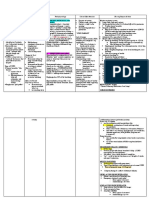
Assessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: Independent
Diunggah oleh
Abdullah Mascardo BarabagDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Assessment Scientific Basis Plan of Care Intervention With Rationale Evaluation Subjective: Independent
Diunggah oleh
Abdullah Mascardo BarabagHak Cipta:
Format Tersedia
ASSESSMENT SUBJECTIVE: As verbalized by the pt SO: nagalisod man ug ginhawa ang ako baby.
SCIENTIFIC BASIS Preterm infants have great difficulty initiating respirations at birth because pulmonary capillaries are still so immature. Lung surfactant does not form in adequate amounts until about 34th to 35th week of pregnancy. Inadequate lung surfactant leads to alveolar collapse with each expiration. This condition forces an infant to use maximum strength to inflate lung alveoli each time.
PLAN OF CARE After 8hrs of nursing intervention: patient will be able to meet the exact amount of oxygen needed.
INTERVENTION WITH RATIONALE INDEPENDENT: 1. Assessed respiratory status, noting signs of respiratory distress (e.g., tachypnea, nasal flaring, grunting, retractions, rhonchi, or crackles). Tachypnea indicates respiratory distress esp when respi are >75cpm/min after the first 5 hours of life. Expiratory grunting represents attempt to maintain alveolar expansion; nasal flaring is a compensatory mechanism to increase diameter of nares & increase Oxygen intake.
EVALUATION Goal met. As evidence by patient manifests normal sign of breathing. Oxygen Saturation 100% RR= 54
OBJECTIVE: - Dyspnea noted - RR= 64 -rapid, equal chest expansion Oxygen Saturation: 98% Nursing Diagnosis: Impaired Gas exchange r/t immature pulmonary functioning.
2. Assessed skin color
for devt of cyanosis. Lack of Oxygen will result in cyanosis.
3. Promoted rest, minimize stimulation & energy expenditure. To decrease the metabolic rate & Oxygen consumption. *COLLABORATIVE: 1. Monitored lab/diagnostic studies as appropriate. Reveals & prevents any further complications.
ASSESSMENT SUBJECTIVE:
SCIENTIFIC BASIS
Babies born before 34 weeks often can't feed Wala pa na siya'y from a bottle or breast kaon , as pt SO because they have stated.. trouble coordinating sucking, breathing, and swallowing. Also, newborns with breathing problems, OBJECTIVE: very low oxygen levels, gagging, -found patient lying on circulatory problems, bed supine with IV blood infection, or D5IMB 500 other illnesses might -small for gestational not be able to feed age. through a nipple (orally). Preterm babies lose more Nursing Diagnosis: water through the skin or respiratory tract Altered nutrition: less than babies born at than body full term. Also, the requirements r/t to kidneys in a small stomach premature baby have capacity & prematurity not grown enough to as evidenced by weak control water levels in feeding reflexes & the body. Such babies NPO status. can become dehydrated or
INTERVENTION WITH RATIONALE After 24hrs of INDEPENDENT: continuous nursing 1. Assessed presence intervention, pt will of reflexes associated demonstrate steady wt with feeding (i.e gain in a normal curve swallowing, sucking & (@ least 20-30g/day) coughing). and also maintained growth. Determines the appropriate feeding method for the infant. 2. Initiated intermittent or tube feedings as indicted. Gavage feedings may be necessary to provide adequate nutrition in infant who has a poorly coordinated suck-andswallow reflex or who becomes fatigued during oral feedings. 3. Positioned infant on right side or prone with HOB elevated @ 30 degrees.
PLAN OF CARE
EVALUATION After 24hrs,pt was seen beside mother, exhibiting good suckand-swallow reflex. Child will exhibit no further weight loss and, if malnourished, will gain 2.2 lb (1 kg) per week. Goal met.
overhydrated. The NICU team keeps track of how much premature babies urinate (by weighing their diapers) to make sure that their fluid intake and urine output are balanced. Blood tests are also done to monitor electrolyte levels.
