Association of Vitamin D Level With Alopecia Areata: Background
Diunggah oleh
randy_suryawan_Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Association of Vitamin D Level With Alopecia Areata: Background
Diunggah oleh
randy_suryawan_Hak Cipta:
Format Tersedia
1
ORIGINAL ARTICLE
Iranian Journal of Dermatology, Vol 16, No 1, Spring 2013
Association of vitamin D level with alopecia areata
Background: Alopecia areata (AA) is an autoimmune disorder of
hair follicles. We aimed to find the association between Vitamin
D level and AA.
Method: Eligible AA patients and controls were enrolled in
this case-control study and serum samples were assessed for
25-hydroxy vitamin D (25-(OH)-D3). The levels of 25-(OH)-D3
were categorized as deficient (<10ng/ml), insufficient (10 to
<30 mg/ml) and sufficient (>30ng/dl) and the SALT (Severity
of Alopecia Tool) score was used to assess the severity of the
disease. The data was analysed and the association between
vitamin D levels and AA, disease distribution, and the pattern
of hair loss was investigated.
Result: Twenty eight patients (19 males, 9 females) and 44
healthy controls (16 males, 28 females) were assessed. There
was no statistically significant difference between patients and
controls with regard to the level of 25(OH)D
3
when the data was
adjusted for gender (Ordinal odds ratio: 0.49 (0.18-1.34 and 95%
CI, p-value=0.16). The level of 25(OH)D
3
was lower in patients
with nail involvement in contrast to those without it (P=0.02);
moreover, no significant difference was found between patients
with different patterns of hair loss.
Conclusion: After adjustment for gender, there was no association
between AA and the level of vitamin D.
Keywords: 25-hydroxyvitamin D3, alopecia areata, severity of alopecia
tool score, vitamin D
Soheila Nassiri, MD
1
Zahra Saffarian, MD
1
Shima Younespour
2
1. Skin Research Center, Shahid
Beheshti University of Medical
Sciences, Tehran, Iran
2. Department of Epidemiology and
Biostatistics, School of Public
Health, Tehran University of Medical
Sciences, Tehran, Iran
Corresponding Author:
Zahra Saffarian, MD
Skin Research Center, Shahid
Beheshti University of Medical
Sciences, Shohada-e-Tajrish Hospital,
Tehran, Iran
E-mail: saffarianz@yahoo.com
Conflict of interest: none to declare
INTRODUCTION
Alopecia areata (AA) is a common inflammation-
induced hair loss disorder that is associated with
increased risk of other autoimmune disorders
1,2
.
Although 0.1 to 0.2% of the general population are
affected
3
, the lifetime risk of disease is estimated
around 2%
4
. Patients in all ages may be affected;
however, the majority of the cases are younger
than 30 years of age. Moreover, the disease is
shown to be more severe in males and those who
are affected in early childhood
5
. AA is a common
comorbidity in patients with rickets; on the other
hand, mutations in vitamin D receptor (VDR),
which is proposed as the underlying cause of
AA in some rickets patients, has highlighted the
importance of vitamin D in the pathogeneses of
this disorder
6
.
Vitamin D is a steroid hormone that primarily
regulates calcium metabolism; it is synthesized
from cholesterol under the effect of ultraviolet on
keratinocytes of the skin and after modification
in the kidney and liver, changes to an activated
form. Calcitriol or 1,25(OH)
2
D
3
is the active form of
vitamin D which bounds to VDR, a member of the
steroid-thyroid-retinoid receptor gene superfamily
of nuclear transcription factors, and regulates the
expression of several genes
6
.
Iran J Dermatol 2013; 16: 1-5
Received: 17 July 2012
Accepted: 19 September 2012
Nassiri et al
2
Iranian Journal of Dermatology
2013 Iranian Society of Dermatology
Although the effect of vitamin D on keratinocytes
and its effect on the pathogenesis of different
dermatologic disorders is studied and reviewed
7,8
,
there is not enough data regarding vitamin D
effects on AA. The aim of this study was to find
the association between AA and level of vitamin D.
PATIENTS AND METHODS
We conducted this case-control study to evaluate
the association of the serum level of vitamin D
and AA in patients attending the dermatology
clinics of Loghman-e-Hakim and Shohada-e-Tajrish
University Hospitals from September 2010 through
March 2012. The study protocol was designed in
accordance with the Declaration of Helsinki and
was implemented after obtaining the approval of
the Ethics Board of Shahid Beheshti University of
Medical Sciences.
Eligible patients were those with at least 10
years of age in whom the diagnosis of AA of the
scalp was made by a dermatologist. As for the
control group, we recruited healthy volunteers who
accompanied patients with different dermatology
problems at their attendance in our clinics.
In both groups, participants with the following
conditions were excluded from the study: taking
vitamin D or calcium supplements, frequent
ingestion of alcohol, gastrointestinal problems,
bone or renal disease, sarcoidosis, or any other
metabolic and systemic disorder that could affect
25(OH)D
3
absorption, metabolism, or serum
level, treatment by systemic or topical steroids,
barbiturates, bisphosphonates, sulfasalazine, or
receiving PUVA or NBUVB during the previous
three months.
