989104
Diunggah oleh
diyan110Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
989104
Diunggah oleh
diyan110Hak Cipta:
Format Tersedia
April 2007 - Vol.
156 Issue 4 Page 613-791
Snippets
RESEARCH SNIPPETS
pages xvixvi
Cutaneous biology
Expression of matrilysin (matrix metalloproteinase-7) in primary cutaneous and metastatic
melanoma
K. Kawasaki, T. Kawakami, H. Watabe, F. Itoh, M. Mizoguchi and Y. Soma
pages 613619
The distribution of melanin in skin determined in vivo
P.J . Matts, P.J . Dykes and R. Marks
pages 620628
Scratching and noxious heat stimuli inhibit itch in humans: a psychophysical study
G. Yosipovitch, M.I. Duque, K. Fast, A.G. Dawn and R.C. Coghill
pages 629634
Clinical and laboratory investigations
Coexistence of IgA antibodies to desmogleins 1 and 3 in pemphigus vulgaris, pemphigus foliaceus
and paraneoplastic pemphigus
L.F. Mentink, M.C.J .M. de J ong, G.J . Kloosterhuis, J . Zuiderveen, M.F. J onkman and
H.H. Pas
pages 635641
Association between the insertion/deletion polymorphism of the angiotensin I-converting enzyme
gene and risk for psoriasis in a Chinese population in Taiwan
Y-C. Chang, W-M. Wu, C-H. Chen, S-H. Lee, H-S. Hong and L-A. Hsu
pages 642645
Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis
K. Kingo, R. Mssner, S. Kks, R. Rtsep, U. Krger, E. Vasar, K. Reich and H. Silm
pages 646652
Early increase in serum levels of the angiogenesis-inhibitor endostatin and of basic fibroblast growth
factor in melanoma patients during disease progression
P. Kurschat, S. Eming, D. Nashan, T. Krieg and C. Mauch
pages 653658
Palmoplantar pustulosis and gluten sensitivity: a study of serum antibodies against gliadin and tissue
transglutaminase, the duodenal mucosa and effects of gluten-free diet
G. Michalsson, G. Kristjnsson, I. Pihl Lundin and E. Hagforsen
pages 659666
Itch Severity Scale: a self-report instrument for the measurement of pruritus severity
C.J . Majeski, J .A. J ohnson, S.N. Davison and G.J . Lauzon
pages 667673
Contact dermatitis and allergy
Double-blind, placebo-controlled study of sublingual immunotherapy in patients with latex-induced
urticaria: a 12-month study
E. Nettis, M.C. Colanardi, A.L. Soccio, M. Marcandrea, L. Pinto, A. Ferrannini, A. Tursi
and A. Vacca
pages 674681
Dermatological surgery and lasers
Application of topical mitomycin C to the base of shave-removed keloid scars to prevent their
recurrence
J .N.R. Bailey, A.E. Waite, W.J . Clayton and M.H.A. Rustin
pages 682686
To freeze or not to freeze: a cost-effectiveness analysis of wart treatment
M.R. Keogh-Brown, R.J . Fordham, K.S. Thomas, M.O. Bachmann, R.C. Holland, A.J .
Avery, S.J . Armstrong, J .R. Chalmers, A. Howe, S. Rodgers, H.C. Williams and I.
Harvey
pages 687692
Epidemiology and health services research
Lifetime prevalence of self-reported atopic diseases in a population-based sample of elderly subjects:
results of the ESTHER study
M. Wolkewitz, D. Rothenbacher, M. Lw, C. Stegmaier, H. Ziegler, M. Radulescu, H.
Brenner and T.L. Diepgen
pages 693697
Early allergen exposure and atopic eczema
J .M. Harris, H.C. Williams, C. White, S. Moffat, P. Mills, A.J . Newman Taylor and P.
Cullinan
pages 698704
Paediatric dermatology
Idiopathic facial aseptic granuloma: a multicentre prospective study of 30 cases
F. Boralevi, C. Laut-Labrze, S. Lepreux, S. Barbarot, J . Mazereeuw-Hautier, C.
Eschard and A. Taeb, on behalf of the Groupe de Recherche Clinique en Dermatologie
Pdiatrique
pages 705708
Subcutaneous fat necrosis of the newborn: a systematic evaluation of risk factors, clinical
manifestations, complications and outcome of 16 children
E. Mah, N. Girszyn, S. Hadj-Rabia, C. Bodemer, D. Hamel-Teillac and Y. De Prost
pages 709715
Photobiology
The relation between sun protection factor and amount of suncreen applied in vivo
A. Faurschou and H.C. Wulf
pages 716719
Therapeutics
Inhibitory or scavenging action of ketoconazole and ciclopiroxolamine against reactive oxygen
species released by primed inflammatory cells
T. Nakashima, E. Sato, Y. Niwano, M. Kohno, W. Muraoka and T. Oda
pages 720727
Pimecrolimus cream 1% for papulopustular rosacea: a randomized vehicle-controlled double-blind
trial
S. Weissenbacher, J . Merkl, B. Hildebrandt, A. Wollenberg, M. Braeutigam, J . Ring and
H. Hofmann
pages 728732
Concise communication
Ear, nose and throat manifestations in pemphigus vulgaris
A. Espaa, S. Fernndez, J . del Olmo, M. Marquina, M. Pretel, D. Ruba and A. Snchez-
Ibarrola
pages 733737
Case reports
Pulmonary carcinoid associated with melanoma: two cases and a review of the literature
R. Rajaratnam, J .R. Marsden, J . Marzouk and I. Hero
pages 738741
Szary syndrome in a patient receiving infliximab for ankylosing spondylitis
J .N. Dauendorffer, J . Rivet,A. Allard and H. Bachelez
pages 742743
Gene corner
A recurrent splice-site mutation in the human hairless gene underlies congenital atrichia in Irish
families
G.M. O'Regan J ., Zurada, A. Martinez-Mir, A.M. Christiano and A.D. Irvine
pages 744747
Correspondence
AL amyloidosis enhances development of amyloid A amyloidosis
J .C.H. van der Hilst, J .W.M. van der Meer, J .P.H. Drenth, A. Simon
pages 748749
Extensive mucinous metaplasia of the vulva arising within Zoon's vulvitis
M.A. Thomson, R.A. Carr, R. Ganesan and F. Humphreys
pages 750752
Scrotal cutaneous chylous reflux
H-Y. Huang, S-L. Hu
pages 752754
A woman with iatrogenic androgenetic alopecia responding to finasteride
J -B. Hong H-C. Chiu J -Y. Chan R-J . Chen S-J . Lin
pages 754755
Immunohistochemical characterization of elastofibroma and exclusion of ABCC6 as a predisposing
gene
M. Naouri, P. Michenet, N. Chassaing and L. Martin
pages 755758
The efficacy of tetracycline antibiotics for treatment of lichen planus: an open-label clinical trial
B.M. Hantash and M.H. Kanzler
pages 758760
Multiple huge cutaneous horns overlying verrucae vulgaris induced by human papillomavirus type
2: a case report
Wang Chen Wang Wei, Lei Yan-J un, Wang J i-Ying, Dong Xiao-Ping, Wang Jian, Sheng
Rui-Hong, Pan Zi-Ang, Zhu Wen-Yuan, You Li-Ping, Peng Hong-Xia and Xu Xin-Ye
pages 760762
Subcutaneous phaeohyphomycosis caused by Exophiala oligosperma in a renal transplant recipient
M.A. Gonzlez-Lpez, R. Salesa, M.C. Gonzlez-Vela, H. Fernndez-Llaca, J .F. Val-
Bernal and J . Cano
pages 762764
Bullous eosinophilic cellulitis associated with ulcerative colitis: effective treatment with sulfasalazine
and glucocorticoids
J . Utikal, W.K. Peitsch, N. Kemmler, N. Booken, R. Hildenbrand, R. Gladisch, S. Goerdt
and M. Goebeler
pages 764766
Hypohidrosis colocalized with Becker's naevus
J .E. Do, Y.J . Kim, H.Y. Kang
pages 766767
Mutation hotspots of SCN9A in primary erythermalgia
L-L. Zhang, Z-M. Lin, Z-H. Ma, Z. Xu, Y-L. Yang and Y. Yang
pages 767769
Cost-effectiveness of treatment of superficial basal cell carcinoma: surgical excision vs. imiquimod
5% cream
F. Vanaclocha, E. Daudn, X. Bada, C. Guilln, J .S. Conejo-Mir, M. Sainz de los
Terreros, L. Hamel and M.A. Llorens for the HEIS Study Group
pages 769771
Comparative efficacy of topical antipsoriatic treatments, systemic treatment and biologics: is severity
assessment beyond Psoriasis Area and Severity Index a necessity?
P.C.M. van de Kerkhof, U. Mrowietz, S. Segaert and K. Kragballe
pages 771772
Ultraviolet B exposure could influence the interpretation of serum S100 levels in patients with
malignant melanoma
J . Vitzthum, H.D. Drr and V. Meineke
pages 772773
Erythema gyratum repens-like eruption in a patient with epidermolysis bullosa acquisita associated
with ulcerative colitis
A. Espaa C. Sitaru M. Pretel L. Aguado and J . J imenez
pages 773775
Blindness due to the IgA variant of epidermolysis bullosa acquisita, and treatment with osteo-odonto-
keratoprosthesis
N.H. Cox, M.A. Bearn, J . Herold, G. Ainsworth and C. Liu
pages 775777
A patient with alopecia, nail dystrophy, palmoplantar hyperkeratosis, keratitis, hearing difficulty
and micrognathia without GJB2 or GJB6 mutations: a new type of hidrotic ectodermal dysplasia?
M. Nakamura and O. Ishikawa
pages 777779
Successful treatment of scalp actinic keratoses with photodynamic therapy using ambient light
R.J . Batchelor, G.I. Stables, M.R. Stringer
pages 779781
Folliculotropic Szary syndrome: a new variant of cutaneous T-cell lymphoma
P. Gerami, J . Guitart
pages 781783
Bortezomib-associated rash: a new recognizable and avoidable side-effect
B. Villarrubia, I. Betlloch, J . Mataix, A. Lucas, C. Botella
pages 784785
Primary cutaneous peripheral T-cell lymphoma, unspecified, that completely regressed after skin
biopsy
V. Madan, N.H. Cox
pages 785786
Do we need a revised public health policy on sun exposure?
P.E. Hutchinson, J .E. Osborne
pages 786788
Do we need a revised public health policy on sun exposure? Response from Brian Diffey
B. Diffey
pages 788788
Allergic contact dermatitis complicating pustular psoriasis in two patients
R.P. Katugampola, T.M. Hughes, C.M. Mills and N.M. Stone
pages 788790
News and Notices
News and Notices
pages 790791
Erratum
Erratum
pages 791791
Original article printed in: British J ournal of Dermatology 156:3 p. 528 doi:
10.1111/j.1365-2133.2006.07617.x
RESEARCH SNI PPETS DOI 10. 1111/j . 1365- 2133. 2007. 07823. x
Association analysis of IL19, IL20 and IL24 genes in palmoplantar
pustulosis
Up to 24% of patients with palmoplantar pustulosis (PPP) concomitantly
have plaque-type psoriasis; however, no common genetic factors have been
identied so far. Kingo et al. have studied the genes encoding the interleukin
(IL)-19 subfamily of cytokines (IL-19, IL-20 and IL-24), the members of
which have recently been discovered as important mediators in the
pathophysiology of psoriasis, as possible genetic risk factors for PPP. They
found that an extended IL19/IL20 haplotype was associated with an increased
susceptibility to PPP while carriers of an extended IL20/IL24 haplotype
appeared to have a smaller risk for PPP. A similar constellation has previously
been established in patients with plaque-type psoriasis compared with
healthy individuals. It seems possible that the IL19 gene cluster represents a
susceptibility region shared by PPP and plaque-type psoriasis, and is a part of
the genetic basis underlying the frequent coexistence of PPP and plaque-type
psoriasis.
Kingo K, Mossner R, Koks S et al. Association analysis of IL19, IL20 and IL24
genes in palmoplantar pustulosis. Br J Dermatol 2007; 156:64652.
Early increase in serum levels of the angiogenesis-inhibitor endostatin and of basic broblast growth factor in melanoma
patients during disease progression
Effective therapeutic options are still not available for advanced-stage melanoma. Early detection of primary tumours and of
limited locoregional metastases is the best way to decrease mortality. A tumour marker indicating early metastatic spread would
be of great value. The melanoma marker S-100 B is frequently elevated in patients with organ metastases, but usually fails to
indicate lymph node metastases. Kurschat et al. show that the angiogenesis-related factors basic broblast growth factor and
endostatin are elevated in a substantial number of patients with stage III disease. Although not specic for melanoma, they might
be valuable in the follow-up of patients with melanoma.
Kurschat P, Eming S, Nashan D et al. Early increase in serum levels of the angiogenesis-inhibitor endostatin and of basic broblast
growth factor in melanoma patients during disease progression. Br J Dermatol 2007; 156:6538.
To freeze or not to freeze: a cost-effectiveness analysis of wart treatment
The cost-effectiveness of treating cutaneous (nongenital) warts is questionable. The
cost-effectiveness of treatments was assessed using a decision analytic Markov model
based on systematic review evidence. Results suggest that salicylic acid (SA) is the most
cost-effective over-the-counter treatment examined in the model and that it is more
cost-effective for general practitioners to prescribe SA than to administer cryotherapy.
Nurse-administered cryotherapy is a potentially cost-effective alternative to general
practitioner-administered cryotherapy, but if rigorous trials verify the effectiveness
estimates of duct tape occlusion therapy, its use as the primary treatment for cutaneous warts could be more cost-effective than
either over-the-counter SA or nurse-administered cryotherapy.
Keogh-Brown MR, Fordham RJ, Thomas KS et al. To freeze or not to freeze: a cost-effectiveness analysis of wart treatment. Br J
Dermatol 2007; 156:68792.
Early allergen exposure and atopic eczema
Harris et al. investigated the role of aeroallergens in causing eczema in a British birth cohort study. They did not nd any linear
associations between early exposure to house dust mite or cat allergen and subsequent risk of eczema, and found a nonsignicant
decrease in eczema risk at the highest levels of allergen at birth. This lack of any clear exposuredisease relationship argues against
allergen exposure as being a major factor causing eczema. Interventions aimed at reducing house dust mite in early infancy could
paradoxically increase the risk of subsequent eczema.
Harris JM, Williams HC, White C et al. Early allergen exposure and atopic eczema. Br J Dermatol 2007; 156:698704.
Duct
OTC CR
OTC SA
GP SA
CR1
CRNurse
COMB
SACR
CR3
CRSA
DN
CR2
0
10
20
30
40
50
60
70
80
90
0 5 10 15 20 25 30 35 40 45
Incremental effectiveness (percentage cured)
I
n
c
r
e
m
e
n
t
a
l
c
o
s
t
(
)
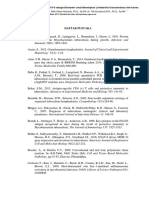
Table 3 Results of haplotype analysis of the IL19, IL20
and IL24 genes
Controls
(n 149)
PPP patients
(n 43) P-value OR (95% CI)
IL19 haplotypes
GACACCG 705 791 0116 158 (089282)
GATGATA 138 62 0057 041 (016105)
CTTGATA 67 58 0766 086 (031236)
IL20 haplotypes
TAA 673 683 0868 104 (062175)
GGG 214 115 0039* 048 (023098)
GAA 77 166 0014* 239 (117486)
TGG 22 25 0894 110 (023528)
IL24 haplotypes
AAAC 485 429 0357 080 (049130)
GGGT 394 487 0125 146 (090236)
GAGT 82 71 0744 085 (0340214)
OR, odds ratio; CIs, condence interval.
The haplotype frequencies (%) and haplotypic ORs with their 95%
CI and P-values in palmoplantar pustulosis (PPP) patients compared
with controls are indicated. Haplotype-phenotype associations were
estimated using an expectation-maximization (EM) algorithm.
*P-value < 005 haplotypic differences compared with the controls.
CUTANEOUS BI OLOGY DOI 10. 1111/j . 1365- 2133. 2006. 07678. x
Expression of matrilysin (matrix metalloproteinase-7)
in primary cutaneous and metastatic melanoma
K. Kawasaki, T. Kawakami, H. Watabe, F. Itoh,* M. Mizoguchi and Y. Soma
Departments of Dermatology and *Internal Medicine, St Marianna University School of Medicine, 2-16-1 Sugao, Miyamae-ku, Kawasaki, Kanagawa
216-8511, Japan
Correspondence
Tamihiro Kawakami.
E-mail: tami@marianna-u.ac.jp
Accepted for publication
18 August 2006
Key words
matrilysin, matrix metalloproteinase-7, melanoma,
metastasis
Conicts of interest
None declared.
Summary
Background Matrilysin (MMP-7), a member of the matrix metalloproteinase (MMP)
family of proteins, is expressed in various types of malignant tumours. There
have been no previous studies of the correlation between matrilysin expression
and melanoma.
Objectives Protein expression of matrilysin was evaluated in human cutaneous mela-
nomas, metastatic melanomas, acquired common melanocytic naevi and Spitz
naevi, and the data were corrected with the clinicopathological factors.
Methods We retrospectively investigated 18 primary melanomas, 15 metastatic
melanomas, 10 common melanocytic naevi and ve Spitz naevi samples at our
clinic using immunohistochemistry (IHC). Both promatrilysin and active matri-
lysin were found in the melanoma tissue extracts by Western immunoblotting.
In situ hybridization demonstrated that melanoma cells selectively express matri-
lysin mRNA.
Results Of the melanoma samples, 29 of 33 (879%) were positive for matrilysin,
including 14 of 18 (778%) primary cutaneous melanomas and 15 of 15
(100%) metastatic melanomas. In contrast, matrilysin was not expressed in com-
mon naevi or Spitz naevi. The matrilysin IHC staining score in primary mela-
nomas was associated with the presence of metastases, tumour thickness and
TNM staging (P 0001, 0025 and 0021, respectively). The 5-year overall sur-
vival was 263% for matrilysin-positive cases and 100% for matrilysin-negative
cases among melanoma specimen.
Conclusions We found matrilysin expression in primary melanomas and in meta-
static melanomas. We further demonstrated that the matrilysin IHC staining score
was associated with invasive depth of primary melanoma lesions and metastases.
Our observations indicate that matrilysin may be associated with melanoma pro-
gression, and may enhance melanoma tumour cell invasion. Therefore, matrilysin
may be potentially valuable as a prognostic indicator to predict the clinical beha-
viour of melanoma.
Tumour cell invasion and metastasis are complex and multi-
step processes, in which tumour cells detach from the primary
tumour, invade surrounding tissues and basement membranes
(BM), intravasate into the lymphatic or blood systems, and
nally adhere and extravasate in distant organs to form a sec-
ondary tumour. The spread of malignant tumours requires the
degradation or breakdown of the extracellular matrix (ECM)
and connective tissue surrounding the tumour cells. Matrix
metalloproteinases (MMPs) degrade all components of the
ECM and the BM, events that are essential in cell motility,
angiogenesis and cancer metastasis. The MMP gene family is
composed of at least 26 different Zn
2+
metalloproteinases and
MMPs are believed to contribute to the complex processes of
invasion and metastasis of malignant tumours. The role of
MMPs in invasion and metastasis in many types of tumour has
been reviewed extensively.
1,2
Studies employing immuno-
histochemistry (IHC) and/or in situ hybridization have demon-
strated that tumour cells and stromal cells express MMPs.
36
Among the MMPs, matrilysin (MMP-7) is the smallest owing
to its lack of COOH-terminal haemopexin-like domain. This
compound exhibits high activities against a wide range of sub-
strates, including components of the BM such as collagen,
laminin and entactin.
7,8
Matrilysin expression has been report-
ed predominantly in deeply invading human gastric and
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619 613
oesophageal cancer cell nests, especially at the invasive front
of carcinomas.
9
Cutaneous melanoma is characterized by its high capacity
for invasion and metastasis. Melanoma is a potentially lethal
melanocytic neoplasm with a propensity for distant metastasis
and may arise de novo or within basal naevi.
10,11
Spitz naevi are
uncommon, benign melanocytic neoplasms that share many
clinical and histological features with melanoma. During mela-
noma progression, different proteolytic enzyme systems,
including the MMP family, play important roles.
12,13
Recent
studies indicate that the balance between MMPs and their tis-
sue inhibitors (TIMPs) may be particularly critical in deter-
mining this process. Hofmann et al.
14
proposed the
involvement of adhesion molecules and of the MMP/TIMP
balance in melanoma progression, based on studies of mela-
noma cells in vitro and in vivo and on expression proles of
human melanocytic lesions. In order to characterize the clin-
ical relevance of matrilysin to cutaneous melanoma, we exam-
ined matrilysin expression at both the protein and mRNA
levels in specimens from common melanocytic naevi, Spitz
naevi, primary melanomas and metastatic melanomas. To our
knowledge, this is the rst report to address questions regard-
ing the involvement of matrilysin in cutaneous melanoma.
Methods
Clinical investigation and tissue samples
Routine histological examination was performed on haematox-
ylin and eosin-stained sections. Special stains, such as S100,
HMB45 and MIB-1, may be useful in the histological diagno-
sis of melanoma. Specimens examined covered major types of
melanocytic proliferation, including acquired common melan-
ocytic naevi (n 10: three compound naevi, three junctional
naevi, two intradermal naevi and two epidermal naevi), Spitz
naevi (n 5), primary cutaneous melanomas of different
tumour thickness (n 18) and metastatic melanomas (n
15). All subjects were Japanese. A summary of the characteris-
tics of the patients in this study is shown in Table 1. Of the
15 metastatic melanomas examined, eight lesions were
obtained from lymph nodes, six were obtained from skin
metastases, and the remaining lesion was collected from the
small intestine. Breslow tumour thickness was measured in
millimetres from the granular layer vertically to the deepest
point of tumour invasion, according to Breslow.
15
Primary
cutaneous melanomas were classied into four clinical sub-
types: acral lentiginous melanoma (ALM); supercial spread-
ing melanoma (SSM); nodular melanoma (NM); lentigo
maligna (LM). Melanoma staging was based on the histo-
pathological TNM classication system.
16
According to Fitz-
patrick skin types, 10 of 18 patients with primary melanoma
were classied as having type IV; four patients had type II,
and the other four patients had type III.
The study protocol was based on the ethical principles of
Good Clinical Practice and was approved by the St Marianna
University School of Medicine Institutional Review Board for
Human Subjects Research (No. 1103).
Immunohistochemistry analysis
IHC staining of tissues was obtained using a monoclonal anti-
matrilysin antibody (F-82) diluted at 1 : 100 (Daiichi Fine
Chemical Ltd, Takaoka, Japan). Serial 4-lm sections from each
specimen were de-waxed using xylene and were then hydrat-
ed using graded ethanol. Before immunostaining, antigen
retrieval was performed by microwave treatment (600 W,
82 C) with 001 mol L
)1
sodium citrate ve times for 5 min
each. After hydration in phosphate-buffered saline (PBS), sec-
tions were incubated with each antibody for 1216 h at 4 C.
These sections were then processed using the avidinbiotin
peroxidase complex (ABC) method. For negative controls, we
used normal mouse immunoglobulin in place of the specic
antibody. The criteria for scoring the stained sections were as
follows: negative ()), < 10% of the whole tumour mass
stained; weakly positive (+ 1), 1025% of the whole tumour
mass stained; moderately positive (+ 2), 2550% of the
whole tumour mass stained; and strongly positive (+ 3),
> 50% of the tumour showed positive. Immunostaining sig-
nals were scored by two independent observers.
Western immunoblotting of matrilysin
The supernatants (60 lg protein per lane) of the tissue homo-
genates were subjected to sodium dodecyl sulphatepolyacryl-
Table 1 Patient characteristics
Melanocytic
naevi
(n 10)
Spitz naevi
(n 5)
Primary
melanoma
(n 18)
Metastatic
melanoma
(n 15)
Sex (M/F) 6 : 4 3 : 2 8 : 10 7 : 8
Mean age (years) 272 95 565 605
Range (years) 149 515 3290 3290
Tumour site
Face and head 2 0 3
Trunk 4 2 5
Lower extremity 2 3 6
Foot and hand 2 0 4
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
614 Matrilysin expression in melanoma, K. Kawasaki et al.
amide gel electrophoresis (125% total acrylamide) under
reducing conditions. Proteins separated in the gels were elect-
rophoretically transferred onto nitrocellulose lters. The lters
were then incubated for approximately 16 h at 23 C with
monoclonal antibodies (10 lg mL
)1
) specic to promatrilysin
(141-7B2; Oncogene Research Products, Boston, MA, U.S.A.)
or active matrilysin (176-5F12; Oncogene Research Products)
after blocking nonspecic binding with 3% bovine serum
albumin. The blots were developed using ECL Western blot-
ting detection reagents (Amersham Pharmacia Biotech,
Amersham, Bucks, U.K.). Relative levels of matrilysin were
corrected with b-actin as the internal standard.
In situ hybridization
A 357-bp DNA fragment corresponding to the nucleotide
positions 104460 of human matrilysin cDNA was subcloned
into pBlueScript SK()) vector (Stratagene Japan, Tokyo, Japan)
and was used for generation of sense or antisense RNA probes.
For in situ hybridization, parafn sections were mounted on
slides coated with polylysine under RNAse-free conditions.
After treatment with xylene and rehydration through an
ethanol series and PBS, the specimens were xed with 4%
paraformaldehyde in PBS for 15 min. We carried out hybrid-
ization with digoxigenin-labelled RNA probes at 58 C for
16 h. The bound label was detected using NBT-BCIP (Roche,
Mannheim, Germany), an alkaline phosphatase colour sub-
strate, and tissue slides were stained with Kernechtrot stain
solution.
Statistical analysis
Fishers exact test (StatView 50 for Windows, SAS Institute
Inc., Cary, NC, U.S.A.) was applied to determine the signi-
cance of correlation; the level of signicance was set at
P < 005 in all cases. SPSS 100 software (SPSS Inc., Chicago,
IL, U.S.A.) was used to perform the Students t-test to analyse
the relationship between the matrilysin IHC staining score and
clinical parameters including age, sex, tumour subtype and
metastasis. The correlation between the matrilysin IHC stain-
ing score in primary melanoma and variation of Breslow
tumour thickness or TNM staging levels was assessed by
Spearmans rank correlation test. Survival analyses were per-
formed using the KaplanMeier method. Comparison of the
survival between the matrilysin-positive staining group and
the negative group in melanoma was performed using the
log-rank test.
Results
Matrilysin expression in melanoma by
immunohistochemistry
We performed IHC on tissue biopsies ranging from benign
tumours to metastatic melanomas. As shown in Figure 1(a,b),
matrilysin staining was absent in common melanocytic naevi
and in Spitz naevi. We did not nd any signicant distinction
between nondysplastic and dysplastic naevi on matrilysin
IHC staining. Matrilysin in primary cutaneous melanomas is
expressed abundantly in melanoma cells compared with
benign common melanocytic naevi (Fig. 1c), and the immu-
nostaining is distributed throughout the cytoplasm. Matrilysin
was also strongly expressed in metastatic melanoma lesions
(Fig. 1e). Matrilysin was expressed not only in the melanoma
cells but also in the surrounding stroma. Matrilysin was
expressed in 879% (29/33) of melanoma examined, includ-
ing 14 of 18 (778%) primary cutaneous melanomas and 15
of 15 (100%) metastatic melanomas. Ten (303%) of the 33
melanoma specimens were strongly positive (+ 3), 11
(333%) stained moderately (+ 2), and eight (242%) stained
weakly (+ 1). Negative controls are shown in Figure 1(d,f).
Detection of matrilysin by Western immunoblotting
Tissue from a 60-year-old male with a 2-year history of
melanoma (Breslow thickness 363 mm: T3bN2M0; tumour
subtype NM) located on the left lower extremities and
lymph nodal metastases was used for Western immunoblot
assessment. We had enough fresh material of melanoma
and nonmelanoma tissue samples available for protein
extraction from them. After the operations, the tissue sam-
ples including melanoma, metastases and nonmelanoma tis-
sue were embedded without xation in OCT compound
(Sakura Finetechnical Co. Ltd, Tokyo, Japan) and snap-
frozen. Frozen sections were made using a cryostat and
melanoma nests and normal tissue were carefully separated
by a needle under a light microscope. The scraped tissues
were homogenized in 50 mmol L
)1
Tris-HCl buffer, pH
75, containing 015 mol L
)1
NaCl
2
, 10 mmol L
)1
M CaCl
2
and 005% Brij35 on ice. The supernatants were prepared
by centrifugation. Immunoblot analysis demonstrated a def-
inite band corresponding to promatrilysin of 28 kDa in
melanoma tissue extracts (Fig. 2a). Active matrilysin of
18 kDa was also identied in the same samples (Fig. 2b).
In accordance with the immunohistochemical ndings, nor-
mal tissue showed negligible or no protein band for
promatrilysin and active matrilysin. Western immunoblotting
in skin metastatic tissue samples from a colon carcinoma
was regarded as a positive control (Fig. 2a,b).
Expression of matrilysin mRNA in primary melanoma
and metastatic melanoma
To identify the cells expressing matrilysin mRNA, in situ
hybridization was performed in ve primary melanoma cases
and three melastatic melanoma cases. In 80% of primary mela-
nomas (four of ve cases), signals were detected in melanoma
cells (Fig. 3a). The distribution pattern of the matrilysin trans-
cript in all melastastic lesions was similar to that observed in
primary lesions (Fig. 3c). The same sample was hybridized
with the sense probe of matrilysin as a negative control
(Fig. 3b,d).
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
Matrilysin expression in melanoma, K. Kawasaki et al. 615
Correlation between matrilysin immunohistochemistry
expression and other clinical features among primary
melanoma cases
Table 2 lists the clinical features of primary melanoma patients
with matrilysin-positive or matrilysin-negative IHC staining.
We found matrilysin-positive cases had a variety of clinical
subtypes. In contrast, all cases of matrilysin-negative cases
were of the ALM subtype except for one case, which had an
in situ subtype. However, no correlation was observed between
matrilysin staining and other clinical factors, including sex
and mean age at onset.
(a) (b)
(c) (d)
(e) (f)
Fig 1. Stain intensity of matrilysin in various melanocytic lesions. Immunohistochemistry (IHC) was performed using the avidinbiotin
peroxidase complex method. Matrilysin expression was not detected in benign melanocytic naevi, compound naevi (a) or Spitz naevi (b).
IHC showed abundant matrilysin expression in primary melanoma tissues (c). Matrilysin expression was detected in melanoma metastatic lesions
(e). No specimens were positively stained in melanoma tissues when reacted with nonimmune mouse IgG (d, f). Original magnications:
a,b, 100; c,d, 50; e,f, 50.
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
616 Matrilysin expression in melanoma, K. Kawasaki et al.
Correlation of matrilysin immunohistochemistry staining
scores and disease severity
In primary melanoma specimens, cases with metastases
showed a signicantly higher matrilysin IHC staining score
compared with those whose tumours had not metastasized
(23 vs. 08; P 0001). There was a signicant positive
correlation between the matrilysin staining score and Bre-
slow tumour thickness (Spearman rs 054, P 0025;
Fig. 4a). Further, signicant differences in matrilysin expres-
sion were found between melanomas that had metastasized
and those that had not. A similar correlation was also seen
between the degree of matrilysin staining score and TNM
staging (Spearman rs 056, P 0021; Fig. 4b). Survival
time was analysed in 10 patients whose melanoma tissue
was positive for matrilysin IHC staining and four patients
whose melanoma tissue was negative for matrilysin IHC
staining. The positive patients had a signicantly shortened
survival time compared with the negative patients (P
0041; Fig. 5). The 5-year overall survival rates of the matri-
lysin-positive and the matrilysin-negative patient groups were
263% and 100%, respectively.
(a)
(b)
Fig 2. Immunoblotting analysis of promatrilysin and active matrilysin
protein. The samples of primary melanoma, metastatic melanoma and
nonmelanoma skin tissue in a melanoma patient were shown. In
positive control, skin metastatic tissue extracts from a colon carcinoma
was noted (a,b). Promatrilysin (a) protein expression was highest in
metastatic melanoma tissue extracts. Primary melanoma tissue extracts
were weakly expressed compared with control sample. Note the
increased active matrilysin (b) expression of both primary melanoma
and metastatic melanoma tissue extracts compared with the
nonmelanoma normal tissue extracts.
(a) (b)
(c) (d)
Fig 3. In situ hybridization analysis of matrilysin mRNA in melanoma tissues. Signals for matrilysin mRNA in primary melanoma cells with the
antisense probe were detectable by the blue staining of the nuclei (a). The sense (control) probe did not show a detectable signal (b). In the
metastatic melanoma lesion, the signals were positive (c). Very faint signals in the sense (control) probe were noted (d). Original magnications:
ad, 200.
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
Matrilysin expression in melanoma, K. Kawasaki et al. 617
Discussion
The results of IHC for matrilysin showed that primary and
metastatic melanoma specimens express moderate to high
levels of matrilysin at the protein level, whereas acquired
common melanocytic naevi and Spitz naevi do not. Our data
demonstrate that matrilysin is expressed and produced pre-
dominantly by melanoma tissues. We found that > 80% of
the primary melanoma lesions are positive for matrilysin while
all the analysed metastatic lesions are positive. In situ hybridiza-
tion revealed that only melanoma cells were labelled with the
antisense RNA (four of ve primary melanoma cases and three
of three metastatic melanoma cases) and were the major pro-
ducers of matrilysin. During cancer progression, cancer cells
interact with each other and with the ECM. Because of its
strong degradative activity on the ECM and its localization on
cancer cells, matrilysin can be an important determinant of
tumour progression. Matrilysin expression has been reported
in head, neck and lung carcinomas,
17
in breast carcinomas,
4
in stomach and in colon carcinomas
18,19
as well as in prostate
carcinomas.
20
These ndings indicate that the high expression
of matrilysin on melanoma cells may result in the degradation
of the ECM, and subsequently play an important role in
tumour invasion or metastasis. Matrilysin is secreted in a pro-
enzyme and activated extracellularly; the activation is a pre-
requisite to its functioning in the local tissues. We noted the
active matrilysin protein in both primary and metastatic mela-
noma tissue by Western blotting. There is increasing evidence
that matrilysin may have various potential functions in mela-
noma progression. One possible mechanism in melanoma
invasion is that matrilysin activation may be involved in an
early step in the formation of secondary metastatic lesions, so
its role in tumour dissemination would probably be due to its
ability to mediate cell migration.
We investigated the relationship between matrilysin expres-
sion by IHC in patients with melanoma and these clinical
features. In matrilysin-positive cases of the primary lesion,
matrilysin was found to be expressed in various clinical
Table 2 Comparison of clinical features in matrilysin-positive and
matrilysin-negative primary melanoma cases (using immunohisto-
chemistry staining)
Matrilysin positive
(n 14)
Matrilysin negative
(n 4)
Sex (M/F) 7 : 7 2 : 2
Mean age (years) 575 530
Range (years) 3290 3474
Tumour site
Face and head 3 0
Trunk 5 0
Lower extremity 5 1
Foot and hand 1 3
Tumour subtype
ALM 2 4
SSM 4 0
NM 6 0
LM 2 0
ALM, acral lentiginous melanoma; SSM, supercial spreading
melanoma; NM, nodular melanoma; LM, lentigo maligna.
(a)
(b)
Fig 4. Correlation of matrilysin immunohistochemistry (IHC) staining
score in primary melanomas with tumour thickness or TNM staging.
(a) Positive correlation between Breslow tumour thickness (mm) and
matrilysin IHC staining score in primary melanomas. Breslow tumour
thickness is shown on the ordinate, and staining scores are shown on
the abscissa (Spearman rs 054, P 0025). (b) Positive correlation
between TNM staging and matrilysin IHC staining score in primary
melanomas. TNM staging is shown on the ordinate and staining
scores are shown on the abscissa (Spearman rs 056, P 0021).
Fig 5. KaplanMeier curve for overall survival of patients with
melanoma. The 5-year survival was 100% and 263% for matrilysin
negative and positive patients, respectively. The difference between
the two groups was statistically signicant (P 0041).
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
618 Matrilysin expression in melanoma, K. Kawasaki et al.
melanoma subtypes. The nding suggests that the melanoma
clinical subtype does not correlate with matrilysin IHC stain-
ing. The matrilysin IHC staining score was related to Breslow
tumour thickness and TNM staging of melanoma. Over-
production of matrilysin in human melanoma would appear
to increase with the depth of tumour invasion and metastasis.
The 5-year survival curves show a 100% survival for all matri-
lysin-negative patients, compared with the 263% survival rate
for the matrilysin-positive patients. These results indicate that
elevated matrilysin expression in melanomas enhances tumour
cell growth and metastasis and reduces survival rate. The stain-
ing score of matrilysin expression in primary cutaneous
melanomas may be a reliable prognostic marker. Identifying
matrilysin expression may provide new insights into the
design of novel therapeutic strategies for melanoma. Detection
of matrilysin would offer the opportunity for a novel thera-
peutic approach, i.e. matrilysin could be a potential target for
therapeutic intervention. Analysis of matrilysin expression in
melanoma tissues could provide basic data for such novel
therapeutic strategies.
Acknowledgments
This work was supported by grants from the Scientic
Research Fund of the Ministry of Education, Science, Sports
and Culture, Japan (Grant-in Aid for Scientic Research, No.
16591121 and 18591261).
References
1 Coussens LM, Werb Z. Matrix metalloproteinases and the develop-
ment of cancer. Chem Biol 1996; 3:895904.
2 Westermarck J, Kahari VM. Regulation of matrix metalloproteinase
expression in tumor invasion. FASEB J 1999; 13:78192.
3 Okada A, Bellocq JP, Rouyer N et al. Membrane-type matrix metallo-
proteinase (MT-MMP) gene is expressed in stromal cells of human
colon, breast, and head and neck carcinomas. Proc Natl Acad Sci USA
1995; 92:27304.
4 Heppner KJ, Matrisian LM, Jensen RA, Rodgers WH. Expression of
most matrix metalloproteinase family members in breast cancer
represents a tumor-induced host response. Am J Pathol 1996;
149:27382.
5 Nielsen BS, Timshel S, Kjeldsen L et al. 92 kDa type IV collagenase
(MMP-9) is expressed in neutrophils and macrophages but not in
malignant epithelial cells in human colon cancer. Int J Cancer 1996;
65:5762.
6 Ueno H, Nakamura H, Inoue M et al. Expression and tissue
localization of membrane-types 1, 2, and 3 matrix metallo-
proteinases in human invasive breast carcinomas. Cancer Res 1997;
57:205560.
7 Sires UI, Grifn GL, Broekelmann TJ et al. Degradation of entactin
by matrix metalloproteinases. Susceptibility to matrilysin and iden-
tication of cleavage sites. J Biol Chem 1993; 268:206974.
8 Imai K, Yokohama Y, Nakanishi I et al. Matrix metalloproteinase 7
(matrilysin) from human rectal carcinoma cells. Activation of the
precursor, interaction with other matrix metalloproteinases and
enzymic properties. J Biol Chem 1995; 270:66917.
9 Adachi Y, Itoh F, Yamamoto H et al. Matrix metalloproteinase
matrilysin (MMP-7) participates in the progression of human gas-
tric and esophageal cancers. Int J Oncol 1998; 13:10315.
10 Sauder DN. The etiology of malignant melanoma. J Cutan Med Surg
1999; 3:287.
11 Rigel DS, Carucci JA. Malignant melanoma: prevention, early detec-
tion, and treatment in the 21st century. CA Cancer J Clin 2000;
50:21536.
12 Vaisanen A, Kallioinen M, Taskinen PJ, Turpeenniemi-Hujanen T.
Prognostic value of MMP-2 immunoreactive protein (72 kD type IV
collagenase) in primary skin melanoma. J Pathol 1998; 186:518.
13 Airola K, Karonen T, Vaalamo M et al. Expression of collagenas-
es-1 and -3 and their inhibitors TIMP-1 and -3 correlates with
the level of invasion in malignant melanomas. Br J Cancer 1999;
80:73343.
14 Hofmann UB, Westphal JR, Van Muijen GN, Ruiter DJ. Matrix
metalloproteinases in human melanoma. J Invest Dermatol 2000;
115:33744.
15 Breslow A. Thickness, cross-sectional areas and depth of invasion in
the prognosis of cutaneous melanoma. Ann Surg 1970; 172:9028.
16 Kung JX, Ackerman AB. Staging of melanoma: a critique of the
most recent (2002) system proposed by the American Joint Com-
mittee on Cancer. Am J Dermatopathol 2005; 27:1657.
17 Muller D, Breathnach R, Engelmann A et al. Expression of collage-
nase-related metalloproteinase genes in human lung or head and
neck tumours. Int J Cancer 1991; 48:5506.
18 McDonnell S, Navre M, Coffey RJ Jr, Matrisian LM. Expression and
localization of the matrix metalloproteinase pump-1 (MMP-7) in
human gastric and colon carcinomas. Mol Carcinog 1991; 4:52733.
19 Yamashita K, Azumano I, Mai M, Okada Y. Expression and tissue
localization of matrix metalloproteinase 7 (matrilysin) in human
gastric carcinomas. Implications for vessel invasion and metastasis.
Int J Cancer 1998; 79:18794.
20 Knox JD, Wolf C, McDaniel K et al. Matrilysin expression in human
prostate carcinoma. Mol Carcinog 1996; 15:5763.
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp613619
Matrilysin expression in melanoma, K. Kawasaki et al. 619
CUTANEOUS BI OLOGY DOI 10. 1111/j . 1365- 2133. 2006. 07706. x
The distribution of melanin in skin determined in vivo
P.J. Matts, P.J. Dykes* and R. Marks*
Procter & Gamble, Rusham Park Technical Centre, Egham, Surrey TW20 9NW, U.K.
*Cutest Systems Ltd, 214 Whitchurch Rd, Cardiff CF14 3ND, U.K.
Correspondence
P.J. Matts.
E-mail: matts.pj@pg.com
Accepted for publication
25 July 2006
Key words
chromophore mapping, eumelanin, haemoglobin
Conicts of interest
P.J.M. is employed by Procter & Gamble.
Summary
Background There continues to be a need for objective, noninvasive methods to
measure melanin concentration in vivo in human skin, independent of the con-
founding chromophore, haemoglobin. Existing methods are limited by a lack of
specicity and inability to resolve the spatial distribution of these chromophores.
Objectives To validate and calibrate the measurement of eumelanin in vivo using
SIAscopic
TM
techniques, relating this with histologically and analytically
determined eumelanin concentrations in nonsun-exposed skin from subjects of
Fitzpatrick skin types IVI.
Methods Observations were made in ve subjects from each of the Fitzpatrick skin
types IVI using chromophore mapping by contact and noncontact SIAscopy and
other noninvasive spectrophotometric means. Measurements were performed on
the inner aspect of both upper arms. Subsequently two 4 mm punch biopsies
were taken from the inner upper arm, one per arm after injection of local anaes-
thesia. One biopsy was xed in formalin and processed for histology; specically,
sections were stained for melanin using a silver staining technique and the
amount of melanin was graded microscopically. The other biopsy was subjected
to an analytical assay to yield precise quantitative measures of melanin. The cor-
relation between the different methods of melanin measurement was determined.
Results Clear, signicant correlations were obtained between contact and noncontact
SIAscope-derived eumelanin values and actual eumelanin tissue content (deter-
mined both histologically and analytically), across the full range of Fitzpatrick skin
types. There was no correlation between SIAscope-derived eumelanin and haemo-
globin values, indicating efcient separation of the two chromophores.
Conclusions New contact and noncontact chromophore SIAscopic mapping tech-
niques provide robust, rapid noninvasive measures of the concentration and spa-
tial distribution of eumelanin in vivo, independent of haemoglobin, which
correspond to true tissue values for this chromophore.
Human skin coloration is dependent almost exclusively on the
concentration and spatial distribution of the chromophores
melanin and haemoglobin, where melanin plays the dominant
role in driving constitutive coloration.
14
Melanin is synthe-
sized in membrane-bound organelles (melanosomes) within
specialized cells (melanocytes) that supply these packets of
pigment via dendritic processes to surrounding epidermal ker-
atinocytes. Melanin is synthesized as two chemically distinct
types, namely a brown or black pigment eumelanin and a
yellow or red pigment phaeomelanin. Both these complex
heteropolymers derive from dopaquinone (an oxidation prod-
uct of tyrosine), although eumelanin consists of 5,6-
dihydroxyindole and 5,6-dihydroxyindole-2-carboxylic acid
units, whereas phaeomelanin consists primarily of sulphur-
rich benzothiazine derivatives. Of these two pigments, eumel-
anin is the dominant chromophore both in terms of epidermal
fraction volume and perceived colour, phaeomelanin provi-
ding subtle nuances of skin hue.
1
As eumelanin plays such a fundamental role, not only in
skin appearance but also as the primary constitutive and indu-
cible photoprotective molecule within human skin, there is
considerable enduring interest in, and need for, methods to
measure this chromophore in vivo. The Fitzpatrick skin typing
system
5
is wrongly held by many to represent a subjective
scale of pigmentation intensity it was, of course, never
intended as this and only reects this attribute by inference.
Other attempts to assess skin pigmentation subjectively by the
human eye are almost always confounded by the presence
of haemoglobin. In simple terms, while the human eye
has superb contrast sensitivity
6
(down to only 2% of full
2007 The Authors
620 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
brightness) and can distinguish adjacent browns and reds with
ease, it becomes virtually impossible to separate visually and/or
communicate reliably the relative contributions of melanin
and haemoglobin when they overlay one another, as is the
case both in young or photoprotected skin (very homogen-
eous distribution of each chromophore) and older photo-
damaged skin (e.g. colocation of telangiectasia and lentigos or
diffuse hyperpigmentation). Visual assessment, therefore, is at
best semiquantitative and certainly not linear.
Objective approaches to determining skin colour in vivo cen-
tre around spectrophotometric or colorimetric approaches and
the use of derived colour coordinates such as L*a*b*, and var-
ious digital imaging and image analysis techniques, reviewed
in full by Pierard.
7
While these measures certainly bring
objectivity to the measurement of skin colour, they still are
not able to separate the individual contributions of the
chromophores responsible for either the measured, integrated
remittance spectrum or the nal photographic image (no mat-
ter how high a quality it may be). Consequently, we have
seen the development of the Melanin Index and Erythema
Index (MI and EI, respectively), to try and provide a linear
interval data scale for these chromophores.
4,711
Instruments
that derive MI and EI [for example, the Mexameter
TM
(Cour-
age & Khazaka GmbH, Cologne, Germany), the DermaSpectro-
meter
TM
(Cortex Technology, Hadsund, Denmark) and the
Erythema/Melanin Meter
TM
(DiaStron Ltd, Andover, U.K.)]
utilize the same basic approach, taking the log of ratios of
reectance within two or three selected wavebands in the vis-
ible and infrared. These approaches represent a signicant step
forward in the quantication of the chromophores responsible
for skin colour, but are limited by (i) their limited measure-
ment area (a maximum of approximately 10 mm diameter),
(ii) their integration over the measured area, with no resolu-
tion of spatial distribution, (iii) their direct contact with the
skin surface (which can lead to artefacts such as blanching
through excessive applied probe pressure) and (iv) the inabil-
ity of the log-ratio method completely to separate contribu-
tions from the two chromophores (see below).
A new measurement capability, SIAscopy (spectrophotomet-
ric intracutaneous analysis),
1215
developed by Cotton and
Claridge
12
and then Astron Clinica (Cambridge, U.K.), oper-
ates on the principle of chromophore mapping, that is, the
in vivo measurement of the concentration and distribution of
eumelanin, oxyhaemoglobin and dermal collagen, to produce
mutually exclusive greyscale concentration maps of these chro-
mophores. The SIAscope (Astron Clinica) is now a commer-
cially available instrument and, while it has been shown to
have excellent sensitivity and specicity in the early identica-
tion of malignant melanoma, the principle of chromophore
mapping that it employs can be readily applied to normal,
healthy skin.
1215
The technique is based upon a unique com-
bination of dermatoscopy, contact remittance spectrophoto-
metry and hyperspectral imaging. In short, the SIAscope is
able to obtain a high resolution composite white-light image
of the skin over a dened area and provides four additional,
mutually exclusive chromophore maps that display the con-
centration of epidermal melanin and haemoglobin, collagen
and melanin in the papillary dermis, pixel by pixel. The der-
mal melanin endpoint is the key diagnostic criterion used in
the diagnosis of melanoma, although this is not of concern
with regards to normal skin.
These images (corresponding to a 12 mm diameter circular
eld of view) now represent 8-bit 1024 1024 greyscale
maps of chromophore concentration in PNG format image
les. An example of these chromophore maps, obtained using
a SIAscope II instrument, can be seen in Figure 1.
The contact SIAscope comprises a hand-held scanner with
a at glass-fronted probe, placed in contact with the skin
using light, but rm, pressure (to avoid blanching). Further
research by Astron Clinica has yielded noncontact SIAscopy
TM
(NCS) that overcomes the limitations of a skin contact probe.
By necessity, this approach needs to be insensitive to local
geometry and illumination intensity, in other words, the
unavoidable artefacts of measuring 3D objects, rather than
at surfaces.
NCS is implemented
16
using an essentially conventional
(although nely calibrated) digital camera and lighting system
and may be used to acquire large-eld eumelanin and oxyhae-
moglobin chromophore maps. In deploying NCS, the camera
is treated not so much as an imaging device, but more as a
three-waveband spectrometer, making use of the RGB Bayer
lter mosaic over the charge-coupled device (CCD). The spec-
tral power distribution of the light source and the raw
response of the CCD are determined accurately over the visible
range (400700 nm) and are supplied as calibration data to
the NCS algorithms, based on the SIA mathematical model of
light transport within skin. In short, for every pixel of the ori-
ginal RAW image, NCS calculations are performed to yield
exclusive concentrations of eumelanin and oxyhaemoglobin.
When recombined as an array, a parametric greyscale concen-
tration map is produced, directly analogous to those calculated
(a) (b)
(c) (d)
Fig 1. Example of SIAscope
TM
II chromophore maps taken from
inner upper arm skin of subject 1 (type I skin; 12 mm diameter).
(a) Composite white light image, (b) oxyhaemoglobin concentration
map, (c) eumelanin concentration map, (d) collagen concentration map.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
Distribution of melanin in skin, P.J. Matts et al. 621
using the contact technique. It should be noted that a fully
cross-polarized lighting system is needed, to eliminate specular
reection (that, by nature, contains no subsurface informa-
tion). An example of the NCS technique applied to a whole
face can be seen in Figure 2.
While both the contact and noncontact chromophore map-
ping approaches described above yield maps of eumelanin
corresponding to a theoretical linear concentration scale, we
wanted to validate and calibrate these approaches in compar-
ison with other objective techniques, determined by histologi-
cal and analytical means. The methods used and results from
this work are described below.
Materials and methods
Ethical considerations
The study was designed to comply with the Guidelines for
Medical Experiments in nonpatient human volunteers, initially
published in the U.K. by the Association of the British Phar-
maceutical Industry in March 1988 and further amended in
May 1990. Ethical approval was obtained from the South East
Wales Local Research Ethics Committee, Cardiff. The study
complied with the current revision of the World Medical
Associations Declaration of Helsinki (2000) concerning bio-
medical research involving human subjects.
Subjects
Thirty healthy nonpatient volunteer subjects aged 18 years or
over who had given their witnessed, informed consent were
recruited for the study. The study included 18 female and 12
male subjects. Subjects were recruited such that ve subjects
fullled one of each of the six categories given in the
Fitzpatrick skin classication (Table 1),
5
yielding the total 30
subjects.
Measurement and biopsy sites
Measurements and biopsies were all taken from a 5 5 cm
area delineated (by indelible marker) on skin within the cen-
tre of the inner aspect of each upper arm. This anatomical site
was chosen because it should receive an extremely low
lifetime dose of erythemal ultraviolet radiation (UVR), thus
helping to ensure a minimum of chronic photodamage
and, consequently, a homogeneous, normal distribution of
eumelanin.
Contact chromophore mapping
A SIAscope II commercial instrument was used to obtain con-
tact eumelanin maps from within the measurement sites. A
small drop of 20% (v/v) ethanol in water solution was placed
on to the at glass window at the front of the probe, before it
was placed with gentle pressure (to avoid blanching) on to
the skin in the centre of each 5 5 cm site (the ethanol in
water acts as a matching uid, eliminating optical aberration
due to the refractive index of air). The acquisition time for
the measurement was approximately 6 s, during which time
the operator held the probe steady to avoid blurring of the
nal image set. Once the measurement was complete, the SIA-
scope II laptop computer calculated and displayed the respect-
ive chromophore maps, allowing immediate, real-time quality
control over the images obtained. Each map represented a cir-
cular area of skin, 12 mm in diameter.
Eumelanin maps were saved as 8-bit 1024 1024 greyscale
maps in PNG image le format, giving 256 possible concen-
trations of eumelanin and oxyhaemoglobin [where 0 (darkest
greyscale) highest chromophore concentration and 256
(lightest greyscale) lowest chromophore concentration].
These concentration maps are, therefore, readily amenable to
sophisticated image analysis techniques for calculation of a
variety of relevant endpoints. In this case, custom algorithms
written within image analysis software [Optimas
TM
6.5 (Media
Cybernetics LP, Silver Spring, MD, U.S.A.)] batch processed
regions of interest that specied the entire captured eld of
the eumelanin map, to yield a mean greyscale value corres-
ponding to the theoretical mean epidermal eumelanin concen-
tration for that area.
Noncontact chromophore mapping
A Fuji S2 Pro 62 megapixel single lens reex camera
equipped with a Nikon AF Micro Nikkor 105 mm 1 : 28 lens
was used to capture images of each inner upper arm, saved in
both Fuji RAW and uncompressed TIFF format at a resolution
of 3277 2226 pixels and 72 d.p.i. Lighting was provided by
(a) (b) (c)
Fig 2. Example of full-face noncontact SIAscope
TM
chromophore
maps (female subject aged 35 years). (a) Original cross-polarized
white-light digital photograph, (b) eumelanin concentration map,
(c) oxyhaemoglobin concentration map.
Table 1 Fitzpatrick skin type classication
Skin type Appearance Tanning ability
I Very white or freckled Always burn
II White Usually burn
III White to olive Sometimes burn
IV Brown Rarely burn
V Dark brown Very rarely burn
VI Black Never burn
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
622 Distribution of melanin in skin, P.J. Matts et al.
a Sigma EF-500 DG Super ash source, operating in manual
mode. Full cross-polarization was achieved by xing a shaped
polarizing sheet over both the camera lens and the ash aper-
ture (orthogonally opposed to one another). All optical com-
ponents within this imaging system, i.e. the CCD of the
camera, the ash source and the polarizing lter had been pre-
viously calibrated by Astron Clinica to allow construction of
noncontact eumelanin and oxyhaemoglobin chromophore
concentration maps.
Custom SIA
TM
algorithms batch processed the resulting
RAW les to produce eumelanin and oxyhaemoglobin grey-
scale concentration maps analogous to those derived from
contact chromophore mapping. Using image analysis software
(Optimas
TM
6.5), a region of interest (ROI) was selected to
encompass the entire 5 5 cm area in each chromophore
map. Custom algorithms then batch processed these ROIs to
yield mean greyscale values corresponding to theoretical mean
epidermal eumelanin concentration for those areas.
Reectance spectrophotometry
An unmodied commercial hand-held multiple angle reect-
ance spectrophotometer (X-Rite
TM
MA68II, Elcometer Instru-
ments Ltd, Manchester, U.K.) was used to obtain remittance
spectra across the visible waveband (400700 nm with a
10 nm spectral interval; the instrument was used with 10
s
standard observer and D
65
illuminant) from within the cen-
tre of each 5 5 cm skin site (12 mm diameter circular
sampling port). The instrument was calibrated before each
measurement session using a dark-zero and white ceramic
calibration standard. In use, it was placed on the skin surface
with gentle pressure (to avoid blanching) and then held still
during the 2 s acquisition time. Triplicate measures were
obtained from each site. Data were exported as spectral per-
centage reection values to a spreadsheet format for subse-
quent analysis.
Mexameter
TM
measurements
An unmodied Mexameter
TM
MX18 (Courage & Khazaka)
commercial instrument was used to obtain a noninvasive
index of skin melanin content (MI) and an erythema index
(EI). The instrument calibration was checked before each
measurement session to ensure it was within the manufac-
turers limits. In use, it was placed gently on to the skin
surface (to avoid blanching) and held still while the measure-
ment was obtained (< 1 s; 5 mm diameter circular sampling
port). Triplicate measures were obtained from each site and
numerical MI and EI data recorded as hard copy for sub-
sequent entry in to a spreadsheet format for analysis.
Skin biopsy
Skin samples were taken after the noninvasive measures had
been performed. The skin was rst anaesthetized using an
intracutaneous injection of 1% lignocaine and a disposable
4 mm diameter trephine (Steifel Laboratories (UK) Ltd, High
Wycombe, U.K.) within the centre of each 5 5 cm skin
site. For each subject, one biopsy was placed immediately
into 10% buffered formalin for subsequent histological pro-
cessing and the other was placed into a sealed sample tube
and placed immediately on dry ice for subsequent analytical
work-up.
Melanin determination by microscopic examination
of histological samples
The skin biopsies were xed in 10% buffered formalin, dehy-
drated in graded alcohols and embedded in parafn wax. They
were then sectioned on a microtome at 5 lm and the sections
stained (Von Kossa staining protocol). After mounting and
drying, the sections were examined using an Olympus binocu-
lar microscope in a standardized manner using a 20 objec-
tive lens. The sections were scored blind using a continuous
visual analogue scale electronic meter (Vasmeter
TM
, Innova-
derm Recherches Inc., Montreal, QC, Canada) where a score
of 0 signied no pigment and a score of 10 the heaviest pig-
ment deposition possible. Examples of the degree of pigmen-
tation observed are given in Figure 3. To obtain the scores,
the microscope slide was placed with the coded label on the
right side of the microscope stage and the rst and third sec-
tions were assessed. Three adjoining elds in each section
were scored and a mean value of the six elds used as the
score for that specimen.
Melanin determination by analytical assay
Punch biopsies reserved for this analysis were rst weighed,
frozen ()70 C) and then lyophilized, before transport to the
laboratories of Professor Shosuke Ito and Dr Kazu Wakamatsu,
Fujita Health University, School of Health Sciences, Toyoake,
Aichi, Japan. Each biopsy was subjected to the microanalytical
techniques developed by these researchers, based on the
formation of pyrrole-2,3,5-tricarboxylic acid (PTCA) by
permanganate oxidation of eumelanin and of 4-amino-3-
hydroxyphenylalanine (4-AHP) by hydriodic acid reductive
hydrolysis of phaeomelanin, respectively.
17
These specic
degradation products were analysed quantitatively by high
performance liquid chromatography (with UVR detection for
PTCA and electrochemical detection for 4-AHP). For this, 1 ng
PTCA approximated to 160 ng eumelanin and 1 ng 4-AHP
approximated to 9 ng phaeomelanin. These assays, thus,
yielded semiquantitative data expressed as ng mg
)1
wet tissue
of melanin type.
Statistical analysis
To analyse the relationship between mean greyscale data
derived from both contact and noncontact melanin concentra-
tion maps and those from other endpoints, simple regression
analyses were performed to yield the correlation coefcient r
2
and a P value for the slope of the correlation. The mean
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
Distribution of melanin in skin, P.J. Matts et al. 623
greyscale over the ROI in both contact and noncontact eumel-
anin maps was chosen as the summary metric because analysis
of the distribution of greyscale values clearly showed a normal
distribution of greyscale for all eumelanin maps (examination
of greyscale frequency histograms for each map revealed a
symmetrical distribution around both mean and median val-
ues, conrmed by associated skewness values). This conrmed
the appropriateness of choice of a nonsun-exposed site such as
the inner upper arm for this study. Simple regression analysis
was chosen because, according to the rst principles of the
SIA method,
13,15
melanin and haemoglobin chromophore tis-
sue concentration should, in theory, be linearly and inversely
related to pixel greyscale (where darker pixels indicate higher
chromophore concentrations for the purposes of intuitive map
display). To compare all endpoints as a function of skin type,
one-way ANOVA analyses were performed, using skin type as
the main factor. The results of these analysis were then plotted
as least signicant difference means with associated 95% con-
dence intervals.
Results
Comparison of contact and noncontact SIAscope
eumelanin greyscale
When mean greyscale values, corresponding to theoretical
mean eumelanin concentration, obtained by both contact and
noncontact techniques, were compared by simple regression
analysis (Fig. 4a), an excellent linear correlation was observed
(r
2
88%; P < 0001). The regression line did not go
through the origin, reecting a small offset in greyscale
between the differing camera systems (that can be taken
account of in calibration vs. actual eumelanin values, reported
later).
Comparison of contact and noncontact SIAscope
eumelanin greyscale measurement with density of
melanin staining in histological samples
When both contact and noncontact SIAscope mean greyscale
values were compared with corresponding values for mean
density of silver staining (Von Kossa protocol) in histological
samples by simple regression analysis (Fig. 4b,c), clear corre-
lations were obtained for each (r
2
70%, P < 00001 and
80%, P < 00001, respectively).
Comparison of contact and noncontact SIAscope
eumelanin greyscale measurement with absolute
eumelanin and phaeomelanin tissue concentration
When both contact and noncontact SIAscope mean greyscale
values were compared with corresponding values for mean
eumelanin concentration (ng mg
)1
wet tissue) by simple
regression analysis (Fig. 4d,e), clear correlations were
obtained for each (r
2
84%, P < 00001 and 77%,
P < 00001, respectively). In contrast, there was no correla-
tion for both contact and noncontact SIAscope methods vs.
phaeomelanin (r
2
01%, P 089 and 03%, P 079,
respectively).
Comparison of contact and noncontact SIAscope
eumelanin greyscale measurement with Mexameter
melanin index
When both contact and noncontact SIAscope mean greyscale
values were compared with corresponding values for MI
obtained using the Mexameter, clear correlations were
obtained for each (r
2
98%, P < 00001 and 86%,
P < 00001, respectively).
(a)
(b)
(c)
Fig 3. Examples of Von Kossa staining of epidermal melanin in
different Fitzpatrick skin types (original magnication 200).
(a) Type I, (b) type IV, (c) type VI.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
624 Distribution of melanin in skin, P.J. Matts et al.
Analysis of contact and noncontact SIAscope eumelanin
and oxyhaemoglobin greyscale measurements,
Mexameter-derived melanin and erythema indices,
melanin density and absolute eumelanin tissue
concentration by Fitzpatrick skin type
Comparison of the distribution of melanin values obtained
from contact and noncontact SIAscope measurements, the
Mexameter and the biopsy-derived melanin determinations by
Fitzpatrick skin type yielded very similar trends (Fig. 5ae).
Melanin values over skin types IIV increased incrementally,
followed by a larger step increase to type V and the greatest
increase to type VI.
Visual inspection of the distribution of both contact and
noncontact SIAscope oxyhaemoglobin greyscale values by Fitz-
patrick skin type (Fig. 5f,g) shows that there appears to be no
relationship between the two parameters (corroborated by
simple regression analysis comparing eumelanin and oxyhae-
moglobin values derived from contact and noncontact SIA-
scope measurements, yielding weak correlations, r
2
35%
(a) (b)
(c)
(e)
(d)
Fig 4. (a) Simple regression analysis of contact SIAscope eumelanin map mean greyscale vs. noncontact SIAscope eumelanin map mean greyscale,
(b) simple regression analysis of contact SIAscope eumelanin map mean greyscale vs. mean silver stain density per eld, (c) simple regression
analysis of noncontact SIAscope eumelanin map mean greyscale vs. mean silver stain density per eld, (d) simple regression analysis of contact
SIAscope eumelanin map mean greyscale vs. analytically determined eumelanin tissue concentration (ng mg
)1
wet tissue), (e) simple regression
analysis of noncontact SIAscope eumelanin map mean greyscale vs. analytically determined eumelanin tissue concentration (ng mg
)1
wet tissue).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
Distribution of melanin in skin, P.J. Matts et al. 625
(a) (b)
(c) (d)
(e) (f)
(g) (h)
Fig 5. (a) Means and 95% least signicant difference (LSD) intervals for contact SIAscope eumelanin map mean greyscale values (256 ) map
value) vs. Fitzpatrick skin type), (b) means and 95% LSD intervals for noncontact SIAscope eumelanin map mean greyscale values (256 ) map
value) vs. Fitzpatrick skin type), (c) means and 95% LSD intervals for Mexameter melanin index vs. Fitzpatrick skin type), (d) means and 95%
LSD intervals for melanin silver stain density vs. Fitzpatrick skin type), (e) means and 95% LSD intervals for eumelanin concentration (ng mg
)1
wet tissue) vs. Fitzpatrick skin type), (f) means and 95% LSD intervals for contact SIAscope haemoglobin map mean greyscale values vs. Fitzpatrick
skin type, (g) means and 95% LSD intervals for noncontact SIAscope haemoglobin map mean greyscale values vs. Fitzpatrick skin type, (h) means
and 95% LSD intervals for Mexameter erythema index vs. Fitzpatrick skin type.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
626 Distribution of melanin in skin, P.J. Matts et al.
and 21%, respectively). In contrast, the Mexameter EI values
yielded a distribution by Fitzpatrick skin type (Fig. 5h) very
similar to that of the other melanin endpoints (and, indeed, if
Mexameter melanin and erythema indices are compared by
simple regression analysis, a clear correlation between the two
is conrmed, r
2
79%).
Reectance spectrophotometric analysis of Fitzpatrick
skin types
Figure 6 shows a spectral plot of percentage reectance (400
700 nm) for Fitzpatrick skin types IVI, using data derived
from the X-Rite MA68II reectance spectrophotometer (data
taken from the 15 detector). The plot clearly shows the
incremental decrease in reectance across the entire 400
700 nm bandwidth with skin type, consistent with the stead-
ily increasing epidermal fraction volume of melanin. As noted
with the objective and analytical determinations of melanin
above, the most dramatic change occurs between types V and
VI. The plot also shows the characteristic attening of the
remittance spectrum of skin with increasing melanin concen-
tration, with the gradual loss of the haemoglobin peaks seen
in type I skin.
Discussion
The results demonstrate clear correlations between the
eumelanin greyscale values produced by both the contact and
noncontact SIAscope techniques and both histological and
analytical values for melanin within the same specic area of
human skin, across the whole range of Fitzpatrick skin types.
It should also be noted that (i) there was no correlation of
the SIAscope eumelanin values to analytically determined
phaeomelanin tissue concentrations and (ii) likewise, no cor-
relation between SIAscope eumelanin and oxyhaemoglobin
values.
The same cannot be said for the other objective instrumen-
tal measure employed, the Mexameter, typical of approaches
deriving MI and EI. While there was a relatively strong corre-
lation between MI and SIAscope eumelanin values, there was
also a clear relationship between Mexameter-derived melanin
and erythema indices. No such relationship was observed for
the SIAscope-derived eumelanin and oxyhaemoglobin end-
points. This phenomenon can be predicted from rst princi-
ples. The Mexameter integrates reectance within three
specic wavebands with k
max
at 568 nm (relatively strong
absorption for the melanins), 660 nm and 870 nm (relatively
weak absorption for the haemoglobins). Equations 1 and 2
below show how the Mexameter MI and EI values are derived
mathematically, where R denotes reectance at the stated
waveband:
Equation 1: MI log
10
R
870nm
=R
660nm
1000
Equation 2: EI log
10
R
660nm
=R
568nm
1000:
Visual inspection of the spectral plots of raw reectance in
Figure 6 and consideration of the algorithms above demon-
strates how such a strong correlation can be possible between
MI and EI in skin tissue of static blood status, but increasing
pigment concentration. It can be seen that melanin has relat-
ively greater absorption at 568 nm than at 660 nm. It could
be predicted from Equation 2, therefore, that tissue with
increasing melanin content but with static haemoglobin con-
tent (as is the case in this study) would give an increase in EI,
proportional to MI. This is precisely what is observed in
Figure 5h.
To summarize simply, the log-ratio method employed in a
variety of commercial melanin and erythema meters is a very
useful adjunct to skin colour measurement, in that it goes
some way to measuring the chromophores responsible for the
observed appearance. These methods are limited, however, by
their inability to provide completely exclusive measurements
of melanin and haemoglobin and, thus, the real risk of provi-
ding false positive readings where extremes of either chromo-
phore coincide one with another (as is often the case in
diseased or photodamaged skin).
The approach adopted by the SIAscope method is consider-
ably more robust in that it employs algorithms incorporating
a rigorous model of light transport, describing in full the
possible intracutaneous interactions of light with human skin
tissue. This unique approach allows inverse mapping, that is,
from tissue colour to its precise histological values. The quan-
tities of melanin, haemoglobin (and, for the contact approach,
collagen) derived are then used to construct mutually exclu-
sive parametric greyscale concentration maps. This array
of pixels, therefore, representing the concentration of the
chromophores responsible for human skin coloration, may be
interrogated by sophisticated image analysis algorithms to
yield quantitative information regarding the distribution of
these entities. This is not possible with the point measurement
employed by MI or EI instruments. The importance of
spatially resolved chromophore measurements cannot be
I
II
III
IV
V
VI
400
0
10
20
30
40
50
60
450 500 550 600 650 700
Wavelength (nm)
X
-
R
i
t
e
M
A
6
8
I
I
%
r
e
f
l
e
c
t
i
o
n
(
)
Fig 6. Spectral plot of percentage reectance (400700 nm) for
Fitzpatrick skin types IVI; data derived from X-Rite MA68II
reectance spectrophotometer (15 angle observer).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
Distribution of melanin in skin, P.J. Matts et al. 627
over-emphasized as they now provide the investigator with a
means to understand and explain, on a molecular basis, non-
homogeneities in the colour appearance of the skin tissue in
question.
Importantly, this noninvasive method for eumelanin deter-
mination is potentially useful as a new clinical tool, for example
in the measurement, quantication and tracking of photodam-
age endpoints (e.g. lentigos and diffuse hyperpigmentation),
skin disease states (e.g. pigmentation disorders such as vitiligo)
and induced melanogenesis (e.g. UVR therapy, delayed pigment
darkening endpoints), independent of haemoglobin-based
features.
In summary, these data provide condence that both con-
tact and noncontact SIAscope chromophore mapping tech-
niques provide robust and rapid noninvasive measures of the
concentration and spatial distribution of eumelanin in vivo,
which correspond to true tissue values for this chromophore.
Acknowledgments
The authors wish to acknowledge the expert technical assist-
ance of S.D. Cotton PhD and R. Morse PhD of Astron Clinica,
Cambridge, U.K. and also thank Professors Ito and Wakamatsu
for their analysis of samples from this study.
References
1 Anderson RR, Parrish JA. The optics of human skin. J Invest Dermatol
1981; 77:1319.
2 Bashkatov AA, Genina EA, Kochubey VI, Tuchin VV. Optical prop-
erties of human skin, subcutaneous and mucous tissues in the
wavelength range from 400 to 2000 nm. J Phys D Appl Phys 2005;
38:254355.
3 Dawson JB, Barker DJ, Ellis DJ et al. A theoretical and experimental
study of light absorption and scattering by in vivo skin. Phys Med Biol
1980; 25:695709.
4 Zonios G, Bykowski J, Kollias N. Skin melanin, hemoglobin, and
light scattering properties can be quantitatively assessed in vivo using
diffuse reectance spectroscopy. J Invest Dermatol 2001; 117:14527.
5 Fitzpatrick TB. The validity and practicality of sun-reaction skin
types I through VI. Arch Dermatol 1988; 124:86971.
6 Campbell FW, Robson JG. Application of Fourier analysis to the
visibility of gratings. J Physiol 1968; 197:55166.
7 Pierard GE. EEMCO guidance for the assessment of skin colour.
J Eur Acad Dermatol Venereol 1998; 10:111.
8 Diffey BL, Oliver RJ, Farr PM. A portable instrument for quantify-
ing erythema induced by ultraviolet radiation. Br J Dermatol 1984;
111:66372.
9 Feather JW, Ellis DJ, Leslie G. A portable reectometer for the
rapid quantication of cutaneous haemoglobin and melanin. Phys
Med Biol 1988; 33:71122.
10 Edwards C. The Mexameter MX16
TM
. In: Bioengineering of the Skin:
Methods and Instrumentation (Berardesca E, Elsner P, Wilhelm KP,
Maibach HI, eds). Boca Raton: CRC Press, 1995; 1279.
11 Stamatas GN, Zmudzka BZ, Kollias N, Beer JZ. Non-invasive meas-
urements of skin pigmentation in situ. Pigment Cell Res 2004;
17:61826.
12 Cotton SD, Claridge E. Developing a predictive model of human
skin colouring. Proc SPIE 1996; 2708:81425.
13 Cotton SD, Claridge E, Hall PN. Non-invasive skin imaging. In:
Proceedings of Information Processing in Medical Imaging. (Duncan J, Gindi
G, eds). London: Springer-Verlag, 1997; 5016.
14 Moncrieff M, Cotton SD, Claridge E, Hall PN. Spectrophotometric
intracutaneous analysis a new technique for imaging pigmented
skin lesions. Br J Dermatol 2002; 146:44857.
15 Cotton SD. A Non-Invasive Imaging System For Assisting in the Diagnosis of
Malignant Melanoma. PhD thesis, Birmingham University, 1998.
16 Preece S, Cotton SD, Claridge E. Imaging the pigments of skin with
a technique which is invariant to changes in surface geometry and
intensity of illuminating light. In: Proceedings of Medical Image Under-
standing and Analysis (Barber D, ed.). Malvern: British Machine Vision
Association, 2003; 1458.
17 Ito S, Wakamatsu K. Quantitative analysis of eumelanin and phaeo-
melanin in humans, mice, and other animals: a comparative
review. Pigment Cell Res 2003 16:52331.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp620628
628 Distribution of melanin in skin, P.J. Matts et al.
CUTANEOUS BI OLOGY DOI 10. 1111/j . 1365- 2133. 2006. 07711. x
Scratching and noxious heat stimuli inhibit itch in humans:
a psychophysical study
G. Yosipovitch,* M.I. Duque,* K. Fast,* A.G. Dawn* and R.C. Coghill
*Departments of Dermatology and Neurobiology and Anatomy, Wake Forest University School of Medicine, Medical Center Boulevard, Winston-Salem, NC
27157, U.S.A.
Correspondence
Gil Yosipovitch.
E-mail: gyosipov@wfubmc.edu
Accepted for publication
1 August 2006
Key words
histamine, innocuous thermal stimuli, noxious
cold, noxious heat, scratching, visual analogue scale
Conicts of interest
The authors have no conicts of interest to declare.
Summary
Background Patients who suffer from chronic itch employ creative techniques to
alleviate their itch, often using painful thermal stimuli, such as hot and very cold
showers, as well as mechanical stimuli, such as scratching.
Objectives The present study examined whether the sensory perception of itch is
attenuated by remote interactions between both thermal and mechanical stimuli
and afferent information related to itch.
Patients and methods Itch was induced with histamine iontophoresis in 21 healthy
young subjects. Repetitive thermal stimuli including innocuous warmth, innocu-
ous cool, noxious cold and noxious heat as well as scratching were applied 3-cm
distal to the area of histamine iontophoresis. Subjects rated their perceived inten-
sity of histamine-induced itch with a computerized visual analogue scale.
Results Itch intensity ratings were signicantly reduced during each period of
scratching and repeated noxious heat and cold. Innocuous cooling and warming
did not signicantly alter itch intensity ratings. Inter-individual differences in
histamine-induced itch sensitivity were unrelated to inter-individual differences
in pain sensitivity.
Conclusions The present psychophysical study demonstrates that repetitive noxious
thermal and scratching stimuli inhibit itch and do not require direct physical
interaction with the area of the skin from which itch originates.
Itch is a complex unpleasant sensory experience with many
similarities to pain. Both experiences are multidimensional
with sensory discriminative, cognitive, evaluative and motiva-
tional components. Much like pain, multiple lines of evidence
indicate that itch can be modulated by thermal stimuli as
well as mechanical stimuli. Firstly, patients suffering from
itch alleviate their itch by cooling the skin or by applying
noxious heat.
1
Secondly, Bickford observed more than
60 years ago that noxious heat as well as painful mechanical
and electrical stimuli inhibit experimental histamine-induced
itch.
2
Bickford demonstrated that histamine did not cause
itching or alloknesis when delivered within 10 cm of a noxi-
ous thermal stimulus and induced diminished itch when the
counterstimulus was beyond 10 cm.
2
Graham et al.
3
demon-
strated that remote noxious mechanical counterstimuli (pin-
prick) reduced itch when conned to the same dermatome as
the pruritic stimulus. Murray and Weaver showed that a
noxious cold stimulus (2 C) reduced itch, even when deliv-
ered to the ngertips contralateral to the pruritic stimulus.
4
More recently, several studies have shown that local noxious
thermal stimuli signicantly reduced experimental itch.
5,6
It
has been suggested that these thermal stimuli may exert a
central inhibitory effect.
4,7
If thermal modulation of itch is, in part, centrally mediated,
then thermal stimuli applied outside of an itchy skin region
would be predicted to reduce itch. However, few quantitative
psychophysical data are currently available. No previous stud-
ies have continuously measured subjects itch perception using
quantitative psychophysical techniques, such as a computer-
ized visual analogue scale (VAS). Moreover, minimal informa-
tion exists about the neural mechanisms by which scratching
inhibits itch. As in the case of thermal stimuli, if scratching-
induced modulation of itch relies, in part, on a central mech-
anism then scratching outside of the itchy area would have a
similar effect. Therefore, the purpose of the current study was
to use quantitative psychophysical techniques to address whe-
ther the sensory perception of itch is attenuated by inter-
actions between both thermal and mechanical stimuli and
afferent information related to itch. As pain and itch involve
similar negative affective and attentional components that may
inuence the perception of these modalities, a second objec-
tive was to assess whether inter-individual differences in itch
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634 629
perception were related to inter-individual differences in pain
sensitivity.
Methods
Subjects
Twenty-one healthy subjects (13 women, eight men)
between 18 and 48 years of age participated in this study.
All procedures were approved by the Institutional Review
Board of Wake Forest University School of Medicine. All vol-
unteers provided written informed consent and were free to
withdraw from the study at any time. None of the subjects
had a history of suffering from atopic eczema or any chronic
skin disease.
Induction of itch sensation
Itch was evoked by iontophoresis of histamine into the skin of
the ventral forearm using a round iontophoresis electrode
14 mm in diameter. For iontophoresis, a 1% solution of hist-
amine was dissolved in 2% methylcellulose gel (Sigma,
St Louis, MO, U.S.A.) and was administered with a current of
200 lA for 30 s (Perilont PF3826 Power device; Perimed
Stockholm, Sweden). A vehicle control stimulus of 09% saline
in 2% methylcellulose gel was administered (200 lA for 30 s)
in order to control for expectations of itch. Iontophoresis was
terminated 30 s prior to any thermal and scratch stimuli. Each
itch trial was separated by 10 min.
Stimuli-modulating itch
All modulatory stimuli were applied to sites on the nondomi-
nant ventral forearm 3-cm distal to the edge of the area of
histamine iontophoresis. In all cases, examinees perceived no
itch in these distal sites prior to the application of modulatory
stimuli.
Thermal stimuli were delivered by a 16 16 mm Peltier
device (TSA 2001, Medoc, Ramat Yishai, Israel). Thermal
stimuli consisted of noxious cold (2 C), innocuous cool
(15 C), innocuous warmth (41 C) and noxious heat
(49 C). The different thermal stimuli were delivered in a
random order, and each stimulus was delivered repetitively
in a single, 4-min trial. Thermal stimulation started 30 s
after termination of histamine iontophoresis and was cycled
between 30-s duration applications of the thermal stimulus
and 30-s duration applications of the neutral control stimulus
(32 C). The rate of temperature increase and decrease was
4 C s
)1
.
Scratching was accomplished by study personnel by repet-
itively moving a cytology brush (Medi-Pak 7-inch cytology
brush 242199; General Medical Corporation, Richmond,
VA, U.S.A.) over the ventral forearm 3-cm distal to the ionto-
phoresis site. Uniformity was controlled by applying suf-
cient pressure to bend skin-facing brush bristles so that the
brush handle touched the skin surface. The bending force of
the cytology brush was equivalent to approximately 29 g on
a digital scale. The cytology brush contains approximately
1000 individual bristles, and the diameter of the brush was
75 mm. In addition, the same member of the research team
(K.F.) applied the cytology brush for all subjects. The time
course of scratching was identical to that of thermal stimula-
tion. Each examinee underwent a training session in which
study personnel applied the cytology brush. The examinee
was asked whether the procedure was similar to their
experience when they scratch their skin. All subjects reported
that they perceived this procedure as closely simulating
scratching. None of the examinees perceived application
of the cytology brush as a painful, pricking or burning
sensation.
Quantitative psychophysical measurements
Subjects used a 100-mm computerized VAS (COVAS, Medoc)
to continuously report perceived intensity of histamine-
induced itch in the presence and absence of modulatory stim-
uli. Firstly, heat pain, cold pain, innocuous warmth and
innocuous cool were rated in the absence of itch. For all stim-
uli, continuous COVAS ratings were anchored with the verbal
descriptors of no sensation and the most intense sensation
imaginable and subjects were instructed verbally to provide
ratings of the appropriate modality. Subjects ratings were
sampled at 9 Hz and were analysed with custom-written soft-
ware. All subjects participated in a practice session in which
they were presented with the same stimuli to be used during
the study.
Statistical analysis
Subjects who reported COVAS ratings of histamine-induced
itch 9/100 were included in the pairwise statistical analy-
ses. To simplify analyses of continuous computerized VAS
data, itch intensity ratings were extracted from the midpoints
of each period of modulatory stimulation and analogous time
points of control stimulation. Psychophysical ratings of itch
were then analysed using two-factor (time modulatory sti-
mulus) repeated measures analyses of variance (JMP software,
SAS Institute Inc., Cary, NC, U.S.A.) to determine changes in
sensations due to modulatory stimuli and due to time. There
were two levels of the modulatory stimulus factor (baseline
vs. modulatory stimulus) and, depending on the modulatory
stimulus, there were six to seven levels of the time factor. A
signicant main effect of either the modulatory stimulus fac-
tor or a signicant interaction between the modulatory sti-
mulus and time factors indicates that the perception of itch
is signicantly inuenced by the presence of the modulatory
stimulus.
To evaluate the relationship between inter-individual differ-
ences in thermal sensitivity and histamine-induced itch sensi-
tivity, Pearsons correlation tests were performed between the
peak intensity ratings of each modulatory stimulus and the
peak intensity ratings of itch.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634
630 Remote inhibition of itch, G. Yosipovitch et al.
Results
Repeated scratching-induced modulation of itch
Histamine-induced itch intensity ratings were signicantly
reduced during each period of scratching (n 10,
P < 00001, Fig. 1). The repeated effect of the stimulus was
taken into account by considering both stimulus and time
interaction. Itch ratings decreased immediately at the onset of
scratching and remained at low levels during the entire period
of scratching. However, upon termination of scratching per-
ceived itch rebounded slightly.
Repeated noxious heat-induced modulation of itch
Histamine-induced itch intensity ratings were signicantly
reduced during each period of noxious heat (n 10,
P < 0004, Fig. 2). Itch ratings decreased immediately at the
onset of heat pain and remained at low levels during the
entire period of stimulation. However, in contrast to scratch-
ing, itch decreased further upon termination of heat pain.
Repeated noxious cold-induced modulation of itch
Histamine-induced itch intensity ratings were signicantly
reduced during noxious cold stimulation (n 9, P < 0001,
Fig. 3). Itch ratings decreased gradually after the onset of
noxious cold. In contrast to scratching where itch ratings were
elevated after each period of stimulation, itch ratings after cold
pain remained lower during the nonstimulated interval.
Effect of innocuous thermal stimuli on itch perception
Histamine-induced itch intensity ratings were not signicant-
ly affected by either innocuous warmth (P < 08) or innocu-
ous cooling (P < 029) (Figs 4, 5). All subjects reported
psychophysical ratings greater than zero for both innocuous
stimuli.
Fig 1. Mean itch intensity with histamine
(baseline) and with histamine and scratching
3-cm distal to site of histamine iontophoresis
(n 10). Scratching immediately reduced
itch. These reductions were sustained for the
duration of the scratching stimuli; moreover,
itch ratings rebounded slightly following
termination of scratching stimuli.
Fig 2. Mean itch intensity with histamine
(baseline) and with histamine and noxious
heat (49 C) 3-cm distal to site of histamine
iontophoresis (n 10). At the onset of
noxious heat stimulation, itch ratings
decreased. In contrast with scratching stimuli,
itch ratings decreased again at the offset of
noxious heat stimulation.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634
Remote inhibition of itch, G. Yosipovitch et al. 631
Fig 3. Mean itch intensity with histamine
(baseline) and with histamine and noxious
cold (2 C) 3-cm distal to site of histamine
iontophoresis (n 9). Itch ratings decreased
gradually during noxious cold stimulation and
exhibited minimal rebound when skin
temperature returned to 32 C.
Fig 4. Mean itch intensity with histamine
(baseline) and histamine with innocuous cool
(15 C) 3-cm distal to site of histamine
iontophoresis (n 10). Innocuous cool was
associated with a lesser reduction of perceived
itch compared with either noxious thermal
stimuli or scratching. Although gradual
declines in itch ratings were noted, these
were not sufciently robust to be statistically
signicant.
Fig 5. Mean itch intensity with histamine
(baseline) and with histamine and innocuous
warmth (41 C) 3-cm distal to site of
histamine iontophoresis (n 10). Innocuous
warm stimuli produced no statistically
signicant effects on perceived itch.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634
632 Remote inhibition of itch, G. Yosipovitch et al.
Inter-individual differences in itch and pain sensitivity
Signicant inter-individual differences in itch sensitivity to
histamine were noted among the healthy subjects; however,
inter-individual differences in itch sensitivity were unrelated
to inter-individual differences in pain sensitivity. Inter-
individual differences in the magnitude of COVAS ratings of
histamine-induced itch intensity were not signicantly correl-
ated to inter-individual differences in the magnitude of heat
pain intensity ratings (r
2
01, P < 02), to inter-individual
differences in cold pain ratings (r
2
007, P < 05) or
to ratings of innocuous warmth (r
2
006, P < 04). Non-
noxious cool intensity ratings exhibited a nonsignicant
correlation with inter-individual differences in itch intensity
perception (r
2
038, P < 008). Furthermore, no signicant
relationship was noted between heat pain sensitivity and heat
pain suppression of itch (r
2
001, P < 07) or cold pain
sensitivity and cold pain suppression of itch (r
2
005,
P < 06).
Discussion
The present results show that heat pain, cold pain and scratch-
ing can attenuate histamine-induced itch in healthy human
subjects. Importantly, this reduction in itch occurs even when
thermal and mechanical stimuli are applied distal to the skin
region where itch was evoked. This observation indicates that
both thermal and mechanical modulators of histamine-induced
itch do not require a direct physical interaction with the skin
region from which itch originates, but instead rely on a more
widespread mechanism that may involve the central nervous
system.
Thermal stimuli have been shown to inhibit itch in
humans and animals.
5,8
It could be argued that this inhibi-
tion is peripherally mediated, as primary afferents that trans-
duce itch have innervation territories that can be as large as
85 mm in diameter in some areas of the body.
9
Studies by
Graham et al.
3
more than a half a century ago demonstrated
that itching induced by the pruritic plant cowhage or by his-
tamine was abolished by painful prick in the same derma-
tome at a distance of 24 cm on the leg and back.
3
Nilsson
et al.
10,11
demonstrated recently that noxious electrical stimuli
applied as far as 10 cm from histamine stimuli suppressed
histamine-induced itch for hours in the areas surrounding
the electrical stimulation. They suggested further that this
inhibition is centrally mediated. The majority of modulatory
stimuli have been delivered directly to the area of itch stim-
uli.
5,6
Cooling, for example, inhibits itch by a direct effect
on peripheral nerves.
5
Conversely, noxious heat potentiates
histamine responses in single C polymodal nociceptors in
canines,
12
despite the observation that noxious heat inhibits
itch in humans.
6
In addition, we have demonstrated that
repetitive, remote scratching and noxious heat pain inhibit
histamine-induced skin blood ow, whereas cooling the skin
does not signicantly affect skin blood ow and warming
the skin increases histamine-induced blood ow.
13
Thus, per-
ipheral interactions alone cannot account for the modulation
of itch by noxious heat pain.
Several studies suggest that thermal modulation of itch
could be a centrally mediated effect.
4,7
Taken together, our
results suggest that this inhibition may be modulated via a spi-
nal or supraspinal mechanism. At the supraspinal level, a pos-
sible explanation for modulation of itch would be that
subjects attention was diverted from itch by the modulatory
stimuli. The most effective stimuli (noxious heat and scratch-
ing) were perceptually robust and readily capable of capturing
attention. Studies using functional magnetic resonance ima-
ging and positron emission tomography have shown extensive
itch-related activation in brain areas important in attention,
such as the prefrontal cortex.
1417
In addition to modulation of itch during the plateau phase
of noxious heat stimulation, itch was also markedly dimin-
ished during the offset of the heat pain stimuli both in the
present investigation and previously.
5
This was a unique
effect noted only in heat pain stimuli. This time-locked
decrease in itch was strikingly similar to an analgesic phe-
nomenon termed offset analgesia.
18
Offset analgesia is a dis-
proportionately large decrease in perceived pain intensity
evoked by slight reductions in noxious stimulus intensity. As
offset analgesia appears to be mediated by a central mechan-
ism,
19
the time-locked decrease in itch during the offset of
noxious thermal stimuli further suggests that this modulation
occurs centrally.
Although patients often state that continuous scratching
relieves their itch, no previous psychophysical study has exam-
ined the effect of scratching distal to the site of histamine
iontophoresis on itch perception. Since the pivotal work in
the early twentieth century by Sherrington on the scratch
reex in dogs whose spinal cords had been transected at the
cervical level,
20
scratching has been considered to be a spinal
reex. Interestingly, no previous studies in humans have
examined the effect of scratching on itch perception. In the
pivotal study by Graham et al.
3
it is noted that scratching
inhibits itch; however, this study used a pinprick stimuli,
which is dissimilar to scratching.
As pain and itch involve similar negative affective and atten-
tional components, one might assume that those subjects who
rate pain higher will rate itch higher. Our study demonstrates
that itch intensity perception does not correlate to pain percep-
tion. Inter-individual differences in perception of itch intensity
do not appear to be scaling effects due to inter-individual dif-
ferences in COVAS scale usage, as ratings of histamine-induced
itch magnitude were not signicantly related to ratings of
warmth, heat pain, cool or cold pain intensity.
Sensitivity to thermal stimuli was not signicantly related to
itch modulation. Future studies involving large samples may
allow assessments of which personality dispositions are stron-
ger predictors of itch intensity in healthy as well as patients
with chronic itch.
In this study, modulatory stimuli were applied 3-cm distal
to the border of the site of histamine iontophresis. It would
be of interest to examine how distal stimuli at varying distan-
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634
Remote inhibition of itch, G. Yosipovitch et al. 633
ces attenuate the itch response. Another limitation is that we
used a small Peltier thermode (16 mm 16 mm), which may
induce a less robust noxious cold stimulus than larger probes
(32 mm 32 mm). This may explain differences between
our results and those reported by Fruhstorfer et al. who dem-
onstrated that cold bath stimulation induced more pronounced
inhibition of itch than heat pain.
5
It would be of great interest to examine whether the same
mechanisms that attenuate itch in healthy volunteers exist in
chronic itch conditions such as atopic dermatitis. Recent stud-
ies have shown that painful stimuli, such as electrical stimuli,
induce itch in eczematous lesions of patients with atopic
dermatitis, suggesting that there are differences in the central
processing of itch and pain in chronic itch conditions.
21
The
present data suggest that mechanisms such as noxious thermal
and scratching stimuli may modulate itch.
Acknowledgments
This research was supported in part by NINDS NS 39426.
References
1 Yosipovitch G. Pruritus: an update. Curr Probl Dermatol 2003;
15:13764.
2 Bickford RG. Experiments in relation to the itch sensationits
peripheral mechanism and central pathways. Clin Sci 1938; 3:377
86.
3 Graham DT, Goodell H, Wolff HG. Neural mechanisms involved
in itch, itchy skin, and tickle sensations. J Clin Invest 1951; 30:37
49.
4 Murray FS, Weaver MM. Effects of ipsilateral and contralateral
counterirritation on experimentally produced itch in human
beings. J Comp Physiol Psychol 1975; 89:81926.
5 Fruhstorfer H, Hermanns M, Latzke L. The effects of thermal
stimulation on clinical and experimental itch. Pain 1986; 24:259
69.
6 Ward L, Wright E, McMahon SB. A comparison of the effects of
noxious and innocuous counterstimuli on experimentally induced
itch and pain. Pain 1996; 64:12938.
7 Mochizuki H, Tashiro M, Kano M et al. Imaging of central itch
modulation in the human brain using positron emission tomo-
graphy. Pain 2003; 105:33946.
8 Carstens E, Jinks SL. Skin cooling attenuates rat dorsal horn neuronal
responses to intracutaneous histamine. Neuroreport 1998; 9:41459.
9 Schmelz M, Schmidt R, Bickel A et al. Specic C-receptors for itch
in human skin. J Neurosci 1997; 17:80038.
10 Nilsson HJ, Psouni E, Schouenborg J. Long term depression of
human nociceptive skin senses induced by thin bre stimulation.
Eur J Pain 2003; 7:22533.
11 Nilsson HJ, Levinsson A, Schouenborg J. Cutaneous eld stimula-
tion (CFS): a new powerful method to combat itch. Pain 1997;
71:4955.
12 Mizumura K, Koda H. Potentiation and suppression of the
histamine response by raising and lowering the temperature in
canine visceral polymodal receptors in vitro. Neurosci Lett 1999; 266:
912.
13 Yosipovitch G, Fast K, Bernhard JD. Noxious heat and scratching
decrease histamine-induced itch and skin blood ow. J Invest Dermatol
2005; 125:126872.
14 Hsieh JC, Hagermark O, Stahle-Backdahl M et al. Urge to scratch
represented in the human cerebral cortex during itch. J Neurophysiol
1994; 72:30048.
15 Drzezga A, Darsow U, Treede RD et al. Central activation by hist-
amine-induced itch: analogies to pain processing: a correlational
analysis of O-15 H
2
O positron emission tomography studies. Pain
2001; 92:295305.
16 McGlone F, Rukweid R, Howard M et al. Histamine-induced
discriminative and affective responses revealed by functional MRI.
In: Itch: Basic Mechanisms and Therapy (Yosipovitch G, Greaves MW,
McGlone F, eds), New York: Marcel Decker, 2004; 5161.
17 Walter B, Sadlo MN, Kupfer J et al. Brain activation by histamine
prick test-induced itch. J Invest Dermatol 2005; 125:3802.
18 Grill JD, Coghill RC. Transient analgesia evoked by noxious stimu-
lus offset. J Neurophysiol 2002; 87:22058.
19 Yelle MD, Rogers JM, Coghill RC. Offset analgesia: a centrally
mediated temporal contrast mechanism. 11th World Congress on Pain
2005 [Abstract].
20 Sherrington CS. Observations on the scratch reex in the spinal
dog. J Physiol Lond 1906; 34:150.
21 Ikoma A, Fartasch M, Heyer G et al. Painful stimuli evoke itch in
patients with chronic pruritus: central sensitization for itch. Neurology
2004; 62:21217.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp629634
634 Remote inhibition of itch, G. Yosipovitch et al.
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07717. x
Coexistence of IgA antibodies to desmogleins 1 and 3
in pemphigus vulgaris, pemphigus foliaceus and
paraneoplastic pemphigus
L.F. Mentink, M.C.J.M. de Jong, G.J. Kloosterhuis, J. Zuiderveen, M.F. Jonkman and H.H. Pas
Center for Blistering Diseases, Department of Dermatology, University Medical Center Groningen, University of Groningen, P.O. Box 30.001,
9700 RB Groningen, the Netherlands
Correspondence
Hendri H. Pas.
E-mail: h.h.pas@derm.umcg.nl
Accepted for publication
18 August 2006
Key words
autoimmunity, desmoglein, IgA, mucosa,
pemphigus, skin
Conicts of interest
None declared.
Summary
Background Pemphigus is a bullous mucocutaneous autoimmune disease character-
ized by IgG autoantibodies to desmoglein (Dsg) 1 and/or Dsg3. Occasionally
direct immunouorescence of pemphigus skin reveals IgA depositions with an
intraepidermal intercellular pattern in addition to the IgG deposition.
Objectives To investigate if pemphigus patients, in addition to having IgG autoanti-
bodies, also generate IgA antibodies to Dsg1 and/or Dsg3.
Patients/methods Sera of 100 pemphigus patients and 36 bullous pemphigoid con-
trols were tested by IgA enzyme-linked immunosorbent assay (ELISA) to the
recombinant extracellular domains of Dsg1 and Dsg3. The patients were selected
on clinical grounds and positive IgG ELISA index values for Dsg1 and/or Dsg3.
They were divided into four groups: patients having IgG to only Dsg1 (n 34),
patients having IgG to both Dsg1 and Dsg3 (n 31), patients having IgG to
only Dsg3 (n 27) and patients who had paraneoplastic pemphigus (PNP)
(n 8).
