Case Study of Coronary Heart Disease by Hannifah Fitriani & Lilis Rahma Yanthi
Diunggah oleh
Hannifah FitrianiHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Case Study of Coronary Heart Disease by Hannifah Fitriani & Lilis Rahma Yanthi
Diunggah oleh
Hannifah FitrianiHak Cipta:
Format Tersedia
CASE REPORT
CORONARY HEART DISESASE / CORONARY ARTERY DISEASE
Paper is submitted to fulfill course of English for Nursing I (EFN 1)
Reported by:
Hannifah Fitriani Lilis Rahma Yanthi
(220110100055) (220110100060)
NURSING FACULTY OF PADJAJARAN UNIVERSITY 2012
Case Study of Coronary Heart Disease
Mr. Bean, 65 years old is a retired of Civil Servant (PNS). He is a Muslim, and his last education was an Economic Bachelor. He complained of pain in his left chest 2 hours before enter to the hospital (December 3rd 2012). He told that the pain like pressure by heavy load, it also spread to the left arm and back, and it was constant. Mr. Bean also complained of nausea, vomiting, and sweating. Mr. Bean has a history of hyperlipidemia since 10 years ago, and his smoking history is (+) 2 packs of cigarette a day but he tries to decrease it 7 month ago. According to Mr. Bean, his family had no heart disease, diabetes mellitus, or hypertension history.
NURSING ASSESSMENT FORM Patients Identity Name Age Gender Address Religion Ethnicity Education Occupation : Mr. Bean : 65 years old : Male : Jatinangor, Sumedang : Muslim : Sundanese : Economic Bachelor : Retired of Civil Servant (PNS)
I.
Admission Date : December 3rd 2012
II. Health History A. The main complain He complained of pain in his left chest and the pain like pressure by heavy load, it also spreads to the left arm and back, and it was constant. Anamneses P: The pain decrease when he takes a rest, and increase when he moves Q: The pain like pressure by heavy load, and constant pain R: The pain is in his left chest and spreads to the left arm and back S: The pain scale is 7 of range 1-10
T: The pain is felt 2 hours before enter to the hospital and it was constant B. Present medical history He feels pain in his left chest and the pain like pressure by heavy load, it also spreads to the left arm and back, and it was constant. He also complained of nausea, vomiting, and sweating. C. Past medical history Mr. Bean has a history of hyperlipidemia since 10 years ago and his smoking history is (+) 2 packs of cigarette a day, but it decrease 7 month ago. D. Family health history Mr. Beans family had no heart disease, diabetes mellitus, or hypertension history. E. Psychosocial history Before: Mr. Bean personal emotion was stable, and he always talks to his wife and children when he had problem. He had a good relationship with his family and other people. After: Mr. Bean worried about his condition who diagnosed with coronary heart disease. This is the first time he had a heart disease / cardiovascular disease. F. Spiritual history He is a Devout Muslim, he always praying five times a day; he believes that his illness is a test from Allah SWT.
III. Functional Pattern of Daily Activities A. Nutrition Food: Mr. Bean eats 3 times a day. He eats beef steak and nasi padang three times a week. Drink: Mr. Bean drinks 8 glass of water a day.
B. Elimination Mr. Bean defecates once a day and urinates four until five times a day. C. Activity and exercise Mr. Bean rarely do exercise, he fills his spare time by watching TV, and he easy to get fatigue and cold sweat when activity. D. Rest and sleep Mr. Bean sleeps about 8 hours a day in the night without being disturbed, and he never naps.
E. Personal hygiene Mr. Bean usually bathing twice a day, brushing his teeth twice a day, washing his hair three times a week, and always changing clothes every day, he can fulfill his personal hygiene by himself.
IV. Physical Examination A. General condition: looks pain B. Consciousness: Compos Mentis (eyes: 4, motoric: 6, verbal: 5) C. Vital sign Weight: 80 kg Height: 160 cm T: 36.5oC BP: 120/90 mmHg P: 80 RR: 23 bpm
D. Skin Elastic skin turgor, brown skin color, there are no lesions and edema. E. Head Hair: Black hair color (mix with grey hair), equitable distribution of hair, clean scalp hygiene, neat hair. Eyes: Conjunctiva anemic, isochors pupil, blurred visions, he could read well with a distance of 15 cm. Ears: Symmetrical shape, no hearing problems, no pain, hygiene maintained. Nose: Symmetrical shape, clean, no secret, able to distinguish the smell of food, and no epistaxis. Mouth: Symmetrical shapes, moist lips, pale oral mucosa, clean teeth, clean tongue. F. Neck No enlargement of the thyroid gland, normal movement G. Chest and lung Inspection: Symmetrical chest shape Auscultation: Clean breath sound Palpation: Normal lung expansion, tenderness on left chest
Percussion: resonance on right ICS 1-4 and left ICS 1&6, dullness on right ICS 56 and left ICS 2-5.
