Treatment of Fractures
Diunggah oleh
Ng Lily KhoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Treatment of Fractures
Diunggah oleh
Ng Lily KhoHak Cipta:
Format Tersedia
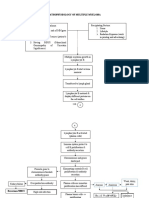
Treatment of Fractures Principles of Treatment Treat the Patient, not only the fracture Treatment of the fracture: Manipulation
ation Splintage Joint movement and function: must be preserved Exercise and early weight bearing Main objs = REDUCE! HOLD! EXERCISE!
Normal alignment of the bone fragments
Methods of reduction 1. Manipulation 2. Mechanical traction 3. Open operation
1. Manipulation Closed manipulation is suitable for 1. All minimally displaced fractures 2. Most fractures in children 3. Fractures that are likely to be stable after reduction 4. 1. Manipulation Unstable fractures are sometimes reduced closed prior to mechanical fixation Three fold maneuver: under anesthesia and muscle relaxation 1. The distal part of the limb is pulled in the line of the bone 2. The fragments are repositioned as they disengage 3. Alignment is adjusted in each plane 2. Mechanical Traction Some fractures are difficult to reduce by manipulation They can often be reduced by sustained mechanical traction, which then serves also to hold the fracture until it starts to unite In some cases, rapid mechanical traction is applied prior to internal fixation Mechanical traction involves repetitive or sustained longitudinal distraction of spinal joints of the neck or low back. With its use we can provide relief of pain and pressure and normalize neurological signs/symptoms i.e. from disc disease/protrusions or spinal arthritis.
The Fracture Quartet Dual Conflict Hold vs Move Speed vs Safety
Closed Fractures
REDUCTION Restoration of the fracture fragments to anatomic alignment and positioning
Types: a. Closed reduction through manipulation or manual traction b. Open reduction internal fixation devices may be used to hold the fragments in position until solid bone healing occurs. REDUCTION No undue delay in attending to the fracture Reduction unnecessary when: REDUCTION Aim of reduction Adequate apposition There is little or no displacement Displacement does not matter Reduction is unlikely to succeed Closed Fractures Closed Fractures
3. Open Operation Indication: 1. When closed reduction fails
2. When there is a large articular fragment that needs accurate positioning 3. For avulsion fractures in which the fragments are held apart by muscle pull 4. When an operation is needed for associated injuries 5. When a fracture will anyhow need internal fixation to hold it Hold Restriction of movement Prevention of displacement Alleviation of pain Promote soft-tissue healing Try to allow free movement of the unaffected parts
used to control muscle spasms and to immobilize an area before surgery Accomplished by using a weight to pull on traction tape or on a foam boot attached to the skin Amount of the weight applied must not exceed the tolerance of the skin Types of SKIN TRACTION a. Bucks extension traction skin traction to the lower leg
Used to immobilized fractures of the proximal femur before surgical fixation Bucks extension traction One nurse elevates and supports the extremity under the patients heel and knee while another nurse places the foam boot under the leg with the patients heel of the boot. The nurse secures Velcro straps around the leg Traction tape overwrapped with elastic bandage in a spiral fashion Then passes the rope affixed to the spreader or footplate over a pulley fastened to the end of the bed and attaches the prescribed weight usually 5-8 lbs to the rope
Splint the fracture, not the entire limb Methods of holding reduction: Sustained traction Cast splintage Functional bracing Internal fixation External fixation
Closed vs. operative methods
1. Sustained Traction Traction is applied to the limb distal to the fracture, so as to exert a continuous pull in the long axis of the bone In most cases a counterforce will be needed Particularly useful for spiral fractures of longbone shafts, which are easily displaced by muscle contraction The hold is not perfect, but it is safe and the patient can move the joints and exercise the muscles. The problem is the lack of speedcomplications
b. Russell Traction Knee is suspended in a sling attached to a rope and pulley on a Balkan frame, creating upward pull from the knee (vertical traction) Weights are attached to the foot of the bed creating horizontal traction. It has vertical and horizontal weights. Used to treat fracture of the femur. It can immobilize more than one bone. Allows patient to move about in bed more freely and permits bending of the knee joint Hip should be flexed at 20-30 degrees. Foot of bed usually elevated by shock blocks to provide counter traction.