Results IgA antibodies to Dsg1 were found in 13 (38%) of the patients with IgG
to Dsg1, in ve (16%) of the patients with IgG to both Dsg1 and Dsg3, in four
(15%) of the patients with IgG to Dsg3 and in none of the PNP patients. IgA
antibodies to Dsg3 were found in one (3%) of the patients with IgG to Dsg1, in
18 (58%) of the patients with IgG to both Dsg1 and 3, in 18 (67%) of the
patients with IgG to Dsg3, and in four (50%) of the PNP patients. Immunouo-
rescence analysis demonstrated intraepidermal intercellular staining IgA antibodies
in serum and intercellular IgA deposits in skin of IgA ELISA-positive patients,
although to a lesser extent than by ELISA.
Conclusions This study shows that in a considerable number of supposedly IgG-
mediated pemphigus patients IgA to Dsg1 and Dsg3 is also present. In most cases
the antigen specicity of the IgA follows the antigen specicity of the IgG,
although in a small number of cases IgA is present against the Dsg not recog-
nized by IgG.
Pemphigus vulgaris (PV), pemphigus foliaceus (PF) and para-
neoplastic pemphigus (PNP) are blistering autoimmune dis-
eases of the skin and/or mucous membranes that are
characterized by circulating IgG to desmoglein (Dsg) 1 and/or
Dsg3.
1,2
In PNP antibodies to members of the plakin protein
family are also present.
3
Dsg1 and Dsg3 belong to the desmo-
somal cadherins and act as intercellular adhesion molecules
that connect the epidermal keratinocytes. The phenotypes of
PV and PF are thought to correlate with the IgG antibody
response to the two subtypes of Dsg. Antibodies to Dsg1 are
held responsible for skin lesions, while antibodies to Dsg3 are
supposed to result in mucosal lesions.
4
An enzyme-linked
immunosorbent assay (ELISA) series of dened pemphigus
patient groups largely conrmed this hypothesis. For most
patients an expected correlation was observed between the
antigen specicity and the clinical phenotype.
410
In a minor-
ity of pemphigus patients the correlation between anti-Dsg
antibody and pemphigus expression failed; they either had
lesions not tting the antibody prole, or lesions but negative
ELISAs or high ELISA titres but no lesions. This suggests that
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641 635
factors other than the Dsg prole may inuence the occur-
rence and the localization of the lesions.
11,12
Direct immuno-
uorescence (DIF) of pemphigus patient skin shows the
typical intercellular substance (ICS) staining pattern of IgG
around the epidermal keratinocytes. Occasionally biopsies
show additional IgA in an ICS staining pattern. The antigen
specicity of this IgA is not known, but it is possible that it
reects an IgA response to these same Dsgs. In pemphigoid,
especially mucous membrane pemphigoid, a dual IgG/IgA
response to the same antigen, BP180, is regularly observed.
1315
The antigens reported to have evoked IgA reactions in pem-
phigus include desmocollin 1, Dsg1 and Dsg3. Desmocollin 1
is the antigen in the pure IgA-pemphigus subtype subcorneal
pustular dermatosis (SPD).
16
IgA antibodies to Dsg1 or Dsg3
have been reported in occasional cases, and also in PV in two
more systematic studies. Spaeth et al.
17
studied anti-Dsg3 IgA
in PV by immunoblotting and found 22 positive cases among
41 patients, while Futei et al.
18
used the recombinant Dsg
ELISA technique and found among 30 PV patients two cases
with additional IgA to Dsg1.
When using DIF to study a PV patient who demonstrated
depositions of both IgG and IgA in the skin, we found by Dsg
ELISA that the serum of this patient also contained IgA to
Dsg3. We therefore decided to test all our pemphigus patients
with high anti-Dsg IgG titres for additional anti-Dsg IgA anti-
bodies. Here we show that, indeed, half of these patients have
such IgA in addition to IgG.
Materials and methods
Patient sera
All sera used in this study were from patients suffering from
pemphigus, either PV, PF or PNP, based on both clinical and
laboratory ndings. The sera were selected on the basis of
anti-Dsg1 or anti-Dsg3 IgG ELISA index values exceeding 75.
The cut-off values of both ELISAs are 20. In serum immuno-
uorescence on monkey oesophagus substrate all sera stained
in an ICS pattern. Only one serum sample was selected from
each patient. All sera had been collected previously and
stored at )80 C. The sera were divided into four groups:
three groups according to the IgG anti-Dsg prole, respec-
tively IgG-Dsg1, IgG-Dsg1+3, IgG-Dsg3 and a fourth group
of PNP patient sera (Table 1). Forty-six of the patients were
seen at our own department; of the other 54 patients we
received material for laboratory diagnosis as part of our
function as a reference centre for blistering diseases in the
Netherlands. The clinical and histological ndings of the
patients seen at our department with IgG to Dsg1 only (15)
best tted PF. When IgG to Dsg3, with or without anti-Dsg1
(16 and 15 patients, respectively), was present the clinical
and histological data suggested PV. All PNP patients had IgG
to Dsg3 and one of these also had accompanying IgG to
Dsg1. As negative controls we used 36 sera of bullous pem-
phigoid (BP) patients with IgG to BP180 and/or BP230. We
also tested these sera by ELISA for IgG to Dsg1 and Dsg3
but all were negative as expected.
Antidesmoglein enzyme-linked immunosorbent assay
IgG titres to Dsg1 and to Dsg3 were determined by the MESA-
CUP Desmoglein TEST Dsg1 and the MESACUP Desmoglein
TEST Dsg3 according to the manufacturers protocol (MBL,
Nagoya, Japan). For measuring IgA to Dsg1 and Dsg3 the
same test was used with one modication. The conjugate
reagent containing the peroxidase-conjugated antihuman IgG
monoclonal antibody provided with the original test was
replaced by a 1 : 5000 solution (048 lg mL
)1
) of peroxi-
dase-conjugated antihuman IgA (a-chain) goat IgG/Fab anti-
body fragments (MBL, Nagoya, Japan). This solution was used
for a 45-min room temperature incubation of the ELISA plate
instead of the anti-IgG conjugate. To exclude the possibility of
IgG cross-reaction we validated the specicity of this IgA assay
by testing puried IgG and IgA-pemphigus serum fractions.
Patient serum containing both anti-Dsg IgG and IgA activity
was subjected to Hi-Trap
TM
protein G column (GE Healthcare
Europe GmbH, Munich, Germany) chromatography. Protein G
binds all four IgG subclasses but has no afnity for IgA. Both
the ow-through and the 01 mol L
)1
glycineHCl pH 30
eluted fraction were collected and tested in the IgG and the
IgA ELISA. As expected, the ow-through reacted only in the
IgA ELISA, while no binding was observed in the IgG ELISA.
Conversely, the acid-eluted fraction reacted only in the IgG
ELISA but was absolutely negative in the IgA ELISA. This
showed that all binding observed in the IgA ELISA is due to
anti-Dsg-specic IgA without interference of cross-reacting
Table 1 IgG-ELISA Dsg1 and Dsg3 index
values for the four selected groups. In the
IgG-Dsg1+3 group all sera had at least either
the Dsg1 or the Dsg3 index exceeding 75
Group n IgG specicity
ELISA IgG
index to Dsg1
minmax (mean)
ELISA IgG
index to Dsg3
minmax (mean)
IgG-Dsg1 34 Dsg1 88289 (1928) 018 (33)
IgG-Dsg1+3 31 Dsg3 + Dsg1 21249 (1035) 46292 (1736)
IgG-Dsg3 27 Dsg3 016 (60) 80258 (1790)
PNP 8 Dsg3 Dsg1 298 (179) 32243 (1231)
ELISA, enzyme-linked immunosorbent assay; Dsg, desmoglein; PNP, paraneoplastic
pemphigus
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
636 Coexistent IgA and IgG in pemphigus, L.F. Mentink et al.
IgG. The cut-off optical density (OD) value above which a
sample was considered positive was determined on the basis
of OD values of the 36 BP control samples. For both the anti-
Dsg1 and the anti-Dsg3 ELISA the mean and the SD were cal-
culated. The mean OD
450
values of the 36 BP sera were 0114
for the anti-Dsg1 IgA ELISA and 0095 for the anti-Dsg3 IgA
ELISA. The SDs were 0027 and 0019, respectively. Calculat-
ing cut-off values as the mean OD plus three times the SD
resulted in values of 0196 for the Dsg1 IgA ELISA and 0151
for the Dsg3 IgA ELISA. All ELISA kits used in these experi-
ments had the same batch number. In each assay a previously
determined positive serum sample was taken as a positive con-
trol. The ODs of this positive control differed less then 15%
between assays.
Immunouorescence microscopy
For DIF, 4-lm thick cryostat sections were placed on micro-
scope slides and air-dried before a fan for 15 min. Sections
were washed in phosphate-buffered saline (PBS) (pH 73) and
then incubated for 30 min at room temperature with either u-
orescein-conjugated Fcc-specic goat F(ab)2 antihuman IgG or
uorescein-conjugated Fcc-specic goat F(ab)2 antihuman IgA
(both from Protos Immunoresearch, Burlingame, CA, U.S.A.)
in PBS supplemented with 1% bovine serum albumin. The
slides were then washed with PBS, coverslipped under PBS
glycerol (1 : 1 v/v), and examined using a Leitz Orthoplan
microscope (Leica Microsystems AG, Wetzlar, Germany)
equipped with a xenon short arc lamp (XBO 75W/2). Indirect
immunouorescence with patient serum was performed on
monkey oesophagus substrate. Patient sera were used at
dilutions of 1/10 and 1/40 in PBS. Secondary antibodies were
as in DIF.
Results
Antidesmoglein IgA enzyme-linked immunosorbent assay
A total of 100 pemphigus patient sera were tested in both
anti-Dsg IgA ELISA tests. Approximately half of these sera (54)
were found to have IgA to one or both Dsgs (Table 2).
Twenty-two patients had IgA to Dsg1 and 41 patients had IgA
to Dsg3 (Fig. 1). Nine patients had IgA to both Dsg1 and
Dsg3. The OD
450
levels in IgA Dsg1 ELISA ranged between
0069 and 2285 and in the IgA Dsg3 ELISA between 0066
and 4589. When we compare the Dsg specicity of the IgA
of each individual serum with its IgG specicity then for most
sera the IgA reacts with the same Dsg subtype as the IgG. IgA
antibodies to Dsg1 were found in 13 (38%) of the IgG-Dsg1
group, in ve (16%) of the IgG-Dsg1+3 group, in four
(15%) of the IgG-Dsg3 group and in none of the PNP
patients. IgA antibodies to Dsg3 were found in one (3%) of
the IgG-Dsg1 group, in 18 (58%) of the IgG-Dsg1+3 group,
in 18 (67%) of the IgG-Dsg3 group and in four (50%) of the
PNP patients. Five patients were found with IgA to the Dsg
subtype not recognized by the IgG, one in the IgG-Dsg1
group and four in the IgG-Dsg3 group.
Serum immunouorescence
Fifty-six sera were evaluated, in a blinded fashion, by serum
immunouorescence on monkey oesophagus substrate for the
presence of ICS staining IgA antibodies. Sera were tested at
Table 2 Distribution of the sera that reacted positive for IgA to Dsg1
or Dsg3 over the four selected groups
Group n IgA against Dsg1 IgA against Dsg3
IgG-Dsg1 34 13 (38%) 1 (3%)
IgG-Dsg1+3 31 5 (16%) 18 (58%)
IgG-Dsg3 27 4 (15%) 18 (67%)
PNP 8 0 4 (50%)
Total 100 22 41
Dsg, desmoglein; PNP, paraneoplastic pemphigus
Fig 1. IgA enzyme-linked immunosorbent assay results of the four
selected groups and controls. The top graph depicts the IgA reactions
to desmoglein (Dsg) 1, the bottom graph IgA to Dsg3. The horizontal
lines at OD
450
0196 and OD
450
0151 represent the cut-off
values.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
Coexistent IgA and IgG in pemphigus, L.F. Mentink et al. 637
1/10 and 1/40 dilutions. Weak dubious staining was consid-
ered negative unless the serum reacted clearly positive in the
other dilution. Three sera gave too much background staining
for proper evaluation. Of the 17 sera that showed ICS IgA
antibodies 15 had a positive IgA ELISA (88%). Of the 36 sera
that were judged negative 17 had a positive ELISA (47%)
(Table 3). In general those sera that were positive in immuno-
uorescence had higher IgA ELISA values.
In vivo intercellular IgA deposition
Thirty-nine of the 100 patients tested had a biopsy taken in
the same period that the serum was collected. Most patients
(35) had blood and biopsy taken on the same day while for
four patients this was within 8 days. Nineteen of these
patients had a negative IgA ELISA and the matching biopsies
of these 19 did not show IgA by DIF. Of the other 20 patients
who had positive IgA ELISAs, seven biopsies had a clear
deposition of IgA in a pemphigus-like ICS pattern (Fig. 2 and
Table 4). Thus in all cases where IgA was present in the skin
the matching serum had anti-Dsg IgA antibodies. Deposition
did not depend on the antigen recognized; two patients had
anti-Dsg1 IgA while the other ve had anti-Dsg3 IgA.
Time course of desmoglein-specic IgG and IgA
serum levels
From two patients both the IgG and IgA anti-Dsg3 titres were
followed during a time period of 15 months (Fig. 3). In both
patients the anti-Dsg IgA and IgG titre apparently behaved
very similarly. However, when looking in more detail at the
phase preceding the exacerbation in patient 1, the IgA here
seemed to be triggered somewhat earlier than the IgG. In add-
ition, when the levels decreased, the IgA in this patient also
disappeared more rapidly.
Sterile pustules in patients with antidesmoglein
IgA antibodies
The pure forms of IgA-pemphigus are vesiculopustular dis-
eases characterized by neutrophilic inltrates. We therefore
retrospectively screened the patient les of the 46 patients
seen at our own clinic, for clinical and laboratory differences
at the time of serum collection. Twenty-three of these 46
patients were positive for anti-Dsg IgA antibodies. Of these
Table 3 IgA ELISA compared with indirect immunouorescence on
monkey oesophagus
ELISA
Indirect immunouorescence
ICS
IgA-positive
(n 17)
ICS
IgA-negative
(n 36)
IgA-Dsg-negative (n 21) 2 19
IgA-Dsg1-positive (n 12) 5 7
IgA-Dsg3-positive (n 14) 7 7
IgA-Dsg1+3-positive (n 6) 3 3
ELISA, enzyme-linked immunosorbent assay; Dsg, desmoglein;
ICS, intercellular substance
(b)
(a)
Fig 2. Direct immunouorescence of a perilesional biopsy
demonstrates both IgG (a) and IgA (b) deposition in the typical
intercellular substance (ICS) pattern specic for pemphigus. The serum
of this patient contained IgG and IgA, both of which reacted with
desmoglein 3 by enzyme-linked immunosorbent assay. Bar is 10 lm.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
638 Coexistent IgA and IgG in pemphigus, L.F. Mentink et al.
patients 32% had sterile pustules, while in contrast no sterile
pustules were found in the 23 IgA-negative patients. However,
the records also showed that some IgA-negative patients had
had sterile pustules in the initial stage of the disease and prior
to treatment with systemic corticosteroids. Moreover, we also
found that in the IgA-negative group 70% had received treat-
ment with systemic corticosteroids, whereas only 30% in the
IgA-positive group had done so. Because in IgA-pemphigus
neutrophils dominate the inltrate we also expected a rela-
tively larger contribution of neutrophils in the IgA-positive
biopsies. However, we could not nd evidence for this, as
inltration of lesional skin with neutrophilic granulocytes was
seen as often in IgA-positive patients as in IgA-negative
patients.
Discussion
In this study we found IgA antibodies to Dsg1 and Dsg3 in a
large selection of randomly selected PV, PF and PNP sera. We
have used IgA ELISA tests against the recombinantly produced
ectodomains of Dsg1 and Dsg3. For anti-Dsg IgG these tests T
a
b
l
e
4
I
g
A
E
L
I
S
A
O
D
v
a
l
u
e
s
o
f
t
h
e
s
e
r
a
t
h
a
t
h
a
d
m
a
t
c
h
i
n
g
I
g
A
-
p
o
s
i
t
i
v
e
o
r
I
g
A
-
n
e
g
a
t
i
v
e
b
i
o
p
s
i
e
s
E
L
I
S
A
(
n
3
9
)
I
C
S
I
g
A
-
p
o
s
i
t
i
v
e
b
i
o
p
s
i
e
s
(
n
7
)
I
C
S
I
g
A
-
n
e
g
a
t
i
v
e
b
i
o
p
s
i
e
s
(
n
3
2
)
N
u
m
b
e
r
o
f
b
i
o
p
s
i
e
s
I
g
A
-
D
s
g
1
(
O
D
-
v
a
l
u
e
a
)
I
g
A
-
D
s
g
3
(
O
D
-
v
a
l
u
e
a
)
N
u
m
b
e
r
o
f
b
i
o
p
s
i
e
s
I
g
A
-
D
s
g
1
(
O
D
-
v
a
l
u
e
a
)
I
g
A
-
D
s
g
3
(
O
D
-
v
a
l
u
e
a
)
I
g
A
-
D
s
g
-
n
e
g
a
t
i
v
e
(
n
1
9
)
0
1
9
0
0
6
5
1
8
0
(
0
1
1
4
1
0
4
)
0
0
6
9
1
7
9
(
0
1
1
6
1
1
0
)
I
g
A
-
D
s
g
1
-
p
o
s
i
t
i
v
e
(
n
5
)
2
0
6
1
7
0
0
5
(
1
3
1
1
3
1
1
)
0
0
7
3
0
8
3
(
0
0
7
8
0
7
8
)
3
0
2
2
2
7
3
0
(
0
4
0
1
2
5
3
)
0
0
9
9
1
7
4
(
0
1
3
4
1
2
8
)
I
g
A
-
D
s
g
3
-
p
o
s
i
t
i
v
e
(
n
1
4
)
5
0
0
7
3
1
9
7
(
0
1
2
8
1
1
6
)
0
3
0
1
5
8
9
(
1
8
4
1
5
9
2
)
9
0
0
7
1
1
9
7
(
0
1
2
6
1
1
1
)
0
2
4
6
7
3
4
(
0
3
5
9
2
9
3
)
I
g
A
-
D
s
g
1
+
3
-
p
o
s
i
t
i
v
e
(
n
1
)
0
1
0
4
5
4
0
3
1
2
E
L
I
S
A
,
e
n
z
y
m
e
-
l
i
n
k
e
d
i
m
m
u
n
o
s
o
r
b
e
n
t
a
s
s
a
y
;
O
D
,
o
p
t
i
c
a
l
d
e
n
s
i
t
y
;
I
C
S
,
i
n
t
e
r
c
e
l
l
u
l
a
r
s
u
b
s
t
a
n
c
e
;
D
s
g
,
d
e
s
m
o
g
l
e
i
n
.
a
S
h
o
w
n
a
r
e
t
h
e
r
a
n
g
e
a
n
d
,
w
i
t
h
i
n
b
r
a
c
k
e
t
s
,
t
h
e
m
e
a
n
a
n
d
t
h
e
m
e
d
i
a
n
o
f
t
h
e
O
D
4
5
0
v
a
l
u
e
s
.
Fig 3. Longitudinal anti-desmoglein 3 IgA and IgG serum levels.
The enzyme-linked immunosorbent assays were performed as
indicated in Materials and methods. The IgA was assayed at the
standard 1 : 100 dilution. To keep the IgG reaction in the quantitative
range the sera had to be additionally diluted to 1 : 200 (patient 1)
and 1 : 500 (patient 2). The samples for the IgG assay were further
diluted from the already prepared samples for the IgA assay. All assays
were performed on the same day. Open squares, IgG; closed circles,
IgA.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
Coexistent IgA and IgG in pemphigus, L.F. Mentink et al. 639
have proven themselves to be reliable, specic and quantitative
measuring tools.
Analysis by serum immunouorescence demonstrated that
most IgA ELISA-positive sera also bound monkey oesophagus
in an ICS IgA-pemphigus pattern. The detection by immuno-
uorescence seems to depend on the actual amount of
anti-Dsg IgA in the serum, as the sera that were negative on
oesophagus had in general lower IgA ELISA values. The ELISA
thereby seems a more sensitive assay than indirect immuno-
uorescence analysis for detecting anti-Dsg IgA antibodies. We
also found two sera that were positive on oesophagus but
negative on ELISA. Possibly the IgA in these sera bind either
Dsg epitopes not present on the recombinant Dsg substrate
coated on the ELISA plate, or other desmosomal keratinocyte
antigen(s). In one patient that we followed for a longer time
an exacerbation occurred, and we noted that the serum IgA
level became slightly elevated before the IgG started to rise.
Whether this observation has any pathogenic relevance or
could be of future use as a practical prognostic parameter
remains to be determined.
The anti-Dsg IgA does deposit in vivo. All biopsies of ELISA-
negative patients were negative for IgA whereas in seven of
the 20 available biopsies of ELISA-positive patients an ICS IgA
pattern was found. Not all ELISA-positive sera had matching
IgA-positive biopsies. The reason for this is not clear but
might be due to a lower absolute anti-Dsg IgA concentration
as the sera with matching positive biopsies had on average
higher IgA ELISA values.
In the PV subgroup two earlier studies of possible anti-
Dsg IgA antibodies exist. Spaeth et al.
17
used immunoblotting
to detect IgA against Dsg3 in PV and, as we did, found a
high percentage of IgA-positive patients. Immunoblotting is
reported to be sensitive for detection of Dsg3 although, in
contrast to ELISA, conformational epitopes may be lost due
to sodium dodecyl sulfate treatment. Studying 41 patient sera
they found IgA against Dsg3 in 60% of acute-onset patients
and in 72% of chronic active patients, but none in patients
in remission. In our group with IgG against Dsg3 we found
by ELISA that 67% of the patients also had IgA against Dsg3
and 15% had IgA against Dsg1. Compared with Spaeth
et al.,
17
we did not select our patients for disease activity,
but included those with anti-Dsg3 ELISA IgG index values
over 75. Futei et al.
18
tested 30 Japanese PV cases by ELISA
and found no patients with IgA against Dsg3, although two
patients were positive for IgA to Dsg1. Of the 19 PF patients
they also tested none showed IgA against either Dsg1 or
Dsg3. It is not clear if the lower number of IgA responders
between Asian and European patients reects ethnic differ-
ences in developing anti-Dsg IgA antibodies, or is a result of
different therapies or is due to minor differences in assay
conditions. We used a polyclonal antibody to human IgA
where Futei et al.
18
used a monoclonal anti-IgA antibody.
Furthermore, we found that the initial anti-Dsg IgA serum
also allowed us to optimize the ELISA assay conditions.
In the group with IgG against Dsg1 we found 38% of the
patients to have IgA against Dsg1 and in one case against
Dsg3. Thus a considerable number of patients with PV or PF
have anti-Dsg IgA antibodies. The smallest group tested due to
the limited number of patients was the PNP group. Also, here
we found that four of eight patients (50%) had IgA against
Dsg3, similar to the patient reported by Preisz et al.
19
No IgA
anti-Dsg1 was found, but this may be in line with Dsg3 being
the major Dsg antigen in PNP.
2022
The autoantigens in IgA-
pemphigus are not Dsg1 and Dsg3. IgA-pemphigus is charac-
terized by pure IgA depositions and is divided into two major
subtypes: intraepidermal neutrophilic dermatosis (IEN) and
subcorneal pustular dermatosis (SPD). The antigen in SPD is
desmocollin 1, a desmosomal cadherin. The identity of the
antigen in IEN is unclear but seems to be located in non-
desmosomal areas.
23
In a review of IgA-pemphigus Hashimoto
described 25 patients of whom six were atypical and could
not be classied as SPD or IEN.
24
Three had a PF-like appear-
ance and were described as having PF-like IgA-pemphigus.
Two had IgA to Dsg1. Interestingly, he also investigated seven
patients with combined IgG and IgA. Six of these patients had
IgG to a Dsg and in ve cases the accompanying IgA was
directed to the same Dsg.
24
Other individual cases with
coexistent IgG and IgA anti-Dsg antibodies have been des-
cribed as IgG/IgA-pemphigus and pemphigus herpetiformis.
25,26
Our data indicate that IgA antibodies to Dsg are far more
common than generally assumed and are also present in
apparently IgG-mediated pemphigus. In seven of 20 biopsies
of patients with anti-Dsg IgA, mixed depositions were present
and these patients formally have to be classied as having
IgG/IgA-pemphigus. But as over half of our patients had cir-
culating anti-Dsg IgA it is feasible that in pemphigus a spec-
trum with increasing IgA contribution exists, ranging from
the pure classical IgG forms via mixed IgG/IgA forms to pem-
phigus types with only IgA against Dsgs. The two PF-like
patients found by Hashimoto et al.
27
to have solely IgA against
Dsg1 may reect this IgA endpoint of the spectrum.
In pemphigoid, especially mucous membrane pemphigoid,
combinations of IgG and IgA to BP180 are well known.
14,15
There, the presence of IgA is reported to mark a more chronic
and severe disease.
15
Whether IgA also plays a role in the
pathogenesis of pemphigus remains to be elucidated. The ster-
ile pustules seen in the IgA-positive group may already reect
a pathological effect of the anti-Dsg IgA, as such pustules were
absent in the IgA-negative group. Furthermore, systemic cor-
ticoids may exert a positive effect on clearing the pustules as
anti-Dsg IgA antibodies were predominantly found in the
group that had not received systemic treatment. From this it is
clear that the effects of IgA antibodies on the phenotype and
the possible consequences for the therapeutic regimen need
further investigation.
References
1 Amagai M. Autoimmunity against desmosomal cadherins in pem-
phigus. J Dermatol Sci 1999; 20:92102.
2 Amagai M. Desmoglein as a target in autoimmunity and infection.
J Am Acad Dermatol 2003; 48:24452.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
640 Coexistent IgA and IgG in pemphigus, L.F. Mentink et al.
3 Anhalt GJ, Kim SC, Stanley JR et al. Paraneoplastic pemphigus. An
autoimmune mucocutaneous disease associated with neoplasia.
N Engl J Med 1990; 323:172935.
4 Amagai M, Tsunoda K, Zillikens D et al. The clinical phenotype of
pemphigus is dened by the anti-desmoglein autoantibody prole.
J Am Acad Dermatol 1999; 40:16770.
5 Harman KE, Gratian MJ, Shirlaw PJ et al. The transition of pemphi-
gus vulgaris into pemphigus foliaceus: a reection of changing
desmoglein 1 and 3 autoantibody levels in pemphigus vulgaris.
Br J Dermatol 2002; 146:6847.
6 Miyagawa S, Amagai M, Iida T et al. Late development of anti-
desmoglein 1 antibodies in pemphigus vulgaris: correlation with
disease progression. Br J Dermatol 1999; 141:10847.
7 Ding X, Aoki V, Mascaro JM Jr et al. Mucosal and mucocutaneous
(generalized) pemphigus vulgaris show distinct autoantibody pro-
les. J Invest Dermatol 1997; 109:5926.
8 Harman KE, Seed PT, Gratian MJ et al. The severity of cutaneous
and oral pemphigus is related to desmoglein 1 and 3 antibody
levels. Br J Dermatol 2001; 144:77580.
9 Harman KE, Gratian MJ, Bhogal BS et al. A study of desmoglein 1
autoantibodies in pemphigus vulgaris: racial differences in fre-
quency and the association with a more severe phenotype. Br J
Dermatol 2000; 143:3438.
10 Toth GG, Pas HH, Jonkman MF. Transition of pemphigus vulgaris
into pemphigus foliaceus conrmed by antidesmoglein ELISA pro-
le. Int J Dermatol 2002; 41:5257.
11 Jamora MJ, Jiao D, Bystryn JC. Antibodies to desmoglein 1 and 3,
and the clinical phenotype of pemphigus vulgaris. J Am Acad Dermatol
2003; 48:9767.
12 Nguyen VT, Lee TX, Ndoye A et al. The pathophysiological signi-
cance of nondesmoglein targets of pemphigus autoimmunity.
Development of antibodies against keratinocyte cholinergic recep-
tors in patients with pemphigus vulgaris and pemphigus foliaceus.
Arch Dermatol 1998; 134:97180.
13 Christophoridis S, Budinger L, Borradori L et al. IgG, IgA and IgE
autoantibodies against the ectodomain of BP180 in patients with
bullous and cicatricial pemphigoid and linear IgA bullous dermato-
sis. Br J Dermatol 2000; 143:34955.
14 Murakami H, Nishioka S, Settereld J et al. Analysis of antigens tar-
geted by circulating IgG and IgA autoantibodies in 50 patients with
cicatricial pemphigoid. J Dermatol Sci 1998; 17:3944.
15 Settereld J, Shirlaw PJ, Kerr-Muir M et al. Mucous membrane
pemphigoid: a dual circulating antibody response with IgG and
IgA signies a more severe and persistent disease. Br J Dermatol
1998; 138:60210.
16 Hashimoto T, Kiyokawa C, Mori O et al. Human desmocollin 1
(Dsc1) is an autoantigen for the subcorneal pustular dermatosis
type of IgA pemphigus. J Invest Dermatol 1997; 109:12731.
17 Spaeth S, Riechers R, Borradori L et al. IgG, IgA and IgE autoanti-
bodies against the ectodomain of desmoglein 3 in active pemphi-
gus vulgaris. Br J Dermatol 2001; 144:11838.
18 Futei Y, Amagai M, Ishii K et al. Predominant IgG4 subclass in
autoantibodies of pemphigus vulgaris and foliaceus. J Dermatol Sci
2001; 26:5561.
19 Preisz K, Horvath A, Sardy Met al. Exacerbation of paraneoplastic pem-
phigus by cyclophosphamide treatment: detection of novel autoanti-
gens and bronchial autoantibodies. Br J Dermatol 2004; 150:101824.
20 Ohyama M, Amagai M, Hashimoto T et al. Clinical phenotype and
anti-desmoglein autoantibody prole in paraneoplastic pemphigus.
J Am Acad Dermatol 2001; 44:5938.
21 Nikolskaia OV, Nousari CH, Anhalt GJ. Paraneoplastic pemphigus
in association with Castlemans disease. Br J Dermatol 2003;
149:114351.
22 Amagai M, Nishikawa T, Nousari HC et al. Antibodies against
desmoglein 3 (pemphigus vulgaris antigen) are present in sera
from patients with paraneoplastic pemphigus and cause acantho-
lysis in vivo in neonatal mice. J Clin Invest 1998; 102:77582.
23 Ishii N, Ishida-Yamamoto A, Hashimoto T. Immunolocalization of
target autoantigens in IgA pemphigus. Clin Exp Dermatol 2004;
29:626.
24 Hashimoto T. Immunopathology of IgA pemphigus. Clin Dermatol
2001; 19:6839.
25 Oiso N, Yamashita C, Yoshioka K et al. IgG/IgA pemphigus with
IgG and IgA antidesmoglein 1 antibodies detected by enzyme-
linked immunosorbent assay. Br J Dermatol 2002; 147:101217.
26 Kozlowska A, Hashimoto T, Jarzabek-Chorzelska M et al. Pemphigus
herpetiformis with IgA and IgG antibodies to desmoglein 1 and IgG
antibodies to desmocollin 3. J Am Acad Dermatol 2003; 48:11722.
27 Hashimoto T, Komai A, Futei Y et al. Detection of IgA autoantibod-
ies to desmogleins by an enzyme-linked immunosorbent assay: the
presence of new minor subtypes of IgA pemphigus. Arch Dermatol
2001; 137:7358.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp635641
Coexistent IgA and IgG in pemphigus, L.F. Mentink et al. 641
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07716. x
Association between the insertion/deletion polymorphism
of the angiotensin I-converting enzyme gene and risk for
psoriasis in a Chinese population in Taiwan
Y-C. Chang, W-M. Wu, C-H. Chen, S-H. Lee, H-S. Hong and L-A. Hsu*
Department of Dermatology and *First Cardiovascular Division, Department of Internal Medicine, Chang Gung Memorial Hospital, Chang Gung University
College of Medicine, No. 199, Tung-Hwa North Road, Taipei, Taiwan
Correspondence
Lung-An Hsu.
E-mail: hsula@adm.cgmh.org.tw
Accepted for publication
13 September 2006
Key words
angiotensin-converting enzyme, polymorphism,
psoriasis
Conicts of interest
None declared.
Summary
Background Genetic factors play an important role in susceptibility for psoriasis.
The angiotensin I-converting enzyme (ACE) is expressed by keratinocytes.
Administration of ACE inhibitors may induce or exacerbate psoriasis in clinical
practice. Thus, ACE gene variants may contribute to the genetic background of
psoriasis.
Objectives To assess the role of the ACE insertion/deletion (I/D) polymorphism in
psoriasis among ethnically Chinese Taiwanese subjects.
Methods In total, 312 patients with psoriasis and 615 control subjects were ana-
lysed for the ACE I/D polymorphism by polymerase chain reaction.
Results A marginally signicant difference (P 0035) was found in the distribu-
tion of ACE I/D genotype frequencies between patients with psoriasis and con-
trols. The frequency of the II genotype in patients with psoriasis was signicantly
higher than that in the control group (551% vs. 467%, respectively, P 0015).
Although the I allele frequency in patients with psoriasis (724%) was higher than
that in the control group (682%), the difference was not signicantly different
(P 0062). After adjusting for age and gender, carriers of the II genotype were
145 (95% condence interval 109192) times more likely than noncarriers to
have psoriasis (P 0010).
Conclusions Our results suggest that the presence of the I allele may confer sus-
ceptibility to development of psoriasis among ethnically Chinese Taiwanese
individuals.
Psoriatic lesions are characterized by skin induration, scaling
and erythema accompanied by histological evidence of inam-
mation, abnormal keratinocyte proliferation/terminal differen-
tiation, and dermal angiogenesis. The inammatory inltrate,
particularly pronounced at the dermal-epidermal junction,
consists largely of activated T cells and antigen-presenting cells
and precedes the development of epidermal hyperprolifera-
tion. Increased levels of inammatory cytokines are detectable
in the lesional psoriatic epidermis, which may result in the
potentiation of T-cell activation
1
as well as hyperproliferation
and accelerated differentiation of keratinocytes.
2
Although the
multifactorial aetiology of psoriasis is well established, family
and twin studies indicate a strong genetic component.
3
Angiotensin I-converting enzyme (ACE), or kininase II, is a
dipeptidyl carboxypeptidase that has a crucial role in blood
pressure regulation and electrolyte balance by hydrolysing
angiotensin I into angiotensin II, a potent vasopressor, and
aldosterone-stimulating peptide.
4
This enzyme also inactivates
bradykinin, a potent mediator capable of promoting symp-
toms of inammation, including vasodilation, plasma extra-
vasation and pain, by activating bradykinin receptors.
5
ACE is
expressed in many tissues, including vascular endothelial cells,
renal epithelial cells, and skin and immune system cells.
69
Although ACE has primarily been studied in the context of its
role in blood pressure regulation, this widely distributed
enzyme has many physiological functions. ACE and its related
substrates or products are known to have wide-ranging effects
on cutaneous immune and inammatory responses.
10,11
Fur-
thermore, treatments with ACE inhibitors have been reported
to induce or aggravate psoriasis manifestations.
12,13
An inser-
tion/deletion (I/D) polymorphism of a 287-base pair repetit-
ive sequence in intron 16 of the ACE gene accounts for a
substantial proportion of the variation of serum ACE activity.
14
The ACE genotype is considered to be associated with various
642 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp642645
cardiovascular diseases, diabetic nephropathy, Alzheimers dis-
ease and autoimmune diseases.
1518
It was recently reported
that the genotype was associated with susceptibility to familial
psoriasis in a Turkish population.
19
Therefore, this study
attempted to conrm these results for a Chinese population.
Materials and methods
Study population
In total, 312 patients with psoriasis and 615 control subjects
were enrolled in the study. Patients with psoriasis were diag-
nosed by clinical and/or histopathological ndings. Patients
were considered to have early onset psoriasis if disease onset
was at any age younger than 40 years (n 191) and late
onset psoriasis if age at onset was after their fortieth birthday.
Control subjects were recruited during routine health exami-
nations and had no clinical evidence of psoriasis. The study
protocol was approved by the hospital ethics committee, and
informed consent was obtained from all subjects.
Genomic DNA extraction and genotyping of the
angiotensin I-converting enzyme gene insertion/deletion
polymorphism
Genomic DNA of patients and controls was isolated from oral
epithelial cells and peripheral blood leucocytes, respectively,
by the standard method using proteinase K digestion of nuclei.
The D and I alleles were identied based on polymerase chain
reaction amplication of the respective segments from intron
16 of the ACE gene as described previously.
20
Statistical analysis
Clinical characteristics of continuous variables are expressed as
mean SD, and were tested using a two-sample t-test. The v
2
test was used to examine the differences in categorical varia-
bles and to compare the allelic and genotype frequencies.
Binary logistic regression analysis was used to evaluate the
independent effect of investigated genotypes on risk for psor-
iasis, after adjusting for age and gender.
Results
In total, 312 patients with psoriasis (235 men, mean SD
age 502 165 years; 77 women, mean SD age 451
191 years) and 615 control subjects (330 men, mean SD
age 451 105 years; 285 women, mean SD age
469 102 years) were enrolled. Table 1 presents allele and
genotype frequencies in patients with psoriasis and control
subjects. No signicant deviation from HardyWeinberg equi-
librium was detected for the ACE I/D polymorphism in either
patients with psoriasis or controls.
Among the 615 controls, the D allele frequency of ACE
gene was 318% and was consistent with ndings obtained in
our previous work.
21
A signicant difference was observed in
the ACE I/D genotype distribution between patients with
psoriasis and controls (P 0035) (Table 1). The frequency
of the II genotype in patients with psoriasis was signicantly
higher than that in the control group (551% vs. 467%,
respectively, P 0015). Although the ACE I allele frequency
in patients (724%) was higher than that in the control group
(682%), the difference did not reach statistical signicance
(P 0062) (Table 1). After adjusting for age and gender, the
ACE II carriers remained signicantly associated with increased
risk of psoriasis (odds ratio 145, 95% condence interval
109192; P 0010). Furthermore, when a comparison was
made between the subgroups of time of disease onset among
patients with psoriasis, no difference was observed for age at
onset in frequencies of ACE alleles and genotypes (Table 1).
Notably, an over-representation of the II genotype was still
observed for early onset and late onset psoriasis subgroups in
comparison with that for the control group (P 0045 and
0080, respectively) (Table 1).
Discussion
This study analysed the association between the ACE gene I/D
polymorphism and the susceptibility for psoriasis in an ethnic-
ally Chinese population in Taiwan. This casecontrol study
demonstrated that the ACE gene II genotype was signicantly
over-represented in patients with psoriasis, as compared with
that in the control group. Thus, it appears that the ACE gene
Table 1 Allele and genotype frequencies of the insertion/deletion (I/D) polymorphism of the angiotensin I-converting enzyme (ACE) gene in the
study population
ACE genotypes
P-value P-value
a
ACE alleles
P-value II (%) ID (%) DD (%) I % D %
Controls 287 (467) 265 (431) 63 (102) 682 318
Psoriasis 172 (551) 108 (346) 32 (103) 0035 0015 724 276 0062
Psoriasis/onset < 40 years 105 (550) 63 (330) 23 (120) 0046 0045 715 285 0230
Psoriasis/onset 40 years 67 (554) 45 (372) 9 (74) 0198 0080 740 260 0076
All P-values are vs. controls.
a
P-value indicates II vs. ID + DD.
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp642645
I/D polymorphism of the ACE gene, Y-C. Chang et al. 643
I/D polymorphism may contribute to the genetic background
of psoriasis.
Genetic factors play an important role in the manifestation
of psoriasis. Genome-wide linkage analysis identied several
susceptible regions across the genome inuencing susceptibil-
ity for psoriasis.
3
Previous reports also showed evidence that
different psoriasis subtypes characterized by early and late
disease onset differ in their genetic background. Gender may
also inuence the presence of genetic association in psoria-
sis.
3
Thus, the genetic basis of psoriasis is complex and prob-
ably reects the actions of a number of genes. Ozkur et al.
reported recently that the ACE II genotype was signicantly
overexpressed in patients with familial psoriasis compared
with those with sporadic psoriasis in a Turkish population
despite no signicant difference in ACE I/D genotype and
allele distributions between patients with psoriasis and con-
trols.
19
Similar to their ndings, this study found that ACE II
carriers have a higher risk for psoriasis than ID and DD carri-
ers. Moreover, these differences remained signicant after
adjusting for gender and age. Although the sample size in
this study is substantially larger than that in the study of
Ozkur et al., the association of ACE I allele with psoriasis
remains marginally signicant. Additionally, both studies have
suspect validity when Bonferroni correction is stringently
applied for multiple tests. Therefore, a larger study than this
would be necessary to assess the signicance of this poly-
morphism accurately. Further analysis of patients with psoria-
sis showed that ACE I/D was not associated with age at
onset. However, the difference of II genotype frequency
between patients with psoriasis and controls was more statis-
tically signicant in the early-onset subgroup compared with
that for the late-onset subgroup. Thus, it appears that the
ACE I/D polymorphism may further predispose the disease
manifestation in this population, and that ACE may act as a
modier gene modulating certain aspects of the disease such
as age at onset.
ACE is expressed by various human skin components,
including vascular endothelial cells, broblasts and keratino-
cytes.
6,8
Administration of ACE inhibitors can induce or
exacerbate psoriasis in clinical practice.
12,13
Many studies
demonstrated that tissue ACE can control the cutaneous
inammatory response by degrading the bradykinin and sub-
stance P, both of which are strong mediators of inamma-
tion.
10,11
Moreover, activation of the kallikreinkinin system in
plasma and tissue has also been associated with psoriasis.
2224
Family studies have suggested that approximately 50% of the
interindividual variability of plasma ACE is attributable to I/D
polymorphism.
14
Plasma and tissue ACE concentrations have
been found to be related to the D allele of the I/D polymorph-
ism, with DD genotypes having the highest and II genotypes
having the lowest ACE activity.
25
Taken together, our data sug-
gest that the ACE II genotype reduces ACE activity in skin and
may prolong or augment activation of the kallikreinkinin
system, thereby increasing the risk for psoriasis. A limitation
of this study is its lack of information on distribution of hyper-
tension among genotypes for patients with psoriasis; therefore,
the possibility of a false-positive association due to potential
stratication of psoriasis with hypertension cannot be excluded.
Nevertheless, the ACE I/D polymorphism was not signicantly
associated with hypertension in the control population (data not
shown), and the DD rather than the II genotype is known to be
associated with hypertension.
15
In conclusion, this casecontrol study extended the results
for a Turkish population and found an association between
ACE I/D polymorphism and psoriasis in an ethnically Chinese
population in Taiwan. Our results suggest that the ACE gene
may be a genetic factor contributing to susceptibility for psor-
iasis. Further studies are needed to examine the role of this
variant on therapeutic response and prognosis for psoriasis.
References
1 Chang EY, Hammerberg C, Fisher G et al. T-cell activation is poten-
tiated by cytokines released by lesional psoriatic, but not normal,
epidermis. Arch Dermatol 1992; 128:147985.
2 Bata-Csorgo Z, Hammerberg C, Voorhees JJ et al. Kinetics and regula-
tion of human keratinocyte stem cell growth in short-term primary
ex vivo culture. Cooperative growth factors from psoriatic lesional
T lymphocytes stimulate proliferation among psoriatic uninvolved,
but not normal, stem keratinocytes. J Clin Invest 1995; 95:31727.
3 Henseler T. The genetics of psoriasis. J Am Acad Dermatol 1997;
37:S111.
4 Hooper NM. Angiotensin converting enzyme: implications from
molecular biology for its physiological functions. Int J Biochem
1991; 23:6417.
5 Bhoola KD, Figueroa CD, Worthy K. Bioregulation of kinins: kallik-
reins, kininogens, and kininases. Pharmacol Rev 1992; 44:180.
6 Noveral JP, Mueller SN, Levine EM. Release of angiotensin I-
converting enzyme by endothelial cells in vitro. J Cell Physiol 1987;
131:15.
7 Hall ER, Kato J, Erdos EG et al. Angiotensin i-converting enzyme in
the nephron. Life Sci 1976; 18:1299303.
8 Smallridge RC, Gamblin GT, Eil C. Angiotensin-converting enzyme:
characteristics in human skin broblasts. Metabolism 1986; 35:899
904.
9 Petrov V, Fagard R, Lijnen P. Effect of protease inhibitors on
angiotensin-converting enzyme activity in human T-lymphocytes.
Am J Hypertens 2000; 13:5359.
10 Scholzen T, Armstrong CA, Bunnett NW et al. Neuropeptides in the
skin: interactions between the neuroendocrine and the skin
immune systems. Exp Dermatol 1998; 7:8196.
11 Scholzen TE, Stander S, Riemann H et al. Modulation of cutaneous
inammation by angiotensin-converting enzyme. J Immunol 2003;
170:386673.
12 Coulter DM, Pillans PI. Angiotensin-converting enzyme inhibitors
and psoriasis. N Z Med J 1993; 106:3923.
13 Wolf R, Tamir A, Brenner S. Psoriasis related to angiotensin-
converting enzyme inhibitors. Dermatologica 1990; 181:513.
14 Rigat B, Hubert C, Alhenc-Gelas F et al. An insertion/deletion poly-
morphism in the angiotensin I-converting enzyme gene accounting
for half the variance of serum enzyme levels. J Clin Invest 1990;
86:13436.
15 Abbud ZA, Wilson AC, Cosgrove NM et al. Angiotensin-converting
enzyme gene polymorphism in systemic hypertension. Am J Cardiol
1998; 81:2446.
16 Ledru F, Blanchard D, Battaglia S et al. Relation between severity of
coronary artery disease, left ventricular function and myocardial
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp642645
644 I/D polymorphism of the ACE gene, Y-C. Chang et al.
infarction, and inuence of the ACE I/D gene polymorphism. Am J
Cardiol 1998; 82:1605.
17 Vleming LJ, van der Pijl JW, Lemkes HH et al. The DD genotype of
the ACE gene polymorphism is associated with progression of dia-
betic nephropathy to end stage renal failure in IDDM. Clin Nephrol
1999; 51:13340.
18 Hu J, Miyatake F, Aizu Y et al. Angiotensin-converting enzyme
genotype is associated with Alzheimer disease in the Japanese
population. Neurosci Lett 1999; 277:657.
19 Ozkur M, Erbagci Z, Nacak M et al. Association of insertion/dele-
tion polymorphism of the angiotensin-converting enzyme gene
with psoriasis. Br J Dermatol 2004; 151:7925.
20 Lindpaintner K, Pfeffer MA, Kreutz R et al. A prospective evaluation
of an angiotensin-converting-enzyme gene polymorphism and the
risk of ischemic heart disease. N Engl J Med 1995; 332:70611.
21 Ko YL, Ko YS, Wang SM et al. Angiotensinogen and angiotensin-I
converting enzyme gene polymorphisms and the risk of coronary
artery disease in Chinese. Hum Genet 1997; 100:21014.
22 Wolf R, Machtey I, Feverman EJ et al. The kallikreinkinin path-
way in psoriasis. Preliminary observations. Biomedicine 1981; 35:
778.
23 Winkelmann RK. Total plasma kininogen in psoriasis and atopic
dermatitis. Acta Derm Venereol (Stockh) 1984; 64:2613.
24 Poblete MT, Reynolds NJ, Figueroa CD et al. Tissue kallikrein and
kininogen in human sweat glands and psoriatic skin. Br J Dermatol
1991; 124:23641.
25 Costerousse O, Allegrini J, Lopez M et al. Angiotensin I-converting
enzyme in human circulating mononuclear cells: genetic poly-
morphism of expression in T-lymphocytes. Biochem J 1993;
290:3340.
2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp642645
I/D polymorphism of the ACE gene, Y-C. Chang et al. 645
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07731. x
Association analysis of IL19, IL20 and IL24 genes in
palmoplantar pustulosis
K. Kingo,* R. Mossner, S. Koks, R. Ratsep, U. Kruger, E. Vasar, K. Reich and H. Silm*
*Department of Dermatology and Venereology, University of Tartu, Tartu, Estonia
Centre of Molecular and Clinical Medicine, University of Tartu, Tartu, Estonia
Department of Dermatology, Georg-August-University, Gottingen, Germany
Department of Physiology, University of Tartu, 19 Ravila Street, 50411 Tartu, Estonia
Correspondence
Sulev Koks.
E-mail: Sulev.Koks@ut.ee
Accepted for publication
27 September 2006
Key words
haplotype, interleukin-19, palmoplantar,
polymorphism, psoriasis, pustulosis
Conicts of interest
None declared.
Summary
Background Interleukin (IL) 19, IL-20 and IL-24 belong to the IL-10 cytokine fam-
ily and have been identied to play a role in the regulation of epidermal func-
tions and in inammation. The genes encoding IL-19, IL-20 and IL-24 are
located within a gene cluster on chromosome 1q3132 and carry frequent gen-
etic variations.
Objectives This study investigated whether variations in the IL19, IL20 and IL24
genes that have previously been associated with plaque-type psoriasis may also
play a role in palmoplantar pustulosis (PPP).
Patients Fifteen polymorphisms were analysed in 43 patients with PPP and in 149
healthy control subjects.
Results The rare allele of IL20 1380 AG (rs2981573) was less frequent in
patients with PPP compared with healthy controls (OR 195, 95% CI 100
379). Haplotype analyses of IL19 and IL20 suggested an increased risk for PPP
associated with IL20 haplotype GAA (OR 239, 95% CI 117486) and a
reduced risk for PPP associated both with IL19 haplotype GATGATA (OR 041,
95% CI 016105) and IL20 haplotype GGG (OR 048, 95% CI 023098).
Extended haplotype analysis revealed an association of IL19/IL20 haplotype
GACACCGGAA with a higher risk for PPP (OR 231, 95% CI 105510) and of
IL20/IL24 haplotype CAAAC with a reduced risk for PPP (OR 012, 95% CI
002082).
Conclusions This exploratory study supports the hypothesis that variations of genes
of the IL-19 subfamily of cytokines inuence susceptibility to PPP. However, due
to the limited size of the study samples, this current concept should be consid-
ered as preliminary and the results need to be conrmed in future independent
studies.
Palmoplantar pustulosis (PPP) is a chronic inammatory skin
disorder in which erythematous, scaly plaques with sterile
pustules develop on palms and soles. There are several simi-
larities between PPP and plaque-type psoriasis. Both diseases
present with sharply delineated scaly and inammatory pla-
ques that are characterized histopathologically by epidermal
hyper- and parakeratosis and the sterile accumulation of
neutrophils. A cytokine imbalance with increased levels of
pro-inammatory cytokines such as interleukin (IL) 6, inter-
feron (IFN) c and tumour necrosis factor (TNF) a is regar-
ded as an important pathophysiological element in both
diseases.
1
Despite these similarities the relationship between PPP and
plaque-type psoriasis is still controversial. Up to 24% of
patients with PPP concomitantly suffer from plaque-type pso-
riasis.
2,3
However, until now, no common genetic back-
ground of plaque-type psoriasis and PPP has been conrmed.
PSORS1, the major susceptibility locus for plaque-type psoriasis
located on 6p21, was not linked with PPP in a recent study.
4
Of several other genetic variations that have been reported to
be associated with plaque-type psoriasis including polymor-
phisms of the genes encoding TNF-a, TNF-b, IL-1b,
57
only
the NcoI polymorphism of the LTA (formerly TNFB) gene was
also associated with PPP in a Japanese population.
8
2007 The Authors
646 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
The cytokines IL-19, IL-20 and IL-24 have recently been
identied as part of the IL-10 family.
9
According to current
concepts, the IL-10 family can be divided into two sub-
families of more closely related ligands: the IL-10 subfamily
and the IL-19 subfamily. The IL-10 subfamily contains IL-
10, IL-22 and IL-26, while the IL-19 subfamily contains IL-
19, IL-20 and IL-24.
10
The members of the IL-19 subfamily
display a signicant amino acid homology and all bind to
the IL-20 receptor beta chain,
1012
indicating that they may
share the same receptor complex (IL20R type I, composed
of IL-20Ra and IL-20Rb subunits) and that their biological
activities could be partially overlapping. A role for the IL-19
subfamily of cytokines in psoriasis is suggested by
observations indicating that they (i) play a major role in
the regulation of epidermal functions, (ii) participate in the
induction of pro-inammatory cytokines such as IL-6
and TNF-a that are elevated in psoriasis and (iii) are excess-
ively expressed in lesional psoriasis compared with nor-
mal skin. Furthermore, transgenic mice that overexpress
IL-20 develop an epidermal phenotype similar to human
psoriasis.
13
The genes IL19, IL20 and IL24 together with IL10 are clus-
tered in a 200 kb region on chromosome 1q3132.
9
The
inuence of polymorphisms of IL19, IL20 and IL24 on gene
expression is unknown at present. However, biological
relevance is suggested by an association of two IL19/IL20
haplotypes with clearance of the hepatitis C virus (HCV) in
African-Americans.
14
Recently, we described an association of variations of genes
of the IL-19 subfamily with susceptibility to plaque-type pso-
riasis.
1517
In the light of the similarities between plaque-type
psoriasis and PPP, the present case-control study was conduc-
ted to test the hypothesis that these polymorphisms also inu-
ence the risk of PPP and that variations of the IL19 subfamily
members, therefore, constitute a common genetic element of
plaque-type psoriasis and PPP.
Materials and methods
Ethical considerations
The study was approved by the Ethics Review Committee on
Human Research of the University of Tartu and written
informed consent was obtained from all participants.
Characteristics of study participants
Unrelated Caucasian patients living in Estonia with a clear
clinical diagnosis of PPP (n 43, 35 female, 8 male, age
range 2675 years, mean age of onset of PPP 478 years)
were enrolled at the Department of Dermatology, University
of Tartu, Estonia. The diagnosis of PPP was made on the
basis of the following criteria: (i) symmetrical erythema and
inltration with pustules and scaling on the palms and/or
soles; (ii) no lesions of eczema or psoriasis on any other
part of the body. The control subjects were 149 healthy
unrelated Caucasians (92 female, 57 male, age range 18
71 years) without a personal or family history of psoriasis,
recruited at the University of Tartu from among medical stu-
dents, healthcare personnel and patients who had presented
at the dermatological outpatient clinic with mild facial telan-
giectasia or skin tags.
Table 1 Description of single nucleotide polymorphisms (SNPs) in the IL19, IL20 and IL24 genes used in current study
Gene SNP ID
Position from
ATG Alleles
Minor allele
frequency
in controls (%)
Minor allele
frequency
in cases (%)
Allelic
P-value OR (95% CI)
IL19 rs2243158 35402 GC 101 116 068 085 (040182)
rs2243168 37149 AT 87 81 086 108 (045258)
rs2073186 38386 CT 268 198 018 149 (083268)
rs2243174 39245 AG 232 174 026 143 (077265)
rs2243188 42232 CA 258 198 025 141 (078255)
rs2243191 43717 CT 258 186 017 152 (084278)
rs2243193 43985 GA 268 186 012 161 (088293)
IL20 rs2981572 )1053 TG 297 291 091 103 (061175)
rs2981573 1380 AG 240 140 0047* 195 (100379)
rs2232360 1462 AG 247 151 0062 184 (096351)
rs1518108 3978 TC 456 465 0882 096 (060156)
IL24 rs3762344 )2506 GA 483 442 0221 118 (073191)
rs1150253 418 AG 423 500 0204 073 (045118)
rs1150256 1956 AG 483 430 0157 124 (076201)
rs1150258 3728 CT 487 430 0174 126 (077204)
OR, odds ratio; CI, condence interval.
Results of association analysis of the genes IL19, IL20 and IL24 in palmoplantar pustulosis (PPP) patients are also indicated. Allelic P-values
were calculated using the v
2
test.
*P-value < 005 allelic differences compared with the controls.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al. 647
Preparation of genomic DNA and analysis of IL19, IL20
and IL24 polymorphisms
Genomic DNA was extracted from whole blood and the SNPs
of the IL19, IL20 and IL24 genes were analysed by the tetra-
primer ARMS-PCR method as described previously.
1517
Statistical analysis
Single marker association analysis and multimarker haplotype
association tests of individuals were performed using the
Haploview program.
18
Allele frequencies were investigated
using the v
2
test. To evaluate deviation from the HardyWein-
berg equilibrium, observed and expected genotype frequencies
were compared using Fishers exact test in the two groups
(cases and controls). For determining haplotype-based associa-
tions an accelerated expectation-maximization (EM) algorithm
similar to the partition/ligation method described by Qin
et al.
19
was used. The haplotype association test was performed
on the set of blocks selected from the linkage disequilibrium.
Pairwise linkage disequilibrium was estimated by a log-linear
model. The extent of disequilibrium was demonstrated by the
standardized D characteristic. Additionally, a value of multi-
allelic D that represents the level of recombination between
the two blocks was calculated. Haplotype analysis was
performed only for the haplotypes with a frequency of 2%.
The intention of this preliminary study was to generate a
hypothesis that may be worth testing in future investigations.
Differences between patients with PPP and healthy control
subjects were tested on an exploratory basis with a signi-
cance level set to 005.
Results
Fifteen single nucleotide polymorphisms (SNPs) of the IL19,
IL20 and IL24 genes were analysed in 43 Estonian patients
with PPP and 149 healthy control subjects. SNPs were inclu-
ded on the basis of a minor allele frequency > 5% as observed
in earlier studies in a cohort of healthy Caucasians living in
Estonia (Table 1).
1517
Genotype frequencies of these polymorphisms did not devi-
ate signicantly from the HardyWeinberg equilibrium in
patients with PPP and control subjects. Allele frequencies of
the 15 polymorphic loci investigated were similar in patients
with PPP and healthy control subjects with the exception of
the IL20 1380 AG (rs2981573) polymorphism. The rare G
allele of this polymorphism was less frequent in patients with
PPP compared with the healthy control group (allele fre-
quency 014 vs. 024; P 0047).
Haplotype analysis of the IL19, IL20, IL24 genes was per-
formed according to the pairwise linkage disequilibrium pat-
tern observed within each of these genes. There was strong
linkage disequilibrium (|D| 077098) between all studied
polymorphisms within the IL19 gene and within the IL24 gene.
There was also a high degree of linkage disequilibrium
between the 1053 TG (rs2981572), the 1380 AG
T
a
b
l
e
2
C
o
m
m
o
n
h
a
p
l
o
t
y
p
e
s
w
i
t
h
a
f
r
e
q
u
e
n
c
y
2
%
,
f
o
r
m
e
d
b
y
s
i
n
g
l
e
n
u
c
l
e
o
t
i
d
e
p
o
l
y
m
o
r
p
h
i
s
m
s
(
S
N
P
s
)
i
n
I
L
1
9
,
I
L
2
0
a
n
d
I
L
2
4
g
e
n
e
s
i
n
t
h
e
p
o
o
l
e
d
s
a
m
p
l
e
s
I
L
1
9
I
L
2
0
I
L
2
4
r
s
2
2
4
3
1
5
8
r
s
2
2
4
3
1
5
8
r
s
2
0
7
3
1
8
6
r
s
2
2
4
3
1
7
4
r
s
2
2
4
3
1
8
8
r
s
2
2
4
3
1
9
1
*
r
s
2
2
4
3
1
9
3
F
r
e
q
u
e
n
c
i
e
s
o
f
h
a
p
l
o
t
y
p
e
(
%
)
r
s
2
9
8
1
5
7
2
r
s
2
9
8
2
5
7
3
r
s
2
2
3
2
3
6
0
F
r
e
q
u
e
n
c
i
e
s
o
f
h
a
p
l
o
t
y
p
e
(
%
)
r
s
3
7
6
2
3
4
4
r
s
1
1
5
0
2
5
3
r
s
1
1
5
0
2
5
6
r
s
1
1
5
0
2
5
8
*
F
r
e
q
u
e
n
c
i
e
s
o
f
h
a
p
l
o
t
y
p
e
(
%
)
G
A
C
A
C
C
G
7
2
4
T
A
A
6
7
5
A
A
A
C
4
7
2
G
A
T
G
A
T
A
1
2
1
G
G
G
1
9
2
G
G
G
T
4
1
5
C
T
T
G
A
T
A
6
5
G
A
A
9
7
G
A
G
T
8
0
T
G
G
2
3
D
9
2
D
0
7
T
h
e
e
x
t
e
n
t
o
f
l
i
n
k
a
g
e
d
i
s
e
q
u
i
l
i
b
r
i
u
m
b
e
t
w
e
e
n
I
L
1
9
,
I
L
2
0
a
n
d
I
L
2
4
g
e
n
e
s
,
e
x
p
r
e
s
s
e
d
i
n
t
e
r
m
s
o
f
H
e
d
r
i
c
k
s
m
u
l
t
i
-
a
l
l
e
l
i
c
D
c
h
a
r
a
c
t
e
r
i
s
t
i
c
i
s
d
e
m
o
n
s
t
r
a
t
e
d
.
*
N
o
n
s
y
n
o
n
y
m
o
u
s
p
o
l
y
m
o
r
p
h
i
s
m
s
.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
648 Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al.
(rs2981573), and the 1462 AG (rs2232360) polymor-
phisms of the IL20 gene. However, there appeared to be a
breakdown of linkage disequilibrium between each of these
polymorphisms and the 3978 TC (rs1518108) polymorph-
ism of the IL20 gene (|D| 002016). This polymorphism
was, therefore, excluded from the further haplotype analysis.
Three common IL19 haplotypes, four common IL20 haplo-
types and three common IL24 haplotypes with an estimated
frequency 2% were identied in the pooled group of study
participants (Table 2). These common haplotypes comprised
910% of all IL19 haplotypes, 987% of all IL20 haplotypes and
967% of all IL24 haplotypes, respectively.
Haplotype analysis revealed a signicantly higher frequency
of IL20 haplotype GAA in patients with PPP than in healthy
individuals (0166 vs. 0077; P 0014, OR 239, 95% CI
117486; Table 3), whereas the IL20 haplotype GGG was less
frequent in the PPP compared with the control group (0115
vs. 0214; P 0039, OR 048, 95% CI 023098). A lower
frequency of the IL19 haplotype GATGATA was observed in
patients with PPP compared with control subjects (0062 vs.
0138), but the difference was only of borderline signicance
(P 0057, OR 041, 95% CI 016105; Table 3). Frequen-
cies of the major IL24 haplotypes were similar between the
investigated groups.
An extended haplotype analysis of the IL19, IL20, and IL24
genes was performed on the basis of the pairwise linkage dis-
equilibrium pattern between the three studied genes (Table 4).
Analysis revealed the existence of two haplotype blocks with
a recombination site between IL20 SNPs rs2232360 and
rs1518108 on human chromosome 1q32. Similar haplotype
blocks have already been identied in an earlier study inclu-
ding patients with plaque-type psoriasis.
17
There were four
common haplotypes in block 1 and ve common haplotypes
in block 2. The common haplotypes in block 1 and in block 2
accounted for approximately 87% and 95% of all haplotypes
among the study participants, respectively (Table 4).
A higher frequency of the extended IL19/IL20 haplotype
GACACCGGAA was found in the PPP group compared with
the control group (0129 vs. 0060; P 004, OR 231, 95%
CI 105510; Table 5). In contrast, the extended IL20/IL24
haplotype CAAAC was less frequent among patients with PPP
than among healthy individuals (0012 vs. 0097; P 00096,
OR 012, 95% CI 002082). Furthermore, the extended
IL20/IL24 haplotype CGGGT was more common in the PPP
group than in the control group (0395 vs. 0280; P 0041,
OR 168, 95% CI 102278).
Discussion
The present report intended to collect the rst information on
the possible role of polymorphisms of genes belonging to the
IL-19 family of cytokines as genetic factors in palmoplantar
pustulosis. The study investigated 15 polymorphisms within
the IL19, IL20 and IL24 genes including two nonsynonymous
polymorphisms [IL19 43717 CT (rs2243191) and IL24
3728 CT (rs1150258)].
No associations between SNPs in the IL19 and IL24 genes
and PPP were found, but the rare allele of the IL20 1380
AG (rs2981573) SNP was less frequent in patients with PPP
than in healthy control subjects. In the haplotype analyses per-
formed, there was evidence that the IL20 haplotype GAA is
associated with an increased (OR 239, 95% CI 117486)
and the IL20 haplotype GGG with a decreased susceptibility
for PPP (OR 048, 95% CI 023098). In these haplotypes,
the IL20 1380 AG (rs2981573) SNP is in the middle posi-
tion, however, it is not possible to discriminate whether the
IL20 SNP 1380 AG (rs2981573) itself or another relevant
variation in linkage disequilibrium with this polymorphism is
Table 3 Results of haplotype analysis of the
IL19, IL20 and IL24 genes
Controls
(n 149)
PPP patients
(n 43) P-value OR (95% CI)
IL19 haplotypes
GACACCG 705 791 0116 158 (089282)
GATGATA 138 62 0057 041 (016105)
CTTGATA 67 58 0766 086 (031236)
IL20 haplotypes
TAA 673 683 0868 104 (062175)
GGG 214 115 0039* 048 (023098)
GAA 77 166 0014* 239 (117486)
TGG 22 25 0894 110 (023528)
IL24 haplotypes
AAAC 485 429 0357 080 (049130)
GGGT 394 487 0125 146 (090236)
GAGT 82 71 0744 085 (0340214)
OR, odds ratio; CIs, condence interval.
The haplotype frequencies (%) and haplotypic ORs with their 95% CI and P-values in
palmoplantar pustulosis (PPP) patients compared with controls are indicated. Haplotype-
phenotype associations were estimated using an expectation-maximization (EM) algorithm.
*P-value < 005 haplotypic differences compared with the controls.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al. 649
responsible for associations of IL20 haplotypes with PPP. Inter-
estingly, the IL20 haplotype GAA has also been found to be
associated with plaque-type psoriasis,
15
suggesting that the
IL20 gene cluster might harbour a common genetic factor for
PPP and plaque-type psoriasis. Further studies with large num-
bers of PPP subjects are necessary to verify this hypothesis.
Several studies have demonstrated the role of extended
haplotypes in clusters of cytokine genes for complex traits, an
approach based on the identication of blocks within gene
clusters as derived from linkage disequilibrium analysis.
20,21
This study conrms the existence of two haplotype blocks
with a recombination site in the 3 UTR region of the IL20
gene within chromosome 1q32. The rst haplotype block
includes SNPs of the IL19 and IL20 genes. The second haplo-
type block includes SNP of the IL20 3 UTR region and several
SNPs of the IL24 gene. Similar haplotype blocks spanning the
IL19, IL20 and IL24 genes have also been demonstrated in HCV
infected patients among African-Americans and European-
Americans.
14
Extended haplotype analysis further supported the hypo-
thesis that genes encoding the IL-19 subfamily of cytokines
inuence the risk of PPP. The extended IL19/IL20 haplotype
GACACCGGAA was associated with an increased susceptibility
for PPP (OR 231, 95% CI 105510) while carriers of the
extended IL20/IL24 haplotype CAAAC appeared to have a
smaller risk for PPP (OR 012, 95% CI 002082). A similar
constellation has previously been observed in patients with
plaque-type psoriasis compared with healthy individuals.
1517
Interpretation has to be with caution because of the small
sample size and preliminary character of this study, but it
seems possible that the IL19 gene cluster represents a suscepti-
bility region shared by PPP and plaque-type psoriasis and is
part of the genetic basis underlying the frequent co-existence
of PPP and plaque-type psoriasis.
In the present study, SNPs with a minor allele frequency
> 5% were used for haplotype reconstruction compared with
the earlier study in plaque-type psoriasis where SNPs with a
minor allele frequency < 10% were excluded.
15
This is a poss-
ible explanation why in the present study haplotype IL19/IL20
GACACCGGAA contains two additional SNPs [(IL19 35402
GC (rs2243158) and IL19 37149 AT (rs2243168)] com-
pared with the IL19/IL20 haplotype CACCGGAA in the previ-
ous study. The former longer version of the extended IL19/
IL20 haplotype was associated with PPP in the present study;
the latter shorter version was associated with plaque-type pso-
riasis. To allow a better comparison of the ndings, we also
analysed the shorter version of the IL19/IL20 haplotype CAC-
CGGAA in the present study. The shorter haplotype was like-
wise associated with PPP (OR 221, 95% CI 101483). At
present, the functional consequence of the investigated poly-
morphisms is unclear. In an earlier study, the IL19 rs2243191,
IL20 rs1400986, rs3024517 and rs2232360 polymorphisms
and also two haplotypes in the IL19/IL20 region had an effect
on HCV clearance in African but not European-American
patients with HCV infection.
14
Although most of the SNPs
selected in our study are distinct from those investigated T
a
b
l
e
4
C
o
m
m
o
n
e
x
t
e
n
d
e
d
h
a
p
l
o
t
y
p
e
s
w
i
t
h
a
f
r
e
q
u
e
n
c
y
2
%
,
f
o
r
m
e
d
b
y
s
i
n
g
l
e
n
u
c
l
e
o
t
i
d
e
p
o
l
y
m
o
r
p
h
i
s
m
s
(
S
N
P
s
)
i
n
I
L
1
9
,
I
L
2
0
a
n
d
I
L
2
4
g
e
n
e
s
i
n
t
h
e
p
o
o
l
e
d
s
a
m
p
l
e
s
a
r
e
i
n
d
i
c
a
t
e
d
I
L
1
9
/
2
0
e
x
t
e
n
d
e
d
h
a
p
l
o
t
y
p
e
s
I
L
2
0
/
I
L
2
4
e
x
t
e
n
d
e
d
h
a
p
l
o
t
y
p
e
s
r
s
2
2
4
3
1
5
8
r
s
2
2
4
3
1
5
8
r
s
2
0
7
3
1
8
6
r
s
2
2
4
3
1
7
4
r
s
2
2
4
3
1
8
8
r
s
2
2
4
3
1
9
1
r
s
2
2
4
3
1
9
3
r
s
2
9
8
1
5
7
2
r
s
2
9
8
2
5
7
3
r
s
2
2
3
2
3
6
0
F
r
e
q
u
e
n
c
i
e
s
o
f
h
a
p
l
o
t
y
p
e
(
%
)
r
s
1
5
1
8
1
0
8
r
s
3
7
6
2
3
4
4
r
s
1
1
5
0
2
5
3
r
s
1
1
5
0
2
5
6
r
s
1
1
5
0
2
5
8
F
r
e
q
u
e
n
c
i
e
s
o
f
h
a
p
l
o
t
y
p
e
(
%
)
G
A
C
A
C
C
G
T
A
A
6
4
3
T
A
A
A
C
3
9
4
G
A
T
G
A
T
A
G
G
G
9
3
C
G
G
G
T
3
0
6
G
A
C
A
C
C
G
G
A
A
7
5
T
G
G
G
T
1
0
9
C
T
T
G
A
T
A
G
G
G
5
6
C
A
A
A
C
7
8
C
G
A
G
T
6
5
D
2
0
T
h
e
e
x
t
e
n
t
o
f
l
i
n
k
a
g
e
d
i
s
e
q
u
i
l
i
b
r
i
u
m
b
e
t
w
e
e
n
f
o
r
m
e
d
h
a
p
l
o
t
y
p
e
b
l
o
c
k
s
i
n
a
r
e
g
i
o
n
o
f
I
L
1
9
s
u
b
f
a
m
i
l
y
g
e
n
e
s
i
s
e
x
p
r
e
s
s
e
d
i
n
t
e
r
m
s
o
f
H
e
d
r
i
c
k
s
m
u
l
t
i
-
a
l
l
e
l
i
c
D
c
h
a
r
a
c
t
e
r
i
s
t
i
c
.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
650 Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al.
in the above study, both studies suggest that carriage of
IL19/IL20 extended haplotypes may inuence inammatory
responses.
In this study, we found the rst evidence for an associ-
ation of variations of the IL-19 gene family with PPP. Similar
ndings have previously been reported in psoriasis vulgaris.
In contrast, genome-wide scans have so far failed to demon-
strate linkage of psoriasis vulgaris to the region on chromo-
some 1q3132, the locus that harbours the IL-19 gene
family. However, because linkage analyses compared with
case-control studies are less sensitive, this does not rule out
the association of variations in this region with psoriasis vul-
garis. Until now, no linkage studies have been conducted in
PPP, probably because of the rarity and the late onset of the
disease.
Clearly, the small sample size is also an important limitation
of this study. Signicant P values for the associations were in
the range of 00100047. Because of the exploratory nature
of the investigation, no correction for multiple comparisons
was performed, and the presence of false positive results can-
not be excluded.
In conclusion, our study provides initial evidence that poly-
morphisms of the genes encoding IL-19, IL-20 and IL-24 may
inuence susceptibility to PPP. Genetic variations within the
IL19 gene cluster may affect both plaque-type psoriasis and
PPP. The results obtained in this study encourage conrmation
studies with larger sample sizes. It remains to be seen whether
variations in the IL19, IL20 and IL24 genes confer susceptibility
to other chronic inammatory skin diseases.
Acknowledgments
This study was supported by the target based funding from
the Estonian Ministry of Education grant No. 0182128s02
(TARNH 2128), by University of Tartu research grant PARFS
05901, by the Estonian Science Foundation Grants No. 5712
and 5688 and by the Centre of Molecular and Clinical Medi-
cine Grant VARMC-TIPP.
References
1 Murakata H, Harabuchi Y, Kataura A. Increased interleukin-6,
interferon-gamma and tumour necrosis factor-alpha production by
tonsillar mononuclear cells stimulated with alpha-streptococci in
patients with pustulosis palmaris et plantaris. Acta Otolaryngol 1999;
119:38491.
2 Enfors W, Molin L. Pustulosis palmaris et plantaris. A follow-
up study of a ten-year material. Acta Derm Venereol 1971; 51:289
94.
3 Ashurst PJ. Relapsing pustular eruptions of the hands and feet. Br J
Dermatol 1964; 76:16980.
4 Asumalahti K, Ameen M, Suomela S et al. Genetic analysis of
PSORS1 distinguishes guttate psoriasis and palmoplantar pustulosis.
J Invest Dermatol 2003; 120:62732.
5 Mossner R, Kingo K, Kleensang A et al. Association of TNF-238
and -308 promoter polymorphisms with psoriasis vulgaris and
psoriatic arthritis but not with pustulosis palmoplantaris. J Invest
Dermatol 2005; 124:2824.
6 Reich K, Mossner R, Konig IR et al. Promoter polymorphisms of
the genes encoding tumor necrosis factor-alpha and interleukin-
1beta are associated with different subtypes of psoriasis character-
ized by early and late disease onset. J Invest Dermatol 2002;
118:15563.
7 Vasku V, Vasku A, Izakovicova Holla L et al. Polymorphisms in
inammation genes (angiotensinogen, TAP1 and TNF-beta) in
psoriasis. Arch Dermatol Res 2000; 292:5314.
8 Hashigucci K, Yokoyama M, Niizeki H et al. Polymorphism in the
tumor necrosis factor B gene is associated with Palmoplantar
pustulosis. Tissue Antigens 1999; 54:28890.
9 Fickenscher H, Hor S, Kupers H et al. The interleukin-10 family of
cytokines. Trends Immunol 2002; 23:8996.
10 Gallagher G, Eskdale J, Jordan W et al. Human interleukin-19 and
its receptor: a potential role in the induction of Th2 responses.
Int Immunopharmacol 2004; 4:61526.
Table 5 Results of extended haplotype
analysis of the genes of IL19 subfamily in
patients with palmoplantar pustulosis (PPP)
Controls
(n 149)
PPP patients
(n 43) P-value OR (95% CI)
IL19/IL20 extended haplotypes
GACACCGTAA 643 650 0904 103 (062170)
GATGATAGGG 107 46 0087 041 (014118)
GACACCGGAA 60 129 0035* 231 (105510)
CTTGATAGGG 56 58 0944 105 (037294)
IL20/IL24 extended haplotypes
TAAAC 387 416 0629 113 (069184)
CGGGT 280 395 0041* 168 (102277)
TGGGT 114 92 0556 078 (035177)
CAAAC 97 12 0010* 012 (002082)
CGAGT 67 58 0766 086 (031236)
OR, odds ratio, CI, condence interval.
The haplotype frequencies (%) and haplotypic ORs with their 95% CIs and P-values in PPP
patients compared with controls are indicated. Haplotype frequencies and haplotype-
phenotype associations were estimated using an expectation-maximization (EM) algorithm.
*P-value < 005 haplotypic differences compared with the controls.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al. 651
11 Dumoutier L, Leemans C, Lejeune D et al. Cutting edge: STAT acti-
vation by IL-19, IL-20 and mda-7 through IL-20 receptor com-
plexes of two types. J Immunol 2001; 167:35459.
12 Wang M, Tan Z, Zhang R et al. Interleukin 24 (MDA-7/MOB-5)
signals through two heterodimeric receptors, IL-22R1/IL-20R2 and
IL-20R1/IL-20R2. J Biol Chem 2002; 277:73417.
13 Boniface K, Lecron JC, Bernhard FX et al. Keratinocytes as targets
for interleukin-10-related cytokines: a putative role in the patho-
genesis of psoriasis. Eur Cytokine Netw 2005; 16:30919.
14 Oleksyk TK, Thio CL, Truelove AL et al. Single nucleotide polymor-
phisms and haplotypes in the IL10 region associated with HCV
clearance. Genes Immun 2005; 6:34757.
15 Kingo K, Koks S, Nikopensius T et al. Polymorphisms in the inter-
leukin-20 gene: relationships to plaque-type psoriasis. Genes Immun
2004; 5:11721.
16 Koks S, Kingo K, Ratsep R et al. Combined haplotype analysis of
the interleukin-19 and -20 genes: relationship to plaque-type
psoriasis. Genes Immun 2004; 5:6627.
17 Koks S, Kingo K, Vabrit K et al. Possible relations between the poly-
morphisms of the cytokines IL-19, IL-20 and IL-24 and plaque-
type psoriasis. Genes Immun 2005; 6:40715.
18 Barrett JC, Fry B, Maller J et al. Haploview: analysis and vis-
ualization of LD and haplotype maps. Bioinformatics 2005;
21:2635.
19 Qin ZS, Niu T, Liu JS. Partition-ligation-expectation-maximization
algorithm for haplotype inference with single-nucleotide polymor-
phisms. Am J Hum Genet 2002; 71:12427.
20 Rioux JD, Silverberg MS, Daly MJ et al. Genomewide search
in Canadian families with inammatory bowel disease reveals
two novel susceptibility loci. Am J Hum Genet 2000; 66:1863
70.
21 Haer DA, Jager PL. Opinion: Applying a new generation of genetic
maps to understand human inammatory disease. Nat Rev Immunol
2005; 5:8391.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp646652
652 Association analysis of IL19, IL20 and IL24 genes in palmoplantar pustulosis, K. Kingo et al.
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07724. x
Early increase in serum levels of the angiogenesis-inhibitor
endostatin and of basic broblast growth factor in
melanoma patients during disease progression
P. Kurschat, S. Eming, D. Nashan,* T. Krieg and C. Mauch
Department of Dermatology and Center for Molecular Medicine CMMC, University of Cologne, Josef-Stelzmann-Str. 9, 50924 Cologne, Germany
*Department of Dermatology, University of Freiburg, Germany
Correspondence
Cornelia Mauch.
E-mail: cornelia.mauch@uk-koeln.de
Accepted for publication
13 September 2006
Key words
angiogenesis, endostatin, broblast growth factor,
melanoma progression, tumour marker, vascular
endothelial growth factor
Conicts of interest
None declared.
Summary
Background Increased serum levels of angiogenesis-related factors such as endo-
statin, vascular endothelial cell growth factor (VEGF) or basic broblast growth
factor (bFGF) have been demonstrated for a variety of solid and nonsolid
tumours. Therefore, these factors have been suggested as diagnostic and in some
studies as prognostic tumour markers.
Objectives The purpose of the present study was to investigate a possible correlation
of endostatin, VEGF or bFGF serum levels with disease progression in melanoma.
Especially, we compared these factors to the established melanoma marker S-100
B, which increases in advanced disease but often fails to indicate early metastatic
spread to regional lymph nodes.
Patients and methods Sera from 197 melanoma patients and 35 healthy controls were
measured by enzyme-linked immunosorbent assay; 72 patients had primary
tumours (American Joint Committee on Cancer stages I and II), 55 had regional
lymph node metastasis (stage III) and 70 patients had distant organ metastasis
(stage IV).
Results Endostatin, VEGF and bFGF serum levels were signicantly elevated in stage
IV disease, compared with the control group. In stage III, endostatin and bFGF,
but not VEGF or S-100 B, were signicantly increased. However, follow-up of
this patient group did not show a correlation with the future clinical course
including time until progression or overall survival, arguing against a role of
endostatin, VEGF or bFGF as prognostic markers.
Conclusions These data indicate that endostatin or bFGF might be useful as diagnos-
tic markers for the early detection of locoregional metastasis.
Malignant melanoma is an extremely aggressive tumour char-
acterized by the early development of locoregional and distant
organ metastasis. During the last few decades the incidence
has increased signicantly worldwide.
1
If diagnosed early most patients can be cured by surgery,
but once the tumour cells have spread to distant sites of the
body the prognosis is generally poor. If satellite and in-transit
metastases are not taken into account, more than 80% of
patients with tumour progression develop regional lymph
node metastases [clinical stage III; American Joint Committee
on Cancer (AJCC) classication from 2000
2
] prior to haemato-
genous organ metastasis (stage IV disease). Once distant organ
metastases have developed, no curative therapeutic options are
available and the 10-year survival rate drops to an average of
69%.
3
Therefore, the detection of early stage III is important and
is the main goal of clinical tumour follow-up examinations. In
the past decade the measurement of serum S-100 B protein
has been integrated into many follow-up programmes for
high-risk melanoma. However, in more than 80% of patients
with stage III disease S-100 B is measured within the normal
range, and it is not elevated until patients have reached stage
IV disease.
4
Accordingly, tumour markers that could detect the
progression to stage III would be of great value.
The growth of solid primary tumours such as malignant
melanoma as well as their lymph node or distant organ meta-
stases beyond a size of 12 mm is always accompanied by the
process of angiogenesis to provide oxygen and nutrients for the
expanding population of malignant cells. The angiogenetic pro-
cess itself is regulated by a variety of inducing and inhibiting
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658 653
factors, and many of them can be measured in the serum
(see reviews
5,6
). Therefore, these factors have been suggested
to be used as tumour markers. The two best known and most
widely investigated inducers of angiogenesis are the vascular
endothelial growth factor (VEGF) and the basic broblast
growth factor (bFGF). Both have been shown to increase in the
serum during progression of various types of tumours.
Endostatin, a proteolytic fragment of collagen type XVIII,
was rst described as a potent inhibitor of angiogenesis.
7
But
as endostatin is generated in areas of increased extracellular
matrix turnover, which also occurs during angiogenesis, it can
be used as an indicator of blood vessel growth. Increased lev-
els of serum endostatin have been demonstrated for different
types of cancer, such as renal cell carcinoma or nonsmall cell
lung cancer.
8,9
We performed this study to evaluate the potential use of
the angiogenesis-related factors endostatin, VEGF and bFGF as
tumour markers for early detection of stage III (locoregional
lymph node metastasis) or stage IV disease (distant organ
metastasis), especially in comparison to the established tumour
marker S-100 B. Additionally, we investigated whether
increased serum levels of these factors are of prognostic value
to predict time until tumour progression or overall survival.
Patients and methods
Denition and characterization of patient groups
All patients included into this study had histologically con-
rmed cutaneous malignant melanoma, either of the super-
cial spreading (SSM) or the nodular (NMM) type. Patients
were consecutively recruited in a hospital-based approach.
Group 1 (72 patients) consisted of patients with primary
tumours (clinical stage I and II according to the criteria of the
AJCC
2
), the mean tumour thickness (Breslow index) was
148 mm, the SD 09 mm. Group 2 (55 patients) included
cases with histologically veried axillar or groin lymph node
metastases (clinical stage III AJCC). In 43 out of 55 cases these
metastases were detectable by clinical examination, the
remaining 12 cases were suspected by routine sonography.
Because the aim was to investigate angiogenesis-related fac-
tors, microscopic disease with positive sentinel lymph node
was excluded from the study. Group 3 (70 patients) was char-
acterized by distant organ metastasis (stage IV AJCC). All
patients included had metastases in at least one of the follow-
ing locations: lung, liver, spleen, bone, skin, small intestine or
adrenal glands. The control group consisted of 35 healthy vol-
unteers (19 female and 16 male individuals, the median age
was 37 years, 14 years below the patient group).
Collection of blood samples
After obtaining informed consent 10 mL of blood per patient
or volunteer was taken from an antecubital vein using a tour-
niquet. The samples were collected before any treatment or
intervention had been performed. Heparin gel was used as
anticoagulant. Samples were centrifuged at 2000 g for 10 min
and serum was stored at )80 C.
Measurement of endostatin, vascular endothelial cell
growth factor and basic broblast growth factor
Samples were thawed and immediately subjected to measure-
ment by enzyme-linked immunosorbent assay (ELISA). Com-
mercially available ELISA kits for endostatin, VEGF and bFGF
were purchased from Chemicon (ChemiKine competitive EIA
kits Cyt 158, Cyt 132 and Cyt 142, respectively; Temecula,
CA, U.S.A.) and used according to the manufacturers instruc-
tions. Standard curves were constructed using serial dilutions
of recombinant proteins provided by the manufacturer. Opti-
cal densities were quantied by a microtitre plate reader at
490 nm, and all samples were run in duplicate. The minimal
detectable concentrations were 0195 ng mL
)1
for VEGF,
195 ng mL
)1
for endostatin and 0488 ng mL
)1
for bFGF.
Statistical analysis
The statistical analysis was performed using the JMP program
package (SAS Institute Inc., Cary, NC, U.S.A.). The signicance
of difference between the groups was determined by the
Students t-test for unpaired groups, and a P-value < 005 was
considered signicant. A P-value < 001 was considered to be
highly signicant.
Results
S-100 B and vascular endothelial cell growth factor
serum levels in melanoma patients
Patients and healthy controls (for denition and characteriza-
tion of these groups see Patients and methods) were assigned
to four different groups according to stage of disease. As
expected and previously reported in the literature,
3
the
tumour marker S-100 B was not elevated in patients with pri-
mary melanoma when compared with the control group
(Table 1). In stage III disease (regional lymph node metasta-
sis) elevated levels (above 012 lg L
)1
) were detected in 19
out of 55 cases (345%, mean of all patients in stage III
014 lg L
)1
, SD 01 lg L
)1
), whereas S-100 B values above
the reference value of 012 lg L
)1
could be detected in all
70 patients with stage IV disease (mean 114 lg L
)1
, SD
065 lg L
)1
). Although several patients in stage III had
increased S-100 B values, only patients with distant organ
metastases had a statistically highly signicant increase when
compared with the control group (P < 0001).
The results from the VEGF measurement resembled the
S-100 B data (Table 1). When compared with the control
group (mean 192 ng mL
)1
, SD 103 ng mL
)1
), this angio-
genesis-inducing factor was elevated only in patients with
stage IV disease (mean 754 ng mL
)1
, SD 337 ng mL
)1
),
reaching statistical signicance (P < 0001), but not in
patients with stage III disease. A more detailed analysis of the
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658
654 Endostatin in sera of melanoma patients, P. Kurschat et al.
values for the individual patients reveals that elevated VEGF
levels were found only in stage IV disease, whereas no patient
in stage III displayed high serum VEGF (Fig. 1a).
In conclusion, both S-100 B and VEGF were elevated in the
majority of cases in the advanced-stage disease group, but they
were only occasionally and slightly increased in patients with
lymph node metastasis and therefore fail to reliably indicate
early metastatic disease.
Serum levels of basic broblast growth factor and
endostatin
As shown in Table 1, in stage IV disease serum levels of bFGF
(mean 148 ng mL
)1
, SD 70 ng mL
)1
) and endostatin (mean
4275 ng mL
)1
, SD 1241 ng mL
)1
) were both elevated, when
compared with the control group (bFGF: mean 745 ng mL
)1
,
SD 425 ng mL
)1
; endostatin: mean 2086 ng mL
)1
, SD
491 ng mL
)1
). The increase of both parameters reached stat-
istical signicance (P < 0001) when compared with the con-
trol group. Interestingly, signicantly increased values could
also be detected in the majority of patients with lymph node
metastases (stage III, mean 1798 ng mL
)1
, SD 546 ng mL
)1
for bFGF and 3611 ng mL
)1
, SD 1138 ng mL
)1
for endo-
statin; P < 0001 in both cases).
When the values for individual patients are analysed it
becomes obvious that bFGF is inconsistently elevated only in
stage IV disease [29 of 70 patients (414%), Fig. 1b]. Endo-
statin serum levels were found to be increased in 814% (57
of 70) of patients in stage IV (Fig. 1c). In stage III, bFGF was
elevated in 745% (41 of 55) of the cases and endostatin in
691% (38 of 55).
These results indicate that in comparison to S-100 B or
VEGF, both bFGF and endostatin might be elevated even in
cases where the tumour had progressed only into the regional
lymph nodes. Furthermore, clinically detectable lymph node
metastases were accompanied by higher bFGF or endostatin
levels than metastases, which were detectable only by ultra-
sound examination (data not shown).
Comparison of the sensitivity of vascular endothelial cell
growth factor, basic broblast growth factor and
endostatin
From the three investigated angiogenesis-regulating factors,
VEGF had the greatest sensitivity to indicate stage IV disease
(65 of 70, 929%). The specicity was high as well, as only
57% of our control had serum levels above our threshold of
398 ng mL
)1
(mean plus twice the SD). However, in stage III
no patient had elevated VEGF levels. Compared with these
results, bFGF was elevated in 41 of 55 of stage III patients
(745%), but only in 29 of 70 of the cases with distant meta-
stases (414%). Therefore, the combination of VEGF together
with bFGF had a sensitivity to detect advanced disease (stage
IV) in only 414% (29 of 70), which was due to the low sen-
sitivity of bFGF (Fig. 1d). In stage III this combination failed
completely, as no patient had elevated VEGF levels.
Endostatin had a sensitivity of 814% (57 of 70) to detect
stage IV, and it was also increased in 691% of patients with
regional metastatic disease. In stage IV disease, both endostatin
and VEGF were positive in 743% (52 of 70) (Fig. 1e), which
was the best result next to the combination of S-100 B with
VEGF (Fig. 1a). The combination of endostatin and bFGF was
not useful in stage IV, but was the best one in stage III disease
(Fig. 1f). Only 314% (22 of 70) of the patients with distant
metastasis had elevated levels for all three factors.
Correlation of vascular endothelial cell growth factor,
basic broblast growth factor and endostatin serum
levels with patient prognosis
To investigate whether VEGF, bFGF and endostatin could be
used to predict the future clinical development we analysed
each group separately. Within each group (primary tumours,
lymph node and organ metastasis) it was determined for every
patient whether the values of the different factors were meas-
ured in the lower third (V1, F1 or E1), the middle third (V2,
F2 and E2) or the upper third (V3, F3 or E3) of the range.
Therefore, the average relative value within the whole group
is 2 for each individual angiogenesis factor and 6 for the com-
bination of all three factors. If subgroups are formed, values
above 2 (or 6 for the combination) indicate that the levels of
the respective factor(s) are higher in this group.
From the 72 patients with primary melanomas (stages I and
II) ve developed regional or distant metastasis during the fol-
low-up period of 60 months (69%). These ve patients had
no signicantly elevated levels for any of the angiogenesis fac-
tors VEGF, bFGF or endostatin. The relative value of these
patients was 64, compared with 60 for the remaining
patients without recurrent disease.
Among the 55 patients with stage III disease, 19 (345%)
had no recurrent disease during the follow-up time of
60 months. The combined relative value for the factors was
Table 1 Serum levels of S-100 B, vascular
endothelial cell growth factor (VEGF), basic
broblast growth factor (bFGF) and
endostatin in healthy controls and melanoma
patients in different stages of disease
Control Stage I/II Stage III Stage IV
S-100 B 006 003 005 003 014 010 114 065
a
VEGF 192 103 140 093 178 051 754 337
a
bFGF 745 425 669 509 1798 546
a
1480 700
a
Endostatin 2086 491 2338 758 3611 1138
a
4275 1241
a
Values are the mean plus SD. Highly signicantly increased values are indicated:
a
P-value < 001, compared with the control group.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658
Endostatin in sera of melanoma patients, P. Kurschat et al. 655
63 (VEGF: 21; bFGF: 22; endostatin: 195). In contrast to
this subgroup, 36 of the 55 patients (655%) developed regio-
nal or distant organ metastasis. But the levels for the angio-
genesis-related factors were not higher within this subgroup,
compared with the patients with no recurrent disease. The
combined relative value was 59 (VEGF: 19; bFGF: 19;
endostatin: 21). Therefore, neither VEGF nor bFGF or endostatin
serum levels were measured higher or lower in patients who
developed recurrent disease at a later time. Additionally, these
factors did not correlate with the time until progression (the
average time until progression/recurrence was 16 months) or
with the further clinical outcome (within the follow-up time
16 patients of the 36 with recurrent disease died after an aver-
age time of 18 months).
(a) (b)
(c) (d)
(e) (f)
Fig 1. Increase of S-100 B, vascular endothelial cell growth factor (VEGF), basic broblast growth factor (bFGF) and endostatin during melanoma
progression. The plots illustrate the correlation between the serum levels of the various factors. (a) S-100 B and VEGF; (b) S-100 B and bFGF;
(c) S-100 B and endostatin; (d) VEGF and bFGF; (e) endostatin and VEGF; (f) endostatin and bFGF. Each point corresponds to one control person
(m) or patient in stage I/II (n), III (s) or IV (d). Dotted lines indicate the upper limit of the S-100 B reference range or the mean value plus
twice the SD. Values above these lines are considered elevated.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658
656 Endostatin in sera of melanoma patients, P. Kurschat et al.
In stage IV disease all patients except one died after an aver-
age time of 45 months after serum samples were collected (it
should be noted that the time of serum sample collection was
not identical with the time point when stage IV disease was
diagnosed). Again, we could not detect a statistically signi-
cant correlation between serum levels of VEGF, bFGF or
endostatin and the remaining survival time, although there
was a tendency towards a correlation of elevated VEGF levels
with shorter survival times. Therefore, our data indicate that
serum levels of these factors are not suitable to predict the
future clinical development of individual patients with distant
organ metastasis.
Discussion
Because effective therapeutic options are still not available for
advanced stage melanoma, the most powerful means to
decrease mortality from this type of cancer are early detection
and surgical removal of the primary tumour and of limited
lymphatic and solitary organ metastases. The detection of early
stage III disease is difcult to achieve and is the main purpose
of various cancer follow-up programmes. The establishment
of parameters indicating early progression which can be
measured in the patients serum would be of great value. In
melanoma, the comparatively melanoma-specic tumour mar-
ker S-100 B is widely used, but it is elevated in only a minor-
ity of stage III patients.
4
Frequently, increased S-100 B serum
levels indicate a high tumour mass, which in most cases
means distant organ metastasis. Therefore, a tumour marker
indicating early metastatic spread, such as locoregional lymph
node metastases, would be of great value.
As all solid tumours depend on tumour angiogenesis for
their growth, a variety of angiogenesis-regulating factors have
been suggested as tumour markers, although these factors are
generally not specic for any special kind of neoplasia.
9
Over the last 10 years a substantial amount of literature has
accumulated showing increased levels, especially of VEGF and
bFGF, presumably the most important inducers of angiogenesis,
during the progression of various types of cancer, such as breast
carcinoma or colorectal cancer (see reviews
10,11
). Concerning
endostatin, a smaller number of reports is available, and there-
fore the correlation between endostatin and advanced malignant
disease is not that well documented. Nevertheless, there are sev-
eral publications demonstrating elevated endostatin serum levels
during tumour progression.
8,9
As for malignant melanoma, Ugurel et al.
12
reported signi-
cantly increased serum values of VEGF, bFGF, interleukin-8 and
angiogenin in melanoma patients with advanced stage disease.
We were able to conrm these alterations for VEGF and bFGF.
Additionally, we included the angiogenesis inhibitor endostatin
into our investigation, and to our knowledge this is the rst
report for this angiogenesis inhibitor in melanoma patients.
Endostatin is a cleavage product of collagen type XVIII with
direct inhibitory abilities on endothelial cell proliferation and
migration.
7
Therefore, one would expect decreased endostatin
levels during tumour progression. Interestingly, endostatin
levels were rather increased with melanoma progression.
Although the mechanism of endostatin generation from colla-
gen type XVIII has not been elucidated completely, various
proteases such as elastase or cathepsin L have been implicated
in this process.
13,14
As the process of angiogenesis is accom-
panied by intensive remodelling of the extracellular matrix,
especially of the basement membrane around pre-existing or
newly formed blood vessels, the degradative action of various
proteases is likely to lead to increased generation of endostatin
from collagen type XVIII, one of the constituents of basement
membranes. As mentioned before, several other groups have
reported increased levels of endostatin in different types
of cancer such as renal cell carcinoma or nonsmall cell lung
cancer.
8,9
In summary, our results indicate that VEGF and to a lesser
degree endostatin are good markers for advanced metastatic
disease, whereas bFGF is elevated only inconsistently. Never-
theless, neither the combination of the three angiogenesis reg-
ulators nor any of these factors alone seem to be superior to
the established marker S-100 B to detect distant organ meta-
stasis. However, in stage III disease the situation is different.
