NEJM Protocol Sample 1
Diunggah oleh
razorazHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
NEJM Protocol Sample 1
Diunggah oleh
razorazHak Cipta:
Format Tersedia
Protocol
This trial protocol has been provided by the authors to give readers additional information about their work. Protocol for: Albert RK, Connett J, Bailey WC, et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med 2011;365:689-98. (PDF updated November 21, 2011.)
Azithromycin for Prevention of COPD Exacerbations Complete Protocol Section A. Section B. Section C. Complete protocol. 1-71 Protocol changes 72-72 References.. 73-85
Section A. Complete protocol Azithromycin for Prevention of COPD Exacerbations Summary: The objective of this proposal is to determine if chronic administration of a macrolide antibiotic will reduce the morbidity of COPD. The rationale supporting the importance of this study is that (1) the prevalence, morbidity, mortality and treatment cost of COPD are high and increasing; (2) a large fraction of the morbidity and cost is attributable to acute exacerbations; (3) macrolide antibiotics have a variety of antibacterial and antiinflammatory properties that, in theory, could reduce acute exacerbations; and (4) long-term administration of macrolide antibiotics has resulted in clinically important improvements in patients with a number of other pulmonary disorders. The specific aim is to determine if administration of azithromycin for one year will decrease the frequency and/or the severity of COPD exacerbations. The research design is a prospective, randomized, double-blind, placebocontrolled clinical trial. The methods involve selecting 1130 patients with at least moderately severe COPD who, based on clinical indicators, have an increased likelihood of experiencing an acute exacerbation during the study period. Exclusion criteria include a variety of conditions or medications known to adversely interact with macrolides. Monitoring will occur monthly and include a careful assessment of possible macrolide-related side effects. The primary endpoint is time to first
COPD exacerbation. Secondary endpoints include the incidence of macrolideresistant bacterial colonization, quality of life and cost-effectiveness.
Research Design This is a prospective, randomized, double-blind, placebo-controlled trial that will enroll 1130 patients with at least moderately severe COPD over a two year period and follow them at monthly intervals for one year (Figure 1). The primary endpoint is time to first acute exacerbation. Secondary endpoints are described below.
Figure 1. Patient Contact Flow Diagram (Time in Months)
0
Enroll
10
11
12
13
Clinic Visit Phone Contact
Clinic Visit Phone Contact
Clinic Visit Phone Contact
Clinic Visit Phone Contact
Clinic Visit Washout Visit
Hypothesis Administration of azithromycin for one year will decrease the frequency and the severity of COPD exacerbations when added to the usual care of these patients.
Inclusion Criteria 1. Male and female subjects, 40 years of age 2. Clinical diagnosis of at least moderate COPD as defined by the GOLD criteria (Pauwels, 2001): a. Postbronchodilator FEV1/FVC < 70%, b. Postbronchodilator FEV1 < 80% predicted, with or without chronic symptoms (i.e., cough, sputum production). 3. Cigarette consumption of 10 pack-years or more. Patients may or may not be active smokers. 4. To enrich the population for patients who are more likely to have acute exacerbations (Niewoehner, 2004), each subject must meet one or more of the following 4 conditions a. Be using supplemental O2. or will have a history of b. Receiving a course of systemic corticosteroids for respiratory problems in the past year, c. Visiting an Emergency Department for a COPD exacerbation within the past year, or d. Being hospitalized for a COPD exacerbation within the past year 5. Willingness to make return visits and availability by telephone for duration of study.
Exclusion Criteria 1. A diagnosis of asthma established by each study investigator on the basis of the recent American Thoracic Society/European Respiratory Society guidelines (Table 3). Table 3: Clinical Features Differentiating COPD & Asthma (Modified from NICE Guidelines, 2004)
History Smoker or ex-smoker Symptom onset < 35 yrs Chronic productive cough Breathlessness
COPD Nearly all Rare Common Persistent and progressive
Asthma Possibly Common Uncommon Variable
Nighttime waking with breathlessness and wheeze Significant diurnal or day-today variation of symptoms
Uncommon
Common
Uncommon
Common
If, after applying the above criteria, the clinicians are still unsure about the distinction in a specific patient bronchodilator testing with inhaled albuterol will be performed and patients with changes in FEV1 > 400 mL will be excluded.
2. The presence of a diagnosis other than COPD that results in the patient being either medically unstable, or having a predicted life expectancy < 3 years. 3. Special patient groups: prisoners, pregnant women, institutionalized patients 4 Women who are at risk of becoming pregnant during the study (premenopausal) and who refuse to use acceptable birth control (hormonebased oral or barrier contraceptive) for the duration of the study. 5. Patients with a history of hypersensitivity to any macrolide antibiotic. 6. Patients taking any of the following medications a. Cisapride (which has been removed from the U.S. market) b. Ergot derivatives: Cafergot, Ergomar, Wigraine, Migrainal, D.H.E.45 c. Pimozide (Orap) d. Disopramide (Norpace) e. Cyclosporin (Gengraf; Neoral; Restasis; Sandimmune) f. Tacrolimus (Prograf; Protopic) g. Nelfinavir (Viracept) h. Bromocriptine (Parlodel) i. Hexobarbital (Evipan; Hexenal; Hexobarbitone)
7. A manually determined QTc interval measured at least one hour after use of any short-acting inhaled 2 agonist that exceeds 450 ms on two
occasions separated by at least one week. Manual determinations are only to be done if the automated QTc estimate exceeds the 450 ms limit.
The method that should be used to determine the QTc interval manually is to measure the mean QT interval from the beginning of the QRS complex to the end of the T wave, in a minimum of 3 cardiac cycles, in leads II and V5 or V6 (using the lead in which the QT is the longest). This QT interval is then corrected for heart rate using Federicias formula (QTc= QT/RR(sec)).
Bundle branch blocks prolong the QT interval. Accordingly, patients with either left or right bundle branch blocks should have the JT interval measured. Subjects with a JT interval > 420 msec (corrected for heart rate) should be excluded.
It is recommended that a cardiologist specializing in arrhythmias and/or ECG interpretation perform the above manual analysis and evaluate all ECGs of patients with bundle branch blocks.
Patients should also be excluded if they have a history suggesting increased risk for developing torsade de pointes (e.g., heart failure, hypokalemia, family history of Long QT syndrome), or if they are taking other medications that prolong the QT interval (table).
Anti-arrhythmic / abnormal heart Amiodarone Cordarone rhythm Anti-arrhythmic / abnormal heart Amiodarone Pacerone rhythm Arsenic trioxide Bepridil Chloroquine Trisenox Vascor Arelan Anti-cancer / Leukemia Anti-anginal / heart pain Anti-malarial / malaria infection Anti-psychotic/ Anti-emetic / Chlorpromazine Thorazine schizophrenia/ nausea
Females>Males,TdP risk regarded as low Females>Males,TdP risk regarded as low
Females>Males
Restricted availability; Cisapride Propulsid GI stimulant / heartburn Females>Males. Clarithromycin Biaxin Antibiotic / bacterial infection Anti-arrhythmic / abnormal heart Disopyramide Norpace rhythm Anti-arrhythmic / abnormal heart Dofetilide Tikosyn rhythm not available in the United Domperidone* Motilium Anti-nausea / nausea States Sedative;Anti-nausea / anesthesia Droperidol Inapsine adjunct, nausea Antibiotic;GI stimulant / bacterial Erythromycin Erythrocin infection; increase GI motility Antibiotic;GI stimulant / bacterial Erythromycin E.E.S. infection; increase GI motility Halofantrine Halfan Anti-malarial / malaria infection Anti-psychotic / schizophrenia, Haloperidol Haldol agitation Females>Males Females>Males Females>Males Females>Males
Anti-arrhythmic / abnormal heart Ibutilide Corvert rhythm Opiate agonist / pain control, Levomethadyl Orlaam narcotic dependence Mesoridazine Serentil Anti-psychotic / schizophrenia Opiate agonist / pain control, Methadone Methadose narcotic dependence Opiate agonist / pain control, Methadone Dolophine narcotic dependence Anti-infective / pneumocystis Pentamidine NebuPent pneumonia Anti-infective / pneumocystis Pentamidine Pentam pneumonia Pimozide Orap Anti-psychotic / Tourette's tics Anti-arrhythmic / abnormal heart Procainamide Pronestyl rhythm Anti-arrhythmic / abnormal heart Procainamide Procan rhythm Anti-arrhythmic / abnormal heart Quinidine Quinaglute rhythm Anti-arrhythmic / abnormal heart Quinidine Cardioquin rhythm Anti-arrhythmic / abnormal heart Sotalol Betapace rhythm Sparfloxacin Thioridazine Zagam Mellaril Antibiotic / bacterial infection Anti-psychotic / schizophrenia Females>Males Females>Males Females>Males Females>Males Females>Males Females>Males Females>Males Females>Males Females>Males
8. Patients taking rifabutin or rifampin (as these medications reduce macrolide plasma levels). 9. Patients with chronic hepatic insufficiency (defined as an INR > 2.0 for subjects not taking warfarin, a serum albumin < 3.0 g/dL, or levels of aspartate and alanine aminotransferases three times the normal value). 10. Patients with chronic renal insufficiency (defined as a serum creatinine > 1.5 mg/dL or an estimated creatinine clearance < 20 mL/min using the simplified equation derived from the Modified of Diet in Renal Disease study [i.e., GFR, in mL/min per 1.73 m2 = 186.3 x ((serum creatinine) -1.154) x (Age-0.203) x (0.742 if female) x (1.21 if African American) (Levey, 1999; 2000). 11. Patients otherwise meeting the inclusion criteria will not be enrolled until they are a minimum of four weeks from their most recent acute exacerbation (i.e., they will not have received a course of systemic corticosteroids, an increased dose of chronically administered systemic corticosteroids, and/or antibiotics for an acute exacerbation for a minimum of four weeks). 12. A clinical diagnosis of bronchiectasis defined as production of > one-half cup of purulent sputum/day. 13. Patients with age-adjusted hearing thresholds 95th percentile at any one of 500, 1000, 2000, and 4000 Hz in either ear on initial screening audiometry, or on formal audiometry testing if the latter is obtained
10
Outcome Measures The primary endpoint of this study is the time to first occurrence of an acute COPD exacerbation during the one-year treatment period. Secondary outcomes are: 1. The number of acute exacerbations occurring within 12 months of randomization 2. The number of ED visits resulting from acute exacerbations 3. The number of hospital admissions resulting from acute exacerbations 4. The number of hospital days resulting from acute exacerbations 5. The incidence of presumed macrolide-related side-effects 6. The incidence of presumed macrolide-related side effects that require cessation of treatment 7. The incidence of macrolide-resistant bacterial colonization of the nasopharynx or sputum 8. The incidence of pneumonia or acute bronchitis in patients who do and do not become colonized with macrolide-resistant bacteria 9. Quality of life 10. Cost-effectiveness
Acute exacerbations are defined as a "complex of respiratory symptoms (increase or new onset) of more than one of the following: cough, sputum, wheezing, dyspnea, or chest tightness with a duration of at least three days
11
requiring treatment with antibiotics and/or systemic steroids " (Niewoehner, 2004).
Acute exacerbations will be graded according to the following scale: 1. Mild (home management, with or without contacting a health care provider) 2. Moderate (requiring a visit to an Emergency Department) 3. Severe (requiring hospitalization) 4. Very severe (requiring intubation and mechanical ventilation)
When patients report that they have had a moderate, severe or very severe exacerbation the hospital records of that encounter will be obtained and reviewed.