Types of traction: 1. SKIN TRACTION
Assess back of the knee for pressure sores; check the leg for signs and symptoms of thrombophlebitis.
b. Thomas splint with Pearson attachment Used with skeletal traction I fractures of the femur , hip should be flexed at 20 degrees. Use footplate to prevent footdrop. Check pressure sore at the inguinal area (groin).
c. Bryant traction Are raised 90 degrees angle to bed. Because the weight of the child is not adequate to provide countertraction. Used for children under 2 years or below 30 pounds to treat fractures of the femur and hip dislocation. Buttocks must be slightly off the mattress. To enhance efficacy of the weight as countertraction. Knees slightly flexed. To prevent hyperextension deformity of the knees. Hyperextension deformity of the knees will make the child unable to bend the knees when walking.
PRINCIPLES IN THE CARE OF THE CLIENT WITH TRACTION The line of pull should be in line with the deformity There should be an adequate countertraction. The weight of the body serves as the countertraction Apply traction continuously Allow the weights to hang freely. Weights should not touch the floor. Turn the client as indicated. Avoid friction. There should be knots along the rope. Do neurovascular check Prevent complications of immobility. Pin site care for skeletal traction Cleanse and apply antibiotic ointment as prescribed. Observe site for signs and symptoms of infection. Eg. Redness, swelling, pain, warmth, drainage. Notify the physician if these findings are noted. 2. Cast Splintage CAST a rigid external immobilizing device that is molded to the contours of the body To immobilize a reduced fracture, to correct a deformity, to apply uniform pressure to underlying soft tissue or to support and stabilize weakened joints
d. Cervical traction Cervical head halter attached to weights that hang over head of bed. Used for soft tissue damage or degenerative disc disease of cervical spine to reduce muscle spasm and maintain alignment. Usually intermittent traction, elevate head of bed to provide countertraction.
e. Pelvic traction Pelvic girdle is secured around iliac crest with extension straps attached to ropes and weights; used for low back to reduce muscle spasm and maintain alignment.
2. Skeletal traction Traction applied directly to the bones using pins, wires, or tongs ( eg. Crutchfield) that are surgically inserted ; used for fractured femur, tibia, humerus and cervical spine.
Types of skeletal traction a. Balanced suspension traction Produce by a counterforce other than the patients weight Extremity floats or balances in the traction apparatus Patient may change position without disturbing the line of traction
Kinds of casting materials: 1. Plaster casts Less costly and achieve a better mold than fiberglass casts Not durable and take longer to dry PLASTER of PARIS impregnated bandages are wet in cool water and applied smoothly to the body Requires 24-72 hours to dry completely
weight, stronger and more durable than plaster Consists of open-weave, nonabsorbent fabric impregnated with cool wateractivated hardeners that bond and reach full rigid strength in minutes Heat is given off while the cast is applied 1970s development of fiberglass casts More light and durable 1990s introduction of new casts lining completely waterproof, allowing patients to bathe, shower, and swim while wearing a cast
equipment Stockinette
Stockinette is usually the first layer applied over the area to be cast. Its ends can be folded over the cast edges to soften them. It may be omitted in acute fracture treatment as it may restrict swelling.
Shoulder spica cast: Minerva cast:
Webril Webril comes in a range of widths from 5-15 cm; the smallest ones are easiest to work with. 5-10 cm webril should be used for the upper extremity and 10-15 cm for the lower extremity. CARE OF THE CLIENT WITH CAST: o Carry the newly- casted body part with the palms of the hand. Elevate the body part with pillow. Expose the cast to dry. Sensation of heat as the cast is drying is normal. The cast should not be covered with a blanket or towel while it is drying because the retained heat can burn the client. Keep the cast clean and dry. PLASTER OF PARIS cast dries within ___ hours or longer especially larger cast. FIBERGLASS CAST may dry in _______ minutes and the client is allowed to have weight bearing in 30 minutes after cast application. Observe hot spots and musty odor, or drainage from the cast. Maintain skin integrity- by petalling (applying adhesive tapes at the edges of the cast to smoothen the areas). Do neurovascular checks the following findings distal to cast application indicate that the cast is TOO TIGHT. Skin color-
sheet wadding stretchable sheets of cotton padding used to cover the skin before a cast is applied. The stretching allows for some extremity edema without the cast becoming too tight.