VEGF or S-100 B are not useful tumour markers to detect
locoregional lymph node metastasis, because both are elevated
only occasionally. In contrast to this, we consider our observa-
tion that in a subgroup of patients endostatin and bFGF might
be elevated already in stage III disease to be of particular inter-
est. During this stage of disease they seem to be superior to
S-100 B and VEGF, which are reliable indicators only for stage
IV disease. Since we performed our study, sentinel lymph
node biopsy has become a standard procedure for melanomas
with a Breslow index of >1 mm. At this point we cannot
answer the question of whether the angiogenic factors endo-
statin and bFGF are already increased in lymph node metastases
measuring just a few millimetres. These tumours cannot be
detected by clinical or ultrasound examination but angiogene-
sis might have already started. If these cases could be detected
in the patients sera this would result in a true benet for the
patients, allowing early diagnosis of stage III disease in cases
where no sentinel lymph node biopsy was performed or where
the biopsy showed a negative result.
When evaluating the potential use of these markers in the
follow-up of tumour patients, several considerations should be
kept in mind. Even in adults the process of angiogenesis is not
specic for malignant growth but rather can be activated in
various physiological and pathological conditions. Basically,
every condition accompanied by general or localized hypoxia
can result in increased levels of angiogenic factors. For exam-
ple, Dunst et al.
15
reported increased VEGF levels in patients
with anaemia, while Asano et al.
16
measured a twofold
increase of the same factor when healthy control persons were
transferred to higher altitudes in the mountains. Furthermore,
pathological conditions with hypoxia were correlated to
increased angiogenesis inducers, in particular in patients with
collagenosis
17
or with ischaemic heart disease.
18
The inuence
of the female cycle is unclear so far, with contradictory
reports.
19,20
All these different inuencing factors strengthen
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658
Endostatin in sera of melanoma patients, P. Kurschat et al. 657
the necessity to thoroughly establish reference values and con-
tribute to the difculty in interpreting elevated levels of angio-
genesis-related factors. It should be noted that despite the fact
that VEGF or bFGF are elevated in many different kinds of
cancer during disease progression these factors have not been
integrated into routine follow-up programmes yet. As for
malignant melanoma, the measurement of S-100 B is recom-
mended for the follow-up of primary tumours with a clinical
stage of Ib or higher in several European countries including
Germany, although a clear benet for patient survival has not
been demonstrated. But the measurement of S-100 B has
reduced the number of chest X-rays and ultrasound examina-
tions of abdominal organs during follow-up.
In stage IV disease a drop of elevated S-100 B levels is
observed frequently following successful therapeutic approa-
ches. Therefore, this marker can be used to monitor therapy.
A decrease of angiogenesis markers following reduction of
tumour mass has been reported for different tumours such as
renal carcinoma or breast cancer.
21
Therefore they might be
suitable to monitor therapy as well.
To answer the question of whether or not VEGF, bFGF or
endostatin could be used as prognostic markers for individual
patients, we investigated whether increased serum levels for
one or more of the different factors were correlated with
the future clinical course. During the follow-up time of
60 months we could not establish a statistically signicant cor-
relation for any stage of the disease. Patients with stage III dis-
ease who developed distant organ metastasis at a later time
had no higher serum levels for angiogenic factors than
patients who had no recurrent disease. Furthermore, high lev-
els of VEGF, bFGF or endostatin were not signicantly correl-
ated with shorter or longer survival times in stage IV disease.
There was only a tendency towards shorter survival times
when VEGF was elevated, but this effect did not reach statistic-
al signicance. The interpretation of these results should be
carried out carefully, as the therapeutic interventions in stage
IV disease are not standardized and our patient groups are not
big enough to allow division into subgroups to eliminate such
differences.
In summary, the present study demonstrates that endostatin
and bFGF might be superior to the established melanoma
tumour marker S-100 B to detect locoregional stage III disease.
This potential use deserves further assessment in a consecutive
study. As sentinel lymph node biopsy has become a routine
staging procedure it will be of particular interest to investigate
whether endostatin and bFGF are already increased in early
lymphatic spread which cannot be detected by clinical or
ultrasound examination.
Acknowledgments
This work has been supported by grants from the Zentrum fur
Molekulare Medizin der Universitat zu Koln (BMFT/IDZ 10,
Grant 01 GB 950/4 to C.M.) and by the Deutsche Forschungs-
gemeinschaft (DFG, Grant KR 558/10-1 to C.M. and K.U.
1497/1-1 to P.K.).
References
1 Garbe C, Blum A. Epidemiology of cutaneous melanoma in Germany
and worldwide. Skin Pharmacol Appl Skin Physiol 2001; 14:28090.
2 Balch CM, Buzaid AC, Atkins MB et al. A new American Joint Com-
mittee on Cancer staging system for cutaneous melanoma. Cancer
2000; 88:148491.
3 Balch CM, Buzaid AC, Soong SJ et al. Final version of the American
Joint Committee on Cancer staging system for cutaneous mela-
noma. J Clin Oncol 2001; 19:363548.
4 Hauschild A, Engel G, Brenner W et al. S100B protein detection in
serum is a signicant prognostic factor in metastatic melanoma.
Oncology 1999; 56:33844.
5 Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch.
Nat Rev Cancer 2003; 3:40110.
6 Huang Z, Bao SD. Roles of main pro- and anti-angiogenic factors
in tumor angiogenesis. World J Gastroenterol 2004; 10:46370.
7 Zatterstrom UK, Felbor U, Fukai N, Olsen BR. Collagen XVIII/
endostatin structure and functional role in angiogenesis. Cell Struct
Funct 2000; 25:97101.
8 Feldman AL, Tamarkin L, Paciotti GF et al. Serum endostatin levels
are elevated and correlate with serum vascular endothelial growth
factor levels in patients with stage IV clear cell renal cancer.
Clin Cancer Res 2000; 6:462834.
9 Suzuki M, Iizasa T, Ko E et al. Serum endostatin correlates with
progression and prognosis of non-small cell lung cancer. Lung Cancer
2002; 35:2934.
10 Kuroi K, Toi M. Circulating angiogenesis regulators in cancer
patients. Int J Biol Markers 2001; 16:526.
11 Szabo S, Sandor Z. The diagnostic and prognostic value of tumor
angiogenesis. Eur J Surg 1998: 582 (Suppl.):99103.
12 Ugurel S, Rappl G, Tilgen W, Reinhold U. Increased serum con-
centration of angiogenic factors in malignant melanoma patients
correlates with tumor progression and survival. J Clin Oncol 2001;
19:57783.
13 Wen W, Moses MA, Wiederschain D et al. The generation of
endostatin is mediated by elastase. Cancer Res 1999; 59:60526.
14 Ferreras M, Felbor U, Lenhard T et al. Generation and degradation
of human endostatin proteins by various proteinases. FEBS Lett
2000; 486:24751.
15 Dunst J, Becker A, Lautenschlager C et al. Anemia and elevated sys-
temic levels of vascular endothelial growth factor (VEGF). Strahlen-
ther Onkol 2002; 178:43641.
16 Asano M, Kaneoka K, Nomura T et al. Increase in serum vascular
endothelial growth factor levels during altitude training. Acta Physiol
Scan 1998; 162:4559.
17 Kikuchi K, Kubo M, Kadano T et al. Serum concentrations of vascu-
lar endothelial growth factor in collagen diseases. Br J Dermatol
1998; 139:104951.
18 Seko Y, Fukuda S, Nagai R. Serum levels of endostatin, vascular
endothelial growth factor (VEGF) and hepatocyte growth factor
(HGF) in patients with acute myocardial infarction undergoing
early reperfusion therapy. Clin Sci 2004; 106:43942.
19 McIlhenny C, George WD, Doughty JC. A comparison of serum
and plasma levels of vascular endothelial growth factor during the
menstrual cycle in healthy female volunteers. Br J Cancer 2002;
86:17869.
20 Benoy I, Vermeulen P, Wuyts H, Dirix L. Vascular endothelial
growth factor (VEGF) serum concentrations change according to
the phase of the menstrual cycle. Eur J Cancer 1998; 34:12989.
21 Dirix LY, Vermeulen PB, Pawinski A et al. Elevated levels of the
angiogenic cytokines basic broblast growth factor and vascular
endothelial growth factor in sera of cancer patients. Br J Cancer
1997; 76:23843.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp653658
658 Endostatin in sera of melanoma patients, P. Kurschat et al.
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07725. x
Palmoplantar pustulosis and gluten sensitivity:
a study of serum antibodies against gliadin and tissue
transglutaminase, the duodenal mucosa and effects of
gluten-free diet
G. Michaelsson, G. Kristjansson,* I. Pihl Lundin and E. Hagforsen
Departments of Dermatology and *Gastroenterology, Medical Sciences, University Hospital, Uppsala, Sweden
Correspondence
Gerd Michae lsson.
E-mail: gerd.michaelsson@medsci.uu.se
Accepted for publication
7 October 2006
Key words
coeliac disease, psoriasis
Conicts of interest
None declared.
Summary
Background Palmoplantar pustulosis (PPP) is a chronic inammatory disease affect-
ing mainly smoking women. Some patients also have psoriasis. A subgroup of
patients with psoriasis has been shown to have silent gluten sensitivity with rele-
vance for their psoriasis. Nothing is known about gluten sensitivity in PPP.
Objectives To nd out whether any patients with PPP are gluten-sensitive and
whether this might be relevant for the PPP activity.
Patients and methods One hundred and twenty-three patients (113 women) with PPP
participated. Screening for IgA antibodies against gliadin and tissue transglutami-
nase (tTG) was performed, the duodenal mucosa in patients with and without
these antibodies was studied and the effect of a gluten-free diet (GFD) was fol-
lowed up.
Results Twenty-two patients (18%) had IgA antibodies against gliadin and nine of
94 (10%) against tTG. Twelve patients with antibodies and 11 without under-
went gastro-duodenoscopy. Four displayed villous atrophy, whereas all other
specimens were judged as essentially normal at routine staining. However, with
immunohistochemistry, the numbers of CD3+ and CD8+ lymphocytes in the
epithelium were found to be increased in patients with any type of antibody,
although they were most numerous in those with both types of antibodies. Seven
of 123 patients (6%) had coeliac disease (three previously diagnosed). Patients
with antibodies who adhered to the GFD displayed total or nearly total clearance
of the skin lesions and normalization of the antibody levels.
Conclusions Patients with PPP should be screened for antibodies against gliadin and
tTG. Those with antibodies can be much improved on a GFD regardless of the
degree of mucosal abnormalities.
Palmoplantar pustulosis (PPP) is a chronic and intensely
inammatory disease with pustules, erythema and scaling
localized to the palms and soles. Ninety per cent of the
patients are women and 95% are smokers at the onset of the
disease.
1
Cessation of smoking can improve PPP,
2
although
some patients do not seem to respond and total clearance is
not achieved. PPP has been considered to be a variant of psor-
iasis and about 18% of the patients also have psoriasis lesions
of the vulgaris type. However, PPP has genetic characteristics
different from those of psoriasis vulgaris.
3
PPP is often treatment-resistant and about 30% of patients
have long periods of sick-leave or have a disability pension
because of their PPP, which is often associated with one or
several other disorders.
1
The lack of regimens with good clin-
ical effects in PPP, as well as the diversity of evaluation mod-
els, were recently addressed in a review by Marsland et al.
4
The target for the inammation in PPP is the palmoplantar
eccrine sweat duct, where neutrophil and also eosinophil gran-
ulocytes migrate outwards to form a pustule in the lowest part
of the stratum corneum.
5,6
In the papillary dermis below the
pustule there is a dense inltration of CD4+ lymphocytes and
mast cells.
5
There is also evidence that the papillary endothelium
is involved, as 47% of PPP sera added to palmar skin sections
from healthy women displayed a reactivity with the endothe-
lium when screened with immunouorescence.
7
If the normal
palmar skin is taken from a smoker, PPP sera also react with the
acrosyringium, where nicotine has been shown to be excreted,
8
which indicates that smoking can upregulate the reactivity.
7
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666 659
It has long been known that among patients with PPP there
is an increased prevalence of autoimmune thyroid disease.
Recently we have also found a high prevalence of abnormal
calcium homeostasis
1
as well as of diabetes type 2 in pa-
tients with PPP. Thus, PPP is associated with autoimmune
co-morbidity, but it is not yet known whether the skin dis-
order and the co-existing diseases have a pathogenetic back-
ground in common.
Coeliac disease is also an autoimmune disorder and involves
production of IgA antibodies against gliadin, endomysium and
tissue transglutaminase (ETG). In our rst study of PPP
5
we
observed a few patients with concomitant coeliac disease in
whom the PPP improved when the patients adhered strictly to
a gluten-free diet (GFD). The importance of this nding is
not fully understood. We have therefore screened a large
group of patients with PPP for the presence of serum anti-
bodies against gliadin and tTG, performed gastro-duodenosco-
py with duodenal biopsies in patients with and without such
serology, and followed up the patients during a long period
on a GFD.
Patients and methods
Patients
Consecutive patients with PPP (113 women and 10 men,
mean age SD at the time of the examination 53
11 years and mean age at the start of PPP 44 13 years)
referred to the outpatient Department of Dermatology at the
University Hospital, Uppsala, Sweden, participated in the
study. The project was approved by the local Ethics Commit-
tee and all patients gave their informed consent. All patients
answered a questionnaire concerning their medical history
and medication, smoking habits, sick-leave and disability
pension.
All patients were examined by the same dermatologist
(G.M.). The severity of the PPP varied. Both yellow and old
brown pustules were counted, the degree of erythema and
scaling was graded 03 and the involved area was marked on
a template. Some patients had 50100 yellow pustules and
erythema and scaling involving the whole plantar surface as
well as the palms, whereas others had only a few pustules and
mild erythema and scaling. The PPP was also recorded as
mild, moderate or severe. Mild PPP was dened as the pres-
ence of only 13 yellow pustules, grade 1 erythema and
desquamation (on a scale of 13), and < 10% involvement of
the palms/soles. The PPP was considered moderate if there
were 320 pustules, the erythema and desquamation graded
as 2, and < 30% of the palms and soles was involved. Severe
PPP was dened as > 20 pustules, grade 3 erythema, desqua-
mation, involvement of 30% of the area.
All patients were asked if they had any of a number of
gastrointestinal symptoms such as nausea, vomiting, abdom-
inal distension, pain, atulence or diarrhoea. Body mass index
(BMI) was calculated as weight (in kg)/[height (in m)].
2
Some anamnestic and clinical data are presented in Table 1.
Blood samples
Blood samples were obtained from all 123 patients for screen-
ing for antibodies against IgA and IgG gliadin (IgA AGA and
IgG AGA, respectively)
9
and from 94 patients for screening
for IgA antibodies against tTG (normal, < 6 U L
)1
). In add-
ition to routine blood examination in all patients, we also
measured antibodies against thyroglobulin and thyroperoxi-
dase, IgG, IgA and IgM, thyroid-stimulating hormone, thyrox-
ine, folic acid and cobalamine in serum.
Table 1 Some data on the medical history and clinical and laboratory
variables of 123 patients with palmoplantar pustulosis (PPP)
Variables n (%)
History of/or concomitant disease
Psoriasis vulgaris 30 (24)
Arthritis (two with
rheumatoid arthritis)
10 (8)
Hyperthyroidism 4 (3)
Hypothyroidism 10 (8)
Coeliac disease (diagnosed before
rst visit for PPP)
3 (2)
Crohn disease 0 (0)
Ulcerative proctitis 3 (2)
Diabetes type 1 3 (2)
Diabetes type 2 10 (8)
Pernicious anaemia 4 (3)
Dermatitis herpetiformis 1 (1)
Vitiligo 2 (2)
Chronic candidiasis 1 (1)
Sweet syndrome 1 (1)
Hypertension/cardiovascular disease 26 (21)
Psychiatric disease [manic-depressive
disease (1), schizophrenia (1),
depression (18)]
20 (16)
Sick-leave/disability pension 54 (44)
Smoking habits
Never 8 (6)
Former 17 (14)
Current 98 (80)
Gastrointestinal symptoms 40 (33)
Body mass index, all patients,
mean (range)
265 43 (17541)
Screening results
IgG antibodies against thyroglobulin
and/or thyroperoxidase (n 110)
23 (21)
IgA antibodies against gliadin 22 (18)
IgG antibodies against gliadin 3 (2)
IgA antibodies against tissue
transglutaminase (n 94)
9 (96)
Medication
Levothyroxine 11 (9)
Insulin 4 (3)
Beta-blockers (4), angiotensin II
antagonists (4), calcium-channel
blockers (5), hydrochlorothiazide (3)
16 (13)
Glibenclamide, metformin 8 (7)
Antidepressives 8 (7)
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
660 PPP and gluten sensitivity, G. Michaelsson et al.
Gastroscopyduodenoscopy with biopsies of the
duodenal mucosa
Patients who gave informed consent and had elevated levels
of antibodies against gliadin and/or tTG were referred to a
gastroenterologist (G.K.). Patients with PPP with no sero-
logical ndings indicating gluten sensitivity, who were
undergoing gastroscopy for other medical reasons, also con-
sented to having an extra biopsy taken for immunohisto-
chemistry. Five mucosal biopsy specimens were taken from
the duodenum distal to the papilla of Vater in conjunction
with upper gastrointestinal endoscopy. One of the specimens
was snap-frozen in chilled isopentane and stored at )70 C,
and the others were xed in 4% formaldehyde and parafn-
embedded separately.
Processing of the specimens
Sections from each of the parafn-embedded specimens from
the duodenal mucosa were stained with haematoxylin and
eosin and Alcian Blueperiodic acid-Schiff and examined at
the Department of Pathology with regard to the villous archi-
tecture and to inammatory cells in the epithelium and lamina
propria. Frozen sections were used for visualization of CD3+,
CD8+ and CD4+ T lymphocytes in the duodenal mucosa as
previously described.
10
Microscopy
The results of the immunohistochemical examinations of the
duodenal specimens were analysed on coded slides with a
Leica Q Win computerized image system with a digital cam-
era, DC 200 (Leica Microscopy and Scientic Instruments
Group, CH-9435 Heerbrugg, Switzerland). The numbers of
CD3+ and CD8+ T lymphocytes per millimetre epithelium
were determined and the percentage of CD3+ and CD4+ areas
in the lamina propria in the villi were analysed as previously
reported.
10
The lamina propria in the villi was chosen for esti-
mation of the CD4 lymphocyte inltration because the area
measured can be dened more easily there than in the lower
parts of the lamina propria. Usually the CD4 staining was esti-
mated in ten elds and only villi cut longitudinally were
chosen for evaluation.
Expression of tTG in palmar skin from a healthy woman
and from involved palmar skin in a patient with PPP was stud-
ied as previously described in nonhairy skin and in lesional
psoriasis.
11
Gluten-free diet
Patients with antibodies against gliadin and/or tTG were asked
to adhere to a GFD for at least 6 months regardless of the
results of the duodenal biopsies, and were followed up for at
least 2 years. Three patients without such antibodies also con-
sented to adhere to a GFD. Before starting the GFD all patients
received detailed information from a dietician.
Statistics
The degree of signicance was tested with the nonparametric
MannWhitney U-test for unpaired two-group comparison.
Results
Anamnestic and clinical data
As is evident from Table 1 psoriasis (indistinguishable from
the vulgaris type), arthritis, thyroid disease, diabetes type 2,
hypertension/cardiovascular disease and depression were com-
mon disorders among the patients with PPP, as was long sick-
leave and disability pension. Twenty-six patients had one or
several autoimmune disorders. Never-smokers had mild PPP.
Thirty patients had severe PPP.
Three patients had coeliac disease that had been diagnosed
previously; in one it was combined with dermatitis herpeti-
formis. One of these patients adhered strictly to a GFD and
had only barely visible and transient PPP during a period of
severe mental stress. The other two did not adhere strictly to
such a diet and the severity of their PPP did not change dur-
ing a 10-year period.
In answer to questions about gastrointestinal symptoms, 40
patients stated that they had some symptom, but patients who
had antibodies against gliadin or tTG did not report more
symptoms than those without. The mean BMI was similar in
those with and without these antibodies.
Three patients had a history of proctitis and one of them
was found to have high levels of AGA and tTG antibodies and
partial villous atrophy.
Screening results
Twenty-two patients (179%) had elevated levels of IgA AGA
( 51 U L
)1
) (Table 1) and three with IgA AGA also had
raised IgG AGA, but none had isolated IgG AGA. Usually the
IgA AGA values were only slightly elevated (51100 U L
)1
).
Increased levels of tTG antibodies were found in nine of 94
sera (96%) (Table 1). Serum from our rst patient with sub-
total villous atrophy was AGA-positive, but no serum for an-
alysis of tTG antibodies was available. Six of nine tTG-positive
sera were AGA-positive. As found in our rst study on PPP,
5
serum-IgA was elevated compared with that in blood donors.
Women with PPP had a serum-IgA level (mean SD) of
28 16 g L
)1
, compared with 21 07 g L
)1
in controls
(P < 00001). The highest value was noted in those with AGA
and/or tTG antibodies, namely 31 19 g L
)1
(n 19), but
the difference between those with and without these anti-
bodies was not signicant.
Duodenal biopsies
In addition to the three patients with previously known gluten
intolerance and villous atrophy mentioned above, 12 patients
with IgA AGA and/or tTG antibodies had undergone gastro-
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
PPP and gluten sensitivity, G. Michaelsson et al. 661
duodenoscopy. (One patient with tTG 7 U L
)1
was not
examined.) Another 11 patients, all without these antibodies,
were included for comparison; ve had arthritis in addition to
PPP and six were investigated for other medical reasons. Fro-
zen biopsy specimens for immunohistochemistry were avail-
able from 18 patients and routine biopsy results from all.
Routine staining of parafn-embedded specimens from 12
patients with AGA and/or tTG antibodies revealed total villous
atrophy in one, subtotal villous atrophy in two and partial
atrophy in one patient. Three of these four patients were not
aware of any gastrointestinal symptoms, whereas one had a
history of proctitis. (Frozen specimens were available from
two of these four patients.)
Specimens from ve other patients with AGA and/or tTG
antibodies displayed a focal increase in intraepithelial lympho-
cytes and an increased number of inammatory cells in the
lamina propria, but were considered as essentially normal;
specimens from two AGA-positive patients and one tTG-posi-
tive but AGA-negative patient were judged by the pathologists
to be normal.
The specimens from the 11 remaining patients with PPP
who were all AGA- and tTG-negative were evaluated as nor-
mal at routine staining.
Immunohistochemistry
Table 2 shows the results of the CD3, CD8 and CD4 staining
of the frozen duodenal biopsy specimens. Figure 1 shows the
individual values for CD3+ and CD8+ lymphocytes in the epi-
thelium in patients (without arthritis) with no antibodies and
those with antibodies only against tTG or gliadin and those
with both these antibodies. The largest mean number of intra-
epithelial CD3+ lymphocytes (P 00527 vs. those with only
AGA or tTG antibodies) and the largest percentage area of
CD4+ lymphocytes in the villi (P 00527) were found in
patients who had both AGA and tTG antibodies and the lowest
number of intraepithelial lymphocytes in those with no AGA
or tTG antibodies and no arthritis. The number of CD3+ cells
in the epithelium was signicantly higher in specimens from
AGA- and/or tTG-positive patients (n 10) than in those
from AGA/tTG-negative patients (n 3) (P < 005).
Table 2 PPP, CD3+ and CD8+ T lymphocytes in the duodenal epithelium (mean SD) and CD3+ and CD4+ T lymphocytes in the lamina
propria of the villi (mean % stained area SD)
n
CD3+ cells
per mm epithelium
CD8+ cells
per mm
epithelium
CD3+ area
in villi (%)
CD4+ area
in villi (%) Comments
PPP with tTG and AGA 3 84 36 61 27 15 11 14 2 Two with
villous atrophy
PPP with tTG, no AGA 2 27 14 17 6 4 08 7 6
PPP with AGA, no tTG 5 38 18 39 25 6 4 6 3
PPP without AGA, no tTG, no arthritis 3 13 14
a
12 12 9 5 9 8
PPP + arthritis, no AGA, no tTG 5 26 19 16 12 11 13 8 7
PPP all without AGA and tTG 8 21 18
b
15 11
c
10 11 8 7
For comparison: corresponding results in psoriasis vulgaris without antibodies against gliadin (n 7): CD3+ cells 9 5, CD8+ cells 9 7
per mm epithelium and CD4+ area in villi (%) 3 1.
10
PPP, palmoplantar pustulosis; AGA, IgA antibodies against gliadin; tTG, IgA anti-
bodies against tissue transglutaminase.
a
P 00280 compared with AGA- and/or tTG-positive;
b
P 00263 compared with all AGA- and/or
tTG-positive;
c
P 00129 compared with all AGA- and/or tTG-positive.
CD3+ lymphocytes
None tTG AGA Both
0
25
50
75
100
125
N
u
m
b
e
r
/
m
m
e
p
i
t
h
e
l
i
u
m
CD8+ lymphocytes
None tTG AGA Both
0
25
50
75
100
N
u
m
b
e
r
/
m
m
e
p
i
t
h
e
l
i
u
m
Fig 1. Individual numbers of CD3+ and CD8+ lymphocytes per
millimetre epithelium in the duodenal mucosa in patients with
palmoplantar pustulosis (PPP) with no antibodies against gliadin or
tTG (none), antibodies only against tTG (tTG), only against gliadin
(AGA) and against both tTG and gliadin (both). Data from patients
with arthritis not included.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
662 PPP and gluten sensitivity, G. Michaelsson et al.
Patients with concomitant arthritis but no AGA and/or tTG
antibodies showed an increased number of epithelial CD3+
cells, but the difference from the three AGA-negative patients
without arthritis was not signicant.
Expression of tissue transglutaminase in palmar skin
Figure 2 shows the expression of tTG in normal palmar skin
and in lesional PPP skin from a patient with no AGA or tTG anti-
bodies. A double staining (not shown in Fig. 2) with anti-tTG
antibody and CD31 showed that tTG was present mainly in the
endothelium, which was highly increased in the inamed skin.
Effects of a gluten-free diet on the severity of the
palmoplantar pustulosis
Table 3 shows the severity of the PPP before and during a
GFD and also some anamnestic and clinical data. In all
patients with raised AGA and/or tTG antibodies who adhered
to the GFD the PPP cleared or greatly improved. The elevated
AGA and tTG values became normalized in those who
adhered to the diet. On the other hand those who did not
adhere to the diet did not improve and the AGA and tTG
levels remained elevated. Improvement was not related to the
degree of mucosal changes. Thus it occurred both in patients
with villous atrophy and in those with a minor lymphocyte
increase.
In two of the patients there was an isolated moderate
increase in tTG antibodies. One of them with disabling PPP
showed no evidence of increased lymphocytes in the duodenal
mucosa and the other with PPP associated with long periods
of sick-leave had a mild increase. Both have had a remarkable
improvement on GFD and have had no sick-leave since the
start of the GFD.
Improvement was usually slow. It occurred in a shorter
timewithin a few monthsin patients with PPP of moder-
ate severity than in those with long-standing severe PPP, in
whom the improvement continued for several years.
As shown in Table 3, the clearance has persisted for years.
Our rst patient with disabling PPP and diagnosed with
coeliac disease who showed total clearance during a period of
10 years on GFD had a recurrence with moderate PPP after
the death of several family members. In contrast to the other
patients, three patients with severe PPP without AGA or tTG
antibodies adhered to GFD for more than 1 year without any
improvement.
Discussion
In this study we have shown that a large subgroup of PPP
patients have IgA antibodies against gliadin and/or tTG despite
absence of gastrointestinal symptoms, that the duodenal mu-
cosal specimens in these patients display a spectrum from total
villous atrophy to normal mucosa, and that most of the anti-
body-positive patients who adhere to a GFD displayed almost
total or total clearance of their PPP.
We have previously reported that among patients with psor-
iasis vulgaris (PsoV)
9
and psoriatic arthritis (PsoA)
12
there is
an increased prevalence of IgA AGA. In this study IgA AGA
was found in a slightly higher proportion of the patients with
PPP than in the other two psoriasis groups and was present
both in patients with and those without PsoV lesions.
In contrast to patients with PsoV and PsoA, the patients
with PPP had a high prevalence of IgA antibodies against tTG,
these being found in nine of 94 patients (96%), all women.
Recently Metzger et al.
13
reported from a population-based
survey that 083% of women had raised levels of tTG anti-
bodies. It is noteworthy that three of 94 (3%) showed an
isolated increase in tTG antibodies. The proportion of patients
with tTG antibodies among those with AGA (six of 22,
272%) was much higher than among PsoV patients with
AGA, where we found only 41% with tTG antibodies, and in
Fig 2. Expression of tissue transglutaminase (tTG) in (a) palmar skin from a healthy woman and (b) lesional skin from a patient with
palmoplantar pustulosis with no AGA or tTG antibodies. Scale bars 50 lm.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
PPP and gluten sensitivity, G. Michaelsson et al. 663
the PsoA group none of the AGA-positive patients had tTG
antibodies.
13
Seven patients with PPP had coeliac disease (four identied
within the study) with total, subtotal or partial villous atrophy
(57%), compared with 027% among Swedish blood
donors.
14
Apart from the specimens from these patients, only
nonspecic inammation or no abnormalities at all were
observed by the pathologists in routinely stained specimens
from patients with antibodies. The moderate to mild increase
in lymphocytes observed with immunohistochemistry was
thus usually not obvious in the routinely stained specimens
and is a nonspecic nding that will require further studies.
The largest number of lymphocytes both in the epithelium
and in the lamina propria in the duodenal specimens was
found in patients with both IgA AGA and tTG antibodies and
villous atrophy, whereas patients with only one of these anti-
bodies showed a modest increase in intraepithelial lympho-
cytes, and those without these antibodies had a normal
number of lymphocytes. These ndings indicate a link
between the presence of antibodies and the lymphocyte
increase.
However, as shown in Table 2, an increase in lymphocytes
can be present in AGA/tTG-negative PPP patients who also
have arthritis, as we recently reported in patients with PsoA
without AGA.
10
Patients with AGA or antibodies against tTG or both were
asked to try to adhere strictly to a GFD regardless of the
results of the duodenal examination. The outcome was very
Table 3 Palmoplantar pustulosis (PPP) and effects of gluten-free diet (GFD)
Patient AGA/tTG Duodenal mucosa
PPP
years
PPP severity
before/on
GFD
Adhered
to GFD
AGA/tTG
during GFD
Follow-up
on GFD Comments
1 AGA Subtotal villous atrophy 9 Severe/cleared Yes Normal 16 years Cleared in 10 years; smoker;
recurrence moderate PPP
after death of family
members
2 AGA, tTG Subtotal villous atrophy 30 Moderate/cleared Yes Normal 2 years Also psoriasis, cleared, slight
worsening after serious
illness in family; smoker
3 AGA, tTG Total villous atrophy 3 Moderate/cleared Yes Normal 4 years Also rheumatoid arthritis;
smoker
4 AGA, tTG Partial villous atrophy 9 Moderate/cleared Yes Normal 5 years Former smoker
5 No AGA,
but tTG
Slight increase in IEL
(CD3, CD8)
13 Moderate/cleared Yes Normal 4 years Previously long sick-leaves,
none on GFD; smoker
6 No AGA
but tTG
Normal 4 Severe/mild Yes Normal 3 years Elevated serum lipids; smoker
7 AGA,
not tTG
Normal 35 Moderate/cleared Yes Normal 2 years Resumed normal diet, mild
recurrence after 3 months;
smoker
8 AGA,
not tTG
Increased IEL (CD3, CD8) 14 Moderate/cleared Yes Normal 6 years Never-smoker
9 AGA,
not tTG
Increased IEL (CD3, CD8) 4 Moderate/cleared Yes Normal 5 years Mild psoriasis, cleared; heavy
smoker
10 AGA, tTG Subtotal villous atrophy 32 Severe/severe Not strict Elevated 10 years Also diabetes type 1; former
smoker
11 AGA
not tTG
Partial villous atrophy 34 Moderate/moderate Not strict Elevated 10 years Also diabetes type 1,
dermatitis herpetiformis,
dapsone; smoker
12 AGA, tTG Increased IEL, some
villi broadened
13 Severe/moderate Not strict Elevated 8 years High levels of antibodies
against thyroperoxidase;
smoker
13 AGA
no tTG
Slight increase in IEL,
some villi broadened
16 Severe/moderate Not strict Elevated 8 years Heavy smoker
14 No AGA,
no tTG
Increased IEL (CD3, CD8) 6 Moderate/moderate Yes Normal 1 year Also arthritis; former smoker
15 No AGA,
no tTG
Increased IEL (CD3, CD8) 6 Severe/severe Yes Normal 1 year Also arthritis; former smoker
16 No AGA,
no tTG
Normal 12 Severe/severe Yes Normal 1 year Former smoker
AGA, IgA antibodies against gliadin; tTG, IgA antibodies against tissue transglutaminase; IEL, intraepithelial lymphocytes; PPP years, duration
of PPP before GFD
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
664 PPP and gluten sensitivity, G. Michaelsson et al.
good in those who adhered to the diet, with almost total or
total clearance of the PPP during the years of follow-up, and
normalization of the levels of antibodies against gliadin and
tTG. In contrast, those who did not adhere to the diet neither
improved nor showed normalization of their antibodies,
which indicates that the reactivity against tTG and gliadin
might be a pathogenetic factor in this group of patients with
PPP. The role of these antibodies is also illustrated by the lack
of effect of the diet in those without antibodies.
AGA has low specicity and sensitivity as a marker of vil-
lous atrophy (coeliac disease).
15
However, it was found in this
study that AGA was associated with an increased number of
lymphocytes in the duodenal epithelium and improvement of
PPP during a GFD. These results indicate that AGA may be a
useful marker for the presence of a discrete lymphocyte
increase in the mucosa, which has relevance for the PPP activ-
ity. However, both the mucosa and the skin lesions need to
be studied further, for example with regard to activated
lymphocytes and transglutaminase reactivity in situ as reported
from the studies of gluten-sensitive cerebellar ataxia.
16
The mechanisms for the effect of GFD in patients with
PPP with AGA and/or tTG antibodies are unknown. tTG is a
multifunctional enzyme that has several roles in coeliac dis-
ease.
17
tTG has a widespread distribution. In the skin it is
expressed in the endothelium, in particular in proliferating
endothelium, and in the basal layer of the epidermis and in
the jejunum there is subepithelial and endothelial expression.
In our previous studies on the effects of GFD in patients
with PsoV with AGA, both the endothelium and the expres-
sion of tTG were strongly reduced after 3 months on GFD.
These changes were accompanied by a decrease in prolifer-
ation both in the endothelium and in dermal inammatory
cells.
11
However, it is not known if this effect is nonspecic
or might be linked to tTG as an autoantigen as proliferaton
of the endothelium is an early and characteristic event in
PsoV irrespective of the presence or absence of AGA/tTG
antibodies.
In lesional PPP skin there is a pronounced proliferation of
the endothelium, which shows strong tTG expression, as seen
in Figure 2 in a specimen from a patient without AGA or tTG
antibodies. The palmoplantar endothelium may be involved in
the pathogenesis of PPP, as we have found that 47% of PPP
sera react with the papillary endothelium from a healthy per-
son.
7
tTG might be one of the possible endothelial autoanti-
gens or in some patients with tTG antibodies it might be a
major autoantigen.
Why is the prevalence of tTG antibodies higher in PPP than
in the other types of psoriasis despite a similar percentage of
gliadin antibodies? A possible explanation might be that PPP
may be a different disorder, as indicated by the results of
recent genetic studies.
3
The female predominance, the high
prevalence of autoimmune disease and the localization to the
palms and soles also illustrate differences compared with PsoV
and PsoA. The fact that 95% of patients with PPP are smokers
at the onset of the disease, that smoking is associated with a
70 times higher risk of developing PPP
1
and that the few
patients with PPP who are never-smokers have only mild PPP
illustrate the role of smoking in PPP. Possibly smoking might
also facilitate the development of antibodies, as has been
shown in patients with rheumatoid arthritis who have citrul-
line antibodies.
18
Several recent reports have discussed the need for more
rened evaluation of seemingly normal mucosa in patients
with serology indicating gluten sensitivity.
19,20
This is also
illustrated by our results, with a discrete increase in lympho-
cytes in patients with AGA and/or tTG antibodies and clear-
ance of long-standing PPP on a GFD, which strongly indicates
that patients with minor mucosal changes may have gluten
sensitivity.
PPP patients with antibodies did not have more gastrointest-
inal symptoms than those without, the BMI was not lower in
the AGA/tTG-positive group and the severity of the PPP was
similar. As there was no anamnestic or clinical evidence of
gluten intolerance, none of the patients found to be gluten-
sensitive would have been identied without screening for
these antibodies.
As the results of our study show that there is a subgroup
of patients with PPP who are gluten-sensitive and that a GFD
can have a very good effect on their PPP, we suggest that
patients with PPP should be screened routinely for antibodies
against gliadin and tTG. Until more is known about gluten
sensitivity in PPP, patients with antibodies should be investi-
gated with gastro-duodenoscopy, although in the future the
presence of these antibodies may be sufcient to recommend
a GFD.
Acknowledgments
This study was supported by grants from the Swedish Psoriasis
Association, the E. Welander and Finsen Foundations, the Swe-
dish Medical Society and the Medical Faculty of the University
of Uppsala.
References
1 Hagforsen E, Michaelsson K, Lundgren E et al. Women with palmo-
plantar pustulosis have disturbed calcium homeostasis and a high
prevalence of diabetes mellitus and psychiatric disorders: a case
control study. Acta Derm Venereol 2005; 85:22532.
2 Michaelsson G, Gustafsson K, Hagforsen E. The psoriasis variant
palmoplantar pustulosis can be improved after cessation of
smoking. J Am Acad Dermatol 2006; 54:7378.
3 Asumalahti K, Ameen M, Suomela S et al. Genetic analysis of
PSORS1 distinguishes guttate psoriasis and palmoplantar pustulosis.
J Invest Dermatol 2003; 120:62732.
4 Marsland AM, Chalmers RJ, Hollis S et al. Interventions for chro-
nic palmoplantar pustulosis. Cochrane Database Syst Rev 2006;
25(1):CD001433.
5 Eriksson MO, Hagforsen E, Pihl Lundin I, Michaelsson G. Palmo-
plantar pustulosis: a clinical and immunohistological study. Br J
Dermatol 1998; 138:3908.
6 Hagforsen E, Nordlind K, Michaelsson G. Skin nerve bres
and their contacts with mast cells in patients with palmoplantar
pustulosis. Arch Dermatol Res 2000; 292:26974.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
PPP and gluten sensitivity, G. Michae lsson et al. 665
7 Hagforsen E, Awder M, Lefvert AK et al. Palmoplantar pustulosis:
an autoimmune disease precipitated by smoking? Acta Derm Venereol
2002; 82:3416.
8 Balabanova S, Buhler G, Schneider E et al. Nicotine excretion by the
apocrine and eccrine sweat in smokers and passive smokers. Hautarzt
1992; 43:736.
9 Michaelsson G, Gerden B, Ottosson M et al. Patients with psoriasis
often have increased serum levels of IgA antibodies to gliadin. Br J
Dermatol 1993; 129:66773.
10 Lindqvist U, Kristjansson G, Pihl-Lundin I et al. Patients with psori-
atic arthritis have an increased number of lymphocytes in the duo-
denal mucosa in comparison with patients with psoriasis vulgaris.
J Rheumatol 2006; 33:9247.
11 Michaelsson G, Ahs S, Hammarstrom I et al. Gluten-free diet in
psoriasis patients with antibodies to gliadin results in decreased
expression of tissue transglutaminase and fewer Ki67+ cells in the
dermis. Acta Derm Venereol 2003; 83:4259.
12 Lindqvist U, Rudsander A, Bostrom A et al. IgA antibodies to glia-
din and coeliac disease in psoriatic arthritis. Rheumatology (Oxford)
2002; 41:317.
13 Metzger MH, Heier M, Maki M et al. Mortality excess in individuals
with elevated IgA anti-transglutaminase antibodies: the KORA/
MONICA Augsburg Cohort Study 19891998. Eur J Epidemiol 2006;
21:35965.
14 Weile I, Grodzinsky E, Skogh T et al. High prevalence rates of adult
silent coeliac disease, as seen in Sweden, must be expected in
Denmark. APMIS 2001; 109:74550.
15 van Heel DA, West J. Recent advances in coeliac disease. Gut 2006;
55:103746.
16 Hadjivassiliou M, Maki M, Sanders D et al. Autoantibody targeting
of brain and intestinal transglutaminase in gluten ataxia. Neurology
2006; 66:3737.
17 Molberg O, Sollid LM. A gut feeling for joint inammationusing
coeliac disease to understand rheumatoid arthritis. Trends Immunol
2006; 27:18894.
18 Klareskog L, Stolt P, Lundberg K et al. A new model for an etiology
of rheumatoid arthritis: smoking may trigger HLA-DR (shared
epitope)-restricted immune reactions to autoantigens modied by
citrullination. Arthritis Rheum 2006; 54:3846.
19 Paparo F, Petrone E, Tosco A et al. Clinical, HLA, and small bowel
immunohistochemical features of children with positive serum
antiendomysium antibodies and architecturally normal small intes-
tinal mucosa. Am J Gastroenterol 2005; 100:22948.
20 Kaukinen K, Maki M, Collin P. Immunohistochemical features in
antiendomysium positive patients with normal villous architecture.
Am J Gastroenterol 2006; 101:6756.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp659666
666 PPP and gluten sensitivity, G. Michaelsson et al.
CLI NI CAL AND LABORATORY I NVESTI GATI ONS DOI 10. 1111/j . 1365- 2133. 2006. 07736. x
Itch Severity Scale: a self-report instrument for the
measurement of pruritus severity
C.J. Majeski, J.A. Johnson,* S.N. Davison and G.J. Lauzon
Division of Dermatology and Cutaneous Sciences, Department of Medicine, University of Alberta, Edmonton, AB T6G 2G3, Canada
*Department of Public Health Sciences, University of Alberta, Edmonton, AB, Canada
Institute of Health Economics, Edmonton, AB, Canada
Division of Nephrology, Department of Medicine, University of Alberta, Edmonton, AB T6G 2G3, Canada
Correspondence
Gilles J Lauzon.
E-mail: glauzon@ualberta.ca
Accepted for publication
1 November 2006
Key words
Itch Severity Scale, pruritus, questionnaire
Conicts of interest
None declared.
Summary
Background Assessing pruritus severity is difcult because of its subjective nature.
A questionnaire that takes into account how the symptom is perceived by the
patient may provide a more accurate representation of the pruritus. However,
recently developed questionnaires do not specically quantify severity of the
symptom.
Objectives To develop a self-report questionnaire to measure pruritus severity and
to provide initial evidence of its validity and reliability.
Methods We modied a previously developed interview for the characterization and
evaluation of pruritus, which was completed along with the RAND-36 Health Status
Inventory and Dermatology Life Quality Index by patients with psoriasis-associated
pruritus. Exploratory factor analysis, studies of internal consistency, and correlation
analyses with health-related quality of life scores were used to help determine
which components of the modied pruritus interview to include in the new ques-
tionnaire, the Itch Severity Scale (ISS). The ISS was then assessed for construct valid-
ity, internal consistency reliability and testretest reliability.
Results Seven of the initial 11 components of the modied pruritus interview were
included in the ISS. ISS scores correlated moderately with physical (r )0483)
and mental (r )0492) health composite scores of the RAND-36 and strongly
with Dermatology Life Quality Index scores (r 0628), evidence of construct
validity. It had an internal consistency reliability of 080 and a testretest reliabil-
ity of 095.
Conclusions Based on this preliminary evidence of validity and reliability, this new
seven-item ISS may be useful in comparing pruritus severity among different dis-
ease populations or in assessing pruritus treatment effectiveness.
Pruritus is perhaps the most commonly described symptom in
dermatology. It is associated with numerous skin conditions
such as atopic dermatitis, urticaria and psoriasis, as well as
with a variety of systemic conditions including chronic renal
failure and hepatic cholestasis. It is a potentially debilitating
symptom associated with considerable psychiatric morbid-
ity,
1,2
sleep disturbances
3,4
and an overall reduced health-
related quality of life (HRQL).
5,6
Generally, the intensity of pruritus, and not its other qualities,
such as how the symptom is perceived by the patient or its
effects on daily life, has been the focus of previous studies. This
is due in part to a lack of standardized questionnaires to quantify
pruritus severity. Two relevant instruments have recently been
developed, however. The rst
7
is based on the long form of the
McGill Pain Questionnaire
8
and includes a detailed list of sen-
sory and affective descriptors, but it does not include any ques-
tions regarding effect on HRQL. It is a self-report questionnaire
that takes about 30 min to complete, hence is quite time consu-
ming and demanding. The second instrument
9
is based on the
short form of the McGill Pain Questionnaire
8
and probes
sensory and affective dimensions, as well as effects on HRQL.
However, it is interviewer administered, a signicant practical
limitation. Further, neither instrument quanties pruritus sever-
ity specically, nor patient burden generally.
Thus, we contend that the development of a practical
questionnaire assessing pruritus severity and resulting patient
burden is required for both clinical evaluation and research.
An ideal instrument would capture patients perception of
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673 667
pruritus severity and allow the comparison of severity among
different disease populations as well as the assessment of the
effectiveness of therapy. The purpose of this study was to
develop a self-report questionnaire to quantify pruritus sever-
ity, based on the instrument constructed by Yosipovitch et al.,
9
and to assess its validity and reliability.
Materials and methods
Overview
We began with the instrument previously developed by
Yosipovitch et al.
9
and modied it to a self-report format
(hereafter referred to as the modied pruritus questionnaire).
The modied pruritus questionnaire was administered to
patients with chronic plaque psoriasis along with the RAND-
36 Health Status Inventory and Dermatology Life Quality
Index (DLQI). Exploratory factor analysis, studies of internal
consistency, and correlation analyses with HRQL scores were
used to determine which components of the modied pruritus
questionnaire were most appropriate to include in the nal
instrument, the Itch Severity Scale (ISS). The nal ISS was then
assessed for construct validity, internal consistency reliability
and testretest reliability. This study was approved by the
Health Research Ethics Board at the University of Alberta.
Sample
Subjects were consecutively recruited from phototherapy and
dermatology clinics in Alberta. Inclusion criteria were as fol-
lows: (i) stable chronic plaque psoriasis involving a minimum
5% body surface area; (ii) psoriasis that had been present for
a minimum of 6 months; (iii) chronic psoriasis-associated
pruritus, dened as at least two episodes of itch per week, the
itch occurring several times a day, lasting for more than
5 min, being bothersome, and having been present for a
minimum of 6 weeks; and subjects (iv) between the ages of
18 and 70 years; (v) able to give informed consent; and
(vi) able to complete the questionnaires in English.
Measures
The questionnaire package included questions on demograph-
ics and comorbidities, plus the following three measures:
Modied pruritus questionnaire
As above, the interviewer-administered instrument was previ-
ously developed by Yosipovitch et al.
9
for the characterization
and evaluation of pruritus. It has no method of scoring with
which to quantify severity of the symptom. The instrument
was modied for this study to a self-report format and inclu-
ded questions on the following: duration; frequency; pattern;
body surface area involved (calculated in the same way as
body surface area in the Self-Administered Psoriasis Area and
Severity Index
10
); intensity as measured by ve-point Likert
scale and Visual Analogue Scale (VAS); current antipruritic
treatment and efcacy; accompanying symptoms; description
of itch sensation and affective descriptors; effect of daily activ-
ities on pruritus; and effect of pruritus on sleep, mood, ability
to concentrate, diet, sexual desire and sexual function.
RAND-36 Health Status Inventory
The RAND-36
11
is a widely used 36-item generic measure of
health status composed of the same questions as the well-
known Short Form-36, but that uses different scoring metho-
dology. Evidence suggests that the RAND scoring approach
may be more valid,
1214
prompting its use, over the Short
Form-36, in this study. It measures eight dimensions of health
status and has two summary scores: the physical health com-
posite (PHC) and the mental health composite (MHC). A score
from 0 to 100 is calculated for each of the eight subscales,
with higher scores indicating better HRQL. The PHC and
MHC are calculated as norm-based T-scores. There are consid-
erable data to support the instruments validity and reliabil-
ity.
11
As suggested by the developer, mean imputation was
performed for missing RAND-36 data.
11
Dermatology Life Quality Index
The DLQI
15
is a skin-specic HRQL questionnaire with evi-
dence for validity and reliability.
16
Scores range from 0 (no
impairment of life quality) to 30 (maximum impairment). A
question left unanswered is scored 0 and if two or more ques-
tions are left unanswered the questionnaire is not scored.
17
Procedure
Patients were briey interviewed to determine if they met the
inclusion criteria. Those satisfying inclusion criteria were
provided with a questionnaire package to be completed at
their convenience. A reminder letter was sent if the question-
naire package had not been returned within 2 weeks.
Itch Severity Scale development
Multiple strategies were used to select the relevant items from
the modied pruritus questionnaire to comprise the nal ISS.
Components that had a relatively weak correlation with pruritus
severity, based on preliminary factor analysis and expert opin-
ion, were eliminated. The remaining, candidate items, were
then subjected to exploratory factor analysis.
18
Principal compo-
nent analysis with varimax rotation was applied to the candidate
items to provide information regarding the nature of the contri-
bution by each item to the measurement of pruritus severity.
Candidate items for the nal scale were further evaluated
based on internal consistency reliability. Correlation analyses
with HRQL scores were also performed based upon the hypo-
thesis that more severe pruritus is associated with poorer
HRQL. Thus, graded correlations in the appropriate direction
were interpreted as indicating a greater association with
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
668 Itch Severity Scale, C.J. Majeski et al.
pruritus severity. In addition, the aspects measured by each
candidate item were compared to eliminate potentially
redundant questions. Lastly, for each question, ambiguous or
missing responses were noted to predict interpretative or other
problems relating to the respective questions. Candidate items
were subsequently chosen for the ISS based on the statistical
analyses, while attempting to maintain a clinically logical
combination that addressed all facets deemed important. Statis-
tical analyses were conducted using SPSS 13.0 (SPSS, Chicago,
IL, U.S.A.); P < 005 was interpreted as statistically signicant.
Instrument validity
Construct validity of the ISS was evaluated through correla-
tions with the accompanying three HRQL measures. Based on
the premise that pruritus severity affects HRQL, it was hypo-
thesized a priori that ISS scores would correlate with the HRQL
scores, i.e. greater pruritus severity would be associated with
lower HRQL. It was also hypothesized at the outset that the
ISS scores would correlate more strongly with the DLQI scores
than with the PHC and MHC scores of the RAND-36, because
a skin-specic measure should be more sensitive to differences
in HRQL caused by a skin condition than a generic measure
of health status. Correlations were measured with Pearsons
correlation coefcient (r) and interpreted as follows: r 03
was interpreted as a weak correlation, 03 < r < 05 as a mod-
erate correlation, and r 05 as a strong correlation.
19
Instrument reliability
We assessed both internal consistency and testretest reliabil-
ity.
20
Internal consistency reliability was determined using the
Cronbachs alpha coefcient. To estimate the testretest reliab-
ility of the ISS, the modied pruritus questionnaire was mailed
to a random sample of the participants to complete again
2 weeks following initial questionnaire completion. Pearsons
correlation coefcient (r) and intraclass correlation coefcients
were used to estimate the testretest reliability of the ISS based
on responses to the modied pruritus questionnaire. We con-
sidered the minimum acceptable values for Cronbachs alpha,
Pearsons correlation coefcient (r) and intraclass correlation
coefcients to be 07 for group-level comparison and 09 for
individual comparison.
20
Clinical interpretation of Itch Severity Scale scores
We dened a clinically important difference for the ISS based
on comparisons with suggested clinically important differences
in scores for the PHC and MHC of the RAND-36 (35
points)
21
and DLQI (25 points)
22
using respective linear
regression formulae.
Results
A total of 93 subjects completed the initial questionnaire pack-
age (Table 1). Most subjects were white (94%), married
(65%) and employed (71%) (Table 1). The modied self-
report version of the instrument of Yosipovitch et al. was
mailed to 40 of the subjects in the testretest subsample.
Thirteen (33%) subjects responded in the retest, between 11
and 17 days following initial completion, with a median of
15 days between responses. There were no statistically signi-
cant differences in demographic characteristics between the
initial and retest samples (Table 1).
Candidate item assessments
Eleven candidate items were identied from the modied pru-
ritus questionnaire: item 1 (days and hours per week of itch),
Table 1 Demographic characteristics
Initial sample
(n 93), n (%)
Retest sample
(n 13), n (%)
Age (years)
<30 12 (13) 1 (8)
3039 16 (17) 2 (15)
4049 21 (23) 3 (23)
5059 27 (29) 5 (38)
60+ 17 (18) 2 (15)
Sex
Male 45 (48) 6 (46)
Female 48 (52) 7 (54)
Marital status
Single 20 (22) 2 (15)
Married/with partner 60 (65) 10 (77)
Separated/divorced/
widowed
13 (14) 1 (8)
Education
Less than high school/
high school graduate
43 (46) 4 (31)
College graduate 50 (54) 9 (69)
Main activity
Working at job 66 (71) 8 (62)
Looking for work 2 (2) 1 (8)
Keeping house 5 (5) 2 (15)
Student 0 0
Unemployed due
to disability
9 (10) 1 (8)
Retired 11 (12) 1 (8)
Income (Canadian $)
Under 10 000 9 (10) 1 (8)
10 00029 999 9 (10) 0
30 00049 999 16 (17) 2 (15)
50 00069 000 16 (17) 2 (15)
70 000 and above 34 (37) 8 (62)
Ethnicity
White 87 (94) 13 (100)
Asian/Oriental 3 (3) 0
East Indian 2 (2) 0
Black 0 0
Native Indian 1 (1) 0
Comorbidities (mean SD) 215 194 146 127
SAPASI score (mean SD) 1331 1073 951 626
SAPASI, Self-Administered Psoriasis Area and Severity Index.
10
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
Itch Severity Scale, C.J. Majeski et al. 669
item 2 (itch description A), item 3 (itch description B), item
4 (frequency), item 5 (pattern), item 6 (effect on sleep), item
7 (effect on mood), item 8 (effect on sexual desire/function),
item 9 (itch intensity using Likert scale), item 10 (itch inten-
sity using VAS) and item 11 (body surface area involved).
Exploratory factor analysis
The principal component analysis identied two meaningful
factors. The rst factor, which could be termed pruritus severity,
explained 508% of the total variance. The loadings on to the
rst factor of items 1 and 11 were negligible and items 4 and
5 were moderate (Table 2). All other items had high loadings
(i.e. > 05) on this overall factor, indicating signicant contri-
bution to the measurement of the severity construct (Table 2).
The second factor, which included the more temporal aspects,
explained 123% of the total variance. Items 1, 4, 5 and 11 all
had high loadings on this factor (Table 2).
Correlations with health-related quality of life scores
Overall, item correlations were stronger with the DLQI than
with the PHC and MHC scores (Table 3), as predicted. Corre-
lations showed inverse relationships, such that higher itch
item score was associated with lower HRQL. Correlations ran-
ged from )0169 to )0488 with the PHC, )0102 to )0414
with the MHC, and 0219 to 0546 with the DLQI.
Items 6 and 7 had moderate correlations with the PHC and
the remainder had weak correlations (Table 3). Correlations
were moderate between the MHC and items 2, 3, 6, 7, 8, 9
and 10. The remainder had weak correlations (Table 3). Item
6 had a strong correlation with the DLQI and item 1 had a
weak correlation. The other items had moderate correlations
with the instrument (Table 3).
Internal consistency reliability
Cronbachs alpha coefcients were calculated for various can-
didate item combinations. Coefcient values were very similar,
ranging from 0793 to 0827. All were above the minimum
acceptable value. These data had negligible inuence on item
selection due to the lack of considerable differences in internal
consistency reliability with varying item combinations.
Missing data
With respect to the data from this sample, six of the 11 items
had one or two missing responses. Items 1, 3 and 8 had ve
missing (54%); item 2 had six missing (65%); and item 5
had 10 missing responses (108%).
Itch Severity Scale development
Item 1 was removed based on low factor loading and weak
correlations with HRQL scores. It was also removed to elimin-
ate a potential redundancy, as this item was thought to meas-
ure an aspect similar to that measured by item 4. This is
evident by the fact that item 1 was strongly correlated with
item 4 (data not shown), more so than with any other indi-
vidual item. Items 2 and 3 were similar in content, strongly
correlated (data not shown), and both performed reasonably
well in our psychometric tests. Item 3 was chosen over item 2
in the nal questionnaire due to its higher factor loading and
stronger correlations with all HRQL scores. Item 5 was
removed based on weak correlations with PHC and MHC
scores as well as due to a concern that the question was not
easily understood as reected in the high number of missing
responses. Lastly, item 9 was chosen over item 10; both items
assessed itch intensity, but in different response formats (i.e.
Likert vs. VAS). Differences in factor loadings and correlations
with HRQL scores were deemed insufcient to warrant the
inclusion of a different response format in the new instrument
and risk potential respondent confusion.
The Itch Severity Scale
The nal ISS (Appendix 1) consists of seven of the original
11 candidate items: item 3 (itch description B), item 4
Table 2 Rotated matrix factor loadings
Factor 1 loading Factor 2 loading
Item 1 0039 0841
Item 2 0767 0388
Item 3 0806 0351
Item 4 0388 0724
Item 5 0419 0587
Item 6 0550 0485
Item 7 0754 0081
Item 8 0799 )0050
Item 9 0646 0486
Item 10 0622 0446
Item 11 0083 0723
Table 3 Candidate item correlations with instrument scores
PHC MHC DLQI
Item 1 )0169 )0102 0219*
Item 2 )0243* )0332* 0362*
Item 3 )0251* )0352* 0396*
Item 4 )0296* )0194 0307*
Item 5 )0217 )0112 0377*
Item 6 )0488* )0410* 0546*
Item 7 )0345* )0414* 0367*
Item 8 )0298* )0329* 0480*
Item 9 )0294* )0323* 0389*
Item 10 )0285* )0358* 0450*
Item 11 )0288* )0231* 0383*
PHC, physical health composite of the RAND-36 Health Status
Inventory; MHC, mental health composite of the RAND-36
Health Status Inventory; DLQI, Dermatology Life Quality Index.
*P < 005.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
670 Itch Severity Scale, C.J. Majeski et al.
(frequency), item 6 (effect on sleep), item 7 (effect on mood),
item 8 (effect on sexual desire/function), item 9 (itch intensity
using Likert scale) and item 11 (body surface area involved).
Scoring of the Itch Severity Scale
The different component responses to each of the seven ques-
tions are summed separately and divided by the highest pos-
sible total score for the respective question. The seven values
are then added together and multiplied by 3 to get a total out
of 21. Total ISS scores can range from 0 (no pruritus) to 21
(most severe pruritus).
Twelve ISS scores were missing due to incomplete question-
naires. For the 81 calculable scores in this sample, the
mean SD was 74 36, with scores ranging from 15
to 168 (Fig. 1). There were no signicant differences in
demographic characteristics between subjects with ISS scores
and those with missing scores.
Itch Severity Scale psychometric properties
The ISS scores correlated moderately with PHC scores
(r )0483) and MHC scores (r )0492) and strongly
with DLQI scores (r 0628). The ISS had an internal consis-
tency reliability of 080, and strong testretest reliability, with
a Pearsons correlation coefcient (r) of 095 and an intraclass
correlation coefcient of 095.
Interpretation of Itch Severity Scale scores
Relative to the PHC, an analogous clinically important differ-
ence in ISS scores is 2135; based on the MHC it is 1931;
and compared with the DLQI it is 2255. Overall, these indi-
cate that a clinically important difference in ISS scores is
approximately two points. Given the SD of the mean ISS score
observed in this sample (i.e. 36), this represents an effect size
estimate of approximately 056, which is consistent with effect
sizes calculated based on minimum clinically important differ-
ences of various instruments.
23
Discussion
Studies evaluating pruritus have tended to focus on the inten-
sity of itch itself, often overlooking how the symptom is per-
ceived by the patient. This is an important decit in light of
the subjective nature of itch. The assessment of severity as a
reection of subjective factors, in addition to itch intensity,
may provide a more accurate representation of the pruritus,
and hence prove to be potentially more useful in research and
clinical practice. The goal of this study was to develop such an
instrument to remedy the perceived decit.
In this study, a self-report questionnaire for the quantication
of pruritus severity, the ISS, was developed based on an inter-
viewer-administered pruritus assessment developed by Yosipov-
itch et al.
9
Our results provide initial evidence of the new
instruments construct validity, as the ISS scores had moderate
correlations with PHC and MHC scores of the RAND-36, and
strong correlations with DLQI scores, conrming our hypothesis
that itch is associated with reduced HRQL and that ISS shows a
greater correlation with the skin-specic instrument (DLQI).
Internal consistency and testretest reliability of the ISS were
above the minimum acceptable value for group-level compar-
ison. Furthermore, testretest reliability was suggestive of suf-
cient reliability for individual comparisons.
While this provides initial evidence of the psychometric
properties of the ISS, our results should be considered in the
light of several limitations. Firstly, generalizability may be lim-
ited due to the relatively tight inclusion criteria. The study
was also limited by a small sample size. Further studies are
required to add to the validity and reliability evidence of the
ISS in other samples and clinics. Additional evidence of valid-
ity should include responsiveness of the ISS to change, as one
desired function of the ISS is to assess treatment effectiveness.
It is also important for further studies to determine the
testretest reliability of the ISS as this study only estimated
testretest reliability based on responses to the modied pruri-
tus questionnaire. Lastly, a clinically important difference in
ISS scores may be reassessed to conrm or refute the observa-
tions in this sample. This would ideally be done as part of a
longitudinal study of responsiveness.
In summary, we developed the ISS which, to our know-
ledge, is the rst self-report questionnaire for the quantica-
tion of global pruritus severity. Results of the study provide
preliminary evidence of the instruments validity and reliabil-
ity. Its self-report nature and short time for completion make
it practical, convenient and applicable for use in the clinic and
through the mail. Such an instrument may be useful to com-
pare pruritus severity among different disease populations and
to assess the effectiveness of treatments for pruritus.
20 15 10 5 0
Itch Severity Scale score
14
12
10
8
6
4
2
0
F
r
e
q
u
e
n
c
y
Fig 1. Itch Severity Scale scores.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
Itch Severity Scale, C.J. Majeski et al. 671
Acknowledgments
The authors acknowledge thanks to Dr Gil Yosipovitch for
granting permission to use the questionnaire for pruritus
assessment. J.A.J. holds a Canada Research Chair and is a Health
Scholar with Alberta Heritage Foundation for Medical Research.
References
1 Gupta MA, Gupta AK, Kirkby S et al. Pruritus in psoriasis: a pros-
pective study of some psychiatric and dermatologic correlates. Arch
Dermatol 1988; 124:10527.
2 Picardi A, Abeni D, Melchi CF et al. Psychiatric morbidity in derma-
tological outpatients: an issue to be recognized. Br J Dermatol 2000;
143:98391.
3 Dahl RE, Bernhisel-Broadbent J, Scanlon-Holdford S et al. Sleep dis-
turbances in children with atopic dermatitis. Arch Pediatr Adolesc Med
1995; 149:85660.
4 Stores G, Burrows A, Crawford C. Physiological sleep disturbance
in children with atopic dermatitis: a case control study. Pediatr
Dermatol 1998; 15:2648.
5 Duque MI, Yosipovitch G, Chan YH et al. Itch, pain, and burning
sensation are common symptoms in mild to moderate chronic
venous insufciency with an impact on quality of life. J Am Acad
Dermatol 2005; 53:5048.
6 Moloney FJ, Keane S, OKelly P et al. The impact of skin disease
following renal transplantation on quality of life. Br J Dermatol
2005; 153:5748.
7 Darsow U, Scharein E, Simon D et al. New aspects of itch patho-
physiology: component analysis of atopic itch using the Eppendorf
Itch Questionnaire. Int Arch Allergy Immunol 2001; 124:32631.
8 Melzack R. The McGill Pain Questionnaire: major properties and
scoring methods. Pain 1975; 1:27799.
9 Yosipovitch G, Zucker I, Boner G et al. A questionnaire for the
assessment of pruritus: validation in uremic patients. Acta Derm
Venereol (Stockh) 2001; 81:10811.
10 Fleischer AB Jr, Rapp SR, Reboussin DM et al. Patient measurement
of psoriasis disease severity with a structured instrument. J Invest
Dermatol 1994; 102:9679.
11 Hays RD. RAND-36 Health Status Inventory. San Antonio, TX: The Psy-
chological Corporation, 1998.
12 Simon GE, Revicki DA, Grothaus L, Vonkorff M. SF-36 summary
scores: are physical and mental health truly distinct? Med Care 1998;
36:56772.
13 Taft C, Karlsson J, Sullivan M. Do SF-36 summary component
scores accurately summarize subscale scores? Qual Life Res 2001;
10:395404.
14 Johnson JA, Maddigan SL. Performance of the RAND-12 and SF-12
summary scores in type 2 diabetes. Qual Life Res 2004; 13:449
56.
15 Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)
a simple practical measure for routine clinical use. Clin Exp Dermatol
1994; 19:21016.
16 Lewis V, Finlay AY. 10 years experience of the Dermatology Life
Quality Index (DLQI). J Investig Dermatol Symp Proc 2004; 9:169
80.
17 Finlay AY, Khan GK. Dermatology Life Quality Index: Information and Condi-
tions Concerning Use. URL: http://www.dermatology.org.uk/portal/
quality/dlqiinstruc.html (accessed 12 December 2005).
18 Fayers PM, Hand DJ. Factor analysis, causal indicators and quality
of life. Qual Life Res 1997; 6:13950.
19 Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality
of life. Ann Intern Med 1993; 118:6229.
20 Hays RD, Anderson R, Revicki D. Psychometric considerations in
evaluating health-related quality of life measures. Qual Life Res 1993;
2:4419.
21 Hays RD, Morales LS. The RAND-36 measure of health-related
quality of life. Ann Med 2001; 33:3507.
22 Hongbo Y, Thomas CL, Harrison MA et al. Translating the science
of quality of life into practice: what do Dermatology Life Quality
Index scores mean? J Invest Dermatol 2005; 125:6594.
23 Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in
health-related quality of life: the remarkable universality of half a
standard deviation. Med Care 2003; 41:58292.
Appendix 1. The Itch Severity Scale
1. For each part of the day, what is the frequency of appearance of the
itch (please put an X in the box that corresponds with your answer)?
Never
itchy
Occasionally
itchy
Often
itchy
Always
itchy
Morning
Noon
Evening
Night
2. To what extent do the each of the following describe the itch
(please put an X in the box that corresponds with your answer)?
Not at all
To a small
extent
To a moderate
extent
To a great
extent
Stinging
Stabbing
Burning
Annoying
Unbearable
Worrisome
3. Please shade in the areas where you tend to be itchy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
672 Itch Severity Scale, C.J. Majeski et al.
4. Please indicate the intensity of itch for each of the following
(please put an X in the box that corresponds with your answer):
None Weak Moderate Strong
Very
strong
Itch in its
average state
Itch in its
worst state
Itch in its
best state
5. Has your mood changed because of the itch (you may circle more
than one answer)?
a. No change
b. Depressed
c. More agitated
d. Difculty in concentration
e. Anxious
6. How has itch affected the following (please put an X in the box
that corresponds to your answer)?
No change Decrease
Sexual desire
Sexual function
7. Please indicate how often any of the following happens (please put
an X in the box that corresponds with your answer):
Never Sometimes
Almost
always
Difculty falling
asleep due to itch
Awakening due
to itch
Use of sleep
medications
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp667673
Itch Severity Scale, C.J. Majeski et al. 673
CONTACT DERMATI TI S AND ALLERGY DOI 10. 1111/j . 1365- 2133. 2006. 07738. x
Double-blind, placebo-controlled study of sublingual
immunotherapy in patients with latex-induced urticaria:
a 12-month study
E. Nettis, M.C. Colanardi, A.L. Soccio, M. Marcandrea, L. Pinto,* A. Ferrannini, A. Tursi and A. Vacca
Section of Allergy and Clinical Immunology, Department of Clinical Medicine, Immunology and Infectious Diseases, University of Bari, 70124 Bari, Italy
*Department of Respiratory Physiopathology, Miulli General Hospital, Acquaviva delle Fonti, Italy
Department of Internal Medicine and Clinical Oncology, University of Bari, Bari, Italy
Correspondence
Eustachio Nettis.
E-mail: e.nettis@allergy.uniba.it
Accepted for publication
3 November 2006
Key words
double-blind placebo-controlled study, natural
rubber latex allergy, randomized controlled trial,
sublingual immunotherapy
Conicts of interest
None declared.
Summary
Background Natural rubber latex (NRL) allergy is a worldwide problem. Although
prevention is sufcient to reduce sensitization, prolonged avoidance is needed to
prevent resensitization or adverse reactions on re-exposure.
Objectives This double-blind, placebo-controlled study was conducted to determine
the efcacy of sublingual immunotherapy (SLIT) with latex.
Methods Forty patients with NRL allergy were enrolled. At diagnosis, 30 presented
urticaria and 10 asthma. Patients were evaluated on their clinical history and an
allergological assessment: skin prick test with latex extract, serum-specic IgE
and provocation tests. Patients were subdivided by complaint (asthma or urti-
caria), and randomized to receive SLIT with latex extract (ALK-Abello, Lainate,
Milan, Italy) or placebo.
Results The evaluable population consisted of 35 patients, 18 treated with SLIT
and 17 with placebo. The results show that 12 months of SLIT improved the
symptoms score and reduced the medication score in all subjects. The subjective
evaluation was corroborated by improved bronchial and glove provocation test
results. The latex-specic IgE levels increased slightly in the SLIT group, and skin
sensitization was reduced at the end of the trial in all the patients treated with
SLIT. The immunotherapy was not complicated by any severe adverse reactions.
Conclusions This is the rst double-blind, placebo-controlled evaluation of the ef-
cacy of SLIT with latex extract conducted in adult patients allergic to NRL. SLIT
with latex can be proposed for subjects with latex allergy, especially those for
whom complete avoidance of latex exposure may be very difcult or even
impossible. More studies are needed to evaluate the efcacy of SLIT in the treat-
ment of subjects with latex allergy who are sensitized to inhalant allergens.
Natural rubber latex (NRL) allergy is encountered worldwide,
although its true prevalence in the general population is esti-
mated at only about 1%. It is recognized as a major occupa-
tional problem among healthcare workers, as sensitization is
observed in 517% of those exposed.
13
Outside the health-
care environment, the people at highest risk of sensitization
due to repeated contact include glove-wearing kitchen work-
ers, housekeeping personnel,
4
workers at plants manufacturing
latex products,
5
gardeners,
6
hairdressers
7
and subjects who
have undergone multiple operations.
8
Assessment in the 1990s of the results of primary preven-
tion showed that removal of powdered latex gloves from
some areas of a hospital or the introduction of low-protein
and/or powder-free gloves was followed by a decline or ces-
sation of latex sensitization.
912
Secondary prevention in sensi-
tized/allergic individuals requires avoidance of all exposure to
NRL products because their further use, or bystander exposure
from other sources such as coworkers, could maintain or wor-
sen the sensitization and lead to potentially life-threatening
reactions. It has been demonstrated that prevention in the
work environment is sufcient to reduce sensitization.
1316
Even so, prolonged avoidance is needed to prevent resensiti-
zation or adverse reactions on re-exposure. The benets of
prevention are, in fact, limited to the duration of avoidance.
2007 The Authors
674 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
Immunotherapy against latex has recently been proposed. This
double-blind, placebo-controlled study was conducted to
determine the efcacy of sublingual immunotherapy (SLIT)
with latex extract.
Materials and methods
Forty patients with latex allergy (11 men and 29 women) aged
1847 years (mean SD 381 64) were enrolled. At diag-
nosis 30 presented urticaria and 10 asthma. Positive results were
obtained to a glove use test and a latex bronchial provocation
test in the two groups, respectively. Patients sensitized to inhal-
ant allergens were excluded, to rule out any interference of
allergies to pollen or house mites, for instance, or of intake of
any other drug, with the evaluation of symptoms.
Patients were recruited at the Department of Allergy and
Clinical Immunology of Bari Polyclinic. The study was
approved by the Ethics Committee of the University of Bari
and all patients gave their written informed consent. Patients
were evaluated on the basis of their clinical history and an
allergological assessment: skin prick test (SPT) with latex
extract, serum-specic IgE (CAP-FEIA; Pharmacia, Uppsala,
Sweden) and provocation tests. They were free from other res-
piratory allergies, had not received specic immunotherapy in
the previous 5 years, and had no other signicant disorders or
chronic/severe asthma.
Patients were subdivided into two groups: those with
asthma and those with urticaria, and were randomized by a
computer-generated list to receive SLIT with latex extract or
placebo. The latex extracts used for immunotherapy and
placebo were manufactured and provided by ALK-Abello
(Lainate, Milan, Italy).
Allergological evaluation
Skin prick tests
SPTs were performed with ALK-Abello latex extract, undiluted
and diluted 1 : 1000, 1 : 100, 1 : 10 in a glycerol-saline
solution. Additional SPTs were performed with food and com-
mon inhalant allergens. The food extracts included avocado,
banana, pineapple, kiwi and chestnut (Stallerge`nes, Paris,
France; Lofarma, Florence, Italy). The inhalant extracts inclu-
ded Dermatophagoides pteronyssinus and D. farinae, grass pollen, olive
pollen, cypress pollen, Parietaria, Artemisia vulgaris, cat dander,
dog dander, Alternaria tenuis and Aspergillus. Histamine dihydro-
chloride (10 mg mL
)1
) was used as positive control, and
physiological saline as negative control. An SPT was consid-
ered positive if the mean diameter of the weal was 3 mm
larger than the weal of the negative control. The latex SPT
was performed at baseline and after 6 months and 12 months.
Serum-specic IgE
Measurement of serum-specic IgE to NRL (Pharmacia CAP
system, RAST FEIA, Uppsala, Sweden) was carried out under
standard conditions, as recommended by the manufacturer. A
positive RAST was dened as a value > 035 kU L
)1
. This test
was performed at baseline and after 6 months and 12 months.
Glove provocation test
The same batch of NRL gloves was used for the glove use test
at baseline and after 12 months (Le Petit; Grandate, Como,
Italy). A ngertip cut from a glove was placed on one nger
for 30 min. If the reaction was negative, a whole glove was
then worn for 30 min. If the reaction was still negative, the
whole glove was worn for 60 min.
16
A vinyl glove was used as control. A positive response was
recorded when itching, redness or contact urticaria appeared
on the nger or hand, or systemic reactions developed. Symp-
toms were scored 1 for local itching without any other mani-
festations, 2 for redness, 3 when weals became apparent, and
4 if any systemic reaction appeared. The glove use test was
performed at baseline and after 12 months.
Latex bronchial provocation test
This was performed according to Pisati et al.
17
Patients were
initially exposed to 2 mL of glycerol-saline solution nebulized
in a 7 m
3
challenge room up to 15 min to ensure that uctu-
ations of forced expiratory volume in 1 s (FEV
1
) were < 10%.
On the next day, ALK-Abello latex was rstly nebulized in the
same room. The patients then entered and remained there for
15 min, except in the event of earlier onset of wheezing and
a 15% fall in FEV
1
with respect to the baseline value. After
exposure, FEV
1
was monitored at 5, 10, 15, 30, 60, 90 and
120 min; if the fall in FEV
1
was < 15%, the patient under-
went the next scheduled nebulization. Each time, 2 mL of
solution was delivered and the concentration of nebulized
extract was increased 10-fold. The initial concentration was a
10-fold dilution of the predetermined skin-test endpoint in
the individual undergoing challenge, and the highest concen-
tration was the undiluted extract. If any nebulization caused a
15% fall in the FEV
1
, no further exposure was conducted
and FEV
1
was monitored hourly for 8 h, and nally after
24 h. FEV
1
measurements were carried out at the same pre-
established times when the highest concentration was reached
without a 15% fall. A latex bronchial provocation test was
performed at baseline and after 12 months.
Immunotherapy protocol
Treatment consisted of ve concentrations of ALK-Abello latex:
5 10
)8
, 5 10
)5
, 5 10
)2
, 5 and 500 lg mL
)1
(Table 1).
The placebo preparation was identical to the active treatment
in terms of composition, appearance, presentation, taste and
colour. A 4-day sublingual induction phase was followed by a
12-month maintenance phase consisting of three administra-
tions per week. In view of the doses employed, dose incre-
ments were supervised in hospital in the presence of a
physician.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
Immunotherapy with latex, E. Nettis et al. 675
SLIT with latex extract was administered to the patient by
the same doctor. Maintenance doses were self-administered at
home in accordance with the detailed instructions provided by
the physician. The drops were always held under the tongue
for 3 min before being swallowed. Patients recorded all doses
in a diary.
Safety of immunotherapy
Patients were asked to keep a record of any side-effect or sus-
pected adverse event that might be related to SLIT, together
with its time of onset and treatment (if any). Reactions were
classed as systemic (asthma, rhinitis, urticaria, angio-oedema,
generalized itching, diarrhoea and vomiting) and local (oral
itching/swelling, oedema of the tongue). Patients were
instructed to contact the centre if they needed medical advice.
All patients were included in the side-effect analysis.
Latex avoidance
After enrolment and before the beginning of immunotherapy,
all patients were informed of the hazards of NRL allergy and
given oral instruction on preventive measures, as well as a
written handout. They were particularly advised to avoid
exposure to NRL in occupational settings and, whenever pos-
sible, at home and to use gloves made of vinyl, polyurethane
and neoprene. Instruction comprised information on latex-
containing products frequently used in daily life (such as
clothes, condoms, air mattresses) and latex-free alternatives.
Patients were instructed to inform physicians of the require-
ment to perform any necessary surgical and medical proced-
ures in a latex-free environment. Risk factors, signs and
symptoms of latex allergy ranging from contact urticaria to
anaphylactic shock were explained. Particular emphasis was
laid on the hazardous forms of exposure, such as anaesthesia,
condoms and other forms of mucosal contact, and avoidance
of cross-reacting foods (kiwi, chestnut, banana, avocado and
pineapple) was recommended.
At diagnosis, ve healthcare workers were employed in the
operating room, two in the emergency room, two in the
obstetric and gynaecology unit, and two in the cardiology
unit. After diagnosis, of the 11 healthcare workers, nine
changed department, while two (belonging to the SLIT group)
changed their job title: three subjects now worked in a central
administration ofce, three in the ambulatory of a neurology
unit, two in the administration ofce of a cardiology unit,
one in a spirometry laboratory, and two in a hospital phar-
macy. After diagnosis, two hairdressers (one from each group)
stopped working.
Diary cards
Patients recorded their daily symptoms: bronchial (cough,
wheezing and shortness of breath), ocular (swelling, itching,
and watery eyes), nasal (itching, sneezing, congestion and
rhinorrhoea) and skin related (itching, redness and weals) on
a scale ranging from 0 (absent) to 3 (severe), as well as their
daily use of medication: one point for antihistamines, one
point for inhaled b
2
-agonists, two points for topical cortico-
steroids and three points for oral corticosteroids. All patients
received appropriate on-demand therapy to control their aller-
gic symptoms in case of exposure to latex or ingestion of
cross-reactive foods. The total symptoms and medication
scores were calculated as means per week. The efcacy of the
treatment was assessed after 6 and 12 months by calculating
the mean scores for weeks 2426 and weeks 5153, respect-
ively, while the baseline evaluation was referred to the
3 weeks before starting the immunotherapy or placebo.
At baseline, 6 months and 12 months, patients also comple-
ted a 10-cm visual analogue score (VAS) indicating the overall
severity of their latex allergy over the previous days, from 0
(none) to 10 (worst).
Table 1 Treatment schedule
Day Vial
Protein concentration
(lg mL
)1
) Drops
Cumulative
dose (lg)
Interval
between doses
Induction phase
1 0 5 10
)8
1 2 10
)5
15 min
10 15 min
1 5 10
)5
1 15 min
10 15 min
2 2 5 10
)2
1 22 15 min
10 15 min
3 5 1 15 min
10 15 min
3 4 500 1 400 15 min
2 15 min
3 15 min
4 15 min
10 15 min
4 4 25 500 15 min
Maintenance phase 4 5 100 2 days
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
676 Immunotherapy with latex, E. Nettis et al.
Statistical analysis
The signicance of differences in age, sex, baseline characteris-
tics and test results was compared using the MannWhitney
test and v
2
test for categorical data. For the efcacy analyses
and comparison of the VAS in each study group and at differ-
ent visits, the Wilcoxon matched-pair test was used. To com-
pare the efcacy and the VAS in the two groups at different
visits the MannWhitney test was performed. P < 005 was
taken as signicant.
Results
The 40 patients were randomized, 20 were treated with SLIT
(14 women and six men) and 20 with placebo (15 women
and ve men). The two groups were matched for age and
sex, serum concentrations of latex-specic IgE and SPT results.
Two patients in the SLIT and three patients in the placebo
group discontinued treatment within the rst 8 weeks owing
to noncompliance (n 3), lack of efcacy (n 1) and
change of residence (n 1).
The evaluable population thus consisted of 35 patients.
Their demographic and baseline characteristics were also well
matched. Dropouts were excluded from the analysis because
of their short treatment duration.
Allergological evaluations
Skin prick tests
At diagnosis all patients had positive SPTs with NRL extract
and there was no signicant difference between the SLIT and
the placebo group. At 6 months, in the SLIT group there was
a signicant difference in terms of a stronger concentration of
latex extract needed to produce a positive weal, as compared
with the baseline response. In addition, there was a signicant
decrease in mean weal diameter in patients with the same
end-point titre as compared with baseline (mean diameter
69 mm vs. 41 mm, range 3585 mm vs. 3065 mm;
P < 005).
At 12 months, the signicant concentration difference
persisted and there was a further difference in mean weal
diameter in patients with the same end-point titre (mean
diameter 77 mm vs. 32 mm, range 6585 mm vs. 30
35 mm; Fig. 1). In the placebo group, skin reactivity to the
extract was signicantly decreased only at 12 months
(P < 005).
Comparison between the two groups thus showed a nonsig-
nicant difference in terms of a decrease of latex SPT positivi-
ty, evaluated as an increased concentration by at least 10-fold,
after 6 months and after 12 months of treatment (P > 005
and P 005, respectively).
At diagnosis, there were no IgE-positive results in the inhal-
ant extracts, whereas 10 of 35 patients (29%), including four
in the SLIT group, had one or more positive IgE tests to cross-
reactive food extracts.
Serum-specic IgE
There were no signicant changes in specic latex serum IgE
concentrations either in the SLIT group or the placebo group.
At 6 months, a nonsignicant increase in IgE levels from 167
to 19 kU L
)1
was observed in the SLIT group; the levels
decreased to 172 kU L
)1
at 12 months. Specic IgE was not
detectable in one patient.
In the placebo group, a nonsignicant decrease was found
both at 6 months and at 12 months (161 kU L
)1
at baseline,
152 kU L
)1
at 6 months, 119 kU L
)1
at 12 months).
Glove provocation tests
Initially, 28 subjects (80%) (14 in each group) had a local
latex reaction: 12 with the ngertip, 16 with the whole glove.
All reactions appeared within 60 min. There were no signi-
cant differences between the groups (reaction onset after a
mean of 423 min vs. 454 min in the SLIT and placebo
group, respectively; P > 005). Eight of 28 patients (29%)
(four placebo and four SLIT) experienced a systemic reaction.
At 12 months a longer exposure was needed to provoke a
reaction in the SLIT group (mean 85 min; P < 005): only
two of 14 patients (14%) had a reaction in the rst 60 min
compared with 60120 min in the other 12 of 14 (86%).
There was also a signicant decrease in the mean score (34
vs. 18; P < 005). A systemic reaction developed in only two
cases.
In the placebo group, the mean score decrease (35 vs. 29)
was not signicant, whereas there was a signicant increase in
the exposure time as compared with baseline (mean 454 min
vs. 615 min). However, this increase was lower than the cor-
responding increase in the SLIT group (P < 005). In ve of
14 subjects (36%) the reaction developed between 30 and
0
2
4
6
8
10
12
14
16
N
o
.
s
u
b
j
e
c
t
s
6 months* 12 months*
SLIT
Placebo
P > 005
P = 005
Fig 1. Decrease of latex skin prick test positivity, evaluated as an
increased concentration by at least 10-fold needed to trigger
a reaction, after 6 months and after 12 months of treatment.
*As compared with baseline, two subjects in the sublingual
immunotherapy (SLIT) group yielded negative results, one at the
6-month evaluation and one at 12 months.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
Immunotherapy with latex, E. Nettis et al. 677
60 min and in nine of 14 (64%) between 60 and 120 min.
Three of the four patients who had initially displayed a sys-
temic reaction continued to do so at 12 months. At the
12-month evaluation there was a signicant difference in the
scores between the two groups (Fig. 2).
Latex bronchial provocation test
At the initial examination, this test was positive in four
patients in the SLIT group and three subjects in the placebo
group. In the SLIT group, one patient reacted to the 1 : 100
dilution, FEV
1
decreasing 5 min after exposure, two reacted to
the 1 : 100 dilution, FEV
1
decreasing 30 min after exposure,
and one patient reacted to the 1 : 1000 latex dilution, FEV
1
decreasing 15 min after exposure.
In the placebo group, one patient reacted to the 1 : 100
dilution, FEV
1
decreasing 10 min after exposure, one reacted
to the 1 : 100 dilution, FEV
1
decreasing 15 min after expos-
ure, and one patient reacted to the 1 : 1000 dilution, FEV
1
decreasing 10 min after exposure.
At 12 months, a stronger concentration was needed to pro-
voke a 15% FEV
1
fall in the SLIT group: two of three
patients previously positive at 1 : 100 now displayed a 15%
FEV
1
fall at 15 and 30 min after exposure to the 1 : 10 dilu-
tion, and the other patient at 30 min after exposure to the
1 : 1 dilution. The fourth patient (previously positive at
1 : 1000) now displayed a FEV
1
decrease at 15 min after
exposure to the 1 : 100 dilution.
Two of the positive patients in the placebo group displayed
a longer interval between exposure and the FEV
1
fall: their
reaction to the 1 : 100 dilution occurred after 30 min,
whereas in the third patient it occurred after 15 min at
1 : 100 dilution (Table 2). There were no > 10% falls of
FEV
1
following exposure to the glycerol-saline solution, either
at baseline or at 12 months. The number of patients is too
limited for reliable statistical analysis to be performed.
Safety of immunotherapy
Four of 35 patients (11%) [three of 18 in the SLIT group
(17%) and one of 17 in the placebo group (6%)] developed
adverse reactions. Two patients in the SLIT group reported
mouth itching and burning and the third reported an episode
of swelling of the lips. These side-effects occurred during the
induction phase and regressed spontaneously. In the placebo
group, one patient reported an asthma episode.
Diary cards
Symptoms scores and medication scores, assessed at baseline
and reported as the mean of the three previous weeks, were
not signicantly different between the two groups (P > 005).
At 6 months, the total symptoms score had decreased by
574% in the SLIT group and 389% in the placebo group
(P > 005). These decreases were signicant as compared with
baseline (P < 005). After 12 months, the score had decreased
by 887% and 43% as compared with baseline, in the active
and placebo groups (P < 005); again, this value was signi-
cant with respect to the 6-month value only in the SLIT group
(P < 005) (Fig. 3). Comparing the two treatment groups, a
0
05
1
15
2
25
3
35
S
c
o
r
e
,
m
e
a
n
Baseline 12 months
SLIT
Placebo
P > 005
P < 005
Fig 2. Changes in the glove use test score in the sublingual
immunotherapy (SLIT) and placebo groups.
Table 2 Latex bronchial provocation test at
baseline and after 12 months of treatment
Baseline 12 months
Patient Positive dilution Exposure (min) Positive dilution Exposure (min)
SLIT group
1 1 : 100 5 1 : 10 15
2 1 : 100 30 1 : 10 30
3 1 : 100 30 1 : 1 30
4 1 : 1000 15 1 : 100 15
Placebo group
1 1 : 100 10 1 : 100 30
2 1 : 100 15 1 : 100 30
3 1 : 1000 10 1 : 100 15
SLIT, sublingual immunotherapy with latex extract.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
678 Immunotherapy with latex, E. Nettis et al.
statistically signicant difference was present at the 12-month
assessment (153 vs. 36; P < 005).
After 6 months, the medication score was signicantly
reduced by 482% in the SLIT group, and a signicant reduc-
tion was also noted in the placebo group (P < 005). There
was no signicant difference between the two groups
(P > 005). Instead, at 12 months the score was signicantly
reduced in the SLIT group ()889%) with respect to the base-
line, the 6-month assessment and the 12-month assessment
values in the placebo group (P < 005) (Fig. 4). In contrast,
in the placebo group, there was no statistical difference at the
12-month assessment as compared with the 6-month, whereas
there was a signicant difference between the 12-month
evaluation and baseline.
There was a signicant improvement in the VAS in the SLIT
group: a mean decrease by 494% after 6 months and 741%
after 12 months (P < 005). These percentages falls were
greater (but reaching statistical signicance only after
12 months) than the corresponding decreases as compared
with baseline in the placebo group, which were 422% and
448%, respectively.
Discussion
This is the rst double-blind, placebo-controlled evaluation of
the efcacy of SLIT conducted in adult patients allergic to
NRL, with cutaneous and respiratory manifestations. Our
results show that 12 months of SLIT improved the symptoms
score and reduced the medication score in the treated subjects.
A self-evaluation of efcacy is not proposed in many trials.
We used a VAS, which is a crude and subjective criterion. We
therefore correlated it with other parameters and found a cor-
relation between the VAS and the global symptoms and medi-
cation score. The subjective evaluation was also corroborated
by the improved bronchial and glove provocation test results.
The NRL-specic IgE levels did not change signicantly in
either group, conrming previous results obtained in trials
with NRL subcutaneous immunotherapy and SLIT performed
in children.
18,19
The slight increase in the SLIT group contrasts
with the decrease in the placebo group, as reported in other
studies.
20
It may thus be deduced that there is no uniform
correlation between latex-specic IgE and the symptoms and
medication scores in these groups.
Skin sensitization was reduced in all the patients in the SLIT
group at the end of the trial: 15 of 18 (83%) showed at least
a 10-fold reduction of SPT reactions to NRL extract, whereas
three of 18 (17%) showed a decrease only in the SPT weal
mean diameter. However, although SPT results are regarded as
a parameter of immunotherapy efcacy, skin and mucosal
mast cells do not appear to behave in a similar fashion.
The glove use test and bronchial provocation test are valid
ways of quantifying NRL sensitivity, and have thus been used,
with some modications, in other studies of the efcacy of
latex immunotherapy.
18,21,22
Our ndings demonstrate an
increased threshold dose in the bronchial test and a more pro-
longed exposure time (more frequent in the SLIT group) to
trigger a reaction, substantiating the efcacy of the immuno-
therapy.
In the placebo group, there was a decrease in both the sub-
jective and the objective parameters used to evaluate NRL
allergy. This could be explained by the fact that because latex
allergy can be life threatening, and all patients had reported
adverse reactions, sometimes severe, to NRL at the beginning
of the study, we had carefully instructed them about how to
avoid exposure to latex. As in previous studies, prevention
induced a reduction of sensitization, but not enough to
impede resensitization or adverse reactions on re-exposure.
16
We studied a selected, small group of subjects with latex
allergy, i.e. monosensitized patients, excluding individuals sen-
sitized to inhaled aeroallergens. This could represent a selection
bias in the study because it is well known that atopy is consid-
ered a risk factor for latex allergy. However, this allowed us to
refer the improvements in the medication score and symptoms
score, and the differences between the two study groups, only
to the immunotherapy and to latex avoidance.
Both in the SLIT group and the placebo group, the fact that
symptoms were present and medication was necessary
throughout the study implies that latex avoidance was not
Symptoms score
0
5
10
15
20
25
30
35
1593
1
7
1
1
2
5
2
9
2
3
3
7
3
1
4
5
4
9
4
3
5
Weeks
M
e
a
n
v
a
l
u
e
SLIT
Placebo
Fig 3. Symptoms score in relation to time (53 weeks). SLIT,
sublingual immunotherapy.
Medication score
0
1
2
3
4
5
6
7
8
9
1593
1
7
1
1
2
5
2
9
2
3
3
7
3
1
4
5
4
9
4
3
5
Weeks
M
e
a
n
v
a
l
u
e
SLIT
Placebo
Fig 4. Medication score in relation to time (53 weeks). SLIT,
sublingual immunotherapy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
Immunotherapy with latex, E. Nettis et al. 679
strictly adhered to, especially in non-healthcare environments.
The fact that the efcacy measures showed a signicant differ-
ence between the two treatment groups only at 12 months
could suggest that up to 6 months, the effects of latex avoid-
ance and latex-specic immunotherapy are similar, while in
later months the benecial effects should be attributed pre-
dominantly to the immunotherapy.
The efcacy of immunotherapy in this setting has not
received much attention.
18,2124
Initially, case reports showed
that both subcutaneous immunotherapy and SLIT were very
effective and all exposure tests yielded negative results.
21,22
Controlled studies using subcutaneous protocols and rush SLIT
have since been performed.
18,23,24
Studies of subcutaneous
immunotherapy have conrmed its feasibility as a means of
inducing tolerance, especially in severely affected subjects,
including heathcare workers, for whom no other causative
treatment can be offered, and allergen avoidance is not always
possible. However, these studies are burdened by a high rate
of adverse events due to the use of unfractionated latex
extracts. In any event, life-threatening reactions are very rare,
and none was observed in our study.
Rolland et al.
25
have proposed the selection of hypoallergenic
preparations for subcutaneous immunotherapy to avoid the risk
of adverse events. They describe the progress made in develop-
ing hypoallergenic preparations of the major latex allergens
Hev b 5 and Hev b 601. Future immunotherapy should target
allergenic components known to cross-react with homologous
proteins in fruits and vegetables, to prevent adverse reactions on
exposure to these substances. The nding that Hev b 601 is one
of the most important allergens in healthcare workers was con-
rmed by Sastre et al.
26
In addition, they reported a signicant
negative correlation between the maximum tolerated dose and
specic IgE to Hev b 601 at baseline, so the levels of specic
IgE to Hev b 601 might predict the maximum tolerated dose of
allergen during immunotherapy.
The only previous study among adults which used a sub-
lingual route, as we have done, was conducted in 12 patients,
but was not a double-blind, placebo-controlled trial.
23
Even
so, it showed that during 3 months of follow up there were
no adverse events and all patients developed a clinical toler-
ance to NRL, characterized by a surprising reduction by 100%
of reactions to cutaneous, mucous and sublingual challenge.
SPT variations were not evaluated. On the other hand, surpris-
ingly, serum-specic IgE decreased in 583% of patients. How-
ever, this was observed in a 3-month study and cannot be
compared with our 12-month trial.
In conclusion, SLIT reduces the symptoms in patients with
NRL allergy. As this therapy is not complicated by severe
adverse reactions, a build-up phase, conducted under medical
supervision, can safely be followed by continuation of ther-
apy at home. It can thus be proposed for subjects with NRL
allergy, especially those for whom complete avoidance to
latex exposure may be very difcult. Nevertheless, in any
case, all latex-allergic subjects should be strongly advised of
the extreme importance of avoiding exposure to latex. More
studies are needed to evaluate the efcacy of SLIT in the
treatment of latex allergy subjects sensitized to inhalant
allergens.
Acknowledgments
This study was partly funded by a grant from the Regione
Puglia which was used to buy treatments from ALK-Abello.
The authors wish to thank Dr. ssa Silvia Pecora for her
corporation.
References
1 Charous B. The puzzle of latex allergy: some answers, still more
questions. Ann Allergy 1994; 73:27781.
2 Vandenplas O, Charous B, Tarlo S. Latex allergy. In: Asthma in the
Workplace (Bernstein D, Bernstein I, Chan-Yeung M, Malo JL, eds),
2nd edn. New York: Marcel Dekker, 1994; 42544.
3 Nettis E, Assennato G, Ferrannini A, Tursi A. Type I allergy to nat-
ural rubber latex and type IV allergy to rubber chemicals in health
care workers with glove related skin symptoms. Clin Exp Allergy
2002; 32:4417.
4 Sussman GL, Lem D, Liss G, Beezhold D. Latex allergy in house-
keeping personnel. Ann Allergy Asthma Immunol 1995; 74:41518.
5 Tarlo SM, Wong L, Roos G, Booth N. Occupational asthma caused
by latex in a surgical glove manufacturing plant. J Allergy Clin Immunol
1990; 85:62631.
6 Carrillo T, Blanco C, Quiralte J et al. Prevalence of latex allergy
among greenhouse workers. J Allergy Clin Immunol 1995; 96:699
701.
7 Nettis E, Dambra P, Soccio AL et al. Latex hypersensitivity: relation-
ship with positive prick test and patch test responses among hair-
dressers. Allergy 2003; 58:5761.
8 Nettis E, Dambra P, Soccio AL et al. Type I allergy to natural rubber
latex and type IV allergy to rubber chemicals in children with risk
factors. Contact Dermatitis 2001; 44:1812.
9 Sussman GL, Liss GM, Deal K et al. Incidence of latex sensitisa-
tion among latex glove users. J Allergy Clin Immunol 1998; 101:171
8.