Statistical Design Sample Size The primary endpoint is time to first acute COPD exacerbation within 12 months of randomization. Because Niewoehner and colleagues (2004) found that identically selected patients had an incidence of acute acute exacerbations of 38% over 6 months, we anticipate that approximately 50% of the subjects in our Control group will have an exacerbation within 12 months. Previous data also indicate a one-year death rate of approximately 3% in similarly selected patients. The treatment effect and the dropout rate (i.e., non-compliance with
12
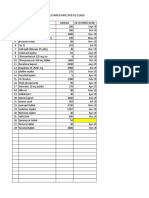
study medication) are not known. Table 1 shows the required total projected sample size for the study, based on plausible assumptions for these parameters. The projected reduction in event rates from the Control group to the Azithromycin-treated group is the most important determinant of sample size. A 25% reduction (50% vs. 37.5%) in perfect compliers yields a required sample size of 724, assuming there is a 20% noncompliance rate with the assigned medication at the end of a year, and that 6% of participants either die or are lost to follow-up. But a 20% reduction, with the other assumptions not changed, requires that 1130 subjects be randomized. Based on the findings of Sin and colleagues (2003) with respect to the effect of other treatments on acute COPD exacerbations, we believe that a 20% treatment effect in perfect compliers is more likely, so our total sample size goal is N = 1130. Table 1: Total Required Sample Size Under Various Assumptions (Two-sided significance level 0.05, power = 85%)
Event Rates (Control vs. Azithromycin, Perfect Compliers) 50% vs 40% 50% vs 40% Death + Loss Non-Compliance Rate To Followup Rate 0% 5% 6% 6% Total Sample Size 870 957
Randomization Method
13
Randomization was stratified by each site with separate schedules created for each. A matched schedule was retained in each site's pharmacy, where separate supplies of capsules containing study drug or placebo were also kept. Only the pharmacist and the staff of the Data Coordinating Center (DCC) knew this schedule and the pharmacists could not know the actual assignment until after the DCC specified an accession number. Treatment assignment was only disclosed in cases of emergency. Randomization will be carried out by linking to the Data Coordinating Center through a website, (http://www.copdcrn.org) using a required COPD Clinical Research Network (CCRN) User ID and password. After securing entry a menu listing the clinical sites appears. The user must choose one of these for example, the Health Partners site is labeled as Center 3b: Health Partners, Minnesota CCRN. After choosing a clinical site and validating the identity of the clinic, a second menu appears that lists a series of activities (e.g., ID assignment, Data Entry, Error Correction, Randomization, Adverse Event Reporting, etc.). To randomize a patient into this protocol the coordinator clicks on the hyperlink labeled Randomization and from there, to the hyperlink labeled Macrolide Randomization. The program will verify that eligibility criteria are met. Verification necessitates that data from all forms bearing on eligibility have been completed and transmitted to the Data Coordinating Center including: 1. Demographics 2. Physical exam
14
3. Medical history 4. Medications 5. Lung function 6. Informed consent Randomization will be halted if required data are missing or if eligibility criteria are not met. If any of these forms are not in the DCC database, or if any eligibility criteria contained in them are not met, a message will appear explaining what the problem is and randomization will be halted. The associated treatment assignment will not be issued until all criteria are met. Each participant may receive only one randomization assignment. Randomization is stratified by each designated site in each clinical center. As an example, the Minneapolis clinical center has three sites: the VA Hospital in Minneapolis, Health Partners, and the Mayo Clinic. Separate schedules are created for each. If all eligibility criteria are met the randomization program will issue a treatment assignment number such as 113. This number matches a schedule that is retained in each site's clinical pharmacy, where separate supplies of capsules containing the active drug and the placebo are also kept. The only person knowing this schedule will be the pharmacist and the DCC. When the clinic coordinator requests pills for treatment assignment #113, the pharmacist will check the schedule and distribute the assigned drug from the appropriate pharmacy supply. The actual assignment will only be revealed in cases of emergencies where caregivers need to know what drugs the person was taking
15
to provide treatment, or to avoid prescribing other medications that might adversely interact with the study drug. Active-drug and placebo capsules will be identical in appearance. Clinic staff will make no attempt to determine the content of any capsules except in cases of emergency. It will be clearly explained to each study participant that they will be assigned to use either active drug (azithromycin) or placebo, that the treatment assignment is random (i.e., cannot be predicted in advance, like the outcome of a coin-flip), and that they should not attempt to discover the content of the capsules. Each time the participant returns for a renewed supply of capsules, the clinic coordinator must request that the pharmacist distribute pills for that specific participants treatment assignment number, referring to the schedule in the pharmacy. If the participants treatment assignment number is lost or forgotten, the information can be obtained by contacting the pharmacy or the DCC.
Data Analysis An appropriate analysis for the primary endpoint is an intent-to-treat analysis based on life-table (i.e., survival analysis) methods. To adjust for differences in pre-randomization factors such as age, gender, prior history of exacerbations, lung function, and other important predictors of exacerbation, a Cox proportionalhazards model analysis will also be carried out, with time-to-first-exacerbation as
16
the outcome variable and treatment group (i.e., azithromycin vs placebo) as the primary variable of interest. Additional analyses will be conducted in which the variable of interest is the repeated occurrence of COPD exacerbations. The methodology in this case will be either Poisson regression, or repeated measures regression for categorical data (implemented in PROC GENMOD in SAS). This analysis also permits entering other variables in the analysis. Secondary analyses will be carried out in which the effects of compliance with the study medication are taken into account. This can be done using Cox
regression with time-dependent covariates (for time-to-event outcomes), or a generalized estimating equation approach. Both permit the inclusion of timevarying risk factors. Additional secondary analyses will be conducted to detect differences in severity of COPD exacerbations. These will include (1) time-to-event analyses for the more severe outcomes (i.e., exacerbations requiring hospitalization or resulting in death), and (2) analyses based on scoring of the severity of exacerbation as described above. These analyses will be carried out using repeated measures analyses based on generalized estimating equation (GEE) methods, which can take the effects of baseline risk factors into account. Analyses of other secondary outcomes (side-effects, bacterial colonization, secondary bacterial infections, etc) will be done similarly using either survivalanalytic approaches to time-to-event data, or repeated measures analyses.
17
Sequential Analysis and Monitoring Boundaries Because approximately 1130 participants will be randomized over an estimated period of two years and will receive either a macrolide antibiotic (AzithromycinTM) or a matched placebo for a period of one year, the study will take a minimum of three years to complete. The Data and Safety Monitoring Board (DSMB) will meet approximately every 6 months to review recruitment, follow-up rates, compliance, safety and efficacy. Repeated reviews of endpoint data involve the problem of multiple statistical testing performed on a set of accumulating data. As a solution to this problem we will adopt a group sequential method of analysis related to that proposed in the 1970s (O'Brien, 1979). Such procedures typically require large critical values (or boundaries) early in the trial that decrease as the trial progresses. Because of the conservatism early in the trial, the critical value of the final analysis is close to the nominal critical value. The specific method we propose is a general approach to group sequential testing developed by Kim and DeMets (1987) for which neither the number of looks nor the increments between looks need to be pre-specified. Rather, the Kim-DeMets approach requires only specification of the rate at which the Type I error (which here will be chosen to be = 0.05) will be spent. This procedure allows spending a little of the at each interim analysis in such a way that, at the end of the study, the total Type I error does not exceed 0.05.
18
The exact sequential monitoring plan ultimately adopted for the trial must be approved by the DSMB before any looks at interim data occur. The following is an example of the kind of plan we will propose: We expect to present efficacy-related analyses to the DSMB beginning 12 months after the first patients are randomized, and continuing at 6-month intervals thereafter until all patients have completed one year of follow-up. Thus, there will be interim looks at efficacy data at the time-points and corresponding information times indicated in Table 2. A final analysis will be conducted at 36 months. Two-sided Table 2. Sequential Analysis Information Time Real Time Upper Boundary Lower Boundary Nominal 2-sided p-values 0.00 0M 0.25 12 M +3.36 - 3.36 0.50 18 M +2.76 -2.76 0.75 24 M +2.36 -2.36 0.88 30 M +2.23 -2.23 1.00 36 M +2.07 -2.07
-0.0008 0.0058 0.0182 0.0258 0.0384
tests of significance will be assumed. For this trial, if randomization occurs at a uniform rate over a two-year period, and the hazard of events is constant with the probability that an exacerbation occurs within 12 months of randomization, the following table illustrates the cumulative information time at each of the DSMB looks at the data [we have chosen an alpha-spending function of the form f(t) = * t,
19
where is the two-sided significance level ( = 0.05), and t is information time (0 < t 1)]. We have specified the exponent = 3.0, which produces conservative boundaries for Z-statistics (Table 5). Use of the alpha-spending function approach to sequential monitoring has the advantage that, if necessary, additional looks at the data can be accommodated without affecting the overall probability of Type I error ( = 0.05). Thus, if recruitment takes longer than expected, analyses of the data for DSMB meetings may occur at information times which are different from those shown above. A disadvantage of the alpha-spending function approach (versus doing a single analysis at the end) is that, although it preserves the overall Type I error level, it results in a small decrease in power (Jennison, 2000). We have specified a total sample size of N = 1130 for this trial to achieve 85% power, as shown in Table 3, on the assumption that one significance test will be performed at the end, and this is probably near the limit of what the participating clinical centers will be able to recruit in a 2-year period. Taking into account the decrease in power associated with this sequential monitoring plan, the power of the trial will be approximately 83% rather than 85%. Judgment concerning the continuation or termination of the study will involve not only the degree of statistical significance observed at the interim analysis, but also the likelihood of achieving significance should enrollment continue to the original projected sample size. As an aid in this assessment, the DCC will supplement the group sequential analysis outlined above with calculations of conditional power based on the method of stochastic curtailment (also known as
20
futility analysis, Halperin, 1982; Lan, 1982; Ware, 1985). This procedure evaluates the conditional probability that a particular statistical comparison will be significant (or not significant) at the end of the trial at the level used in the design, given the hypothesized treatment difference and the endpoint data accumulated to date. Conditional power for the primary endpoint will be computed and provided to the DSMB as part of the interim study reports, and will include calculations based on the originally hypothesized treatment difference as well as the observed treatment difference up to that point in the trial. The DSMB will have a particularly valuable role in its recommendations to the Steering Committee and the NHLBI if there emerges any statistically extreme benefit or harm. The DSMB will need to put any such interim in proper perspective. If protocol modifications are warranted, close consultation among the Steering Committee, the DSMB, and the NHLBI staff will be needed.
21
Schedule of Study Interventions (Figure 2)
Enrollment (two visits) 1. Demographics (including age, gender, ethnic group, smoking history, 02 use were obtained by history), information regarding where the patient might be seen in an emergency department (ED) and/or hospitalized, should this be required during the course of the study, primary care physician name and contact information. 2. A medical history and physical examination that includes recording a list of all medications, allergies, menopausal status (women), whether the
22
patient has received influenza and/or pneumococcal pneumonia vaccination and if so, when, whether they have subjective hearing loss, a list of all coexisting diseases or conditions, whether they have chronic bronchitis (defined in American Thoracic Society, 1987), previous COPDrelated ED visits and hospitalizations (including whether they have previously required invasive or non-invasive mechanical ventilation), a BMI determination, and a resting SpO2 on the prescribed amount of supplemental O2 being given, if any, or on air. 3. FEV1 and FEV6 measured 15 min after inhalation of two puffs of albuterol (Ferguson, 2000; Hankinson, 2003). 4. An ECG 5. The Hearing Handicap Inventory for the Elderly (screening version) questionnaire. Those with scores 10 will be referred for formal audiometry testing. All others will undergo a screening audiogram (with testing at 500, 1000, 2000, and 4000 Hz). Patients with 95th percentile age-adjusted hearing thresholds at 500, 1000, 2000, or 4000 Hz in either ear on either screening audiograms or formal audiometry testing will be excluded unless there is an obvious extenuating explanation (e.g., complete cerumen impaction). Those with 75th and < 95th percentile age-adjusted hearing thresholds at any two frequencies in either ear on screening audiometry will undergo formal audiometry testing to establish their basal level of hearing.
23
6. Quality of life assessment. General quality of life will be assessed by the Medical Outcomes Study 36-Item Short Form (the SF-36) to allow the results to be compared with those in other studies. General quality of life will also be assessed by the Quality of Well-Being Scale to allow estimation of quality-adjusted life years (QALYs), an important element for cost-utility analysis (see below), and to assess the net result of possible gains from the treatment being offset by side-effects that adversely affect health-related quality of life. Sleep quality will be assessed using the Pittsburgh Sleep Quality Index (PSQI). Disease-specific quality of life will be assessed with the St. George's Respiratory Questionnaire, an instrument that was developed and validated in patients with COPD and may be more responsive to the intervention planned than the two general instruments being administered. A change of 4 units between the time point at which the SGRQ is assessed will be considered the minimal clinically important difference and the percent of patients achieving 4 unit change will also be assessed. 7. Cost effectiveness will be assessed by calculating the ratio of incremental costs to the ratio of incremental QALYs. The same methods used to estimate the cost effectiveness of lung volume reduction surgery (National Emphysema Treatment Trial Research Group, 2003) will be employed. QALYs will be determined from the Quality of Well-Being questionnaire as noted above.
24
8. Depression screen. All patients will be given the Hospital Anxiety and Depression Scale (HADS) survey. Patients with depression subscale scores of 11 or greater who are receiving their care from one of the enrolling centers will be referred for depression evaluation and/or treatment. Those receiving their care from providers outside the enrolling centers will, with the patient's permission, have these providers informed of the result of the survey, with the suggestion that they might consider referral for evaluation and/or treatment 9. Laboratory studies to include: a. Complete blood count and platelet count b. Blood urea nitrogen and creatinine c. Liver function tests (i.e., aspartate and alanine aminotransferases, alkaline phosphatase, albumin, total bilirubin, and INR) d. Nasopharyngeal swabs and, when possible, expectorated sputum for culture. Sensitivity testing will be done on all pathogens identified. e. Blood will be drawn for measurement of several biomarkers of inflammation. (See biomarker protocol addendum.) f. Blood will also be drawn and stored for future analyses after the white blood cells and the DNA are extracted and the serum is aliquoted. (See genetic protocol addendum.) g. An -1-antitrypsin level should either be available in the chart or obtained at the time of admission.
25
h. HCG (urine or blood) for pre-menopausal women. 10. Basic education about COPD, its treatment and how to recognize acute exacerbations. Patients will also be given a diary to assist with recalling acute exacerbations that are treated at home, without contact with a health care provider. 11. Azithromycin, 250 mg tablets, or an identically appearing placebo, with instructions that the medication should be taken daily. 12. A wallet card indicating that they are participating in the study, may be receiving azithromycin, and that they should not receive any of the medications listed in the exclusion criteria noted above. The card will also contain instructions about stopping the study medication when they are treated for an acute exacerbation with any antibiotic, and about restarting the study medication after the exacerbation has resolved (defined as being one week after completing the course of antibiotics). A letter containing similar information, along with basic treatment guidelines for COPD will also be sent to each patients primary care physician whenever one is identified. 13. A daily diary, on which subjects may keep track of medication changes and illnesses between visits.
