Lap Adrenalectomy Nca
Diunggah oleh
Perrilyn PereyHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Lap Adrenalectomy Nca
Diunggah oleh
Perrilyn PereyHak Cipta:
Format Tersedia
Demographic profile My Patient is R.H a Filipino male and a Roman Catholic.
He was born on June 4, 1962 and is now 50 years old. He was born and currently residing at Sta. Mesa Manila. He is a retired sea man. Patient has Phil. Health insurance. History Patient has a known case of nephrolithiasis left kidney that was diagnosed last 2011. Two weeks prior to admission, the patients stonogram revealed non obstructing nephrolithiasis and incidental finding of isodense mass on right adrenal gland with suggestive benign features. The patient was advised to undergo Laparascopic Adrenalectomy Possible Open hence admission. Family History: Paternal side: stroke, HPN Maternal side: cancer Assessment Patient was alert, not on cardiorespiratory distress Pink palpebral conjunctiva Symmetrical chest expansion Clear breath sounds Pulse full and equal Diagnostic and Laboratory Procedures Hematology Results -Indicates the total number of blood cells as well as the hemoglobin, hematocrit and RBC indices. White Blood cells a.Lymphocytes = 8.6 g/L b. Monocytes = 13.2% c. Eosinophils = 4.16T/L RBC a. Hematocrit = 0.371 l/ b. Hemoglobin = 122g/L Platelets 393g/L All results are within the normal range.
Ultrasound -To visualize of the upper abdominal area for any stones or calculi formed in the kidney. - There is a cyst in the lateral cortex measuring 1.6 cm with two reflective structures within both measuring 0.3 cm without shadows. - Left renal cyst with reflective structures with no shadowing.
Stonogram - non obstructing nephrolithiasis and incidental finding of isodense mass on right adrenal gland with suggestive benign features
Nurses notes
D>admitted a 50 year old male under the service of Dr. Bolong A>scheduled for lap. Adrenalectomy poss. Open tomorrow at 2 pm R>no complaint made
D>patient scheduled for lap. Adrenalectomy poss. Open at 2 pm A>consent secured IVF started as ordered. Instructed to be NPO at 6am R>patient responded accordingly
Anatomy and Physiology A. Overview of the Endocrine System Functions of the Endocrine System: Metabolism and tissue maturation Ion regulation Water balance Immune system regulation Heart rate and blood pressure regulation Control of blood glucose and other nutrients Control of reproductive functions Uterine contractions and milk release
Focus: Adrenal Glands The adrenal glands or suprarenal glands are two small glands that are located superior to each kidney. Each adrenal gland has an inner part, called the adrenal medulla and an outer art, called the adrenal cortex. The cortex has three indistinct layers: the zona glomerulosa, zona fasciculate, and the zona reticularis. The adrenal cortex hormones control the 3S: SUGAR, SALT, and SEX o Glucocorticoids (Cortisol) Maintain blood glucose levels Enhance gluconeogenesis (protein catabolism and fat catabolism/lipolysis) Have anti-inflammatory effect Decrease new antibody release
Increase gastric acid and pepsin production. May cause GI irritation Maintain emotional stability o Mineralocorticoids (e.g. Aldosterone) Maintain sodium and volume status Increase sodium reabsorption in distal tubules of the kidneys Increase potassium and hydrogen excretion in distal tubules. Aldosterone is pro sodium and anti-potassium o Sex Hormones Responsible for some secondary sex characteristics in females. In males, these hormones work like gonadal steroids. The effects of sympatho-adrenome-dullary response (SAMR) = EVERY FUNCTION IS HIGH AND FAST EXCEPT G.I AND G.U B. Overview of the Urinary System Functions of the Urinary System: Excretion Regulation of blood and volume pressure Regulation of the concentration of solutes in the blood Regulation of extracellular fluid pH Regulation of red blood cell synthesis Vitamin D synthesis