10 Turjanmaa K, Reinikka-Railo T, Reunala T, Palouso T. Continued
decrease in natural rubber latex (NRL) allergen levels of medical
gloves in nationwide market surveys in Finland and co-occurring
decrease in NRL allergy in a large university hospital. J Allergy Clin
Immunol 2000; 104:S373 (Abstract).
11 Tarlo SM, Easty A, Eubanks K et al. Outcomes of a natural rubber
latex control program in an Ontario teaching hospital. J Allergy Clin
Immunol 2001; 108:62833.
12 Liss GM, Tarlo SM. Natural rubber latex-related occupational
asthma: association with interventions and glove changes over
time. Am J Ind Med 2001; 40:34753.
13 Allmers H, Brehler R, Chen Z et al. Reduction of latex aeroallergens
and latex specic IgE antibodies in sensitised workers after removal
of powdered natural rubber latex gloves in a hospital. J Allergy Clin
Immunol 1998; 102:8416.
14 Hamilton RG, Brown RH. Impact of personal avoidance practices
on health care workers sensitised to natural rubber latex. J Allergy
Clin Immunol 2000; 105:83941.
15 Turjanmaa K, Kanto M, Kautianen H et al. Long-term outcome of
160 adult patients with natural rubber latex allergy. J Allergy Clin
Immunol 2002; 110:S704.
16 Nettis E, Colanardi MC, Ferrannini A. Type I latex allergy in health
care workers with latex-induced contact urticaria syndrome: a
follow-up study. Allergy 2004; 59:71823.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
680 Immunotherapy with latex, E. Nettis et al.
17 Pisati G, Barufni A, Bernabeo F, Stanizzi R. Bronchial provocation
testing in the diagnosis of occupational asthma due to latex surgi-
cal gloves. Eur Respir J 1994; 7:3326.
18 Sastre J, Fernandez-Nieto M, Rico P et al. Specic immunotherapy
with a standardized latex extract in allergic workers: a double-blind,
placebo-controlled study. J Allergy Clin Immunol 2003; 111:98594.
19 Bernardini R, Campodonico P, Burastero S et al. Sublingual immu-
notherapy with a latex extract in paediatric patients: a double-blind,
placebo-controlled study. Curr Med Res Opin 2006; 22:151522.
20 Bousquet J, Scheinmann P, Guinnepain MT et al. Sublingualswal-
low immunotherapy (SLIT) in patients with asthma due to house-
dust mites. A double-blind, placebo-controlled study. Allergy 1999;
54:24960.
21 Nucera E, Schiavino D, Buonomo A et al. Latex rush desensitization.
Allergy 2001; 56:867.
22 Pereira C, Rico P, Lourenco M et al. Specic immunotherapy for
occupational latex allergy. Allergy 1999; 54:2913.
23 Patriarca G, Nucera E, Pollastrini E et al. Sublingual desensitization:
a new approach to latex allergy problem. Anesth Analg 2002;
95:95660.
24 Leynadier F, Herman D, Vervloet D, Andre C. Specic immuno-
therapy with a standardized latex extract versus placebo in
allergic healthcare workers. J Allergy Clin Immunol 2000; 106:585
90.
25 Rolland JM, Drew AC, OHehir RE. Advances in development of
hypoallergenic latex immunotherapy. Curr Opin Allergy Clin Immunol
2005; 5:54451.
26 Sastre J, Raulf-Heimsoth M, Rihs HP et al. IgE reactivity to latex
allergens among sensitized healthcare workers before and after
immunotherapy with latex. Allergy 2006; 61:20610.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp674681
Immunotherapy with latex, E. Nettis et al. 681
DERMATOLOGI CAL SURGERY AND LASERS DOI 10. 1111/j . 1365- 2133. 2006. 07714. x
Application of topical mitomycin C to the base of
shave-removed keloid scars to prevent their recurrence
J.N.R. Bailey, A.E. Waite, W.J. Clayton and M.H.A. Rustin
Department of Dermatology, The Royal Free Hospital, London NW3 2QG, U.K.
Correspondence
Jane Bailey.
E-mail: janeNR.Bailey@btopenworld.com
Accepted for publication
16 October 2006
Key words
collagen, broblast, keloid, mitomycin C
Conicts of interest
None declared.
Summary
Background Keloid scars are formed by over-activity of broblasts producing colla-
gen and they cause signicant morbidity both from their appearance and from
their symptoms. Existing treatments are often unsatisfactory. Topical mitomycin
C is known to inhibit broblast proliferation.
Objectives To determine whether application of mitomycin C to the base of shave-
removed keloids would prevent their recurrence.
Methods Ten patients had all or part of their keloid shave-removed. After haemo-
stasis topical mitomycin C 1 mg mL
)1
was applied for 3 min. This application
was repeated after 3 weeks. The keloids were photographed before treatment and
the patients were reviewed every 2 months for a total of 6 months when a nal
photograph of the keloid site was taken. The patients and the Clinical Trials Unit
staff scored the outcome on a linear analogue scale of 010, where 0 dis-
appointed and 10 delighted. The pretreatment and 6-month post-treatment
photographs were also assessed by two dermatologists who were not involved in
the clinical trial.
Results Four of the 10 patients were delighted with the outcome of treatment and
only one was disappointed. On average there was an 80% satised outcome.
Conclusions This new treatment of keloids has been shown to be effective in the
majority of patients but further studies are required to conrm this benet.
Keloids are scars that expand beyond the boundaries of the
original injury as they heal. Histologically there is excessive
accumulation of hyalinized collagen which is thought to arise
from intrinsically normal broblasts responding to an abnor-
mal extracellular signal. Transforming growth factor (TGF)-b
isoforms play a central role in wound healing and brosis and
have been implicated in the pathogenesis of keloids. Indeed,
cultured keloid broblasts have shown increased production
of type I collagen and matrix metalloproteinases regulated by
TGF-b1.
1
Keloids cause signicant morbidity as they are unsightly
and uncomfortable, causing tightness, tenderness and itching,
and impair quality of life.
2
Current treatments include topical
or intralesional steroids,
3
cryotherapy,
4
application of silicone
gel,
5
surgery followed by low-dose radiotherapy, electron
beam irradiation,
6
pulsed dye lasers,
7
high dose rate brachy-
therapy,
8
intralesional bleomycin,
9,10
intralesional 5-uoroura-
cil,
11
and topical imiquimod.
12,13
Interferon alfa-2b, topical
tacrolimus, botulinum toxin and verapamil have also been
tried.
14
Combination therapy is often used; however, no treat-
ment for keloids can produce predictable results.
15
Mitomycin C is an antineoplastic antibiotic. It is an alkylat-
ing agent which inhibits DNA synthesis by forming a cross-
linkage of strands of double helix so that the neoplastic cells
cannot proliferate. It inhibits cell division, broblast prolifer-
ation, protein and collagen synthesis and neoangiogenesis.
This has been demonstrated in vitro
16
and in vivo using the rat
model.
17
In vitro it was shown that by the third week after
application there was a recovery in DNA synthesis and
increased cell count for some of the treated broblasts. In this
study, therefore, topical mitomycin C was re-applied 3 weeks
after the initial application.
Topical mitomycin C has been used in ophthalmology for
over 20 years, during trabeculectomy for glaucoma
18
and in
the treatment of pterygium.
19
Very low concentrations of
mitomycin C (002005 mg mL
)1
) are required in the eye.
20
Initially there were complications with scleral necrosis when
higher concentrations (04 mg mL
)1
) were used.
21
Intraopera-
tive adjunction of mitomycin C during fornix reconstruction
with amniotic membrane resulted in a deeper fornix in 83%
of patients with various causes of cicatrizing conjunctivitis.
22
For the last 5 years mitomycin C has been used in oto-
laryngology to prevent scarring after surgery for laryngeal and
tracheal stenosis
23,24
and choanal atresia.
25
Topical mitomycin
C 04 mg mL
)1
applied for 5 min in a laser-induced injury of
the posterior glottis in rabbits signicantly prevented the gross
2007 The Authors
682 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp682686
injury and subsequent increased collagen content and broblast
proliferation compared with sham-treated controls.
26
There
was also a report at the dermatology section of the Royal Soci-
ety of Medicine of its successful use for the treatment of laryn-
geal mucous membrane pemphigoid after laser therapy.
27
The
only adverse effect was reported recently in otolaryngology
when mitomycin C was used as an adjuvant after CO
2
laser
endoscopic treatment and dilation for upper airway stenosis.
28
Fibrinous debris related to complete broblast inhibition or
cytotoxicity accumulated at the operative site, resulting in
partial airway obstruction and the need for emergency air-
way intervention. Mitomycin C 04 mg mL
)1
was used in 71
cases and only 28% had this complication. Mitomycin C
10 mg mL
)1
was used in 14 recalcitrant cases and 143% had
this complication. However, this occurred in an airway on a
mucosal surface and may not be relevant in dermatology.
There have been two reports of mitomycin C being used as
a treatment for keloids but in both the keloids were excised
and mitomycin C 04 mg mL
)1
was applied for 5 min prior
to skin closure. In the rst paper the authors concluded that
this was an effective treatment.
29
However, in the second
study the mitomycin C did not prevent keloid recurrence.
30
The U.S. Food and Drug Administration usually restricts the
concentration of topical mitomycin C to 04 mg mL
)1
. In
European otolaryngology departments concentrations of
24 mg mL
)1
are being used, usually applied for 2 min.
Although no large studies have yet been carried out, there is
anecdotal evidence that these higher concentrations may be
more effective (Bailey CM, personal communication, 2006).
However, there does not yet appear to be a consensus on
either the concentration or time of application of mitomycin
C. In view of the possible reduced efcacy of mitomycin C
04 mg mL
)1
, a dose of 1 mg mL
)1
was chosen and applied
for 3 min. It was also decided to undertake shave rather than
formal excision of the keloid.
Materials and methods
Ten patients with keloid scars were recruited from dermatol-
ogy outpatients; all but one had had previous unsuccessful
treatments including potent topical steroids. Eight had had
intralesional steroid injections sometimes preceded by cryo-
therapy, and four of these had also tried silicone gel. In add-
ition, three of these four had been treated with pulsed dye
laser treatment and one with low-dose radiotherapy, as
detailed in Table 1. The most recent previous pulsed dye laser
treatment was the sixth session in patient 10 at 6 weeks
before the mitomycin C study and the ninth session in patient
1 at 11 weeks previously. Patient 2 received an intralesional
steroid injection 11 weeks before the study. However, these
treatments had not produced any signicant improvement.
Ethics Committee approval for this study had been granted.
Patients had to read and understand an information sheet
about mitomycin C and the procedure, and only then was
informed written consent obtained. Women of childbearing
age were required not to be pregnant or to conceive during
the study and sexually active patients, both male and female,
were instructed to use effective contraception. There was no
control group as the high risk of a worse recurrence if the
keloid had been shaved off without application of mitomycin
C was not considered ethically acceptable.
The keloid selected for treatment was photographed before
surgery. Local anaesthetic (1% xylocaine) was injected under
and around the keloid, and all, or part of it if extensive, was
shave-removed level with the surrounding skin. Haemostasis
was achieved with hyfrecation. Mitomycin C Kyowa
TM
(Kyo-
wa Hakko Kogyo, Tokyo, Japan) 1 mg mL
)1
was made up in
the hospital Cytotoxic Pharmacy by diluting a vial containing
10 mg mitomycin C, a purple powder, with 10 mL of sterile
water, and 2 mL was provided in a syringe for each patient
and the usual cytotoxic precautions were taken. Four layers of
gauze cut to the shape of the scar were laid over the wound
and the mitomycin C was applied from a syringe until the
gauze became saturated. This required 032 mL, depending
on the size of the lesion. The gauze was gently pressed on for
3 min and, following removal, the site was patted dry and a
dry dressing applied. Patients were instructed to re-dress the
site as necessary and to keep it dry for as long as possible.
Three weeks later any crust was removed. The removal
of this was aided if necessary by soaking with saline on gauze
Table 1 Patient demographics
Patient
Sex/age
(years) Site of keloid Ethnic group Previous treatments
1 F/54 Presternal Oriental ILS/SG/PDL
2 M/34 Upper arm Caucasian ILS
3 M/43 Postauricular South American ILS
4 F/42 Posterior ear lobe Afro-Caribbean ILS/shave removal regrew
5 M/43 Posterior neck Asian Shave removal regrew
6 M/41 Posterior neck Asian None
7 M/42 Presternal Middle Eastern ILS/SG/RTX
8 F/40 Presternal Oriental ILS/SG/PDL
9 F/39 Presternal Mixed ILS
10 M/45 Presternal Caucasian ILS/SG/PDL
ILS, intralesional steroid injections; SG, silicone gel; PDL, pulsed dye laser treatment; RTX,
low-dose radiotherapy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp682686
Mitomycin C for keloid scars, J.N.R. Bailey et al. 683
(in two patients very rm crusts had to be removed by shaving
them level with the skin under local anaesthetic) and mitomycin
C 1 mg mL
)1
was applied to the scar for 3 min as before, fol-
lowed by a dry dressing. The patients were reviewed at 2, 4 and
6 months after the rst application and at each visit the patient
and the Clinical Trials Unit staff assessed the scar and symptoms
arising from the keloid on a linear analogue scale from 0 (disap-
pointed) to 10 (delighted) and any further comments were
noted. At 6 months a nal photograph was taken and two
dermatologists not involved in the study compared the pretreat-
ment and 6-month post-treatment photographs and graded
the response to treatment as: 3, nearly normal skin; 2, great
improvement; 1, slight improvement; 0, no change; )1,
slightly worse; )2, worse; )3, signicantly worse.
Results
During the rst 3 weeks after the shave removal and rst
application of mitomycin C the patients experienced some dis-
comfort, but patients 8 and 10 complained of pain lasting
3 weeks, until the second application of mitomycin C. The
wounds oozed and had to be re-dressed but only patient 10
had an infected wound that required antibiotics. The side-
effects tended to be greater when larger areas of keloid were
shaved off, as in patients 710. After 3 weeks all the sites
were dry and had an adherent crust. Re-application of the
mitomycin C itself was reported as painless.
The sites healed to produce mainly at, pink or pink and
hypopigmented or depigmented scars with some hyper-
pigmentation around the periphery (Figs 1 and 2). The
pigment changes were most noticeable in patients with pig-
mented skin. A small adherent scab in the centre of the treated
area of patient 8 prevented the second application of mito-
mycin C reaching this area and it remained pink and slightly
raised while the surrounding area became at and depigmented
(Fig. 2b), which lends weight to the argument that the
mitomycin C should be re-applied after 3 weeks.
In general, the patients were pleased with this new treat-
ment. The mean patient score at 6 months was 79 and the
Clinical Trials Unit score was 69 (Fig. 3). The most successful
result was in patient 3 who had large postauricular keloids fol-
lowing pinnaplasty; post-treatment, the skin was completely
at and of normal colour. The worst result was in patient 6
with acne keloidalis nuchae whose lesions recurred and were
larger than before treatment. The presternal keloids responded
satisfactorily. Generally the treated areas were atter and the
patients were pleased that their symptoms of tightness, tender-
ness and itching at these sites had resolved.
Assessments of the pretreatment and 6-month post-treat-
ment photographs by two dermatologists not involved in the
study revealed nearly normal skin in two patients: patient 3
(postauricular) and patient 4 (posterior ear lobe), great
improvement in four patients: patient 2 (upper arm), patient
5 (posterior neck) and patients 7 and 8 (both presternal).
Patient 9 (presternal) was graded as great improvement by
one dermatologist and slight improvement by the other,
patient 10 (presternal) was as graded slight improvement by
both dermatologists. Patient 1 (presternal) was graded as slight
improvement by one dermatologist and slightly worse by the
other. Only one patient (patient 6, posterior neck) was graded
as worse (Fig. 4).
Discussion
The results of this preliminary study show that the treatment
of keloids with shave removal and application of mitomycin C
improved the appearance and symptoms in nine of 10 patients
in the study and that this benet was sustained over a 6-month
(a) (b)
Fig 1. Patient 3: postauricular (lower) keloid.
(a) Before treatment; (b) 6 months after
treatment.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp682686
684 Mitomycin C for keloid scars, J.N.R. Bailey et al.
follow-up. No signicant recurrences have been seen with
prolonged follow-up to 18 months. This treatment is most
efcacious for medium-sized keloids and is least efcacious
and possibly should not be used for acne keloidalis nuchae. It
was well tolerated apart from one site becoming infected,
which did not affect the cosmetic outcome.
The treatment requires the Cytotoxic Pharmacy to prepare
the mitomycin C. A 10-mL vial of mitomycin C costs 21;
manufacturing costs to reconstitute it with sterile water to
10 mL increase the price to 34. However, as 2 mL was
provided for each patient, each vial can provide enough mito-
mycin C solution for up to ve patients, so the cost per
patient can be as little as 7. Larger keloids should preferably
be treated in several sessions to minimize the risk of infection
over the raw area. The unpredictablity of the nal pigmentary
state of the keloid is a problem but the patients still preferred
the nal outcome which could at least be concealed with cos-
metic camouage.
Intralesional injection of bleomycin in two pilot studies has
also shown benet. In the rst study 73% of patients (n
14) had complete attening of their keloid and no recurrences
were noted during a mean follow-up of 19 months.
9
In the
second study (n 13) six had complete attening, six had
highly signicant attening and one had signicant atten-
ing.
10
Bleomycin is a similar antineoplastic agent to mitomy-
cin C and the results are comparable, although in the
bleomycin studies the keloids were not removed surgically
before treatment. Some patients in both groups had discom-
fort or pain in the short term after treatment, but in the
longer term their symptoms of pain and pruritus usually
resolved. Also some patients in both groups developed pig-
mentary changes at the treated site. No systemic toxicity has
been reported with low doses of either drug.
Recently imiquimod 5% cream has been applied to the
bases of shave-removed earlobe keloids, with good results. In
the rst study eight earlobes were treated with imiquimod 5%
cream daily for 8 weeks followed by an observation period of
16 weeks. At the end of this period 75% of the imiquimod-
treated sites remained recurrence free. Four patients under-
went bilateral paired comparisons with intralesional steroid
injections. Local irritation required rest periods in three cases.
At the end of the observation period 50% remained recurrence
free in the imiquimod-treated areas while experiencing recur-
rences in the intralesional steroid-treated areas.
12
In the second
study four patients had a total of eight keloids shave-removed
followed by daily application of imiquimod 5% cream for
Fig 2. Patient 8: presternal keloid. (a) Before treatment; (b) 6 months
after treatment.
0
1 2 3 4 5 6 7 8 9 10
1
2
3
4
5
6
7
8
9
10
Patient number
O
u
t
c
o
m
e
s
c
o
r
e
a
t
6
m
o
n
t
h
s
Patient
Clinical Trials Unit staff
Fig 3. Outcome scores at 6 months: 0, disappointed; 10, delighted.
3
2
1
0
1
1 2 3 4 5 6 7 8 9 10
2
3
Patient number
S
c
a
r
q
u
a
l
i
t
y
Dermatologist 1
Dermatologist 2
Fig 4. Comparison of photographs by two independent
dermatologists before and at 6 months after treatment to assess
change in scar quality: 3, nearly normal skin; 2, great improvement;
1, slight improvement; 0, no change; )1, slightly worse; )2, worse;
)3, signicantly worse.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp682686
Mitomycin C for keloid scars, J.N.R. Bailey et al. 685
6 weeks. One patient experienced an episode of cervical
lymphadenopathy. At 6 and 12 months post-treatment there
was an excellent cosmetic result and no evidence of recurrence
of any of the lesions.
13
We believe that on the basis of the positive results in this
preliminary study with mitomycin C, trials should be conduc-
ted to assess the optimum dose, duration and frequency of
application of mitomycin C to give the best outcome. Keloids
produce a major psychological burden and as currently avail-
able treatments are often unsatisfactory there is an urgent
need for therapeutic improvements. Further trials should also
compare mitomycin C with the standard and other new
treatments.
Acknowledgments
The authors thank the following staff at the Royal Free Hospi-
tal: the pharmacists in the Cytotoxic Pharmacy for making up
the mitomycin C solution, the photographers in the Medical
Illustration Department and Dr C.H. Orteu and Dr V.J. Swale
for assessing the photographs. We also thank Mr C.M. Bailey
for help in formulating and submitting the manuscript.
References
1 Fujiwara M, Muragaki Y, Ooshima A. Keloid-derived broblasts
show increased secretion of factors involved in collagen turnover
and depend on matrix-metalloproteinase for migration. Br J Dermatol
2005; 153:295300.
2 Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of
patients with keloid and hypertrophic scarring. Arch Dermatol Res
2006; 297:4338.
3 Chowdri NA, Masarat M, Mattoo A, Darzi MA. Keloids and
hypertrophic scars: results with intraoperative and serial post-
operative corticosteroid injection therapy. Aust N Z J Surg 1999;
69:6559.
4 Fikrle T, Pizinger K. Cryosurgery in the treatment of earlobe
keloids: report of seven cases. Dermatol Surg 2005; 31:172831.
5 OBrien L, Pandit A. Silicon gel sheeting for preventing and treat-
ing hypertrophic and keloid scars. Cochrane Database Syst Rev 2006;
1:CD003826.
6 Maarouf M, Schleicher U, Schmachtenberg A, Ammon J. Radio-
therapy in the management of keloids. Clinical experience with
electron beam irradiation and comparison with X-ray therapy.
Strahlenther Onkol 2002; 178:3305.
7 Alster TS. Laser treatment of hypertrophic scars, keloids, and striae.
Dermatol Clin 1997; 3:41929.
8 Garg MK, Weiss P, Sharma AK et al. Adjuvant high dose rate
brachytherapy (Ir-192) in the management of keloids which have
recurred after surgical excision and external radiation. Radiother Oncol
2004; 73:2336.
9 Saray Y, Gulec AT. Treatment of keloids and hypertrophic scars
with Dermojet injections of bleomycin: a preliminary study. Int J
Dermatol 2005; 44:77784.
10 Espana A, Solano T, Quintanilla E. Bleomycin in the treatment of
keloids and hypertrophic scars by multiple needle punctures. Dermatol
Surg 2001; 27:237.
11 Kontochristopoulos G, Stefanaki C, Panagiotopoulos A et al. Intra-
lesional 5-uorouracil in the treatment of keloids: an open clinical
and histopathologic study. J Am Acad Dermatol 2002; 52:4749.
12 Martin-Garcia RF, Busquets AC. Postsurgical use of imiquimod 5%
cream in the prevention of earlobe keloid recurrences: results of an
open-label, pilot study. Dermatol Surg 2005; 31:13948.
13 Stashower ME. Successful treatment of earlobe keloids with imiqui-
mod after tangential shave excision. Dermatol Surg 2006; 32:3806.
14 Berman B, Villa AM, Ramirez CC. Novel opportunities in the treat-
ment and prevention of scarring. J Cutan Med Surg 2005; 8(Suppl. 3):
326.
15 Al-Attar A, Mess S, Thomassen JM et al. Keloid pathogenesis and
treatment. Plast Reconstr Surg 2006; 117:286300.
16 Simman R, Alani H, Williams F. Effect of mitomycin C on keloid
broblasts: an in vitro study. Ann Plast Surg 2003; 50:716.
17 Ribero F de AQ, Guaraldo L, Borges J de P et al. Clinical and histo-
logical healing of surgical wounds treated with mitomycin C.
Laryngoscope 2004; 114:14852.
18 Chen CW, Huang HT, Bair JS, Lee CC. Trabeculectomy with simul-
taneous topical application of mitomycin C in refractory glaucoma.
J Ocul Pharmacol 1990; 6:17582.
19 Seiler T, Schnelle B, Wollensak J. Pterygium excision using 193-
nm excimer laser smoothing and topical mitomycin C. Ger J
Ophthalmol 1992; 1:42931.
20 Rodriguez JA, Ferrari C, Hernandez GA. Intraoperative application
of topical mitomycin C 0.05% for pterygium surgery. Bol Asoc Med
P R 2004; 96:1002.
21 Rubinfeld RS, Pster RR, Stein RM et al. Serious complications of
topical mitomycin C after pterygium surgery. Ophthalmology 1992;
99:164754.
22 Eschle-Meniconi ME, Ahmad SR, Foster CS. Mucous membrane
pemphigoid: an update. Curr Opin Ophthalmol 2005; 16:3037.
23 Rahbar R, Jones DT, Nuss RC et al. The role of mitomycin in the
prevention and treatment of scar formation in the pediatric aero-
digestive tract: friend or foe? Arch Otolaryngol Head Neck Surg 2002;
128:4016.
24 Perepelitsyn I, Shapshay SM. Endoscopic treatment of laryngeal
and tracheal stenosis has mitomycin C improved the outcome?
Otolaryngol Head Neck Surg 2004; 131:1620.
25 McLeod IK, Brooks DB, Mair EA. Revision choanal atresia repair.
Int J Pediatr Otorhinolaryngol 2003; 67:51724.
26 Roh J. Prevention of posterior glottic stenosis by mitomycin C.
Ann Otol Rhinol Laryngol 2005; 114:55862.
27 Ali I, Wojnarowska F, Wilkinson J. Topical Mitomycin C: an Effective
Therapy for Laryngeal Mucous Membrane Pemphigoid. Case report, Dermatol-
ogy Section, Royal Society of Medicine, 17 April 2003.
28 Hueman EM, Simpson CB. Airway complications from topical
mitomycin C. Otolaryngol Head Neck Surg 2005; 133:8315.
29 Talmi YP, Orenstein A, Wolf M, Kronenberg J. Use of mitomycin
C for treatment of keloid: a preliminary report. Otolaryngol Head Neck
Surg 2005; 132:598601.
30 Sanders KW, Gage-White L, Stucker FJ. Topical mitomycin C in
the prevention of keloid scar recurrence. Arch Facial Plast Surg 2005;
7:1725.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp682686
686 Mitomycin C for keloid scars, J.N.R. Bailey et al.
DERMATOLOGI CAL SURGERY AND LASERS DOI 10. 1111/j . 1365- 2133. 2007. 07768. x
To freeze or not to freeze: a cost-effectiveness analysis of
wart treatment
M.R. Keogh-Brown, R.J. Fordham, K.S. Thomas,* M.O. Bachmann, R.C. Holland, A.J. Avery,*
S.J. Armstrong,* J.R. Chalmers,* A. Howe, S. Rodgers,* H.C. Williams* and I. Harvey
Department of Health Policy and Practice, School of Medicine, University of East Anglia, Norwich, NR4 7TJ, U.K.
*Queens Medical Centre, University of Nottingham, Nottingham, NG7 2RD, U.K.
Correspondence
Marcus Keogh-Brown.
E-mail: m.keogh-brown@uea.ac.uk
Accepted for publication
7 October 2006
Key words
cryotherapy, decision analysis, Markov model,
salicylic acid
Conicts of interest
None declared.
This work was carried out in Norwich, U.K. and
Nottingham, U.K. The views and opinions
expressed in this article are those of the authors
and do not necessarily reect those of the
Department of Health.
Summary
Background Several general practitioner (GP)-prescribed and over-the-counter ther-
apies for warts and verrucae are available. However, the cost-effectiveness of
these treatments is unknown.
Objectives To compare the cost-effectiveness of different treatments for cutaneous
warts.
Methods We designed a decision-analytic Markov simulation model based on sys-
tematic review evidence to estimate the cost-effectiveness of various treatments.
The outcome measures studied are percentage of patients cured, cost of treatment
and incremental cost-effectiveness ratio for each treatment, compared with no
treatment, after 18 weeks.
Results Duct tape was most cost-effective but published evidence of its effective-
ness is sparse. Salicylic acid was the most cost-effective over-the-counter treat-
ment commonly used. Cryotherapy administered by a GP was less cost-effective
than GP-prescribed salicylic acid and less cost-effective than cryotherapy adminis-
tered by a nurse.
Conclusions Duct tape could be adopted as the primary treatment for cutaneous
warts if its effectiveness is veried by further rigorous trials. Nurse-administered
cryotherapy is likely to be more cost-effective than GP-administered cryotherapy.
It is estimated that U.K. general practices treat about 2 million
patients for cutaneous (nongenital) warts each year.
1
If each
treatment prescribed in general practice costs the NHS on
average 20,
2
the total annual cost is about 40 million. Many
other people treat warts themselves, using preparations that
they buy from pharmacies.
Available treatments include surgical curettage, topically
applied treatments and complementary and alternative therap-
ies. The most commonly used treatments are professionally
administered cryotherapy with liquid nitrogen, and topical sali-
cylic acid. More recently, duct tape has proven effective in one
randomized trial,
3
and patient-administered ethylene glycol
cryotherapy has become available over-the-counter. Most warts
tend to disappear within a few years without treatment.
4,5
A
systematic review of randomized trials found little evidence that
the two commonest wart treatments, salicylic acid and cryo-
therapy, were of different effectiveness or that cryotherapy was
better than no treatment,
6,7
although the quantity and quality
of direct comparative evidence was limited.
Wart treatment is very common and so imposes a substan-
tial cost on health services and on society, yet there is still
uncertainty about which treatment is most effective or cost-
effective. To synthesize the diverse evidence on disease
progression, treatment effectiveness and treatment costs, a
quantitative model is needed. The aim of this study was to
compare the cost-effectiveness of different treatments for cuta-
neous warts. We also aimed to assess whether, and if so,
which, randomized trials were still needed in the light of
available evidence and current practice.
Methods
The study was a cost-effectiveness analysis based on a decis-
ion-analysis model. We estimated incremental cost-effective-
ness ratios of each treatment compared with spontaneous
resolution (that is, do nothing) and basic advice from the
general practitioner (GP) (without treatment) as the baseline
comparators. A brief explanation of incremental cost-effective-
ness is provided in the appendix. The GP no treatment base-
line comparator is included to represent the advice-only
management typically offered by the NHS. As salicylic acid is
usually purchased by patients themselves while cryotherapy is
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692 687
predominately supplied by the NHS, we conducted the cost-
effective analysis both from the perspective of the NHS and of
patients using treatment (or no treatment) pathways deter-
mined by the survey data in Thomas et al.
2
The cost-effectiveness model was built using TreeAge Data
Pro software (TreeAge Software Inc., Williamstown, MA,
U.S.A.). The software allows decision-analytic pathways of
accepted treatments to be clearly modelled using estimates of
outcomes and costs found in the literature. These estimates are
set out in Tables 13.
3,814
The model includes a Markov property, to represent recur-
ring events over time (in our case, imaginary weekly checks
of the treatments progress). At the end of each weekly cycle
we consider all patients to be in one of two situations or
Markov states: (i) the patient still has a wart(s) or (ii) the
patient has no wart(s), that is, all warts have resolved or been
cured. Cycle length is set at 1 week. The model includes the
possibilities that uncured patients pass from their rst-line
treatment into a second-line treatment and then, if still
uncured, to spontaneous resolution. Details of the simplifying
assumptions used in the model are given in the report by
Thomas et al.
2
and further details on Markov models are given
in the appendix.
Treatment options
Cure probabilities were estimated from the earlier Cochrane
review,
7
which was recently updated, with the average cure
rates weighted by each trials sample size. We used only
trials reporting numbers of patients cured rather than numbers
of warts cured. Interquartile ranges of cure rates for differ-
ent trials of the same treatment were used in sensitivity ana-
lyses. In the case of duct tape, the uncertainty in probability
estimates was expressed in terms of condence intervals as
the duct tape cure rate was available from only a single
trial. To adapt trial results to the models weekly cycle, the
proportion cured was apportioned equally across the number
of weeks for which the treatments were applied. A summary
of the cure probabilities for different treatments is presented
in Table 1.
Treatment costs
Treatment costs included in the model are shown in Table 1.
Treatment pathways were informed by a combination of
expert opinion, patient survey, structured observation of
practice and focus group discussion with patients, health
Table 1 Cost, cure rate and duration of warts treatments
Intervention Costs included Average cost () Cure rates [duration]
Home treatments
Over-the-counter salicylic acid 475 per pack (per 6 weeks)
Travel pharmacy
2330 57% (IQR 3568%) [12 weeks]
a
Duct tape 250 (10 metres)
Travel to shop
940 85% (95% CI 66594%) [8 weeks]
b
Over-the-counter cryotherapy 11 (35-mL can)
Travel costs
1790 54% (IQR 5358%) [6 weeks]
c
Treatments in primary care
Advice only 20 (GP consultation)
14
Travel to GP
2690 30% [10 weeks]
d
GP-prescribed salicylic acid 20 (GP consultation)
14
Travel to GP
550 (two prescribed items)
14
Dispensing charge
4030 As for over-the-counter salicylic acid
Cryotherapy 20 (initial GP consultation)
14
Travel to surgery
(each consultation or session)
11 per 5-min GP cryotherapy
session
14
OR
250 per 5-min nurse
cryotherapy session
14
8060 for three
GP sessions; 5510
for three nurse sessions
As for over-the-counter cryotherapy
Extras
Travel (to GP, pharmacy or shop) 690 per visit
14
690 Not applicable
GP, general practitioner; IQR, interquartile range.
a
Cure rates pooled from four studies;
811
12 weeks was the most common duration for salicylic acid trials.
b
Cure rates and duration from Focht et al.
3
c
Cure rates pooled from ve studies.
3,8,11,13
Treatment duration of 6 weeks is based on three sessions at 2-week intervals, which has been
shown to be the shortest of the effective interval lengths in Bunney et al.
8
Ethylene glycol cryotherapy has been assumed to be of equal
effectiveness to liquid nitrogen cryotherapy.
d
The most common placebo treatment in Gibbs et al.
7
was of 10 weeks duration with average resolution of 30%. This has been used to
estimate the spontaneous resolution level.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692
688 To freeze or not to freeze, M.R. Keogh-Brown et al.
professionals and pharmacists. Treatment costs are usually in-
dependent of time to cure. Although patients cured before
completing a course of treatment can then cease treatment,
costs of treatment are not usually determined by duration of
treatment because it is generally not sensible to receive only
part of a session of cryotherapy, or to purchase a fraction of a
bottle or tube of salicylic acid. We therefore assumed that
warts remaining uncured after a full course of treatment pass
into the spontaneous resolution (no treatment) branch of the
model. The spontaneous resolution branch of the model per-
mits peoples warts to resolve gradually over weekly cycles. In
this way, spontaneous resolution is modelled in the same way
as other treatments, except that the probability of cure or
resolution in any cycle is lower.
The cost of combined treatments was the sum of the costs
of the individual treatments. The combination of cryotherapy
and salicylic acid was modelled in the same way as a single
treatment, but the probability of cure was adjusted according
to the estimated effectiveness of the combination.
Some treatments work faster than others and the effective-
ness of treatments varies according to the time and frequency
with which they are applied. In order to satisfy the opposing
needs of (i) patients who seek a cure within a reasonable time
period, and (ii) the need for a sufcient duration to allow the
treatment (or treatments in the case of combination therapy)
to be completed, 18 weeks was selected as the minimum time
period for the resolution of warts in our model.
Results
Two baseline treatments are considered in our analysis, one
for primary care treatments and the other for over-the-counter
treatments. Without treatment, 46% of patients warts resolve
by week 18 at no cost (Table 2). This represents the rst base-
line for our cost-effectiveness analysis. The alternative baseline,
of advice only from the GP, has the same cure rate, but costs
2690 (including the cost of a GP consultation and travel).
Several other treatments (e.g. three sessions of cryotherapy,
over-the-counter cryotherapy and cryotherapy by a nurse)
have the same cure rate as each other, but their costs differ
(Table 3).
The lower the incremental cost-effectiveness ratio is, the
more cost-effective is the treatment. The effect of using the
advice only baseline instead of the do nothing baseline is to
reduce all incremental cost-effectiveness ratios (Table 3)
because of the additional cost of the GP consultation. Using
the former baseline also reverses the ranking of self-adminis-
tered and nurse-administered cryotherapy.
Table 2 Home treatment effects and total
cost at 18 weeks
Treatment
Effect
(% cured)
Cost
()
Incremental
effect (%)
Incremental
cost ()
Incremental
cost-effectiveness
ratio
Do nothing 4592 000 000 000
Over-the-counter
salicylic acid
6422 2047 1830 2047 112
Over-the-counter
cryotherapy
6951 1790 2359 1790 076
Duct tape 8827 940 4235 940 022
Table 3 Primary care effect and total cost at 18 weeks
a
compared with both do nothing and advice only baselines
Treatment
Effect
(% cured)
Cost
()
Incremental
effect (%)
Compared with do
nothing baseline
Compared with
advice only baseline
Incremental
cost () ICER
Incremental
cost () ICER
Advice only 4592 2690 000 2690
GP-prescribed salicylic acid 6422 4030 1830 4030 220 1340 073
Cryotherapy 1 application 5227 4480 635 4480 706 1790 282
Cryotherapy 2 applications 6485 5941 1893 5941 314 3251 172
Cryotherapy 3 applications 6951 7067 2359 7067 300 4377 186
Nurse cryotherapy 6951 4927 2359 4927 209 2237 095
Salicylic acid then cryotherapy 8000 6633 3408 6633 195 3943 116
Cryotherapy then salicylic acid 8013 8001 3421 8001 234 5311 156
Combined salicylic acid and cryotherapy 6951 8232 2359 8232 349 5542 235
ICER, incremental cost-effectiveness ratio in per patient cured.
a
Costs and outcomes do not reect the totals outlined in Table 1 as those patients who are cured at each weekly cycle no longer incur
further costs.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692
To freeze or not to freeze, M.R. Keogh-Brown et al. 689
Figure 1 (top and bottom) shows the average costs and
effects (percentage of patients cured) of each option. The
slope of a line between any two treatments represents the
respective incremental cost-effectiveness ratio, which is lowest
when closest to vertical. Thus Figure 1 (top) shows that duct
tape is the most cost-effective home treatment when compared
with do nothing, dominating all other treatments due to its
negligible cost and high cure rate. Over-the-counter cryothera-
py also appears promising in that, if it is shown to be as
effective as professionally administered cryotherapy, it would
provide a cost-effective alternative to over-the-counter salicylic
acid.
Of the single treatments delivered in primary care, cryother-
apy administered by a nurse for three sessions is the most cost-
effective option, followed by salicylic acid prescribed by a GP
(GP SA) (Fig. 1, top). Cost-effectiveness of GP-administered
cryotherapy (whether one, two or three sessions) is less cost-
effective than GP SA. A single application of cryotherapy offers
a 6% greater average improvement compared with spontaneous
resolution, at a much higher incremental cost than other treat-
ments (4480). This high cost is partly due to the usual
requirement for a GP consultation before referral to a wart
clinic. Of the combination therapies, over-the-counter salicylic
acid followed by cryotherapy is similarly cost-effective. How-
ever, over-the-counter salicylic acid followed by cryotherapy
appears cost-effective only because it relies on patients self-
treating for a period of 12 weeks prior to visiting the GP.
An explanation for the better cost-effectiveness of second-line
cryotherapy is that relatively costly cryotherapy is restricted to
the minority of patients whose warts have not already been
cured by salicylic acid.
It is probably more representative of usual clinical practice
to compare the GP-administered treatments with a GP-admin-
istered advice only baseline [Table 3 and Fig. 1 (bottom)].
By introducing this treatment as the baseline, all the incre-
mental cost-effectiveness ratios for alternative treatments
decrease substantially. The most favourable incremental cost-
effectiveness ratio is for GP SA. However, three sessions of
cryotherapy administered by a nurse is almost as cost-effective
as GP SA and is associated with higher cure rates for patients.
The combinations of salicylic acid and cryotherapy treatments
are generally the least cost-effective.
Sensitivity analysis
A sensitivity analysis of the treatment cure probabilities was
performed in order to determine the cure values at which
the choice of most cost-effective treatment would change.
Full details of this analysis are provided in Thomas et al.
2
and
a further explanation of sensitivity analysis is given in the
appendix.
If cryotherapy were shown to be 55% effective (as in our
estimate), GP SA would require a cure rate of only 44% to be
more cost-effective than GP-administered cryotherapy and a
cure rate of 52% to be more cost-effective than nurse-admin-
istered cryotherapy. Taking into account the more rapid cure
rates with cryotherapy, Figure 2 shows equality of cost-effect-
iveness between GP SA and nurse-administered cryotherapy
around the 50% effectiveness threshold. At higher levels of
Duct
OTC CR
OTC SA
GP SA
CR1
CRNurse
COMB
SACR
CR3
CRSA
DN
CR2
0
10
20
30
40
50
60
70
80
90
0 5 10 15 20 25 30 35 40 45
Incremental effectiveness (percentage cured)
I
n
c
r
e
m
e
n
t
a
l
c
o
s
t
(
)
GP SA
CR1
CRNurse
CR2
COMB
SACR
CR3
CRSA
Advice
0
10
20
30
40
50
60
0 5 10 15 20 25 30 35 40
Incremental effectiveness (percentage cured)
I
n
c
r
e
m
e
n
t
a
l
c
o
s
t
(
)
Fig 1. (top) Average incremental costs and effects, and incremental
cost-effectiveness ratio, compared with do nothing option. (bottom)
Primary care treatments only. Average costs and effects and
incremental cost-effectiveness ratio compared with advice only
option. COMB, combination salicylic acid (SA) and cryotherapy;
CRSA, cryotherapy followed by SA, CR3, CR2, CR1 (three, two and
one applications of cryotherapy, respectively); SACR, SA followed by
cryotherapy; CRNurse, cryotherapy administered by a nurse; GP SA,
SA prescribed by a general practitioner (GP); OTC SA, SA bought
over-the-counter; OTC, cryotherapy bought over-the-counter; DUCT,
duct tape treatment; DN, do nothing (baseline), ADVICE, advice only
from a GP.
30
35
40
45
50
55
60
65
70
40 45 50 55 60
GP administered salicylic acid (%)
N
u
r
s
e
a
d
m
i
n
i
s
t
e
r
e
d
c
r
y
o
t
h
e
r
a
p
y
(
%
)
Fig 2. Plot of cure rates at which general practitioner (GP)-
administered salicylic acid and nurse-administered cryotherapy have
equal incremental cost-effectiveness ratios.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692
690 To freeze or not to freeze, M.R. Keogh-Brown et al.
effectiveness for both treatments, cryotherapy would need to
have a higher cure rate than salicylic acid to be equally incre-
mentally cost-effective (and conversely a lower cure rate
below this threshold).
Discussion
Current available evidence suggests that there is little difference
in effectiveness between many commonly used wart treat-
ments, suggesting that the cheapest treatments may be the
most cost-effective. But convenience, speed of cure and pain of
different treatments are highly relevant to patients. For exam-
ple, cryotherapy can be painful and requires a general practice
visit. In such caseswhere the direct costs to patients are rela-
tively small, formal healthcare costs are high, and outcomes
are not signicantly improved by professional interven-
tionpatients may prefer self-treatment. If there is good evi-
dence of a natural resolution of the illness within a reasonably
short time period, or where a patients quality of life is not
particularly reduced, then any intervention may be deemed
unnecessary and not taken up.
15
As two-thirds of warts are
estimated to resolve within 2 years,
4,5
no treatment may be
the best option for those whose warts do not cause discomfort
or affect employment and are not cosmetically undesirable.
The most cost-effective treatments considered in the model
are those that are bought by patients and applied in their
homes, namely over-the-counter salicylic acid, over-the-coun-
ter cryotherapy and duct tape. This is not surprising, as the
treatments do not require a costly initial consultation with the
GP, and appear to be of comparable efcacy to similar pre-
scribed treatments.
Some of the newly emerging home treatments such as duct
tape and home cryotherapy with ethylene glycol may prove to
be highly cost-effective, but effectiveness evidence for these
treatments is limited. Salicylic acid remains the most cost-
effective over-the-counter option but the advent of a reliable
and effective self-administered form of cryotherapy could be
advantageous. Routine use of cryotherapy for the treatment of
warts in primary care may not be justied on the grounds
of cost-effectiveness. However, nurse-led cryotherapy clinics
would be a more cost-effective way of delivering this inter-
vention if the number of cryotherapy sessions is limited to a
maximum of three and if subsequent studies show that nurses
are as effective as GPs when using liquid nitrogen cryotherapy.
A recent survey showed that just 12% of cryotherapy treat-
ments were currently conducted by nurses.
2
Although the evi-
dence suggests that cryotherapy and salicylic acid are of
broadly comparable efcacy, it is possible that cryother-
apy delivers cures more quickly. This faster speed of cure of
cryotherapy compared with topical salicylic acid coupled with
the low direct cost to patients (as the NHS meets the main
costs) may explain its popularity with patients. However, a
shift towards cheaper self-treatment might be benecial to
both the patients and the NHS.
In practice there is a great deal of variation in the applica-
tion of wart treatments in terms of their duration, frequency
of application and adherence. Our model reects best prac-
tice using optimum treatment applications as tend to be used
in clinical trials.
Our ndings suggest that two clinical trials should be
undertaken in primary care settings to ll important gaps in
the current evidence. The rst is a randomized trial of nurse-
led cryotherapy vs. salicylic acid in primary care. A total sam-
ple size of 872 (allowing for a drop-out rate of 10%) would
be required to detect a 10% difference in cure rates in either
direction. This assumes that the cure rate of nurse-led cryo-
therapy is the same as GP-led cryotherapy, i.e. 54%. A second
trial should compare three patient-administered treatments,
namely over-the-counter salicylic acid, duct tape and over-
the-counter cryotherapy. A total sample size of 1308 (allow-
ing for a drop-out rate of 10%) would be required to detect a
10% difference in cure rates in either direction, and assumes a
baseline cure rate of 54%.
Although cutaneous viral warts constitute a low morbidity
problem they nonetheless use signicant primary care
resources. Their management should be guided by further
high-quality randomized trials of new interventions or old
interventions delivered in new ways.
Acknowledgments
The authors would like to express their thanks to the NHS
Research and Development Health Technology Assessment
programme for their nancial provision for the research pro-
ject underlying this publication.
References
1 McCormick A, Fleming D, Charlton J. Morbidity Statistics from General
Practice Fourth National Study 19911992. Newport, Wales: Ofce for
National Statistics (Ofce of population censuses and surveys),
1995; Report 5.
2 Thomas KS, Keogh-Brown MR, Chalmers JR et al. Effectiveness and
cost-effectiveness of salicylic acid and cryotherapy for cutaneous
warts. An economic decision model. Health Technol Assess 2006;
10:iii, ix87.
3 Focht DR III, Spicer C, Fairchok MP. The efcacy of duct tape vs
cryotherapy in the treatment of verruca vulgaris (the common
wart). Arch Pediatr Adolesc Med 2002; 156:9714.
4 Williams HC, Pottier A, Strachan D. The descriptive epidemiology
of warts in British schoolchildren. Br J Dermatol 1993; 128:50411.
5 Massing AM, Epstein WL. Natural history of warts. Arch Dermatol
1963; 87:30610.
6 Gibbs S, Harvey I, Sterling J, Stark R. Local treatments for cutane-
ous warts: systematic review. BMJ 2002; 325:461.
7 Gibbs S, Harvey I, Sterling JC, Stark R. Local treatments for cutane-
ous warts. Cochrane Database Syst Rev 2003 (3):CD001781.
8 Bunney MH, Nolan MW, Williams DA. An assessment of methods
of treating viral warts by comparative treatment trials based on a
standard design. Br J Dermatol 1976; 94:66779.
9 Flindt-Hansen H, Tikjob G, Brandrup F. Wart treatment with
anthralin. Acta Derm Venereol 1984; 64:1779.
10 Spanos NP, Williams V, Gwynn MI. Effects of hypnotic, placebo,
and salicylic acid treatments on wart regression. Psychosom Med
1990; 52:10914.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692
To freeze or not to freeze, M.R. Keogh-Brown et al. 691
11 Steele K, Irwin WG. Liquid nitrogen and salicylic/lactic acid paint
in the treatment of cutaneous warts in general practice. J R Coll Gen
Pract 1988; 38:2568.
12 Connolly M, Basmi K, OConnell M et al. Cryotherapy of viral
warts: a sustained 10-s freeze is more effective than the traditional
method. Br J Dermatol 2001; 145:55547.
13 Erkens AMJL, Kuijpers RJAM, Knottnerus JA. Treatment of verrucae
vulgares in general practicea randomized controlled trial on the
effectiveness of liquid nitrogen and the Histofreezer. J Dermatolog
Treat 1992; 3:1936.
14 Netten A, Curtis L. Unit Costs of Health and Social Care. Canterbury:
PSSRU, University of Kent, 2003.
15 Cohen D, Henderson J. Health, Prevention and Economics, 2nd edn.
Oxford: Oxford Medical Publications, 1993.
16 Web Dictionary of Cybernetics and Systems. http://pespmc1.vub.ac.be/ASC/
SENSIT_ANALY.html (accessed 24 November 2006).
Appendix
Markov model
A stochastic process has the Markov property if the conditional
probability distribution of future states of the process, given
the present state and all past states, depends only upon the
current state and not on any past states.
In our model, the Markov property is used to represent
recurring events over time (e.g. one application of a treatment
requiring several applications). As the patient is the unit of
analysis and in order to model the patients condition with a
Markov model, it is necessary to dene the two entities:
states and cycles.
There are only two patient conditions which are directly rele-
vant to our study: (i) the patient still has a wart (or warty skin),
and (ii) the patient has no wart (or no warty skin), i.e. the wart
has been cured or has resolved. These two conditions are repre-
sented by the two Markov states called, respectively, Wart and
No Wart. This simplifying assumption was necessary for the
model, although in practice there are other eventualities, for
example, cure of some of a patients multiple warts.
Cycles represent the time points at which we consider a
possible transition between the two Markov states [i.e. the
transition from having a wart(s) to the wart(s) being cured].
As wart treatment or resolution times vary, from a few weeks
to several months or even years, we chose cycles of length
1 week. The data from which cure rates are estimated is not
sufciently detailed to allow cure rates to be estimated at
time scales shorter than 1 week. In fact, adapting cure rates to
1-week intervals requires simplifying assumptions. A diagram
of the transitions possible from the Markov states is shown in
Fig. 3.
Sensitivity analysis
Sensitivity analysis is a procedure to determine the sensitivity of
the outcomes of an alternative or, in our case, a treatment, to
changes in its parameters. If a small change in a parameter
results in relatively large changes in the outcomes, the outcomes
are said to be sensitive to that parameter. This may mean that
the parameter has to be determined very accurately or that the
alternative has to be redesigned for low sensitivity.
16
The values of effectiveness in our model are xed by the
deterministic cohort simulation. While they represent the best
point estimates available from the Cochrane review, sensitivity
analysis of the cure probabilities can be used to prove an illus-
tration of the amount of variability in our estimates that
would be required to alter our conclusions (i.e. the robustness
of these results).
Incremental cost-effectiveness ratio
The incremental cost-effectiveness ratio (ICER) is the ratio of
the change in costs divided by the change in effects between
two different courses of action. In our case we compare a
wart treatment with a baseline control (such as no treatment
or advice only). For each treatment, ICERs are calculated
using the following formula:
Cost of treatment being investigatedcost of baseline comparator
Effect of treatment being investigatedeffect of baseline comparator
:
Fig 3. The transitions that are possible from the Markov states.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp687692
692 To freeze or not to freeze, M.R. Keogh-Brown et al.
EPI DEMI OLOGY AND HEALTH SERVI CES RESEARCH DOI 10. 1111/j . 1365- 2133. 2006. 07659. x
Lifetime prevalence of self-reported atopic diseases in a
population-based sample of elderly subjects: results of the
ESTHER study
M. Wolkewitz, D. Rothenbacher,* M. Low,* C. Stegmaier, H. Ziegler, M. Radulescu, H. Brenner* and
T.L. Diepgen
Department of Clinical Social Medicine, Ruprecht-Karls-University Heidelberg, Thibaut-Str. 3, 69115 Heidelberg, Germany
*The German Centre for Research on Ageing, Ruprecht-Karls-University Heidelberg, Heidelberg, Germany
Unit for Health Monitoring, Saarland Ministry for Public Health, Saarbrucken, Germany
Correspondence
T.L. Diepgen.
E-mail: thomas.diepgen@med.uni-heidelberg.de
Accepted for publication
25 September 2006
Key words
adults, atopic diseases, observational study,
prevalence, socioeconomic status
Conicts of interest
None declared.
Summary
Background Prevalence studies of atopic diseases such as atopic dermatitis (AD), hay
fever and allergic asthma have mostly been performed in children. Studies in the
adult population are still rare.
Objectives We estimated the lifetime prevalence of different atopic diseases in an
elderly population in Saarland, Germany. Additionally we investigated the associ-
ation between atopic diseases and sociodemographic factors including age, gen-
der, duration of school education (as a proxy measure of socioeconomic status),
family history, and size of place of residence.
Methods This study was conducted between June 2000 and December 2002 in the
State of Saarland, Germany. Participants aged 5075 years (n 9961) were
recruited by their general practitioner in the context of a general health screening
examination. All lled out a standardized questionnaire and reported whether a
physician had ever diagnosed an atopic disease (hay fever, AD or asthma).
Results Overall, 9949 subjects (mean age 62 years, 45% men) were included in this
analysis. The lifetime prevalence of reported AD, hay fever and asthma was 43%,
83% and 55%, respectively. Lifetime prevalence of AD and asthma among women,
and lifetime prevalence of hay fever among both genders, strongly decreased with
age. Duration of school education ( 9 years, 1011 years, > 11 years) was
strongly associated with AD (37%, 57%, 68%; P trend < 00001) and hay fever
(72%, 112%, 128%; P trend < 00001), but only tentatively with asthma.
Conclusions The lifetime prevalence of AD is considerably lower in the elderly com-
pared with the prevalence reported among younger adults in recent studies.
Adults with a longer duration of school education appeared to have a higher risk
for atopic diseases.
Atopic diseases such as atopic dermatitis (AD), hay fever and
allergic asthma are common in children and adolescents. Their
prevalence has steadily increased during the past decades.
1
Recent studies in children and adolescents have reported a life-
time prevalence of AD between 12% and 37%, of asthma
between 3% and 13% and of allergic rhinitis between 2% and
21%.
2
Only few studies have investigated the prevalence of
atopic diseases in adults.
35
Generally, the prevalence of atopic
diseases is higher in industrial countries than in Eastern Euro-
pean and developing countries. So far, studies on prevalence
and incidence have mainly covered school children,
6
and stud-
ies in adults
7
are still rare.
For investigating the relationship of various measures of
socioeconomic status (SES) with atopy, mostly the parental
educational level has been used.
8
However, the strong and
consistent associations of SES and atopy cannot be fully
explained yet. Individuals with a genetic predisposition are at
increased risk for atopic diseases but environmental factors are
also supposed to play an important role. Among these, infec-
tious diseases during childhood, exposure to allergens, social
and economic status, Western lifestyle and environmental con-
tamination are discussed.
913
The aim of this study was to estimate the lifetime preva-
lence of AD, asthma and hay fever in an elderly population
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp693697 693
aged 5074 years, and to investigate the relationship between
atopic diseases and sociodemographic factors in adults.
Materials and methods
Study population and design
We conducted a population-based cross-sectional study using
baseline data from the ESTHER study (ESTHER Epidemio-
logische Studie zu Chancen der Verhutung, Fruherkennung
und optimierten Therapie chronischer Erkrankungen in der
alteren Bevolkerung). The ESTHER study is a prospective
cohort study on new approaches to the prevention and early
detection of chronic diseases among older adults. The study
recruited 9961 subjects who had a general health check by a
general practitioner between June 2000 and December 2002,
were between 50 and 74 years old, reside in Saarland, and
speak German. These health-screening examinations are
offered biennially free of charge to adults aged more than
35 years by the health insurance system in Germany. For fur-
ther details about the ESTHER study see Low et al.
14
The
ESTHER study was found to be representative for the general
population with regard to a broad variety of sociodemo-
graphic characteristics.
14
Likewise, the age and sex distribution
of cases was very similar to the distribution found in the
population of Saarland.
Besides age no further inclusion or exclusion criteria were
applied except the capability of speaking German. The project
was approved by the ethics committee of the Medical Faculty
of the University of Heidelberg and of the physicians board
of Saarland, and informed consent was obtained from each
participant.
Data collection
For 9949 of 9961 participants complete baseline data were
available which included a comprehensive questionnaire on
demographics, medical and social history, nutrition and life-
style lled out by the patient. Medical data including results of
a physical examination including laboratory evaluations and
data on medication were provided by the physicians.
This analysis is based on information obtained from the
patients questionnaire. Study participants were asked whether
they had ever been diagnosed with one of the following dis-
eases by a physician: AD, asthma or hay fever (the German
terms Neurodermitis, endogenes Ekzem and atopische Der-
matitis were used synonymously for the denition of AD).
Study individuals were requested to specify when the disease
had been diagnosed by a physician for the rst time. In add-
ition, participants were asked about the occurrence of AD,
asthma and hay fever in their parents and siblings.
Statistical analysis
For the main sociodemographic characteristics of the study
population counts and relative frequencies were summarized.
The lifetime prevalences of each atopic disease were calcu-
lated by means of relative frequencies for men and women
in various age groups and the v
2
test was used to assess
differences by gender. The CochranArmitage test for trend
was performed to assess the association of each atopic dis-
ease (response variable) with duration of school education
(explanatory variable with ordered levels) and additionally
with age group. For all tests two-sided P-values were con-
sidered.
A logistic regression model using odds ratio (OR) estimate
plus 95% condence interval (CI) was performed with the
respective atopic disease (AD, hay fever and asthma) as the
dependent variable. Gender, age, size of place of residence
before age of 18 years, school education level and parental
atopy were taken as the independent variables. All analyses
were computed with the Statistical Software Package SAS 8.2
(SAS Institute, Cary, NC, U.S.A.).
Results
Lifetime prevalence of self-reported atopic diseases
The main sociodemographic characteristics of our study popu-
lation (mean age 62 years, 45% men) as well as the corres-
ponding lifetime prevalence rates are presented in Table 1.
In our study population the total lifetime prevalence of AD,
hay fever and asthma was 43%, 83% and 55%, respectively.
As can be seen in Figure 1a the lifetime prevalence of AD
decreased in women from 65% in the age group 5055 years
to 34% in the age group 7075 years (P for trend < 00001).
In men it varied between 44% in the 6065-year age group
and 25% in the 6570-year age group (P for trend 009).
The distribution between women and men was different in a
statistically signicant way (P < 00001). Figure 1b shows the
lifetime prevalence of hay fever in the respective age groups
in women and men. A similar decrease with increasing age
was seen in both women and men (P for trend < 00001).
The distribution between women and men was not different
(P 018). Figure 1c displays lifetime prevalence of asthma.
In women a decrease from 65% in the age group 5055 years
to 46% in the age group 7075 years was seen (P for trend
006). In men it varied between 48% in the 6065-year age
group and 77% in the 6570-year age group (P for trend
003). The difference between women and men was not signi-
cant (P 049).
Association among atopic diseases
Figure 2 shows the prevalence of each atopic disease in our
study population and the concurrent occurrence of two or
three atopic diseases. When evaluating the association among
the various atopic diseases we found a strong association
between AD and hay fever (OR for hay fever given AD 35,
95% CI 2745). Of the adults with present or past AD par-
ticipating in the interview, 21% reported present or past hay
fever, compared with 73% of those without AD. There was
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp693697
694 Lifetime prevalence of self-reported atopic diseases, M. Wolkewitz et al.
also a signicant association between AD and asthma (OR for
asthma given AD 28, 95% CI 2038). Of the adults with
present or past AD, 126% reported present or past asthma,
compared with 49% of those without AD. The OR for hay
fever given asthma was 53 (95% CI 4366).
Size of place of residence before the age of 18 years
The participants were asked whether they grew up in a village
(< 10 000 inhabitants), small town (10 000100 000 inhabi-
tants) or large city (> 100 000 inhabitants). Table 1 shows the
association between size of place of residence and atopic
diseases adjusted for age, gender and school education.
Growing up in a large city was associated with an increased
risk for hay fever (OR 14, 95% CI 1118), but not for
asthma or AD.
School education
The highest school education level [low, 9 years (75%);
middle, 1011 years (14%); high, > 11 years (11%)] has
been used to investigate the association between school educa-
tion and atopic diseases. Table 1 and Figure 3 show the total
lifetime prevalence for the respective diseases with the 95%
CI. In general, subjects with a higher educational level had a
higher risk for atopic diseases. AD showed a steady increase
from 37% in the category low to 68% in the category high
(P for trend < 00001). After controlling for age, gender and
size of place of residence the ORs remained signicant
(low reference, 15, 20). Hay fever showed a similar
increase, although on a different level, from 72% to 128% in
the respective categories (P for trend < 00001). The ORs in
the multivariate model were signicant (low reference, 15,
18) (Table 1). Asthma showed no such increase: the preva-
lence varied between 53% in the category low and 67% in
the category middle and was 60% in the category high (P for
trend 01) (Table 1).
Family history of atopy
In subjects with a positive family history of AD, hay fever or
asthma (at least one parent affected) the prevalence of self-
reported atopic diseases was signicantly higher: in subjects
where at least one parent was affected by AD (n 351) the
prevalence of AD was 256% compared with 34% if no parent
was affected (OR 96, 95% CI 73127). The ndings were
similar for hay fever (prevalence of hay fever 382% if at least
one parent was affected compared with 77% if not; OR 69,
95% CI 5192) and for asthma (prevalence of asthma 132%
if at least one parent was affected compared with 42% if not;
OR 35, 95% CI 2943).
Discussion
This study conducted in 9949 adults aged 5074 years who
participated in a general health check is the rst population-
based study showing the lifetime prevalence of self-reported
atopic diseases in an elderly population. Notably, the lifetime
prevalence of AD was considerably lower in the elderly com-
pared with the prevalence reported among younger adults in
recent studies. Even within the age range of 5074 years the
prevalence of AD and hay fever decreased with increasing age.
Regarding a proxy measure for SES, adults with a longer dura-
tion of school education appeared to have a higher risk for
atopic diseases. In addition, we found a high risk in subjects
with a familial history of atopic diseases.
Table 1 Sociodemographic characteristics in the study population (n 9949), and prevalence of self-reported atopic dermatitis (AD), hay fever
and allergic asthma. Odds ratios (ORs) control for all variables presented in this Table plus family history of AD, hay fever and asthma
Characteristics n (%)
AD Hay fever Asthma
n (%) OR (95% CI) n (%) OR (95% CI) n (%) OR (95% CI)
Gender
Female 5468 (550) 247 (48) 10 454 (87) 10 282 (54) 10
Male 4481 (450) 158 (37) 08 (0610) 344 (79) 09 (0710) 249 (57) 11 (0913)
Age (years)
5059 3407 (342) 173 (53) 10 383 (115) 10 187 (56) 10
6069 4978 (500) 184 (39) 08 (0610) 345 (72) 07 (0608) 265 (55) 10 (0812)
7074 1564 (157) 48 (34) 07 (0510)** 70 (48) 04 (0305)*** 79 (53) 10 (0815)
Duration of school education (years)
9 7245 (747) 253 (37) 10 502 (72) 10 367 (53) 10
1011 1372 (142) 75 (57) 15 (1120) 150 (112) 16 (1319) 90 (67) 13 (1017)
> 11 1081 (112) 71 (68) 17 (1223)*** 137 (128) 18 (1423)*** 64 (60) 13 (1017)
Size of place of residence before age 18 years
Village 6189 (628) 238 (41) 10 444 (75) 10 322 (54) 10
Small town 2342 (241) 105 (47) 10 (0712) 212 (93) 11 (0914) 140 (61) 11 (0913)
Large city 1175 (121) 53 (47) 09 (0613) 130 (114) 14 (1118)*** 61 (54) 10 (0713)
CI, condence interval. P-value of CochranArmitage test for trend **P < 0001, ***P < 00001.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp693697
Lifetime prevalence of self-reported atopic diseases, M. Wolkewitz et al. 695
In our study population the self-reported lifetime prevalence
of AD, hay fever and asthma was 43%, 83% and 55%,
respectively. AD and hay fever occurred more frequently in
women and the prevalence of both diseases decreased with
increasing age. These effects were not seen for asthma.
A Swedish study
3
among 2059-year-old adults showed a
self-reported prevalence of atopic eczema of 146% (total) and
a decreased prevalence in men (56%) compared with women
(141%) in the age group 5059 years. As in our study popu-
lation the prevalence decreased with increasing age. Campello
et al.
4
published the results from the ECHRS study in Verona,
Italy. The prevalence of hay fever (among 2044-year-old
adults) was 169% with no differences owing to sex or age.
The prevalence of an episode of asthma (dened as a self-
reported attack of asthma or treatment for asthma) was 41%.
No differences were found with regard to age and sex. The
NACMAAS study (Manchester Asthma and Allergy Study)
interviewed 5687 adults aged 1845 years.
5
The question
(a)
(b)
(c)
Fig 1. Lifetime prevalence of (a) atopic dermatitis, (b) hay fever and
(c) asthma. Error bars represent 95% condence intervals.
Fig 2. Percentage lifetime prevalence of atopic dermatitis (AD), hay
fever and asthma.
Fig 3. Lifetime prevalence of atopic dermatitis (AD), hay fever and
asthma with respect to school education. Low, 9 years; middle, 10
11 years; high, > 11 years. Error bars represent 95% condence
intervals.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp693697
696 Lifetime prevalence of self-reported atopic diseases, M. Wolkewitz et al.
Has a doctor ever told you that you have eczema/asthma/hay
fever? was included in the questionnaire, and positive replies
were given by 131% (eczema), 206% (hay fever) and 154%
(asthma) of participants, respectively. The proportion of par-
ticipants reporting asthma and eczema was signicantly higher
among women compared with men.
The strong associations with familial history of atopic dis-
eases are in agreement with similar ndings among children
15
and the hypothesis of a strong genetic impact even though the
clustering of other behavioural risk factors within families
might also play a role. Another important result of our study
is the strong association of the school education level with
atopic diseases. People with a higher education seem to have a
higher risk for atopic diseases compared with those with a
lower education level. Other published surveys show corres-
ponding results: using the skin prick test and allergen-specic
IgE to determine sensitization, Schafer et al.
16
showed that
allergic sensitization to common aeroallergens in adults fol-
lows a signicant and linear association with school education.
A possible explanation to be considered for the increased
prevalence of atopic diseases in higher social classes might be
an increased awareness in this population subgroup. However,
it appears unlikely that this possibility would explain com-
pletely the strong gradient found in our study. Furthermore,
social class has been associated with objective markers of atop-
ic diseases in other studies.
9
We propose the school education
level as a useful summary marker for different environmental
and lifestyle factors.
When looking at the results of this study the following limi-
tations should be considered: the analyses in our study are
based on data from an interview in which study participants
were asked whether they had ever been diagnosed with an
atopic disease by a physician. How the physicians diagnosed
the atopic diseases might be different and could cause bias.
Older people tend to have less good memory and the time
since the last symptom may have been longer. This makes the
study prone to information bias such as under- or over-report-
ing and recall bias because of differential medical knowledge,
understanding, reporting and more public awareness of allergy
and atopy due to the mass media.
17
However, other studies
have already demonstrated that self-report with respect to
physician-diagnosed atopic diseases is a valid means to describe
prevalences of atopic diseases in the general population.
35,18
Despite these limitations we can conclude that the preva-
lence of self-reported atopic diseases is considerable lower in
older compared with younger subjects. Within the age range
5074 years the prevalence of AD and hay fever decreased
with increasing age. Furthermore, the atopic diseases consid-
ered in this study very often occur concurrently, and point to
a strong intrafamilial risk pattern. Duration of school educa-
tion seems to be a useful proxy marker for various lifestyle
and environmental factors to characterize the risk for AD and
hay fever and, to a lesser degree, for asthma.
References
1 Diepgen TL. Is the prevalence of atopic dermatitis increasing? In:
Epidemiology of Atopic Eczema (Williams HC, ed.). Cambridge: Cam-
bridge University Press, 2000; 96109.
2 Mortz CG, Lauritsen JM, Bindslev-Jensen C, Andersen KE. Preval-
ence of atopic dermatitis, asthma, allergic rhinitis, and hand and
contact dermatitis in adolescents. The Odense Adolescence Cohort
Study on Atopic Diseases and Dermatitis. Br J Dermatol 2001;
144:52332.
3 Montnemery P, Nihlen U, Goran Lofdahl C et al. Prevalence of self-
reported eczema in relation to living environment, socio-economic
status and respiratory symptoms assessed in a questionnaire study.
BMC Dermatol 2003; 3:4.
4 Campello C, Ferrari M, Poli A et al. Prevalence of asthma and
asthma-like symptoms in an adult population sample from Verona.
ECRHS Verona. European Community Respiratory Health Survey.
Monaldi Arch Chest Dis 1998; 53:5059.
5 Simpson BM, Custovic A, Simpson A et al. NAC Manchester Asthma
and Allergy Study (NACMAAS): risk factors for asthma and allergic
disorders in adults. Clin Exp Allergy 2001; 31:3919.
6 Worldwide variation in prevalence of symptoms of asthma, allergic
rhinoconjunctivitis, and atopic eczema: ISAAC. The International
Study of Asthma and Allergies in Childhood (ISAAC) Steering
Committee. Lancet 1998; 351:122532.
7 Schafer T, Vieluf D, Behrendt H et al. Atopic eczema and other
manifestations of atopy: results of a study in East and West
Germany. Allergy 1996; 51:5329.
8 McNally N, Phillips D. Social factors and atopic dermatitis. In:
Epidemiology of Atopic Eczema (Williams HC, ed.). Cambridge: Cambridge
University Press, 2000; 13947.
9 Diepgen TL. Atopic dermatitis: the role of environmental and social
factors, the European experience. J Am Acad Dermatol 2001; 45
(Suppl. 1):S448.
10 Werfel T, Kapp A. Environmental and other major provocation fac-
tors in atopic dermatitis. Allergy 1998; 53:7319.
11 Porro E, Calamita P, Rana I et al. Atopy and environmental factors
in upper respiratory infections: an epidemiological survey on 2304
school children. Int J Pediatr Otorhinolaryngol 1992; 24:11120.
12 Svanes C, Jarvis D, Chinn S, Burney P. Childhood environment and
adult atopy: results from the European Community Respiratory
Health Survey. J Allergy Clin Immunol 1999; 103:41520.
13 Williams HC, Strachan DP, Hay RJ. Childhood eczema: disease of
the advantaged? BMJ 1994; 308:11325.
14 Low M, Stegmaier C, Ziegler H et al. [Epidemiological investiga-
tions of the chances of preventing, recognizing early and optimally
treating chronic diseases in an elderly population (ESTHER study)].
Dtsch Med Wochenschr 2004; 129:26437.
15 Johansson SG, Hourihane JO, Bousquet J et al. A revised nomencla-
ture for allergy. An EAACI position statement from the EAACI
nomenclature task force. Allergy 2001; 56:81324.
16 Schafer T, Ruhdorfer S, Weigl L et al. School education and allergic
sensitization in adults. Allergy 2001; 56:120610.
17 Williams HC. What is atopic dermatitis and how should it be
dened in epidemiological studies? In: Epidemiology of Atopic Eczema
(Williams HC, ed.). Cambridge: Cambridge University Press,
2000; 324.
18 Montnemery P, Svensson C, Adelroth E et al. Prevalence of nasal
symptoms and their relation to self-reported asthma and chronic
bronchitis/emphysema. Eur Respir J 2001; 17:596603.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp693697
Lifetime prevalence of self-reported atopic diseases, M. Wolkewitz et al. 697
EPI DEMI OLOGY AND HEALTH SERVI CES RESEARCH DOI 10. 1111/j . 1365- 2133. 2006. 07710. x
Early allergen exposure and atopic eczema
J.M. Harris, H.C. Williams,* C. White, S. Moffat, P. Mills, A.J. Newman Taylor and P. Cullinan
Occupational and Environmental Medicine, Imperial College School of Medicine, 1B Manresa Road, London SW3 6LR, U.K.
*Centre of Evidence-Based Dermatology, Queens Medical Centre, University of Nottingham, Nottingham, U.K.
Correspondence
Jessica Harris.
E-mail: jessica.harris@imperial.ac.uk
Accepted for publication
17 August 2006
Key words
cat allergen, childhood, eczema, house dust mite
allergen
Conict of interest
None declared.
Summary
Background The relationship between exposure to indoor aeroallergens in early life
and subsequent eczema is unclear. We have previously failed to show any signi-
cant associations between early life exposure to house dust mite and cat fur
allergens and either sensitization to these allergens or wheeze. We have also pre-
viously reported a lower prevalence of parent-reported, doctor-diagnosed eczema
by age 2 years for children exposed to higher concentrations of house dust mite,
but no other associations with other denitions of eczema or for exposure to cat
allergen.
Objectives To extend the exposureresponse analysis of allergen exposure and
eczema outcomes measured up to age 8 years, and to investigate the role of
other genetic and environmental determinants.
Methods A total of 593 children (924% of those eligible) born to all newly preg-
nant women attending one of three general practitioner surgeries in Ashford,
Kent, were followed from birth to age 8 years. Concentrations of house dust
mite and cat allergen were measured in dust samples collected from the home at
8 weeks after birth. The risk of subsequent eczema as dened by the U.K. diag-
nostic criteria was determined according to different levels (quintiles) of allergen
exposure at birth.
Results By age 8 years, 150 (253%) children had met the diagnostic criteria for
eczema at least once. Visible exural dermatitis was recorded at least once for
129 (280%). As in other studies, parental allergic history was positively associ-
ated with most eczema outcomes, as were higher maternal education and less
crowded homes. No clear linear associations between early exposure to house
dust mite or cat allergen were found, regardless of the denition of eczema used.
The risk of eczema appeared to increase for the three lowest quintiles of house
dust mite allergen exposure (odds ratio, OR 137 for third quintile compared
with rst), and then to fall for the two highest quintiles (OR 066 and 071)
even after controlling for confounding factors.
Conclusions The lack of any clear exposuredisease relationship between allergens
in early life and subsequent eczema argues against allergen exposure being a
major factor causing eczema. If the lower levels of eczema at higher levels of
house dust mite are conrmed, then interventions aimed at reducing house dust
mite in early infancy could paradoxically increase the risk of subsequent eczema.
The prevalence of atopic eczema (synonym atopic dermatitis
or eczema using the World Allergy Association new nomen-
clature
1
) in children in the U.K. has been estimated to be
between 14% and 20%
24
but little is known about its causes.
There is little published material concerning cat exposure and
childhood eczema, although in a large study of 35 552 Japan-
ese schoolchildren current cat ownership was found to be
related to a signicantly lower prevalence of atopic derma-
titis.
5
The role of house dust mite aeroallergens in initiation
and continuation of eczema has been proposed for some time
although results are inconclusive. In a recent review
6
the
authors stated: The fact that patients with atopic eczema/
dermatitis syndrome react consistently to dust mites supports
the view that mite exposure is a major cause of the disease.
Earlier studies of house dust mite exposure and childhood
eczema tended to be uncontrolled tests of an intervention with
2007 The Authors
698 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
patients removed from their usual environments. Many repor-
ted improvements in symptoms
712
although the one study
which also measured allergen exposure
10
found no correlation
between changes in eczema severity and changes in house
dust mite concentrations.
Several randomized controlled trials of interventions aimed
at reducing exposure to house dust mites have been conduc-
ted, usually by comparing a placebo group with an active mite
avoidance group. Mite avoidance has been achieved by the use
of mattress covers, frequent cleaning of bedrooms and other
measures. Four such studies
1317
reported signicant associa-
tions between allergen avoidance and reduction in eczema
symptoms. Two further trials
18,19
demonstrated improvement
in symptoms but little evidence that this could be directly
related to Der p 1 concentrations. In a trial of feeding practices
among high-risk infants,
20
house dust mite exposure was not
associated with eczema at age 1 year. The most recently repor-
ted trials have been larger and associations between house dust
mite and eczema less convincing: three randomized birth
cohort studies
2123
have all failed to demonstrate associations
between mite avoidance and childhood eczema. There are few
reported observational studies that have evaluated the risk of
eczema in relation to quantitative data on house dust mite in
early life. One study from Taiwan
24
of 931 healthy newborns
reported a signicantly higher incidence of eczema at age
3 years among children exposed to 1 lg g
)1
house dust
mite (216%) compared with those exposed to < 1 lg g
)1
(53%; P 00156).
In contrast, in an earlier publication from a U.K. birth
cohort we reported a protective role of higher house dust mite
exposure among children with parent-reported, doctor-diag-
nosed eczema by age 2 years,
2
although there were no other
associations between house dust mite or cat allergen exposure
and other measures of eczema by that age. One possible rea-
son for such a lack of association was the reliance on parental
report of diagnosed eczema.
We have also recently reported ndings from this birth
cohort in relation to early life exposure to house dust mite
and cat allergens and subsequent atopy, wheeze and atopic
wheeze at age 5
1
2
years.
25
We found no clear linear association
between early life exposure to house dust mite or cat allergen
and these outcomes: the exposureresponse associations
appeared to rise steeply at low levels of exposure and to
become attenuated at higher levels of exposure. Alongside
these allergic respiratory symptoms we have collected infor-
mation on eczema as dened by the full U.K. diagnostic cri-
teria as well as visible exural eczema up to age 8 years, and
here report the extension of the exposureresponse analyses to
these outcomes.
Materials and methods
Assembly of birth cohort
Recruitment to the birth cohort began in November 1993. All
newly pregnant women presenting for antenatal care to one
of three general practitioner surgeries in Ashford, Kent were
approached to join. In total, 710 were invited and 658 (93%)
agreed to participate. At recruitment, all but three of the
mothers and 542 (87%) of their partners underwent skin
prick tests to three common allergens (Dermataphagoides pteronyssi-
nus, cat fur and mixed grass pollens; Allergopharma, Hamburg,
Germany). An adult was considered to be atopic if at least one
mean weal diameter was at least 3 mm greater than the nega-
tive (saline) control. Also at this stage, information on family
size and other lifestyle factors was collected, including occupa-
tional details necessary for allocating social class according to
the Registrar Generals 1990 classication. In total, 642 babies
were born. Children were visited annually from birth until
they were aged 8 years and details on various aspects of their
health over the preceding 12 months were collected by ques-
tionnaires administered to a parent.
Dust sampling
Approximately 8 weeks after birth each baby was visited at
home and dust samples were collected from the living room
oor. These samples were assayed for concentrations of house
dust mite and cat allergen using standard techniques as
described previously.
26
These exposure measurements were
available for 624 (97%) of the cohort children.
Denitions of eczema used
Questions regarding the dryness of the childs skin and other
features of atopic eczema were asked at all annual visits, and an
examination of each child for evidence of visible exural derma-
titis as per photographic protocol (http://www.nottingham.
ac.uk/dermatology/eczema/index.html) was completed where
possible. A child was considered to have eczema if he/she had
experienced an itchy skin in the past 12 months and had at least
three of the following: a history of exural involvement, a
history of a generally dry skin, a history of allergic disease in
parents or siblings or visible dermatitis as per photographic
protocol. In this way, we could estimate the annual point preva-
lences of eczema according to the U.K. criteria and of visible
dermatitis, and calculate the proportion of children who had
ever had these outcomes. At each annual visit, we also recorded
whether the parent felt the child had eczema, and whether a
doctor had ever diagnosed eczema. Information up to age
8 years was available for 593 (924%) of cohort children.
Finally, all available medical records (n 594; 925%) were
reviewed at ages 3, 6 and 8 years by research nurses and a
documented diagnosis, or possible diagnosis, of eczema was
recorded.
At ages 5
1
2
and 8 years, with the agreement of both the par-
ent and the child, skin tests were performed on the children.
Atopy was dened as at least one mean weal diameter (pollen
mixture, D. pteronyssinus and cat fur; ALK-Abello, Hrsholm,
Denmark) at least 2 mm greater than that from the negative
(saline) control. Skin tests were performed on 552 (860%)
and 548 (854%) children at each occasion.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
Early allergen exposure and atopic eczema, J.M. Harris et al. 699
The study was approved by the local ethics committee and
a parent or guardian of each participant provided informed
consent.
Statistical analysis
Allergen concentrations were categorized into preplanned
quintiles of equal size. Comparisons between exposure quin-
tiles and subsequent measures of eczema were computed
using v
2
tests for trend. Logistic regression techniques were
used to quantify independent determinants of the eczema
outcomes. A forward stepwise procedure was implemented
for each outcome with the exposure measurements forced
into each model. Likelihood ratio tests were used to esti-
mate the contribution made to the model for each deter-
minant. A range of determinants was considered, and all
with a P-value < 025 from univariate analysis were indivi-
dually entered into the base model. The factor with the
smallest P-value (< 015) arising from the likelihood ratio
tests was then added to the model. This procedure was
repeated for all considered determinants until there were no
more with P < 015. All analyses were completed using SAS
(Cary, NC, U.S.A.) and Stata (College Station, TX, U.S.A.)
software.
Results
Prevalence of eczema
By age 8 years, 150 (253%) children had met the diagnostic
criteria for eczema at least once, with the annual point preva-
lence lying between 83% and 106% (Fig. 1). Only seven of
these children (47%) were deemed to have eczema using
these criteria, at each visit. Of those with sufcient skin test
information (n 533; 830%), 130 (244%) were atopic.
Fifty children (87% of cohort; 333% of those with eczema)
were atopic and met the U.K. diagnostic criteria for eczema.
Point prevalence of visible exural dermatitis varied between
48% and 71% (Fig. 1) with a positive identication occur-
ring at least once for 129 (280%) children. Of these 129 chil-
dren, most had visible dermatitis observed on only one (n
84; 651%) or two annual visits (n 25; 194%); just two
children (16%) had visible exural dermatitis each time they
were examined up to age 8 years.
Of the 150 children with eczema at some point by age
8 years, 85 (567%) were identied by age 2 years. Almost
half (432%) of the children with eczema by age 2 years were
atopic at either skin test compared with 18 (327%) of those
whose eczema was identied at a later age. Many of the chil-
dren with eczema identied by age 2 years also had eczema at
later ages (n 58; 682%). Sixty-nine children had visible
exural dermatitis witnessed by the research nurses at the time
of their visits at age 1 year or 2 years; for 27 (391%) of these
this was not evident after this age. Fifty-ve children (444%
of 129) had exural dermatitis at least once between the ages
of 3 years and 8 years, and not before the age of 2 years.
There are few missing data on visible exural dermatitis
for children seen at home up to age 4 years (maximum
29%) but as the visits at ages 5
1
2
years and 8 years were con-
ducted at school some data are missing (90% and 58%,
respectively).
Parents of over half of the children (n 375; 619%) felt
that their child had had eczema at some point before their
eighth birthday; 328 (547%) recalled a doctors diagnosis.
This gure was similar to the number of children who
received a diagnosis of eczema, or possible eczema, which
was recorded on their notes (n 312; 525%). Agreement
between the parent-reported diagnoses and actual recorded
diagnosis was 775%, with a similar number of children
whose parents reported having had a diagnosis where none
was recorded (n 72) as children whose parents did not
report having had a diagnosis where one was recorded in the
medical notes (n 60).
Of those children whose parents believed they had eczema,
most reported this before age 2 years (283; 755%). A diag-
nosis of eczema or possible eczema was also more often recor-
ded in the childs medical notes before age 2 years (222;
712%).
Exposureresponse associations
The observed associations between house dust mite quintiles
and eczema prevalence were clearly nonlinear (Fig. 2); the
rates of eczema according to the U.K. criteria by age 8 years
rose at lower levels of exposure but was reduced at higher
levels. This pattern was also observed for the other primary
outcomes of interest of eczema according to the U.K. criteria
with atopy, visible exural dermatitis and visible exural
dermatitis with atopy. Similar patterns were observed for the
three secondary outcomes with nonsignicant associations
(data not shown; P
trend
021 for doctor-diagnosed eczema,
034 for parent-reported, doctor-diagnosed eczema and 067
for parental opinion of eczema).
1 2 3 4 5/6
Age
14
12
10
8
6
4
2
0
U.K. diagnostic criteria for AE
Visible flexural dermatitis
P
e
r
c
e
n
t
a
g
e
8
Fig 1. Annual point prevalence of eczema (AE) according to U.K.
diagnostic criteria and annual point prevalence of visible dermatitis.
Age is given in years.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
700 Early allergen exposure and atopic eczema, J.M. Harris et al.
The associations between cat allergen quintiles and the main
outcomes were also not linear (Fig. 3): they broadly followed
similar patterns as found for house dust mite. Again, these
were replicated for the secondary outcomes (data not shown;
P
trend
041 for doctor-diagnosed eczema, 091 for parent-
reported, doctor-diagnosed eczema and 047 for parental
opinion of eczema).
For each exposure, similar ndings were observed when
the outcomes were restricted to children who were sensitized
to that allergen: house dust mite exposure quintiles vs. house
dust mite-sensitized children with eczema (n 29; data not
shown; P
trend
089) and cat allergen exposures vs. cat-sensi-
tized children with eczema (n 32; data not shown; P
trend
016). Stratied analysis by birth order demonstrated the same
inverted U shape associations for rstborns and approximately
at associations for those born later (data not shown).
The exposureresponse analysis was repeated for those chil-
dren with no older siblings (n 270; 42%); results were very
similar to those derived from the total cohort (data not
shown).
Multivariate modelling
In three models (Tables 1 and 2) there was no evidence
to suggest any clear exposure-response association between
domestic aeroallergen exposure and subsequent eczema. In
only one adjusted model did the association between exposure
to aeroallergens in early life and eczema approach statistical
signicance (Table 2; cat allergen exposure and the risk of
visible exural dermatitis with atopy; P 008) although
there was little evidence that this pattern was linear (P
058) if the term was included as a linear term).
The results from the three secondary outcomes were similar
both in respect to nonlinear exposureresponse associations
and to specic risk factors (data not shown). Maternal allergy
and/or paternal atopy were signicantly associated with in-
creased risk of each secondary eczema outcome and there was
evidence of increased risk with decreased crowding, higher
social class and increased maternal education.
Other ndings
There were some other ndings of interest. The risk of
eczema according to the U.K. criteria increased with maternal
history of allergic disease, paternal atopy and paternal age
(Table 1). Maternal history of allergic disease and paternal
atopy were also associated with increased risk of eczema
with atopy, along with increased risk observed for children
with mothers of higher educational experience and less
crowded homes. Mothers with higher numbers of years in
education were also more likely to have children with exu-
ral dermatitis (Table 2; P 003), with maternal and pater-
nal history of allergic disease and a less crowded home also
positively associated with visible exural dermatitis. Boys
were signicantly less likely to have visible exural dermatitis
(odds ratio, OR 059, 95% condence interval, CI 038
091; P 002). When analysis was restricted to those who
were also atopic, the only factor which remained signicant
was the low crowding index (OR 440, 95% CI 223870;
P < 0001).
Discussion
We have failed to nd any clear linear association between
house dust mite or cat allergen exposure quantied in early
life and subsequent occurrence of eczema, measured in a vari-
ety of ways. One adjusted model did demonstrate a borderline
signicant association between cat allergen exposure and the
risk of visible exural dermatitis with atopy; however, this
association was clearly nonlinear, with the highest prevalence
recorded for the second lowest exposure category.
The exposure estimates in this study are based on a single
measurement taken at one time point and setting for each
individual child. Other studies of domestic allergen concentra-
tions in similar settings
2729
have demonstrated a good degree
of reliability and we have evidence of internal validity (for
example, cat ownership vs. cat allergen).
0
0
2
2
7
0
2
8
8
1
0
8
2
2
2
2
2
3
7
5
7
7
6
3
8
4
9
7
0
0
2
2
7
0
2
8
8
1
0
8
2
2
2
2
2
3
7
5
7
7
6
3
8
4
9
7
0
0
2
2
7
0
2
8
8
1
0
8
2
2
2
2
2
3
7
5
7
7
6
3
8
4
9
7
0
0
2
2
7
0
2
8
8
1
0
8
2
2
2
2
2
3
7
5
7
7
6
3
8
4
9
7
U.K. diagnostic criteria
for eczema
P(trend) = 046
60
50
40
30
P
e
r
c
e
n
t
a
g
e
20
10
0
P(trend) = 048 P(trend) = 061 P(trend) = 061
U.K. diagnostic criteria
for eczema + atopy
Visible flexural
dermatitis
Visible flexural
dermatitis + atopy
Fig 2. House dust mite exposure quintiles and primary eczema
outcomes.
60
50
40
30
P
e
r
c
e
n
t
a
g
e
20
10
0
U.K. diagnostic criteria
for eczema
P(trend) = 051 P(trend) = 039
P(trend) = 084 P(trend) = 099
U.K. diagnostic criteria
for eczema + atopy
Visible flexural
dermatitis
Visible flexural
dermatitis + atopy
0
0
1
4
4
0
4
5
0
4
1
0
5
3
3
3
3
4
4
4
7
2
4
4
7
3
1
4
1
5
1
3
2
0
0
1
4
4
0
4
5
0
4
1
0
5
3
3
3
3
4
4
4
7
2
4
4
7
3
1
4
1
5
1
3
2
0
0
1
4
4
0
4
5
0
4
1
0
5
3
3
3
3
4
4
4
7
2
4
4
7
3
1
4
1
5
1
3
2
0
0
1
4
4
0
4
5
0
4
1
0
5
3
3
3
3
4
4
4
7
2
4
4
7
3
1
4
1
5
1
3
2
Fig 3. Cat allergen exposure quintiles and primary eczema outcomes.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
Early allergen exposure and atopic eczema, J.M. Harris et al. 701
Other ndings were similar to our previous report
2
where
parental history of allergic disease and parental atopy were
associated with the measures of eczema. As before, we also
found some evidence of increased prevalence among children
whose mothers had stayed in education longer, and for chil-
dren from less crowded homes. These ndings support earlier
reports of increasing prevalence of eczema among more
advantaged social groups.
30
Our reported prevalence of eczema was similar to other
studies. Findings from a large cohort study recently reported
period prevalence of 210%, 256%, 232% and 199% at 6,
18, 30 and 42 months, respectively.
31
Another study using
the same cohort reported visible eczema at age 5 years in
122% of children.
32
A 1-year prevalence of 115% and cumu-
lative incidence of 20% were reported among primary school
children aged between 3 and 11 years in 1989 in Birming-
ham.
3
Shamssain and Shamsian
33
reported a cumulative inci-
dence of 278% in NE England among children aged
67 years.
Although many controlled and uncontrolled studies have
shown associations between house dust mite avoidance and
eczema,
717,24
the ability to relate this directly to house dust
mite exposure has been limited.
10,18,19
Our ndings are in
agreement with our earlier report
2
and more recent, larger,
randomized birth cohort studies.
2123
The shape of the expos-
ureresponse associations described here is also consistent
with those previously reported for sensitization and wheeze at
age 5
1
2
years,
25
with a tendency for reduced risk in the higher
exposure quintiles. As in this report, we found a heightened
effect among rstborns compared with those born later.
Although the CIs for the higher quintiles overlap, this nding
was consistent across different measures of eczema.
Even though our cohort study was not very large, our data
are mostly complete and are likely to be representative. The
cohort was assembled by approaching all women seeking ante-
natal care irrespective of allergic history and the recruitment
and retention rates were very high. There was no evidence in
this cohort that exposures to house dust mite or cat allergen
were different with an allergic parent or sibling so it is unlikely
that behavioural factors have biased these results.
Our study ndings demonstrate that allergen exposure is
not generally associated with subsequent eczema in children.
Previous advice provided by investigators regarding the use
of bedcovers and other allergen avoidance methods is
Table 1 Determinants of eczema by U.K. criteria derived from logistic regression
Eczema by U.K. criteria (n 150) Eczema by U.K. criteria + atopy (n 50)
n (%) Adjusted
a
OR (95% CI) P-value n (%) Adjusted OR (95% CI) P-value
Maternal allergy
No 70 (204) 100 0001 20 (60) 100 001
Yes 80 (321) 195 (130293) 30 (126) 244 (122488)
Paternal atopy
No 69 (221) 100 002 23 (75) 100 005
Yes 68 (306) 164 (109247) 23 (110) 199 (099399)
Crowding index
High 28 (60) 100 001
Low 22 (206) 275 (131578)
Maternal education beyond age 16 years
None 12 (53) 100 004
< 2 years 16 (78) 125 (051305)
2 years 20 (149) 284 (117689)
Paternal age 104 (101109) 003
Quintile of house dust mite exposure
1 (lowest) 27 (235) 100 015 8 (71) 100 033
2 32 (276) 101 (053192) 11 (100) 094 (032272)
3 37 (316) 137 (074255) 15 (132) 187 (069503)
4 23 (192) 066 (034129) 7 (60) 074 (023235)
5 (highest) 27 (231) 071 (037137) 7 (62) 068 (021218)
Quintile of cat allergen exposure
1 (lowest) 22 (198) 100 084 5 (45) 100 015
2 35 (294) 142 (072281) 12 (105) 403 (1021590)
3 30 (252) 141 (071279) 10 (87) 305 (0741257)
4 27 (237) 131 (065262) 13 (119) 437 (1091745)
5 (highest) 33 (271) 141 (072275) 9 (76) 218 (053899)
OR, odds ratio; CI, condence interval.
a
Only terms which met the necessary level of signicance were included in the nal model; all terms in this nal model are adjusted for all
others included.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
702 Early allergen exposure and atopic eczema, J.M. Harris et al.
unlikely to have much impact upon the development of
eczema in childhood. The reported ndings of increased risk
associated with higher maternal education and less crowded
homes may be consistent with the concept that different
early life exposures to some environmental agents increase
risk of allergic disease.
Acknowledgments
Since the start, this study has been generously supported by
the Colt Foundation. The authors are grateful to all the fam-
ilies who have contributed to this research, and to the general
practitioners who granted access to the childrens medical
records.
References
1 Johansson SG, Bieber T, Dahl R et al. Revised nomenclature for
allergy for global use: report of the Nomenclature Review Com-
mittee of the World Allergy Organization, October 2003. J Allergy
Clin Immunol 2004; 113:8326.
2 Harris JM, Cullinan P, Williams HC et al. Environmental asso-
ciations with eczema in early life. Br J Dermatol 2001; 144:795
802.
3 Kay J, Gawkrodger DJ, Mortimer MJ et al. The prevalence of child-
hood atopic eczema in a general population. J Am Acad Dermatol
1994; 30:359.
4 Leung DY, Hanin JM, Charlesworth EN et al. Disease management
of atopic dermatitis: a practice parameter. Joint Task Force on Prac-
tice Parameters, representing the American Academy of Allergy,
Asthma and Immunology, the American College of Allergy, Asthma
and Immunology, and the Joint Council of Allergy, Asthma and
Immunology. Work Group on Atopic Dermatitis. Ann Allergy Asthma
Immunol 1997; 79:197211.
5 Kurosaka F, Nakatani Y, Terada T et al. Current cat owner-
ship may be associated with the lower prevalence of atopic
dermatitis, allergic rhinitis, and Japanese cedar pollinosis in
schoolchildren in Himeji, Japan. Pediatr Allergy Immunol 2006; 17:
228.
6 Capristo C, Romei I, Boner AL. Environmental prevention in atopic
eczema dermatitis syndrome (AEDS) and asthma: avoidance of
indoor allergens. Allergy 2004; 59 (Suppl. 78):5360.
7 Adinoff AD, Tellez P, Clark RA. Atopic dermatitis and aeroallergen
contact sensitivity. J Allergy Clin Immunol 1988; 81:73642.
Table 2 Determinants of visible exural dermatitis derived from logistic regression
Visible exural dermatitis (n 129) Visible exural dermatitis + atopy (n 46)
n (%) Adjusted
a
OR (95% CI) P-value n (%) Adjusted OR (95% CI) P-value
Maternal allergy
No 65 (243) 100 003
Yes 64 (330) 161 (104250)
Paternal allergy
No 82 (302) 100 008
Yes 44 (240) 067 (043105)
Crowding index
High 97 (256) 100 015 27 (62) 100 < 0001
Low 32 (390) 152 (087264) 19 (204) 440 (223870)
Maternal education beyond age 16 years
None 40 (216) 100 003
< 2 years 47 (283) 132 (079221)
2 years 39 (365) 217 (122388)
Sex
F 65 (337) 100 002
M 64 (239) 059 (038091)
Quintile of house dust mite exposure
1 (lowest) 22 (259) 100 032 6 (58) 100 032
2 27 (300) 117 (058234) 13 (130) 253 (090713)
3 30 (345) 173 (087346) 12 (114) 216 (076620)
4 23 (247) 088 (043181) 8 (77) 151 (049465)
5 (highest) 26 (252) 096 (047194) 6 (55) 118 (036390)
Quintile of cat allergen exposure
1 (lowest) 22 (256) 100 061 6 (59) 100 008
2 30 (326) 128 (064256) 14 (137) 293 (104823)
3 22 (234) 075 (036155) 6 (56) 086 (026285)
4 28 (308) 118 (059238) 12 (121) 176 (060515)
5 (highest) 27 (281) 096 (048191) 8 (71) 103 (033318)
OR, odds ratio; CI, condence interval.
a
Only terms which met the necessary level of signicance were included in the nal model; all terms in this nal model are adjusted for all
others included.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
Early allergen exposure and atopic eczema, J.M. Harris et al. 703
8 Clark RA, Adinoff AD. The relationship between positive aeroaller-
gen patch test reactions and aeroallergen exacerbations of atopic
dermatitis. Clin Immunol Immunopathol 1989; 53:S13240.
9 Clark RA, Adinoff AD. Aeroallergen contact can exacerbate atopic
dermatitis: patch tests as a diagnostic tool. J Am Acad Dermatol 1989;
21:8639.