A problem in measuring 25(OH)D
3
was the
seasonal changes in its levels; the highest and the
lowest levels are seen at the end of the summer and
at the end of the winter, respectively; Therefore,
the number of controls who were enrolled in each
season was proportionate to the number of patients
enrolled in the same season.
The active form of vitamin D (1,25 (OH)2D3)
is not a good indicator of serum vitamin D levels
due to its short half-life and low serum levels;
instead, the circulating form of vitamin D or 25(OH)
D
3
has a longer half-life and higher serum levels
and is more convenient to measure. Therefore, we
measured 25(OH) D
3
in our study
9
.
Baseline characteristics of the participants of both
groups were documented. In order to assess the
severity of alopecia in patients, our dermatologists
used the SALT (Severity of Alopecia Tool) score,
which is devised by National AA Foundation
working committee
10
. In this scoring system, the
scalp is divided to four areas of vertex, the right
profile of the scalp, the left profile of the scalp, and
the posterior aspect of the scalp which as account
for 40%, 18%, 18%, and 24% of the scalp surface
area, respectively. The SALT score is calculated
by summation of hair loss percentage in these
four areas.
In order to measure 25(OH)D
3
, 3.5 to 5 ml
venous blood was obtained from the antecubital
area by the hospital laboratory technicians while
the participant was in the prone position for 10
minutes. The blood samples were centrifuged
at 3000 rpm and the plasma was collected and
stored at -80C in the lab refrigerator for later
measurement. The samples were sent to a reference
laboratory in a container and after thawing, the
level of 25(OH)D
3
was measured by LIAISON kits
(Diasorin LIAISON, Stillwater, Mn, USA) and
via automated chemiluminescence immunoassay
(CLIA). According to the levels of 25(OH)D
3
, the
status of Vitamin D in the participants was graded
as deficient (<10 ng/ml), insufficient (10 through
<30 ng/ml), and sufficient (30 ng/ml).
All statistical analyses were performed using
the statistical software SPSS 16.0.0. (SPSS Inc.
Chicago, IL, USA). Two-sided P values less than
0.05 were considered statistically significant.
Continuous variables were expressed as meanSD
or as median with total and interquartile (25
th
-75
th
percentiles) ranges. In this study, multivariable
ordinal logistic regression (which considers cut-off
values for 25 (OH) D) was applied to determine
the characteristics associated with the vitamin D
status. The participants were categorized into 3
ordinal categories of vitamin D status: 0 to <10,
10 to <30, and 30 ng/mL. First, unadjusted
ordinal logistic regression models were fitted to
examine the association of vitamin D status with
the participants sex and group status (patients or
healthy controls). Factors for which the unadjusted
odds ratios (ORs) had a P value less than 0.20
were included in the multivariable ordinal logistic
regression model.
The serum concentration of 25 (OH) D was
Association of 25(OH)D
3
with alopecia areata
3
Iranian Journal of Dermatology, Vol 16, No 1, Spring 2013
compared in patients with nail involvement versus
patients with no involvement of nails using the
Mann-Whitney-U test. The Kruskal-Wallis test was
applied to compare the concentration of 25 (OH)
D among the patients with different patterns of
hair loss.
RESULTS
This study included 28 patients with AA (9
women and 19 men) and 44 healthy controls (28
women and 16 men). Baseline demographics and
clinical characteristics of the patients with AA
and healthy controls are summarized in Table 1.
The distribution of participants across the ranges
of 25-hydroxy vitamin D is illustrated in Table 2.
In the unadjusted ordinal logistic regression
models, low 25 (OH) D concentrations were less
likely to be observed in participants who were
male and had AA (P=0.001). In our multivariable
ordinal logistic regression model, the group status
adjusted for participants sex was not statistically
associated with the 25 (OH) D status (p=0.16).
In this study, the serum concentration of 25(OH)
D was significantly lower in patients with nail
involvement when compared to patients with no
involvement of the nails (p=0.02, Mann-Whitney-
U-test). No significant differences were observed
among the patients with different patterns of hair
loss according to their serum concentrations of
25(OH) D (p=0.75, Kruskal-Wallis test). According
to our findings, the median serum concentration
of 25(OH) D was lower in patients with active hair
loss although the difference was not statistically
significant (p=0.07).
