Periodontal Emergencies
Diunggah oleh
Ammar AldawoodyehJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Periodontal Emergencies
Diunggah oleh
Ammar AldawoodyehHak Cipta:
Format Tersedia
Periodontal Emergencies (Acute Periodontal Conditions)
It seems that the Dr was using different slides than what I have received, for this reason I included the actual script (what the Dr said during the lecture) in a box, you can find it in page #7&8, the rest of this document is a copy of what was written in the slides. Acute conditions are: Characterized by a rapid onset and rapid course. Frequently accompanied by pain and discomfort. Not necessarily related to the presence of pre-existing gingivitis or periodontitis. Periodontal Emergencies includes: 1. 2. 3. 4. 5. Abscess of the Periodontium. Pericoronitis. Endo-perio lesion. Herpetic infections. Necrotizing periodontal diseases.
Abscess of the Periodontium
Abscess of the periodontium is an acute infection involving a localized collection of pus in the periodontium.
Symptoms of Abscess of the Periodontium: - The patient comes to the dental office complaining of pain and swelling of the gingiva. - The patient may also complain of difficulty in mastication or bad taste in the mouth. - Elevated body temperature is a sign that the abscess of the periodontium is spreading; so this is a serious sign if present. Clinical Examination reveals: - A circumscribed swelling of the soft tissue; may involve the gingiva only or may involve both the gingiva and the mucosa - Slight mobility. - Vital teeth.
In this picture abscess has broken through the tissue:
Causes of Abscess of the Periodontium: - Blockage of the opening of an existing periodontal pocket. - Forcing a foreign object into the supporting tissues of a tooth. - Incomplete calculus removal: Can occur in a site with deep pocket where calculus deposits are removed only in the most coronal aspects of the pocket near the gingival margin. Removal of only the more coronal calculus allows the gingival margin to heal and tighten around the tooth. Bacterial toxins are trapped in the pocket and bacteria can result in the formation of an abscess. Types of abscesses of the Periodontium: Can be either: - Gingival Abscess. - Periodontal Abscess.
Gingival Abscess
Characterized by: - Periodontally healthy mouth (normally is not associated with per-existing periodontal diseases). - Foreign object is forced into a healthy sulcus. - Limited to gingival margin. - Localized swelling. - Painful. - Purulent exudates may be present. So it involves the marginal gingiva or interdental papilla:
Gingival abscess treatment: - Elimination of foreign object. - Drainage through sulcus with probe or light scaling (make sure that the area is clean and no calculus in the sulcus). - Control of discomfort. - Follow-up after 24-48 hours. - Recommend warm saline rinses. Normally it heals without any complications.
Periodontal Abscess
- A localized purulent infection within the tissues adjacent to the periodontal pocket. - Occurs at a site with preexisting periodontal pockets. - Usually affects deeper structures of the periodontium (PDL and Bone destruction). - Not limited to the gingival margin. - Usually there is impaction or lodgment of a piece of calculus or any foreign body and there is no way for escape of the fluid from the tissue, so it will end with the tissue forming an abscess, and it may form fistula and you know that abscess in general follow the path of the weakest structures for drainage, most of the cases it can be treated and the condition is reversible.
Factors associated with abscess development: Occlusion of pocket orifice (by healing of marginal gingiva following supragingival scaling): So you have to be careful and make sure when you do scaling or root planning, you need to flush, especially with root planning, because if the calculus is detached from the root surface but stayed inside the periodontal pocket, sometimes healing occurs and the epithelium has tendency to close the pocket and there will be entrapment of this piece of calculus and there will be abscess. Furcation involvement: because of difficult instrumentation sometimes we left behind calculus or foreign body and it gives rise to formation of periodontal abscess. Long term treatment of systemic antibiotic (allowing overgrowth of resistant bacteria) Diabetes Mellitus: of course they have more tendencies for formation of periodontal abscesses and in general periodontal disease and periodontitis.
