Uremic Encephalopathy Guide: Causes, Symptoms, Treatment
Diunggah oleh
Sandi BeyJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Uremic Encephalopathy Guide: Causes, Symptoms, Treatment
Diunggah oleh
Sandi BeyHak Cipta:
Format Tersedia
http://emedicine.medscape.
com/article/239191-overview#a0104
Uremic Encephalopathy
Author: James W Lohr, MD; Chief Editor: Vecihi Batuman, MD, FACP, FASN
Uremic encephalopathy is an organic brain disorder. It develops in patients with acute or chronic renal failure, usually when creatinine clearance (CrCl) levels fall and remain below 15 mL/min.[1,
2, 3, 4]
Manifestations of this syndrome vary from mild symptoms (eg, lassitude, fatigue) to severe symptoms (eg, seizures, coma). Severity and progression depend on the rate of decline in renal function; thus, symptoms are usually worse in patients withacute renal failure. Prompt identification of uremia as the cause of encephalopathyis essential because symptoms are readily reversible following initiation ofdialysis.[5, 6]
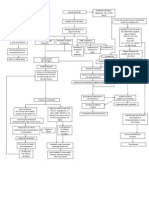
Pathophysiology
Uremic encephalopathy has a complex pathophysiology, and many toxins that accumulate in kidney failure may be contributive. Parathyroid hormone (PTH) likely contributes to uremic encephalopathy.[7] Secondary hyperparathyroidism, which occurs in kidney failure, causes an increase in calcium content in the cerebral cortex. In animal models with uremia, EEG changes were typical of those observed in patients with renal failure. Inuremic patients with secondary hyperparathyroidism, EEG changes have been shown to improve after medical suppression of PTH or parathyroidectomy. The specific mechanism by which PTH causes disturbance in brain function is unclear, but it may be caused by increases in intracellular concentration of calcium in brain cells. However, since the encephalopathy improves with dialysis, which does not have a marked effect on PTH levels, hyperparathyroidism is not thought to be the main cause. Another theory about the etiology of uremic encephalopathy suggests imbalances of neurotransmitter amino acids within the brain. During the early phase of uremic encephalopathy, plasma and cerebrospinal fluid (CSF) determinations indicate that levels of glycine increase and levels of glutamine and GABA decrease; additionally, alterations occur in metabolism of dopamine and serotonin in the brain, which may lead to early symptoms (eg, sensorial clouding). As uremia progresses, it has been proposed that the accumulation of guanidino compounds results in activation of excitatory N-methyl-D-aspartate (NMDA) receptors and inhibition of inhibitory GABA receptors, which may cause myoclonus and seizures.[5, 8, 9] A study of acute kidney injury in mice found evidence of a blood-brain barrier disruption from such injury, with increased neuronal pyknosis and microgliosis. In addition, proinflammatory chemokines were increased in brain tissue.[10] Numerous other uremic toxins may contribute to uremic encephalopathy, but there has been a notable lack of research in this area. Although the encephalopathy correlates roughly with BUN level, urea is not itself thought to be causative.
History
Early symptoms Anorexia Nausea Restlessness Drowsiness Diminished ability to concentrate Slowed cognitive functions More severe symptoms Vomiting Emotional volatility Decreased cognitive function Disorientation Confusion Bizarre behavior As uremic encephalopathy progresses, patients may develop myoclonus, asterixis, seizures, stupor, and coma.
Physical
Altered mental status (confusion) Cranial nerve signs (nystagmus) Papilledema Hyperreflexia, clonus, asterixis Stupor Coma occurs only if uremia remains untreated and progresses. Penyebab GGA dan CKD
Laboratory Studies
Electrolytes, BUN, creatinine, and glucose[12] Markedly elevated BUN and creatinine levels are seen in uremic encephalopathy. Obtain serum electrolyte and glucose measurements to rule outhyponatremia, hypernatremia, hyperglycemia, and hyperosmolar syndromes as the cause of encephalopathy. Obtain a complete blood cell count to detect leukocytosis, which may suggest an infectious cause and determine whether anemia is present. (Anemia may contribute to the severity of mental alterations.) Obtain serum calcium, phosphate, and PTH levels to determine the presence ofhypercalcemia, hypophosphatemia, and severe hyperparathyroidism, which cause metabolic encephalopathy. Serum magnesium levels may be elevated in a patient with renal insufficiency, particularly if the patient is ingesting magnesium-containing antacids.Hypermagnesemia may manifest as encephalopathy. Order a toxicology screen in all patients. Medication levels Determine drug levels because medications may accumulate in patients with kidney failure and contribute to encephalopathy (eg, digoxin, lithium).
