Lecture 20 Systems Physiology
Diunggah oleh
Robin StewartHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Lecture 20 Systems Physiology
Diunggah oleh
Robin StewartHak Cipta:
Format Tersedia
Lecture 20 Systems Physiology What makes up the brain, the spinal cord or your peripheral nerves?
Neurons are the cell o Cell body o Nucleus o Axon o Dendrite Nervous System Neuron: Structural and functional unit. o Cell Body: metabolic engine for axons o Dendrites: branching extensions of the soma (dendritic tree) Major area of synaptic input o Axon: diameter and length varies with neuron type. Axon hillock- AP is generated 12 o # of Neurons: 10 Neuroglia, or glia: supportive cells, sustain metabolically and physically, isolate individual neurons and help maintain internal milieu 13 o # of Neuroglial cells: 10 Neurons Network O2 binding-protein, neuroglobin Brain uses 20% of total resting O2 and 50% of glucose consumed in the body Brain = 2% of body weight: receives 15%- 20 % of blood pumped out by the heart Brain Damage Occurs o O2 deprivation for 4- 5 minutes o Glucose supply is cut off > 10-15 minutes. o Blood supply to the brain is related to strokes Average # of neurons in the brain = 100 billion # of synapses for a "typical" neuron = 1,000 to 10,000 Heart cells are not exactly muscle cells they have specialized features to be able to process neural information and conduct electrical information Axon hillock: area where the cell body connects with axon Brain requires approx. 3.3mL of O2/ 100g of brain tissue a minute o Body responds to lowered blood oxygen by redirecting blood to the brain & increasing cerebral blood flow o Blood flow may increase to up to 2x as much but no more o If increased flow is sufficient to supply brain's O2 then no further symptoms will result If blood flow cannot increase or if 2x blood flow does not satisfy, symptoms of cerebral hypoxia will appear o Mild symptoms: difficulties w/ complex learning tasks & reduction in short term memory o If O2 deprivations occur: cognitive disturbances, decreased motor control, skin appears bluish (cyanosis) & heart rate increases o After this if O2 deprivation continues: fainting, long term loss of consciousness, coma, seizures, cessation of brain stem reflexes & brain death o Severity of cerebral hypoxia depends on cause Blood oxygen saturation may be used for hypoxic hypoxia but generally meaningless in other forms of hypoxia o Hypoxic Hypoxia: insufficient O2 available to lungs (blocked airway or reduction in partial pressure of lungs) o In hypoxic hypoxia, 95-100% saturation is normal o 91-94% is considered mild o 86-90% is considered moderate & anything below 86% is severe Neuron Consists of: dendrites, a cell body (soma), & an axon with a terminal ending. Dendrites receive input, have a large surface area, & electrical signals are graded and sent to the cell body Soma contains a nucleus, Nissl bodies stacks of ER, golgi, mitochondria, neurofilaments & microtubules o It integrates graded potentials from dendrites Classifications o Structural: Multipolar, Bipolar, & Unipolar o Functional Sensory/Afferent:Inform CNS about conditions in external & internal environment Motor/Efferent: Carry instructions from CNS to effector organs (muscles & glands) Interneurons: Found entirely in CNS Responsible for: Integrating afferent info. and formulating an efferent response & Higher mental functions associated w/ mind
Axonal transport: cellular process responsible for movement of mitochondria, lipids, synaptic vesicles, proteins and other organelles to % from a neuron's cells body through the cytoplasm of its axon Fast axonal transport:100-400 mm/day o Utilizes kinesins, dyneins & microtubules o Actively walks vesicles up or down along microtubule Slow axonal transport: 1- 5 mm/day o Carries enzymes etc. that are not quickly consumed o Utilizes axoplasmic flow 2+ Need energy from glucose & Ca ions for transport to occur Microtubules system to guide the transport by means of cross bridges Motor proteins: kinesin and dynein o Have foot like domains that bind to & move along microtubule o Most dyneins move toward the minus end of tubule and kinesins move in opposite o Kinesin walks along a microtubule, dragging its cellular freight w/ it. Phosphate groups transfer ATP to drive movement Anterograde: from cell body to axon terminals o Kinesin: replenishment of synaptic vesicles and enzymes for the synthesis of neurotransmitters. Retrograde: from axon terminal to cell body o Dynein: recycled vesicles to the soma. Synaptic vesicles utilize fast transport. From the soma of motor neuron to the neuromuscular junction
