Bar Dram 2000
Diunggah oleh
Prasetyö AgungHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bar Dram 2000
Diunggah oleh
Prasetyö AgungHak Cipta:
Format Tersedia
Original article
Rapid rehabilitation in elderly patients after laparoscopic colonic resection
L. Bardram, P. Funch-Jensen and H. Kehlet
Department of Surgical Gastroenterology 435, Hvidovre University Hospital, DK-2650 Hvidovre, Denmark Correspondence to: Dr L. Bardram
Background: Introduction of the laparoscopic surgical technique has reduced hospital stay after colonic
resection from about 810 to 46 days. In most studies, however, specic attention has not been paid to changes in perioperative protocols required to maximize the advantages of the minimally invasive procedure. In the present study the laparoscopic approach was combined with a perioperative multimodal rehabilitation protocol. Methods: After laparoscopically assisted colonic resection, patients were treated with epidural local anaesthesia for 2 days, early mobilization and enteral nutrition. Routine use of morphine and traditional tubes, drains and prolonged bladder catheterization was avoided. Results: Laparoscopic resection was intended in 50 consecutive patients, of median age 81 years. The conversion rate to open resection was 22 per cent. In patients in whom the procedure was completed laparoscopically the median hospital stay was 25 days; defaecation occurred in 92 per cent of patients within 3 days. Patients were mobilized for more than 8 h daily from day 2. Conclusion: Recovery after colonic surgery was improved considerably by combining the use of a laparoscopic technique with a multimodal rehabilitation protocol of pain relief, early mobilization and oral nutrition.
Paper accepted 28 April 2000 British Journal of Surgery 2000, 87, 15401545
Introduction
The indications for laparoscopic colonic resection remain controversial1, and data from four randomized studies have shown only slight improvements in short-term morbidity and hospital stay26. However, a common feature of both the randomized26 and non-randomized79 comparisons between laparoscopic and open colonic resection is that the general perioperative care protocol has not been adjusted to take account of recent scientic data on the use of optimal pain relief, which facilitates early mobilization, reduces postoperative ileus and permits early enteral nutrition10,11. Moreover, most studies have not avoided routine use of gastrointestinal tubes, drains and prolonged urinary bladder catheterization10,11. Interestingly, hospital stay has been reduced to between 2 and 5 days in non-randomized series of open colonic resection with revision of the perioperative care protocol and use of multimodal rehabilitation with optimal pain relief, early mobilization and nutrition1215. These results compare favourably with laparoscopic series that have employed traditional postoperative care
1540
protocols29. In a preliminary study of eight elderly and/ or high-risk patients who underwent laparoscopic colonic resection, multimodal rehabilitation with continuous epidural analgesia, enforced early mobilization and enteral nutrition decreased hospital stay to 23 days16. The present study represents the cumulative experience in 50 consecutive elderly or high-risk patients with intended laparoscopic colonic resection combined with this postoperative rehabilitation protocol.
Patients and methods
Patients Fifty consecutive elderly or high-risk patients scheduled for elective colonic resection in the years 19941996 were studied. Patients with malignant disease were included if they were aged at least 75 years, or 70 years or more and receiving treatment for chronic cardiopulmonary disease. Patients with benign disease were included if they were aged 70 years or more. Furthermore, inclusion required that
2000 Blackwell Science Ltd
British Journal of Surgery 2000, 87, 15401545
L. Bardram, P. Funch-Jensen and H. Kehlet Laparoscopic colonic resection in the elderly 1541
patients were self caring and admitted directly from home. Patients with tumours in the transverse colon or rectum were not included. All patients were informed orally and in writing about the laparoscopic procedure and the postoperative protocol of epidural analgesia, early feeding and mobilization, and the expected discharge on day 2 after operation, provided that all organ functions were normalized. Preoperative mechanical bowel preparation was performed with macrogol 3000 balanced electrolyte solution (hospital pharmacy product). A single peroperative dose of antibiotics (cefuroxime and metronidazole) was given intravenously. Anaesthesia and postoperative analgesia A thoracic epidural catheter was inserted at T7T9 and 69 ml 05 per cent bupivacaine was administered before operation. Thereafter general anaesthesia was induced by midazolam 015 mg/kg, fentanyl 01025 mg and enurane and nitrous oxideoxygen. The epidural blockade was maintained with 05 per cent bupivacaine 4 ml/h during operation and continued after operation for 48 h with 025 per cent bupivacaine 4 ml/h. At the end of surgery 20 ml 025 per cent bupivacaine was injected beneath the fascia and subcutaneously in the largest incision. After operation, oral tenoxicam 20 mg or paracetamol 2 g 12 hourly was given daily for 6 days. Rescue analgesia included ibuprofen 600 mg every 8 h. Opioids were not given routinely in order to avoid cerebral and bowel motility