Gangguan Jiwa Psikotik
Diunggah oleh
Anizatun NuskiyatiDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Gangguan Jiwa Psikotik
Diunggah oleh
Anizatun NuskiyatiHak Cipta:
Format Tersedia
STEP 1 Stressor : keadaan2 atau peristiwa yang dapat menimbulkan stress. Waham : keyakinan yang salah.
alah. Orang tsb meyakini keyakinan yang salah meskipun ada orang lain yang menjelaskan bahwa keyakinan tsb salah.tapi org tsb tak percaya. Halusinasi : persepsi panca indra tanpa rangsangan pada reseptor2 panca indra itu sendiri. Fungsi okupasi dan fungsi psikososial Zat psikoaktif : zat yang bisa menimbulkan perubahan perilaku,persepsi, psikologi
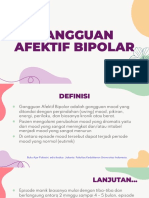
STEP 2 1. Mengapa dia sering marah marah tanpa sebab dan bicara kacau? 2. Definisi gangguan jiwa psikotik? 3. Apakah ada hubungan gejala tsb dengan masalah pekerjaannya? 4. Perbedaan waham dg halusinasi ? 5. Terapi apa saja yang diberikan oleh dokter? 6. Definisi fungsi global (GAF) ? 7. Apa maksud dari px.status mental dan itu mengindikasikan apa? 8. Mengapa terjadi penurunan Fungsi okupasi dan fungsi psikososial ? 9. Bagaimana cara untuk mengetahui pasien tsb kalau mengalami gangguan jiwa ? 10. Macam macam kelompok gangguan jiwa apa saja ? knp pasien tsb digolongkan pada gangguan jiwa yang berat ? 11. Macam macam waham ? 12. Macam macam halusinasi? 13. Macam macam stressor ? dan sebutkan derajat derajat stressor ? 14. Pengertian gangguan jiwa ? dan berikan gejalanya! 15. DD? STEP 3 1. Definisi gangguan jiwa psikotik? Seseorang individu punya persepsi dan pemikiran abnormal dan tak mampu menilai realita yang ada dan juga mengalami waham dan halusinasi, gangguan organik (di SSP dan di luar SSP) dan fungsional ( hanya ganggua kejiwaan saja). Organik ; demensia , delirium Fungsional; gangguan di tataran molekuler, neurotransmitter, skizofrenia, psikotik akut. 2. Definisi fungsi global (GAF) ? 3. Pengertian gangguan jiwa ? dan berikan gejalanya! Suatu sindroma atau pola prilaku yang secara klinis bermakna, disertai adanya penderitaan; yang menyakitkan dan kecacatan co. Gang.fungsi
1. Gangguan kognisi pada persepsi ; kayak mendengar bisikan2 2. Gangguan kemauan ; mengalami kemauan yang lemah 3. Gangguan emosi ; suka merasa gembira berlebihan, atau sedih berlebih 4. Gang.psikomotor ; hiperaktif ; berlari gak jelas Gangguan jiwa menimbulkan GK : Adanya sindrom psikologik; ada 2 persepsi penderitaan yang dialami oleh penderita tsb. Nyeri, disfungsi organ, disabilitas (gangguan mandi, makan) 4. Macam macam kelompok gangguan jiwa apa saja ? knp pasien tsb digolongkan pada gangguan jiwa yang berat ? Gangguan jiwa ada 2 : Psikosis dan neurosis Psikosis ( berat) ditandai hilangnya daya realita dan hilangnya fungsi mental ( halusinasi, waham) co. Skizofrenia, psikotik akut,gang jiwa akibat zat2 psikoaktif Neurosis ; non psikotik kronis dan rekuren GK : cemas, obsesif, fobia. 5. Mengapa dia sering marah marah tanpa sebab dan bicara kacau? Orang gangguan jiwa ada gangguan pada neurotransmitterr. Gampang berubah emosinya. Kalau ngomong juga kacau. Dan sering mengalami disorientasi (Dopamin, Serotonin) Marah marah : paratimik ( tak cocok anatara kenyataan dan prilakunya) Bicara kacau : inkoherensi ( gang. Arus fikir ; bicara yang tak dipahami) 6. Apakah ada hubungan gejala tsb dengan masalah pekerjaannya? Berhub dengan fungsi psikososial dari masy. Dan keluarga (HPA aksis) bisa melepaskan glukokortikoid merangsang aktifasi HPA aksis stress menetap glukokortikoid makin banyak hipokampus peka banget sama glukokortikoid ( reseptornya banyak) HPA aksis berubah menetap HPA aksis menstimulasi dopaminergik eksitatorik memicu saraf ....... gelisah, persepsi, halusinasi. STEP 7
Multiple observations regarding these systems suggest that glutamatergic pathways, presumably emanating from the cerebral cortex, exert a strong inhibitory and stabilizing effect on an array of subcortical, potentially psychosis-inducing mechanisms, involving both monoaminergic and cholinergic pathways. The mechanism underlying this stabilizing glutamatergic function appears to be complex. In part it seems to be located postsynaptically to the (limbic) striatum, where corticostriatal pathways control both direct and indirect striatopallidothalamic pathways, as detailed in Figure 10.1. These pathways appear to regulate the sensory input to the cerebral cortex as well as the arousal. The direct and indirect pathways are mutually antagonistic, the former being activating and the latter inhibitory on the thalamocortical glutamatergic projections. Both the direct