DISCUSSION
The levels of vitamin D were lower in controls
in comparison with the patients in this study;
however, no significant difference was detected
25-hydroxy vitamin D
Groups of study Sex <10 ng/mL 10 to <30 ng/mL 30 ng/mL Total
Patients
Male 5 10 4 19
Female 4 4 1 9
Total 9 (31.1%) 14 (50.0%) 5 (17.9%) 28
Healthy controls
Male 4 11 1 16
Female 19 9 0 28
Total 23 (52.3%) 20 (45.4%) 1 (2.3%) 44
Table 2. Distribution of 25-hydroxy vitamin D
Patients with
alopecia
areata
(n=28)
Healthy
controls
(n=44)
Age, years
MeanSD 27.757.97 33.1612.52
Median (range) 27.5 (18-48) 30.5 (10-83)
Gender, no. (%)
Female 9 (32.14%) 28 (63.63%)
Age at onset of disease, years
MeanSD 19.909.65 -
Median (range) 18.5 (4-42) -
Duration of disease, years
Median (range) 6 (0.5-20) -
Subgroups of hair loss duration
<3 months 0 -
312 months 1 (3.57%) -
1224 months 1 (3.57%) -
>25 years 5 (17.86%) -
>5 years 21 (75.00%) -
SALT
score
0-24 6 (21.40%) -
25-49 4 (14.30%) -
50-74 1 (3.60%) -
75-99 0 -
100 17 (60.70%) -
Pattern of hair loss
Patchy 10 (35.70%) -
Totalis 8 (28.60%) -
Universalis 9 (32.10%) -
Ophiasis pattern 1 (3.60%) -
Body hair loss
None 12 (42.86%) -
Some 10 (35.71%) -
100% 6 (21.43%) -
Nail involvement, no. (%) 10 (35.71%) -
Activity of hair loss 14 (50.00%) -
History of PTSD before onset of
disease
10 (35.71%) -
History of thyroid disease 3 (10.71%) -
Family history of alopecia areata 1 (3.57%) 0
History of atopic 8 (28.57%) -
Table 1. Baseline demographics and clinical characteristics of
patients with alopecia areata and healthy controls
* Values are meanSD unless otherwise noted
SALT: Severity of Alopecia Tool Score ranges from 0 to 100, with 0
indicating no alopecia areata and 100 indicating severe disease
Nassiri et al
4
Iranian Journal of Dermatology
2013 Iranian Society of Dermatology
fluctuates with changes in the levels of vitamin
D along with seasonal changes
19
. In addition, the
prevalence of psoriasis is higher toward the poles
and decreases in the areas around the equator
20
and a case-control study demonstrated lower
levels of vitamin D in these patients in contrast
to healthy controls
21
.
AA i s a CD8
+
T l ymphocyt e- dependent
autoimmune disease; in rat models, depleting CD8
+
T-cells leads to hair restoration
22
. Transferring
T-cells from an affected mouse to a normal model
can lead to AA
23
. The collapse of constitute immune
privilege is hypothesized to be the underlying
cause of AA
24
. This hypothesis states that in the
presence of immune signals, other immune system
components, preexisting auto-activated CD8
+
lymphocytes can attack hair follicles
25
. On the other
hand, vitamin D implies its immunomodulatory
effects via its nuclear receptors expressed in antigen-
presenting cells (APCs) and T-lymphocytes
26
. The
rate limiting enzyme in converting 25(OH) D3 to the
active form of vitamin D, namely 1--hydroxylase,
is expressed by macrophages and unlike its renal
form, not only is this enzyme under regulation
of immune system signals but also no negative
feedback is implied by the end product. This
enzyme is also expressed by dendritic cells, another
important APC
27,28
. In dendritic cells, calcitriol
inhibits IL-12 production and hence, suppresses
T-cells activation. In addition, vitamin D can
promote helper T-cells type 2 (Th
2
) proliferation
and increase the production of IL-4, IL-5, IL-10,
interferon-gamma (IF-) in antigen-stimulated CD4
+
T-cells
29
. Therefore, if any association exists between
AA and vitamin D, it would be from the effects
on the immune system and modulation of T-cells
functions rather than the VDR polymorphism.
Our study could neither link the vitamin D
levels to AA nor reject such an association; it
might be to some extent due to the small sample
size and not matching patients for gender. The
levels of exposure to the UV, seasonal changes
and altitude, level of activity, and body mass
index (BMI) should be considered to justify the
level of vitamin D in patients in further studies;
moreover, the gender was a confounding factor
in our study and participants must be matched
for gender. This pilot study was the first study
that examined the association of vitamin D levels
and AA. Further investigation with focus on the
between patients with AA and healthy controls
after adjustment for sex. The proportion of female
participants was 63% and 32% of the patients and
controls, respectively. Lower levels of 25(OH)D
3
were more frequently found in female patients
rather than males in both groups, which is most
likely due to the womens limited exposure to
UV because of religious and regional dress codes.
The role of vitamin D in the pathogenesis of
AA has been a matter of interest for many years;
the evidence has arisen from the reports of AA
in patients with hereditary vitamin D resistant
rickets (HVDRR)
11
; in fact, the mutation of VDR is
demonstrated to be the cause of hair loss in these
patients. On the other hand, the effect of vitamin
D on protecting hair follicles from chemotherapy-
induced alopecia
12,13
provides further evidence for
the role of vitamin D in hair growth and possibly
hair loss; however, this effect also depends on the
applied chemotrapeutic agent
8
. While most of
the studies have investigated the role of vitamin
D in AA in HVDRR, there is limited clinical or
experimental research focusing on the role of
vitamin D in the pathogenesis of AA in the general
population. In contrast to HVDRR, the prevalence
of AA in the general population, the autoimmune
nature of disease, and its reversibility cannot be
explained by a single receptor mutation; that is
to say, there are differences in genotype with
regard to ethnicity
14
. In one study in Turkey, no
relationship was found between AA and VDR gene
polymorphism
15
. Therefore, the mechanism of the
pathogenesis in AA might be the effect of vitamin
D on immune cells rather than changes in VDR.