side-effects. Intraoperative intravenous uid was restricted to a maximum of 1500 ml, unless bleeding indicated otherwise. Surgical procedures Colonic resections were performed using a laparoscopically assisted technique as described previously16. Postoperative care protocol Gastrointestinal tubes were not used after operation. Oral feeding was initiated within a few hours of operation with uids up to 1000 ml, including two protein-enriched drinks in the afternoon or evening of operation. From day 1 after operation enteral nutrition with solid food and four protein drinks daily plus free uid intake aiming at at least 2000 ml was initiated. The urinary bladder catheter was removed on the morning after operation. Mobilization was enforced according to a xed schedule aiming at 2 h on the day of surgery, 6 h on the rst day and 8 h or more from day 2. Cisapride 20 mg was given every 12 h. The epidural catheter was removed before noon on the second day and discharge planned that afternoon (approximately 48 h after opera 2000 Blackwell Science Ltd
tion). A consultation in the outpatient clinic was arranged 10 days after operation for removal of stitches, information on histological ndings and registration of data. Pain, nausea and fatigue were recorded from days 1 to 10 using a four-point scale (03 representing none, slight, moderate and severe respectively). The need for additional analgesics, oral intake, vomiting, defaecation and duration of mobilization were recorded for 10 days after operation. After discharge the patients completed a specic questionnaire recording these variables. Registration of complications and need for rehospitalization was recorded for the rst 30 days after operation. The patients received written information and the telephone numbers of the surgeons responsible and the department. One month after operation patients were asked whether they were content with the regimen, including pain management and early discharge from hospital.
Results
Fifty patients with a median age of 81 (range 7093) years were included. Five patients aged between 70 and 75 years were included as they had benign disease and/or severe cardiopulmonary disease. Seventeen patients were American Society of Anesthesiologists (ASA) grade I, 25 patients ASA II and eight patients ASA III. Twenty-six patients were receiving medical treatment for cardiovascular and/or pulmonary disease. Of 45 patients with malignant disease, 25 had Dukes' B, 17 Dukes' C and two had Dukes' `D' lesions, and one patient had colonic stenosis due to ovarian cancer (not diagnosed before operation). The operative procedures performed are listed in Table 1. Thirty-nine operations were completed laparoscopically while 11 (22 per cent) needed conversion to an open procedure because of tumour invasion of neighbouring organs, unclear anatomy, ovarian cancer or an intraoperative tear in the anastomotic line following removal of the
Surgical procedures performed in 50 elderly patients (median age 81 years) who underwent intended laparoscopic colonic resection
Procedure Right hemicolectomy Left hemicolectomy Sigmoid resection* Ileotransversostomy Total Completed laparoscopically 24 4 11 0 39 Converted to open procedure 2 1 7 1 11 Total 26 5 18 1 50
Table 1
*Synchronous small bowel resection (two), hysterectomy and salpingooophorectomy (one)
www.bjs.co.uk
British Journal of Surgery 2000, 87, 15401545
1542
Laparoscopic colonic resection in the elderly L. Bardram, P. Funch-Jensen and H. Kehlet
Table 2
Reasons for conversion and postoperative course in 11 patients whose operation was converted to open surgery
n Intended operation Left hemicolectomy Sigmoid resection Right hemicolectomy Reasons for conversion Cancer growth into neighbouring organs Unclear anatomy Technical difficulty Ovarian cancer with sigmoid stenosis Rectovesical fistula (diverticulitis) Postoperative complications Colonic necrosis Anastomotic leakage Duodenal ulcer Hospital stay (days) Uncomplicated cases Complicated cases
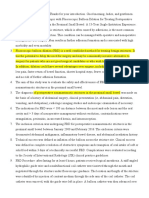
18 16 14 Daily mobilization (h)
1 7 3 6 2 1 1 1 1 1 1 10 (515)* 37 and 64
12 10 8 6 4 2
10
Time after operation (days)
Fig. 1 Median (range) postoperative mobilization in 36 elderly
*Values are median (range); one patient with disseminated disease stayed in hospital until death 75 days after operation
Table 3
patients (median age 81 years) after completed laparoscopic colonic resection (three patients were excluded because of reoperation in the early postoperative period)
Postoperative gastrointestinal function in 39 elderly patients (median age 81 years) after laparoscopic colonic resection
No. of patients Day 1 Nausea Vomiting Oral intake > 2000 ml/day Defaecation 3 3 26 29 Day 2 2 1 34 34 Day 3 2 1 n.a. 36
abdominal incision was 7 (range 412) cm. Median intraoperative blood loss was 50 (range 0200) ml. Gastrointestinal function Recovery of gastrointestinal function is shown in Table 3. Most patients operated on laparoscopically had defaecation within 48 h of operation. Thirty-four of the 39 patients had an oral intake of at least 2000 ml within 48 h of operation. Three patients had reoperation in the early postoperative period (Table 4). Pain, fatigue and mobilization The median postoperative pain score after discharge was 1 (slight), and only ve patients in the laparoscopic group took morphine tablets (10 mg) within the 10-day postoperative period. Postoperative mobilization was normalized early (Fig. 1). The median fatigue score was 15 (range 02) during the rst 6 days and thereafter 05 (range 02). Hospital stay Twenty-six of the 39 patients operated on laparoscopically were discharged on day 2 (17 patients) or day 3 (nine), median stay was 25 days (Fig. 2). The reasons for staying in hospital beyond the scheduled 2 days included complications (Table 4), difculty in re-establishing the patient's usual home care service (four patients), chronic hip arthritis pain (one) or a non-functioning epidural catheter (two)
