5):598-609. 19. Illouz YG. Body contouring by lipolysis: a 5year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-597.
20. Hetter GP. Optimum vacuum pressures for lipolysis. Aesthetic Plast Surg. 1984;8(1):23-26. 21. Hetter GP. The effect of low-dose epinephrine on the hematocrit drop following lipolysis. Aesthetic Plast Surg. 1984;8(1):19-21. 22. Teimourian B, Adham MN. Anterior periosteal dermal suspension with suction curettage for lateral thigh lipectomy. Aesthetic Plast Surg. 1982;6(4): 207-209. 23. Klein JA. Anesthesia for liposuction in dermatologic surgery. J Dermatol Surg Oncol. 1988;14(10): 1124-1132. 24. Klein JA. The tumescent technique. Anesthesia and modified liposuction technique. Dermatol Clin. 1990;8(3):425-437. 25. Klein JA. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol. 1990;16(3):248-263. 26. Rohrich RJ. The increasing popularity of cosmetic surgery procedures: a look at statistics in plastic surgery. Plast Reconstr Surg. 2000;106(6):1363-1365. 27. Rohrich RJ, Beran SJ. Is liposuction safe? Plast Reconstr Surg. 1999;104(3):814. 28. Rubin P, Bierman C, Rosow CE, et al. The tumescent technique: the effect of high tissue pressure and dilute epinephrine on absorption of lidocaine. Plast Reconstr Surg. 1999;103(3):990-996. 29. Commons GW, Halperin B, Chang CC. Largevolume liposuction: a review of 631 consecutive cases over 12 years. Plast Reconstr Surg. 2001;108 (6):1753-1763. 30. Hunstad JP. Body contouring in the obese patient. Clin Plast Surg. 1996;23(4):647-670. 31. Rohrich RJ, Kenkel JM, Janis JE, Beran SJ, Fodor PB. An update on the role of subcutaneous infiltration in suction-assisted lipoplasty. Plast Reconstr Surg. 2003;111(2):926-927. 32. Trott SA, Beran SJ, Rohrich RJ, et al. Safety considerations and fluid resuscitation in liposuction: an analysis of 53 consecutive patients. Plast Reconstr Surg. 1998;102(6):2220-2229. 33. Gringrass M. Lipoplasty complications and their prevention. Clin Plast Surg. 1999;26(3):341-354. 34. Gilliland MD, Coates N. Tumescent liposuction complicated by pulmonary edema. Plast Reconstr Surg. 1997;99(1):215-219. 35. Rubenstein EH. An anesthesiologists perspective of lipoplasty. Clin Plast Surg. 1999;26(3):423429. 36. Miller RD. Local anesthetics. In: Anesthesia. 6th ed. Philadelphia, PA: Churchill Livingston; 2005:592. 37. de Jong RH. Lidocaine dosing duality in liposuction: safe only when highly diluted. Plast Reconstr Surg. 2003;111(2):926-927. 38. Rohrich RJ, Jenis JE. Lidocaine dosing duality in liposuction: safe only when highly diluted: reply. Plast Reconstr Surg. 2004;113(5):1514-1515. 39. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340(19):1471-1475. 40. Fodor PB, Watson JP. Wetting solutions in
AORN JOURNAL
599
OCTOBER 2008, VOL 88, NO 4
Logan Broughton
ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26(2):289-293, ix. 41. Rohrich RJ, Beran SJ, Kenkel JM. UltrasoundAssisted Liposuction. St Louis, MO: Quality Medical Publishing, Inc; 1998. 42. Coldiron BM. Office surgical incidents: 19 months of Florida data. Dermatol Surg. 2002;28(8): 710-712. 43. Coldiron BM, Healy C, Bene NI. Office surgery incidents: what seven years of Florida data show us. Dermatol Surg. 2008;34(3):285-291. 44. Clayman MA, Caffee HH. Office surgery safety and the Florida moratoria. Ann Plast Surg. 2006;56 (1):78-81. 45. Clayman MA, Seagle BM. Office surgery safety: the myths and truths behind the Florida moratoria six years of Florida data. Plast Reconstr Surg. 2006; 118(3):777-785.
MAJ Judith M. Logan, RN, BSN, CNOR, MBA, is a head nurse in the OR at Landstuhl Regional Medical Center, Landstuhl, Germany. MAJ Logan has no declared affiliation that could be perceived as a potential conflict of interest in publishing this article. COL George Broughton II, MD, PhD, is the chief, Department of Plastic and Reconstructive Surgery at Landstuhl Regional Medical Center, Landstuhl, Germany. COL Broughton has no declared affiliation that could be perceived as a potential conflict of interest in publishing this article.