Facilitates gastric emptying & prevents reflux. COLLABORATIVE: 1. Feed as frequently as indicated based on infants weight & estimated stomach capacity. Infants <1250g are usually fed q 2hrs; infants b/w 1500 & 1800g are fed q 3hrs.
2. Administered supplemental vitamins & minerals, esp Vit A, B, C, D, & E and Iron as prescribed. Replaces low nutrient stores to promote adequate nutrition & reduce risk on infection
ASSESSMENT Subjective: N/A Objective: Gestational age of 33 weeks. Current weight: 1.85 kgs Neurological status: LOC: Lethargic Capillary refill time of 3 seconds. Integumentary Status: pale legs, Moderate pallor cool and dry skin neonate is placed in the isolation room Temperature: 35.5 C Baby is placed in an extended position Poor muscle tone
SCIENTIFIC BASIS The preterm newborn has a great deal of difficulty attaining body temperature because she has a relatively large surface area per kilogram of body weight. In addition, because the infant does not flex the body well but remains in an extended position. Rapid cooling from evaporation is likely to occur. The preterm infant has little subcutaneous fat for insulation and poor muscular development does not allow the child to move actively as the older infant does to promote heat. The preterm infant
PLAN OF CARE After 1 hour of nursing intervention, patient will maintain normal body temperature from 36.5-37.5 1. Staff members will take steps to maintain neonates body temperature at normal level. Pt. will have a and warm, dry skin
INTERVENTION WITH RATIONALE INDEPENDENT: Monitored the neonates body temperature until discharge To determine the need for intervention and the effectiveness of therapy.
EVALUATION After 1 hour of intervention, the goal is fully met. The neonate maintained a stable body temperature at 36 .7C evidenced by: 1. staff members kept neonates body temperature at normal level. neonate has warm, dry skin
Dried the newborn thoroughly and quickly and discard the wet blanket. Place the infant under a pre warmed radiant warmer. Drying quickly and placing and placing
Nursing Diagnosis: Ineffective thermoregulation related to immaturity and lack of subcutaneous and brown fat.
also has limited amount of brown fat; special tissue present in newborns to maintain body temperature. Source: Maternal and Child Health Nursing, 4th Ed. By Pillitteri, p.741
on a warm, dry surface prevent heat loss from evaporation. Avoided placing infant on cold surface or using cold instrument in assessment. Cold surface and instrument increase heat loss by conduction Provided Ambient temperature of the room where the newborn is kept should be monitored To prevent excessive cooling Mummified and used thick blankets to cover the patient. Helps conserve heat in the body
2. parents will express understanding of neonates thermoregulatory disturbance and thermoregulation
2. parents expressed understanding of neonates thermoregulatory disturbance and thermoregulation
Teach the mother about the infants need for warmth and to keep the infants head covered The infants head provides a large surface area for heat loss
Taught family members about: Signs and symptoms of altered body temperature, such as cool extremities. Factors in home that contribute to neonatal heat loss and ways to minimize heat loss. Importance of contacting a health care provider when problems related to temp regulation. Careful teaching allows family members to take an
active role in maintaining the neonates health
ASSESSMENT Subjective: n/a since a potential diagnosis Objective: -patient is diagnosed with neonatal sepsis upon admission -RR; 58 cycles/min -HR: 148 bpm
SCIENTIFIC BASIS The newborns immune system is not fully activated until some time after birth. Limitation in the newborns inflammatory response result in failure to recognize, localize, and destroy invasive bacteria thus, increasing risk for infection.