Clinic visits Patients will be seen at months 1, 3, 6, 9, and 12 of treatment at which time they will again queried about
26
1. Whether any acute exacerbations occurred within the previous month, and 2. Possible macrolide-related side effects including: (a) Neural: headache, hallucinations, paresthesias, syncope, seizures, aggressive behavior, somnolence, tinnitus, hearing loss, or vertigo. (b) (c) Hypersensitivity: rash, pruritis, tongue or facial swelling Gastrointestinal: diarrhea, vomiting, nausea, abnormal taste, heartburn, or abdominal pain. 3. Patients will also have the following laboratory tests targeting macroliderelated side effects and microbiologic changes: (a) Liver function tests to include: alkaline phosphatase, albumin, aspartate and alanine aminotransferase, INR and bilirubin (b) Nasopharyngeal swabs and, when possible, expectorated sputum for culture. Sensitivity testing will be done on all pathogens cultured. (c) Blood will be drawn for measurement of several biomarkers of inflammation. (See biomarker protocol addendum.) This will occur at visit months 3 and 12. 4. The patient's self-assessment of compliance with the medical regimen will be recorded, as will a pill count and a recording of the output of the MedicTM ECMTM electronic compliance monitor. 5. At each clinic visit patients will be asked to show their study identification wallet card.
27
6. A repeat ECG will be obtained at one month seeking evidence of QT prolongation. 7. Patients receiving phenytoin or digoxin will have drug levels checked every week after beginning the study, with appropriate dose adjustments, until therapeutic levels have been attained. Patients receiving warfarin will have prothrombin times and INRs measured weekly, and those taking theophylline will have theophylline levels measured weekly after starting treatment with appropriate adjustments in dosages until the INR or the theophylline levels are stable and therapeutic. 8. Pre-menopausal women will be queried about their contraceptive use and pregnancy status. Those not using acceptable birth control will be removed from study medication. 9. Patients complaining of worsening tinnitus or the development of, or worsening hearing loss, will have repeat screening audiograms. Those with 95th percentile age-adjusted hearing thresholds at 500, 1000, 2000, or 4000 Hz in either ear will have the study drug discontinued and will undergo formal audiology testing. All others will continue the medication until they undergo formal audiology testing. If, on formal testing 95th percentile age-adjusted hearing loss at 500, 1000, 2000, or 4000 Hz in either ear is found, or if 10 db hearing loss at two frequencies in either ear is confirmed in comparison with previous formal audiometry testing, the patient will no longer take the study medication and will undergo formal testing every months x 3, or until the patient returns to < 95th
28
percentile loss or to their pre-study dB thresholds. All others will remain on the study drug until their subsequent contact. 10. At months six and 12 months the SF-36, the St. George Respiratory Questionnaire, the Quality of Well-Being Scale and post-bronchodilator spirometry will be repeated as will the screening audiogram. Patients with 95th percentile age-adjusted hearing thresholds at 500, 1000, 2000, or 4000 Hz in either ear will have the study drug discontinued and will undergo formal audiology testing. If 95th percentile age-adjusted hearing thresholds in either ear is found, or if 10 db hearing loss at two frequencies is confirmed in either ear in comparison with previous formal audiometry testing, they will no longer take the study medication and formal testing will be repeated every months x 3, or until the patient returns to < 75th percentile loss. All others will remain on the study drug until the subsequent contact. 11. At months three and 12 the Hospital Anxiety and Depression Questionnaire (HADS) and the Pittsburgh Sleep Quality Index (PSQI) will be repeated.
Monthly phone contact and intermittent studies. Patients will be contacted by phone monthly, between clinic visits and queried about 1. Whether any acute exacerbations occurred within the previous month, and
29
2. Whether the patient has any possible macrolide-related side effects (see above) 3. Patients with any of these side effects will be assessed for severity, specifically with regard to whether the medication should be discontinued or reduced in dose. 4. Pre-menopausal women will be queried about their contraceptive use and pregnancy status. Those not using acceptable birth control will be removed from study medication. 5. Patients complaining of worsening tinnitus or the development of, or worsening hearing loss, will have repeat screening audiograms. Those with 95th percentile age-adjusted hearing thresholds at 500, 1000, 2000, or 4000 Hz in either ear will have the study drug discontinued and will undergo formal audiology testing. All others will continue the medication until they undergo formal audiology testing. If, on formal testing 95th percentile age-adjusted hearing loss at 500, 1000, 2000, or 4000 Hz in either ear is found, or if 10 db hearing loss at two frequencies in either ear is confirmed in comparison with previous formal audiometry testing, the patient will no longer take the study medication and will undergo formal testing every months x 3, or until the patient returns to < 95th percentile loss or to their pre-study dB thresholds. All others will remain on the study drug until their subsequent contact.
Wash-out visit
30
Patients will be seen one month after completing the one-year period of treatment and have nasopharyngeal swabs and, when possible, expectorated sputum sent for culture. Sensitivity testing will be done on all pathogens identified. Spirometry will be repeated. Blood will be drawn for measurement of several biomarkers of inflammation. (See biomarker protocol addendum.) Patients will subsequently be contacted by phone at six-month intervals for the duration of the study to inquire about hospitalizations in the preceding month and whether they are or are not continuing to use azithromycin.
Nasopharyngeal swab processing. Nasopharyngeal samples were obtained on enrollment and at months 1, 3, 6, 9 and 12 for culture. Local laboratories identified isolates of S. aureus, Moraxella spp., Haemophilus spp. and S. pneumoniae in any quantity. Isolates were shipped to a central laboratory for storage and batch processing. Organism identification was verified by the central laboratory according to standard guidelines (P. R. Murray, E. J. Baron, J. H. Jorgensen, M.L. Landry, and M. A. Pfaller, (ed.), Manual of clinical microbiology, 9th ed. ASM Press, Washington, DC., 2007). Susceptibility testing was performed by broth microdilution using commercially available panels (TREK Diagnostics Inc., Cleveland, OH). Clarithromycin susceptibility was performed using Etest (AB bioMrieux, Solna, Sweden). All susceptibility testing was performed according to the methods (Clinical and Laboratory Standards Institute. Methods for dilution antimicrobial susceptibility
31
tests for bacteria that grow aerobically; approved standard. 8th ed. Document M07-A8. Wayne, PA: CLSI; 2009) and interpretative criteria recommended by the Clinical Laboratory Standards Institute (Clinical and Laboratory Standards Institute. 2010. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria. Approved guideline M45-A2. CLSI, Wayne, PA.) with the exception of Moraxella spp, for which EUCAST breakpoints were used (European Committee on Antimicrobial Susceptibility Testing (EUCAST, Home page at: http://www.eucast.org). When patients had more than one isolate for which macrolide susceptibility was performed at a given visit, only the most resistant isolate was included. Differences between groups were determined using chi square analysis.
Method for Analyzing Hearing Changes The mean difference in hearing thresholds in patients receiving azithromycin or placebo was determined by comparing the mean thresholds measured at 1000, 2000, 3000 and 4000 Hz in both ears. Differences in thresholds were compared between measurements made on enrollment and at three months, and between enrollment and 12 months.
Method for determining compliance taking study drug as prescribed. The stop date was taken as the date of death if the patient died during the study or the date of the last clinic visit attended prior to the wash-out visit (with a 30 day window for the last scheduled visit).
32
Compliance was determined by dividing the actual number of pills taken by number of days pills should have taken, and was recorded as being 100% if patients took more than the prescribed number of pills during a given time period. Compliances over all time periods were averaged to determine an overall percent compliance/patient. Calculations excluded 25 patients who attended no visits. Since adherence was assessed post hoc the correlations sought between compliance and AECOPDs should not be considered as intention to treat analyses.
Reasons for study drug discontinuation There are five instances in which the study drug might be discontinued: 1. At the start, and for one week following, an acute exacerbation Patients are instructed as to what constitutes an acute exacerbation as described above. In brief, qualifying exacerbations require that the patient be treated with antibiotics and/or systemic corticosteroids. Cards summarizing this information are also given to each patient and sent to their primary care physicians. Patients are instructed to stop the study medication if and when they begin antibiotics, and restart the study medication one week following completion of the course. 2. Development of symptoms that might represent medication-related side
effects. Prior to beginning the study patients are instructed about what might constitute a macrolide-related side effect and whom they should notify should such symptoms develop. They are also queried at each clinic visit and phone
33
contact about a specific list of possible macrolide-related side effects (see above). If potential side effects develop, study personnel will assess the severity of the problem and decide whether the study medication should be discontinued or reduced in dose. Diarrhea is expected to be the most common complaint. Should this be severe enough to warrant intervention we will reduce the study medication to one pill three times a week. If the diarrhea persists on this lower dose the study drug will be discontinued. Although the literature predicts that hearing loss should be rare, if patients complain of a change in their hearing we will repeat their audiograms. Those with documented decrements will have the study drug discontinued. Hypersensitivity and toxic hepatic reactions rarely or never occur as a result of metabolism of azithromycin. Nonetheless, we will measure the standard battery tests used to evaluate the liver at each clinic visit. The study drug will be discontinued in all who have values > three times normal. 3. Intercurrent illness. We anticipate that during the one year treatment period some patients will develop medical and/or surgical problems that are unrelated to COPD or to a possible azithromycin-related side effect but warrant treatment. In these instances the patient's treating physicians will decide whether the specific problem encountered warrants discontinuation of the study medication. Each patient will carry a wallet card for the duration of the study that provides
34
information regarding the study and how unmasking of treatment can be accomplished should the indication merit (see below). 4. If the QTc on ECGs recorded one month after starting the study medication increases to > 500 ms or > 60 ms from the patients baseline value. 5. For patients with a bundle branch block, if the JTc interval increases 60 ms from the patients baseline value.
Recruitment and Retention Enrollment Each of the ten Clinical Centers in the COPD Clinical Research Network plans to enroll patients from up to four separate medical centers and/or from a number of associated outpatient practices (Table 6). We have budgeted 3 hours/week, 48 hours/year for two years for Clinical Coordinator time to be spent on recruiting. This time will be used to visit primary and appropriate specialty care clinics, describe the study to the treating physicians and be available for screening. Each Clinical Center includes outpatient clinics that treat large numbers of patients with COPD and each has experience with advertising to the public and/or to selected groups (e.g., COPD patient support groups, local lung associations). Many of the Centers have dedicated personnel and standardized approaches to advertising that will facilitate the process. The Clinical Coordinator will screen records of patients giving HIPPAcompliant consent, and will seek consent for study participation from all those meeting entry criteria.
35
Retention A variety of factors contribute to patients failing to complete trials or comply with prescribed regimens. We will address issues in each area in an effort to achieve maximal retention and compliance as Rotor and colleagues (1998) found that programs employing educational, behavioral and motivational components are more effective than any single approach. We have developed a comprehensive plan to address each of five domains identified as contributing to patient's adhering to prescribed medical regimens. Socioeconomic factors. In addition to the cost of buying medications patients frequently need sufficient financial resources to cover the cost of traveling to the health care provider, arranging childcare, taking time off from work. Unstable living conditions, low levels of education and poor social support systems contribute to these problems. Patients agreeing to participate in this study will bear no additional expense for medications or testing, and will be reimbursed for their travel-related time and effort. Information regarding the study will be printed in easily understood language aimed at patients with no more than a grade school education. Healthcare team and healthcare system-related factors. Organizational factors such as the time spent with the health care provider, the continuity of care, and the communication style of the provider may improve retention and adherence to a prescribed regimen (Albaz, 1997; Abbott, 1999). We will structure the initial evaluation and all follow-up phone contacts and clinic visits
36
such that the patients interact with the same study coordinator on each occasion. Lack of awareness and knowledge about adherence problems on the part of health care providers may contribute to the problem. Accordingly, all the investigators and coordinators will receive and review the recent WHO report that summarizes the pertinent issues pertaining to adherence (Sebate, 2003). The importance of continuous attention to retention and adherence, and the fact that facilitating compliance is a dynamic process will be emphasized.