o o o
Plaster of Paris Plaster is the most commonly used casting material because of its ease of use. Immersion in water initiates an exothermic reaction in the plaster causing it to harden. Once applied, it will feel hard within 4 minutes, however, it takes 23 days to dry completely. o
Bucket The bucket should be filled with water at or below room temperature. Cooler water decreases the risk of burning the patients skin as the plaster sets and also allows for more working time with the casting material. o
2. Fiberglass Casts Composed of water-activated polyurethane materials that have the versatility of plaster but lighter in
pallor, cyanosis Skin temperature cold skin Sensation numbness, tingling Mobility
with an elastic compression bandage to maintain immobilization 5. To control swelling and promote circulation, the extremity is elevated (but no higher than heart level, to minimize the effect of gravity on perfusion of the tissues.)
inability to move the body part Pulse absence of pulse ----6 Ps. P- oikilothermia P- aresthesias P- allor P- ain P- aralysis P- ulselessness o CARE OF THE CLIENT WITH CAST: WINDOWING done to facilitate observation under the cast. It is also done to assess pulse or prevent cast syndrome. The procedure involves REMOVAL OF THE PART OF THE CAST. CAST SYNDROME may occur if the client has body cast. It is manifested by bloated feeling prolonged nausea, repeated vomiting, abdominal dissention, vague abdominal pain.. shortness of breath. BIVALVING- is done for wound care or x-rays. It is also done when the cast is too tight or when healing process has occurred. The procedure involves SPLITTING OF THE CAST. Procedure for bivalving a cast
Health Teachings should include telling the pt about the following :
Until the cast has properly set, avoid direct heat such as hot water bottles. Rest the limb as much as possible to promote healing. Use the techniques shown to you by nursing staff to walk or manage day-to-day activities. For example, you risk further injury if you use crutches incorrectly. Avoid any lifting or driving until the fracture has healed. If you experience an itch, dont poke anything between the cast and your limb (such as a coat hanger or pencil). Do not use a hairdryer to blow cool air into the cast. Avoid getting your cast wet, as wet plaster becomes soft and does not provide the necessary support. Wet plaster can also cause skin irritation. When showering, wrap the cast in a plastic bag and tape it directly to the skin, keeping the area water-tight. Keep the cast clean and dry. Check for cracks or breaks in the cast. Rough edges can be padded to protect the skin from scratches. Do not scratch the skin under the cast by inserting objects inside the cast. Do not put powders or lotion inside the cast. Cover the cast while your child is eating to prevent food spills and crumbs from entering the cast. Prevent small toys or objects from being put inside the cast. Health Teachings should include telling the pt about the following :
1. With a cast cutter, a longitudinal cut is made to divide the cast in half. 2. The underpadding is cut with scissors. 3. The cast is spread apart with cast spreaders to relieve pressure and to inspect and treat the skin without interrupting the reduction and alignment of the bone 4. After the pressure is relieved, the anterior and posterior parts of the cast are secured together
See your doctor immediately if you experience swelling, blueness or loss of movement of the fingers or toes, pins and needles, numbness or increased pain. Elevate the cast above the level of the heart to decrease swelling. Encourage your child to move his/her fingers or toes to promote circulation. Do not use the abduction bar on the cast to lift or carry the child. Complications of cast splintage Liable to appear once the patient has left the hospital; added risk of delay before the problem is attended to 1. Tight cast 2. Pressure sores 3. Skin abrasion or laceration 4. Loose cast 3. Functional Bracing Prevents joint stiffness while still fracture splintage and loading permitting
Risk depends on: the patient, the surgeon, the facilities
Indications for internal fixation Fractures that cannot be reduced except by operation Fractures that are inherently unstable and prone to re-displacement after reduction Fractures that unite poorly and slowly Pathological fractures Multiple fractures Fractures in patients who present severe nursing difficulties
Complications of internal fixation Most are due to poor technique, equipment, or operating conditions Infection Iatrogenic infection is now the most common cause of chronic osteomyelitis Complications of internal fixation
Most commonly for fractures of the femur or tibia Since its not very rigid, it is usually applied only when the fracture is beginning to unite Comes out well on all four of the basic requirements: hold move speed safe
Non-union Excessive stripping of the soft tissues unnecessary damage to the blood supply in the course of operative fixation rigid fixation with a gap between the fragments
Indicated for longer use than splints May be made of plastic and other materials such as cloth, leather, metal, elastic and Velcro Functional arm brace Knee brace
Implant failure Refracture
5. External Fixation With external fixation, pins are inserted through the skin into the bone and held in place by an external frame. most successful in superficial bones e.g. tibial shaft. Avoid it in deeper bones e.g. the femur or humerus - here the chance of pin tract sepsis is greater.