Some medications cannot be detected and are excreted by the kidney. These may also accumulate in patients with kidney failure, resulting in encephalopathy (eg, penicillin, cimetidine, meperidine, baclofen).
Imaging Studies
Severe symptoms Obtain an MRI or head CT scan for a uremic patient who presents with severe neurologic symptoms to rule out structural abnormalities (eg, cerebrovascular accident, intracranial mass). A CT scan does not demonstrate any characteristic findings for uremic encephalopathy. With milder symptoms, initially treat the patient with dialysis and observe for neurologic improvement.
Other Tests
Electroencephalogram An EEG is commonly performed on patients with metabolic encephalopathy. Findings typically include the following: (1) slowing and loss of alpha frequency waves, (2) disorganization, and (3) intermittent bursts of theta and delta waves with slow background activity. Reduction in frequency of EEG waves correlates with the decrease in renal function and the alterations in cerebral function. After the initial period of dialysis, clinical stabilization may occur while the EEG findings do not improve. Eventually, EEG results move toward normal. Aside from the routine EEG, evoked potentials (EPs) (ie, EEG signals that occur at a reproducible time after the brain receives a sensory stimulus [eg, visual, auditory, somatosensory]) may be helpful in evaluating uremic encephalopathy. Chronic renal failure prolongs latency of the cortical visual-evoked response. Auditory-evoked responses are generally not altered in uremia, but delays in the cortical potential of the somatosensory-evoked response do occur. Cognitive function tests: Several cognitive function tests are used to evaluate uremic encephalopathy. Uremia may result in worse performance on the trail-making test, which measures psychomotor speed; the continuous memory test, which measures short-term recognition; and the choice reaction time test, which measures simple decision making. Alterations in choice reaction time appear to correlate best with renal failure.
Procedures
Lumbar puncture Lumbar puncture is not routinely performed; however, it may be indicated to find other causes of encephalopathy if a patient's mental status does not improve after initiation of dialysis. No specific CSF finding indicates uremic encephalopathy.
Medical Care
No medications are specific to the treatment of encephalopathy.
The presence of uremic encephalopathy in a patient with either acute kidney failure or chronic kidney failure is an indication for the initiation of dialytic therapy (ie, hemodialysis, peritoneal dialysis, continuous renal replacement therapy). After beginning dialysis, the patient generally improves clinically, although EEG findings may not improve immediately. In patients with end-stage renal disease (ESRD), EEG abnormalities generally improve after several months but may not completely normalize. Address the following factors when treating uremic encephalopathy, which are also included in the standard care of any patient with ESRD:
o o o
Adequacy of dialysis Correction of anemia Regulation of calcium and phosphate metabolism
Consultations
Consult a neurologist if symptoms do not improve upon initiation of dialysis therapy. Consult a vascular surgeon for placement of vascular access in patients with ESRD. Refer patients with ESRD to a dietitian familiar with renal diseases.
Diet
To avoid malnutrition in patients with ESRD, maintain adequate protein intake (>1 g/kg/d) and initiate dialysis (despite the presence of encephalopathy).
Activity
Instruct patients with significant symptoms to continue bed rest.
Further Inpatient Care
Admit patients for dialysis and further workup.
Further Outpatient Care
Schedule maintenance hemodialysis for patients who have ESRD. Carefully monitor mental status.
Inpatient & Outpatient Medications
Administer medications (eg, iron, erythropoietin, phosphate binders, vitamin D analogues) for patients with ESRD to optimize their quality of life. Avoid sedatives.
