The Magic Glue Hyaluronan and Its Eraser Hyaluronidase: A Biological Overview
Diunggah oleh
alessandro8265Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The Magic Glue Hyaluronan and Its Eraser Hyaluronidase: A Biological Overview
Diunggah oleh
alessandro8265Hak Cipta:
Format Tersedia
Life Sciences 80 (2007) 1921 1943 www.elsevier.
com/locate/lifescie
Minireview
The magic glue hyaluronan and its eraser hyaluronidase: A biological overview
K.S. Girish , K. Kemparaju
Department of Biochemistry, University of Mysore, Manasagangothri, Mysore, Karnataka State, 560007, India Received 2 November 2006; accepted 19 February 2007
Abstract Hyaluronan (HA) is a multifunctional high molecular weight polysaccharide found throughout the animal kingdom, especially in the extracellular matrix (ECM) of soft connective tissues. HA is thought to participate in many biological processes, and its level is markedly elevated during embryogenesis, cell migration, wound healing, malignant transformation, and tissue turnover. The enzymes that degrade HA, hyaluronidases (HAases) are expressed both in prokaryotes and eukaryotes. These enzymes are known to be involved in physiological and pathological processes ranging from fertilization to aging. Hyaluronidase-mediated degradation of HA increases the permeability of connective tissues and decreases the viscosity of body fluids and is also involved in bacterial pathogenesis, the spread of toxins and venoms, acrosomal reaction/ovum fertilization, and cancer progression. Furthermore, these enzymes may promote direct contact between pathogens and the host cell surfaces. Depolymerization of HA also adversely affects the role of ECM and impairs its activity as a reservoir of growth factors, cytokines and various enzymes involved in signal transduction. Inhibition of HA degradation therefore may be crucial in reducing disease progression and spread of venom/toxins and bacterial pathogens. Hyaluronidase inhibitors are potent, ubiquitous regulating agents that are involved in maintaining the balance between the anabolism and catabolism of HA. Hyaluronidase inhibitors could also serve as contraceptives and anti-tumor agents and possibly have antibacterial and anti-venom/toxin activities. Additionally, these molecules can be used as pharmacological tools to study the physiological and pathophysiological role of HA and hyaluronidases. 2007 Elsevier Inc. All rights reserved.
Contents Introduction Hyaluronan . . . . . . . . . . . . HA binding proteins and receptors . . . . . . . Extracellular hyaladherins. . . . . . . . . . . . HA receptorscellular hyaladherins . . . . . . Hyaluronan and cancer . . . . . . . . . . . . . Biological activities of HA and HA oligomers . Hyaluronidases . . . . . . . . . . . . . . . . . Mammalian hyaluronidases . . . . . . . . . . . Venom hyaluronidases . . . . . . . . . . . . . Microbial hyaluronidases . . . . . . . . . . . . Hyaluronidase inhibitors . . . . . . . . . . . . Medical applications of hyaluronan. . . . . . . Treatment of osteoarthritis . . . . . . . . . . . Surgery and wound healing. . . . . . . . . . . Embryo implantation . . . . . . . . . . . . . . As a disease indicator. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1922 1922 1923 1923 1925 1925 1927 1927 1928 1929 1931 1933 1934 1934 1934 1934
Corresponding author. Department of Orthopedics, Cobb hall, BO57, P.O. Box # 800374, University of Virginia, Charlottesville, Virginia-22908, USA. Tel.: +1 434 924 1717 (o), +1 412 805 1951 ; fax: +1 434 924 1691. E-mail address: ksgbaboo@yahoo.com (K.S. Girish). 0024-3205/$ - see front matter 2007 Elsevier Inc. All rights reserved. doi:10.1016/j.lfs.2007.02.037
1922
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
Hyaluronan in drug delivery. . . . . Medical application of hyaluronidase Concluding remarks . . . . . . . . . Acknowledgements . . . . . . . . . References . . . . . . . . . . . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
. . . . .
1935 1936 1936 1937 1937
Introduction Hyaluronan Meyer and Palmer first biochemically purified hyaluronan [HA] from bovine vitreous humour and solved its structure in 1954 (Meyer and Palmer, 1934; Weissman and Meyer, 1954). Further studies have shown HA to be an acidic, negatively charged, high molecular weight polysaccharide having an uniformly repetitive, linear polysaccharide comprised of disaccharide units of N-acetyl-D-glucosamine (GlcNac) and Dglucuronic acid (GlcA) (Laurent, 1970; Laurent and Fraser, 1992; Scott and Heatley, 2002). Though classified as a glycosaminoglycan (GAG), it differs from other GAGs (Table 1). HA is a megadalton molecule, with a typical molecular weight between 2 105 to 10 107 Da and an extended length of 225 m. Whereas other GAGs are relatively smaller in size (b 50 kDa, commonly 1520 kDa) with a short chain length. Also, HA is synthesized at the inner face of the plasma membrane as a free linear polymer without any protein core, while other GAGs are synthesized by resident Golgi enzymes and covalently attached to core proteins (Laurent and Fraser, 1992; Lee and Spicer, 2000; Toole, 2004). The biosynthesis of HA is regulated by three transmembrane glycosyltransferase isoenzymes: HAS1, HAS2 and HAS3. The active site of these enzymes protrudes from the inner face of the plasma membrane. HA is extruded through the plasma membrane onto the cell surface or into the ECM as it is being synthesized (Weigel et al., 1997). The isoenzymes are unique in that they possess two enzymatic components (i.e., Glycosyltransferases), one to add on the GlcUA and another to add on the GlcNAc. Although the amino acid sequences of these isozymes are 50 to 71% identical, the gene sequences are located on different chromosomes (hCh19-HAS1, hCh8-HAS2, and hCh16-HAS3) and encode three different proteins with distinct enzymatic properties (Spicer and McDonald, 1998; Itano et al., 1999). HAS3 synthesizes shorter forms of HA molecules (b 3 105 Da) and is thought to be more active than HAS1 and HAS2, both of which produce high molecular mass HA molecules
Table 1 Sugar composition of glycosaminoglycans Name Hyaluronan (HA) Chondroitin sulfate (CS) Dermatan sulfate (DS) Keratan sulfate (KS) Heparan sulfate (HS) Heparin + = positive; = negative. Sugar composition GlcA/GlcNAc GlcA/GalNAc GlcA or IdoA/GalNAc Gal/GlcNAc GlcA or IdoA/GlcNAc GlcA or IdoA/GlcNAc Sulfation Protein Linkage core + + + + + + + + + + (1,3) (1,3) (1,3) (1,4) (1,4) (1,4)
(3.9 106 Da). Mouse and human HA synthase genes are located on different chromosomes, suggesting that gene duplication and divergent evolution has resulted in differing gene regulation and kinetic properties of the encoded synthases (Table 2). The function of hyaluronan synthase (HAS) isoforms appears to be cell and tissue specific, but their exact function and role in cell signaling remains to be elucidated. Misregulation of HAS genes results in abnormal production of HA and promotion of aberrant biological processes such as transformation and metastasis (Toole, 2004; Adamia et al., 2005). HA is present in almost every tissue of all vertebrates but is most abundant in the ECM of soft connective tissues (Fraser et al., 1983). Depending on the tissue source, the polymer usually consists of 200025,000 disaccharide units with various functions. It is also found on the surface of certain pathogenic Streptococcus and Pasteurella bacteria. In mammals, a high concentration of HA is found in connective tissues such as umbilical cord, skin, synovial fluid and the vitreous humour. HA performs three basic molecular functions. First, it interacts in an autocrine manner with cell surface HA receptors on the same cell. Second, it interacts in a paracrine manner with a variety of ECM molecules on neighboring cells. Due to its giant physical structure, HA can interact with more than one cell. Such interactions have been shown to be essential in the structure and assembly of several tissues (Tammi et al., 2002; Turley et al., 2002; Toole, 2004). A single HA polymer can bind to hundreds of ECM proteins, which can in turn bind additional matrix proteins. These large matrix complexes can also be linked to the cell surface via HA receptors (Toole, 2004; Spicer and Tien, 2004). Third, newly synthesized HA may be secreted and subsequently interact with several cell surface receptors, including cluster determinant 44 (CD44), receptor for hyaluronate-mediated motolity (RHAMM), lymphatic vessel endothelial HA receptor (LYVE-1), hyaluronan receptor for endocytosis (HARE), liver endothelial cell clearance receptor (LEC receptor) and TLR-4. These interactions mediate three important physiological processes: signal transduction, the formation of pericellular coats and receptor-mediated internalization (Laurent et al., 1996; Vercruysse et al., 1999; Toole et al., 2002; Turley et al., 2002; Toole, 2004; Spicer and Tien, 2004; Adamia et al., 2005; Taylor and Gallo, 2006). HA binding proteins and receptors Hyaladherins are a heterogeneous group of proteins with the ability to bind HA. These proteins can be grouped according to
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1923
their location (extracellular/cellular) and by the sequence of HA binding site (Table 3). Most of the known HA binding proteins and receptors share a common 100 amino acid globular binding domain called the link module, which was first described in cartilage protein. The link module region is comprised of an immunoglobulin domain and two adjacent link modules. The immunoglobulin domains are most likely responsible for the link proteinproteoglycan interaction, whereas the link modules mediate binding to HA (Day and Prestwich, 2002; Spicer et al., 2003). This molecular architecture is common in G1-domains of aggrecan, versican, neurocan and brevican. Extracellular hyaladherins Extracellular hyaladherins are a group of HA-binding proteoglycans that include aggrecan, neurocan and brevican, constituting a gene family collectively termed hyalectins. These proteoglycans are components of the ECM and each proteoglycan has a characteristic distribution, with versican present in different soft tissues, aggrecan prominent in cartilage, and neurocan and brevican prominent in the central nervous system (CNS). In cartilage, HA functions as the central filament of proteoglycan aggregates, which are responsible for cartilage's resistance to compression. Acting as a scaffold, HA stabilizes the ECM structure through its interaction with several matrix hyaladherins. The major cartilage proteoglycan, aggrecan, can interact strongly with HA through the HA-binding domain (link module) on the intact proteoglycan molecule. The binding of proteoglycans to the HA chain is strengthened greatly by the link-protein. The retention of proteoglycans within the ECM is based on their interaction with HA, and thus they are the major
Table 3 Hyaladherin family proteins Cellular CD44 family, RHAMM, cdc37, p68 (gelqR), HBP (hepatocyte binding protein), IHABP4, TSG-6, LYVE-1, LEC, Extracellular Versican, link protein, aggrecan, neurocan, brevican, fibrinogen, Trypsin inhibitor (II)
matrix hyaladherins (Rauch et al., 1992; Blundell et al., 2004; Seyfried et al., 2006). HA receptorscellular hyaladherins CD44, considered the principal receptor for HA, is a multifunctional single-pass transmembrane glycoprotein consisting of four functional domains. CD44 is expressed in a number of different isoforms, due to alternate splicing of multiple variant exons, and variations in CD44 polypeptide sequence, glycosylation, and oligomerization influence its affinity for HA binding (Ponta et al., 1998). The distal extracellular domain is primarily responsible for the HA binding. Recent studies have revealed that CD44 binds to HA via a single extracellular link domain. Mutations in this region stall CD44 attachment to HA and inhibit the affinity of anti-CD44 monoclonal antibodies that block HA binding (Day and Prestwich, 2002). In addition to HA, CD44 interacts with several other molecules, many of which bind to carbohydrate side groups that are attached to spliced-in regions. Other ligands of CD44 include fibroblast growth factor, osteopontin (Knudson and Knudson, 2004), matrix metalloproteases (Toole, 2004), SRC kinases (Thorne et al., 2004), RHO GTPases (Ponta et al., 2003), VAV2, GAB1, ezrin (Toole, 2004), and ankyrin (Zhu and Bourguignon, 2000). CD44 is transcriptionally up-regulated by pro-inflammatory cytokines such as IL-1 and growth factors such as epidermal growth factor (EGF), transforming growth factor-beta (TGF-) and bone morphogenic protein (BMP-7) (Knudson and Knudson, 2004; Heldin, 2003). IL-1 increases CD44 mRNA and protein expression level in both chondrocytes and vascular smooth muscle cells (Ohno et al., 2005; Iacob and Knudson, 2006). In chondrocytes, the increased CD44 expression results in an increased capacity for HA binding, internalization and degradation. IL-1-induced elevation of CD44 increases the capacity of smooth muscle cells to bind HA. In atherosclerotic lesions, the increased expression of CD44 and HA may influence the proliferation and migration of smooth muscle cells, which contributes to the development of pathological lesions (Evanko et al., 1998; Wight and Merrilees, 2004). Furthermore, EGF up-regulates CD44 expression in fibroblasts, several tumor cell types, and epithelial cells (Toole, 2004; Knudson and Knudson, 2004). HACD44 interactions participate in a wide variety of cellular functions, including cellcell aggregation, retention of pericellular matrix, matrixcell and cellmatrix signaling, receptor-mediated internalization/degradation of HA, and regulating aspects of cell movement and cellcell adhesion (Li et al., 2000a; Knudson et al., 2002; Toole, 2002, 2004; Knudson, 2003; Spicer and Tien, 2004). Studies of embryonic
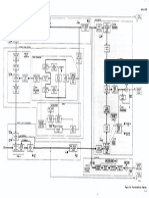
Table 2 Chromosomal location of hyaluronidase and hyaluronan synthase genes Family HA synthase Species Human Chromosomal location 19q13.313.4 8q24.12 16q22.1 17 15 8 3p21.3 Gene HAS1 HAS2 HAS3 Has1 Has2 Has3 HYAL1 HYAL2 HYAL3 HYAL4 SPAM1 HYALP1 Hyal1 Hyal2 Hyal3 Hyal4 Spam1 Hyalp1 Hyal5 Protein HAS1 HAS2 HAS3 Has1 Has2 Has3 Hyal1 Hyal2 Hyal3 Hyal4 HPH-20 HYAL1 HYAL2 HYAL3 HYAL4 PH-20 HYAL5 pH optimum 34 4, 7.5 ND ND 4, 7.5 ND 34 4, 7.5 ND ND 4, 7.5 ND 4, 7.5