Condition-related factors. Condition-related factors include those related to the severity of symptoms, the level of physical, psychological, social and vocational disabilities, the rate of progression, the availability of effective treatments, and the co-existence of depression. To reduce the possibility that these factors will limit compliance with the protocol we will attempt to assure that patients are receiving the optimal treatment for their disease. The co-investigators in this trial concur with the COPD treatment guidelines that are summarized in the GOLD initiative and will utilize these when caring for all of the patients for whom they have responsibility. Unfortunately, this standardized treatment approach cannot be used for all patients as some will be treated by physicians who are not part of the COPD Clinical Research Network. To increase the likelihood that as many patients as possible will receive what is currently perceived to be optimal therapy for their disease all patients will receive an informational pamphlet that reviews appropriate treatment of COPD and recommendations concerning this treatment will also be communicated to their primary care physicians. All patients will be
37
screened for depression. When found treatment will either be administered or recommended. Therapy-related factors. The most important therapy-related factors affecting compliance are the complexity of the medical regimen, the duration of treatment, frequent changes in treatment, the immediacy of beneficial effects, the frequency of side effects, and the availability of medical support to deal with them. In an attempt to facilitate compliance with the prescribed regimen we have chosen a daily dosing regimen (250 mg once daily) despite the fact that it will provide a slightly higher total weekly dose, and run the risk of causing a slightly higher rate of side effects than the 500 mg three times weekly dose that was alternately considered. Patients will be educated as to the side effects that might be expected, and what changes in dosing might occur should they develop. Patients will have ready access to study personnel who will assist them with the appropriate response to any side effect that develops. Patient-related factors. Patient-related factors include their knowledge and perceptions about their illness and their motivations and expectations regarding self-management of their symptoms. To address these factors all patients will receive education about their disease as described above and information pertaining to COPD Support Groups in their respective areas, and they will be queried on a monthly basis about their disease management, their understanding of their treatment instructions and the success or lack thereof they are seeing in response to the intervention. We will also attempt to increase the patients motivation by discussing the perceived importance of adherence, and by
38
teaching self-management skills (e.g., correct bronchodilator inhalation techniques, the importance of exercise, purse-lipped breathing). Choice of macrolide Azithromycin was chosen over the other macrolides for the following reasons: 1. The incidence of medication-related side effects and drug-drug interactions is considerably lower with azithromycin than with clarithromycin or erythromycin.
Clarithromycin and erythromycin are nonspecific P450 enzyme inhibitors, specifically CYP3A4, the enzyme involved with the metabolism of the largest number of medications (i.e., calcium channel blockers, statins, dihydropyridines, disopyramide, benzodiazepines, quinidine, protease inhibitors, non-sedating antihistamines, and many psychiatric medications).
Azithromycin does not interact with the cytochrome P-450 system. There is a single case report of azithromycin interacting with disopyramide, and a number of studies have shown that azithromycin does not interact with statins, non-sedating antihistamines, psychiatric medications, and benzodiazepines.
Contraindications.
39
The only contraindication listed in the package insert for azithromycin is giving it to patients with known hypersensitivity to macrolide antibiotics.
Warnings. Warnings included in the package insert are for serious allergic reactions and antibiotic-associated pseudomembranous colitis from C. difficile toxin.
Precautions. The package insert cautions against giving azithromycin to patients with impaired hepatic function and those with glomerular filtration rates < 10 mL/min. We are excluding patients with INRs > 2.0 (unless they use warfarin), a serum albumin < 3.0 g/dL, a serum AST or ALT > 3 times normal, or patients with a serum creatinine > 1.5 mg/dL or an estimated creatinine clearance < 20 mL/min.
Prolonged QTc intervals, with the attendant risk of cardiac arrhythmias (including torsades de pointes), have been seen in patients treated with macrolides other than azithromycin. This repolarization delay is results from blockade of specific potassium channels, and is most commonly seen with erythromycin (generally with intravenous administration), clarithromycin, and patients with preexisting heart disease (Iannini, 2002). QTc prolongation is also seen when macrolides are given with other medications that are metabolized by cytochrome CYP3A4 (e.g., the non-
40
sedating antihistamines and cisapride). Harris and colleagues (1995) found that azithromycin (500 mg for 1 day and 250 mg on 4 subsequent days) did not prolong the QTc interval and had no additive effect on terfenadine-induced QTc prolongation. Strle and Maraspin (2002) prospectively studied 47 patients given azithromycin (3 g divided over 5 days). All were previously healthy. The median QTc increased from 406 to 419 ms (P = NS) and the same proportion of patients had QTc > 440 ms prior to, and after treatment. In vitro studies indicate that, despite have similar effects on QT prolongation, erythromycin and clarithromycin have greater pro-arrhythmic potentials compared with azithromycin (Milberg, 2002). Nonetheless, the package insert states cautions that an effect of azithromycin on the QTc interval "cannot be completely ruled out in patients at increased risk for prolonged cardiac repolarization". We are excluding patients with a QTc interval > 440 msec on either their screening ECG or on an ECG repeated one month after beginning the study. The risk of development of drug-resistant bacteria is also mentioned as a precaution (see below).
Drug Interactions. The package insert lists the following drug interactions:
41
(a) Co-administration of nelfinavir increases azithromycin concentrations. Accordingly, use of nelfinavir is one of our exclusion criteria. (b) Azithromycin does not affect the prothrombin time or INR in response to a single dose of warfarin but concurrent use of macrolides and warfarin has been associated with increased anticoagulant effects. We will follow the package insert recommendation and monitor the INR in all patients taking warfarin as noted above. (c) Therapeutic doses of azithromycin cause a "modest" effect on the pharmacokinetics of atorvastatin, carbamazepine, cetirizine, didanosine, efavirenz, fluconazole, idinavir, midazolam, rifabutin, sildenafil, theophylline, triazolam, trimethoiprim/sulfamtehoxazole and zidovudine. Co-administration with efavirenz or fluconazole has a "modest" effect on the pharmacokinetics of azithromycin. "[N]o dosage adjustment of either drug is recommended". (d) Although interactions with digoxin, ergotamines, terfenadine, cyclosporine, hexobarbital and phenytoin have not been reported in clinical trials, no specific drug-interaction studies have been performed to evaluate potential interactions with these medications, and other macrolides have been found to increase digoxin levels or result in severe peripheral vasospasm and dysesthesias in patients taking ergotamines,. Monitoring terfenadine, cyclosporine, hexobarbital and phenytoin concentrations is advised. Accordingly, we will monitor drug levels on all patients enrolling in the study who are taking phenytoin or digoxin.
42
Patients taking ergot alkaloids, terfenadine, cyclosporine, or hexobarbital are excluded.
Medication-related side effects Gastrointestinal. With long-term administration of azithromycin diarrhea occurs in from 0% [with 250 mg given either daily (Wolter, 2002) or three times per week for 3 months (Gerhardt, 2003)] to 25% of subjects [in those receiving 500 mg twice-weekly for six months (Cymbala, accepted pending review, personal communication)]. In the largest study, diarrhea occurred in 20% of treated patients compared with 8% of controls (Saiman, 2003). The need to discontinue therapy because of diarrhea is rare, however, (maximum reported occurrence 8% (Cymbala, accepted pending revision, personal communication). Nausea occurs in 29% of patients (compared with 16% of controls), but does not seem to result in study drop-out (Saiman, 2003).
If patients develop diarrhea that is severe enough to warrant intervention we will first attempt to reduce the frequency of the study medication to three times a week. If the diarrhea persists on the lower dose the study drug will be discontinued.
Ototoxicity. The incidence of ototoxicity is 21% in patients taking 4 g/day of erythromycin (Swanson, 1992). Symptoms can begin within the first
43
week of treatment but are usually reversible within 30 days of discontinuing the drug (Brummett, 1993). Irreversible changes have been reported with intravenous administration, however. The mechanism of this adverse reaction is unknown but is thought to be dose-dependent (Taylor, 1981; Swanson, 1992), and predisposing factors include renal abnormalities, advance age, high doses, and concurrent use of other ototoxic medications (Haydon, 1984; Umstead, 1986; Vasquez, 1993).
Ototoxicity has only rarely been reported with azithromycin but the incidence is unknown (Wallace, 1994). Saiman and colleagues (2003) reported that two of 185 patients reported hearing impairment and that two others noted tinnitus. Interestingly, these complaints were equally divided between patients receiving azithromycin and placebo.
We will inquire about hearing and balance problems in all patients prior to instituting therapy, obtain a screening audiogram, and obtain additional audiograms on all patients reporting tinnitis or the development of hearing impairment during the course of the study.
Hepatotoxicity and hypersensitivity reactions. Hypersensitivity and toxic hepatic reactions occur in response to nitrosoalkanes formed from the metabolism of erythromycin. Nitrosoalkanes rarely or never form as a result of metabolism of azithromycin. We will measure the standard
44
battery tests used to evaluate the liver at each clinic visit and stop treatment if they are elevated to the extent described above.
2. Although clarithromycin produces higher mean and maximum plasma concentrations, a greater area under the 24-hour plasma concentrationtime curve, and a higher concentration in alveolar lining fluid and alveolar macrophages than azithromycin when given in comparable doses (Patel, 1996; Rodveld, 1997; Zhanel, 2001), the studies documenting these differences were all done in normal subjects. All of the macrolides concentrate in areas of inflammation due to their basic charge. Azithromycin is dibasic so this occurs to an even greater extent. Accordingly, the data reported in normals may not be relevant to patients with pulmonary inflammation. 3. Although many studies document the clinical benefit of erythromycin or clarithromycin when given to patients with a variety of pulmonary conditions (Table 2), most of these studies utilized observational designs. Two randomized, controlled trials have documented the clinical benefit of azithromycin in patients with cystic fibrosis (Wolter, 2002; Saiman, 2003), and a third showed utility in patients with panbronchiolitis [although a third small, randomized, crossover trial only found that treatment had no substantive effect on airway inflammation and only was associated with fewer uses of additional antibiotics (Equi, 2002)].
45
Choice of dose. The dose of any medication should be the lowest possible that produces clinical effectiveness, taking into account issues that pertain to maximizing compliance with the prescribed regimen. There are no published studies comparing the efficacy or side-effects of different doses of long-term azithromycin. Accordingly, the choice of dose for this study must be empiric. A review of the pertinent literature is as follows:
Efficacy. The two double-blind trials showing efficacy in patients with cystic fibrosis used azithromycin, either 250 mg once daily for three months, or 250 or 500 mg (depending on whether body weight was above or below 40 kg) three days a week for 168 days (Wolter, 2002; Saiman, 2003). One unpublished study in 12 patients with bronchiectasis found reduced sputum volume and fewer exacerbations with azithromycin, 500 mg twice weekly (Cymbala, in press pending revision).
Side-effects and compliance. No subjective sides effects were reported in 61 cystic fibrosis patients who received 250 or 500 mg of azithromycin daily for 6 months (Equi, 2002). In a
second study of cystic fibrosis patients, 6 (25%) of those receiving azithromycin (250 mg daily) did not complete three months of treatment, as did 9 (30%) receiving placebo. Failure to complete therapy was thought to be likely or
46
possibly related to medication-related side effects only 3 of these 15. Compliance, assessed by retrospective questioning, indicated that 29% of the patients receiving azithromycin reported missing doses compared with 40% of those receiving placebo (Wolter, 2002). Side effects in the largest study in cystic fibrosis patients (N = 185) who were treated with 250 or 500 mg of azithromycin three times a week or a placebo were considered to be mild or moderate and included only nausea in 33% vs 16% (azithromycin vs placebo, respectively), diarrhea (23 vs 8%) and wheezing (17 vs 4%) (Saiman, 2003). The dose of the study drug was reduced, or stopped and restarted in 4 (5%) of the treated patients and in 4 (4%) of the controls, and was discontinued in 3 (3%) treated patients and 2 (2%) controls. Pill counts indicated that the patients took 93% of the azithromycin doses and 89% of the placebo. Cymbala and colleagues (unpublished data provided courtesy of Guy Amsden, PharmD) treated 12 patients with bronchiectasis (mean age 71 years, mean weight 76 kg) with azithromycin, 500 mg twice a week, for six months. Three (25%) complained of diarrhea. In one, the dose was decreased to 250 mg three times a week with improvement. Compliance assessed by pill counts ranged from 85 to 108%. We have opted to use a dose of 250 mg daily because it is high enough to exclude the possibility that a negative result is not due to an insufficient dose, and daily (as opposed to three times a week) administration is likely to facilitate compliance (see below).
47
Other or Concomitant Therapy All the investigators in the COPD Clinical Research Network agree with the treatment guidelines summarized in the GOLD initiative (Pauwels, 2001) and, accordingly, will be treating those patients for whom they are the primary care giver in a similar fashion. Patients whose primary care giver is not one of investigators in the Network may be treated differently. To minimize this, each patient will receive a tutorial and printed material summarizing the recommended treatment of his or her disease at the beginning of the study. Letters will also be sent to their primary care physician summarizing these same recommendations.
Non-COPD-related Given the expected age of the patients we will be enrolling many are likely to have one or more medical conditions in addition to COPD. Therapy for these problems will be continued at the direction of each patient's treating physician with the exceptions of the medications listed in the exclusion criteria.
