Physio Reviewer Renal To Acid Base
Diunggah oleh
Nicole ChanDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Physio Reviewer Renal To Acid Base
Diunggah oleh
Nicole ChanHak Cipta:
Format Tersedia
RENAL 1 Functions of kidneys: Excretory, regulatory, endocrine, metabolic Anatomy Paired extraperitoneal organs that lie posteriorly Divided
ded into the cortex and medulla Nephron- functional unit of the kidney Renal corpuscle/glomerulus o Glomerular capillaries- supplied by afferent arterioles; drained by efferent arterioles o Bowmans capsule- visceral layer formed by podocytes; bowmans space between the parietal and visceral layers o Mesangium- consists of mesangial cells and mesangial matrix; secrete EC matrix, prostaglandin and cytokines Renal tubules o Proximal tubules, descending thin limb, loop of Henle (LH), ascending thin limb, ascending thick limb (TALH), distal tubules, collecting ducts (CD) 2 types: o Cortical nephron ! 75%; located in the outer cortex ! short LH ! fxn: reabsorption and secretion ! DOES NOT take part of hypertonic medullary interstitium o Juxtamedullary nephron ! 25%; lie deep in the cortex near the medulla ! long LH that enter deep medulla ! generates OSMOTIC gradient for reabsorption of water Macula densa Monitors the composition of the fluid in the tubular lumen at the TALH Juxtaglomerular apparatus Consists of macula densa, extraglomerular mesangial cells, juxtaglomerular cells One of the components of tubuloglomerular feedback mechanism involved in autoregulation Capillary beds: Glomerular capillaries o HIGH pressure where FLUID is filtered Peritubular capillaries o LOW pressure where SOLUTES & FLUID are absorbed Vascular supply: Arranged in series; separated by efferent arterioles Efferent arterioles continue to the outer medulla to become: o Peritubular capillaries ! Supply tubules of cortical nephrons o Vasa recta ! Specialized peritubular capillaries that supply the LH of the juxtamedullary nephron
Urine Formation 3 processes: Glomerular filtration o Ultrafiltration of the protein-free plasma o Movement of large volume of fluid: glomerular capillaries ! Bowmans space Tubular reabsorption o Regulated transport of substance: tubular urine ! back to capillary blood Tubular secretion o Capillary blood ! tubular urine 4 mechanisms: Freely filtered not reabsorbed or secreted o Excretion rate = filtration rate o Creatinine Freely filtered but partly reabsorbed back to the blood o Excretion < Filtration o Excretion rate = Filtration rate reabsorption rate o Electrolytes Freely filtered but all are reabsorbed o Nothing is excreted o Amino acids, glucose Freely filtered not reabsorbed but secreted from capillary blood to renal tubules o Excretion rate = filtration rate + tubular secretion o Organic acids and bases Properties of Filtratition barrier: 3 major layers (same as glomerular capillaries): Endothelial cells of the capillaries o Fenestrated ! Freely permeable to water, small solutes (Na, urea, glucose) ! IMPERMEABLE to RBC, WBC, platelets o Negatively-charged glycoprotein surface o Synthesize vasoactive substances ! Dilator- NO ! Constrictor- endothelin Basement membrane o Prevent filtration of plasma protein o CHARGE-SELECTIVE FILTER- porous matrix of NEGATIVELY- charged protein o Gel-like structure of proteoglycans Foot processes of podocytes o Long finger-like processes that completely encircle the outer surface of the capillaries o Interdigitates to cover the basement membrane o SIZE-SELECTIVE FILTER- separated by filtration slits that keeps proteins & macromolecules from entering the Bowmans space Filtration of macromolecules Determined by size and valence or charge
!"#$%&'()*+,-')
./0)12/)3456)
Neutral molecules with smaller radius- filtered freely Size of 20-42 A- depends on charge Positively-charged- easily filtered (remember negatively-charged glycoprotein on surface of BM + negative podocytes) Some low MW substances are bound to plasma protein- NOT freely filtered
less effect on urine volume due to renal autoregulation and glomerulotubular balance ($reabsorption rate when $GFR)
Dynamics of Ultrafiltration: Net ultrafiltration pressure: Kf x (PGC PBS -- "GC ) Determinants: PGC o hydrostatic glomerular capillary pressure o glomerular capillary ! Bowmans space o primary means for GFR regulation PBS o hydrostatic Bowmans space pressure o opposes filtration "GC o oncotic glomerular capillary pressure o opposes filtration "BS o oncotic Bowmans space pressure o nearly 0 because protein-free so no influence on filtration DECREASE GFR Physical Determinants #Kf !#GFR $PBS ! #GFR $"GC ! #GFR #PGC ! #GFR #APressure! #GFR #REfferent! #GFR $ RAfferent! #GFR
"GC Alterations: arterial plasma oncotic pressure = $"GC; #GFR filtration fraction o fraction of renal plasma flow (RPF) that is filtered by glomerular capillaries o FF= GFR/RPF o $FF = $"GC = #GFR o determines the effect of RBF on GFR o $resistance of afferent and efferent arterioles = # RBF = $FF o #RBF < #GFR = $FF = $"GC = # net filtration GFR & Clearance GFR rate at which plasma is filtered by the glomerulus per unit time index of kidney fxn, severity,course of kidney disease decreases with age and renal disease normal GFR= 125mL/min or 180L/day Sx to measure GFR o Freely filtered o Not reabsorbed nor secreted o Not metabolized nor produced o Not alter the GFR; physiologically inert Inulin o Ideal substance however, not used because it has to infused IV Creatinine o Overestimates filtration rate because it is secreted to a small extent by proximal tubule o Endogenous substance, end product of muscle metab o Inversely proportional to GFR Renal Clearance Volume of plasma from w/c all substances has been remove and excreted per unit time Compares glomerular filtration rate with kidneys excretion rate Estimate GFR Based on Ficks principle: substances that are neither synthesized nor metabolized, the amt that enters the kidneys = amount that leaves the kidneys Input source: renal artery Output sources: renal veins, ureters Cl= (urine conc x volume)/ plasma conc Considers only the rate at which a sx is excreted into the urine Renal Blood Flow Cortical BF > medullary BF Lower blood flow in medulla by the vasa rectamaintain hyperosmolar environment in concentrated urine formation