4. Internal Fixation holds securely with precise reduction movements can begin at once (no stiffness and edema) speed: patient can leave hospital as soon as wound is healed, but full weight bearing is unsafe for some time safety= biggest problem! SEPSIS!!!
Permits adjustment of length and angulation Some allow reduction of the fracture in all 3 planes. Especially applicable to the long bones and the pelvis.
3. Inflamed or septic skin about a pin (not loose) Appropriate (oral) antibiotic 4. Septic Loose Pin - remove, and replace with another through normal skin Exercise Restore function to the injured parts and the patient as a whole
Indications: 1. Fractures associated with severe softtissue damage where the wound can be left open for inspection, dressing, or definitive coverage. 2. Severely comminuted and unstable fractures, which can be held out to length until healing commences. 3. Fractures of the pelvis, which often cannot be controlled quickly by any other method. 4. Fractures associated with nerve or vessel damage.
Objectives: Restore circulation Prevent soft tissue adhesions Promote fracture healing Reduce edema Swellingtissue tension and blistering, joint stiffnes Soft Tissue care: elevate and exercise, never dangle, never force
5. Infected fractures, for which internal fixation might not be suitable. 6. Un-united fractures, where dead or sclerotic fragments can be excised and the remaining ends brought together in the external fixator; sometimes this is combined with elongation in the normal part of the shaft
Preserve joint movement Restore muscle power Guide patient back to normal activity
1. RANGE-OF-MOTION EXERCISES (ROM)
a. Active ROM- done by the patient. It increases and maintains muscle tone and joint mobility. b. Passive ROM- done for the patient. It maintains joint mobility. 1. RANGE-OF-MOTION EXERCISES (ROM) Active-assistive ROM- patient moves body part as far as possible and the health worker completes the exercise; or the stronger arm and leg perform exercises to the weaker arm and leg. Active- resistive ROM- is contraction of muscle against an opposing force or weight. It increases muscle power.
Complications of external fixation High degree of training and skill! Often used for the most difficult fractures increased likelihood of complications Damage to soft-tissue structures Over-distraction No contact between the fragments union delayed/prevented
Pin Care
Pin-track infection 2. ISOTONIC EXERCISES involves change in both muscle length and tension.
1. Clean the skin / pin interface of all discharges twice daily 2. Antiseptic dressings - "Betadine" (povidone) ointment
3. ISOMETRIC EXERCISES active exercise that involves alternate contraction and relaxation of muscle. There is no joint movement; the length of muscle does not change. It maintains muscle strength and size.
the cane and the affected leg are advanced together. To shift the weight unto the cane.
B. WALKER instruct client to use lift and walk technique (lift the walker forward, then make few small steps toward the walker) the height of the walker should be hip level. B. WALKER
a. Hamstring or Quadriceps setting alternate tension and relaxation of THIGH muscles. o o On supine position The client pushes the back of the knee against the mattress to contract thigh muscles. Hold for 5-10 seconds Repeat the exercise 10 times each hour when awake.