Mouse
Hyaluronidase
Human
7p31.3
Mouse
9F1F2
6 A2
# Human and mouse hyaluronidase genes are located in equivalent locations of respective chromosomes.
1924
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
development, regeneration and healing, cancer and vascular disease have demonstrated that pericellular matrices surrounding proliferating and migrating cells are highly enriched in HA (Toole, 2004; Knudson et al., 2002). Interactions of HA with CD44 or hyaluronan synthase, versican, aggrecan, tumor necrosis factor-stimulated gene-6 (TSG-6), inter--trypsin inhibitor (II) and other hyaladherins in this matrix create a complex, hydrated microenvironment that supports and promotes the cellular characteristics of dividing and migrating cells (Toole, 2004; Spicer and Tien, 2004). In recent investigations, three approaches were used to manipulate endogenous HAprotein interaction. First, overexpression of soluble hyaladherins, which completely displace HA from its endogenous cell surface receptors (Peterson et al., 2000; Ahrens et al., 2001; Ward et al., 2003). Second, administration of HA oligomers, compete for endogenous polymeric HAreceptor interactions, thus resulting in lowvalency, low-affinity binding rather than polyvalent, high affinity interactions with receptors (Toole, 2004). Overexpression of soluble hyaladherins and administration of HA oligomer leads to inhibition of in vivo growth, local invasion and metastasis of melanoma cells (Lesley et al., 2000; Ghatak et al., 2002). The presence of HA oligomers in tissues is only speculation, but the influence of HA oligomers may affect different signals resulting from native HA interactions with different receptors. However, recent study confirmed the presence of HA fragments (b 100 kDa) in sterile UVB-induced inflammation in vivo (Averbeck et al., 2007). Third, treatment with antibodies that block HACD44 interaction, inhibits tumor growth and invasion (Lesley et al., 2000; Ghatak et al., 2002). Among these approaches, overexpression of soluble receptors and administration of HA oligomers, could have multiple biochemical effects with differing downstream consequences. RHAMM is a HA receptor that can be present at the cell surface, within the cytoplasm, and in the nucleus depending on alternative splicing of the transcript. RHAMM is expressed by several cell types and, depending on which isoform is present, contributes to HA mediate migration, rearrangement of the cytoskeleton and intracellular signal transduction. Interactions of HA with RHAMM can trigger a number of cellular signaling pathways, including those that involve protein kinase C, focal adhesion kinase (FAK), MAP kinases, nuclear factor-B, RAS, phosphatidylinositol kinase (PI3K), tyrosine kinases, and cytoskeletal components (Hall et al., 1996; Fieber et al., 1999; Politz et al., 2002; Ponta et al., 2003; Thorne et al., 2004; Toole, 2004). RHAMM has also been implicated in cell motility. Several studies have demonstrated its involvement in the locomotion of transforming growth factor--stimulated fibroblasts, smooth muscle cells, and macrophages, as well as in ras-transformed fibroblasts (Savani et al., 2001). RHAMM dependent cell migration appears to regulate the turnover of focal adhesions via a protein tyrosine phosphorylation pathway. Of the two major isoforms of RHAMM, cell surface RHAMM has been implicated in promoting the motility and invasion of a number of cell types by a HA-dependent mechanism (Zhang et al., 1998). The intracellular variant of RHAMM (referred to as
intracellular HA binding protein [IHABP]) is localized in the centrosome and modulates cell cycle control and mitotic spindle formation and integrity through crosslinking and association with dynein. It has been shown to associate with actin and microtubule cytoskeletal elements (Zhang et al., 1998; Turley et al., 2002). The genes stabilin-1 and stabilin-2 encode the MS-1 antigen and hepatic HA clearance receptor, respectively. These functional HA receptors are present on the surface of endothelial cells and activated macrophages present in the liver, placenta, spleen and the lymph node. The hepatic HA clearance receptor is thought to be important for removing of HA from the blood during steady-state tissue remodeling (Politz et al., 2002; Spicer and Tien, 2004). LYVE-1 (lymphatic vascular endothelial hyaluronan receptor) is a recently discovered HA binding protein expressed only in lymph vessel endothelium. LYVE-1 is structurally related to CD44 and other binding proteins that contain a consensus HAbinding domain (Link module). LYVE-1 cDNA codes for a 322residue integral membrane glycoprotein with a single link module located at the N-terminal of the extracellular domain. The membrane proximal domain is predicted to be heavily oglycosylated with an unpaired cysteine residue. Overall, LYVE1 is 43% similar to CD44 (Jackson et al., 2001; Jackson, 2003; North et al., 2004). LYVE-1 is abundantly expressed in the lymphatic endothelium of humans, mice, and rats. It is also expressed in discrete populations of activated tissue macrophages and in the sinusoidal endothelium of the liver and spleen, the sites where uptake and degradation of high molecular weight HA is known to occur (Jackson, 2004). Recent studies revealed that the interaction between LYVE-1 and HA in lymphatics is tightly regulated and that the mechanisms may be broadly similar to those that regulate CD44HA interactions in blood vasculature (Jackson et al., 2001; Banerji et al., 1999). It is considered to be HA specific since it has no affinity for any other GAGs tested (Jackson, 2003). Layilin is a recently cloned and characterized HA receptor. Layilin exhibits a membrane-binding site for talin, a member of the ERM superfamily of linkers between the actin cytoskeleton and the cell membrane. The receptor has therefore been proposed to contribute to cell migration and morphology (Bono et al., 2001). Studies have revealed that layilin is a functional HA receptor capable of mediating cell adhesion. Layilin shares no sequence homology to the other known HA receptors; it does not contain a link domain, a common HA binding module found in many ECM proteins and cell surface receptors. However, layilin contains a C-type lectin domain that may account for its ability to bind HA. A recent study suggests merlin, the neurofibromatosis type 2 tumor suppressor protein, and radixin, as two novel binding partners for layilin (Bono et al., 2005). Both proteins contain a FERM domain at their Nterminus, suggesting that layilin may mediate signals from ECM to cell cytoskeleton through interaction with different binding partners. TSG-6 (tumor necrosis factor-stimulated gene-6) is a multifunctional protein that is up-regulated in many physiological and pathological conditions associated with inflammation
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1925
and tissue remodeling, such as in the sera and joints of arthritis patients (Bayliss et al., 2001). Several studies using a murine arthritis model have been demonstrated the anti-inflammatory and chondroprotective effects of TSG-6. A number of mechanisms might contribute to these effects. First, recombinant TSG-6 down-regulates the protease network and inhibits matrix metalloproteinase. Second, the anti-plasmin activity of II is significantly increased by TSG-6. This is supported by the observation of inflamed paw joints of TSG-6 deficient mice compared to wild type mice in arthritis model. Third, TSG-6 inhibits neutrophil migration in vivo, causing 50% inhibition in an air pouch model of acute inflammation (Cao et al., 2004; Mahoney et al., 2005) by modulating the protease network in conjunction with II (Milner and Day, 2003). TSG-6 also interacts with a broad spectrum of GAG and protein ligands, including HA, heparin, chondroitin 4-sulfate, aggrecan, versican, II, pentraxin-3, and thrombospondin-1. The interactions of TSG-6 with HA, heparin, and the aggrecan G1-domain are sensitive to pH. Therefore the functions of TSG6 are likely to be tissue specific and dependent on pH and GAG content (Milner et al., 2006). In cartilage, TSG-6 may inhibit the formation of HAprotein aggregates, promote aggregate dissociation, or modulate CD44 function. In certain tissue locations, TSG-6 can associate with inter--inhibitor (II), and this TSG-6/II complex may be able to stabilize the ECM by crosslinking with HA chains (Milner et al., 2006). These studies suggest that hyaladherins and HA binding proteins participate in several important functions, such as the retention of HA-rich ECM and signal transduction events mediated via cellmatrix interactions. Disruption of the interaction between HA and its receptors/binding proteins by HA oligosaccharides, antibodies, hyaluronidase and HA degradation, antisense oligonucleotides can induce a cascade of events resulting in the activation of both catabolic and anabolic pathways. Hyaluronan and cancer A large amount of experimental evidence from animal models shows that epithelial and connective tissue cancers are associated with high levels of HA. Histological studies on various tumors, using a specific probe, have shown greater HA enrichment of extracellular matrices surrounding tumors than found in parenchymal regions (Toole, 2004; Toole and Hascall, 2002; Paiva et al., 2005). In human cancers, HA concentrations are usually higher in tumors than in normal tissues. Human breast, lung, prostate, ovarian, nephroblastomas, and colon cancer are considered to enriched with HA (Heldin, 2003; Toole, 2004; Adamia et al., 2005). In these tumors, HA may support tumor growth by stimulating anchorage-independent growth and proliferation of tumor cells. Moreover, HA may also actively promote tumor metastasis by promoting tumor cell adhesion and migration and may also protect against immune surveillance (Itano et al., 2004; Paiva et al., 2005). Additionally, tumor cells may take advantage of HA-rich extracellular matrices to invade more easily into the surrounding tissues. HA-induced tissue hydration physically creates spaces through
which tumor cells may migrate and invade. HA-rich matrices within the tumor-associated stroma are also infiltrated with newly forming blood vessels (Toole, 2004). It is well known that HA stimulated cell migration and signaling are accomplished through the interactions mediated by the HA cell surface receptors CD44 and RHAMM, both of which promote tumor progression. As mentioned earlier, the interaction of HA with CD44 and RHAMM has been implicated in cell proliferation, migration and angiogenesis. CD44 also mediates a variety of intracellular signaling cascades and interacts with cytoskeletal proteins that are essential for the normal functioning of the cells. However, abnormal activation of these signaling pathways can lead to malignant behavior (Toole, 2004; Adamia et al., 2005). Manipulation of HA biosynthesis in tumor cells has shown its importance in metastasis (Liu et al., 2001). HA synthesis by HAS can facilitate tumor progression through reorganization of the cytoskeleton, including lamellipodial formation which is a prerequisite for cell spreading and metastatic development (Itano et al., 2004; Adamia et al., 2005; Paiva et al., 2005). Numerous studies demonstrated the overexpression of HAS proteins and subsequent overproduction of HA molecules in metastatic development of fibrosarcoma, and prostate and mammary carcinoma (Itano et al., 1999; Simpson et al., 2002; Heldin, 2003). Overexpression of HAS1 or HAS2 results in the synthesis of high molecular weight HA, which may activate hyaluronidase, the enzyme that degrades HA is up-regulated or down-regulated during the progression of cancer (Lokeshwar et al., 2002). HYAL1 is the main hyaluronidase expressed in tumors and is active only at acidic pHs (Stern, 2003, 2004). Shorter fragments of HA resulting from HA degradation have been found in tumor extracts (Toole, 2004). Several studies have shown that HA oligosaccharides or HA fragments promote angiogenesis (West et al., 1985). These studies suggest that HA not only stimulates malignant characteristics in cancer cells, but its degradation products might also promote tumor progression through the stimulation of angiogenesis. Biological activities of HA and HA oligomers HA is known to be involved in fundamental physiological and pathological process such as embryological development, migration, adhesion, proliferation and differentiation of cells (Manzel and Farr, 1988; Heldin, 2003; Spicer and Tien, 2004), immune surveillance, inflammation (Termeer et al., 2003; George and Stern, 2004; Day and de la Motte, 2005; Jiang et al., 2005), wound healing (Chen and Abatangelo, 1999), multi-drug resistance (Toole, 2004), angiogenesis, malignant transformation, and water homeostasis and viscoelasticity of ECM (West et al., 1985; Frost et al., 1996; McDonald and Camenisch, 2002; Toole, 2004; Adamia et al., 2005). The biological functions exhibited by HA depend on the chain length, molecular mass and on the circumstances under which it is synthesized (Noble, 2002; Toole, 2004). High and low molecular weight forms of HA exhibit opposite effects on cell behaviour. Extracellular high molecular
1926
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
weight HA (HMWHA) inhibits endothelial cell growth, and is thereby anti-angiogenic in nature. The HMWHA polymers have an increased ability to bind fibrinogen; this is one of the first reactions to occur in clot formation, which are critical in early wound healing (Chen and Abatangelo, 1999). These HA polymers are also anti-inflammatory and immunosuppressive in nature (Day and de la Motte, 2005; Milner et al., 2006). Fetal circulation and amniotic fluid contain high concentrations of HMWHA, which may account for some of the immunosuppression in the developing fetus. HMWHA inhibits scar formation in fetal wounds, whereas HA degradation products contribute to scar formation (Noble, 2002). Furthermore, production of HMWHA is increased at sites of inflammation, often correlating with leukocyte adhesion and migration. Several studies suggest that HMWHA can be organized to generate wide superstructures with multiple architectures and functional activities by its association with specific binding proteins (Day and de la Motte, 2005; Milner et al., 2006). Recently, it has been observed that peripheral blood monocytes are stimulated through their binding to HMWHA chains but this interaction induces the expression of growth factors and matrix components rather than pro-inflammatory mediators (Day and de la Motte, 2005). This indicates a counter-inflammatory or anti-inflammatory role of highly crosslinked HMWHA. Low molecular weight HA (LMWHA) fragments interact with a different set of receptors that trigger signaling cascades and profound changes in cell behavior. LMWHA has been shown to promote angiogenesis in several experimental models (West et al., 1985; Noble, 2002; Toole, 2004). Also, LMWHA enhances the synthesis of type I and VIII collagen, which are ECM molecules of the endothelial cell angiogenic phenotype. Low and intermediate molecular weight (2 1044.5 105) HA oligosaccharides are potent stimulators of inflammatory cytokine and adhesion molecules (Noble et al., 1993). HA oligomers increased cell migration and gene expression of MMP-9 and MMP-13 in Lewis Lung Carcinoma (3LL) cells and in primary embryonic fibroblasts (Fieber et al., 2003). Studies on activated macrophages have shown that HA fragments induce the expression of chemokine genes such as macrophage inflammatory protein (MIP)-1, MIP-1, crg-2, RANTES and monocyte chemotactic protein-1 (MCP-1), the functions of which are crucial in initiating and maintaining the inflammatory response (McKee et al., 1996). Furthermore, expression of HAS-2, aggrecan, MMP-3, MMP-13 and iNOS was stimulated by HA oligosaccharides in bovine chondrocytes and human articular chondrocytes (Knudson and Knudson, 2004; Iacob and Knudson, 2006). Shorter HA fragments have been reported to promote cell proliferation of chondrocytes, endothelial cells and fibroblasts. Iacob and Knudson (2006) have shown that the HA fragments activate nitric oxide synthase and the production of nitric oxide by articular chondrocytes. The activation of NO production by HA fragments has been shown in macrophages, rat liver endothelial cells, Kupffer cells, T-24, HeLa, MCF7, and J774 cells. In some cases, the stimulatory effects of HA fragments were shown to be mediated by activation by nuclear factor (NF)-. Conversely, IL-10 and interferon- were found to
inhibit LMWHA-induced cytokine production in mouse bone marrow-derived macrophages (Horton et al., 1999). Smaller HA oligomers (620 kDa size range) are potent activators of dendritic cells, the antigen presenting cells of the immune system. Thus HA fragments tend to be angiogenic, immuno-stimulatory, and inflammatory (Noble, 2002; Termeer et al., 2002; Rossler and Hinghofer-Szalkay, 2002; Stern, 2003). Angiogenic HA fragments stimulate endothelial cell proliferation, adhesion, and migration by activating focal adhesion kinase and mitogen activated protein (MAP) kinase pathways (Rossler and Hinghofer-Szalkay, 2002; Murai et al., 2004). Most pro-inflammatory HA fragments can signal through TLR4 in dendritic cells and endothelial cells (Termeer et al., 2002; Taylor et al., 2004). Recent studies confirmed that HA oligomers require MyD88 and both toll like receptor 4 (TLR4) and TLR2 in vitro and in vivo to initiate the inflammatory response in acute lung injury (Jiang et al., 2005). Very small HA oligosaccharides also have unique specific biological activities. Oligomers of six disaccharides promote differentiation of the endothelial cells induced in response to the angiogenic effect of larger HA fragments (Takahashi et al., 2005). Moreover, control of migration, maturation and signaling in skin keratinocytes is also closely associated with small HA oligomers. Recently, Takahashi et al. investigated the effects of HA oligomer (HA12) on differentiation of endothelial cells at the molecular level, by using microarray approach. The data revealed that the HA oligomer (HA12) induces 2-fold upregulation of the Vil2 gene, which encodes ezrin, the protein that is associated with activated CD44 and participates in cell shape changes, adhesion, motility, endocytosis/exocytosis, and signal-transduction pathways. In addition, HA12 induces expression of the myosin 1b gene, which belongs to myosin I family of proteins and participates in a variety of cellular processes, including membrane fusion/vesicle scission (Takahashi et al., 2005). Tetra and hexasaccharides are predominant products of hyaluronidase-mediated degradation. Tetrasaccharides induce expression of heat shock proteins (Hsps) and are anti-apoptotic, suppressing cell death in cultures undergoing hyperthermia (Xu et al., 2002). Other studies have demonstrated that the addition of tetrasaccharides inhibits anchorage-independent growth of several tumor cell types by suppressing the phospho-inositol-3kinase/Akt survival pathway (Ghatak et al., 2002). Ohano et al. have shown that hexasaccharides act as antagonists to HMWHA, interfering with normal bovine chondrocyte cell matrix interactions such as assembly of pericellular matrix. In addition, expression of transcription factors such as AP-1, NFB, p53, Sp1, and Stat4 was markedly up-regulated in bovine articular chondrocytes after treatment with hexasaccharides (Ohno et al., 2005). From these observations, it can be concluded that HA catabolism depends on individual hyaluronidase activities under pathological conditions and the products generated during catabolic pathway with contrasting biological activities. In addition, it would be more interesting to compare the biological effects of HA degradation products generated by enzyme dependent and independent pathways.
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1927
For normal tissue organization and function, a balance between HA synthesis and degradation is important. The turnover of HA is relatively rapid compared to other ECM molecules (Laurent and Fraser, 1986; Tammi and Tammi, 2006). High molecular weight tissue HA is degraded extracellularlly by chemical/mechanical means or enzymatic degradation by HA degrading enzymes. Non-enzymatically, HA is degraded by reactive oxygen species (ROS) such as superoxide anion radical (O2 ), hydrogen peroxide (H2O2) and especially by OH radicals yielding several intermediate end products under oxidative conditions (Deguine et al., 1998; Vercruysse et al., 1999; Yamazaki et al., 2003). This type of degradation generally occurs at sites of inflammation, tissue injury, and tumorigenesis (Uchiyama et al., 1990). Interestingly, hyaluronidases are endoglucosaminidases, whereas ROS degrade HA randomly at internal glycosidic linkages. Hyaluronidases The hyaluronidases are a group of enzymes distributed throughout the animal kingdom. In recent years hyaluronidases have received attention and importance due to their regulatory function in HA metabolism. Duran-Reynals observed that extracts of mammalian testis and other tissues contain a spreading factor which facilitated the diffusion of dyes and antiviral vaccines injected subcutaneously (Duran-Reynals, 1928; Chain and Duthie, 1940). Karl Meyer introduced the term hyaluronidase to denote the enzymes that degrade HA. Meyer classified hyaluronidases into three different groups based on biochemical analysis and generated end products (Meyer, 1971). The three groups include: (1) Mammalian hyaluronidases (testis type) (E.C. 3.2.1.35) that are endo--Nacetlyhexosaminidases and randomly cleave -1-4 glycosidic linkages in HA, chondroitin and chondroitin sulfates (A and C) to yield even numbered oligosaccharides (tetra and hexa) as the major end products, with N-acetylglucosamine at the reducing terminal. Enzymes of this class have both hydrolytic and transglycosidase activities (e.g. testicular hyaluronidase) present in mammalian spermatozoa, lysosomes and the venom of snakes, reptiles and hymnoptera (Cramer et al., 1994). (2) Hyaluronate-3-glycanohydrolases (E.C. 3.2.1.36) (Leech hyaluronidase) are endo--D-glucuronidases that cleave glucuronate linkages of HA and are inert towards other GAGs. Tetrasaccharides and hexasaccharides are the main end products with glucuronic acid at the reducing end of the product. This class includes enzymes present in salivary glands of leeches and hook worms (Hotez et al., 1992). (3) Microbial hyaluronidases (E.C. 4.2.99.1) cleave HA at 1-4 glycosidic linkages using the elimination process and yield 45 unsaturated oligosaccharides. These are different from the two other groups of hyaluronidases, as they do not use hydrolysis in their activity. Enzymes in this class include HA lyases from Streptococcus pneumoniae (S. PHL) and S. agalactiae. In addition, hyaluronidases are loosely classified into two groups based on their pH dependent activity profile. Acid active hyaluronidases are active between pH 3 and 4, and this group includes human liver and serum hyaluronidases. Neutral active