Neuroglia (AKA glial cells) Unlike neurons, they do not initiate or conduct nerve impulses Do communicate with neurons and among themselves via chemical signals Serve as Connective Tissue of CNS: Physically, metabolically, and functionally support interneurons 4 major types of glial cells in CNS: o Astrocytes: Named for starlike shape (astro = star) Most abundant glial cells Main glue of CNS holds neurons together Guide neurons during fetal brain development Induce capillaries of brain to undergo changes that aid in establishment of blood-brain barrier Important in repair of brain injuries and in neural scar formation Play role in neurotransmitter activity Take up and degrade Glutamate and GABA Take up excess K+ from brain ECF Helps maintain optimal ion conditions for neural excitability Have lots of branches to grab vessels to bring in nutrients Along with other glial cells enhance synapse formation and modify synaptic transmission o Oligodendrocytes: Form myelin sheaths around axons in CNs o Microglia: immune defense cells of CNS (phagocytes) In resting state release low levels of growth factors that help neurons & other glial cells survive and thrive Nerve Growth Factor: helps neurons and glial cells survive o Ependymal cells: Line internal, fluid filled cavities of CNS In ventricles of brain, help form and circulate cerebrospinal fluid with their cilia Serve as neural stem cells w/ potential to form new neurons & glial cells Types of glial cells in PNS o Schwann Cells: form myelin sheath of PNS. 1 Schwann cells wraps 1 neuron o Satellite Cells: in the ganglia & are like astrocytes in that they are positions around the cell body
Fluid Volumes in Humans Total body water = 2/3 body weight o 1 liter H2O = 1 kg o 60%-70% bodys weight = water Variability among individuals amount of adipose tissue % Body water varies with age. o Newborns= 75% o Age of 1 year = 60% Intracellular volume = 2/3 total body water o 40% body weight Extracellular volume = 1/3 total body water o 20% body weight o Interstitial volume = 2/3 extracellular volume = 2/9 total body water o Plasma volume = 1/3 extracellular volume = 1/9 total body water Body water as function of body weight The average urine output for adults is about 1.5 liters (6.3 cups) a day You lose close a liter of water a day through breathing, sweating and bowel movements Food accounts for 20% of your total fluid intake, so if you consume 2 liters of water or other beverages a day (a little more than 8 cups) along with your normal diet, you will typically replace the lost fluids. Weight Content as Percentage of Total Body Weight by Age & Sex "8 x 8 rule" drink 8, 8-oz glasses of water a day (about 1.9 liters) Age Male Female o Approach isn't supported by scientific evidence, many Infant 65% 65% people use this basic rule as a guideline 1-9 62% 62% 10-16 59% 57% Electrolyte concentration in ECF and ICF 17-39 61% 51% Primary ECF cation is sodium & primary ICF cation is potassium. 40-59 55% 47% This difference is maintained by basolateral Na+/K+ ATPases o Transport 3 Na+ out if the cell in exchange for 2 K+ 60+ 52% 46% molecules into the cell.
Functions of Cell Membranes Compartmentalize: providing continuous, relatively unbroken sheets Prevent unrestricted exchange of molecules providing a selectively permeable barrier Contain machinery for physical transport of substances from one side of the membrane to the other Involved in response of the cell to external stimuli via signal transduction Allow cells to recognize one another, to adhere, & exchange materials in an intracellular interaction Provide a means to organize cellular biochemical activities through extensive framework w/in which components can be arranged for effective interaction Maintain cell polarity Involved in process of energy transduction (conversion of 1 type of energy to another) Picture on top: Fluid mosaic model is shown. Plasma membrane is composed of lipid bilayer embedded with proteins. Integral proteins extend through thickness of the membrane or are partially submerged in membrane & peripheral proteins are loosely attached to surface. Short carbohydrate chains attach to proteins or lipids on the outer surface only. Plasma Membrane: Extremely thin layer of lipids and protein that form outer boundary of every cell Controls movement of molecules between the cell and its environment Participated in joining cells to form tissues and organs Plays an important role in the ability of a cell to respond to changes in he cells' environment Structure: Fluid lipid bilayer embedded with proteins o Lipid Bilayer: consists of two sheets of phospholipid molecules oriented in opposite directions The heads of the phospholipids face outward Attracted to water environments inside and outside the cell The hydrophobic phospholipid tails are sandwiched between the heads Minimizes their interactions with water o Most abundant lipids are phospholipids Polar end (Head) is hydrophilic & negatively charged Nonpolar end (Tail) is hydrophobic & uncharged o Contains small amount of carbohydrates on outer surface only o Contains cholesterol tucked between phospholipid molecules Contributed to fluidity & stability of cell membrane o Proteins: attached to or inserted w/in lipid bilayer Span membrane to form water-filled pathways, or channels across lipid bilayer Passive transport protein: channels that passively enable 1 or more substances to cross a membrane Some are always open. Others have molecular gates that close and open in controlled ways Active transport proteins: also called ATPase pumps. Energy provided by ATP makes them pump actively pump Receptor proteins: docks for diverse hormones and other signals. Recognition proteins: are identity tags by which cells recognize non-self and self; located on surface Glycoproteins with sugar side chains projecting above the membrane Adhesion proteins (CAMs): help one cell adhere to another cell or to a protein component of an extracellular matrix Communication proteins: in plasma membrane of one cell match up with identical proteins on another cell Together the proteins form a channel that connects the cytoplasm of the cells and enables communication of signals between them
Distribution of Solutes in Body Depends on: Selective permeability of cell membrane& Transport mechanisms available Water is in osmotic equilibrium (free movement across membranes) Ions and most solutes are in chemical disequilibrium (e.g., Na-K ATPase Pump) o There is an uneven concentration of ions: more sodium outside than inside cell, more potassium inside than outside Electrical disequilibrium between ECF and ICF o Membrane potential The Cerebrospinal fluid (CSF) fills the ventricles of the brain, the spinal canal and the subarachnoid space (and in humans has a total volume of approximately 140 ml) o In humans the choroid plexuses weigh about 2 g in total so that the rate of CSF secretion is approximately 0.2 ml min-1 per g of tissue Membrane Transport Cell membrane is selectively permeable 2 properties of particles influence whether they can permeate cell membrane w/out assistance o Relative solubility of particle in lipid o Size of the particle Assisted: one is more concentrated than the other side (Described in detail later) o Carrier-mediated transport: help substance go through membrane o Facilitated transport: no expenditure of energy o Active transport: energy use Unassisted: Gradient from higher to lower solute concentration o Diffusion Simple Passive Diffusion: uniform spreading out of molecules due to their random intermingling Molecules move from area of high to low concentration Process is crucial to survival of every cells Exchange of O2 and CO2 between blood and air in lungs Movement of substances across kidney tubules o Osmosis: process by which water moves through a semi-permeable membrane from a region of lower solute concentration to a higher 1 Movement of water is down its concentration gradient Water moves freely in body until osmotic equilibium is reached Osmotic pressure: the amount of pressure required to stop the process of osmosis in a system Determined by the # of molecules in that solution Not dependable on size, mass or chemical nature of molecules Opposes movement of water across a membrane Osmotic pressure is calculated by vant Hoffs Law & is measured in atmospheres(atm). = iMRT or = NCRT = osmotic pressure (torr) ( is not equal to 3.14 in this situation) n= number of dissociable particles per molecule C= total solute concentration (molar) R= gas constant (L atm mol1 K1) T= temperature in degrees Kelvin 298K (25 C) Hypertonic or hyperosmotic: Solution with high solute concentration Hypotonic or hyposmotic: Solution with lower solute concentration The cells recovers from a hypotonic or hypertonic shock by ridding or bringing in itself of K+, Cl- & Na+ ions Isotonic or Isosmotic: when internal and external fluids have the same cellular solute concentration Water channels: aquaporins The expression of the aquaporins has not been systematically studied in choroid plexus. However, there is evidence that AQP1 and AQP4 are expressed in this epithelium Mobasheri and Marples (2004) have demonstrated that the choroid plexus exhibits the highest expression of AQP1 of any human tissue using microarray methods AQP1 is likely to have major role in mediating water transport across apical membrane during CSF secretion It has been shown that CSF production is significantly reduced in transgenic mice in which AQP1 has been deleted AQP4 is widely expressed in the brain Next page of pictures show different situations of osmosis