Periodontal Abscess
Clinical Features: Smooth, shiny swelling of the gingiva. Painful, tender to palpation. Purulent exudates. Increased probing depth. Mobile and/or percussion sensitive. Tooth usually vital.
Periodontal Vs. PeriapicalAbscess
Periodontal Abscess: Vital tooth No caries Pocket Periapical Abscess: Non-vital tooth Caries No pocket
Treatment of periodontal abscess Anesthesia Antibiotics Establish drainage: Incision and drainage Extraction
Pericoronitis
- Localized infection within the tissue surrounding the crown of a partially erupted tooth. - Mandibular third molars in young adults, usually caused by impaction of debris under the soft tissue flap.
Pericoronal Abscess: - An abscess of the periodontium that involves tissues around the crown of a partially erupted tooth. - Also referred to as Pericoronitis. - Most frequently seen around mandibular third molars. - The flap of tissue covers part of the occlusal surface (operculum).
Clinical Features Operculum (soft tissue flap). Localized red, swollen tissue . Area painful to touch. Tissue trauma from opposing tooth common. Purulent exudate, trismus, and fever. Treatment Options Debride/irrigate under pericoronal flap. Tissue recontouring (removing tissue flap).
Extraction of involved and/or opposing tooth. Antimicrobials (local and/or systemic as needed). .
Endo-Perio Lesion
There are basically 3 ways of communication between the pulp and the connective tissue (PDL): 1- The apical foramen: when the abscess is formed from it it's called Periapical abscess or periodontal apical abscess, which results from the infection of the pulp, and later on may result in infection and resorption of the bone, and as you know the bone is considered as a part of the periodontal system. 2- Lateral and accessory canals: which are mostly available in the apical third, and maybe also in the Furcation area, lateral accessory canals are mostly present with the lateral incisor. 3- Dentinal tubules: which contains the odontoblasts and the nerve endings that maybe responsible for the patient hypersensitivity. so these maybe source of communication for the infection between the pulp and the periodontium, these ways are present in normal anatomy. There are other types for communication which are pathological: 1- Dental malformation. 2- Vertical root fracture and perforations: in vertical root fracture and in dental malformation (like grooves) there will be a line of radiolucency, here after you do RCT and the periodontal treatment you'll find the still there is radiolucency, so I may search for vertical root fracture or grooves, here the cone beam CT may be useful in detecting them. 3- Iatrogenic factors: which are caused by a mistake of the Dr. himself, mostly when the Dr causes a perforation in the canal during RCT, which will result in radiolucency after the treatment .
There are 5 types of Endo-perio lesions: 1- Primary endodontic disease: here the lesion starts from the pulp, the pulp here is not vital, this type is treated by RCT. 2- Primary periodontal disease: when it starts from the periodontium (like if we have deep pocket and attachment loss), the pulp here is mostly vital, this type is treated by scaling and root planing. In these 2 types we have problem in 1 of them only. 3- Primary endo and secondary perio: where the lesion starts in the pulp and spreads to the periodontium, it can spread either from the apex or from the accessory canals. 4- Primary perio and secondary endo: where a lesion from the periodontium reaches the apex and causes endo problem which can also spread either from the apex or from the accessory canals. It can be differentiated by horizontal bone loss, Periapical radiolucency and the crown is intact (no caries or restorations) and the vitality test gives negative results. 5- Combined lesion: where there are perio problem and in the same time endo problem, it can be advanced where there is a communication between them and huge destruction of the bone, or you can find it in a stage before this communication, we start the treatment with RCT then perio treatment. The type of bacteria is different between the pulp and the periodontium lesions, and here we have a synergistic effect to damage the bone and the soft tissue. The Dr talked about a picture and said: here we have a true combined lesion and mostly we have angular bone resorption and huge bone resorption from the two sides. When we want to differentiate between these lesions it's very important to check the vitality of the teeth, we also we use Periapical radiographs, percussion, palpation and probing for the pocket, also we can see if we have a sinus tract or whatever. If we have a periodontal abscess in primary periodontal disease the tooth usually would be vital. Important: when we have an endo-perio lesion usually we start the treatment with RCT, because I cannot stop the infection the periodontium and still I have an infection in the pulp, so after I start do initial removal of the calculus I go immediately and do RCT and then we go to the perio treatment.