Transfer
Patients may require transfer to a facility that can provide emergent hemodialysis.
Deterrence/Prevention
Refer patients with chronic kidney disease to a nephrologist for regular monitoring of CrCl so that dialysis may be initiated before encephalopathy develops.
Complications
Seizures Coma Death
Prognosis
With prompt dialytic therapy, the mortality rate is low.
Anda mungkin juga menyukai
- Uremic EncephalopathyDokumen12 halamanUremic EncephalopathyRAechelle_Marc_4102Belum ada peringkat
- Hypertension Pathophysiology and Treatment PDFDokumen6 halamanHypertension Pathophysiology and Treatment PDFBella TogasBelum ada peringkat
- Obstructive Uropathy Secondary To Benign Prostatic HyperplasiaDokumen74 halamanObstructive Uropathy Secondary To Benign Prostatic HyperplasiaGregory Litang100% (1)
- 403 Full PDFDokumen10 halaman403 Full PDFKuroto YoshikiBelum ada peringkat
- HCVDDokumen5 halamanHCVDkhrizaleehBelum ada peringkat
- Risk For Bleeding - Cirrhosis NCPDokumen2 halamanRisk For Bleeding - Cirrhosis NCPPaula AbadBelum ada peringkat
- Closed Humerus Fracture With Radial PalsyDokumen35 halamanClosed Humerus Fracture With Radial PalsyEryn Farahin ZainalBelum ada peringkat
- Tarlac State University College of Nursing case study on choledocholithiasisDokumen53 halamanTarlac State University College of Nursing case study on choledocholithiasisCzarina ManinangBelum ada peringkat
- CHF Group 3 Ncmb312 RleDokumen39 halamanCHF Group 3 Ncmb312 RleMaica Lectana50% (2)
- Pathophysiology of ESRD: Organ Dysfunctions & Associated AbnormalitiesDokumen5 halamanPathophysiology of ESRD: Organ Dysfunctions & Associated AbnormalitiesCarl JardelezaBelum ada peringkat
- Hypertensive Cardiovascular DiseaseDokumen16 halamanHypertensive Cardiovascular DiseaseTintin Ponciano100% (1)
- Pathophysiology of BPHDokumen1 halamanPathophysiology of BPHJerome Matthew Hautea Amorado0% (1)
- Pathophysiology of CholangitisDokumen4 halamanPathophysiology of CholangitisAmni 'Pam' Zulkifar100% (1)
- Human Diseases Case Study 18 ADokumen4 halamanHuman Diseases Case Study 18 Aairickann100% (1)
- Hypertensive UrgencyDokumen8 halamanHypertensive UrgencyTony A.Belum ada peringkat
- NCP CvaDokumen4 halamanNCP CvaMariquita BuenafeBelum ada peringkat
- Schematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesDokumen3 halamanSchematic Diagram: Signs and Symptoms: Headache, Unconsciousness, Nausea and Vomiting, Visual DisturbancesJosett RomanoBelum ada peringkat
- Path o PhysiologyDokumen9 halamanPath o PhysiologyKyle Ü D. CunanersBelum ada peringkat
- HNP Case Scenario For Case StudyDokumen2 halamanHNP Case Scenario For Case StudyDeinielle Magdangal RomeroBelum ada peringkat
- NSTEMIDokumen33 halamanNSTEMIwaazalimahwahidBelum ada peringkat
- Acute Lymphocytic LeukemiaDokumen12 halamanAcute Lymphocytic Leukemiajustin_saneBelum ada peringkat
- CAP and Hypertension: Predisposing and Precipitating FactorsDokumen5 halamanCAP and Hypertension: Predisposing and Precipitating FactorsLeonaPunzalanBelum ada peringkat
- Pathophysiology of Portal HYPERTENSION PDFDokumen11 halamanPathophysiology of Portal HYPERTENSION PDFCamilo VidalBelum ada peringkat
