AntibioticGuidelines Primary
Diunggah oleh
Handriyato SukmaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
AntibioticGuidelines Primary
Diunggah oleh
Handriyato SukmaHak Cipta:
Format Tersedia
Antibiotic Guidelines for
Primary Care
West Coast District Health Board 2013
_____________________________________________________
PREPARED BY: WCDHB Infection Control Committee 2009
REVIEWED AND UPDATED BY: WCDHB Infection Control Committee September 2013
Source of Guidelines
These guidelines are based on 2012 West Coast District Health Board antibiotic susceptibility
statistics, the Australian 2011 Antibiotic Guideline, BPAC Antibiotics choices for common
conditions 2013 edition and local availability. They have been reviewed by WCDHB clinical and
pharmacy staff, Dr Anja Werno Medical Microbiologist Canterbury Health Laboratories and Dr
Holt Chairman of the Infection Control committee. The guidelines are endorsed by the West
Coast Primary Health Organisations and co-ordinate with WCDHB inpatient guidelines
Oral versus parenteral (IV, IM) antibiotics
Oral therapy is generally preferred. Exceptions include:
The patient cannot take anything orally (e.g., swallowing problems) or is unlikely to
absorb the antibiotic (e.g., vomiting, severe diarrhea)
An oral antibiotic with suitable spectrum is not available
High doses are required for difficult sites of infection (e.g., endocarditis, meningitis,
osteomyelitis, septic arthritis)
Urgent treatment for severe or rapidly progressive infection
The patient is unlikely to adhere to oral therapy
Penicillin and cephalosporin cross-reactivity
There is a 3-10% cross-reaction rate between penicillins and cephalosporins.
If a patient has a mild penicillin allergy or adverse reaction (e.g., mild rash, diarrhea)
then you may prescribe a cephalosporin (and vice versa)
If a patient has a severe penicillin allergy (e.g., severe rash, urticaria, angioedema,
anaphylaxis, hypotension or bronchospasm) then do not prescribe a cephalosporin
(and vice versa).
Infection Prevention & Control
Hand Hygiene as per the World Health Organization 5 moments of hand hygiene
1. Before Patient Contact
2. Before a Procedure
3. After a Procedure or Body Fluid Risk
4. After Patient Contact
5. After Contact with a Patients Surroundings
Wear non sterile gloves and apron if having patient contact with infected skin or if a multi-drug
resistant organism (e.g., MRSA) is suspected or known.
Wear a surgical mask within 1 metre of a patient with droplet-transmitted infection, such as
meningococcal, whooping cough or influenza infection.
Wear a NIOSH certified N95 respirator mask when having contact with a patient with suspected
or confirmed airborne- transmitted infection, such as TB or chicken pox.
Antibiotic Guidelines Empiric Choices
Infection First choice Alternatives Comments
Bites animal or
human
Amox/clavulanate
625mg (child:
10mg Amoxycillin
/kg/dose) tds for 7
days
Metronidazole
plus either
Doxycycline
1
or
Cotrimoxazole
3
Prophylaxis for 5 days with same
antibiotics if bite 8 hours ago; wound
unable to be debrided adequately;
wound on hands, feet or face; involves
bone, joint or tendon; or in
immunocompromised person. Debride
non-viable tissue. Consider tetanus
toxoid. Refer if joint involved.
Blastocystis
hominis
gastroenteritis
Nil As for giardiasis
Usually a non-pathogenic commensal
ignore. If persistent diarrhea, where no
other cause found, give trial of therapy
Boils
Flucloxacillin
500mg (child:
12.5mg/kg/dose)
qds for 5-7days
Erythromycin; if
MRSA: consider
Cotrimoxazole
(only if sensitive)
Small lesions can be treated with
drainage alone. If recurrent (e.g., more
than 10 boils over more than 3 months)
consider decolonization
Bordetella
pertussis
See Whooping cough
Breast post-
partum mastitis or
abscess
Flucloxacillin
500mg qds for 7
days
Erythromycin
400mg qds for 7
days or
Cephalexin
500mg qds for 7
days
Continue breastfeeding throughout
infection. If fail, swab for Candida
Breast non-
puerperal infection
Amox/clavulanate
625mg tds 7 days
Clindamycin
2
Sub-areolar infections usually involve
anaerobes
Bronchiolitis
under 1 yr or
wheezy bronchitis
in children
Nil RSV and other viruses are the cause.
Exclude from pre-school/ school until
coryzal phase is over
Bronchitis
acute in adults, no
underlying lung
disease
Nil Most cases viral. Purulent sputum alone
is not an indication for antibiotics. Give
antibiotics if bacterial infection
diagnosed in laboratory or for patients
with severe infection, underlying medical
co-morbidity or advanced age
1. Doxycycline: do not use in children under 12 years, in pregnancy after 16 weeks gestation or if
breastfeeding
2. Clindamycin: subsidized only with specialist endorsement; please consult in individual case.
3. Cotrimoxazole: do not use in pregnancy
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Bronchitis
exacerbation in adults with
COPD
Amoxycillin 500mg
TDS for 5 days
Doxycycline
1
200mg stat then
100mg daily for 4
days
Campyl obacter
gastroenteritis treat only if
severe or prolonged
Nil usually self-
limited
Erythromycin
Ethyl Succinate
(EES) 400mg
(child: 10 mg/kg)
qds for 5 days
Treatment only if severe or
prolonged; may also be justified
in late (third trimester)
pregnancy or in food handlers
and childcare workers.