The associ ati on of vi tami n D l evel s wi th
autoimmune diseases including diabetes mellitus
16
,
systemic lupus erythematosus
17
, and rheumatoid
arthritis
16
has been already investigated. The serum
level of vitamin D has also been assessed in another
autoimmune disease, i.e. vitiligo. In a cohort study,
25(OH) D3 demonstrated bimodal distribution in
vitiligo vulgaris patients; there were some patients
with normal levels while low levels were detected in
others. In addition, they demonstrated incremental
changes in vitamin D levels as the skin complexion
became lighter according to Fitzpatrick skin type
classification
18
. Evidence suggests a relationship
between autoimmune diseases and UV radiation
and therefore vitamin D, with respect to latitude.
For example, the course of multiple sclerosis
Association of 25(OH)D
3
with alopecia areata
5
Iranian Journal of Dermatology, Vol 16, No 1, Spring 2013
immunomodulatory effects of vitamin D in the
pathogenesis or treatment of this disease would
disclose the role of vitamin D in AA.
REFERENCES
1. Barahmani N, Schabath MB, Duvic M, et al. History of
atopy or autoimmunity increases risk of alopecia areata. J
Am Acad Dermatol 2009;61:581-91.
2. Chu SY, Chen YJ, Tseng WC, et al. Comorbidity profiles
among patients with alopecia areata: the importance of
onset age, a nationwide population-based study. J Am
Acad Dermatol 2011;65:949-56.
3. Safavi K. Prevalence of alopecia areata in the First
National Health and Nutrition Examination Survey. Arch
Dermatol 1992;128:702.
4. Finner AM. Alopecia areata: Clinical presentation,
diagnosis, and unusual cases. Dermatol Ther
2011;24:348-54.
5. Xiao FL, Yang S, Liu JB, et al. The epidemiology of
childhood alopecia areata in China: a study of 226
patients. Pediatr Dermatol 2006;23:13-8.
6. Malloy PJ, Feldman D. The role of vitamin D receptor
mutations in the development of alopecia. Mol Cell
Endocrinol 2011;347:90-6.
7. Lehmann B. Role of the vitamin D3 pathway in healthy
and diseased skin--facts, contradictions and hypotheses.
Exp Dermatol 2009;18:97-108.
8. Amor KT, Rashid RM, Mirmirani P. Does D matter? The
role of vitamin D in hair disorders and hair follicle cycling.
Dermatol Online J 2010;16:3.
9. Holick MF. Vitamin D status: measurement, interpretation,
and clinical application. Ann Epidemiol 2009;19:73-8.
10. Olsen EA, Hordinsky MK, Price VH, et al. Alopecia areata
investigational assessment guidelines--Part II. National
Alopecia Areata Foundation. J Am Acad Dermatol
2004;51:440-7.
11. Brooks MH, Bell NH, Love L, et al. Vitamin-D-
dependent rickets type II. Resistance of target organs to
1,25-dihydroxyvitamin D. N Engl J Med 1978;298:996-9.
12. Jimenez JJ, Yunis AA. Vitamin D3 and chemotherapy-
induced alopecia. Nutrition 1996;12:448-9.
13. Wang J, Lu Z, Au JL. Protection against chemotherapy-
induced alopecia. Pharm Res 2006;23:2505-14.
14. Park BS, Park JS, Lee DY, et al. Vitamin D receptor
polymorphism is associated with psoriasis. J Invest
Dermatol 1999;112:113-6.
15. Akar A, Orkunoglu FE, Ozata M, et al. Lack of association
between Vitamin D receptor FokI polymorphism and
alopecia areata. Eur J Dermatol 2004;14:156-8.
16. Liu E, Meigs JB, Pittas AG, et al. Plasma
25-hydroxyvitamin D is associated with markers of the
insulin resistant phenotype in nondiabetic adults. J Nutr
2009;139:329-34.
17. Kamen DL, Cooper GS, Bouali H, et al. Vitamin D
deficiency in systemic lupus erythematosus. Autoimmun
Rev 2006;5:114-7.
18. Silverberg JI, Silverberg AI, Malka E, Silverberg NB. A
pilot study assessing the role of 25 hydroxy vitamin D
levels in patients with vitiligo vulgaris. J Am Acad Dermatol
2010;62:937-41.
19. Visscher BR, Detels R, Coulson AH, et al. Latitude,
migration, and the prevalence of multiple sclerosis. Am J
Epidemiol 1977;106:470-5.