2000 Blackwell Science Ltd
Three patients underwent reoperation in the early postoperative period. n.a., Data not available
Table 4
Postoperative complications in 39 elderly patients (median age 81 years) after laparoscopic colonic resection
No. of patients Complications Anastomotic leak Small bowel perforation Mechanical bowel obstruction Wound haematoma Renal dysfunction Death 8 2 1 3 1 1 2
surgical stapler in one patient. The postoperative course of the patients whose operation was converted is shown in Table 2. In the 39 patients in whom the operation was completed laparoscopically, the median duration of operation was 180 (range 120270) min and the median length of the
British Journal of Surgery 2000, 87, 15401545 www.bjs.co.uk
L. Bardram, P. Funch-Jensen and H. Kehlet Laparoscopic colonic resection in the elderly 1543
18 16 No. of patients discharged 14 12 10 8 6 4 2 0 1 2 3 4 5 6 7 10 13 70 90 Time after operation (days)
given. One patient thought she had been discharged too early (on day 3). With this exception, time of discharge was well accepted and, as described above, also modied individually depending on social factors.
Discussion
Fig. 2 Day of discharge in 38 elderly patients (median age
81 years) after completed laparoscopic colonic resection. Median stay was 25 days
which required treatment with narcotics that resulted in delayed defaecation. Hospital stay of the patients whose operation was converted to an open procedure is shown in Table 2. Complications Postoperative complications are shown in Table 4. Among the patients with complications, two had been discharged on day 2 and 3. One patient was readmitted with signs of small bowel obstruction on day 5 and underwent reoperation on day 9; the other patient was readmitted on day 9 with abdominal pain and had reoperation for anastomotic leakage. No other patients were readmitted. Complications that occurred in the 11 patients whose operation was converted to an open procedure are shown in Table 2. Port-site metastasis One patient with a Dukes' B tumour in the caecum and invasion into the abdominal wall developed metastases at trocar sites 4 months after operation. One patient with a Dukes' C tumour had widespread intra-abdominal tumour growth including tumour invasion near a trocar site 1 year after operation. Patient satisfaction Patients who did not experience major complications were all satised with the pain management and the information
2000 Blackwell Science Ltd
Postoperative recovery and hospital stay after colonic resection depends on several factors including the magnitude of surgical trauma, pain, paralytic ileus, fatigue, organ dysfunction as well as use of traditional regimens with gastrointestinal tubes and restriction of oral intake10. Single-modality intervention with laparoscopically assisted colonic resection has improved recovery and reduced hospital stay after colonic resection from 810 to 46 days19. In previous studies, however, no specic attention has been paid to changes in perioperative protocols required to maximize the advantages of the reduced trauma response obtained by the minimally invasive technique. In the present study, the laparoscopic approach was combined with a multimodality effort to improve postoperative rehabilitation and reduce hospital stay. Optimal pain relief was ensured by use of epidural local anaesthetics. Early postoperative mobilization and enteral nutrition was enforced. Other factors that may limit early rehabilitation, such as use of gastrointestinal tubes, drains and prolonged bladder catheterization, were avoided. The results of the present study conrm the initial observations in eight patients; such a regimen may signicantly enhance postoperative recovery after colonic resection in elderly or highrisk patients and reduce median postoperative hospital stay to 23 days in patients with a median age of 81 years16. It represents a potential major advance compared with previous results19,17. An important nding was that the conventional paralytic ileus period could apparently be reduced to 12 days with the combined regimen of laparoscopic surgery, epidural local anaesthetic blockade (without opioids) and early enteral nutrition. Recently Neudecker et al.18 failed to conrm the positive effect of epidural analgesia in laparoscopic sigmoidectomy. However, in that study a low (T9 T12) thoracic epidural analgesia was used, which may explain the side-effects with motor blockade and the insignicant effect on paralytic ileus. Furthermore, the postoperative care protocol was not modied to the same extent as in the present study. The lack of signicant cardiopulmonary complications after completed laparoscopic operations suggests that the multimodal regimen with optimal pain relief, early mobilization and reduced surgical trauma response may reduce postoperative organ dysfunction in these elderly patients.