PLAN OF CARE After 8 hours of nursing interventions the infant will not experience spread of infection as manifested by Infants HR remains <160 bpm RR is <60 cycles/ min
INTERVENTION WITH RATIONALE INDEPENDENT: (1) Ensured that all people coming in contact with infant wash their hands well before & after touching the baby. hand washing prevents the spread of pathogens coming from the infant to the caregiver and vice versa (2) Ensure that all
EVALUATION After 8 hours of nursing interventions, the goal is fully met. The infant did not experienced spread of infection as manifested by Infants HR remained <160 bpm RR was <60 cycles/ min
Nursing Diagnosis: Risk for infection r/t spread of pathogens secondary to identified
sepsis and immature immune system
Source: Ladewig et al. Contemporary Maternal-Newborn Nursing care 6th ed. P. 580
equipment used for infant is sterile, scrupulously clean & disposable. Do not share equipment with other infants This would prevent the spread of pathogens to the infant from equipment (3) Placed infant in isolate/ isolation room per hospital policy Placing the infant in an isolette allows close observation of the ill neonate & protects other infants from infection
(4) Maintained neutral thermal environment A neutral thermal environment decreases the metabolic needs of the
infant. The ill neonate has difficulty maintaining a stable temp.
(5) Assessed TPR & BP, auscultate breath sounds Assessments provide information about the spread of infection, increased RR and HR, decreased BP are signs of sepsis. Spread of infection may cause resp. distress
(6) Provided respiratory support (oxyhood)
Respiratory support may be needed during the acute phase of the infection to prevent additional physiological stress
(7) Feed infant as ordered. Nutritional needs may increase during infection while the infant may feed poorly. OG feedings ensure that nutrient needs are met if the infant is too ill to suck effectively
(8) Monitored lab results as obtained.
Notify care giver of abnormal findings Lab results provide information about the pathogen and infants response to illness and treatment
(9) Monitored infant for hypoglycemia, jaundice, development of thrush, or signs of bleeding. Assessments coagulationprovide information about the development of complications of infection: hypoglycemia, hyperbilirubenia, opportunistic infections, and coagulation deficits
Collaborative: (10) administer IV fluids as ordered (D5IMB) -IV fluidsnhelp maintain fluid balance (11) administer antibiotics as ordered - antibiotics act to inhibit the growth of bacteria and destruction of bacteria.
ASSESSMENT Subjective: N/A Objective: Patient is on phototherapy for 3 days Dry skin Patient in supine position Has no clothes on during phototherapy, only mittens, socks, and diapers. Nursing Diagnosis: Risk for Impaired skin integrity related to exposure to high intensity light secondary to phototherapy
SCIENTIFIC BASIS The newborn lies in one position for a long period of time that may result in skin breakdown. Due to lack of adipose tissue, the pressure exerted by bony prominences on the skin is greater thus increases the risk of skin breakdown. Source: Ladewig et al. Contemporary Maternal-Newborn Nursing care 6th ed. P763
PLAN OF CARE After 8 hours of nursing intervention 1. Patients skin will remain intact
INTERVENTION WITH RATIONALE INDEPENDENT: Changed position every 2 hours Patient position changes will allow exposure of the phototherapy lights to all areas of the body that are uncovered. Pressure areas may develop if newborn lies in one position for an extended period of time.
EVALUATION After 8 hours of nursing intervention, goal is fully met. Patients skin remained intact as evidenced by: No signs of skin breakdown
No signs of skin breakdown
Monitored skin for rashes and bronzing every 8 hours. Patient may develop a maculopapular rash which is transient side effect of
phototherapy Inspected perianal area after each diaper change for signs of breakdown Newborns under phototherapy lights have increased loose green acidic stools which can be irritating to the skin. The diaper area should be thoroughly cleaned after each soiled diaper to prevent skin breakdown
Avoided using lotions or ointments on the newborns skin Lotions and ointments may cause skin to burn if applied to exposed areas during phototherapy.