hyaluronidases are active between pH 5 to 8 and include PH-20, snake venom, and bee venom hyaluronidases (Kreil, 1995; Stern, 2004; Kemparaju and Girish, 2006). Mammalian hyaluronidases The enzymatic degradation of HA in mammals is mediated through the coordinated activity of three separate enzymes, namely a hyaluronidase, an endoglycosidase and two other exoglycosidases that remove the terminal sugars, a -glucuronidase and -N-acetyl hexosaminadase. The initial degradation accomplished by hyaluronidase generates oligosaccharides of different chain length and these are substrates for the two exoglycosidases (Roden et al., 1989). Human hyaluronidases have been reported and some of them are well characterized from a number of tissues (Frost et al., 1996; Stern, 2003). Six hyaluronidase like gene sequences have been identified in humans. These hyaluronidase genes are also referred to as hyaluronoglucosaminidase (HYAL) genes. These six paralogs of HYAL genes are known to share about 40% of their identity with one another. However, the expression of each gene has a unique tissue distribution. HYAL1, HYAL2 and HYAL3 are located on chromosome 3p21.3. Another set of three genes, HYAL4, PHYAL1 (a pseudogene), and sperm adhesion molecule 1 (SPAM 1) are clustered in a similar fashion on chromosome 7p31.3. Hyal1 and Hyal2 are the major hyaluronidases expressed in human somatic tissues (Csoka et al., 2001). In contrast, the mouse genome has seven hyaluronidaselike gene sequences (Miller et al., 2007; Reitinger et al., 2007). Six of the seven genes are clustered in groups of three at two chromosomal locations. Hyal1, Hyal2, and Hyal3 are located on chromosome 9F1F2. Hyal4, Spam1/PH-20, and Hyalp1 are located on chromosome 6A2 (Csoka et al., 2001; Baba et al., 2002; Zhang et al., 2005). The seventh mouse hyaluronidaselike gene, tentatively called Hyal5, is localized in close proximity to the cluster at chromosome 6A2 (Kim et al., 2005; Reitinger et al., 2007). Both Hyalp1 and Hyal5 share a high degree of sequence similarity with biochemically characterized hyaluronidases. Hyal5 has a broad optimal pH range and is active in both neutral and extracellular ionic pH (Reitinger et al., 2007). Besides mice, Hyal5 is also present in rats (accession number BC091219), suggesting that further gene duplication has occurred in rodents (Zhang et al., 2005; Reitinger et al., 2007). Mature spermatozoa of Spam1 deficient mouse are fertile and exhibit hyaluronidase activity. This could be due to the presence of functionally active Hyal5 on the surface of Spam1 deficient spermatozoa. Furthermore, we can assume both SPAM1 and HYAL5 enzymes participate in spermatozoa fertilization of the egg. Hyal1 was the first somatic hyaluronidase isolated and characterized from human plasma (Csoka et al., 1999; Afify et al., 1993). It is an acid active 57 kDa single polypeptide glycoprotein that is also present in a processed 45 kDa form generated by two endoprotease reactions. Only the high molecular weight isoform is present in the circulation, and both isoforms occur in urine, in tissue extracts and cultured cells (Csoka et al., 1997). Hyal1 can use HA of any size as a substrate
1928
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
and generates predominantly tetrasaccharides/hexasaccharides. Moreover, the mouse ortholog has also been cloned, expressed and was observed to be 73% identical to the human enzyme (Stern, 2004; Csoka et al., 1998). Hyal2, also acid active, is anchored to plasma membrane by a glycosylphosphatidyl-inositol (GPI) link (Lepperdinger et al., 1998, 2001). It also occurs in a processed soluble form. Hyal2 cleaves high molecular weight HA to intermediate sized fragments (approximately 20 kDa). Hyal1 and Hyal2 have similar structures but produce different reaction products. Hyal2 is considered the more important enzyme of the two, Hyal2 null mutation in the mouse is embryonically lethal and the Hya1 mutation is not. However, recent evidence indicates that the Hyal2 knockout mice is not an embryonic lethal and that knockout mouse has now been generated (Flamion B., personal communication). Hya12 also functions as a receptor for Jaagsiekte sheep retrovirus (JRSV) and enzootic nasal tumor virus (ENTV). Human Hyal2 binds to the envelope proteins of these viruses and serves as a functional receptor. Hyal2 from mice, however, does not bind to envelope proteins nor does it mediates entry of either virus (Duh et al., 2005). Hyal3 is widely expressed, but no activity can be detected using the available hyaluronidase assays (Csoka et al., 2001). It occurs in chondrocytes, testis and bone marrow, and its expression increases when fibroblasts undergo chondrocyte differentiation (Flannery et al., 1998; Nicoll et al., 2002). Hyal3 and Hyal2 are up-regulated by inflammatory cytokines such as IL-1 and tumor necrosis factor-alpha (TNF-), whereas Hyal1 is not (Flannery et al., 1998). The biochemical and functional characteristics of hyaluronidase genes were reviewed by Robert Stern (Stern, 2003). Recently, Jedrzejas and Stern proposed the 3D model structures for human Hyal enzymes Hyal14 and PH-20 (Jedrzejas and Stern, 2005). The catalytic cleft and the active sites of these enzymes are highly conserved. However, the C-terminal domain differs both in sequence and structural functionality among all the Hyal enzymes. All known hyaluronidases are active at acidic pH, consistent with a lysosomal location, except PH-20 and Hyal2, which are active over a broad optimal pH range (Vigdorovich et al., 2005). In addition, Gatphayak et al. (2004) characterized a cluster of porcine three hyaluronidase genes (HYAL1, HYAL2 and HYAL3). The porcine hyaluronidase genes share approximately 40% homology with one another. The porcine cDNA and protein sequences share homologies to human orthologs of 85% and 81% for HYAL1, 87% and 89% for HYAL2 and 86% and 83% for HYAL3 respectively. Research on these enzymes was barely investigated until recently due to their instability and other associated problems such as isolation, purification and activity assays. The vertebrate enzymes are hydrolases, while the enzymes from microbial source are eliminases. The microbial hyaluronidases can be assayed by spectrophotometric methods that detect the formation of an unsaturated bond during the enzymatic degradation of substrates (Baker et al., 2002; Jedrzejas, 2004; Stern and Jedrzejas, 2006). The hydrolases are relatively deserted in comparison with other glycosidase, most likely due to the unavailability of simple and sensitive assay method that measure
degradation of substrate (Manzel and Farr, 1988; Afify et al., 1993; Kemparaju and Girish, 2006). The most commonly used hyaluronidase assays were based upon the measurement of the generation of new reducing N-acetyl glucosamine or loss of viscosity or turbidity. These methods are either less sensitive or lack of specificity. In addition, there are problems associated with the presence of hyaluronidase inhibitors and proteins present in medium, cell and tissue extracts. However, recent superior detection procedures for vertebrate hyaluronidase activity such as substrate gel assay, ELISA like assay and fluorescence-based assays have facilitated their identification and isolation (Afify et al., 1993; Csoka et al., 1997; Jedrzejas and Stern, 2005; Stern and Jedrzejas, 2006). Among the mammalian hyaluronidases, testis hyaluronidases are very well studied and characterized. Mammalian sperm have a GPI-anchored hyaluronidase which is known as PH-20 and also as SPAM-1. PH-20 is located on the sperm surface and in the lysosome-derived acrosome, where it is bound to the inner acrosomal membrane. PH-20 facilitates penetration of sperm through the cumulus ECM and zona pellucida of the ovum, and is also necessary for fertilization. Several studies have confirmed that PH-20 is the only hyaluronidase in mammalian sperm, including the sperm of guinea pigs, rats, macaques and humans (Cherr et al., 2001; Zheng et al., 2001). It is originally synthesized as a polypeptide with an apparent molecular weight of 64 kDa. During the course of sperm maturation, part of PH-20 is processed into two fragments that are linked through disulfide bridges, such as one at N-terminal domain of 4148 kDa and a C-terminal domain of 27 kDa. PH-20 is unique among hyaluronidases, in that it shows enzyme activity at both acidic and neutral pH and that these activities appear to involve two different domains in the protein (Gmachl and Kreil, 1993; Cherr et al., 2001; Oettl et al., 2003). Using more sensitive techniques involving PCR analysis, PH20 have been detected in the epididymis, seminal vesicles, prostate, female genital tract, breast, placenta and fetal tissue, as well as in certain malignancies (Beech et al., 2002; Zhang and Martin-DeLeon, 2003; Oettl et al., 2003). These studies have further confirmed that PH-20 is a multifunctional enzyme that is not sperm-specific and also has functions in addition to its hyaluronidase activity. Venom hyaluronidases Hyaluronidases are often found in all types of animal venoms. Hyaluronidase activity has been detected in the venom of snakes (Kudo and Tu, 2001; Girish et al., 2004b; Kemparaju and Girish, 2006), bees (Gmachl and Kreil, 1993; MarkovicHousley et al., 2000), stonefish (Poh et al., 1992; Ng et al., 2005), scorpions (Ramanaiah et al., 1990; Pessini et al., 2001; Morey et al., 2006), spiders (Rash and Hodgson, 2002; Nagaraju et al., 2006), lizards (Tu and Hendon, 1983), wasps (Kreil, 1995), caterpillars (da C B Gouveia et al., 2005) and hornets (Lu et al., 1995). In all animal venoms, the hyaluronidase causes local tissue damage and is generally referred to as a spreading factor. The spreading property of the enzyme is presumed to be the critical event in spreading toxins
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1929
from the site of injection to systemic circulation. This process is accomplished by the degradation of HA and the eventual loss of integrity in the ECM of soft connective tissues surrounding the blood vessels, leading to the easy diffusion of the toxic components of venom (Girish et al., 2004b; Kemparaju and Girish, 2006). Many venom hyaluronidases have a sequence homology of about 36% with that of spermatozoan PH-20 (Table 4). The first marine hyaluronidase was isolated and cloned from venom of the stonefish Synanceja horrida. The purified enzyme is a -endo-N-acetyl hexosaminidase, acts on -14 glycosidic linkages and yields tetrasaccharides as the major end product. The enzyme is a 62 kDa glycoprotein with a pI of 9.2 and is non-toxic in nature (Poh et al., 1992; Ng et al., 2005). Hyaluronidase from lizards, scorpions, spiders, caterpillars, wasps and hornets have been isolated and characterized to some extent (Kemparaju and Girish, 2006, references therein). Among these, the enzyme from bee venom has been investigated in depth, being the first eukaryotic hyaluronidase cloned via cDNA by using the N-terminal sequence. The mature enzyme is a globular protein composed of 349 amino acids with a calculated molecular mass of 40.746 kDa (Gmachl and Kreil, 1993). It is secreted as a basic glycoprotein and has 7% carbohydrate content when compared to the total protein mass. It contains four cysteine residues that are present as disulfide bonds in the extracellular enzyme. The enzyme is acid-active and has three potential N-glycosylation sites, though only one site appears to be glycosylated. This enzyme is derived from a precursor containing a signal peptide of 24 or 28 amino acids and a short pro-segment. Bee hyaluronidase is an endo-Nacetyl-D-glucosaminidase and yields tetrasaccharides as a major end product (Gmachl and Kreil, 1993). Expression of the cloned cDNA in E. coli resulted in a polypeptide with hyaluronidase
Table 4 Biochemical and biophysical properties of animal venom hyaluronidases Venom A. acutus A. contortrix contortrix N. naja (isoforms) H. fulvipes T. serrulatus A. mellifera S. horrida H. horridum horridum L. oblique (isoforms) L. reclusa (isoforms) D. maculata V. germanica C. limpidus limpidus P. regosus V. vulgaris Palamneus gravimanus Molecular pI weight (kDa) 33 59.2 70.4 52 82 51 41 62 63 49 53 33 63 39 42 47.5 36 43 52 10.3 9 9.2 9.7 ND ND 9 9.2 5.1 ND ND ND ND ND ND ND ND ND ND Optimum Optimum PAS pH temp. C staining 5 6 5 5 4 6 6 6 5 67 67 56.6 56.6 56 56 56 56 56 4.5 37 37 37 37 30 40 37 37 Sensitive 37 37 37 37 37 37 37 37 37 37 + ND ND ND + ND + ND ND ND ND ND ND ND ND + ND
acitivity. Markovic-Housley et al. (2000) co-crystallized bee venom hyaluronidase with HA tetramer. The crystal structure analysis revealed the presence of an unusual overall fold, a (/ )7 barrel instead of a regular (/)8 barrel. The HA binding site is situated at the C-terminal end of the barrel and is lined with many conserved amino acids. Moreover, the structure of complex strongly suggests an acid-base catalytic mechanism, with Glu113 acting as a proton donor and the N-acetyl carboxyl groups of HA acting as the nucleophilic base. The enzyme is closely related to human PH-20 and human plasma hyaluronidase. The amino acid sequence of hornet venom hyaluronidase has also been determined via cDNA cloning. The enzyme is comprised of 331 amino acids, of which 56% are identical to bee venom hyaluronidase (Lu et al., 1995). Hyaluronidase, an ubiquitous enzyme in snake venom originally known as spreading agent, has not been well studied. Recently, we reported the purification of two hyaluronidase isoforms from Indian cobra (Naja naja) venom and provided systematic evaluation of the spreading property of the enzyme. The hyaluronidases NNH1 and NNH2 were purified through gel permeation and ion exchange chromatography. The molecular mass NNH1 was found to be 70.406 kDa by MALDI-TOF mass spectrometry, and it has a pI of 9.2. Both the isoforms are active at pH 5 to 7 and belong to the group of neutral active enzymes. Enzymes show absolute specificity for HA and generate tetrasaccharides as the final end product having N-acetylglucosamine at the reducing terminal. Hyaluronidases cleave 1,4-glycosidic linkage and belong to a group of endo--N-acetyl hexosaminidases. The enzyme indirectly potentiates the myotoxicity of VRV-PL-VIII, a phospholipolytic myotoxin, and also the hemorrhagic potency of hemorrhagic complex-I. Localization of hyaluronan in human skin section and selective degradation by venom hyaluronidase NNH1 and NNH2 corroborate the plausible in vivo degradation of hyaluronan in the ECM, resulting in the easy dissemination of VRV-PL-VIII myotoxin and hemorrhagic complex-I (Girish et al., 2004b; Girish and Kemparaju, 2005a). Hyaluronidase is a major allergen of scorpions, bees, hornets and wasps that can induce serious and occasionally fatal systemic IgE-mediated anaphylactic reactions in humans (Lu et al., 1995; Kolarich et al., 2005). Knowledge of the structural determinants responsible for its allergic potency is expected to have important clinical implications. Furthermore, it will be exiting to understand the in vivo fragmentation of HA by venom hyaluronidases and the subsequent effects on pathophysiology of envenomation. Microbial hyaluronidases In microbes, HA lyases are virulence factors involved in pathogenesis and disease progression caused by the pathogen. Often HA lyases directly interact with host tissues or conceal the bacterial surface from host-defense mechanisms. The enzymatic degradation of ECM components of host tissues facilitates the invasion of pathogens (Table 5). Enhanced tissue permeability caused by the action of HA lyases on ECM appears to play a major role in wound infections, pneumonia
PAS = periodic acid staining; ND = not determined; + = positive; = negative.
1930
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Table 6 List of hyaluronate lyase producing microorganisms Gram-negative bacteria Aeromonas, Vibrio, Beneckea, Proteus vulgaris, Bacteroides fragilis, B. vulgatus, B. ovatus, B. melaninogenicus, B. asaccharolyticus, B. tgetaiotaomicron, Fusobacterium mortiferum, Treponema pallidum and T. pertenue. Gram-positive bacteria Streptococcus pneumoniae, S. intermedicus, S. constellatus, S. dysgalactiae, S. uberis, S. suis, Staphylococcus hyicus subsp. hyicus, S. aureus. Clostridium difficile, C. perfringens, C. septicum, C. chauvoei. Mycoplasma alligatoris, M. crocodyli, Propionibacterium acnes, P. granulosum, Streptomyces coelicolor, S. hyalurolyticus, S. griseus. Peptostreptococcus. Bacteriophage Streptococcus pyogenes, S. equi Fungi Candida albicans, C. tropicalis, C. guillermondii, C. parapsilosis, C. krusei. Paracoccidioides brasiliensis, Pygocelis adeliae, Dasypus novemcinctus
and other types of sepsis such as bacteremia and meningitis (Sutherland, 1995; Matsushita and Okabe, 2001; Jedrzejas, 2001, 2004; Makris et al., 2004). The HA degrading activities of microbes may facilitate adhesion, colonization and provide nutrients (Hynes and Walton, 2000). Disaccharides are the major end products of HA degradation and these can be transported and metabolized intracellularlly to supply needed nutrients (as a carbon source) for a pathogen as it replicates and spreads (Matsushita and Okabe, 2001; Jedrzejas, 2001, 2004; Makris et al., 2004). In host tissues, high molecular mass HA is involved in the regulation of immune system and is antiinflammatory in nature (Toole, 2004). In contrast, HA oligomers generated by microbial HAases are potent inflammatory agents and promote microbial-friendly environment (Hynes and Walton, 2000). HA lyases are produced by many different genera of bacteria. In gram-positive bacteria, the HA lyases are often secreted and are thought to have a role in pathogenesis (Hynes and Walton, 2000; Spellerberg, 2000; Makris et al., 2004). It has been noted that all gram-positive bacteria that produce HA lyases appear to be capable of causing infections in animals (Table 6). Grampositive organisms capable of producing HA lyases include various species of Streptococcus, Staphylococcus, Peptostreptococcus, Propionibacterium, Streptomyces and Clostridium. HA lyase production has been reported in Streptococci groups A, B, C and G as well as S. pneumoniae (Fitzgerald and Gannon, 1983; Berry et al., 1994; Gunther et al., 1996). HA lyase is also produced by gram-negative bacteria but is less likely to play a role in pathogenesis. HA lyase and chondroitin lyase activities have been reported from Aeromonas, Vibrio, Beneckea and Proteus. Bacteroides fragilis, Bacteroides vulgatus, B. ovatus, B. melaninogenicus and Fusobacterium mortiferum are also reported to produce hyaluronidase. The pathogens Treponema pallidum and T. pertenue both produce surface associated HA lyases, whereas the non-pathogenic T. denticola and T. vencentii do not produce such an enzyme (Linhardt et al., 1986; Sting et al., 1990). Generally, HA lyases from gram positive and
Table 5 Biochemical and biophysical properties of HA lyases Source Molecular pI weight (kDa) 10.3 9.28 4.4 8.9 5.0 9.3 pH 5 6 Temp. Substrate C specificity 37 37 HA HA HA, C0S HA, C0S, C6S HA, C0S HA, C0S, C4S, C6S HA HA. C4S, C6S HA, C4S, C6S
Streptomyces 33 hyalurolyticus Streptococcus pyogenes 39.5 H4489A Clostridium perfringens 48 Streptomyces 121 agalactiae S. dysgalactiae 55 S. intermedicus 115 Staphylococcus aureus Propionibacterium acnes Peptostreptococcus sps 84 85 160
5.76.1 37 6.3 37 5.8 5 40 37 37 37 37
7.47.9 4.86 ND 55.8 ND 6.5
HA = hyaluronan; C0S = chondroitin sulfate; C4S = chondroitin 4 sulfate; C6S = chondroitin 6 sulfate; ND = not determined.
negative organisms are high molecular weight proteins compared to phage related hyaluronidases. The well-characterized hyaluronidases reported thus far have varied molecular weight, as represented by S. pneumoniae (107 kDa) S. agalactiae (121 kDa), C. perfringens (114 kDa), S. aureus (92 kDa) P. acnes (82 kDa) and two enzymes from Streptomyces sp (77 and 84 kDa). The molecular weight of other non-sequenced HA lyases also vary from 50 to 160 kDa (Sting et al., 1990; Kostyukova et al., 1995; Hynes and Walton, 2000). HA lyases are known to be involved in spreading toxins and pathogens in various disease conditions, including gas gangrene, meningitis, synovitis, hyperplasia, nephritis, mycoplasmosis, periodontal disease, mastitis, pneumonia, septicemia, syphilis and toxic shock syndrome (Li et al., 2000b; Spellerberg, 2000; Hynes and Walton, 2000; Jedrzejas, 2001; Makris et al., 2004). Among microbial hyaluronidases, the HA lyases from S. pneumoniae (S. PHL) and P. agalactiae are well characterized. The 3D X-ray crystal structure of S. PHL indicates that the enzyme is a globular protein with two distinct structural domains connected by a short peptide linker. The two domains are spherical and are of similar size. The N-terminal -helical domain contains the first 361 amino acid residues of the functional form of the enzyme. The C-terminal -sheet domain contains 347 residues, and Asn 349, His 399 and Tyr 408 are identified as catalytic residues in the active enzyme. Moreover, a recent X-ray crystallography report on the structure of S. agalactiae HA lyase has revealed the similar structure of S. PHL in the architecture of the entire enzyme as well as in the active site geometry (Jedrzejas, 2001, 2000; Stern and Jedrzejas, 2006). The active center of these HA lyases is composed of two main parts, a catalytic group responsible for substrate degradation and an aromatic patch responsible for the selection of cleavage sites on the substrate chains (Jedrzejas, 2000). The hyaluronate lyases from S. pneumoniae, S. agalactiae and S. aures showed a high degree of similarity, with global similarities above 65% and local similarities of about 80% (Jedrzejas, 2000; Baker et al., 2002; Stern and Jedrzejas, 2006). Through X-ray crystallography studies including (a) native enzyme, (b) complexes between the enzyme and degradation
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1931