Ambulatory Facility Accreditation May Improve Outcomes
new study based on data from an Internet-reporting system showed that accredited ambulatory surgery centers can be as safe as inpatient surgery centers, according to a June 24, 2008, news release from the American Association for Accreditation of Ambulatory Surgery Facilities (AAAASF). The study involved more than 1.1 million outpatient procedures reported over a five-and-a-half-year period in facilities accredited by the AAAASF.
During the analysis period, only one death occurred because of an intraoperative adverse event. More than half of the 23 reported deaths in the study population were caused by pulmonary embolism.
New study demonstrates high level of safe surgeries performed in accredited facilities. Gurnee, IL: American Association for Accreditation of Ambulatory Surgery Facilities; June 24, 2008.
Disinfecting Desks and Hands Reduces School Absences
llness-related student absences may be reduced by disinfecting frequently touched surfaces and using alcohol-based hand sanitizers in elementary schools, according to a June 2, 2008, news release from Childrens Hospital, Boston, Massachusetts. Specifically, these infection control measures reduced absences related to gastrointestinal (GI) illness. The study involved 285 third, fourth, and fifth graders. In classrooms where teachers used disinfecting wipes on student desks and children used alcohol-based hand sanitizers, absenteeism rates for GI illnesses decreased 9% during an eight-week period compared to classrooms where usual hand washing and cleaning procedures were followed. No
effect was seen on respiratory illness during the study. According to researchers, the germs that cause GI infections can be easily passed between children on the hands and can survive on surfaces for hours or even days. The researchers concluded that elementary school staff members could reduce illness-related absences by adopting infection control practices, such as disinfecting desks once a day and ensuring students use hand sanitizers before and after lunch.
Study findings show infection control intervention helps keep kids in school [news release]. Boston, MA: Childrens Hospital Boston; June 2, 2008.
600 AORN JOURNAL
Anda mungkin juga menyukai
- Abdominoplasty Classic Principles and TechniqueDokumen18 halamanAbdominoplasty Classic Principles and TechniqueJonathan Zenteno JiménezBelum ada peringkat
- TULUA Springer PDFDokumen10 halamanTULUA Springer PDFCésar Cuadros SerranoBelum ada peringkat
- TULUA Lipoabdominoplasty 2020Dokumen18 halamanTULUA Lipoabdominoplasty 2020Antonio Cardenas100% (1)
- Plastic & Hand Surgery in Clinical Practice: Classifications and DefinitionsDari EverandPlastic & Hand Surgery in Clinical Practice: Classifications and DefinitionsBelum ada peringkat
- Sec 4 - Techniques 2Dokumen31 halamanSec 4 - Techniques 2Karem TubeBelum ada peringkat
- Modified and Radical Neck Dissection TechniqueDokumen19 halamanModified and Radical Neck Dissection TechniquethtklBelum ada peringkat
- The Open Brow LiftDokumen8 halamanThe Open Brow LiftdoctorbanBelum ada peringkat
- 10-16-01 Cleft Lip and Palate Part 1Dokumen52 halaman10-16-01 Cleft Lip and Palate Part 1Zoilo NuñezBelum ada peringkat
- Facial Analysis LRDokumen36 halamanFacial Analysis LRdestiBelum ada peringkat
- Liposuccion Cervical Haack2006Dokumen7 halamanLiposuccion Cervical Haack2006ever renteriaBelum ada peringkat
- Smile Restoration After Facial PalsyDokumen6 halamanSmile Restoration After Facial PalsyJimmie CooperBelum ada peringkat
- LiposuctionDokumen8 halamanLiposuctionnikitagustiBelum ada peringkat
- TULUA Lipoabdominoplasty Transversal Aponeurotic.12Dokumen14 halamanTULUA Lipoabdominoplasty Transversal Aponeurotic.12Carolina Ormaza Giraldo100% (1)