Anda mungkin juga menyukai
- Cassette-Clinics OF Obstetrics & Gynaecology: Asetof 9 Case Presentations (Mp3 CD) and A BookletDokumen27 halamanCassette-Clinics OF Obstetrics & Gynaecology: Asetof 9 Case Presentations (Mp3 CD) and A BookletChaitanya Ghule100% (2)
- Focused AssessmentDokumen5 halamanFocused AssessmentPiyali SahaBelum ada peringkat
- Nurse Compentency ChecklistDokumen17 halamanNurse Compentency ChecklistMary ElizabethBelum ada peringkat
- Dr. Reckeweg Reference Guide - United RemediesDokumen4 halamanDr. Reckeweg Reference Guide - United RemediesshubhamformeBelum ada peringkat
- Clinical Exercise, ZeballosDokumen339 halamanClinical Exercise, ZeballosJavier Ivan Lasso ApraezBelum ada peringkat
- Textbooks of Pulmonary RehabilitationDokumen383 halamanTextbooks of Pulmonary RehabilitationMaghiar Ioana67% (3)
- Pneumonia AlgorithmDokumen3 halamanPneumonia AlgorithmBien ChuBelum ada peringkat
- Neonatal Danger SignsDokumen6 halamanNeonatal Danger Signsmarkus_danusantosoBelum ada peringkat
- Step 2Dokumen64 halamanStep 2Irfan MajeedBelum ada peringkat
- Care of Iugr and Low Birth Weight BabiesDokumen30 halamanCare of Iugr and Low Birth Weight BabiesjessyBelum ada peringkat
- The Pearls For NCLEX Review in Publisher March PDFDokumen34 halamanThe Pearls For NCLEX Review in Publisher March PDFKim Medairos100% (3)
- Newborn CareDokumen120 halamanNewborn Carejuly3ciaBelum ada peringkat
- Newborn CareDokumen120 halamanNewborn CareMike CalipayanBelum ada peringkat
- Checklist For Student Newborn CareDokumen7 halamanChecklist For Student Newborn CarePrecious SorianoBelum ada peringkat
- NCP NewbornDokumen21 halamanNCP NewbornGil Aswigui81% (27)
- Newborn CareDokumen51 halamanNewborn CareHurley ReefBelum ada peringkat
- Neonatal ResuscitationDokumen15 halamanNeonatal Resuscitationpriyanka88% (8)
- New Born Care 1Dokumen12 halamanNew Born Care 1Tsuyoshi BangBelum ada peringkat
- Neonatal Resuscitation: Vineetha.T 1 Year MSC NursingDokumen106 halamanNeonatal Resuscitation: Vineetha.T 1 Year MSC NursingVineetha ThachedathBelum ada peringkat
- Sample Patient HistoryDokumen2 halamanSample Patient HistoryRojan Cardinal100% (1)
- Adult Health Nursing McqsDokumen27 halamanAdult Health Nursing McqsMuhammad Zeeshan100% (1)
- Drug StudyDokumen13 halamanDrug StudyAbdullah Mascardo BarabagBelum ada peringkat
- Nursing Care PlanDokumen7 halamanNursing Care PlanDaniel Marcos80% (10)
- Evaluation, Tests and Measures in Physical TherapyDokumen339 halamanEvaluation, Tests and Measures in Physical TherapywanderlastBelum ada peringkat
- Care NewbornDokumen38 halamanCare NewbornRaja0% (1)
- Pulmonary EosinophiliaDokumen19 halamanPulmonary EosinophiliaOlga GoryachevaBelum ada peringkat
- High Risk NewbornDokumen19 halamanHigh Risk Newbornsantosh s u100% (1)
- Baby at Risk (NBU) NotesDokumen131 halamanBaby at Risk (NBU) NotesMercy KeruboBelum ada peringkat
- Seminar ON Incubator Care: Maa Tripura College of Nursing, Jhabua (M.P.)Dokumen5 halamanSeminar ON Incubator Care: Maa Tripura College of Nursing, Jhabua (M.P.)amitBelum ada peringkat
- High Risk NeonateDokumen102 halamanHigh Risk NeonateJaya Prabha100% (2)
- Neonatal ResuscitationDokumen16 halamanNeonatal ResuscitationPrecilla C. Stephen100% (3)
- ScabiesDokumen15 halamanScabiesAbdullah Mascardo BarabagBelum ada peringkat
