Salmonellasis Typhoid Fever Campylobacter Jejuni Yersinosis Shigellosis
Diunggah oleh
Farhana Azmira AsmadiDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Salmonellasis Typhoid Fever Campylobacter Jejuni Yersinosis Shigellosis
Diunggah oleh
Farhana Azmira AsmadiHak Cipta:
Format Tersedia
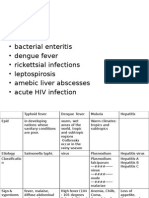
Symptoms
Diarrhoea fever headache
diarrhoea Fever
Diarrhoea
abdominal pain, vomiting,
tender abdomen
malaise, cramping
bloody abdominal pain
tenesmus, cramps, blood & mucous in stools Inflammation of ileum and colon Ulceration of intestine
Diseases/M icrobe
Salmonellasis
Typhoid fever
Campylobacter jejuni
Yersinosis
Shigellosis
S.enteritidis
Salmonella Typhi
Campylobacter jejuni
Yersinia enterocolytica
S. dysenteriae (Most severe) S. flexneri (less sever) S. sonnei (common,mild) S. boydii (rare) Reservoir humans Does not survive in the environment Faecal/ oral route Person to person Enrichment: selenite or gram negative (GN) broth Plate: MAC, XLD, Salmonella-Shigella agar, TSI & SIM Non-lactose fermenting, alkaline colonies Confirmation: biochemical or serological tests
Causes
poultry, eggs, cheese
faecal/oral route Faulty sewage systems
Contaminated meat especially raw or undercook pork products or unpasteurized milk
Sources
Culture: blood, bone-marrow or stool Enrichment: selenite broth Media Culture: XLD and BSA Confirmation: Biochemical tests
Culture: blood, bone-marrow or stool Enrichment: selenite broth Media Culture: XLD and BSA, Salmonella-Shigella agar, TSI & SIM Confirmation: Biochemical tests Antibody detection: Widal Test Main: Ceftriaxone Alternatives: Ampicillin, Chloramphenicol.
Laboratory Identification
Microaerophilic environment o (~5% O2), 42 C, Skirrows medium
best and motile at 25 C Confirmation: biochemical tests or serology
Treatment
Unnecessary, self-limiting
Aminglycosides, trimethoprim, cephalosporins
Ampicillin, chloramphenicol, trimethoprimare
Symptoms
diarrhoea Can overgrow when patient is on broadspectrum antibiotics Often severe
diarrhea Nausea and explosive vomiting Begins 1-6 hours after ingestion Nausea and vomiting begin 1 to 5 hours after the contaminated food is eaten Duration: 6-24 hours
Watery diarrhea and abdominal pain 8-16 hours of incubation, after consumption of contaminated food Duration 12-24 hrs
diarrhoea Abdominal pains, cramps,
-12 hours after ingestion-severe diarrhea, abdominal cramps-loss fluid and electrolyte-intestinal epithelial damage caused by desquamation of epithelial cells at villustips -self-limiting
Bacteria/d iseases Causes
Clostridium difficile
Staphylococcal Food Poisoning S. aureus Normal flora, creams, tarts, custard processed food where competing bacteria are inhibited (ham)
Bacillus cereus (Vomiting syndrome)
Bacillus cereus (Diarrheal type)
Clostridium perfringens
B. cereus Boiled rice that is held Meat for prolonged period at vegetable dishes, ambient temperature sauces, and then quick-fried pasta, before serving desserts Dairy products dairy products Pasta Culture: Sheep Blood Agar -hemolytic frost-glass colonies Gram stain: long rods Spore stain positive Motile
Clostridium perfringens meat, stew etc
Sources
S. aureusis often undetectable (killed off during cooking) Latex agglutination test for enterotoxin Ironically treatment is by Metronidazole, vancomycin Possible newer therapy includes a probioticmilkshake containing L. bulgaricus, L. caseiand S. thermophilusto prevent diarrhea