Necrotizing Periodontal Diseases
- Necrotizing Ulcerative Gingivitis (NUG) - Necrotizing Ulcerative Periodontitis (NUP)
Necrotizing Ulcerative Gingivitis
Necrotizing Ulcerative Gingivitis is an infection characterized by gingival necrosis presenting as punched-out papillae, with gingival bleeding and pain. Distinguishing Characteristics: - Necrosis (death of the cells). - Ulceration. - Loss of the gingival epithelium. - Pseudomembrane (a gray-white layer covering the necrotic areas of the gingiva). - Punched out papillae (destruction of papillae).
Historical terminology: Vincents disease. Trench mouth. Acute necrotizing ulcerative gingivitis (ANUG). Necrotizing Ulcerative Gingivitis: - Necrosis limited to gingival tissues. - Estimated prevalence 0.6% in general population. - Young adults (mean age 23 years). - More common in Caucasians. - Bacterial flora: Spirochetes (Treponema sp.).
Prevotella intermedia. Fusiform bacteria. Clinical Features: Gingival necrosis, especially tips of papillae. Punched out or cratered papillae. Pain. Extreme halitosis. Pseudomembrane formation (Gray-white). Bleeding upon slight manipulation. Swollen lymph nodes. Elevated body temperature.
Predisposing Factors: Emotional stress. Poor oral hygiene. Cigarette smoking. Poor nutrition. Immunosuppression. ***Necrotizing Periodontal diseases are common in immunocompromised patients, especially those who are HIV (+).
Necrotizing Ulcerative Periodontitis
An infection characterized by necrosis of gingival tissues, periodontal ligament ,and alveolar bone.
Clinical Features:
Clinical appearance of NUG. Severe deep aching pain. Very rapid rate of bone destruction. Deep pocket formation not evident.
Necrotizing Periodontal Diseases Treatment:
Local debridement: Most cases adequately treated by debridementand sc/rp. Anesthetics as needed. Consider avoiding ultrasonic instrumentation dueto risk of HIV transmission Oral hygiene instructions Oral rinses: frequent, at least until pain subsides allowing effective OH) Chlorhexidine gluconate 2 x daily. Hydrogen peroxide/water. Povidone iodine. Pain control Antibiotics (systemic or severe involvement): Metronidazole. Modify predisposing factors. Proper follow-up.
Another picture of necrotizing Ulcerative Gingivitis:
Typical Treatment of NUG: First appointment: Gentle removal of pseudomembrane. Limited supragingival instrumentation. Self-care restricted to removal of debris with soft toothbrushing. Chlorhexidine rinses twice daily. Alternatively, equal parts hydrogen peroxide andwarm water every 2 to 3 hours.
Second appointment: 2 days after initial appointment. Subgingival instrumentation. Further self-care instructions. Third appointment: 5 days after initial appointment. Complete subgingival instrumentation. Antibiotics may be necessary. Fourth appointment: Following infection resolution. Comprehensive clinical assessment. Identify any underlying chronic periodontal disease.
Herpetic Infections
Herpes Simplex Virus, Acute viral infection of the oral mucosa: - Redness. - Multiple vesicles. - Painful ulcers. - Fever. - One to Two weeks. Treatment: Bed rest. Fluids. Nutrition. Antipyretics. Anti-viral. Recurrent Herpetic Infections Virus reactivation:
Fever. Systemic infection. Ultraviolet radiation. Stress. Immune system changes. Trauma.