Focus: Kidneys The kidneys are two-bean shaped organs located retroperitoneally at the level of the 12th thoracic and 3rd lumbar vertebra The right kidney is slightly lower than the left kidney due to the presence of the liver on the right side of the abdomen The kidneys are divided into renal cortex, medulla and pelvis. The medulla is composed of series of pyramids. The functional units of the kidneys are the nephrons. The nephron is composed of glomerulus and the renal tubules The glomerulus is a tuft semi-permeable capillaries, surrounded by the Bowmans capsule The primary function of the nephron is formation of urine Through the formation of the urine, the kidneys remove waste products from the body, regulate fluid volume, and maintain electrolyte concentration, blood pressure and pH within the body. GFR: 125ml/min
Pathophysiology A. NEPHROLITHIASIS
PATHOPHYSILOGY OF NEPHROLITHIASIS AS MANIFESTED BY THE PATIENT
Nephrolithiasis refers to stones (calculi) in the kidney. Stone formation is not clearly understood, and there are a number of theories about their causes. One theory is that there is a deficiency of substances that normally prevent crystallization in the urine such a citrate, magnesium, nephrocalcin, and uropontin. Another theory relates to fluid status of the patient. Certain factors favour the formation of stones, including infection, urinary stasis, and periods of immobility, all of which slow renal drainage and alter calcium metabolism. In addition, increased calcium concentrations in the blood and urine promote precipitation of calcium and formation of stones.
B. Adrenocortical adenomas Adrenocortical adenomas are benign neoplasms of adrenocortical cells. Although most are non-functional, some secrete steroids independently from ACTH or the reninangiotensin system. Many are discovered incidentally on abdominal imaging studies (adrenal incidentalomas), while others present with symptoms of hormonal excess. After the initial discovery of an adrenal mass, subsequent evaluation should determine whether it is benign or malignant, and whether it is functional or non-functional, in order to determine the treatment needed. The cause of adrenal adenomas is unknown, but the current accepted theory is that they arise because of mutations (changes) in certain genes (which are not yet identified).Adrenal adenomas are more common in some inherited diseases, including multiple endocrine neoplastic type I, Beckwith-Wiedemann syndrome and the Carney complex. Also, patients with genetic defects of the body systems that manufacture steroid hormones (eg congenital adrenal hyperplasia), especially whose condition is poorly controlled, may have a higher risk of adrenal adenomas. However, most adrenal adenomas are not linked with an inherited disease. The likelihood of developing an adenoma increases with age. Benign adrenal adenomas are found in 1 to 32 per cent of people at autopsy, with most studies showing a detection rate of about 5 per cent. About 6 per cent of patients over 60 years of age harbour an adrenal adenoma. No other predisposing factors have been defined, and prevention is not possible.
Discussion of the OR procedure Left Anterior Laparoscopic Adrenalectomy Laparoscopic left adrenalectomy is a procedure in which the adrenal gland is surgically removed
Rationale for the surgery: Adrenal glands usually need to be removed because they either have a tumor, are secreting too much of a particular hormone, or both. Once adrenal lesions are greater than 3 to 6 cm in diameter, the risk of malignancy increases to approximately 10% to 20%. Due to the increased cancer risk, patients should have them removed. All patients undergo biochemical testing of their blood and urine to determine if the adrenal glands are secreting too much of a particular hormone or if a tumor is secreting hormones. Baseline screening tests include a 24-hour urine for catecholamines and cortisol, as well as a serum aldosterone. All tumors that secrete hormones must be removed regardless of size. Benign tumors up to 15 cm or malignant tumors smaller than 8 cm can be removed safely using laparoscopic techniques. In addition, the following diagnoses can be treated using laparoscopic adrenalectomy: Cushings Disease, adrenal adenoma, aldosteronoma, pheochromocytoma, leiomyoma, angiomyolipomas, adrenal cysts, and malignancies from other sites. What are the risks? The risks unique to adrenalectomy include bleeding, infection, and conversion to open. These complications occur in less than 1% of patients treated laparoscopically. Other risks associated with surgery in general include pneumonia and blood clots, also occurring in less than 1% of patients.