Changes in cell volume in hypertonic, isotonic and hypotonic solutions Dehydration: NaCl solution i.v. --> Rehydration Blood loss: Isotonic NaCl solution i.v -->Restore blood volume
Tonicity: osmotic concentration of solutions administered clinically is generally compared to the osmotic concentration of plasma The osmotic concentration depends on the gram molecular weight of the solute and its dissociability Isotonic Solutions: having the same osmotic concentration as plasma o Administration wont alter intracellular volume. o Solutions containing 300 mOsm of nonpenetrating solute Hypotonic Solutions: having a lesser osmotic concentration than plasma o Administration will tend to expand intracellular volume o Solutions containing <300 mOsm of non-penetrating solute Hypertonic Solutions: having a greater osmotic concentration than plasma o Administration will tend to contract intracellular volume o Solutions containing >300 mOsm of non-penetrating solute Types of Assisted Membrane Transport Current therapeutic drugs act on four main types of molecular targets: enzymes, receptors, ion channels and transporters, among which a major part (6070%) are membrane proteins Carrier-mediated transport: accomplished by membrane carrier flipping its shape o Facilitated diffusion, active & passive transport occur via this o Specificity, Saturation, & Competition determine the kind and amount of material that can be transferred across the membrane Facilitated Diffusion: look at picture below
Active Transport: Moves a substance against its concentration gradient o Requires a carrier molecule o Saturation: there is a maximum amount of transport (all carriers occupied) o Antiport: the ports are in different directions o Uniport (Symport): same direction o Primary active transport: Requires direct use of ATP Energy of ATP is required in phosphorylation - dephosphorylation cycle of the carrier to transport the molecule uphill from a region of low to high region of concentration Primary Active Transporters Names Type of Transport + + Na -K -ATPase or sodium-potassium pump Antiport 2+ Ca -ATPase Uniport + H -ATPase or proton pump Uniport + + H -K -ATPase Antiport Primary Transporter - Ion ATP-ase (Ion Pump): (Na+, K+)-ATPase, in plasma membranes of most animal cells, is an antiport ion pump. It catalyzes ATP-dependent transport of Na+ out of a cell in exchange for K+ entering the cell & created polarity
Secondary active transport: driven by an ion concentration gradient established by a primary active transport system Examples of Secondary Active Transporters Symport Carriers Antiport Carriers Sodium-dependent transporters + + + + Na -K -2Cl (NKCC) Na -H (NHE) + + 2+ Na -glucose (SGLT) Na -Ca (NCX) + Na -Cl + Na -HCO3 + Na amino acids (several types) + Na -bile salts (small intestine) + Na -choline uptake (nerve cells) + Na -neurotransmitter uptake (nerve cells) Nonsodium-dependent transporters + H -peptide symporter (pepT) HCO3 , Cl
Vesicular Transport: Material is moved into or out of the cell wrapped membrane o Active method of membrane transport o 2 types of vesicular transport Endocytosis: process by which substances move into cell Substance is progressively enclosed by an enfolding portion of plasma membrane This forms a vesicle which will pinch off the plasma membrane & enter cytosol where it is digested Pinocytosis (aka bulk-phase endocytosis): nonselective uptake of ECF (picture on left) Literally means cell-drinking A bit of infolding plasma membrane surrounds a droplet of extracellular fluid containing dissolved molecules. This creates a tiny membranous vesicle. Most cells routinely perform this Unlike phagocytosis, pinocytosis is unselective Phagocytosis: selective uptake of multimolecular particle Literally cell-eating (Yellow picture on next page) Cytoplasmic extensions called pseudopods reach out and grab large, solid material such as a clump of bacteria or cell debris, and then engulf it. The resulting vesicle is called a phagosome Usually, the phagosome fuses with a lysosome, a membranous organelle that contains digestive enzymes, and its contents are digested. Macrophages and white blood cells are the most phagocytic cells in the body.