When GOING UP, USE THE WALKER AT THE BACK. WHEN GOING DOWN, USE THE WALKER IN FRONT. The walker is used to protect the client form falls. C. CRUTCHES 1. FOUR POINT GAIT Advance the right crutch, followed by the left foot then the left crutch, followed by the right foot. Weight bearing is allowed. left foot left crutch right
o o
b. Gluteal setting is alternate tension and relaxation of gluteus muscles. The client presses the buttocks together then release. It prevents thrombophlebitis. Gluteal setting
Right crutch foot
C. CRUTCHES
2. TWO POINT GAIT Advance the right crutch and left foot together, then the left crutch and the right foot together. Weight- bearing is allowed. Right crutch and left foot right foot C. CRUTCHES left crutch and
1. Position patient supine with legs extended if possible 2. Instruct patient to contract the muscles of the butocks 3. Encourage patient to hold the contraction for 5 to 10 seconds 4. Let the patient relax 5. Have patient repeat the exercise 10 times each hour when awake 3. ISOMETRIC EXERCISES
3. THREE POINT GAIT Advance both crutches and affected leg together, followed by the unaffected leg. Little or no weight- bearing is allowed, eg. After total hip replacement or total knee replacement. Both crutches and affected leg leg C. CRUTCHES unaffected
c. Kegels exercise is alternate tension and relaxation of pubococcygeal muscles. It helps regain control of voiding among incontinent clients.
4. SWING- TO GAIT Advance both crutches , swing the body so that the FEET WILL BE TO THE LEVEL OF THE CRUTCHES. C. CRUTCHES
ASSISTIVE DEVICES FOR WALKING A. CANE the client must hold cane on the unaffected hand
5. SWING- THROUGH GAIT
Advance both crutches, swing the body so that the FEET WILL BE PAST THE LEVEL OF THE CRUTCHES. C. CRUTCHES
Sterility and Antibiotic cover The wound must be kept covered until the patient reaches the operating theatre Antibiotics ASAP Most cases: Benzylpenicillin and flucloxacillin Even better: 2nd generation cephalosporin, every 6 hrs/48 hrs If heavily contaminated, cover for Gram (-) organisms and anaerobes by adding gentamicin or metronidazole and continuing treatment for 4 or 5 days Debridement and Wound Excision In the operating theatre, never in the ER! Under GA Maintain traction on injured limb and hold it still Remove clothing Replace dressing with sterile pad Clean and shave surrounding skin Remove pad and irrigate wound with A LOT of warm normal saline Do not use a tourniquet! Extend wound and excise ragged margins healthy skin edges Remove foreign materials and tissue debris Wash out wound again with warm NS (6-12 L) Remove devitalized tissue Best to leave cut nerves and tendons alone Wound Closure to close, or not to close the skin= difficult decision Uncontaminated types 1 and 2 wounds may be sutured All other wounds: delayed primary closure Type 3 wounds may occasionally have to be debrided more than once and skin closure may call for plastic surgery.
Going UP and down the stairs using CRUTCHES UP WITH THE GOOD; DOWN WITH THE BAD When going up the stairs, advance the good leg (unaffected leg) FIRST, followed by the bad leg and crutches. When going down the stairs, advance the bad leg (affected leg) and the crutches FIRST, followed by the good leg. Note: the bad leg should always be with the crutches to provide support.
-End OPEN FRACTURES Initial Management At the scene of the accident In the hospital
Types of Open Fractures The incidence of wound infection correlates directly with the extent of soft-tissue damage, <2% in type 1 >10% in type 3 rises with increasing delay in obtaining soft tissue coverage of the fracture.
Principles of Treatment of Open Fractures All open fractures assumed to be contaminated Prevent infection! The essentials: Prompt wound debridement Antibiotic prophylaxis Stabilization of the fracture Early definitive wound cover Repeated examination of the limb because open fractures can also be associated with compartment syndrome
Skin grafting= most appropriate if the wound cant be closed w/o tension and the recipient bed is clear, free of obvious infxn, and well vascularized
Stabilization of the Fracture Stability of the fracture is imp in Reducing the likelihood of infxn Assisting in recovery of the soft tissues
Method of fixation depends on: Degree of contamination Length of time from injury to operation Amount of soft tissue damage
Open fractures of all grades up to 3A treated as for closed injuries More severe injuries: combined approach by plastic and ortho surgeons The precise method depends on the type of soft-tissue cover that will be employed, although external fixation using a circular frame can accommodate to most problems
Aftercare and Team Work Post-op Limb is elevated Circulation carefully monitored Antibiotic cover continued; swab samples will dictate whether a diff. antibiotic is needed If wound has been left open, inspect in 2-3 days. Delayed primary suture is then often safe or, if there has been much skin loss, plastic surgery for grafting may be necessary
Teamwork For optimal results, open fractures with skin and soft-T damage are best managed by a partnership of ortho and plastic surgeons, ideally from the outset rather than by later referral If no plastic surgeon on site, use a digital camera for image transmission by internet to communicate and consult.