and the indirect pathways are also controlled by dopaminergic projections, whereby the former are activating (via D1 receptors) and the latter inhibitory (via D2 receptors). In addition, glutamatergic and glutamatergic/GABAergic pathways seem to control the monoaminergic neurons themselves by means of an accelerator and a brake mechanism, respectively (Carlsson et al., 2001). These observations support glutamatergic involvement in schizophrenia and emphasize the interaction of glutamate with other, largely subcortical transmitter systems and open up possibilities for a multifactorial dysregulation in complex neurocircuits where, besides glutamate, GABAergic, monoaminergic and cholinergic systems participate in the psychotogenic process (Carlsson and Carlsson, 1990). Several drugs in different states of development will probably shed additional light on the multifactorial aspects of psychotogenesis, for example, agonists acting at the glycine site of the NMDA receptor, glycine-reuptake inhibitors, ampakines, drugs acting on the metabotropic glutamate receptors, partial dopamine receptor agonists and dopaminergic stabilizers lacking intrinsic activity on dopamine receptors (Carlsson et al., 2001). Systems Pathology in Schizophrenia: The Limbic Cortex In looking for sites of pathophysiology in the cerebral cortex, several lines of evidence point to abnormal limbic function. Decades of postmortem research in schizophrenia have reported structural, histologic, and neurochemical changes in limbic cortex (Jakob and Beckmann, 1989). Abnormalities in hippocampal size (Bogerts et al., 1985), axial orientation (Scheibel and Kovelman, 1981), neuronal and nonneuronal number (Benes et al., 1991, 1998; Heckers et al., 1991; Jeste and Lohr, 1989), and changes in neurochemical markers of transmission and development (Akbarian et al., 1993; Gao et al., 2000; Tsai et al.,
Postmortem Limbic Cortex Abnormalities in Schizophrenia: Structural Changes Much focused work in the human limbic cortex in schizophrenia began after Scheibel and Kovelman (1981) described an alteration in pyramidal cell apical dendrite orientation in the hippocampus, in its anterior and middle section, particularly at the subicularCA1 border. In a later extension of this work, they correlated symptom severity with the extent of the dendritic disorientation (Kovelman and Scheibel, 1984). However, other studies have not uniformly replicated these fi ndings (Altshuler et al., 1987; Christison et al., 1989; Vogel et al., 1997), but the original fi ndings are still often referenced as evidence for neuroanatomical abnormalities in the hippocampus. Weinberger (1996) highlights several studies describing cytoarchitectural abnormalities in the entorhinal cortex (including the specifi c loss of NADPH-diaphorase neurons Nicotinamide Adenosine Dinucleotide Phosphate) as providing the best evidence for neuropathological fi ndings (Akbarian et al., 1993; Arnold et al., 1991; Jakob and Beckmann, 1986). Other studies have reported signifi cant reductions in the volumes or cross-sectional areas of the entorhinal cortex or hippocampus in schizophrenia (Bogerts et al., 1985; Brown et al., 1986; Colter et al., 1987; Falkai and Bogerts, 1986; Falkai et al.,