Pathophysiologic/physiologic causes Renal disease, DM, HTN Urinary tract obstruction (stones) # RBF, $ plasma proteins (look below) Small effect only due to autoreg # angiotensin II (ACE inhibitors) $ sympathetic activity, vasoconstrictor hormones (NE, endothelin)
PGC Alterations: changes to AFFERENT arteriolar resistance o #resistance ! $PGC, $GFR o constant afferent: PGC % efferent arteriolar resistance o constant efferent: PGC 1/% afferent arteriolar resistance o PGC x afferent = efferent (??) changes to EFFERENT arteriolar resistance o #resistance ! #PGC, #GFR o BIPHASIC EFFECT!! o Moderate vasoconstriction = $GFR o Severe vasoconstriction = $RBF; $filtration fraction; $"GC; # net filtration pressure changes to renal arteriolar pressure o $BP = $PGC o autoregulation maintains PGC and GFR at relatively constant values (80-180mmHg) o <80 mmHg = #PGC; #GFR
!"#$%&'()*+,-')
./0)12/)3456)
$rate of Na filtered = $ O2 consumption
Autoregulation RBF and GFR are maintained relatively constant as arterial BP is 80-180 mmHg Achieved by changes in vascular resistance by afferent arteriole Myogenic o Pressure-sensitive o Responds to changes in arterial pressure o $ arterial pressure ! afferent arteriole stretches ! smooth muscle contracts ! $afferent arteriole resistance = offsets pressure increase o # arterial pressure ! # stretch ! renin release by JG cells ! $BP Tubuloglomerular Feedback o NaCl- dependent mechanism o Responds to changes in NaCl concentration o Ensure constant delivery of NaCl to the distal tubule o NaCl is sensed by macula densa of JG app o $ GFR ! $ NaCl entry via Na-K-2Cl symporter ! $ATP & adenosine ! constrict ! # GFR o # GFR ! # flow rate ! $ reabsorption ! #NaCl conc at MD cells ! # formation of ATP and adenosine ! dilation of afferent Hormones that affect GFR & RBF: Stimulus Effect Vasoconstrictors Sympa # ECFV Constrict afferent arterioles; enhance Na reabs Angiotensin # ECFV Constrict aff and II eff arterioles; (#BP, more effect on eff; #volume) aff protected by NO & prostaglandin Endothelin $stretch, Cpmstrict afferemt arterioles epi, A-II, bradykinin; # ECFV Vasodilate PGE #ECFV; Dampen constrictor effect $shear of sympa & A-II stress , A-II Nitric oxide $ shear Counteract const. (EDNO/ by A-II, stress, EDRF) catecholamines bradykinin, Ach, ATP, histamine Bradykinin $ PGE; Stim. NO and PGE release #ACE Dopamine Inhibits renin sec. Natriuretic $ ECFV Dilate afferent peptides Constrict efferent
RENAL 2 Urinary Excretion = Glomerular Filtration- Tubular reabsorption + Tubular secretion I. Tubular Reabsorption Passive o Diffusion o Facilitated diffusion ! Channels- Na, K ! Uniport- Glucose ! Coupled: Antiport- Na-H Symport- Na-glucose Solvent drag Active o Primary- coupled to Na-K ATPase o Secondary- coupled to indirect energy source such as ion gradient (glucose) o Endocytosis of proteins Transcellular route- through cellular membrane Paracellular route- through junctional and intercellular space Ultrafiltration (bulk flow)- mediated by hydrostatic and oncotic forces Proximal Tubule (PT) Reabsorbs 2/3 (67%) of fluid filtered by glomeruli ISOMOTIC volume reabsorption Reabsorbs solute (glucose, aa) by 2 active transport driven by Na-cotransports Protons are ACTIVELY SECRETED via Na-H antiport st 1 half: H, glucose, Na o CO2 + H2O ! H + HCO3 o H exits with Na entering via Na-H antiporter o Na back to blood via Na-K ATPase o HCO3 enters blood with Na Na & glucose both enter via 2 active transport o Na to blood via Na-K ATPase o Glucose to blood passive diffusion nd 2 half: Na, Cl o H-anion dissociates to H and anion o Na-H antiporter o Anion brought out and recycled with H o Anion exit coupled with Cl entering the cell o Cl undergoes paracellular transport creating a + lumen so Na will be repelled and reabsorbed paracellularly also o
GFR #
RBF #
NC / $ $
$ $ $
$ $ NC
Loop of Henle (LH) Thin descending limb of LH (dLH) o Has AQUAPORIN-1 water channels o Very permeable to water, less permeable to solutes (reabsorbs 15% water) Thin ascending limb of LH o Passively reabsorb NaCl; impermeable to H2O
!"#$%&'()*+,-')
./0)12/)3456)
Thick ascending limb of LH (TALH) o Reabsorbs 25% filtered Na,Cl,K by Na-K-2Cl co-transporter ! Inhibited by FUROSEMIDE (loop) o Impermeable to water o Reabsorb Mg, Ca, K, HCO3- paracellularly o Reabsorb Na and secrete H- Na-H antiporter o Tubular fluid becomes diluted or HYPOSMOTIC o DILUTING SEGMENT
Cation o o o o
MDR1 and OCTN used to bring cations to the tubules OCTN (OC goes to tubule; H enters the cell) Basolateral membrane has NaK ATPase and OCT (brings in OC from blood) p-glycoprotein also transports OC