Laboratory Identification
Nagleragar (egg yolk media) anaerobically Blood Agar: Beta-haemolytic
Treatment
Replace fluids & electrolytes Recovery usually in 24 hours
Unnecessary Self-limiting
intensive supportive (respiratory)
progressive muscle weakness flaccid paralysis Neurological symptoms: blurred vision-speech difficulties-descending flaccid paralysis
Symptoms
Weakness, dizziness, dryness of mouth, nausea, vomiting
Profuse diarrhea rice-water stools
2-48 hrs after ingestion (average 12 hours) abrupt severe (bloody) diarrhea with cramps
Abortions Meningitis Septicaemia
Bacteria/diseases Causes
Clostridium botulinum
Botulism
Cholera Vibrio cholerae
Vibrio parahaemolyticus
Listeriosis Listeria monocytogenes raw foods, such as uncooked meats, raw milk and vegetables, soft cheeses Pregnant women should avoid high risk foods such as pates, soft cheeses, unpasteurised dairy products and uncooked seafood. on HBA, -hemolytic, small white colonies-highly motileCAMP test, but smaller lysis zone
home preserved, alkaline food or commercial canning failures
Sources
spores in soils (and honey)
Faecal contamination of water or food
Food poisoning from sea food
Anaerobic culture Cooked meat media -10 days Non-hemolytic on blood agar Toxin: radioimmunoassay, ELISA
Fecal gram stain presumptive Enrichment: alkaline peptone water Plate: TBCS agar - yellow colonies Identification: serology Fluids and electrolytes -very important! Tetracycline may be given Reports of resistance
Treatment
Laboratory Identification
Differentiated from V. cholera green colonies on TCBS-needs NaClto grow
Diarrhoea ranging from mild to severe
Diarrhoea
Moderate to severe watery diarrhea
Symptoms
Inflammation of mucous layer of the stomach duodenal ulcers
Amoebic dysentery: mucous, pus and blood in faeces Complication Perforated intestine leading to peritonitis Trophozoite travels in blood to liver & forms abscess
abdominal cramps, nausea, vomiting, flatulence, greasy stools
May also have nausea, vomiting, abdominal cramps and lowgrade fever
Asymptomatic or vague intestinal discomfort
Usually self-limiting
Bacteria/d iseases
Helicobacter Pylori
Amoebic Dysentry
Giardasis
Cryptospridosis
Tapeworm Infestation
Causes
Entamoeba histolytica
Giardia Lamblia
Cryptosporidium parvum carried by man and other warmblooded animals fecal-oral; water contaminated with human or cattle feces
Taenia solium Taenia saginata
Cysts digested in food or water Sometimes also through anal sex
Food Water
Taenia solium (undercooked pork) Taenia saginata (undecooked beef)
Sources
Biopsy (clotest) breath test antibodies Microaerophillic, Skirrowsmedium, CHA, 37C for 3-6 days Amoxicillin, clarithromycin
Laboratory Identification
Microscopic examination: Four-nucleate cyst in stool Series of samples collected: differentiate from nonpathogenic species such as Entamoebacoli Metronidazole
Examination of stools for cysts
Examination of faecesfor oocysts Detected by floatation and acid-fast stain PCR Not treated unless patient is immunocompromised Spiramycincan be used
Examination of faeces for scolices
Treatme nt
Metronidazole, tinidazole Mepacrine hydrochloride
Niclosamide, praziquantel
Symptoms
Cysts
Itching
Intestinal bleeding anaemia& lethargy
Abdominal infection Pulmonary symptoms
