Early Amniotomy
Diunggah oleh
Indah Mayang SariDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Early Amniotomy
Diunggah oleh
Indah Mayang SariHak Cipta:
Format Tersedia
Research
www. AJOG.org
OBSTETRICS
The efficacy of early amniotomy in nulliparous
labor induction: a randomized controlled trial
George A. Macones, MD; Alison Cahill, MD; David M. Stamilio, MD; Anthony O. Odibo, MD
OBJECTIVE: The purpose of this study was to assess whether early am-
niotomy reduces the duration of labor or increases the proportion of
subjects who are delivered within 24 hours in nulliparous patients who
undergo labor induction.
STUDY DESIGN: We performed a randomized controlled trial that com-
pared early amniotomy to standard management in nulliparous labor inductions. Inclusion criteria were nulliparity, singleton, term gestation,
and a need for labor induction. Subjects were assigned randomly to
early amniotomy (artificial rupture of membranes, 4 cm) or to standard treatment. There were 2 primary outcomes: (1) time from induc-
tion initiation to delivery and (2) the proportion of women who delivered
within 24 hours.
RESULTS: Early amniotomy shortens the time to delivery by 2 hours
(19.0 vs 21.3 hours) and increases the proportion of induced nulliparous
women who deliver within 24 hours (68% vs 56%). These improvements in
labor outcomes did not come at the expense of increased complications.
CONCLUSION: Early amniotomy is a safe and efficacious adjunct in nul-
liparous labor inductions.
Key words: amniotomy, nulliparous labor induction
Cite this article as: Macones GA, Cahill A, Stamilio DM, et al. The efficacy of early amniotomy in nulliparous labor induction: a randomized controlled trial. Am J
Obstet Gynecol 2012;207:403.e1-5.
ates of labor induction are rising.
Recent data from the National Center for Health Statistics demonstrate an
induction rate of 22% in 2006, which
was more than double what it was in
1990 and impacted 900,000 births in
the United States that year.1 Although
many recent studies have offered evidence for the improvement in methods
for labor induction, 2-7 the induction of
labor remains a significant risk factor for
cesarean delivery,8,9 which highlights the
critical need for additional tools to refine
induction practice.
Amniotomy, generally thought to be
low-tech, inexpensive, and safe, has received little research attention, and stud-
From the Department of Obstetrics and
Gynecology, Washington University in St. Louis
School of Medicine, St. Louis, MO.
Received Feb. 27, 2012; revised June 1, 2012;
accepted Aug. 21, 2012.
The authors report no conflict of interest.
Reprints: George A. Macones, MD, Professor
and Chair, Department of Obstetrics and
Gynecology, Washington University in St Louis,
School of Medicine, 4911 Barnes Jewish
Hospital Plaza, St. Louis, MO 63110.
maconesg@wustl.edu.
0002-9378/$36.00
2012 Mosby, Inc. All rights reserved.
http://dx.doi.org/10.1016/j.ajog.2012.08.032
ies to date have neglected to investigate
the efficacy of amniotomy in nulliparous
women, despite the fact that more inductions are performed in nulliparous
women than their multiparous peers.1
Based on clinical trials from those in
spontaneous labor,10 early amniotomy
timing in labor inductions may shorten
the duration of labor. Clinical concern
for the rare complications of umbilical
cord prolapse and theoretic concerns
that rupturing the membranes earlier
will lead to a longer overall duration of
rupture of membranes with potentially
increased rates of chorioamnionitis,
neonatal sepsis, and neonatal intensive
care unit (NICU) admission have limited the empiric use of the practice of
amniotomy in nulliparous labor inductions without level I evidence to
support it.
The specific aim of this study was to
assess whether early amniotomy, defined
as artificial rupture of the membranes, at
4-cm dilation, reduces the duration of
labor or increases the proportion of subjects delivered within 24 hours in term
nulliparous patients who undergo labor
induction. We also sought to assess the
safety of early amniotomy, as measured
by adverse obstetric outcomes and measures of maternal and neonatal infectious morbidities.