Distal Convoluted Tubule (DCT) Reabsorbs Na, K, Cl Impermeable to water and urea ! HYPOOSMOTIC Reabsorbs 5% NaCl via Na-Cl cotransporters o Inhibited by THIAZIDE diuretic Late Distal Tubule & Cortical Collecting Tubule Reabsorbs 3-18% filtered H2O with ADH control Impermeable to urea 2 cell types o Principal cells ! Na & H2O reabsorption creating a lumen so K is secreted (due to channels) ! Aldosterone- $ Na channel activity ! Acted on by AMILORIDE (block Na channels) and SPIRINOLACTONE (aldosterone competitive antagonist) o Intercalated cells ! Reabsorb K ions and secrete H using H-ATPase (1 active) ! Acid base regulation Medullary Collecting Duct Reabsorbs <10% filtered H2O and Na FINAL site for processing urine- determines final urine output of Na and H2O ADH controlled= $ADH ! #urine volume ! $conc PERMEABLE to urea- $ interstitium osmolality ! concentrates urine Secretes H against gradient II. Tubular Secretion Excrete metabolism by-products Anion o MRP 2 and OAT 4 are used to bring out organic anions to the tubules o For every OA brought to tubules, 1 &-KG enters the cell (OAT4) o Basolateral membrane has Na-K ATPase, NaDC (Na and &-KG from blood enters cell), OAT1, 3 (&KG to the blood, OA enters from blood; powered by NaK ATPase and NaDC) o &-KG is recycled (enters the cell via NaDC and goes back to the blood via OAT 1,3)
III. Tubular Reabsorption Regulation: Glomerulotubular balance o $ filtered Na load = $ Na& H2O reabsorption o despite variable GFR, fraction of Na & H2O reabsorption is constant (67%) o helps prevent overloading of distal tubule (DT will reabsorb those not previously reabsorbed by proximal tubule) Peritubular capillary and renal interstitial fluid physical forces (Starlings forces) o Regulate NaCl and water reabsorption across PT into capillaries o Starlings forces favor solutes & H2O ! capillaries ("cap, Pi- reabsorption) o Opposing forces: ("I, Pc- leakage to urine) o No effect on LH, DT, CD Hormonal control o Aldosterone ! Secrted by zona glomerulosa ! 1 site- principal cells of cortical CT ! stimulates NaK ATPase ($ Na reabsorption, $ K secretion) ! $ Na permeability ! $Na reabsorbed=$H2O reabsorbed o Angiotensin II ! MOST POWERFUL Na retaining hormone ! Stimulates aldosterone secretion ! Constricts efferent arterioles ! Directly stimulates Na reabsorption in PT, LH, DT, CT o ADH ! MOST IMPORTANT hormone ! $ H2O permeability in DT, CT and collecting duct ! Binds with V2 receptors = $ cAMP ! protein kinase ! $ aquaporin 2 water channels in apical membrane o ANP and BNP ! Volume distention ! inhibits Na & H2O reabsorption ! $ urinary secretion of Na & H2O ! blood volume returns to normal ! Inhibits ADH- stimulated water reabsorption ! ANP natriuresis > BNP natriuresis o Sympathetic
!"#$%&'()*+,-')
./0)12/)3456)
Constricting renal arterioles ! #GFR ! # Na & H2O excretion ! $ Na & H2O reabsorption ! $ renin release and A-II ! tubular reabsorption ! # Na excretion Urodilantin ! Not present in systemic circulation ! MORE POTENT than ANP ! Inhibit NaCl & H2O reabsorption in CD Dopamine ! Opposite NE and Epi ! Directly inhibits NaCl & H2O reabsorption in PT Uroguanylin ! Produced by neuroendocrine cells in the intestine in response to ORAL ingestion of NaCl ! inhibit NaCl & H2O reabsorption Adrenomedullin ! Induces a marked diuresis ! STIMULUS # ECV $ renin $ A-II, $ K $Posm, ECV $ ECV $ ECV $ ECV ORAL ingestion of NaCl HTN, CHF SITE OF ACTION PT, TALH, DT/CD PT, TALH, DT/CD TALH, DT/CD DT/CD PT CD CD PT, CD EFFECT ON TRANSPORT $ NaCl and H2O reabsorption
Countercurrent exchangers o Vasa recta o Maintain the gradient ADH function o Alter permeability of the late distal tubule and collecting ducts to water o Concentrates urine bec H2O is reabsorbed Obligatory Urine volume Max concentration- 1200 1400 mOsm/L 600mOsm/day / 1400 mOsm/L= 0.444 L/day obligatory water loss COUNTERCURRENT MECHANISM interaction between loop of Henle (multiplier) and vasa recta (exchanger) goal- maintain hyperosmotic interstitium dissipation of medullary osmotic gradient is prevented due to vasa recta equilibrating with interstitial fluid Steps in countercurrent multiplication o Na is pumped out of the TALH with max gradient of 200 mOsm/L single effect o Water flows out of the descending tubule osmolality rises to 400 mOsm/L o Osmolality equilibrates between tubule and interstitium o Fluid shifts As the loop becomes longer, the greater is the longitudinal gradient ADH Urea
HORMONE Sympathetic nerves A-II Aldosterone ADH Dopamine ANP Urodilantin Uroguanylin Adrenomedulin
# NaCl and H2O reabsorption
Secreted from the posterior pituitary Conserve water to decrease urine output Binds to receptors in the distal and collecting tubules Stimulates insertion of water channels/ aquaporins to transport solute-free water back to the blood # plasma osmolality and $ urine osmolality
Autoregulation of RBF and GFR Keep RBF and GFR constant through 90-180mmHg Precise control of renal excretion of water & solutes 2 mechanisms: Myogenic mechanism o Pressure-sensitive mechanism o Responds to changes in arterial BP (stretch) o Prevents overdistention of vessel o Q= 'P/R Tubuloglomerular feedback mechanism o NaCl concentration-dependent o $GFR ! $NaCl conc sensed by macula densa of JG apparatus ! afferent arteriole increase resistance ! normal RBF and GFR Urine Concentration and Dilution Countercurrent multipliers o Loops of Henle o Establish interstitial osmotic gradient that increases from cortex to tip of papilla