Unmasking Emergency situations may arise in which it is necessary to discontinue the study drug and unmask treating physicians, Emergency Department personnel, clinic personnel, or the patient to the assigned treatment. Participants will be given a wallet-size card explaining that they are in a research study and that they are assigned to take either azithromycin capsules (250 mg/day) or a matched placebo. The card will include telephone numbers of their site's pharmacy, the
48
responsible investigator and the DCC. Patients will be instructed to carry the card at all times; compliance with this instruction will be checked at clinic visits (see above). Situations that require unmasking are expected to be rare. In most emergency situations it will be sufficient to have the participant discontinue taking either the drug or the placebo until the event is resolved. It is possible, however, that emergency personnel or treating physicians might feel it is necessary to know the medication the participant was taking to decide upon a rational course of treatment, or to ensure that other medications are not given that might adversely interact with azithromycin. In such cases the treating medical personnel should call the clinic pharmacy (first choice) or the DCC to obtain the treatment assignment. Adverse events or hypersensitivity reactions may occur which are believed to be definitely or probably associated with the use of azithromycin, and which result in discontinuation of the use of the assigned medication by the participant. In such cases, the participant should be informed of the study drug prescription. The reason for this is to provide information to the participant regarding their use of azithromycin in the future. If the study drug is azithromycin, then the participant should be told that there have been indications that he/she is hypersensitive or reactive to this drug and use of it in the future should be avoided. The participant should also be informed if the study drug is placebo, so that his/her use of azithromycin in the future will not be restricted.
49
Such events must be thoroughly and carefully documented, and an Unmasking Report for the event must be completed and transmitted promptly to the DCC. Such events must be reported to the DSMB on at least a quarterly basis.
12. Data Management
Training A training session for the study personnel who are conducting the protocol (clinic coordinators PIs, pharmacists, lung function techs, others) will be held in a central location (Denver or Minneapolis) prior to startup. Material will be presented covering: 1. Background and rationale for the study (Dr. Albert) 2. Design of the study (Dr. Connett) 3. Recruiting goals and strategies (Dr. Connett and others) 4. Determining eligibility (Dr. Albert and others) 5. Informed consent 6. Randomization procedures and drug dispensation; role of the pharmacy (DCC) 7. Follow-up visit schedule 8. Forms and forms completion 9. Data entry, error correction (DCC) 10. Exacerbations: determination and documentation (Dr. Albert) 11. Adverse events: notification and documentation (DCC)
50
12. Dose adjustment or termination; breaking the blind (Dr. Albert) 13. Monitoring of recruitment, adherence to protocol, compliance, visit completion, other; role of the DSMC (DCC) 14. Post-treatment follow-up (Dr. Niewoehner) 15. Technical procedures (Arranged by DCC): a. Lung function testing b. Blood draws, lab work, and shipping c. Audiometry d. Other 16. Ancillary study: biomarkers (Drs. Albert and Woodruff) a. Background, rationale, and goals b. Procedures to obtain specimens, specimen handling; schedule 17. Closeout and notification of participants (DCC, Dr. Albert) The session will be conducted as an interactive process with questions and answers and practice in procedures, interviews, forms completion, data entry and transmission, and other activities and testing built in. Training of new or replacement personnel will be conducted by sending them to the DCC. Personnel who have unsatisfactory records with respect to performance or error rates will be required to undergo central re-training.
51
Site Visits Each clinical center will be visited at least twice during follow-up by a team assembled by the DCC. Site visitors will review the following aspects of operation: 1. Organizational structure of the clinical center 2. Recruiting methods and strategies 3. Adherence to protocol 4. Visit scheduling, visit completion rates, adherence rates 5. Error rates and timeliness of corrections in data entry 6. Handling of adverse events; unblinding events 7. Compliance 8. Agreement of entered data with raw source documents (review of records) 9. Satellite clinics; communications 10. Exit interview with clinic PI, clinic coordinators, and other staff A brief written report on each site visit will be prepared by the DCC after each site visit and sent to the clinical center PI, the clinic coordinator, and the NHLBI Project Office.
Data flow Data from interviews, lab reports, and most other sources of information will be collected on printed paper forms. Spirometry will be obtained using studystandard systems.
52
After forms have been completed, personnel in each Clinical Center will enter the data by accessing the website (http://www.copdcrn.umn.edu). A CCRN User ID and password will be required to link to this site. After securing entry, a menu of clinical sites will appear. The user must choose one of these. After choosing a site and validating the identity of the clinic, a second menu will appear that lists the available activities (see above). For data entry, clinic personnel will need to click on 'Data Entry'. A list of currently open studies will appear. The data enterer will select Macrolide Study from a hyperlinked list of all forms. The data enterer will then select the specific form to be used. Data will be edited at the time of entry. The data entry program inserts data directly into the database at the DCC. An additional and more comprehensive edit will take place each day at the DCC. This may result in requests for error correction that will be e-mailed to the clinical center. Data management at the DCC makes use of Oracle databases running on a Unix network. All files are automatically backed up, with backup files stored offsite, on a daily basis. To ensure confidentiality and security, all data transmitted to or from the DCC, whether through the CCRN website or via e-mail, is fully encrypted. The DCC will make available current reports on recruitment, randomization, visit completion rates, forms completion and accuracy, adherence to protocol, compliance, serious adverse events, and other information, both by clinical center and for all centers combined. These will be regularly posted on the CCRN
53
website. They will be accessible only to personnel with registered User IDs and passwords.
Quality Assurance and Quality Control Assurance of data quality will be facilitated by: 1. Online availability of a study-specific Manual of Procedures 2. Clear, well-designed forms and form-modules with most terminology defined on the forms themselves 3. Training of clinic personnel in the following aspects of the study: a. Design and rationale b. Target population and recruitment c. Eligibility d. Informed consent procedures e. Randomization f. Allocation of assigned medication g. Follow-up visit scheduling and procedures h. Reporting COPD exacerbations i. j. Reporting adverse events Data entry, transmission, and error correction
k. Spirometry and associated data transmission l. Audiometry
m. Unmasking treatment assignment n. Reporting protocol violations
54
o. Closeout of the study for the participant 4. Interactive editing at the time of data entry 5. Comprehensive editing of data at the DCC 6. Site visits by DCC and other study personnel 7. Regular, frequent preparation of monitoring reports, and review of these reports with clinic coordinators 8. Monitoring of quality of lung function testing; over reading of spirometry data 9. Frequent communication by phone and e-mail between the DCC and clinic personnel 10. Periodic review of data on safety, toxicity, efficacy, and study operation by the Data and Safety Monitoring Committee A special consideration regarding data quality in this study is the review and definitive classification of COPD exacerbations by (1) an expert coder in the DCC, and (2) a 3-member panel of investigators who will be masked to participant ID and treatment assignment. The panel will review admission and discharge summaries for all hospitalizations, emergency department visits, and physician summaries for all outpatient events, assess whether each event was in fact a COPD exacerbation and, if so, whether it was mild, moderate, severe or very severe. The same panel will review any patient deaths that occur during the study attempt to determine the primary and secondary causes.
Reports to Data and Safety Monitoring Board
55
Interim reports to the Data and Safety Monitoring Board (DSMB) will be carried out at monthly and 6-monthly intervals. Monthly reports will include a graphical comparison of actual and target enrollments. Six-monthly reports will include follow-up rates, adverse events, mortality, levels of compliance, losses to follow-up, and data on the primary and secondary outcomes. We are proposing a group-sequential monitoring plan to provide guidelines for termination of the trial in the event that the results are strongly positive, as discussed in the Sequential Analysis and Monitoring Boundaries section on page 9. The DCC will establish a secure website and a process for e-mail notification that will expedite reviews of serious adverse events by the DSMB while maintaining subject privacy. Reports of adverse events and study results will be presented in a manner that maintains blinding of the DSBM with regard to treatment assignment but the DCC will be prepared to identify the treatment groups (independently for adverse events and study results) if requested by the DSMB.
Limitations Exclusion of patients with asthma. The degree of reversibility after bronchodilator inhalation has previously been used to distinguish patients with asthma from those with COPD. There are, however, a number of problems with this approach. First, there is no consensus regarding what variable to use to define reversibility. Second, regardless of how
56
one defines reversibility, there is no consensus regarding the degree of reversibility needed to conclude that patients have asthma. A recent study of 660 COPD patients found that the maximum change in FEV1 in response to salbutamol (expressed as a percent of the normal predicted FEV1) was 12%. When both salbutamol and ipratropium were given together, however, the percent increase was as much as 26% (Calverley, 2003). The maximum absolute change in FEV1 was 0.7 L, and the change in FEV1 (expressed as a percent of the pre-bronchodilator FEV1) was as much as 70% (Calverley, 2003). In patients with very low FEV1s some suggest using the absolute increase in the FEV1 to define reversibility, but the degree of change distinguishing asthma has been variable (e.g., 200 or 400 mL) and arbitrary. Others have found that the absolute change in FEV1 is unrelated to the FEV1 whereas the percent change was correlated (Tweeddale, 1987; Calverley, 2003). Third, there is considerable day-to-day variability in the change in FEV1 in response bronchodilators, both between and within individuals (Anthonisen, 1986; Tweeddale, 1987; Nisar, 1992). Fourth, bronchodilator testing can yield different results if the test is performed with different inspiratory maneuvers (Santus, 2003). Bronchodilator testing was included in previous British Thoracic Society guidelines and in the GOLD initiative, but is not recommended in the latest ATS/ERS guidelines that goes on to suggest that asthma can be excluded by a combination of the clinical history, signs and baseline spirometry, and that reversibility testing does not add any additional information. This position is supported by a recent study of patients diagnosed as having either COPD or
57
asthma on the basis of the clinical history who subsequently underwent bronchial biopsy and had induced sputum evaluated for differential cell counts. The authors found that the clinical diagnosis was correct when the pattern of inflammation observed was used as the gold standard (Fabbri, 2003).
13. Microbial Resistance. Long-term antibiotic treatment raises the concern of colonization or infection with macrolide-resistant organisms. Prevalence of S. pneumoniae resistance. Resistance of S. pneumoniae to macrolide antibiotics is increasing. From 1995-1998, resistance to erythromycin increased from 11% to 15% (Whitney, 2000). From 1995 to 1999 data from the Centers for Disease Control found resistance rates increased from 10.6% to 20.4% (Hyde, 2001). Data from the SENTRY Antimicrobial Surveillance Program collected from 1997-1999 found resistance rates to clarithromycin of 16% (and 2.1% and 0.4% for H. influenza and M. catarrhalis, respectively) (Hoban, 2001). Doern and colleagues (2001) found a 26% rate of resistance (and 78% resistance in penicillin-resistant S. pneumoniae). Guchev and colleagues (2004) reported that resistance rates of S. pneumoniae to azithromycin increased from 0 to as much as 40% when patients were cultured 14 weeks after 8 weeks of therapy had been completed.
Mechanisms of resistance. The most common mechanisms of resistance to macrolides are ribosomal methylation and upregulation of efflux pumps.
58
A. Methylation of rRNA. Ribosomal methylation is the most common mechanism of resistance to macrolides, occurring in S. aureus, S. pneumoniae, and H. influenzae. It is mediated by the erm gene that codes for a methyltransferase that methylates adenine 2058 in 23S rRNA, probably resulting in steric hindrance of the macrolide attaching to its binding site (Weisblum, 1995; Poehlsgaard, 2003). Erm(A) is common in staphylocci and S. pyogenes but rare in S. pneumoniae. Erm(B) is most common in S. pneumoniae (depending on geography, see below), other streptococci and enterococci. The mechanism by which macrolides induce erm RNA is not yet known but may be dependent on concentration (i.e., at low concentration too few ribosomes might be occupied to allow for sufficient erm synthesis).