1988), but these results have not been uniformly replicated (Benes et al., 1991; Heckers et al., 1991). Hippocampal size is reduced bilaterally, albeit mildly, in the illness especially in anterior areas (Becker et al., 1996; Bilder et al., 1995; Bogerts et al., 1990; Suddath et al., 1989. Shape analyses of the hippocampus have suggested regional abnormalities of volume in schizophrenia. Importantly, regional shape abnormalities are predominantly localized to the head, implicating only a delimited area within hippocampus as abnormal (Csernansky et al., 1998). Neurochemical Changes Changes in GABAA receptor density, in GABA release and in glutamate-related transmitters and their enzymes in hippocampus have been reported in the illness (Simpson et al., 1992; Tsai et al., 1995). While there appears to be no change in the density of hippocampal NMDA glutamate receptors (Ishimaru et al., 1992; Kerwin et al., 1990; Kornhuber et al., 1989), kainate binding, particularly in CA2 has been found reduced in several studies (Kerwin et al., 1988, 1990; Simpson et al., 1992) but not consistently (Deakin et al., 1989). Reduced levels of non-NMDA receptor binding (Kerwin et al., 1990) and lower concentrations of non-NMDA receptor mRNA (Harrison et al., 1991), have both been reported in CA3. The previous fi nding of an alteration in the NR1 subunit and an increase in NR2B in postmortem tissue from schizophrenia (Gao et al., 2000) suggests a reduction in excitatory glutamate transmission at hippocampal NMDA receptors in this illness. In addition, considerable evidence of compromised cognitive function, especially short-term memory and attention, exists in schizophrenia (Green, 1996; Gruzelier et al., 1988; Venables, 1992). These dysfunctions may represent the behavioral correlates of hippocampal pathology. In Vivo Functional Limbic Cortex Change in Schizophrenia Functional studies of human brain in schizophrenia have directly demonstrated an alteration in neuronal activity in the limbic cortex in the illness (Fletcher, 1998; Haznedar et al., 1997; Heckers et al., 1998; Medoff et al., 2001; Nordahl et al., 1996; Tamminga et al., 1992). Anterior cingulate cortex consistently shows alterations in schizophrenia when persons are imaged medication-free and matched for performance. Moreover, connectivity analyses suggest that the anterior cingulate rCBF is not tightly coupled to hippocampal activity during tasks of learning and memory, as it is in normal persons. Although the entire body of these data have not yet suggested the pivotal limbic pathology, they do implicate abnormal function of these structures in the illness. Moreover, as suggested in the preclinical studies, such pathology could destabilize the function of subcortical brain areas in psychosis. An analysis of connectivity in auditory discrimination experiments
directly suggests that a systems failure occurs within limbic cortex in schizophrenia. A malfunction within the limbic cortex and the subsequent disruption of related neocortical areas and secondary dysregulation of subcortical structures may underlie the manifestations of schizophrenia. This working hypothesis suggests that it may be the resultant misbehavior of the limbic system itself that generates positive and cognitive symptoms in schizophrenia, possibly through its connections with neocortical and subcortical structures. These speculations raise the possibility that the primary origin of the circuit dysfunction could be varied, but inevitably result in a characteristic psychosis circuit abnormality (Figure 10.2). Functional Effects of D2 Dopamine Receptor Blockade The clinical evidence of a systems basis of psychosis, along with the preclinical data suggesting multiple and complex neurotransmitter interactions within these symptoms, builds a plausible psychosis circuit for schizophrenia and potentially for its treatment. The effective functioning of the human brain to facilitate cognitive, motor and affective performance, is dependent not only on the proper functioning of individual regional neuronal groups dedicated to specifi c tasks, but also to interacting brain systems which function to connect neural systems to perform a particular mental task and systematically to direct information fl ow in the brain. Because schizophrenia is not characterized primarily by a neural or behavioral defi cit, but rather by productive symptoms and by a confusion of neural activity with resulting mental malfunction, a system hypothesis of schizophrenia pathology is plausible. The idea that psychosis is the consequence of dysfunction somewhere within the limbic cortex, seen during cognitive work and even during routine mental function is supported by a great deal of research. This putative dysfunction is prominently manifest in the anterior components of the limbic system. Hence this change primarily infl uences the frontal regions of the neocortex, leaving the posterior hippocampus and the posterior neocortex relatively unaffected. Exactly where the primary limbic pathology is located within these anterior areas is a matter of speculation, but it could be multiple sites with a single resultant systems dysfunction. Importantly, this idea allows for the real possibility that other drug actions can be exerted at other sites within the relevant