Anda mungkin juga menyukai
- Chapter 1Dokumen38 halamanChapter 1synap5esBelum ada peringkat
- - الملف الذهبي رقم 1+2 CorrectedDokumen49 halaman- الملف الذهبي رقم 1+2 Correctedmohammed alsaad100% (1)
- Difference Between Mandibular First Molar and Second MolarDokumen51 halamanDifference Between Mandibular First Molar and Second MolarDrShweta Saini75% (4)
- The Effect of A "Resin Coating" On The Interfacial Adaptation of Composite InlaysDokumen8 halamanThe Effect of A "Resin Coating" On The Interfacial Adaptation of Composite InlaysAli Al-QaysiBelum ada peringkat
- Ranula Cyst, (Salivary Cyst) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandRanula Cyst, (Salivary Cyst) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Vincent’s Angina, (Trench Mouth) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandVincent’s Angina, (Trench Mouth) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Understanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsDari EverandUnderstanding Periodontitis: A Comprehensive Guide to Periodontal Disease for Dentists, Dental Hygienists and Dental PatientsBelum ada peringkat
- Oral MedicineDokumen136 halamanOral Medicineganang19Belum ada peringkat
- Acute Periodontal LesionsDokumen30 halamanAcute Periodontal LesionsJorge CabreraBelum ada peringkat
- Oral OdourDokumen4 halamanOral Odourerwin sutonoBelum ada peringkat
- Oral Complain of Denture-Waering Elderly PPL Living in Nursing Home in Istanbul, TurkeyDokumen9 halamanOral Complain of Denture-Waering Elderly PPL Living in Nursing Home in Istanbul, TurkeytwinforsyriaBelum ada peringkat
- Dent 355-10 Keratoses and Related Disorders of Oral MucosaDokumen23 halamanDent 355-10 Keratoses and Related Disorders of Oral MucosaHamna FitriahBelum ada peringkat
- Gingivitis Experimental LoeDokumen11 halamanGingivitis Experimental LoeCarla Itzel C SánchezBelum ada peringkat
- Periodontal AbscessDokumen40 halamanPeriodontal AbscessDrDebasish Mishra100% (1)
- Periodontal MedicineDokumen24 halamanPeriodontal MedicineMoola Bharath Reddy100% (1)
- Diseases of the Oral Cavity: Signs, Symptoms and ManagementDokumen117 halamanDiseases of the Oral Cavity: Signs, Symptoms and ManagementRamanujam SridharBelum ada peringkat
- Tongue DisordersDokumen31 halamanTongue DisordersMaphoto Xola0% (1)
- 1981 Erwin P. Barrington. An Overview of Periodontal Surgical ProceduresDokumen11 halaman1981 Erwin P. Barrington. An Overview of Periodontal Surgical ProceduresAlejandro MorenoBelum ada peringkat
- A Guide To Clinical Differential Diagnosis of Oral Mucosal LesionDokumen46 halamanA Guide To Clinical Differential Diagnosis of Oral Mucosal LesionFasmiya ShariffBelum ada peringkat
- 3 Extracted Pages From Anna B. Fuks, Benjamin Peretz Eds. Pediatric Endodontics Current Concepts in Pulp Therapy For Primary and Young Permanent TeethDokumen32 halaman3 Extracted Pages From Anna B. Fuks, Benjamin Peretz Eds. Pediatric Endodontics Current Concepts in Pulp Therapy For Primary and Young Permanent TeethMona CameliaBelum ada peringkat
- Endo-Perio Lesion PDFDokumen23 halamanEndo-Perio Lesion PDFamaniBelum ada peringkat
- Periodontal Pocket and Bone Loss GuideDokumen25 halamanPeriodontal Pocket and Bone Loss GuideAmit KumarBelum ada peringkat