B. Efflux pumps Constitutively expressed efflux pumps having a broad spectra of substrates are thought to account for the poor susceptibility of many Gram-negative organisms to macrolides (Leclercq, 2002; Van Bambeke, 2003). Macrolideinducible pumps in Gram-positive bacteria have narrow spectra resulting in isolates of S. pneumoniae that are susceptible to clindamycin but resistant to macrolides as a result of the effects of mefA (Jones, 1996; Nishijima, 1999). Waites and colleagues found that 97.6% of mefA+ S. pneumoniae isolates had MICs 32 g/ml for clarithromycin, while 97.1% of ermB+ isolates had MICs >
59
256 g/ml. Waites and colleagues (2000) have suggested that the predominance of low-level resistance conferred by mefA may account for the observation that there are only rare reports of treatment failure with macrolides despite increasing in-vitro macrolide resistance, and widespread use of these antibiotics to treat respiratory ailments. A similar conclusion was reached by Nuermberger and Bishai (2004). The etiology of macrolide resistance varies markedly by geographic region (Lynch, 2002): two-thirds of resistant isolates in North America are the result of mefA whereas ermB accounts for the majority of the resistance found in Europe and South Africa, and the marked increase in resistance seen since 1993 is the result of mefA (Gay, 2000; Hyde, 2001). This geographic disparity is such that in many European countries macrolides are no longer recommended as first-line therapy for conditions in which S. pneumoniae or S. aureus are likely organisms (Mulazimoglu, in press). Animal studies. Clarithromycin improves survival in neutropenic mice infected with 8 of 9 macrolide-resistant mefA-producing strains of S. pneumoniae with MICs to clarithromycin ranging from 0.5 to 16 ug/ml, but azithromycin improved survival in only 2 of the 9 strains (with azithromycin MICs of 1-32 ug/mL). Neither medication improved survival in ermB-producing isolates that had MICs > 63 ug/mL (Hoffman, 2003). Tessier and colleagues (2002) found that colony counts decreased in the same model when animals with macrolide-resistant S. pneumoniae were treated with clarithromycin when MICs were as high as 4 g/mL but not when the strain had MICs of 8 g/mL. Unfortunately, these data
60
are difficult to extrapolate to what might be the case in human subjects. First, use of a neutropenic model is a problem in that macrolides (particularly azithromycin) are concentrated within, and carried to sites of infection by, neutrophils. Second, administering S. pneumoniae via the trachea generally results in bacteremia such that outcomes may more likely to depend on serum rather than intraparenchymal drug levels and the latter is thought to be more important in human S. pneumoniae infections as most are not bacteremic. Clinical data. A number of case reports and small series report break-through bacteremia in patients with macrolide-resistant S. pneumoniae who were treated with macrolides [Fogarty, 2000 (N=3); Kelley 2000 (N = 4); Waterer, 2000 (N=1); Musher, 2002 (N=1); Lonks, 2002 (N=19); van Kerkhoven, 2003 (N=4)]. Lisby and colleagues (2001) note, however, that break-through bacteremia also occurs with macrolide-sensitive strains. In addition, most (but not all) of the instances of break-through bacteremia occurred in patients taking oral therapy for species with MICs > 8 g/mL. The study by Lonks and colleagues (2002) in which 19 cases were reported, was conducted over a 13-year period in four hospitals. Only one of these isolates had MICs < 16 g/mL. Nuermberger and Bishai (2004) suggest that (1) while high-level ermB-mediated resistance is associated with occasional treatment failure, the risk of treatment failure in this group of patients is unknown, (2) the risk of treatment failure in patients whose organisms have MICs < 16 mediated by efflux pumps has not been substantiated, and (3) because treatment failures can also occur in patients with drug-susceptible
61
organisms, observing failure in patients with resistant organisms does not establish cause and effect. Several studies have found a survival benefit when macrolides are used to treat either community acquired pneumonia, or bacteremic S. pneumoniae pneumonia (Gleason, 1999; Stahl, 1999; Waterer, 2001; Rello, 2002; Martinez, 2003), and the morbidity and mortality associated with treating community acquired pneumonia with macrolides seems to be the same regardless of whether patients have macrolide-sensitive or macrolide-resistant infections (Ewig, 1999). In summary, many patients are treated with macrolide antibiotics for pneumonia and reports of treatment failure are extremely rare, despite evidence of increasing in vitro macrolide resistance. Clinical consequences of long-term macrolide treatment. Colonization with macrolide-resistant bacteria occurred in a group of HIV-positive patients who were given 12 weeks of either clarithromycin (500 mg twice daily) or azithromycin (1200 mg weekly) as prophylactic treatment for M. avium (Aberg, 2001), but was not observed in a study of cystic fibrosis patients who received azithromycin, 250 mg daily, for three months, (Wolter, 2002). In 10 patients with panbronchiolitis treated with long-term clarithromycin sputum cultures turned negative at 0.5 years in two, one year in two more, and at two years in another, and these patients continued to have negative sputum cultures up to four years of treatment. The remaining 5 patients had continually positive sputum cultures, but with fewer colony forming units (Kadota, 2003). S. pneumoniae that was resistant to erythromycin was isolated from one of these five at one and two
62
years of treatment, but the organism was replaced by S. aureus during the next follow-up period. No patient was hospitalized with acute exacerbation of infection during the four years of treatment (Kadota, 2003). In 73 children receiving clarithromycin for eight weeks or longer for chronic otitis media with effusion and/or sinusitis no change was found in the carriage of drug-resistant pathogens, and the authors concluded the medication worked as a result of its antiinflammatory rather than its antibacterial effects (Iino, 2003).
We will obtain nasopharyngeal swabs and, when possible, expectorated sputum quarterly, and will do sensitivity testing on any pathologic organisms cultured. This will allow us to determine the emergence rate of macrolide-resistance organisms prospectively in both macrolide-treated patients and controls.
Macrolide-related side-effects Discussed above.
14. Medication compliance A recent review of medication compliance indicates that the rate of nonadherence to a prescribed medical regimen ranges from 0% to 100% (20% to 80% in patients with asthma), averages between 50% and 80%, is not related to sociodemographic factors, intelligence or education but decreases as the frequency of dosing, cost and duration of treatment increase (Claxton, 2001; MacDonald, 2002).
63
Although an extensive literature addresses issues relating to compliance and ways to improve it in patients with hypertension, diabetes, epilepsy, psychiatric disorders and, to a lesser extent, asthma and transplantation, information on patients with COPD is limited. On the basis of responses to a questionnaire James and colleagues (1985) found that only 33% of 185 patients with COPD were fully compliant with their prescribed treatment regimen and compliance was not related to the number of medications prescribed. Gallefoss and Bakke (1999) performed a randomized controlled trial of a standardized education program and self-management plan in patients with mild to moderate asthma (N = 78) and COPD (N = 62) assessing compliance from monthly printouts of pharmacy registers. The education program had no effect on compliance with inhaled steroids in the patients with COPD (58% and 50% compliance at one year in the control and intervention group, respectively) but did reduce the amount of short-acting inhaled 2-agonists dispensed. The ability of a macrolide antibiotic to reduce the frequency or severity of acute COPD exacerbations can be determined by assessing its efficacy or its effectiveness. Efficacy studies determine the benefit the drug under optimal circumstances with considerable effort directed at obtaining maximum adherence to the regimen and careful monitoring of compliance so that the effects of poor compliance can be distinguished from the regimen being ineffective. Effectiveness studies are designed to test the effect of the intervention under conditions of standard practice in which compliance is not formally monitored. Effectiveness studies have a greater likelihood of demonstrating that the
64
intervention being tested is beneficial but the results may not extrapolate to what occurs under normal daily practice. In response to the Protocol Review Committee's suggestions to increase the extent of compliance monitoring, to change the dosing regimen and educate the patients to facilitate compliance, we propose the following:
Compliance monitoring. Compliance with a medical regimen can be quantified by patient selfassessment, pill counting, inspection of pharmacy databases, checking blood or urine samples for the presence of a medication or a marker substance, and/or by electronic monitoring of dispenser use. Unfortunately, is no gold standard for measuring compliance because (1) all of the current approaches have important limitations, and (2) there are varying recommendations regarding what defines good and bad compliance and little experimental data to support any of the recommendations (Timmreck, 1993; Farmer, 1999). Patient self-assessment of compliance is easy to record, but the accuracy of the information is questionable. Patients who admit to not following prescribed regimens tend to describe their compliance accurately (Cramer, 1987) while those who claim good compliance may be consciously falsifying their response or have inaccurate recall (Spector, 1986). Pill counting is also easy to accomplish, but also generally overestimates compliance. Finding excessive numbers of pills clearly indicates poor
65
compliance, but finding the appropriate number of pills does not confirm that the medication was actually taken, or that it was taken regularly (Matsui, 1994). Similar problems apply to inspection of pharmacy databases. While finding that patients do not refill prescriptions at the appropriate rates indicates poor compliance, the opposite may not true. In addition, the data may be inaccurate if patients use more than one pharmacy. Electronic monitoring systems utilize microprocessors to record the time and date that a medication container was opened or when a blister pack was accessed. Although these are considered to be the best single method of compliance assessment they are expensive and still have limitations. As with the other methods, data indicating poor compliance are accurate, but patients can still remove their medications regularly but fail to ingest them. Systems that assess pill bottle or blister pack opening have limited utility if patients use daily pill containers that are filled once weekly. Measuring blood or urine levels of a medication, or of a biological marker that can be added to a medication, is expensive, and will identify whether patients have recently taken recently taken a dose. These methods cannot confirm regular use and, depending on the medication being monitored, the tests can partially depend on factors that are unrelated to compliance (e.g., diet, absorption and rate of excretion) (Vitolins, 2000). Finally, all monitoring methods are susceptible to the Hawthorne effect, i.e., compliance being improved because the patients know that their drug use is being monitored.
66
No single measurement strategy has won uniform approval as a representative 'gold standard' and, accordingly, a multi-method approach that combines self-reporting and other objective measures is generally recommended (Sabate, 2003). We have elected to monitor compliance by self-reporting, pill counting, and blister packs containing microprocessors (MedicTM ECMTM).
Human Subject Issues Risks and measures designed to minimize the risks. Discussed above. Procedure for obtaining consent. Described above.
Enrollment of minorities and women Minority patients The prevalence of at least moderate COPD (defined by spirometry), the number of COPD-related office visits and the COPD-related death rate are lower in minority patients than in Whites, but Blacks have a higher prevalence of ED visits and hospitalization (Table 6).
Table 6. Prevalence, Morbidity and Mortality of COPD by Race (Centers of Disease Control and Prevention, 2002) Black Prevalence of Moderate COPD by Spirometry (per 1,000) Office Visits for COPD (per 1,000) 30.4 46.9 55.8 White 67.1 Other 52.8
67
ED Visits (per 10,000) Hospitalizations (per 10,000) Death rates (per 100,000)
130.8 36 42.9
84.8 31.5 70.1 21.3 30.6
Data describing the prevalence, morbidity and mortality in Hispanics are both very limited and over 20 years old. The ability to compare morbidity and mortality between races is limited, however, because there are numerous potential confounders of these data. The observed minority visits in seven clinical centers is summarized in Table 7 (prior to completing the protocol three additional centers were added to the original nine to facilitate patient enrollment).
Table 7. The percentages of women and minority patients seen in seven Clinical Centers Center Hospital Women (%) Black Hispanic American Indian/ Alaska Native Baltimore University inpt* University outpt* VA* Birmingham University VA 58 53 6 50 51 75 35 30 0 0 0 0 0 0 0 0 0 0 0 0 45 22 51 70 Asian/ Pacific Islander White
68
Boston
Brigham/Womens* MGH* BDMC
56 49 52 55 50 50 10 30 50 50 10 55
12 3 8 14 4 8 4 15
5 3 2 55 3 7 6 4
0 0 0 1 0 4 0 0 30 0 7 0 0 0 1
81 92 85 5 80 51 58 74
Denver
Denver Health*1 National Jewish*1 University*1 VA*1
Los Angles Minneapolis
Harbor/UCLA* Health Partners4 Mayo Clinic VA
San Francisco Mean
Moffit-Long*
10
13
60
43
21
60
* Data pertain to COPD patients specifically
1
Combined in-patient and out-patient
Previous studies indicate that fewer Black and Hispanic patients agree to participate in clinical studies. Accordingly, we estimate that despite 21% of the patients seen in the seven Clinical Centers being Black, Blacks may represent only 12% of the study population after enrollment is complete. Similarly, while
69
7% of the patients in the Clinical Centers are Hispanic, perhaps only 4 or 5% of the final study population will be Hispanic. Our target minority enrollment estimate is that the final study population will include 15% minority patients. This would seem to be a realistic objective given the percentage of minority patients seen in seven Clinical Centers after adjusting for lower rates of enrollment in minority patients.
Women Although women have a higher rate of self-reported COPD than men, and the prevalence of COPD is increasing in women but not in men, there is a higher prevalence of moderate COPD (defined by spirometry) in men, and men have a higher death rate (Table 8, Centers of Disease Control and Prevention, 2002).
Table 8. Prevalence, Morbidity and Mortality of COPD by Gender (MMWR, 2002)
Men Prevalence of Moderate COPD by Spirometry (per 1,000) Office Visits for COPD (per 1,000) ED Visits (per 10,000) Hospitalizations (per 10,000) Death rates (per 100,000) 46.8 80.7 42.4 82.6 74.3
Women 58.2
43.4 94.4 40.2 56.7
70
The well documented spirometric progression of COPD, together with the fact that the annual COPD-related death rate is increasing in women but not in men, suggests that, on the average, the severity of COPD in women is less than in men. This difference could affect enrollment in the proposed study. The higher prevalence of ED visits in women argues against this suggestion, however. Accordingly, our target enrollment estimate is that the final study population will include 45% women. The large male predominance in the armed services results in the fact that patients in any study that has Veteran's hospitals as enrollment sites will be disproportionately male unless special enrollment strategies are employed to assure a more equal gender distribution. Seven of the ten Clinical Centers in the COPD CRN include VA hospitals as enrollment sites. Accordingly, strategies specifically targeting enrollment of women from the other sites will be will be needed for this study. Plans for accomplishing this at each Center were developed prior to starting the study.
71
Section B. Protocol Changes Pertaining to Possible QT Prolongation During the trial two protocol changes were made: (1) Because only 15.4%, 11.2% and 9.4% of participants were able to produce sputum at enrollment and at the one- and three-month clinic visits, respectively, we elected to stop collecting expectorated sputum after month three. (2) Fifteen months after enrollment began the heart rate exclusion criteria and the methods used to determine the QTc interval were modified in response to a new publication suggesting that clarithromycin was associated with an increased risk of cardiovascular mortality (Jespersen, 2006). New exclusion criteria included: a. A resting heart rate > 100 beats/min b. A manually determined QTc interval measured at least one hour after use of any short-acting inhaled 2 agonist that exceeds 450 ms on two occasions separated by at least one week. Manual determinations are only to be done if the automated QTc estimate exceeds the 450 ms limit. The method for determining the QTc interval manually is to measure the mean QT interval from the beginning of the QRS complex to the end of the T wave, in a minimum of 3 cardiac cycles, in leads II and V5 or V6 (using the lead in which the QT is the longest). This QT interval is then corrected for heart rate using Federicias formula (QTc= QT/RR(sec)1/3). Bundle branch blocks prolong the QT interval. Accordingly, patients with either left or right bundle branch blocks should have the JT interval measured.