Receptor-mediated endocytosis Molecules that can be taken up via RME are enzymes, hormones, LDL (bad cholesterol), flu viruses & diphtheria toxin Receptors for the molecule to be ingested by a cell are on the PM Different cells have different receptors & thus take up different molecules A macromolecule will bind with its particular receptor & then these receptor macromolecule complexes cluster together, invaginate & are internalized Exocytosis: Provides mechanism for secreting large polar molecules Literally means "out of the cell" Enables cell to pass specific components to membrane Accounts for hormone secretion, neurotransmitter release, mucus secretion, & ejection of wastes o Inside the cell, the substance to be exported is enclosed in a membranous sac called a vesicle. o The vesicle will migrate to the PM fuse with it, and then rupture, spilling the contents into the extracellular space
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- AfCFTADokumen2 halamanAfCFTAeltonBelum ada peringkat
- Clasament CNE#2Dokumen7 halamanClasament CNE#2Dan JurcaBelum ada peringkat
- Cleaning Services for Petrochemical PlantsDokumen24 halamanCleaning Services for Petrochemical PlantstriplbingaziBelum ada peringkat
- Module 4 - Laying of Underground Cables - T&GDokumen42 halamanModule 4 - Laying of Underground Cables - T&GDeepak100% (2)
- Speaking 2024Dokumen6 halamanSpeaking 2024Ngoc KimBelum ada peringkat
- POB Pekerja Demobilisasi Rip 1500 HP - 061121Dokumen3 halamanPOB Pekerja Demobilisasi Rip 1500 HP - 061121didikhartadiBelum ada peringkat
- 3 Wheeler Spare Parts Catalogue for Bajaj, Piaggio & Mohindra ModelsDokumen204 halaman3 Wheeler Spare Parts Catalogue for Bajaj, Piaggio & Mohindra ModelsBhusarapu Srinivas100% (1)
- MAN 6-cylinder D2066 truck enginesDokumen4 halamanMAN 6-cylinder D2066 truck enginesUsman Shah75% (4)
- Senate Hearing, 110TH Congress - Cruise Ship Safety: Examining Potential Steps For Keeping Americans Safe at SeaDokumen84 halamanSenate Hearing, 110TH Congress - Cruise Ship Safety: Examining Potential Steps For Keeping Americans Safe at SeaScribd Government DocsBelum ada peringkat
- Garuda Indonesia e-ticket receipt for domestic flightDokumen2 halamanGaruda Indonesia e-ticket receipt for domestic flightNUR FAUZIAHBelum ada peringkat
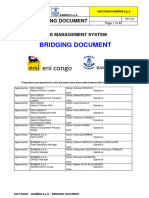
- ENI CONGO - Bambini Spa Bridging DocumentDokumen45 halamanENI CONGO - Bambini Spa Bridging DocumentBitsindouBelum ada peringkat
- Synopsis Online Cruise Ship Tour and Travel AdministrationDokumen20 halamanSynopsis Online Cruise Ship Tour and Travel AdministrationRaj BangaloreBelum ada peringkat
- Student's Lived Experiences Living Far Away From SchoolDokumen38 halamanStudent's Lived Experiences Living Far Away From SchoolCarl Lelis100% (1)
- MCJ 21 Cargo PaySlipDokumen9 halamanMCJ 21 Cargo PaySlipyhanie punioBelum ada peringkat
- Vaccines For Roads: Third EditionDokumen48 halamanVaccines For Roads: Third EditiongoguBelum ada peringkat
- DWCL HS (PhySci) NoApplicDokumen6 halamanDWCL HS (PhySci) NoApplicPRC BoardBelum ada peringkat
- ResumeDokumen3 halamanResumechavanshital855Belum ada peringkat
- Effect of Airline Choice and Temporality On - 2020 - Journal of Air Transport MDokumen19 halamanEffect of Airline Choice and Temporality On - 2020 - Journal of Air Transport MFernanda RojasBelum ada peringkat
- Dialysis ExperimentDokumen3 halamanDialysis ExperimentParis Panganiban BelberBelum ada peringkat
- Ud Quester First GenDokumen17 halamanUd Quester First GenSitichoke SemamonBelum ada peringkat
- Technical Specifications: Hydraulic ExcavatorDokumen12 halamanTechnical Specifications: Hydraulic ExcavatorArvind HarryBelum ada peringkat
- DieDokumen4 halamanDieLino HuaracalloBelum ada peringkat
- Vehicle Inspection Report SummaryDokumen1 halamanVehicle Inspection Report SummaryKanageswary AnandanBelum ada peringkat
- Career Edge - Let's Solve A GuesstimateDokumen13 halamanCareer Edge - Let's Solve A GuesstimateDEVIKA ARUNGUPTA IET Lucknow StudentBelum ada peringkat
- Life Cycle Assessment of Packaging Materials For Milk and Dairy ProductsDokumen12 halamanLife Cycle Assessment of Packaging Materials For Milk and Dairy Productsmanisha maniBelum ada peringkat
- Ground Services Training SchoolDokumen5 halamanGround Services Training SchoolJerome VelascoBelum ada peringkat
- Manual Issue-2 - NewDokumen96 halamanManual Issue-2 - NewGiuro Kralev80% (5)
- Gas BallastDokumen7 halamanGas BallastMiraNurhayaniBelum ada peringkat
- Strength Analysis of Hull Structures in TankersDokumen40 halamanStrength Analysis of Hull Structures in TankersMahdiBelum ada peringkat
- SAMP CHatlogDokumen35 halamanSAMP CHatlogredBelum ada peringkat