Vomiting and diarrhoeafor 4-7 days Large number of virionsshed in faeces Cough and coryzaare quite common Rotavirus
Diarrheal disease Damages mucosa of small intestine
Bacteria/ diseases
Hydatid diseases (Tapeworm) Echinococcus granulosis
Nematode Infestation (pinworm) Enterobius vermicularis
Causes
Eggs in feces Cysts in organs
Pinworm Via contaminated fingers
Worm Infection (Hookworms & roundworms) Hookworm: Ancylostoma duodenale & Necator americanus Roundworm: Trichuris Hookworm: Soil-transmitted helminth: Infect by active skin penetration by infective larvae transmitted primarily by walking barefoot on contaminated soil. ingestion of larvae. Roundworm: undercooked pork
Ascariasis
Norovirus
Ascaris lumbricoides
Reovirusfamily
Caliciviridaefamily
undigested food
Faecal-oral route food & water, direct contact
Faecal-oral route E.g. shell-fish harvested from polluted water
Sources
Laboratory Identification
Examination of stools for adult pinworms microscopic examination for eggs Cysts must be surgically removed Pyrantelpamoate, mebendazole Medendazole Mebeddazole
Electron microscopy of faeces ELISA for viral antigen Fluid and electrolyte replacement essential Vaccines in trial
Electron microscopy of faeces ELISA
Treatment
Anda mungkin juga menyukai
- Ricardo A. Caicedo, MD: Pediatric Gastroenterology University of FloridaDokumen20 halamanRicardo A. Caicedo, MD: Pediatric Gastroenterology University of FloridaAsma SikanderBelum ada peringkat
- Lab Diagnosis of Diarrheal DiseasesDokumen37 halamanLab Diagnosis of Diarrheal DiseasesGIST (Gujarat Institute of Science & Technology)Belum ada peringkat
- Enterobacteriaceae - Non Lactose Fermenters - La 2020Dokumen111 halamanEnterobacteriaceae - Non Lactose Fermenters - La 2020GiselleBelum ada peringkat
- 1 Approach To DiarrheaDokumen37 halaman1 Approach To DiarrheamusabBelum ada peringkat
- Acute GastroenteritisDokumen39 halamanAcute Gastroenteritisslicvic169Belum ada peringkat
- Dirrhoea Dysentery & Food PoisoningDokumen17 halamanDirrhoea Dysentery & Food PoisoningAbcdefg HijklBelum ada peringkat
- Stool ExaminationDokumen93 halamanStool ExaminationWajid SultanBelum ada peringkat
- What Is Food Poisoning?: W Hotel Talents 6 April 2016Dokumen10 halamanWhat Is Food Poisoning?: W Hotel Talents 6 April 2016Dhani AnggaraBelum ada peringkat
- Diarrhea: Presented by Dwi Aprila Putri 12-083Dokumen28 halamanDiarrhea: Presented by Dwi Aprila Putri 12-083Dwi Aprila PutriBelum ada peringkat
- Acute Gastroenteritis in ChildrenDokumen39 halamanAcute Gastroenteritis in ChildrenIra Mikkaella GenobisBelum ada peringkat
- FECALYSISDokumen14 halamanFECALYSISMarl EstradaBelum ada peringkat
- NematodesDokumen110 halamanNematodesRussel Bob BorromeoBelum ada peringkat
- Travelers DiarrheaDokumen23 halamanTravelers Diarrheakakang chuBelum ada peringkat
- Food Waterborne Bacterial DiseasesDokumen29 halamanFood Waterborne Bacterial Diseasesracf0106Belum ada peringkat
- Laboratory Diagnosis of Parasitic DiseasesDokumen57 halamanLaboratory Diagnosis of Parasitic DiseasesAmanuel MaruBelum ada peringkat
- DIARRHEADokumen6 halamanDIARRHEAGaurav ThapaBelum ada peringkat
- Evaluation of Acute DiarrheaDokumen129 halamanEvaluation of Acute Diarrheasidvic97Belum ada peringkat
- Salmonella SPP.: Hirendra D. Tadvi Unit: Clinical BacteriologyDokumen19 halamanSalmonella SPP.: Hirendra D. Tadvi Unit: Clinical BacteriologyMeet VaghelaBelum ada peringkat