10 Henderson AJ, Kennedy CT, Thompson SJ et al. Temporal associ-
ation between Der p 1 exposure, immediate hypersensitivity and
clinical severity of eczema. Allergy 1990; 45:44550.
11 Sanda T, Yasue T, Oohashi M et al. Effectiveness of house dust-mite
allergen avoidance through clean room therapy in patients with
atopic dermatitis. J Allergy Clin Immunol 1992; 89:6537.
12 Casimir GJ, Duchateau J, Gossart B et al. Atopic dermatitis: role of
food and house dust mite allergens. Pediatrics 1993; 92:2526.
13 Arshad SH, Hide DW. Effect of environmental factors on the devel-
opment of allergic disorders in infancy. J Allergy Clin Immunol 1992;
90:23541.
14 Hide DW, Matthews S, Matthews L et al. Effect of allergen avoid-
ance in infancy on allergic manifestations at age two years. J Allergy
Clin Immunol 1994; 93:8426.
15 Hide DW, Matthews S, Tariq S et al. Allergen avoidance in infancy
and allergy at 4 years of age. Allergy 1996; 51:8993.
16 Nishioka K, Yasueda H, Saito H. Preventive effect of bedding
encasement with microne bers on mite sensitization. J Allergy Clin
Immunol 1998; 101:2832.
17 Ricci G, Patrizi A, Specchia F et al. Effect of house dust mite avoid-
ance measures in children with atopic dermatitis. Br J Dermatol
2000; 143:37984.
18 Tan BB, Weald D, Strickland I et al. Double-blind controlled trial of
effect of housedust-mite allergen avoidance on atopic dermatitis.
Lancet 1996; 347:1518.
19 Endo K, Fukuzumi T, Adachi J et al. [Effect of vacuum cleaning of
room oors and bed clothes of patients on house dust mite counts
and clinical scores of atopic dermatitis. A double blind control
trial]. Arerugi 1997; 46:101324.
20 Burr ML, Miskelly FG, Butland BK et al. Environmental factors and
symptoms in infants at high risk of allergy. J Epidemiol Community
Health 1989; 43:12532.
21 Custovic A, Simpson BM, Simpson A et al. Effect of environmental
manipulation in pregnancy and early life on respiratory symptoms
and atopy during rst year of life: a randomised trial. Lancet 2001;
358:18893.
22 Koopman LP, van Strien RT, Kerkhof M et al. Placebo-controlled trial
of house dust mite-impermeable mattress covers: effect on symp-
toms in early childhood. Am J Respir Crit Care Med 2002; 166:30713.
23 Horak F Jr, Matthews S, Ihorst G et al. Effect of mite-impermeable
mattress encasings and an educational package on the development
of allergies in a multinational randomized, controlled birth-cohort
study 24 months results of the Study of Prevention of Allergy in
Children in Europe. Clin Exp Allergy 2004; 34:12205.
24 Huang JL, Chen CC, Kuo ML et al. Exposure to a high concentration
of mite allergen in early infancy is a risk factor for developing
atopic dermatitis: a 3-year follow-up study. Pediatr Allergy Immunol
2001; 12:1116.
25 Cullinan P, MacNeill SJ, Harris JM et al. Early allergen exposure,
skin prick responses, and atopic wheeze at age 5 in English chil-
dren: a cohort study. Thorax 2004; 59:85561.
26 Atkinson W, Harris J, Mills P et al. Domestic aeroallergen exposures
among infants in an English town. Eur Respir J 1999; 13:5839.
27 Heinrich J, Holscher B, Douwes J et al. Reproducibility of allergen,
endotoxin and fungi measurements in the indoor environment.
J Expo Anal Environ Epidemiol 2003; 13:15260.
28 Kalra S, Crank P, Hepworth J et al. Absence of seasonal variation in
concentrations of the house dust mite allergen Der p 1 in south
Manchester homes. Thorax 1992; 47:92831.
29 Kuehr J, Frischer T, Karmaus W et al. Natural variation in mite
antigen density in house dust and relationship to residential
factors. Clin Exp Allergy 1994; 24:22937.
30 Williams HC, Strachan DP, Hay RJ. Childhood eczema: disease of
the advantaged? BMJ 1994; 308:11325.
31 Wadonda-Kabondo N, Sterne JA, Golding J et al. A prospective
study of the prevalence and incidence of atopic dermatitis in chil-
dren aged 042 months. Br J Dermatol 2003; 149:10238.
32 Perkin MR, Strachan DP, Williams HC et al. Natural history of atop-
ic dermatitis and its relationship to serum total immunoglobulin E
in a population-based birth cohort study. Pediatr Allergy Immunol
2004; 15:2219.
33 Shamssain MH, Shamsian N. Prevalence and severity of asthma,
rhinitis, and atopic eczema: the North East study. Arch Dis Child
1999; 81:31317.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp698704
704 Early allergen exposure and atopic eczema, J.M. Harris et al.
PAEDI ATRI C DERMATOLOGY DOI 10. 1111/j . 1365- 2133. 2006. 07741. x
Idiopathic facial aseptic granuloma: a multicentre
prospective study of 30 cases
F. Boralevi, C. Leaute-Labre`ze, S. Lepreux,* S. Barbarot, J. Mazereeuw-Hautier, C. Eschard and A. Ta eb,
on behalf of the Groupe de Recherche Clinique en Dermatologie Pediatrique
Pediatric Dermatology Unit and *Laboratory of Pathology, Hopital Pellegrin-Enfant, Place Ame lie Raba-Le on, 33076 Bordeaux cedex, France
Department of Dermatology, Hotel-Dieu, Nantes, France
Pediatric Dermatology Unit, Childrens Hospital CHU Purpan, Toulouse, France
Department of Dermatology, CHU Robert Debre , Reims, France
Correspondence
Franck Boralevi.
E-mail: franck.boralevi@chu-bordeaux.fr
Accepted for publication
14 June 2006
Key words
children, facial nodule, granuloma, granulomatous
rosacea, idiopathic facial aseptic granuloma,
pilomatrixoma
Conicts of interest
None declared.
Summary
Background Idiopathic facial aseptic granuloma (IFAG) was recently described in a
single-centre retrospective study as a skin condition that occurs specically in
childhood.
Objectives To improve our epidemiological, clinical and pathological knowledge on
IFAG, to search for an infectious aetiology, and to assess therapeutic recommen-
dations.
Methods Children presenting with one or several acquired nodules on the face,
lasting for at least 1 month, with no evidence of any other recognizable clinical
entity such as infantile acne, pilomatrixoma, furuncle, tumour or vascular malfor-
mation, were enrolled in a prospective multicentre study from June 2001 to June
2004, involving the main French paediatric dermatology outpatient units. We
recorded clinical details about the nodule and its duration, ultrasound study pat-
tern, cultures for bacteria and mycobacteria, and Bartonella henselae and Apia felis
antibody testing.
Results Thirty children (17 boys and 13 girls, mean age 38 years) were enrolled.
Ultrasound studies revealed a solid well-demarcated hypoechoic lesion without
calcium deposit. Cultures for bacteria were negative in 70% of cases. Cultures for
mycobacteria and cat scratch disease serologies were negative. Antibiotic therapy
was ineffective; the lesion healed spontaneously with a mean duration of
11 months. Histological examination, performed in ve cases, showed a chronic
dermal lymphohistiocytic granuloma with numerous foreign body-type giant cells.
Conclusions IFAG is characterized by a painless facial nodule, presenting as a single
lesion localized on the cheek, with a prolonged course but spontaneous healing.
Oral or local antibiotics are usually ineffective. Regarding the pathophysiology, our
study rules out a primary infectious disease, and allows considering IFAG either as
a granulomatous process appearing around an embryological residue or as a mani-
festation to include in the spectrum of granulomatous rosacea in childhood.
Idiopathic facial aseptic granuloma (IFAG) was recently
described by Roul et al.
1
as a skin condition that occurs spe-
cically and not uncommonly in childhood. Because IFAG
looks like an abscess with very slight inammatory signs, we
rst proposed to name this condition pyodermite froide in
French,
2
which means cold pyoderma/abscess. It is character-
ized by painless red nodules, often located on the cheeks,
which heal spontaneously and usually without scarring after
a benign course of a few months to a year. In our rst
report, histological examination, performed in ve cases,
showed a dermal inammatory granuloma similar to that
observed after foreign body penetration or infections due to
mycobacteria, but direct examination and cultures performed
in selected cases were negative. In order to improve our
epidemiological, clinical and pathological knowledge on
IFAG, to search more extensively for an infectious aetiology,
and to assess therapeutic recommendations, we performed a
prospective multicentre study.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp705708 705
Patients and methods
The study was carried out prospectively at several centres in
France (listed in the Acknowledgments) from June 2001 to
June 2004. All children with a facial lesion suggestive of an
IFAG, i.e. presenting with one or several acquired nodules or
papulonodules on the face, lasting for at least 1 month, with
no evidence of any other recognizable clinical entity such as
infantile acne, pilomatrixoma, furuncle, tumour or vascular
malformation, were enrolled. A standardized questionnaire
detailing the medical history, the history of the lesion, epi-
demiological data and previous therapies was completed by
the parents. Clinical examination provided clinical details
about the facial nodule and possible associated conditions,
with special attention to keratosis pilaris or comedones. This
was followed by an ultrasound study of the lesion, Bartonella
henselae and Apia felis antibody testing, and cultures for bacteria
and mycobacteria after minimal local incision. A liquid culture
medium MB Redox (Heipha Diagnostika/Biotest Diagnostics,
Heidelberg, Germany) was used for detection of mycobacte-
ria.
3
Histological examination of a skin sample from a punch
biopsy or complete excision was proposed in cases of persist-
ent lesions but was not strictly required by the protocol. Then,
a 2-week therapy with amoxicillin-clavulanic acid (or with
josamycin in cases of suspected allergy to penicillin) was sys-
tematically given. Follow-up visits were planned 1 month later
and every 2 months until the disappearance of the lesion or
for at least 1 year in patients with persistent lesions. Photo-
graphs were taken at each visit, and all the cases were jointly
reassessed during meetings of our clinical research group.
Results
Forty patients were enrolled from seven of the 10 regional or
university centres involved in the study. After a collegial
evaluation, 10 were considered not to have IFAG and were
excluded. Five of them were considered to have infantile acne,
two had folliculitis, one had pilomatrixoma, one had pyogenic
granuloma and one had atypical Spitz naevus. The remaining
30 patients (17 boys and 13 girls) had a mean age of
38 years (range 8 months13 years). A single nodule was
noted in 27 cases (90%; Fig. 1), two patients had two lesions,
and one had three lesions. A previous similar lesion was
reported for one child, with a slightly visible scar (Fig. 2),
and the occurrence of a new lesion was observed in three
patients during follow up, two involving the upper eyelid and
one the contralateral cheek. Lesions were located on the
cheeks in most cases, as shown in the summary drawing
(Fig. 3). The mean size was 10 mm (range 325). A localized
mild trauma preceding the lesion was mentioned by the par-
ents in four cases. We observed no association with keratosis
pilaris, found in ve cases, or presence of comedones. No
patient had recently travelled overseas. In two cases, the par-
ents mentioned that the nodule was preceded by a slight but
palpable subcutaneous lesion for at least 1 year. The ultra-
sound studies, performed in 14 cases, always revealed a solid
and well-demarcated hypoechoic lesion, without calcium
deposit or microcalcications (Fig. 4). Cultures for bacteria,
obtained in 27 cases, were negative in 19 cases, or showed
Staphylococcus aureus (four cases), Streptococcus species (three cases)
and Enterococcus faecalis (one case). In those cases with positive
cultures for bacteria, a history of a recent modication or
increase in size of the lesion was usually reported by the par-
ents, leading consequently to a referral to our clinics. Cultures
for mycobacteria were negative and antibodies to B. henselae
and A. felis were not found. Antibiotic therapy, given in 26
cases, was followed by dramatic improvement only in four
cases, but was considered as ineffective in the rest of the stud-
ied population. In most of the cases, the lesion healed sponta-
Fig 1. A single nonpainful nodule on the cheek with a course of
several months in a 2-year-old boy.
Fig 2. Appearance of a second lesion on the lower eyelid of a young
girl, with visible scar of the previous lesion on the contralateral cheek
(arrow).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp705708
706 Idiopathic facial aseptic granuloma, F. Boralevi et al.
neously with a mean duration of 11 months (range 224),
and required a surgical excision in two cases because of the
long duration of the lesion, exceeding 12 years. Histological
examination was performed in ve cases, including three
biopsies and two complete excisions, and showed a chronic
dermal inammatory granuloma mainly composed of lympho-
cytes, histiocytes, neutrophils and numerous foreign body-
type giant cells. No calcium deposit or shadow cells were
seen. In one case, the granuloma developed around a nonrup-
tured epidermoid cyst (Fig. 5).
Discussion
IFAG is a newly recognized entity, dened by a chronic and
painless facial nodule, presenting usually as a single lesion
localized on the cheek, with a red or purplish appearance, and
Fig 3. Hot spots. This picture summarizes all the localizations of
idiopathic facial aseptic granuloma lesions on the cheeks. The lesions
involved the same triangular area in two-thirds of cases.
Fig 4. Ultrasound study of an idiopathic facial aseptic granuloma
lesion, showing a solid and demarcated hypoechoic lesion (arrows).
(a)
(b)
(c)
Fig 5. (a) Histological examination showing an inammatory
granuloma of the upper and deep dermis, with a ring of lymphocytes,
histiocytes, neutrophils and rare eosinophils (haematoxylin, eosin and
safranin; original magnication 25). (b) In this case, an epidermal cyst
was present, lled with neutrophils (haematoxylin, eosin and safranin;
original magnication 100). (c) Clinical appearance of this case.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp705708
Idiopathic facial aseptic granuloma, F. Boralevi et al. 707
a soft or elastic consistency. There is no common predisposing
factor, no family history, and no associated clinical features,
including no satellite lymph nodes. A local incision may dis-
charge pus or a ow of blood mixed with pus, and cultures
for bacteria are usually negative, except in cases of superinfec-
tion, which may be suspected when the size of the lesion
increases rapidly. As illustrated in Figure 3, IFAG seems to
involve selectively a restricted area affecting the middle part of
the cheeks. Ultrasonography shows a well-demarcated hypo-
echoic dermal lesion without features suggestive of piloma-
trixoma, i.e. an oval echogenic or hyperechogenic lesion with
an acoustic shadow, a peripheral halo and calcications.
4
The main differential diagnoses are the following: localized
infectious pyodermas, paucisymptomatic nodulocystic acne,
pilomatrixoma, cutaneous leishmaniasis, botryomycosis and
pyogenic granuloma. In contrast to pyoderma, IFAG is painless
and perilesional inammation is absent, and culture for bac-
teria remains negative except in cases of superinfection. In
nodulocystic infantile acne, lesions appear between 6 and
16 months of age, especially in boys.
5
Usual presentations of
infantile acne with supercial inammatory papules and come-
dones are quite easy to distinguish from IFAG, while cases with
only one or two nodules or nodulocysts pose more problems.
In those cases, a careful search for the presence of comedones
may favour a diagnosis of acne. Pilomatrixoma is one of the
most frequent benign tumours that may involve the face in
children, usually as a bluish and rm single subcutaneous nod-
ule. In rare cases, pilomatrixoma may appear as an ulcerated
nodule, but pathological examination is specic.
68
The cheek
is a frequent location in cutaneous leishmaniasis, and a single
nodule prior to a prolonged ulceration may be confused with
an IFAG. Thus, in geographical areas where cutaneous leish-
maniasis is common, cytological or histological examination
and specic staining may be required to distinguish IFAG and
leishmaniasis. Botryomycosis may exceptionally occur in young
children and on the cheeks. The clinical and histological fea-
tures differ from those observed in IFAG. In our cases, features
suggestive of botryomycosis, including sinuses, stulae, deeper
abscesses, and small yellowish grains in the pus after a minimal
incision were never seen.
9
Moreover, the benign course of
IFAG lesions argues against the diagnosis.
The pathophysiology of IFAG remains unclear. An infectious
cause, including an inoculation disease such as cat scratch dis-
ease, seems highly unlikely according to this study. The late
inammatory manifestation of a naevoid condition or embryo-
logical residue was a hypothesis based on the frequent cheek
location, suggesting the involvement of a cutaneous fusion
line. The remnant of an epidermoid cyst found in one case is
the only argument for this hypothesis in this series. As previ-
ously mentioned in our rst report, eyelid involvement may
be observed, either simultaneously or after some time of
follow up (Fig. 2). This association was also observed in
several personal unpublished cases after the completion of this
study, with a dramatic improvement after oral metronidazole
therapy. These recent observations suggest that IFAG could
belong to the spectrum of childhood rosacea.
10
To summarize, IFAG is a paediatric condition characterized
by a chronic painless nodule on the cheek, without identied
predisposing factors and without evidence for a microbial
cause, which should be recognized and managed nonaggres-
sively.
Acknowledgments
Participants (members of the Groupe Francais de Recherche
Clinique en Dermatologie Pediatrique): S. Barbarot (Nantes),
C. Bodemer (Paris), F. Boralevi (Bordeaux), C. Eschard
(Reims), F. Grange (Colmar), J.P. Lacour (Nice), C. Leaute-
Labre`ze (Bordeaux), G. Lorette (Tours), J. Mazereeuw-Hautier
(Toulouse), P. Plantin (Quimper) and A. Ta eb (Bordeaux).
The preliminary results of this study have been presented at
the Annual Meeting of the British Association of Dermatolo-
gists, Brighton 2003, on behalf of the French Clinical Research
Group on Paediatric Dermatology.
References
1 Roul S, Leaute-Labre`ze C, Boralevi F et al. Idiopathic aseptic facial
granuloma (pyodermite froide du visage): a pediatric entity? Arch Dermatol
2001; 137:12535.
2 Leaute-Labre`ze C, Maleville J, Ta eb A. Dermatoses bacteriennes.
In: Dermatologie et Maladies Sexuellement Transmissibles (Saurat JH, Gross-
hans E, Laugier P, Lachapelle JM, eds), 3rd edn. Paris: Masson,
1999; 11421.
3 Koemoth P, Fraselle R, Corea de Brito JM. Filtration of Bactec
7H12 broth cultures for identication of Mycobacterium tuberculosis
complex by Accuprobe. J Clin Microbiol 1996; 34:2301.
4 Hughes J, Lam A, Rogers M. Use of ultrasonography in the diag-
nosis of childhood pilomatrixoma. Pediatr Dermatol 1999; 16:341
4.
5 Cunliffe WJ, Baron SE, Coulson IH. A clinical and therapeutic
study of 29 patients with infantile acne. Br J Dermatol 2001;
145:4636.
6 Yencha MW. Head and neck pilomatricoma in the pediatric age
group: a retrospective study and literature review. Int J Pediatr
Otorhinolaryngol 2001; 57:1238.
7 Ohnishi T, Nakamura Y, Watanabe S. Perforating pilomatricoma in
a process of total elimination. J Am Acad Dermatol 2003; 49:S1467.
8 Strobl H, Emshoff R. Pilomatrixoma of the cheek: report of case.
J Oral Maxillofac Surg 1995; 53:13557.
9 Ellerbe DM, Parsons DS, Cook PR. Botryomycosis: improved ther-
apy for a difcult infection. Int J Pediatr Otorhinolaryngol 1997;
41:3639.
10 Lacz NL, Schwartz RA. Rosacea in the pediatric population. Cutis
2004; 74:99103.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp705708
708 Idiopathic facial aseptic granuloma, F. Boralevi et al.
PAEDI ATRI C DERMATOLOGY DOI 10. 1111/j . 1365- 2133. 2007. 07782. x
Subcutaneous fat necrosis of the newborn: a systematic
evaluation of risk factors, clinical manifestations,
complications and outcome of 16 children
E. Mahe, N. Girszyn, S. Hadj-Rabia, C. Bodemer, D. Hamel-Teillac and Y. De Prost
Department of Dermatology, Necker-Enfants Malades Hospital, Assistance Publique-Hopitaux de Paris, Paris, France
Correspondence
Emmanuel Mahe .
E-mail: emmanuel.mahe@apr.aphp.fr
Accepted for publication
24 August 2006
Key words
hypercalcaemia, newborn, subcutaneous fat
necrosis, thrombosis
Conicts of interest
None declared.
Preliminary results of this study were presented
at the 83rd Annual Meeting of the British
Association of Dermatologists, Brighton, U.K.,
July 2003.
Summary
Background Subcutaneous fat necrosis (SFN) of the newborn is a rare acute tran-
sient hypodermatitis that develops within the rst weeks of life in term infants.
It often follows a difcult delivery. Prognosis is generally good except for the
development of hypercalcaemia in severe cases. Only several case reports or small
patients series have been published.
Objectives To evaluate risk factors, complications and outcomes of SFN in 16
consecutive patients seen from 1996 to 2002 in our Department of Paediatric
Dermatology.
Methods On a case-report form created for the study, we recorded putative risk
factors concerning the mother, pregnancy and delivery, clinical aspects of SFN,
and early and late outcomes. The study was conducted in two stages: the rst
was a retrospective analysis of the observations and the second analysed data col-
lected on children and their parents during a new consultation (n 10).
Results All the children were born at term. Lesions appeared a mean of 4 days after
delivery. Three-quarters of the children had diffuse SFN. Risk factors identied
were newborn failure to thrive (12/16), forceps delivery (7/16), maternal high
blood pressure (3/10) and/or diabetes (2/10), and newborn cardiac surgery
(1/16). Putative novel risk factors were macrosomia (7/16), exposure to active
(4/10) or passive (3/10) smoking during pregnancy, putative or known mater-
nal, paternal or newborn risk factors for thrombosis (5/10), and dyslipidaemia
(2/10). Complications were hypercalcaemia (9/16), pain (4/16), dyslipidaemia
(1/16), renal insufciency (1/16) and late subcutaneous atrophy (6/6).
Conclusions This study on 16 newborns with SFN provides new information.
Familial or newborn risk factors for thrombosis are frequent. Macrosomia, famil-
ial dyslipidaemia and smoking should be evaluated. The main complications
identied were severe pain, hypercalcaemia and subcutaneous atrophy.
Subcutaneous fat necrosis (SFN) of the newborn is an acute
transient hypodermatitis that develops within the rst weeks
of life. It is a rare disorder that appears in infants born at term
or post-term. Prognosis is considered good, with complete
regression within a few weeks. The main acute complications
are hypercalcaemia that may be life threatening, dyslipidaemia
and thrombopenia. The pathophysiology of SFN remains
unknown. The most common hypothesis advanced to date is
that generalized or local (forceps) conditions might induce
subcutaneous hypoxaemia and adipocyte necrosis.
1,2
Identied predisposing factors for this condition are:
(i) maternal, including gestational diabetes mellitus, pre-
eclampsia, cocaine or calcium blocker use during pregnancy;
14
(ii) delivery complications including hypothermia, infections,
hypoxaemia and cutaneous trauma;
1,2,510
and (iii) newborn
anaemia or thrombocytosis.
11,12
Only case reports or small patient series have been pub-
lished. We evaluated 16 consecutive patients with SFN seen in
our Department of Paediatric Dermatology. The aim of the
study was to analyse systematically SFN risk factors (familial,
fetal, delivery and newborn), its clinical aspects and outcome.
Patients and methods
Patients
We retrospectively analysed the clinical histories of 16 con-
secutive patients with SFN, nine (56%) boys and seven (44%)
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715 709
girls, seen between 1996 and 2002 in our department. To be
included in the study, SFN had to be diagnosed and followed
by a paediatric dermatologist. SFN was diagnosed based on
well-described typical clinical manifestations in nine patients,
and conrmed by skin biopsy in the seven other newborns.
Case-report form for evaluation
A protocol for dermatological evaluation was implemented,
using a specic case-report form especially created for the
study. It comprised 79 items. Information was obtained on
several broad categories: parental data (age of the mother,
medical history of parents, number of pregnancies), medical
history during pregnancy (events, treatments, cocaine use),
delivery (term, modality), infant data (sex, weight, medical
problems during the rst month of life), dermatological
aspects of SFN (number, location, time after delivery, time
until diagnosis, appearance, pain, skin biopsy, radiological
explorations), early (3 months after diagnosis) and late out-
comes (from 3 months to 6 years after diagnosis), and local
and general complications.
Two stages: retrospective analysis and new consultation
for children
During the rst stage of the study, information concerning
the medical history of each patient was extracted from the
standardized form. During the second stage we wrote letters
to all the families requesting them to telephone investigators
(E.M., N.G.) for a new consultation, intended to evaluate
better parental risk factors for SFN, and conducted a physical
examinations of the children to evaluate local outcome
of the SFN. Kidney function (renal insufciency) was also
evaluated.
Evaluation of risk factors for subcutaneous fat necrosis
The maternal risk factors systematically evaluated were gesta-
tional diabetes mellitus, high blood pressure and forceps deliv-
ery. Moreover, the childs medical history during the month
following delivery was studied.
Because of a suspected role of hypoxaemia in the patho-
physiology of SFN, we questioned parents about their risk
factors for thrombosis (i.e. previous unexplained deep
venous thrombosis) and their smoking habits (active or pas-
sive) during the pregnancy. Because of a hypothesized
anomaly of lipid metabolism in the pathophysiology of
SFN, we asked the parents about familial histories of
dyslipidaemia; however, no blood lipid analyses were
performed for the study.
Results
Sixteen newborns with SFN, nine boys and seven girls, were
evaluated for the retrospective stage of the study. Eleven
(69%) families called in response to the letter: among them,
six (38%) came for a new consultation, four (25%) answered
the questions about risk factors by telephone, and one (6%)
refused to participate in the study. Five (31%) families had
moved and we did not nd their new addresses. Thus the
second stage was based on information obtained from 10
families.
Pregnancy and delivery
The mean age of the mothers at time of delivery was 33 years
(range 2142). On average, it had been the third pregnancy
(range 17); 10 of the 16 pregnancies had been uncompli-
cated. Among the other six mothers, three had high blood
pressure (mothers of patients 5, 9 and 12), two had gesta-
tional diabetes (mothers of patients 9 and 13), one had an
antiphospholipid syndrome on enoxaparin and aspirin during
pregnancy (mother of patient 4) and one was taking valproic
acid during pregnancy (mother of patient 14) for a history of
epilepsy (Table 1).
All 16 children were born at term (mean term 394 weeks,
range 3842). Six (38%) infants were delivered by caesarean
section because of fetal distress; seven (44%) others required
forceps. Thirteen of 16 (81%) newborns had general poor
condition during or immediately after the delivery (Table 1);
11 had infections. Among the latter, infections were suspected
(newborn failure to thrive + febrile newborn and/or mother)
in patients 1, 5, 7, 11, 13 and 15 and were conrmed for the
other ve by bacteriological and/or mycological cultures:
Escherichia coli in urine (patient 4) and in ear samples (patient
10), Candida albicans and Staphylococcus epidermidis in blood cultures
(patient 2), C. albicans alone in stools and urine (patient 12),
and S. epidermidis alone on skin (patient 14). These infections
always resolved with the use of appropriate antibiotics. Seven
of 16 (44%) newborns were macrosomic (dened as the 95th
percentile of normal birth weight). Other delivery complica-
tions are detailed in Table 1.
Putative novel risk factors for subcutaneous fat necrosis
Risk factors for thrombosis were identied in ve of 10 famil-
ies participating in the second stage (Table 2). Patient 4s
mother had antiphospholipid syndrome, patient 9s mother
reported unexplained deep venous thrombosis in an arm
before the pregnancy, patient 7s maternal grandmother and
great aunt reported unexplained deep venous thrombosis and
patient 14s mother took valproic acid during pregnancy.
Patient 14 developed portal vein thrombosis and had docu-
mented protein C deciency. Patient 15s father had a history
of unexplained deep venous thrombosis.
Two of 10 (20%) mothers had dyslipidaemia. The rst had
familial hypertriglyceridaemia, and it had been diagnosed in
this mother after delivery. Her child (patient 4) developed
severe hypertriglyceridaemia. The second had hypercholester-
olaemia diagnosed several months after the delivery (patient
15). Four of 10 (40%) mothers and three of 10 (30%) fathers
smoked during the pregnancy (Table 1).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
710 Subcutaneous fat necrosis of the newborn, E. Mahe et al.
T
a
b
l
e
1
P
a
r
e
n
t
a
l
a
n
d
d
e
l
i
v
e
r
y
r
i
s
k
f
a
c
t
o
r
s
f
o
r
s
u
b
c
u
t
a
n
e
o
u
s
f
a
t
n
e
c
r
o
s
i
s
i
n
1
6
n
e
w
b
o
r
n
s
P
a
t
i
e
n
t
/
s
e
x
M
e
d
i
c
a
l
h
i
s
t
o
r
y
a
t
d
e
l
i
v
e
r
y
a
n
d
d
u
r
i
n
g
r
s
t
w
e
e
k
o
f
l
i
f
e
(
n
1
6
)
M
o
t
h
e
r
(
n
1
0
)
F
a
t
h
e
r
(
n
1
0
)
F
a
i
l
u
r
e
t
o
t
h
r
i
v
e
I
n
f
e
c
t
i
o
n
M
e
c
o
n
i
u
m
-
s
t
a
i
n
e
d
a
m
n
i
o
t
i
c
u
i
d
R
e
d
-
c
e
l
l
a
l
l
o
i
m
m
u
n
i
z
a
t
i
o
n
H
y
p
o
x
a
e
m
i
a
C
o
m
a
S
e
i
z
u
r
e
s
H
y
p
o
g
l
y
c
a
e
m
i
a
C
a
r
d
i
a
c
s
u
r
g
e
r
y
F
o
r
c
e
p
s
M
a
c
r
o
s
o
m
i
a
a
R
i
s
k
f
a
c
t
o
r
s
f
o
r
t
h
r
o
m
b
o
s
i
s
b
H
i
g
h
b
l
o
o
d
p
r
e
s
s
u
r
e
c
D
i
a
b
e
t
e
s
c
R
i
s
k
f
a
c
t
o
r
s
f
o
r
t
h
r
o
m
b
o
s
i
s
b
D
y
s
l
i
p
i
d
a
e
m
i
a
A
c
t
i
v
e
s
m
o
k
i
n
g
c
R
i
s
k
f
a
c
t
o
r
s
f
o
r
t
h
r
o
m
b
o
s
i
s
b
A
c
t
i
v
e
s
m
o
k
i
n
g
c
1
/
F
+
+
+
+
2
/
M
+
+
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
3
/
F
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
4
/
M
+
+
+
+
+
+
5
/
F
+
+
+
+
+
+
+
+
6
/
M
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
7
/
M
+
+
+
+
8
/
F
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
9
/
M
+
+
+
+
+
+
1
0
/
M
+
+
+
+
+
+
1
1
/
F
+
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
1
2
/
M
+
+
+
+
+
+
+
1
3
/
M
+
+
+
+
+
1
4
/
F
+
+
+
+
+
1
5
/
M
+
+
+
+
+
+
+
1
6
/
F
+
N
E
N
E
N
E
N
E
N
E
N
E
N
E
T
o
t
a
l
1
1
5
1
7
3
2
3
1
7
7
1
3
2
4
2
4
1
3
N
E
,
n
o
t
e
v
a
l
u
a
t
e
d
.
a
M
a
c
r
o
s
o
m
i
a
i
s
d
e
n
e
d
a
s
t
h
e
9
5
t
h
p
e
r
c
e
n
t
i
l
e
o
f
n
o
r
m
a
l
b
i
r
t
h
w
e
i
g
h
t
.
b
T
h
r
o
m
b
o
s
i
s
r
i
s
k
f
a
c
t
o
r
s
a
r
e
d
e
t
a
i
l
e
d
i
n
T
a
b
l
e
2
.
c
D
u
r
i
n
g
p
r
e
g
n
a
n
c
y
.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
Subcutaneous fat necrosis of the newborn, E. Mahe et al. 711
Dermatological characteristics of subcutaneous
fat necrosis
Lesions appeared a mean of 4 days (range 29) after delivery.
Diagnosis was made a mean of 12 days (range 361) later.
Mean time to recovery from SFN was 86 days (range 25
180).
Three of 16 (19%) children had localized SFN (fewer than
four nodules; patients 2, 7 and 12) and 13 of 16 (81%) had
diffuse SFN (four or more nodules). The trunk was involved
in nine of 16 (56%) cases, the arms in seven of
16 (44%) (Fig. 1a), the head and cervical areas in seven of 16
(44%) each, and the legs in four of 16 (25%). In three of 16
(19%) infants SFN was very severe with back and limb
involvement (patients 4, 9 and 14). Four of 16 (25%) experi-
enced pain; two required morphine to control it.
Skin biopsies were taken from seven of 16 (44%) children.
Histological examination showed typical elements of SFN: gran-
ulomatous necrosis in the subcutis with crystal-like structures
in adipocytes and giant cells.
Skin ultrasonography, performed in ve of 16 (31%)
children, showed subcutaneous homogeneous high echo sig-
nals without calcications. Nuclear magnetic resonance was
performed on one child and showed low signal intensity
on T
1
-weighted images and high signal intensity on
T
2
-weighted sequences of the subcutaneous layer of
involved skin.
Complications of subcutaneous fat necrosis
Nine children (among 13 for whom calcaemia was evaluated,
69%) had hypercalcaemia (mean 33 mmol L
)1
, range 28
48, normal 2226). The mean time from the development
of SFN lesions to the diagnosis of hypercalcaemia was 24 days
(range 461). The latter resolved within 36 days (range
786) after being diagnosed. Patient 14 had symptomatic
hypercalcaemia (sleepiness, constipation).
Renal ultrasonography was performed on six of nine chil-
dren with hypercalcaemia, and detected nephrocalcinosis in
patients 4, 10 and 14. These three newborns had severe dif-
fuse SFN and their hypercalcaemia was more severe (mean
42 mmol L
)1
, range 3348) compared with the infants with-
out nephrocalcinosis (mean 29 mmol L
)1
, range 2829).
Nephrocalcinosis always resolved within 311 months. Patient
14 developed transient renal insufciency.
In newborns 4, 10 and 14 with the most severe hyper-
calcaemia (calcaemia > 3 mmol L
)1
, nephrocalcinosis, and
symptomatic hypercalcaemia), systemic treatment was neces-
sary: furosemide, prednisone and ketoconazole for patient
4, furosemide and pamedronate for patient 14, and furosem-
ide alone for patient 10. Calcaemia normalized in these three
infants in < 7 days. In the other six patients, low calcium diet
and vitamin D restriction were sufcient.
Blood lipids were analysed only in patient 4. This infant
had a severe hypertriglyceridaemia (72 mmol L
)1
, normal
< 18), without hypercholesterolaemia, that resolved sponta-
neously. His mother had familial dyslipidaemia. Glycaemia
and platelet count were not evaluated during SFN.
(b)
(a)
Fig 1. (a) Subcutaneous fat necrosis on the arm of a 15-day-old girl.
(b) Subcutaneous atrophy in the same area 3 years later.
Table 2 Thrombosis risk factors in ve
patients
Patient Family member Thrombosis risk factor
4 Mother Antiphospholipid syndrome
7 Maternal grandmother
and great aunt
Unexplained deep venous thrombosis
9 Mother Unexplained deep venous thrombosis in an arm
10 years earlier
14 Child Protein C deciency
Mother Valproic acid treatment during pregnancy
15 Father Unexplained deep venous thrombosis in the leg
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
712 Subcutaneous fat necrosis of the newborn, E. Mahe et al.
Six children underwent the second-stage dermatological
evaluation. Their mean age was 32 months (range 972). All
had a subcutaneous atrophy with no supercial skin changes
in SFN areas (Fig. 1b).
Discussion
In this study, we systematically evaluated risk factors, clinical
manifestations, complications and outcomes of SFN in 16 chil-
dren. Because of the suspected role of hypoxaemia in SFN
pathogenesis, we looked for novel putative familial risk fac-
tors, e.g. thrombosis and smoking.
Our study has several limitations that should be addressed.
The newborns were identied in a single paediatric depart-
ment of a university hospital, and may reect more severe
forms of SFN. For example, the high frequency of hypercal-
caemia might be an overestimation, reecting the rate of this
complication only in severe SFN. In addition, our report is
limited by the retrospective nature of some data. The evalua-
tion of risk factors was not exhaustive (10 families evaluated,
no blood analyses performed). Calcaemia, platelet counts and
lipid determinations were not monitored in all the newborns.
The low frequency of symptomatic hypercalcaemia could also
be explained by this retrospective evaluation. Irritability, con-
stipation and failure to thrive of these infants were not sys-
tematically evaluated during the rst consultation and may be
under-reported.
We documented a high frequency of poor general condi-
tions of newborns with SFN (e.g. infection or hypoxaemia) or
forceps delivery. Previously reported risk factors for SFN
maternal high blood pressure, gestational diabetes and new-
born cardiac surgery
1,2,10,13
were found for only a few
of our newborns. In the study by Burden and Krafchik, four
of 11 newborns had birth weights exceeding 4 kg and six of
nine mothers were at least 31 years old.
1
The results of our
study also support the roles of macrosomia, which could con-
tribute to local trauma, and relatively older maternal age,
which could increase the frequency of general maternal risk
factors, as putative risk factors for SFN.
Active or passive smoking during pregnancy was recorded
for 40% and 30%, respectively, of our study population. In
France, active smoking during pregnancy was evaluated at
19%.
14
No data are available in our country about passive
smoking during pregnancy. This apparently high frequency of
smoking herein needs to be conrmed as a risk factor for
SFN.
Another novel element systematically evaluated in our study
was familial and/or newborn risk factors for thrombosis
which were identied for ve patients (Table 2): three moth-
ers (antiphospholipid syndrome, unexplained deep venous
thrombosis and family history of unexplained deep venous
thrombosis), one father (unexplained deep venous thrombo-
sis) and one infant whose mother was taking valproic acid
during pregnancy had documented protein C deciency. Val-
proate was previously incriminated in the occurrence of deep
venous thrombosis.
15
This high frequency of thrombosis risk
factors (38%) suggests that they could be another key element
in SFN pathogenesis. Thrombosis may induce hypoxaemia
either during pregnancy or labour via microthrombosis of pla-
cental vessels (maternal thrombophilia) or after delivery in the
newborn (maternal and paternal genetic risk factors). There-
fore, systematic evaluation of thrombosis risk factors in infants
with SFN could be highly informative, not only to explain
SFN, but also to prevent later deep venous thrombosis.
Familial dyslipidaemia was previously reported and identi-
ed only when the newborn had dyslipidaemia during
SFN.
16,17
In our study, two mothers had dyslipidaemia. It was
previously postulated that lipid metabolism anomalies might
be involved in SFN pathogenesis.
2
To conrm that hypothesis,
it would be necessary to evaluate systematically blood lipid
values in the mothers of newborns with SFN.
Evaluation of immediate clinical manifestations and out-
comes of SFN conrmed previous descriptions. SFN develops
soon after delivery (mean 4 days; up to 9 days) in term
infants. It mainly affects the back, head and arms, and sponta-
neous regression is always observed within 25 months. The
initial lesions were frequently painful (25%).
3,1821
This
immediate complication must be systematically taken into
consideration so that appropriate analgesia can be adminis-
tered. The time between appearance of the rst lesion and
diagnosis (mean 12 days) suggests, rstly, lack of awareness
of this entity for some physicians and, secondly, that it is
probably underdiagnosed, especially for less severe cases.
In our study, the main immediate SFN complication
was hypercalcaemia, in agreement with previous publica-
tions.
1,5,7,8,2028
Most often, this hypercalcaemia was moder-
ate (< 3 mmol L
)1
) without clinical symptoms. Kidney
calcium deposits were identied in three infants who had
the highest blood calcium levels. One of them developed
transient renal insufciency. Among the nine newborns with
hypercalcaemia, long-term monitoring showed complete
resolution of hypercalcaemia, nephrocalcinosis and renal
insufciency. The results of this study conrmed the need
for monitoring of blood calcium levels. In our study, the
latest onset of hypercalcaemia was 2 months after diagnosis
of SFN. As no systematic monitoring of blood calcium was
carried out during the retrospective phase of the study, we
cannot state that hypercalcaemia may not start before
2 months after the appearance of the lesions. However, high
blood calcium levels were detected up to 86 days after
diagnosis of SFN. Therefore, we can recommend systematic
monitoring for 23 months of blood calcium levels in
newborns with SFN. The frequency of these determinations
will depend on the severity of SFN, results of the previous
blood analysis, and the clinical symptoms of hypercalcaemia.
For every infant with SFN we recommend at least a weekly
evaluation at the beginning of severe SFN.
The authors of many reports described calcium deposits in
kidneys,
16,23,24
vessels,
21,22
heart,
21
liver
21
or skin.
10,24,26
However, we did not nd any clinical complication directly
linked to those deposits and, thus, systematic evaluation of
heart or kidney does not seem mandatory.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
Subcutaneous fat necrosis of the newborn, E. Mahe et al. 713
The results of this study conrmed that severe dyslipidaemia
may complicate SFN. Based on our observations and previ-
ously reported cases, hypertriglyceridaemia developed after
skin lesions and resolved with the regression of those lesions.
Neither thrombopenia nor hypoglycaemia were documented
in our newborn population. However, dyslipidaemia, thrombo-
penia and hypoglycaemia, early systemic complications of
SFN,
1,6,8,16,17,2834
were not systematically evaluated herein.
Pertinently, we now think that these factors should be evalu-
ated, especially in diffuse SFN, to determine their true fre-
quency and to manage them adequately.
Our ndings highlighted the systematic progression of SFN
to subcutaneous atrophy. This complication is underevaluated
in the literature, primarily because of the absence of long-
term follow-up.
30
In our experience, parents know this skin
anomaly of their children. There is no known medical compli-
cation of this atrophy, other than diffuse atrophy over the
entire back in a few case reports, which were also limited by
their short-term follow-up. Later complications linked to skin
atrophy cannot be excluded. For example, subcutaneous atro-
phy of the buttocks might render sitting uncomfortable or
induce pain.
In conclusion, SFN is a rare event compared with the fre-
quency of newborns failing to thrive, maternal gestational dia-
betes or high blood pressure, and forceps deliveries. Hence,
multiple risk factors, as observed herein (Table 1), are prob-
ably implicated in the onset of SFN. These risk factors may be
divided in three groups: (i) maternal factors during pregnancy
including diabetes, high blood pressure, perhaps active or pas-
sive smoking and thrombosis risk factors; (ii) hypoxaemia of
the newborn, either generalized, as suggested by the high fre-
quency of poor general condition, or limited, induced by local
trauma (forceps) or more diffuse cutaneous trauma of macro-
somic infants; and (iii) a predisposing genetic background
supporting the declared family histories of dyslipidaemia and
suggesting lipid metabolism anomalies, and familial thrombo-
sis risk factors suggesting putative thrombophilia in these
newborns. All three groups of factors might be necessary to
develop SFN and should be evaluated in prospective controlled
studies.
References
1 Burden AD, Krafchik BR. Subcutaneous fat necrosis of the new-
born: a review of 11 cases. Pediatr Dermatol 1999; 16:3847.
2 Mahe E, Descamps V, Bela ch S, Crickx B. La cytosteatonecrose du
nouveau-ne. Presse Med 2002; 31:61216.
3 Rosbotham JL, Johnson A, Haque KN, Holden CA. Painful subcuta-
neous fat necrosis of the newborn associated with intra-partum use
of a calcium channel blocker. Clin Exp Dermatol 1998; 23:1921.
4 Carraccio C, Papadimitriou J, Feinberg P. Subcutaneous fat necrosis
of the newborn: link to maternal use of cocaine during pregnancy.
Clin Pediatr 1994; 33:31718.
5 Kruse K, Irle U, Uhlig R. Elevated 1,25-dihydroxyvitamin D serum
concentrations in infants with subcutaneous fat necrosis. J Pediatr
1993; 122:4603.
6 Oswalt GC, Montes LF, Cassady G. Subcutaneous fat necrosis of the
newborn. J Cutan Pathol 1978; 5:1939.
7 Norwood-Galloway A, Lebwohl M, Phelps RG, Raucher H.
Subcutaneous fat necrosis of the newborn with hypercalcemia.
J Am Acad Dermatol 1987; 16:4359.
8 Hicks MJ, Levy ML, Alexander H, Flaitz CM. Subcutaneous fat nec-
rosis of the newborn and hypercalcemia: case report and review of
the literature. Pediatr Dermatol 1993; 10:2716.
9 Walker WP, Smith RJH, Cohen MB. Fine-needle aspiration biopsy
of subcutaneous fat necrosis of the newborn. Diagn Cytopathol 1993;
9:32932.
10 Chuang SD, Chiu HC, Chang CC. Subcutaneous fat necrosis of the
newborn complicating hypothermic cardiac surgery. Br J Dermatol
1995; 132:80510.
11 Varan B, Gurakan B, Ozbek N, Emir S. Subcutaneous fat necrosis of
the newborn associated with anemia. Pediatr Dermatol 1999; 16:
3813.
12 Turba F, Bianchi C, Cella D, Rondanini GF. Thrombocytosis and neo-
natal subcutaneous adiponecrosis. Minerva Pediatr 1994; 46:3436.
13 Glover MT, Catterall MD, Atherton DJ. Subcutaneous fat necrosis in
two infants after hypothermic cardiac surgery. Pediatr Dermatol 1991;
8:21012.
14 Conference de Consensus Grossesse et Tabac. Texte des recomman-
dations (version courte). J Gynecol Obstet Biol Reprod 2005; 34:3S9
14.
15 Heckmann JG, Tomandl B, Erbguth T et al. Cerebral vein thrombo-
sis and prothrombin gene (G20210A) mutation. Clin Neurol Neurosurg
2001; 103:1913.
16 Vonk J, Janssens PMW, Demacker PNM, Folkers E. Subcutaneous
fat necrosis in a neonate, in association with aberrant plasma lipid
and lipoprotein values. J Pediatr 1993; 123:4624.
17 Janssens PMW, Vonk J, Demacker PNM. Hypertriglyceridaemia in a
case of subcutaneous fat necrosis in a newborn. Ann Clin Biochem
1993; 30:4824.
18 Ponte C, Bombart-Thoreux M, Bonte C, Neidhardt A. La cytoste-
atonecrose du nouveau-ne. Etude clinique et histochimique dune
observation avec calcications. Pediatrie 1968; 23:8215.
19 Shulzke S, Buchner S, Fahnenstich H. Subcutaneous fat necrosis of
the newborn. Swiss Med Wkly 2005; 135:1223.
20 Wiadrowski TP, Marshman G. Subcutaneous fat necrosis of the
newborn following hypothermia and complicated by pain and
hypercalcaemia. Australas J Dermatol 2001; 42:20710.
21 Dudink J, Walther FJ, Beekman RP. Subcutaneous fat necrosis of
the newborn: hypercalcemia with hepatic and atrial myocardial
calcication. Arch Dis Child Fetal Neonatal Ed 2003; 88:F3435.
22 Cunningham K, Atkinson SA, Paes BA. Subcutaneous fat necrosis
with hypercalcemia. Can Assoc Radiol J 1999; 41:1589.
23 Khan N, Licata A, Rogers D. Intravenous bisphosphonate for hyper-
calcemia accompanying subcutaneous fat necrosis: a novel treat-
ment approach. Clin Pediatr 2001; 40:21719.
24 Gu LL, Daneman A, Binet A, Kook SW. Nephrocalcinosis and
nephrolithiasis due to subcutaneous fat necrosis with hypercal-
cemia in two full-term asphyxiated neonates: sonographic ndings.
Pediatr Radiol 1995; 25:1424.
25 Scales JW, Krowchuk DP, Schwartz RP, Jorizzo JL. An infant with
rm, xed plaques. Arch Dermatol 1998; 134:4256.
26 Sharlin DN, Koblenzer P. Necrosis of subcutaneous fat with hyper-
calcemia. A puzzling and multifaceted disease. Clin Pediatr 1970;
9:2904.
27 Puzenat E, Aubin F, Zyka F et al. Cytosteatonecrose du nouveau-ne
compliquee dune hypercalcemie. Ann Dermatol Venereol 2000;
127:10879.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
714 Subcutaneous fat necrosis of the newborn, E. Mahe et al.
28 Thao Tran J, Sheth AP. Complications of subcutaneous fat necrosis
of the newborn: a case report and review of the literature. Pediatr
Dermatol 2003; 20:25761.
29 Marani M, Biasini A, Lotti V et al. Adiponecrosi del neonato associ-
ata a ipercalcemia e dislipidemia (descrizione di un caso). Ped Med
Chir 1982; 4:5634.
30 Lewis A, Cowen P, Rodda C, Dyall-Smith D. Subcutaneous
fat necrosis of the newborn complicated by hypercalcaemia
and thrombocytopenia. Australas J Dermatol 1992; 33:141
4.
31 Sharata H, Postellon DC, Hashimoto K. Subcutaneous fat necrosis,
hypercalcemia, and prostaglandin E. Pediatr Dermatol 1995; 12:437.
32 Chen TH, Shewmake SW, Hansen DD, Lacey HL. Subcutaneous
fat necrosis of the newborn. A case report. Arch Dermatol 1981;
117:367.
33 Wolach B, Raas-Rothschild A, Vogel R et al. Subcutaneous fat nec-
rosis with thrombocytopenia in a new born infant. Dermatologica
1990; 181:545.
34 Caple JI, Reyes S. Subcutaneous fat necrosis of the newborn: a case
presentation. J Perinatol 1996; 16:1401.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp709715
Subcutaneous fat necrosis of the newborn, E. Mahe et al. 715
PHOTOBI OLOGY DOI 10. 1111/j . 1365- 2133. 2006. 07684. x
The relation between sun protection factor and amount of
suncreen applied in vivo
A. Faurschou and H.C. Wulf
Department of Dermatology, D92, Bispebjerg Hospital, Bispebjerg Bakke 23, DK-2400 Copenhagen NV, Denmark
Correspondence
Annesoe Faurschou.
E-mail: Af16@bbh.hosp.dk
Accepted for publication
30 August 2006
Key words
application thickness, sun protection factor,
sunscreen
Conicts of interest
None declared.
Summary
Background The declared sun protection factor (SPF) is based on the use of a sun-
screen layer of 2 mg cm
)2
. However, only around a quarter (05 mg cm
)2
) of
this amount is applied by sunbathers. Theoretical calculations have suggested that
the effective SPF is related to sunscreen quantity in an exponential way but this
was not conrmed in vitro and has not been studied in vivo.
Objectives To investigate the relation between SPF and sunscreen amount in vivo.
Subjects and methods On the backs of 20 healthy volunteers, ve areas of 34 cm
2
each were marked. One area was phototested to determine the ultraviolet (UV)
sensitivity. Four areas were treated with a sunscreen SPF 4 in different amounts:
05, 1, 2 and 4 mg cm
)2
. Thirty minutes after sunscreen application a phototest
was conducted on each area. The effective SPF was calculated 2226 h after irradi-
ation using the UV dose needed to produce just perceptible erythema (minimal
erythema dose) on protected and unprotected skin.
Results In all areas the mean SPF was signicantly different from an SPF of 1 (no
protection) (P 00001) and the SPFs of the areas with the various amounts of
sunscreen differed signicantly from each other (P 00008). The relation
between the sunscreen amount applied and the SPF provided was most likely to
follow exponential growth (r
2
0903).
Conclusions This study indicates that the relation between SPF and sunscreen quan-
tity follows exponential growth. Application of 1 mg cm
)2
or 05 mg cm
)2
makes the SPF fall as the square or fourth root, respectively, and 4 mg cm
)2
results in an almost squared SPF.
The World Health Organization (WHO) recommends simple
precautions to prevent sunburn such as wearing protective clo-
thing, avoiding sun exposure in the middle of the day and
using a sunscreen.
1
Yet, studies have shown that on a sunny
day no more than 6567% of Danish sunbathers used one or
more suncreens at the beach and only 46% of the sunscreen
users applied the sunscreen all over the body.
24
Moreover,
the median sun protection factor (SPF) was 56 although an
SPF of at least 15 is advised.
1,3
Sunscreens must be used in an amount of 2 mg cm
)2
to
give the SPF claimed on the container (U.S. Food and Drug
Administration, FDA).
5
However, in real life the amount of
sunscreen applied was on average 05 mg cm
)2
(range: 039
079 mg cm
)2
), independent of skin type.
3,68
Dermatologists generally believe the relation between SPF
and sunscreen quantity to be linear. On a theoretical basis, the
relation between the SPF and the amount of sunscreen used
has been suggested to be exponential.
3
Hence, SPF 16 will be
reduced to SPF 2 when applied in an amount of 05 mg cm
)2
.
A study on this matter in vitro has not been able to conrm
either the exponential or linear model.
9
The theoretical
decrease in protection has however never been experimentally
proven in vivo.
3,10
We conducted this study in order to investi-
gate the relation between the sunscreen amount used and the
SPF obtained.
Subjects and methods
Subjects
Twenty healthy volunteers were recruited by advertising (age
range, 2362; females/males, 16/4). Only Fitzpatrick skin
types IIII were included.
11
One participant had skin type I,
nine subjects had skin type II and 10 had skin type III. Exposure
to the sun or a solarium was not allowed in the 4 weeks pre-
ceding the study and during the study period. Approval
was obtained from the Copenhagen Ethical Committee (KF
01-272662) and the study was performed according to the
2007 The Authors
716 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp716719
principles of the Helsinki Declaration. All the participants agreed
to take part in the trial after oral and written information.
Sunscreen treatment
Five areas of 34 cm
2
each were marked on the upper back of
each participant. The location of the areas was randomized
using a computer-generated scheme to avoid any area effect.
Four of these areas were treated with different amounts of a
commercially available sunscreen preparation SPF 4 (Garnier
Ambre Solaire, Paris, France) containing the lters terephthaly-
lidene decamphor sulphonic acid (Mexoryl SX), titanium
dioxide, butyl methoxydibenzoylmethane and benzyl salicy-
late. This level of SPF would allow us to use both thinner and
thicker layers and still be within a testable SPF. The sunscreen
was tested before the study to ensure that the SPF was close to
4 as described on the sunscreen tube. The sunscreen was
applied 30 min before irradiation in different amounts: 05,
1, 2 and 4 mg cm
)2
.
Radiation source and procedure
The ultraviolet (UV) source was a bank of broadband Philips
TL12 UVB tubes (Philips, Eindhoven, the Netherlands). Irra-
diance was measured with a UV spectroradiometer (Sola-
Hazard; Solatell, Cornwall, U.K.). The calibration of this
equipment is traceable to the National Physical Laboratory
(NPL) of the U.K. All UV doses were quantied using the
standard erythema dose (SED) of 10 mJ cm
)2
at 298 nm
(using the CIE erythema action spectrum).
12
One phototest
was conducted on each sunscreen-treated area and on one
untreated control area using a template (MED Test Patch,
Chromo-Light, Copenhagen, Denmark) lying directly on the
skin with six windows allowing UV radiation to pass
through with a dose increment of 25% (Fig. 1). Each irradi-
ated test site was 12 12 cm. A test of the transmission in
the windows was performed using an IL1700 with an SED
240 detector (International Light; Newburyport, MA, U.S.A.)
and the dose transmitted was used when calculating the SPF.
The irradiation was conducted at a distance of 50 cm. The
control area was tested 1 day prior to the sunscreen testing
to determine the UV dose needed to produce erythema in
the sunscreen-treated areas.
The induced erythema was graded visually 2024 h post-
exposure according to an established ve-point scale. The dose
to (+), the just perceptible erythema reaction, was used as the
minimal erythema dose (MED) because it can be determined
with the best precision.
13
The SPF was determined by the fol-
lowing equation: SPF MED on treated skin/MED on non-
treated skin.
Data analysis
A P-value < 005 was considered signicant. The mean and
SD was used to describe the data according to the recommen-
dations of the FDA.
5
The mean SPFs obtained in the different
areas were compared with each other using the unpaired
t-test. The relation between the amount of sunscreen used and
the SPF provided was tested for deviation from linearity and
showed a signicant nonlinear relation. The results were for
that reason analysed by nonlinear regression. The start of the
line was set to be (x,y) (0,1) because SPF is 1 when no
sunscreen is used. Data were analysed with GraphPad Prism
Version 4.03 (GraphPad Software, Inc., San Diego, CA,
U.S.A.).
Results
One patient did not attend the second visit and 19 patients
completed the study (age range, 2362 years; females/males,
16/3).
The mean SPF obtained in the various areas is given in
Table 1. In all areas the mean SPF was signicantly differ-
ent from an SPF of 1 corresponding to no protection
(P 00001). The SPFs of the different layers were signi-
cantly different from each other (P 00008). The relative SD
was calculated for each area (SD/mean) and is shown in
Table 1. The relative SD was comparable for the areas of 05,
Fig 1. The back of one of the participants showing the phototesting
setup in the four areas treated with sunscreen. In each area, a
minimal erythema dose (MED) test patch was placed directly on
the skin with six windows allowing ultraviolet radiation to pass
through with a dose increment of 25%. Each irradiated test site was
12 12 cm.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp716719
The relation between SPF and amount of suncreen applied in vivo, A. Faurschou and H.C. Wulf 717
1 and 4 mg cm
)2
. Application of 2 mg cm
)2
resulted in a
lower relative variation.
The relation between the amount of sunscreen applied and
the SPF provided was signicantly nonlinear (P 0001). The
data was therefore tested using second, third and fourth order
polynomial ts and exponential growth. The resulting r
2
val-
ues were between 090 and 091. Therefore, the method of
Akaikes Information Criterion (AIC)
14
was used to determine
which model was more likely to be correct. The probability of
the exponential growth curve to be correct was the highest
followed by the third order polynomial t (523% vs. 477%
when compared with each other). Figure 2 illustrates the
exponential t together with the linear relation showing the
latter to be unacceptable.
Table 1 shows the experimental SPFs calculated from the
linear and exponential curve ts and the theoretical SPFs esti-
mated from the use of the mean SPF of 47 in the eld protec-
ted with 2 mg cm
)2
(the value dened by the FDA
5
) and
assuming an ideal exponential or linear relation.
Discussion
Suncreens are used to prevent erythema formation from sun
exposure. The decreased amount of UV radiation reaching the
skin through sunscreens may furthermore reduce the risk of
sun-induced skin cancer.
1517
According to the FDA,
5
the sunscreen amount applied on the
skin should be 2 mg cm
)2
to secure a protection correspond-
ing to the SPF given on the sunscreen tube. However, only
around a quarter (05 mg cm
)2
) of this quantity of sunscreen
is generally used by consumers during sunbathing.
68
The SPF
is thus reduced considerably.
3,10
On a theoretical basis, it is
suggested that the effective SPF of a sunscreen is related in an
exponential way to the amount of sunscreen applied.
3
The con-
sequence of this mathematical model is that the effective SPF
cannot exceed 3 when 05 mg cm
)2
sunscreen is used even if a
sunscreen had an SPF of 81.
3
This hypothesis is based on calcu-
lations assuming that sunscreen is applied uniformly onto a at
plane, which is not the case in real life. Applied to the skin sur-
face, sunscreen tends to accumulate in the cutaneous lines,
leaving the ridges relatively unprotected and the SPF in practice
may be less than the expected SPF. Furthermore, in vitro studies
of human skin have not been able to conrm the exponential
relation.
9
However, conclusions should not be drawn from
mathematical calculations or in vitro studies, as only in vivo
studies will provide the settings matching real life.
We therefore conducted this study on human volunteers.
We demonstrated that the relation between SPF and sunscreen
quantity is most likely to follow exponential growth. As illus-
trated in Figure 2, a linear relation between sunscreen quan-
tity and SPF was not a good t.
The result of an exponential relation is that a declared SPF of,
for instance, 4, 8 and 16 yields an effective SPF on the skin
of only 14, 17 and 20, respectively, when an amount of
05 mg cm
)2
is used. However, it has been stated that an effect-
ive SPF of 2 may actually be sufcient to prevent sunburn in an
average person during an average day with risk behavior.
18
Yet,
for very sun-sensitive persons, for persons who wish a better
protection than just preventing sunburn or during long-lasting
exposure to high UV doses a greater amount of sunscreen is
Table 1 The mean sun protection factor (SPF) obtained after application of a sunscreen with a declared SPF 4 in different amounts
Sunscreen quantity
(mg cm
)2
) 05 1 2 4
Experimentally measured values Mean SPF (SD) 18 (046) 25 (059) 47 (069) 168 (380)
Calculated values Exponential t 14 20 41 169
Linear t 27 44 78 146
Theoretical values Exponential t 15 22 47 221
Linear t 19 29 47 84
The SPF was determined using the ultraviolet dose needed to produce a (+) reaction corresponding to just perceptible erythema (minimal
erythema dose) on sunscreen-treated and -untreated skin. The values of the exponential t are calculated based on the experimental data
and the equation is given in Figure 2. The theoretical SPF is in addition given using the SPF measured in the area with 2 mg cm
)2
(the true value according to FDA) to calculate the SPF when a layer of 05, 1 and 4 mg cm
)2
is applied assuming an ideal linear relation
(y 1 + 195x) or an ideal exponential growth relation based on the theoretical calculations of Wulf et al.
3
Fig 2. The relation between sunscreen quantity on the skin and the
effective sun protection factor (SPF) measured by phototesting a
sunscreen with a declared SPF 4. The equation of the linear regression
line is y 1 + 3408x but testing departure from linearity showed a
signicant nonlinear relation. The equation of the exponential t was
y 1
*
e
(07061x)
, r
2
09032.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp716719
718 The relation between SPF and amount of suncreen applied in vivo, A. Faurschou and H.C. Wulf
needed to achieve protection. Thus, a sunscreen SPF 16 must be
used at the proper thickness (2 mg cm
)2
) as an increase in SPF
can never compensate for a too thin layer of sunscreen.
The variation in SPF among the participants in the area treat-
ed with 4 mg cm
)2
looks pronounced in Figure 1. However,
when calculating the relative SD, the variation in the areas 05,
1 and 4 mg cm
)2
was similar. Application of 2 mg cm
)2
resulted in the outcome with the lowest relative variation con-
rming the FDAs statement that this is the preferred amount
of sunscreen to use in testing situations.
5
When SPF increases, greater steps of absolute UV doses (8
18 SED depending on skin type) must be used in a test area
in order to achieve erythema. To provoke erythema in the area
treated with 4 mg cm
)2
, the difference in UV dose passing
through the windows of the MED test patch was thus much
bigger than in the other areas. This could have resulted in a
less secure determination of the UV dose to MED but the rel-
ative SD did not conrm this.
We used a UVB source to provoke erythema in the partici-
pants. This source is not a perfect match to the solar spectrum.
However, this source can irradiate a huge area at one time,
and because the SPFs should be used only as relative numbers,
a small deviation in absolute SPF due to this choice of irradi-
ation source was unimportant. Furthermore, small differences
in SPF may of course occur using different sunscreens depend-
ing on the type and combination of lters.
A sunscreen with an SPF higher than 4 was not used
because application of 4 mg cm
)2
would result in an SPF too
high to test. This would require us to use quantities of sun-
screen below 05 mg cm
)2
to do the testing procedure and
amounts that low are simply not possible to apply uniformly
to an area. As Danish sunbathers in general use sunscreens
with an SPF of 56, the SPF used in our study is relevant.
3
Moreover, as calculated theoretically, we believe the exponen-
tial relation between sunscreen quantity and SPF obtained is
also applicable for sunscreens with higher SPFs, which are
regularly recommended in disease states.
3
In conclusion, this study indicates that the relation between
SPF and sunscreen amount follows exponential growth. The SPF
effect on the skin therefore falls approximately as the square
root when 1 mg cm
)2
is applied and by the fourth root when
05 mg cm
)2
is used instead of the recommended amount.
References
1 World Health Organization. Sun Protection Message for Tourists. Available
at: http://www.who.int/uv/publications/en/tourists.pdf (accessed
6 October 2006).
2 Stender IM, Lock-Andersen J, Wulf HC. Sun-protection behaviour
and self-assessed burning tendency among sunbathers. Photodermatol
Photoimmunol Photomed 1996; 12:1625.
3 Wulf HC, Stender IM, Lock-Andersen J. Sunscreens used at the
beach do not protect against erythema: a new denition of
SPF is proposed. Photodermatol Photoimmunol Photomed 1997; 13:129
32.
4 Stender IM, Andersen JL, Wulf HC. Sun exposure and sunscreen
use among sunbathers in Denmark. Acta Derm Venereol 1996; 76:31
3.
5 U.S. Food and Drug Administration, U.S. Food and Drug Administra-
tion, Department of Health and Human Services FDA. Sunscreen
drug products for over-the-counter human use. Available at: http://
www.fda.gov/cder/otcmonographs/Sunscreen/sunscreen(352).pdf
(accessed 6 October 2006).
6 Bech-Thomsen N, Wulf HC. Sunbathers application of sunscreen
is probably inadequate to obtain the sun protection factor assigned
to the preparation. Photodermatol Photoimmunol Photomed 1992/1993;
9:2424.
7 Neale R, Williams G, Green A. Application patterns among partici-
pants randomized to daily sunscreen use in a skin cancer preven-
tion trial. Arch Dermatol 2002; 138:131925.
8 Autier P, Boniol M, Severi G, Dore J-F. Quantity of sunscreen used
by European students. Br J Dermatol 2001; 144:28891.
9 Stokes R, Diffey B. How well are sunscreen users protected? Photo-
dermatol Photoimmunol Photomed 1997; 13:1868.
10 Diffey B. Sunscreen isnt enough. J Photochem Photobiol B 2001;
64:1058.
11 Fitzpatrick TB. The validity and practicality of sun-reactive skin
types I through VI. Arch Dermatol 1988; 124:86971.
12 Wulf HC, Lock-Andersen J. The Scandinavian Photodermatology
Research Group. Standard erythema dose. Skin Res Technol 1996;
4:192.
13 Lock-Andersen J, Wulf HC. Threshold level for measurement of
UV sensitivity: reproducibility of phototest. Photodermatol Photoimmunol
Photomed 1996; 12:15461.
14 Akaike H. A new look at the statistical model identication. IEEE
Transactions On Automatic Control 1974; 19:71623.
15 Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by
regular sunscreen use. N Engl J Med 1993; 329:114751.
16 Naylor MF, Boyd A, Smith DW et al. High sun protection factor
sunscreens in the suppression of actinic neoplasia. Arch Dermatol
1995; 131:1705.
17 Wulf HC, Poulsen T, Brodthagen H, Hou Jensen K. Sunscreens for
delay of ultraviolet induction of skin tumors. J Am Acad Dermatol
1982; 7:194202.
18 Thieden E, Philipsen PA, Sandby-Mller J, Wulf HC. Sunscreen use
related to UV exposure, age, sex and occupation based on personal
dosimeter readings and sun-exposure behaviour diaries. Arch Dermatol
2005; 141:96773.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp716719
The relation between SPF and amount of suncreen applied in vivo, A. Faurschou and H.C. Wulf 719
THERAPEUTI CS DOI 10. 1111/j . 1365- 2133. 2006. 07655. x
Inhibitory or scavenging action of ketoconazole and
ciclopiroxolamine against reactive oxygen species released
by primed inammatory cells
T. Nakashima, E. Sato,* Y. Niwano,* M. Kohno,* W. Muraoka and T. Oda**
NITE Biological Research Center (NBRC), National Institute of Technology and Evaluation (NITE), Chiba 292-0812, Japan
*New Industry Creation Hatchery Center, Life Particle Interaction Engineering Creation, Tohoku University, Sendai 980-8579, Japan
Research Center for Functional Food Materials, Sunny Health Co., Ltd, Saito Biotechnology Incubator, 7-7-15 Saito-Asagi, Ibaraki, Osaka 567-0085, Japan
Graduate School of Science and Technology, Nagasaki University, Nagasaki 852-8521, Japan
**Division of Biochemistry, Faculty of Fisheries, Nagasaki University, 114 Bunkyo-machi, Nagasaki 852-8521, Japan
Correspondence
Takuji Nakashima.
E-mail: takuji.nakashima@nifty.com
Accepted for publication
17 August 2006
Key words
antifungal agent, inammatory cells, NADPH
oxidase, reactive oxygen species, seborrhoeic
dermatitis
Conicts of interest
None declared.
Summary
Background Reactive oxygen species (ROS) released from inammatory cells consti-
tute one of the critical causative factors in inammatory skin diseases such as
seborrhoeic dermatitis and atopic dermatitis.
Objectives To investigate inhibitory effects of ketoconazole (KCZ) and ciclopiroxol-
amine (CPO), both of which have been used for the treatment of seborrhoeic
dermatitis, on ROS released from inammatory cells.
Methods The methyl-Cypridina-luciferin analogue-dependent chemiluminescence
method was employed for the detection of ROS production by phorbol 12-myri-
state 13-acetate (PMA)-stimulated inammatory cells. Moreover, the radical
scavenging activities of both agents were examined by using a hypoxanthine
xanthine oxidase system and the stable radical 1,1-diphenyl-2-picrylhydrazyl
(DPPH). NADPH oxidase activity was determined in particulate (membrane) frac-
tions prepared from PMA-stimulated RAW 2647 cells, a macrophage-like cell line.
Results Both of these antifungal agents inhibited PMA-stimulated ROS production.
However, only CPO signicantly scavenged both ROS generated by the hypoxan-
thinexanthine oxidase system and DPPH, and the scavenging activity of CPO
seemed to act on ROS other than superoxide anions. Although KCZ inhibited
PMA-stimulated ROS production, it did not show radical-scavenging activities.
The inhibition of ROS production by KCZ is probably attributable to the inhibi-
tion of NADPH oxidase activity.
Conclusions The mechanism of the inhibitory action of KCZ against PMA-stimulated
ROS production is distinct from that of CPO. Knowledge of the inhibitory or
scavenging effects of both antifungal agents on ROS released from inammatory
cells may be useful in developing a therapeutic strategy for dermatitis.
Seborrhoeic dermatitis is a chronic inammatory disorder fre-
quently seen in the head and trunk where sebaceous glands
are most prominent. The disease causes a pale redness, with
white and itchy scales. It is also common in patients with Par-
kinsons disease or human immunodeciency virus infec-
tion.
1,2
Although many factors including hormonal balance
3
and lipophilic yeasts of the genus Malassezia
4
have been impli-
cated, the aetiology of seborrhoeic dermatitis remains
unknown.
The mechanisms for the development of seborrhoeic
dermatitis caused by Malassezia yeasts are not fully understood.
However, it has been speculated that free fatty acids produced
by lipase of Malassezia stimulate the inammatory cells
58
to
generate reactive oxygen species (ROS). The activation of
inammatory cells is considered to be a consequence of
overaggressive inammatory response in patients with sebor-
rhoeic dermatitis.
2,3
Combinations of anti-inammatory and antifungal agents
are often applied for the treatment of seborrhoeic dermatitis.
Topical corticosteroids as anti-inammatory agents rapidly
reduce the severity of this disease, but allow early relapse of
the dermatitis after discontinuing treatment. In addition,
2006 The Authors
720 Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
chronic use of stronger steroids may lead to a rebound phe-
nomenon, steroid dermatitis and rosacea-like lesions.
8,9
Anti-
fungal agents do not produce such adverse reactions with
repeated use. Therefore, antifungal agents with an anti-inam-
matory potential may be benecial for the treatment of
patients with seborrhoeic dermatitis.
Ketoconazole (KCZ) and ciclopiroxolamine (CPO) have
been used for the treatment of seborrhoeic dermatitis.
6
KCZ
and CPO are synthetic antifungal agents derived from
imidazole and hydroxypyridone respectively (Fig. 1). Both
agents have also been reported to exert anti-inammatory
activities.
1015
It has been reported that KCZ inhibits thromboxane syn-
thase, an enzyme in the synthetic pathway of thromboxane A2
that acts as a potent pulmonary vasoconstrictor and aggregator
of platelets and neutrophils.
12
This antifungal agent also inhib-
its 5-lipoxygenase, an enzyme necessary to generate leucotri-
enes, which results in a decreased leucotriene B
4
production.
12
It has been reported that CPO inhibits synthesis of prostaglan-
din and leucotriene in human neutrophils.
13
CPO may also
exert anti-inammatory effects by inhibition of 5-lipoxgenase
and cyclooxygenase.
11
In this study, we found that either CPO or KCZ inhibits
ROS production by a mouse macrophage cell line, RAW 2647
cells, and address the proposed mechanisms of their inhibitory
action.
Materials and methods
Animals
Five-week-old female ddY mice (Kyudo Co., Ltd, Fukuoka,
Japan) were used for preparation of peritoneal polymorpho-
nuclear leucocytes (PMN). Mice were housed with controlled
lighting (12 h light/12 h dark) at 21 C and given food and
water ad libitum. All animal experiments were performed
according to the guidelines for the care and use of animals
approved by Nagasaki University.
Reagents
KCZ was purchased from Wako Pure Chemical Industries, Ltd
(Tokyo, Japan). CPO was purchased from Sigma-Aldrich Co.
(St Louis, MO, U.S.A.). Stock solutions of antifungal agents
were prepared in dimethyl to a concentration of 10 mg mL
)1
.
Reagents were purchased from the following sources: methyl-
Cypridina-luciferin analogue (MCLA) was from Tokyo Kasei
Kogyo Co., Ltd (Tokyo, Japan); phorbol 12-myristate 13-acetate
(PMA), hypoxanthine, L-ascorbic acid, phenylmethylsulphonyl
uoride (PMSF), 1,1-diphenyl-2-picrylhydrazyl (DPPH), ethyl-
eneglycol bis-(2-aminoethylether)-N,N,N,N-tetraacetic acid
(EGTA), N-acetyl-L-cysteine and mannitol were from Wako Pure
Chemical Industries, Ltd; and xanthine oxidase, catalase and
superoxide dismutase (SOD) were from Sigma-Aldrich Co.
Preparation of mouse peritoneal polymorphonuclear
leucocytes
Each mouse was injected intraperitoneally with 2 mL of 5%
(w/v) casein dissolved in sterile saline and, 6 h after the
injection, were killed by cervical dislocation. The lavage uid
(4 mL) was collected in a syringe, and exudated peritoneal
cells were precipitated by centrifugation. PMN were further
puried from the peritoneal cells by Percoll stepwise density
gradient (1090 and 1070 g mL
)1
) centrifugation (600 g for
20 min at 4 C). The purity of PMN was 95% as determined
by staining with MayGrunwaldGiemsa. Resulting PMN were
suspended in KrebsRinger phosphate (KRP) buffer containing
11 mmol L
)1
glucose (pH 74) at a concentration of
5 10
6
cells mL
)1
.
Preparation of RAW 2647 cells
RAW 2647 cells (a mouse macrophage cell line) were obtained
from the American Type Culture Collection (Rockville, MD,
U.S.A.), and cultured in RPMI 1640 supplemented with 10%
fetal bovine serum, penicillin (100 lg mL
)1
) and streptomycin
(100 lg mL
)1
) as described previously.
16
The adherent cells in
the asks were washed twice with sterile phosphate-buffered
saline (PBS). The cells were subsequently scraped using a cell
scraper (Becton Dickinson and Co., Franklin Lakes, NJ, U.S.A.)
and were then resuspended in KRP buffer containing
11 mmol L
)1
glucose at a concentration of 5 10
6
cells mL
)1
.
Reactive oxygen species production by phorbol
12-myristate 13-acetate-stimulated polymorphonuclear
leucocytes and RAW 2647 cells
ROS production by PMA-stimulated inammatory cells was
measured as previously described.
17
The cell suspension was
dispensed in a 100-lL volume (5 10
5
cells per well) using
(a)
(b)
Fig 1. Structures of ketoconazole (a) and ciclopirox olamine (b).
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
Inhibition of ROS by antifungal agents, T. Nakashima et al. 721
a multichannel pipette into 96-well microtitre plates (Dynex
Microlite
TM
1; Dynex Technologies, Chantilly, VA, U.S.A.),
and then MCLA (at a nal concentration of 10 lmol L
)1
) and
each antifungal agent (at nal concentrations ranging from 0
to 100 lg mL
)1
) or an inhibitor (SOD, catalase, N-acetyl-L-
cysteine or mannitol) was added. After incubation for 3 min
at 37 C, the reaction was initiated by the addition of PMA (at
a nal concentration of 1 lg mL
)1
), and the chemilumines-
cence intensity of each well was recorded continuously for
30 min and 15 min at 37 C in PMN and RAW 2647 cells,
respectively, using a chemiluminescence microplate recorder
(Mithras LB940; Berthold Technologies GmbH and Co. KG,
Bad Wildbad, Germany).
Hypoxanthinexanthine oxidase cell-free system
To study the scavenging ability of KCZ or CPO in a cell-free
system, the hypoxanthinexanthine oxidase reaction was
applied for ROS generation. Twenty microlitres of the reaction
mixture containing 100 lmol of MCLA, 50 mU of xanthine
oxidase and 06 mmol of ethylenediamine tetraacetic acid in
50 mmol L
)1
TrisHCl buffer (pH 74) was put into each well
of a 96-well microtitre plate. Sixty microlitres of KCZ or CPO
solution was then added to each well at nal concentrations
ranging from 1 to 100 lg mL
)1
. After incubation for 07 min
at 37 C, the reaction was triggered by the addition of 100 lL
of 1 mmol L
)1
hypoxanthine, and the chemiluminescence
intensity of each well was recorded continuously for 57 min
as described above.
1,1-Diphenyl-2-picrylhydrazyl-scavenging activity
The DPPH-scavenging activity was analysed by the following
method. DPPH was dissolved in dimethylformamide
(10 mg mL
)1
) and then diluted with 01 mol L
)1
TrisHCl
buffer (pH 76) containing 5% Triton X-100 at a concentra-
tion of 120 lmol L
)1
. Eight hundred microlitres of KCZ or
CPO solution was then added to 200 lL of a 120 lmol L
)1
DPPH solution at nal concentrations ranging from 25 to
100 lg mL
)1
.
After incubation for 20 min in the dark at room temperature,
the absorbance at 517 nm was measured. The solvent and
100 lg mL
)1
of ascorbic acid were used as a negative and a
positive control, respectively. A decrease in the absorbance of
DPPH was measured and the radical scavenging activity was cal-
culated using the following equation: radical scavenging activity
(%) [1 ) (As ) Ap)/(An ) Ap)] 100, where Ap is the
absorbance of the ascorbic acid, An is the absorbance of the
control reaction containing all reagents except the test com-
pound and As is the absorbance of the test compound.
Measurement of NADPH oxidase activity in subcellular
fractions
The effects of the antifungal agents on NADPH oxidase activity
were evaluated using the Triton X-100 method, basically as
described previously.
18
In brief, RAW 2647 cells
(2 10
7
cells mL
)1
) were pretreated with 100 lg mL
)1
of
KCZ or CPO at 37 C for 10 min. Subsequently, 90 lL of the
cells (approximately 2 10
6
cells) were stimulated by the
addition of 10 lL of 100 lmol L
)1
PMA. After incubation at
37 C for 10 min in order to make maximal NADPH oxidase
activity (Fig. 2d,e), the cell suspension was centrifuged at
1500 g for 5 min at 4 C. The pellet was resuspended in
Triton X-100 lysis buffer (1% Triton X-100 in TrisHCl,
pH 74, containing 5 mmol L
)1
EGTA, 1 mmol L
)1
PMSF,
10 mmol L
)1
aprotinin, 10 mmol L
)1
leupeptin and
10 mmol L
)1
pepstatin). The cells were disrupted three times
by sonication for 10 s on ice using a Handy Sonic (Tomy
Seiko Co., Ltd, Tokyo, Japan). After standing for 10 min on
ice, the intact cells were removed by centrifugation at 500 g
for 5 min at 4 C. The sonicates were centrifuged at
100 000 g for 30 min at 4 C. After the supernatant was
removed, the pellet was washed with iced PBS and gently
resuspended in KRP buffer containing 11 mmol L
)1
glucose
(pH 74) at a nal concentration of 10 mg mL
)1
protein and
was used as a membrane fraction. The NADPH oxidase activity
of the membrane fraction was measured by adding an aliquot
of NADPH at a nal concentration of 400 lmol L
)1
.
18
NADPH
oxidase activity was determined by the intensity of MCLA-
dependent chemiluminescence measured using a chemilumi-
nescence microplate recorder (Mithras LB940).
Statistical analysis
Data are presented as the mean SD of triplicate measure-
ments. Individual treatment groups were compared with
appropriate controls using Dunnetts multiple comparison test.
Results
Effect of antifungal agents on reactive oxygen species
production by phorbol 12-myristate 13-acetate-
stimulated polymorphonuclear leucocytes and RAW 2647
cells
The MCLA-dependent chemiluminescence method was
employed for the detection of ROS production by PMN or
RAW 2647 cells. The addition of PMA to PMN or RAW
2647 cells caused an increase in MCLA-dependent chemilumi-
nescence intensity. In PMA-stimulated PMN and RAW 2647
cells, the chemiluminescence intensity continued to increase
and reached a peak in PMN and RAW 2647 cells at approxi-
mately 20 and 10 min, respectively, after the addition of PMA
(Fig. 2a,b,d,e). SOD (10 U) inhibited the chemiluminescence
response by 715 09% and 732 11% in PMA-stimulated
PMN and RAW 2647 cells, respectively. As shown in Figure 2,
KCZ and CPO had potent inhibitory activity towards ROS
production by PMA-stimulated PMN and RAW 2647 cells
in a concentration-dependent manner. In both cases, the
magnitude of inhibition at 25 lg mL
)1
of KCZ and 50
100 lg mL
)1
of CPO was comparable with that given by
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
722 Inhibition of ROS by antifungal agents, T. Nakashima et al.
10 U of SOD. KCZ had slightly more potent inhibitory activity
than CPO on PMA-stimulated ROS production.
Effect of antifungal agents on reactive oxygen species
levels generated by hypoxanthinexanthine oxidase
cell-free system
A cell-free system with hypoxanthinexanthine oxidase was
used to measure the scavenging ability of KCZ and CPO against
ROS. The addition of CPO (100 lg mL
)1
) signicantly reduced
the amount of ROS released in the hypoxanthinexanthine oxid-
ase system (P < 0.05, Fig. 3), but the magnitude of inhibition
was relatively poor when compared with that given by SOD.
KCZ had no effect on ROS production under these conditions.
Effect of antifungal agents on the stable radical
1,1-diphenyl-2-picrylhydrazyl
The radical-scavenging test using the stable radical DPPH is
widely used to evaluate antioxidant activity. Figure 4 illustrates
0
1000
2000
3000
Time (min)
0
0 20 40 60 80 100 0 20 40 60 80 100
20
40
60
80
100
Concentration (g mL
1
)
0
20
40
60
80
100
Concentration (g mL
1
)
0
0 5 10 15
0 5 10 15
0 5 10 15
20 25 30
0 5 10 15 20 25 30
1000
2000
3000
Time (min)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
(
i
n
t
e
n
s
i
t
y
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
(
i
n
t
e
n
s
i
t
y
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
r
e
s
p
o
n
s
e
(
%
o
f
c
o
n
t
r
o
l
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
r
e
s
p
o
n
s
e
(
%
o
f
c
o
n
t
r
o
l
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
(
i
n
t
e
n
s
i
t
y
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
(
i
n
t
e
n
s
i
t
y
)
0
1000
2000
3000
Time (min)
0
1000
2000
3000
Time (min)
(a)
(b)
(d)
(c)
(e)
(f)
Fig 2. Effect of antifungal agents on reactive oxygen species (ROS) production by phorbol 12-myristate 13-acetate (PMA)-stimulated
polymorphonuclear leucocytes (PMN) and RAW 2647 cells. Ketoconazole (KCZ) and ciclopiroxolamine (CPO) in 50% dimethyl (DMSO) (nal
concentration 5% DMSO) were added to PMN or RAW 2647 cells (5 10
5
cells per well) in each well of a 96-well microplate. The control
consisted of 5% DMSO in KrebsRinger phosphate buffer containing 11 mmol L
)1
glucose, pH 74. The chemiluminescence response to ROS
production by PMA-stimulated PMN (ac) and RAW 2647 cells (df) is shown. The time-course of methyl-Cypridina-luciferin analogue-dependent
chemiluminescence intensity in PMA-stimulated ROS production for CPO (a, d) and KCZ (b, e) is shown: PMA alone (dark grey triangles),
25 lg mL
)1
of CPO (dark grey circles), 50 lg mL
)1
of CPO (light grey circles), 100 lg mL
)1
of CPO (unshaded circles), 25 lg mL
)1
of KCZ
(dark grey squares), 50 lg mL
)1
of KCZ (light grey squares) and 100 lg mL
)1
of KCZ (unshaded squares). (c, f) Inhibitory effects of KCZ (dark
circles) and CPO (unshaded circles) on PMA-stimulated ROS production. Total chemiluminescence counts were integrated for 30 min in PMN (c)
and for 15 min in RAW 2647 cells (f). Experiments were performed in triplicate. Error bars represent SD.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
Inhibition of ROS by antifungal agents, T. Nakashima et al. 723
the DPPH-scavenging activity of KCZ and CPO. CPO signi-
cantly decreased the DPPH level in a concentration-dependent
manner. KCZ had no effect on the DPPH level even at the
highest concentration (100 lg mL
)1
).
Effect of antifungal agents on NADPH oxidase activity
ROS production by macrophages depends on the assembly
of cytosolic and membrane-associated components to form
active NADPH oxidase through a process regulated by pro-
tein kinase.
19
As an experimental system for the assembly
of NADPH oxidase components, a membrane fraction was
prepared from PMA-stimulated RAW 2647 cells pretreated
with each antifungal agent, and the NADPH oxidase activity
was determined. As shown in Figure 5, the activation of
NADPH oxidase by PMA stimulation was signicantly in-
hibited by KCZ as well as by staurosporine, which is an
inhibitor of protein kinase C. CPO showed approximately
20% inhibition of NADPH oxidase activity when compared
with that in the control (PMA alone) but the difference
was not signicant.
Effect of authentic inhibitors on reactive oxygen species
production by phorbol 12-myristate 13-acetate-
stimulated RAW 2647 cells
To identify ROS that could be detected by MCLA-dependent
chemiluminescence assay in this study, the following inhi-
bitors were used: SOD, catalase, N-acetyl-L-cysteine and
mannitol. As shown in Figure 6, SOD (1000 U mL
)1
) and
N-acetyl-L-cysteine (10 mmol L
)1
) had potent inhibitory
activity towards ROS production by PMA-stimulated RAW
2647 cells but neither catalase nor mannitol was effective. It
has been reported that N-acetyl-L-cysteine scavenges hydroxyl
radical (
OH), hypochlorous acid (HOCl) and hydrogen per-
oxide (H
2
O
2
), but this compound has no scavenging activity
against superoxide anion (O
2
).
20,21
Therefore, these results
suggest that not only O
2
but also other ROS produced by
PMA-stimulated RAW 2647 cells can be detected by MCLA-
dependent chemiluminescence assay.
Discussion
As a result of an improved understanding of the pathogenesis
of seborrhoeic dermatitis, it has been recognized that treat-
ment with antifungal agents is an effective therapy with
advantages over other agents such as topical corticosteroids.
22
*
**
**
**
0
20
40
60
80
100
Control CPO KCZ SOD
C
h
e
m
i
l
u
n
i
n
e
s
c
e
n
c
e
r
e
s
p
o
n
s
e
(
%
o
f
c
o
n
t
r
o
l
)
Fig 3. The inhibitory effect on production of superoxide anions by
the hypoxanthinexanthine oxidase system. Superoxide anions were
measured by the chemiluminescence method in a reaction mixture
consisting of 50 mmol L
)1
TrisHCl buffer (pH 74) containing
0.6 mmol L
)1
ethylenediamine tetraacetic acid, methyl-Cypridina-
luciferin analogue and xanthine oxidase. The antifungal agents
ketoconazole (KCZ) or ciclopiroxolamine (CPO) or superoxide
dismutase (SOD) were added at various concentrations: antifungal
agents at the nal concentration of 1 lg mL
)1
(dark grey bars),
10 lg mL
)1
(light grey bars) or 100 lg mL
)1
(unshaded bars);
SOD at the nal concentration of 1 U mL
)1
(dark grey bar),
10 U mL
)1
(light grey bar) or 100 U mL
)1
(unshaded bar).
Control (black bar) is an alternative to test compounds. Generation
of superoxide anions was initiated by the addition of hypoxanthine
to the reaction mixture. Experiments were performed in triplicate.
Error bars represent SD. Signicant differences between the control
and treatment groups are indicated: *P < 005; **P < 001.
*
40
60
80
100
KCZ CPO
S
c
a
v
e
n
g
i
n
g
a
c
t
i
v
i
t
y
(
%
o
f
c
o
n
t
r
o
l
)
*
**
Fig 4. Effects of the antifungal agents ketoconazole (KCZ) or
ciclopiroxolamine (CPO) on the stable radical 1,1-diphenyl-2-
picrylhydrazyl (DPPH). The stable DPPH radical was used for the
antioxidant assay of antifungal agents. Each antifungal agent was
added to DPPH solution at various concentrations (dark grey bars,
25 lg mL
)1
; light grey bars, 50 lg mL
)1
; unshaded bars,
100 lg mL
)1
), and the reaction mixture was incubated for 30 min at
room temperature. The reaction mixtures were measured at 517 nm.
Experiments were performed in triplicate. Error bars represent SD.
Signicant differences between the control and treatment groups are
indicated: *P < 005; **P < 001.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
724 Inhibition of ROS by antifungal agents, T. Nakashima et al.
As antifungal agents with anti-Malassezia activity led to many
successful outcomes in patients with seborrhoeic dermatitis,
Malassezia yeasts are considered to be causative organisms in
this disease.
11,2224
Although simple overgrowth of Malassezia is
unlikely to be the cause of seborrhoeic dermatitis, the several
lines of evidence suggest that the organisms are very import-
ant in its aetiology. For instance, it has been reported that the
release of free fatty acids by lipase from Malassezia species
might cause the activation of inammatory cells.
47
ROS,
including H
2
O
2
and free radicals, produced by the activation
of primed inammatory cells, have potentially deleterious
effects on the biological system as they can damage proteins,
lipids and nucleic acids.
2527
Several types of inammatory cells such as neutrophils and
macrophages play an important role in acute inammatory
processes. However, in chronic and overaggressive inamma-
tory conditions, ROS may also be released into the extracellu-
lar compartment, and may cause local propagation of the
inammatory reaction and tissue damage.
28,29
Therefore, the
inhibition of ROS production or scavenging of the released
ROS may be important in preventing excess tissue damage in
dermatitis.
In this study, we examined the effects of KCZ and CPO,
both of which are antifungal agents used for the treatment of
seborrhoeic dermatitis, on ROS produced by PMA-stimulated
PMN or RAW 2647 cells (a macrophage cell line). The ROS
levels were reduced by both antifungal agents in a concentra-
tion-dependent manner (Fig. 2). The inhibitory activity of
KCZ was slightly more potent than that of CPO. The magni-
tude of ROS reduction at 25 lg mL
)1
of KCZ and 50
100 lg mL
)1
of CPO was comparable with that given by
10 U of SOD.
To elucidate the mechanisms by which both antifungal
agents reduced the level of ROS, we tested radical-scavenging
effects of both antifungal agents on ROS generated by the
hypoxanthinexanthine oxidase system and the stable radical
DPPH. As shown in Figures 3 and 4, CPO, but not KCZ,
showed radical-scavenging activities in both systems in a con-
centration-dependent manner. In addition, it was suggested
that KCZ and CPO exert no scavenging effect on O
2
because
both drugs showed no effects on SOD-inhibitable reduction of
cytochrome c in the hypoxanthinexanthine oxidase system
(data not shown). MCLA has been conrmed to be sensitive
to ROS other than O
2
, such as singlet oxygen (
1
O
2
) and
OH.
3032
Moreover, as shown in Figure 6, ROS released from
PMA-stimulated RAW 2647 cells were inhibited by N-acetyl-
L-cysteine, which is known as a scavenger of
OH, HOCl and
H
2
O
2
but not O
2
. These results raise the possibility that CPO
has scavenging activities towards ROS other than O
2
. The
specication of ROS scavenged by CPO needs to be conrmed
by further investigation.
Although KCZ inhibited ROS production by PMA-stimulated
PMN or RAW 2647 cells, this antifungal agent had no effect
0
**
**
20
40
60
80
100
Drug
free
PMA +KCZ +CPO +STA
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
r
e
s
p
o
n
s
e
(
%
o
f
c
o
n
t
r
o
l
)
Fig 5. Effects of ketoconazole (KCZ) and ciclopiroxolamine (CPO)
on subcellular NADPH oxidase activity. RAW 2647 cells
(2 10
7
cells mL
)1
) were pretreated with 100 lg mL
)1
of KCZ or
CPO at 37 C for 10 min. The cells were subsequently stimulated
with phorbol 12-myristate 13-acetate (PMA) at 37 C for 10 min, and
nally, their membranes were fractionated. Generation of reactive
oxygen species was initiated by adding NADPH to the membrane
aliquots. NADPH oxidase activity was measured as the intensity of
methyl-Cypridina-luciferin analogue-dependent chemiluminescence.
Staurosporine (STA, 05 lg mL
)1
nal concentration), which is an
inhibitor of protein kinase C, was used as positive control.
Experiments were performed in triplicate. Error bars represent SD.
Signicant differences between the groups with and without each
antifungal agent are indicated: **P < 001 vs. control.
0
**
**
20
40
60
80
100
P
M
A
a
l
o
n
e
+
S
O
D
(
1
0
0
0
U
m
L
1
)
+
C
a
t
a
l
a
s
e
(
1
0
0
0
U
m
L
1
)
+
N
-
a
c
e
t
y
l
-
L
-
c
y
s
t
e
i
n
e
(
1
0
m
M
)
+
M
a
n
n
i
t
o
l
(
1
0
m
M
)
C
h
e
m
i
l
u
m
i
n
e
s
c
e
n
c
e
r
e
s
p
o
n
s
e
(
%
o
f
c
o
n
t
r
o
l
)
Fig 6. Effects of various inhibitors on reactive oxygen species
production by phorbol 12-myristate 13-acetate (PMA)-stimulated
RAW 2647 cells. Each inhibitor was added to RAW 2647 cells
(5 10
5
cells per well) in each well of a 96-well microplate. Brackets
denote the nal concentration of each inhibitor. After incubation of
the mixture for 3 min at 37 C, the reaction was initiated by the
addition of PMA. The intensity of methyl-Cypridina-luciferin analogue-
dependent chemiluminescence was recorded continuously over
15 min for PMA-stimulated RAW 2647 cells. Experiments were
performed in triplicate. Error bars represent SD. Signicant differences
between the groups are indicated: **P < 001 vs. control. SOD,
superoxide dismutase.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
Inhibition of ROS by antifungal agents, T. Nakashima et al. 725
on ROS generated by the hypoxanthinexanthine oxidase sys-
tem and the stable radical DPPH. To elucidate the inhibitory
mechanism of KCZ towards ROS production by PMA-stimula-
ted RAW 2647 cells further, we examined the effect on
NADPH oxidase activity by using a cell-free system. As shown
in Figure 5, KCZ, but not CPO, signicantly inhibited the acti-
vation of NADPH oxidase in PMA-stimulated RAW 2647 cells.
However, KCZ could not completely inhibit the NADPH oxid-
ase activity, whereas this drug almost completely inhibited
ROS production by PMA-stimulated RAW 2647 cells (Fig. 2).
The inhibitory rates at 100 lg mL
)1
of KCZ were approxi-
mately 97% and 60% in PMA-stimulated RAW 2647 cells and
the NADPH oxidase cell-free system, respectively. Inamma-
tory cells such as PMN and macrophages generate the various
ROS species including O
2
, H
2
O
2
and
OH during the respira-
tory burst.
3335
We suggest that RAW 2647 cells treated with
PMA produce ROS other than O
2
because the ROS level was
reduced by N-acetyl-L-cysteine, an inhibitor of ROS other than
O
2
(Fig. 6). Therefore, it is possible that KCZ inhibits
NADPH-dependent production of O
2
and other ROS. It is
strongly suggested that KCZ and CPO reduce the level of ROS
produced by PMA-stimulated PMN and RAW 2647 cells but
that there are differences between KCZ and CPO in the inhibi-
tory mechanism.
Hegemann et al. have reported that KCZ showed no inhibi-
tory effect on the PMA-induced release of O
2
from human
neutrophils by using the method of SOD-inhibitable reduction
of cytochrome c.
36
Their assay method for the detection of
ROS was different from that used in our study. The SOD-inhi-
bitable reduction of cytochrome c method has been widely
used for the detection of ROS released from neutrophils and
macrophages, and can specically detect O
2
.
37,38
In this
study, the inhibitory activity of KCZ against PMA-stimulated
ROS production was detected by MCLA-dependent chemilumi-
nescence instead of the cytochrome c method. MCLA has been
used as a hypersensitive chemiluminescence probe for the
detection of various ROS.
39
The mechanism of reaction
between MCLA and ROS involves a dioxetane analogue
produced by decarboxylation and protonation of an excited
carbonyl compound, and light at 465 nm is emitted by
de-excitation.
31
The O
2
generated by NADPH oxidase serves
as a starting material for the production of a large variety of
reactive oxidants, including oxidized halogens, free radicals
and
1
O
2
.
40
The O
2
through NADPH oxidase may be rapidly
transformed into other ROS as secondary products by physio-
logical and physical factors, and the ROS, of which KCZ can
reduce the production, may be detected by the MCLA method.
Therefore, differences in the detection of PMA-stimulated ROS
production may account for these discrepancies.