- Periodontal DiseaseDokumen2 halamanPeriodontal Diseasekiki119100% (1)
- DARDEN - SMT1 - 2019 - Medical Emergency in Dental Office A ReviewDokumen8 halamanDARDEN - SMT1 - 2019 - Medical Emergency in Dental Office A ReviewGita RizkiBelum ada peringkat
- IRTDokumen2 halamanIRTIgnacioBelum ada peringkat
- Midline Diastema Treatment OptionsDokumen6 halamanMidline Diastema Treatment OptionsnandaBelum ada peringkat
- Oral Leukoplakia: A ReviewDokumen60 halamanOral Leukoplakia: A ReviewdimasahadiantoBelum ada peringkat
- Pediatric dental care guidelines for cancer patientsDokumen7 halamanPediatric dental care guidelines for cancer patientsMariele Pototski AmenabarBelum ada peringkat
- OSCE Pediatric Dentistry Lecture-AnswersDokumen40 halamanOSCE Pediatric Dentistry Lecture-AnswersR MBelum ada peringkat
- Daftar Pustaka Coated TongueDokumen1 halamanDaftar Pustaka Coated TongueAgatha Pratiwi Part IIBelum ada peringkat
- Periodontal Instruments GuideDokumen10 halamanPeriodontal Instruments Guideama_rubBelum ada peringkat
- Oral Medicine FinalDokumen29 halamanOral Medicine Finallenami_91Belum ada peringkat
- Tooth Wear An Authoritative Reference For Dental Professionals and Students (Andrew Eder, Maurice Faigenblum, (Eds.) ) (Z-Library)Dokumen313 halamanTooth Wear An Authoritative Reference For Dental Professionals and Students (Andrew Eder, Maurice Faigenblum, (Eds.) ) (Z-Library)Diego DuranBelum ada peringkat
- Leukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandLeukoplakia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- The Ins and Outs of Root Resorption - British Dental JournalDokumen10 halamanThe Ins and Outs of Root Resorption - British Dental JournalAileen LooBelum ada peringkat
- A Cavernous Sinus Infection A Root Canal CaseDokumen4 halamanA Cavernous Sinus Infection A Root Canal CaseCarmen-BadeaBelum ada peringkat
- Oral Pathology - Tongue LesionDokumen26 halamanOral Pathology - Tongue Lesionneji_murniBelum ada peringkat
- Dentistry EmergenciesDokumen5 halamanDentistry EmergenciesSofia PereiraBelum ada peringkat
- Pulpectomy and Root Canal Treatment (RCT) in Primary Teeth: Techniques and MaterialsDokumen31 halamanPulpectomy and Root Canal Treatment (RCT) in Primary Teeth: Techniques and MaterialsSofeaBelum ada peringkat
- Periodontal Osseous Defects A Review PDFDokumen8 halamanPeriodontal Osseous Defects A Review PDFLorenaCastanoGarzonBelum ada peringkat
- CDTGuide 2019Dokumen37 halamanCDTGuide 2019Rahul SrivastavaBelum ada peringkat
- 2016-2017 Oral Path BookletDokumen8 halaman2016-2017 Oral Path Bookletpreeti_malhotra_12Belum ada peringkat
- Practical ApplicationsDokumen9 halamanPractical ApplicationsCristian OneaBelum ada peringkat
- Mucogingival Conditions in The Natural DentitionDokumen10 halamanMucogingival Conditions in The Natural DentitionMartty BaBelum ada peringkat
- The Hall Technique 10 Years On: Questions and Answers: GeneralDokumen6 halamanThe Hall Technique 10 Years On: Questions and Answers: GeneralamilescoBelum ada peringkat
- Periodontal AbscessDokumen27 halamanPeriodontal AbscessAhmed Tawfig GamalBelum ada peringkat