H. Heart S1 heart sound heard clearly on the left at the fifth ICS midclavicula line, second heart sound heard clearly in ICS 2 parasternal left and right. Heart sounds is pure, no murmurs or gallops. I. Abdomen Symmetrical shape, there is no lesion and intestine sound 8 per minute. J. Extremity Acral warm, CRT > 4 seconds, no edema, no clubbing finger.
V. Additional Diagnostic Test A. Laboratory result Total Cholesterol Total Triglyceride LDL Cholesterol HDL Cholesterol Lipoprotein Homocysteine B. Chest roentgen Enlargement of the left heart C. Electrocardiogram (ECG) ST elevation I, II, III avF 243 mg/dL 376 mg/dL 120 mg/dL 28 mg/dL 21 mg/dL 8.44 umol/L Normal: < 200 mg/dL Normal: < 150 mg/dL Normal: < 100 mg/dL Normal: > 60 mg/dL Normal: 0 30 mg/dL Normal: 5.4 11.9 umol/L
VI. Therapies Mr. Bean treatment are oxygen 2L/minutes, Pethidine 2 mgr, Fortanes 30 mg/30 cc, Aspilet 2x1 tablet, KCL 25 meq in the first 4 hours, Ca gluconate 1 amp.
Anda mungkin juga menyukai
- NURSING HEALTH HISTORYup.Dokumen5 halamanNURSING HEALTH HISTORYup.romelynBelum ada peringkat
- MS CaseDokumen28 halamanMS CaseJuwaka OsakaBelum ada peringkat
- Age - For SubmissionDokumen27 halamanAge - For SubmissionAdrian MallarBelum ada peringkat
- I. Demographic Profile: Treatments/MedicationDokumen4 halamanI. Demographic Profile: Treatments/MedicationGrace MellaineBelum ada peringkat
- ADOLESCENT - History TakingDokumen3 halamanADOLESCENT - History TakingdocamyBelum ada peringkat
- GERD (Gastroesophageal Reflux Disease)Dokumen112 halamanGERD (Gastroesophageal Reflux Disease)Mharj Alfelor Cecilio100% (7)
- Case Study (Group 2a)Dokumen14 halamanCase Study (Group 2a)Aishleen OrmandoBelum ada peringkat
- Sagun Pls Dont Dilit Huhuhhuhhu 123Dokumen85 halamanSagun Pls Dont Dilit Huhuhhuhhu 123Star SagunBelum ada peringkat
- Ii. Chief ComplaintsDokumen4 halamanIi. Chief ComplaintsArianne_Danglo_2118Belum ada peringkat
- Knee Replace Care PlanDokumen11 halamanKnee Replace Care PlanLaura Romness100% (2)
- Multinodular Colloid Goiter With Intrathoracic Extension: Admission/Final DiagnosisDokumen39 halamanMultinodular Colloid Goiter With Intrathoracic Extension: Admission/Final DiagnosisKirsten CajayonBelum ada peringkat
- Nursing Upper Gi BleedingDokumen23 halamanNursing Upper Gi BleedingLord Pozak Miller100% (3)
- Flail Chest (Tayug)Dokumen25 halamanFlail Chest (Tayug)Adrian MallarBelum ada peringkat
- Example Write Up #1: A Patient With Diarrhea: Problem ListDokumen8 halamanExample Write Up #1: A Patient With Diarrhea: Problem ListMaher AltaeeBelum ada peringkat
- BPHDokumen15 halamanBPH'mYk FavilaBelum ada peringkat
- Health History: I. Personal DataDokumen7 halamanHealth History: I. Personal DataromelynBelum ada peringkat
- NCMA121.HAs RLE Nursing Health History Format 1Dokumen5 halamanNCMA121.HAs RLE Nursing Health History Format 1Antonette Africa MercadoBelum ada peringkat
- History PCGH PXDokumen3 halamanHistory PCGH PXAgape Love AbonadorBelum ada peringkat
- IM Clinics History 2Dokumen4 halamanIM Clinics History 2LucyellowOttemoesoeBelum ada peringkat
- Last Name: Full Name Middle NameDokumen4 halamanLast Name: Full Name Middle NameMiss GBelum ada peringkat
- Case StudyDokumen29 halamanCase StudyGerome ValderamaBelum ada peringkat
- College of Nursing: Panpacific University North PhilippinesDokumen20 halamanCollege of Nursing: Panpacific University North PhilippinesMar OrdanzaBelum ada peringkat
- Incomplete AbortionDokumen22 halamanIncomplete AbortionAJ Dalawampu100% (2)