Notifiable
Candida vulvo-vaginal
or oral thrush
Topical azole or
Nystatin
Fluconazole
2
150mg single
dose (vulvo-
vaginal) or 100mg
daily for 7-14
days (oral)
If recurrent vulvo-vaginal thrush
(4 or more symptomatic
episodes/yr), induce remission
with topical azole or oral
Fluconazole 50mg daily (takes 2
wk to 6 mo) then maintain with
weekly vaginal cream or oral
Fluconazole 150 to 300mg.
Treat partner
Cellulitis
Flucloxacillin
500mg qds for 7 to
10 days (child: 100
mg/kg/day)
Erythromycin
Keep affected area elevated. Do
not use NSAIDs (increased risk
of necrotizing fasciitis)
Cellulitis periorbital in
child
Amox/clavulanate
(child:75-100mg/kg
per day)
Cefaclor Refer to Paediatrician in all but
very mild cases
Cellulitis periorbital in
adult or in any age if
associated with stye,
dacryocystitis, impetigo or
wound
Flucloxacillin
Cefaclor Seek specialist advice
urgently
Chlamydia and other
non-gonococcal urethritis or
cervicitis
Azithromycin 1g
(10mg/kg for
children) single
dose
Doxycycline
1
100mg BD for 7
days
Erythromycin (500mg QID for 7
days then test for cure after 3
weeks) has an A safety rating
in pregnancy; Azithromycin is
B1 BPAC Amoxycillin 500mg tds for
7days in pregnancy d/w O&G
Clostridium difficile -
toxin-positive diarrhea
Metronidazole
400mg (child 10
mg/kg) orally TDS
for 7-10 days
Stop other antibiotics is possible.
Avoid anti-diarrhoeals. If
unresponsive, relapsing or
severe, consult specialist
Common cold upper
respiratory tract viral
infection
Nil Antibiotics do not prevent
bacterial infection. Nasal
purulence does not predict
response to antibiotics
1. Doxycycline: do not use in children under 12 years; in pregnancy after 16 weeks gestation or if breastfeeding
2. Fluconazole: do not use in pregnancy. 150mg stat needs endorsement with vaginal candidiasis, other
regimens need specialist endorsement
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Conjunctivitis
See Topical - conjunctivitis
COPD
See Bronchitis exacerbation
in patients with COPD
Dental infections
See Tooth abscess or
Gingivitis
Diabetic foot
infections
Amox/clavulanate
625mg tds for 7
days
Clindamycin
2
plus
Ciprofloxacin
3
Refer all foot ulcers for
hospital assessment. Bone
infection more likely if ulcer
>2cm
2
, positive probe to bone,
ESR >70, substantially raised
CRP or abnormal plain X-ray
Topical azole,
Oral Terbinafine
6
,
oral Itraconazole
1
Oral treatment indicated if
culture-proven and has either
failed topical treatment, is
widespread, involves scalp or
nail or is being treated with
concomitant topical steroid
Dientamoeba fragilis
gastroenteritis
Doxycycline
4
100mg (child >12
yrs: 2.5 mg/kg)
BD for 3 to 7 days
Metronidazole 400mg
(child: 10mg/kg) TDS
for 3 to 7 days
Treat only if symptomatic.
Epiglottitis
Refer for hospital assessment
Gastroenteritis
acute, cause unknown
Nil Fluid replacement is mainstay
of treatment. Exclude from
pre-school, school or work
until symptoms settle. Some
causes are notifiable and a
few may benefit from antibiotic
treatment see individual
organisms
Giardiasis
Metronidazole 2g
(child: 30mg/kg)
orally daily for 3
days
Ornidazole 1.5g
(child: 40mg/kg) in
evening for 1-2 days
Treat only if symptomatic. If
fails, try Metronidazole 400mg
(child: 10mg/kg) TDS for 7
days. Notifiable
Gingivitis
acute ulcerative (trench
mouth, Vincents disease)
Metronidazole
400mg (child:
10mg/kg) BD for
5 days
Antibiotics are only an adjunct
to debridement, plaque control
and chlorhexidine mouthwash
(e.g., Rivacol) BD or TDS.
Consider HSV
Gonorrhoea
Ciprofloxacin
3
500mg orally as
single dose
Ceftriaxone
5
250 mg
IM if acquired in
Auckland or overseas
or if pharyngeal or
ano-rectal infection
Treat for Chlamydia as well
1. Itraconazole: use with caution in pregnancy. Subsidized only with specialist endorsement;
2. Clindamycin: subsidized only with specialist endorsement; please consult in individual case
3. Ciprofloxacin: use with caution in children under 14 years and in pregnancy
4. Doxycycline: do not use in children under 12 years, in pregnancy after 16 weeks gestation or breastfeeding
5. Ceftriaxone: subsidized on prescription or PSO for ciprofloxacin-resistant gonorrhoea
6. Terbinafine: B1 classification in pregnancy
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Influenza
NIL antibiotics,
may consider
Tamiflu (Oseltamivir)
1
75mg BD for 5 days
Treat only if onset 48 hr.