7. Macam macam waham ? Waham gang pada isi pikir 5 syarat waham -isi pikiran salah -bertentangan dg realita -tdk diterima logika -yakin dg kepercayaannya -tdk mau dikasi tau Waham sistematik isi pikirannya tersistematik STEP 7 WAHAM Adl suatu keyakinan atau pikiran yg salah karena bertentangan dg kenyataan Sifat atau ciri2 waham : 1. Buah pikiran ini selalu mengenai diri sendiri atau egosentris 2. Selalu bertentangan dengan realitas
3. Selalu bertentangan dg logika 4. Penderita percaya 100% terhadap kebenaran pikiran 5. Tidak dpt dirubah oleh orang lain, sekalipun dg jalan yg logis dan rasional Jenis jenis waham : Waham dikejar Waham curiga lain. Wahampersekutorik oleh orang lain Waham curiga : pasien merasa selalu disindir oleh orang lain : penderita merasa diganggu, ditipu atau disiksa : penderita merasa dikejar2 olah orang lain : penderita merasa selalu di sindir oleh orang
(curiga terhadap sekitar, cth : orang lain tersenyum, tetapi diartikan spt menyindir dirinya) Waham cemburu : pasien merasa sll cemburu pd orang lain, cth :
penderita sll cemburu dg pasangannya (berlebihan) Waham hipokondria : keprihatinan yg berlebihan ttg kesehatan
pasien yg didasarkan bukan pd patologi organic yg nyata. Waham somatic : keyakinan palsu menyangkut fungsi tubuh
pasian, cth : keyakianan bahwa otak penderita mencair, jantung bocor Bizareisi pikiran kacau, banyak cabang - Taught of insertion : isi pikiran asing dari luar masuk ke pikirannya - Taught of broadcasting ; meniarkan isi pikirannya ke halayak umum - Taught of withdrawl ; isi pikirannya diambil dari luar dirinya Kriteria untuk dg.skizofrenia. Nihilistik kosong Somatikwaham merasa dirinya sakit Paranoid merasa dirinya besar,dikejar kejar,curagaan 8. Macam macam halusinasi? Halusinasi gangguan persepsi Ada 2 interaksi rangsang sensorik dan proses dari kita yang mengolah rangsang sensorik tsb Tak ada rangsang tapi si x ada memproses rangsang. - Auditorik : skizofren - Gustatorik - Visual - Olfaktorik - Taktil
Haptik : bersentuhan dengan manusia lain dan benda benda lain Kinestetik ; anggota tubuh terlepas dari tubuhnya : skizofren Autoskopi : melihat dirinya sendiri dihadapannya
Ilusi Ada rangsangan tapi diinterpretasikannya salah. 9. Perbedaan waham dg halusinasi ? Halusinasi : gangguan persepsi tanpa ada rangsangan dari luar - Terkait sama panca indra - Bisa diubah - Bisa terjadi pada orang normal Waham - Tak terkait dg panca indra - Tak bisa diubah keyakinannya - Gak bisa terjadi pada orang normal 10. Macam macam stressor ? dan sebutkan derajat derajat stressor ? Macam 1. Stressor episodik : kecelakaan blm lama terjadi, perselisihan sama org lain tak selesai selesai 2. Squenstressor : perceraian, kematian orang yang tercinta, pekerjaan 3. Periodik : kedokter gigi gara- gara sakit gigi terus.... terus terusan, sakit pinggang 4. Kronis : penyakit permanen, masalah suami istri yang berlarut larut, maslaah keuangan,. Derajat derajatnya ? STEP 7 what is stress? Stress is often described as a feeling of being overloaded, woundup tight, tense and worried. We all experience stress at times. It can sometimes help to motivate us to get a task finished, or perform well. But stress can also be harmful if we become over-stressed and it interferes with our ability to get on with our normal life for too long. what are the signs of stress? When we face a stressful event, our bodies respond by activating the nervous system and releasing hormones such as adrenalin and cortisol. These hormones cause physical changes in the body which help us to react quickly and effectively to get through the stressful situation. This is sometimes called the fight or flight response.