- History Taking (Mercado, AA)Dokumen4 halamanHistory Taking (Mercado, AA)Antonette Africa MercadoBelum ada peringkat
- PEDIA Case - Pneumonia 2 VSDDokumen17 halamanPEDIA Case - Pneumonia 2 VSDGrace Antonette PatiBelum ada peringkat
- Geri SOAPsampleDokumen8 halamanGeri SOAPsampleJacquelineBelum ada peringkat
- Gastritis Nursing AssistanceDokumen10 halamanGastritis Nursing AssistancedirzahBelum ada peringkat
- CKD Case PresentationDokumen64 halamanCKD Case PresentationGenevieve MundalaBelum ada peringkat
- BY: Shazlin Bt. Sabaah Salwa Hanim Bt. Mohd. Saifuddin Kamarulzaman B. MuzainiDokumen61 halamanBY: Shazlin Bt. Sabaah Salwa Hanim Bt. Mohd. Saifuddin Kamarulzaman B. MuzainiJohn Christopher LucesBelum ada peringkat
- IM Gastro FinalDokumen10 halamanIM Gastro FinalIzzyMaxinoBelum ada peringkat
- Adult Patient History & Physical Assessement: Central Philippine UniversityDokumen11 halamanAdult Patient History & Physical Assessement: Central Philippine UniversityJoshua Elli BajadaBelum ada peringkat
- DocxDokumen6 halamanDocxScott Russell McGillivray89% (9)
- TrixiaVillasotoo CasestudyDokumen26 halamanTrixiaVillasotoo CasestudyAllyza Trixia Joyce VillasotoBelum ada peringkat
- History of Past and Present IllnessDokumen10 halamanHistory of Past and Present IllnessRenea Joy ArruejoBelum ada peringkat
- Intensive Case Study: Nursing Health History Biographic DataDokumen15 halamanIntensive Case Study: Nursing Health History Biographic Databojums67% (3)
- For Printing Grand Case Group1Dokumen37 halamanFor Printing Grand Case Group1Joco Bordeos AripBelum ada peringkat
- Case AppendicitisDokumen10 halamanCase AppendicitisNiña Montejo EaldamaBelum ada peringkat
- A. Biographical DataDokumen6 halamanA. Biographical DataDRABelum ada peringkat
- Laryngeal MassDokumen36 halamanLaryngeal MassJayson de GuzmanBelum ada peringkat
- Medical WardDokumen15 halamanMedical WardImnot You100% (1)
- A Narrative Report On: Physical AssesmentDokumen11 halamanA Narrative Report On: Physical AssesmentchelseyBelum ada peringkat
- PEDIA Case 4.1. Dengue FeverDokumen10 halamanPEDIA Case 4.1. Dengue Feverotartil_nimanBelum ada peringkat
- Comprehensive Nursing ProcessDokumen17 halamanComprehensive Nursing Processm100% (1)
- A-G IbmsDokumen4 halamanA-G IbmsAubrey Unique EvangelistaBelum ada peringkat
- Lapkas Nadya - English FIXDokumen38 halamanLapkas Nadya - English FIXclaraBelum ada peringkat
- CWU 1 SurgeryDokumen23 halamanCWU 1 SurgeryAmelia AkmarBelum ada peringkat
- Physical Asessment TomiDokumen6 halamanPhysical Asessment Tomirhegell100% (1)
- Case Study Colorectal CancerDokumen23 halamanCase Study Colorectal CancerLeogalvez BedanoBelum ada peringkat
- Family Case SampleDokumen25 halamanFamily Case SampleGrInDoVe9097Belum ada peringkat
- Hemorrahge Secondary To Multiple Stab WoundDokumen26 halamanHemorrahge Secondary To Multiple Stab Wounddodong skyroseBelum ada peringkat
- Bab I: A. Identitas PasienDokumen12 halamanBab I: A. Identitas PasienRondiah DyahBelum ada peringkat
- Ward Paper LegitDokumen13 halamanWard Paper LegitLuigi FranciscoBelum ada peringkat
- Case Presentation COPDDokumen25 halamanCase Presentation COPDBenfranson Benoza III0% (1)
- Pancreatic CancerDokumen15 halamanPancreatic CancerMutiana Muspita JeliBelum ada peringkat
- Sample HADokumen8 halamanSample HAFlorenceUyBelum ada peringkat
- H&P FormatDokumen7 halamanH&P FormatRaffy Gutman100% (1)
- IBS Irritable Bowel Syndrome A Gastroenterologist Answers Your Questions: What Is It? Why Do I Have It? How Can I Get Well?Dari EverandIBS Irritable Bowel Syndrome A Gastroenterologist Answers Your Questions: What Is It? Why Do I Have It? How Can I Get Well?Belum ada peringkat