products such as disaccharides, tetrasaccharides and hexasaccharides, and (c) site-directed mutagenesis, Jedrzejas (Jedrzejas, 2000; Stern and Jedrzejas, 2006) proposed a detailed catalytic mechanism called the proton acceptance and donation (PDA) mechanism. This mechanism involves an acceptance of proton by the enzyme followed by the donation of a different proton from the enzyme to the 1-4 glycosidic oxygen. The degradation process consists of five distinctive steps: (1) enzyme binds negatively charged substrate in the binding cleft using electropositive residues constituting the hydrophobic patch; (2) a catalytic step involving catalytic residues Asn 349, His 399, and Tyr 408 results in the cleaving of 1-4 bond with the generation of disaccharide end product; (3) hydrogen exchange between enzyme and the water microenvironment in order to return the enzyme to its natural state ready for the next round of catalysis; (4) the irreversible step of the release of the disaccharide product by utilizing negative patch in the cleft, and finally (5) a translocation of the remaining HA by one disaccharide unit towards the substrate's reducing end. Several bacteriophages from the HA-encapsulated group A Streptococci are known to synthesize a bound form of HA lyase (Baker et al., 2002). It has been suggested that the biological function of bacteriophage HA lyase is to degrade the HA capsule of the bacterial host cell, thereby facilitating attachment of phage to the cell wall. Phage HA lyases are low molecular weight (25 to 45 kDa) enzymes compared to bacterial hyaluronidases (50160 kDa). Several bacteriophages from HA-capsulated group A streptococci are known to produce hyaluronidases and nucleotide sequences of hyaluronidase genes hylPp1 and hylPp2 from two bacteriophage of Streptococcus pyogenes H4489A and 10403 respectively, have been reported. The sequences of hylPp1 and hylPp2 are similar but showed no sequence homology with the HA lyases from S. pneumoniae and S. agalactiae. Phage HA lyases degrade HA and other GAGs to a limited extent (Hynes and Ferretti, 1989; Jedrzejas, 2001; Baker et al., 2002; Jedrzejas et al., 2002). Candida and Paracoccidioides species are the most prevalent invasive fungal pathogens affecting human. The fungal infection affects lungs and can invade other organs and tissues, forming secondary lesions in the mucous membranes, skin, lymph nodes and adrenal glands. These strains produce various enzymes, including HAases. Reports indicate that HAases and chondroitinases play an important role in pathogenecity of fungi, particularly species of genus Candida and Pracoccidiodes (Shimizu et al., 1995; de Assis et al., 2003). However, none of the enzymes from the fungal species have been well characterized. Hyaluronidase inhibitors As mentioned earlier, the key role of hyaluronidases has been recognized in a number of physiological and pathological processes such as embryogenesis, angiogenesis, inflammation,
disease progression, wound healing, bacterial pathogenesis and the diffusion of systemic toxins/venoms. Therefore, identification and characterization of hyaluronidase inhibitors would be valuable for developing contraceptives, anti-tumor agents, antimicrobial and anti-venom/toxin agents. Inhibitors of hyaluronidases are potent, ubiquitous regulating agents which are involved in maintaining the balance between the anabolism and catabolism of HA. In general, documented hyaluronidase inhibitors are of different chemical forms namely proteins, glycosaminoglycans, polysaccharides, plant derived bioactive components and synthetic organic compounds (Table 7) (Mio and Stern, 2002; Khanum et al., 2005; Salmen et al., 2005; Girish and Kemparaju, 2005a,b; Isoyama et al., 2006; Machiah et al., 2006). Haas, for the first time reported the existence of a circulating inhibitor of hyaluronidase in serum (Haas, 1946). Furthermore, a number of clinical studies report increased levels of inhibitor in the serum of patients with cancer, liver disease and dermatological disorders (Grais and Glick, 1948; Snively and Glick, 1950; Newman et al., 1955; Kolarova, 1975). Based on these studies, Mio et al. (2000) purified a high molecular mass (120 kDa), thermolabile glycoprotein hyaluronidase inhibitor from mouse serum. The inhibitory activity was protease sensitive and magnesium dependent and showed maximum inhibition at pH between 6 and 8. The inhibitor also inhibits bovine testis, snake and bee venom enzymes to a varied extent, but no inhibition towards Streptomyces HA lyase. The level of serum inhibitor in mice was increased following CCl4 or IL-1 injection, inducers of the acute phase response. This inhibitor has tentatively been identified as a member of inter--inhibitor family (Mio et al., 2000). Heparin is an acidic, negatively charged and highly sulfated GAG having repeating disaccharide units of glucuronate-2sulfate (or Iduronic-2-sulfate) and N-sulfo-D-glucosamine-6sulfate linked by an (14) glycosidic linkage, and is a known and well-characterized inhibitor of hyaluronidase (Wolf et al., 1984). It inhibits the HA degradation activity of hyaluronidase through a non-competitive mechanism, suggesting that heparin does not bind to the catalytic site of the enzyme. This was further confirmed by chemical modification of hyaluronidase by aldehyde dextran (Maksimenko et al., 2001). In this study, the inhibitory effect of heparin decreased with increased modification of surface aminogroups of hyaluronidase, indicating that the inhibitor does not bind to the catalytic site but instead interacts with surface amino groups of the enzyme. At lower concentrations, heparin inhibits venom hyaluronidases more efficiently than bovine enzyme. In contrast, leech and Streptomyces hyaluronidases were not sensitive to heparin (Mio and Stern, 2002). In addition, heparan sulfate and dermatan sulfate inhibit human serum and venom hyaluronidase (Afify et al., 1993; Girish and Kemparaju, 2005a,b). Furthermore, heparin also inhibits several snake venom PLA2 enzymes through the formation of electrostatic interactions between negatively charged GAG and basic PLA2 enzymes (Melo and Ownby, 1999; Mors et al., 2000). Toida et al. (1999) reported the inhibitory activity of Osulfated HA fragments on hyaluronidase. Their inhibitory
1932
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
Table 7 List of different class of hyaluronidase inhibitors Type of compound Alkaloids Antioxidants Anti-inflammatory drugs Terpenoids/ flavonoids Synthetic compounds Compounds Aristolochic acid, ajmaline, reserpine Ascorbic acid, NDGA, N-propyl gallate, BHT, chlorogenic acid, curcumin, tannic acid Dexamethasone, indomethacin, sodium cromoglycate, salicylates, tranilast, sodium aurothiomalate, myocrisin, gossypol, Flavone, Fenoprofen, Quercetin, Apigenin, Kaempferol, Silybin, Luteolin, Hesperidin, Triterpenes, Rutin, Myricetin, Glycyrrhizin, Glycyrrhetinic acid PS53 (Hydroquinone-sulfonic acid-formaldehyde polymer), phosphorylated hesperidin, polymer of poly (styrene-4-sulfonate), sodium cellulose sulfate, 1-tetradecane sulfonic acid, L-arginin derivatives, traxanox, norlignane, urolithin B, aescin, diphenylacrylic acids, diphenyl propionic acids, indole derivatives, chalcone derivatives. Heparin, heparan sulfate, dermatan sulfate, chondroitin sulfate (A, C, D), O-sulfated HA, linamarin, amygdalin, Saturated (C10:0 to C22:0), cis-unsaturated fatty acids (C14:1 to C24:1) Chitosans, dextran sulfate, sodium alginate, planteose derivatives, hydrochinone digalactoside, 2-hydroxyphenyl manolactobioside, sulphated neomycin, verbascose, lanostanoids Withania somnifera glycoprotein (WSG), Serum hyaluronidase inhibitor HCN, L-NAME, L-arginine, Guanidium HCl Source of hyaluronidase Snake venom Snake venom, microbial Snake venom, bee venom, testis Snake venom, testis, microbial Snake venom, bee venom, testis, Hyal-1
Glycosaminoglycans and glycosides, Fatty acids Polysaccharides/ oligosaccharides Other proteins Other reagents
Snake venom, human serum, bee venom, testis Microbial, testis Snake venom, testis, bee venom, HA lyase Snake venom, bee venom, Hyal-1, testis HA lyase
strength is greater than other known inhibitors and O-sulfated GAGs. Inhibition increased with increasing size of the sulfate oligomer. Small sulfated oligosaccharides such as tetra to decasaccharides did not show any significant inhibition, while oligomers (1620) inhibit the enzyme through competitive and non-competitive basis. These results confirmed that the inhibition is not only due to the electrostatic interaction but also depends on the chain length of O-sulfated HA oligosaccharides. Recently, Isoyama et al. (2006) evaluated the activity of 21 different HAase inhibitors against HYAL-1, testicular, honeybee and Streptomyces HAases. Among the inhibitors tested, polymers of poly (styrene-4-sulfonate) and O-sulfated HA derivatives were found to be most effective. HYAL-1 and bee venom HAase were found more sensitive than testicular HAase. In contrast, Streptomyces HAase showed resistance to all inhibitors except PSS 990.000 and VERSA-TL 502 (PSS 10 6 Da). Other well-known HAase inhibitors, including heparin, gossypol, fenoprofen, sodium-aurothiomalate, 1-tetradecane sulfonic acid, and glycerrhigic acid, were not effective. Among these, gossypol and fenoprofen did not show any effect on all the HAases. Furthermore, 1-tetradecane sulfonic acid and glycerrhigic acid only weakly inhibited HYAL-1 activity. Both PSS and O-sulfonated HA derivatives showed mixed inhibition mechanisms (Compitative and uncompitative) towards HAases. This report demonstrated that the HAase inhibitors showed selectivity towards acidic and basic HAases. Chitosan is a positively charged homopolymer of glucosamine units with (1-4) linkages and is a deacetylated derivative of chitin. This polysaccharide mediates a variety of biological effects, including antiangiogenesis (Harish Prashanth and Tharanathan, 2005; Kato et al., 2005), antimicrobial (Rabea et al., 2003), and immune enhancing activities (Singla and Chawla, 2001; Senel and McClure, 2004). In addition, chitosan inhibits HA degradation by venom and bovine testicular hyaluronidases. The inhibitory property is directly related to the chain length and inhibition varies in proportion to molecular
weight: high molecular weight N medium molecular weight N low molecular weight of chitosan (Girish and Kemparaju, 2005a). Denuziere et al. (2000) reported the complex formation between chitosan and HA that resulted from the electrostatic + interaction between the NH3 functionalities of chitosan and COO groups of HA. The complex formation limits the substrate available for the enzyme, and this could possibly be the reason for exertion of in vitro inhibition. Furthermore, Asada et al. (1997) examined the effect of various types of alginic acid consisting of L-glucuronic acid and D-mannuronic acid, on the bovine testicular hyaluronidase. These studies were stimulated by the structural resemblance of alginic acid to HA. Hyaluronidase inhibition also depends on the molecular mass of sodium alginate, as inhibition increases with increasing mass. Suzuki et al. (2002) screened saturated and unsaturated fatty acids for hyaluronidase and chondroitinase inhibition. Among the studied fatty acids, saturated fatty acids did not show any inhibition of ovine testis, Streptomyces hyalurolyticus and Streptococcus dysgalactiae hyaluronidases. In contrast, cisunsaturated fatty acids containing one double bond inhibit the hyaluronidase of S. dysgalactiae and four chondroitinases from microbial sources. However, the fatty acids did not inhibit testis and Streptomyces hyaluronolyticus hyaluronidases. Moreover, isomers of oleic acid such as eicosatrienoic acid and nervonic acid inhibit hyaluronidases and chondroitinases through a noncompetitive mechanism. These results clearly indicate that the cis-unsaturated fatty acids can inhibit the enzyme and existence of the double bond is essential for inhibition. However, the position of the double bond and the cis-trans form of the fatty acid molecule did not greatly influence inhibition, and fatty acids bind to a different site other than active site of enzyme. Zaneveld et al. (2002) identified and showed that the polymer obtained from mandelic acid condensation polymer inhibits the hyaluronidase activity as well as acrosin. The authors claimed that the polymer is not cytotoxic to Lactobacilli and it has no effect on the percentage of moving spermatozoa
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1933
(sperm motility). It is an effective inhibitor of HIV, herpes viruses 1 and 2 (HSV-1 and HSV-2), Neisseria gonorrhoeae and has some effect on Chlamydia trachomatis. It is not mutagenic, has low acute and oral toxicity and it is safe in the rabbit vaginal irritation assay. Authors considered the mandelic acid condensation polymer to be a very safe contraceptive with broad-spectrum antimicrobial activity. Recently, Garg et al. (2005) showed that sulphonated hesperidin, a citrus flavonoid glycoside, completely inhibits the sperm enzyme hyaluronidase. It was also found to inhibit various sexually transmitted pathogens, including HIV and HSV-2. Ascorbic acid is a well known antioxidant and is involved in many biological processes. Botzki et al. (2004) reported the inhibition of HA lyase from S. pneumoniae (S. pnHL) by ascorbic acid and also reported the crystal structure of the enzyme with vitamin C. It indicates that only one vitamin C molecule binds S. pnHL at the active site and forms about 25 interactions with seven residues (mainly from the N-terminus and only one from the C-terminal domain) of S. pnHL. In addition, Okorukwu and Vercruysse (2003) reported inhibition by structural analogs of vitamin C on bovine testis and S. hyalurolyticus HAases. Among those tested, L-ascorbic acid and D-isoascorbic acid inhibited both the enzymes but showed stronger inhibitory capacity towards the HA lyase. But these analogs were observed to degrade the substrate, HA, by themselves. In contrast, D-saccharic 14 lactone did not inhibit testicular enzyme but exhibited over 50% inhibition towards HA lyase and chondroitinase ABC without affecting the physico-chemical stability of HA. Since these are virulence factors produced by a number of causative pathogenic organisms, saccharic acid can serve as a potent inhibitor of HA lyases and as a novel antibacterial agent, thus providing an alternative to antibiotics. Furthermore, vitamin C did not inhibit N. naja venom and ovine testicular hyaluronidases up to the studied concentration of 500 mM (Girish and Kemparaju, 2005a,b). Akhtar and Bhakuni (2003) screened Gdn HCl (guanidine hydrochloride), L-arginine, C-NAME (nitro-L-arginine methyl ester) and GdnHSCN (guanidine isothiocyanate) for its antihyaluronate lyase activity. All these compounds inhibited the enzymatic activity of S. pnHL in a dose dependent manner. Guanidine HCl completely inhibited the enzyme activity (about 350 mM) without altering structural properties of the enzyme. These observations suggested that GdnHCl, L-arginine, LNAME, and GdnHSCN affect the active site of the enzyme at a concentration much lower than that required for bringing out any significant structural change in the enzyme. Therefore, the authors have claimed that these studies present a new chemical entity that can be exploited for better designing of inhibitors for S. pnHCL. Aristolochic acid (8-methoxy-6-nitrophenanthro (3,4,D-) 1,3-dioxole-5-corboxylic acid) is a nitro compound with a phenanthrene nucleus. Aristolochic acid completely neutralizes ovine testis and snake venom hyaluronidases. In contrast, ajmaline and reserpine inhibits the enzyme activities considerably less than aristolochic acid. It completely inhibits the hyaluronidases from N. naja venom through a non-
competitive mechanism. The interaction of aristolochic acid with hyaluronidase was confirmed by spectoflurophotometer analysis in which the aristolochic acid quenched the pronounced fluorescence intensity of hyaluronidase. The quenching was found to increase with increasing concentration. From these studies, it is clear that the aristolochic acid does not bind to the catalytic site but interacts with exposed tyrosine and tryptophan residues of hyaluronidase. In addition, the aristolochic acid completely neutralized the enzyme-mediated potentiation of toxicity of VRV-PL-VIII myotoxin and hemorrhagic complex-I. Inhibition of HA degradation by hyaluronidase in human skin and muscle tissue sections by aristolochic acid supports the possible contribution of in vivo degradation of HA in hyaluronidase mediated enhanced toxicity of toxins. Interestingly, aristolochic acid increased the survival time of experimental mice injected with N. naja venom (Girish and Kemparaju, 2005a, 2006). Certain anti-inflammatory drugs including salycylates, indomethacin and dexamethasone also exert anti-hyaluronidase activity (Mio and Stern, 2002; Girish and Kemparaju, 2005a,b). These drugs may prevent HA degradation by hyaluronidases, though the degradation products of HA are potent inducers of inflammatory cytokines (Horton et al., 1998; Noble, 2002). Anti-allergic drugs such as disodium cromoglycate, sodium aurothiomalate, and transilist were evaluated and found to possess hyaluronidase inhibitory activity. Sodium cromoglycate and sodium aurothiomalate completely inhibited venom hyaluronidase. In addition, these two drugs neutralized the local (edema, hemorrhage) as well as systemic (myotoxicity, survival time) toxicity exhibited by Naja kauothia and Calloselasma rhodostoma venoms (Yingprasertchai et al., 2003). Dexamethasone, phenyl butazo indomethacin, oxybutazone and fenofrofen inhibited snake venom hyaluronidase in a dose dependent manner (Szary et al., 1975; Girish and Kemparaju, 2005a,b). These inhibitors of snake venom hyaluronidases can be used as first-aid components for snakebite therapy. Generally, plant derived bioactive compounds are used to block hyaluronidase activity. These include flavonoids (Kuppusamy and Das, 1991; Pessini et al., 2001; Hertel et al., 2006), tannins (Kakegawa et al., 1985), antioxidants (Girish and Kemparaju, 2005a), pectins, curcumins (Tonnesen, 1989), coumarins, gylcyrrhizin (Furuya et al., 1997), hydrogenols from hydrangea (Kakegawa et al., 1988), glycoproteins (Machiah et al., 2006), anti-inflammatory compounds and alkaloids (Szary et al., 1975; Girish and Kemparaju, 2005a). These compounds have traditionally been used as contraceptives, to promote wound healing, as anti-inflammatory agents and to treat snakebite, presumably through their ability to inhibit hyaluronidase activity in respective conditions. Some of the plant extracts are also used in folk medicines to block several hyaluronidases (Joyce et al., 1986; Mio and Stern, 2002; Girish et al., 2004a; Ushanandini et al., 2006). Medical applications of hyaluronan HA plays an important physiological role in many organisms and it has been used principally in biomedical applications
1934
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
(Larsen and Balazs, 1991; Vercruysse and Prestwich, 1998; Moreland, 2003; Liao, 2005). It is an extremely attractive polymer material because it is a natural product that degrades into simple sugars. Its hygroscopic and highly viscoelastic nature makes it suitable for various medical and pharmaceutical applications. This section details the medical and pharmaceutical uses of HA. Treatment of osteoarthritis The viscoelasticity of the HA is responsible for lubrication and mechanical support of joints. However, in osteoarthritic joints, HA molecular mass and concentration can decline as a result of the pro-inflammatory cytokines and free radicals (Balazs and Denlinger, 1993; Stern, 2003). Changes in the viscoelasticity of the synovial fluid results in joint related problems. Intra-articular injection of HA is approved for the treatment of osteoarthritis in many countries including the United States, Canada, Japan and some part of the European Union. Commercially available products for this application contain sodium HA with different molecular mass, for example Hyalgan (Fidia, Italy), Artz (Seikagaku, Japan) and Orthovisc (Anika, USA). The therapeutic effects of HA injection products on osteoarthritic joints have been extensively investigated in vitro, in vivo and clinically (Altman, 2000; Uthman et al., 2003; Hamburger et al., 2003). Results from these studies indicate that HA suppresses cartilage degeneration and release of proteoglycans from the extracellular matrix in cartilage tissues, protects the surface of articular cartilage, normalizes the properties of synovial fluids, and reduces pain perception. The analgesic effect obtained after administration of HA was found to be comparable or superior to either corticosteroids or nonsteroidal anti-inflammatory drugs (Altman, 2000; Kirwan, 2001). However, the mechanism of these effects of HA on osteoarthritic joints is unclear (Ghosh and Guidolin, 2002). Many researchers believe that HA can confer mechanical and lubricating effects and protect joint tissues by its viscosupplementation, viscoaugmentation and viscoprotection properties, which are independent of its molecular mass. The pharmacological role of HA may be related to its antiinflammatory and immunoregulatory properties. Surgery and wound healing HA is commonly used in eye surgery in conjunction with the implantation of artificial intraocular lens and other commercially available products. HA is also used in surgical procedures as a viscoelastic gel to aid healing and regenerative processes of surgical wounds. In the case of cataract surgery, HA gels are used to maintain operative space (depth of the anterior chamber) and to protect the endothelial layer of the cornea (acting as a lubricant) or other tissues from physical damage (Ghosh and Guidolin, 2002; Ghosh and Jassal, 2002). Furthermore, HA appears to promote corneal, diabetic foot, tendon, bone, nasal mucosal, and venous leg ulcer wound healing (Miller et al., 1997; Liao, 2005). Miyazaki et al. (1996) suggested that HA promoted corneal wound healing is partially due to its ability to