www.bjs.co.uk British Journal of Surgery 2000, 87, 15401545
1544
Laparoscopic colonic resection in the elderly L. Bardram, P. Funch-Jensen and H. Kehlet
The surgical complications (anastomotic leakage, mechanical bowel obstruction) seem not to be inuenced by the multimodal regimen applied. The institution of early enteral nutrition has been demonstrated to be safe in several randomized controlled clinical trials10,11,19. As noted in previous studies19,17 intended laparoscopic colonic resection is not always possible and a conversion rate between of 10 and 20 per cent is often reported. In this study, the majority of patients had malignant disease, and the main cause for conversion was tumour growth into neighbouring organs. Patients whose operation was converted received standard postoperative therapy after open surgery, which included epidural analgesia (containing morphine) and did not include the other elements of the multimodal regimen. Registration of gastrointestinal function, mobilization, pain and fatigue was not performed in these patients as there was no intention of comparing these two groups. The potential economic benet of laparoscopic colonic resection is controversial19,19,20, mostly because no major reduction in hospital stay has been achieved and because the overall costs in patients with operations converted to open resection have been high20,21. An economic analysis was not performed in the present study and assessment of potential differences will require studies with similar postoperative care protocols for laparoscopically completed, converted and open procedures. Previous randomized studies comparing hospital stay and morbidity in laparoscopic versus open colonic resection have not demonstrated substantial advantages for the laparoscopic technique26. However, revision of perioperative care protocols and introduction of multimodal rehabilitation regimens are important for improving outcome10,11, and there is therefore a need to reconsider the design of future randomized trials designed to compare the two types of surgical technique. In this context it is important to emphasize that preliminary observations have demonstrated that the use of multimodal rehabilitation protocols, similar to those used in the present study, have enhanced recovery and reduced hospital stay to between 2 and 5 days after open colonic resection1215. These ndings should be taken into consideration in future randomized trials comparing laparoscopic and open colonic resection.
References
1 Tomita H, Marcello PW, Milsom JW. Laparoscopic surgery of the colon and rectum. World J Surg 1999; 23: 397405. MJ, Delgado S, Campo 2 Lacy AM, Carcia-Valdecasas JC, Pique E, Bordas JM et al. Short-term outcome analysis of a randomised study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc 1995; 9: 11015.
British Journal of Surgery 2000, 87, 15401545 www.bjs.co.uk
3 Stage JG, Schulze S, Mller P, Overgaard H, Andersen M, Rebsdorf-Pedersen VB et al. Prospective randomized study of laparoscopic versus open colonic resection for adenocarcinoma. Br J Surg 1997; 84: 3916. 4 Schwenk W, Bo hm B, Mu ller JM. Postoperative pain and fatigue after laparoscopic or conventional colorectal resections. A prospective randomized trial. Surg Endosc 1998; 12: 11316. 5 Schwenk W, Bo hm B, Witt C, Junghans T, Gru ndel K, Mu ller JM. Pulmonary function following laparoscopic or conventional colorectal resection: a randomized controlled evaluation. Arch Surg 1999; 134: 612. 6 Milson JW, Bo hm B, Hammerhofer KA, Fazio V, Steiger E, Elson P. A prospective, randomized trial comparing laparoscopic versus conventional techniques in colorectal cancer surgery: a preliminary report. J Am Coll Surg 1998; 187: 4655. 