Anesthesia General anesthesia is required for laparoscopic adrenalectomy with adjuncts for pain management, such an epidural or subcutaneous local anesthetic pain pump, left to the discretion of the surgeon and anesthesiologist. Constant communication with the anesthesiologist is essential in patients with hormonally or vaso-active tumors. Appropriate intraoperative monitoring includes an arterial line and urinary catheter. Careful preoperative management and control of the physiologic effects of hormonally or vaso-active tumors should involve an endocrinologists expertise. Equipment A standard laparoscopic tray, including laparoscopic graspers and scissors, is used for a laparoscopic right adrenalectomy. A laparoscopic right angle dissector, laparoscopic Kittner, and hook electrocautery are often helpful in the dissection of the inferior vena cava and adrenal vein. A laparoscopic suction/irrigator is often required to ensure adequate visualization during dissection and after gland removal to ensure hemostasis. Other useful instruments, depending on surgeon preference, include a liver retractor, specimen retrieval bag, and an electrosurgical instrument. The authors' preference for electrosurgical instruments include the Harmonic Scalpel (Ethicon EndoSurgery, Inc, Cincinnati, OH) or LigaSure (Valleylab, Boulder, CO); however, other devices such as the Gyrus PKS Cutting Forceps (Gyrus ACMI, Maple Grove, MN) or EnSeal Tissue Sealing and Hemostasis System (SurgRx, Redwood City, CA) can be used depending on surgeon preference. A 10-mm clip applier is often used to ligate the adrenal vein, but in some cases, a vascular-load endoscopic stapling device may be necessary.
Position of the Patient The patient is positioned in the lateral right decubitus position. A pillow is placed under the flank and the table is angled to increase the space between the costal margin and iliac crest. The surgeon stands on the right of the table with the monitor across behind the head of the patient. The assistant stands opposite to the patient.
Placement of Trocars
The first trocar for the camera is placed in the umbilicus using the open technique. In the case of an obese patient a separate camera trocar is placed below and underneath the trocars for the instruments.These four additional trocars are placed along a subcortal line. The first one is placed in the midline to accommodate the endoretractor. The remaining three are placed at 5-cm intervals with the last outer one as laterally as possible. All trocars are 1012 mm diameter in order to accommodate all the necessary instruments expect the very lateral one,which can be a 5-mm one.
Step I: Mobilization of the Left Colonic Flexure/Exposure of the Upper Pole of the Left Kidney and Pancreas The left colonic flexure and descending colon are mobilized inferiorly and medially in order to expose the underlying upper pole of the left kidney. The tip of the surgeons working instrument could sense the hard surface of the kidney behind the Gerotas fascia and the overlying retroperitoneal fat. Further division of the gastrocolic ligament and mobilization of the transverse colon downward allows exposure of the pancreas.
Step II: Mobilization of the Inferior Border of the Pancreas Along with the Lower Pole of the Spleen; Exposure of the Left Adrenal Tumor The retroperitoneum along the inferior border of the pancreas is opened with diathermy.The attachment of the lower pole of the spleen to the upper pole of the kidneys is divided. The main purpose is the upward mobilization of the inferior surface of the pancreas along with the spleen. The characteristic yellow color of the adrenal tumor will now start appearing behind Gerotas fascia. The laparoscopic retractor is now inserted to keep the pancreas away from the adrenal. Step III: Mobilization of the Adrenal Tumor 1. We start the mobilization of the tumor from its inner border in the essentially avascular space between the pancreas (that is retracted and protected by the endoretractor) and the adrenal. We continue deep along this plan mobilizing most of the posterior surface of the tumor. 2. We then move along the superior surface that again is essentially without major vessels requiring separate clip ligation. 3. We continue mobilizing the external border of the tumor from the inner surface of the superior pole of the kidney.There are few vessels requiring careful hemostasis to keep the vision clear.