Anda mungkin juga menyukai
- NMAT Practice Set Part IIDokumen32 halamanNMAT Practice Set Part IIAlfred Benjamin Cajita93% (107)
- The Balance of PaymentsDokumen5 halamanThe Balance of PaymentsNg Lily Kho100% (1)
- Classroom RulesDokumen3 halamanClassroom RulesNg Lily KhoBelum ada peringkat
- Assembly of God Church Ozamiz City PhilippinesDokumen1 halamanAssembly of God Church Ozamiz City PhilippinesNg Lily KhoBelum ada peringkat
- Helping The EldersDokumen1 halamanHelping The EldersNg Lily KhoBelum ada peringkat
- PE of a Toy Skateboard on an Inclined PlaneDokumen1 halamanPE of a Toy Skateboard on an Inclined PlaneNg Lily KhoBelum ada peringkat
- BEC-PELC 2010 - EnglishDokumen26 halamanBEC-PELC 2010 - Englishmarcrisostomo60% (5)
- ResumeDokumen2 halamanResumeNg Lily KhoBelum ada peringkat
- Brilliance: What Are We Going To Sell During The Fair?Dokumen2 halamanBrilliance: What Are We Going To Sell During The Fair?Ng Lily KhoBelum ada peringkat
- The Passionate Shepherd To His LoveDokumen1 halamanThe Passionate Shepherd To His LoveNg Lily KhoBelum ada peringkat
- International TradeDokumen20 halamanInternational TradeNg Lily KhoBelum ada peringkat
- RelationshipsDokumen8 halamanRelationshipsNg Lily KhoBelum ada peringkat
- Everyman & Pardoner's TaleDokumen1 halamanEveryman & Pardoner's TaleNg Lily KhoBelum ada peringkat
- A Basketball Player Throws Up A Ball 5Dokumen2 halamanA Basketball Player Throws Up A Ball 5Ng Lily KhoBelum ada peringkat
- 11 - ACTW - Planning Reports and Proposals - Part 1Dokumen14 halaman11 - ACTW - Planning Reports and Proposals - Part 1Ng Lily KhoBelum ada peringkat
- BrillianceDokumen3 halamanBrillianceNg Lily KhoBelum ada peringkat
- 18eKeyQuestionAnswers Ch26Dokumen1 halaman18eKeyQuestionAnswers Ch26Pau LaguertaBelum ada peringkat
- The Big FourDokumen2 halamanThe Big FourNg Lily KhoBelum ada peringkat
- A Basketball Player Throws Up A Ball 5Dokumen1 halamanA Basketball Player Throws Up A Ball 5Ng Lily KhoBelum ada peringkat
- An Introduction To MacroeconomicsDokumen14 halamanAn Introduction To MacroeconomicsNg Lily KhoBelum ada peringkat
- Enron and Andersen Scandal-SynopsisDokumen6 halamanEnron and Andersen Scandal-SynopsisNg Lily KhoBelum ada peringkat
- Revenue CycleDokumen18 halamanRevenue CycleNg Lily KhoBelum ada peringkat
- ACTW - IntroductionDokumen18 halamanACTW - IntroductionNg Lily KhoBelum ada peringkat
- 107 RenaissancePeriodPresentationDokumen31 halaman107 RenaissancePeriodPresentationMarcos Dos SantosBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- VPDokumen20 halamanVPsales_vpnutritionBelum ada peringkat
- Usmle Step 2 CK Recalls 2021 3jz DR NotesDokumen22 halamanUsmle Step 2 CK Recalls 2021 3jz DR Notesmed student100% (2)
- Astigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedDokumen12 halamanAstigmidwife Vlogs Online Tutorial: All Rights Are Reserved. No Part of This Publication May Be ReproducedLynden BulanBelum ada peringkat
- Sympo Pokdi 1aDokumen96 halamanSympo Pokdi 1aQisti AshariBelum ada peringkat