Avian or pandemic influenza
is notifiable
Laryngitis/Croup
Nil Almost always viral
Leptospirosis
Penicillin for 5-7 days Doxycycline
2
100mg BD for 5-7 d
Start within 1 wk of onset.
Notifiable
Mastitis
See: Breast
Meningococcal
infection, meningitis or
severe sepsis prior to
transport to hospital
Ceftriaxone
3
50 mg/kg up to 2g IV
or IM
Adult: Penicillin
1.2g IV or IM
Child: Penicillin 25-
50mg/kg IV or IM
Give if haemorrhagic rash in
febrile person or in a
suspected case in whom the
delay to assessment in
hospital is likely to be greater
than 30 minutes. Notifiable
Otitis media
See Comments Antibiotics
NOT usually indicated
Amoxycillin 40-80
mg/ kg/day in 2 to 3
divided doses for 5
days (7-10 days if <2
yr, underlying
medical condition,
perforated drum or
chronic or recurrent
infection)
If fails or persists
try Amoxycillin/
clavulanate.
If penicillin-allergic
use Erythromycin
or Cefaclor 10
mg/kg up to 250
mg TDS for 5 days
Spontaneous resolution
common. Benefit of
antibiotics is small; consider
if under 2 yr or with bilateral
or severe infection. For
others, educate and give
paracetamol and antibiotic
prescription to redeem if
unresolved at 48-72 hrs
Pharyngitis/ tonsillitis
see comments before
deciding to treat
Penicillin 500mg
(child: 10mg/kg) BD
for 10 days or
Amoxycillin child
<30kg 750mg daily;
child >30kg 1500mg
daily for 10 days
Erythromycin
400mg (child
20mg/kg/dose) BD
for 10 days
Usually viral. Give antibiotics
only if:
Key features of group A
strep. Infection (fever >
38 0C, tender cervical
nodes, tonsillar exudates
and no cough), esp. if
aged 3 to 14 yrs. If
uncertain, swab throat
Patient aged 2 to 25 yrs
and high risk group for
rheumatic fever (Maori or
Pacific Islander from
Northland, Hawkes Bay,
Counties/Manukau, Waikato
Gisborne, or Bay of Plenty)
Existing rheumatic heart
disease (treat at any age)
Scarlet fever (Notifiable)
?peritonsillar abscess
(trismus, refer to hospital)
Exclude from school until 24
hrs after antibiotics started.
1. Oseltamivir: use with caution in pregnancy; not subsidized
2. Doxycycline: do not use in children under 12 years in pregnancy after 16 weeks gestation or breastfeeding
3. Ceftriaxone: subsidized for prescription or PSO for suspected meningitis
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Pneumonia child ( >4
months to 15 yr)
Amoxycillin 25
mg/kg TDS for 7
days (Maximum of
500mg/dose if <5
yrs; 1000mg/dose if
>5 yrs)
If penicillin allergy or
no response in 48 hr
review diagnosis and
consider
Erythromycin
10mg/kg/dose QDS
for 7 days
If <5yrs, most are viral. In a
young child, suspect
pneumonia if tachypnoea,
grunting, indrawing and high
fever in absence of wheeze
(auscultatory findings
uncommon) If <4 months,
seek advice
Pneumonia adult,
suspect aspiration
Amox/clavulanate
for 7 days
Clindamycin
2
Prophylaxis for
endocarditis in patients with
heart valve lesions prior to
dental procedures or
tonsillectomy/adenoidectomy
See:
http://www.heartfoundation.o
rg.nz/uploads/Infective%20E
ndocarditis%20Guide(3).pdf
Prostatitis acute
As for UTI - cystitis
in adult men (treat
for 2 wks)
Consider checking for STI
pathogens
Prostatitis chronic
Norfloxacin
3
400mg
BD for 4 weeks, or
Ciprofloxacin
4
500mg orally BD
for 4 weeks
Trimethoprim 300mg
daily for 4 weeks, or
Doxycycline
1
200mg
orally BD for 4 weeks
90% of chronic prostate pain
not due to infection and has
no proven treatment avoid
repeated courses of empiric
antibiotics. Test urine and
expressed prostate
secretions and treat it
possible. Consider STIs
Pyelonephritis
See UTI - pyelonephritis
Ringworm
See Dermatophytoses
Salivary gland
infection acute
bacterial/suppurative
Flucloxacillin
500mg (child
12.5mg/kg/dose)
QID for 10 days
Cefaclor,
Clindamycin
2
Typically in elderly and
neonates usually
Staphylococcus aureus. May
need surgical drainage
1. Doxycycline: do not use in children under 12 years, in pregnancy after 16 weeks gestation or breastfeeding
2. Clindamycin: subsidized only with specialist endorsement; please consult in individual case
3. Norfloxacin: use with caution in children under 14 years and in pregnancy. More than 6 tablets subsidized
only with specialist endorsement; please consult in individual case
4. Ciprofloxacin: use with caution in children under 14 years and in pregnancy.
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Salmonella
gastroenteritis only if
severely ill or
immunocompromised
Cotrimoxazole
1
960mg (child
24mg/kg) BD for 3-5
days
Ciprofloxacin
4
500mg daily for 7-
10 days (14 days if
immuno-
compromised)
Antibiotics generally make
no difference to outcome
and may prolong infectivity.
