March Case Study
Diunggah oleh
api-247490129Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
March Case Study
Diunggah oleh
api-247490129Hak Cipta:
Format Tersedia
1 Katrina Lee March Case Study March 31, 2014 Palliative Treatment Planning - Whole Brain and Sacrum
History of Present Illness: Patient W is a 72 year old male undergoing palliative external beam radiation treatment to his brain and sacrum. The patient presented to his primary clinic in January 2014 with pain in his sacral region. The patient was sent for a computed technology, or CT scan. The images did not initially show any acute pathology to the lower spine. The patient was evaluated by an endocrinologist who performed a CT biopsy using guided fluoroscopy to the spine. The results showed that the patient had significant metastatic disease in the sacrum. By March 2014, the patient had consulted with a neurologist and radiation oncologist to determine a course of treatment. Further testing revealed that the patient had brain metastasis in addition to the sacrum. Metastatic disease frequently requires whole brain treatment techniques.1 The radiation oncologist suggested that the patient receive palliative external beam radiation therapy treatment to both the sacrum and the brain. The physician discussed the risks, benefits, and potential side effects due to treatment. The patient elected to undergo external beam radiation therapy treatment to the sacrum and brain. Past Medical History: The patient has a history of prostate cancer, with a score of Gleason 9. The Gleason score is a histological grading system that is used to differentiate the microscopic distribution of a prostate.2 Gleason values range from 2 (low) to 10 (high). The pathology of prostate cancer by way of the Gleason score is strongly correlated with the incidence of metastasis.3 High grade tumors are more likely to have spread the disease to the lymph nodes.3 Determination of a patient's Gleason score is done through a needle biopsy, in which a needle is inserted into the perineum and samples of the tissue are taken to be analyzed. The patient received external beam intensity-modulated radiation therapy, or IMRT, treatment to the prostate in the summer of 2010. Patient W's prostate treatment was prescribed to 7380 cGy over the course of 41 fractions at 180 cGy per fraction. Seven fields were used in the IMRT treatment. The patient's PSA levels were checked regularly following the radiation treatment. The patient's medical history also includes hypertension, anemia, lung carcinoma, hypokalemia, adrenal mass, dermatitis, cataracts, and polyps of the large intestine.
2 Social/Family History: Patient W is a retired veteran who served in the Vietnam war. The patient has a history of smoking off and on for the past 50 years, and claimed to have quit in 2010. The patient currently resides in an assisted living facility, but was fully independent prior to having intense low back pain. The patient's family history includes a grandfather who died from colon cancer. Medications: Patient W uses the following medications: Dexamethoson, Oxycodone, Amlodipine, Asprin, Lisinopril, Senokot, Tamsulosin, Actaminophen, ALOH/MGOH/Simethxtra strength, Lactulose solution, Prochlorperazine, Polyethylene glycol, Lidocaine. Diagnostic Imaging: Multiple imaging studies were used to help the physicians diagnose and initiate a treatment plan. The patient underwent an MRI study, without contrast, of the brain and lumbar region. The sacral MRI study revealed a secondary malignant neoplasm of the bone and bone marrow. The MRI study of the brain revealed solitary brain metastasis in the cerebellum impinging on that patient's fourth ventricle. Radiation Oncologist Recommendations: The radiation oncologist recommended that the patient undergo palliative external beam radiation to both the brain and the sacrum. The Plan (prescription): The radiation oncologist prescribed both areas to be treated to 2000 cGy at 400 cGy per day over the course of 5 fractions. Patient Setup/Immobilization: Two CT simulations treatment planning scans were performed. A 2.5 cm mat was placed on the treatment couch for both plans to aid in the patient's comfort and ability to stay in position. Initially, the patient was positioned prone on the CT simulation couch to image the patient's pelvis. The patient was positioned in a prone position to get better dose to the sacral tumor and avoid the previously irradiated area. The patient's head rested on a prone pillow and a small knee sponge was used to increase comfort. Figure 1 shows the patient set up for the sacral tumor treatment. The patient then flipped over into a supine position with the head placed on a head rest and an aquaplast mask used to immobilize the head for treatment. A large knee sponge was placed under the patient's legs and the feet were banded together on a foam block. Figures 2 and 3 show the patient set up for the whole brain treatment. Anatomical Contouring: Both CT data sets were sent to the Phillips Pinnacle 9.0 treatment planning system, TPS. For the sacral treatment plan, the medical dosimetrist contoured the