- Ethnic and Gender Considerations in The Use of Facial Injectables: Male PatientsDokumen4 halamanEthnic and Gender Considerations in The Use of Facial Injectables: Male PatientsLuiggi FayadBelum ada peringkat
- Bahan Local FlapDokumen72 halamanBahan Local FlapChandrawati PramanaBelum ada peringkat
- Structural Fat GraftingDokumen19 halamanStructural Fat GraftingGautam KalraBelum ada peringkat
- Manual of Surgery Volume Second: Extremities—Head—Neck. Sixth Edition.Dari EverandManual of Surgery Volume Second: Extremities—Head—Neck. Sixth Edition.Belum ada peringkat
- Plastic SurgeryDokumen6 halamanPlastic SurgeryYing Hui LiewBelum ada peringkat
- Volume Facial e IdadeDokumen6 halamanVolume Facial e IdadeJeniffer RafaelaBelum ada peringkat
- Dr. Rani - Surgical Management of Pressure SoreDokumen19 halamanDr. Rani - Surgical Management of Pressure SoreOtto NaftariBelum ada peringkat
- Auric Recon Slides 070516Dokumen92 halamanAuric Recon Slides 070516Yudhistira AdeBelum ada peringkat
- Facial Nerve Palsy in Newborn PeriodDokumen5 halamanFacial Nerve Palsy in Newborn PeriodjajBelum ada peringkat
- Abdominal Liposuction InstructionDokumen3 halamanAbdominal Liposuction InstructionDizon HenryBelum ada peringkat
- Laser Liposuction Scientific ReseachDokumen31 halamanLaser Liposuction Scientific ReseachBilal HasenBelum ada peringkat
- Tumescent TAPP Laparoscopic Inguinal Hernia RepairDokumen6 halamanTumescent TAPP Laparoscopic Inguinal Hernia RepairUmer KhanBelum ada peringkat
- Gynecomastia Surgery - Power Assisted LiposuctionDokumen4 halamanGynecomastia Surgery - Power Assisted LiposuctionAlfredo Callanta,M.D.Belum ada peringkat
- Reconstructive Conundrums in Dermatologic Surgery: The NoseDari EverandReconstructive Conundrums in Dermatologic Surgery: The NoseDesiree S. RatnerBelum ada peringkat
- Jcad 13 2 33Dokumen11 halamanJcad 13 2 33ntnquynhproBelum ada peringkat
- Complications of BlepharoplastDokumen8 halamanComplications of BlepharoplastdoctorbanBelum ada peringkat
- Update On The Management of Keloids: A. Paul Kelly, MDDokumen6 halamanUpdate On The Management of Keloids: A. Paul Kelly, MDBudi KusumaBelum ada peringkat
- Aesthetic Surgery of The Orbits and EyelidsDokumen31 halamanAesthetic Surgery of The Orbits and EyelidsdoctorbanBelum ada peringkat
- History of RhinoplastyDokumen9 halamanHistory of RhinoplastySyamsul RizalBelum ada peringkat
- Neligan Vol 4 Chapter 10 MainDokumen20 halamanNeligan Vol 4 Chapter 10 MainisabelBelum ada peringkat
- Microsurgical Free FlapsDokumen24 halamanMicrosurgical Free FlapsTaufik Akbar Faried LubisBelum ada peringkat
- Dual Plane ApproachDokumen14 halamanDual Plane ApproachAndreea GhitaBelum ada peringkat
- Flap Selection in Head and Neck Cancer ReconstructionDokumen14 halamanFlap Selection in Head and Neck Cancer ReconstructionFerry RusdiansaputraBelum ada peringkat
- Facial PlasticsDokumen116 halamanFacial Plasticssyed imdadBelum ada peringkat
- Fat Burning Lasers For Surgical Body SculptingDokumen5 halamanFat Burning Lasers For Surgical Body SculptingsrimatsimhasaneshwarBelum ada peringkat
- Kuliah Gangguan Palpebra Dan KonjungtivaDokumen159 halamanKuliah Gangguan Palpebra Dan KonjungtivadudidumBelum ada peringkat
- Asian Rhinoplasty1Dokumen19 halamanAsian Rhinoplasty1drbantmBelum ada peringkat
- Serdev Suture Techniques Breast Lift - Prof Nikolay P Serdev MD PHDDokumen4 halamanSerdev Suture Techniques Breast Lift - Prof Nikolay P Serdev MD PHDjobetobaBelum ada peringkat
- Aesthetic, Breast 2001 PDFDokumen124 halamanAesthetic, Breast 2001 PDFAhmed AttiaBelum ada peringkat
- BJPS 1984 Cormack Classification of FlapsDokumen8 halamanBJPS 1984 Cormack Classification of FlapsS EllurBelum ada peringkat
- Principles Plastic SurgeryDokumen2 halamanPrinciples Plastic SurgeryIulia DabijaBelum ada peringkat
- Suture Lift and Liposculpture-Chapter 8 PDFDokumen10 halamanSuture Lift and Liposculpture-Chapter 8 PDFAnonymous 8hVpaQdCtrBelum ada peringkat