Some treat if <1 yr, >50 yr,
vascular grafts or prosthetic
joint. Notifiable
School sores
See Topical section
Septicaemia or
overwhelming infection
See Meningitis (for empiric
antibiotics prior to urgent
transfer)
Shigella gastroenteritis
Cotrimoxazole
1
if
susceptible 960mg
(child: 24 mg/kg) BD
for 5 days)
Norfloxacin
2
400mg
(child: 10 mg/kg)
BD for 5 days
Treat all cases. Use
Ciprofloxacin if
immunocompromised.
Notifiable
Sinusitis acute
See Comments Antibiotics
NOT usually indicated use
analgesia, saline spray or
douches, intranasal steroids
and decongestants
Amoxycillin 500mg
(child: 15mg/kg) TDS
for 5 to 7 days
If fails, try Amox/
clavulanate for 7 to
14 days
Cefaclor 500mg
(child: 10mg/kg)
TDS for 5 to 7 days
or Doxycycline
3
100mg (child >
12yr: 2.5 mg/kg)
daily for 5 to 7 days
Consider antibiotics only
if 3 of:
Mucopurulent nasal drip
for 7days
Facial pain
Tenderness over the
sinuses, esp. unilateral
Maxillary tenderness
Tenderness on
percussion of upper
teeth (which cannot be
attributed to a single
tooth)
Thrush
See Candida
Tinea
See Dermatophytoses
Tonsillitis
See Pharyngitis
Tooth abscess
superficial (involving canine
or buccal space)
Penicillin 500mg
(child 10mg/kg) QID
for 5 days
If unresponsive add
Metronidazole or use
Amox/clavulanate
If penicillin allergic
use Clindamycin
5
alone
Antibiotic treatment is only
an adjunct to an appropriate
dental procedure. Give
antibiotics only if face
swelling, systemic symptoms
or fever. If spread to neck,
hospitalize
Travelers diarrhea
Norfloxacin
2
800mg
(child 20mg/kg)
single dose
Norfloxacin
2
400mg
(child 10mg/kg) BD
for 2 to 3 days
Many causes, especially
enterotoxigenic E. coli.
Antibiotics only for moderate
to severe cases. Antimotility
agents indicated in adults
without fever or bloody
stools
1. Cotrimoxazole: do not use in pregnancy
2. Norfloxacin: use with caution in children under 14 years and in pregnancy. More than 6 tablets subsidized
only with specialist endorsement; please consult in individual case
3. Doxycycline: do not use in children under 12 years, in pregnancy after 16 weeks gestation or breastfeeding
4. Ciprofloxacin: use with caution in children under 14 years and in pregnancy
5. Clindamycin: subsidized only with specialist endorsement; please consult in individual case.
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Trichomoniasis
Metronidazole 2g
single dose
If relapse, use Metronidazole
400mg BD for 7 days. Treat
partners
Tuberculosis
See comment Refer for hospital assessment
Notifiable on suspicion
Ulcers leg or foot,
acute infection (excessive
purulent discharge,
redness and pain
Flucloxacillin Erythromycin Increase local cares (lavage,
debridement, absorptive
dressings); consider
cadexomer iodine or silver
dressings. Swab if
Flucloxacillin fails
Ulcers leg or foot,
possible low-grade,
chronic infection (purulent
discharge, non-healing)
Regular dressing
changes,
cadaxemar iodine
or silver
dressings,
debridement
If fails, take a swab to
guide antibiotic choice.
Cleanse/wipe with saline
to remove secretions
before swabbing
The presence of bacteria on
superficial swabs does not
alone indicate a need for
antibiotics. It no leucocytes on
microscopy, infection much
less likely
Urinary tract
infection cystitis in
adult women
Trimethoprim
1
300 mg/d for 3
days
Nitrofurantoin
3
50 mg
QID for 5 days
Asymptomatic bacteriuria
common in elderly women;
treat if pregnant, renal
transplant or pre- or post-
urological procedure.
In pregnancy, repeat urine
culture to ensure cure
Urinary tract
infection cystitis in
adult men
Trimethoprim
1
300 mg/d for 7
days
Nitrofurantoin 50 mg QID
for 7 days
Often underlying urinary tract
abnormality or co-existent
prostatitis or epididymitis.
Investigate all males with UTI
for underlying anatomical or
functional abnormality
Urinary tract
infection pyelo-
nephritis; mild with low
fever and no nausea or
vomiting
Amox/clavulanate
500+125 mg TDS
for 10-14 days
Cotrimoxazole
1
960mg
BD for 10-14 days, or
Cefaclor 500mg TDS for
10-14 days
Identify underlying anatomical
or functional abnormalities,
especially obstruction. If
moderate severity or resistant
organisms, use Ciprofloxacin
500mg BD for 10-14 days. If
severe or vomiting refer for IV
treatment
Urinary tract
infection indwelling
catheter
Amox/clavulanate
500+125 mg TDS
for 10-14 days if
cant wait for
results of culture
Norfloxacin
2
Asymptomatic bacteriuria and
pyuria are common and should
not be treated. Culture urine
and treat only if febrile or
rigors, patient has risk factors
(e.g., neutropenia,
transplantation, pregnancy) or
before urological surgery.