The hormones increase our heart rate, breathing, blood pressure, metabolism and muscle tension. Our pupils dilate and our perspiration rate increases. While these physical changes help us try to meet the challenges of the stressful situation, they can cause other physical or psychological symptoms if the stress is ongoing and the physical changes dont settle down. These symptoms can include: Headaches, other aches and pains Sleep disturbance, insomnia Upset stomach, indigestion, diarrhoea Anxiety Anger, irritability Depression Fatigue Feeling overwhelmed and out of control Feeling moody, tearful Difficulty concentrating Low self-esteem, lack of confidence High blood pressure Weakened immune system Heart disease
changes to the things that are within your control 11. Apa maksud dari px.status mental dan itu mengindikasikan apa? Waham bizare Halusinasi akustik 12. Mengapa terjadi penurunan Fungsi okupasi dan fungsi psikososial ? 13. Bagaimana cara untuk mengetahui pasien tsb kalau mengalami gangguan jiwa ? Punya masalah apa gak Anamnesis riwayat psikiatrik
14. Terapi apa saja yang diberikan oleh dokter? Obat antipsikotik ARS : risperidon, klozapin ARD : Ketidaskseimbangan dopamin di prefrontal (mesokortikal) dan mesolimbik (mesensephalon) HPAaksis dopaminergik.
Terapi psikososial 15. DD? Depresi Skizofrenia Skizotipal
STEP 4
STRESSOR DERAJAT
GANGGUAN JIWA
SKALA GAF
PSIKOTIK
NONPSIKOTIK
PSIKOSIS
NEUROSIS
HALUSINASI AUDITORIK, OLFAKTORIK
WAHAM BIZARE, SOMATIK
CEMAS, OBSESIF, FOBIA
Anda mungkin juga menyukai
- Bab IiDokumen25 halamanBab IiILham AKbarBelum ada peringkat
- Stres PsikososialDokumen13 halamanStres Psikososialyodha baktiBelum ada peringkat
- Referat - MannerismDokumen14 halamanReferat - MannerismEisBelum ada peringkat
- Mekanisme SkizofreniaDokumen5 halamanMekanisme SkizofreniaTriBelum ada peringkat
- Beberapa Penelitian Telah Menginformasikan Penelitian Di Bidang IniDokumen5 halamanBeberapa Penelitian Telah Menginformasikan Penelitian Di Bidang IniSulistia PratiwiBelum ada peringkat
- 2021 - Apoteker - Studi Kasus Dan Pembahasan Clinical ScienceDokumen11 halaman2021 - Apoteker - Studi Kasus Dan Pembahasan Clinical ScienceayuBelum ada peringkat
- SkizofreniaDokumen46 halamanSkizofreniamedic100% (1)
- Referat JiwaDokumen38 halamanReferat JiwaAisia NovitaBelum ada peringkat
- PATOFISIOLOGIDokumen4 halamanPATOFISIOLOGIhikariii100% (4)
- Psikotik PBL 5 Blok 256Dokumen24 halamanPsikotik PBL 5 Blok 256ihdaBelum ada peringkat
- SkizofreniaDokumen8 halamanSkizofreniaAfrida Ayu NaniBelum ada peringkat
- SKENARIO 2 PSIKIATRI - NewDokumen110 halamanSKENARIO 2 PSIKIATRI - NewRusydina NahjanBelum ada peringkat
- Laporan PBL Kelompok 4 Modul Kejang Skenario IDokumen78 halamanLaporan PBL Kelompok 4 Modul Kejang Skenario IvivalaninaBelum ada peringkat