Our results suggest that both CPO and KCZ can reduce the
level of ROS released from primed inammatory cells by
different mechanisms, which might contribute to their anti-
inammatory action. This information may be useful not only
in the treatment of seborrhoeic dermatitis but also of other
dermatitides associated with inammation such as atopy and
dermatophytosis.
Acknowledgments
We are grateful to co-workers in the Division of Biochemistry,
Faculty of Fisheries, Nagasaki University for their technical
help.
References
1 Schaub NA, Drewe J, Sponagel L et al. Is there a relation between
risk groups or initial CD4 T cell counts and prevalence of seborr-
heic dermatitis in HIV-infected patients? Dermatology 1999;
198:1269.
2 Martignoni E, Godi L, Pacchetti C et al. Is seborrhea a sign of auto-
nomic impairment in Parkinsons disease? J Neural Transm 1997;
104:1295304.
3 Zouboulis CC, Xia L, Akamatsu H et al. The human sebocyte culture
model provides new insights into development and management
of seborrhoea and acne. Dermatology 1998; 196:2131.
4 Bergbrant IM. Seborrhoeic dermatitis and Pityrosporum yeasts. Curr
Top Med Mycol 1995; 6:95112.
5 Brunke S, Hube B. MfLIP1, a gene encoding an extracellular lipase
of the lipid-dependent fungus Malassezia furfur. Microbiology 2006;
152:54754.
6 Potter BS, Burgoon CF Jr, Johnson WC. Pityrosporum folliculitis.
Report of seven cases and review of the Pityrosporum organism rela-
tive to cutaneous disease. Arch Dermatol 1973; 107:38891.
7 Ran Y, Yoshiike T, Ogawa H. Lipase of Malassezia furfur: some prop-
erties and their relationship to cell growth. J Med Vet Mycol 1993;
31:7785.
8 Inoue Y, Isobe M, Shiohara T, Hayashi H. Inhibitory activity of
CX-659S, a novel diaminouracil derivative, against the rebound
phenomenon following withdrawal of corticosteroid therapy for
chronic contact hypersensitivity responses. Int Arch Allergy Immunol
2003; 131:14352.
9 Litt JZ. Steroid-induced rosacea. Am Fam Physician 1993; 48:6771.
10 Bernard GR, Artigas A, Brigham KL et al. The AmericanEuropean
Consensus Conference on ARDS. Denitions, mechanisms, relevant
outcomes, and clinical trial coordination. Am J Respir Crit Care Med
1994; 149:81824.
11 Hanel H, Smith-Kurtz E, Pastowsky S. Therapy of seborrheic
eczema with an antifungal agent with an antiphlogistic effect.
Mycoses 1991; 34 (Suppl. 1):913.
12 Lelcuk S, Huval WV, Valeri CR et al. Inhibition of ischemia-induced
thromboxane synthesis in man. J Trauma 1984; 24:3936.
13 Abrams B, Hanel H, Hoehler T. Ciclopirox olamine: a hydroxypyri-
done antifungal agent. Clin Dermatol 1992; 9:4717.
14 Rosen T, Schell BJ, Orengo I. Anti-inammatory activity of antifun-
gal preparations. Int J Dermatol 1997; 36:78892.
15 Williams JG, Maier RV. Ketoconazole inhibits alveolar macrophage
production of inammatory mediators involved in acute lung
injury. Surgery 1992; 112:2707.
16 Higuchi S, Tamura T, Oda T. Cross-talk between the pathways
leading to the induction of apoptosis and the secretion of tumor
necrosis factor-a in ricin-treated RAW 2647 cells. J Biochem 2003;
134:92733.
17 Nakashima T, Kurachi M, Kato Y et al. Characterization of bacter-
ium isolated from the sediment at coastal area of Omura Bay in
Japan and several biological activities of pigment produced by this
isolate. Microbiol Immunol 2005; 49:40715.
18 Tsunawaki S, Yoshikawa K. Relationships of p40(phox) with
p67(phox) in the activation and expression of the human respira-
tory burst NADPH oxidase. J Biochem 2000; 128:77783.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
726 Inhibition of ROS by antifungal agents, T. Nakashima et al.
19 Nauseef WM. Assembly of the phagocyte NADPH oxidase. Histochem
Cell Biol 2004; 122:27791.
20 Aruoma OI, Halliwell B, Hoey BM, Butler J. The antioxidant action
of N-acetylcysteine: its reaction with hydrogen peroxide, hydroxyl
radical, superoxide, and hypochlorous acid. Free Radic Biol Med 1989;
6:5937.
21 Gillissen A, Scharling B, Jaworska M et al. Oxidant scavenger
function of ambroxol in vitro: a comparison with N-acetylcysteine.
Res Exp Med (Berl) 1997; 196:38998.
22 Gupta AK, Nicol K, Batra R. Role of antifungal agents in the treat-
ment of seborrheic dermatitis. Am J Clin Dermatol 2004; 5:41722.
23 Bohn M, Kraemer K. The dermatopharmacologic prole of ciclopi-
rox 8% nail lacquer. J Am Podiatr Med Assoc 2000; 90:4914.
24 Pierard GE. Seborrheic dermatitis today, gone tomorrow? The link
between the biocene and treatment. Dermatology 2003; 206:1878.
25 Miller DM, Buettner GR, Aust SD. Transition metals as catalysts of
autoxidation reactions. Free Radic Biol Med 1990; 8:95108.
26 Slater TF. Free-radical mechanisms in tissue injury. Biochem J 1984;
222:115.
27 Fridovich I. Biological effects of the superoxide radical. Arch Biochem
Biophys 1986; 247:111.
28 Cochrane CG. Cellular injury by oxidants. Am J Med 1991; 91
(Suppl. 3C):2330.
29 Weiss SJ. Tissue destruction by neutrophils. N Engl J Med 1989;
320:36576.
30 Hosaka S, Itagaki T, Kuramitsu Y. Selectivity and sensitivity in the
measurement of reactive oxygen species (ROS) using chemilumi-
nescent microspheres prepared by the binding of acridinium ester
or ABEI to polymer microspheres. Luminescence 1999; 14:34954.
31 Nakano M. Detection of active oxygen species in biological
systems. Cell Mol Neurobiol 1998; 18:56579.
32 Oosthuizen MM, Engelbrecht ME, Lambrechts H et al. The effect of
pH on chemiluminescence of different probes exposed to super-
oxide and singlet oxygen generators. J Biolumin Chemilumin 1997;
12:27784.
33 Cheung K, Lark J, Robinson MF et al. The production of hydroxyl
radical by human neutrophils stimulated by arachidonic acid
measurements by ESR spectroscopy. Aust J Exp Biol Med Sci 1986;
64:15764.
34 Green MR, Hill HA, Okolow-Zubkowska MJ, Segal AW. The pro-
duction of hydroxyl and superoxide radicals by stimulated human
neutrophils measurements by EPR spectroscopy. FEBS Lett 1979;
100:236.
35 Moseley R, Walker M, Waddington RJ, Chen WY. Comparison of
the antioxidant properties of wound dressing materials carboxy-
methylcellulose, hyaluronan benzyl ester and hyaluronan, towards
polymorphonuclear leukocyte-derived reactive oxygen species.
Biomaterials 2003; 24:154957.
36 Hegemann L, Webster GF, Wolff K. Selective calmodulin antago-
nists fail to inhibit phorbol ester-induced superoxide anion release
from human neutrophils: effects of antifungal azole derivatives.
Br J Dermatol 1996; 135:199203.
37 Azzi A, Montecucco C, Richter C. The use of acetylated ferricyto-
chrome c for the detection of superoxide radicals produced in bio-
logical membranes. Biochem Biophys Res Commun 1975; 65:597603.
38 Babior BM, Kipnes RS, Curnutte JT. Biological defense mechanisms.
The production by leukocytes of superoxide, a potential bacteri-
cidal agent. J Clin Invest 1973; 52:7414.
39 Hosaka S, Obuki M, Nakajima J, Suzuki M. Comparative study of
antioxidants as quenchers or scavengers of reactive oxygen species
based on quenching of MCLA-dependent chemiluminescence.
Luminescence 2005; 20:41927.
40 Apel K, Hirt H. Reactive oxygen species: metabolism, oxidative
stress, and signal transduction. Annu Rev Plant Biol 2004; 55:37399.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp720727
Inhibition of ROS by antifungal agents, T. Nakashima et al. 727
THERAPEUTI CS DOI 10. 1111/j . 1365- 2133. 2006. 07669. x
Pimecrolimus cream 1% for papulopustular rosacea:
a randomized vehicle-controlled double-blind trial
S. Weissenbacher, J. Merkl, B. Hildebrandt, A. Wollenberg,* M. Braeutigam, J. Ring and H. Hofmann
Department of Dermatology and Allergy Biederstein, Technical University of Munich, Biedersteinerstrasse 29, 80802 Munich, Germany
*Department of Dermatology and Allergy, Ludwig-Maximilian-University of Munich, Frauenlobstrasse 9-11, 80337 Munich, Germany
Novartis Pharma, Roonstrasse 25, 90429 Nuremberg, Germany
Correspondence
Heidelore Hofmann.
E-mail: h.hofmann@lrz.tum.de
Accepted for publication
27 August 2006
Key words
pimecrolimus, randomized controlled trial, rosacea
Conicts of interest
M.B. is employed by Novartis Pharma, the
manufacturer of Elidel
(pimecrolimus).
Summary
Background Rosacea remains difcult to treat, despite many therapeutic options.
Objectives To investigate the effect of pimecrolimus cream 1% (Elidel
; Novartis
Pharma, Nuremberg, Germany) in the treatment of papulopustular rosacea.
Methods Forty patients with rosacea (25 men and 15 women, mean age 58 years)
were enrolled in a randomized, vehicle-controlled, double-blind study. For 4
8 weeks, patients applied pimecrolimus cream or vehicle twice daily to the
involved areas on the face. Rosacea severity score, subjective severity assessment
and quality of life assessment were obtained, along with photographic documen-
tation.
Results Both treatment groups of 20 patients showed an improvement after
4 weeks. The differences were not signicant (P > 005) with regard to mean
absolute values, mean percentage changes from baseline, or mean absolute values
as differences from baseline for the total score or scores of the different clinical
signs (erythema, papulation, scaling and pustules). In the subjective severity
score and the quality of life assessment, there was also no signicant difference
between pimecrolimus and the vehicle (P > 005).
Conclusions Treatment of rosacea for 48 weeks with the topical calcineurin inhibi-
tor pimecrolimus cream 1% was not more efcacious than treatment with the
vehicle cream.
Rosacea is a chronic inammatory disease of the face with
remissions and relapses, occurring typically between the
ages of 30 and 50 years. It can be classied into four sub-
types: (i) an erythematotelangiectatic subtype with ushing,
telangiectatic vessels and persistent facial erythema; (ii) a
papulopustular subtype with inammatory papules and pus-
tules; (iii) a phymatous subtype due to hypertrophy of the
sebaceous glands of the nose; and (iv) an ocular subtype
presenting with blepharitis, conjunctivitis and keratitis. The
severity of each type can be graded as mild, moderate or
severe.
13
The cause of rosacea is unknown. Several factors
have been implicated in its pathogenesis. Sunlight, heat,
cosmetics, spicy foods, alcohol and hot beverages can trig-
ger ushing reactions in patients with rosacea, as well as
release of vasoactive mediators such as substance P. The
vasodilation leads to damage of dermal connective tissue
and to hyperthermia.
4
The higher facial skin temperature in
patients with rosacea can change microbial growth. Dahl
et al.
5
found that Staphylococcus epidermidis was b-haemolytic in
patients with rosacea whereas it was nonhaemolytic in con-
trol subjects. In addition, organisms such as Propionibacterium
acnes and Demodex folliculorum might play a pathogenic role. A
relation between a Helicobacter pylori infection and rosacea is
controversially discussed. The eradication of H. pylori by
antibiotics might lead to improvement or remission of rosa-
cea. On the other hand, metronidazole alone also improves
rosacea irrespective of H. pylori infection.
4,6
Despite an incomplete understanding of the pathogenesis of
rosacea, there are various therapeutic options depending on
the subtype.
7,8
Besides the avoidance of sun and trigger fac-
tors, possible approaches include topical medications such as
metronidazole,
9
azelaic acid
10
or tretinoin, or systemic medi-
cations such as tetracyclines,
11
azithromycin,
12
metronidazole
or isotretinoin.
13
Further options include laser and intense
pulsed-light treatment of facial telangiectasia.
7
There are few data on the efcacy of calcineurin inhibitors
in the treatment of rosacea. Tacrolimus was recently reported
to improve steroid-induced rosacea.
14
Pimecrolimus cream 1%
2006 The Authors
728 Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp728732
produced a rapid improvement of inammatory lesions in
patients with different forms of rosacea.
1518
Pimecrolimus (SDZ ASM 981), an ascomycin derivative, is
an anti-inammatory and immunomodulatory macrolactam. It
blocks T-cell activation, inhibits the synthesis of inammatory
cytokines [interleukin (IL)-2, IL-3, IL-4, IL-5, IL-10, tumour
necrosis factor-a] and prevents the release of cytokines from
T cells and mast cells by inhibition of the phosphatase
calcineurin.
19,20
The aim of our study was to evaluate the
anti-inammatory effect of pimecrolimus cream 1% in the
treatment of rosacea.
Materials and methods
Forty patients (25 men and 15 women; age range 3676
years, mean 58) with papulopustular rosacea were investi-
gated in a single-centre, randomized, double-blind, vehicle-
controlled study. Before enrolment in the study, all patients
gave their informed consent. The study was approved by the
Ethics Committee of the Medical Faculty of the Technical Uni-
versity of Munich.
On day 0 the rosacea severity score for each sign ery-
thema, papules, scaling, pustules and the total score were
graded as none (0), mild (0510), moderate (1520) or
severe (2530) for each patient.
21
Only patients with a
total severity score of 60 as well as a score of 2 for
erythema and a score of 1 for scaling were included.
Moreover, a subjective severity assessment was performed
using a visual analogue scale (0 mm no skin changes;
100 mm very severe skin changes) and a quality of life
assessment was performed as well as photographic docu-
mentation. In the quality of life assessment according to
Finlay and Khan
22
the patients were asked whether the skin
changes were burning or itching, and whether they were
affected in their activities concerning sports, occupation and
free time or in their choice of clothes. The patients had
to apply the study medication pimecrolimus cream 1%
(Elidel
; Novartis Pharma, Nuremberg, Germany) or vehicle
cream to the face twice daily (duration of treatment
28 4 days), followed by an open phase of the study
(application of pimecrolimus 1% cream twice daily for a
further 4 weeks). Visits were scheduled at baseline, day 7,
day 14, day 28 and after 8 weeks. Rosacea severity score,
subjective severity assessment and photographic documenta-
tion were performed throughout the study. The quality of
life assessment was made on day 0 and day 28. A tube
weighing was performed on day 7, day 14 and day 28.
Statistical analysis
Rosacea severity scores as percentage of baseline, absolute val-
ues and absolute values as difference from baseline, subjective
severity assessment and quality of life assessment were ana-
lysed using the WilcoxonMannWhitney test. Differences are
presented together with 95% condence intervals and associ-
ated P-values. A 5% signicance level was used throughout.
Results
Forty patients were screened; all were treated and all comple-
ted the study. Thirty-seven of 40 patients treated with pi-
mecrolimus or vehicle showed a reduction of the total
rosacea severity score, although this was only minimal in
some. Two of 40 patients showed worsening and one patient
was unchanged after 8 weeks. The differences between the
treatment groups, each consisting of 20 patients, were not sig-
nicant in any statistical analysis.
Regarding the mean absolute values for the total score,
there was a reduction from 688 (day 0) to 468 (day 28) for
the pimecrolimus group and from 700 (day 0) to 433 (day
28) for the vehicle group; the difference was not signicant
(P 059). Comparing the mean percentage change from
baseline for both groups, the results showed an improvement
of 32% on day 28 in the pimecrolimus group and an
improvement of 37% on day 28 in the control group (P
039) (Fig. 1). The mean absolute values expressed as
difference from baseline showed changes of 220 and 268 in
the pimecrolimus and vehicle group after 4 weeks (P 050),
respectively. Regarding the scores of the different clinical
signs erythema, papules, scale and pustules, there were no
signicant differences between both groups (P > 005).
In the subjective severity score, patients indicated an
improvement of the mean absolute value from 5345 to 4895
(pimecrolimus) and from 6475 to 4335 (vehicle) (P
048) (Fig. 2). The quality of life impairment showed a
reduction of the mean absolute value from 550 to 310 and
from 670 to 370 after 4 weeks of treatment with pimecro-
limus and vehicle, respectively (P 075) (Fig. 3).
Thirty-one of 40 patients were treated in an open phase
with pimecrolimus cream 1% for a further 4 weeks. Seven of
40 patients refused a further therapy with pimecrolimus cream
1% and two of 40 patients received doxycycline due to the
severity of their disease and ocular involvement. Seventeen of
31 patients showed a further improvement in the total severity
score during the open treatment phase at week 8 either after
Fig 1. Percentage change from baseline for the total rosacea score in
the groups treated with pimecrolimus (Elidel
; n 20) and vehicle
(n 20) (day 0day 28). Results are shown as mean 95%
condence interval.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp728732
Pimecrolimus for papulopustular rosacea, S. Weissenbacher et al. 729
continuing the pimecrolimus cream 1% therapy or after chan-
ging from vehicle cream to pimecrolimus cream 1% (Fig. 4).
The mean absolute value of the total score at week 8 as com-
pared with week 4 showed an improvement of 14. Some
patients showed a deterioration of the total severity score after
the open phase. In four of 31 patients, the rosacea worsened
after switching from vehicle to pimecrolimus cream 1%
(Fig. 5).
Safety
One patient complained of tightness of facial skin and another
of pruritus. No serious adverse events were seen. The study
procedures were well tolerated.
Discussion
In our study, a 48-week treatment of rosacea with the topical
calcineurin inhibitor pimecrolimus was not more efcacious
than treatment with the vehicle cream. Rosacea improved in
approximately one-third of the patients (32% in the pimecro-
limus group and 37% in the vehicle group). This was surpri-
sing as we had previously observed good results in individual
cases of erythematotelangiectatic rosacea, especially in steroid-
induced rosacea. In addition, other authors have repeatedly
reported positive results with pimecrolimus cream 1% in the
treatment of various forms of rosacea.
1518
Wollenberg et al.
23
had shown in a similar study that pimecrolimus was effective
in perioral dermatitis, which is similar to rosacea in many
aspects. In order to reach the requirement of a score of 60
we only included patients with the papulopustular form of
rosacea. This preselection may be one reason for the lack of
efcacy of pimecrolimus in our study.
Various immune factors such as eicosanoids, proinammatory
cytokines and mediators such as neuroendocrine transmitters
or enzymes may be involved in the erythematotelangiectatic
subtype of rosacea.
4,24,25
Pimecrolimus, an anti-inammatory
and immunomodulatory pharmacological agent, inhibits
the synthesis of proinammatory cytokines produced by
Th1 and Th2 cells.
20
The erythematotelangiectatic type might
respond better to pimecrolimus than the papulopustular
Fig 3. Quality of life impairment (Dermatology Life Quality Index
22
)
in the groups treated with pimecrolimus (Elidel
; n 20) and vehicle
(n 20) (day 0day 28). Results are shown as mean 95%
condence interval.
(a) (b)
Fig 4. Improvement of rosacea in a patient
after 8 weeks of therapy with pimecrolimus:
(a) week 0; (b) week 8.
Fig 2. Subjective severity score in the groups treated with
pimecrolimus (Elidel
; n 20) and vehicle (n 20) (day 0day 28).
Results are shown as mean 95% condence interval.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp728732
730 Pimecrolimus for papulopustular rosacea, S. Weissenbacher et al.
type. Bamford et al.
26
treated erythematotelangiectatic and
papulopustular rosacea with tacrolimus and showed that
erythema was signicantly improved in both subtypes,
whereas the number of papulopustular lesions did not
decrease.
We treated patients with pimecrolimus cream 1% for only
48 weeks, which may have been too short a period. The
duration of therapy in other studies with the calcineurin
inhibitors pimecrolimus or tacrolimus was at least
12 weeks.
26,27
In the study of Crawford et al.
17
who showed,
in contrast to our study, an improvement of both rosacea sub-
types, patients were treated for 1218 weeks.
Moreover, the measurement of the severity of rosacea is dif-
cult. There are no standardized measures. Bamford et al.
27
showed that the assessment of the severity of rosacea differs
among investigators and between physicians and patients.
Because the symptoms of rosacea vary rapidly depending on
exacerbating factors such as heat, cold, stress or sunlight,
1
the
severity score gives only a momentary measurement which
means that an improvement of symptoms may be difcult to
document.
On the other hand, there was an improvement of rosacea in
some patients who were treated only with vehicle. While
vehicles are lack active pharmacological substances, they are
not technically placebos.
28,29
They have their own effects such
as improvement of the epidermal barrier function and reduc-
tion of roughness and scaling. One of our patients who
improved after treatment with vehicle had a steroid-induced
rosacea. It is known that a gradual discontinuation of topical
steroids leads to an improvement of skin disease. Specic ther-
apy is often not necessary.
In conclusion, the therapeutic efcacy of pimecrolimus
cream 1% in our study did not differ signicantly from that
of the vehicle cream, in contrast to single cases observed by
ourselves and the previously published, promising results
described by other authors. More studies are needed to dene
the exact place of pimecrolimus cream 1% in the treatment of
the different subtypes of rosacea.
Acknowledgments
We thank Ulrich Stefenelli, Department of Statistics, University
of Wurzburg, for the statistical analyses.
References
1 Powell FC. Rosacea. N Engl J Med 2005; 352:793803.
2 Wilkin J, Dahl M, Detmar M et al. Standard classication of rosacea:
report of the National Rosacea Society Expert Committee on the
Classication and Staging of Rosacea. J Am Acad Dermatol 2002;
46:5847.
3 Plewig G, Kligman AM. Acne and Rosacea, 3rd edn. Berlin: Springer-
Verlag, 2000.
4 Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogene-
sis, and subtype classication. J Am Acad Dermatol 2004; 51:32741.
5 Dahl MV, Ross AJ, Schlievert PM. Temperature regulates bacterial
protein production: possible role in rosacea. J Am Acad Dermatol
2004; 50:26672.
6 Grilli R, Fernandez M. Helicobacter pylori: related to rosacea? J Am Acad
Dermatol 2000; 42:5367.
7 Pelle MT, Crawford GH, James WD. Rosacea: II. Therapy. J Am Acad
Dermatol 2004; 51:499512.
8 Heymann WR. Rosacea subtype-directed therapy. J Am Acad Dermatol
2004; 51:902.
9 Dahl MV, Jarrat M, Kaplan D et al. Once-daily topical metronidazole
cream formulations in the treatment of the papules and pustules of
rosacea. J Am Acad Dermatol 2001; 45:72330.
10 Thiboutot D, Thieroff-Ekerdt R, Graupe K. Efcacy and safety of
azelaic acid (15%) gel as a new treatment for papulopustular rosa-
cea: results from two vehicle-controlled, randomized phase III
studies. J Am Acad Dermatol 2003; 48:83645.
(a) (b)
Fig 5. Worsening of rosacea in a patient after
8 weeks of therapy with pimecrolimus:
(a) week 0; (b) week 8.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp728732
Pimecrolimus for papulopustular rosacea, S. Weissenbacher et al. 731
11 Torresani C, Pavesi A, Manara GC. Clarithromycin vs. doxycycline
in the treatment of rosacea. Int J Dermatol 1997; 36:9426.
12 Bakar O
, Demircay Z, Oya G. Therapeutic potential of azithromycin
in rosacea. Int J Dermatol 2004; 43:1514.
13 Hofer T. Continuous microdose isotretinoin in adult recalcitrant
rosacea. Clin Exp Dermatol 2004; 29:196205.
14 Goldmann D. Tacrolimus ointment for the treatment of steroid-
induced rosacea: a preliminary report. J Am Acad Dermatol 2001;
44:9958.
15 Chu CY. The use of 1% pimecrolimus cream for the treatment of
steroid-induced rosacea. Br J Dermatol 2005; 152:3969.
16 Cunha PR, Rossi AB. Pimecrolimus cream 1% is effective in a case
of granulomatous rosacea. Acta Derm Venereol (Stockh) 2006; 86:712.
17 Crawford KM, Russ B, Bostrom P. Pimecrolimus for treatment of
acne rosacea. Skinmed 2005; 4:14750.
18 Kim BS, Chang SH, Cho MK. Safety and efcacy of pimecrolimus
cream in adults with erythematotelangiectatic rosacea. J Eur Acad
Dermatol Venereol 2005; 19 (Suppl. 2): 76 (abstr.).
19 Gupta AK, Chow M. Pimecrolimus: a review. J Eur Acad Dermatol
Venereol 2003; 17:493503.
20 Grassberger M, Steinhoff M, Schneider D, Luger TA. Pimecrolimus
an anti-inammatory drug targeting the skin. Exp Dermatol 2004;
13:72130.
21 Wollenberg A, Oppel T. Scoring of skin lesions with the Perioral
Dermatitis Severity Index (PODSI). Acta Derm Venereol (Stockh) 2006;
86:2512.
22 Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) a
simple practical measure for routine clinical use. Clin Exp Dermatol
1994; 19:21016.
23 Wollenberg A, Pavicic T, Wetzel S et al. Pimecrolimus cream 1%
is effective in rosacea-like perioral dermatitis results of a ran-
domized, double blinded, vehicle controlled clinical trial involving
40 patients. J Eur Acad Dermatol Venereol 2005; 19 (Suppl. 2): 8
(abstr.).
24 Bamford JT. Rosacea: current thoughts on origin. Semin Cutan Med
Surg 2001; 20:199206.
25 Millikan LE. Rosacea as an inammatory disorder: a unifying
theory? Cutis 2004; 73:58.
26 Bamford JT, Elliott BA, Haller IV. Tacrolimus effect on rosacea.
J Am Acad Dermatol 2004; 50:1078.
27 Bamford JT, Gessert CE, Renier CM. Measurement of the severity
of rosacea. J Am Acad Dermatol 2004; 51:697703.
28 Pugshaupt C. Eigenwirkung von Vehikeln Systematik und
Gedanken zur Vehikelwahl. Deutsche Dermatologe 1992; 40:114455.
29 Fluhr JW, Rigano L. Clinical effects of cosmetic vehicles on skin.
J Cosmet Sci 2004; 55:189205.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp728732
732 Pimecrolimus for papulopustular rosacea, S. Weissenbacher et al.
CONCI SE COMMUNI CATI ON DOI 10. 1111/j . 1365- 2133. 2007. 07783. x
Ear, nose and throat manifestations in pemphigus vulgaris
A. Espana, S. Fernandez,* J. del Olmo, M. Marquina, M. Pretel, D. Ruba* and A. Sanchez-Ibarrola
Departments of Dermatology, *Otorhinolaryngology and Immunology, University Clinic of Navarra, School of Medicine, University of Navarra, 31080 Pamplona,
Navarra, Spain
Correspondence
Agust n Espana.
E-mail: aespana@unav.es
Accepted for publication
27 November 2006
Key words
ear nose and throat manifestations, mucosal
manifestations, pemphigus vulgaris
Conicts of interest
None declared.
Summary
Background Pemphigus vulgaris (PV) is an autoimmune disease characterized by
mucocutaneous intraepithelial blisters and pathogenic autoantibodies against
desmoglein 3. There are two clinical forms: mucosal (MPV) and mucocutaneous
(MCPV). The frequency of ear, nose and throat (ENT) involvement in PV is not
clearly dened. Only a few isolated individual cases have been reported.
Objectives The objective of our study was to determine the incidence of ENT
involvement in patients with PV.
Patients We studied prospectively all 16 patients diagnosed with PV and treated in
the Department of Dermatology of the University Clinic of Navarra between
2001 and 2005. They were 10 cases of MPV and six cases of MCPV. All patients
were evaluated for ENT manifestations by endoscopic examination.
Results Of the 16 patients, 13 presented with throat symptoms (81%), 12 pharyn-
geal (75%) and seven laryngeal symptoms (44%). Fourteen patients (88%) had
active PV lesions on endoscopic evaluation (eight patients had active lesions on
both pharyngeal and laryngeal mucosa, four had PV lesions only on laryngeal
mucosa and two had PV lesions on pharyngeal mucosa). Laryngeal lesions were
most commonly present in MPV patients. The frequency of nasal symptoms
(38%) was lower than active PV lesions (62%) found on ENT examination. Oral
symptoms and oral active PV lesions were the most frequent ndings (94%).
Only three patients with MCPV showed erosions on the external auditory canal.
Conclusions As ENT endoscopy allows more extensive areas of mucosa to be exam-
ined than simple visual inspection, we recommend that it be included in the
examination of all patients with PV. By obtaining more complete information
concerning the extent of the disease, a more accurate diagnosis can be made,
better choice of drug and dose may be decided and, ultimately, response to
treatment may be improved.
Pemphigus vulgaris (PV) is an autoimmune bullous disease,
characterized by the development of acantholysis on the skin
and/or mucosa secondary to IgG antibody synthesis against a
desmosomal glycoprotein, desmoglein (Dsg), present in kera-
tinocytes.
1
Two clinical subtypes of PV have been dened. The
mucosal form of PV (MPV) is characterized by a predominant
anti-Dsg3 autoimmune response. In contrast, the mucocutane-
ous form (MCPV) shows a combined anti-Dsg3 and anti-Dsg1
autoantibody response, the patients mucosa is affected and
over ve skin lesions are present.
2
The frequency of ear, nose
and throat (ENT) involvement in PV is not known. Only a
few isolated individual cases have been reported,
317
most
published in ENT journals. Recently, Hale and Bystryn
18
des-
cribed laryngeal and nasal ndings in 53 patients with PV,
although only 11 underwent ENT examination. In the present
report, ENT manifestations in 16 patients with PV, examined
by ENT endoscopy, are presented.
Patients and methods
This prospective study includes 16 sequential patients with
PV, 10 cases of MPV and six of MCPV. All attended the
Department of Dermatology of the University Clinic of Nava-
rra between 2001 and 2005. Criteria used for diagnosis of PV
are described elsewhere.
2
Briey, patients with MPV showed
predominant oral erosions with limited skin involvement,
fewer than ve or six scattered or isolated erosions or blisters,
and each <5 cm in diameter. Patients with MCPV showed
extensive skin involvement in addition to oral involvement. If
more than six erosions or blisters >5 cm in diameter were
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp733737 733
T
a
b
l
e
1
C
l
i
n
i
c
a
l
a
n
d
e
a
r
,
n
o
s
e
a
n
d
t
h
r
o
a
t
(
E
N
T
)
m
a
n
i
f
e
s
t
a
t
i
o
n
s
i
n
1
6
p
a
t
i
e
n
t
s
w
i
t
h
p
e
m
p
h
i
g
u
s
v
u
l
g
a
r
i
s
(
P
V
)
P
a
t
i
e
n
t
n
u
m
b
e
r
T
y
p
e
o
f
P
V
T
i
m
e
f
r
o
m
t
h
e
b
e
g
i
n
n
i
n
g
o
f
P
V
(
m
o
n
t
h
s
)
T
h
r
o
a
t
s
y
m
p
t
o
m
s
p
h
a
r
y
n
x
/
l
a
r
y
n
x
P
h
a
r
y
n
g
e
a
l
e
n
d
o
s
c
o
p
y
n
d
i
n
g
s
L
a
r
y
n
g
e
a
l
e
n
d
o
s
c
o
p
y
n
d
i
n
g
s
N
a
s
a
l
s
y
m
p
t
o
m
s
N
a
s
a
l
e
n
d
o
s
c
o
p
y
n
d
i
n
g
s
O
r
a
l
s
y
m
p
t
o
m
s
O
r
a
l
e
n
d
o
s
c
o
p
y
n
d
i
n
g
s
E
a
r
s
y
m
p
t
o
m
s
E
a
r
c
l
i
n
i
c
a
l
n
d
i
n
g
s
I
C
S
E
L
I
S
A
D
s
g
1
/
D
s
g
3
B
a
c
t
e
r
i
a
l
-
p
o
s
i
t
i
v
e
c
u
l
t
u
r
e
o
f
m
u
c
o
s
a
C
a
n
d
i
d
a
-
p
o
s
i
t
i
v
e
c
u
l
t
u
r
e
o
f
m
u
c
o
s
a
1
M
P
V
1
+
/
+
+
+
)
)
+
+
)
)
1
:
8
0
)
/
4
8
)
+
2
M
P
V
3
0
+
/
+
+
+
+
+
+
+
)
)
1
:
6
4
0
)
/
2
4
4
+
+
3
M
P
V
2
+
/
)
+
+
)
)
+
+
)
)
1
:
8
0
5
3
/
1
6
3
+
+
4
M
P
V
6
+
/
+
+
+
)
+
+
+
)
)
1
:
2
0
)
/
4
2
)
)
5
M
P
V
7
+
/
+
+
+
)
+
+
+
)
)
1
:
1
0
)
/
2
6
)
)
6
M
P
V
3
6
+
/
+
)
+
+
+
+
+
)
)
N
e
g
1
9
1
/
2
0
0
)
)
7
M
P
V
2
4
+
/
)
+
+
)
+
+
+
)
)
1
:
3
2
0
)
/
1
7
5
+
+
8
M
P
V
9
+
/
)
)
+
)
+
+
+
)
)
N
e
g
)
/
1
4
2
+
)
9
M
P
V
3
5
)
/
+
)
+
)
)
+
+
)
)
1
:
8
0
)
/
1
0
4
)
)
1
0
M
P
V
4
)
/
)
)
+
)
)
+
+
)
)
N
e
g
4
1
/
1
7
3
)
)
1
1
M
C
P
V
1
0
+
/
)
+
+
)
)
+
+
)
)
1
:
6
4
0
1
8
2
/
2
5
3
)
)
1
2
M
C
P
V
1
1
+
/
+
+
+
+
+
+
+
+
+
1
:
2
0
5
5
/
2
1
5
)
)
1
3
M
C
P
V
6
0
+
/
)
+
)
+
+
+
+
+
+
1
:
8
0
9
9
/
1
6
0
+
)
1
4
M
C
P
V
1
0
+
/
)
+
)
+
+
+
+
)
)
1
:
6
4
0
1
8
5
/
1
8
4
)
)
1
5
M
C
P
V
3
6
)
/
)
)
)
+
+
+
+
+
+
1
:
6
4
0
2
2
2
/
2
5
9
+
+
1
6
M
C
P
V
3
)
/
)
)
)
)
)
)
)
)
)
1
:
2
0
1
8
8
/
9
0
)
)
T
o
t
a
l
1
6
1
2
/
7
1
0
1
2
6
1
0
1
5
1
5
3
3
6
5
M
P
V
,
M
u
c
o
s
a
l
p
e
m
p
h
i
g
u
s
v
u
l
g
a
r
i
s
;
M
C
P
V
,
m
u
c
o
c
u
t
a
n
e
o
u
s
p
e
m
p
h
i
g
u
s
v
u
l
g
a
r
i
s
;
I
C
S
,
i
n
t
e
r
c
e
l
l
u
l
a
r
s
u
b
s
t
a
n
c
e
a
n
t
i
b
o
d
i
e
s
;
N
e
g
,
n
e
g
a
t
i
v
e
;
D
s
g
,
d
e
s
m
o
g
l
e
i
n
.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp733737
734 ENT manifestations in PV, A. Espana et al.
present on the skin, the patient was considered to have the
mucocutaneous type of PV.
2
If patients meeting the mucosal-
type criteria had positive anti-Dsg1 and anti-Dsg3 antibodies,
these cases were considered to have mucosal-dominant PV, as
has been established by other authors.
19
Initial symptoms and
clinical lesions in our patients had been observed for between
1 and 60 months before the patient came to our department
for the rst medical visit (Table 1). In all patients the
treatment consisted of high doses of corticosteroids
(0.31 mg kg
)1
daily), together with immunosuppressive
drugs (azathioprine 115 mg kg
)1
daily or mycophenolate
mofetil 3 g daily). Only patient 1 had not been treated before
coming to our department. The dose of corticosteroids and
immunosuppressive treatment was adjusted at each follow-up
visit based on the cutaneous and mucosal manifestations
of PV, and the mucosal involvement observed by ENT
endoscopy.
All patients were evaluated for ENT manifestations by endo-
scopic examination at the rst medical visit to our hospital,
whether or not they had symptoms. All ENT examinations
were carried out by one of the authors (S.F.). After the rst
ENT examination, each patient was evaluated by endoscopic
examination at subsequent follow-up visits only when ENT
symptoms were persistent or active PV lesions had been
observed in the previous ENT examination. ENT examination
was also carried out when a patient had a new are of PV
lesions. As a result, the number of ENT examinations was dif-
ferent for each patient. Mucosal cultures were taken in those
patients in whom a bacterial, viral or fungal mucosal infection
was suspected. If patients had previously been evaluated in
other hospitals, and had already presented with ENT symp-
toms or clinical lesions related to PV, or had undergone previ-
ous ENT endoscopy, that information was always included in
their medical records. Table 1 includes complete clinical and
serological information for each patient. Table 2 shows the
complete symptomatology presented by our 16 patients from
the beginning of their mucosal and skin manifestations.
Results
Oral symptoms and active oral PV lesions were the most fre-
quent ndings in our study. The oral symptoms reported were
pain or stinging in the oral cavity (94% of all the patients
with PV) (Table 2). To date, only one patient with MCPV has
not had active oral mucosal lesions at some time during the
course of the disease (Table 1). Oral symptoms appeared at
the beginning of the clinical manifestations of PV.
Of the 16 patients with PV, 13 presented with throat symp-
toms (81%) (either pharyngeal or laryngeal symptoms, or
both), but 14 (88%) had active PV lesions as determined by
endoscopic evaluation (Table 1). Symptoms affecting the phar-
yngeal mucosa most often manifested as tenderness in the
throat or pain on swallowing; these symptoms occurred in 12
patients (75% of all the patients with PV, both symptoms)
(Table 2). Symptoms related to the laryngeal mucosa were
reported by seven patients (44%), including hoarseness
and/or dysphonia (31% and 44%, respectively) (Table 2).
These symptoms appeared when PV rst occurred, and when
some patients experienced a are of their symptoms including
new blisters and erosions on skin and/or mucosa. Overall, 12
patients presented with active lesions on the laryngeal mucosa
(75% of the patients with PV) and 10 patients presented with
active lesions on the pharyngeal mucosa (62% of PV patients);
eight patients had active PV lesions on both pharyngeal and
laryngeal mucosa, four had PV lesions only on the laryngeal
mucosa, and two patients had erosions only on the pharyngeal
mucosa (Table 1). Surprisingly, while all patients with MPV
presented with laryngeal lesions (100% of patients with
MPV), this was the case with only two of the patients with
MCPV (33% of patients with MCPV) (Table 1). However, the
frequency of active erosions on pharyngeal mucosa was sim-
ilar in patients with either MCPV or MPV (60% and 67%,
respectively) (Table 1).
Of all the 16 patients with PV, only six had nasal symptoms
(38%). However, 10 cases (62%) presented with active
mucosal PV lesions, such as crusting and erosions, on ENT
examination (Table 1). Six of these 10 cases had MPV (60%
of the patients with MPV) and four had MCPV (67% of
patients with MCPV). Nasal symptoms appeared at the begin-
ning of the mucocutaneous disease, or with ares of PV. The
symptoms reported were epistaxis (38%), presence of a
blood-tinged mucus (19%) or stufness (25%) (Table 2).
Ear symptoms were the least frequent symptom and clinical
nding in the 16 patients with PV. All three patients with ear
symptoms presented with pain and ear canal obstruction
(Table 2). Ear symptoms appeared when the patients had a
are of PV lesions. These symptoms followed an evolution
similar to that of skin lesions after administration of cortico-
steroids and immunosuppressive drugs. These three patients
Table 2 Frequency of ear, nose and throat symptoms in 16 patients
with pemphigus vulgaris
Symptoms
Frequency of symptoms
Number of patients %
Throat 13 81
Pharyngeal mucosa 12 75
Tenderness 12 75
Pain on swallowing 12 75
Laryngeal mucosa 7 44
Hoarseness 5 31
Dysphonia 7 44
Nasal mucosa 6 38
Epistaxis 6 38
Blood-tinged mucus 3 19
Stufness 4 25
Ear 3 19
Pain 3 19
Ear canal obstruction 3 19
Oral 15 94
Pain 15 94
Stinging 15 94
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp733737
ENT manifestations in PV, A. Espana et al. 735
had MCPV. No ear lesions were observed in patients with
MPV.
In some patients, active lesions were found on mucosae
other than those of the ear, nose or throat. These included
anal (patients 3 and 13), genital (patients 1, 3, 5 and 7) and
conjunctival mucosae (patients 5, 7 and 13).
Some patients were asymptomatic for pharyngeal, laryngeal
or nasal symptoms despite active lesions demonstrated by
endoscopy (e.g. patients 4, 5, 7, 8 and 10). Those patients
with more extensive mucosal active PV lesions received higher
doses of corticosteroids and were treated for longer than those
patients with fewer mucosal PV manifestations.
In several patients ENT symptoms could have been due to
mucosal inammation, as six cases had cultures positive for
Staphylococcus aureus on nasal mucosa, and ve patients had cul-
tures positive for Candida spp. (Table 1). These patients were
treated with antibiotics and anticandidal therapy, along with
corticosteroids and immunosuppressive drugs.
Discussion
This study reveals that a high number of patients with PV may
present with active ENT lesions. Therefore, all dermatologists
should be aware of which ENT manifestations might be pre-
sent in patients with PV at some time during the course of
this disease. Most of the data related to ENT manifestations in
PV have been in reports of individual cases.
317
However,
Hale and Bystryn
18
described laryngeal and/or nasal ndings
in 53 patients with PV, although only 11 underwent ENT
examination. Our study underlines the importance of explor-
ing ENT mucosa by endoscopic techniques in all patients with
PV, in order to determine the real extent of active PV lesions.
Overall, all of our patients except one (patient 16) had some
active erosions on ENT mucosa together with one or more
symptoms. However, individual symptoms were missing in
some patients where erosions were found (Table 1). Also, our
ndings show that ENT manifestations in patients with PV are
not in fact associated with a more aggressive form of PV.
Indeed, most of our patients presented a mucosal form with
active lesions apparently localized only on the oral mucosa
(Table 1).
Although many patients may experience ENT symptoms
during their disease, our study shows that the presence of act-
ive lesions on mucosal surfaces may be more extensive than
was originally thought. This difference between symptoms
and clinical ndings by ENT examinations was most striking
in the nasal cavity. Nasal symptoms were reported in 38% of
patients (mainly epistaxis and stufness) (Table 2), but ero-
sions and crusting on nasal mucosa were detected in 62% of
cases. Patients with MPV usually reported no discomfort in the
nasal fossa, but ENT examination frequently revealed erosions
and crusting (Table 1). In contrast, all the patients with MCPV
with nasal symptoms also presented active PV lesions on the
nasal mucosa by ENT examination (Table 1). Hale and Bystryn
reported nasal symptoms in 23% of their patients, but ENT
evaluation was recommended only in four, and active nasal
PV lesions were found in only three.
18
These authors noted,
as was also the case in our study, that these symptoms were
usually related to a are of PV. Of the six patients with cul-
tures positive for S. aureus on nasal mucosa in our study, only
three had some discomfort in the nasal fossa. Perhaps the role
of these bacteria in the presentation of nasal symptoms was
minor in our patients.
The most surprising ndings in this study were related to
laryngeal manifestations. Only 44% of patients presented with
symptoms associated with the larynx, mainly hoarseness and
dysphonia (Table 2). However, 75% had active PV lesions on
the laryngeal mucosa on ENT examination. Even more inter-
esting is the fact that these lesions were found mostly in
patients with MPV. Only two patients with MCPV had lesions
on this mucosa (Table 1). Hale and Bystryn
18
found laryngeal
symptoms in 40% of patients with PV. Only seven of these
patients had an ENT evaluation, and active laryngeal lesions
were found in four of them. The difference between laryngeal
symptoms and the ndings of active PV lesions may be related
to the area of larynx affected. Only erosions on the vocal folds
produced dysphonia or hoarseness, while active lesions on the
epiglottis produced tenderness in the throat or pain on swal-
lowing. We do not know the reason for the high frequency of
active laryngeal lesions almost exclusively in patients with
MPV. In general, this kind of PV symptom is associated with a
are of PV lesions. On the other hand, Candida spp. infection
on the laryngeal mucosa could contribute to hoarseness in our
patients, as has been established by other authors.
7
Both
symptoms and infection of Candida spp. were more prevalent
in patients with MPV. As yet, we can offer no reason for these
ndings.
There are some data in the dermatological literature related
to ear involvement in PV.
13
Our study found only three
patients showing erosions in the auricle and auditory canal of
the ear. All three patients presented with MCPV. These nd-
ings may reect one more characteristic clinical manifestation
of MCPV.
Our ndings show that the management of PV must be an
interdisciplinary process. ENT manifestations should be exam-
ined by an ENT specialist with experience of PV patients, and
endoscopic techniques should be used. Other diagnoses to be
considered when using direct broendoscopy are Wegeners
granulomatosis, blistering mucosal disease, such as cicatricial
pemphigoid, or nonspecic membranous mucositis. Further-
more, ENT endoscopy may be useful for obtaining additional
information related to the viral, bacterial or fungal agents
causing the infection on the inamed mucosa in patients
with PV.
In summary, ENT endoscopy allows more extensive areas of
mucosa to be examined than simple visual inspection. Conse-
quently, we recommend that it be included in the examina-
tion of all patients with PV. By obtaining more complete
information concerning the extent of the disease, a more accu-
rate diagnosis can be made, a better choice of drug and dose
may be decided and, ultimately, response to treatment may be
improved.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp733737
736 ENT manifestations in PV, A. Espana et al.
References
1 Stanley JR. Pemphigus and pemphigoid as paradigms of organ-
specic, autoantibody-mediated diseases. J Clin Invest 1989; 83:
14438.
2 Amagai M, Tsunoda K, Zillikens D et al. The clinical phenotype of
pemphigus is dened by the anti-desmoglein autoantibody prole.
J Am Acad Dermatol 1999; 40:16770.
3 Zalesska-Krecicka M, Kolodziej TJ, Kreicicki T et al. Changes of
laryngeal mucosa in the course of pemphigus vulgaris. Otolaryngol
Pol 2005; 59:5335.
4 Frangogiannis NG, Gangopadhyay S, Cate T. Pemphigus of the lar-
ynx and esophagus. Ann Intern Med 1995; 122:8034.
5 Gibb AG. Mucous membrane pemphigus. J Laryngol Otol 1958;
72:799806.
6 Jijakli-Somville J. Pemphigus vegetans of the buccal, pharyngeal and
laryngeal mucosa. Arch Belg Dermatol Syphiligr 1962; 18:4950.
7 Samy LL, Girgis IH, Wasef SA. Pharyngeal and laryngeal pemphi-
gus. J Laryngol Otol 1968; 82:11121.
8 Wallaner LJ, Alexander RW. Pemphigus of the larynx. Laryngoscope
1964; 74:57586.
9 Wallaner LJ, Alexander RW. Pemphigus of the larynx. Trans Am
Laryngol Rhinol Otol Soc 1964; 44:195206.
10 Weinstein S, Sachs AR. Pemphigus of the oropharynx and larynx;
report of a case. AMA Arch Otolaryngol 1955; 62:21417.
11 Obregon G. Pemphigus of larynx. Ann Otol Rhinol Laryngol 1957;
66:64955.
12 Boussagol C, Hadida A, Marchand J. Problems of bullous lesions in
ENT. Based upon two cases. Ann Otolaryngol Chir Cervicofac 1980;
97:3859.
13 Bucur A. Pemphigus of the external ear. Rev Chir Oncol Radiol O R L
Oftalmol Stomatol Otorinolaringol 1987; 32:1379.
14 Grant WJ. Mucous membrane pemphigus. J Laryngol Otol 1965;
79:4947.
15 Stangeland N. Pemphigus of the mucosa. Tidsskr Nor Laegeforen 1972;
92:18667.
16 Taylor J, Westfried M, Lyneld YL. Pemphigus vulgaris localized to
the nose. Cutis 1984; 34:3945.
17 Saunders MS, Gentile RD, Lobritz RW. Primary laryngeal and nasal
septal lesions in pemphigus vulgaris. J Am Osteopath Assoc 1992;
92:9337.
18 Hale EK, Bystryn JC. Laryngeal and nasal involvement in pemphi-
gus vulgaris. J Am Acad Dermatol 2001; 44:60911.
19 Zagorodniuk I, Weltfriend S, Shtruminger L et al. A comparison of
anti-desmoglein antibodies and indirect immunouorescence in the
serodiagnosis of pemphigus vulgaris. Int J Dermatol 2005; 44:5414.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp733737
ENT manifestations in PV, A. Espana et al. 737
CASE REPORT DOI 10. 1111/j . 1365- 2133. 2006. 07650. x
Pulmonary carcinoid associated with melanoma: two cases
and a review of the literature
R. Rajaratnam, J.R. Marsden, J. Marzouk* and I. Hero
Skin Oncology Service, University Hospital Birmingham NHS Foundation Trust, Selly Oak Hospital, Birmingham B29 6JD, U.K.
*Department of Thoracic Surgery, Birmingham Heartlands and Solihull NHS Trust, Bordesley Green, Birmingham, U.K.
Department of Pathology, University Hospital Birmingham NHS Foundation Trust, Edgbaston, Birmingham, U.K.
Correspondence
R. Rajaratnam.
E-mail: ratnarajaratnam@doctors.org.uk
Accepted for publication
25 August 2006
Key words
amine precursor uptake and decarboxylation,
melanoma, neuroendocine pulmonary carcinoid
Conicts of interest
None declared.
Summary
To our knowledge, this is the rst report in the British literature documenting
the co-occurrence of melanoma and pulmonary carcinoid. The only other report
is from America and documents pulmonary carcinoid in association with a para-
thyroid hormone-producing melanoma. We report two patients with melanoma
who presented with nodules on chest X-ray. Both underwent resection of
assumed lung metastasis which unexpectedly revealed primary pulmonary carci-
noid. Evidence of an association between these two tumours which show striking
biological and pathological similarities is discussed. The incidence of pulmonary
carcinoid is increasing and with the improved power of radiological assessment
we may see additional accounts of such an association in the near future.
We report two patients with melanoma presenting with solit-
ary nodules on chest X-ray. A computed tomography (CT)
scan conrmed this and identied an additional nodule in one
patient. Both underwent resection of what was assumed to be
metastatic disease. Unexpectedly, in both cases the resected
specimen was primary pulmonary carcinoid. Evidence in sup-
port of a possible association between melanoma and carci-
noid, both of which fall under the amine precursor uptake
and decarboxylation (APUD) classication of Pearse, is
discussed.
1
Case reports
Patient 1
A 46-year-old woman presented in March 1998 with an irre-
gular pigmented lesion arising from a scar site on her lower
back. The scar was from a prior excision of a mole which was
reported as histologically benign. The new lesion was excised
and histological examination conrmed a supercial spreading
melanoma which was 10 mm thick, Clark level IV, T2a/
bN0M0 clinical stage 1B (Fig. 1a,b). In view of this, the le-
sion excised 4 years previously was reviewed. This was a junc-
tional naevus with cytological atypia. Clinical examination was
normal and a chest X-ray showed no evidence of metastatic
disease. The patient underwent a 2-cm further wide local exci-
sion, with excision margins being tumour free.
She remained well until August 2000 when a routine chest
X-ray detected an opacity in the left lung. A chest CT scan
conrmed this as a 3-cm lesion medially in the left lower lobe
associated with subsegmental collapse. A staging CT scan of
the head, abdomen and pelvis was normal. The patient pro-
ceeded to a left lower lobectomy. The tumour measured
27 mm in diameter. Microscopy showed a well-circumscribed
tumour composed of islands, trabeculae and acinar structures.
The cells had abundant eosinophilic cytoplasm and showed
moderate pleomorphism with prominent small nucleoli in
places. There were occasional mitoses seen. Immunohisto-
chemical studies showed that the tumour cells were not
expressing S100, Melan A or HMB-45. They were, however,
expressing the epithelial markers Ber EP4, epithelial-specic
antigen and Cam 5.2. The neuroendocrine markers neurone-
specic enolase, protein gene product (PGP) 9.5 and chromo-
granin were strongly positive, in keeping with a diagnosis of
carcinoid tumour (Fig. 2a,b). The resection margins of the
lobectomy were tumour free and the patient remains well to
date.
Patient 2
A 61-year-old man had a nodular melanoma excised from his
left chest wall in July 1997. The lesion was 8 mm thick and
was invading the reticular dermis, Clark level IV, T4a/bN0M0
clinical stage 2B (Fig. 3a,b). Clinical examination was normal
and a chest X-ray was clear. The patient underwent a 3-cm
wide local excision. He remained well until June 2005. A rou-
tine chest X-ray detected a rounded opacity at the left lung
base and a CT scan conrmed a 1-cm intrapulmonary nodule
2006 The Authors
738 Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp738741
at the lowermost extent of the left upper lobe. There was a
further nodule in the right lung at the margin of epicardial
fat. A staging CT scan of the abdomen, pelvis and head was
normal. The patient proceeded to have excision of both his
lung lesions.
Macroscopically, the lesion in the left lung was a nodule
measuring 5 mm. On microscopy, there were nests of clear
cells with regular nuclei. These cells strongly expressed CD56,
chromogranin, synaptophysin and PGP 9.5 (Fig. 4). They
were negative for cytokeratin 7 (CK7), epithelial membrane
antigen, Melan A, CD68, thyroid transcription factor (TTF)
and S100. ZiehlNeelsen stain for acid-fast bacilli and Grocott
stain for fungi were both negative. This was in keeping with a
carcinoid tumour.
The lesion in the right lung macroscopically was a 14-mm
nodular lesion composed of nests of medium-sized regular
cells with regular nuclei and some with small nucleoli
(Fig. 5). These cells had cytoplasm which was eosinophilic in
areas. The tumour cells expressed broad-spectrum cytokeratin
and focally expressed CK7 and TTF strongly. Also focally
expressed were synaptophysin, CD56, chromogranin and PGP
9.5. The melanoma marker S100 was negative and Melan A
was equivocal. These appearances are consistent with a
carcinoid tumour and this patient had bilateral pulmonary
carcinoid.
Discussion
To our knowledge, this is only the second report document-
ing the association between melanoma and pulmonary carci-
noid. There is a report of pulmonary carcinoid associated with
parathyroid hormone-producing melanoma, suggesting an
association between melanoma and the multiple endocrine
neoplasia (MEN) syndrome.
2
Since then, there have been other reports of melanoma
associated with MEN syndromes.
3
One report of seven cases
of melanoma occurring in patients with MEN I noted that all
patients exhibited classic features of MEN I, with hyperpara-
thyroidism and a minimum of one other feature.
3
This study
also analysed the involvement of the MEN1 gene in melanoma
development and concluded that there was a potential role of
this gene in the tumorigenesis of a subgroup of melanoma.
Pulmonary carcinoid is one of the less frequent tumours inclu-
Fig 2. Patient 1. (a) Carcinoid histology, showing the islands of
round blue cells and blood vessels conrming the diagnosis
(haematoxylin and eosin; original magnication 100). (b) Carcinoid
immunohistochemistry: the neuroendocrine marker chromogranin is
strongly positive (original magnication 100).
Fig 1. Patient 1. Melanoma histology. (a) Upward extension of the
melanoma and dermal involvement of the tumour. (b) Pagetoid
ascension of the mitotically active tumour. Haematoxylin and eosin;
original magnication: (a) 10, (b) 40.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp738741
Pulmonary carcinoid associated with melanoma, R. Rajaratnam et al. 739
ded in the MEN I classication. Neither of our patients had
evidence of any other component of the MEN I syndrome, i.e.
endocrine tumours of the parathyroid, anterior pituitary or
pancreas. Therefore it would be ambitious to extrapolate this
association between MEN and melanoma in our patients.
However, cytochemical and immunological studies have
shown that melanomas and carcinoid share many features.
Pearse rst applied the descriptive term APUD to cells with the
ability to produce amines or polypeptide hormones.
1
Accord-
ing to this concept, both melanoma and carcinoid were APUD
tumours. Pearse also hypothesized that these cells, which were
morphologically and functionally similar, shared a common
embryological origin from the neural crest. While the melano-
blasts origin from the neural crest has been veried, the neural
crest origin of other APUD tumours is less clear.
4
Despite this difculty of afrming a common embryological
origin, the similarities between the neuroendocrine carcinoid
tumour and melanoma are compelling. Carcinoids have been
shown to contain melanosomes and melanin in addition to
neurosecretory granules, suggesting a common origin.
5
There
have also been reports of unequivocal melanomas showing
neuroendocrine differentiation.
6
In addition to S100 and
HMB-45, typical of melanoma, there was immunostaining for
neuroendocrine markers such as chromogranin, synaptophysin
and neurolament protein. Moreover, ultrastructural studies
with light and electron microscopy revealed neuroendocrine
granules.
Further evidence of functional similarity between these two
tumours is shown by the ability of melanomas to produce
hormonal polypeptides. There are reports of melanoma produ-
cing adrenocorticotropic hormone and, more strikingly, mela-
noma associated with the production of serotonin.
7
In this
study, a considerable amount of serotonin was detected in
lung tumour tissue of melanoma.
7
Hyperserotinaemia and
hypersecretion of urinary 5-hydroxyindoleacetic acid are most
associated with carcinoid tumours which produce a large
amount of serotonin and more rarely with oat cell carcinoma
of the lung.
Dacarbazine chemotherapy is used to treat advanced meta-
static melanoma, with regression rates of about 10%.
8
Based
Fig 5. Patient 2. Carcinoid histology, right lung, showing
circumscription of the tumour (haematoxylin and eosin; original
magnication 20).
Fig 4. Patient 2. Carcinoid immunohistochemistry, left lung: CD56
neuroendocrine marker is strongly positive (original magnication
100).
Fig 3. Patient 2. (a) Melanoma histology: pleomorphic, mitotically
active epithelioid tumour cells inltrating the dermis (haematoxylin
and eosin; original magnication 40). (b) Melanoma
immunohistochemistry: tumour cells are immunopositive for S100
antigen.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp738741
740 Pulmonary carcinoid associated with melanoma, R. Rajaratnam et al.
on the idea that APUD cell tumours may contain a common
mechanism that can be exploited by a particular cytotoxic
agent, the use of dacarbazine has been extended to other
APUD tumours including carcinoid. A study of patients with
malignant APUD tumours which included carcinoid concluded
that nine of the 11 patients beneted from the dacarbazine
treatment.
9
More recently, a phase II/III study using dacarba-
zine as a second-line treatment for metastatic carcinoid after
failure with doxorubicin, uorouracil and steptozocin conclu-
ded a response rate of 82% with the crossover.
10
While the occurrence of pulmonary carcinoid and mela-
noma in these two patients suggests a causal relationship, this
report does not exclude the possibility of a chance association.
Pulmonary carcinoids are rare neuroendocrine neoplasms of
the lung. They comprise 12% of all lung tumours. Twenty-
ve per cent of patients are asymptomatic, as in both our
cases, and are diagnosed incidentally.
11
The incidence of pul-
monary carcinoids is increasing although this may be due to
ascertainment bias of more sensitive imaging modalities.
In conclusion, we present two patients with melanoma pre-
senting years later with solitary pulmonary nodules on chest
X-ray. Solitary pulmonary nodules in patients with melanoma
are most likely to be indicative of metastatic disease. CT scan
conrmed the presence of an additional nodule in patient 2.
Both patients underwent excision of their lung lesions. Un-
expectedly, this showed pulmonary carcinoid which has a far
more favourable outcome with a 5-year survival of 7092%
vs. metastatic melanoma in which only 4% are alive at
4 years.
12,13
This is the second case in the literature reporting
the association between pulmonary carcinoid and melanoma.
There are reports suggesting that melanoma is associated with
the MEN syndrome of which pulmonary carcinoid is a
component.
Regardless of the difculty of proving a common origin of
melanoma and carcinoid it is useful to consider these two
neoplasms under the umbrella of the APUD theory of Pearse.
The overwhelming similarities, histochemically and biologic-
ally, cannot be overlooked. This report does not exclude the
possibility of a rare association and additional accounts will be
required to strengthen the association. With positron emission
tomography and more advanced imaging becoming widely
available to characterize asymptomatic pulmonary nodules,
this may well be the case. This interesting observation
deserves further investigation.
Acknowledgments
We thank Dr T. Saleem, Dr P. Colloby and Dr C. Roberts for
their help with the histological analysis and photographs.
References
1 Pearse AG. Common cytochemical and ultrastructural characteristics
of cells producing polypeptide hormones (the APUD series) and
their relevance to the thyroid and ultimobronchial C cells and cal-
citonin. Proc R Soc Lond (Biol) 1968; 170:7180.
2 Wagner RF, Sklarek HM, Kulkarni GA et al. Pulmonary carcinoid as-
sociated with a parathormone producing melanoma. J Dermatol Surg
Oncol 1983; 9:5626.
3 Nord B, Platz A, Smoczynski K et al. Malignant melanoma in
patients with multiple endocrine neoplasia type 1 and involvement
of the MEN1 gene in sporadic melanoma. Int J Cancer 2000;
87:4637.
4 Andrew A, Kramer B, Rawdon B. The origin of gut and pancreatic
neuroendocrine (APUD) cells the last word? J Pathol 1998;
186:11718.
5 Gal AA, Koss MN, Hochholzer L et al. Pigmented pulmonary carci-
noid tumour. An immunohistochemical and ultrastructural study.
Arch Pathol Lab 1993; 117:8326.
6 Eyden B, Pandit B, Banerjee SS. Malignant melanoma with neuro-
endocrine differentiation: clinical, histological, immunohistochemi-
cal and ultrastructural features of three cases. Histopathology 2005;
47:4029.
7 Horai T, Nishihara H, Hattori S et al. Malignant melanoma produ-
cing serotonin. Cancer 1979; 43:2948.
8 Comis RL. DTIC in malignant melanoma: perspective. Cancer Treat
Rep 1976; 60:16576.
9 Kessinger A, Foley JF, Lemon HM. Therapy of malignant APUD cell
tumours. Effectiveness of DTIC. Cancer 1983; 51:7904.
10 Sun W, Lipsitz S, Catalano P et al. Eastern Cooperative Oncology
Group. Phase II/III study of doxorubicin with uorouracil com-
pared with streptozocin with uorouracil or dacarbazine in the
treatment of advanced carcinoid tumours: Eastern Cooperative
Oncology Group Study E1281. J Clin Oncol 2005; 23:4897904.
11 Ducrocq X, Thomas P, Massard G et al. Operative risks and prog-
nostic factors of typical bronchial carcinoid tumours. Ann Thorac Surg
1998; 65:141014.
12 Harpole DH, Johnson CM, Wolfe WG et al. Analysis of 945 cases
of pulmonary metastatic melanoma. J Thorac Cardiovasc Surg 1992;
103:74350.
13 Martini N, Zaman MB, Bain MS et al. Treatment and prognosis in
bronchial carcinoids involving the regional lymph nodes. J Thorac
Cardiovasc Surg 1994; 107:17.
2006 The Authors
Journal Compilation 2006 British Association of Dermatologists British Journal of Dermatology 2007 156, pp738741
Pulmonary carcinoid associated with melanoma, R. Rajaratnam et al. 741
CASE REPORT DOI 10. 1111/j . 1365- 2133. 2006. 07713. x
Sezary syndrome in a patient receiving iniximab for
ankylosing spondylitis
J.N. Dauendorffer, J. Rivet,* A. Allard and H. Bachelez
Department of Dermatology and *Department of Pathology, Hopital Saint-Louis, AP-HP, Universite Paris 7, 1 avenue Claude Vellefaux, 75475 Paris cedex 10,
France
Correspondence
Herve Bachelez.
E-mail: herve.bachelez@sls.aphp.fr
Accepted for publication
13 September 2006
Key words
ankylosing spondylitis, cutaneous T-cell lymphoma,
iniximab, Se zary syndrome, tumour necrosis
factor-a
Conicts of interest
None declared.
Summary
Iniximab, a tumour necrosis factor (TNF)-a antagonist, has shown striking
efcacy in the treatment of chronic inammatory rheumatological diseases
such as rheumatoid arthritis and ankylosing spondylitis. However, long-term
follow-up studies support that treatment with iniximab is associated with an
increased risk of non-Hodgkin lymphoma. So far, few cases of cutaneous
lymphoma have been reported in patients receiving TNF-a-blocking agents.
We report a patient who developed Sezary syndrome 17 months after the
onset of iniximab therapy for ankylosing spondylitis. Cutaneous lesions parti-
ally remitted following iniximab withdrawal and methotrexate treatment.
Although the causal link between iniximab and the emergence of Sezary syn-
drome is uncertain, the present case raises the need for exhaustive long-term
registries of malignancies, including primary cutaneous lymphomas, in patients
receiving TNF-a-blocking agents.
Iniximab is a chimeric humanmouse monoclonal antibody
that binds specically to human tumour necrosis factor
(TNF)-a, and neutralizes its biological activities. It has been
approved for the treatment of rheumatoid arthritis, juvenile
rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis,
moderate-to-severe psoriasis and Crohn disease. We report a
case of Sezary syndrome occurring in a patient treated with
iniximab for ankylosing spondylitis.
Case report
A 75-year-old man was referred in October 2004 for the
investigation of diffuse erythematous and squamous plaques.
He had been treated for ankylosing spondylitis, initially with
nonsteroidal anti-inammatory drugs, then with prednisone
10 mg daily for 6 months, and thereafter treatment was
switched to iniximab. He received 17 consecutive intraven-
ous infusions of iniximab 3 mg kg
)1
at 2-monthly intervals,
starting in September 2001. From January 2003, he had pro-
gressively developed inltrated, erythematosquamous plaques
mostly involving the trunk. Pruritus was intense. Histological
examination of a skin biopsy showed a dense dermal lympho-
cytic inltrate, and mild lymphocyte exocytosis into the epi-
dermis. A second skin biopsy performed in May 2004 showed
atypical lymphocytes in an epidermal location, isolated or
forming microabscesses, and a dense dermal inltrate of
regular small lymphocytes in the supercial dermis. In situ
immunophenotypic analysis of the skin inltrate was
performed on a frozen skin sample, revealing the CD3+ CD4+
CD45RO+ predominant phenotype of the dermal and epider-
mal inltrate.
Clinical examination revealed diffuse erythematosquamous,
inltrated plaques (Fig. 1), keratoderma involving palms and
soles, and diffuse supercial lymphadenopathy. Cytological
examination of a peripheral blood sample revealed the pres-
ence of 3300 Sezary cells mm
)3
. Immunophenotyping analysis
of peripheral blood lymphocytes revealed that 92% of them
displayed a CD3+ CD4+ phenotype, with a CD4/CD8 ratio of
51. Cytological examination of an enlarged axillary lymph
node revealed a massive involvement by Sezary cells. Chest
X-ray and abdominal ultrasound examination were otherwise
normal. Skin biopsy showed the same histological lesions as
previously described, but with rare Sezary cells in the super-
cial dermis. Immunohistochemical staining was positive for
CD2, CD3, CD4 and CD5, and negative for CD7, CD8, CD20
and CD30. Molecular analysis of clonality by using Vc-Jc
polymerase chain reaction (PCR) analysis revealed the presence
of an identical predominant clonal rearrangement in peripheral
blood lymphocytes and in a lesional skin biopsy. The diagno-
sis of Sezary syndrome was established, and further conrmed
by the detection of T-plastin expression in peripheral blood
lymphocytes using reverse transcriptionPCR analysis, as previ-
ously described (data not shown).
1
Given the possible causal
role of iniximab, this latter treatment was stopped and was
replaced by oral methotrexate 20 mg weekly, leading to the
regression of most cutaneous lesions.
2007 The Authors
742 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp742743
Discussion
Since their approval for the treatment of rheumatoid arthritis
and Crohn disease, anti-TNF-a-blocking agents, mostly inix-
imab and etanercept, have been associated with an increased in-
cidence of lymphoproliferative disorders.
2
Although this latter
nding is in accordance with the physiological role of TNF-a in
innate immunity and anticancer surveillance, it remains unclear
whether the development of lymphoma in a given individual
receiving anti-TNF-a is due to the immune dysregulation rela-
ted to the underlying disease, or to the TNF-a-blocking agent
itself. Indeed, patients with rheumatoid arthritis are known to
be at increased risk of lymphoproliferative disease compared
with the general population, whether or not they receive TNF-
a-blocking agents.
3
More recently, it has been suggested that
patients with rheumatoid arthritis receiving TNF-a blockers,
mostly iniximab, had an additional increase of the risk for
lymphoid malignancy, although controversial results have been
provided in other studies.
47
On the other hand, the impact of
ankylosing spondylitis on the risk of lymphoid malignancy is
still a matter of debate, and the specic risk of anti-TNF-a
agents in this latter context is unknown. Thus, while Au et al.
suggested that HLA-B27 carriers with ankylosing spondylitis
would have a predisposition for lymphoid malignancies, no
increased risk of haematopoietic malignancies was observed in
a Swedish cohort study conducted by Feltelius et al.
8,9
Rare cases of systemic lymphomas with cutaneous involve-
ment have been reported following treatment with anti-TNF-a
agents. Mahe et al. reported a patient treated with ciclosporin
and iniximab for psoriasis who developed a CD30+ T-cell
lymphoma involving both skin and inguinal lymph nodes.
10
Moreover, a case of systemic anaplastic large cell lymphoma
with cutaneous involvement has recently been reported in
a patient receiving iniximab for Crohn disease.
11
To our
knowledge, only one case of primary cutaneous lymphoma
has previously been reported in a patient treated with anti-
TNF-a agents. In this latter case, a 69-year-old patient with
psoriatic arthritis developed Sezary syndrome 18 months after
the onset of etanercept therapy.
11
Even though the causal role of iniximab in the development
of Sezary syndrome cannot be fully ascertained in the present
case, the partial regression of skin symptoms following inix-
imab withdrawal supports the contribution of iniximab in the
onset of this case of cutaneous lymphoma. Nevertheless, this
latter hypothesis does not rule out the role of other putative
factors such as the chronic inammatory rheumatological dis-
order itself, and the prior history of methotrexate treatment.
3
In conclusion, the present observation, which is the rst
reported case of Sezary syndrome occurring under iniximab
therapy, emphasizes the need for clinicians to include primary
cutaneous lymphomas in the spectrum of lymphoid malignan-
cies emerging in patients receiving anti-TNF-a therapy. It also
raises the need for well-established, long-term registries of
any lymphoid malignancies, including primary cutaneous
lymphomas, in patients receiving TNF-a-blocking agents.
Acknowledgments
We are grateful to Laurence Michel for providing results of
T-plastin expression.
References
1 Su MW, Dorocicz I, Dragowska WH et al. Aberrant expression of
T-plastin in Sezary cells. Cancer Res 2003; 63:71227.
2 Lori Brown S, Greene MH, Gershon SK et al. Tumor necrosis factor
antagonist therapy and lymphoma development. Arthritis Rheum
2002; 46:31518.
3 Georgescu L, Quinn GC, Schwartzman S, Paget SA. Lymphoma in
patients with rheumatoid arthritis: association with the disease state
or methotrexate treatment. Semin Arthritis Rheum 1997; 26:794804.
4 Geborek P, Bladstrom A, Turesson C et al. Tumor necrosis factor
blockers do not increase overall tumor risk in patients with
rheumatoid arthritis, but may be associated with an increased risk
of lymphomas. Ann Rheum Dis 2005; 64:699703.
5 Wolfe F, Michaud K. Lymphoma in rheumatoid arthritis: the effect
of methotrexate and anti-tumor necrosis factor therapy in 18,572
patients. Arthritis Rheum 2004; 50:174051.
6 Askling J, Fored CM, Baecklund E et al. Haematopoietic malignan-
cies in rheumatoid arthritis: lymphoma risk and characteristics after
exposure to tumour necrosis factor antagonists. Ann Rheum Dis
2005; 64:141420.
7 Scott DL, Kingsley GH. Tumor necrosis factor inhibitors for
rheumatoid arthritis. N Engl J Med 2006; 355:70412.
8 Au WY, Hawkins BR, Cheng N et al. Risk of haematological malig-
nancies in HLA-B27 carriers. Br J Haematol 2001; 115:3202.
9 Feltelius N, Ekbom A, Blomqvist P. Cancer incidence among
patients with ankylosing spondylitis in Sweden 196595: a popula-
tion based cohort study. Ann Rheum Dis 2003; 62:11858.
10 Mahe E, Descamps V, Grossin M et al. CD30+ T-cell lymphoma
in a patient with psoriasis treated with ciclosporin and iniximab.
Br J Dermatol 2003; 149:1703.
11 Adams AE, Zwicker J, Curiel C et al. Aggressive cutaneous T-cell
lymphomas after TNFa blockade. J Am Acad Dermatol 2004; 51:6602.
Fig 1 Diffuse erythematous, inltrated plaques involving the lower
dorsal area.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp742743
Sezary syndrome under iniximab therapy, J.N. Dauendorffer et al. 743
Gene Corner
A recurrent splice-site mutation in the human hairless gene underlies congenital atrichia in Irish
families
DOI: 10.1111/j.1365-2133.2006.07742.x
Atrichia with papular lesions (APL) (OMIM 209500) is a form
of irreversible alopecia that is inherited in an autosomal reces-
sive manner. It was rst described clinically in 1950 as a rare
disease characterized by normal hair at birth with subsequent
loss of hair and formation of cutaneous follicular cysts.
1
Clini-
cally, individuals with APL are characterized by a lack of scalp
hair, sparse eyebrows and eyelashes, lack of secondary hair,
few to numerous cutaneous papules, and whitish hypo-
pigmented streaks on the scalp. Recently, rened diagnostic
criteria have been proposed to aid in the diagnosis of APL
2
and distinguish it from other forms of total alopecia, specic-
ally alopecia universalis. The combination of a clinical history
of hair that is shed within the rst few months of life
with lack of subsequent re-growth, together with the presence
of papules with typical histology, and a recessive pattern of
inheritance reliably discriminates APL from other forms of
total alopecia, and is virtually pathognomonic. Although alo-
pecia may accompany several different forms of congenital
ectodermal dysplasias, patients with APL display no defects in
other ectodermal structures such as nails, sweat glands or
teeth.
Although APL has been recognized clinically for decades,
its genetic basis remained unclear until 1998, when this
form of atrichia and the human homologue of the hairless
gene were both linked to the same region of chromosome
8.
3
The hairless gene product has been shown to be a puta-
tive transcription factor with a single zinc-nger domain
that is highly expressed in the brain and the skin. In
humans, the hairless protein appears to function at the
transition from the natal to the rst adult hair cycle. In its
absence, hair growth completely ceases and a new hair is
never induced, resulting in a complete form of inherited
atrichia.
4
Since the initial discovery of the pathogenetic mutations
underlying APL, a total of 29 mutations in the hairless gene in
humans have been described.
5,6
To date, families with APL
have been reported from 17 backgrounds, including Pakistani,
Japanese, Polish, German, Israeli, Palestinian, Mexican, Italian,
Korean and Mediterranean populations. The mutations have
ranged from homozygous missense, nonsense, deletion/inser-
tion and splice-site mutations
617
to compound heterozygous
mutations.
5,1820
In this study, we report a homozygous splice-site mutation
in intron 12 of the hairless gene, IVS12+2insT, in an affected
individual. This mutation likely abrogates normal splicing of
exon 12 and thus potentially generates a frameshift-induced
downstream premature termination codon. Interestingly, we
have identied the same mutation, IVS12+2insT, in a second
family from Ireland with APL, raising the possibility of a recur-
rent pathogenic allele in this population.
Patient and methods
A 2-year-old Irish girl was referred to the Department of Der-
matology, Our Ladys Hospital for Sick Children, Crumlin,
Dublin, for assessment of scalp alopecia. At birth she was noted
to have ne, downy scalp hair limited to the occiput. This was
shed over the rst 3 months of life, with absence of subse-
quent re-growth, resulting in near-total scalp alopecia by
3 months of age. Examination revealed an occasional individ-
ual scalp hair with ne eyebrow and eyelash hair and faint
hypopigmented streaks in a linear distribution on the scalp.
Nails and dentition were normal. Papular lesions were not ini-
tially evident; however, they were noted subsequently from
5 years of age on her forearms and lateral thighs. Her examina-
tion was otherwise unremarkable with the exception of a slight
lividoid appearance to the skin (Fig. 1). She was the rst-born
child from a nonconsanguineous union, with no family history
of similar alopecia (Fig. 2a).
Following informed consent, we obtained genomic DNA
from the unaffected parents and their affected daughter and
extracted it using the PureGene DNA Isolation Kit (Gentra Sys-
tems, Minneapolis, MN, U.S.A.). To screen for a mutation in
the human hairless gene, all exons and splice-site junctions
were amplied by polymerase chain reaction (PCR) and
sequenced directly in an ABI Prism 310 Automated Sequencer,
using the ABI Prism Big Dye Terminator Cycle Sequencing
Ready Reaction Kit (Perkin-Elmer Applied Biosystems, Foster
City, CA, U.S.A.), following purication with Centriex Gel
Filtration Cartridges (Edge Biosystems, Gaithersburg, MD,
U.S.A.). To amplify the PCR fragment containing intron 12 of
the human hairless gene, the following primers were used:
5-AGCTGTTCTACTGCCCTTAC-3 (exon 12, sense) and
5-CTACAGGAGGAGACAGAACG-3 (exon 12, antisense).
The entire coding portion and intronexon borders of the
hairless gene were sequenced in each of the individuals and
2007 The Authors
744 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp744747
analysed for mutations. Sequence analysis of the PCR product
corresponding to exon 12 revealed a mutation at nucleotide
position 2776 characterized by the insertion of a T nucleotide
at position +2 of the donor splice site of intron 12 (Fig. 2b).
The mutation was in the homozygous state in the affected
individual and in the heterozygous state in the parents, con-
rming the clinical ndings. To ensure that the mutation did
not represent a neutral polymorphism in this population, we
screened a panel of 50 unrelated, unaffected northern Euro-
pean control individuals for the mutation. The absence of the
mutation in the 100 control chromosomes supported the
notion that this sequence variant does not represent a poly-
morphism. Sequence analysis of exon 6 also revealed a hetero-
zygous GA transition at nucleotide position 1859, resulting
in an arginine-to-glutamine amino acid substitution at codon
620 (R620Q) in the proband.
Results and discussion
We previously reported the discovery of a sequence variant
(R620Q) in exon 6 within the critical zinc-nger domain
Fig 1. Clinical presentation of the proband with atrichia with papular
lesions. Note scalp atrichia, sparse eyebrows and hypopigmented
linear scalp lines.
(a)
(b)
Fig 2. Genetic analysis of the family with atrichia with papular
lesions. (a) Pedigree of proband and parents. (b) Automated DNA
sequence analysis of exon 12/intron 12 of the hairless gene. DNA
sequences are shown from an unrelated, unaffected control individual
(wild type); a parent of the proband (heterozygous mutation); and
the proband (homozygous mutation). The arrow indicates the site of
the mutation IVS12+2insT found in the proband. This is also the
same mutation found in the affected individuals from a previously
reported Irish family.
8
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp744747
Recurrent splice-site mutation and congenital APL in Irish families, G.M. ORegan et al. 745
of the hairless gene in a large inbred Irish family with con-
genital atrichia.
8
This variant was also identied in the het-
erozygous state in the proband in this study. After the
discovery of this sequence variant, it was identied inde-
pendently in the homozygous state
21
in a single unrelated
unaffected individual, arguing against its role in the patho-
genesis of APL. Upon sequencing the proband in this study
and identifying the splice-site mutation, we revisited the
original Irish family and found the same splice-site muta-
tion (IVS12+2insT) in the homozygous state in the affected
individuals,
8
suggesting the possibility of a recurrent allele
in this population. Of note, the original Irish family was
comprised of Irish Travellers, an indigenous minority with
a long-shared history of nomadism, cultural values and cus-
toms in Irish society.
22
This group also has a high rate of
fertility and consanguineous marriages, both of which have
contributed to the relative frequency of rare gene defects in
this population.
23
Interestingly, the mutation we have iden-
tied in our Irish families has also been previously reported
in the compound heterozygous state (2776+2insT/Q478X)
in a family of English descent,
20
perhaps due to shared
ancestry within the English population.
In each of these families, the splice-site mutation may have
deleterious consequences on hairless expression. For example,
the disruption of intron 12 may inhibit the ability of the pre-
ceding exon to be recognized by splicing factors, leading to
skipping of exon 12 and subsequent splicing of exon 11 to
exon 13.
24
Exon skipping is a well-known potential conse-
quence of mutations that disrupt consensus splicing
sequences.
25
It can result in a frameshift-induced premature
termination codon in a downstream exon, thus generating an
mRNA that would likely be degraded by nonsense-mediated
mRNA decay.
26
However, the occurrence of exon skipping
could not be assessed due to the lack of available mRNA sam-
ples. Nevertheless, we examined the effect of this mutation,
which changes the consensus sequence from (exon 12)GC/
gtaagt (intron 12) to (exon12)GC/gttaag (intron 12), on spli-
cing efciency and calculated scores of 78.65 and 49.64 for
the wild-type and mutant sequences, respectively.
27
This nd-
ing suggests a signicant decrease in splicing efciency as a
result of the mutation.
In summary, we have identied a recurrent mutation,
IVS12+2insT, in two Irish families with APL. Continued eluci-
dation of population-specic alleles will assist in tailoring gen-
etic testing for APL and in differentiating APL from alopecia
universalis. Further advancements in the diagnosis of APL will
spare patients with inherited atrichia unnecessary and ineffec-
tive treatment due to misdiagnosis.
G. M. O RE GAN
J . ZURADA*
A. MARTI NE Z - MI R*
A. M. CHRI S TI ANO*
A. D. I RVI NE
Department of Paediatric Dermatology,
Our Ladys Hospital for Sick Children,
Crumlin, Dublin 12, Ireland
*Department of Dermatology,
Columbia University, New York, NY, U.S.A.
Correspondence Alan D. Irvine.
E-mail: alan.irvine@olhsc.ie
References
1 Fredrich HC. Zur Kenntnis der kongenitale Hypotrichosis. Dermatol
Wochenschr 1950; 121:40810.
2 Zlotogorski A, Martinez-Mir A, Green J et al. Evidence for pseudo-
dominant inheritance of atrichia with papular lesions. J Invest Derma-
tol 2002; 118:8816.
3 Ahmad W, Faiyaz ul Haque M, Brancolini V et al. Alopecia univer-
salis associated with a mutation in the human hairless gene. Science
1998; 279:7204.
4 Panteleyev AA, Botchkareva NV, Sundberg JP et al. The role of the
hairless (hr) gene in the regulation of hair follicle catagen trans-
formation. Am J Pathol 1999; 155:15971.
5 Ahsoor GG, Greenstein RM, Lam H et al. Novel compound hetero-
zygous nonsense mutations in the hairless gene causing atrichia
with papular lesions. J Dermatol Sci 2005; 40:2933.
6 John P, Aslam M, Raq MA et al. Atrichia with papular lesions in
two Pakistani consanguineous families resulting from mutations in
the human hairless gene. Arch Dermatol Res 2005; 297:22630.
7 Chincon S, Anker M, Vogt IR et al. Cloning genomic organization,
alternative transcripts and mutational analysis of the gene respon-
sible for autosomal recessive universal congenital alopecia. Hum Mol
Genet 1998; 7:16719.
8 Ahmad W, Irvine AD, Lam H et al. A missense mutation in the
zinc-nger domain of the human hairless gene underlies congen-
ital atrichia in a family of Irish travellers. Am J Hum Genet 1998;
63:98491.
9 Kruse K, Cichon S, Anker M et al. Novel hairless mutations in two
kindreds with autosomal recessive papular atrichia. J Invest Dermatol
1999; 113:9549.
10 Sprecher E, Bergman R, Szargel R et al. Identication of a genetic
defect in the hairless gene in atrichia with papular lesions: evi-
dence for phenotypic heterogeneity among inherited atrichias.
Am J Hum Genet 1999; 64:13239.
11 Sprecher E, Lestringant GG, Szargel R. Atrichia with papular lesions
resulting from a nonsense mutation within the human hairless
gene. J Invest Dermatol 1999; 113:68790.
12 Aita VW, Ahmad W, Panteleyev AA et al. A novel missense muta-
tion (C622G) in the zinc-nger domain of the human hairless
gene associated with congenital atrichia with papular lesions.
Exp Dermatol 2000; 9:15762.
13 Djabali K, Zlotogorski A, Metzker A et al. Interaction of hairless
and thyroid hormone receptor is not involved in the pathogene-
sis of atrichia with papular lesions. Exp Dermatol 2004; 13:
2516.
14 Zlotogorski A, Ahmad W, Christiano AM. Congenital atrichia in
ve Arab Palestinian families resulting from a deletion mutation in
the human hairless gene. Hum Genet 1998; 103:4004.
15 Zlotogorski A, Panteleyev AA, Aita VM, Christiano AM. Clinical
and molecular diagnostic criteria of congenital atrichia with papu-
lar lesions. J Invest Dermatol 2002; 118:88790.
16 Paradisi M, Chuang GS, Angelo C et al. Atrichia with papular
lesions resulting from a novel homozygous missense mutation in
the hairless gene. Clin Exp Dermatol 2003; 28:5358.
17 Masse M, Martinez-Mir A, Lam H et al. Identication of a recurrent
mutation in the human hairless gene underlying atrichia with pap-
ular lesions. Clin Exp Dermatol 2005; 30:3635.
18 Henn W, Zlotogorski A, Lam H et al. Atrichia with papular lesions
resulting from compound heterozygous mutations in the hairless
gene: a lesson for differential diagnosis of alopecia universalis.
J Am Acad Dermatol 2002; 47:51923.
19 Indelman M, Bergman R, Lestringant GG et al. Compound hetero-
zygosity for mutations in the hairless gene causes atrichia with
papular lesions. Br J Dermatol 2003; 148:5537.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp744747
746 Recurrent splice-site mutation and congenital APL in Irish families, G.M. ORegan et al.
20 Paller AS, Varigos G, Metzker A et al. Compound heterozygous
mutations in the hairless gene in atrichia with papular lesions.
J Invest Dermatol 2003; 121:4302.
21 Hillmer AM, Kruse R, Betz RC et al. Variant 1859GA (Arg620Gln)
of the hairless gene: absence of association with papular atrichia or
androgenic alopecia. Am J Hum Genet 2001; 69:2357.
22 Gmelch G, Gmelch SB. Irelands Travelling People: A Comprehen-
sive Bibliography, 4th edn. J Gypsy Lore Soc 1977; 1:15969.
23 Flynn MP, Martin MC, Moore PT et al. Type II hyperprolinaemia in
a pedigree of Irish travellers (nomads). Arch Dis Child 1989;
64:1699707.
24 Talerico M, Berget SM. Effect of 5 splice site mutations on spli-
cing of the preceding intron. Mol Cell Biol 1990; 10:6299305.
25 Kon A, Pulkkinen L, Ishida-Yamamoto A et al. Novel COL7A1
mutations in dystrophic forms of epidermolysis bullosa. J Invest
Dermatol 1998; 111:5347.
26 Zhang J, Sun X, Qian Y et al. At least one intron is required for the
nonsense-mediated decay of triosephosphate isomerase mRNA:
a possible link between nuclear splicing and cytoplasmic translation.
Mol Cell Biol 1998; 18:527283.
27 Shapiro MB, Senapathy P. RNA splice junctions of different classes
of eukaryotes: sequence statistics and functional implications in
gene expression. Nucleic Acids Res 1987; 15:715574.
Accepted for publication: 20 September 2006
Key words: alopecia, atrichia with papular lesions, congenital atrichia, human
hairless gene, Irish travellers
Conicts of interest: none declared.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp744747
Recurrent splice-site mutation and congenital APL in Irish families, G.M. ORegan et al. 747
Correspondence
AL amyloidosis enhances development
of amyloid A amyloidosis
DOI: 10.1111/j.1365-2133.2006.07709.x
SIR, In the April issue of this journal, Rekhtman et al. describe
an interesting case of a patient with concomitant AL (also
referred to as primary or myeloma-associated amyloidosis)
and amyloid A (AA) amyloidosis.
1
The authors state that the
pathogenesis of dual amyloidosis is not clear nor is the rela-
tionship of dual deposits with rapid progression. However,
our recent advances in the knowledge of the pathogenesis of
amyloidosis may explain both enigmas.
The amyloidoses constitute a group of disorders that are
characterized by deposition of protein brils in organs and tis-
sues leading to organ dysfunction.
2
The brils are aggregates
of a precursor protein that has a typical b-pleated-sheet con-
formation. So far at least 23 different precursor proteins have
been identied that can aggregate into brils, including Ab
peptide in Alzheimer plaques and b2 microglobulin in haemo-
dialysis-associated amyloidosis.
3
Amyloidosis develops when
the precursor protein is over-expressed [e.g. increased expres-
sion of acute phase protein serum amyloid A protein (SAA)
during inammation in AA amyloidosis] or when a mutation
in a constitutively expressed protein leads to a greater ten-
dency to aggregate (e.g. in familial ATTR amyloidosis). In
type AA amyloidosis SAA has to be proteolytically cleaved into
AA amyloid fragments before these can be incorporated into
brils.
The kinetics of amyloidosis is characterized by a lag phase
during which all the prerequisites are present but no brils
are formed. Once a critical nucleus of amyloid is formed, the
conditions change to favour aggregation with very fast kinet-
ics.
4
The lag phase can last from weeks to years. For example,
in a mouse model for AA amyloidosis, amyloid brils are
formed in the spleen in response to injection of an inamma-
tory stimulus after a lag phase of 34 weeks. It has been
known for a long time that this lag period can be shortened
dramatically to 3 days by the simultaneous injection of
extracts of spleen from amyloidotic mice.
5
The activity of this
amyloid-enhancing factor (AEF) has been shown to depend
on small molecules with a b sheet structure. It acts as a tem-
plate for amyloid brillogenesis to begin, similar to a snow-
ake that starts growing from a speck of dirt.
6
Not only AEF
generated from AA brils can thus shorten the lag period, but
other types of amyloid brils have also been shown to act as
AEF in AA amyloidosis, including AL amyloid brils.
7,8
Therefore, we suggest the following cascade of events in
this patient with dual amyloid deposits. First, plasma cell dys-
crasia induced amyloid brils of the AL type. These brils of
the AL type act as an AEF for AA amyloidogenesis, making the
patient far more susceptible to any other type of amyloidosis
The systemic inammation secondary to mucocutaneous bul-
lous amyloidosis will have resulted in elevated serum concen-
tration of SAA in this patient. Because of the presence of AL
type amyloid brils acting as AEF, this rapidly resulted in AA
amyloid deposition.
To test this hypothesis we used a well-dened cell culture
model of AA amyloidosis in which isolated human monocytes
are incubated with recombinant SAA (150 mg L
)1
) for
7 days, with or without mouse spleen-derived AEF.
9,10
Mono-
cytes were isolated from a patient suffering from AL amyloid-
osis and four healthy volunteers. Amyloid brils were detected
by staining the cells with Congo red. As shown in Figure 1,
after 7 days of incubation cells of healthy volunteers make
amyloid brils only when they are simultaneously exposed to
AEF. However, monocytes from the patient with AL amyloid-
osis showed extensive AA amyloid deposition even without
co-incubation with AEF. This suggests that the previous expos-
ure to AL amyloid brils acts as an AEF to enhance AA amyl-
oid formation. In conclusion, AL amyloid brils may act as
AEF for AA amyloidogenesis.
This could well explain the dual expression of AA and AL
amyloidosis in the same patient and the rapid progressive
course.
J . C. H. VAN DE R HI L S T*
J . W. M. VAN DE R ME E R*
J . P. H. DRE NT H
A. SI MON*
Departments of *General Internal
Medicine (463), and
Gastroenterology and Hepatology,
Radboud University Medical Centre St
Radboud, Geert Grooteplein 8,
PO Box 9101, 6500 HB Nijmegen, the Netherlands
National Institute of Arthritis and Musculoskeletal
and Skin Diseases, National Institutes of Health,
Bethesda, MD, U.S.A.
E-mail: j.vanderhilst@aig.umcn.nl
References
1 Rekhtman N, Hash KS, Moresi JM. Mucocutaneous bullous
amyloidosis with an unusual mixed protein composition of amyl-
oid deposits. Br J Dermatol 2006; 154:7514.
2 van der Hilst JC, Simon A, Drenth JP. Hereditary periodic fever
and reactive amyloidosis. Clin Exp Med 2005; 5:8798.
2007 The Authors
748 Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
3 Westermark P, Benson MD, Buxbaum JN et al. Amyloid bril pro-
tein nomenclature2002. Amyloid 2002; 9:197200.
4 Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl
J Med 2003; 349:58396.
5 Axelrad MA, Kisilevsky R, Willmer J et al. Further characterization
of amyloid-enhancing factor. Lab Invest 1982; 47:13946.
6 Magy N, Liepnieks JJ, Benson MD et al. Amyloid-enhancing factor
mediates amyloid formation on broblasts via a nidus/template
mechanism. Arthritis Rheum 2003; 48:14307.
7 Johan K, Westermark G, Engstrom U et al. Acceleration of amyloid
protein A amyloidosis by amyloid-like synthetic brils. Proc Natl
Acad Sci USA 1998; 95:255863.
8 Ganowiak K, Hultman P, Engstrom U et al. Fibrils from synthetic
amyloid-related peptides enhance development of experimental AA-
amyloidosis in mice. Biochem Biophys Res Commun 1994; 199:30612.
9 Kluve-Beckerman B, Liepnieks JJ, Wang L et al. A cell culture system
for the study of amyloid pathogenesis. Amyloid formation by peri-
toneal macrophages cultured with recombinant serum amyloid A.
Am J Pathol 1999; 155:12333.
10 Kluve-Beckerman B, Manaloor JJ, Liepnieks JJ. A pulse-chase study
tracking the conversion of macrophage-endocytosed serum amyloid
A into extracellular amyloid. Arthritis Rheum 2002; 46:190513.
Conicts of interest: none declared.
(a) (b)
(c) (d)
(e) (f)
Fig 1. Congo red and haematoxylin staining of cultured monocytes. (a) and (b) Monocytes derived from healthy volunteer cultured for 7 days with
150 mg L
)1
SAA (a) and AEF (b), showing amyloid (arrows) only when cells are simultaneously exposed to AEF. (c) and (d) Monocytes derived from
a patient suffering from AL amyloidosis incubated only with SAA (c) showing extensive amyloid deposits (arrows). No amyloid is seen when cells are
cultured in the absence of SAA (d). (e) Detailed image of an amyloid deposit from the AL patient showing typical apple-green birefringence under
polarized light (f). Original magnication (ad) 10, (e and f) 40. SAA, serum amyloid A protein; AEF, amyloid enhancing factor.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 749
Extensive mucinous metaplasia of the vulva
arising within Zoons vulvitis
DOI: 10.1111/j.1365-2133.2006.07712.x
SIR, Mucinous metaplasia of the genital skin is a rare entity
characterized by mucin-containing cells within or replacing
the stratied squamous epithelium. We report a case of exten-
sive mucinous metaplasia of the vulva with haemosiderin
deposition arising within Zoons vulvitis. We discuss the
pathogenesis and differential diagnosis of mucinous epithe-
lium in the lower genital tract.
A 67-year-old woman initially presented with a small, well-
demarcated, red/brown macule on the labia minora. A biopsy
from 1995 (Fig. 1) had been reported as lichen sclerosus and
serial biopsies from 20022004 conrmed chronic inamma-
tion, without neoplasia, but did not give a specic diagnosis
for the inammatory process. On review in 2005, she now
had a 10-year history of vulval soreness which had not
responded to conjugated oestrogen cream and potent topical
steroids. The lesions had gradually enlarged to involve the
inner aspects of both labia minora, the clitoral hood and one
side of the introitus (Fig. 2a). The differential diagnosis inclu-
ded purpura secondary to lichen sclerosus, Zoons vulvitis,
extramammary Pagets disease, vulval intra-epithelial neoplasia
and melanoma.
All of the biopsies were reviewed. The 1995 biopsies
showed a thinned epidermis with spongiosis and lozenge-
shaped keratinocytes, and a dense, band-like plasma cell-rich
inltrate in the corium without overt interface damage, in
keeping with Zoons vulvitis.
1
There were plasma cells,
lymphocytes and scanty neutrophils in the corium. In add-
ition, there were dilated capillaries, some red cell extravasation
and mild haemosiderin deposition (Fig. 1ad). Biopsies taken
between 2002 and 2004 showed focal residual features of
(a) (b)
(c) (d)
Fig 1. Biopsy from 1995 showing features of Zoons vulvitis. (a) There is thinned epidermis and a dense band of inammatory cells in the
corium (haematoxylin and eosin, H&E; original magnication 100). (b) Lozenge-shaped keratinocytes in the thinned epidermis with mild
spongiosis (H&E; original magnication 1000). (c) Plasma cells make up approximately 50% of the inltrate in the corium, accompanied by
lymphocytes, a few histiocytes and sparse neutrophils (H&E; original magnication 1000). (d) Moderate haemosiderin deposition is evident
(Perls stain; original magnication 400).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
750 Correspondence
Zoons vulvitis (Fig. 2b) but large areas in which the squa-
mous epithelium was replaced by pseudostratied columnar
cells (Fig. 2c,d) having apical acidic (alcian blue+, blue) and
neutral (diastase periodic acidSchiff+, purple) mucins
(Fig. 2e,f). The supercial corium showed variable, but in
areas striking, deposition of haemosiderin (Fig. 2c,e) with a
relatively sparse inammatory inltrate including occasional
plasma cells. The columnar mucinous cells stained positively
for carcinoembryonic antigen, epithelial membrane antigen,
cytokeratin 7 and CAM 5.2, conrming the glandular nature
of the epithelium. Staining for cytokeratin 20 was negative.