- Low Birth Weight NoteDokumen9 halamanLow Birth Weight Notesushma shrestha100% (1)
- Nursing Health Assessment Practice QuestionsDokumen22 halamanNursing Health Assessment Practice QuestionsSraddha PatelBelum ada peringkat
- Newborn ResuscitationDokumen34 halamanNewborn ResuscitationVarna MohanBelum ada peringkat
- Newborn Adaptation FinalDokumen28 halamanNewborn Adaptation Finalsanthiyasandy91% (11)
- Nursing Care of The High - Risk Newborn To 2018Dokumen325 halamanNursing Care of The High - Risk Newborn To 2018Keane Andal67% (3)
- New Born CareDokumen17 halamanNew Born CareHarrison Tallod100% (1)
- MCNDokumen12 halamanMCNIan CarodanBelum ada peringkat
- Newborn Lecture HandoutDokumen57 halamanNewborn Lecture HandoutChesca LayosaBelum ada peringkat
- Nursing Diagnosis Rationale Goals/ Objectives Nursing Interventions Rationale EvaluationDokumen20 halamanNursing Diagnosis Rationale Goals/ Objectives Nursing Interventions Rationale EvaluationElaine Grace Timbol-Babasa100% (1)
- NB Nursing DiagnosisDokumen2 halamanNB Nursing Diagnosisnursingmvd92% (13)
- SgaDokumen4 halamanSgaLovely Princess Balaba ToraynoBelum ada peringkat
- MCN FinalsDokumen40 halamanMCN Finalsmolderoirish600Belum ada peringkat
- Care of The Newborn PDFDokumen5 halamanCare of The Newborn PDFzhai bambalan100% (2)
- Week 9 NCM 109 LectureDokumen63 halamanWeek 9 NCM 109 LecturePolicarpio AprilBelum ada peringkat
- Baby at Risk - Koros E.k-1-1-1-1Dokumen132 halamanBaby at Risk - Koros E.k-1-1-1-1victorBelum ada peringkat
- Immediate Care of The New Born: ObjectivesDokumen127 halamanImmediate Care of The New Born: ObjectivesSwati SharmaBelum ada peringkat
- Reproductive Nursing System: Neonatus (In 6 Hours, 6 Hour) Nursing Care Plan + WOC (Pathophysiology + Nursing Problem)Dokumen11 halamanReproductive Nursing System: Neonatus (In 6 Hours, 6 Hour) Nursing Care Plan + WOC (Pathophysiology + Nursing Problem)Nofri YanTiBelum ada peringkat
- 10 Newborn1Dokumen129 halaman10 Newborn1Gerlian Kyle QueridoBelum ada peringkat
- Post Mature Newborn: Gervacio, Jonah Micah NDokumen20 halamanPost Mature Newborn: Gervacio, Jonah Micah NJessa BorreBelum ada peringkat
- Managing Birth Asphyxia August 2022Dokumen21 halamanManaging Birth Asphyxia August 2022f.abrahamBelum ada peringkat
- LatePretermGuidelines Phillips ResArt 2013 PDFDokumen18 halamanLatePretermGuidelines Phillips ResArt 2013 PDFTia Amalia Puti RenaeryBelum ada peringkat
- Pedia 2Dokumen30 halamanPedia 2regBelum ada peringkat
- Conclusion 4.1. Summary: TH THDokumen3 halamanConclusion 4.1. Summary: TH THhengkihanggaraBelum ada peringkat
- Case StudyDokumen7 halamanCase StudyCaren MarquezBelum ada peringkat
- High-Risk Newborn: Complications Associated With Gestational Age and DevelopmentDokumen97 halamanHigh-Risk Newborn: Complications Associated With Gestational Age and DevelopmentALYSSA NICOLE GINESBelum ada peringkat
- Review UNIT XI High Risk NewbornDokumen20 halamanReview UNIT XI High Risk NewbornShehana ShihabBelum ada peringkat
- Care of The NewbornDokumen19 halamanCare of The NewbornAnivasa KabirBelum ada peringkat
- High RiskDokumen52 halamanHigh Riskmounika ChittempallyBelum ada peringkat
- Presentation Resuscitation - Power PointDokumen45 halamanPresentation Resuscitation - Power PointRouquia ManzoorBelum ada peringkat