7 Chen HH, Wexner SD, Weiss EG, Nogueras JJ, Alabaz O, Iroatulam AJN et al. Laparoscopic colectomy for benign colorectal disease is associated with a signicant reduction in disability as compared with laparotomy. Surg Endosc 1998; 12: 1397400. 8 Franklin ME Jr, Rosenthal D, Abrego-Medina D, Dorman JP, Glass JL, Norem R et al. Prospective comparison of open vs. laparoscopic colon surgery for carcinoma: ve-year results. Dis Colon Rectum 1996; 39(Suppl 10): S3546. 9 Khalili TM, Fleshner PR, Hiatt JR, Sokol TP, Manookian C, Tsushima G et al. Colorectal cancer: comparison of laparoscopic with open approaches. Dis Colon Rectum 1998; 41: 8328. 10 Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997; 78: 60617. 11 Wexner SD. Standardized perioperative care protocols and reduced length of stay after colon surgery. J Am Coll Surg 1998; 186: 58993 (Editorial). 12 Miniche S, Bu low S, Hesselfeldt P, Hestbk A, Kehlet H. Convalecence and hospital stay after colonic surgery with balanced analgesia, early oral feeding, and enforced mobilisation. Eur J Surg 1995; 161: 2838. 13 Liu SS, Carpenter RL, Mackey DC, Thirlby RC, Rupp SM, Shine TSJ et al. Effects of perioperative analgesic technique on rate of recovery after colon surgery. Anesthesiology 1995; 83: 75765. 14 Bradshaw BGG, Liu SS, Thirlby RC. Standard perioperative care protocols and reduced length of stay after colon surgery. J Am Coll Surg 1998; 186: 5016. 15 Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg 1999; 86: 22730. 16 Bardram L, Funch Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet 1995; 345: 7634. 17 Stewart BT, Stitz RW, Lumley JW. Laparoscopically assisted colorectal surgery in the elderly. Br J Surg 1999; 86: 93841.
2000 Blackwell Science Ltd
L. Bardram, P. Funch-Jensen and H. Kehlet Laparoscopic colonic resection in the elderly 1545
18 Neudecker J, Schwenk W, Junghans T, Pietsch S, Bo hm B, Mu ller JM. Randomized controlled trial to examine the inuence of thoracic epidural analgesia on postoperative ileus after laparoscopic sigmoid resection. Br J Surg 1999; 86: 12925. 19 Reissman P, Teoh T-A, Cohen SM, Weiss EG, Nogueras JJ, Wexner SD. Is early oral feeding safe after elective colorectal surgery? A prospective randomized trial. Ann Surg 1995; 222: 737.
20 Philipson BM, Bokey EL, Moore JWE, Chapuis PH, Bagge E. Cost of open versus laparoscopically assisted right hemicolectomy for cancer. World J Surg 1997; 21: 21417. 21 Bouvet M, Manseld PF, Skibber JM, Curley SA, Ellis LM, Giacco GG et al. Clinical, pathologic, and economic parameters of laparoscopic colonic resection for cancer. Am J Surg 1998; 176: 5548.
2000 Blackwell Science Ltd
www.bjs.co.uk
British Journal of Surgery 2000, 87, 15401545
Anda mungkin juga menyukai
- Top Trials in Gastroenterology & HepatologyDari EverandTop Trials in Gastroenterology & HepatologyPenilaian: 4.5 dari 5 bintang4.5/5 (7)
- Top Trials in Gastroenterology & Hepatology, 2nd EditionDari EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionBelum ada peringkat
- Acute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineDokumen6 halamanAcute Rehabilitation Program After Laparoscopic Colectomy Using Intravenous LidocaineKu Badlisyah Ku AzizBelum ada peringkat
- Karlsson 2015Dokumen6 halamanKarlsson 2015fayzaBelum ada peringkat
- Jurnal DewiDokumen8 halamanJurnal DewiAD MonikaBelum ada peringkat
- Post-Oesophagectomy Early Enteral Nutrition Via A Needle Catheter Jejunostomy: 8-Year Experience at A Specialist UnitDokumen8 halamanPost-Oesophagectomy Early Enteral Nutrition Via A Needle Catheter Jejunostomy: 8-Year Experience at A Specialist UnitEssoulaymani FirdawsBelum ada peringkat
- Fast-Track Recovery Programme After Pancreatico-Duodenectomy Reduces Delayed Gastric EmptyingDokumen7 halamanFast-Track Recovery Programme After Pancreatico-Duodenectomy Reduces Delayed Gastric EmptyinghoangducnamBelum ada peringkat