72
Subjects with a JT interval > 420 msec (corrected for heart rate) should be excluded. It is recommended that a cardiologist specializing in arrhythmias and/or ECG interpretation perform the above manual analysis and evaluate all ECGs of patients with bundle branch blocks. In addition, two additional reasons for drug discontinuation were added: a. If the QTc on ECGs recorded one month after starting the study medication increases to > 500 ms or > 60 ms from the patients baseline value. b. For patients with a bundle branch block, if the JTc interval increases 60 ms from the patients baseline value.
73
References Abbott PJ et al.Retrospective analyses of additional services for methadonemaintenance patients. Journal of Substance Abuse Treatment, 1999;17:129137. Aberg JA, Wong MK, Flamm R, Notario GF, Jacobson MA. 2001. Presence of macrolide resistance in respiratory flora of HIV infected patients receiving either clarithromycin or azithromycin for Mycobacterium avium complex prophylaxis. HIV Clin Trials 2:453-9. Albaz RS. Factors affecting patient compliance in Saudi Arabia. Journal of Social Sciences, 1997, 25:5-8. American Thoracic Society. 1987. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. Am Rev Respir Dis 136:225-44. Anthonisen NR, Wright EC, IPPB Trial Group. 1986. Bronchodilator response in chronic obstructive pulmonary disease. Am Rev Respir Dis 133:814-9. Brummett RE. 1993. Ototoxic liability of erythromycin and analogues. Otolaryngol Clin North Am 26:811-819. Calverley PMA, Burge PS, Spencer S, Anderson JA, Jones PW, for the ISOLDE Study Investigators. 2003. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax 58:659-64. Centers of Disease Control and Prevention. 2002. Surveillance Summaries, August 2, MMWR 51:(No. SS-6).
74
Claxton AJ, Cramer J, Pierce C. 2001. A systematic review of the associations between dose regimens and medication compliance. Clin Ther 23:12961310. Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. 1989. How often is medication taken as prescribed. JAMA 261:3273-7. Cymbala AA, Edmonds LC, Bauer MA, et al. An open label, randomised, crossover design pilot study of the disease modifying effects of twice weekly oral azithromycin in patients with bronchiectasis. Treat Resp Med, in press pending revision. Doern GV, Heilmann KP, Huynh HK, et al. Antimicrobial resistance among clinical isolates of Streptococcus pneumoniae in the United States during 1999-2000, including a comparison of resistance rates since 19994-1995. Antimicrob Agents Chemother 45:1721-9. Equi A, Balfour-Lynn IM, Bush A, Rosenthal M. 2002. Long-term azithromycin in children with cystic fibrosis: a randomized, placebo-controlled crossover trial. Lancet 360:978-84. Ewig S, Ruiz M, Torres A, et al. 1999. Pneumonia acquired in the community through drug resistant Streptococcus pneumoniae. Am J Respir Crit Care Med 159:1835-42. Fabbri LM, Romagnoli M, Corbetta L, Casoni G, Busljetic K, Turato G, et al. 2003. Differences in airway inflammation in patients with fixed airflow obstruction due to asthma or chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 167:418424
75
Farmer KC. 1999. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics 21:1074-1090. Ferguson, GT, Enright, PL, Buist, AS, et al Office spirometry for lung health assessment in adults: a consensus statement from the National Lung Health Education Program. Chest 2000;117,1146-1161 Fogarty C, Goldschmidt R, Bush K. 2002. Bacteremic pneumonia due to multidrug-resistant pneumococci in 3 patients treated unsuccessfully with azithromycin and successfully with levofloxacin. Clin Infect Dis 31:613-5. Gallefoss F, Bakke PS. 1999. How does patient education and selfmanagement among asthmatics and patients with chronic obstructive pulmonary disease affect medication? Am J Respir Crit Care Med 160: 20005. Gay K, Baughman W, Miller Y, et al. 2000. The emergence of Streptococcus pneumonia resistant to macrolide antimicrobial agents: a 6-year population-based assessment. J Infect Dis 182;1417-24. Gearhardt SG, McDyer JF, Girgis RE, Conte JV, Yange SC, Orens JB. 2003. Maintenance azithromycin therapy for bronchiolitis obliterans syndrome. Results of a pilot study. Am J Respir Crit Care Med 168:121-5. Gleason PP, Meehan TP, Fine JM, Galusha DH, Fine MJ. 1999. Associations between initial antimicrobial therapy and medical outcomes for hospitalized elderly patients with pneumonia. Arch Intern Med 159:256272.
76
Guchev IA, Gray GC, Klochkov OI. 2004. Two regimens of azithromycin prophylaxis against community-acquired respiratory and skin/soft tissue infections among military trainees. CID 38:1095-1101. Hankinson, JL, Crapo, RO, Jensen, RL Spirometric reference values for the 6-s FVC maneuver. Chest 2003;124,1805-1811 Halperin M, Lan KKG, Ware JH et al. (1982). And aid to data monitoring in longterm clinical trials. Controlled Clin Trials 3:311-323. Harris S, Hilligoss DM, Colangeol PM, Eller M, Okerhaom R. 1995. Azithromycin and terfenadine: lack of drug interaction. Clin Pharmacol Ther 58:310-5. Haydon RC, Thelin JW, Davis WE. 1984. Erythromycin ototoxicity: analysis and conclusions based on 22 case reports. Otolaryngol Head Neck Surg 92:678-684. Hoban DJ, Doern GV, Fluit AC, Roussel-Delvallez M, Jones RN. 2001. Worldwide prevalence of antimicrobial resistance in Streptococcus pneumonia, Haemophilus influenzae, and Moraxella catarrhalis in the SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Inf Dis 32:S81-S93. Hoffman HL, Klepser ME, Ernst EJ, Petzold CR, Sa'adah LM, Doern DV. 2003. Influence of macrolide susceptibility on efficacies of clarithromycin and azithromycin against Streptococcus pneumoniae in a murine lung infection model. Antimicrob Agents Chemother 47:739-46.
77
Hyde TB, Gay K, Stephens DS, et al. 2001. Macrolide resistance among invasive Streptococcus pneumoniae isolates. JAMA 286:1857-62. Iannini PB. 2002. Cardiotoxicity of macrolides, ketolides and fluoroquinolones that prolong the QTc interval. Expert Opin Drug Saf 1:121-128. Iino Y, Sasaki Y, Miyazawa T, Kodera K. 2003. Nosopharyngeal flora and drug susceptibility in children with macrolide therapy. Laryngoscope 113:17805. James PN, Anderson JB, Prior JG, White JP, Henry JA, Cochrane GM. 1985. Patterns of drug taking in patients with chronic airflow limitation. Postgrad Med J 61:7-10. Jennison C, Turnbull BW (2000) Group Sequential Methods with Applications to Clinical Trials. Chapman & Hall/CRC, Chap. 7, Table 7.1. Jespersen CM, Als-Nielsen B, Damgaard M, Hansen JF, Hansen S, Helo OH, Hildebrandt P, Hilden J, Hensen GB, Kolmos HJ, Keller E, Lind I, Nikelsen J, Petersen L, Gluud C, the CLARICOR Trial Group. Randomized placebo controlled multicenter trial to assess short term clarithromycin for patients with stable coronary heart disease: CLARICOR trial. BMJ 2006;332:22-27 Jones RN, Cormican MC, Wanger A. 1996. Clindamycin resistance among erythromycin-resistant Streptococcus pneumoniae. Diagn Microbiol Infect Dis 25:201-4. Kadota J, Mukae H, Kshii H, Nagata T, Kaida H, Tomono K, Kohno S. 2003. Long-term efficacy and safety of clarithromycin treatment inpatients with diffuse panbronchiolitis. Resp Med 97:844-50.
78
Kelley MA, Weber DJ, Gilligan P, Cohen MS. 2000. Breakthrough pneumococcal bacteremia in patients treated with azithromycin and clarithromycin. Clin Infect Dis 31:1008-11. Kim K, DeMets DL (1987) Design and analysis of group sequential tests based on the type I error spending rate function. Biometrika 74, 149-154. Lan KKG, Simon R, Halperin M.(1982) Stochastically curtailed tests in long-term clinical trials. Commun. Stat., Sequential Analysis. 1:207-219. Leclercq R. 2002. Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis 34:482-492. Levey AS; Bosch JP; Lewis JB; Greene T; Rogers N; Roth D. 1999. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461-70. Levey, AS, Greene, T, Kusek, JW, Beck, GJ, and MDRD study group. 2000. A simplified equation to predict glomerular filtration rate from serum creatinine (abstract). J Am Soc Nephrol 11:155A. Lisby G, Brasholt MS, Teglbjerg L. 2001. Bacteremia and meningitis caused by macrolide-sensitive strain of Streptococcus pneumoniae during treatment with azithromycin. Clin Infect Dis 33:415-6. Lonks JR, Garau J, Gomez L. 2002. Failure of macrolide antibiotic treatment in patients with bacteremia due to erythromycin-resistant Streptococcus pneumoniae. Clin Infect Dis 35:556-64.
79
Lynch JP, Martinez FJ. 2002. Clinical relevance of macrolide-resistant Streptococcus pneumoniae for community-acquired pneumonia. Clin Infect Dis 34 (Suppl 1):S27-46). MacDonald HP, Garg AX, Haynes RB. 2002. Interventions to enhance patient adherence to medication prescriptions. JAMA 288:2868-79. Malazimoglu L, Tulkens PM, Van Bambek R. Macrolides. In: VL Yu, R Weber, D Raoult (eds), Antimicrobial Therapy and Vaccines (Volume II), in press. Martinez JA, Horcajada JP, Almela M, et al. Addition of a macrolide to a lactam-based empirical antibiotic regimen is associated with lower inhospital mortality for patients with bacteremic pneumococcal pneumonia. Clin Inf Dis 36:389-95. Matsui D et al. 1994. Critical comparison of novel and existing methods of compliance assessment during a clinical trial of an oral iron chelator. Journal of Clinical Pharmacology 34:944-949. Milberg P, Eckardt L, Bruns W, et al. 2002. Divergent proarrhythmic potential of macrolide antibiotics despite similar QT prolongation: fast phase 3 repolarization prevents early after depolarizations and torsade de pointes. J Pharmacol Exp Ther 303;218-25. Musher DM, Dowel ME, Shortridge VD. 2002. Emergence of macrolide resistance during treatment of pneumococcal pneumonia. N Engl J Med 346:630-1.
80
National Emphysema Treatment Trial Research Group. Cost effectiveness of lung-volume-reduction surgery for patients with severe emphysema. N Engl J Med 2003;348:2092-102. NICE Guidelines on COPD. 2004. National clinical guideline on management of COPD in adults in primary and secondary care. Diagnosing COPD. Thorax 59 (Suppl 1):i27-38. Niewoehner D, Rice K, Cote C, Paulson D, Cooper JA, Korducki L, Cassimo C, Kesten S. 2004. Reduced COPD exacerbations and associated health care utilization with once-daily tiotropium (TIO) in the VA Medical System. Am J Respir Crit Care Med 169: A207 (abstract). Nisar M, Earis JE, Pearson MG, Calverley PM. 1992. Acute bronchodilator trials in chronic obstructive pulmonary disease. Am Rev Respir Dis 146:555-9. Nishijima T, Saito Y, Aoki A, Toriya M, Toyonaga Y, Fujii R. 1999. Distribution of mefE and ermB genes in macrolide-resistant strains of Streptococcus pneumoniae and their variable susceptibility to various antibiotics. J Antimicrob Chemother 43:637-43. Nuermberger E, Bishai WR. 2004. The clinical significance of macrolideresistnat Streptococcus pneumoniae: Its all relative. CID 38:99-103. OBrien PC, Fleming TR (1979). A multiple testing procedure for clinical trials. Biometrics 35:549-556. O'Connor CM, Dunne MW, Pfeffer MA, Muhlestein JB, Yao L, Gputa S, Benner RJ, Fisher MR, Coor TD for the investigators in the WIZARD study. 2003. Azithromycin for the secondary prevention of coronary heart disease
81
events. The WIZARD study: A randomized controlled trial. JAMA 290:1459-66. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS; The GOLD Scientific Committee. 2001. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 163:1256-76. Poehlsgaard J, Douthwaite S. 2003. Macrolide antibiotic interaction and resistance on the bacterial ribosome. Curr Opin Investig Drugs 4:140-148. Rello J, Catalan M, Diaz E, Bodi M, Alvarez B. 2002. Associations between empirical antimicrobial therapy at the hospital and mortality in patients with severe community-acquired pneumonia. Inten Care Med 28:1003-5. Roter DL et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Medical Care, 1998, 36:1138-1161. Sabate E. 2003. Adherence to Long-Term Therapies. Evidence for Action. World Health Organization, Geneva. Saiman L, Marshall BC, Mayer-Hamblett N, Burns JL, Quittner AL, Cibene DA, Coquillette S, Fieberg AY, Accurso FJ, Campbell PW, III. 2003. Azithromycin in patients with cystic fibrosis chronically infected with Pseudomonas aeruginosa: a randomized controlled trial. JAMA 290:17491756.
