2 Issls 2006
Diunggah oleh
Saad Al HelyJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
2 Issls 2006
Diunggah oleh
Saad Al HelyHak Cipta:
Format Tersedia
Lumbar Facet Loads During Physiological Range of Motion
Goel VK, Yap MC, Shaw MN, Vishnubhotla S, Felon L, Faizan A Spine Research Center, University of Toledo, Medical University of Ohio, Toledo, OH Facet Solutions, Inc. Logan, UT
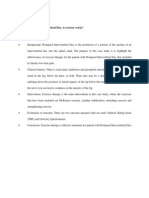
INTRODUCTION Motion preserving spinal implant technologies have emerged as attractive alternatives to fusion in the treatment of degenerative lumbar conditions. These new technologies allow surgeons to treat a patients pain while providing benefits over contemporary methods of treatment. The development of facet joint replacements in the spine requires basic research as a foundation for its design and evaluation. Among the many considerations that enter into the development of a facet joint replacement system is an understanding of the loading conditions within the facet joint itself. Both experimental and finite element model analysis facet load data have been reported. The reported facet loads and finite element analyses in the literature1-10 focus on data resulting from loading conditions up to and including maximum physiological bending moments (10Nm)2 and axial preload applications (400N)3. The study of facet joint loads is essential for the determination and justification of appropriate parameters for pre-clinical safety and effectiveness testing of facet joint replacement implants. METHODS A 3-dimensional, non-linear, ligamentous, experimentally validated, finite element model of the L3-S1 segment shown in Figure 1 was used to determine the facet loads at L3/4, L4/5, and L5/S1. The details of the model are as follows. The L3-S1 intact model consists of 31,054 elements, 38,664 nodes, and is symmetric about the mid-sagittal plane (Figure 1). Model dimensions were obtained from computer tomography (CT) scans (transverse sections of 1.5 mm thickness) of a healthy, deformity free cadaveric spine. A lordotic curve of approximately 8 was simulated at the L3-L5 level. The model was constructed and analyzed with the commercial software package ABAQUS 6.4. The intact L3-L5 model was validated at The University of Toledo, Spine Research Center against the in vitro cadaver test data11,12. The vertebral bodies and posterior bone was defined as a cancellous bone core surrounded by a 0.5mm thick cortical bone shell (Table 1). All of the bony elements were constructed with a threedimensional hexagonal element (C3D8). A C3D8 element is defined using eight nodes with each node possessing three degrees of freedom. Anatomically, the inferior and superior facets contain a thin cartilaginous layer lining the articular surface. This thin layer was simulated with three dimensional gap contact elements (GAPUNI). These elements transfer force along a single direction as a specified gap closes between nodes. An initial gap of 0.5mm was assumed based on CT images of cadaveric specimens. The thin cartilaginous layer was simulated with ABAQUSs softened contact parameter which adjusts force transfer between nodes exponentially, depending on the gap size. Upon full closure of the gap, the stiffness of the joint assumed the same stiffness as the surrounding bone. The lumbar facet joints are oriented at an inclination of 72 from horizontal, determined from several CT images. The intervetebral disc was modeled as a composite of a solid matrix with embedded fibers in concentric rings around a pseudofluid nucleus. Seven concentric rings of ground substance about the nucleus each contained two evenly spaced layers of fibers (plus one ground substance ring with one layer of fibers) oriented at 30 to the horizontal. The fibers were defined via the REBAR command. It was assumed that an overall collagenous fiber content of 16% of the annular volume was distributed amongst the seven layers. The fiber thickness and stiffness increased in the radial direction and is shown in Table 1. A no compression option was defined for the annulus fibers so that the fibers resist tension only. The hydrostatic properties of the nucleus were simulated with hexagonal C3D8 elements assigned low stiffness (1MPa) values and near incompressibility (Poissons ratio is 0.4999). All seven major ligaments were