- Diificult AirwayDokumen13 halamanDiificult AirwayBhi-An BatobalonosBelum ada peringkat
- Fast Track Programme in Liver Surgery - BJS 2013Dokumen6 halamanFast Track Programme in Liver Surgery - BJS 2013RobiViBelum ada peringkat
- Ambulatory Laparoscopic CholecystectomyDokumen6 halamanAmbulatory Laparoscopic CholecystectomyJesús ReyesBelum ada peringkat
- Case Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseaseDokumen4 halamanCase Report: Regional Anaesthesia - Anaesthesia of Choice in Chronic Kidney DiseasetafalubisBelum ada peringkat
- 01 HepatogastroDokumen3 halaman01 Hepatogastroyacine26Belum ada peringkat
- Jimbo 2017Dokumen15 halamanJimbo 2017Sahily MoralesBelum ada peringkat
- Transanal Endorectal PullthroughDokumen8 halamanTransanal Endorectal PullthroughMuhammad Harmen Reza SiregarBelum ada peringkat
- A Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisDokumen5 halamanA Prospective Treatment Protocol For Outpatient Laparoscopic Appendectomy For Acute AppendicitisBenjamin PaulinBelum ada peringkat
- Postoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?Dokumen5 halamanPostoperative Management After Loop Ileostomy Closure: Are We Keeping Patients in Hospital Too Long?shah hassaanBelum ada peringkat
- Usefulness of Gum Chewing To Decrease Postoperative Ileus in Colorectal Surgery With Primary Anastomosis: A Randomized Controlled TrialDokumen5 halamanUsefulness of Gum Chewing To Decrease Postoperative Ileus in Colorectal Surgery With Primary Anastomosis: A Randomized Controlled TrialTay LiMinBelum ada peringkat
- Gum Chewing SurgeryDokumen3 halamanGum Chewing SurgeryTony YuliantoBelum ada peringkat
- Corto y Largo PlazoDokumen6 halamanCorto y Largo PlazoElard Paredes MacedoBelum ada peringkat
- Conventional Versus Laparoscopic Surgery For Acute AppendicitisDokumen4 halamanConventional Versus Laparoscopic Surgery For Acute AppendicitisAna Luiza MatosBelum ada peringkat
- Journal Medicine: The New EnglandDokumen7 halamanJournal Medicine: The New England'Muhamad Rofiq Anwar'Belum ada peringkat
- Laproscopic Vagotony PaperDokumen4 halamanLaproscopic Vagotony Paperpeter_mrBelum ada peringkat
- Pi Is 2213576614000049Dokumen3 halamanPi Is 2213576614000049Ditha FadhilaBelum ada peringkat
- Gum Chewing Stimulates Early Return of Bowel Motility After Caesarean SectionDokumen6 halamanGum Chewing Stimulates Early Return of Bowel Motility After Caesarean Sectionstepharry08Belum ada peringkat
- Post LaparosDokumen3 halamanPost Laparosvin1891Belum ada peringkat
- Outcomes of Early Versus Delayed Cholecystectomy in Patients With Mild To Moderate Acute Biliary Pancreatitis: A Randomized Prospective StudyDokumen36 halamanOutcomes of Early Versus Delayed Cholecystectomy in Patients With Mild To Moderate Acute Biliary Pancreatitis: A Randomized Prospective StudyAnonymous Uh2myPxPHBelum ada peringkat
- Cirugía de Colon Abierta Con "Fast Track" o Recuperación AceleradaDokumen10 halamanCirugía de Colon Abierta Con "Fast Track" o Recuperación AceleradaManuelEduardoSanchezSotoBelum ada peringkat
- Asghar Ali OADokumen4 halamanAsghar Ali OAshah hassaanBelum ada peringkat
- 15 Original ArticleDokumen4 halaman15 Original ArticleNayan ChaudhariBelum ada peringkat
- Duct Cholecystectomy: Major LaparoscopicDokumen10 halamanDuct Cholecystectomy: Major LaparoscopicShahnawaz AhangarBelum ada peringkat
- General Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueDokumen3 halamanGeneral Surgery: Ruptured Liver Abscess: A Novel Surgical TechniqueRahul SinghBelum ada peringkat
- Surgical Endoscopy 6Dokumen102 halamanSurgical Endoscopy 6Saibo BoldsaikhanBelum ada peringkat
- Periop UrologyKoubaartikelDokumen4 halamanPeriop UrologyKoubaartikeljustin_saneBelum ada peringkat
- Stapled Rectal Mucosectomy vs. Close HemorrhoidectomyDokumen9 halamanStapled Rectal Mucosectomy vs. Close HemorrhoidectomyNadllely Garcia ZapataBelum ada peringkat