82
Santus P, Pecchiari M, Carlucci P, Boveri B, Di Marco F, Castagna F, Centanni S. 2003. Bronchodilation test in COPD: effect of inspiratory manoeuvre preceding forced expiration. Eur Respir J 21:82-5.
Sin DD, McAlister FA, Man SF, Anthonisen NR. 2003. Contemporary management of chronic obstructive pulmonary disease: scientific review. JAMA 290(17):2301-12. Spector SL et al. 1986. Compliance of patients with asthma with an experimental aerosolized medication: implications for controlled clinical trials. Journal of Allergy & Clinical Immunology 77:65-70. Stahl JE, Barza M, DesJardin J, Martin R, Eckman MH. 1999. Effect of macrolides as part of initial empiric therapy on length of stay in patients hospitalized with community-acquired pneumonia. Arch Intern Med 159:2576-80. Strle R, Maraspin V. 2002. Wien Kiln Wochenschr 112:396-9. Swanson DJ, Sung RJ, Fine MJ, Orloff JJ, Chu SY, Yu VL. 1992. Erythromycin ototoxicity: prospective assessment with serum concentrations and audiograms in a study of patients with pneumonia. Am J Med 92:61-68. Taylor R, Schofield IS, Ramos JM, Bint AJ, Ward MK. 1981. Ototoxicity of erythromycin in peritoneal dialysis patients. Lancet 2:935-936. Tessier PR, Kim MK, Zhou W, Xuan D, Li C, Ye M, Nightingale CH, Nicolau DP. 2002. Pharmacodynamic assessment of clarithromycin in a murine model of pneumococcal pneumonia. Antibmcrob Agents Chemother 46:1425-34.
83
Timmreck TC, Randolph JF. 1993. Smoking cessation: clinical steps to improve compliance. Geriatrics 48:63-66. Tweeddale PM, Alexander F, McHardy GJ. 1987. Short term variability in FEV1 and bronchodilator responsiveness in patients with obstructive ventilatory defects. Thorax 42:487-90. Umstead GS, Neumann KH. 1986. Erythromycin ototoxicity and acute psychotic reaction in cancer patients with hepatic dysfunction. Arch Intern Med 146:897-899. Van Bambeke F, Glupczynski Y, Plesiat P, Pechere JC, Tulkens PM. 2003. Antibiotic efflux pumps in prokaryotic cells: occurrence, impact on resistance and strategies for the future of antimicrobial therapy. J Antimicrob Chemother 51:1055-1065. Van Kerkhoven D, Peetermans WE, Verbist L, Verhaegen J. 2003. Breathhrough pneumococcal bacteraemia in patients treated with clarithromycin or oral -lactams. J Antimicrob Chemother 51:691-6. Vasquez EM, Maddux MS, Sanchez J, Pollak R. 1993. Clinically significant hearing loss in renal allograft recipients treated with intravenous erythromycin. Arch Intern Med 153:879-882. Vitolins MZ et al. 2000. Measuring adherence to behavioral and medical interventions. Controlled Clinical Trials, 2000, 21:188S-194S. Waites K, Johnson C, Gray B, Edwards K, Crain M, Benjamin W Jr. (2000) Use of clinicamycin disks to detect macrolide resistance mediated by ermB and
84
mefE in Streprococcus pneumoniae isolates from adults and children. J Clin Microbiol 38:1731-4. Wallace MR, Miller LK, Nguyen MT, Shields AR. 1994. Ototoxicity with azithromycin. Lancet 343:241. Ware JH, Muller JE, Braunwald E. (1985) The futility index, a approach to the cost-effective termination of randomized clinical trials. Am J Cardiol 78:636-664. Waterer GW, Wunderink RG, Jones CB. 2000. Fatal pneumococcal pneumonia attributed to macrolide resistance and azithromycin monotherapy. Chest 118:1839-40. Waterer GW, Somes GW, Wunderink RG. 2001. Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumonia. Arch Intern Med 161:1837-42. Whitney CG, Farley MM, Hadler J, Harrison LH, Lexau C, Reingold A, Lefkowitz L, Cieslak PR, Cetron M, Zell ER, Jorgensen JH, Schuchat A. Active Bacterial Core Surveillance Program of the Emerging Infections Program. 2000. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med 343:1917-24. Weisblum B. 1995. Erythromycin resistance by ribosome modification. Antimicrob Agents Chemother 39:577-585. Wolter J, Seeney S, Bell S, Bowler S, Masel P, McCormack J. 2002. Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomized trial. Thorax 57:212-6.
85
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Acs 20 ReviewDokumen7 halamanAcs 20 ReviewrazorazBelum ada peringkat
- PseudodementiaDokumen10 halamanPseudodementiarazorazBelum ada peringkat
- CPG Management of Atrial Fibrillation PDFDokumen119 halamanCPG Management of Atrial Fibrillation PDFZee YongBelum ada peringkat
- R C S I D R A F T M e D I C A L G R A D U A T e P R o F I L eDokumen8 halamanR C S I D R A F T M e D I C A L G R A D U A T e P R o F I L erazorazBelum ada peringkat
- True But TrueDokumen20 halamanTrue But TruerazorazBelum ada peringkat
- Laser Treatment For Varicose VeinsDokumen5 halamanLaser Treatment For Varicose VeinsrazorazBelum ada peringkat
- Registration FormDokumen2 halamanRegistration FormrazorazBelum ada peringkat
- PG Respiratory Summit Registration Form 2013Dokumen2 halamanPG Respiratory Summit Registration Form 2013razorazBelum ada peringkat
- IC1 - Arrhythmia - 2012 EDITEDDokumen42 halamanIC1 - Arrhythmia - 2012 EDITEDrazorazBelum ada peringkat
- GKM Final Year Book ClearanceDokumen6 halamanGKM Final Year Book Clearancerandom.mail.scsm7112Belum ada peringkat
- Cataract LectureDokumen7 halamanCataract LecturerazorazBelum ada peringkat
- Literature Review of Bariatric Surgery For The Treatment of Morbid ObesityDokumen1 halamanLiterature Review of Bariatric Surgery For The Treatment of Morbid ObesityrazorazBelum ada peringkat
- RCPI Management of Early Pregnancy MiscarriageDokumen24 halamanRCPI Management of Early Pregnancy MiscarriagerazorazBelum ada peringkat
- Gut 2013 - 23 - 25th August 2013, PenangDokumen12 halamanGut 2013 - 23 - 25th August 2013, PenangPierce ChowBelum ada peringkat
- CVR02 - EcgDokumen3 halamanCVR02 - EcgrazorazBelum ada peringkat
- Dangerous Diplopia - PansinusitisDokumen4 halamanDangerous Diplopia - PansinusitisrazorazBelum ada peringkat
- In Austere Financial Times, Which Procedures Should Be Rationed and Who Should Decide?Dokumen13 halamanIn Austere Financial Times, Which Procedures Should Be Rationed and Who Should Decide?razorazBelum ada peringkat
- How To Write A Great Research Paper by Simon Peyton JonesDokumen46 halamanHow To Write A Great Research Paper by Simon Peyton JonesrazorazBelum ada peringkat
- Cataract LectureDokumen7 halamanCataract LecturerazorazBelum ada peringkat
- PneumoniaDokumen37 halamanPneumoniarazorazBelum ada peringkat
- NSAIDsDokumen2 halamanNSAIDsrazoraz100% (1)
- Surgical Safety ChecklistDokumen8 halamanSurgical Safety ChecklistrazorazBelum ada peringkat
- The Medical Short Case Preview 2011Dokumen20 halamanThe Medical Short Case Preview 2011Lim Thien Thien100% (2)
- Secrets Alto Sax MelodyDokumen3 halamanSecrets Alto Sax MelodyrazorazBelum ada peringkat
- GCE Biology Unit 6 TSM Final (Unit 6 Guide and Examples From Edexcel)Dokumen76 halamanGCE Biology Unit 6 TSM Final (Unit 6 Guide and Examples From Edexcel)razoraz90% (10)
- ETHICON Encyclopedia of Knots (Noduri Chirurgicale PDFDokumen49 halamanETHICON Encyclopedia of Knots (Noduri Chirurgicale PDFoctav88Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Drugs For Allergic Rhinitis Cough and ColdDokumen26 halamanDrugs For Allergic Rhinitis Cough and ColdChandana Sri LalamBelum ada peringkat
- Baguio Gen. 2Dokumen1 halamanBaguio Gen. 2TinTin CjBelum ada peringkat
- Drug StudyDokumen4 halamanDrug StudyNicole GonzalesBelum ada peringkat
- PR and Government Relations Plan For A Multinational Pharmaceutical FirmDokumen5 halamanPR and Government Relations Plan For A Multinational Pharmaceutical FirmGene Gregorio100% (1)
- Investor Update On R&D Pipeline 24th August FinalDokumen52 halamanInvestor Update On R&D Pipeline 24th August FinalDeep Run WatersBelum ada peringkat
- Reverse Phase-Hplc Method Development and Validation For The Simultaneous Estimation of Azilsartan Medoxomil and Chlortalidone in Pharmaceutical Dosage FormsDokumen10 halamanReverse Phase-Hplc Method Development and Validation For The Simultaneous Estimation of Azilsartan Medoxomil and Chlortalidone in Pharmaceutical Dosage FormsjamonlineBelum ada peringkat
- Pharmacy CQI in FloridaDokumen21 halamanPharmacy CQI in FloridaasgbalajiBelum ada peringkat
- Complications of Intravenous TherapyDokumen29 halamanComplications of Intravenous TherapyKrizia BonillaBelum ada peringkat
- Pharm Exam1Dokumen17 halamanPharm Exam1Jill Putman Beistline75% (4)
- School Nursing Common DRUG STUDYDokumen10 halamanSchool Nursing Common DRUG STUDYMaria Francheska OsiBelum ada peringkat
- Dietary Guidelines and Drug-Herb Interactions For People Taking WarfarinDokumen4 halamanDietary Guidelines and Drug-Herb Interactions For People Taking WarfarinLabu KundurBelum ada peringkat
- Trade NameDokumen5 halamanTrade Namevijay_nimsBelum ada peringkat
- Drugs in Pk.Dokumen23 halamanDrugs in Pk.hmBelum ada peringkat
- SPARC Licenses Xelprosâ (Latanoprost BAK-free) To Sun Pharma (Company Update)Dokumen2 halamanSPARC Licenses Xelprosâ (Latanoprost BAK-free) To Sun Pharma (Company Update)Shyam SunderBelum ada peringkat
- Charts For PharmacologyDokumen3 halamanCharts For PharmacologyAditi100% (1)
- Cannafest 2012 - Medical Cannabis in Israel v6Dokumen39 halamanCannafest 2012 - Medical Cannabis in Israel v6cannajoyBelum ada peringkat
- ACE Inhibitors - Blood HypertensionDokumen2 halamanACE Inhibitors - Blood HypertensionErik SilvaBelum ada peringkat
- Herbal PatchDokumen6 halamanHerbal PatchRiana Maya OktavianiBelum ada peringkat
- Sun Pharma Announces Distribution Alliance With Mitsubishi Tanabe Pharma Corporation in Japan (Company Update)Dokumen3 halamanSun Pharma Announces Distribution Alliance With Mitsubishi Tanabe Pharma Corporation in Japan (Company Update)Shyam SunderBelum ada peringkat
- A Review of Antibiotic Use in Pregnancy: EY OrdsDokumen11 halamanA Review of Antibiotic Use in Pregnancy: EY Ordsnoname19191Belum ada peringkat
- International Journal of Research in Pharmacy and ScienceDokumen10 halamanInternational Journal of Research in Pharmacy and ScienceAat Prayoga MuhtarBelum ada peringkat
- Medicines For BaguioDokumen3 halamanMedicines For BaguioMaielyne Keith DalilisBelum ada peringkat
- CoatingDokumen28 halamanCoatingVikrant Saluja0% (1)
- Treatment of Typhoid Fever Using Antibiotics: Class SummaryDokumen8 halamanTreatment of Typhoid Fever Using Antibiotics: Class SummaryRani Henty NovitaBelum ada peringkat
- Aminophylline GuidelinesDokumen2 halamanAminophylline GuidelinesChristian Reza100% (1)
- National Drug Policy Programs OverviewDokumen101 halamanNational Drug Policy Programs OverviewAngelica BolosBelum ada peringkat
- DHA Past Paper 2Dokumen11 halamanDHA Past Paper 2Kumar Usmle Dyoode89% (28)
- Drug Study: Date/ Time Ordered Route/Dosage/ Time Interval Precaution Contra-Indications Nursing ResponsibilitesDokumen3 halamanDrug Study: Date/ Time Ordered Route/Dosage/ Time Interval Precaution Contra-Indications Nursing ResponsibilitespjcolitaBelum ada peringkat
- Administering Oral MedicationsDokumen24 halamanAdministering Oral MedicationsRhenier S. Ilado100% (2)
- Leaflet Interaksi ObatDokumen4 halamanLeaflet Interaksi ObatHabibahBelum ada peringkat