represented in the intact spine model. These ligaments are as follows: anterior longitudinal, posterior longitudinal, intertransverse, ligamentum flavum, interspinous, supraspinous, and capsular. The ligaments were modeled as three dimensional, two node truss elements (T3D2) and assigned nonlinear material properties such that at initially low strains, the ligaments exhibit low stiffness, but as the strains increase the ligament stiffness increases. This material property was simulated using the hypoelastic material designation which allows the axial stiffness to be a function of axial strain. The material properties as well as cross-sectional areas of the ligaments are given in Table 1 and were chosen based on literature. The models ligament elements were aligned in the direction of anatomical fiber orientation. Material properties defined in the above mentioned model are summarized in Table 1. The model material properties were assumed to be isotropic and homogenous. The ligament material properties were nonlinear and hypoelastic. The inferior most nodes of S1 were fully constrained in all directions allowing unconstrained motion of all superior elements. These nodes included the S1 vertebral body and posterior elements. Compressive loads were equally distributed amongst the superior most nodes of the L3 vertebral body simulating physiological spinal loading conditions. The compressive loads were applied normal to the vertebral body throughout analysis, thus the load acted as a follower load. Loads of 400N and 1200N were applied to predict facet loads under axial compression. A compressive load of 400N was also applied for analysis along with 10 Nm of moment. This model was used to predict facet loads in extension, lateral bending and axial rotation modes. RESULTS The total load transmitted across one facet as well as its components along the three axes in axial compression, extension, lateral bending and axial rotation are shown in Table 2. The x, y, z, directions are shown in Figure 1. The y-axis is the anteroposterior direction and z-axis the cephalad-caudal direction. DISCUSSION The finite element model study yielded facet joint loads resulting from the application of axial compressive loads and/or pure bending moments considered to be physiological maximums The model analyses show that the total load across a L5-S1 facet joint can reach 182.9N for 10 N-m of axial torque and 400 N of axial compression. As one would expect, these values are a function of the facet joint morphology, the external loads applied to the model and the material properties of the spinal elements. The anatomic based design and biomechanically accurate material properties of the finite element model along with the application of maximum physiologic loading make this data useful for developing mechanical testing criteria and design requirements for facet joint replacements.
Superior Facet Annulus Fibrosis L3 Pedicle
L3/4 Disc Nucleus Pulposus L4 Inferior Facet
L4/5 Disc Lamina L5 L5/S1 Disc S1
Spinous Process
Y X Figure 1: Intact L3-S1 finite element mesh and a midsagittal cross-section of L3-S1 lumbar spine finite element model indicating important anatomical features. X axis represents lateral (Lat), Y axis Anterior posterior (A-P) and Z axis represents axial (Ax).
Element Set Bony Regions Vertebral Cortical Bone Vertebral Cancellous Bone Posterior Cortical Bone Posterior Cancellous Bone Intervertebral Disc Annulus (Ground Substance) Annulus Fibers Nucleus Pulposus Joints Apophyseal Joints Ligaments Anterior Longitudinal Posterior Longitudinal Intertransverse Ligamentum Flavum Interspinous Supraspinous Capsular 216 144 30 21 21 9 84 T3D2 T3D2 T3D2 T3D2 T3D2 T3D2 T3D2 15.6 20.0 10.0 20.0 12.0 59.0 13.0 19.5 9.8 12.0 8.8 15.0 8.48 32.9 0.30 0.30 0.30 0.30 0.30 0.30 0.30 74 14.4 1.8 40 40 30 34 216 GAPUNI Softened, 12000 5376 2685 1920 C3D8 REBAR C3D8 1.2 357.5 - 550 1.0 0.45 0.30 0.4999 0.00601 0.00884 3312 10608 3632 1834 C3D8 C3D8 C3D8 C3D8 12000 100 12000 100 0.30 0.20 0.30 0.20 Number of Elements ABAQUS Element Library Type Modulus of Elasticity (MPa) Poissons Ratio, Cross-Sectional Area (mm2)
Table 1: Material property definitions and element types for the intact L3-S1 finite element spine model. For bilateral structures (facet joints and capsular ligaments), the total number of elements is listed12.