- The IBS Healing Plan: Natural Ways to Beat Your SymptomsDari EverandThe IBS Healing Plan: Natural Ways to Beat Your SymptomsPenilaian: 3 dari 5 bintang3/5 (9)
- Essenza Refurbished Siemens MRI MachineDokumen2 halamanEssenza Refurbished Siemens MRI Machinetech.arnicahealthBelum ada peringkat
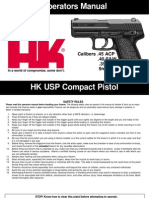
- HK USP CompactDokumen56 halamanHK USP CompactJonathan CrenshawBelum ada peringkat
- DalmatiaDokumen265 halamanDalmatiaomissam2Belum ada peringkat
- Nonlinear Analysis and Optimal Design of Reinforced Concrete Plates and ShellsDokumen17 halamanNonlinear Analysis and Optimal Design of Reinforced Concrete Plates and Shellsrodain najjarBelum ada peringkat
- QW PDFDokumen45 halamanQW PDFkarthikeyan PBelum ada peringkat
- Power System Analysis and Design EE-461: Tassawar Kazmi Lecturer, EE Department, Seecs, NustDokumen10 halamanPower System Analysis and Design EE-461: Tassawar Kazmi Lecturer, EE Department, Seecs, NustShahab SaqibBelum ada peringkat
- The Effective SpanDokumen4 halamanThe Effective SpanMohamed FarahBelum ada peringkat
- Darmoatmodjo 2023Dokumen7 halamanDarmoatmodjo 2023mayaBelum ada peringkat
- Cryogenic Insulation TechnologyDokumen61 halamanCryogenic Insulation Technologyeduard.turon100% (1)
- Bosch Rexroth EFC3600 Manual PDFDokumen238 halamanBosch Rexroth EFC3600 Manual PDFHomero Rios PeñaBelum ada peringkat
- TNM Sites May 2023Dokumen24 halamanTNM Sites May 2023Joseph ChikuseBelum ada peringkat
- Beautiful Results: Simple Procedure 1. Etch 2. Bond 3. RestoreDokumen4 halamanBeautiful Results: Simple Procedure 1. Etch 2. Bond 3. RestoreEuclides Soza CalvoBelum ada peringkat
- Urgent Medical Device CorrectionDokumen4 halamanUrgent Medical Device CorrectionVladimir OsunaBelum ada peringkat
- Norma ASTM C171Dokumen2 halamanNorma ASTM C171Jony Gutiérrez100% (1)
- Zen Intro To Buddhism & Practice of ZazenDokumen33 halamanZen Intro To Buddhism & Practice of ZazendudcomeonBelum ada peringkat
- Astm D3078-02Dokumen3 halamanAstm D3078-02Geoff EricksonBelum ada peringkat
- Zeolites and Ordered Porous Solids - Fundamentals and ApplicationsDokumen376 halamanZeolites and Ordered Porous Solids - Fundamentals and ApplicationsHenrique Souza100% (1)
- Unusual and Marvelous MapsDokumen33 halamanUnusual and Marvelous MapsRajarajan100% (1)
- Nukote Aegis SubmittalDokumen112 halamanNukote Aegis SubmittalMarco Dos Santos NevesBelum ada peringkat
- Rolling Fig Q A AnalysisDokumen11 halamanRolling Fig Q A AnalysisRavinder Antil100% (9)
- ME4542/ME4542-G: N and P-Channel 30-V (D-S) MOSFETDokumen7 halamanME4542/ME4542-G: N and P-Channel 30-V (D-S) MOSFETfelipe ayalaBelum ada peringkat
- Mechanical Components SectionDokumen428 halamanMechanical Components Sectionxristo xristovBelum ada peringkat
- 0 Act Sunum 2020 NewwDokumen58 halaman0 Act Sunum 2020 NewwPınar AdsızBelum ada peringkat
- Line CodingDokumen27 halamanLine CodingshridonBelum ada peringkat
- P&S U V PracticeDokumen4 halamanP&S U V PracticeHari KrushnaBelum ada peringkat
- PEPSIDokumen99 halamanPEPSIkingloiyaBelum ada peringkat
- IAL Hemanta Kumar KarDokumen639 halamanIAL Hemanta Kumar KarTalita Abrani100% (4)
- What Is Geyi - V MairDokumen31 halamanWhat Is Geyi - V MairbodhitanBelum ada peringkat
- Starlift MetricDokumen2 halamanStarlift MetricCralesBelum ada peringkat
- Wolfi Landstreicher - Willful Disobedience - Number 3Dokumen32 halamanWolfi Landstreicher - Willful Disobedience - Number 3populaererBelum ada peringkat