from protein breakdown of liver interstitium back to loop of Henle (urea recycling) major osmole in the urine freely filtered in the glomerulus 50% reabsorbed in proximal tubule thin loops of henle- recycled; enters passively TALH- impermeable Cortical collecting ducts- impermeable Medullary collecting ducts- reabsorbed due to ADH
COUNTERCURRENT EXCHANGER Vasa recta- critical to the maintenance of the osmotic gradient Specialized hairpin structure- allows blood to reach inner medulla Highly permeable to water and solutes Provides nutrients and O2 to the medullary tissues Maintain medullary interstitial gradients is flow dependent
!"#$%&'()*+,-')
./0)12/)3456)
Formation of CONCENTRATED urine At TALH- active reabsorption of NaCl accumulates in the medullary interstitium = $ osmolality Filtrate becomes diluted at DCT and CCT WITH ADH- $H2O reabsorption = $tubular osmolality Interstitial fluid osmolality progressively increases from corticomedullary jxn to papilla + ADH- $urea permeability = $ interstitial osmolality can be as high as 1200 mOsm/kg; 0.5 L/day Formation of DILUTED urine no ADH secretion making the collecting ducts impermeable to water no water reabsorption occurs after the active reabsorption of Na in TALH can be as low as 50 mOsm/kg; 18 L/day Free water clearance ability of the kidneys to generate solute-free water diluted urine- solute-free water is excreted concentrated urine- solute-free water is returned factors for excretion: o absent ADH o normally functioning tubular segments ! TALH- most important o reduced delivery of tubular fluid to ascending thin LH, TALH, DT, CD impairs the ability of kidneys to maximally excrete solute-free water Factors needed to excrete maximally-concentrated urine maximal ADH normal NaCl tubular reabsorption o TALH- most important adequate delivery of tubular fluid hyperosmotic medullary interstitium maintained by NaCl reabsorption of Henles loop and urea accum. Factors that modulate urinary concentration and dilution Osmotic gradient o Length of LH ! Longer loop- more concentrated o Rate of active NaCl reabsorption in TALH ! $ luminal Na delivery to TALH = $ Na reabsorption ! High NaK ATP pump - $ NaCl reabsorption Protein content of diet o $ protein content = $ urea accumulation = $concentrating ability Medullary blood flow o # blood flow = $ high interstitial osmolality o $ blood flow = # concentrating ability Osmotic permeability of CT and CD to water o $AVP = $ H2O permeability = $ H2O reabsorption Luminal flow in LH and CD
$ flow = # countercurrent multiplier efficiency = #interstitium osmolality = $ conc Pathophysiology o Diabetic insipidus reduced AVP levels or responsiveness to AVP o
Micturition Urinary bladder empties when it is filled Sympathetic Innervation o T10-L2 o Hypogastric nerves o &-adrenergic receptors in bladder neck o Bladder storage, closure of urethra Parasympathetic Innervation o S2-S4 o Muscarinic o Sustained bladder contraction Somatic Innervation o Motor S2-S4 o Pudendal nerves o Controls voluntary muscles of external sphincter Micturition Reflex Storage Phase o Filling of bladder triggers micturition reflex o (-) parasympathetic o (+) pudendal nerves o relaxation of detrussor muscle o contraction of urethral sphincter Voiding Phase o Voluntary relaxation of external urethral sphincter o Relaxation of internal urethral sphincter o (+) parasympathetic o (-) pudendal nerves o contraction of detrussor muscle o relaxation of urethral sphincter Urge to void= 150 mL Sensation of bladder fullness= 400-500 mL
!"#$%&'()*+,-')
./0)12/)3456)
FLUID AND ELECTROLYTES Osmolality = water balance ECF volume = sodium balance Osmolarity = solutes per liter Osmolality = solutes per kg (not affected by temperature) 0.6 x BW = adult males = total body water o 2/3s intracellular o 1/3s extracellular ! ! of ECF = plasma volume ! " of ECF = interstitial fluid Major Cations and Anions in ECF o Na+ (145) o Cl- (105) o HCO3- (25) o pH= 7.4 ICF o K+ (150) o Phosphorus (100) o pH=7.1 More protein in plasma than interstitial fluid More water in thin than fat people Inc Hypertonic solution (10% NaCl) o Inc osmolality o Dec ICF volume o Inc ECF volume o Inc plasma Na+ o Inc urine Na+ Inc Water (hypotonic) o Dec osmolality o Dec plasma Na+ o Inc ECF and ICF volume o Inc urine Na+ Inc Isotonic (0.9% NaCl) o No change in osmolality o Inc ECF volume only o Inc urine Na+ Starlings forces o Filtration and reabsorption ! Filtration = algebraic sum (+) = net force at arterial end ! Absorption = (-) = net force at venous end o Edema, nephrotic syndrome, CHF Maximally concentrated urine = 1200 mOsm/kg H2O ; 500 ml/24 hours Total osmolality = effective + ineffective osmoles Effective osmole = cannot cross cell membrane; restricted to ECF only o Sodium, glucose, mannitol o Affects total osmolality and tonicity Ineffective osmoles o Crosses freely o Found in both compartments o Total osmolality not tonicity o Cannot affect water shifts o Urea, ethanol, methanol o Urea in blood = ineffective osmole