- The Normal Periodontium 1-GingivaDokumen34 halamanThe Normal Periodontium 1-GingivaHeba S Radaideh100% (1)
- Implant-Supported Overdentures: Part 2: ClinicalDokumen7 halamanImplant-Supported Overdentures: Part 2: ClinicalDhanasriBelum ada peringkat
- Nine Steps To Occlusal Harmony FamdentDokumen5 halamanNine Steps To Occlusal Harmony FamdentGhenciu Violeta100% (1)
- Dental Practicality IndexDokumen4 halamanDental Practicality Indexdorasani99Belum ada peringkat
- Periodicity DentalGuideDokumen52 halamanPeriodicity DentalGuideSalam BataienehBelum ada peringkat
- 2 Extracted Pages From Anna B. Fuks, Benjamin Peretz Eds. Pediatric Endodontics Current Concepts in Pulp Therapy For Primary and Young Permanent TeethDokumen22 halaman2 Extracted Pages From Anna B. Fuks, Benjamin Peretz Eds. Pediatric Endodontics Current Concepts in Pulp Therapy For Primary and Young Permanent TeethMona CameliaBelum ada peringkat
- Glossitis and Tongue Disorders GuideDokumen12 halamanGlossitis and Tongue Disorders GuideInna CheEsterBelum ada peringkat
- Inter-Proximal Enamel Reduction in Contemporary OrthodonticsDokumen7 halamanInter-Proximal Enamel Reduction in Contemporary OrthodonticsAly OsmanBelum ada peringkat
- Development of A Classification System For Periodontal Diseases and Conditions - Armitage 1999Dokumen6 halamanDevelopment of A Classification System For Periodontal Diseases and Conditions - Armitage 1999csryderBelum ada peringkat
- Odontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)Dokumen4 halamanOdontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)ML90Belum ada peringkat
- Cairo Clasificaion ResecionDokumen7 halamanCairo Clasificaion ResecionMartty BaBelum ada peringkat
- Practical Procedures in The Management of Tooth Wear 9781119389842 9781119389866Dokumen348 halamanPractical Procedures in The Management of Tooth Wear 9781119389842 9781119389866z6f9cw8vwvBelum ada peringkat
- Polyp DKKDokumen45 halamanPolyp DKKNadya Beatrix Yohanna NapitupuluBelum ada peringkat
- Guidelines BookDokumen16 halamanGuidelines BookAdel ElaroudBelum ada peringkat
- CADCAM Vs Traditional Ceramic InlayDokumen10 halamanCADCAM Vs Traditional Ceramic InlayAya Ibrahim YassinBelum ada peringkat
- Vital Therapy in Carious ToothDokumen9 halamanVital Therapy in Carious ToothAsh PeiBelum ada peringkat
- Inlay Onlay Preparation KitDokumen4 halamanInlay Onlay Preparation KitDominic TorettoBelum ada peringkat
- Fixed AppliancesDokumen16 halamanFixed AppliancesAmmar Aldawoodyeh100% (1)
- Lecture 6 Acrylic RPDDokumen23 halamanLecture 6 Acrylic RPDAmmar AldawoodyehBelum ada peringkat
- Slide 1 Perio Endo Compatibility Mode PDFDokumen9 halamanSlide 1 Perio Endo Compatibility Mode PDFAmmar AldawoodyehBelum ada peringkat
- Template DenturesDokumen22 halamanTemplate DenturesAmmar AldawoodyehBelum ada peringkat
- Review ArticleDokumen5 halamanReview ArticleJaime Moncayo PinosBelum ada peringkat
- Assignment 1 - PicoDokumen12 halamanAssignment 1 - Picoapi-596913754Belum ada peringkat
- Cleft Lip & Palate Care GuideDokumen10 halamanCleft Lip & Palate Care GuideFarhaana ShaboodienBelum ada peringkat
- Does The Dimension of The Graft Influence Patient Morbidity and Root Coverage Outcomes PDFDokumen9 halamanDoes The Dimension of The Graft Influence Patient Morbidity and Root Coverage Outcomes PDFImplant DentBelum ada peringkat