- Risk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryDokumen31 halamanRisk of Failure in Pediatric Ventriculoperitoneal Shunts Placed After Abdominal SurgeryWielda VeramitaBelum ada peringkat
- Presentation Sheets Zhang Dong-Yang Feb.22nd的副本Dokumen3 halamanPresentation Sheets Zhang Dong-Yang Feb.22nd的副本YangBelum ada peringkat
- Sumber Jurnal ReadingDokumen15 halamanSumber Jurnal ReadingagungBelum ada peringkat
- Ahbps-24-44 Appendicitis After Liver Transplantation JournalDokumen8 halamanAhbps-24-44 Appendicitis After Liver Transplantation JournalIndah JamtaniBelum ada peringkat
- World Journal of Surgical Oncology: Alternative Reconstruction After PancreaticoduodenectomyDokumen4 halamanWorld Journal of Surgical Oncology: Alternative Reconstruction After PancreaticoduodenectomyPra YudhaBelum ada peringkat
- Ne en WhippleDokumen9 halamanNe en WhippleOscar VillacresBelum ada peringkat
- Laparoscopic Cholecystectomy Under Spinal Anaesthesia: A Prospective StudyDokumen4 halamanLaparoscopic Cholecystectomy Under Spinal Anaesthesia: A Prospective Studyrazaqhussain00Belum ada peringkat
- Impact of Postoperative Morbidity On Long-Term Survival After OesophagectomyDokumen10 halamanImpact of Postoperative Morbidity On Long-Term Survival After OesophagectomyPutri PadmosuwarnoBelum ada peringkat
- Protocol oDokumen8 halamanProtocol oCynthia ChávezBelum ada peringkat
- Utd 04524 Clinical - Article KunduzDokumen5 halamanUtd 04524 Clinical - Article Kunduzzenatihanen123Belum ada peringkat
- Pancreatitis AgudaDokumen6 halamanPancreatitis AgudaElias Emmanuel JaimeBelum ada peringkat
- Medical Surgical NotesDokumen17 halamanMedical Surgical NotesNP YarebBelum ada peringkat
- Anestesia ObesidadDokumen7 halamanAnestesia ObesidadPablo GuioteBelum ada peringkat
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDokumen7 halamanPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahBelum ada peringkat
- Anesthesia For Emergency AppendectomyDokumen44 halamanAnesthesia For Emergency AppendectomyPrincess Lorenzo MiguelBelum ada peringkat
- CreonDokumen12 halamanCreonNikola StojsicBelum ada peringkat
- Noninvasive Ventilation For Prevention of Post-Extubation Respiratory Failure in Obese PatientsDokumen8 halamanNoninvasive Ventilation For Prevention of Post-Extubation Respiratory Failure in Obese PatientsLestat80Belum ada peringkat
- Journal ClubDokumen23 halamanJournal ClubThagoon KanjanopasBelum ada peringkat
- Farach 2014Dokumen5 halamanFarach 2014mia widiastutiBelum ada peringkat
- Evidencia 1Dokumen6 halamanEvidencia 1Ricardo Uzcategui ArreguiBelum ada peringkat
- Enhanced Recovery After SurgeryDokumen47 halamanEnhanced Recovery After SurgeryPeri HidayatBelum ada peringkat
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Dokumen5 halamanLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaBelum ada peringkat
- Volume 15, Number 3 March 2011Dokumen152 halamanVolume 15, Number 3 March 2011Nicolai BabaliciBelum ada peringkat
- Togasj 6 25Dokumen6 halamanTogasj 6 25Prabowo SuryaningtyasBelum ada peringkat
- Acute Respiratory Distress in A 3-Year-Old at Daycare: (Enlarge Image)Dokumen4 halamanAcute Respiratory Distress in A 3-Year-Old at Daycare: (Enlarge Image)Ju Lie AnnBelum ada peringkat
- Randomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal SurgeryDokumen7 halamanRandomized Clinical Trial Investigating The Stress Response From Two Different Methods of Analgesia After Laparoscopic Colorectal Surgeryvalerio.messinaBelum ada peringkat
- Jurnal Nanang Beleng PDFDokumen12 halamanJurnal Nanang Beleng PDFKartika KadirBelum ada peringkat
- Intermitten Feeding SchedulesDokumen19 halamanIntermitten Feeding SchedulesPrasetyö AgungBelum ada peringkat
- An Article About Nutrition by Enteral FeedingDokumen6 halamanAn Article About Nutrition by Enteral FeedingPrasetyö AgungBelum ada peringkat