Urea in urine = effective osmole = keeps medullary interstitium hyperosmotic Total osmolality = 2 Na + (Glucose/18) + (BUN /2.8) + (every solute/mol wt) Estimation of osmolality = 2 x (plasma Na) Control of ECF osmolality o Osmoreceptor ADH system ! High plasma osmolality " inc ADH " dec UO, perspiration; inc water reabsorption, vasoconstriction, BP " to dec plasma osmolality ! Low plasma osmolality " dec ADH o Thirst mechanism ! Respond only to effective osmoles ! Inc plasma osmolality " thirst center stmulation " inc water intake ! Inc plasma osmolality " excretion of hyperosmotic urine ! " to dec plasma osmolality ! Set point = 295 mOsm Because kidneys cannot concentrate urine greater than 1200 mOsm Threshold o If below 280 mOsm/ kg water = no ADH release o If > 280 = ADH is released o Direct linear relationship o Steep = minute changes can lead to response o Change of 3-5% in setpoint (275-290 mOsm) " ADH release Baroreceptors o Low pressure receptors = pulmonary vasculature = responds to high volume o High pressure = carotid sinus and aorta = responds to high pressure o 5-10% drop in BP = ADH release Actions of ADH: o Inc permeability of CD to water o Inc permeability of medullary portion of CD to urea o ADH stimulates reabsorption of NaCl by TALH, DT and CD Change in plasma osmolality is more potent stimulator of ADH secretion than change in blood volume or pressure (+) water balance = low osmolality = low Na (-) water balance = high osmolality = high sodium (+) na balance = hypervolemia/ volume expansion (-) na balance = hypovolemia = volume depletion Where sodium goes, water follows Effective circulating volume is directly related to: o ECF volume o Arterial BP o CO Volume sensors: o
!"#$%&'()*+,-')
./0)12/)3456)
Low pressure = responds to fullness/ stretch ! ANP, BNP o High pressure responds to changes in pressure ! Carotid sinus, aortic arch, JG apparatus of kidneys in afferent arteriole Signals of ECF volume and renal NaCl excretion o RAAS JG cells release renin o Sympathetic NS " afferent > efferent vasoconstriction " dec capillary hydrostatic pressure " dec GFR ! Dec GFR ! Inc renin, nacl reabsorption in PT, TALH, DT and CD o ANP opposite of RAAS and SNS ! Inc GFR ! Dec renin, aldosterone, sodium and water reabsorption in CD ! Dec ADH effect on CD Euvolemia o CD is main segment where Na reabsorption is adjusted o CD determines amt of sodium that will be excreted in urine o Operates on glomerulotubular mechanism o Normal sodium excretion = 1% Hypovolemia o Inc RAAS and SNS activity o Dec GFR o Inc na reabsorption in PT and CD o Dec renal na excretion = 0% Hypervolemia o Dec RAAS and SNS o Inc ANP, urodilatin from DT o Inhibit ADH o Dec renin "dec angiotensin 2 o Inc renal sodium excretion = 6% o Osm Regulation Volume Regulation Effective circulating volume HIGH and LOW pressure baroreceptors: Carotid sinus Afferent arteriole Atria RAAS SNS ANP ADH Urine Na excretion
Stimulus Sensors
Plasma osmolality Hypothalamic osmoreceptors
Effectors
ADH Thirst Urine osmolality and intake (thirst)
Response
POTASSIUM Major intracellular cation Important for repolarization
Dec K = difficult to stimulate Inc K = inactivation of fast sodium channels PT = passive K absorption TALH = recycles K back into lumen DT o Principal cell = K secretion o Intercalated cell = K absorption Physiologic factors: o Epinephrine ! Alpha receptors = K release ! Beta receptors = K uptake o Insulin major regulator of plasma K level o Aldosterone - K excretion Pathophysiologic factors: o Acid base balance ! Low pH " low K uptake " low intracellular K and displace K for H+ " K exits o Inc plasma osmolality " cell shrinks " inc intracellular K " K exits o Cell lysis " inc K in ECF o Exercise " inc K in ECF ! Walking = inc by 0.3 mEqs/ L ! Vigorous = inc up to 2 mEqs/ L Drugs that induce hyperK o Dietary supplement o Ace inhibitor o K sparing diuretic spirinolactone o Heparin Acidosis = K efflux Alkalosis = K influx Inc plasma K " inc K secretion Aldosterone " inc NaKATPase in basolateral membrane " K secretion o Inc aldosterone " in NaKATPase " K inside, sodium outside " inc ENaC, inc SGK " inc CAP " K permeability to lumen " K secretion Inc tubular flow rate " inc K secretion o Inc flow " cilia bends " activation of PKD1/ PKD2 and calcium entry " calcium influx activates MAXI-K " K secretion o Inc flow " Na influx Inc glucocorticoids " inc GFR, K secretion ENaC amiloride sensitive epithelial sodium channel o Sodium goes in/ reabsorbed " lumen becomes negative o K is secreted by ROMK and MAXI-K to make lumen (+) electrochemical gradient o Amiloride inhibits ENaC ROMK channel o Low conductance o Basal K secretion MAXI-K o High conductance o Calcium activated o Flow stimulated K secretion Acute acidosis " dec K secretion
!"#$%&'()*+,-')
./0)12/)3456)
Chronic acidosis " inc K secretion Low ECV " inc aldosterone " inc K excretion o
CALCIUM Bone formation Regulators: o PTH " inc plasma Ca = bone resorption o Calcitriol " inc plasma Ca = from kidney : activated form of VitD ! Inc calcium absorption in gut o Calcitonin " dec plasma Ca = bone formation Inc plasma Ca " inc calcitonin Dec plasma Ca " inc PTH PT = transcellular (20%) and paracellular (20%) TALH no paracellular calcium is not reabsorbed by solvent drag because TALH is impermeable to water o 20% transcellular DT = active transport Ca reabsorption o Exclusively transcellular o No paracellular in DT and TALH o Ca enters through Ca permeable epithelial channel (TRPV5/6) o Calcium inside binds to calbindin " calbindin-Ca complex " deliver Ca to basolateral membrane o At basolateral membrane " calcium is extruded via Ca-ATPase (PMCa1b) or 3Na1Ca antiporter (NCX1) Phosphate Inc excretion o inc PTH o Phosphate loading o Volume expansion o Acidosis o Glucocorticoids Dec excretion o Dec PTH o P depletion o Volume contraction o Alkalosis o GH Calcitonin o Major stimulus hypercalcemia ! inc bone formation ! dec bone resorption ! minor effect on kidney and GIT ! overall effect: dec calcium PTH, calcitonin, calcitriol " inhibits Ca excretion Dec plasma Ca " inc PTH " inc P excretion and dec Ca excretion via kidneys Inc plasma Ca " inc calcitonin " inc P excretion and dec Ca excretion via kidneys PT = mainly transcellular o Uptake via Na-P symporter (NPT1, NPT2, NPT3) ! NPT1 = 2Na-1P