L3-L4 Axial Compression x(Lat) y(A-P) z (Ax) 400N 1200N Extension 0N+10Nm Lateral Bending 0N+10Nm 400N & 10Nm Axial Rotation 0N+10Nm 103.7 400N & 10Nm 109.8 78.1 82.8 62.1 143.9 103.6 65.7 152.4 114.6 78.0 86.4 62.0 143.7 111.9 68.6 159.1 131.8 84.4 99.3 67.0 155.4 78.9 182.9 32.1 48.9 24.2 36.8 19.2 29.3 44.5 67.9 30.5 43.7 23.0 32.9 18.2 26.1 42.3 60.6 44.7 62.0 33.7 46.7 26.8 37.1 62.0 86.1 93.0 70.1 82.1 55.7 129.1 93.6 70.5 83.9 56.0 129.9 66.7 154.6 83.2 92.6 62.7 69.8 49.8 115.4 55.5 128.6 400N & 10Nm 109.0 65.2 151.2 111.4 14.3 44.7 10.8 33.7 8.6 26.8 19.8 62.0 15.1 47.0 L4-L5 11.4 35.4 9.0 28.1 20.9 23.4 L5-S1 17.6 96.8 14.0 32.5 Total x(Lat) y(A-P) z (Ax) Total x(Lat) y(A-P) z (Ax) Total 65.2 128.5 77.0 178.4
REFERENCE 1. Hooper, D.M., Goel, V.K., Aleksiev, A., Spratt, K., Bolte, K.M. and Pope, M.; Three-dimensional Moments in the Lumbar Spine During Asymmetric Lifting. Clinical Biomec 13, 386-393, 1998. 2. Lorenz M, et al; Load bearing characteristics of lumbar facets in normal and surgically altered spinal segments. Spine 8(2): 122-130, 1983. 3. Wilson D; Does implantation of a dynamic posterior stabilizing device reduce loading in the facet joints? Presentation at SAS4, Global Symposium on Interbertebral Disc Replacements and Non-Fusion Technology, 4-7 May 2004, Vienna, Austria 4. Shendel MJ, et al; Experimental measurement of ligament force, facet force and segment motion in the human lumbar spine. J Biomech 26:427-438, 1993. 5. Moumene M; The effect of artificial disc placement on facet loading: mobile core versus fixed core, Roundtables in Spine Surgery: Spine Biomechanics, Vol. 1, No. 1: 38-44, 2005. 6. Lee KK, et al; Effect of facetectomy on lumbar spinal stability under sagittal plane loadings. Spine, 29(15):1624-31, 2004. 7. Dooris A, et al; Load sharing between anterior and posterior elements in a lumbar motion segment implanted with an artificial disc. Spine, Vol. 26, No. 6: E122-E129, 2001. 8. Natarajan R, et al; Study on effect of graded facetectomy on change in lumbar motion segment torsional flexibility using three-dimensional continuum contact representation for facet joints. J Biomech Eng 121: 215-221, 1999. 9. Panjabi M, et al; Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg [Am] 76:413-424, 1994. 10. Panjabi MM & Goel VK. Adjacent-level effects: design of a new test protocol and finite element model simulations of disc replacement, Roundtables in Spine Surgery: Spine Biomechanics, 1(1): 45-55, 2005. 11. Kong W.; Clinically relevant biomechanical parameters in the lumbar spine- a theoretical and in vitro experimental investigation. Biomedical Engineering Department: University of Iowa, Iowa City, IA 1995. 12. Goel VK, Grauer J, Patel TG, Biyani A, Sairyo K, Vishnubhotla S, Matyas A, Cowgill I, Shaw M, Long R, Dick D, Panjabi MM, Serhan H.; Effects of Charite Artificial Disc on the Implanted and Adjacent Spinal Segments Mechanics Using a Hybrid testing Protocol. Spine, December 2005.