- Laporan Tutorial Demensia Pada Penyakit ParkinsonDokumen39 halamanLaporan Tutorial Demensia Pada Penyakit ParkinsonMuhammad Adil100% (1)
- Contoh Resume JurnalDokumen7 halamanContoh Resume Jurnaltrisnaparama05Belum ada peringkat
- REHABILITASI PSISKOSOSIALDokumen22 halamanREHABILITASI PSISKOSOSIALrizuka-chanBelum ada peringkat
- ParkinsonDokumen44 halamanParkinsonAnonymous iWsaMSBelum ada peringkat
- PNI HPADokumen40 halamanPNI HPARifni Arneswari FardianingtyasBelum ada peringkat
- Patofisiologi Skizofrenia 01Dokumen4 halamanPatofisiologi Skizofrenia 01Gusti Ferri SandariaBelum ada peringkat
- Dokumen - Tips - Patofisiologi Skizofrenia 5634fa97dc242 PDFDokumen4 halamanDokumen - Tips - Patofisiologi Skizofrenia 5634fa97dc242 PDFGusti Ferri SandariaBelum ada peringkat
- Gangguan BipolarDokumen23 halamanGangguan BipolarPratiwi 'Wulan' DhariBelum ada peringkat
- Definisi InsomniaDokumen3 halamanDefinisi InsomniaAdipta KurniawanBelum ada peringkat
- Aspek Neurobiologi Dan Psikofarmakologi Gangguan MoodDokumen35 halamanAspek Neurobiologi Dan Psikofarmakologi Gangguan MoodfarlylaurelBelum ada peringkat
- Li LBM 3Dokumen7 halamanLi LBM 3WJ AjaBelum ada peringkat
- Go GDDGGDokumen40 halamanGo GDDGGJosua LouisBelum ada peringkat
- Jurnal SkizofreniaDokumen10 halamanJurnal Skizofreniasyifacippe100% (1)
- Tugas DR TimbangDokumen22 halamanTugas DR TimbangvidiBelum ada peringkat
- Jtptunimus GDL Ikapurnawa 7619 3 Bab2Dokumen15 halamanJtptunimus GDL Ikapurnawa 7619 3 Bab2Indah nurhamidahBelum ada peringkat
- JR - Obat-Obat Glutamatergik Pada Pengobatan SkizofreniaDokumen16 halamanJR - Obat-Obat Glutamatergik Pada Pengobatan SkizofreniaAzmi JabbarBelum ada peringkat
- Gangguan AfektifDokumen25 halamanGangguan AfektifSamiaji GilangBelum ada peringkat
- OGS B - Putri Wijayanti - 1806185683Dokumen17 halamanOGS B - Putri Wijayanti - 1806185683PutriWijayaJayantiBelum ada peringkat
- lbm1 Jiwa MadinDokumen38 halamanlbm1 Jiwa MadinAnizatun NuskiyatiBelum ada peringkat
- Aspek Biologi DepresiDokumen13 halamanAspek Biologi DepresiRismanto TorsioBelum ada peringkat
- Faktor dan NeurotransmitterDokumen3 halamanFaktor dan NeurotransmitterAl AlfannisyahBelum ada peringkat
- Referat Neurotransmitter Pada Pasien SkizofreniaDokumen24 halamanReferat Neurotransmitter Pada Pasien SkizofreniaDiastri N S DewiBelum ada peringkat
- Refarat Gangguan Psikotik OrganikDokumen9 halamanRefarat Gangguan Psikotik OrganikJezy Reisya100% (1)
- INS_PATOFISIOLOGIDokumen8 halamanINS_PATOFISIOLOGIDeviBelum ada peringkat
- Diagnosis BandingDokumen6 halamanDiagnosis Banding2Idiots G&ABelum ada peringkat
- Pola Tidur Pada Pasien SkizofreniaDokumen4 halamanPola Tidur Pada Pasien SkizofreniaI Putu DiatmikaBelum ada peringkat