- Introduction - MIDokumen10 halamanIntroduction - MIkhimiiiBelum ada peringkat
- Fractures, PathophysiologyDokumen1 halamanFractures, Pathophysiology4kscribdBelum ada peringkat
- Dr. Sunatrio - Management Hypovolemic ShockDokumen59 halamanDr. Sunatrio - Management Hypovolemic ShockArga Putra SaboeBelum ada peringkat
- InTech-Diabetic Foot and GangreneDokumen25 halamanInTech-Diabetic Foot and GangrenePutu Reza Sandhya PratamaBelum ada peringkat
- What Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistDokumen12 halamanWhat Is Stroke?: BY: Luis Alberto Sanchez Hernandez Physical TherapistLidiaAMonroyRBelum ada peringkat
- Anatomy and Physiology PneumoniaDokumen4 halamanAnatomy and Physiology PneumoniaJohnson MallibagoBelum ada peringkat
- Pathophysiology of HyperthyroidismDokumen4 halamanPathophysiology of HyperthyroidismKitty YuffieBelum ada peringkat
- OUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisDokumen20 halamanOUR LADY OF FATIMA UNIVERSITY Case Study on Post Streptococcal GlomerulonephritisMikaCasimiroBalunanBelum ada peringkat
- Group-1b Myocardial InfarctionDokumen39 halamanGroup-1b Myocardial InfarctionJean ReyesBelum ada peringkat
- Pathophysiology of Meniere FinalDokumen1 halamanPathophysiology of Meniere Final1S VILLEGAS GabrielBelum ada peringkat
- Predisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryDokumen2 halamanPredisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryChloé Jane HilarioBelum ada peringkat
- CHOLANGITISDokumen1 halamanCHOLANGITISKirk Torregosa PañaresBelum ada peringkat
- Congestive Heart FailureDokumen28 halamanCongestive Heart Failuresarguss1480% (5)
- Schematic Diagram Pathophysiology (Book-Based) COPD and TuberculosisDokumen1 halamanSchematic Diagram Pathophysiology (Book-Based) COPD and Tuberculosispragna novaBelum ada peringkat
- Stevens-Johnson Syndrome CASEDokumen38 halamanStevens-Johnson Syndrome CASEChristy Rose AgrisBelum ada peringkat
- Liver CancerDokumen1 halamanLiver CancerTarantado67% (3)
- Myocardial Infarction (Diseases For Oral Revalida)Dokumen12 halamanMyocardial Infarction (Diseases For Oral Revalida)Suzette PipoBelum ada peringkat
- Uremic EncephalophatyDokumen48 halamanUremic EncephalophatySindi LadayaBelum ada peringkat
- Qtsoi Concept MapDokumen5 halamanQtsoi Concept MapGenella BabantoBelum ada peringkat
- Pathophysiology HeadinjuryDokumen1 halamanPathophysiology HeadinjuryK.b. Dequiña100% (1)
- Cardiogenic ShockDokumen21 halamanCardiogenic ShockIslamOteshBelum ada peringkat
- Pathophysiology of DMDokumen4 halamanPathophysiology of DMNicole Louise N. VillanuevaBelum ada peringkat
- PathophysiologyDokumen1 halamanPathophysiologyHazel PalomaresBelum ada peringkat
- Osteoarthritis 1583-170210113823Dokumen34 halamanOsteoarthritis 1583-170210113823Angelic khanBelum ada peringkat
- Benign Prostatic HyperplasiaDokumen9 halamanBenign Prostatic Hyperplasiaanju rachel joseBelum ada peringkat
- PATHOPHYSIOLOGY OF CORONARY ARTERY DISEASEDokumen2 halamanPATHOPHYSIOLOGY OF CORONARY ARTERY DISEASEPamela DomingoBelum ada peringkat
- LacipilDokumen2 halamanLacipilianecunarBelum ada peringkat