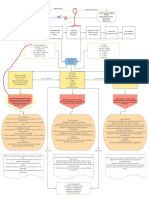
3 rectum, as that was the area of concern for previous radiation overlap. The physician then contoured the sacral tumor volume, and the CT data set was ready to have beams placed. The brain was contoured by the medical dosimetrist on the second CT data set. The contoured image data set was ready for treatment planning. Beam Isocenter/Arrangement: The radiation oncologist placed an isocenter onto each dataset in the CT simulator. For treatment of the sacrum, isocenter was positioned on the posterior aspect of the patient's rectal wall. The physician placed a right lateral field at 270 and the anterior jaws were closed up to the isocenter. The field was copied and opposed to have an equally blocked left lateral field (90) incorporated in the treatment plan, and a 50/50 beam weighting was given to each field. Independent jaws were used to block the previous radiated areas and to further protect the patient's rectum. Figure 4 shows the two beams, left and right lateral, used for the sacral treatment plan. The patient's whole brain treatment data set was sent to the TPS and the physician drew the block for a 270 right lateral field to protect the anterior aspect of the eyes. The block was drawn so that radiation would infiltrate the portion of the brain located between the posterior surface of the patient's eyes.1 The beam was copied and opposed so that a left lateral field (90) would contribute to the treatment plan, and a 50/50 beam weighting was given for both fields. Treatment Planning: The radiation oncologist prescribed a palliative dose of radiation to the sacrum and to the whole brain. The sacral tumor was planned first. The physician wanted to reduce the amount of toxicity that the patient would receive to the rectum based on the patient's prior radiation exposure. Independent jaws were used to block that portion of the field from being irradiated. A prescription point (pxpt-JS) was added to the plan and placed in the contoured tumor volume, away from the edge of the field. The plan was calculated using the CC Convolution algorithm and analyzed. A 15 wedge was placed on both treatment fields to push the dose distribution further into the defined tumor volume. The plan, shown in Figure 5, was recalculated and viewed by the physician. Figure 6 shows the dose volume histogram, DVH, the radiation oncologist used to analyze the rectal dose and ultimately approve the treatment plan. The radiation oncologist carefully drew the blocks used for the whole brain treatment plan. Figure 7 shows the digitally reconstructed radiographs (DRR) for both treatment fields with the MLC blocks positioned. A dose grid was drawn around the patient and the beams were set to the
4 CC Convolution algorithm to compute the treatment plan. The physician approved the treatment plan, shown in Figure 8. Quality Assurance/Physics Check: The monitor units (MUs) were double checked for each treatment plan using the MU check program. The acceptable tolerance at the hospital between the TPS and MU check program is to be within 3% for each field. The MU checks for the sacral treatment plan and the whole brain treatment are shown in Figure 9 and Figure 10, respectively. Also, the physician prescribed portal images for the first treatment and for the treatment plans to be peer reviewed by the hospital's other physicians. Conclusion: The treatment planning process needed to be completed quickly, as the patient started treatment the following afternoon. It was challenging to ensure that the sacral treatment field would block the previously irradiated area. The radiation therapy team made it a priority to compare the previous treatment field location and approve the new field placement. The treatment planning system does not allow composite plans to be generated from two different data sets, so the radiation oncology team had to scrutinize the previous plan to approve of the new beam placement. In addition to comparing the previous treatment plan, ensuring that the patient could maintain a prone position through the sacral treatment was challenging. In analyzing the finished treatment plan, the sacral tumor volume could have had a better dose distribution by adjusting the beam weighting. Increasing the weight of the patient's left lateral field might have given full dose to the tumor volume, and reduced the large areas of high dose within the treatment plan. The plan would have then been cooler, potentially reducing the adverse effects following radiation treatment.
5 References 1. Bentel G. Radiation Therapy Planning. 2nd ed. New York, NY: McGraw-Hill; 1996: 336-341 2. Held-Warmkessel, J. Contemporary Issues in Prostate Cancer - A Nursing Perspective. 2nd ed. Mississauga, Ontario: Jones and Bartlett Publishers Canada; 2006: 117-119. 3. Washington CM, Leaver D. Principles and Practice of Radiation Therapy. 3rd ed. St Louis, MO: Mosby-Elsevier; 2010: 823-865.