promote the growth of corneal epithelial cells. In addition, HA is used as an anti-adhesion and anti-scar drug in general surgery. It acts as an antioxidant for inflamed body tissues, protecting body tissue from free radical damage and supporting immune function by inhibiting germs and viruses from moving between cells and getting into cells. In addition, HA also has been reported to decrease neutrophil elastase promoted alveolar injury after inhalation (Liao, 2005). The study suggested that the protective mechanism was due to specific binding between HA and lung elastic fibers. However, the molecular mechanism of HA-induced wound healing has yet to be identified. Embryo implantation Higher concentrations of HA during estrus and ovulation suggest that HA has a function prefertilization through embryonic development. HA has been found to be a suitable replacement for albumin in culture media for in vivo fertilization (Simon et al., 2003). The presence of HA as an alternate to albumin has not resulted in any harmful effects on the development of frozen-thawed mouse and sheep embryos. In addition, the presence of HA in culture media could act as a cryopreservative of human embryos by maintaining their viability during thawing. More studies have investigated the effect of HA in murine, porcine and bovine embryo development and viability after culture in HA-based media (Figueiredo et al., 2002; Abeydeera, 2002; Jang et al., 2003). Simon et al. (2003) reported that HA-based human embryo transfer medium showed a better pregnancy and implantation rate than albuminbased medium. Recently, studies reported that exogenous HA significantly increased the expression of insulin like growth factor-II gene and reduced the expression of apoptosis (Bax), oxidative stress (SOX), and embryo cell-to cell adhesion associated with embryo compaction (Ecad) genes. Furthermore, the general fine structure of embryos cultured with HA was noticeably improved in comparison with the respective controls. Based on these studies, it is confirmed that supplemental HA could improve the quality of the embryo and developmental rates of blastocytes (Palasz et al., 2006). As a disease indicator HA occurs in many forms, circulating freely in the blood stream and lymphatic system and loosely/tightly interacting with ECM. Normally, low concentrations of HA circulate in the blood stream, whereas increases in tissue bound and circulating HA occur very early in wound healing and during periods of rapid cell turnover following tissue injury (Fraser et al., 1997; Lee and Spicer, 2000). Rapid increases in circulating HA also occur in response to major stress, such as blood loss, shock, ischaemic stroke, and septicemia following massive trauma, major surgical procedures and extensive burns (Berg, 1997; George and Stern, 2004; Al'qteishat et al., 2006). Increased serum HA is also one of the earliest indicators of liver cirrhosis, liver fibrosis, knee osteoarthritis and rejection following liver transplantation. Clearly, increased HA provides a rapid response survival mechanism following major injuries and several
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1935
diseases (George and Stern, 2004). HA, as a biomarker has the potential for use clinically to detect the early changes following injuries and diseases as well as for screening drugs. Hyaluronan in drug delivery In recent years, HA has had significant use in the development of dermal and transdermal drug delivery systems. The outermost layer of the skin acts as a protective barrier and prevents the access of drug molecules into and across the skin. The beneficial effect of HA on the dermal delivery of diclofenac has been thoroughly investigated in vitro, in vivo and in clinical studies (Wolf et al., 2001; Brown et al., 2002). In vitro studies reported that HA significantly enhances both the partitioning of diclofenac into human skin and its retention and localization in the epidermis when compared with a control and other commonly used pharmaceutically acceptable gelling agents (Brown and Martin, 2001). HA also has been reported to produce similar effects with cyclosporine, ibuprofen, and clindamycin phosphate (Nazir et al., 2001; Brown et al., 2002). HA has been used as a vehicle for topical ophthalmic and nasal drugs due to its viscoelasticity and mucoadhesive capacity (Lapcik et al., 1998; Castellano and Mautone, 2002). Several studies have reported that HA is capable of the prolonging residence and/or increasing the bioavailability of molecular drugs such as pilocarpine, vasopressin, 1-deamino-8-D-arginine vasopressin, tropicamide, timolol, xylometazoline, gentimycin, arecaidine propargyl ester and [ S]-aceclidine in solution (Morimoto et al., 1991; Liao, 2005). The increased bioavailability of drugs conferred by HA was found to be molecular mass dependent, with the high molecular mass HA fractions promoting an increase in bioavailability while low molecular mass HA had no effect (Morimoto et al., 1991). Mucoadhesive and viscoelastic properties of HA are thought to be primarily responsible for the prolonged precorneal residence of the drugs. Furthermore, a HA-based microparticulate delivery system showed increased mucoadhesive properties compared to chitosan-based microparticulates. In addition, the mucoadhesive properties of microparticulates were not affected by the presence of gentamycin. The bioavailability of intranasally administered gentamycin was significantly higher in HA/ chitosan microspheres compared to drug particles or chitosanbased particles and HA-based particles alone. Therefore, researchers assumed that HA mainly acts as a mucoadhesive agent whereas chitosan had a penetration enhancement function (Lim et al., 2000, 2002). The non-immunogenic nature of HA was used in parental/ pulmonary drug delivery systems to obtain constant release or to prolong the retention of drugs/hormone/anticancer agents. Direct conjugates of low molecular mass HA to cytotoxic drugs such as butyric acid, paclitaxel, and doxorubicin have been reported (Luo et al., 2000). It has been shown that these bioconjugates are internalized into cancer cells through receptor-mediated endocytosis followed by intracellular release of active drugs, thus restoring their original cytotoxicity For example, taxol, an anticancer drug, when chemically linked to HA was found to selectively target human colon, ovarian and
breast cancer cell lines in vitro (Luo et al., 2000). In addition, HA enhances the anti-inflammatory activity of conjugated proteins in mice. The HA-modified liposomes provided more efficiently encapsulated of anticancer drug, doxorubicin and epidermal growth factor relative to unmodified liposomes (Peer et al., 2003; Liao, 2005). Recently, HA has been used to prepare DNAHA matrices and microspheres with the goal of achieving sustained gene delivery (Yun et al., 2004). To obtain optimal properties for mechanical strength, drug delivery or biostability, a variety of HA-grafted co-polymers have been prepared. For example, collagen crosslinking with polyethylene glycol (PEG)-grafted-HA co-polymer, polypyrrole-functionalized HA polymer, benzyl-functionalized HA polymer, and methacrylic anhydride-functionalized HA polymer were developed for the delivery of drugs and water-soluble peptides. In addition, HA has been utilized to develop an implantable delivery to achieve long-term delivery of antibiotic and anti-inflammatory drugs. Surini et al. (2003) produced a chitosan and HA implant containing insulin and achieved programmed release profiles of insulin. The release rate of insulin was dictated by chitosan-to-HA mixing ratios and the amount of insulin loaded. Moreover, several strategies have been developed to make implants of HA-fibronectin and HAcollagen/gelatin to enhance cell interactions with HA (Ghosh et al., 2006). Recently, Ji et al. (2006) fabricated a threedimensional (3D) modified HA nanofibrous scaffold based on electrospinning to mimic the architecture of natural ECM. When NIH 3T3 fibroblasts were seeded on a fibronectinadsorbed HA scaffold for 24 h in vitro, fibroblasts attached to the scaffold and spread, demonstrating an extended dendritic morphology within the scaffold. This suggests potential application of HA scaffolds in cell encapsulation and tissue regeneration (Ji et al., 2006). In another study, Lepidi et al. (2006) implanted a HA-based graft (HYAFF 11 tube, diameter 2 mm, length 1.5 cm) in an end-to-end fashion in the abdominal aorta of rats and allowed for 7, 21, and 90 days. The data indicated that the HA-based graft allowed complete regeneration of a newly formed vascular tube in which all the cellular and extracellular components are present and organized in a well-defined architecture similar to the native artery (Lepidi et al., 2006). Hydrogels (hylans) based on crosslinked HA are potentially good biomaterials for soft-tissue engineering applications because they are highly non-antigenic and non-immunogenic. The previous biomedical uses for hylans have capitalized on their bio-inert characteristics; a potentially useful future application for these highly biocompatible natural matrixderived materials is as cell scaffolds for soft tissue engineering, for example vascular remodeling (Hoffman, 2001; Ramamurthi and Vesely, 2003, 2005; Shi et al., 2002; Hou et al., 2005; Hahn et al., in press). To overcome the high rate of in vivo turn over, crosslinking methods have been used to stabilize the HA polymers. Some of these methods include water-soluble carbodimide crosslinking, polyvalent hydrazide crosslinking, disulfide crosslinking, divinyl sulfone crosslinking, and photocrosslinking hydrogels through glycidyl methacrylateHA conjugates. Covalent crosslinking of HA
1936
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
provides the ability to improve the desirable biological and mechanical properties of HA. The various crosslinking models of HA prolong the in vivo degradation and provide long-term stability. Thus, crosslinking HA polymers results in different pore sizes and degradation profiles that have been used for biomedical applications such as orthopedics, cardiovascular medicine, and dermatology. HA gels crosslinked with divinyl sulfone (DVS) are highly biocompatible and can be structurally modified to obtain desired mechanical properties. However, some studies have indicated that the high anionic nature of hylan gels results in poor interaction with cells in vitro (Ramamurthi and Vesely, 2003). Additionally, crosslinked hylan gels are highly (N 95% w/w) hydrated and exhibit smooth surfaces that oppose cell attachment and bioactivity. Ramamurthi and Vesely (2003) observed significantly higher levels of attachment and proliferation of neonatal rat smooth muscle cells on the surface of ultraviolet (UV) irradiated and dehydrated-irradiated hylan gels compared to unmodified gels. This modification micro-textures the smooth gel surface to provide sites for cell anchorage and causes limited scission of native long-chain HA, yielding smaller fragments. In addition, when neonatal rat aortic smooth muscle cells were cultured on hylan gels coated with matrix molecules such as collagen I, matrigel, laminin, and fibronectin for 4 weeks, significant cell attachment was seen on coated gels compared to uncoated gels. Moreover, the matrix molecules coating the hylan gels and the surface topography of the gels influenced cell morphology. These results indicate that cell attachment and proliferation can be enhanced by surface texturizing and subsequent surface treatment with matrix molecules (Ramamurthi and Vesely, 2002). Recently, Amarnath et al. (2006) studied the interaction between UV-irradiated hylan gels and human blood cells (RBCs, platelets) and coagulation proteins at physiological temperature. Relative to the positive controls, both un-irradiated and UVirradiated gels prolonged the formation of coagulum through extrinsic and intrinsic pathways. UV-irradiated gels also induced lower contact activation and also very low levels of hemolysis. Furthermore, Joddar and Ramamurthi (2006) evaluated the fragment size and dose specific effects of HA on matrix synthesis by vascular smooth muscle cells. These findings suggest that the HA derived grafts and implants can be used as tissue engineering scaffolds to modulate vascular regeneration. HA is a unique molecule with viscoelastic, hydrophilic, nonimmunogenic and lubricious properties that make possible its use in various medical and pharmaceutical applications. It is a distinctive biomaterial, which provides itself to crosslinking and immobilizing in numerous ways to produce biocompatible grafts and implants. Ongoing research developments regarding incorporation of HA into biomaterials for biomedical applications have the potential to transform the clinical future of drug delivery and tissue engineering. Medical application of hyaluronidase The biomedical applications of hyaluronidase are limited compared to HA. Hyaluronidase is an endoglycosidase. By
cleaving HA in tissues, it increases the membrane permeability, reduces viscosity and renders tissues more permeable to injected fluids (spreading effect). Thus, these enzymes could be used therapeutically to increase the speed of absorption, to promote resorption of excess fluids, to increase the effectiveness of local anesthesia and to diminish tissue destruction by subcutaneous and intramuscular injection of fluids (Frost et al., 1996; Farr et al., 1997). Hyaluronidase has been used to reduce the extent of tissue damage following extravasation of parental nutrition solution, electrolyte infusions, antibiotics, aminophyline, mannitol and chemotherapeutic agents including Vinca alkaloids (vincristine, vinblastine and vinorelbine). Hyaluronidase can be used to decrease myocardial infarction size, as demonstrated in biomedical studies on animals. Borrelli et al. shown that combined administration of hyaluronidase (2500 IU/kg) with urokinase (40,000 IU/kg) into rats with myocardial infarction significantly decreased mortality data, where the lethal index for combination of preparations was 12.5% against 29.5% for urokinase (Muckenschnabel et al., 1997). Hyaluronidases are widely used in many fields, including orthopaedia, surgery, ophthalmology, internal medicine, oncology, dermatology and gynaecology. Sperm hyaluronidase plays an important role in successful fertilization in most mammals, including human (Manzel and Farr, 1988; Frost et al., 1996; Borrelli et al., 1986; Primakoff et al., 1985; Lin et al., 1994; Klocker et al., 1995). Hyaluronidase has been investigated as an additive to chemotherapeutic drugs for augmentation of anticancer activity (Muckenschnabel et al., 1997, 1998; Spruss et al., 1995; Baumgartner, 1998). There is evidence that hyaluronidase may have intrinsic anticancer effects and can suppress tumor development. Furthermore, it was reported that treatment with hyaluronidase blocks lymph node invasion by tumor cells in an animal model of T cell lymphoma (Zahalka et al., 1995). Concluding remarks HA is an abundant polysaccharide in the ECM and is involved in many physiological and pathological processes. The biosynthesis, uptake and degradation of HA are well balanced under normal homeostasis. Despite the intensive studies carried out thus far, our understanding of the complete function of HA in eukaryotes is unclear. HA appears to be a very important molecule since its aberrant production and turnover results in many pathological and inherited disease conditions. Furthermore, HAcell interactions and cellular signaling induced by HA and its degraded products from the metabolism of HA have a major impact on normal and diseased cell behavior. HA degradation by hyaluronidases is also critical in a number of important regulatory processes that range from embryonic development to wound healing. Thorough knowledge of enzyme dependent HA degradation will be helpful in understanding the complete process of HA catabolism. The molecular mechanism of HA degradation by vertebrate hyaluronidase is still under investigation; however, it will
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943
1937
be interesting to know the in vivo hyaluronidase dependent HA degradation products under normal and pathological conditions. It will also be exciting to know the in vivo fragmentation of HA by venom and microbial hyaluronidases and its subsequent effects on pathophysiology of envenomation/ pathogenesis. Identification of inhibitors associated with hyaluronidase during the HA degradation may be helpful in understanding regulation of HA metabolism, crucial changes in tissues/ lymphatic system and in the search for rational therapeutic approaches to prevent several disorders. In addition, identification and characterization of hyaluronidase inhibitors from natural sources may lead to valuable antimicrobial contraceptives, antitumor agents and alternatives to complement anti-venom as well as first aid agents in venomous bite/hymenoptera sting therapy. Acknowledgements We thank Prof. B.S. Vishwanath, Department of Biochemistry, University of Mysore for his valuable suggestions during the preparation of the article. We are also grateful to Prof. Periasamy Selvaraj, Dr. K.D. Machaiah, Dr. M. Vedavathi, and Dr. R. Shasidharamurthy and S. Nagaraju for their suggestions and critical reading of the manuscript. KSG extend sincere thanks to the Council of Scientific and Industrial Research (CSIR), New Delhi, India, for the financial assistance. We also apologize to the authors of many interesting studies that were omitted due to limited space. References
Abeydeera, L.R., 2002. In vitro production of embryos in swine. Theriogenology 57, 257273. Adamia, S., Maxwell, C.A., Pilarski, L.M., 2005. Hyaluronan and hyaluronan synthases: potential therapeutic target in cancer. Current Drug Targets. Cardiovascular & Haematological Disorders 5, 314. Afify, A.M., Stern, M., Guntenhoener, M., Stern, R., 1993. Purification and characterization of human serum hyaluronidase. Archives of Biochemistry and Biophysics 305, 434441. Ahrens, T., Sleeman, J.P., Schempp, C.M., Howells, N., Hofmann, M., Ponta, H., Herrlich, P., Simon, S.C., 2001. Soluble CD44 inhibits melanoma tumor growth by blocking cell surface CD44 binding to hyaluronic acid. Oncogene 20, 33993408. Akhtar, M.S., Bhakuni, V., 2003. Streptococcus pneumoniae hyaluronate lyase contains two non-cooperative independent folding/unfolding structural domains: characterization of functional domain and inhibitors of enzymes. Journal of Biological Chemistry 278, 2550925516. Al'qteishat, A., Gaffney, J., Krupinski, J., Rubio, F., West, D., Kumar, S., Kumar, P., Mitsios, N., Slevin, M., 2006. Changes in hyaluronan production and metabolism following ischaemic stroke in man. Brain 129, 21582176. Altman, R.D., 2000. Intra-articular sodium hyaluronate in osteoarthritis of the knee. Seminars in Arthritis and Rheumatism 30, 1118. Amarnath, L.P., Srinivas, A., Ramamurthi, A., 2006. In vitro hemocompatibility testing of UV-modified hyaluronan hydrogels. Biomaterials 27, 14161424. Asada, M., Sugie, M., Inoue, M., Nakagomi, K., Hongo, S., Murata, K., Irie, S., Takeuchi, T., Tomizuka, N., Oka, S., 1997. Inhibitory effect of alginic acids on hyaluronidase and on histamine release from mast cells. Bioscience, Biotechnology, and Biochemistry 61, 10301032. Averbeck, M., Gebhardt, C.A., Voigt, S., Beilharz, S., Anderegg, U., Termeer, C.C., Sleeman, J.P., Simon, J.C., 2007. Differential regulation of hyaluronan metabolism in the epidermal and dermal compartments of human skin by UVB irradiation. Journal of Investigative Dermatology 127, 687697.
Baba, D., Kashiwabara, S., Honda, A., Yamagata, K., Wu, Q., Ikawa, M., Okabe, M., Baba, T., 2002. Mouse sperm lacking cell surface hyaluronidase PH-20 can pass through the layer of cumulus cells and fertilize the egg. Journal of Biological Chemistry 277, 3031030314. Baker, J.R., Dong, S., Pritchard, D.G., 2002. The hyaluronan lyase of Streptococcus pyogenes bacteriophage H4489A. Biochemical Journal 365, 317322. Balazs, E.A., Denlinger, J.L., 1993. Viscosupplementation: a new concept in the treatment of osteoarthritis. Journal of Rheumatology 20, 39. Banerji, S., Ni, J., Wang, S.X., Clasper, S., Su, J., Tammi, R., Jones, M., Jackson, D.G., 1999. LYVE-1, a new homologue of the CD44 glycoprotein is a lymphspecific receptor for hyaluronan. Journal of Cell Biology 144, 789801. Baumgartner, G., 1998. The impact of extracellular matrix on chemoresistance of solid tumorsexperimental and clinical results of hyaluronidase as additive to cytostatic chemotherapy. Cancer Letters 131, 12. Bayliss, M.T., Howat, S.L., Dudhia, J., Murphy, J.M., Barry, F.P., Edwards, J.C., Day, A.J., 2001. Up-regulation and differential expression of the hyaluronan-binding protein TSG-6 in cartilage and synovium in rheumatoid arthritis and osteoarthritis. Osteoarthritis and Cartilage 9, 4248. Beech, D.J., Madan, A.K., Deng, N., 2002. Expression of PH-20 in normal and neoplastic breast tissue. Journal of Surgical Research 103, 203207. Berg, 1997. Hyaluronan turnover in relation to infection and sepsis. Journal of Internal Medicine 242, 7377. Berry, A.M., Lock, R.A., Thomas, S.M., Rajan, D.P., Hansman, D., Paton, J.C., 1994. Cloning and nucleotide sequence of the Streptococcus pneumoniae hyaluronidase gene and purification of the enzyme from recombinant Escherichia coli. Infection and Immunity 62, 11011108. Blundell, C.D., Seyfried, N.T., Day, A.J., 2004. Structural and functional diversity of hyaluronan binding proteins. In: Garg, H.G., Hales, C.A. (Eds.), Chemistry and Biology of Hyaluronan. Elsevier Press, Amsterdam, pp. 184204. Bono, P., Rubin, K., Higgins, J.M., Hynes, R.O., 2001. Layilin, a novel integral membrane protein, is a hyaluronan receptor. Molecular Biology of the Cell 12, 891900. Bono, P., Cordero, E., Johnson, K., Borowsky, M., Ramesh, V., Jacks, T., Hynes, R.O., 2005. Layilin, a cell surface hyaluronan receptor, interacts with merlin and radixin. Experimental Cell Research 308, 177187. Borrelli, F., Antonetti, F., Martelli, F., Caprino, L., 1986. The co-operative action of hyaluronidase and urokinase on the isoproterenol-induced myocardial infarction in rats. Thrombosis Research 42, 153164. Botzki, A., Rigden, D.J., Braun, S., Nukui, M., Salmen, S., Hoechstetter, J., Bernhardt, G., Dove, S., Jedrzejas, M.J., Buschauer, A., 2004. L-Ascorbic acid, 6-hexadecanoate, a potent hyaluronidase inhibitor. X-ray structure and molecular modeling of enzymeinhibitor complexes. Journal of Biological Chemistry 279, 4599045997. Brown, M.B., Martin, G.P., 2001. Comparison of the effect of hyaluronan and other polysaccharides on drug skin partitioning. International Journal of Pharmacology 225, 113121. Brown, M.B., Forbes, B., Martin, G.P., 2002. The use of hyaluronan in topical drug delivery. In: Kennedy, J., Phillips, G.O., Williams, P.A., Hascall, V.C. (Eds.), Hyaluronan: Biomedical, Medical and Clinical Aspects. Woodhead publishers, Cambridge, pp. 249256. Cao, T.V., La, M., Getting, S.J., Day, A.J., Perretti, M., 2004. Inhibitory effects of TSG-6 Link module on leukocyte-endothelial cell interactions in vitro and in vivo. Microcirculation 11, 615624. Castellano, F., Mautone, G., 2002. Decongestant activity of a new formulation of xylometazoline nasal spray: a double-blind, randomized versus placebo and reference drugs controlled, doseeffect study. Drugs Under Experimental and Clinical Research 28, 2735. Chain, E., Duthie, E.S., 1940. Identity of hyaluronidase and spreading factor. British Journal of Experimental Pathology 21, 324338. Chen, W.J.Y., Abatangelo, G., 1999. Functions of hyaluronan in wound repair. Wound Repair and Regeneration 7, 7989. Cherr, G.N., Yudin, A.I., Overstreet, J.W., 2001. The dual functions of GPIanchored PH-20: hyaluronidase and intracellular signaling. Matrix Biology 20, 515525. Cramer, J.A., Bailey, L.C., Bailey, C.A., Miller, R.T., 1994. Kinetic and mechanistic studies with bovine testicular hyaluronidase. Biochimica et Biophysica Acta 1200, 315321.