- Acute GastroenteritisDokumen48 halamanAcute Gastroenteritisansam kamalBelum ada peringkat
- Stoolexamination DR 160521051722Dokumen86 halamanStoolexamination DR 160521051722kathrynBelum ada peringkat
- Slide Kuliah Infectious DiareDokumen75 halamanSlide Kuliah Infectious DiareFany Raihan PadilahBelum ada peringkat
- Lecture Diarrhea and ConstipationDokumen63 halamanLecture Diarrhea and ConstipationKrittin NaravejsakulBelum ada peringkat
- Characteristic of Enteric BacteriaDokumen56 halamanCharacteristic of Enteric BacteriaAlpesh SutharBelum ada peringkat
- 112GIT BacteriologyDokumen57 halaman112GIT Bacteriologykane.20602Belum ada peringkat
- SalmonellaDokumen12 halamanSalmonellaJay Ann EmanBelum ada peringkat
- Presentasi Kelompok 8Dokumen45 halamanPresentasi Kelompok 8meida astriani gozaziBelum ada peringkat
- PARASITOLOGYDokumen77 halamanPARASITOLOGYZac Bornilla RodriguezBelum ada peringkat
- Colibacillosis: Cause: E. ColiDokumen37 halamanColibacillosis: Cause: E. ColiDianventi RiandaniBelum ada peringkat
- 4.special Methods and Clinical Identification in Digestive SystemDokumen37 halaman4.special Methods and Clinical Identification in Digestive SystemToafan MegaBelum ada peringkat
- STAPHYLOCOCCIDokumen26 halamanSTAPHYLOCOCCIDaud Rehman KhanBelum ada peringkat
- Mastitis Presented by Bishal BhattachanDokumen20 halamanMastitis Presented by Bishal BhattachanRabinBelum ada peringkat
- DR Jimoh - Enterobacteriaceae - LectureDokumen42 halamanDR Jimoh - Enterobacteriaceae - LectureSUfyan RaZiBelum ada peringkat
- FECALYSISDokumen43 halamanFECALYSISKen LaguiabBelum ada peringkat
- Stool ExaminationDokumen108 halamanStool ExaminationBig ZeroBelum ada peringkat
- Persistent Diarrhoea & Chronic DiarrhoeaDokumen34 halamanPersistent Diarrhoea & Chronic DiarrhoeanilmbbsBelum ada peringkat
- Helicobacter CampylobacterDokumen13 halamanHelicobacter CampylobacterNaing Lin SoeBelum ada peringkat
- Stool ExaminationDokumen82 halamanStool Examinationambadepravin100% (2)
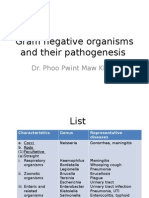
- Gram Negative Organisms and Their Pathogenesis (Print)Dokumen72 halamanGram Negative Organisms and Their Pathogenesis (Print)lathaBelum ada peringkat
- Chronic DiarrheaDokumen38 halamanChronic DiarrheaShujina ZainabBelum ada peringkat
- 12 Aerobic Gram-Positive BacilliDokumen68 halaman12 Aerobic Gram-Positive BacilliClarence SantosBelum ada peringkat
- Vibrio: Dr. Azwar, SPMK, SPTHT-KL Laboratorium Mikrobiologi FK UnsyiahDokumen18 halamanVibrio: Dr. Azwar, SPMK, SPTHT-KL Laboratorium Mikrobiologi FK UnsyiahmuslimBelum ada peringkat
- Puro Sito LogiaDokumen77 halamanPuro Sito LogiaNecesario BanaagBelum ada peringkat
- c1fd6bbd Ff7a 480d A20e C93bd3a3cedfDokumen35 halamanc1fd6bbd Ff7a 480d A20e C93bd3a3cedfapi-26938624Belum ada peringkat
- Salmonella: DR - Vasanthi .R Professor Dept Microbiology ChriDokumen52 halamanSalmonella: DR - Vasanthi .R Professor Dept Microbiology ChrividhyashreeBelum ada peringkat
- Food Science POISONINGDokumen34 halamanFood Science POISONINGArthur p90Belum ada peringkat
- C ParvumDokumen21 halamanC ParvumSamyuktha SivakumarBelum ada peringkat
- 2017-2018 - GI Infectious DiseasesDokumen57 halaman2017-2018 - GI Infectious Diseasesbahadar94Belum ada peringkat
- Vibrio Campy and Hpylori Notes MBCHBDokumen35 halamanVibrio Campy and Hpylori Notes MBCHBMuthianiBelum ada peringkat