- Combined Technique of Superficial Liposuction With Ultrasonic Liposculpture PDFDokumen8 halamanCombined Technique of Superficial Liposuction With Ultrasonic Liposculpture PDFeiad-mahmoudBelum ada peringkat
- Congenital Infiltrating Lipomatosis of The Face Case Report PDFDokumen4 halamanCongenital Infiltrating Lipomatosis of The Face Case Report PDFfeli2010Belum ada peringkat
- Aging Facial Skeleton PrsDokumen10 halamanAging Facial Skeleton PrsJorge TreviñoBelum ada peringkat
- A Randomised Controlled Study For The Treatment of Acne Vulgaris Using High Intensity 414nm Solid State Diode ArraysDokumen29 halamanA Randomised Controlled Study For The Treatment of Acne Vulgaris Using High Intensity 414nm Solid State Diode ArraysCaerwyn AshBelum ada peringkat
- Neuromodulators Injection On The ForeheadDokumen24 halamanNeuromodulators Injection On The ForeheadJennifer GomezBelum ada peringkat
- Z-Plasty For Sculpturing of The Bifid Scrotum in Severe Hypospadias Asscociated With Penoscrotal TranspositionDokumen5 halamanZ-Plasty For Sculpturing of The Bifid Scrotum in Severe Hypospadias Asscociated With Penoscrotal TranspositionneonitesBelum ada peringkat
- Emerging Trends in Botulinum Neurotoxin A Resistance - An International Multidisciplinary Review and Consensus - Ho, 2022Dokumen11 halamanEmerging Trends in Botulinum Neurotoxin A Resistance - An International Multidisciplinary Review and Consensus - Ho, 2022Rafael Autran Cavalcante AraújoBelum ada peringkat
- 2005 Mesotherapy For Body ContouringDokumen5 halaman2005 Mesotherapy For Body ContouringDra. Tatiane FariaBelum ada peringkat
- Integrated Management of The Thick-Skinned Rhinoplasty PatientDokumen6 halamanIntegrated Management of The Thick-Skinned Rhinoplasty PatientFabian Camelo OtorrinoBelum ada peringkat
- 10 16 02CleftLipandPalatePart2 PDFDokumen93 halaman10 16 02CleftLipandPalatePart2 PDFalinutza_childBelum ada peringkat
- Lower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANDokumen3 halamanLower Blepharoplasty: How To Avoid Complications: Dr. Vincent KH KWANHadi FirmansyahBelum ada peringkat
- Nasolabial Flap For Oral Cavity ReconstructionDokumen10 halamanNasolabial Flap For Oral Cavity ReconstructionJamesBelum ada peringkat
- Gox 1 E07 PDFDokumen2 halamanGox 1 E07 PDFUmer HussainBelum ada peringkat
- Alternative Technique For Tip Support in Secondary RhinoplastyDokumen8 halamanAlternative Technique For Tip Support in Secondary RhinoplastydoctorbanBelum ada peringkat
- Laser Skin Treatment in Non-Caucasian PatientsReview ArticleDokumen8 halamanLaser Skin Treatment in Non-Caucasian PatientsReview ArticledoctorbanBelum ada peringkat
- Assessment of Nasal Function After Tip Surgery With A Cephalic Hinged Flap of The Lateral CruraDokumen9 halamanAssessment of Nasal Function After Tip Surgery With A Cephalic Hinged Flap of The Lateral CruradoctorbanBelum ada peringkat
- Are There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemDokumen8 halamanAre There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemdoctorbanBelum ada peringkat
- Ethnic Considerations in Hair Restoration SurgeryReview ArticleDokumen11 halamanEthnic Considerations in Hair Restoration SurgeryReview ArticledoctorbanBelum ada peringkat
- Scar Treatment Variations by Skin TypeReview ArticleDokumen10 halamanScar Treatment Variations by Skin TypeReview ArticledoctorbanBelum ada peringkat
- Repair of A Large Defect of The Upper LipDokumen4 halamanRepair of A Large Defect of The Upper LipdoctorbanBelum ada peringkat
- Microfat Grafting in Nasal SurgeryDokumen17 halamanMicrofat Grafting in Nasal SurgerydoctorbanBelum ada peringkat