- PathophysiologyDokumen1 halamanPathophysiologynitlihpBelum ada peringkat
- Case Study 18 CKDDokumen7 halamanCase Study 18 CKDapi-301049551Belum ada peringkat
- Fracture Closed Complete Displaced Middle Third Femur Right Secondary To FallDokumen102 halamanFracture Closed Complete Displaced Middle Third Femur Right Secondary To FallRaidis PangilinanBelum ada peringkat
- Bacls PDFDokumen23 halamanBacls PDFAngelo Domingo0% (1)
- HCVD KoDokumen10 halamanHCVD KoMarianne BaquilalaBelum ada peringkat
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Nephrology Encephalopathy GuideDokumen6 halamanNephrology Encephalopathy GuideMasriyaniBelum ada peringkat
- Diagnosis Management Hepatic Encephalopathy Diagnosis Dan Penatalaksanaan Ensefalopati HepatikDokumen21 halamanDiagnosis Management Hepatic Encephalopathy Diagnosis Dan Penatalaksanaan Ensefalopati HepatikKadek Rudita YasaBelum ada peringkat
- Hepatic EncephalopathyDokumen16 halamanHepatic Encephalopathyjh_ajjBelum ada peringkat
- ReadmeDokumen1 halamanReadmeHadi SumantriBelum ada peringkat
- Jegol Nov Dec Jan 31-1-19Dokumen1 halamanJegol Nov Dec Jan 31-1-19Sandi BeyBelum ada peringkat
- Sandi Medabots GameDokumen89 halamanSandi Medabots GameSandi BeyBelum ada peringkat
- Proshow Gold CrackDokumen1 halamanProshow Gold CrackSandi BeyBelum ada peringkat
- Salala BumbumDokumen1 halamanSalala BumbumSandi BeyBelum ada peringkat
- PlatinumDokumen1.357 halamanPlatinumHafiezal MuhamadBelum ada peringkat
- PlatinumDokumen1.357 halamanPlatinumHafiezal MuhamadBelum ada peringkat
- Daftar Pustak1Dokumen2 halamanDaftar Pustak1Sandi BeyBelum ada peringkat
- Tingkat Pengetahuan Tentang Cara Penularan Hiv-Aids Sebelum Dan Sesudah Penyuluhan Pada Siswa Sman 1 Gaung Anak Serka Kabupaten Indragiri HilirDokumen10 halamanTingkat Pengetahuan Tentang Cara Penularan Hiv-Aids Sebelum Dan Sesudah Penyuluhan Pada Siswa Sman 1 Gaung Anak Serka Kabupaten Indragiri HilirSandi BeyBelum ada peringkat
- Tangga L Pekerjaan Banyak Harga Di Pegang 1 1 2 3 4 5 1 2 3 4 5 3 1 2 3 4 5 4 1 2 3 4 5 5 1 2 3 4 5 6 1 2 3 4 5Dokumen5 halamanTangga L Pekerjaan Banyak Harga Di Pegang 1 1 2 3 4 5 1 2 3 4 5 3 1 2 3 4 5 4 1 2 3 4 5 5 1 2 3 4 5 6 1 2 3 4 5Sandi BeyBelum ada peringkat
- Salala BumbumDokumen1 halamanSalala BumbumSandi BeyBelum ada peringkat
- PC ConfigDokumen1 halamanPC ConfigSandi BeyBelum ada peringkat
- Higher Algebra - Hall & KnightDokumen593 halamanHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Link Space Brother AnimeDokumen12 halamanLink Space Brother AnimeSandi BeyBelum ada peringkat
- Pattern Approach For Diseases of Mesenteric Small Bowel On Barium StudiesDokumen18 halamanPattern Approach For Diseases of Mesenteric Small Bowel On Barium StudiesSandi BeyBelum ada peringkat
- Higher Algebra - Hall & KnightDokumen593 halamanHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- 1 Reading DefinitionsDokumen11 halaman1 Reading DefinitionsSandi BeyBelum ada peringkat
- AkiDokumen42 halamanAkimarauder_popBelum ada peringkat
- Pathophysiology of Chronic Renal Failure PDFDokumen4 halamanPathophysiology of Chronic Renal Failure PDFDewa Made Rendy SanjayaBelum ada peringkat