- Gastrointestinal Communicable DiseasesDokumen7 halamanGastrointestinal Communicable DiseasesFreeNursingNotes100% (1)
- Pitri - GI.Pemicu 4. GE+ Tifus AbdominalisDokumen154 halamanPitri - GI.Pemicu 4. GE+ Tifus AbdominalisCunCunAlAndraBelum ada peringkat
- Enterococci and Other GPCS: Clinical BacteriologyDokumen32 halamanEnterococci and Other GPCS: Clinical BacteriologyJhenille SalasBelum ada peringkat
- Diseases of Live Stock & PoultryDokumen42 halamanDiseases of Live Stock & PoultryNitric AcidBelum ada peringkat
- 08 - Gastrointestinal and Exocrine Pancreatic FunctionDokumen7 halaman08 - Gastrointestinal and Exocrine Pancreatic Functionhamadadodo7Belum ada peringkat
- "Bloody Scours": Swine DysenteryDokumen29 halaman"Bloody Scours": Swine DysenteryleaBelum ada peringkat
- Animal Health Ii: DR Deepak SapkotaDokumen14 halamanAnimal Health Ii: DR Deepak SapkotaSushil AcharyaBelum ada peringkat
- Urinary Symptoms - DR RashaDokumen70 halamanUrinary Symptoms - DR RashaRasha TelebBelum ada peringkat
- Infcetions Intestinal Protozoal InfectionsDokumen40 halamanInfcetions Intestinal Protozoal InfectionsDr.P.NatarajanBelum ada peringkat
- Prepared By: Melody Gay M. Igcasenza, PTRP, RNDokumen122 halamanPrepared By: Melody Gay M. Igcasenza, PTRP, RNtishpatBelum ada peringkat
- No Gallbladder Diet Cookbook: Discover Flavorful and Nourishing Recipes to Revitalize Your Metabolism After Gallbladder Surgery [III EDITION]Dari EverandNo Gallbladder Diet Cookbook: Discover Flavorful and Nourishing Recipes to Revitalize Your Metabolism After Gallbladder Surgery [III EDITION]Penilaian: 5 dari 5 bintang5/5 (24)
- Tut2 Exam QuestionsDokumen2 halamanTut2 Exam QuestionsFarhana Azmira AsmadiBelum ada peringkat
- Treatment and Prevention of Pulmonary TuberculosisDokumen42 halamanTreatment and Prevention of Pulmonary TuberculosisFarhana Azmira AsmadiBelum ada peringkat
- Exam Saq Revision QuestionsDokumen5 halamanExam Saq Revision QuestionsFarhana Azmira AsmadiBelum ada peringkat
- Hypersensitivity ReactionsDokumen6 halamanHypersensitivity ReactionsFarhana Azmira AsmadiBelum ada peringkat
- Tutorial 6 - Apoptosis & HIVDokumen6 halamanTutorial 6 - Apoptosis & HIVFarhana Azmira AsmadiBelum ada peringkat
- Tutorial 4 - Haematopoeisis & Blood Clotting CascadeDokumen5 halamanTutorial 4 - Haematopoeisis & Blood Clotting CascadeFarhana Azmira AsmadiBelum ada peringkat
- Tutorial 2 - Cell CycleDokumen3 halamanTutorial 2 - Cell CycleFarhana Azmira AsmadiBelum ada peringkat
- Cell Wall Synthesis InhibitorsDokumen5 halamanCell Wall Synthesis InhibitorsFarhana Azmira AsmadiBelum ada peringkat
- Disease (Virus) Genome Virus Properties Transmission Outcome Diagnosis PreventionDokumen2 halamanDisease (Virus) Genome Virus Properties Transmission Outcome Diagnosis PreventionFarhana Azmira AsmadiBelum ada peringkat
- Proposition 1B Project Close-Out ProcessDokumen4 halamanProposition 1B Project Close-Out ProcessFarhana Azmira AsmadiBelum ada peringkat
- Revision MBB DR Hue FullDokumen14 halamanRevision MBB DR Hue FullFarhana Azmira Asmadi0% (1)
- Case Study of AmoebiasisDokumen7 halamanCase Study of Amoebiasisbuzz Q75% (4)
- Apolon paraDokumen4 halamanApolon paraHanin ArakamaBelum ada peringkat
- PARASITOLOGYDokumen12 halamanPARASITOLOGYBr1nfoBelum ada peringkat
- GI MnemonicsDokumen14 halamanGI Mnemonicsjonnyahn100% (1)
- Presentation - AMEBIASISDokumen37 halamanPresentation - AMEBIASISRajanBelum ada peringkat