! NPT 2 and 3 = 3Na 1P ! NPT 2 is most important Inorganic phosphate exits basolateral membrane using inorganic phosphate anion antiporter
ACID-BASE PHYSIOLOGY Acid proton donor Base proton acceptor Volatile acids CO2, ketones o Excreted by lungs Non-volatile acids/ fixed/ metabolic acid lactic acid o Excreted by kidney Normal blood pH = 7.35-7.45 Low pH = acidosis High pH = alkalosis Acidosis o Decrease in pH o Dec base or inc acid = dec pH = inc H+ concentration o Inc pCO2, dec HCO3 Alkalosis o Inc in pH o Dec pCO2, inc HCO3 Compensation o There is return to normal blood pH o 20:1 ratio (HCO3/ pCO2) Acid base balance Buffer ability to minimize changes in pH pH expression of H+ concentration o varies inversely with H+ concentration o low pH = high H+ Bicarbonate buffer pKa = 6.1 most important buffer in ECF because of high concentration can maintain pCO2 at constant level Phosphate buffer pKa = 6.8 o not far from 7.4 o better chemical buffer in a closed system than bicarbonate but with low plasma concentration important in renal tubular fluids impt in ICF where phosphate is abundant Protein buffer most powerful buffer most plentiful in the body, pK of proteins are not far from 7.4 with dissociated carboxyl groups on acidic amino acids = multiple negative charges bone buffers calcium bicarbonate for prolonged metabolic acid-base disorders
!"#$%&'()*+,-')
./0)12/)3456)
TIME TO COMPENSATE chemical buffers = seconds respiratory = mins to hours renal = hours to days Intracellular buffers organic and inorganic phosphates hemoglobin o major buffer for H+ produced in RBC ! deoxyHgb more powerful than oxyHgb " oxy unloading " inc CO2 carriage (Haldane effect) ! chloride shift chloride goes in RBC, hco3 goes out to plasma o 6x more impt quantitatively than plasma proteins ! Concentration is twice as much ! Each hgb molecule = 3x more histidine residues than average plasma protein Imidazole group = can provide buffering capacity at physiologic pH (pK=6.8) Isohydric principle = any condition that causes H+ concentration to change " all buffer systems change at the same time " buffer system buffers each other by shifting H+ from one to another buffer system Studying the behavior of one buffer system is adequate Renal regulation of acid base balance: H+ ion secretion " excretion of H+ as titrable acid (H2PO4-); excretion of H+ as NH4+ Bicarbonate reabsorption Production of new bicarbonate ions H+ secretion in PT is responsible for 90% of filtered bicarbonate Na-H linked transport system (Na-H antiporter) " influx of Na " H+ secretion to lumen Presence of carbonic anhydrase on brush border of PT " reabsorption of HCO3 DT No carbonic anhydrase H+ secreted is mostly buffered by phosphate buffer o Occurs in intercalated cells o HATPase pump are responsible for movement of H+ ions into lumen o Maximally acidic urine production
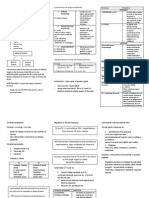
Ammonia = NH3:H = 1:1 o More important quantitatively o Urinary H+ excretion (2/3 of excreted H+ due to ammonia) o Most acidic region = CD o Ammonium formation in PT o Ammonium reabsorption in TALH to prevent loss of NH4 o Ammonium trapping in CD o Dec pH " inc H+ secretion " inc NH4 production o Inc pCO2 " inc H+ secretion " inc NH4 production o Dec K " in renal ammonia production " inc H+ secretion in exchange for K absorption o Aldosterone " H+ secretion and Na absorption Condition Etiology Primary Compensatory biochemica mechanism l alteration Respi Impaired respi Inc pCO2 Intracellular acidosis drive (narcotics, buffers " RBC CNS lesion) generate HCO3 b exchanging Chest wall Na, K ions with disorder (burns, H+ (acute) scoliosis) Increased renal Respi muscle acid excretion weakness " inc synthesis (spinal cord of HCO3 injury, severe (chronic) hypoK) Airway obstruction (laryngospasm) Pulmonary disorders (COPD) Hypoxemia " hyperventilation
Respi alkalosis
Dec pCO2
Reduce HCO3 production in RBC Decreased renal acid excretion " decrease plasma HCO3 Increase serum HCO3 levels Hyperventilatio n to dec pCO2 Inc urinary excretion of H+
Metaboli c acidosis
Inc anion gap (ketoacidosis, uremia) Normal anion gap (GI loss of HCO3, exogenous administration of chloride) Loss of GI secretions (vomiting)
Dec HCO3
Urine buffers Phosphate buffers o Depends on phosphate intake o PO4:H ratio = 5:4 o Cannot increase in response to acid load o Little regulation of acid excretion
Metaboli c alkalosis
Inc HCO3
Dec HCO3 levels Hypoventilation
!"#$%&'()*+,-')
./0)12/)3456)
Diuretics " bicarbonate rich fluid in ECF " contraction alkalosis Rapid correction of chronic hypercapnea Inc mineralocorticoi d activity Severe hypoK
to inc pCO2 Inc excretion of HCO3
ANION GAP = Na (Cl + HCO3) Normal = 12+- 4 mEq/L (8-12) Law of electroneutrality o Total cation = total anion UA UC = anion gap For differential diagnosis of metabolic acidosis Normal anion gap metabolic acidosis Dec HCO3 " inc Cl to compensate "normal AG o Hyperchloremic acidosis o Isotonic solution infusion o Diarrhea = alkaline pH of stool = normal AG o Acetazolamide = carbonic anhydrase inhibitor = low HCO3 absorption = normal AG High anion gap metabolic acidosis Excess acid If non-chloride acid is introduced Dec HCO3 " Cl no change " high AG Hypertonic solution infusion Methanol, uremia, DKA, paraldehyde, ischemia (lactic acidosis), isoniazid, ethanol, salicylates Parameters pH pCO2 HCO3 pO2 Normal Values 7.35-7.45 35-45 22-26 80-100