- Classification of DSM IVDokumen14 halamanClassification of DSM IVAlfiah Amalia NurandaniBelum ada peringkat
- Rickettsial DiseasesDokumen44 halamanRickettsial DiseasesPrince AlexBelum ada peringkat
- Eye Ear Nursing1Dokumen16 halamanEye Ear Nursing1Arafah RahmaBelum ada peringkat
- Review Notes 2000 - Community MedicineDokumen40 halamanReview Notes 2000 - Community Medicineroberto10101985100% (2)
- Sally Magnusson - WHERE MEMORIES GO - 1st Chapter PDFDokumen15 halamanSally Magnusson - WHERE MEMORIES GO - 1st Chapter PDFThe Sunday TimesBelum ada peringkat
- Theresia Was Admitted With An Acute Pelvic Inflammatory DiseaseDokumen5 halamanTheresia Was Admitted With An Acute Pelvic Inflammatory DiseaseDessy Choerunnisa SuhermanBelum ada peringkat
- Dermatology MCQ With AnswersDokumen27 halamanDermatology MCQ With Answershesham0% (1)
- Psychiatric Care of The Older Adult Essay AssignmentDokumen9 halamanPsychiatric Care of The Older Adult Essay Assignmentapi-238869728Belum ada peringkat
- Pathophysiology of Multiple Myeloma OkDokumen3 halamanPathophysiology of Multiple Myeloma OkRifa'atul MahmudahBelum ada peringkat
- Disorders of Thought and SpeechDokumen50 halamanDisorders of Thought and SpeechTilarupa BhattaraiBelum ada peringkat
- Irritable Bowel SyndromeDokumen4 halamanIrritable Bowel SyndromeJehanzeb ZebBelum ada peringkat
- Bedside Rounds ZCMC Ward 8: History Taking and Physical ExaminationDokumen28 halamanBedside Rounds ZCMC Ward 8: History Taking and Physical ExaminationneilaldentanBelum ada peringkat
- Betty NeumanDokumen22 halamanBetty NeumanDONALDBelum ada peringkat
- Dress Syndrome A Review and UpdateDokumen5 halamanDress Syndrome A Review and UpdateCarlos Alberto Torres LópezBelum ada peringkat
- NBME Practice Test 2 Pt. 2Dokumen13 halamanNBME Practice Test 2 Pt. 2Zoë IndigoBelum ada peringkat
- CVD Case Study: Cerebrovascular Disease & HypertensionDokumen92 halamanCVD Case Study: Cerebrovascular Disease & HypertensionJohnMichaelDominguezBelum ada peringkat
- Coconut Water As MediumDokumen5 halamanCoconut Water As MediumCandy Kim50% (2)
- Malassezia furfur clinical syndrome and treatmentDokumen3 halamanMalassezia furfur clinical syndrome and treatmentJohn Christopher Luces100% (1)
- Asthma Treatment GuidlineDokumen56 halamanAsthma Treatment GuidlineEsther OdumanyeBelum ada peringkat
- Therapeutic Implications of DanceDokumen16 halamanTherapeutic Implications of DancekarinadapariaBelum ada peringkat
- MelatoninDokumen22 halamanMelatoninVassily RubachofBelum ada peringkat
- Resource Chart Medical Eligibility Contraceptives EnglishDokumen1 halamanResource Chart Medical Eligibility Contraceptives EnglishGoh Zheng YuenBelum ada peringkat
- Huron Hometown News - July 26, 2012Dokumen8 halamanHuron Hometown News - July 26, 2012schaffnerpubBelum ada peringkat
- XXXDokumen134 halamanXXXrhlzuraBelum ada peringkat
- Gordon's Functional Health PatternsDokumen2 halamanGordon's Functional Health PatternsKara GloriaBelum ada peringkat
- NCM 417 - Final Exam 2015Dokumen12 halamanNCM 417 - Final Exam 2015Mae DacerBelum ada peringkat