Table 2: Facet loads in newtons (N) in the x, y, and z directions for loading modes with 400N or 1200N compression load or with 10Nm bending moment and 0N or 400N compression load.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- AbbrevaitionDokumen155 halamanAbbrevaitionSaad Al HelyBelum ada peringkat
- AnnaDokumen99 halamanAnnaSaad Al HelyBelum ada peringkat
- NimaDokumen110 halamanNimaSaad Al HelyBelum ada peringkat
- Ali BadiDokumen234 halamanAli BadiSaad Al HelyBelum ada peringkat
- Ali BadiDokumen234 halamanAli BadiSaad Al HelyBelum ada peringkat
- Finite Element Analysis of Stresses Caused by External Holes in Hydraulic CylindersDokumen11 halamanFinite Element Analysis of Stresses Caused by External Holes in Hydraulic CylindersSaad Al HelyBelum ada peringkat
- Out 2Dokumen6 halamanOut 2Saad Al HelyBelum ada peringkat
- My LifeDokumen4 halamanMy LifeSaad Al HelyBelum ada peringkat
- Inventor Professional 2010 Installation InstructionsDokumen8 halamanInventor Professional 2010 Installation InstructionsSaad Al HelyBelum ada peringkat
- Illustrator Cs 5Dokumen19 halamanIllustrator Cs 5Saad Al HelyBelum ada peringkat
- Illustrator Cs 5Dokumen19 halamanIllustrator Cs 5Saad Al HelyBelum ada peringkat
- Design Girder Bridge EurocodeDokumen139 halamanDesign Girder Bridge Eurocodetomnubi100% (2)
- Non Linear Analysis of Spur Gear Using Matlab CodeDokumen105 halamanNon Linear Analysis of Spur Gear Using Matlab CodehazemismaeelradhiBelum ada peringkat
- Full Text 01Dokumen60 halamanFull Text 01Saad Al HelyBelum ada peringkat
- Modeling and Visualization Analysis Reference: Abaqus/CAE User's Guide Abaqus Analysis User's GuideDokumen1 halamanModeling and Visualization Analysis Reference: Abaqus/CAE User's Guide Abaqus Analysis User's GuideSaad Al HelyBelum ada peringkat
- Finite Element Formulation For BeamsDokumen27 halamanFinite Element Formulation For BeamsPalash JainBelum ada peringkat
- 08 Plasticity 01 IntroductionDokumen11 halaman08 Plasticity 01 Introductionabhi16Belum ada peringkat
- Advance Steel 2015 Starting GuideDokumen40 halamanAdvance Steel 2015 Starting Guidegranjero_mxBelum ada peringkat
- As User Guide 2015 en Metric 140408Dokumen170 halamanAs User Guide 2015 en Metric 140408Saad Al HelyBelum ada peringkat
- Corel Draw 2010Dokumen33 halamanCorel Draw 2010Saad Al HelyBelum ada peringkat
- Weld Geometry 1Dokumen127 halamanWeld Geometry 1Saad Al Hely100% (1)
- StructEngII Connections 276-327Dokumen52 halamanStructEngII Connections 276-327Saad Al HelyBelum ada peringkat
- Bs Steel CodeDokumen14 halamanBs Steel CodeA.K.A. HajiBelum ada peringkat
- Corel Draw 2010Dokumen33 halamanCorel Draw 2010Saad Al HelyBelum ada peringkat
- Advance Steel 2015 Starting GuideDokumen40 halamanAdvance Steel 2015 Starting Guidegranjero_mxBelum ada peringkat
- Ansys Lab2Dokumen16 halamanAnsys Lab2Saad Al HelyBelum ada peringkat
- Chapter 9 - Welding DefectsDokumen18 halamanChapter 9 - Welding Defectsbibin2010100% (1)
- SimXpert2013 ThermalDokumen230 halamanSimXpert2013 ThermalSaad Al HelyBelum ada peringkat
- LS DynaLab2Dokumen15 halamanLS DynaLab2Mohammed A. Maher100% (1)
- Mohammad SarairehDokumen176 halamanMohammad SarairehamilcarsoaresBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- King A 2002 - Injury To The Thoracolumbar Spine and PelvisDokumen37 halamanKing A 2002 - Injury To The Thoracolumbar Spine and PelvisO “Banzai” CBelum ada peringkat