- My Paediatric NotesDokumen14 halamanMy Paediatric NotesTicky TomBelum ada peringkat
- Initiating and Maintaining RespirationsDokumen2 halamanInitiating and Maintaining Respirationsitsjamyca najorraBelum ada peringkat
- B Hand Out Care of High Risk NewbornDokumen4 halamanB Hand Out Care of High Risk NewbornLecery Sophia WongBelum ada peringkat
- The NeonatesDokumen117 halamanThe NeonatesAirene AalaBelum ada peringkat
- Seminar On - Essential and Immediate Newborn CareDokumen26 halamanSeminar On - Essential and Immediate Newborn CareJyothi Singh SuryavanshiBelum ada peringkat
- Newborn SeminarDokumen43 halamanNewborn SeminarRawat PragatiBelum ada peringkat
- High Risk NewbornDokumen83 halamanHigh Risk NewbornChari RivoBelum ada peringkat
- 2022LP4Dokumen15 halaman2022LP4Alyssa DagandanBelum ada peringkat
- Neonatal ResuscitationDokumen51 halamanNeonatal ResuscitationAbdulkadir HasanBelum ada peringkat
- New Born Care 1Dokumen12 halamanNew Born Care 1gilbertgarciaBelum ada peringkat
- Activity 4 NCM 109Dokumen10 halamanActivity 4 NCM 109Angelica BernalesBelum ada peringkat
- Normal Newborn CareDokumen21 halamanNormal Newborn CareRinothja RajaratnamBelum ada peringkat
- Birth AsphyxiaDokumen10 halamanBirth Asphyxiasarita Singh MaharjanBelum ada peringkat
- Mental StatusDokumen8 halamanMental StatusAbdullah Mascardo BarabagBelum ada peringkat
- Nursing Care Plan For Mentally ChallengeDokumen2 halamanNursing Care Plan For Mentally ChallengeAbdullah Mascardo Barabag0% (1)
- Eliminate Symptoms of Food AllergiesDokumen2 halamanEliminate Symptoms of Food AllergiesAbdullah Mascardo BarabagBelum ada peringkat
- Common Medical AbbreviationDokumen25 halamanCommon Medical AbbreviationKim Glaidyl BontuyanBelum ada peringkat
- Sir ClanDokumen109 halamanSir ClanJames AbendanBelum ada peringkat
- Preoperative EvaluationDokumen7 halamanPreoperative EvaluationPiny Elleine CesarBelum ada peringkat
- Leoprolide Drug StudyDokumen2 halamanLeoprolide Drug Studyhappymee927Belum ada peringkat
- ACPICR Standards 2015Dokumen94 halamanACPICR Standards 2015Irene Chrysovalanto Themistocleous50% (2)
- Alterations in VentilationDokumen10 halamanAlterations in VentilationCharisma Pastor100% (1)
- NCM 112 EvalDokumen16 halamanNCM 112 EvalMartin T ManuelBelum ada peringkat
- MBF7823423Dokumen425 halamanMBF7823423Pete PetersBelum ada peringkat
- Emergency Chest ImagingDokumen156 halamanEmergency Chest ImagingAshutosh KafleBelum ada peringkat
- Blood TransfusionDokumen41 halamanBlood TransfusionajBelum ada peringkat
- Nursing Care Plan HF FinalDokumen10 halamanNursing Care Plan HF FinalCristina L. JaysonBelum ada peringkat
- Leopando Hospice-Palliative3Dokumen2 halamanLeopando Hospice-Palliative3Judy Ignacio EclarinoBelum ada peringkat
- Nursing Management of Patient With Community Acquired PneumoniaDokumen5 halamanNursing Management of Patient With Community Acquired PneumoniaSummer SuarezBelum ada peringkat
- Princess NCP COPDDokumen3 halamanPrincess NCP COPDPrincess Faniega SugatonBelum ada peringkat
- COPD Guideline Ver 1.8Dokumen9 halamanCOPD Guideline Ver 1.8Dina AyupnBelum ada peringkat
- Chest Pain / Discomfort: DR (Brig) YD Singh Prof & Head Unit of MedicineDokumen36 halamanChest Pain / Discomfort: DR (Brig) YD Singh Prof & Head Unit of MedicinenarmaBelum ada peringkat