- Entamoeba HistolyticaDokumen18 halamanEntamoeba HistolyticaMayuri VohraBelum ada peringkat
- Balantidium ColiDokumen12 halamanBalantidium ColiSalsabila Putri AmrilBelum ada peringkat
- اسئلة طفيليات MCQ مهمة جدا PDFDokumen15 halamanاسئلة طفيليات MCQ مهمة جدا PDFفواطم صائب عباس فاضلBelum ada peringkat
- MCQ ParasitologyDokumen7 halamanMCQ ParasitologyMontassar Dridi100% (1)
- PROVIDO-Atlas No.1 The AmebasDokumen32 halamanPROVIDO-Atlas No.1 The AmebasCatherine Kaye ProvidoBelum ada peringkat
- Activity 1 - Intestinal ProtozoansDokumen47 halamanActivity 1 - Intestinal ProtozoansRocel LomedaBelum ada peringkat
- Sarcomastigophora: A Phylum of PROTOZOA Subphyla: SARCODINA and Have Flagella or PseudopodiaDokumen20 halamanSarcomastigophora: A Phylum of PROTOZOA Subphyla: SARCODINA and Have Flagella or Pseudopodiaabel semuBelum ada peringkat
- Journals On AmoebiasisDokumen7 halamanJournals On AmoebiasisAlma CayapBelum ada peringkat
- Protogyl PDFDokumen5 halamanProtogyl PDFpushkar078Belum ada peringkat
- 1 7.MCQ'SDokumen15 halaman1 7.MCQ'SSketchy Seven100% (2)
- Balantidium ColiDokumen10 halamanBalantidium ColisuqylBelum ada peringkat
- CodeDokumen88 halamanCodeGLADYSBelum ada peringkat
- 8-Human Health and Disease Extra Questions-1Dokumen14 halaman8-Human Health and Disease Extra Questions-1Poonam PathakBelum ada peringkat
- Albendazole in PediatricsDokumen38 halamanAlbendazole in PediatricsKishore ChandkiBelum ada peringkat
- 0812 Model Answers Winter 2015 PDFDokumen37 halaman0812 Model Answers Winter 2015 PDFRutujaBelum ada peringkat
- Human Health & DiseasesDokumen55 halamanHuman Health & DiseasesSAGAR PADALKARBelum ada peringkat
- Tabel IcdDokumen214 halamanTabel IcdSusilo HendroBelum ada peringkat
- Table of Differentiation of ParasitesDokumen18 halamanTable of Differentiation of ParasitesManuel RendonBelum ada peringkat
- Stuart Bloom (Editor), George Webster (Editor), Daniel Marks (Editor) - Oxford Handbook of Gastroenterology & Hepatology (Oxford Medical Handbooks) - Oxford University Press (2021)Dokumen1.146 halamanStuart Bloom (Editor), George Webster (Editor), Daniel Marks (Editor) - Oxford Handbook of Gastroenterology & Hepatology (Oxford Medical Handbooks) - Oxford University Press (2021)aliakbar178Belum ada peringkat
- CD PresentationDokumen225 halamanCD PresentationHersy Marie Azores GarayBelum ada peringkat
- Patient-Centered Family-Focused Community-Oriented: Case: AmoebiasisDokumen3 halamanPatient-Centered Family-Focused Community-Oriented: Case: Amoebiasisk.n.e.d.Belum ada peringkat
- COMMUNICABLE DISEASES - Power Point PDFDokumen143 halamanCOMMUNICABLE DISEASES - Power Point PDFGel Marie LobatonBelum ada peringkat
- Medical Parasitology QuestionsDokumen5 halamanMedical Parasitology QuestionsAlaa ZiyadBelum ada peringkat
- Medical para Health-1Dokumen504 halamanMedical para Health-1Yordanos AsmareBelum ada peringkat
- Biology Project: Topic: Human Health and DiseasesDokumen17 halamanBiology Project: Topic: Human Health and DiseasesSagar Kumar0% (1)

























































![No Gallbladder Diet Cookbook: Discover Flavorful and Nourishing Recipes to Revitalize Your Metabolism After Gallbladder Surgery [III EDITION]](https://imgv2-2-f.scribdassets.com/img/word_document/591540228/149x198/6ba6cc3b38/1713999276?v=1)








