Treat for 10 to 14 days.
Always change catheter
1. Cotrimoxazole (or trimethoprim alone): do not use in pregnancy
2. Norfloxacin: use with caution in children <14 yr; do not use in pregnancy. More than 6 tablets subsidized
only with specialist endorsement; please consult in individual case.
3. Nitrofurantoin: avoid at 36+weeks pregnancy or in significant renal impairment.
Antibiotic Guidelines Empiric Choices (continued)
Infection First choice Alternatives Comments
Urinary tract
infection - child
Cotrimoxazole 24 mg/kg
up to 960mg BD for 5
days
Amox/clavulanate
12.5mg/kg of
Amoxycillin up to
500mg BD for 5 days,
or
Cefaclor 50mg/kg/day
in 3 divided doses for 5
days
Accurate diagnosis very
important make every
effort to collect a sample
before starting treatment.
Re-culture urine 48 hours
after treatment to ensure
cure. Refer for inpatient
treatment if very unwell or <
6 mo old. Discuss with
Paediatrician if <2 yrs. Refer
for ultrasound if >2 yrs
Urinary tract
infection Candida
sp.
Fluconazole
1
200mg
(child: 5mg/kg) daily for 7
days and change or
remove any catheter or
stent
Frequently a meaningless
colonizer, especially with
indwelling catheter. Treat if
symptomatic, neutropenic,
imminent urological
manipulation or infant of low
birth weight
Vaginosis -
bacterial
Metronidazole 400mg BD
for 7 days or 2g stat if
compliance a concern
Ornidazole 500mg BD
for 5 days
If pregnant use Clindamycin
2
Avoiding sex or using
condoms increases cure
rate by 50%
Whooping cough
(Bordetella pertussis)
Azithromycin child <
6mths:10mg/kg daily for
5 days; >6mths 10mg/kg
on day 1(max 500mg)
then 5mg/kg daily (max
250mg) for 4 more days,
Adults: 500mg on day 1
then 250mg daily for 4
more days
Erythromycin Ethyl
Succinate (EES)
400mg (child >1
month: 10 mg/kg to
max 400mg) QID for 14
days. If allergy to
macrolides:
Cotrimoxazole
Admit if cyanotic spells.
Treatment after early
paroxysmal cough phase
(approx. 21 days) has no
effect on illness or infectivity.
Exclude from school until 5
days after treatment started.
Notifiable on suspicion
Wound infection
deep penetrating or
post-operative
Amox/clavulanate
NB: for post-operative
infections consult the
operating surgeon
urgently
Cefaclor, Clindamycin
2
(add Ciprofloxacin
4
to
Clindamycin if
abdominal wound)
Drainage and irrigation are
often all that is needed.
Culture pus to guide
antibiotic choice. Give
tetanus toxoid if indicated.
1. Fluconazole: do not use in pregnancy. Subsidized only with specialist endorsement;
2. Clindamycin: subsidized only with specialist endorsement; please consult in individual case
3. Cotrimoxazole: do not use in pregnancy
4. Ciprofloxacin: use with caution in children under 14 years and in pregnancy.
Topical Antibacterial Agents
Resistance rates for Staphylococcus aureus to Mupirocin and Fusidic acid have increased
dramatically in New Zealand over the last decade as a result of overuse of these agents.
Please use them only when indicated see below.
Infection First choice Alternatives Comments
Burns prevention of
infection
Silver
sulphadiazine
cream 1%
(Flamazine)
Very broad spectrum, painless,
soothing and well studied.
Infected burns need systemic
antibiotic treatment. If ?deep,
dont use until fully assessed as
disguises depth
Conjunctivitis
bacterial
Mild: cleansing and
lubricants +/-
Propamidine drops
or ointment (OTC)
Moderate or severe:
Chloramphenicol eye
drops during day +/-
ointment at night
Swab neonates or if suspect STI
treat chlamydial and
gonococcal conjunctivitis
systemically. Consult specialist
if meningococcal conjunctivitis.
If contact lens wearer, swab and
assess for keratitis
Decolonisation of
MRSA in health-care
workers or S. aureus in
patients with recurrent
boils
Mupirocin ointment
1
2%
Chlorhexidine body
wash
Fusidic acid cream or
ointment 2%
Best used as part of
comprehensive decolonization
protocol including oral antibiotics,
antiseptic body wash and
environmental cleaning. Contact
Infection Control ext 2651 to
discuss protocol
Impetigo/school sores
localized; treatment of
other minor skin infection
Topical hydrogen
peroxide 1% (e.g.,
Crystacide)
(Povidone iodine
probably not
effective)
If Impetigo generalized
or severe use oral
Flucloxacillin or
Erythromycin
For impetigo, wash crusts off.
Exclude from pre-school or
school until treatment started
and ensure sores completely
covered with water-tight dressing
Eczema - infected
A steroid/antibiotic
combination e.g.
Pimafucort
Severely infected eczema needs
targeted systemic antibiotic
treatment as per cellulitis
Otitis externa acute
diffuse
Sofradex drops
3
4 to 6 drops 2 to 3
times a day
Keep ear canal dry, consider
suction. Swab and treat
empirically with flucloxacillin or
cefaclor if fever, spread to pinna
or folliculitis
Prevention of
infection in
superficial wounds
- traumatic or post-
operative
Povidone iodine
10% ointment,
hydrogen peroxide
1% cream
(Crystacide)
Almost any topical
antiseptic or
antibacterial agent
probably works, even
honey or manuka oil.