20. Raychaudhuri SP, Farber EM. The prevalence of psoriasis
in the world. J Eur Acad Dermatol Venereol 2001;15:16-7.
21. Orgaz-Molina J, Buendia-Eisman A, Arrabal-Polo MA, et
al. Deficiency of serum concentration of 25-hydroxyvitamin
D in psoriatic patients: A case-control study. J Am Acad
Dermatol 2012; 67:931-8.
22. McElwee KJ, Spiers EM, Oliver RF. In vivo depletion of
CD8+ T cells restores hair growth in the DEBR model for
alopecia areata. Br J Dermatol 1996;135:211-7.
23. McElwee KJ, Freyschmidt-Paul P, Hoffmann R, et al.
Transfer of CD8(+) cells induces localized hair loss
whereas CD4(+)/CD25(-) cells promote systemic alopecia
areata and CD4(+)/CD25(+) cells blockade disease
onset in the C3H/HeJ mouse model. J Invest Dermatol
2005;124:947-57.
24. Paus R, Nickoloff BJ, Ito T. A hairy privilege. Trends
Immunol 2005;26:32-40.
25. Gilhar A, Etzioni A, Paus R. Alopecia areata. N Engl J Med
2012;366:1515-25.
26. van Etten E, Mathieu C. Immunoregulation by
1,25-dihydroxyvitamin D3: basic concepts. J Steroid
Biochem Mol Biol 2005;97:93-101.
27. Overbergh L, Decallonne B, Valckx D, et al. Identification
and immune regulation of 25-hydroxyvitamin D-1-alpha-
hydroxylase in murine macrophages. Clin Exp Immunol
2000;120:139-46.
28. Hewison M, Freeman L, Hughes SV, et al. Differential
regulation of vitamin D receptor and its ligand in
human monocyte-derived dendritic cells. J Immunol
2003;170:5382-90.
29. Lehmann B. The vitamin D3 pathway in human skin and
its role for regulation of biological processes. Photochem
Photobiol 2005;81:1246-51.
Anda mungkin juga menyukai
- Marina Eloi, Daniela Vargas Horvath, João Carlos Ortega, Monica Simon Prado, Luis Eduardo Coelho Andrade, Et AlDokumen2 halamanMarina Eloi, Daniela Vargas Horvath, João Carlos Ortega, Monica Simon Prado, Luis Eduardo Coelho Andrade, Et AlSitha WisesaBelum ada peringkat
- 1472 6890 11 8 PDFDokumen6 halaman1472 6890 11 8 PDFTyaspermataBelum ada peringkat
- Ijn2021 6684276Dokumen6 halamanIjn2021 6684276EdiSusantoAhmadTasiBelum ada peringkat
- The Use of The 25 (OH) D Saliva Test As A Substitute For The 25 (OH) D Serum Test in Healthy PeopleDokumen15 halamanThe Use of The 25 (OH) D Saliva Test As A Substitute For The 25 (OH) D Serum Test in Healthy PeopleRomina DatuBelum ada peringkat
- Comparison of Vitamin D Levels Between Healthy Individuals and Cancer Patients-41195Dokumen6 halamanComparison of Vitamin D Levels Between Healthy Individuals and Cancer Patients-41195yayikyayik9Belum ada peringkat
- Jurnal Hidung 1Dokumen5 halamanJurnal Hidung 1indripatraBelum ada peringkat
- Research ArticleDokumen5 halamanResearch ArticleiwanBelum ada peringkat
- Sindrome Metabolico y Vit D Prasad2015Dokumen34 halamanSindrome Metabolico y Vit D Prasad2015Richard Callomamani CallomamaniBelum ada peringkat
- Artigo Hiv AidsDokumen5 halamanArtigo Hiv AidsViviana Paula SoaresBelum ada peringkat
- Investigacion CanadaDokumen9 halamanInvestigacion CanadaAgustín CerraBelum ada peringkat
- Association Between Vitamin D and Systemic Lupus Erythematosus Disease Activity Index in Children and Adolescents - A Systematic Review and Meta-AnalysisDokumen9 halamanAssociation Between Vitamin D and Systemic Lupus Erythematosus Disease Activity Index in Children and Adolescents - A Systematic Review and Meta-AnalysiswatiBelum ada peringkat
- Vit D3Dokumen6 halamanVit D3Waqar GhoryBelum ada peringkat
- Translate Vit DDokumen3 halamanTranslate Vit DErvin MaulanaBelum ada peringkat
- Assessment of Serum Vitamin D Levels in Children.99825Dokumen5 halamanAssessment of Serum Vitamin D Levels in Children.99825yuliBelum ada peringkat
- Tools For Practice: WWW - Acfp.caDokumen3 halamanTools For Practice: WWW - Acfp.camargui miguel requenaBelum ada peringkat
- Vitamin D in Colombian Patients With Systemic Lupus Erythematosus and Its Correlation With Disease ActivityDokumen8 halamanVitamin D in Colombian Patients With Systemic Lupus Erythematosus and Its Correlation With Disease ActivityHalima DiyahBelum ada peringkat