PaO2 changes with age Corrected PaO2 = 80 minus age in years above 60 AaDO2 difference between alveolar O2 (PAO2) and arterial O2 (PaO2) Inc AaDO2 = abnormal O2 exchange Normal = less than 15 mmHg Value increases normally approximates 3 mmHg per decade of life Less than 25 mmHg is considered the upper limit of normal AaDO2
!"#$%&'()*+,-')
./0)12/)3456)
Anda mungkin juga menyukai
- Practical Gastroenterology and Hepatology Board Review ToolkitDari EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultBelum ada peringkat
- ShockDokumen21 halamanShockMin-Joo Esther ParkBelum ada peringkat
- Physiology of VomitingDokumen24 halamanPhysiology of VomitingKingWayne Tagatac BajoBelum ada peringkat
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Regional AnesthesiaDokumen54 halamanRegional AnesthesiaIdza Fariha AfriBelum ada peringkat
- 1 - Fluid and Electrolytes (Schwartz Based)Dokumen52 halaman1 - Fluid and Electrolytes (Schwartz Based)Alexandra RebosuraBelum ada peringkat
- Cholinergics and Anticholinergics DrugsDokumen50 halamanCholinergics and Anticholinergics Drugsjoeyjose18Belum ada peringkat
- Ks Module 12Dokumen29 halamanKs Module 12jerinthomasrajanBelum ada peringkat
- Renal PhysiologyDokumen75 halamanRenal PhysiologyAmanuel Maru100% (1)
- MicturitionDokumen7 halamanMicturitionOsama MohamedBelum ada peringkat
- Renal PathologyDokumen5 halamanRenal PathologyEmmanuel De LeonBelum ada peringkat
- Review of Anatomy and PhysiologyDokumen7 halamanReview of Anatomy and PhysiologyKyla CalzadoBelum ada peringkat
- GastrointestinalDokumen39 halamanGastrointestinalالمسوول الاعلاميBelum ada peringkat
- Presented By: DR Sharmila G SDokumen76 halamanPresented By: DR Sharmila G SSharmila Shivakumar G SBelum ada peringkat
- Urinary SystemDokumen2 halamanUrinary SystemCharlayne AnneBelum ada peringkat
- Acidification of UrineDokumen30 halamanAcidification of UrineNanditha SureshBelum ada peringkat
- Blood Pressure Regulation-2Dokumen40 halamanBlood Pressure Regulation-2Juliza FelicianoBelum ada peringkat
- 2018 Overview Digestive System HandoutDokumen11 halaman2018 Overview Digestive System HandoutdraganBelum ada peringkat
- Water and Electrolyte ImbalanceDokumen17 halamanWater and Electrolyte Imbalancemhairat6043100% (1)
- Department of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaDokumen39 halamanDepartment of Kriyasharir: Mahatma Gandhi Ayurved College Hospital & Research Centre Salod (H), WardhaAvanti ShendurjaneBelum ada peringkat
- Urine Formation: Reabsorption and Secretion, and Water ConservationDokumen5 halamanUrine Formation: Reabsorption and Secretion, and Water ConservationAshraf Moby100% (1)
- Opioid Analgesics & Antagonists: Dr. Hayder B Sahib Ph.D. PharmacologyDokumen47 halamanOpioid Analgesics & Antagonists: Dr. Hayder B Sahib Ph.D. Pharmacologyarham pirachaBelum ada peringkat
- Hepatobiliary Disorders: Katrina Saludar Jimenez, R. NDokumen42 halamanHepatobiliary Disorders: Katrina Saludar Jimenez, R. NKatrinaJimenezBelum ada peringkat
- Heme Degradation & HyperbilirubinemiasDokumen30 halamanHeme Degradation & HyperbilirubinemiasSubhi MishraBelum ada peringkat
- Lung Transplant PathwayDokumen39 halamanLung Transplant PathwayMohana Preethi MBelum ada peringkat
- Renal Failure PresentationDokumen65 halamanRenal Failure PresentationBhawna JoshiBelum ada peringkat
- Renal Reabsorption and SecretionDokumen5 halamanRenal Reabsorption and SecretionTawhid ZihadBelum ada peringkat
- Physiological Regulation of Arterial Blood PressureDokumen36 halamanPhysiological Regulation of Arterial Blood PressureFrancesBelum ada peringkat
- NocturiaDokumen10 halamanNocturiaKousik AmancharlaBelum ada peringkat
- X.0Y Control of Peripheral Circulation: OutlineDokumen4 halamanX.0Y Control of Peripheral Circulation: OutlineAya ARBelum ada peringkat
- Pgi Chandigarh May 2010 EbookDokumen49 halamanPgi Chandigarh May 2010 EbookJeetendra Singh100% (2)
- The Gastro-Intestinal SystemDokumen12 halamanThe Gastro-Intestinal SystemRenelyn ComiaBelum ada peringkat
- Drugs Affecting Calcium BalanceDokumen63 halamanDrugs Affecting Calcium BalanceRd Chandane100% (1)
- Fluid and Electrolyte Imbalance and Nutritional ProblemDokumen98 halamanFluid and Electrolyte Imbalance and Nutritional ProblemPaul EbenezerBelum ada peringkat
- Hepatobiliary Disorders 2Dokumen21 halamanHepatobiliary Disorders 2KatrinaJimenezBelum ada peringkat
- Pathophysiology 2Dokumen92 halamanPathophysiology 2Princess AgarwalBelum ada peringkat
- Internal CapsuleDokumen25 halamanInternal CapsuleMadan KumarBelum ada peringkat
- INTUSSUSCEPTIONDokumen3 halamanINTUSSUSCEPTIONS GBelum ada peringkat
- Jaundice 03Dokumen24 halamanJaundice 03kuldeep sainiBelum ada peringkat
- Carcinoma of The Breast - Bailey & LoveDokumen5 halamanCarcinoma of The Breast - Bailey & LoveKeyshia Yazid100% (1)
- The Cardiac CycleDokumen9 halamanThe Cardiac CycleKaylababy Hamilton BlackBelum ada peringkat
- CVS Lect 6 Blood Pressure, PathophysiologyDokumen13 halamanCVS Lect 6 Blood Pressure, PathophysiologySherwan R Shal100% (5)
- Burns Pathophysiology 2Dokumen1 halamanBurns Pathophysiology 2Monique Ann DanoyBelum ada peringkat
- 18 NCP Ileal ConduitDokumen11 halaman18 NCP Ileal ConduitICa MarlinaBelum ada peringkat
- Renal 2 MTC PDFDokumen55 halamanRenal 2 MTC PDFDrbee10Belum ada peringkat