Topical antibiotics reduce risk of
infection. Consider especially in
patients with face wounds,
heavily contaminated wounds,
immuno-compromised or
previous cellulitis in that region.
Please avoid agents that have
key roles in other conditions
(e.g., mupirocin, fusidic acid,
silver sulphadiazine)
Ulcers - chronic
Nil Not effective. May delay healing
1. Mupirocin Ointment 2% (Bactroban): only partially subsidized; extra cost approximately $8.80.
2. Sofradex Drops: only partially subsidized; extra cost approximately $9.10
Contacts
Dr Anja Werno, Medical Microbiologist Canterbury Health Laboratory
Dr Paul Holt, Infection Control Committee Chairman, Grey Hospital, Greymouth
Acknowledgements:
Australia Antibiotic Guidelines 2006
West Coast District Health Board Inpatient Antibiotic Guidelines
Endorsed by West Coast Primary Health Organization
Anda mungkin juga menyukai
- Common Medical NotationsDokumen3 halamanCommon Medical NotationssaltarisBelum ada peringkat
- Paediatric DoseDokumen12 halamanPaediatric DoseYohanes AdiputraBelum ada peringkat
- Antiarrhythmic Medication Chart - EBM Consult v3Dokumen2 halamanAntiarrhythmic Medication Chart - EBM Consult v3Linlin100% (1)
- Criticalcaredrugs PDFDokumen2 halamanCriticalcaredrugs PDFtomywekaBelum ada peringkat
- Northern Ireland Management of Infection Guidelines For Primary and Community Care 2016Dokumen48 halamanNorthern Ireland Management of Infection Guidelines For Primary and Community Care 2016dreneavalentinstefanBelum ada peringkat
- Carnatic Music NotationDokumen6 halamanCarnatic Music Notationksenthil kumar100% (1)
- Know Common Disease ManagementDokumen14 halamanKnow Common Disease Managementcdx25Belum ada peringkat
- Paediatric Syrup-Injection-DropsDokumen13 halamanPaediatric Syrup-Injection-DropsAminulBelum ada peringkat
- Common MedicationsDokumen4 halamanCommon MedicationsFatima CarricoBelum ada peringkat
- FormulaDokumen5 halamanFormulaEloiseBalasbasBelum ada peringkat
- The GP Book KeralaDokumen44 halamanThe GP Book KeralaMuhammed Abrar100% (1)
- Antibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019Dokumen2 halamanAntibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019RL100% (1)
- Diabetes Mellitus Drug ChartDokumen3 halamanDiabetes Mellitus Drug Chartlui.stephanie1751100% (1)
- UbatopdDokumen4 halamanUbatopdKhai RyBelum ada peringkat
- Create PDF Book App in Android Studio - Download Free PDF Book Source Code PDFDokumen6 halamanCreate PDF Book App in Android Studio - Download Free PDF Book Source Code PDFshafiq09090% (1)
- Antibiotics - Pathogen ChartDokumen3 halamanAntibiotics - Pathogen ChartYanling LiBelum ada peringkat
- 2015 Pain Management For PediatricDokumen2 halaman2015 Pain Management For Pediatricdiany astutiBelum ada peringkat
- Top Drugs: 1. ACETAMINOPHEN (Tylenol)Dokumen12 halamanTop Drugs: 1. ACETAMINOPHEN (Tylenol)epingBelum ada peringkat
- Drug Side EffectsDokumen2 halamanDrug Side EffectsAngelic khanBelum ada peringkat
- Common OPD DrugsDokumen22 halamanCommon OPD DrugsAira Jhamaica DimacaleBelum ada peringkat
- Common TreatmentsDokumen5 halamanCommon TreatmentsRaj MandumulaBelum ada peringkat
- Admitting OrdersDokumen4 halamanAdmitting OrdersRommel OliverasBelum ada peringkat
- American Rifleman - March 2019 PDFDokumen94 halamanAmerican Rifleman - March 2019 PDFHandriyato Sukma100% (3)
- Common Prescribed DrugsDokumen33 halamanCommon Prescribed DrugsGlessica You50% (4)
- Essenc I Al TherapyDokumen9 halamanEssenc I Al TherapyFabian Ramirez HincapiéBelum ada peringkat
- Ans 2 PDFDokumen101 halamanAns 2 PDFrab yoBelum ada peringkat
- Dosage Calculation 09.04.21Dokumen24 halamanDosage Calculation 09.04.21PHARMACOLOGY SMVMCBelum ada peringkat
- Acute MedicineDokumen54 halamanAcute MedicineTipuBelum ada peringkat
- Drugs in Medicine by Medad Team FinalDokumen5 halamanDrugs in Medicine by Medad Team Finalعبد الرحمن100% (2)
- Theories of EmotionDokumen11 halamanTheories of EmotionNoman ABelum ada peringkat