- Combined Vestibular Mucosal Advancement and Island Pedicle Flaps For The Repair of A Defect Involving The Cutaneous and Vermilion Upper LipDokumen4 halamanCombined Vestibular Mucosal Advancement and Island Pedicle Flaps For The Repair of A Defect Involving The Cutaneous and Vermilion Upper LipdoctorbanBelum ada peringkat
- Scar Treatment Variations by Skin TypeReview ArticleDokumen10 halamanScar Treatment Variations by Skin TypeReview ArticledoctorbanBelum ada peringkat
- The Role of Gravity in Periorbital andDokumen15 halamanThe Role of Gravity in Periorbital anddoctorbanBelum ada peringkat
- The Pinch Rhytidectomy A Safe, Effective, Low SMAS Variation On The ThemeDokumen17 halamanThe Pinch Rhytidectomy A Safe, Effective, Low SMAS Variation On The ThemedoctorbanBelum ada peringkat
- Repair of A Large Defect of The Upper LipDokumen4 halamanRepair of A Large Defect of The Upper LipdoctorbanBelum ada peringkat
- Are There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemDokumen8 halamanAre There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemdoctorbanBelum ada peringkat
- Repair of A Large Defect of The Upper LipDokumen4 halamanRepair of A Large Defect of The Upper LipdoctorbanBelum ada peringkat
- Are There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemDokumen8 halamanAre There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemdoctorbanBelum ada peringkat
- Comparison Study of Fractional Carbon Dioxide Laser Resurfacing Using Different Fluences and Densities For Acne Scars in AsiansDokumen8 halamanComparison Study of Fractional Carbon Dioxide Laser Resurfacing Using Different Fluences and Densities For Acne Scars in AsiansdoctorbanBelum ada peringkat
- Comparison Study of Fractional Carbon Dioxide Laser Resurfacing Using Different Fluences and Densities For Acne Scars in AsiansDokumen8 halamanComparison Study of Fractional Carbon Dioxide Laser Resurfacing Using Different Fluences and Densities For Acne Scars in AsiansdoctorbanBelum ada peringkat
- Combined Vestibular Mucosal Advancement and Island Pedicle Flaps For The Repair of A Defect Involving The Cutaneous and Vermilion Upper LipDokumen4 halamanCombined Vestibular Mucosal Advancement and Island Pedicle Flaps For The Repair of A Defect Involving The Cutaneous and Vermilion Upper LipdoctorbanBelum ada peringkat
- Are There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemDokumen8 halamanAre There Differences Between The Upper and Lower Parts of The Superficial Musculoaponeurotic SystemdoctorbanBelum ada peringkat
- You Have Full Text Access To This ContentTransient Median and Ulnar Neuropathy Associated With A Microwave Device For Treating Axillary HyperhidrosisDokumen4 halamanYou Have Full Text Access To This ContentTransient Median and Ulnar Neuropathy Associated With A Microwave Device For Treating Axillary HyperhidrosisdoctorbanBelum ada peringkat
- Aging BlepharoplastyDokumen6 halamanAging BlepharoplastydrbantmBelum ada peringkat
- A Simple, Reliable, and Validated Method For Measuring Brow Position.Dokumen5 halamanA Simple, Reliable, and Validated Method For Measuring Brow Position.doctorbanBelum ada peringkat
- The Ulnar Palmar Perforator FlapDokumen7 halamanThe Ulnar Palmar Perforator FlapdoctorbanBelum ada peringkat
- Overlooked Complication ofDokumen9 halamanOverlooked Complication ofdoctorbanBelum ada peringkat
- You Have Full Text Access To This ContentMultimodal Keloid Therapy With Excision, Application of Mitomycin C, and RadiotherapDokumen3 halamanYou Have Full Text Access To This ContentMultimodal Keloid Therapy With Excision, Application of Mitomycin C, and RadiotherapdoctorbanBelum ada peringkat
- The Open Brow LiftDokumen8 halamanThe Open Brow LiftdoctorbanBelum ada peringkat
- Bilobed Flap For Reconstruction of Small Alar Rim DefectsDokumen4 halamanBilobed Flap For Reconstruction of Small Alar Rim DefectsdoctorbanBelum ada peringkat
- Mechanical Analysis of Eyelid MorphologyDokumen9 halamanMechanical Analysis of Eyelid MorphologydoctorbanBelum ada peringkat