- Acute Renal FailureDokumen5 halamanAcute Renal FailureJean De Vera MelendezBelum ada peringkat
- Non Viral HepatitisDokumen40 halamanNon Viral Hepatitisostaz2000100% (1)
- Jugular Venous PressureDokumen9 halamanJugular Venous Pressuremoh86-Belum ada peringkat
- Cardiovascular System: by DR - Nuha Abdel GhaffarDokumen41 halamanCardiovascular System: by DR - Nuha Abdel GhaffarMohammed Alaa EldeanBelum ada peringkat
- 3.0 Grand Physiology Finals Compilation - Batch 2017Dokumen89 halaman3.0 Grand Physiology Finals Compilation - Batch 2017Sheryl Layne Lao-SebrioBelum ada peringkat
- Endocrine DisordersDokumen3 halamanEndocrine DisordersIrish OrleansBelum ada peringkat
- Pre AnaestheticsDokumen69 halamanPre AnaestheticsPraney SlathiaBelum ada peringkat
- Fluid and Electrolyte ImbalanceDokumen27 halamanFluid and Electrolyte ImbalanceSimmi Sidhu100% (1)
- Anatomy and PhysiologyDokumen24 halamanAnatomy and PhysiologyGillarhymesBelum ada peringkat
- Disorders of The Reproductive SystemDokumen10 halamanDisorders of The Reproductive SystemRose Kathreen Quintans AuxteroBelum ada peringkat
- Physiology of PainDokumen35 halamanPhysiology of PainJauhar Firdaus50% (2)
- Posture and EquilibriumDokumen26 halamanPosture and Equilibriumshwetha pc100% (1)
- AntibioticsDokumen30 halamanAntibioticsRoza RahbeniBelum ada peringkat
- Anatomy of EsophagusDokumen18 halamanAnatomy of Esophagusgabbyneng0% (1)
- Revalida ReviewerDokumen15 halamanRevalida ReviewerNicole ChanBelum ada peringkat
- Nephrotic SyndromeDokumen66 halamanNephrotic SyndromeNicole ChanBelum ada peringkat
- Derma MegatableDokumen21 halamanDerma MegatableNicole ChanBelum ada peringkat
- Fpgee ProcessDokumen3 halamanFpgee ProcessNicole ChanBelum ada peringkat
- Nad / Nadp: 3. Coenzyme Q / UbiquinoneDokumen4 halamanNad / Nadp: 3. Coenzyme Q / UbiquinoneNicole ChanBelum ada peringkat
- The Parts of The Human Reproductive System and Their FunctionsDokumen13 halamanThe Parts of The Human Reproductive System and Their FunctionsRhodora Rendon OrizonteBelum ada peringkat
- Respiratory SystemDokumen2 halamanRespiratory Systemlim.angelyne0126Belum ada peringkat
- Weight Training: Abs, Legs & Butt: Firm Up From The Waist DownDokumen6 halamanWeight Training: Abs, Legs & Butt: Firm Up From The Waist Downbloom manelBelum ada peringkat
- 16 Immune System Review SheetDokumen2 halaman16 Immune System Review Sheetjohn gusmanBelum ada peringkat
- Branchial Cleft CystsDokumen8 halamanBranchial Cleft CystsHere LeafsBelum ada peringkat
- Updated NCM 107 Lecture Week 7Dokumen27 halamanUpdated NCM 107 Lecture Week 7Quencee CalaycayBelum ada peringkat
- Autoimmune Protocol Ebook 6 19Dokumen306 halamanAutoimmune Protocol Ebook 6 19Hrvoje100% (12)
- Unit 7 - Respiratory SystemDokumen51 halamanUnit 7 - Respiratory SystemAbdullah MohammedBelum ada peringkat
- FA16Dokumen22 halamanFA16Jay ZBelum ada peringkat
- Cell PlantDokumen7 halamanCell PlantEbiz MarkBelum ada peringkat
- Abortion - PPT For 2nd MSCDokumen1 halamanAbortion - PPT For 2nd MSCArjesa TakaBelum ada peringkat
- Structured - Biology HLDokumen14 halamanStructured - Biology HLnur shahirahBelum ada peringkat
- Atlas Human Anatomy Ciba NetterDokumen641 halamanAtlas Human Anatomy Ciba Netterxxxx79% (28)
- CellsDokumen19 halamanCellsAulia Safri NahriyahBelum ada peringkat
- Grade 6 ScienceDokumen10 halamanGrade 6 ScienceSanjeev NBelum ada peringkat
- Biological Membranes A Biology Questions AQA OCR Edexcel PDFDokumen3 halamanBiological Membranes A Biology Questions AQA OCR Edexcel PDFbekoBelum ada peringkat
- Meningitis Ein 3Dokumen42 halamanMeningitis Ein 3Rifqi FuadiBelum ada peringkat
- Basic Cardiac Structure and FunctionDokumen13 halamanBasic Cardiac Structure and FunctiondeaBelum ada peringkat
- Joseph Pilates - 34 Classic Mat Exercises - LongversionDokumen11 halamanJoseph Pilates - 34 Classic Mat Exercises - Longversionmxpxaxo100% (1)
- Hematology & Immune SystemDokumen81 halamanHematology & Immune SystemAmanuel Maru100% (1)
- Cell Structure and Function: Powerpoint Presentations Prepared by Mindy Miller-Kittrell, North Carolina State UniversityDokumen96 halamanCell Structure and Function: Powerpoint Presentations Prepared by Mindy Miller-Kittrell, North Carolina State UniversityVia SongcalBelum ada peringkat
- Gingival Absorption of Rat Periodontal Disease Model and Rat Tooth Movement ModelDokumen7 halamanGingival Absorption of Rat Periodontal Disease Model and Rat Tooth Movement ModelLouis HutahaeanBelum ada peringkat
- Morphology of Moulds/ Molds A. ThallusDokumen3 halamanMorphology of Moulds/ Molds A. ThallusJane LappaoBelum ada peringkat
- Human Anatomy,: First Edition Mckinley & O'LoughlinDokumen77 halamanHuman Anatomy,: First Edition Mckinley & O'LoughlinHarman BainzBelum ada peringkat
- WOAg B7 My 1 HJmy GGN EYOFDokumen41 halamanWOAg B7 My 1 HJmy GGN EYOFandrewmanshionBelum ada peringkat
- Pschology 2Dokumen35 halamanPschology 2Sarah Mae SaringanBelum ada peringkat
- Hereditary Spherocytosis and Hereditary ElliptocytosisDokumen40 halamanHereditary Spherocytosis and Hereditary ElliptocytosisJosh Matthew RosalesBelum ada peringkat
- Reproduction in Animals: Plants" in Class Seventh. Now You WillDokumen18 halamanReproduction in Animals: Plants" in Class Seventh. Now You WillvenkataBelum ada peringkat
- Local Media5289763584533511516Dokumen8 halamanLocal Media5289763584533511516Haniya KhanBelum ada peringkat
- Chapter 8 The Endocrine SystemDokumen56 halamanChapter 8 The Endocrine SystemSainuddinSaddinBelum ada peringkat