- Hao, K. 2019. Application of Ozone Therapy in Interventional MedicineDokumen4 halamanHao, K. 2019. Application of Ozone Therapy in Interventional MedicineMoi RoksBelum ada peringkat
- Prolapse Lumbar DiscDokumen40 halamanProlapse Lumbar DiscAlfred BantigueBelum ada peringkat
- JurnalDokumen5 halamanJurnalQorin Diin ArifniBelum ada peringkat
- Case StudyDokumen30 halamanCase StudyNur SolehahBelum ada peringkat
- 2 Year Physical Therapy NotesDokumen129 halaman2 Year Physical Therapy Notesthwiseman94% (17)
- Rehabilitation in The Dynamic Stabilization of Lumbar SpineDokumen41 halamanRehabilitation in The Dynamic Stabilization of Lumbar SpineYip Song ChongBelum ada peringkat
- An Innovative Treatment For Discogenic Pathologies: Clinical ReferencesDokumen2 halamanAn Innovative Treatment For Discogenic Pathologies: Clinical ReferencesKaustubh KeskarBelum ada peringkat
- Spinal Fusion Surgery GuideDokumen19 halamanSpinal Fusion Surgery GuideLate ArtistBelum ada peringkat
- Lower Back Pain and DisordersDokumen74 halamanLower Back Pain and DisordersZdenek93Belum ada peringkat
- Herniated Nucleus Pulposus in Dr. Hasan Sadikin General Hospital Bandung IndonesiaDokumen7 halamanHerniated Nucleus Pulposus in Dr. Hasan Sadikin General Hospital Bandung Indonesiawulan dwi yulistiaBelum ada peringkat
- Anatomy and Physiology 5th Edition Marieb Test BankDokumen19 halamanAnatomy and Physiology 5th Edition Marieb Test Bankstephenthanh1huo100% (29)
- HNP Lumbal L5-S1Dokumen13 halamanHNP Lumbal L5-S1Christina KonoBelum ada peringkat
- Elective EntropyDokumen21 halamanElective EntropyDavidroy IRITSBelum ada peringkat
- ICD 10 FisioterapiDokumen38 halamanICD 10 FisioterapiJasmine FrisyaBelum ada peringkat
- Cervical SpineDokumen69 halamanCervical Spineveravero100% (3)
- Biomechanics of The Spine I PDFDokumen9 halamanBiomechanics of The Spine I PDFCambriaChicoBelum ada peringkat
- Biomechanics of The SpineDokumen18 halamanBiomechanics of The SpineSudheer Jayaram100% (1)
- Diagnostic Challenges in Musculoskeletal Radiology PDFDokumen182 halamanDiagnostic Challenges in Musculoskeletal Radiology PDFphuong mai leBelum ada peringkat
- Chiropractic ICD-10 Code ListDokumen5 halamanChiropractic ICD-10 Code ListDale100% (1)
- Spinal Disc HerniationDokumen5 halamanSpinal Disc HerniationJoshua Hong100% (1)
- Lumbar Disk HerniationDokumen6 halamanLumbar Disk HerniationShivaji DeshmukhBelum ada peringkat
- All Previous Essay SurgeryDokumen170 halamanAll Previous Essay Surgeryalsfyabdullah2021Belum ada peringkat
- Astri - Neck Cailliet ExerciseDokumen116 halamanAstri - Neck Cailliet ExerciseAstri Arf100% (1)
- Erler Zimmer (Watermark) - PasswordDokumen260 halamanErler Zimmer (Watermark) - Passwordmat kool100% (1)
- Nucleus Arthroplasty Volume IIDokumen55 halamanNucleus Arthroplasty Volume IIHelifunoBelum ada peringkat
- Benzakour-Benzakour2019 Article DiscHerniationAndDiscDiseaseTh PDFDokumen6 halamanBenzakour-Benzakour2019 Article DiscHerniationAndDiscDiseaseTh PDFLee제노Belum ada peringkat
- Classification of Intervertebral Disc Disease - 2020Dokumen17 halamanClassification of Intervertebral Disc Disease - 2020Alice PaimBelum ada peringkat
- Internal Disc Disruption ArticleDokumen2 halamanInternal Disc Disruption ArticleHazem BBelum ada peringkat
- Electrodiagnosisofcervical Radiculopathy: Kevin Hakimi,, David SpanierDokumen12 halamanElectrodiagnosisofcervical Radiculopathy: Kevin Hakimi,, David Spanierkashif mansoorBelum ada peringkat