- Referat Saraf Yusda Kris Sari WijayaDokumen26 halamanReferat Saraf Yusda Kris Sari Wijayachief_doom8800Belum ada peringkat
- SKIZOFRENIADokumen59 halamanSKIZOFRENIAHerman Purnomo100% (1)
- Dwi Yulianto Li LBM 3 JiwaDokumen23 halamanDwi Yulianto Li LBM 3 JiwaRezki KurniantoBelum ada peringkat
- LBM 6 GANGGUAN JALANDokumen10 halamanLBM 6 GANGGUAN JALANUlin Nuha100% (1)
- Gangguan Psikotik Akibat Kondisi Medis UmumDokumen9 halamanGangguan Psikotik Akibat Kondisi Medis UmumSandri AndeskiBelum ada peringkat
- Nurlaila Halimatussa'diah (170301054) Skizofrenia-Dikonversi PDFDokumen4 halamanNurlaila Halimatussa'diah (170301054) Skizofrenia-Dikonversi PDFRian RiskipatiBelum ada peringkat
- Skizoafektif Tipe DefresifDokumen25 halamanSkizoafektif Tipe Defresifamanthe_richkey0% (1)
- Isi PBL SK 4 Blok 6.2Dokumen74 halamanIsi PBL SK 4 Blok 6.2Fathur RachmanBelum ada peringkat
- PatofisiologiDokumen3 halamanPatofisiologiReni Ramba100% (1)
- MENGAMUKDokumen13 halamanMENGAMUKRio KristianBelum ada peringkat
- SKIZOFRENIA DAN WAHAMDokumen19 halamanSKIZOFRENIA DAN WAHAMHyoranBelum ada peringkat
- LP DepresiDokumen26 halamanLP DepresijusmitaBelum ada peringkat
- Terapi Modalitas PsikiatriDokumen99 halamanTerapi Modalitas PsikiatriAskar Affandy IIBelum ada peringkat
- Otak dan Gangguan JiwaDokumen39 halamanOtak dan Gangguan JiwaMuhamad zainsa asfarBelum ada peringkat
- Gangguan Afektif Bipolar: Definisi, Etiologi, Epidemiologi, dan KlasifikasiDokumen9 halamanGangguan Afektif Bipolar: Definisi, Etiologi, Epidemiologi, dan KlasifikasiRiska MDBelum ada peringkat
- Tugas Faal Sesi 12Dokumen3 halamanTugas Faal Sesi 12izzarBelum ada peringkat
- Otak dan Gangguan JiwaDokumen39 halamanOtak dan Gangguan JiwaHarton MuhammadBelum ada peringkat
- Kesehatan mental dan gangguan psikologis: Apa itu dan bagaimana cara kerjanyaDari EverandKesehatan mental dan gangguan psikologis: Apa itu dan bagaimana cara kerjanyaBelum ada peringkat
- PSIKOLOGI KECEMASAN Mengetahui untuk memahami mekanisme fungsinyaDari EverandPSIKOLOGI KECEMASAN Mengetahui untuk memahami mekanisme fungsinyaPenilaian: 5 dari 5 bintang5/5 (8)
- PSIKOLOGI PERKEMBANGAN ANAK DAN DISTURBILITAS PADA USIA EVOLUTIF: Apa itu dan bagaimana cara kerjanyaDari EverandPSIKOLOGI PERKEMBANGAN ANAK DAN DISTURBILITAS PADA USIA EVOLUTIF: Apa itu dan bagaimana cara kerjanyaBelum ada peringkat
- PLANNING MINIPRODokumen6 halamanPLANNING MINIPROAnizatun NuskiyatiBelum ada peringkat
- Demam Berdarah Dengue DBDDokumen21 halamanDemam Berdarah Dengue DBDAggiFitiyaningsihBelum ada peringkat
- Transfusi Darah PDFDokumen30 halamanTransfusi Darah PDFJabbarTapiheruBelum ada peringkat
- Dokjok - OD Katarak Senilis Insipien+glaukomaDokumen30 halamanDokjok - OD Katarak Senilis Insipien+glaukomaAnizatun NuskiyatiBelum ada peringkat