6 Figures
Figure 1. Patient set up for treating the sacral tumor
Figure 2. Patient set up to treat the whole brain
Figure 3. Patient set up for whole brain treatment
Figure 4. The left and right lateral fields used closed to isocenter. The prescription point, in blue, is shown
Figure 5. Sacral treatment plan at the prescription point (pxpt-JS) shows wedge orientation
Figure 6. The DVH for the sacral tumor volume treatment plan.
Figure 7. The DRR for the whole brain treatment plan with the MLC blocks.
10
Figure 8. Whole brain radiation treatment at isocenter
11
Figure 9. MU check for the sacral treatment plan
12
Figure 10. MU check for the whole brain treatment plan
Anda mungkin juga menyukai
- Hybrid Esophagus Irradiation Katrina LeeDokumen11 halamanHybrid Esophagus Irradiation Katrina Leeapi-247490129Belum ada peringkat
- LeeaffevlsDokumen9 halamanLeeaffevlsapi-247490129Belum ada peringkat
- LeeelectroncompDokumen2 halamanLeeelectroncompapi-247490129Belum ada peringkat
- Leeimrt 3Dokumen3 halamanLeeimrt 3api-247490129Belum ada peringkat
- Daleaconformal 17Dokumen3 halamanDaleaconformal 17api-247959633Belum ada peringkat
- LeebrachycompsDokumen3 halamanLeebrachycompsapi-247490129Belum ada peringkat
- Leeimrt 3Dokumen3 halamanLeeimrt 3api-247490129Belum ada peringkat
- Medical DosimetristDokumen2 halamanMedical Dosimetristapi-247490129Belum ada peringkat
- Budget ActivityDokumen2 halamanBudget Activityapi-247490129Belum ada peringkat
- LeeelectroncompsummaryDokumen6 halamanLeeelectroncompsummaryapi-247490129Belum ada peringkat
- Qa ChecklistDokumen1 halamanQa Checklistapi-247490129Belum ada peringkat
- Lab Katrina - BrainDokumen2 halamanLab Katrina - Brainapi-247490129Belum ada peringkat
- Sample BudgetDokumen6 halamanSample Budgetapi-247490129Belum ada peringkat
- LeebrachysummaryDokumen7 halamanLeebrachysummaryapi-247490129Belum ada peringkat
- LeesummaryDokumen11 halamanLeesummaryapi-247490129Belum ada peringkat
- LeeaffectivesummaryDokumen15 halamanLeeaffectivesummaryapi-247490129Belum ada peringkat
- Lee Summer PhotonsummaryDokumen7 halamanLee Summer Photonsummaryapi-247490129Belum ada peringkat
- Lee Imrt EportDokumen3 halamanLee Imrt Eportapi-247490129Belum ada peringkat
- Mentoring ActivityDokumen7 halamanMentoring Activityapi-247490129Belum ada peringkat
- 2014 CnsassignmentfinalDokumen1 halaman2014 Cnsassignmentfinalapi-247959633Belum ada peringkat
- April Case StudyDokumen10 halamanApril Case Studyapi-247490129Belum ada peringkat
- Master Competency FormDokumen1 halamanMaster Competency Formapi-254189301Belum ada peringkat
- Lee Photon EportDokumen3 halamanLee Photon Eportapi-247490129Belum ada peringkat
- Parotid LabDokumen3 halamanParotid Labapi-237266632Belum ada peringkat
- Lab Katrina - LungDokumen3 halamanLab Katrina - Lungapi-247490129Belum ada peringkat
- Lab Katrina - PelvisDokumen3 halamanLab Katrina - Pelvisapi-247490129Belum ada peringkat
- Ama Challenge 2012Dokumen3 halamanAma Challenge 2012api-174496267Belum ada peringkat
- February Case StudyDokumen7 halamanFebruary Case Studyapi-247490129Belum ada peringkat
- Statistics ActivityDokumen5 halamanStatistics Activityapi-239878826Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Consent To Surgery/Anaesthesia: Ilocos Sur Provincial Hospital-Gabriela SilangDokumen1 halamanConsent To Surgery/Anaesthesia: Ilocos Sur Provincial Hospital-Gabriela SilangRyrey Abraham PacamanaBelum ada peringkat
- Tetagam P: Human Tetanus Immunoglobulin IM 250 IUDokumen25 halamanTetagam P: Human Tetanus Immunoglobulin IM 250 IUhamilton lowisBelum ada peringkat