1938
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Furuya, T., Yamagata, S., Shimoyama, Y., Fujihara, M., Morishima, N., Ohtsuki, K., 1997. Biochemical characterization of glycyrrhizin as an effective inhibitor for hyaluronidases from bovine testis. Biological & Pharmaceutical Bulletin 20, 973977. Garg, A., Anderson, R.A., Zaneveld, L.J., Garg, S., 2005. Biological activity assessment of a novel contraceptive antimicrobial agent. Journal of Andrology 26, 414421. Gatphayak, K., Knorr, C., Beck, J., Brenig, B., 2004. Molecular characterization of porcine hyaluronidase genes 1, 2, and 3 clustered on SSC13q21. Cytogenetics and Genome Research 106, 98106. George, J., Stern, R., 2004. Serum hyaluronan and hyaluronidase: very early markers of toxic liver injury. Clinica Chimica Acta 348, 189197. Ghatak, S., Misra, S., Toole, B.P., 2002. Hyaluronan oligosaccharides inhibit anchorage-independent growth of tumor cells by suppressing the phosphoinositide 3-kinase/Akt cell survival pathway. Journal of Biological Chemistry 277, 3801338020. Ghosh, P., Guidolin, D., 2002. Potential mechanism of action of intra-articular hyaluronan therapy in osteoarthritis: are the effects molecular weight dependent? Seminars in Arthritis and Rheumatism 32, 1037. Ghosh, S., Jassal, M., 2002. Use of polysaccharide fibres for modem wound dressings. Indian Journal of Fibre and Textile Research 27, 434450. Ghosh, K., Ren, X.D., Shu, X.Z., Prestwich, G.D., Clark, R.A.F., 2006. Fibrinectin functional domains coupled to hyaluronan stimulate adult human dermal fibroblast responses critical for wound healing. Tissue Engineering 12, 601613. Girish, K.S., Kemparaju, K., 2005a. A low molecular weight isoform of hyaluronidase: purification from Indian cobra (Naja naja) venom and partial characterization. Biochemistry (Moscow) 70, 708712. Girish, K.S., Kemparaju, K., 2005b. Inhibition of Naja naja venom hyaluronidase by plant-derived bioactive components and polysaccharides. Biochemistry (Moscow) 70, 948952. Girish, K.S., Kemparaju, K., 2006. Inhibition of Naja naja venom hyaluronidase: role in the management of poisonous bite. Life Sciences 78, 14331440. Girish, K.S., Mohankumari, H.P., Nagaraju, S., Vishwanath, B.S., Kemparaju, K., 2004a. Hyaluronidase and protease activities from Indian snake venoms: neutralization by Mimosa pudica root extract. Fitoterapia 75, 378390. Girish, K.S., Shashidhara Murthy, R., Nagaraju, S., Gowda, T.V., Kemparaju, K., 2004b. Isolation and characterization of hyaluronidase a spreading factor from Indian cobra (Naja naja) venom. Biochimie 86, 193202. Gmachl, M., Kreil, G., 1993. Bee venom hyaluronidase is homologous to a membrane protein of mammalian sperm. Proceedings of the National Academy of Sciences of the United States of America 90, 35693573. Grais, M.L., Glick, D., 1948. Mucolytic enzyme systems. II Inhibition of hyaluronidase by serum in skin diseases. Journal of Clinical Dermatology 11, 259273. Gunther, E., Ozegowski, J.H., Kohler, W., 1996. Occurrence of extracellular hyaluronic acid and hyaluronate lyase in Streptococci of groups A, B, C, and G. Zentralblatt fur Bakteriologie 285, 6473. Haas, E., 1946. On the mechanism of invasion. I. Antinvasin I, An enzyme in plasma. Journal of Biological Chemistry 164, 6388. Hahn, S.K., Kim, J.S., Shimobouji, T., in press. Injectable hyaluronic acid microhydrogels for controlled release formulation of erythropoietin. Journal of Biomedical Material Research A 80, 916924. Hall, C.L., Lange, L.A., Prober, D.A., Zhang, S., Turley, E.A., 1996. Pp60 (c-src) is required for cell locomotion regulated by the hyaluronan receptor RHAMM. Oncogene 13, 22132224. Hamburger, M.I., Lakhanpal, S., Mooar, P.A., Oster, D., 2003. Intra-articular hyaluronans: a review of product-specific safety profiles. Seminars in Arthritis and Rheumatism 32, 296309. Harish Prashanth, K.V., Tharanathan, R.N., 2005. Depolymerized products of chitosan as potent inhibitors of tumor-induced angiogenesis. Biochimica et Biophysica Acta 1722, 2229. Heldin, P., 2003. Importance of hyaluronan biosynthesis and degradation in cell differentiation and tumor formation. Brazilian Journal of Medical and Biological Research 36, 967973. Hertel, W., Peschel, G., Ozegowski, J.H., Muller, P.J., 2006. Inhibitory effects of triterpenes and flavonoids on the enzymatic activity of hyaluronic acid
Csoka, A.B., Frost, G.I., Wong, T., Stern, R., 1997. Purification and microsequencing of hyaluronidase isoenzymes from human urine. FEBS Letters 417, 307310. Csoka, A.B., Frost, G.I., Heng, H.H., Scherer, S.W., Mohapatra, G., Stern, R., 1998. The hyaluronidase gene HYAL1 maps to chromosome 3p21.2p21.3 in human and 9F1F2 in mouse, a conserved candidate tumor suppressor locus. Genomics 48, 6370. Csoka, A.B., Scherer, A.W., Stern, R., 1999. Expression analysis of six paralogous human hyaluronidase genes clustered on chromosomes 3p21 and 7q31. Genomics 60, 356361. Csoka, A.B., Frost, G.I., Stern, R., 2001. The six hyaluronidase-like genes in the human and mouse genomes. Matrix Biology 20, 499508. da C B Gouveia, A.I., da Silveira, R.B., Nader, H.B., Dietrich, C.P., Gremski, W., Veiga, S.S., 2005. Identification and partial characterisation of hyaluronidases in Lonomia obliqua venom. Toxicon 45, 403410. Day, A.J., de la Motte, C.A., 2005. Hyaluronan cross-linking: a protective mechanism in inflammation. Trends in Immunology 26, 637643. Day, A.J., Prestwich, G.D., 2002. Hyaluronan-binding proteins: tying up the giant. Journal of Biological Chemistry 277, 45854588. de Assis, C.M., Gandra, R.F., Gambale, W., Shimizu, M.T., Paula, C.R., 2003. Biosynthesis of chondroitinase and hyaluronidase by different strains of Paracoccidioides brasiliensis. Journal of Medical Microbiology 52, 479481. Deguine, V., Menasche, M., Ferrari, P., Fraisse, L., Pouliquen, Y., Robert, L., 1998. Free radical depolymerization of hyaluronan by Maillard reaction products: role in liquefaction of aging vitreous. International Journal of Biological Macromolecules 22, 1722. Denuziere, A., Ferrier, D., Domard, A., 2000. Interactions between chitosan and glycosaminoglycans (chondroitin sulfate and hyaluronic acid): physicochemical and biological studies. Annals of Pharmacology (France) 58, 4753. Duh, F.M., Dirks, C., Lerman, M.I., Miller, A.D., 2005. Amino acid residues that are important for Hyal2 function as a receptor for Jaagsiekte sheep retrovirus. Retrovirology 2, 5969. Duran-Reynals, F., 1928. Exaltation de l'activit du virus vaccinal par les extraits de certains organs. Comptes Rendus des Sances de la Socit de Biologie et de Ses Filiales 99, 67. Evanko, S.P., Raines, E.W., Ross, R., Gold, L.I., Wight, T.N., 1998. Proteoglycan distribution in lesions of atherosclerosis depends on lesion severity, structural characteristics, and the proximity of platelet-derived growth factor and transforming growth factor-beta. American Journal of Pathology 152, 533546. Farr, C., Menzel, J., Seeberger, J., Schweigle, B., 1997. Clinical pharmacology and possible applications of hyaluronidase with reference to Hylase Dessau. Wiener Medizinische Wochenschrift 147, 347355. Fieber, C., Plug, R., Sleeman, J., Dall, P., Ponta, H., Hofmann, M., 1999. Characterisation of the murine gene encoding the intracellular hyaluronan receptor IHABP (RHAMM). Gene 226, 4150. Fieber, C., Baumann, P., Vallon, R., Termeer, C., Simon, J.C., Hofmann, M., Angel, P., Herrlich, P., Sleeman, J.P., 2003. Hyaluronan-oligosaccharides-induced transcription of metalloproteases. Journal of Cell Science 117, 359367. Figueiredo, F., Jones, G.M., Thouas, G.A., Trounson, A.O., 2002. The effect of extracellular matrix molecules on mouse preimplantation embryo development in vitro. Reproduction, Fertility and Development 14, 443451. Fitzgerald, T.J., Gannon, E.M., 1983. Further evidence for hyaluronidase activity of Treponema pallidum. Canadian Journal of Microbiology 29, 15071513. Flannery, C.R., Little, C.B., Hughes, C.E., Caterson, B., 1998. Expression and activity of articular cartilage hyaluronidases. Biochemical and Biophysical Research Communications 252, 824829. Fraser, J.R.E., Appelgren, L.E., Laurent, T.C., 1983. Tissue uptake of circulating hyaluronic acid. A whole body autoradiographic study. Cell and Tissue Research 233, 285293. Fraser, J.R., Laurent, T.C., Laurent, U.B., 1997. Hyaluronan: its nature, distribution, functions and turnover. Journal of Internal Medicine 242, 27S33S. Frost, G.I., Csoka, T., Stern, R., 1996. The hyaluronidases: a chemical, biological and clinical overview. Trends in Glycoscience and Glycotechnology 8, 419434.
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 splitting enzymes. Archives of Pharmaceutical Chemistry and Life Sciences 339, 313318. Hoffman, A.S., 2001. Hydrogels for biomedical applications. Annals of the New York Academy of Sciences 944, 6273. Horton, M.R., McKee, C.M., Bao, C., Liao, F., Farber, J.M., Hodge-DuFour, J., Purae, E., Oliver, B.L., Wright, T.M., Noble, P.W., 1998. Hyaluronan fragments synergize with interferon-gamma to induce the CXC chemokines mig and interferon-inducible protein-10 in mouse macrophages. Journal of Biological Chemistry 273, 3508835094. Horton, M.R., Shapiro, S., Bao, C., Lowenstein, C.J., Noble, P.W., 1999. Induction and regulation of macrophage metalloprotease by hyaluronan fragments in mouse macrophages. Journal of Immunology 162, 41714176. Hotez, P.J., Narasimhan, S., Haggerty, J., Milstone, L., Bhopale, V., Schad, G.A., Richards, F.F., 1992. Hyaluronidase from infective Ancylostoma hookworm larva and its possible function as a virulence factor in tissue invasion and in cutaneous larva miigrans. Infection and Immunity 60, 10181023. Hou, S., Xu, Q., Tian, W., Cui, F., Cai, Q., Ma, J., Lee, I.S., 2005. The repair of brain lesion by implantation of hyaluronic acid hydrogels modified with laminin. Journal of Neuroscience Methods 148, 6070. Hynes, W., Ferretti, J., 1989. Sequence analysis and expression in Escherichia coli of the hyaluronidase gene of Streptococcus pyogenes bacteriophage H4489A. Infection and Immunity 57, 533539. Hynes, W.L., Walton, S.L., 2000. Hyaluronidases of Gram-positive bacteria. FEMS Microbiology Letters 183, 201207. Iacob, S., Knudson, C.B., 2006. Hyaluronan fragments activate nitric oxide synthase and the production of nitric oxide by articular chondrocytes. International Journal of Biochemistry and Cell Biology 38, 123133. Isoyama, T., Thwaites, D., Selzer, M.G., Carey, R.I., Barbucci, R., Lokeshwar, V.B., 2006. Differential selectivity of hyaluronidase inhibitors toward acidic and basic hyaluronidases. Glycobiology 16, 1121. Itano, N., Sawai, T., Yoshida, M., Lenas, P., Yamada, Y., Imagawa, M., Shinomura, T., Hamaguchi, M., Yoshida, Y., Ohnuki, Y., Miyauchi, S., Spicer, A.P., McDonald, J.A., Kimata, K., 1999. Three isoforms of mammalian hyaluronan synthases have distinct enzymatic properties. Journal of Biological Chemistry 274, 2508525092. Itano, N., Sawai, T., Atsumi, F., Miyaishi, O., Taniguchi, S., Kannagi, R., Hamaguchi, M., Kimata, K., 2004. Selective expression and functional characteristics of three mammalian hyaluronan synthases in oncogenic malignant transformation. Journal of Biological Chemistry 279, 1867918687. Jackson, D.G., 2003. The lymphatics revisited: new perspectives from the hyaluronan receptor LYVE-1. Trends in Cardiovascular Medicine 13, 17. Jackson, D.G., 2004. Biology of the lymphatic marker LYVE-1 and applications in research into lymphatic trafficking and lymphangiogenesis. Acta Pathologica, Microbiologica et Immunologica Scandinavica 112, 526538. Jackson, D.G., Prevo, R., Clasper, S., Banerji, S., 2001. LYVE-1, the lymphatic system and tumor lymphangiogenesis. Trends in Immunology 22, 317321. Jang, G., Lee, B.C., Kang, S.K., Hwang, W.S., 2003. Effect of glycosaminoglycans on the preimplantation development of embryos derived from in vitro fertilization and somatic cell nuclear transfer. Reproduction, Fertility and Development 15, 179185. Jedrzejas, M.J., 2000. Structural and functional comparison of polysaccharidedegrading enzymes. Critical Reviews in Biochemistry and Molecular Biology 35, 221251. Jedrzejas, M.J., 2001. Pneumococcal virulence factors: structure and function. Microbiology and Molecular Biology Reviews 65, 187207. Jedrzejas, M.J., 2004. Extracellular virulence factors of Streptococcus pneumoniae. Frontier in Bioscience 9, 891914. Jedrzejas, M.J., Stern, R., 2005. Structures of vertebrate hyaluronidases and their unique enzymatic mechanism of hydrolysis. Proteins (Structure Function and Bioinformatics) 61, 227238. Jedrzejas, M.J., Mello, L.V., de Groot, B.L., Li, S., 2002. Mechanism of hyaluronan degradation by Streptococcus pneumoniae hyaluronate lyase. Structures of complexes with the substrate. Journal of Biological Chemistry 277, 2828728297. Ji, Y., Ghosh, K., Shu, X.Z., Li, B., Sokolov, J.C., Prestwich, G.D., Clark, R.A.F., Rafailovich, M.H., 2006. Electrospun three-dimensional hyaluronic acid nanofibrous scaffolds. Biomaterials 27, 37823792.
1939
Jiang, D., Liang, J., Fan, J., Yu, S., Chen, S., Luo, Y., Prestwich, G.D., Mascarenhas, M.M., Garg, H.G., Quinn, D.A., Homer, R.J., Goldstein, D.R., Bucala, R., Lee, P.J., Medzhitov, R., Noble, P.W., 2005. Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nature Medicine 11, 11731179. Joddar, B., Ramamurthi, A., 2006. Fragment size- and dose-specific effects of hyaluronan on matrix synthesis by vascular smooth muscle cells. Biomaterials 27, 29943004. Joyce, C.L., Mack, S.R., Anderson, R.A., Zaneveld, L.J.D., 1986. Effect of hyaluronidase, -glucuronidase and -N-acetylglucosaminidase inhibitors on sperm penetration of the mouse oocyte. Biology of Reproduction 35, 336346. Kakegawa, H., Mitsuo, N., Matsumoto, H., Satoh, T., Akagi, M., Tasaka, K., 1985. Hyaluronidase-inhibitory and anti-allergic activities of the photoirradiated products of tranilast. Chemical and Pharmaceutical Bulletin (Tokyo) 33, 37383744. Kakegawa, H., Matsumoto, H., Satoh, T., 1988. Inhibitory effects of hydrangenol derivatives on the activation of hyaluronidase and their antiallergic activities. Planta Medica 54, 385389. Kato, Y., Onishi, H., Machida, Y., 2005. Contribution of chitosan and its derivatives to cancer chemotherapy. In Vivo 19, 301310. Kemparaju, K., Girish, K.S., 2006. Snake venom hyaluronidase: a therapeutic target. Cell Biochemistry and Function 24, 712. Khanum, S.A., Murari, S.K., Vishwanath, B.S., Shashikanth, S., 2005. Synthesis of benzoyl phenyl benzoates as effective inhibitors for phospholipase A2 and hyaluronidase enzymes. Bioorganic & Medicinal Chemistry Letters 15, 41004104. Kim, E., Baba, D., Kimura, M., Yamashita, M., Kashiwabara, S., Baba, T., 2005. Identification of a hyaluronidase, Hyal5, involved in penetration of mouse sperm through cumulus mass. Proceedings of the National Academy of Sciences of the United States of America 102, 404410. Kirwan, J., 2001. Is there a place for intra-articular hyaluronate in osteoarthritis of the knee? Knee 8, 93101. Klocker, J., Sabitzer, H., Raunik, W., Wieser, S., Schumer, J., 1995. Combined application of cisplatin, vindesine, hyaluronidase and radiation for treatment of advanced squamous cell carcinoma of the head and neck. American Journal of Clinical Oncology 8, 425428. Knudson, C.B., 2003. Hyaluronan and CD44: strategic players for cellmatrix interactions during chondrogenesis and matrix assembly. Birth Defects Research (Part C) Embryo Today 69, 174196. Knudson, C.B., Knudson, W., 2004. Hyaluronan and CD44: modulators of chondrocyte metabolism. Clinical Orthopaedics and Related Research 427S, S152S162. Knudson, W., Chow, G., Knudson, C.B., 2002. CD44-mediated uptake and degradation of hyaluronan. Matrix Biology 21, 1523. Kolarich, D., Leonard, R., Hemmer, W., Altmann, F., 2005. The N-glycans of yellow jacket venom hyaluronidases and the protein sequence of its isoform in Vespula vulgaris. FEBS Journal 272, 51825190. Kolarova, M., 1975. Hosttumor relationship XXXIII. Inhibitor of hyaluronidase in blood serum of cancer patients. Neoplasma 22, 435439. Kostyukova, N.N., Volkova, M.O., Ivanova, V.V., Kvetnaya, A.S., 1995. A study of pathogenic factors of Streptococcus pneumoniae strains causing meningitis. FEMS Immunology and Medical Microbiology 10, 133137. Kreil, G., 1995. Hyaluronidasesa group of neglected enzymes. Protein Science 4, 16661669. Kudo, K., Tu, A.T., 2001. Characterization of hyaluronidase isolated from Agkistrodon contortrix contortrix (Southern Copperhead) venom. Archives of Biochemistry and Biophysics 386, 154162. Kuppusamy, U.R., Das, N.P., 1991. Inhibitory effects of flavonoids on several venom hyaluronidases. Experientia 47, 11962000. Lapcik, L., Lapcik, L., De Smaedt, S., Demester, J., Chabrecek, P., 1998. Hyaluronan: preparation, structure, properties, and applications. Chemical Reviews 98, 26632684. Larsen, N.E., Balazs, E.A., 1991. Drug delivery systems using hyaluronan and its derivatives. Advanced Drug Delivery Reviews 7, 279293. Laurent, T.C., 1970. The structure of hyaluronic acid. In: Balazs, E.A. (Ed.), Chemistry and Molecular Biology of the Intercellular Matrix. Academic Press, New York, pp. 703732.