4. The most difficult part of this mobilization comes on the inferior border o f the adrenal tumor especially recognizing and dividing the left adrenal vein that comes off the left renal vein 23 cm from the hilum of the kidney.The pulsating left renal artery needs also to be recognized and protected. Most left adrenal arteries and veins are small and only the left main adrenal vein (and occasionally another medial accessory vein coming from the inferior phrenic) needs clip ligation. Monopolar diathermy and/or other sources of energy (Ultracision,Ligasure)provide safe and fast hemostasis.
Step IV: Removal of the Tumor/ Drainage The tumor is grasped by the left adrenal vein remnant or surrounding nonadrenal tissue, trying to avoid rupture of its capsule. It is positioned in the Endobag, which is retracted through the initial umbilical port. The umbilicus has the advantage that we can easily extend the incision to accommodate large tumors with minimal esthetic cost. A drain is positioned for 24 h.
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Bubbles HeDokumen39 halamanBubbles HePerrilyn PereyBelum ada peringkat
- LaminectomyDokumen6 halamanLaminectomyPerrilyn Perey100% (1)
- Excess Fluid Volume PPT (Case Press)Dokumen10 halamanExcess Fluid Volume PPT (Case Press)Perrilyn PereyBelum ada peringkat
- Stages of LaborDokumen30 halamanStages of LaborPerrilyn Perey100% (1)
- Acute Renal FailureDokumen4 halamanAcute Renal FailurePerrilyn PereyBelum ada peringkat
- Hematologic DiseasesDokumen11 halamanHematologic DiseasesPerrilyn Perey100% (2)
- Arrest of DescentDokumen5 halamanArrest of DescentPerrilyn PereyBelum ada peringkat
- Leg or Foot Amputation Pref CardDokumen2 halamanLeg or Foot Amputation Pref CardPerrilyn PereyBelum ada peringkat
- 5 P - S of LaborDokumen19 halaman5 P - S of LaborPerrilyn PereyBelum ada peringkat
- Critcare PDFDokumen20 halamanCritcare PDFPerrilyn PereyBelum ada peringkat
- Anxiety Related 2010Dokumen17 halamanAnxiety Related 2010Perrilyn PereyBelum ada peringkat
- Nihms281140.pdf BibliographyDokumen13 halamanNihms281140.pdf BibliographyPerrilyn PereyBelum ada peringkat
- OR TermsDokumen1 halamanOR TermsPerrilyn PereyBelum ada peringkat
- Drug NameDokumen1 halamanDrug NamePerrilyn PereyBelum ada peringkat
- Health Assessment Form Scribd.Dokumen1 halamanHealth Assessment Form Scribd.Perrilyn PereyBelum ada peringkat
- MenstruationDokumen1 halamanMenstruationPerrilyn PereyBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Cell AnalogyDokumen24 halamanCell AnalogyBOBOBOYS TVBelum ada peringkat
- Pengaruh Pemberian Terapi Latihan Metode SchrothDokumen7 halamanPengaruh Pemberian Terapi Latihan Metode SchrothsulaimanBelum ada peringkat
- The Morphology of The Post-Gastric Alimentary CanalDokumen18 halamanThe Morphology of The Post-Gastric Alimentary CanalAnca MihalcescuBelum ada peringkat
- Liver CirrhosisDokumen76 halamanLiver Cirrhosiskathy100% (2)
- Multiple Myeloma: NCCN Guidelines For PatientsDokumen78 halamanMultiple Myeloma: NCCN Guidelines For PatientsAchmad Farodisi AfnaniBelum ada peringkat
- SpermiogenesisDokumen1 halamanSpermiogenesispoiwertBelum ada peringkat