- Laporan KasusDokumen20 halamanLaporan KasusAnizatun NuskiyatiBelum ada peringkat
- REKOMENDASI Penatalaksanaan Status Epileptikus PDFDokumen17 halamanREKOMENDASI Penatalaksanaan Status Epileptikus PDFzahra nabila latama0% (1)
- Congestive Heart Failure: by Anizatun NuskiyatiDokumen50 halamanCongestive Heart Failure: by Anizatun NuskiyatianizatunBelum ada peringkat
- Kasus Iship Jiwa 1Dokumen44 halamanKasus Iship Jiwa 1Anizatun NuskiyatiBelum ada peringkat
- Post Test RistiDokumen3 halamanPost Test RistiAnizatun NuskiyatiBelum ada peringkat
- Menu Makanan Diet DMDokumen1 halamanMenu Makanan Diet DMAnizatun NuskiyatiBelum ada peringkat
- CacingDokumen1 halamanCacingAnizatun NuskiyatiBelum ada peringkat
- Laporan Kasus Refkas ThalassemiaDokumen10 halamanLaporan Kasus Refkas ThalassemiaAnizatun NuskiyatiBelum ada peringkat
- Ani Atlas HistologiDokumen39 halamanAni Atlas HistologiAnizatun NuskiyatiBelum ada peringkat
- Peningkatan Berat Badan Dan Kadar Trigliserida Serum Pada Orang Yang Diberi Margarin Dipengaruhi Oleh Adanya Kandungan Asam Lemak TransDokumen1 halamanPeningkatan Berat Badan Dan Kadar Trigliserida Serum Pada Orang Yang Diberi Margarin Dipengaruhi Oleh Adanya Kandungan Asam Lemak TransAnizatun NuskiyatiBelum ada peringkat
- Pamflet Kejang DemamDokumen3 halamanPamflet Kejang DemamAnizatun NuskiyatiBelum ada peringkat
- Journal GilutDokumen10 halamanJournal GilutArum DiannitasariBelum ada peringkat
- Anizatun JurnalDokumen10 halamanAnizatun JurnalAnizatun NuskiyatiBelum ada peringkat
- RHINITIS ALERGIDokumen32 halamanRHINITIS ALERGIAnizatun NuskiyatiBelum ada peringkat
- Translate JurdingDokumen13 halamanTranslate JurdingAnizatun NuskiyatiBelum ada peringkat
- Referat StrokeDokumen28 halamanReferat StrokeVerdiana Wilistyanita100% (13)
- Glaukoma AbsolutDokumen34 halamanGlaukoma AbsolutAnizatun NuskiyatiBelum ada peringkat
- Kritik JurnalDokumen25 halamanKritik JurnalIntan ApriliyaniBelum ada peringkat
- Glaukoma AbsolutDokumen29 halamanGlaukoma AbsolutArum DiannitasariBelum ada peringkat
- TranslateDokumen13 halamanTranslateAnizatun NuskiyatiBelum ada peringkat
- Glaukom Post TrabekulotomiDokumen28 halamanGlaukom Post TrabekulotomiAnizatun NuskiyatiBelum ada peringkat
- Laporan Kasus Vertigo FixDokumen48 halamanLaporan Kasus Vertigo FixAnizatun NuskiyatiBelum ada peringkat
- Laporan Kasus Dan CBD Ulil SNHDokumen22 halamanLaporan Kasus Dan CBD Ulil SNHAnizatun NuskiyatiBelum ada peringkat
- Journal Reading Ani AldiDokumen11 halamanJournal Reading Ani AldiAnizatun NuskiyatiBelum ada peringkat
- Laporan Kasus LBP Et Causa Spondilosis LumbalisDokumen12 halamanLaporan Kasus LBP Et Causa Spondilosis LumbalisAnizatun NuskiyatiBelum ada peringkat
- Dops AnizatunDokumen5 halamanDops AnizatunAnizatun NuskiyatiBelum ada peringkat