- TLS FinalDokumen69 halamanTLS FinalGrace Arthur100% (1)
- Pediatric Musculoskeletal Summary For Osce ExamDokumen53 halamanPediatric Musculoskeletal Summary For Osce Examopscurly100% (2)
- CKD + HPN Concept Map DRAFTDokumen1 halamanCKD + HPN Concept Map DRAFTInah Floresta BesasBelum ada peringkat
- Sensus Harian TGL 02 Maret 2022...........Dokumen121 halamanSensus Harian TGL 02 Maret 2022...........Ruhut Putra SinuratBelum ada peringkat
- Factors Affecting The Extent of Compliance of Adolescent Pregnant Mothers On Prenatal Care ServicesDokumen29 halamanFactors Affecting The Extent of Compliance of Adolescent Pregnant Mothers On Prenatal Care ServicesNicole LabradoBelum ada peringkat
- English GuideDokumen85 halamanEnglish GuideanandkishoreBelum ada peringkat
- Frequency of Depression, Anxiety and Stress in Patients Referred For Endoscopy With Symptoms of DyspepsiaDokumen5 halamanFrequency of Depression, Anxiety and Stress in Patients Referred For Endoscopy With Symptoms of DyspepsiaSana SajidBelum ada peringkat
- Ibuprofen 150mg + Paracetamol 500mg (Combodex)Dokumen15 halamanIbuprofen 150mg + Paracetamol 500mg (Combodex)ddandan_2Belum ada peringkat
- Arihant Hospital & Research CentreDokumen30 halamanArihant Hospital & Research CentreSourabhSharmaBelum ada peringkat
- UBYT 2019 Yılı Dergi - ListesiDokumen904 halamanUBYT 2019 Yılı Dergi - ListesicemalBelum ada peringkat
- PleuraDokumen6 halamanPleuraameerabest100% (1)
- Legal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DDokumen6 halamanLegal Medicine: Legal Medicine (2011) Antonio Rebosa, LL.B, M.DarciblueBelum ada peringkat
- Emteaz OphthalmologyDokumen16 halamanEmteaz OphthalmologyRaouf Ra'fat SolimanBelum ada peringkat
- Delivery Room Emergencies: Amanda Louise Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistDokumen44 halamanDelivery Room Emergencies: Amanda Louise Du, MD, DPPS, DPSNBM Pediatrician-NeonatologistLyn LynBelum ada peringkat
- LeukocoriaDokumen5 halamanLeukocoriabahaashakirBelum ada peringkat
- Oxford GastroenterologyDokumen673 halamanOxford Gastroenterologymymamym100% (1)
- The Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusDokumen4 halamanThe Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusFiqoh Puteri FauziBelum ada peringkat
- Pes Planus Concept MapDokumen2 halamanPes Planus Concept MapVeronica Jean U. TubaonBelum ada peringkat
- Rajasekhar2021 Article TheUsefulnessOfGenelynEmbalminDokumen4 halamanRajasekhar2021 Article TheUsefulnessOfGenelynEmbalminyordin deontaBelum ada peringkat
- DementiaDokumen26 halamanDementianadya100% (4)
- Objectives For Critical Care RotationDokumen9 halamanObjectives For Critical Care Rotationsteviestevie333Belum ada peringkat
- Pudendal Neuralgia and Osteopathy Template1Dokumen3 halamanPudendal Neuralgia and Osteopathy Template1LauraBelum ada peringkat
- Financial Analyst or Trader or BAnkerDokumen2 halamanFinancial Analyst or Trader or BAnkerapi-79318002Belum ada peringkat
- Assignment On DislysisDokumen10 halamanAssignment On DislysisSanhati Ghosh Banerjee100% (1)
- Is It Okay To Drink Alcohol On Steroids - Google SearchDokumen1 halamanIs It Okay To Drink Alcohol On Steroids - Google SearchEsin SyurmeliBelum ada peringkat
- Achalasia: Tova Rainis Gastroenterology Unit Bnai-Zion Medical CenterDokumen34 halamanAchalasia: Tova Rainis Gastroenterology Unit Bnai-Zion Medical CenterHasan Al-HabsyiBelum ada peringkat
- Struktur Permukaan BumiDokumen162 halamanStruktur Permukaan BumifitrawatiBelum ada peringkat
- When Are Focused Assessments ConductedDokumen26 halamanWhen Are Focused Assessments ConductedNozomi YukiBelum ada peringkat