- Genetic Sequence Variants in Vitamin D Metabolism Pathway Genes, Serum Vitamin D Level and Outcome in Head and Neck Cancer PatientsDokumen8 halamanGenetic Sequence Variants in Vitamin D Metabolism Pathway Genes, Serum Vitamin D Level and Outcome in Head and Neck Cancer PatientsFrancine Rossetti DelboniBelum ada peringkat
- Kadar Kalsium Pada Talasemia Berdasarkan Tingkat Insufisiensi, Defisiensi Dan Normal Vitamin DDokumen10 halamanKadar Kalsium Pada Talasemia Berdasarkan Tingkat Insufisiensi, Defisiensi Dan Normal Vitamin Dtri hutomo yugiBelum ada peringkat
- A Study of Vitamin - D Status in Epileptic Children in Age Group of 2-15 YearsDokumen5 halamanA Study of Vitamin - D Status in Epileptic Children in Age Group of 2-15 YearsRatnaBelum ada peringkat
- Nutrients: Vitamin D and Graves' Disease: A Meta-Analysis UpdateDokumen15 halamanNutrients: Vitamin D and Graves' Disease: A Meta-Analysis Updatedebby claudiBelum ada peringkat
- Vitamin D: Fat-Soluble Vitamins & MicronutrientsDokumen7 halamanVitamin D: Fat-Soluble Vitamins & MicronutrientsMehak SharmaBelum ada peringkat
- Vitamina DDokumen6 halamanVitamina DYuri YasuBelum ada peringkat
- Assessment of Vitamin D Deficiency Level by The Physiological Response of Parathyroid Hormone in Turkish AdultsDokumen8 halamanAssessment of Vitamin D Deficiency Level by The Physiological Response of Parathyroid Hormone in Turkish AdultsOSMAN EVLİYAOĞLUBelum ada peringkat
- Vitamin D: Fat-Soluble Vitamins & MicronutrientsDokumen6 halamanVitamin D: Fat-Soluble Vitamins & MicronutrientsMehak SharmaBelum ada peringkat
- Ijmb 22 71Dokumen4 halamanIjmb 22 71Research OfficeBelum ada peringkat
- Vitamin D Pada Anak EpilepsiDokumen7 halamanVitamin D Pada Anak EpilepsiMad MadBelum ada peringkat
- EBM TerbaruDokumen5 halamanEBM TerbaruTetty PrasetyaBelum ada peringkat
- Jurnal RhinoDokumen7 halamanJurnal RhinoElvienBelum ada peringkat
- Research Article: Fall in Vitamin D Levels During Hospitalization in ChildrenDokumen7 halamanResearch Article: Fall in Vitamin D Levels During Hospitalization in ChildrenAMALIA RAMADANIBelum ada peringkat
- Some Oxidative Stress Related Parameters in Patients With Head and Neck CarcinomaDokumen3 halamanSome Oxidative Stress Related Parameters in Patients With Head and Neck Carcinomaabby_5100% (2)
- Vitamin D Deficiency and Anemia: A Cross-Sectional Study: Original ArticleDokumen6 halamanVitamin D Deficiency and Anemia: A Cross-Sectional Study: Original ArticleMuhammad HidayatBelum ada peringkat
- Study of Serum Vitamin D Levels in Men With Premature Androgenetic AlopeciaDokumen4 halamanStudy of Serum Vitamin D Levels in Men With Premature Androgenetic AlopeciaPedro ConsoliniBelum ada peringkat
- D Inhealth and DiseaseDokumen3 halamanD Inhealth and DiseaseSheila GouveiaBelum ada peringkat
- Efficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..Dokumen5 halamanEfficacy of Supplementary Vitamin D On Improvement of Glycemic Parameters in Patients With Type 2 Diabetes Mellitus A..ariahenkusBelum ada peringkat
- Vitamin D Deficiency in AdultsDokumen15 halamanVitamin D Deficiency in AdultsAnabel Pinedo Carrasco100% (1)
- 2022 Are Serum 25-Hydroxyvitamin D Deficiency and Insufficiency Risk Facttors For The Incidence of DynapeniaDokumen9 halaman2022 Are Serum 25-Hydroxyvitamin D Deficiency and Insufficiency Risk Facttors For The Incidence of Dynapeniamariasol63Belum ada peringkat
- Vitamin D deficiency in Europe: standardized data reveal high prevalenceDokumen12 halamanVitamin D deficiency in Europe: standardized data reveal high prevalencecarlos huertaBelum ada peringkat
- Low Serum 25-Hydroxyvitamin D Concentrations Are Associated With Increased Likelihood of Having Depressive Symptoms Among Japanese WorkersDokumen2 halamanLow Serum 25-Hydroxyvitamin D Concentrations Are Associated With Increased Likelihood of Having Depressive Symptoms Among Japanese WorkersfricotalumewoBelum ada peringkat