- Standard Treatment Guidelines and Essential Medicine List For Primary Health Care 7th Edition - 2020Dokumen626 halamanStandard Treatment Guidelines and Essential Medicine List For Primary Health Care 7th Edition - 2020Finger TladiBelum ada peringkat
- Mu 002Dokumen10 halamanMu 002chandanBelum ada peringkat
- GP Notes-1Dokumen126 halamanGP Notes-1Fida AnjumBelum ada peringkat
- The Kids Are Alright Pediatric Trauma PearlsDokumen21 halamanThe Kids Are Alright Pediatric Trauma PearlsDaniel Torres CutivaBelum ada peringkat
- Pediatric Notes Draft 12 1Dokumen98 halamanPediatric Notes Draft 12 1Aljon S. TemploBelum ada peringkat
- Las Math 2 Q3 Week 1Dokumen6 halamanLas Math 2 Q3 Week 1Honeyjo Nette100% (7)
- Emergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine SulfateDokumen15 halamanEmergency Drugs: Drug Action Indications Adverse Effects Contraindications Nursing Management Atropine Sulfate092109Belum ada peringkat
- Antimicrobial Renal DosingDokumen5 halamanAntimicrobial Renal DosingdamondouglasBelum ada peringkat
- Clinical Guidelines and Care ProtocolsDari EverandClinical Guidelines and Care ProtocolsPenilaian: 5 dari 5 bintang5/5 (1)
- Drug HandBookDokumen10 halamanDrug HandBookAhmed FekryBelum ada peringkat
- Managing Common Infections Summary TablesDokumen8 halamanManaging Common Infections Summary TablesAlessandro ZadraBelum ada peringkat
- Elsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Dokumen160 halamanElsharnoby Pediatric Made Easy Up Load Waheed Tantawy 2014Emad AdelBelum ada peringkat
- Who Hand Hygiene Observation MethodDokumen8 halamanWho Hand Hygiene Observation MethodHandriyato SukmaBelum ada peringkat
- A Drug For IntDokumen58 halamanA Drug For IntVajirawit PetchsriBelum ada peringkat
- Pediatric Drug Dosage - All in OneDokumen15 halamanPediatric Drug Dosage - All in OneBJ Tiew100% (1)
- Malaria Treatment IndiaDokumen1 halamanMalaria Treatment IndiaSubzer OmerBelum ada peringkat
- Paediatrics Drug DosesDokumen9 halamanPaediatrics Drug DosesRayhan 'sBelum ada peringkat
- Pediatric Guidelines For MedicationsDokumen24 halamanPediatric Guidelines For MedicationsjonatasmartinezBelum ada peringkat
- сестр главы9 PDFDokumen333 halamanсестр главы9 PDFYamikBelum ada peringkat
- Danmachi Volume 15Dokumen319 halamanDanmachi Volume 15Muhammad Fazrul Rahman100% (1)
- 1st Lecture of Respiratory Histology by DR RoomiDokumen24 halaman1st Lecture of Respiratory Histology by DR RoomiMudassar Roomi100% (1)
- Pediatric Dosing For OTCsDokumen5 halamanPediatric Dosing For OTCsCareyTranBelum ada peringkat
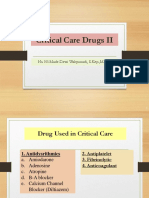
- Critical Care Drugs 2Dokumen23 halamanCritical Care Drugs 2Asri Ernadi100% (1)
- Primary Care Antibiotic Guideline FINAL May 2015Dokumen10 halamanPrimary Care Antibiotic Guideline FINAL May 2015Atta Muhammad MemonBelum ada peringkat
- Paediatric DosesDokumen2 halamanPaediatric DosesEdio PathicBelum ada peringkat
- Fall Risk Assessment Form: Total Score - A Total Score of 10 or More Indicates A Resident "At Risk" For FallsDokumen1 halamanFall Risk Assessment Form: Total Score - A Total Score of 10 or More Indicates A Resident "At Risk" For FallswaheedmohsinBelum ada peringkat
- Drug FormularyDokumen16 halamanDrug FormularySunil BasnetBelum ada peringkat
- 8 IV Medication DripDokumen10 halaman8 IV Medication DripGoez Aditya NugrahaBelum ada peringkat
- PHC EmergencyDokumen42 halamanPHC Emergencyمحمداحمد محمدنور ابايزيدBelum ada peringkat
- Antiarrhythmic Drugs: More To Inactivated Na Channels Arrhythmias During Myocardial Ischaemia or Due To DigoxinDokumen3 halamanAntiarrhythmic Drugs: More To Inactivated Na Channels Arrhythmias During Myocardial Ischaemia or Due To DigoxinChia Yin NgBelum ada peringkat
- Essential ENT by Rogan J Corbridge MB BS, BSC, 2nd Ed 2011 2 PDFDokumen1 halamanEssential ENT by Rogan J Corbridge MB BS, BSC, 2nd Ed 2011 2 PDFMariam Qais100% (1)
- Standard Treatment GuidelineDokumen261 halamanStandard Treatment GuidelineEmaBelum ada peringkat
- Dams - Last Look - Pharmacology2Dokumen29 halamanDams - Last Look - Pharmacology2skBelum ada peringkat
- Pediatrics HandnoteDokumen10 halamanPediatrics HandnoteAbdullah Al - JubairBelum ada peringkat