- Mammalogy Practice Lab ExamDokumen12 halamanMammalogy Practice Lab ExamKylie GoodyearBelum ada peringkat
- CL 1 Malocclusion 5TH DR Mouayad 20200531084732Dokumen57 halamanCL 1 Malocclusion 5TH DR Mouayad 20200531084732israa fuadBelum ada peringkat
- Vestibuloplasty: Related TermsDokumen29 halamanVestibuloplasty: Related Termsمظفر منعم ميران عباسBelum ada peringkat
- Xylitol Stops Tooth DecayDokumen7 halamanXylitol Stops Tooth DecaypresidentistBelum ada peringkat
- 10.2341@1559 2863 29 2 1Dokumen124 halaman10.2341@1559 2863 29 2 1enimaBelum ada peringkat
- Everything You Need to Know About Frictionless Loop MechanicsDokumen104 halamanEverything You Need to Know About Frictionless Loop Mechanicsjohn suryavardhanBelum ada peringkat
- Turner P. Clinical Guide To Oral Implantology... 3ed 2018Dokumen226 halamanTurner P. Clinical Guide To Oral Implantology... 3ed 2018Daniel EmilevBelum ada peringkat
- Repair Versus Replacement of RestorationDokumen77 halamanRepair Versus Replacement of Restorationmrkhalid.sobhy67100% (2)
- Semidirect Vital Tooth Onlay Restoration: A Case ReportDokumen5 halamanSemidirect Vital Tooth Onlay Restoration: A Case ReportResa YudhistiBelum ada peringkat
- IMP-Ankylos-Acuris-Manual and Product catalog-32671509-USX-1808Dokumen24 halamanIMP-Ankylos-Acuris-Manual and Product catalog-32671509-USX-1808Fariba KhayatiBelum ada peringkat
- CI and LI Prelims Oral AnatomyDokumen5 halamanCI and LI Prelims Oral AnatomySir France Tamayo CastilloBelum ada peringkat
- Non-Vital Bleaching RisksDokumen6 halamanNon-Vital Bleaching Riskspiece_of_mindzz1969Belum ada peringkat
- Clinical Management of The MARADokumen59 halamanClinical Management of The MARAShannon Victor Peter100% (1)
- Modified Beggs / Orthodontic Courses by Indian Dental AcademyDokumen202 halamanModified Beggs / Orthodontic Courses by Indian Dental Academyindian dental academyBelum ada peringkat
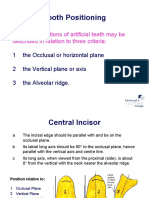
- Tooth Positioning: The Basic Positions of Artificial Teeth May Be Described in Relation To Three CriteriaDokumen19 halamanTooth Positioning: The Basic Positions of Artificial Teeth May Be Described in Relation To Three CriteriaCherine SnookBelum ada peringkat
- Mouth Preparation For Removable Partial DentureDokumen84 halamanMouth Preparation For Removable Partial DentureDrVarun Menon100% (2)
- Frankel 4Dokumen10 halamanFrankel 4Lisdany BecerraBelum ada peringkat
- Review of LiteratureDokumen4 halamanReview of LiteraturearvindBelum ada peringkat
- Retention, Stability & SupportDokumen40 halamanRetention, Stability & Supportjohn mwambu100% (1)
- Dentistry Faculty Prize Listing with ConditionsDokumen10 halamanDentistry Faculty Prize Listing with Conditionsuhurtuy0% (1)
- The Importance of Width and Length Ratios in Anterior Pemanent Dentition PDFDokumen11 halamanThe Importance of Width and Length Ratios in Anterior Pemanent Dentition PDFEddy Mazariegos100% (1)
- 2001 Lara G. BakaeenDokumen10 halaman2001 Lara G. Bakaeen謎超人Belum ada peringkat
- Errors in Impression MakingDokumen86 halamanErrors in Impression MakingArinaBelum ada peringkat