- Higher Cord Blood 25-Hydroxyvitamin D - Fix - LGDokumen44 halamanHigher Cord Blood 25-Hydroxyvitamin D - Fix - LGchkdnshBelum ada peringkat
- Oleh Ilham Syifaur Pembimbing Dr. Rahmad Syuhada, Sp. MDokumen20 halamanOleh Ilham Syifaur Pembimbing Dr. Rahmad Syuhada, Sp. MMeta MedianaBelum ada peringkat
- Vitamin D Deficiency in Children With Beta Thallasemia Major and IntermediaDokumen6 halamanVitamin D Deficiency in Children With Beta Thallasemia Major and IntermediaChristian NasirBelum ada peringkat
- Gold Ner 2008Dokumen6 halamanGold Ner 2008Matej MatejBelum ada peringkat
- Risk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpDokumen12 halamanRisk Factors of Vitamin D Deficiency in Children With Epilepsy Taking Anticonvulsants at Initial and During Follow-UpSari MustikaBelum ada peringkat
- Association of Vitamin D Status and Acute RhinosinusitisDokumen6 halamanAssociation of Vitamin D Status and Acute RhinosinusitisnicloverBelum ada peringkat
- Status of Red Blood Cell Indices in Iron Deficiency Anemia and B A Comparative StudyDokumen6 halamanStatus of Red Blood Cell Indices in Iron Deficiency Anemia and B A Comparative StudyKishor Chandra PalBelum ada peringkat
- Vitamin D Deficiency 2011Dokumen20 halamanVitamin D Deficiency 2011Emilia CavalittoBelum ada peringkat
- Postoperative HypocalsemiaDokumen6 halamanPostoperative HypocalsemiaAdinda PasaribuBelum ada peringkat
- GAUGRIS Vitamin D InadequacyDokumen10 halamanGAUGRIS Vitamin D InadequacyDwikani Oklita AnggirulingBelum ada peringkat
- Association Between Serum Vitamin D Deficiency and Knee OsteoarthritisDokumen5 halamanAssociation Between Serum Vitamin D Deficiency and Knee OsteoarthritisMuhammad Bayu Zohari HutagalungBelum ada peringkat
- 2022 - ALIZADE - Effects of Age, Sex, Breed, Diet, Reproductive Status and Housing Condition Ontheamountsof 25 (OH) Vitamind Inthe Serumofhealthydogs ReferencevaluesDokumen7 halaman2022 - ALIZADE - Effects of Age, Sex, Breed, Diet, Reproductive Status and Housing Condition Ontheamountsof 25 (OH) Vitamind Inthe Serumofhealthydogs Referencevaluescnicipor4873Belum ada peringkat
- Detection of Some Antioxidant Markers in Saliva of Patients With Beta Thalassemia MajorDokumen11 halamanDetection of Some Antioxidant Markers in Saliva of Patients With Beta Thalassemia MajorReshmaa RajendranBelum ada peringkat
- Vitamin D Levels in Children Diagnosed With Acute Otitis MediaDokumen5 halamanVitamin D Levels in Children Diagnosed With Acute Otitis MediamuthiafadhilahBelum ada peringkat
- Comparative Evaluation of Blood Parameters in Chronic Periodontitis Patients and Healthy Patients For Signs of AnemiaDokumen7 halamanComparative Evaluation of Blood Parameters in Chronic Periodontitis Patients and Healthy Patients For Signs of AnemiaInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Jurnal 3Dokumen7 halamanJurnal 3Fida NadhirBelum ada peringkat
- s 1368980016001762 ADokumen10 halamans 1368980016001762 Atihemex618Belum ada peringkat
- Vitamin D May Influence Risk of Thyroid DiseasesDokumen6 halamanVitamin D May Influence Risk of Thyroid Diseasesdebby claudiBelum ada peringkat
- Jcrpe 1 266Dokumen5 halamanJcrpe 1 266ASADBelum ada peringkat
- Complementary and Alternative Medical Lab Testing Part 19: MiscellaneousDari EverandComplementary and Alternative Medical Lab Testing Part 19: MiscellaneousBelum ada peringkat
- Complementary and Alternative Medical Lab Testing Part 16: HematologyDari EverandComplementary and Alternative Medical Lab Testing Part 16: HematologyBelum ada peringkat
- Complementary and Alternative Medical Lab Testing Part 13: DermatologyDari EverandComplementary and Alternative Medical Lab Testing Part 13: DermatologyPenilaian: 5 dari 5 bintang5/5 (4)
- Jurnal RandyDokumen28 halamanJurnal Randyrandy_suryawan_Belum ada peringkat
- Capter 2.1 (Tugas Genetika)Dokumen5 halamanCapter 2.1 (Tugas Genetika)randy_suryawan_Belum ada peringkat
- Chromosome ReplicationDokumen38 halamanChromosome Replicationrandy_suryawan_Belum ada peringkat