1940
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Markovic-Housley, Z., Miglierini, G., Soldatova, L., Rizkallah, P.J., Muller, U., Schirmer, T., 2000. Crystal structure of hyaluronidase, a major allergen of bee venom. Structure 8, 10251035. Matsushita, O., Okabe, A., 2001. Clostridial hydrolytic enzymes degrading extracellular components. Toxicon 39, 17691780. McDonald, J.A., Camenisch, T.D., 2002. Hyaluronan: genetic insights into the complex biology of a simple polysaccharide. Glycoconjugate Journal 19, 331339. McKee, C.M., Penno, M.B., Cowman, M., Burdick, M.D., Strieter, R.M., Bao, C., Noble, P.W., 1996. Hyaluronan fragments induce chemokine gene expression in alveolar macrophages. The role of HA size and CD44. Journal of Clinical Investigation 15, 24032413. Melo, P.A., Ownby, C.L., 1999. Ability of wedelolactone, heparin, and parabromophenayl bromide to antagonize the myotoxic effects of two crotaline venoms and their PLA2 myotoxins. Toxicon 37, 199215. Meyer, K., 1971. Hyaluronidases. In: Boyer, P.D. (Ed.), The Enzymes. Academic press, New York, pp. 307320. Meyer, K., Palmer, J.W., 1934. The polysaccharide of the vitreous humor. Journal of Biological Chemistry 107, 629634. Miller, J.A., Ferguson, R.L., Powers, D.L., Burns, J.W., Shalaby, S.W., 1997. Efficacy of hyaluronic acid/nonsteroidal anti-inflammatory drug systems in preventing postsurgical tendon adhesion. Journal of Biomedical Material Research 38, 2533. Miller, K.A., Shao, M., Martin-Deleon, P.A., 2007. Hyalp1 in murine sperm function: evidence for unique and overlapping functions with other reproductive hyaluronidases. Journal of Andrology 28, 6776. Milner, C.M., Day, A.J., 2003. TSG-6: a multifunctional protein associated with inflammation. Journal of Cell Science 116, 18631873. Milner, C.M., Higman, V.A., Day, A.J., 2006. TSG-6: a pluripotent inflammatory mediator? Biochemical Society Transactions 34, 446450. Mio, K., Stern, R., 2002. Inhibitors of the hyaluronidases. Matrix Biology 21, 3137. Mio, K., Carrette, O., Maibach, H.I., Stern, R., 2000. Evidence that the serum inhibitor of hyaluronidase may be a member of the inter-alpha-inhibitor family. Journal of Biological Chemistry 275, 3241332421. Miyazaki, T., Miyauchi, S., Nakamura, T., Takeshita, S., Horie, K., 1996. The effect of sodium hyaluronate on the growth of rabbit cornea epithelial cells in vitro. Journal of Ocular Pharmacology and Therapeutics 12, 409415. Moreland, L.W., 2003. Intra-articular hyaluronan (hyaluronic acid) and hylans for the treatment of osteoarthritis: mechanisms of action. Arthritis Research and Therapy 5, 5467. Morey, S.S., Kiran, K.M., Gadag, J.R., 2006. Purification and properties of hyaluronidase from Palamneus gravimanus (Indian black scorpion) venom. Toxicon 47, 188195. Morimoto, K., Yamaguchi, H., Iwakura, Y., Morisaka, K., Ohashi, Y., Nakai, Y., 1991. Effects of viscous hyaluronatesodium solutions on the nasal absorption of vasopressin and an analog. Pharmacological Research 8, 471474. Mors, W.B., Nascimento, M.C., Pereira, B.M., Pereira, N.A., 2000. Plant natural products active against snake bitethe molecular approach. Phytochemistry 55, 627642. Muckenschnabel, I., Bernhardt, G., Spruss, T., Buschauer, A., 1997. Hyaluronidase pretreatment produces selective melphalan enrichment in malignant melanoma in nude mice. Cancer Chemotherapy and Pharmacology 38, 8894. Muckenschnabel, I., Bernhardt, G., Spruss, T., Buschauer, A., 1998. Pharmacokinetics and tissue distribution of bovine testicular hyaluronidase and vinblastine in mice: an attempt to optimize the mode of adjuvant hyaluronidase administration in cancer chemotherapy. Cancer Letters 131, 7184. Murai, T., Miyazaki, Y., Nishinakamura, H., Sugahara, K.N., Miyauchi, T., Sako, Y., Yanagida, T., Miyasaka, M., 2004. Engagement of CD44 promotes Rac activation and CD44 cleavage during tumor cell migration. Journal of Biological Chemistry 279, 45414550. Nagaraju, S., Mahadeshwaraswamy, Y.H., Girish, K.S., Kemparaju, K., 2006. Biochemical and pharmacological characterization of venom from the spiders H. partita, H. aglenoides and H. mahabaleshwarensis tikadar and malhotra. Comparative Biochemistry and Physiology C 149, 19.
Laurent, T.C., Fraser, J.R., 1986. The properties and turnover of hyaluronan. CIBA Foundation Symposium 124, 929. Laurent, T.C., Fraser, J.R., 1992. Hyaluronan. FASEB Journal 6, 23972404. Laurent, T.C., Laurent, U.B., Fraser, J.R., 1996. Serum hyaluronan as a disease marker. Annals of Medicine 28, 241253. Lee, J.Y., Spicer, A.P., 2000. Hyaluronan: a multifunctional, megadalton, stealth molecule. Current Opinion in Cell Biology 12, 581586. Lepidi, S., Grego, F., Vindigini, V., Zavan, B., Tobello, C., Deriu, G.P., Abatangelo, G., Cortivo, R., 2006. Hyaluronan biodegradable scaffold for small-caliber artery grafting: preliminary results in an animal model. European Journal of Vascular and Endovascular Surgery 32, 411417. Lepperdinger, G., Strobl, B., Kreil, G., 1998. HYAL2, a human gene expressed in many cells, encodes a lysosomal hyaluronidase with a novel type of specificity. Journal of Biological Chemistry 273, 2246622470. Lepperdinger, G., Mullegger, J., Kreil, G., 2001. HYAL2less active, but more versatile? Matrix Biology 20, 509514. Lesley, J., Hascall, V.C., Tammi, M., Hyrnan, R., 2000. Hyaluronan binding by cell surface CD44. Journal of Biological Chemistry 275, 2696726975. Li, H., Guo, L., Li, J.W., Liu, N., Qi, R., Liu, J., 2000a. Expression of hyaluronan receptors CD44 and RHAMM in stomach cancers: relevance with tumor progression. International Journal of Oncology 17, 927932. Li, S., Kelly, S.J., Lamani, E., Ferraroni, M., Jedrzejas, M.J., 2000b. Structural basis of hyaluronan degradation by Streptococcus pneumoniae hyaluronate lyase. EMBO Journal 19, 12281240. Liao, Y.H., 2005. Hyaluronan: pharmaceutical characterization and drug delivery. Drug Delivery 12, 327342. Lim, S.T., Martin, G.P., Berry, D.J., Brown, M.B., 2000. Preparation and evaluation of the in vitro drug release properties and mucoadhesion of novel microspheres of hyaluronic acid and chitosan. Journal of Controlled Release 66, 281292. Lim, S.T., Forbes, B., Berry, D.J., Martin, G.P., Brown, M.B., 2002. In vivo evaluation of novel hyaluronan/chitosan microparticulate delivery systems for the nasal delivery of gentamicin in rabbits. International Journal of Pharmacology 231, 7382. Lin, Y., Mahan, K., Lathrop, W.F., Myles, D.G., Primakoff, P., 1994. A hyaluronidase activity of the sperm plasma membrane protein PH-20 enables sperm to penetrate the cumulus cell layer surrounding the egg. Journal of Cell Biology 125, 11571163. Linhardt, R.J., Galliher, P.M., Cooney, C.L., 1986. Polysaccharide lyases. Applied Microbiology and Biotechnology 12, 135176. Lokeshwar, W.B., Schroeder, G.L., Carey, R.L., Soloway, M.S., Iida, N., 2002. Regulation of hyaluronidase activity by alternative mRNA splicing. Journal of Biological Chemistry 277, 3365433663. Liu, N., Gao, F., Han, Z., Xu, X., Underhill, C.B., Zhang, L., 2001. Hyaluronan synthase 3 overexpression promotes the growth of TSU prostate cancer cells. Cancer Research 61, 52075214. Lu, G., Kochoumian, L., King, T.P., 1995. Sequence identity and antigenic cross reactivity of white face hornet venom allergen, also a hyaluronidase, with other proteins. Journal of Biological Chemistry 270, 44574465. Luo, Y., Ziebell, M.R., Prestwich, G.D., 2000. A hyaluronic acid-taxol antitumor bioconjugate targeted to cancer cells. Biomacromolecules 1, 208218. Machiah, K.D., Girish, K.S., Gowda, T.V., 2006. A glycoprotein from a folk medicinal plant, Withania somnifera, inhibits hyaluronidase activity of snake venoms. Comparative Biochemistry and Physiology C 143, 158161. Mahoney, D.J., Mulloy, D.J., Forster, M.J., Blundell, C.D., Fries, E., Milner, C.M., Day, A.J., 2005. Characterization of the interaction between tumor necrosis factor-stimulated gene-6 and heparin: implications for the inhibition of plasmin in extracellular matrix microenvironments. Journal of Biological Chemistry 280, 2704427055. Makris, G., Wright, J.D., Ingham, E.I., Holland, K.T., 2004. The hyaluronate lyase of Staphylococcus aureusa virulence factor? Microbiology 150, 20052013. Maksimenko, A.V., Petrova, M.L., Tischenko, E.G., Schechilina, Y.V., 2001. Chemical modification of hyaluronidase regulates its inhibition by heparin. European Journal of Pharmacology and Biopharmacology 51, 3338. Manzel, E.J., Farr, C., 1988. Hyaluronidases and its substrate: biochemistry, biological activities and therapeutic uses. Cancer Letters 131, 311.
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Nazir, T., Martin, G.P., Brown, M.B., 2001. Dermal delivery of cyclosporin A entrapped liposomal gels-preformulation Franz cell diffusion studies using silastic membranes. Pharmacology Science 3, S1429. Newman, J.K., Berenson, G.S., Mathews, M.B., Goldwasser, E., Dorfman, A., 1955. The isolation of the non-specific hyaluronidase inhibitor of human blood. Journal of Biological Chemistry 217, 3141. Ng, H.C., Ranganathan, S., Chua, K.L., Khoo, H.E., 2005. Cloning and molecular characterization of the first aquatic hyaluronidase, SFHYA1, from the venom of stonefish (Synanceja horrida). Gene 346, 7181. Nicoll, S.B., Barak, O., Csoka, A.B., Bhatnagar, R.S., Stern, R., 2002. Hyaluronidases and CD44 undergo differential modulation during chondrogenesis. Biochemical and Biophysical Research Communications 292, 819825. Noble, P.W., 2002. Hyaluronan and its catabolic products in tissue injury and repair. Matrix Biology 21, 2529. Noble, P.W., Lake, F.R., Henson, P.M., Riches, D.W.H., 1993. Hyaluronate activation of CD44 induces insulin-like growth factor-2 expression by a tumor necrosis factor- dependent mechanism in murine macrophages. Journal of Clinical Investigation 91, 23682377. North, P.E., Kahn, T., Cordisco, M.R., Dadras, S.S., Detmar, M., Frieden, I.J., 2004. Multifocal lymphangioendotheliomatosis with thrombocytopenia: a newly recognized clinicopathological entity. Archives of Dermatology 140, 599606. Oettl, M., Hoechstetter, J., Asen, I., Bernhardt, G., Buschauer, A., 2003. Comparative characterization of bovine testicular hyaluronidase and a hyaluronate lyase from Streptococcus agalactiae in pharmaceutical preparations. European Journal of Pharamaceutical Sciences 18, 267277. Ohno, S., Im, H.J., Knudson, C.B., Knudson, W., 2005. Hyaluronan oligosaccharide-induced activation of transcription factors in bovine articular chondrocytes. Arthritis and Rheumatism 52, 800809. Okorukwu, O.N., Vercruysse, K.P., 2003. Effects of ascorbic acid and analogs on the activity of testicular hyaluronidase and hyaluronan lyase on hyaluronan. Journal of Enzyme Inhibition and Medicinal Chemistry 18, 377382. Paiva, P., Damme, M.V., Tellbach, M., Jones, R.L., Jobling, T., Salamonsen, L.A., 2005. Expression patterns of hyaluronan, hyaluronan synthases and hyaluronidases indicate a role for hyaluronan in the progression of endometrial cancer. Gynecologic Oncology 98, 193202. Palasz, A.T., Rodriguez-Martinez, H., Beltran-Brena, P., Perez-Garnelo, S., Martinez, M.F., Gutierrez-Adan, A., De la Fuente, J., 2006. Effects of hyaluronan, BSA, and serum on bovine embryo in vitro development, ultrastructure, and gene expression patterns. Molecular Reproduction and Development 73, 53455355. Peer, D., Florentin, A., Margalit, R., 2003. Hyaluronan is a key component in cryoprotection and formulation of targeted unilamellar liposomes. Biochimica et Biophysica Acta. Biomembranes 1612, 7682. Pessini, A.C., Takao, T.T., Cavalheiro, E.C., Vichnewski, W., Sampaio, S.V., Giglio, J.R., Arantes, E.C., 2001. A hyaluronidase from Tityus serrulatus scorpion venom isolation characterization and inhibition by flavonoids. Toxicon 39, 14951504. Peterson, R.M., Yu, Q., Stamenkovic, I., Toole, B.P., 2000. Perturbation of hyaluronan interactions by soluble CD44 inhibits growth of murine mammary carcinoma cells in ascites. American Journal of Pathology 156, 21592167. Poh, C.H., Yuen, R., Chung, M.C.M., Khoo, H.E., 1992. Purification and partial characterization of hyaluronidase from stonefish (Synanceja horrida) venom. Comparative Biochemistry and Physiology 101B, 159163. Politz, O., Gratchev, A., McCourt, P.A., Schledzewski, K., Guillot, P., Johansson, S., Svineng, G., Franke, P., Kannicht, C., Kzhyshkowska, J., Longati, P., Velten, F.W., Goerdt, S., 2002. Stabilin-1 and -2 constitute a novel family of fasciclin-like hyaluronan receptor homologues. Biochemical Journal 362, 155164. Ponta, H., Wainwright, D., Herrlich, P., 1998. The CD44 protein family. International Journal of Biochemistry and Cell Biology 30, 299305. Ponta, H., Shernan, L., Herrlich, P., 2003. CD44: from adhesion molecules to signaling regulators. Nature Reviews. Molecular Cell Biology 4, 3345. Primakoff, P., Hyatt, H., Myles, D.G., 1985. A role for the migrating sperm surface antigen PH-20 in guinea pig sperm binding to the egg zona pellucida. Journal of Cell Biology 101, 22392244.
1941
Rabea, E.I., Badawy, M.E., Stevens, C.V., Smagghe, G., Steurbaut, W., 2003. Chitosan as antimicrobial agent: applications and mode of action. Biomacromolecules 4, 14571465. Ramamurthi, A., Vesely, I., 2002. Smooth muscle cell adhesion on crosslinked hyaluronan gels. Journal of Biomedical Material Research 60, 195205. Ramamurthi, A., Vesely, I., 2003. Ultraviolet light-induced modification of crosslinked hyaluronan gels. Journal of Biomedical Materials Research (Part A) 66, 317329. Ramamurthi, A., Vesely, I., 2005. Evaluation of the matrix-synthesis potential of crosslinked hyaluronan gels for tissue engineering of aortic heart valves. Biomaterials 26, 9991010. Ramanaiah, M., Parthasarathy, P.R., Venkaiah, B., 1990. Isoaltion and characterisation of hyaluronidase from scorpion (Heterometrus fulvipus) venom. Biochemistry International 20, 301310. Rash, L.D., Hodgson, W.C., 2002. Pharmacology and biochemistry of spider venoms. Toxicon 40, 225254. Rauch, U., Karthikeyan, L., Maurel, P., Margolis, R.U., Margolis, R.K., 1992. Cloning and primary structure of neurocan, a developmentally regulated aggregating chondroitin sulfate proteoglycan of brain. Journal of Biological Chemistry 267, 1953619547. Reitinger, S., Laschober, G.T., Fehrer, C., Greiderer, B., Lepperdinger, G., 2007. Mouse testicular hyaluronidase-like proteins, SPAM1 and Hyall5 but not Hyalp1 degrade hyaluronan. Biochemical Journal 401, 7985. Roden, L., Campbell, P., Fraser, J.R., Laurent, T.C., Pertoft, H., Thompson, J.N., 1989. Enzymatic pathways of hyaluronan catabolism. CIBA Foundation Symposium 143, 6086. Rossler, A., Hinghofer-Szalkay, H., 2002. Hyaluronan fragments: an information-carrying system? Hormone and Metabolic Research 35, 6768. Salmen, S., Hoechstetter, J., Kasbauer, C., Paper, D.H., Bernhardt, G., Buschauer, A., 2005. Sulphated oligosaccharides as inhibitors of hyaluronidases from bovine testis, bee venom and Streptococcus agalactiae. Planta Medica 71, 727732. Savani, R.C., Cao, G., Pooler, P.M., Zaman, A., Zhou, Z., DeLisser, H.M., 2001. Differential involvement of the hyaluronan (HA) receptors CD44 and receptor for HA-mediated motility in endothelial cell function and angiogenesis. Journal of Biological Chemistry 276, 3677036778. Scott, J.E., Heatley, F., 2002. Biological properties of hyaluronan in aqueous solution are controlled and sequestered by reversible tertiary structures, defined by NMR spectroscopy. Biomacromolecules 3, 547553. Senel, S., McClure, S.J., 2004. Potential applications of chitosan in veterinary medicine. Advanced Drug Delivery Reviews 56, 14671480. Seyfried, N.T., Day, A.J., Almond, A., 2006. Experimental evidence for all-ornone co-operative interactions between the G1-domain of versican and multivalent hyaluronan oligosaccharides. Matrix Biology 25, 1419. Shi, Y., Ramamurthi, A., Vesely, I., 2002. Towards tissue engineering of a composite aortic valve. Biomedical Sciences Instrumentation 38, 3540. Shimizu, M.T., Jorge, A.O.C., Unterkircher, C.S., Fantinato, V., Paula, C.R., 1995. Hyaluronidse and chondroitin sulphatase production by different species of Candida. Journal of Medical and Veterinary Mycology 33, 2731. Simon, A., Safran, A., Revel, A., Aizenman, E., Reubinoff, B., Porat-Katz, A., Lewin, A., Laufer, N., 2003. Hyaluronic acid can successfully replace albumin as the sole macromolecule in a human embryo transfer medium. Fertility and Sterility 79, 14341438. Simpson, M.A., Wilson, C.M., McCarthy, J.B., 2002. Inhibition of prostate tumor cell hyaluronan synthesis impairs subcutaneous growth and vascularization in immunocompromised mice. American Journal of Pathology 161, 849857. Singla, A.K., Chawla, M., 2001. Chitosan: some pharmaceutical and biological aspectsan update. Journal of Pharmacy and Pharmacology 53, 10471067. Snively, G.G., Glick, D., 1950. Mucolytic enzyme systems. X. Serum hyaluronidase inhibitor in liver disease. Journal of Clinical Investigation 29, 10871090. Spellerberg, B., 2000. Pathogenesis of neonatal Streptococcus agalactiae infections. Microbes and Infection 2, 17331742. Spicer, A.P., McDonald, J.A., 1998. Characterization and molecular evolution of a vertebrate hyaluronan synthase gene family. Journal of Biological Chemistry 273, 19231932.