- Autotrophic Nutrition Heterotrophic NutritionDokumen1 halamanAutotrophic Nutrition Heterotrophic NutritionAditya KediaBelum ada peringkat
- Worksheet For Kinder - q1w6Dokumen20 halamanWorksheet For Kinder - q1w6lccyu9Belum ada peringkat
- The Morphology of Human Blood Cells - IllustrationDokumen86 halamanThe Morphology of Human Blood Cells - Illustrationalphaceta100% (3)
- CAPE Biology Syllabus With Specimen Papers - Split - 2Dokumen5 halamanCAPE Biology Syllabus With Specimen Papers - Split - 2Enz JosephBelum ada peringkat
- Dental Pulp Stem Cells - Function, Isolation and Applications in Regenerative Medicine PDFDokumen12 halamanDental Pulp Stem Cells - Function, Isolation and Applications in Regenerative Medicine PDFmiguelBelum ada peringkat
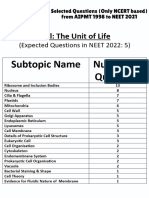
- Cell - The Unit of Life - NCERT Based PYQsDokumen9 halamanCell - The Unit of Life - NCERT Based PYQsAkhil singhBelum ada peringkat
- Developing Human Clinically Oriented Embryology 10th Edition Moore Test BankDokumen23 halamanDeveloping Human Clinically Oriented Embryology 10th Edition Moore Test Bankpulmonicfold.m7zz100% (25)
- A Nervous TripDokumen12 halamanA Nervous TripMark Owen BaldoBelum ada peringkat
- Muscular SystemDokumen43 halamanMuscular SystemJonalyn ChewacheoBelum ada peringkat
- MCqs On Hematological Disorder Provided by MirhaDokumen4 halamanMCqs On Hematological Disorder Provided by MirhaAkml KhanBelum ada peringkat
- SB7.1p HormonesDokumen9 halamanSB7.1p HormonesHisokagenBelum ada peringkat
- Forensic 2 Module 1-ContentDokumen12 halamanForensic 2 Module 1-ContentSheri Ann PatocBelum ada peringkat
- Blood Pressure - QuestionsDokumen5 halamanBlood Pressure - QuestionsErjus HoxhajBelum ada peringkat
- GametogenesisDokumen25 halamanGametogenesisJoanne Crishna MiguelBelum ada peringkat
- Physiological Changes During Pregnancy 2-1Dokumen32 halamanPhysiological Changes During Pregnancy 2-1PATRICK ROSHAN ABelum ada peringkat
- The Facts On File Illustrated Guide To The Human Body - Digestive System PDFDokumen113 halamanThe Facts On File Illustrated Guide To The Human Body - Digestive System PDFlevBelum ada peringkat
- Lecture 10Dokumen5 halamanLecture 10bibifamelaganieBelum ada peringkat
- Transfusion Related Immunomodulation (Trim) : By/ Aymen OmerDokumen14 halamanTransfusion Related Immunomodulation (Trim) : By/ Aymen OmeraymenBelum ada peringkat
- DIGESTIVE Lecture Notes PDFDokumen20 halamanDIGESTIVE Lecture Notes PDFAaliya Minar100% (4)
- Muscular SystemDokumen8 halamanMuscular Systemtheodore_estradaBelum ada peringkat
- Part of BodyDokumen4 halamanPart of Bodyanon_535068952Belum ada peringkat
- Giant Juvenile Fibroadenoma of Breast Mimicking Phylloides Tumour - A Case ReportDokumen8 halamanGiant Juvenile Fibroadenoma of Breast Mimicking Phylloides Tumour - A Case ReportsridharBelum ada peringkat
- Anatomy and Physiology of The Nervous SystemDokumen5 halamanAnatomy and Physiology of The Nervous SystemNicole Anne TungolBelum ada peringkat
- Important Questions For Class 11 Biology - Cell The Unit of LifeDokumen7 halamanImportant Questions For Class 11 Biology - Cell The Unit of LifeAli WarisBelum ada peringkat