- NOte BookDokumen81 halamanNOte BookDr abdiaziz osman JamaBelum ada peringkat
- Stony Brook University HospitalDokumen1 halamanStony Brook University HospitalHandriyato SukmaBelum ada peringkat
- Autosomal Dominant Microcephaly With Mental Retardat Ion: of of of ofDokumen3 halamanAutosomal Dominant Microcephaly With Mental Retardat Ion: of of of ofHandriyato SukmaBelum ada peringkat
- Building Tomorrow TalentDokumen247 halamanBuilding Tomorrow TalentHandriyato SukmaBelum ada peringkat
- Fundamental of ForcastingDokumen169 halamanFundamental of ForcastingHandriyato Sukma0% (1)
- Analisis Ketaatan Karyawan Dalam Pemeriksaan Kesehatan Berkala Di Rumah Sakit Pku Muhammadiyah Kota YogyakartaDokumen10 halamanAnalisis Ketaatan Karyawan Dalam Pemeriksaan Kesehatan Berkala Di Rumah Sakit Pku Muhammadiyah Kota YogyakartaHandriyato SukmaBelum ada peringkat
- Design Analisa Kebutuhan Pelaporan Hasil Medical Check Up Di Laboratorium Kualita MedicaDokumen18 halamanDesign Analisa Kebutuhan Pelaporan Hasil Medical Check Up Di Laboratorium Kualita MedicaHandriyato SukmaBelum ada peringkat
- FPPE - OPPE Best PracticesDokumen29 halamanFPPE - OPPE Best PracticesMaharani100% (1)
- HVA Tool User GuideDokumen4 halamanHVA Tool User GuidewiraandiniBelum ada peringkat
- RR 5417Dokumen144 halamanRR 5417Handriyato SukmaBelum ada peringkat
- CDC-45703-1A: Central Line Insertion ChecklistDokumen1 halamanCDC-45703-1A: Central Line Insertion ChecklistHandriyato SukmaBelum ada peringkat
- Ps 202PET Manual enDokumen7 halamanPs 202PET Manual enStiv KisBelum ada peringkat
- Brocade MIB ReferenceDokumen1.212 halamanBrocade MIB ReferencejessiwattsBelum ada peringkat
- Analyzing Text - Yuli RizkiantiDokumen12 halamanAnalyzing Text - Yuli RizkiantiErikaa RahmaBelum ada peringkat
- Car Radiator AssignmentDokumen25 halamanCar Radiator AssignmentKamran ZafarBelum ada peringkat
- Policing System Indonesia PolicingDokumen5 halamanPolicing System Indonesia Policingdanilo bituin jrBelum ada peringkat
- CS101 Solved File For Final Term MCQS 1 To 45 LecturesDokumen130 halamanCS101 Solved File For Final Term MCQS 1 To 45 LecturesHisan Mehmood64% (28)
- Arendi v. GoogleDokumen16 halamanArendi v. GooglePriorSmartBelum ada peringkat
- Mouth Tongue and Salivary GlandsDokumen52 halamanMouth Tongue and Salivary GlandsIrfan FalahBelum ada peringkat
- R WaseemDokumen3 halamanR WaseemWaseem RajaBelum ada peringkat
- Artikel Andi Nurindah SariDokumen14 halamanArtikel Andi Nurindah Sariapril yansenBelum ada peringkat
- Making Electric Vehicles ProfitableDokumen18 halamanMaking Electric Vehicles ProfitablevjslkumarBelum ada peringkat
- Case Study: Direct Selling ConceptDokumen20 halamanCase Study: Direct Selling Conceptbansi2kk0% (1)
- Real Number System.Dokumen7 halamanReal Number System.samuel1436Belum ada peringkat
- Ring Spinning Machine LR 6/S Specification and Question AnswerDokumen15 halamanRing Spinning Machine LR 6/S Specification and Question AnswerPramod Sonbarse100% (3)
- IRS McqsDokumen7 halamanIRS McqsIbrahimGorgageBelum ada peringkat
- Lesson Plan Design: Ccss - Ela-Literacy - Rf.2.3Dokumen6 halamanLesson Plan Design: Ccss - Ela-Literacy - Rf.2.3api-323520361Belum ada peringkat
- Age of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Dokumen4 halamanAge of Sigmar AoS - Battletome - Hedonites of Slaanesh - Errata 2023-01Ughu RajaBelum ada peringkat
- Audit QuestionnaireDokumen7 halamanAudit QuestionnaireEmz Pleños ValerosoBelum ada peringkat
- All This Comand Use To Type in NotepadDokumen9 halamanAll This Comand Use To Type in NotepadBiloul ShirazBelum ada peringkat
- Family Advent Devotions 1Dokumen3 halamanFamily Advent Devotions 1collingdalenazBelum ada peringkat
- Kumpulan Soal UPDokumen16 halamanKumpulan Soal UPTriono SusantoBelum ada peringkat
- Monthly Film Bulletin: 1T1IcqDokumen12 halamanMonthly Film Bulletin: 1T1IcqAlfred_HitzkopfBelum ada peringkat
- Parkin 8e TIF Ch27Dokumen51 halamanParkin 8e TIF Ch27Pranta SahaBelum ada peringkat
- Softwash ComparatorDokumen5 halamanSoftwash ComparatorFaheem MushtaqBelum ada peringkat