- Chromosome ReplicationDokumen38 halamanChromosome Replicationrandy_suryawan_Belum ada peringkat
- LipidDokumen65 halamanLipidrandy_suryawan_Belum ada peringkat
- Anak Undecensus TestisDokumen45 halamanAnak Undecensus Testisrandy_suryawan_Belum ada peringkat
- 1 WhoDokumen37 halaman1 Whorandy_suryawan_Belum ada peringkat
- Anak Undecensus TestisDokumen45 halamanAnak Undecensus Testisrandy_suryawan_Belum ada peringkat
- Chapter 7 - DNA To Protein - 2Dokumen71 halamanChapter 7 - DNA To Protein - 2randy_suryawan_Belum ada peringkat
- Second Announcement JASS RevisiDokumen28 halamanSecond Announcement JASS RevisiPoco BlueBelum ada peringkat
- Another 365 Things That People Believe That Aren't TrueDokumen85 halamanAnother 365 Things That People Believe That Aren't TrueMohaideen SubaireBelum ada peringkat
- PREBORD NLE8part1Dokumen671 halamanPREBORD NLE8part1Bryan NorwayneBelum ada peringkat
- Asthma and COPDDokumen79 halamanAsthma and COPDDawit g/kidanBelum ada peringkat
- Deviated Nasal Septum: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarDokumen13 halamanDeviated Nasal Septum: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarSuhas IngaleBelum ada peringkat
- CDC Boys 0 - 36 Mths - Length-For-AgeDokumen1 halamanCDC Boys 0 - 36 Mths - Length-For-AgepmverlaanBelum ada peringkat
- Dr. F. BatmanghelidjDokumen18 halamanDr. F. BatmanghelidjSilas Yenbon SebireBelum ada peringkat
- 2 Anatomy of TMJDokumen117 halaman2 Anatomy of TMJSugandhi PidaparthiBelum ada peringkat
- Cerebellar SyndromeDokumen3 halamanCerebellar SyndromePirasan Traditional Medicine CenterBelum ada peringkat
- Essentials 4eDokumen874 halamanEssentials 4eJehada AbdukadilBelum ada peringkat
- How acupuncture points modulate autonomic functionDokumen2 halamanHow acupuncture points modulate autonomic functionTrung Hiệp ĐàoBelum ada peringkat
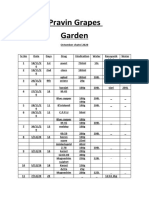
- Pravin Grapes Garden Octomber chatni 2020 recordsDokumen9 halamanPravin Grapes Garden Octomber chatni 2020 recordsPravin ShindeBelum ada peringkat
- Benzene MSDSDokumen12 halamanBenzene MSDSTom Jose KooduthottiyilBelum ada peringkat
- When I hear the noiseDokumen2 halamanWhen I hear the noiseh00nguy0n-18Belum ada peringkat
- Module Essential Newborn CareDokumen26 halamanModule Essential Newborn CareMichtropolisBelum ada peringkat
- Societe Belge de Biochimie Et de Biologie Moleculaire Belgische Vereniging Voor Biochemie en Moleculaire BiologieDokumen30 halamanSociete Belge de Biochimie Et de Biologie Moleculaire Belgische Vereniging Voor Biochemie en Moleculaire BiologieAmirBelum ada peringkat
- Heart Rate Analysis (R)Dokumen72 halamanHeart Rate Analysis (R)Raja LakshmiBelum ada peringkat
- The Logframe ApproachDokumen28 halamanThe Logframe ApproachashkuchiyaBelum ada peringkat
- Main PDFDokumen3 halamanMain PDFAlmira RahmaBelum ada peringkat
- Ocumentation: Analysis of The Situation and Trends in Sunscreen ProductsDokumen4 halamanOcumentation: Analysis of The Situation and Trends in Sunscreen ProductsEvelyn GómezBelum ada peringkat
- Thesis OphthalmologyDokumen7 halamanThesis OphthalmologyJames Heller100% (2)
- Dr. Sterling Clarren Retirement AnnouncementDokumen1 halamanDr. Sterling Clarren Retirement AnnouncementfasdunitedBelum ada peringkat
- Manual Lab Audiology - For StudentDokumen12 halamanManual Lab Audiology - For StudentAnnisa Alifia AksaniBelum ada peringkat
- Bioinformatics PaperDokumen8 halamanBioinformatics PaperrashigaurBelum ada peringkat
- Invasive Ductal CarcinomaDokumen51 halamanInvasive Ductal CarcinomaGiselle Eclarino100% (2)
- Routine Medical Checkup PublicationDokumen11 halamanRoutine Medical Checkup Publication백만호Belum ada peringkat
- AnginaDokumen16 halamanAnginaMc_Lopez_1761Belum ada peringkat
- Pill CameraDokumen21 halamanPill CameraAnil DsouzaBelum ada peringkat
- Report 1Dokumen114 halamanReport 1sirsinto100% (1)
- Recombinant DNA: Advancing Medicine and AgricultureDokumen2 halamanRecombinant DNA: Advancing Medicine and AgricultureJay PeeBelum ada peringkat