The histological appearances were of extensive mucinous
metaplasia of the vulva in association with Zoons vulvitis and
prominent haemosiderin deposition giving rise to clinical
pigmentation.
Mucinous metaplasia of the external genitalia is rare. Cases
affecting the glans penis
2,3
and foreskin
3
have occurred in the
setting of severe chronic inammation and, possibly more
specically, with Zoons balanitis. To our knowledge, vulval
mucinous metaplasia has been reported previously only twice,
in association with Zoons vulvitis
4
and lichen sclerosus.
5
The presence of mucin-containing cells in the surface epi-
thelium of the vulva usually leads to a diagnosis of extramam-
mary Pagets disease. However, the uniformity of the surface
layer of columnar epithelium replacing rather than inltrating
the squamous epithelium and the absence of cellular atypia
and pagetoid pattern negated the diagnosis of Pagets disease.
Mullerianosis (misplaced endocervical, endometrial or ciliated
Fallopian tubal-type epithelium), which has been described in
the posterior bladder and pelvic peritoneum,
6
was considered
in the differential diagnosis, but to our knowledge this process
has not been reported in the vulva. In addition, the lower part
of the vagina and the vulva are derived from the urogenital
sinus rather than the Mullerian ducts and therefore the appear-
ance of mucinous epithelium resembling the cervical canal
would be unexpected. The mucinous metaplasia in our patient
(a)
(b)
(d)
(c)
(e) (f)
Fig 2. Biopsies taken between 2002 and 2004 showing focal residual features of Zoons vulvitis and features of mucinous metaplasia of the vulva.
(a) Well-demarcated, reddish brown macules on both labia minora, the clitoral hood and one side of the introitus. (b) Features of residual Zoons
vulvitis (haematoxylin and eosin, H&E; original magnication 100) and (c) large areas in which the surface epithelium is replaced by
pseudostratied columnar type (H&E; original magnication 100) shown under high power (d) (H&E; original magnication 1000).
(e) Apical acidic mucin (blue) and scanty neutral mucin (purple) in the mid-epithelium (alcian blue/diastase periodic acidSchiff; original
magnication 400). Striking haemosiderin deposition in supercial corium (c) is highlighted by Perls stain (f) (original magnication 1000).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 751
was also pseudostratied in comparison with the single layer
of mucinous epithelium seen in the endocervical canal and
endocervical Mullerianosis (endocervicosis).
Vaginal adenosis, which describes nonepithelialized colum-
nar glandular epithelium in the vagina, has been reported only
in the upper vagina and in our patient the typical glands or
remnant cysts in the corium were absent. The aetiology of this
mucinous change is uncertain but all cases reported in male
genitalia have occurred in the setting of severe inammation
and Zoons balanitis in particular,
3
supporting the view that
this phenomenon is metaplastic. Recurrent ulceration may be
a factor and regeneration from the ducts of the local (modi-
ed sweat) glands might give rise to the surface columnar
mucinous phenotype. The predominance of associated Zoons
balanitis/vulvitis may reect the severity of the inammation
in this condition.
The aetiology of the striking haemosiderin deposition in
our case is uncertain but might be secondary to local trauma,
recurrent ulceration or injury to the delicate metaplastic epi-
thelium and/or increased fragility of vessels secondary to
potent topical steroids. Dilated vessels, red cell extravasation
and haemosiderin deposition are a recognized feature of
Zoons vulvitis
1
and this has led to the alternative designation
chronic vulvar purpura
7
for this condition. One further con-
sideration for the haemosiderin deposition was underlying
lichen aureus, which has been reported once previously in the
vulva.
8
Our case had similar clinical ndings but histological
features (epidermal changes and plasma cell-rich inltrate)
were considered diagnostic of Zoons vulvitis.
We have presented a third case of mucinous metaplasia of
the vulva and the second arising in association with Zoons
(plasma cell) vulvitis. This condition should not be confused
with extramammary Pagets disease but the risk for malignant
transformation in benign mucinous metaplasia is unknown.
We would therefore advise close follow-up in these patients.
M. A. THOMS ON
R. A. CARR*
R. GANE S AN
F. HUMP HRE YS
Departments of Dermatology and
*Pathology, Warwick Hospital, Warwick
CV34 5BW, U.K.
Department of Histopathology, Birmingham
Womens Hospital, Birmingham B15 2TG, U.K.
Correspondence: Michelle Thomson, 19 Yew Tree Road,
Edgbaston, Birmingham B15 2LX, U.K.
E-mail: micksthomson@lineone.net
References
1 Calonje E, Neill S. Diseases of the genital skin. Chapter 11. In: Pathol-
ogy of the Skin (McKee PH, Calonje E, Granter SR, eds), 3rd edn. Lon-
don: Elsevier Mosby, 2005; 4878.
2 Val-Bernal JF, Hernandez-Nieto E. Benign mucinous metaplasia of
the penis. A lesion resembling extramammary Pagets disease. J Cutan
Pathol 2000; 27:769.
3 Fang AW, Whittaker MA, Theaker JM. Mucinous metaplasia of the
penis. Histopathology 2002; 40:1779.
4 Coghill SB, Tyler X, Shaxted EJ. Benign mucinous metaplasia of the
vulva. Histopathology 1990; 17:3735.
5 Rakha E, Mayne C, Brown L. Mucinous metaplasia of the vulva in a
case of lichen sclerosus. A case report. J Clin Pathol 2005; 58:121718.
6 Young RH. Pseudoneoplastic lesion of the urinary bladder and
urethra. Semin Diagn Pathol 1997; 14:13346.
7 Kato T, Kuramoto Y, Tadaki T et al. Chronic vulvar purpura. Dermatol-
ogica 1990; 180:1746.
8 Li Q, Leopold K, Carlson JA. Chronic vulvar purpura: persistent pig-
mented purpuric dermatitis (lichen aureus) of the vulva or plasma
cell (Zoons) vulvitis? J Cutan Pathol 2003; 30:5626.
Conicts of interest: none declared.
Scrotal cutaneous chylous reux
DOI: 10.1111/j.1365-2133.2006.07715.x
SIR, Chylous reux from the skin is usually associated with an
underlying defect in the lymphatic vessels. We report an
unusual case of scrotal cutaneous chylous reux with clinically
numerous vesicles over the scrotum and large amounts of
milky uid draining intermittently from these vesicles.
A 17-year-old boy had had intermittent whitish discharge
from the vesicles of the scrotum for 23 years. Each episode
could be resolved after compression and bed rest. The size of
the vesicles increased after the patient stood for a long time.
There was no oedema of the bilateral lower extremities or
erectile dysfunction. There was no history of surgery or trauma.
His development and growth were within normal limits.
Physical examination showed numerous 26 mm diameter
whitish to yellowish vesicles conuent over the scrotum, with
thickening of the scrotal skin (Fig. 1a). In addition, several 1
2 mm diameter whitish vesicles were scattered over the base
of the penis and three or four whitish vesicles were grouped
over the medial aspect of the upper right thigh. Large amounts
of milk-like uid discharged intermittently from these vesicles
after abrasion (Fig. 1b).
Laboratory studies, including haematology, urinalysis, fasting
blood sugar, serum cholesterol, triglyceride, protein, albumin,
blood urea nitrogen, creatinine, aspartate aminotransferase and
alanine aminotransferase, were all within normal limits.
Aspirated uid from the vesicles showed a milk-like colour and
the triglyceride level was 35.5 mmol L
)1
(the triglyceride level
of serum was normal). Abdominal and pelvic computed
tomographic (CT) scan showed no evidence of tumours.
Biopsy from the right upper medial thigh showed saccular
dilatation of lymphatic vessels lined by a single layer of endo-
thelial cells over the upper dermis (Fig. 2). There were
enlarged and dilated lymphatic vessels with thickened walls in
the lower dermis and subcutaneous tissue. According to the
clinical and pathological ndings, scrotal cutaneous chylous
reux was diagnosed.
Chyle originates in the intestinal lacteals and drains into
the mesenteric lymphatics. Chyle eventually drains into the
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
752 Correspondence
thoracic duct via the cisterna chyli and nally enters the
bloodstream. The term chylous reux refers to the backow
of chyle from its normal route.
1
Primary chylous reux
suggests the absence of an apparent aetiology and may be due
to congenital lymphangiectasia with or without lymphatic
obstruction. Secondary chylous reux can be caused by irradi-
ation, malignancy, surgery, trauma or infection by lariasis.
It has been considered that malformation of the cisterna
chyli and mesenteric lymph nodes are two basic anatomical
abnormalities involved in the primary cutaneous chylous
reux.
2
The valves in the dilated varicose lymph vessels
become incompetent and lymph mixed with chyle reuxes
into the lower limbs or the genitalia.
3
Depending on the sites
of the dilated lymphatics and lymphatic disruption, patients
might also present with chylous ascites, chylothorax, chylopty-
sis, chylopericardium, chylometrorrhoea or chyluria.
Clinical manifestations of cutaneous chylous reux vary
according to the velocity of the chylous reux.
4
Slow-forming
white papules have been called xanthomas.
5
These solid
papules are local accumulations of white to creamy yellow
chyle that are usually mixed with macrophages and
histiocytes. If the chylous reux is more rapid and forceful,
the formation of vesicles occurs. These vesicles are not true
vesicles but are dilated cutaneous lymphatics that approach the
epidermal surface and mimic vesicles clinically. If the valvular
insufciency allows chylous reux to the extremities, this
results in chylous lymphoedema.
5
Lymphoedema of a limb
may occur before or after the cutaneous lesions. Chronic loss
of chyle leads to anaemia, hypoproteinaemia, hypocalcaemia,
hypolipidaemia, immunocompromise and malnourishment.
The ruptured lymphatic vesicles also serve as an entry point
for bacteria, causing cellulitis or lymphangitis.
The diagnosis of chylous uid was conrmed by two or
more of the following evaluations: the appearance of milky
uid, a triglyceride level >124 mmol L
)1
, and lipoprotein
analysis for the presence of chylomicrons.
3
In contrast to chy-
lous uid, the content of lymphangioma is clear uid. CT scan
or magnetic resonance imaging should be arranged to exclude
underlying malignancy.
Procedures for diagnostic imaging include lymphangio-
graphy and lymphoscintigraphy.
6
Lymphangiography is
recommended to determine lymphatic anatomy and the site of
the lymphatic leak. However, it is no longer the method of
choice because of the disadvantages of exposure of the lym-
phatic vessels, pressure injection, contrast-induced lymphatic
injury and low resolution. Lymphoscintigraphy provides ima-
ges representative of the function of the lymphatic system.
The aim of treatment is to stop the chylous reux by dimin-
ishing retrograde ow of lymph emanating from intestinal lac-
teals.
3
Nonsurgical management of patients for cutaneous
chylous reux includes a low-fat medium chain triglyceride
diet to decrease chyle production, diuretics, and compression
garments to reduce lymphoedema. Antibiotics are given to
patients with cellulitis or lymphangitis. The surgical manage-
ment for chylous reux includes resection of retroperitoneal
and mesenteric lymphatics with or without sclerotherapy of
Fig 1. (a) Numerous whitish to yellowish vesicles over the scrotum.
(b) Large amount of milk-like uid draining out from these vesicles.
Fig 2. Dilation of lymphatic vessels lined by a single layer of
endothelial cells over the upper dermis (haematoxylin and eosin;
original magnication 40).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists 2007 156, pp748791
Correspondence 753
lymphatics. Surgery should be considered in low-risk patients
with signicant symptoms such as malnutrition.
3
We did not arrange lymphoscintigraphy for the patient
because his parents did not give consent. We are managing
the patient with conservative treatments. Further close follow
up of the clinical condition is necessary.
H- Y. HUANG
S- L. HU
References
1 Kinmonth JB, Taylor GW. Chylous reux. 1964; i:52932.
2 Chern LC, Lin CS, Wong CK. Cutaneous chylous reux.
1989; 120:695700.
3 Noel AA, Gloviczki P, Bender CE Treatment of symptomatic
primary chylous disorders. 2001; 34:78591.
4 Johnson WT. Cutaneous chylous reux: the weeping scrotum.
1979; 115:4646.
5 Karg E, Bereczki C, Kovacs J Primary lymphoedema associated
with xanthomatosis, vaginal lymphorrhoea and intestinal lymph-
angiectasia. 2002; 146:1347.
6 Witte CL, Witte MH, Unger EC Advances in imaging of lymph
ow disorders. 2000; 20:1697719.
Conicts of interest: none declared.
A woman with iatrogenic androgenetic
alopecia responding to nasteride
DOI: 10.1111/j.1365-2133.2006.07719.x
SIR, Finasteride, a type II 5a-reductase inhibitor, has long been
proposed to treat androgenetic alopecia in women.
1
Although
female hair loss associated with hyperandrogenism can
respond to nasteride,
2
there has been no report on its ef-
cacy for rare cases of androgenetic alopecia that develops in
women undergoing androgen therapy. We describe a woman
receiving exogenous androgen supplementation who devel-
oped Hamilton type hair loss and responded well to a med-
ium-high dose of nasteride (25 mg daily).
In 2005, we began treating a 47-year-old woman with a
2-year history of progressive scalp hair loss. At the age of
24 years, she was diagnosed with a right ovarian dysgermi-
noma presenting with right lower abdominal distension and
underwent a total hysterectomy and bilateral salpingoophorec-
tomy followed by two courses of chemotherapy [Adriamycin
(doxorubicin) and cisplatin]. She was then given Disemone
(4 mg estradiol valerate, 902 mg testosterone enanthate)
monthly for her surgically menopausal status, which caused
discomfort including hot ushing. In 2003, her hormonal
supplementation was increased to nearly twice monthly, better
to control her menopausal symptoms. Afterwards, progressive
hair thinning on the scalp developed.
In 2005, she presented to our dermatology clinic for evalu-
ation of progressive hair loss. Physical examination revealed a
nonscarring Hamilton type IVV alopecia on the vertex with
signicant frontotemporal recession (Fig. 1a). The hair shafts
and scalp skin were normal. She also had clinical signs of
hyperandrogenism, including facial hirsutism, muscular body
habitus, and a deepened voice. Thus, we suspected that she
had developed an iatrogenic androgen-induced alopecia.
Reviewing the literature, we found no evidence that na-
steride might have an adverse effect on a patient with dysger-
minoma who had undergone complete surgery and had been
recurrence-free for 23 years. She was treated with a medium-
high dose of nasteride (25 mg daily). After the rst
6 months, her hair loss stabilized. By 10 months, despite still
receiving androgen supplementation, she had noticeable
improvement of hair coverage on the scalp (Fig. 1b, Hamilton
type III) as compared with that at baseline (Fig. 1a). She also
reported decreased hirsutism and a higher pitch of her voice.
Hair loss generates considerable anxiety in both men and
women. However, male-pattern alopecia is often more socially
acceptable and has well-established treatment regimens such as
nasteride. Finasteride 1 mg daily is highly effective in treat-
ing male-pattern alopecia,
3
but has less clear efcacy in female
(a)
(b)
Fig 1. Clinical pictures of the patient before treatment (a) and after
10 months of therapy with nasteride (b).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists 2007 156, pp748791
754 Correspondence
androgenetic alopecia. In 2000, a multicentre, randomized,
double-blind, placebo-controlled study of postmenopausal
women treated with nasteride 1 mg daily showed no
improvement in increasing hair growth or slowing the pro-
gression of hair thinning.
4
In contrast, in 2001 a noncon-
trolled study of 42 pre- and postmenopausal women with
female-pattern hair loss and SAHA syndrome (seborrhoea,
acne, hirsutism and alopecia) revealed that nasteride 25 mg
daily effectively increased hair growth.
5
Recently, another study supported the efcacy of medium-
high doses of nasteride in the treatment of female-pattern
hair loss. Approximately two-thirds of the 37 women without
clinical evidence of hyperandrogenism responded well to a
medium-high dose of nasteride (25 mg daily).
1
The authors
stated that the concomitant use of the oral contraceptive dro-
spirenone may also have contributed to the hair growth due
to its antiandrogenic effect. Marked efcacy was also observed
for higher doses of nasteride (12550 mg daily) in women
with normo- or hyperandrogenism in recent reports.
2,6
As
these higher doses of nasteride differ from the standard male
androgenetic alopecia dose of 10 mg daily, an important un-
answered question arises: whether androgenetic alopecia in
women demonstrates a dose-dependent therapeutic response
or whether some patients respond due to their relative andro-
gen levels. Indeed, in one case report, a woman with andro-
genetic alopecia had limited response to nasteride 05 mg
daily and beneted well from dutasteride, a more potent
5a-reductase inhibitor.
7
In our case, we cannot rule out that a lower dose of na-
steride may have been effective. Further study is necessary to
establish the optimal dose regimen for nasteride in female
androgenetic alopecia due to androgen supplementation. Prac-
titioners need to be aware that Hamilton type hair loss can
occur in women given androgen supplementation, especially
at higher doses. In our patient, androgen-induced alopecia
was effectively treated with a medium-high dose of nasteride
(25 mg daily) despite her continued androgen supplementa-
tion. Taking her surgically menopausal status into account, the
testosterone adjunct to oestrogen replacement therapy may
benet our patient by reducing anxiety and depression, pro-
tecting against breast cancer
8
and delaying Alzheimers dis-
ease.
9
We recommend that hormonal supplementation with
androgen be appropriately reduced and maintained at a rea-
sonable dose when iatrogenic androgenetic alopecia is found.
J - B. HONG*
H- C. CHI U*
J - Y. CHAN*
R- J . CHE N
S- J . LI N*
*Department of Dermatology and
Department of Obstetrics and Gynecology,
National Taiwan University Hospital and
National Taiwan University College of Medicine,
No.7, Chun-Shan South Road, Taipei 100, Taiwan
Department of Dermatology, Cathay General Hospital,
Taipei, Taiwan
Department of Dermatology, Yun-Lin Branch,
National Taiwan University Hospital, Taipei, Taiwan
Correspondence: Ruey-Jien Chen and Sung-Jan Lin.
E-mail: rjchen@ha.mc.ntu.edu.tw; sjlin@ha.mc.ntu.edu.tw
References
1 Iorizzo M, Vincenzi C, Voudouris S et al. Finasteride treatment of
female pattern hair loss. Arch Dermatol 2006; 142:298302.
2 Shum KW, Cullen DR, Messenger AG. Hair loss in women with
hyperandrogenism: four cases responding to nasteride. J Am Acad
Dermatol 2002; 47:7339.
3 Kaufman KD, Oslen EA, Whiting D et al. Finasteride in the treatment
of men with androgenetic alopecia. J Am Acad Dermatol 1998;
39:57888.
4 Price VH, Roberts JL, Hordinsky M et al. Lack of efcacy of naster-
ide in postmenopausal women with androgenetic alopecia. J Am Acad
Dermatol 2000; 43:76876.
5 Camacho F. Hirsutismo: enfoque clinico terapeutico. Act Terap
Dermatol 2001; 24:190206.
6 Trueb RM, Swiss Technology Study Group. Finasteride treatment of
patterned hair loss in normoandrogenic postmenopausal women.
Dermatology 2004; 209:2027.
7 Olszewska M, Rudnicka L. Effective treatment of female androgenic
alopecia with dutasteride. J Drugs Dermatol 2005; 4:63740.
8 Dimitrakakis C, Zhou J, Wang J et al. A physiologic role for testo-
sterone in limiting estrogenic stimulation of the breast. Menopause
2003; 10:2928.
9 Papasozomenos SC, Shanavas A. Testosterone prevents the heat
shock-induced overactivation of glycogen synthase kinase-3 beta but
not of cyclin-dependent kinase 5 and c-Jun NH
2
-terminal kinase
and concomitantly abolishes hyperphosphorylation of tau: implica-
tions for Alzheimers disease. Proc Natl Acad Sci USA 2002; 99:
11405.
Conicts of interest: none declared.
Immunohistochemical characterization of
elastobroma and exclusion of ABCC6 as a
predisposing gene
DOI: 10.1111/j.1365-2133.2006.07735.x
SIR, Elastobroma (EF) is a subcutaneous broelastic pseudo-
tumour that usually presents in adulthood at the lower end of
the subscapular space. Microscopy reveals adipose tissue, bun-
dles of collagen interspersed with dystrophic (globular or bea-
ded) elastic bres, and spindle-shaped cells dispersed in the
connective tissue.
1
Multiple and familial EF have been repor-
ted, supporting the possibility of a hereditary predisposition.
2
We carried out an immunohistochemical study of EF to char-
acterize further the elastic bres and cells, and a mutation
analysis of ABCC6, the gene responsible for pseudoxanthoma
elasticum (PXE). One recent paper reported a patient with two
EFs and PXE, and questioned a genetic link between both rare
conditions with dystrophic elastic bres.
3
Four EF tumours from three unrelated patients were inclu-
ded in the study. All individuals gave informed consent for
search for ABCC6 mutations. The EF sections were incubated
with antibodies against actin, desmin, vimentin, elastin,
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 755
O
r
c
V
i
m
S
i
a
F
b
n
O
s
t
E
l
a
V
i
t
A
c
t
D
e
s
F
i
g
1
.
O
r
c
e
i
n
(
O
r
c
)
s
t
a
i
n
i
n
g
a
n
d
i
m
m
u
n
o
l
a
b
e
l
l
i
n
g
o
n
e
l
a
s
t
o
b
r
o
m
a
.
O
r
c
s
t
a
i
n
i
n
g
r
e
v
e
a
l
e
d
d
y
s
t
r
o
p
h
i
c
b
e
a
d
e
d
e
l
a
s
t
i
c
b
r
e
s
(
o
r
i
g
i
n
a
l
m
a
g
n
i
c
a
t
i
o
n
1
0
0
)
.
N
e
g
a
t
i
v
e
a
c
t
i
n
(
A
c
t
)
a
n
d
d
e
s
m
i
n
(
D
e
s
)
s
t
a
i
n
i
n
g
r
u
l
e
d
o
u
t
t
h
e
h
y
p
o
t
h
e
s
i
s
t
h
a
t
s
p
i
n
d
l
e
-
s
h
a
p
e
d
c
e
l
l
s
a
r
e
m
y
o
b
r
o
b
l
a
s
t
s
.
V
i
m
e
n
t
i
n
(
V
i
m
)
w
a
s
p
o
s
i
t
i
v
e
o
n
s
p
i
n
d
l
e
-
s
h
a
p
e
d
c
e
l
l
s
.
E
l
a
s
t
i
n
(
E
l
a
)
a
n
d
v
i
t
r
o
n
e
c
t
i
n
(
V
i
t
)
l
a
b
e
l
l
i
n
g
w
a
s
s
t
r
o
n
g
l
y
p
o
s
i
t
i
v
e
i
n
e
l
a
s
t
i
c
b
r
e
s
.
B
o
n
e
s
i
a
l
o
p
r
o
t
e
i
n
(
S
i
a
)
l
a
b
e
l
l
i
n
g
w
a
s
s
t
r
o
n
g
l
y
p
o
s
i
t
i
v
e
i
n
b
r
o
b
l
a
s
t
c
y
t
o
p
l
a
s
m
,
a
n
d
o
n
l
y
m
o
d
e
r
a
t
e
a
n
d
p
a
t
c
h
y
o
n
e
l
a
s
t
i
c
b
r
e
s
.
N
o
s
i
g
n
i
c
a
n
t
s
t
a
i
n
i
n
g
w
a
s
s
e
e
n
w
i
t
h
b
r
o
n
e
c
t
i
n
(
F
b
n
)
o
r
o
s
t
e
o
n
e
c
t
i
n
(
O
s
t
)
(
o
r
i
g
i
n
a
l
m
a
g
n
i
c
a
t
i
o
n
2
0
0
)
.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
756 Correspondence
brillin-1, vitronectin, bronectin, bone sialoprotein and
osteonectin. Von Kossa staining and immunolabellings were
performed simultaneously on control biopsy sections of nor-
mal young skin and skin conditions with elastic tissue dys-
trophy (PXE, solar elastosis), and read by two independent
observers. Mutation detection was performed as previously
published.
4
Von Kossa staining was positive on PXE sections but nega-
tive on EF and other samples. The labellings were identical in
all EFs (Fig. 1). Actin and desmin were negative in connective
tissue areas and in spindle-shaped cells. Vimentin was positive
on the latter cells. Elastin was strongly positive on elastic
bres. No signicant staining was seen with the antibrillin-1
antibody. Vitronectin was strongly positive on elastic bres
with patchy reinforcement. Bone sialoprotein was strongly
positive in cell cytoplasm, and only patchy on EF elastic bres.
No signicant staining was seen with antibronectin or anti-
osteonectin antibodies. The immunolabelling prole was sim-
ilar overall to that observed in PXE (Fig. 2) and elastotic skin
samples, but not to that of healthy skin (not shown). Indeed,
vitronectin was strongly positive on elastotic samples and to a
lesser extent only on elastic bres in young skin. Bone sialo-
protein and osteonectin were absent in young skin dermis but
were present to a slight extent in broblasts and in the elasto-
tic material. ABCC6 gene mutation detection did not reveal any
sequence variation in the three patients.
The present study extends the characterization of EF. EF
elastic bres do contain elastin, but the presence of brillin-1
was not demonstrated. Elastorrhexis is absent and von Kossa
staining is negative in EF. It has been hypothesized that aber-
rant accumulation of vitronectin, bone sialoprotein and osteo-
nectin was responsible for the mineralization of the elastic
bres in PXE.
5
The unique responsibility of these matrix
glycoproteins is questionable as we notice here a similar
immunohistochemical prole for dystrophic elastic bres and
cells in EF, elastosis and PXE. Several hypotheses may be pro-
posed to resolve this discrepancy. Firstly, elastorrhexis might
be a long-term process that is not fully completed in acquired
conditions such as EF or elastosis. Secondly, the mineralization
in PXE may be specically due to osteonectin and/or other
still unrecognized molecules that are absent in EF bres.
Lastly, PXE patient serum lacks fetuin-A, a systemic inhibitor
of mineralization.
6
Bone sialoprotein has been shown to be
associated with vascular calcication in patients with end-stage
Ela
Ost
Vit
Sia
Fig 2. Immunolabelling on pseudoxanthoma elasticum skin samples. Elastorrhexic bres were strongly positive for elastin (Ela) and vitronectin
(Vit), and to a lesser extent only for osteonectin (Ost) and bone sialoprotein (Sia). Dermal broblasts were strikingly positive for Sia (original
magnication 200).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 757
renal disease,
7
but the latter also have low serum fetuin-A lev-
els. Therefore it may be hypothesized that a common process
exists that determines skin (and vascular) elastic bre dystro-
phy. This process includes the biosynthesis by connective tis-
sue cells of glycoproteins with afnity for calcium salts in
response to various stimuli (e.g. mechanical stress, ultraviolet
irradiation), but mineralization is not constant. Systemic
and/or local promotion of mineralization could represent
second hits and critical differences between EF and PXE.
Here no EF cells stained positively for desmin or actin: they
are not myobroblasts but have immunohistochemical features
evocative of osteoblast differentiation. The histogenesis of EF
remains controversial. Recent cytogenetic ndings evidencing
chromosomal instability and/or clonal changes suggest a neo-
plastic process.
8
However, the location of the tumours in areas
prone to repetitive mechanical trauma also supports a reac-
tive process. Abnormal admixture of microbril glycoproteins
could affect elastic bre formation.
1
Interestingly, abnormal
elastogenesis has also recently been suspected for PXE.
9
Histo-
genesis may also be in favour of acquired degeneration of
elastic bres. The presence within EF of lysozyme, that is
regarded as a useful marker of damage to elastic bres, has
also been identied in the lesions of PXE and elastosis.
10
In
this setting of complex disturbance of elastic brillogenesis,
the importance of a predisposing genetic background remains
to be determined. We can assume that there are no germinal
ABCC6 mutations in patients with EF.
Acknowledgments
We thank Jacques Jourdas for technical assistance, and Vincent
Pasquier for help in artwork.
M. NAOURI
P. MI CHE NE T*
N. CHAS S AI NG
L. MART I N
Departments of Dermatology and *Pathology,
Hopital Porte-Madeleine, CHR dOrle ans, BP 2439,
F-45032 Orle ans cedex, France
Department of Genetics,
CHU Purpan, Toulouse, France
Correspondence: L. Martin.
E-mail: ludovic.martin@chr-orleans.fr
References
1 Enzinger FM, Weiss SW. Benign brous tissue tumors. In: Enzinger
and Weisss Soft Tissue Tumors (Weiss SW, Goldblum JR, eds), 4th edn.
St Louis: Mosby, 2001; 2869.
2 Nagamine N, Nohara Y, Ito E. Elastobroma in Okinawa. A clinico-
pathologic study of 170 cases. Cancer 1982; 50:1794805.
3 Belgnaoui F, Bensahraoui M, Hannoud S et al. [Pseudoxanthoma
elasticum and elastobroma. Is there a link?]. Ann Dermatol Venereol
2005; 132:5646 (in French).
4 Chassaing N, Martin L, Mazereeuw J et al. Novel ABCC6 muta-
tions in pseudoxanthoma elasticum. J Invest Dermatol 2004; 122:
60813.
5 Baccarani-Contri M, Boraldi F, Taparelli F et al. Matrix proteins with
high afnity for calcium ions are associated with mineralization
within the elastic bers of pseudoxanthoma elasticum dermis. Am J
Pathol 1996; 148:56977.
6 Hendig D, Schulz V, Arndt M et al. Role of serum fetuin-A, a major
inhibitor of systemic calcication, in pseudoxanthoma elasticum.
Clin Chem 2006; 52:22734.
7 Chen NX, Moe SM. Vascular calcication in chronic kidney disease.
Semin Nephrol 2004; 24:618.
8 Hisaoka M, Hashimoto H. Elastobroma: clonal brous prolifer-
ation with predominant CD-34 positive cells. Virchows Arch 2005;
17:15.
9 Le Saux O, Bunda S, van Wart C et al. Serum factors from pseudo-
xanthoma elasticum patients alter elastic ber formation in vitro.
J Invest Dermatol 2006; 126:1497505.
10 Albrecht S, From L, Kahn HJ. Lysozyme in abnormal dermal elastic
bers of cutaneous aging, solar elastosis and pseudoxanthoma
elasticum. J Cutan Pathol 1991; 18:7580.
Conicts of interest: none declared.
The efcacy of tetracycline antibiotics for
treatment of lichen planus: an open-label
clinical trial
DOI: 10.1111/j.1365-2133.2006.07733.x
SIR, Lichen planus (LP) is an inammatory condition which
may involve skin, hair and mucosa. Although its exact patho-
genesis remains unknown, LP probably results from a cell-
mediated immunological response to an unidentied antigen
processed by Langerhans cells.
1
In this type IV hypersensitivity
response, epidermotropic T lymphocytes are stimulated to
attack keratinocytes, releasing cytokines that perpetuate the
lichenoid tissue reaction and eventual epidermal destruction.
2
Classically, a band-like inltrate of lymphocytes, histiocytes
and Langerhans cells disrupts the dermalepidermal junction.
3
Therapies for cutaneous LP are limited by short-term ef-
cacy, toxicity and inconvenience. Severe LP responds to retin-
oids and immunosuppressive agents, but chronic use is often
required.
4
Some patients may benet from psoralen and ultra-
violet A, although high relapse rates upon discontinuation were
reported.
5,6
These and other limitations underscore the need
for novel LP treatments with improved side-effect proles.
The anti-inammatory properties of tetracycline antibiotics
have previously been studied, with recent evidence pointing to
a mechanism involving antibiotic-mediated inhibition of the
T-lymphocyte response.
7
To date, however, nostudies have deter-
mined the utility of tetracyclines for treatment of cutaneous LP,
although one case report described the efcacy of topical tetra-
cycline for erosive oral LP,
8
and another showed improvement
of lichen planus pemphigoides after treatment with tetracycline
and nicotinamide.
9
We therefore initiated an open-label pilot
study, investigating the role of tetracycline antibiotics for the
treatment of LP, hypothesizing that a dampening of this patho-
logically robust lymphocytic response may be achieved.
The study was approved by the Research and Human Sub-
jects Review Committee of Santa Clara Valley Medical Center.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
758 Correspondence
Informed consent was obtained from all participating subjects.
Inclusion criteria were the presence of active biopsy-proven LP
and age over 18 years. Some subjects refused biopsy but were
included if classic LP was discovered on physical examination.
Women were allowed to participate if they were postmeno-
pausal, practising abstinence, or using a documented form of
birth control during the entire study period. Exclusion criteria
were tetracycline allergy, pregnancy, breast-feeding, women
of child-bearing age not using appropriate contraception, and
patients on oral immunosuppression.
Fifteen subjects were enrolled. They were treated with tetra-
cycline 500 mg or doxycycline 100 mg, both twice daily. All
adverse events were recorded and subjects followed monthly
until their LP cleared or for 6 months after therapy initiation.
At each visit, the size and lesion number were evaluated to
determine the response to treatment. Complete remission des-
cribed those patients whose initial lesions and pruritus resolved.
Partial response was less than total clearing, but at least a 25%
regression of skin lesions and pruritus. Nonresponders inclu-
ded those with disease progression or < 25% improvement.
All statistical calculations were performed using Microsoft Excel.
Thirteen of 15 enrolled subjects completed the open-label
study (Table 1). Two male subjects were lost to follow-up after
the initial visit and were not included in the analysis. The age
range spanned 3179 years (mean 54). Study demographics
are summarized in Table 1. The mean disease duration was
13 months (range 230). Hepatitis C virus status was negative
for six of 13 (46%) study subjects, undetermined in six, and
positive in one (data not shown). The distribution of primary
lesions was variable and biopsy conrming the diagnosis of LP
was available in nine of 13 (69%) subjects.
Of the 13 subjects who completed the study, six (46%)
reported no response to either doxycycline or tetracycline
(Table 1). Six of 13 (46%) subjects reported a partial response,
while only one patient experienced a complete remission
(Table 1). Although the sample size was small, the rate of
response for subjects on monotherapy with tetracycline (two of
four) was similar to that of those on doxycycline (ve of eight).
No correlation was found between length of therapy and ef-
cacy (data not shown). The mean treatment period for respond-
ers was 36 months (range 16) compared with a mean of
30 months (range 15) for nonresponders, with a mean fol-
low-up period of 35 months. Although a correlation between
distribution of primary lesions and efcacy of treatment was
not clinically observed during follow-up visits, no rm conclu-
sions could be reached in our study due to small sample size.
Overall, both doxycycline and tetracycline were well tolerated,
with no serious adverse events reported. Three subjects reported
a total of four nonserious adverse events (Table 1).
Tetracyclines possess several nonantibiotic properties and
have recently been found effective therapies for bullous pem-
phigoid and sarcoidosis.
7
Although we expected that LP might
similarly respond to antibiotics, the results from this small,
open-label pilot study were disappointing. The complete
response observed in only one of our 13 patients treated
with tetracycline or doxycycline would be expected from the
natural disease course, where spontaneous remittance after
months to years is common.
Partial responses shown in open-label studies may fre-
quently be the result of both patient and investigator bias.
Several promising therapies based on positive results from
early open-label studies fail to hold up to the scrutiny of
well-controlled double-blind studies. The disappointing results
of tetracycline and doxycycline as therapeutic agents in our
patients with LP do not appear to warrant the undertaking of a
larger double-blind trial.
Acknowledgments
We thank Joanna L. Chan, MD, for her help in manuscript
preparation.
B. M. HANTAS H*
M. H. KANZ L E R*
*Department of Dermatology,
Stanford University School of Medicine,
257 Campus Drive, Stanford, CA 94305, U.S.A.
Division of Dermatology, Santa Clara
Valley Medical Center, San Jose, CA, U.S.A.
E-mail: bhantash@stanford.edu
References
1 Scully C, Beyli M, Ferreiro MC et al. Update on oral lichen planus:
etiopathogenesis and management. Crit Rev Oral Biol Med 1998; 9:86
122.
Table 1 Patient demographics, study distribution, and adverse events
Number of patients enrolled 15
Completed study
a
13
Age (years), range 3179
Age (years), mean SD 54 15
Gender
Male 4
Female 9
Race
African 1
Asian 4
Caucasian 3
Hispanic 5
Disease duration
Range (months) 230
Mean SD (months) 13 10
Response prole
None 6
Partial 6
Complete 1
Adverse events
b
Diarrhoea
c
1
Dyspepsia 1
Taste disturbance 1
Loss of appetite 1
a
Two of 15 enrollees were lost to follow-up.
b
Adverse events
were recorded in three of 13 subjects.
c
Diarrhoea with tetra-
cycline, remaining with doxycycline.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 759
2 Boyd AS, Neldner KH. Lichen planus. J Am Acad Dermatol 1991;
81:294319.
3 Akasu R, From L, Kahn HJ. Lymphocyte and macrophage subsets in
active and inactive lesions of lichen planus. Am J Dermatopathol 1993;
15:21723.
4 Cribier B, Frances C, Chosidow O. Treatment of lichen planus. An
evidence-based medicine analysis of efcacy. Arch Dermatol 1998;
134:152130.
5 Karvonen J, Hannuksela M. Long term results of topical trioxsalen
PUVA in lichen planus and nodular prurigo. Acta Derm Venereol (Stockh)
1985; 120:535.
6 Helander I, Jansen CT, Meurman L. Long-term efcacy of PUVA
treatment in lichen planus: comparison of oral and external meth-
oxsalen regimens. Photodermatology 1987; 4:2658.
7 Sapadin AN, Fleischmajer R. Tetracyclines: nonantibiotic properties
and their clinical implications. J Am Acad Dermatol 2006; 54:25865.
8 Walchner M, Messer G, Salomon N et al. Topical tetracycline treat-
ment of erosive oral lichen planus. Arch Dermatol 1999; 135:923.
9 Fivenson DP, Kimbrough TL. Lichen planus pemphigoides: combin-
ation therapy with tetracycline and nicotinamide. J Am Acad Dermatol
1997; 36:63840.
Conicts of interest: none declared.
Multiple huge cutaneous horns overlying
verrucae vulgaris induced by human
papillomavirus type 2: a case report
DOI: 10.1111/j.1365-2133.2006.07734.x
SIR, We report a patient from a town in rural China who had
multiple huge cutaneous horns overlying verrucae vulgaris.
A 41-year-old man had had numerous wart-like skin lesions
on his hands and feet for more than 30 years and numerous
horny excrescences for 8 years. He was admitted to the
Department of Dermatology, ChinaJapan Friendship Hospital,
in June 2005. In 1972, he had noticed a single warty lesion
on the dorsum of his right foot. The lesions gradually grew
in size and increased in number and involved all four
extremities. He had worked as a pig butcher from 1979 to
1990. The older lesions ultimately changed into elongated,
hard, horn-like projections. None of his family members had
a similar disorder. Physical examination did not reveal any
abnormality. Dermatological examination revealed several
hundred dense and conuent, huge, hard cutaneous horns on
both hands and feet. The horns ranged from 05 to 5 cm in
diameter, and from 05 to 21 cm in length. The horns were
dull yellowish brown in colour, with a vertical ridge
(Fig. 1a). Laboratory tests revealed only slightly elevated
alanine aminotransferase (66 IU L
)1
, normal 040) and a
slight decrease in natural killer cells (170 cells mm
)3
, normal
175567). X-ray showed marked absorption of the terminal
phalanges, narrowed joint spaces of wrist and ankle, and
thinning of bone cortex in the metacarpals and metatarsals
(Fig. 1b).
Lesional skin biopsy revealed hyperkeratosis, parakeratosis
and acanthosis of the epidermis. There were groups of vacuo-
lated cells in the granular layer and upper stratum spinosum.
(a)
(b)
Fig 1. (a) Clinical appearance before treatment: horns over the right
hand and sporadic common warts on the right hand and right foot.
(b) X-ray of the right hand, showing dense horns in the ngertips
and absorption of the terminal phalanges.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
760 Correspondence
The nuclei of vaculated cells were round, very deeply baso-
philic, and surrounded by a clear zone. Marked mononuclear
cell inltration, angiogenesis and vasodilation were observed
in the dermis (Fig. 2).
Total DNA was extracted from lesional tissue. A polymerase
chain reaction (PCR) screening methodology for human papillo-
mavirus (HPV) types 150 was applied: only the preparation
using HPV-2-specic primers gave an amplied band. BLAST
sequencing results showed that this 372-bp PCR fragment
shared 100% identity with HPV-2a reference strain
(NC_001352). Complete viral genome sequencing showed
overall identity of 9958% with the HPV-2a reference strain,
indicating an HPV-2a variant. In addition to some nonsynony-
mous mutations, several variations have been identied in this
strain, including amino acid (aa) 56 changing from Val to
Ala, aa 185 from Ala to Thr and aa 190 from Thr to Asn
within E1 open reading frame (ORF); aa 190 changing from
Thr to Ala, aa 235 from Ser to Pro, aa 287 from Tyr to His
and aa 293 from Ser to Arg within E2 ORF; aa 84 changing
from Val to Gly within E4 ORF; aa 275 changing from Leu to
Arg within L1 ORF; and a histidine insertion between the
39th and 40th aa of E7 ORF.
Our patient was treated with tretinoin (acitretin) 40 mg
daily and interferon alfa-2b 5 10
6
U 3 days per week for
1 month. The bases of the cutaneous horns became soft and
clear. The cutaneous horns were removed surgically. Treatment
was continued with the same dosages of acitretin and inter-
feron alfa-2b described above. Electron beam radiation or
X-irradiation were applied for local lesions, in which the hands
were treated ve times over 3 weeks with 20 MeV electron
beam radiation at a total dosage of 2000 cGy, while the feet
were treated ve times over 3 weeks with 6 MV X-irradiation
at a total dosage of 400 cGy each time. The lesions began
to improve markedly 3 months after radiation therapy. The
functions of the hands and feet have gradually recovered. At
follow-up, 1 year after discharge from hospital, physical and
X-ray examinations showed almost normal appearance of the
hands (Fig. 3). His normal daily activity ultimately recovered.
Cutaneous horn is produced because of unusual cohesive-
ness of keratinized material. It has been reported in a man
who had seven swellings on the scalp, with the largest horn
35 cm in circumference and 20 cm long.
1
The majority of
cutaneous horns occurring over the scalp originated from
sebaceous cysts. The authors, however, assigned this term spe-
cically to those cases which had a keratin mass above the
skin surface projecting for at least 10 mm or at least as high as
its width. Cutaneous horns may be benign,
1
premalignant
1,2
Fig 2. Histopathology. (a) At low magnication, showing typical
hyperkeratosis, acanthosis and papillomatosis. The rete ridges elongate
and bend inwards at both margins and appear to point radially
towards the centre. (b) At high magnication, groups of large,
vacuolated cells lie in the upper stratum malpighii and in the granular
layer. A tier of parakeratotic cells lies over the crest of a papillomatous
elevation. Haematoxylin and eosin; original magnication: (a) 16,
(b) 160.
(b)
Fig 3. (a) Clinical appearance and (b) X-ray of the hands at
18 months after therapy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 761
or malignant (squamous cell carcinoma).
13
The cutaneous
horns in the present report probably originated from long-
standing verruca vulgaris lesions. It had been widely accepted
that the horn arising from an exaggerated verruca vulgaris sel-
dom reaches a height of 05 cm, but the horns in this case
were exceptionally large, with the longest one reaching
21 cm, possibly indicating very special individual features.
Verrucae vulgaris (skin warts) are kinds of benign prolifer-
ating lesions in epithelia, often on hands, and are usually
caused by HPV infection. The present case contained intact
HPV-2a genome sequences, which may present in episomal
form. Whole genome alignment analyses of this isolate
revealed very high homology with the HPV-2a prototype.
Although several mutations have been identied in various
regions, e.g. in E1, E7 and the long control region (LCR),
even a nucleotide exchange in the potential E2 binding site in
the LCR, it is hard simply to ascribe the presence of multiple
horns to virus infection, as none of our patients family
members or close contacts appeared to have a similar disorder
during a period exceeding 30 years.
Although it has been reported that HPV-2-related warts
respond only modestly to treatment, as they persisted in
approximately 50% of all patients for more than 6 additional
months,
4
the patient infected with HPV-2a in this study was
successfully cured with a combined therapeutic protocol of
systemic administration of tretinoin (acitretin) and interferon
alfa-2b, and local irradiation with X-rays or electron beams.
No recurrence of warts on the extremities or trunk has been
observed. Radiation may directly suppress active epidermal
proliferation. Tretinoin inhibits hyperkeratosis of epidermis,
induces growth arrest of actively proliferating epidermal cells
and increases the sensitivity of HPV-infected cells to radi-
ation.
5
Although the mechanism of appearance of hundreds of
horns in this case still remains unknown, the combined use of
antiviral agents and physical and chemical inhibitors of epithe-
lial proliferation seemed to be effective in removing the infec-
ted lesions and in preventing recurrence.
WANG CHE N
WANG WE I *
LE I YAN- J UN
WANG J I - YI NG
DONG XI AO- PI NG
WANG J I AN*
SHE NG RUI - HONG
PAN ZI - ANG
ZHU WE N- YUAN
YOU LI - PI NG
PE NG HONG- XI A
XU XI N- YE
ChinaJapan Friendship Hospital,
Beijing 100029, China
*Beijing Genomics Institute, Chinese
Academy of Sciences, Beijing, China
State Key Laboratory for Infectious
Disease Prevention and Control,
National Institute for Viral Disease
Control and Prevention, Chinese Center for
Disease Control and Prevention,
Beijing, China
The First Afliated Hospital, Nanjing
Medical University, Nanjing, China
The Second Hospital, Liangshan
Administrative Division of Sichuan
Province, Sichuan, China
Health Department, Peking University,
Beijing, China
E-mail: xyxumail@sina.com.cn
References
1 Thappa DM, Garg BR, Thadeus J, Ratnakar R. Cutaneous horn: a
brief review and report of a case. J Dermatol 1997; 24:347.
2 Melchers W, de Mare S, Kuitert E et al. Human papillomavirus and
cutaneous warts in meat handlers. J Clin Microbiol 1993; 31:25479.
3 Phelps WC, Barnes JA, Lobe DC. Molecular targets for human
papillomaviruses: prospects for antiviral therapy. Antivir Chem Chemo-
ther 1998; 9:35977.
4 Rubben A, Kalka K, Spelten B, Grussendorf-Conen EI. Clinical fea-
tures and age distribution of patients with HPV 2/27/57-induced
common warts. Arch Dermatol Res 1997; 289:33740.
5 Faluhelyi Z, Rodler I, Csejtey A et al. All-trans retinoic acid (ATRA)
suppresses transcription of human papillomavirus type 16 (HPV16)
in a dose-dependent manner. Anticancer Res 2004; 24:8079.
Conicts of interest: none declared.
Subcutaneous phaeohyphomycosis caused by
Exophiala oligosperma in a renal transplant
recipient
DOI: 10.1111/j.1365-2133.2006.07732.x
SIR, Phaeohyphomycosis encompasses a heterogeneous group
of infections caused by dematiaceous (darkly-pigmented)
fungi, which grow in tissue as hyphae, pseudohyphae or
yeast-like forms. They have been classied as: (i) supercial,
(ii) cutaneous and corneal, (iii) subcutaneous and (iv) system-
ic forms.
1
The aetiological agents of phaeohyphomycosis are
numerous species belonging to different genera such as Alternaria,
Phialophora and Exophiala, among others.
2
We report an unusual
case of subcutaneous phaeohyphomycosis caused by the
recently recognized species Exophiala oligosperma.
3
A 72-year-old woman presented in March 2005 with a
3-month history of progressive, asymptomatic cutaneous
lesions on her right leg. She did not recall having any previous
injury of that area. The patient had undergone renal trans-
plantation 7 years previously. She was receiving immunosup-
pressive therapy with mycophenolate mofetil 500 mg daily,
prednisone 15 mg daily and tacrolimus 1 mg daily.
Examination revealed multiple, tender, reddish-brown sub-
cutaneous nodules measuring 0.51 cm in diameter grouped
in the affected zone (Fig. 1). There was no lymphadenopathy.
A skin biopsy specimen was obtained for histopathological
study and microbiological cultures. The histopathology
revealed a suppurative granulomatous inammation in the deep
dermis and hypodermis composed of lymphocytes, epithelioid
macrophages, multinucleated giant cells and aggregations of
neutrophils in the centre of the granulomas (Fig. 2a). Periodic
acid-Schiff (PAS) stain showed round-shaped fungal structures
within a clear space in the cytoplasm of some giant cells, asso-
ciated with extracellular fungal hyphae (Fig. 2b). Polymerase
chain reaction (PCR)enzyme-linked immunosorbent assay
(ELISA) for the IS6110 gene region of Mycobacterium tuberculosis
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
762 Correspondence
was negative. Cultures for bacteria and acid-fast bacilli were
both sterile. Fungal cultures were performed on Sabouraud chl-
oramphenicol agar and Sabouraud chloramphenicol cyclohexi-
mide agar (Bio-Rad, Hercules, CA, U.S.A.), and incubated at
30 C. After 10 days of incubation, velvety colonies developed
on all media which were oliveblack with a blackish reverse.
Microscopic examination of these colonies revealed brown
septate hyphae, annellidic conidiogenous cells and oval conidia.
Molecular identication was performed by amplication and
sequencing of the internal transcribed spacer (ITS) region
dened by primers ITS5 and ITS4 (incorporating ITS1, the 5.8S
gene and ITS2). The sequence obtained (552 bp) was com-
pared with those in the GenBank DNA database. This sequence
showed a 98% similarity with a strain of E. oligosperma misiden-
tied as Exophiala jeanselmei (accession no. AJ866273).
A diagnosis of subcutaneous phaeohyphomycosis due to
E. oligosperma was made. The patient was treated with itracona-
zole 100 mg twice daily over a period of 3 months, without
observing any interaction with tacrolimus. An improvement
was observed after the second week, which led to complete
resolution of the lesions. No recurrences have been observed
after 15 months of follow-up.
Exophiala organisms are ubiquitous dematiaceous fungi found
in soil, wood and plant matter.
4
They are saprophytic but may
(a)
(b)
Fig 2. (a) The skin biopsy showed a suppurative granulomatous
inammation in the deep dermis and hypodermis composed of
lymphocytes, epithelioid macrophages, multinucleated giant cells and
aggregated of neutrophils in the centre of the granulomas (Periodic
acid-Schiff staining; original magnication 100). (b) Presence of
round-shaped fungal structures in the centre of a clear space in the
cytoplasm of some giant cells (Periodic acid-Schiff staining; original
magnication 1000).
Fig 1. Multiple red-brown nodular lesions on the posterior aspect of
the right leg.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 763
cause human infections, particularly in immunocompromised
hosts.
5
The predominant clinical manifestations due to Exophiala
species are cutaneous and subcutaneous infections. The most
common pathogenic Exophiala species is E. jeanselmei,
68
although
others such as Exophiala dermatitidis,
9
Exophiala spinifera and Exophi-
ala pisciphila have also been implicated.
2,4,5
We report here a case
of subcutaneous phaeohyphomycosis caused by E. oligosperma.
This recently recognized species has been identied as a causal
agent of human keratitis, olecranon bursitis and mycetoma,
among others.
3,10
As far as we know, however, subcutaneous
phaeohyphomycosis due to this rare species has not been docu-
mented previously.
Subcutaneous phaeohyphomycosis usually presents as an
asymptomatic, solitary nodule or abscess, usually located on
an extremity. The infection commences as a small nodule that
enlarges over time and may develop a pseudocapsule, giving a
cyst-like appearance (phaeohyphomycotic cyst).
8
It has rarely
been reported as multiple lesions.
6
In this context, it is note-
worthy that in our case there was a cluster of inammatory
nodular lesions. In our patient, the inoculation mechanism of
the fungus is unknown. In other cases a history of prior
trauma with splinters or other contaminated material occurred
months before the appearance of the lesions.
4
Seeing that the
clinical features are nonspecic, subcutaneous phaeohypho-
mycosis may be confused with other entities and a high index
of suspicion is required for early diagnosis.
The histopathological picture is characterized by a granulo-
matous inltrate, sometimes encapsulated by brous tissue.
4,8
Diagnosis depends on visualization of hyphal or yeast-like ele-
ments in tissue, and should be conrmed by isolation on cul-
ture and the morphological identication of the causal fungus.
Moreover, differentiation down to the species level is recom-
mended, as different species may have a different virulence or
resistance to antifungal therapy.
2
E. oligosperma has a colony
morphology similar to those of E. jeanselmei and E. spinifera,
with an oliveblack colour, a black reverse and a velvety
appearance.
10
In our case, identication of the causative agent
E. oligosperma was achieved by sequencing of the rDNA ITS
domain.
The optimum treatment for subcutaneous phaeohypho-
mycosis is still not standardized, although surgical excision is
considered to be the treatment of choice when dealing with
solitary, well-delimited lesions.
7,8
Numerous systemic antifun-
gal therapies have been employed with variable responses.
Among these, it appears that itraconazole is the most effective
therapy.
7
Our patient was successfully treated with this agent.
M. A. GONZ A
L E Z - LO
P E Z
R. SAL E S A*
M. C. GONZ A
L E Z - VE L A
H. FE RNA
NDE Z - LL ACA
J . F. VAL - BE RNAL
J . CANO
Departments of Dermatology,
*Microbiology and
Pathology, Hospital Universitario Marque s
de Valdecilla, Santander
Unit of Microbiology, Facultat de
Medicina i Cie ncies de la Salut, Universitat
Rovira i Virgili, Reus, Tarragona, Spain
Correspondence: J. Fernando Val-Bernal.
E-mail: apavbj@humv.es
References
1 Fader RC, McGinnis MR. Infections caused by dematiaceous fungi:
chromoblastomycosis and phaeohyphomycosis. Infect Dis Clin North
Am 1988; 2:92538.
2 De Hoog GS, Guarro J, Gene J, Figueras MJ. Atlas of Clinical Fungi,
2nd edn. Utrecht: Centraal bureau voor Schimmelcultures and
Reus: Universitat Rovira i Virgili, 2000.
3 De Hoog GS, Vicente V, Caligiorne RB et al. Species diversity and
polymorphism in the Exophiala spinifera clade containing opportunis-
tic black yeast-like fungi. J Clin Microbiol 2003; 41:476778.
4 Sudduth EJ, Crumbley AJ III, Farrar WE. Phaeohyphomycosis due
to Exophiala species: clinical spectrum of disease in humans.
Clin Infect Dis 1992; 15:63944.
5 Singh N, Chang FY, Gayowski T, Marino IR. Infections due to
dematiaceous fungi in organ transplant recipients. Case report and
review. Clin Infect Dis 1997; 24:36974.
6 Ukim HU, Kang SH, Matsumoto T. Subcutaneous phaeohypho-
mycosis caused by Exophiala jeanselmei in a patient with advanced
tuberculosis. Br J Dermatol 1998; 138:3513.
7 Monbrison F, Piens MA, Ample B et al. Two cases of subcutaneous
phaeohyphomycosis due to Exophiala jeanselmei in cardiac transplant
and renal transplant recipients. Br J Dermatol 2004; 150:5978.
8 Xu X, Low DW, Palevsky HI, Elenitsas R. Subcutaneous phaeo-
hyphomycotic cysts caused by Exophiala jeanselmei in a lung transplant
recipient. Dermatol Surg 2001; 27:3436.
9 Woollons A, Darley CR, Pandian S et al. Phaeohyphomycosis caused
by Exophiala dermatitidis following intra-articular steroid injection. Br J
Dermatol 1996; 135:4757.
10 Bossler AD, Richter SS, Chavez AJ et al. Exophiala oligosperma causing
olecranon bursitis. J Clin Microbiol 2003; 41:477982.
Conicts of interest: none declared.
Bullous eosinophilic cellulitis associated with
ulcerative colitis: effective treatment with
sulfasalazine and glucocorticoids
DOI: 10.1111/j.1365-2133.2006.07729.x
SIR, A 42-year-old white man presented with tense blisters that
had developed on erythematous macules and plaques the day
before (Fig. 1). He complained of burning and itching coinci-
ding with gastrointestinal symptoms and reported that he had
had repeated urticarial rashes for several years. He had a history
of ulcerative colitis that had been diagnosed 10 years previously.
The ulcerative colitis was treated with methylprednisolone 10 mg
daily, azathioprine 100 mg daily and mesalazine 1 g daily.
Skin biopsy from the lower left arm showed subepidermal
blister formation, oedema of dermis and subcutis (Fig. 2a)
and a dense inammatory inltrate consisting of eosinophils,
neutrophils, lymphocytes and mononuclear cells. Furthermore,
foci of degenerated necrotic collagen bres and degranulating
eosinophils were apparent. The granular material focally
aggregated around collagen bres and showed a tendency
to form ame gures (Fig. 2b). No parasites, vasculitis or
granuloma formation were detectable on histological examin-
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
764 Correspondence
ation. Direct immunouorescence microscopy was negative.
Laboratory tests revealed thrombocytosis (511 10
9
L
)1
),
leucocytosis (119 10
9
L
)1
) and elevated C-reactive protein
(146 mg L
)1
). Indirect immunouorescence using monkey
oesophagus and NaCl-split skin as substrates showed no circu-
lating IgG or IgA autoantibodies. Ultrasound of the abdomen,
chest X-ray and colonoscopy were all unremarkable.
Based on the clinical and histopathological ndings a diag-
nosis of bullous eosinophilic cellulitis was made. A short
course of methylprednisolone 40 mg daily which was reduced
to 5 mg daily combined with sulfasalazine 2 g daily resulted
in a rapid resolution of skin lesions. The patient has been free
of symptoms for more than 6 months.
Wells syndrome or eosinophilic cellulitis is a rare, often
recurrent inammatory skin disorder that has been reported to
be precipitated by drugs, arthropod bites and various kinds of
infection.
13
It has also been observed in patients with malignan-
cies such as squamous cell carcinoma, nasopharyngeal carcinoma
and adenocarcinoma of the colon.
4
Wells syndrome most often
presents with erythematous or urticarial plaques, while vesico-
bullous lesions are rare.
5
In addition to cutaneous manifestations,
peripheral blood eosinophilia, leucocytosis and thrombocytosis
may occur.
6,7
While potentially associated infectious or mali-
gnant diseases could be excluded in the case presented here,
there may be a relationship to our patients ulcerative colitis,
especially as skin manifestations coincided with gastrointestinal
symptoms. To our knowledge, Wells syndrome has not
previously been reported in association with ulcerative colitis.
Treatment options for eosinophilic cellulitis include antihist-
amines, corticosteroids, dapsone, minocycline and ciclosporin
as well as interferon alfa in severe, refractory cases.
8
Here, we describe the successful use of sulfasalazine, a
member of the sulphone family that is widely used for the
treatment of ulcerative colitis and Crohn disease. In sulfasala-
zine, salicylic acid is attached to an aminophenyl group that is
also a part of the structure of dapsone and sulfapyridine. In the
colon, sulfasalazine is cleaved into mesalazine (5-aminosalicylic
acid) and sulfapyridine.
9,10
While mesalazine is considered to
be the active metabolite responsible for the therapeutic efcacy
in chronic inammatory bowel disease, sulfapyridine, like
dapsone, may be the agent effective in eosinophilic cellulitis.
Our case illustrates that sulfasalazine may be an efcient treat-
ment option in cases of concomitant Wells syndrome and
Fig 2. (a) Histopathology of a skin biopsy obtained from the lower
left arm showing subepidermal blistering (haematoxylin and eosin;
original magnication 100). (b) Mixed-cell inltrates of lymphocytes
with innumerable eosinophils can be seen in the upper and lower
dermis and in the subcutaneous adipose tissue. Eosinophils are
scattered around dermal collagen bundles. Foci of degenerated
necrotic collagen bres as well as degranulating eosinophils (arrow)
are apparent and form ame gures (Giemsa stain; original
magnication 400).
Fig 1. Erythematous macules and plaques with bullae on the lower
left arm.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 765
colitis. Furthermore, it may be used when hepatotoxicity to
dapsone requires discontinuation of the latter. However, sulfa-
salazine should not supplement dapsone in patients with dap-
sone-induced agranulocytosis because such an adverse reaction
may occur in either case.
9
J . UTI KAL
W. K. PE I TS CH
N. KE MML E R
N. BOOKE N
R. HI L DE NB RAND*
R. GL ADI S CH
S. GOE RDT
M. GOE B E L E R
Department of Dermatology,
Venereology and Allergology,
*Department of Pathology and
4th Medical Department,
University Medical Center
Mannheim, Ruprecht-Karl
University of Heidelberg,
Theodor-Kutzer-Ufer 13, D-68135
Mannheim, Germany
E-mail: jochen.utikal@haut.ma.uni-heidelberg.de
References
1 Miescher G. Akutes esosinophiles Inltrat der Haut mit Facialislah-
mung und hochgradiger Eosinophilie im Blut. Dermatologica 1952;
105:2647.
2 Wells GC. Recurrent granulomatous dermatitis with eosinophilia.
Trans St Johns Hosp Dermatol Soc 1971; 57:4656.
3 Wells GC, Smith NP. Eosinophilic cellulitis. Br J Dermatol 1979;
100:1019.
4 Hirsch K, Ludwig RJ, Wolter M et al. Eosinophilic cellulitis (Wells
syndrome) associated with colon carcinoma. J Dtsch Dermatol Ges
2005; 3:5301.
5 Consigny S, Courville P, Young P et al. Histological and clinical
forms of the eosinophilic cellulitis. Ann Dermatol Venereol 2001;
128:21316.
6 Anderson CR, Jenkins D, Tron V, Prendiville JS. Wells syndrome
in childhood: case report and review of the literature. J Am Acad
Dermatol 1995; 33:85764.
7 Gaigl Z, Becker L, Goebeler M. Swelling and erythema of the right leg
in a 62-year-old patient. Wells syndrome. Hautarzt 2001; 52:3578.
8 Husak R, Goerdt S, Orfanos CE. Interferon alfa treatment of a
patient with eosinophilic cellulitis and HIV infection. N Engl J Med
1997; 337:6412.
9 Goebeler M, Seitz C, Rose C et al. Successful treatment of linear IgA
disease with salazosulphapyridine and intravenous immunoglobulins.
Br J Dermatol 2003; 149:91214.
10 Cohen HD, Das KM. The metabolism of mesalamine and its
possible use in colonic diverticulitis as an anti-inammatory agent.
J Clin Gastroenterol 2006; 40:1504.
Conicts of interest: none declared.
Hypohidrosis colocalized with Beckers naevus
DOI: 10.1111/j.1365-2133.2006.07723.x
SIR, Beckers naevus is a common unilateral hyperpigmented
hairy cutaneous hamartoma.
1
An association of Beckers nae-
vus with other developmental anomalies, such as ipsilateral
breast hypoplasia and musculoskeletal anomalies, tends to
show a regional correspondence, and these conditions are
assumed to be the manifestations of chromosomal mosai-
cism.
1,2
We describe a man with hypohidrosis colocalized
with a Beckers naevus.
A 20-year-old man presented with a dark brownish patch
with hypertrichosis on the right back and shoulder, which had
developed over a period of 10 years. Interestingly, he stated
decreased sweating within the pigmented lesion during exer-
tion (Fig. 1a). A starchiodine test following 15 min of exer-
cise revealed a denite localization of hypohidrosis that
colocalized with the Beckers naevus (Fig. 1b). A thorough his-
tory and review of systems revealed no other cutaneous
abnormalities. Skin biopsies were obtained from the back lesion
and from contralateral normal skin. The lesional skin showed
hyperkeratosis and acanthosis with basal hyperpigmentation of
the epidermis, which were consistent with Beckers naevus.
The number and luminal diameter of eccrine glands in lesional
skin were slightly reduced compared with the normal skin.
Beckers naevus has been known to be associated with
several developmental anomalies, such as ipsilateral breast
hypoplasia, supernumerary nipples, accessory scrotum,
musculoskeletal anomalies and congenital adrenal hyper-
plasia.
14
However, localized hypohidrosis in Beckers naevus
is an unusual phenomenon. To our knowledge, this is the rst
reported case of hypohidrosis in association with Beckers nae-
vus. In our patient, it is possible that the decreased numbers
of sweat glands may be the cause of the decreased sweating.
Beckers naevus manifests when postzygotic mutation occurs
in the developing embryo and results in a mosaic population of
homozygous or hemizygous cells. Mosaicism in broblasts
derived from one sporadic Beckers naevus lesion has been docu-
mented.
5
Developmental anomalies associated with Beckers
naevus may also be manifestations of chromosomal mosaicism.
2
Urbani and Betti
6
suggested that the coexistence of poly-
mastia with Beckers naevus could originate from one common
postzygotic mutation during embryonic development or from
single mutations in the two different developmental elds.
We suggest an explanation for the hypohidrosis localized in
our patients Beckers naevus from a review of cases of hypo-
hidrotic ectodermal dysplasia (HED).
7,8
Segmental or localized
hypohidrosis without other cutaneous anomalies could be
found in heterozygous carriers or postzygotic mutation carri-
ers of X-linked HED in whom diminished sweat glands were
the only important diagnostic clues, without any hair and
teeth abnormalities.
7
Interestingly, the gene responsible for
HED (EDA1) is localized at Xq12131 and this locus is near
to where the androgenic receptor gene (Xq11212) is
located.
9
The androgen stimulation associated with an
increased number of androgen receptors and elevated mRNA
levels in the lesion is a well-known nding in Beckers
naevus.
10
As these two genes are closely related, it is possible
that the development of Beckers naevus is associated with
postzygotic mutation of the androgenic receptor gene, and
concomitant hypohidrosis could occur within the lesion by a
similar mutagenic insult to the nearby EDA1 gene. To observe
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
766 Correspondence
the status of the androgen receptor in our patients Beckers
naevus, we performed immunohistochemical staining with
the antiandrogen receptor monoclonal antibody MU256-UC
(BioGenex, San Ramon, CA, U.S.A.), which revealed strong
androgen receptor immunoreactivity to the nuclei of epider-
mal keratinocytes, compared with normal skin (data not
shown). The two distinct anomalies might originate from one
common postzygotic mutation arising during the initial stage
of embryonic development.
In summary, we report a case of hypohidrosis conned
within a Beckers naevus lesion, and consider the possibility
of postzygotic mutation of a common genetic locus. In the
Beckers naevus, the specic relationship linking the gene
involved and the developmental elds are far from clear, and
therefore additional investigations at the molecular genetic
level are needed.
J . E. DO
Y. J . KI M
H. Y. KANG
Department of Dermatology,
Ajou University School of Medicine, 5 Wonchon-Dong,
Yeongtong-Gu, Suwon 443-721, Korea
Correspondence: Hee Young Kang.
E-mail: hykang@ajou.ac.kr
References
1 Juanes JS, Galache C, Curto R et al. Acneiform lesion in Beckers
nevus and breast hypoplasia. Int J Dermatol 2002; 41:699700.
2 Lucky AW, Saruk M, Lerner AB. Beckers nevus associated with
limb asymmetry. Arch Dermatol 1981; 117:243.
3 Szylit JA, Grossman ME, Luyando Y et al. Beckers nevus and an
accessory scrotum. A unique occurrence. J Am Acad Dermatol 1986;
14:9057.
4 Urbani CE, Betti R. Supernumerary nipples and Beckers nevus: a
previously undescribed association. Report of 9 patients including
a subset with uropathies. Eur J Dermatol 1995; 5:6857.
5 Lamber JR, Willems P, Abs R et al. Beckers nevus associated with
chromosomal mosaicism and congenital adrenal hyperplasia. J Am
Acad Dermatol 1994; 30:6557.
6 Urbani CE, Betti R. Supernumerary nipples occurring together with
Beckers naevus: an association involving one common paradomi-
nant trait? Hum Genet 1997; 100:38890.
7 Cambiaghi S, Restano L, Paakkonen K et al. Clinical nding in
mosaic carriers of hypohidrotic ectodermal dysplasia. Arch Dermatol
2000; 136:21724.
8 Rouse C, Siegfried E, Breer W et al. Hair and sweat glands in fam-
ilies with hypohidrotic ectodermal dysplasia. Arch Dermatol 2004;
140:8505.
9 Martinez F, Millan JM, Orellana C, Prieto F. X-linked anhidrotic
(hypohidrotic) ectodermal dysplasia caused by a novel mutation in
EDA1 gene: 406T > G (Leu55Arg). J Invest Dermatol 1999; 113:2856.
10 Pearson JR, Longcope C. Beckers nevus: an androgen-mediated
hyperplasia with increased androgen receptors. J Am Acad Dermatol
1984; 10:2358.
Conicts of interest: none declared.
Mutation hotspots of SCN9A in primary
erythermalgia
DOI: 10.1111/j.1365-2133.2006.07727.x
SIR, Primary erythermalgia (OMIM 133020; also called erythro-
melalgia) is an autosomal dominant disorder characterized by
recurrent burning pain and redness in the extremities in
response to mild thermal stimuli or exercise. A previous study
established the linkage of primary erythermalgia to a 794-cM
interval on chromosome 2q.
1
We subsequently narrowed down
the susceptibility locus to a 598-cM region by linkage analysis
and identied missense mutations of highly conserved residues
(I848T and L858H) in SCN9A in two Chinese cases with pri-
mary erythermalgia.
2
Here we report two sporadic cases, in a
13-year-old girl and a 10-year-old boy, and a family in which
an adult man and his 11-year-old son were affected. We also
summarize mutation hotspots in SCN9A in this disorder.
The four patients experienced intermittent episodes of red-
ness and burning pain in the extremities provoked by moder-
ate warmth or exercise since the age of 810 years. The
attacks were refractory to routine pharmacotherapy and the
patients often put their limbs into icy water to relieve pain
during episodes. Their presentations fullled the diagnostic
criteria for primary erythermalgia.
3
Following informed con-
sent, genomic DNA samples of the patients were prepared
(a) (b)
Fig 1. (a) Dark brownish patch and
hypertrichosis on the right back and shoulder.
Inset: decreased sweating was localized in the
Beckers naevus after exercise. (b) Starch
iodine test.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 767
from their peripheral blood leucocytes. All exons of SCN9A
and their anking sequences were amplied and sequenced.
In the two patients with sporadic erythermalgia we identi-
ed the heterozygous missense mutation T2543C which results
in the change I848T in the amino acid residue. In the affected
father and son, we found the heterozygous mutation C1185G
which leads to the change N395K in the polypeptide. Neither
of the mutations was found in 50 unaffected control subjects.
The mutation T2543C has been reported previously
2,4
but the
mutation C1185G is compatible with the mutation C1185A
described in a Dutch family
4
and shared the same amino acid
substitution of N395K.
SCN9A encodes a voltage-gated sodium channel Nav1.7
a-subunit that is expressed primarily in sensory and sympa-
thetic ganglia. The biophysical properties of mutant Nav1.7
a-subunit have recently been investigated, and gain-of-function
changes of dorsal root ganglion neurones are considered to be
the pathophysiological keystone of primary erythermalgia.
510
To date, nine familial cases and four sporadic cases including
the cases we depict here have been reported, and eight substi-
tution mutations have been identied (Table 1). Besides the
pathogenic mutations, the amino acid changes of P610T and
R1150W in the Nav1.7 a-subunit have been described as poly-
morphisms possibly unrelated to the disorder.
10
These families
and sporadic patients came from various countries with inde-
pendent genetic background, and some of them were shown to
be de novo mutations.
2,5
Of interest, very similar and in some
cases even the same SCN9A mutation spots can be detected.
From Figure 1 we can see that L858, I848 and N395 are
the most frequent mutation spots, described in nine of the 13
cases reported to date. All of the six Chinese cases we identi-
ed were found to have mutations in these three spots.
2,5
Remarkably, the three spots are located in the sodium channel
pore regions which regulate Na
+
moving down its concentra-
tion gradient into the cytoplasm to trigger the action potential.
Mutations in these regions have a substantial impact on bio-
physical properties of the channel.
5,9
Although we cannot rule
out the possibility that the same mutation occurring in appar-
ently unrelated patients may come from a founder effect, the
100% penetrance of this disease reported so far and the same
mutation shared by cases from distant areas or different coun-
tries suggest that they were unlikely to have the same founder.
Thus L858, I848 and N395 may be mutation hotspots in
Nav1.7 a-subunit in primary erythermalgia.
Acknowledgments
We thank the families for their cooperation in this study. This
study is supported by the National Natural Science Foundation
of China (30400168) and Beijing Science and Technology
Project (H020220020610).
L- L. ZHANG
Z- M. LI N
Z- H. MA*
Z. XU
Y- L. YANG
Y. YANG
Departments of Dermatology and
Paediatrics, Peking University First Hospital,
Beijing, China
*Department of Dermatology, Mudanjiang Medical College,
Mudanjiang, China
Department of Dermatology,
Beijing Childrens Hospital, Beijing, China
Correspondence: Yong Yang.
E-mail: dryongyang@bjmu.edu.cn; yongyang81@yahoo.com.cn
References
1 Drenth JP, Finley WH, Breedveld GJ et al. The primary erythermalgia-
susceptibility gene is located on chromosome 2q3132. Am J Hum
Genet 2001; 68:127782.
2 Yang Y, Wang Y, Li S et al. Mutations in SCN9A, encoding a
sodium channel alpha subunit, in patients with primary eryther-
malgia. J Med Genet 2004; 41:1714.
3 Drenth JP, Michiels JJ. Erythromelalgia and erythermalgia: diagnos-
tic differentiation. Int J Dermatol 1994; 33:3937.
4 Drenth JP, te Morsche RH, Guillet G et al. SCN9A mutations
dene primary erythermalgia as a neuropathic disorder of voltage
gated sodium channels. J Invest Dermatol 2005; 124:13338.
5 Han C, Rush AM, Dib-Hajj SD et al. Sporadic onset of erythermal-
gia: a gain-of-function mutation in Nav1.7. Ann Neurol 2006;
59:5538.
6 Dib-Hajj SD, Rush AM, Cummins TR et al. Gain-of-function muta-
tion in Nav1.7 in familial erythromelalgia induces bursting of sen-
sory neurons. Brain 2005; 128:184754.
7 Michiels JJ, te Morsche RH, Jansen JB et al. Autosomal dominant
erythermalgia associated with a novel mutation in the voltage-
gated sodium channel alpha subunit Nav1.7. Arch Neurol 2005;
62:158760.
8 Harty TP, Dib-Hajj SD, Tyrrell L et al. Na(V)1.7 mutant A863P
in erythromelalgia: effects of altered activation and steady-state
inactivation on excitability of nociceptive dorsal root ganglion
neurons. J Neurosci 2006; 26:1256675.
Table 1 Mutations in SCN9A reported in primary erythermalgia cases
Mutation
spots
Geographical
distribution
Number
of cases
L858H A Chinese family
2
1
L858F A Chinese family
5
and a Canadian family
4
2
I848T A French family
4
and three sporadic
Chinese patients
2,a
4
N395K A Chinese family
a
and a Dutch family
4
2
F1449V An American family
6
1
F216S A French family
4
1
S241T A Flemish family
7
1
A863P An American patient
8
1
a
The cases we report here.
N395K
F216S
S241T
1
I848T
A863P
L858H
L858F
F1449V
1977
Fig 1. Map of the mutations described so far in primary
erythermalgia. The horizontal line represents the amino acid sequence
of Nav1.7 a-subunit. Triangles represent Chinese cases; squares
represent cases reported from other countries.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
768 Correspondence
9 Cummins TR, Dib-Hajj SD, Waxman SG. Electrophysiological prop-
erties of mutant Nav1.7 sodium channels in a painful inherited
neuropathy. J Neurosci 2004; 24:82326.
10 Waxman SG, Dib-Hajj S. Erythermalgia: molecular basis for an
inherited pain syndrome. Trends Mol Med 2005; 11:55562.
Conicts of interest: none declared.
Cost-effectiveness of treatment of supercial
basal cell carcinoma: surgical excision vs.
imiquimod 5% cream
DOI: 10.1111/j.1365-2133.2006.07726.x
SIR, Basal cell carcinoma (BCC) is the most common malig-
nancy in white people, with an incidence increasing world-
wide by 10% a year.
1
Surgery is often the rst-line treatment
and the modality with the lowest failure rate.
2
Less invasive,
nonsurgical therapies are welcomed as they may offer treat-
ment without the use of destructive modalities. Imiquimod is
an immune response modier that acts through toll-like recep-
tor 7 to induce cytokine production and a subsequent innate
and adaptive cell-mediated immune response.
3,4
Clinical and
histological clearance of supercial BCC (sBCC) with imiqui-
mod 5% cream has been reported.
5,6
We compared direct costs
of treatment of sBCC by means of surgical excision or topical
imiquimod within the Spanish public healthcare system.
The cost per patient cured with imiquimod 5% cream
applied ve times a week for 6 weeks vs. excisional surgery in
patients with a single sBCC smaller than 2 cm was estimated
using a decision analysis model. The model assumed that
patients not cured with rst-line treatment were re-treated with
excisional surgery until 100% tumour clearance was achieved,
so that additional costs or savings per cured patient were also
evaluated. Although initial diagnosis of sBCC was established in
dermatology services, excisional surgery could be performed in
either dermatology or nondermatology services (e.g. plastic
surgery, general surgery, otorhinolaryngology). The time frame
was 1 year. Inputs in the model for excisional surgery were
obtained from a retrospective review of the patients medical
records. No real data from clinical practice for imiquimod were
available in the literature because the study was conducted
before approval of imiquimod for the indication of sBCC by
the European Medicines Agency. Thus, four expert dermatolo-
gists validated the resources associated with topical imiquimod
treatment, consistently choosing the worst scenario in terms of
number of sachets per treatment, outpatient visits, biopsies, etc.
Participating physicians examined the medical records of all
consecutive patients with sBCC having undergone excisional
surgery from June 2001 to December 2002. In total, 209
medical records collected from 23 dermatology services were
included. Of these patients, 178 were treated in dermatology
services and 31 in nondermatology services. Data on effective-
ness and resource utilization were collected for the following
periods: diagnosis, time from diagnosis until surgical excision,
surgical procedure and 1-year post-treatment. Unit costs for
the resources used in the model regarding health personnel,
materials and laboratory tests were obtained from the Spanish
SOIKOS healthcare costs database.
7
An analysis was made
based on the hypothesis that differences could exist depending
on the site where surgical excision was carried out (dermatol-
ogy vs. nondermatology services). A sensitivity analysis was
performed to evaluate the robustness of the model using the
lower (76%) and upper (87%) limits of the 95% condence
interval (CI) of the rate of histological clearance with imiqui-
mod 5% cream reported in the study of Geisse et al.
8
The efcacy of topical imiquimod used in the model was
82%.
8
The experts established that three boxes (36 sachets) of
imiquimod 5% cream would be used to complete treatment
although the summary of product characteristics indicated that
two and a half boxes (30 sachets) are needed. A rst visit to
the dermatologist including biopsy, an average of 25 visits to
Table 1 Average unit cost of resources for management of supercial
basal cell carcinoma
Resource Unit cost (euros)
Diagnosis
Biopsy 5750
Visits
Dermatologist 5490
Anaesthetist 5380
Surgeon 8830
Haematologist 12170
Radiologist 3070
General practitioner 2100
Nurse 1470
Surgical procedure (cost min
)1
)
Surgeon/dermatologist
a
064
Anaesthetist 046
Scrub nurse 026
Assistant nurse 018
Anaesthesia
Local 3710
General 16760
Complementary tests
Blood tests 700
Coagulation 1560
Electrocardiogram 920
X-ray 2000
Anticoagulant therapy 3150
Antibiotic prophylaxis 420
Site of care
Outpatient 11460
Inpatient 38130
Sterile operating room (cost min
)1
) 539
a
The unit costs available from an ofcial source were available
only for a nondermatology surgeon. For the purpose of analysis,
it was assumed that this cost was the same when a dermato-
logist performed the surgery.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 769
the dermatologist after starting treatment, and a visit to the
primary care physician were also assumed. The effectiveness
of surgical excision according to the medical records was 97%
for dermatology and 90% for nondermatology services. The
average unit cost of resources is shown in Table 1. Mean cost
per patient cured by surgical excision was 676 euros at
dermatology services and 1051 euros at nondermatology ser-
vices compared with 621 and 676 euros for topical imiqui-
mod (Table 2). The higher costs in nondermatology services
were mainly due to more expensive surgical procedures and
postoperative care. Savings per patient cured with topical
imiquimod in dermatology and nondermatology services were
55 and 375 euros, respectively.
When the lower (76%) and upper (87%) limits of the 95%
CI for histological clearance with imiquimod 5% cream were
considered,
8
the corresponding treatment costs were 651 and
597 euros for dermatology services and 719 and 641 for non-
dermatology services, resulting in savings for imiquimod of
25 and 79 euros in the dermatology services and 332 and
410 euros in nondermatology services.
The generalizability of our ndings is limited because
resource utilization and associated costs apply to the Spanish
national healthcare system. The 5-year recurrence rate is
unknown and the cost of treating the failures and the follow-
up of possible failures has not been calculated. This study,
however, shows that the use of imiquimod 5% cream for the
treatment of sBCC reduces cost per patient cured compared
with surgery in dermatology and nondermatology services.
Topical application of imiquimod 5% cream is a cost-effective
alternative to excisional surgery in patients with sBCC.
Acknowledgments
The HEIS Study Group comprises: Jose D. Dom nguez, Hospi-
tal Doce de Octubre, Madrid; Pilar Burkhardt and Ramon Nar-
anjo, Hospital Cl nico San Cecilio, Granada; Alberto Miranda,
Hospital Cl nico, Valladolid; Francisco Carapeto and Ana C.
Lazaro, Hospital Cl nico Universitario Lozano Blesa, Zaragoza;
Mariano Casado and Carmen Vidaurrazaga, Hospital La Paz,
Madrid; Pablo de Unamuno, Monica Roncero, Ana Mart nez
de Salinas and Francisca Izquierdo, Hospital Cl nico Universi-
tario, Salamanca; Enrique Gimeno and Fernando Millan, Hos-
pital Arnau de Vilanova, Valencia; Eduardo Nagore, Instituto
Valenciano de Oncolog a, Valencia; Luis R os and Silvia Perez,
Hospital La Princesa, Madrid; Lorenzo Perez, Hospital General
de Albacete, Albacete; Diego de Argila, Hospital Infanta Cristi-
na, Badajoz; Anna Tuneu, Jose Zubizarreta and Arantxa Lopez,
Hospital Donostia, San Sebastian; Jose M. Fernandez-Vozmedi-
ano and Antonio Gonzalez-Cabrerizo, Hospital Universitario
Puerto Real, Puerto Real, Cadiz; Pablo Umbert and Jaume Mas-
sana, Hospital del Sagrado Corazon, Barcelona; Amalia Serrano,
Hospital Virgen del Roc o, Seville; Jose M. Ricart, Montserrat
Evole, Miguel A. Navarro and Antranick Massmanian, Hospital
La Fe, Valencia; Isabel Betlloch, Isabel Belinchon and Mar
Blanes, Hospital General Universitario, Alicante; Jesus Luelmo
and Mireia Sabat, Hospital Parc Taul , Sabadell, Barcelona; Lor-
eto Carrasco and Isabel Nieto, Hospital Naval San Carlos, San
Fernando, Cadiz; Ander Zulaica, Jose M. Fabeiro and Jose L.
Caeiro, Hospital Xeral Cies, Vigo; Mercedes Alcalde and
Francisca Simon, Hospital Torrecardenas, Almer a; Carmen
Brufau, Hospital General Universitario, Murcia; and Manuel
Cruces and A
ngeles Florez, Hospital Provincial, Pontevedra.
F. VANACL OCHA
E. DAUDE
N*
X. BADI
A
C. GUI L L E
N
J . S. CONE J O- MI R
M. SAI NZ DE L OS TE RRE ROS **
L. HAME L
M. A. LL ORE NS **
F OR THE HEI S
STUDY GROUP
Department of Dermatology,
Hospital Doce de Octubre,
Carretera de Andaluc a km 5.4, E-28041 Madrid,
Spain *Department of Dermatology,
Hospital Universitario La Princesa,
Madrid, Spain
Department of Clinical Epidemiology and
Public Health, Hospital de la Santa Creu i Sant Pau,
Barcelona, Spain
Health Outcomes Research Europe, Barcelona, Spain
Department of Dermatology,
Instituto Valenciano de Oncolog a, Valencia, Spain
Department of Dermatology,
Hospital Universitario Virgen del Roc o, Seville, Spain
**3M Healthcare, Madrid, Spain
3M Sante , Cergy-Pontoise, France
E-mail: pvanse@hotmail.com
References
1 Wong CSM, Strange RC, Lear JT. Basal cell carcinoma. BMJ 2003;
327:7948.
2 Bath-Hextall F, Bong J, Perkins W, Williams H. Interventions for
basal cell carcinoma of the skin: systematic review. BMJ 2004;
329:705.
Table 2 Average cost per patient cured and incremental cost per
patient cured for imiquimod 5% cream and excisional surgery in
dermatology and nondermatology services
Data
Dermatology
services
Nondermatology
services
Surgery Imiquimod Surgery Imiquimod
Efcacy, %
First-line treatment 97 82 90 82
Total 100 100 100 100
Costs (euros)
Diagnosis 11250 11250 11250 11250
Diagnosisexcision
a
5750 16130
First-line treatment 30060 22400
b
36390 24000
b
Follow-up 19080 19600 34210 19600
Second-line
treatment
1470 8800 7060 12700
Total cost
(euros/patient)
676 621 1051 676
Savings imiquimod
(euros/patient)
55 375
a
Procedures/tests performed between diagnosis and surgical
excision.
b
Average weighted cost by level of reimbursement
according to the proportion of retired subjects ( 65 years of
age).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
770 Correspondence
3 Taylor M. Imiquimod and supercial skin cancers. J Drugs Dermatol
2005; 4:598606.
4 Oldeld V, Keating GM, Perry CM. Imiquimod: in supercial basal
cell carcinoma. Am J Clin Dermatol 2005; 6:195202.
5 Schulze HJ, Cribier B, Requena L et al. Imiquimod 5% cream for
the treatment of supercial basal cell carcinoma: results from a ran-
domized vehicle-controlled phase III study in Europe. Br J Dermatol
2005; 152:93947.
6 Gollnick H, Barona CG, Frank RG et al. Recurrence rate of supercial
basal cell carcinoma following successful treatment with imiquimod
5% cream: interim 2-year results from an ongoing 5-year follow-up
study in Europe. Eur J Dermatol 2005; 15:37481.
7 Brosa M. Base de Datos Costes Sanitarios. Barcelona: SOIKOS, 2004.
8 Geisse J, Caro I, Lindholm J et al. Imiquimod 5% cream for the treatment
of supercial basal cell carcinoma: results from two phase III, random-
ized, vehicle-controlled studies. J Am Acad Dermatol 2004; 50:72233.
Conicts of interest: M.S. de los T, L.H. and M.A.Ll. are employed by
3M, the manufacturer of Aldara
(imiquimod).
Comparative efcacy of topical antipsoriatic
treatments, systemic treatment and biologics:
is severity assessment beyond Psoriasis Area
and Severity Index a necessity?
DOI: 10.1111/j.1365-2133.2006.07747.x
SIR, A retrospective analysis recently appeared in the International
Journal of Dermatology summarizing data from six multicentre
studies including 2452 patients on the efcacy and safety of
the two-compound product calcipotriol/betamethasone dipro-
pionate ointment.
1
In 541% of these patients with moderate
to severe psoriasis a reduction of the Psoriasis Area and Sever-
ity Index (PASI) of at least 75% (PASI 75) was already reached
after 4 weeks. When this result is compared with PASI 75 data
of biologic treatments after 12 weeks, only iniximab was
found to be as effective as the two-compound topical product.
This message challenges the common belief that the efcacy
of a topical treatment is inferior to that of systemic treatments.
However, we felt that some critical notes have to be made
with respect to the design of comparative analyses between
populations eligible for topical treatment, systemic treatment
and biologics and, furthermore, with respect to the use of
PASI as sole outcome criterion to assess severity of psoriasis
symptoms at baseline and efcacy of treatments.
As practising dermatologists we know that in those patients
who do not respond adequately any more to topical treatments
or photo(chemo)therapy a systemic treatment may be started,
as monotherapy or in combination with a topical treatment. In
patients not responding adequately to these classical approaches
a biologic may be indicated. Patients who respond well to a
topical treatment are not eligible for a systemic treatment or
biologic. Study data derived from populations eligible for a
topical treatment vs. data derived from populations on systemic
treatment or biologics cannot be compared without consider-
ing that the populations are very different. This is not necessar-
ily apparent when comparing study populations as described
with respect to inclusion and exclusion criteria. The question
arises of whether interstudy comparison can provide meaning-
ful data when analysing subgroups with a similar severity.
The assessment of efcacy of dermatological treatments
in psoriasis is almost exclusively performed by using the PASI.
This score is widely accepted, although advantages and dis-
advantages have been intensively discussed. The PASI is further
used to compare the efcacy of different treatment modalities
among each other. This can be done by calculating the change
of PASI in relation to baseline or the percentage of patients
achieving a reduction of PASI from baseline of at least 50%
(PASI 50) or 75% (PASI 75). The PASI is a reliable instrument in
patients with moderate to severe psoriasis; however, in patients
with mild disease the PASI shows a high degree of variability.
The question here is: to what extent does the PASI help to
dene patient groups in terms of severity before initiation of a
treatment? In order to answer this question an audit on clinical
severity assessment in clinical practice was carried out by the
Copenhagen Psoriasis Working Group.
2
Baseline severity scores
such as PASI and affected body surface area (BSA) were ana-
lysed in relation to the subsequent choice of treatment (topical
or systemic including phototherapy). There was a large overlap
in the range of baseline PASI and BSA scores for both the top-
ical and the systemic treatment groups. A standardized protocol
for the evaluation of psoriasis severity based on established
severity scores (PASI, BSA) appeared to be unrealistic in day-
to-day clinical practice. In everyday dermatology there is no
cut-off point for objective severity scores beyond which a top-
ical treatment is no longer indicated. The substantial improve-
ment (PASI 75) reached in 54% of the patients with extensive
disease (BSA > 10% and PASI baseline values > 17) treated
with the two-compound ointment calcipotriol/betamethasone
dipropionate underscores the position that dermatologists have
to consider topical treatments also in patients with extensive
disease. However, in a comparative analysis between different
studies, a comparable baseline PASI in the treatment groups by
no means guarantees that these groups had a similar disease
severity before treatment. A host of factors can be dened
behind the decision to start a systemic treatment. In addition
to the current state of the disease, the disease severity in terms
of responsiveness to previous treatments and also the dynamics
of the disease are important aspects to reconcile before select-
ing a treatment. Kirby et al. have proposed the Salford Psoriasis
Index, which is a three-digit severity index comprising one
digit for objective severity, one for quality of life and one for
historical severity, reecting the need in a patient to prescribe
a systemic treatment for reason of failure of topicals.
3
Such an
attempt to integrate other meaningful criteria into psoriasis
severity scoring may be helpful in future studies.
In conclusion, comparisons between topical and systemic
treatments and biologics with respect to efcacy require
prospective randomized studies according to the principles of
evidence-based medicine. For now, we appreciate the efcacy
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 771
of the two-compound ointment calcipotriol/betamethasone
dipropionate, but the question remains regarding what the
efcacy of this treatment would have been in the same group of
patients who actually have been treated with the biologics. The
PASI is insufcient to estimate disease activity as it reects the
current status of the patient and does not take into account
the disease activity and the response to previous treatment.
P. C. M. VAN DE KE RKHOF
U. MROWI E T Z *
S. SE GAE RT
K. KRAGB AL L E
Department of Dermatology, Radboud
University Nijmegen Medical Centre,
Nijmegen, the Netherlands
*Psoriasis-Center, Department of Dermatology,
University of Kiel, Kiel, Germany
Department of Dermatology, University Hospital
Sint-Rafael, Leuven, Belgium
Department of Dermatology, A
rhus University Hospital,
A
rhus, Denmark
E-mail: p.vandekerkhof@derma.umcn.nl
References
1 Anstey AV, Kragballe K. Retrospective assessment of PASI 50 and
PASI 75 attainment with a calcipotriol/betamethasone dipropionate
ointment. Int J Dermatol 2006; 45:9705.
2 van de Kerkhof PCM, Kragballe K. Psoriasis: severity assessment in
clinical practice. Conclusions from workshop discussions and a pros-
pective multicentre survey of psoriasis severity. Eur J Dermatol 2006;
16:16771.
3 Kirby B, Fortune DG, Bhushan M et al. The Salford Psoriasis Index: an
holistic measure of psoriasis severity. Br J Dermatol 2000; 142:72832.
Conicts of interest: none declared.
Ultraviolet B exposure could inuence the
interpretation of serum S100b levels in
patients with malignant melanoma
DOI: 10.1111/j.1365-2133.2006.07737.x
SIR, Since its rst description by Moore in 1965,
1
S100 pro-
tein has been the subject of numerous investigations. It has
been classied into a family of proteins with several isoforms
found in different tissues, and the diagnostic value of these
has constantly risen. Among these protein isoforms, the S100b
protein is found predominantly in cells of the central nervous
system, Langerhans cells and melanocytes. It has been proven
to be of clinical use in indicating brain damage
2
after trauma
or ischaemia, and has also been proposed as a marker
for different skin disorders.
3,4
The most established application
of S100b is as a serum tumour marker with prognostic value
for the course of malignant melanoma, indicating macro-
metastasis but not micrometastasis.
5,6
Recently, Domingo-
Domenech et al.
7
found a predictive value for serum levels of
S100b under novel melanoma treatment strategies. As the
therapeutic decisions based on such markers are important,
improving specicity and sensitivity is a common aim for
interpretation of elevated serum S100b levels.
Tronnier et al.
8
found an inuence of ultraviolet (UV) B
irradiation of the skin on serum S100b levels in four of 13
healthy volunteers investigated who had been whole-body
exposed to UV radiation at suberythemal doses. The serum
level rose to values comparable with pathological values from
a melanoma patient study. As the endpoint was 72 h after UV
irradiation, it remains unclear whether other individuals of the
volunteer group would also have shown elevated S100b levels.
To investigate a possible UVB-induced S100b excretion into
extracellular uid by normal nontumorigenic, nonimmortal-
ized melanocytes, we set up an experimental model. Primary
adult human melanocytes derived from plastic surgery (Pro-
mocell GmbH, Heidelberg, Germany) were cultivated in spe-
cial medium with additives as supplied by the distributor.
Cells were kept routinely at 37 C and 5% CO
2
protected from
light. Twenty-four hours prior to irradiation cells were pas-
saged, plated into multichamber slides and allowed to adhere
overnight. UVB irradiation was performed using a UVB spec-
trum lamp (Waldmann 501T; Waldmann GmbH, Villingen-
Schwenningen, Germany).
After covered sham-irradiation under the same room condi-
tions or true UVB irradiation at 50 mJ or 100 mJ, the cham-
ber slides were put back into the incubator. For each time
point, uid from the melanocyte cultures was taken off and
centrifuged gently at 139 g for cell removal; the superna-
tants were kept at )20 C until protein assay. The adherent
cells on the slides were xed using ethanol and stored for
further evaluation.
S100b levels were measured using an enzyme-linked immuno-
sorbent assay (ELISA) technique (IBL GmbH, Hamburg, Germany)
in a 96-well plate and read at 620 nm. All ELISA probes were
double-detected; the standard curve and intra-assay variability
were in accordance with the manufacturers manual.
Hours after irradiation
0 20 40 60 80
S
1
0
0
(
n
g
l
1
)
150
200
250
300
350
400
Control
50 mJ : level of significance 48 h
P < 001 (**), 72h P < 005 (*)
100 mJ : level of significance 48 h,
72 h P < 001 (**)
Fig 1. S100b levels in normal human melanocyte cell supernatants at
05, 6, 24, 48 and 72 h after irradiation with ultraviolet B. Error bars
represent SD of three independent experiments.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
772 Correspondence
Figure 1 summarizes the ndings of S100b levels in mel-
anocyte supernatants after 05, 6, 24, 48 and 72 h. A slight
increase in S100b can be observed even in the controls, but
the difference between control and irradiated cells increases
over time after irradiation and is also dose dependent. We
consider the slight increase of S100b level in controls to be
caused either by the fact that cells could not be prepared in
the total absence of light, resulting in melanocyte activation,
or possibly by a cumulative increase of cell depletion. The cell
doubling time was 456 h in both controls and irradiated
cells, resulting in similar cell counts after each measurement.
To our knowledge, we show for the rst time that S100b
levels in extracellular uid derived from normal human skin
melanocytes increase after irradiation with suberythemal as
well as erythemal UVB doses. Taking this nding together
with the observations of Tronnier et al., who found elevated
serum S100b levels after UVB exposure in some individuals
of a small group of volunteers, we conclude that UVB
exposure of skin cells can indeed inuence serum S100b
levels. Further investigation is needed to provide correct
interpretation of elevated S100b levels in dermatology as well
as in neurology.