- Overlooked Complication ofDokumen9 halamanOverlooked Complication ofdoctorbanBelum ada peringkat
- Community Health Nursing Bag Technique PDFDokumen2 halamanCommunity Health Nursing Bag Technique PDFRachael50% (2)
- Service Delivary Organization Realignment: A Message From Karen Herd, Deputy Minister of Manitoba Health, Seniors and Active LivingDokumen4 halamanService Delivary Organization Realignment: A Message From Karen Herd, Deputy Minister of Manitoba Health, Seniors and Active LivingmatthewtrevithickBelum ada peringkat
- Clinical Trial Transparency - A Key To Better and Safer Medicines (Till Bruckner and Beth Ellis 2017)Dokumen21 halamanClinical Trial Transparency - A Key To Better and Safer Medicines (Till Bruckner and Beth Ellis 2017)Till BrucknerBelum ada peringkat
- Practical Standard Prescriber, 7th EditionDokumen505 halamanPractical Standard Prescriber, 7th EditionTonyScaria60% (5)
- What Is Sonography? What Does A Diagnostic Medical Sonographer Do? What Are The Career Opportunities?Dokumen2 halamanWhat Is Sonography? What Does A Diagnostic Medical Sonographer Do? What Are The Career Opportunities?yogimgurtBelum ada peringkat
- Healing TouchDokumen6 halamanHealing TouchDelia Do Rosario100% (1)
- Finalized ResumeDokumen3 halamanFinalized Resumeapi-510470035Belum ada peringkat
- Emergency Protocol ProcedureDokumen14 halamanEmergency Protocol Procedurejmmos207064Belum ada peringkat
- Nclex-Rn Essential Questions and RationalesDokumen96 halamanNclex-Rn Essential Questions and RationalesGloryJane100% (1)
- Latisha Kelly Resume AssignmentDokumen3 halamanLatisha Kelly Resume Assignmentapi-324927307Belum ada peringkat
- Somalia Launches First Ever-Cleft Lip and Palate Surgery ClinicDokumen4 halamanSomalia Launches First Ever-Cleft Lip and Palate Surgery ClinicAMISOM Public Information ServicesBelum ada peringkat
- IsosorbideDokumen2 halamanIsosorbideSBelum ada peringkat
- Comfort Room PDFDokumen1 halamanComfort Room PDFPixaaaBelum ada peringkat
- Know Your Magnetic FieldDokumen75 halamanKnow Your Magnetic FieldAtma Jnani100% (5)
- Basic ECGDokumen152 halamanBasic ECGTuấn Thanh VõBelum ada peringkat
- Liver Function TestDokumen20 halamanLiver Function TestAvi VermaBelum ada peringkat
- Manual of Basic Techniques For A Health Laboratory (Part1) - WHODokumen114 halamanManual of Basic Techniques For A Health Laboratory (Part1) - WHOcholinchuchuBelum ada peringkat
- Nursing Care Plan Breast-CancerDokumen2 halamanNursing Care Plan Breast-CancerGreg Llandelar100% (2)
- Flap HemisoleusDokumen6 halamanFlap HemisoleuscweetblueBelum ada peringkat
- Healthcare System and Reforms in The United States Revised Essay 3Dokumen4 halamanHealthcare System and Reforms in The United States Revised Essay 3api-272097622Belum ada peringkat
- MEdical Surgical REVEWERDokumen86 halamanMEdical Surgical REVEWERennaedBelum ada peringkat
- Infants and Children - Pediatric EmergenciesDokumen27 halamanInfants and Children - Pediatric EmergenciesIlmiah BagusBelum ada peringkat
- CV 2017 VirginiaDokumen4 halamanCV 2017 Virginiaapi-353693776Belum ada peringkat
- FTHHHDokumen17 halamanFTHHHSaad khanBelum ada peringkat
- Final Past Papers With Common MCQS: MedicineDokumen17 halamanFinal Past Papers With Common MCQS: MedicineKasun PereraBelum ada peringkat
- Fingertips Injury: Literature ReviewDokumen24 halamanFingertips Injury: Literature ReviewDonny Artya KesumaBelum ada peringkat
- Ebp PaperDokumen8 halamanEbp Paperapi-250304529Belum ada peringkat
- Hyper Parathyroid IsmDokumen7 halamanHyper Parathyroid IsmEllene Mae Dejapa VillasisBelum ada peringkat
- Guidelines For Prescribing EyeglassesDokumen18 halamanGuidelines For Prescribing Eyeglassesratujelita100% (1)
- Anticoagulants 2019Dokumen11 halamanAnticoagulants 2019Srijan VermaBelum ada peringkat