1942
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Tu, A.T., Hendon, R.R., 1983. Characterization of lizard venom hyaluronidase and evidence for its action as a spreading factor. Comparative Biochemistry and Physiology. Part B, Biochemistry & Molecular Biology 76, 377383. Turley, E.A., Noble, P.W., Bourguignon, L.Y.W., 2002. Signaling properties of hyaluronan receptors. Journal of Biological Chemistry 277, 45894592. Uchiyama, H., Dobashi, Y., Ohkouchi, K., Nagasawa, K., 1990. Chemical change involved in the oxidative reductive depolymerization of hyaluronic acid. Journal of Biological Chemistry 265, 77537759. Ushanandini, S., Nagaraju, S., Harish kumar, K., Vedavathi, M., Deepa, K.M., Kemparaju, K., Vishwanath, B.S., Gowda, T.V., Girish, K.S., 2006. The anti snake venom properties of Tamarindus indica (Leguminosae) seed extract. Phytotherapy Research 20, 851858. Uthman, I., Raynauld, J.P., Haraoui, B., 2003. Intra-articular therapy in osteoarthritis. Postgraduate Medical Journal 79, 449453. Vercruysse, K.P., Prestwich, G.D., 1998. Hyaluronate derivatives in drug delivery. Critical Reviews in Therapeutic Drug Carrier Systems 15, 513555. Vercruysse, K.P., Ziebell, M.R., Prestwich, G.D., 1999. Control of enzymatic degradation of hyaluronan by divalent cations. Carbohydrate Research 318, 2637. Vigdorovich, V., Strong, R.K., Miller, A.D., 2005. Expression and characterization of a soluble, active form of the Jaagsiekte sheep retrovirus receptor, Hyal2. Journal of Virology 79, 7986. Ward, J.A., Huang, L., Guo, H., Ghatak, S., Toole, B.P., 2003. Perturbation of hyaluronan interactions inhibits malignant properties of glioma cells. American Journal of Pathology 162, 14031409. Weigel, P.H., Hascall, V.C., Tammi, M., 1997. Hyaluronan synthases. Journal of Biological Chemistry 272, 1399714000. Weissman, B., Meyer, K.J., 1954. American Chemical Society 76, 17531757. West, D.C., Hampson, I.N., Arnold, F., Kumar, S., 1985. Angiogenesis induced by degradation products of hyaluronic acid. Science 228, 13241326. Wight, T.N., Merrilees, M.J., 2004. Proteoglycans in atherosclerosis and restenosis: key roles for versican. Circulation Research 94, 11581167. Wolf, R.A., Glogar, D., Chaung, L.Y., Garrett, P.E., Ertl, G., Tumas, J., Braunwald, E., Kloner, R.A., Feldstein, M.L., Muller, J.E., 1984. Heparin inhibits bovine testicular hyaluronidase activity in myocardium of dogs with coronary artery occlusion. American Journal of Cardiology 53, 941944. Wolf, J.E., Taylor, J.R., Tschen, E., Kang, S.W., 2001. Topical 3.0% diclofenac in 2.5% hyaluronan gel in the treatment of actinic keratoses. International Journal of Dermatology 40, 709713. Xu, X., Ito, T., Tawada, A., Maeda, H., Yamanokuchi, H., Isahara, K., Yoshida, K., Uchiyama, Y., Asari, A., 2002. Effect of hyaluronan oligosaccharides on the expression of heat shock protein 72. Journal of Biological Chemistry 277, 1730817314. Yamazaki, K., Fukuda, K., Matsukawa, M., Hara, F., Yoshida, K., Akagi, M., Munakata, H., Hamanishi, C., 2003. Reactive oxygen species depolymerize hyaluronan: involvement of the hydroxyl radical. Pathophysiology 9, 215220. Yingprasertchai, S., Bunyasrisawat, S., Ratanabanangkoon, K., 2003. Hyaluronidase inhibitors (sodium cromoglycate and sodium auro-thiomalate) reduce the local tissue damage and prolong the survival time of mice injected with Naja kaouthia and Calloselasma rhodostoma venoms. Toxicon 42, 635646. Yun, Y.H., Goetz, D.J., Yellen, P., Chen, W., 2004. Hyaluronan microspheres for sustained gene delivery and site-specific targeting. Biomaterials 25, 147157. Zahalka, M.A., Okon, E., Gosslar, U., Holzmann, B., Naor, D., 1995. Lymph node (but not spleen) invasion by murine lymphoma is both CD44- and hyaluronate-dependent. Journal of Immunology 154, 53455355. Zaneveld, L.J.D., Anderson, R.A., Diao, X.-H., Walker, D.P., Chany II, C., Feathergill, K., Doncel, G., Cooper, M.D., Herold, B., 2002. Use of mandelic acid condensation polymer (SAMMA), a new antimicrobial contraceptive agent, for vaginal prophylaxis. Fertility and Sterility 78, 11071115. Zhang, H., Martin-DeLeon, P.A., 2003. Mouse Spam1 (PH-20) is a multifunctional protein: evidence for its expression in the female reproductive tract. Biology of Reproduction 69, 446454.
Spicer, A.P., Tien, J.Y.L., 2004. Hyaluronan and morphogenesis. Birth Defects Research C Embryo Today 72, 89108. Spicer, A.P., Joo, A., Bowling Jr., R.A., 2003. A hyaluronan binding link protein gene family whose members are physically linked adjacent to chondroitin sulfate proteoglycan core proteins genes: the missing links. Journal of Biological Chemistry 278, 2108321091. Spruss, T., Bernhardt, G., Schnenberger, H., Schiess, W., 1995. Hyaluronidase significantly enhances the efficacy of regional vinblastine chemotherapy of malignant melanoma. Journal of Cancer Research and Clinical Oncology 121, 193202. Stern, R., 2003. Devising a pathway for hyaluronan catabolism: are we there yet? Glycobiology 13, 105R115R. Stern, R., 2004. Hyaluronan catabolism: a new metabolic pathway. European Journal of Cell Biology 83, 317325. Stern, R., Jedrzejas, M.J., 2006. Hyaluronidases: their genomics, structures, and mechanisms of action. Chemical Reviews 106, 818839. Sting, R., Schaufuss, P., Blobel, H., 1990. Isolation and characterization of hyaluronidases from Streptococcus dysgalactiae, S. zooepidemicus and S. equi. Zentralblatt fur Bakteriologie 272, 276282. Surini, S., Akiyama, H., Morishita, M., Takayama, K., Nagai, T., 2003. Polyion complex of chitosan and sodium hyaluronate as an implant device for insulin delivery. STP Pharma Sciences 13, 265268. Sutherland, I.W., 1995. Polysaccharide lyases. FEMS Microbiology Reviews 16, 323347. Suzuki, K., Terasaki, Y., Uyeda, M., 2002. Inhibition of hyaluronidase and chondroitinases by fatty acids. Journal of Enzyme Inhibition and Medicinal Chemistry 17, 183186. Szary, S.H., Kowalczyk-Bronisz, Gieldanowski, J., 1975. Indomethacin as inhibitor of hyaluronidase. Archivum Immunologiae et Therapiae Experimentalis (Warszawa) 23, 131134. Takahashi, Y., Li, L., Kamiryo, M., Asteriou, T., Moustakas, A., Yamashita, H., Heldin, P., 2005. Hyaluronan fragments induce endothelial cell differentiation in a CD44 and CXCL1/GRO1-dependent manner. Journal of Biological Chemistry 280, 2419524204. Tammi, M.I., Tammi, R., 2006. Hyaluronan in the Epidermis. http://www. glycoforum.gr.jp/science/hyaluronan/hyaluronanE.html. Tammi, M.I., Day, A.J., Turley, E.A., 2002. Hyaluronan and homeostasis: a balancing act. Journal of Biological Chemistry 277, 45814584. Taylor, K.R., Gallo, R.L., 2006. Glycosaminoglycans and their proteoglycans: host-associated molecular patterns for initiation and modulation of inflammation. FASEB Journal 20, 922. Taylor, K.R., Trowbridge, J.M., Rudisill, J.A., Termeer, C.C., Simon, J.C., Gallo, R.L., 2004. Hyaluronan fragments stimulate endothelial recognition of injury through TLR4. Journal of Biological Chemistry 279, 1707917084. Termeer, C., Benedix, F., Sleeman, J., Fieber, C., Voith, U., Ahrens, T., Miyake, K., Freudenberg, M., Galanos, C., Simon, J.C., 2002. Oligosaccharides of hyaluronan activate dendritic cells via toll-like receptor 4. Journal of Experimental Medicine 195, 99111. Termeer, C., Sleeman, J.P., Simon, J.C., 2003. Hyaluronanmagic glue for the regulation of the immune response? Trends in Immunology 24, 112114. Thorne, R.F., Legg, J.W., Isacke, C.M., 2004. The role of the CD44 transmembrane and cytoplasmic domains in coordinating adhesive and signaling events. Journal of Cell Science 117, 373380. Toida, T., Ogita, Y., Suzuki, A., Toyoda, H., Imanari, T., 1999. Inhibition of hyaluronidase by fully O-sulfonated glycosaminoglycans. Archives of Biochemistry and Biophysics 370, 233241. Tonnesen, H.H., 1989. Studies on curcumin and curcuminoids. XIV. Effect of curcumin on hyaluronic acid degradation in vitro. International Journal of Pharmacology 50, 9195. Toole, B.P., 2002. Hyaluronan promotes the malignant phenotype. Glycobiology 12, 37R42R. Toole, B.P., 2004. Hyaluronan: from extracellular glue to pericellular cue. Nature Reviews. Cancer 4, 528539. Toole, B.P., Hascall, V.C., 2002. Hyaluronan and tumor growth. American Journal of Pathology 161, 745747. Toole, B.P., Wight, T.N., Tammi, M., 2002. Hyaluronancell interactions in cancer and vascular disease. Journal of Biological Chemistry 277, 45934596.
K.S. Girish, K. Kemparaju / Life Sciences 80 (2007) 19211943 Zhang, S., Chang, M.C., Zylka, D., Turley, S., Harrison, R., Turley, E.A., 1998. The hyaluronan receptor RHAMM regulates extracellular-regulated kinase. Journal of Biological Chemistry 273, 1134211348. Zhang, H., Shertok, S., Miller, K., Taylor, L., Martin-DeLeon, P.A., 2005. Sperm dysfunction in the Rb (6.16)-and Rb (6.15)- bearing mice revisited: involvement of Hyalp1 and Hyal5. Molecular Reproduction and Development 72, 404410.
1943
Zheng, Y., Deng, X., Zhao, Y., Martin-DeLeon, P.A., 2001. SPAM1 (PH-20) mutations and sperm dysfunction in mice with the Rb (6.16) or Rb (6.15) translocation. Biology of Reproduction 64, 17301838. Zhu, D., Bourguignon, L.Y., 2000. Interaction between CD44 and the repeat domain of ankyrin promotes hyaluronic acid mediated ovarian tumor cell migration. Journal of Cellular Physiology 183, 182195.
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- An Automated Design Framework For Multicellular Recombinase LogicDokumen7 halamanAn Automated Design Framework For Multicellular Recombinase Logicalessandro8265Belum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Technical Aspects of The Production and Growth of Hybridomas PDFDokumen112 halamanTechnical Aspects of The Production and Growth of Hybridomas PDFalessandro8265Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- How To Select The Best Secondary Antibody - Biomol Blog - Resources - Biomol GMBH - Life Science ShopDokumen3 halamanHow To Select The Best Secondary Antibody - Biomol Blog - Resources - Biomol GMBH - Life Science Shopalessandro8265Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- US20080300160A1 Patent Decontaminant SolutionDokumen32 halamanUS20080300160A1 Patent Decontaminant Solutionalessandro8265Belum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- BioTechniques Molecular Biology Techniques Forums - View Topic - More Info On Home Recipe For RNase Zap Solution PDFDokumen1 halamanBioTechniques Molecular Biology Techniques Forums - View Topic - More Info On Home Recipe For RNase Zap Solution PDFalessandro8265Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Polyvinylsulfonic Acid A Low Cost RNase Inhibitor For Enhanced RNA Preservation and Cell Free Protein TranslationDokumen9 halamanPolyvinylsulfonic Acid A Low Cost RNase Inhibitor For Enhanced RNA Preservation and Cell Free Protein Translationalessandro8265Belum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Linking High Throughput Cell Culture, Multivariate Analysis and Economics For More Effective Process IntegrationDokumen229 halamanLinking High Throughput Cell Culture, Multivariate Analysis and Economics For More Effective Process Integrationalessandro8265Belum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Production of Ant Proteins and Monoclonal Antibodies - Techno-Economical Evaluation of The Production MethodsDokumen117 halamanProduction of Ant Proteins and Monoclonal Antibodies - Techno-Economical Evaluation of The Production Methodsricky_connollyBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- How To Properly Clean Laboratory GlasswareDokumen3 halamanHow To Properly Clean Laboratory Glasswarealessandro8265Belum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- PatentDokumen17 halamanPatentalessandro8265Belum ada peringkat
- Antibody PurificationDokumen162 halamanAntibody PurificationkostrenarijekaBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- G Tran Series Pirani Gauge Box UnitDokumen2 halamanG Tran Series Pirani Gauge Box Unitalessandro8265Belum ada peringkat
- How To Properly Clean Laboratory GlasswareDokumen3 halamanHow To Properly Clean Laboratory Glasswarealessandro8265Belum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Comparison of Real-Time SYBR Green Dengue Assay With Real-Time Taqman RT-PCR Dengue Assay and The Conventional Nested PCR For Diagnosis of Primary and Secondary Dengue Infection PDFDokumen16 halamanComparison of Real-Time SYBR Green Dengue Assay With Real-Time Taqman RT-PCR Dengue Assay and The Conventional Nested PCR For Diagnosis of Primary and Secondary Dengue Infection PDFalessandro8265Belum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Delphi - Delphi Component Writer's Guide - Delphi For WindowsDokumen163 halamanDelphi - Delphi Component Writer's Guide - Delphi For WindowsjuanmdqBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- An Example Calculation To Aid The Adjustment and Testing of The Protecting Corona-Rings in A Specific HV Probe PDFDokumen3 halamanAn Example Calculation To Aid The Adjustment and Testing of The Protecting Corona-Rings in A Specific HV Probe PDFalessandro8265Belum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Build Gel BoxDokumen15 halamanBuild Gel BoxJorge Luis Castaño MartinezBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Application Note 171-1Dokumen4 halamanApplication Note 171-1alessandro8265Belum ada peringkat
- Basics of High Voltage Probe DesignDokumen14 halamanBasics of High Voltage Probe DesignAmol LandgeBelum ada peringkat
- Novel Absorption Detection Techniques For Capillary Electrophores PDFDokumen169 halamanNovel Absorption Detection Techniques For Capillary Electrophores PDFalessandro8265Belum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- HP 8405A Schematic Diagrams04Dokumen1 halamanHP 8405A Schematic Diagrams04alessandro8265Belum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Boostrap OP AmpsDokumen8 halamanBoostrap OP AmpsLakin OjekunleBelum ada peringkat
- Instruction Manual: MillivoltmeterDokumen51 halamanInstruction Manual: Millivoltmeteralessandro8265100% (1)
- Pirani GaugeDokumen4 halamanPirani Gaugealessandro8265Belum ada peringkat
- A Simple Pirani GaugeDokumen5 halamanA Simple Pirani Gaugealessandro8265Belum ada peringkat
- 1362 Uhf OscDokumen28 halaman1362 Uhf Oscalessandro8265Belum ada peringkat
- 00400-HP Voltmeter Service ManualDokumen44 halaman00400-HP Voltmeter Service Manualalessandro8265Belum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- TcgaugeDokumen11 halamanTcgaugealessandro8265Belum ada peringkat
- Building A Thermocouple Vacuum GaugeDokumen8 halamanBuilding A Thermocouple Vacuum Gaugealessandro8265Belum ada peringkat
- (Medicine and Biomedical Sciences in Modern History) Ornella Moscucci (Auth.) - Gender and Cancer in England, 1860-1948-Palgrave Macmillan UK (2016)Dokumen347 halaman(Medicine and Biomedical Sciences in Modern History) Ornella Moscucci (Auth.) - Gender and Cancer in England, 1860-1948-Palgrave Macmillan UK (2016)Federico AnticapitalistaBelum ada peringkat
- Literature Is An Important Component of A Total Language Arts Program at All Grade Levels Because of The Many Benefits It OffersDokumen1 halamanLiterature Is An Important Component of A Total Language Arts Program at All Grade Levels Because of The Many Benefits It Offersbersam05Belum ada peringkat
- Offsites Engineering Works For The Erbil Refinery 40,000 B/D Expansion ProjectDokumen12 halamanOffsites Engineering Works For The Erbil Refinery 40,000 B/D Expansion ProjectSardar PerdawoodBelum ada peringkat
- Lesson10 Sacraments of InitiationDokumen76 halamanLesson10 Sacraments of InitiationInsatiable CleeBelum ada peringkat
- Addendum PDFDokumen2 halamanAddendum PDFIbaiMitxelenaSanchezBelum ada peringkat
- Taxation During Commonwealth PeriodDokumen18 halamanTaxation During Commonwealth PeriodLEIAN ROSE GAMBOA100% (2)
- Auditing The Purchasing Process: Mcgraw-Hill/IrwinDokumen18 halamanAuditing The Purchasing Process: Mcgraw-Hill/IrwinFaruk H. IrmakBelum ada peringkat
- How 50 Actors Got Their Agents and ManagersDokumen5 halamanHow 50 Actors Got Their Agents and ManagersОля МовчунBelum ada peringkat
- Fila 1Dokumen4 halamanFila 1Karolina Sanchez83% (6)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Ks3 English 2009 Reading Answer BookletDokumen12 halamanKs3 English 2009 Reading Answer BookletHossamBelum ada peringkat
- EPM Key Design Decisions - Design PhaseDokumen7 halamanEPM Key Design Decisions - Design PhaseVishwanath GBelum ada peringkat
- Pengaruh Suhu Pengeringan Terhadap Karakteristik Kimia Dan Aktivitas Antioksidan Bubuk Kulit Buah Naga MerahDokumen9 halamanPengaruh Suhu Pengeringan Terhadap Karakteristik Kimia Dan Aktivitas Antioksidan Bubuk Kulit Buah Naga MerahDika CodBelum ada peringkat
- OS W2020 3140702 APY MaterialDokumen2 halamanOS W2020 3140702 APY MaterialPrince PatelBelum ada peringkat
- Research Papers Harvard Business SchoolDokumen8 halamanResearch Papers Harvard Business Schoolyquyxsund100% (1)
- Earthquake EnggDokumen6 halamanEarthquake EnggAiko VillaluzBelum ada peringkat
- THE THIRD TEST - No AnswersDokumen11 halamanTHE THIRD TEST - No Answersdniela .fdrsairBelum ada peringkat
- (Susan Harris-Hümmert) Evaluating Evaluators An (BookFi)Dokumen299 halaman(Susan Harris-Hümmert) Evaluating Evaluators An (BookFi)Muhammad FitrahullahBelum ada peringkat
- A Game Is A Structured Form of PlayDokumen5 halamanA Game Is A Structured Form of PlayNawa AuluddinBelum ada peringkat
- Hse Check List For Portable Grinding MachineDokumen1 halamanHse Check List For Portable Grinding MachineMD AbdullahBelum ada peringkat
- Coursebook Answers Chapter 28 Asal ChemistryDokumen3 halamanCoursebook Answers Chapter 28 Asal ChemistryAditiBelum ada peringkat
- Iris Sofía Tobar Quilachamín - Classwork - 16-09-2022Dokumen4 halamanIris Sofía Tobar Quilachamín - Classwork - 16-09-2022IRIS SOFIA TOBAR QUILACHAMINBelum ada peringkat
- ALA - Application Guide 2023Dokumen3 halamanALA - Application Guide 2023Safidiniaina Lahatra RasamoelinaBelum ada peringkat
- Highway MidtermsDokumen108 halamanHighway MidtermsAnghelo AlyenaBelum ada peringkat
- BE 601 Class 2Dokumen17 halamanBE 601 Class 2Chan DavidBelum ada peringkat
- 4-String Cigar Box Guitar Chord Book (Brent Robitaille) (Z-Library)Dokumen172 halaman4-String Cigar Box Guitar Chord Book (Brent Robitaille) (Z-Library)gregory berlemontBelum ada peringkat
- GSRTCDokumen1 halamanGSRTCAditya PatelBelum ada peringkat
- PhonemeDokumen4 halamanPhonemealialim83Belum ada peringkat
- Two Dimensional Flow of Water Through SoilDokumen28 halamanTwo Dimensional Flow of Water Through SoilMinilik Tikur SewBelum ada peringkat
- Case 1 - Mr. ReyesDokumen3 halamanCase 1 - Mr. ReyesJasper Andrew AdjaraniBelum ada peringkat
- CASE STUDY GGHDokumen4 halamanCASE STUDY GGHSanthi PriyaBelum ada peringkat
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceDari EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RacePenilaian: 4.5 dari 5 bintang4.5/5 (516)
- Masterminds: Genius, DNA, and the Quest to Rewrite LifeDari EverandMasterminds: Genius, DNA, and the Quest to Rewrite LifeBelum ada peringkat
- Tales from Both Sides of the Brain: A Life in NeuroscienceDari EverandTales from Both Sides of the Brain: A Life in NeurosciencePenilaian: 3 dari 5 bintang3/5 (18)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincDari EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincPenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Gut: the new and revised Sunday Times bestsellerDari EverandGut: the new and revised Sunday Times bestsellerPenilaian: 4 dari 5 bintang4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (3)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsDari EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsPenilaian: 4.5 dari 5 bintang4.5/5 (6)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperDari EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperPenilaian: 4.5 dari 5 bintang4.5/5 (15)