- 7297 19768 4 PBDokumen5 halaman7297 19768 4 PBpujiindah lestariBelum ada peringkat
- Oral Manifestations of Chronic Kidney Disease-An OverviewDokumen4 halamanOral Manifestations of Chronic Kidney Disease-An OverviewrinakartikaBelum ada peringkat
- Manajemen Nutrisi Pada Pasien Gangguan GinjalDokumen37 halamanManajemen Nutrisi Pada Pasien Gangguan GinjalReski Kusuma DewiBelum ada peringkat
- CKD 2016Dokumen39 halamanCKD 2016husnaBelum ada peringkat
- Enteric Dialysis Journal of Nephrology Therapeutics 2018 by DR - RanganDokumen9 halamanEnteric Dialysis Journal of Nephrology Therapeutics 2018 by DR - RanganWobik HopeBelum ada peringkat
- Nursing Path o CardsDokumen194 halamanNursing Path o CardsDanielle Shull100% (1)
- Drug Use in Special Conditions - CLD and CKDDokumen93 halamanDrug Use in Special Conditions - CLD and CKDadamu mohammadBelum ada peringkat
- QweqDokumen7 halamanQweqJackieBelum ada peringkat
- Similarity CheckDokumen10 halamanSimilarity Checkmohamed othmeniBelum ada peringkat
- Hot Bath For The Treatment of Chronic Renal FailureDokumen6 halamanHot Bath For The Treatment of Chronic Renal FailureDanish SanyasiBelum ada peringkat
- Seminar On: Chronic Kidney DiseaseDokumen15 halamanSeminar On: Chronic Kidney DiseaseGargi MPBelum ada peringkat
- NCP Chronic Renal FailureDokumen15 halamanNCP Chronic Renal FailureNurul BariyyahBelum ada peringkat
- DialysisDokumen19 halamanDialysisSachin Singh100% (2)
- Nursing management of renal disordersDokumen53 halamanNursing management of renal disordersalexandermarcusBelum ada peringkat
- ORAL MANIFESTATIONS OF SYSTEMIC DISEASES Part 1Dokumen97 halamanORAL MANIFESTATIONS OF SYSTEMIC DISEASES Part 1Shreya singhBelum ada peringkat
- Fluids and Electrolytes PediaDokumen10 halamanFluids and Electrolytes Pediajulesubayubay5428Belum ada peringkat
- Early Risk Score Predicts Treatment for GI BleedingDokumen4 halamanEarly Risk Score Predicts Treatment for GI BleedingjimotivaBelum ada peringkat
- McCance Patho Review QsDokumen17 halamanMcCance Patho Review Qsiamdara100% (1)
- © Medi - Lectures DR Shubham UpadhyayDokumen27 halaman© Medi - Lectures DR Shubham Upadhyayashu13bBelum ada peringkat
- Acute Renal Failure & Chronic Renal FailureDokumen39 halamanAcute Renal Failure & Chronic Renal FailureMarie MayBelum ada peringkat
- Exam #4 - Urinary and Renal-1Dokumen14 halamanExam #4 - Urinary and Renal-1aerislina100% (6)
- Non-Protein Nitrogen CompoundsDokumen6 halamanNon-Protein Nitrogen CompoundspixiedustBelum ada peringkat
- 2021 Hemodialysis Emergencies Core Curriculum 2021Dokumen14 halaman2021 Hemodialysis Emergencies Core Curriculum 2021Ale GutiérrezBelum ada peringkat
- Chronic Kidney DiseaseDokumen11 halamanChronic Kidney DiseaseSalma Mohamed RezkBelum ada peringkat
- Gagal Ginjal Kuliah FarmakoterapiDokumen39 halamanGagal Ginjal Kuliah FarmakoterapiriyuBelum ada peringkat
- Acute Renal FailureDokumen13 halamanAcute Renal FailureGlorianne Palor100% (2)
- ABC Dictionary of Urinary SystemDokumen26 halamanABC Dictionary of Urinary Systemaby_romero9750% (2)
- Renal History and ExamDokumen6 halamanRenal History and ExamTom MallinsonBelum ada peringkat