- Tube Feeding by GravityDokumen26 halamanTube Feeding by GravityPrasetyö AgungBelum ada peringkat
- Acut Myelognus PneumoniaDokumen52 halamanAcut Myelognus PneumoniaPrasetyö AgungBelum ada peringkat
- Umsurabaya 1912 Arfenesupr 21 1 Hubungan ADokumen6 halamanUmsurabaya 1912 Arfenesupr 21 1 Hubungan ADhoe LiekowglBelum ada peringkat
- Sketchup-Rhino Cheat SheetDokumen1 halamanSketchup-Rhino Cheat Sheetxanext7Belum ada peringkat
- Armor MagazineDokumen32 halamanArmor Magazine"Rufus"100% (1)
- Method Statement For Cable Trays & Cable Ladders InstallationDokumen7 halamanMethod Statement For Cable Trays & Cable Ladders InstallationJamal Budeiri0% (1)
- Milviz F-15e Poh V 2Dokumen499 halamanMilviz F-15e Poh V 2Jose Ramon Martinez GutierrezBelum ada peringkat
- Accuity: High Speed Automated 2D & 3D Optical Gauging Single Click Setup and InspectionDokumen4 halamanAccuity: High Speed Automated 2D & 3D Optical Gauging Single Click Setup and InspectionAPPLEBelum ada peringkat
- In-Service Welding of Pipelines Industry Action PlanDokumen13 halamanIn-Service Welding of Pipelines Industry Action Planعزت عبد المنعم100% (1)
- FAJASDokumen891 halamanFAJASCecilia GilBelum ada peringkat
- THE WEATHER LISTENING - Stalin GuañunaDokumen1 halamanTHE WEATHER LISTENING - Stalin GuañunaSTALIN JESUS GUA�UNA CHICAIZABelum ada peringkat
- CAC Bubble DiagramsDokumen12 halamanCAC Bubble Diagramsangst6250Belum ada peringkat
- IPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedDokumen1 halamanIPC's 2 Edition of Guidance Manual For Herbs and Herbal Products Monographs ReleasedRakshaBelum ada peringkat
- Egt Margen From The Best ArticalDokumen6 halamanEgt Margen From The Best ArticalakeelBelum ada peringkat
- Yadea User Manual For e Scooter 1546004910Dokumen44 halamanYadea User Manual For e Scooter 1546004910Danthe ThenadBelum ada peringkat
- Sudip Praposal - 1Dokumen20 halamanSudip Praposal - 1Usha BbattaBelum ada peringkat
- RMHE08Dokumen2.112 halamanRMHE08Elizde GómezBelum ada peringkat
- Case StudyDokumen61 halamanCase StudyA GBelum ada peringkat
- Opex and CapexDokumen5 halamanOpex and CapexATM Shafiq Ul AlamBelum ada peringkat
- Intumescent Paint For Steel NZ - Coating - Co.nzDokumen8 halamanIntumescent Paint For Steel NZ - Coating - Co.nzPeter ThomsonBelum ada peringkat
- Southwest Airlines Final ReportDokumen16 halamanSouthwest Airlines Final Reportapi-427311067Belum ada peringkat
- Siemens Internship ReportDokumen84 halamanSiemens Internship Reportujjawalbhojawala100% (1)
- AD1 Elements of Architectural Composition For Placemaking PDFDokumen4 halamanAD1 Elements of Architectural Composition For Placemaking PDFAndre Yap100% (1)
- Physics 101Dokumen21 halamanPhysics 101Kuna KunavathiBelum ada peringkat
- Clinical Case StudyDokumen20 halamanClinical Case Studyapi-252004748Belum ada peringkat
- Sheet Metal Manufacturing Companies NoidaDokumen9 halamanSheet Metal Manufacturing Companies NoidaAmanda HoldenBelum ada peringkat
- Leadership Games and ActivitiesDokumen38 halamanLeadership Games and ActivitiesWilliam Oliss100% (1)
- Project Title Discipline Project Stage Client Attendance CirculationDokumen4 halamanProject Title Discipline Project Stage Client Attendance CirculationgregBelum ada peringkat
- Cell Wall Synthesis InhibitorsDokumen6 halamanCell Wall Synthesis InhibitorsRPh Krishna Chandra JagritBelum ada peringkat
- Course Structure and Content For Mechatronics, Systems and CDokumen32 halamanCourse Structure and Content For Mechatronics, Systems and CAnimonga HajimeBelum ada peringkat
- LighthouseDokumen4 halamanLighthousejaneborn5345Belum ada peringkat
- Chapter 5 AGVDokumen76 halamanChapter 5 AGVQuỳnh NguyễnBelum ada peringkat
- Manual Nice9000v A04Dokumen151 halamanManual Nice9000v A04hoang tamBelum ada peringkat