Acknowledgments
The authors thank I. Nuyken for excellent technical assistance.
J . VI TZ T HUM
H. D. DO
RR
V. ME I NE KE
Bundeswehr Institute of Radiobiology,
Munich, Germany
E-mail: jannisvitzthum@bundeswehr.org
References
1 Moore BW. A soluble protein characteristic of the nervous system.
Biochem Biophys Res Commun 1965; 19:73944.
2 Cotena S, Piazza O, Storti M. The S100B protein and traumatic brain
injury. J Neurosurg 2006; 104 (Suppl. 6):4356.
3 Gupta SK, Nigam S, Mandal AK, Kumar V. S-100 as a useful auxi-
liary diagnostic aid in tuberculoid leprosy. J Cutan Pathol 2006;
33:4826.
4 Weiss T, Weber L, Scharffetter-Kochanek K, Weiss JM. Solitary cuta-
neous dendritic cell tumor in a child: role of dendritic cell markers
for the diagnosis of skin Langerhans cell histiocytosis. J Am Acad
Dermatol 2005; 53:83844.
5 Jury CS, McAllister EJ, MacKie RM. Rising levels of serum S100 pro-
tein precede other evidence of disease progression in patients with
malignant melanoma. Br J Dermatol 2000; 143:26974.
6 Acland K, Evans AV, Abraha H et al. Serum S100 concentrations are
not useful in predicting micrometastatic disease in cutaneous
malignant melanoma. Br J Dermatol 2002; 146:8325.
7 Domingo-Domenech J, Molina R, Castel T et al. Serum protein s-100
predicts clinical outcome in patients with melanoma treated with
adjuvant interferon comparison with tyrosinase rtPCR. Oncology
2005; 68:3419.
8 Tronnier M, Missler U, Grotrian K, Kock N. Does ultraviolet radi-
ation exposure inuence S100b protein plasma levels? Br J Dermatol
1998; 138:1098100.
Conicts of interest: none declared.
Erythema gyratum repens-like eruption in a
patient with epidermolysis bullosa acquisita
associated with ulcerative colitis
DOI: 10.1111/j.1365-2133.2006.07746.x
SIR, Epidermolysis bullosa acquisita (EBA) is an acquired auto-
immune bullous disease of the skin and mucous membranes
characterized by IgG autoantibodies to type VII collagen,
the main constituent of the anchoring brils of the dermal
epidermal juction.
1,2
Inammatory bowel diseases (IBD) may
be associated with autoimmunity to type VII collagen.
3,4
Ery-
thema gyratum repens (EGR), an obligate paraneoplastic syn-
drome, may occur in patients with pemphigoid diseases.
59
To the best of our knowledge, EGR has not been previously
described in EBA. We report a most unusual clinical manifest-
ation of EGR-like lesions in a patient with EBA and ulcerative
colitis (UC).
A 35-year-old woman presented with 2-year history of
bullous skin lesions on the trunk and extremities and ero-
sions on the oral mucosa. In addition, 6 months before her
rst visit to our department, she developed progressive diar-
rhoea and asthenia. Following further investigation by endo-
scopy with biopsy of colonic mucosa a diagnosis of UC was
made. A computed tomographic scan ruled out the presence
of a neoplastic process. Physical examination revealed wide-
spread blistering, erosions, scarring and milia formation on
her hands (Fig. 1a), feet (Fig. 1b), legs and arms. In add-
ition, erythematous lesions with a wood-grained appearance
were observed on the thighs and trunk (Fig. 1c). Bullous
lesions were associated with gurate erythematous lesions on
the knees and legs (Fig. 1d). Examination of the oral cavity
revealed erosions and scarring of jugal and lingual mucosa.
Histopathological examination of a blister showed a subepi-
dermal split and a massive inltrate mainly consisting of
neutrophils in the upper dermis (Fig. 2a). Direct immuno-
uorescence (IF) of the perilesional skin demonstrated linear
deposits of IgG and C3 at the basement membrane zone.
Indirect IF on NaCl-split skin revealed circulating IgG auto-
antibodies binding to the dermal side (titre 1 : 320). These
antibodies belonged to the IgG1, IgG3 and IgG4 subclasses
(Fig. 2b). By immunoblotting using a recombinant form of
the noncollagenous (NC) 1 domain of type VII collagen,
10
our patients serum demonstrated type VII collagen-specic
IgG4 autoantibodies (data not shown). Serum tumoral mark-
ers, including s-CA 199, s-CA 125 and s-CEA, were within
the normal range. Enzyme-linked immunosorbent assay
analysis using recombinant antigen did not reveal reactivity
against the immunodominant XVII NC domain of BP180.
Our patient was started on a regimen of prednisone 40 mg
daily, oral sulfasalazine 2 g daily and mycophenolate mofetil
2 g daily. Under this treatment, an important clinical and
serological improvement was noted at the follow-up visit
3 months later.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 773
Several clinical manifestations of EBA are described, includ-
ing the classic mechanobullous, the generalized inammatory,
and the cicatricial pemphigoid-like types.
2
Interestingly, our
patient presented features of both the mechanobullous and the
inammatory forms of EBA, with acral lesions, scarring, milia
formation and an erythematous inammatory eruption on the
trunk. Nevertheless, the gurate eruption resembling EGR rep-
resents a particular clinical feature of this patient that has not
yet been reported in patients with EBA. EGR may be very
rarely associated with pemphigoid diseases.
59
Although EGR
Fig 1. Blisters, erosions, scarring and milia formation on (a) patients left hand and (b) feet. (c) On thighs, erythematous lesions with a wood-
grained appearance were observed. (d) Figurate erythematous lesions accompanied the bullous eruption.
Fig 2. (a) Subepidermal blistering and a neutrophil-rich inammatory inltrate were observed within the upper dermis (haematoxylin and eosin;
original magnication 40). (b) Circulating autoantibodies of IgG1, IgG3 and IgG4 subclasses binding to the dermal side of 1 mol L
)1
NaCl-split
skin were detected by indirect immunouorescence microscopy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
774 Correspondence
usually represents an ominous sign heralding an associated
neoplasm, our patient as well as several previously reported
cases
6,7,9
clearly demonstrate that in patients with autoim-
mune blistering diseases such gurate erythema may occur in
the absence of neoplasia.
Irrespective of its clinical manifestation, EBA is associated
with autoantibodies to type VII collagen.
1,3
Patients autoanti-
bodies belonging to different IgG subclasses mainly target epi-
topes within the NC1 domain of type VII collagen.
1
IgG
autoantibodies to type VII collagen mainly belong to the IgG1
and IgG4 and to the IgG3 subclasses in EBA and IBD, respect-
ively. Consistent with these ndings, our patient presented
IgG1, IgG3 and IgG4 autoantibodies to type VII collagen.
While the blister-inducing potential of autoantibodies to type
VII collagen is established,
2
their contribution to the patho-
genesis of IBD and EGR-like lesions is still unclear. IBD occur
in approximately 30% of patients with EBA. Thus EBA is
mainly associated with Crohns disease, but rarely with UC.
4,7
The causes and pathomechanisms underlying the association
of EBA with IBD are poorly understood. The detection of type
VII collagen expression in the colonic mucosa led to the hypo-
thesis that, in the context of chronic inammation and dam-
age to the overlying mucosa, antigenic epitopes of the type
VII collagen molecule are exposed. These newly exposed anti-
genic epitopes may invoke production of autoantibodies,
which, in some patients, also cross-react with type VII colla-
gen and trigger blister formation in the skin.
7
Why EBA asso-
ciates more often with Crohns disease compared with UC is
even less clear.
When IBD and EBA are associated, the onset of IBD usually
precedes by several years the rst manifestations of the blister-
ing disease. Interestingly, in our patient, the onset of EBA
clearly predated the manifestations of UC.
In conclusion, we report that an EGR-like eruption may occur
in EBA associated with UC. Our results emphasize the notion
that EBA is clinically a heterogeneous disease and suggest EGR
to be one of its possible manifestations. Therefore, the differ-
ential diagnosis in patients with EGR-like eruptions should
also include EBA and other autoimmune blistering skin diseases.
A. ES P AN
A
C. SI T ARU*
M. PRE TE L
L. AGUADO
J . J I ME NE Z
Department of Dermatology, University Clinic of
Navarra, University of Navarra, School of Medicine,
PO Box 4209, Pamplona 31080, Navarra, Spain
*Department of Dermatology, University of Lubeck,
Germany
Department of Gastroenterology, Hospital of
Navarra, Pamplona, Navarra, Spain
E-mail: aespana@unav.es
References
1 Sitaru C, Zillikens D. Mechanisms of blister induction by autoanti-
bodies. Exp Dermatol 2005; 14:86175.
2 Hallel-Halevy D, Nadelman C, Chen M, Woodley DT. Epidermo-
lysis bullosa acquisita: update and review. Clin Dermatol 2001;
19:71218.
3 Chen M, OToole EA, Sanghavi J et al. The epidermolysis bullosa
acquisita antigen (type VII collagen) is present in human colon
and patients with Crohns disease have autoantibodies to type VII
collagen. J Invest Dermatol 2002; 118:105964.
4 Oostingh GJ, Sitaru C, Zillikens D et al. Subclass distribution of type
VII collagen-specic autoantibodies in patients with inammatory
bowel disease. J Dermatol Sci 2005; 37:1824.
5 Graham-Brown RA. Bullous pemphigoid with gurate erythema
associated with carcinoma of the bronchus. Br J Dermatol 1987;
117:3858.
6 Caputo R, Bencini PL, Vigo GP et al. Eruption resembling erythema
gyratum repens in linear IgA dermatosis. Dermatology 1995;
190:2357.
7 Breathnach SM, Wilkinson JD, Black MM. Erythema gyratum
repens-like gurate eruption in bullous pemphigoid. Clin Exp Dermatol
1982; 7:4016.
8 Hauschild A, Swensson O, Christophers E. Paraneoplastic bullous
pemphigoid resembling erythema gyratum repens. Br J Dermatol
1999; 140:5502.
9 Wozniak K, Kowalewski C, Hashimoto T et al. Penicillin-induced
anti-p200 pemphigoid: an unusual morphology. Acta Derm Venereol
(Stockh) 2006; 86:4436.
10 Sitaru C, Kromminga A, Hashimoto T et al. Autoantibodies to type
VII collagen mediate Fcgamma-dependent neutrophil activation
and induce dermalepidermal separation in cryosections of human
skin. Am J Pathol 2002; 161:30111.
Conicts of interest: none declared.
Blindness due to the IgA variant of
epidermolysis bullosa acquisita, and treatment
with osteo-odonto-keratoprosthesis
DOI: 10.1111/j.1365-2133.2006.07739.x
SIR, We describe a woman who initially presented in 1994, at
age 47 years, with numerous groups of blisters in an annular
arrangement on the trunk, strongly suggestive of linear IgA
disease (LAD). Biopsy with immunouorescence conrmed
intense linear dermoepidermal IgA deposition which was felt
to support the diagnosis of LAD, although recent re-evaluation
using indirect immunouorescence and salt-split skin has
shown that the binding of IgA is predominantly dermal, thus
suggesting that she actually has IgA-epidermolysis bullosa
acquisita (IgA-EBA). No cause or associated disease have
become apparent over 12 years of follow-up.
Some therapeutic aspects of this patient were included in an
earlier report of vitamin E prophylaxis for dapsone-induced
headache
1
(her initial treatment was with dapsone) but her
treatments and response are further documented here as they
are remarkable for the lack of efcacy. Treatments (individually
or in combination) have included dapsone (with vitamin E);
sulfapyridine; numerous topical (including ocular, buccal and
vaginal) and systemic (oral and pulsed intravenous) cortico-
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 775
steroids; emollients/lubricants; topical and oral antibiotics;
ciclosporin; mycophenolate mofetil; cyclophosphamide; intra-
venous immunoglobulin (six courses of infusions, each
2 g kg
)1
over 5 days); subconjunctival mitomycin C; and
subcutaneous interferon alfa (3 MIU three times weekly).
Azathioprine was suggested but refused. Interferon, used on
the basis of a single report in a patient who also had hepatitis
C,
2
was the most effective agent but caused signicant anaemia
and had to be discontinued.
Over the years the main problem in this patient has been
progressive mucosal scarring, notably of conjunctivae, but also
of nails. She has also had blistering which was mainly truncal
but has increasingly localized to perineum and eyes, but also
to scalp, neck, and oral mucosa. In 1996 she presented with
cicatricial trichiasis and corneal epithelial instability. This was
treated with frequent lubrication, punctal occlusion and epila-
tion. Local ocular treatment with retinoic acid, aprotinin and
steroid appeared ineffective. Eyelid surgery was performed in
1997 (lid eversion to avoid corneal abrasion by the eyelashes)
but the right eye deteriorated rapidly, resulting in corneal per-
foration, suppurative keratitis, endophthalmitis and retinal
detachment. She had to stop working in 1999 and by 2000 the
right eye was blind. The left eye also progressed rapidly, again
resulting in corneal scarring, vascularization and perforation
which healed with contact lens and topical treatment. By the
end of 2002 the left vision was a mere perception of light.
Corneal transplant to restore vision was not feasible as the
eye was dry (therefore unable to lubricate) and still prone to
active blistering and further scarring. She was therefore
referred for an osteo-odonto-keratoprosthesis (OOKP) proced-
ure to the left eye (her right eye retinal detachment meant
that any anterior eye procedure would not produce benet).
The operation was technically successful (although recovery
was complicated by cephalosporin-induced toxic epidermal
necrolysis), and the patient gives a graphic description, once
bandaging was removed, of being able to see faces for the rst
time for many years, to read large print words and to read the
time from a wall-mounted clock. Two years later, she has 6/6
vision and reads N5 print, and has normal ocular pressure.
She still requires occasional division of adhesions and has had
problems with trichiatic eyelashes, which have required
removal on several occasions. All procedures still tend to pro-
voke conjunctival blistering.
The OOKP procedure has been described in detail else-
where.
3,4
It is indicated for situations where a cadaveric corneal
transplant would inevitably fail due to irreversible changes in
the corneal environment and stem cell failure/compromise. It
has been used for scarring with dry eye due to burns or chem-
ical injury; from a dermatological perspective it can be useful
for scarring secondary to inammatory and immunobullous
dermatoses such as StevensJohnson syndrome, toxic epidermal
necrolysis, cicatricial pemphigoid or, as demonstrated in this
case, IgA-EBA. For example, a large study of 204 patients (181
treated with the two-stage procedure described below) included
39 with mucous membrane pemphigoid and 10 with sequelae
of toxic epidermal necrolysis/StevensJohnson syndrome.
5
Briey, the procedure involves two stages. The rst involves a
buccal mucosal graft being transferred to the eye to replace
damaged conjunctiva with a vascularized graft (stage IA) and
harvesting of a tooth and adjacent bone which are cut to the
correct shape and size (about 10 15 255 mm thick); the
crown is removed, pulp removed, but periosteum retained, and
the dentine of the root is drilled to accommodate an optical cyl-
inder (stage IB); the tooth and optical cylinder are then placed
in a submuscular pouch (usually the lower lid of the other eye)
in order to allow soft tissue to invest into the bone pores of the
lamina, and to allow the lamina to recover from any thermal
damage due to the drilling process. The tooth is needed for sup-
port of the optical cylinder and is felt to integrate better than
nonbiological skirts made of materials such as Dacron. The
optical cylinder itself is made of polymethylmethacrylate, a
material that is highly resistant to scratching, and is biconvex-
ended to act as a lens that maximizes optical efcacy. The optical
aspects are described in more detail elsewhere.
4
Stages IA and IB
are sometimes performed separately to ensure mucosal graft
survival before harvesting a tooth. In stage II, 24 months later,
the tooth with its optical cylinder is retrieved and implanted
into the eye (Figs 1 and 2). This involves removal of the iris,
removal of the lens if present (to create aphakia), and the lamina
(a)
(b)
Fig 1. (a) Right-sided conjunctival scarring and left-sided prosthesis
in this patient. (b) Close-up of optical cylinder in situ.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
776 Correspondence
around the dentine support is then able to be sutured into posi-
tion (Fig. 2).
The main problems are potential technical difculties, infec-
tion, longer-term complications such as glaucoma, and, in situa-
tions such as cicatricial pemphigoid or a patient such as ours
with largely mucosal IgA-EBA, there is a potential problem of
obtaining an adequate nonscarred mucosal graft. Although the
eld of vision is reduced (to about 40) compared with the nor-
mal eye (about 160), this is a life-altering procedure for a dry
keratinized eye and should be more widely recognized by der-
matologists as a treatment option for such patients. IgA-EBA is a
rare condition, and blindness due to this has only been described
occasionally,
6,7
but it is a further indication for this procedure.
Acknowledgments
Many clinicians have seen this patient at various times and in
various parts of the country; we would like to thank all con-
cerned for their advice, especially Professor F. Wojnarowska,
Dr P. Frith and Mr J. Dart.
N. H. COX
M. A. BE ARN*
J . HE ROL D
G. AI NS WORTH
C. LI U
Departments of Dermatology and
*Ophthalmology, Cumberland Inrmary, Carlisle
CA2 7HY, U.K.
Department of Maxillofacial Surgery, Royal Sussex
County Hospital, Brighton, U.K.
Sussex Eye Hospital, Brighton, U.K.
E-mail: neil.cox@ncumbria-acute.nhs.uk
References
1 Cox NH. Vitamin E for dapsone-induced headache. Br J Dermatol
2002; 146:174 (Letter).
2 Chan LS, Cooper KD. Interferon alfa for linear IgA bullous dermato-
sis. Lancet 1992; 340:425.
3 Liu C, Sciscio A, Smith G et al. Indications and technique of modern
osteo-odonto-keratoprosthesis surgery. Eye News 1998; 5:1722.
4 Liu C, Paul B, Tandon R et al. The osteo-odonto-keratoprosthesis
(OOKP). Semin Ophthalmol 2005; 20:11328.
5 Falcinelli G, Falsini B, Taloni M et al. Modied osteo-odonto-kerato-
prosthesis for treatment of corneal blindness: long-term anatomical
and functional outcomes in 181 cases. Arch Ophthalmol 2005;
123:131929.
6 Bauer JW, Schaeppi H, Metze D et al. Ocular involvement in IgA-
epidermolysis bullosa acquisita. Br J Dermatol 1999; 141:88792.
7 Caux F, Kirtschig G, Lemarchand-Venencie F et al. IgA-epidermolysis
bullosa acquisita in a child resulting in blindness. Br J Dermatol 1997;
137:2705.
Conicts of interest: none declared.
A patient with alopecia, nail dystrophy,
palmoplantar hyperkeratosis, keratitis,
hearing difculty and micrognathia without
GJB2 or GJB6 mutations: a new type of
hidrotic ectodermal dysplasia?
DOI: 10.1111/j.1365-2133.2007.07752.x
SIR, Cloustons hidrotic ectodermal dysplasia is a rare autosomal
dominant ectodermal dysplasia characterized by hypotrichosis,
nail dystrophy and palmoplantar hyperkeratosis.
1
Teeth and
eccrine gland development are normal. Mutations in the gap
junction protein connexin 30 (GJB6 gene) have been reported
in patients of different ethnic origin.
2,3
We report a sporadic
case, presenting Cloustons hidrotic ectodermal dysplasia,
hypotrichosis, nail dystrophy and palmoplantar hyperkeratosis,
while having no mutation in GJB6 or GJB2 which encode conn-
exin 30 and 26, respectively.
A 31-year-old man had had alopecic regions on the scalp,
scant eyelashes and eyebrows, and micrognathia since his early
Buccal mucosal graft
Host cornea
Sclera
Host
conjunctiva
Aniridic
Aphakic
OOKP
lamina
Dentine
Alveolar
ligament
Bone
Cement
Optical cylinder
Vitreous
Fig 2. Diagram to show insertion of tooth
and optical cylinder. OOKP, osteo-odonto-
keratoprosthesis.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 777
childhood (Fig. 1a,b). At the age of 15 years, hearing difcul-
ties progressed in both ears, and hyperkeratosis occurred on
the palms and soles, especially on the weight-bearing area
(Fig. 1d). Longitudinal ssures and distal onycholysis appeared
both in ngernails and in toenails from his adolescence
(Fig. 1c). Congenital corneal opacity of the right eye was
diagnosed as a keratitis by the ophthalmologist. Hearing dif-
culty was diagnosed by an otologist as being conductive rather
than sensorineural. Teeth development, sweating, mental con-
dition and intelligence were apparently normal. There was no
family history of a similar clinical manifestation or of consan-
guineous marriage. Light microscopic examination of a skin
biopsy from the forearm revealed no abnormality in sweat
glands, epidermis or dermis.
After obtaining written informed consent, genomic DNA
was extracted from the patients broblasts (Qiagen, Hilden,
Germany). Genomic DNA from a Japanese man with no
apparent skin disease was used as a control. The coding exon
and anking regions of the GJB2 and GJB6 genes were ampli-
ed by polymerase chain reaction (PCR) using the specic
primers described previously.
2,4
PCR products were puried
using a QIAquick gel extraction kit (Qiagen) and directly
sequenced. We could identify no mutation in GJB2 or GJB6.
Mutations in GJB2 are responsible for the keratitis-ichthyo-
sis-deafness (KID) syndrome, Vohwinkel syndrome, Bart
Pumphrey syndrome and hystrix-like ichthyosis and deafness
syndrome.
4,5
Although our patient had keratitis and deafness,
no ichthyotic skin changes were present on the trunk and
extremities. Mutations in GJB6 are also responsible for a partic-
ular type of KID syndrome.
6
This might be due to a high
homology between GJB2 and GJB6, mutation of which is
responsible for Cloustons hidrotic ectodermal dysplasia.
Connexins are transmembrane proteins that assemble to
form hexameric aqueous channels or connexons in the cell
membrane.
7
Connexons in adjacent cells form an intercellular
passage, the gap junction. Gap junction assembly can be
heterotypical, with different connexins making up a connex-
on, or homotypical with the same connexon. Therefore, even
if a defect in a certain connexin takes place, other connexins
compensate for that connexin by forming a heterotypical
connexon assembly. This may explain why mutations in
GJB2 give rise to various types of diseases and why there are
sporadic cases without any similar symptoms in their
kindreds.
In summary, this patient had no mutation in GJB2 or GJB6
and his condition may be classied as another type of hidrotic
ectodermal dysplasia caused by an unknown gene.
M. NAKAMURA
O. I S HI KAWA
Department of Dermatology, Gunma University
Graduate School of Medicine, 3-39-22
Showamachi, Maebashi, Gunma 371-8511, Japan
E-mail: motonaka@med.gunma-u.ac.jp; motonaka@kuhp.kyoto-u.ac.jp
(a) (b)
(c)
(d)
Fig 1. Clinical appearance: (a) scant
eyebrows and micrognathia; (b) alopecia on
the scalp; (c) dystrophic nail and (d) plantar
hyperkeratosis on the weight-bearing area.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
778 Correspondence
References
1 Clouston HR. A hereditary ectodermal dystrophy. Can Med Assoc J
1929; 21:1831.
2 Lamartine J, Essenfelder GM, Kibar Z et al. Mutations in GJB6 cause
hidrotic ectodermal dysplasia. Nat Genet 2000; 26:1424.
3 Smith FJD, Morley SM, McLean WHI. A novel connexin 30 muta-
tion in Clouston syndrome. J Invest Dermatol 2002; 118:5302.
4 Richard G, White TW, Smith LE et al. Functional defects of Cx26
resulting from a heterozygous missense mutation in a family with
dominant deaf-mutism and palmoplantar keratoderma. Hum Genet
1998; 103:3939.
5 Richard G, Rouan F, Willoughby CE et al. De novo mutation in the
gene encoding connexin-26 (GJB-2) in a sporadic case of keratitis-
ichthyosis-deafness (KID) syndrome. Am J Hum Genet 1980;
70:13418.
6 Jan AY, Amin S, Ratajczak P et al. Genetic heterogeneity of KID syn-
drome: identication of a Cx30 gene (GJB6) mutation in a patient
with KID syndrome and congenital atrichia. J Invest Dermatol 2004;
122:110813.
7 van Steensel MAM. Gap junction diseases of the skin. Am J Med Genet
2004; 131C:1219.
Conicts of interest: none declared.
Successful treatment of scalp actinic keratoses
with photodynamic therapy using ambient
light
DOI: 10.1111/j.1365-2133.2007.07755.x
SIR, The prevalence of actinic keratoses (AKs) increases with
age and is a particular problem affecting the scalps of bald
elderly men. There are many effective treatments for AK,
1
but
they are not without side-effects and are limited in extensive
disease. Several studies have shown the benet and safety of
topical 5-aminolaevulinic acid photodynamic therapy (5-ALA
PDT) in patients with AKs, using a visible light source;
2
how-
ever, this can be a time- and resource-consuming procedure.
To simplify the procedure, we investigated the efcacy and
tolerability of ambient light in combination with 5-ALA PDT
in the treatment of this condition.
A 90-year-old man was under our care with multiple scalp
AKs. He had received treatment with 5-uorouracil ointment
and cryotherapy with some success, but had developed new
lesions. On examination he had multiple AKs on his balding
scalp. After ethical approval was given by the Leeds (West)
Ethics Committee, his scalp was photographed (Fig. 1a) and
each AK was graded; 1 mild (slightly palpable, more eas-
ily felt than seen), 2 moderate (moderately thick, easily
felt) or 3 severe (very thick and/or obvious AK).
3
5-ALA
cream (Crawford Pharmaceuticals, Milton Keynes, U.K.) was
applied at approximately 1 mm thickness to the whole of the
scalp, up to the anterior and temporoparietal hairlines, with
the patient then free to leave the clinic and go about his nor-
mal daily activities. He was asked not to cover his head unless
his scalp was uncomfortable and not to wash his scalp until
he returned a week later when a further treatment was pro-
posed. When he attended 1 week after the rst application of
5-ALA, the scalp was very inamed (Fig. 1b) and so treatment
was delayed a further week, when it was repeated, with a
third treatment performed another week later. The patient was
reviewed 10 weeks later and displayed an excellent response
(Fig. 1c), which was maintained 11 months later (Fig. 1d).
Prior to each treatment, the patient was asked to score
symptoms of erythema, dryness, desquamation, pigmentation,
blistering, stinging/burning and itching as 0 (none), 1
(mild), 2 (moderate) or 3 (severe), and scarring as yes or
no. These symptoms generally reduced over the treatment
period, other than dryness and desquamation. The total num-
ber of AKs, of all grades, fell by 61% during treatment and
the number of grade 2 AKs reduced by over 87% (Fig. 2).
However, there was a small increase in grade 1 lesions over
this period, probably because higher grade lesions reduced in
grade with treatment. The patient was asked to record any
symptoms affecting the scalp during the study period in a
diary and used terms such as burning sensation and itching
nearly unbearably in the days following treatment and my
scalpis far better than it has been for years after the nal
treatment. Our patient is still under follow-up and we have
advised him of the importance of sun protection, particularly
of the scalp.
The use of 5-ALA PDT in malignant and premalignant con-
ditions relies on adequate synthesis and accumulation of
protoporphyrin IX (PpIX) in the abnormal cells, allowing
selective photodestruction of those cells. For 5-ALA PDT, red
light matching the smaller absorption peak of PpIX centred
around 630 nm is often used for photoactivation, due to
greater tissue penetration of longer wavelength light. The
ground-level solar irradiance is highest around the 630 nm
absorption peak of PpIX (M.R. Stringer, personal communica-
tion) and so it would seem reasonable that irradiation of
5-ALA-induced PpIX with ambient light would lead to
adequate photoactivation.
Topical PDT with 5-ALA has been used successfully in
extensive scalp AKs;
2,3
subclinical lesions can be treated and
cure rates of 91% are quoted.
4
Although effective in many
conditions, a practical limitation of PDT is the delay between
application of the 5-ALA cream and irradiation with a light
source. Moseley et al.
5
recently piloted a study of ambulatory
PDT in the treatment of Bowens disease. Their results were
encouraging and may lead to wider use of this technique so
that more patients can be treated more conveniently and at
lower cost. In our case, the premise was even simpler and
cheaper: using ambient daylight in combination with topical
5-ALA, which led to an excellent cosmetic outcome. We chose
the summer period for the treatment as more ambient light
would be available and asked the patient to wear a hat if his
scalp became uncomfortable. Our patient did experience dis-
comfort, burning and desquamation during the rst week, but
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 779
these are all potential side-effects of other treatment modalities
such as topical 5-uorouracil and imiquimod.
We appreciate that there may be variability of response
depending on the level of ambient light that a patient is
exposed to, and that this is difcult to standardize. Clearly,
longer follow-up of this patient and a larger study of this
method of delivering PDT for scalp AKs is necessary before
nal conclusions can be made. This simple concept could lead
to a more cost-effective and efcient use of PDT in the treat-
ment of scalp AKs.
R. J . BAT CHE L OR
G. I . STAB L E S
M. R. ST RI NGE R*
Department of Dermatology,
Leeds General Inrmary,
Leeds LS1 3EX, U.K.
*Institute of Microwaves and Photonics,
School of Electronic and Electrical Engineering,
University of Leeds, Leeds LS2 9JT, U.K.
E-mail: rjbatchelor@doctors.org.uk
References
1 Kurwa HA, Yong-Gee SA, Seed PT et al. A randomised paired com-
parison of photodynamic therapy and topical 5-uorouracil in the
treatment of actinic keratoses. J Am Acad Dermatol 1999; 41:41418.
2 Markham T, Collins P. Topical 5-aminolaevulinic acid phototherapy
for extensive scalp actinic keratoses. Br J Dermatol 2001; 145:5024.
3 Freeman M, Vinciullo C, Francis D et al. A comparison of photo-
dynamic therapy using topical methyl aminolevulinate (Metvix)
with single cycle cryotherapy in patients with actinic keratosis: a
prospective, randomized study. J Dermatolog Treat 2003; 14:99106.
4 Jeffes EW, McCullough JL, Weinstein GD et al. Photodynamic ther-
apy of actinic keratosis with topical 5-aminolaevulinic acid. A pilot
dose-ranging study. Arch Dermatol 1997; 133:72732.
(a) (b)
(c) (d)
Fig 1. (a) Scalp pretreatment. (b) Scalp 1 week after rst treatment with 5-aminolaevulinic acid photodynamic therapy (5-ALA PDT). (c) Scalp
10 weeks after last treatment with 5-ALA PDT. (d) Scalp 11 months after last treatment with 5-ALA PDT.
20
15
10
5
N
u
m
b
e
r
o
f
l
e
s
i
o
n
s
0
Pre-treatment
Number and grade of actinic keratoses
pre- and post - treatment
Post-treatment
Grade 1
Grade 2
Grade 3
Fig 2. Number and grade of scalp actinic keratoses before and
10 weeks after treatment.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
780 Correspondence
5 Moseley H, Allen JW, Ibbotson S et al. Ambulatory photodynamic
therapy: a new concept in delivering photodynamic therapy. Br J
Dermatol 2006; 154:74750.
Conicts of interest: none declared.
Folliculotropic Sezary syndrome: a new variant
of cutaneous T-cell lymphoma
DOI: 10.1111/j.1365-2133.2007.07756.x
SIR, The new WHOEORTC (World Health Organization
European Organization for Research and Treatment of Cancer)
classication system for cutaneous lymphomas incorporates a
follicular variant of mycosis fungoides. Although it is consid-
ered a variant of classic mycosis fungoides, it is discussed sep-
arately because of its distinct clinicopathological features.
1
These features include the marked folliculotropism of lympho-
cytes, clinically resulting in follicular papules, cysts or alope-
cia. This variant of mycosis fungoides has been reported to
have a more aggressive clinical course than classic mycosis
fungoides and to be frequently refractory to standard therap-
ies.
2
Prognostic studies have shown 5- and 10-year survival
rates of 64% and 14%, respectively, similar to tumour-stage
mycosis fungoides.
2
Sezary syndrome is the leukaemic phase
of mycosis fungoides and also has a poor prognosis, with
medial survival of 23 years.
3
We report the clinical and histo-
pathological features of two patients from our multidiscipli-
nary cutaneous lymphoma clinic with a condition we refer to
as folliculotropic Sezary syndrome.
Patient 1. A 60-year-old white man was referred for a 3-year
history of persistent erythroderma. Numerous skin biopsies
from the last several years were interpreted as being nonspe-
cic and consistent with an eczematous process. The patient
was refractory to several therapies including etanercept, myco-
phenolate mofetil and acitretin with narrow-band ultraviolet
(UV) B radiation. There was 80% body surface area involve-
ment with erythroderma. Multiple coalescing follicular papules
were identied on the head and neck area (Fig. 1a). Several
larger lesions were also noted on the body. The facial skin
showed furrows and development of leonine facies. There was
no signicant lymphadenopathy. A blood cell count showed
an elevated white blood cell count of 280 10
9
L
)1
with
130 10
9
L
)1
lymphocytes. A Sezary count showed
120 10
9
L
)1
Sezary cells and T-cell receptor (TCR) analysis
showed a peripheral blood T-cell clone. Two skin biopsies
were performed. The rst was taken from an erythematous
plaque and the second from a follicular papule. The rst
biopsy showed an irregularly acanthotic epidermis with
hyperkeratosis and hypergranulosis. There were only rare
epidermotropic cells. The dermis contained a dense lichenoid
inammatory inltrate with > 50% of the cells consisting of
large irregular lymphocytes. The second biopsy showed an
unremarkable epidermis with multiple dilated follicular units
in the dermis. The follicles showed massive epidermotropism
of lymphocytes into the follicular epithelium (Fig. 1c,d). The
lymphocytes were small to intermediate in size with only
occasional larger cells. In both cases, the lymphocytes were
CD3+CD4+ with some loss of CD7. The cells were CD30).
The overlying interfollicular epidermis did not have epidermo-
tropic cells. A diagnosis of folliculotropic Sezary syndrome
was established and the patient was started on interferon
(IFN) at 12 10
6
units ve times weekly with PUVA (psora-
len with UVA) therapy, resulting in moderate improvement
over the last 6 months. The patients white blood cell count
has dropped to 120 10
9
L
)1
.
Patient 2. A 46-year-old African-American woman presented
with a 1-year history of erythroderma and follicular papules
on the face and body (Fig. 1b). Several palpable lymph nodes
approximately 2 cm in size were identied in the bilateral cer-
vical area. A skin biopsy showed psoriasiform hyperplasia of
the epidermis with mild spongiosis without exocytosis of
lymphocytes into the epidermis. There was a dense band-like
inltrate of lymphocytes in the underlying dermis with
> 50% of cells consisting of large atypical lymphocytes. A sec-
ond skin biopsy from a follicular papule showed an unremark-
able epidermis without epidermotropism. A dilated follicular
unit was noted with extensive folliculotropism of intermedi-
ate-sized irregular lymphocytes into the follicular epithelium.
In both biopsies, the tumour cells were CD3+CD4+ with
some loss of CD7. The cells were CD30). The patients white
blood cell count showed 40 10
9
L
)1
with > 10 10
9
L
)1
Sezary cells. Flow cytometry showed 23% of her peripheral
blood cells to be CD4+CD3+CD7) and TCR analysis showed
a peripheral blood T-cell clone. A diagnosis of folliculotropic
Sezary syndrome was established. The patient failed treatment
with acitretin (Soriatane
; Connetics Corp., Palo Alto, CA,
U.S.A.) and PUVA. An experimental protocol with lenalido-
mide and subsequent treatment with alemtuzumab resulted in
temporary improvement and subsequent relapse. She has
shown moderate improvement with high-dose IFN but contin-
ues to have signicant disease.
Mehta et al.
4
have recently reported one patient with both
follicular mycosis fungoides and Sezary syndrome. There
are only rare other reports in the literature of patients sus-
pected to have Sezary syndrome with folliculotropism.
Tremeau-Martinage et al.
5
reported a patient with folliculo-
tropic cutaneous lymphoma with CD30+ large cells and
circulating Sezary cells. This patient probably had folliculo-
tropic Sezary syndrome with CD30+ large cell transform-
ation. Interestingly, both of our patients had biopsies from
nonfollicular areas showing prominent large cells. In 1982,
Westfried et al.
6
also described a patient with Sezary syn-
drome and follicular papules. However, the biopsy only
showed a nondiagnostic suppurative folliculitis. This patient
had a rapid course and died within 2 years of presentation.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 781
(a) (b)
(c)
(d)
Fig 1. (a) Patient 1 with erythroderma, folliculotropic papules of the head and neck, deep facial furrows, rhinophyma-like changes of the nose
and leonine facies. (b) Patient 2 with erythroderma, follicular papules and alopecia of scalp and eyebrow areas. (c) Section showing a large dilated
follicular unit distended by mucin and inltrated by lymphocytes. The adjacent interfollicular epithelium is uninvolved. Haematoxylin and eosin;
original magnication 40. (d) Section at higher magnication showing prominent inltration of lymphocytes into the follicular epithelium.
Haematoxylin and eosin; original magnication 100.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
782 Correspondence
There are also two reports in the literature of patients with
Sezary syndrome with follicular mucinosis. These patients
could also be classied as having folliculotropic Sezary syn-
drome.
7,8
Additionally, in the study of 51 patients with fol-
licular mycosis fungoides by van Doorn et al.,
2
three patients
had erythroderma. However, it is not mentioned whether
these patients had the blood criteria for Sezary syndrome.
The two patients we report here have Sezary syndrome with
prominent folliculotropism.
It is important to characterize this unique group of
patients with folliculotropic Sezary syndrome for several rea-
sons. These patients have two variations of cutaneous T-cell
lymphoma (CTCL)folliculotropism and leukaemic involve-
mentwhich have both been associated with a more
aggressive clinical course and are known to be recalcitrant to
skin-directed therapies used in classical mycosis fungoides.
Additionally, the presence of folliculotropism in Sezary
syndrome further emphasizes the fact that mycosis fung-
oides and Sezary syndrome are part of the same disease
spectrum.
Clinically, both patients were characterized by advanced
disease at the time of presentation and poor response to
a variety of treatments. Interestingly, the patient reported
by Mehta et al.
4
also presented after only 4 months with
advanced disease involving both the bone marrow and
lymph nodes. The patient described by Tremeau-Martinage
et al.,
5
if truly a case of folliculotropic Sezary syndrome,
had CD30+ large cell transformation at the time of presen-
tation, which is also consistent with an advanced state of
disease at the time of presentation. As mentioned above,
the patient reported by Westfried et al.
6
died within 2 years
of the initial presentation. Follow-up data on other patients
were not available.
In regards to treatment, it is possible that the deep follicular
epithelium serves as a sanctuary for lymphoma cells, making
them relatively inaccessible to skin-targeted therapy. However,
it remains to be determined if patients with folliculotropic
Sezary syndrome have a worse overall survival than other
patients with Sezary syndrome. Both of our patients are still
alive with persistent disease at 5 and 2 years, respectively,
from the time of presentation, although both have received
aggressive treatment.
The histological ndings in folliculotropic Sezary syndrome
are dependent on the site of biopsy. In both of our patients
where nonfollicular areas were biopsied the changes were
those of irregular acanthosis overlying a dense lichenoid inl-
trate without epidermotropism. These changes are probably
related to severe pruritus associated with both follicular myco-
sis fungoides and Sezary syndrome. However, in both patients
> 50% of the lymphoid cells were atypical and large. This
coincides with the tendency to present with advanced disease
both clinically and histologically.
Biopsy of follicular papules shows lymphocytes inltrating
the follicular epithelium with or without follicular mucino-
sis. In our patients, the epidermis adjacent to the follicular
epithelium was not inltrated by lymphocytes. Patients with
Sezary syndrome frequently have nonspecic biopsy changes
and seldom have signicant epidermotropism or Pautriers
abscesses. Similarly, in the largest series to date on follicular
mycosis fungoides, only ve of 51 patients showed epider-
motropism of the nonfollicular epithelium.
2
This lack of
epidermotropism is common in both conditions, Sezary syn-
drome and follicular mycosis fungoides,
9
making the histo-
logical diagnosis difcult if a follicle is not part of the
sampled specimen.
In summary, we have known for some time that features
of mycosis fungoides and Sezary syndrome can coexist in
patients with CTCL. Now, we introduce the concept of folli-
culotropism in association with Sezary syndrome. These
reports support the concept that CTCL is a disease entity of
skin-homing lymphocytes, which in the majority of patients
features epidermotropism of lymphocytes into the overlying
epidermis but can also show follicultropism into the follicu-
lar epithelium. Hence, we believe that CTCL is a valid unify-
ing concept incorporating mycosis fungoides, follicular
mycosis fungoides, Sezary syndrome and folliculotropic
Sezary syndrome.
P. GE RAMI
J . GUI TART
Northwestern University and the Feinberg
School of Medicine, 676 N.
St Claire Street, Chicago, IL 60611, U.S.A.
E-mail: pgerami@nmff.org
References
1 Willemze R, Jaffe E, Burg G et al. WHOEORTC classication for
cutaneous lymphoma. Blood 2005; 105:376885.
2 van Doorn R, Scheffer E, Willemze R. Follicular mycosis fungoides,
a distinct disease entity with or without associated follicular
mucinosis: a clinicopathologic and follow-up study of 51 patients.
Arch Dermatol 2002; 138:1918.
3 Klemke C, Mansmann U, Poenitz N et al. Prognostic factors
and prediction of prognosis by the CTCL Severity Index in myco-
sis fungoides and Sezary syndrome. Br J Dermatol 2005; 153:118
24.
4 Mehta A, Dhungel B, Khan MF. Mycosis fungoides/Sezary
syndrome: report of an unusual case. J Cutan Pathol 2006; 33:
1215.
5 Tremeau-Martinage C, Gorguet B, Lamant L et al. CD30 positive
pilotropic lymphoma. Ann Dermatol Venereol 1999; 126:4348.
6 Westfried M, Rosenthal JC, Coppola A, Rapp Y. Sezary syndrome
presenting as a follicular dermatosis. Cutis 1982; 29:3902.
7 LeBoit PE, Abel EA, Cleary ML et al. Clonal rearrangement of
the T cell receptor beta gene in the circulating lymphocytes
of erythrodermic follicular mucinosis. Blood 1988; 71:1329
33.
8 Rivers JK, Norris PG, Greaves MW, Smith NP. Follicular mucinosis
in association with Sezary syndrome. Clin Exp Dermatol 1987;
12:20710.
9 Cerroni L, Fink-Puches R, Back B, Kerl H. Follicular mucinosis: a
critical reappraisal of clinicopathologic features and association
with mycosis fungoides and Sezary syndrome. Arch Dermatol 2002;
138:1829.
Conicts of interest: none declared.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 783
Bortezomib-associated rash: a new
recognizable and avoidable side-effect
DOI: 10.1111/j.1365-2133.2007.07757.x
SIR, For several decades, the therapeutic management of mul-
tiple myeloma has mainly involved regimens based on the use
of glucocorticoids, cytotoxic chemotherapeutics and blood
stem cell transplantation. New strategies in the treatment of
relapsed multiple myeloma have been developed with the
introduction of a new class of antineoplastic agents known as
proteasome inhibitors. These drugs, which are being studied
as a form of therapy for a wide variety of cancers, appear to
act directly on important intracellular processes, such as the
nuclear factor jB pathway. Bortezomib (Velcade
; Millennium
Pharmaceuticals, Inc., Cambridge, MA, U.S.A.) is the rst of
these proteasome inhibitors to be approved for the treatment
of refractory multiple myeloma.
1,2
We describe a patient with
relapsed multiple myeloma who developed a peculiar rash
after bortezomib treatment.
In June 2002, a 59-year-old man had been diagnosed with
stage IIIA IgG k multiple myeloma. The patient was treated
with four cycles of VAD (vincristine, adriamycin, dexametha-
sone) followed by autologous peripheral blood stem cell
transplantation with complete remission being achieved
according to the European Group for Blood and Marrow
Transplantation (EBMT) criteria.
3
In April 2006, the patient
had progression of multiple myeloma and a second-line treat-
ment with bortezomib was started at a dose of 13 mg m
)2
on days 1, 4, 8 and 11, every 21 days. The rst cycle was
well tolerated. On day 4 of the second cycle, several painless
erythematous nodules, which were not associated with fever
or itching, developed on his trunk, back and neck (Fig. 1a).
Skin biopsy was obtained for histological examination and
showed a perivascular and periadnexal lymphoid inltrate.
Hydropic degeneration of basal cells with isolated necrotic
keratinocytes was also observed (Fig. 1b).
The rash resolved within 3 days after treatment with predni-
sone (30 mg daily) and hydroxyzine (25 mg every 12 h).
After resolution of the rash, prednisone was discontinued. On
day 2 of the third cycle, the rash reappeared in the same
location, this time more severe and widespread, and resolved
after 7 days of treatment with prednisone and hydroxyzine. To
prevent recurrence of the rash, intravenous premedication with
dexamethasone (20 mg) and chlorpheniramine (5 mg) before
every infusion of bortezomib was administered from the
fourth cycle onwards. The bortezomib-associated rash (BAR)
did not recur in subsequent cycles with this premedication. A
partial response after eight cycles was obtained with respect to
the patients multiple myeloma according to EBMT criteria.
3
Bortezomib is generally well tolerated and does not have
the severe systemic side-effects usually seen with other cyto-
toxic drugs. Most of the side-effects of bortezomib are mild to
moderate. The most common side-effects were asthenia,
gastrointestinal symptoms, thrombocytopenia and peripheral
neuropathy, with the latter usually being reversible.
4
Cutane-
ous eruption is a relatively common toxicity seen in patients
with multiple myeloma treated with bortezomib, but it has
not been well characterized. Moreover, most of the reported
cases lack histological conrmation. Where reported, its inci-
dence in clinical trials ranged from 8% to 18%.
4
Typically,
skin lesions induced by bortezomib are characterized by a ma-
culopapular or nodular rash located on the back, trunk and
face.
59
BAR is usually asymptomatic and not associated with
constitutional symptoms. In the majority of cases, the rash
appeared after at least two cycles of bortezomib,
8
typically
during the second cycle, and recurred with more severity with
subsequent cycles. It usually resolved with a combination of
systemic corticosteroids and antihistamines.
57,9
Spontaneous
recovery has also been described.
9
The severity of BAR usually
does not lead to modication of the standard dose regimen or
to prompt cessation of drug usage. It does not appear to be
dose dependent.
8
To prevent the recurrences, it is usually
necessary to administer systemic corticosteroids before every
infusion of bortezomib.
5,7
The role of antihistamines as pre-
medication remains unclear.
5
Although the clinical appearance is very similar in all cases,
biopsies of skin lesions show heterogeneous histological
(a)
(b)
Fig 1. (a) Several painless erythematous nodules on the back.
(b) Photomicrograph of punch biopsy showing a perivascular and
interface inammatory pattern mainly composed of lymphocytes.
Haematoxylin and eosin; original magnication 40.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
784 Correspondence
features. The characteristic features are the presence of a peri-
vascular and periadnexal inammatory inltrate throughout
the dermis, a varying degree of interface dermatitis and scat-
tered dyskeratotic keratinocytes within the epidermis. In add-
ition, our review of the literature revealed that the previously
described cases of BAR can also be subdivided into two
groups: those with an inammatory inltrate mainly com-
posed of lymphocytes
5,7
and those with a predominance of
neutrophils and features of leucocytoclastic vasculitis.
6,8,9
The
signicance of these two different histological patterns remains
unclear but, notably, they do not seem to result in differences
in clinical features. Nevertheless, the small number of histo-
logically examined cases precludes the drawing of denitive
conclusions, and therefore further reports are needed to clarify
their true signicance.
A phase II study in 140 patients with non-Hodgkin lymph-
oma has suggested a correlation between the development of
BAR and the antineoplastic efcacy of the drug.
8
Prospective
randomized studies are needed to conrm the relationship
between the rash and clinical benet.
As use of these agents becomes more prevalent, it is crucial
to be familiar with cutaneous side-effects associated with this
new class of antineoplastic agents to assess and manage these
patients properly.
B. VI L L ARRUB I A*
I . BE T L L OCH
J . MAT AI X
A. LUCAS
C. BOTE L L A*
Departments of Dermatology and
*Haematology, Hospital General de Alicante,
Avenida Pintor Baeza s/n, Alicante 03010, Spain.
Correspondence: J. Mataix.
E-mail: mataixdiaz@hotmail.com
References
1 Richardson PG, Barlogie B, Berenson J et al. A phase 2 study of bor-
tezomib in relapsed, refractory myeloma. N Engl J Med 2003;
348:260917.
2 Richardson PG, Sonneveld P, Schuster MW et al. Bortezomib or
high-dose dexamethasone for relapsed multiple myeloma. N Engl J
Med 2005; 352:248798.
3 Blade J, Samson D, Reece D et al. Criteria for evaluating disease
response and progression in patients with multiple myeloma treated
by high-dose therapy and haemopoietic stem cell transplantation.
Br J Haematol 1998; 102:111523.
4 Kane RC, Farrel AT, Sridhara R, Pazdur R. United States Food and
Drug Administration approval summary: bortezomib for the treat-
ment of progressive multiple myeloma after one prior therapy.
Clin Cancer Res 2006; 12:295560.
5 Pour L, Hajek R, Zdenek A et al. Skin lesions induced by bortezomib.
Haematologica 2005; 90:10.
6 Agterof MJ, Biesma DH. Images in clinical medicine. Bortezomib-
induced skin lesions. N Engl J Med 2005; 352:2534.
7 Wu KL, Heule F, Lam K, Sonneveld P. Pleomorphic presentation of
cutaneous lesions associated with the proteasome inhibitor bortez-
omib in patients with multiple myeloma. J Am Acad Dermatol 2006;
55:897900.
8 Gerecitano J, Goy A, Wright J et al. Drug-induced cutaneous vasculi-
tis in patients with non-Hodgkin lymphoma treated with the novel
proteasome inhibitor bortezomib: a possible surrogate marker of
response? Br J Haematol 2006; 134:3918.
9 Min CK, Lee S, Kim YJ et al. Cutaneous leucoclastic vasculitis (LV)
following bortezomib therapy in a myeloma patient; association
with pro-inammatory cytokines. Eur J Haematol 2006; 76:2658.
Conicts of interest: none declared.
Primary cutaneous peripheral T-cell lymphoma,
unspecied, that completely regressed after
skin biopsy
DOI: 10.1111/j.1365-2133.2007.07751.x
SIR, We read with interest the report by Kamiya et al.
1
descri-
bing two patients with the small cell variant of CD30+ pri-
mary cutaneous T-cell lymphoma whose lesions regressed
completely after incisional skin biopsies. The authors sugges-
ted that even primary cutaneous T-cell lymphomas without
anaplastic large cell cytology should be immunohistochem-
ically examined for expression of CD30 as CD30+ lymphomas
have a very favourable prognosis when conned to the skin.
However, such good prognosis and spontaneous or biopsy-
induced resolution may not be conned to CD30+ lympho-
mas. We report a case of primary cutaneous peripheral T-cell
lymphoma, unspecied type, that was CD30) but that also
underwent complete regression after a skin biopsy.
A 31-year-old woman presented with a 3-month history of
a rapidly enlarging asymptomatic nodule on her central fore-
head (Fig. 1). There was no history of preceding trauma and
the patient was systemically well. On examination, a soft, non-
tender, noncompressible, dome-shaped erythematous nodule
12 cm in diameter and studded with tiny yellow follicular
structures was seen on her central forehead (Fig. 1a). Systemic
examination was normal and there was no palpable lymph-
adenopathy. A 4-mm punch biopsy showed normal epidermis
overlying a narrow Grenz zone. The entire dermis was occu-
pied by a dense inltrate comprising small lymphocytes and
scattered blast cells. Dilated, and in places keratin-plugged, fol-
licles were present, some with mild focal epitheliotropism by
lymphoid cells. Immunohistochemistry showed strong CD2
and CD5, and weaker CD3, staining, conrming that the inl-
trate contained T cells with varied size, some being large and
blastic. Five to ten per cent of nuclei expressed Ki-67. The
atypical cells also expressed BCL2, CD4, CD45RO (weaker) and
there was heterogeneous expression of CD23. Specic negative
stains were CD30, CD10, BCL6, cyclin D1, S100, cytokeratins
and perforin. The only CD8 expression was in some small reac-
tive T cells, and few B cells were identied. The best-t diag-
nosis in the WHOEORTC (World Health Organization
European Organization for Research and Treatment of Cancer)
classication
2
was primary cutaneous peripheral T-cell lymph-
oma, unspecied (most cells being small to medium size, pleo-
morphic, but without a cytotoxic phenotype). Full blood count
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 785
and routine blood biochemistry including b2 microglobulin
were normal. Serum lactate dehydrogenase (LDH) was raised
at 801 IU L
)1
(normal 285577 IU L
)1
). A computed tomo-
graphic scan of neck, chest, abdomen and pelvis was normal.
Following skin biopsy, the nodule spontaneously and steadily
decreased in size and completely regressed within 2 months,
leaving macular pigmentation. Repeat LDH measurement at this
time was 564 IU L
)1
(just within normal range). The follicular
prominence remains, although the lesion is at and pale
(Fig. 1b).
Bekkenk et al. studied the characteristics of peripheral cuta-
neous T-cell lymphomas, unspecied, and analysed the prog-
nostic factors in a group of 82 patients.
3
It was found that
primary cutaneous small- to medium-sized T-cell lymphomas
had a much better prognosis than either primary cutaneous
CD30) large T-cell lymphomas or than patients presenting
with both cutaneous and extracutaneous disease. Complete
spontaneous resolution was noted in three of 82 lesions.
However, trauma-induced resolution of peripheral cutaneous
T-cell lymphoma, unspecied, has not been previously de-
scribed. It is possible that trauma of punch biopsy may have
initiated resolution of our patients lesion.
Acknowledgments
We are grateful to the pathologists involved: Drs S. Mathews,
M. Gangopadhyay and B.S. Wilkins.
V. MADAN
N. H. COX
Department of Dermatology,
Cumberland Inrmary, Carlisle CA2 7HY, U.K.
Correspondence: Neil Cox.
E-mail: neil.cox@ncumbria-acute.nhs.uk
References
1 Kamiya T, Saga K, Yanagisawa K et al. Small cell variant of CD30+
primary cutaneous T-cell lymphoma with epidermotropism that
completely regressed after incisional skin biopsy. Br J Dermatol 2006;
155:4847.
2 Slater DN. The new World Health OrganizationEuropean Organiza-
tion for Research and Treatment of Cancer classication for cutane-
ous lymphomas: a practical marriage of two giants. Br J Dermatol
2005; 153:87480.
3 Bekkenk MW, Vermeer MH, Jansen PM et al. Peripheral T-cell
lymphomas unspecied presenting in the skin: analysis of prognos-
tic factors in a group of 82 patients. Blood 2003; 102:221319.
Conicts of interest: none declared.
Do we need a revised public health policy on
sun exposure?
DOI: 10.1111/j.1365-2133.2007.07758.x
SIR, We read Professor Diffeys article
1
with interest. However,
we were surprised at his apparent scepticism of the reported
protective effect of sun exposure on systemic cancer and the
implication that sunlight exposure in the U.K. results in ade-
quate vitamin D
3
status. We believe that such views may lead
to complacency about vitamin D
3
status in the U.K.
Professor Diffey does not directly challenge the validity of
studies showing a protective effect of sun exposure but presents
opposing evidence with a geographical comparison of occur-
rence/mortality of carcinoma of the breast, prostate and colon.
While Australia is at a lower latitude and exposed to higher solar
ultraviolet (UV) B irradiation than the U.K., there is no apparent
protective effect on these cancers. However, we have performed a
literature search revealing 20 formal epidemiological studies of
geographical associations (latitude, region, air pollution, season,
measured annual solar energy and sun exposure questionnaire)
with occurrence/mortality of one or more of these cancers.
221
In 18 papers there was a favourable association, statistically
signicant in 15, and no association in two.
Professor Diffey further argues that since 1975 the inci-
dence of certain systemic cancers in the U.K. has increased
despite increasing sun exposure of the population, as evi-
denced by the increasing incidence of malignant melanoma
(MM). MM incidence is a dubious marker of UVB exposure
and there is evidence that both the incidence
22
and mortality
23
of MM are related to UVA, which does not induce cutaneous
synthesis of vitamin D
3
, rather than UVB exposure. An alter-
(a)
(b)
Fig 1. Forehead nodule (a) before and (b) 2 months after punch
biopsy.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
786 Correspondence
native possibility is that effective UVB exposure has in fact
been decreasing from increased sun protection.
In debating the effects of sun exposure, it is important to
not lose sight of the central issue, i.e. vitamin D
3
status,
which, alternatively, may be enhanced by vitamin D
3
supple-
mentation. Professor Diffey expresses no view on the protect-
ive role of vitamin D
3
in cancer. There is very strong
evidence, in addition to epidemiological sun exposure data,
based on the laboratory demonstration of relevant effects on
cellular growth, differentiation, apoptosis, malignant cell inva-
sion and metastasis, and the associations of occurrence/
outcome of cancers with functional polymorphisms of the
vitamin D receptor and serum 25(OH)D
3
levels.
24
With regard to the second point, Professor Diffey implies
that the vitamin D
3
status in the U.K. is adequate: we receive
more than enough sun exposure during recreational activities.
His evidence is based on estimates of the standard erythemal
dose based on estimates of time spent outside and estimates of
areas of exposure but does not state whether these exposure
times and areas are compatible with the SunSmart guidelines.
25
An area of doubt is his elective exposure, which includes
sun exposure during weekends and holidays, when an appre-
ciable area of the body surface is likely to be exposed for one
or more hours in largely unshaded sunshine. He also advo-
cates lunch-time exposure during the working week, i.e. at a
time when the SunSmart message is to stay in the shade. Profes-
sor Diffeys estimates of the adequacy of current sun exposure
to maintain vitamin D
3
status may or may not be accurate.
What is necessary is hard evidence based on serum 25(OH)D
3
levels. Such evidence has recently been reported from the
U.S.A., much of which is situated at a lower latitude than the
U.K., concluding that a majority of Americans receive insuf-
cient solar UV to maintain vitamin D
3
status even if not using
sunscreen.
26
Furthermore, there is evidence that however ade-
quate vitamin D
3
status may be in the summer in the U.K.,
winter levels are inadequate. A recent study showed that mor-
tality was greater from breast and lung cancer if presenting in
the winter.
21
There is also good evidence in older patients in
the U.K. of inadequate vitamin D
3
status.
27,28
It is salutary to consider that skin cancer, of all types, causes
15% of all cancer deaths in the U.K. while the above mentioned
three major cancers cause 25%. A 1% increase in mortality
would cause 388 deaths in these cancers, compared with 23
from skin cancer (using Cancer Research UK data from 2004
29
).
A recent large study, in which serum 25(OH)D
3
was predicted
from a multivariate 25(OH)D
3
intake model, estimated that an
increase of 17% in total cancer incidence and 29% in mortality
is associated with a decrease of 25 nmol L
)1
(10 ng mL
)1
) in
serum 25(OH)D
3
.
30
Similarly, a recent analysis of four reported
observational studies of colon cancer risk and serum 25(OH)D
3
found that a 50% increase in incidence was associated with a
decrease of 21 ng mL
)1
(from 33 ng mL
)1
).
31
If current expos-
ure is not adequate and there is no vitamin D
3
supplementation,
then serious implications on total cancer mortality are likely.
Professor Diffeys estimates of vitamin D
3
synthesis ade-
quacy are perhaps optimistic for the general public but there
must be real concerns about skin cancer patients, particularly
older patients with multiple solar keratoses/squamous cell car-
cinomas who are advised to rigorously avoid sunshine. We
believe that vitamin D
3
status should be investigated in these
individuals, with vitamin D
3
supplementation as necessary.
In summary we believe that vitamin D
3
status is a central
issue. There is good evidence that sun exposure is protective
against internal cancer, most authors favouring vitamin D
3
as
the intermediary, and Professor Diffeys contrary evidence is
unconvincing. Evidence is needed that most individuals are
receiving his assumed sun exposures, that these are within the
SunSmart guidelines and that vitamin D
3
status is adequate from
such exposure. Misplaced complacency about vitamin D
3
status
will have serious implications on total cancer mortality.
P. E. HUTCHI NS ON
J . E. OS B ORNE
Department of Dermatology,
Leicester Royal Inrmary,
University Hospitals of Leicester,
Inrmary Square, Leicester LE1 5WW, U.K.
Correspondence:
E-mail: dermat@doctors.org.uk
References
1 Diffey B. Do we need a revised public health policy on sun exposure?
Br J Dermatol 2006; 154:104651.
2 Garland CF, Garland FC. Do sunlight and vitamin D reduce the
likelihood of colon cancer? Int J Epidemiol 1980; 9:22731.
3 Gorham ED, Garland CF, Garland FC. Acid haze air pollution and
breast and colon cancer mortality in 20 Canadian cities. Can J Public
Health 1989; 80:96100.
4 Garland C, Garland F, Gorham E. Sunlight, sulfur dioxide and breast
and colon cancer in Italy. In: Proceedings of the San Diego Research Exchange,
April 1989. La Jolla, CA: University of California San Diego, 1989.
5 Garland FC, Garland CF, Gorham ED et al. Geographic variation in
breast cancer mortality in the United States: a hypothesis involving
exposure to solar radiation. Prev Med 1990; 19:61422.
6 Gorham ED, Garland FC, Garland CF. Sunlight and breast cancer
incidence in the USSR. Int J Epidemiol 1990; 19:8204.
7 Schwartz GG, Hulka BS. Is vitamin D deciency a risk factor for
prostate cancer? (Hypothesis). Anticancer Res 1990; 10:130711.
8 Hanchette CL, Schwartz GG. Geographic patterns of prostate cancer
mortality. Evidence for a protective effect of ultraviolet radiation.
Cancer 1992; 70:28619.
9 John EM, Schwartz GG, Dreon DM, Koo J. Vitamin D and breast
cancer risk: the NHANES I Epidemiologic follow-up study, 1971
1975 to 1992. National Health and Nutrition Examination Survey.
Cancer Epidemiol Biomarkers Prev 1999; 8:399406.
10 Luscombe CJ, French ME, Liu S et al. Prostate cancer risk: asso-
ciations with ultraviolet radiation, tyrosinase and melanocortin-1
receptor genotypes. Br J Cancer 2001; 85:15049.
11 Freedman DM, Dosemeci M, McGlynn K. Sunlight and mortality
from breast, ovarian, colon, prostate, and non-melanoma skin can-
cer: a composite death certicate based casecontrol study. Occup
Environ Med 2002; 59:25762.
12 Grant WB. An estimate of premature cancer mortality in the U.S.
due to inadequate doses of solar ultraviolet-B radiation. Cancer
2002; 94:186775.
13 Grant WB. An ecologic study of dietary and solar ultraviolet-B links
to breast carcinoma mortality rates. Cancer 2002; 94:27281.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 787
14 John EM, Dreon DM, Koo J et al. Residential sunlight exposure is
associated with a decreased risk of prostate cancer. J Steroid Biochem
Mol Biol 2004; 8990:54952.
15 Grant WB. A multicountry ecologic study of risk and risk reduction
factors for prostate cancer mortality. Eur Urol 2004; 45:2719.
16 Robsahm TE, Tretli S, Dahlback A et al. Vitamin D3 from sunlight
may improve the prognosis of breast-, colon- and prostate cancer
(Norway). Cancer Causes Control 2004; 15:14958.
17 Mizoue T. Ecological study of solar radiation and cancer mortality
in Japan. Health Phys 2004; 87:5328.
18 Moan J, Porojnicu AC, Robsahm TE et al. Solar radiation, vitamin D
and survival rate of colon cancer in Norway. J Photochem Photobiol B
2005; 78:18993.
19 Grant WB, Garland CF. The association of solar ultraviolet B (UVB)
with reducing risk of cancer: multifactorial ecologic analysis
of geographic variation in age-adjusted cancer mortality rates.
Anticancer Res 2006; 26:268799.
20 Colli JL, Colli A. International comparisons of prostate cancer
mortality rates with dietary practices and sunlight levels. Urol Oncol
2006; 24:18494.
21 Lim HS, Roychoudhuri R, Peto J et al. Cancer survival is dependent
on season of diagnosis and sunlight exposure. Int J Cancer 2006;
119:15306.
22 Moan J, Dahlback A, Setlow RB. Epidemiological support for an
hypothesis for melanoma induction indicating a role for UVA
radiation. Photochem Photobiol 1999; 70:2437.
23 Garland CF, Garland FC, Gorham ED. Epidemiologic evidence for
different roles of ultraviolet A and B radiation in melanoma mor-
tality rates. Ann Epidemiol 2003; 13:395404.
24 Osborne JE, Hutchinson PE. Vitamin D and systemic cancer: is this
relevant to malignant melanoma? Br J Dermatol 2002; 147:197213.
25 See http://info.cancerresearchuk.org/healthyliving/sunsmart/ (acces-
sed 22 November 2006).
26 Godar DE, Grant WB, Holick MF. Solar UV doses of adult Ameri-
cans are insufcient for sufcient vitamin D3 production. In:
Conference Proceedings of the Thirteenth Workshop on Vitamin D. Victoria, BC,
Canada: 2006; 156.
27 Hirani V, Primatesta P. Vitamin D concentrations among people
aged 65 years and over living in private households and institutions
in England: population survey. Age Ageing 2005; 34:48591.
28 Burleigh E, Potter J. Vitamin D deciency in outpatientsa Scottish
perspective. Scott Med J 2006; 51:2731.
29 Cancer Research UK. UK cancer mortality statistics. Available at http://
info.cancerresearchuk.org/cancerstats/mortality/?a 5441
(accessed 22 November 2006).
30 Giovannucci E, Liu Y, Rimm EB et al. Prospective study of predic-
tors of vitamin D status and cancer incidence and mortality in
men. J Natl Cancer Inst 2006; 98:4519.
31 Gorham ED, Garland CF, Garland FC et al. Vitamin D and prevention
of colorectal cancer. J Steroid Biochem Mol Biol 2005; 97:17994.
Conicts of interest: none declared.
Do we need a revised public health policy on
sun exposure? Response from Brian Diffey
DOI: 10.1111/j.1365-2133.2007.07759.x
SIR, I thank Drs Hutchinson and Osborne for their comments
on my article.
1
My purpose in comparing cancer incidence between northern
Europe and Australasia was not to dismiss any possible protect-
ive role of sun exposure in some systemic cancersindeed I
acknowledged this possibilitybut simply to show by applica-
tion of Ockhams razor that the association is by no means obvi-
ous and we should not interpret recent (and accumulating)
casecontrol studies as a licence for indiscriminate exposure.
Drs Hutchinson and Osborne are being a little mischievous
when they suggest that I am implying that vitamin D
3
status in
the U.K. is adequate simply because we receive more than
enough sun exposure during our recreational activities in the
summer months. In my article I make it absolutely clear that in
the winter months there is insufcient ambient ultraviolet light
to synthesize vitamin D
3
, especially when low ambient temper-
atures mean it is unlikely that anything more than the hands
and face will be exposed when outdoors. The point I stress is
that our current sun exposure pattern is not sufcient to main-
tain adequate vitamin D
3
levels, notwithstanding that the deni-
tion of adequate remains uid. But simply tinkering with
SunSmart messages
2
is unlikely to alter this given our latitude, cli-
mate and overwhelmingly indoor and time-pressured lifestyle.
Contrary to their interpretation, my article did not advocate
year-round compliance with SunSmart messages, but rather
stressed the need for avoiding excessive exposure in strong
sunshine coupled with a relaxed approach to sun exposure at
other times of the year, a view I have consistently expressed
in the pages of this journal for almost a decade.
3,4
B. DI F F E Y Regional Medical Physics Department,
Newcastle General Hospital, Newcastle NE4 6BE, U.K.
Correspondence:
E-mail: b.l.diffey@ncl.ac.uk
References
1 Diffey BL. Do we need a revised public health policy on sun exposure?
Br J Dermatol 2006; 154:104651.
2 http://info.cancerresearchuk.org/healthyliving/sunsmart/ (accessed
on 22 November 2006).
3 Diffey BL. Sun protection: have we gone too far? Br J Dermatol 1998;
138:5623.
4 Diffey BL. Is daily use of sunscreens of benet in the UK? Br J Dermatol
2002; 146:65962.
Conicts of interest: none declared.
Allergic contact dermatitis complicating
pustular psoriasis in two patients
DOI: 10.1111/j.1365-2133.2007.07776.x
SIR, Psoriasis, including its pustular form, can be triggered or
exacerbated by many endogenous and exogenous factors. We
describe two patients with long-standing pustular psoriasis
who developed coexistent allergic contact dermatitis (ACD).
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
788 Correspondence
Avoidance of the relevant allergens led to improvement in the
control of their pustular psoriasis.
Patient 1. A 35-year-old woman with life-long pustular psoria-
sis was patch tested due to a history of irritation from certain
topical products including Cetraben
(Sankyo, Amersham,
U.K.) cream and an associated are of facial and scalp psoria-
sis. She was tested to an extended British Contact Dermatitis
Society (BCDS) standard series, a medicament and hairdressing
series, and her own products. She had positive reactions to
fragrance mix 1, sorbitan sesquioleate, eugenol, isoeugenol,
amylcinnamaldehyde and Cetraben
cream (as is). These were
all of past and current relevance to her psoriasis treatment,
being present in shampoo, cosmetics and plug-in air freshener
used at home. Further testing to the individual constituents of
Cetraben
cream was negative, suggesting a compound allergy
to Cetraben
. Avoidance of the allergens led to improvement
of her facial and scalp inammation.
Patient 2. A 51-year-old man had a 30-year history of general-
ized pustular psoriasis requiring several systemic therapies
including acitretin and methotrexate, and repeated hospital
admissions due to recurrent ares of pustular psoriasis at ex-
ural sites, mainly the groin and inner thighs. He was patch
tested to an extended BCDS standard series and a medicament
and textile series. He had positive reactions to wool alcohols,
amerchol, parabens, ethylenediamine, nystatin, framycetin,
budesonide and hydrocortisone 17-butyrate (relevant to cur-
rent and previous topical treatments), and positive reactions to
disperse blue dyes 106 and 124, and ethylene urea melamine
formaldehyde resin (relevant to his use of dark-coloured
underwear, jeans and pyjamas). Avoidance of dark clothing,
permanent-press underwear and relevant medicaments led
to a signicant improvement in his pustular psoriasis. He
had one further hospital admission with a are of exural
pustular psoriasis after he returned to wearing black jeans and
dark blue pyjamas. Since then, he has avoided dark clothing
altogether, with marked improvement in his psoriasis. He has
been discharged from dermatology care and all systemic treat-
ment has been withdrawn.
Only two detailed case reports in the literature describe
ACD associated with pustular psoriasis in body sites excluding
palms and soles.
1,2
In both cases, stable plaque psoriasis was
transformed to pustular psoriasis as a result of ACD to zinc
pyrithione in a shampoo, which was conrmed on patch
testing. Studies of ACD complicating psoriasis are sparse
(summarized in Table 1
39
). Comparable rates of patch test-
positive reactions have been reported in patients with psoriasis
and nonpsoriatic general dermatology outpatients in some
studies.
4,7
As in our two patients, a predominance of sensitiv-
ity to topical medicaments and fragrances has been noted in
the patients with psoriasis.
4,8
One study reports a single
patient with psoriasis vulgaris being patch test-positive to an
organic dye.
9
There are no other reports of ACD to dyes or
the textile series in patients with psoriasis.
A history of psoriasis for 5 years or longer was associated
with a higher rate of positive patch test results compared with
a shorter disease duration (P < 001) in one study
4
and is
likely to be relevant to our two patients who have used numer-
ous topical treatments during their life-long history of psoria-
sis. Correlation between the site of psoriasis and positive patch
tests was seen only in some studies
5
and not in others.
3,4
There are many theoretical reasons why psoriasis might be
associated with ACD. Psoriasis and ACD share a T helper 1 cell
immune basis. Compromise in skin barrier function, decreased
thickness of the epidermis overlying elongated dermal papillae
Table 1 Summary of studies on allergic contact dermatitis in psoriasis
Number of
patients (Ref.) Type of psoriasis (number of patients)
Most frequently positive allergens
(% of patients tested positive to each allergen)
Overall patch
test positivity
305
3
Psoriasis vulgaris (219)
Palmoplantar including pustular (80)
Other forms not specied (6)
Nickel (111%), diaminodiphenylmethane (32%),
neomycin (26%), thiomersal (26%),
p-phenylenediamine (26%)
24%
200
4
Chronic plaque psoriasis (200) Dithranol (65%), nickel (6%), fragrance mix (5%),
neomycin (2%), nitrofurazone (2%)
216%
140
5
Stable plaque (89)
Active (51)
Tar (85%), nickel (57%),
corticosteroids mixture (56%), thiomersal (5%)
23%
75
6
Chronic plaque, guttate and pustular
(numbers of each type not stated)
Nickel (106%), fragrance mix (53%), coal tar (4%),
colophony (4%), neomycin (27%)
25%
74
7
Chronic plaque (67)
Pustular (3)
Erythrodermic (2)
Flexural only (2)
Tar (27%), dithranol (13%)
a
Not stated
55
8
Psoriasis vulgaris (43)
Palmoplantar including pustular (12)
Nickel (9%) 254%
47
9
Psoriasis vulgaris (35)
Other forms: pustular, inverse,
erythrodermic (5)
Seborrhoeic psoriasis (7)
Tar (319%), perfume (148%), nickel (106%),
balsam of Peru (85%)
68%
a
Patients tested only to coal tar, dithranol, ichthammol and tixocortol pivalate in this study.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Correspondence 789
and use of keratolytics
9
might increase penetration of aller-
gens. Prolonged use of multiple topical medicaments for psor-
iasis increases exposure to potential allergens. ACD could also
act as a Kobnerizing stimulus
7
on a psoriatic background.
We report our two patients to highlight the potential
association between ACD and pustular psoriasis, and to
encourage a higher index of suspicion and lower threshold for
patch testing similar patients, especially those with a chronic
history of treatment-resistant disease or recurrent involvement
of the same body sites.
R. P. KATUGAMP OL A
T. M. HUGHE S
C. M. MI L L S
N. M. STONE
Department of Occupational Dermatology,
Royal Gwent Hospital, Friars Road,
Newport NP20 4EZ, U.K.
E-mail: ruwanik@hotmail.com
The two patients discussed in this correspondence were presented at
the British Contact Dermatitis Society meeting, British Association of
Dermatologists Annual Meeting, Manchester, U.K. in July 2006.
10
References
1 Nielsen NH, Menne T. Allergic contact dermatitis caused by zinc
pyrithione associated with pustular psoriasis. Am J Contact Dermat
1997; 8:1701.
2 Jo JH, Jang HS, Ko HC et al. Pustular psoriasis and the Kobner
phenomenon caused by allergic contact dermatitis from zinc
pyrithione-containing shampoo. Contact Dermatitis 2005; 52:1424.
3 Barile M, Cozzani E, Anonide A et al. Is contact allergy rare in
psoriatics? Contact Dermatitis 1996; 35:11314.
4 Malhotra V, Kaur I, Saraswat A, Kumar B. Frequency of patch-test
positivity in patients with psoriasis: a prospective controlled study.
Acta Derm Venereol (Stockh) 2002; 82:4325.
5 Pigatto PD. Atopy and contact sensitization in psoriasis. Acta Derm
Venereol (Stockh) 2000; 211 (Suppl.): 1920.
6 Fleming CJ, Burden AD. Contact allergy in psoriasis. Contact Dermatitis
1997; 36:2746.
7 Burden AD, Muston H, Beck MH. Intolerance and contact
allergy to tar and dithranol in psoriasis. Contact Dermatitis 1994;
31:1856.
8 Stinco G, Frattasio A, De Francesco V et al. Frequency of delayed-
type hypersensitivity to contact allergens in psoriatic patients.
Contact Dermatitis 1999; 40:3234.
9 Heule F, Tahapary GJM, Bello CR, Joost TH. Delayed-type hyper-
sensitivity to contact allergens in psoriasis. A clinical evaluation.
Contact Dermatitis 1998; 38:7882.
10 Katugampola RP, Hughes TM, Mills CM, Stone NM. Allergic con-
tact dermatitis complicating pustular psoriasis. Br J Dermatol 2006;
155 (Suppl. 1):72 (abstr).
Conicts of interest: none declared.
News and Notices
DOI: 10.1111/j.1365-2133.2007.07824.x
Congress: 2nd International Congress on Psoriasis
Dates: JUNE 2124, 2007
Venue: Paris, Palais des congre`s, FRANCE
Web site: http://www.pso2007.com
Contact:
PSO 2007 c/o MCI
24 rue Chauchat
75009 Paris
FRANCE
Phone: +33 (1) 53 85 82 59
Fax: +33 (1) 53 85 82 83
Email: pso2007info@mci-group.com
Main topics:
Scoring and monitoring the severity of the disease
Management of the severe clinical manifestations
Psoriasis in children and pregnancy
Difcult to treat localisations
Topical Treatment: what to choose and how to use
Risk management and treatment optimisation: combination
and rational strategies
Phototherapies: what to choose and how to use
Alternative treatment
Biologics
Extracutaneous manifestations in Psoriasis
International Short Course on Dermoscopy
Date: July 1721, 2007
Venue: Department of Dermatology, Medical University of
Graz, Auenbruggerplatz 8, A-8036 Graz
Organizer: Medical University of Graz, Department of Derma-
tology
Type of Event: Course
Language: English
Contact:
Katrin Steinmann, Graz, Austria
Telephone: +43-699-11081567
Fax: +43-316-696110
Email: katrin@steinmann.org
Website: http://www.meduni-graz.at/dermoscopy/
Description: This course is for residents in dermatology
and for dermatologists from universities or private practice
as well as for physicians or nurses interested in the diagnosis
of pigmented skin lesions.
Congress: 8
th
Annual Meeting of the Austrian Academy of
Cosmetic Surgery in cooperation with the American and
Asian Academy of Cosmetic Surgery
Venue and date: Vienna/Austria Hotel Marriott, September
1316, 2007
Main topics: Safety in Cosmetic Surgery, Facial Surgery,
Anatomy, Laser Therapy, Breast Operations, Liposuction,
Abdominoplasty, Brachioplasty, Leg-Lift, Medico-Cosmetics,
Hormonal Therapy, Botox, Fillers, New Methods and Tech-
nologies
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
790 News and Notices
Chair:
Dr Peter Lisborg, Vienna Medical Academy
Phone: +43/1/405 13 83 10
Fax: +43/1/407 82 74
e-mail: cosmeticsurgery2007@medacad.org
Information:
A
rztezentrale Med.Info
Helferstorferstrasse 4, A-1014 Wien
Phone: (+43/1) 531 16 75
Fax: (+43/1) 531 16 61
e-mail: azmedinfo@media.co.at
Erratum
DOI: 10.1111/j.1365-2133.2007.07825.x
The Family Dermatology Life Quality Index: measuring the
secondary impact of skin disease. Br J Dermatol 2007, Basra
et al.
In the above mentioned article
1
there was an error in the
Appendix entitled Family Dermatology Life Quality Index
(FDLQI). The Appendix as it should have appeared is shown
below.
Appendix: the Family Dermatology Life Quality
Index (FDLQI)
Name: ................................................ FDLQI Score
Relationship with patient: .........................................
Patients diagnosis (if known): ....................................... Date:
...........................
The questions relate to the impact of your relative/partners
skin disease on your quality of life over the last month.
Please read the questions carefully and tick one box for
each.
1. Over the last month how much emotional distress have you
experienced due to your relative/partners skin disease (e.g.
worry, depression, embarrassment, frustration)?
Not at all/Not relevant uA little uQuite a lot uVery much u
2. Over the last month how much has your relative/partners
skin disease affected your physical well-being (e.g. tiredness,
exhaustion, contribution to poor health, sleep/rest disturb-
ance)?
Not at all/Not relevant uA little uQuite a lot uVery much u
3. Over the last month how much has your relative/partners
skin disease affected your personal relationships with him/her
or with other people?
Not at all/Not relevant u A little u Quite a lot u Very much u
4. Over the last month how much have you been having
problems with other peoples reactions due to your relative/
partners skin disease (e.g. bullying, staring, need to explain to
others about his/her skin problem)?
Not at all/Not relevant u A little u Quite a lot u Very much u
5. Over the last month how much has your relative/partners
skin disease affected your social life (e.g. going out, visiting or
inviting people, attending social gatherings)?
Not at all/Not relevant u A little u Quite a lot u Very much u
6. Over the last month how much has your relative/partners
skin disease affected your recreation/leisure activities (e.g. holi-
days, personal hobbies, gym, sports, swimming, watching TV)?
Not at all/Not relevant u A little u Quite a lot u Very much u
7. Over the last month how much time have you spent on look-
ing after your relative/partner (e.g. putting on creams, giving
medicines or looking after their skin)?
Not at all/Not relevant u A little u Quite a lot u Very much u
8. Over the last month how much extra housework have you
had to do because of your relative/partners skin disease (e.g.
cleaning, vacuuming, washing, cooking)?
Not at all/Not relevant u A little u Quite a lot u Very much u
9. Over the last month how much has your relative/partners
skin disease affected your job/study (e.g. need to take time off,
not able to work, decrease in the number of hours worked, hav-
ing problems with people at work)?
Not at all/Not relevant u A little u Quite a lot u Very much u
10. Over the last month how much has your relative/partners
skin disease increased your routine household expenditure (e.g.
travel costs, buying special products, creams, cosmetics)?
Not at all/Not relevant u A little u Quite a lot u Very much u
Thank you for completing the questionnaire.
MKA Basra, AY Finlay. Cardiff University 2005.
The FDLQI is copyright. For more information please contact
the authors.
The Publisher apologises for these errors.
References
1 Basra MKA, Sue-Ho R, Finlay AY. The Family Dermatology Life
Quality Index: measuring the secondary impact of skin disease. Br J
Dermatol 2007; 156:52838.
2007 The Authors
Journal Compilation 2007 British Association of Dermatologists British Journal of Dermatology 2007 156, pp748791
Erratum 791
Anda mungkin juga menyukai
- Position Therapeutic Potential of Antimicrobial Peptides in Atopic Dermatitis PDFDokumen2 halamanPosition Therapeutic Potential of Antimicrobial Peptides in Atopic Dermatitis PDFViswa VittalBelum ada peringkat
- Posters FinalDokumen70 halamanPosters FinalShkelzen KomoniBelum ada peringkat
- Tinea Capitis - UpToDateDokumen7 halamanTinea Capitis - UpToDatejotaere RobBelum ada peringkat
- JAAD Case Reports Article List - YmjdDokumen4 halamanJAAD Case Reports Article List - YmjdYilianeth Mena DazaBelum ada peringkat
- Fitzpatricks Dermatology 9th Edition 3127Dokumen1 halamanFitzpatricks Dermatology 9th Edition 3127DennisSujayaBelum ada peringkat
- S2 2021 435724 BibliographyDokumen5 halamanS2 2021 435724 BibliographyCinthia AsawistaBelum ada peringkat
- References 1, 2, 3Dokumen7 halamanReferences 1, 2, 3d2mvb7zr7kBelum ada peringkat
- ReferencesDokumen2 halamanReferencesIwan MarionoBelum ada peringkat
- Dapus NumeroDokumen5 halamanDapus NumerodiankdsaputriBelum ada peringkat
- Thesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentDokumen6 halamanThesis Title Role of Guidelines For Pregnant Women On Malaria Prevention and TreatmentPhillip TaylorBelum ada peringkat
- Dafpus PaDokumen4 halamanDafpus PaTharie ElBelum ada peringkat
- Aanensen, D. M. & B. G. Spratt. 2005. The Multilocus Sequence Typing NetworkDokumen10 halamanAanensen, D. M. & B. G. Spratt. 2005. The Multilocus Sequence Typing NetworkAli BabaBelum ada peringkat
- 00006123-200802001-00013 Infections and InfestationsDokumen1 halaman00006123-200802001-00013 Infections and InfestationsJosé Luis Navarro RomeroBelum ada peringkat
- Daftar PustakaDokumen5 halamanDaftar PustakaHasryani HaluddinBelum ada peringkat
- DOK1Dokumen10 halamanDOK1RIZKI RAHMAWANBelum ada peringkat
- Daftar Pustaka Emedicine MedscapeDokumen7 halamanDaftar Pustaka Emedicine MedscapeAyesha Nabilla Putri0% (1)
- Daftar Pustaka: Health. 2009 3 (1) :81-98. Doi:10.2217/17455111.3.1.81Dokumen2 halamanDaftar Pustaka: Health. 2009 3 (1) :81-98. Doi:10.2217/17455111.3.1.81ErvinaKusumaWardaniBelum ada peringkat
- MedicalDokumen4 halamanMedicalSeyi CampbellBelum ada peringkat
- Slow Transmissible Diseases of the Nervous System: Pathogenesis, Immunology, Virology, and Molecular Biology of the Spongiform EncephalopathiesDari EverandSlow Transmissible Diseases of the Nervous System: Pathogenesis, Immunology, Virology, and Molecular Biology of the Spongiform EncephalopathiesBelum ada peringkat
- Recognition. Bionanoscience. 7, 449-455. Release. Adv Mater. 30, 1705436. 4. Nano. 12, 8646-8661Dokumen10 halamanRecognition. Bionanoscience. 7, 449-455. Release. Adv Mater. 30, 1705436. 4. Nano. 12, 8646-8661Pravin KaleBelum ada peringkat
- Tamburrini G., Caldarelli M., Di Rocco C. Section of Pediatric Neurosurgery Catholic University Medical School, RomeDokumen2 halamanTamburrini G., Caldarelli M., Di Rocco C. Section of Pediatric Neurosurgery Catholic University Medical School, RomeBhayu RizallinoorBelum ada peringkat
- Dafpus ReferatDokumen4 halamanDafpus ReferatwahyuaBelum ada peringkat
- Table of Contents YmicDokumen4 halamanTable of Contents YmicKhadiga AhmadBelum ada peringkat
- DAFTAR PUSTAKA IntipDokumen12 halamanDAFTAR PUSTAKA Intipputri rizkiBelum ada peringkat
- Salmonella RefDokumen3 halamanSalmonella RefTochukwu IbekweBelum ada peringkat
- Germfree Research: Biological Effect of Gnotobiotic EnvironmentsDari EverandGermfree Research: Biological Effect of Gnotobiotic EnvironmentsBelum ada peringkat
- Dafpus KtiDokumen8 halamanDafpus KtiRaka BlackBelum ada peringkat
- Advances in Immunopharmacology: Proceedings of the Second International Conference on Immunopharmacology, July 1982, Washington, USADari EverandAdvances in Immunopharmacology: Proceedings of the Second International Conference on Immunopharmacology, July 1982, Washington, USABelum ada peringkat
- Daftar Pustaka PDFDokumen10 halamanDaftar Pustaka PDFgunawanmulyana12Belum ada peringkat
- Dapus Case 1Dokumen2 halamanDapus Case 1Imam Taqwa DrughiBelum ada peringkat
- Daftar PustakaDokumen3 halamanDaftar PustakaHeru SigitBelum ada peringkat
- Daftar PustakaDokumen7 halamanDaftar PustakaAnesthesiology FKUBBelum ada peringkat
- Daftar Pustaka Dewi UploadDokumen10 halamanDaftar Pustaka Dewi Uploadhotland sitorusBelum ada peringkat
- Daftar PustakaDokumen2 halamanDaftar PustakaEka NurjannahBelum ada peringkat
- OTITISDokumen21 halamanOTITISAzís Humberto Gastelum ZatarainBelum ada peringkat
- S2 2022 435655 BibliographyDokumen6 halamanS2 2022 435655 BibliographyUsmel RamadhaniaBelum ada peringkat
- Immunity 59 (6) : 1905-1910.: Daftar PustakaDokumen11 halamanImmunity 59 (6) : 1905-1910.: Daftar PustakaQaira KyleBelum ada peringkat
- Daftar PustakaDokumen6 halamanDaftar PustakaMitrahusada OfficialBelum ada peringkat
- Contents BjaDokumen3 halamanContents BjaJustin DodaneBelum ada peringkat
- Daftar PustakaDokumen6 halamanDaftar PustakaMerliana DebyantiBelum ada peringkat
- DAFPUSDokumen4 halamanDAFPUSNera MayaditaBelum ada peringkat
- Phytopathology in PlantsDokumen331 halamanPhytopathology in PlantsJulissa O CastilloBelum ada peringkat
- 8 TocDokumen2 halaman8 TocAriBelum ada peringkat
- Fita Radio Fix-DikonversiDokumen34 halamanFita Radio Fix-Dikonversifachira rusdiBelum ada peringkat
- Human Anti-Human Gammaglobulins, Their Specificity and Function: Proceedings of the International Symposium Held in Lund, October 1969Dari EverandHuman Anti-Human Gammaglobulins, Their Specificity and Function: Proceedings of the International Symposium Held in Lund, October 1969R. GrubbBelum ada peringkat
- Epidermodysplasia-Verruciformis YmjdDokumen1 halamanEpidermodysplasia-Verruciformis YmjdAndrés WunderwaldBelum ada peringkat
- Format ReferatDokumen4 halamanFormat ReferatDoctor AnonymousBelum ada peringkat
- 50 Years Ago in em T Span Class Small He Span 14Dokumen1 halaman50 Years Ago in em T Span Class Small He Span 14davidisnice123Belum ada peringkat
- Jamadermatology Wang 2019 Lo 1900191 PDFDokumen3 halamanJamadermatology Wang 2019 Lo 1900191 PDFvijaya abburamBelum ada peringkat
- Bener Dapus NewestDokumen9 halamanBener Dapus NewestnunungBelum ada peringkat
- ForrásDokumen4 halamanForrásMárton AlexaBelum ada peringkat
- IBI-Kualifikasi PustakaDokumen11 halamanIBI-Kualifikasi PustakatrioBelum ada peringkat
- Surgery, Winn HR (Ed), 6: Daftar PustakaDokumen5 halamanSurgery, Winn HR (Ed), 6: Daftar Pustakasistri ajeng gmBelum ada peringkat
- Conflict of Interests: Aspergilosis Cutánea Secundaria Pustulosa en Paciente InmunosuprimidoDokumen4 halamanConflict of Interests: Aspergilosis Cutánea Secundaria Pustulosa en Paciente InmunosuprimidoJuana de los Milagros Chiroque Zeta.Belum ada peringkat
- Daftar PustakaDokumen2 halamanDaftar PustakaMeylinda LinBelum ada peringkat
- Annual Report 10192020 FInalDokumen58 halamanAnnual Report 10192020 FInalanonimouse indonesiaBelum ada peringkat
- 2014 JulyDokumen28 halaman2014 JulyMoisés J. Duran CanevaroBelum ada peringkat
- Khilyatul Mufida 22010111120040 Lap - Kti Bab 8Dokumen27 halamanKhilyatul Mufida 22010111120040 Lap - Kti Bab 8Hafid JuniorBelum ada peringkat
- FK - PD.96 Seo P Daftar PustakaDokumen7 halamanFK - PD.96 Seo P Daftar PustakaSiti Sinar Dewi AmeliaBelum ada peringkat
- Cell - London.Garland Science.: Daftar PustakaDokumen7 halamanCell - London.Garland Science.: Daftar PustakaamaliaBelum ada peringkat
- DHF Menurut WHO 2011Dokumen212 halamanDHF Menurut WHO 2011Jamal SutrisnaBelum ada peringkat
- Inflammatory Response Following Diffuse Axonal InjuryDokumen7 halamanInflammatory Response Following Diffuse Axonal Injurydiyan110Belum ada peringkat
- Daftar Pustaka LapsusDokumen2 halamanDaftar Pustaka Lapsusdiyan110Belum ada peringkat
- Daftar PustakaDokumen2 halamanDaftar Pustakadiyan110Belum ada peringkat
- Inflammatory Response Following Diffuse Axonal InjuryDokumen7 halamanInflammatory Response Following Diffuse Axonal Injurydiyan110Belum ada peringkat
- Lirik Maher ZainDokumen1 halamanLirik Maher Zaindiyan110Belum ada peringkat
- Across The UniverseDokumen1 halamanAcross The Universediyan110Belum ada peringkat
- Jirayu - Just A SecondDokumen2 halamanJirayu - Just A Seconddiyan110Belum ada peringkat
- Love Part 8Dokumen15 halamanLove Part 8diyan110Belum ada peringkat
- One More NightDokumen1 halamanOne More Nightdiyan110Belum ada peringkat
- Dermatitis PerioralDokumen4 halamanDermatitis Perioraldiyan110Belum ada peringkat
- KiyomiDokumen2 halamanKiyomiKevs DumalascoBelum ada peringkat
- Kamasean - How Could YouDokumen1 halamanKamasean - How Could Youdiyan110Belum ada peringkat
- Jirayu - Just A SecondDokumen2 halamanJirayu - Just A Seconddiyan110Belum ada peringkat
- GamesDokumen2 halamanGamesdiyan110Belum ada peringkat
- GamesDokumen2 halamanGamesdiyan110Belum ada peringkat
- PSY GentlemenDokumen1 halamanPSY Gentlemendiyan110Belum ada peringkat
- Glee's SongDokumen7 halamanGlee's Songdiyan110Belum ada peringkat
- Skeletal MuscleDokumen3 halamanSkeletal Musclekrystal1994Belum ada peringkat
- Hormones As Signals, Classification of HormonesDokumen22 halamanHormones As Signals, Classification of HormonesHarini BalasubramanianBelum ada peringkat
- 385163146classificationof Algae by FritschDokumen16 halaman385163146classificationof Algae by FritschAnshita RajputBelum ada peringkat
- NBRI MarigoldDokumen2 halamanNBRI MarigoldShailendra RajanBelum ada peringkat
- Haploid ProductionDokumen25 halamanHaploid Productionitube100% (2)
- Classification of OrganismsDokumen42 halamanClassification of OrganismsLOUIS BENITO.SANTOSOBelum ada peringkat
- Karyotype Analysis of Lablab PurpureusDokumen1 halamanKaryotype Analysis of Lablab PurpureusZain JawadBelum ada peringkat
- Catalog Roche 2012Dokumen180 halamanCatalog Roche 2012MrmohanakBelum ada peringkat
- Handbook of Shanti Swarup Bhatnagar Prize Winners (1958 - 1998)Dokumen118 halamanHandbook of Shanti Swarup Bhatnagar Prize Winners (1958 - 1998)Hazari ChauhanBelum ada peringkat
- Soft Tissue Injury - Chapter 22Dokumen49 halamanSoft Tissue Injury - Chapter 22David CBelum ada peringkat
- Bacillus Megaterium Biodegradation Glycophate: September 2019Dokumen8 halamanBacillus Megaterium Biodegradation Glycophate: September 2019Harem OmerBelum ada peringkat
- Lab Report #2 MicrobioDokumen18 halamanLab Report #2 Microbioariana villarrealBelum ada peringkat
- Reaction Paper On The Real EveDokumen2 halamanReaction Paper On The Real EveJoy Marisol Flores ManiaulBelum ada peringkat
- B Acte CheckDokumen126 halamanB Acte CheckMarie LlanesBelum ada peringkat
- Watermelon Seedless ColchicineDokumen12 halamanWatermelon Seedless ColchicineCatalina BanuBelum ada peringkat
- Final EssayDokumen9 halamanFinal Essayapi-582840410Belum ada peringkat
- Artikel Nida Anisa 1731011010Dokumen7 halamanArtikel Nida Anisa 1731011010Nida AnisaBelum ada peringkat
- Fisiologia Asa de HenleDokumen24 halamanFisiologia Asa de HenleOscar SotoBelum ada peringkat
- Laboratory Exercise 4. Microscopic Observation of MicroorganismsDokumen9 halamanLaboratory Exercise 4. Microscopic Observation of MicroorganismsNesly Joy CaballeganBelum ada peringkat
- Chapter 3Dokumen4 halamanChapter 3Al Cris BarroBelum ada peringkat
- Organic Molecules Assignment MenuDokumen3 halamanOrganic Molecules Assignment Menuapi-434671855Belum ada peringkat
- Digestion and Absorption of Carbohydrate Lecture For 1st Yr MBBS by DR WaseemDokumen33 halamanDigestion and Absorption of Carbohydrate Lecture For 1st Yr MBBS by DR WaseemIMDCBiochem100% (2)
- Hematopoietic Stem Cell Transplantation For Thalassemia: Javid Gaziev and Guido LucarelliDokumen14 halamanHematopoietic Stem Cell Transplantation For Thalassemia: Javid Gaziev and Guido LucarelliRatna AzizahBelum ada peringkat
- Feeding The SkinDokumen12 halamanFeeding The SkinsunnybeaBelum ada peringkat
- What Is Human Cloning?Dokumen10 halamanWhat Is Human Cloning?OwethuBelum ada peringkat
- Chemical and Physical Properties of Nucleic AcidsDokumen6 halamanChemical and Physical Properties of Nucleic AcidsSherlock Wesley ConanBelum ada peringkat
- C995 12 PDFDokumen14 halamanC995 12 PDFdanzan1Belum ada peringkat
- Solution Manual For Cell and Molecular Biology 8th Edition Gerald Karp Janet Iwasa Wallace MarshallDokumen34 halamanSolution Manual For Cell and Molecular Biology 8th Edition Gerald Karp Janet Iwasa Wallace Marshallevenehautpas.g0rmkq100% (47)
- AntigensDokumen33 halamanAntigensSandeep Pokhrel100% (2)
- Digestive System and Respiratory SystemDokumen10 halamanDigestive System and Respiratory SystemKathMae BoaBelum ada peringkat