M ETHODS
We performed an unblinded, randomized controlled trial at Washington University in St. Louis and the University of
Pennsylvania with approval from the Institutional Review Boards at both institutions. Inclusion criteria for this clinical
trial were nulliparity, singleton, term
gestation (defined as 37 weeks 0 days),
and a need for labor induction as determined by the treating physician. Exclusion criteria included HIV infection or
cervical dilation of 4 cm at admission
examination.
Eligible subjects were approached by
trained research nurses and were offered
enrollment into the clinical trial. Patients
who consented were then randomly assigned to early amniotomy, which was
defined as artificial rupture of the membranes at 4 cm or to standard management, which was amniotomy at 4 cm
dilation. In the early amniotomy group,
amniotomy was performed as early as
could be done safely. Decisions about the
exact timing of rupture (after random
assignment) were made by a team that
included residents, fellows, and attendings. There were no specific instructions
given regarding the timing of amniotomy
in the standard treatment group; this decision was left to the treating physicians. The
NOVEMBER 2012 American Journal of Obstetrics & Gynecology
403.e1
Research
Obstetrics
www.AJOG.org
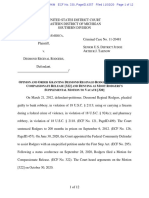
FIGURE
Flowchart
749 assessed for eligibility
164 excluded
84 not meeting inclusion criteria
80 refused to participate
0 other reasons
585 randomized
292 assigned to early amniotomy
270 received intervention as assigned
22 did not receive assigned intervention
(Clinical concern)
293 assigned to standard management
280 received intervention as assigned
13 did not receive assigned intervention
(Clinical concern)
0 lost to follow-up
0 lost to follow-up
292 included in analysis
0 excluded from analysis
293 included in analysis
0 excluded from analysis
Macones. Early amniotomy in nulliparous labor induction. Am J Obstet Gynecol 2012.
primary method of induction was at the
discretion of the treating physician, as were
all other intrapartum/postpartum decisions. Random assignment was accomplished centrally. A permuted block
randomization procedure was used to
formulate assignment lists to assure close
to equal numbers of subjects in each treatment group. A uniform block size of 4 was
used.
There were 2 primary outcomes. The
first was time from initiation of induction, defined as time at delivery of the
first induction method to delivery. The
second was the proportion of women delivered within 24 hours from the initiation of induction. Although it may seem
unusual to have 2 primary endpoints, we
believed that both were equally clinically
relevant and should be treated as primary outcomes. This decision was made
a priori. We also assessed a number of
403.e2
secondary endpoints that included cesarean delivery rates and indications for
cesarean delivery, chorioamnionitis (oral
temperature 38C during labor), postpartum fever (oral temperature 38C on
2 separate occasions 6 hours apart, 24
hours from delivery), wound infection
(defined as purulent discharge from the
incision), endomyometritis (defined as
fundal tenderness and fever that require
treatment with antibiotics), NICU admission, and suspected neonatal sepsis. Trained
research nurses collected all baseline information, information on the course of labor,
and information on maternal and neonatal
outcomes.
Statistical analyses were performed
with the intent-to-treat principle. Continuous outcomes were compared with
the use of the Student t test or MannWhitney U dependent on their distributions; dichotomous outcomes were as-
American Journal of Obstetrics & Gynecology NOVEMBER 2012
sessed with 2 tests or Fisher exact test
where appropriate. Time to delivery was
not normally distributed and was compared with the use of the Mann-Whitney
U test. Relative risks by group and 95%
confidence intervals (CIs) were estimated for the percent of women who delivered within 24 hours and each of the
secondary outcomes. Our sample size
estimate was based on 1 of our primary
outcomes: the proportion of women
who delivered within 24 hours. We assumed an alpha error of .05, a beta error
of .20 (or 80% power), an incidence of
delivery within 24 hours of 50% based on
published data, a minimum detectable
relative risk of 0.75, and a 1:1 allocation
ratio. With these assumptions in mind,
we estimated that we would need 290
subjects per group. This strategy for
sample size calculation gave us tremendous power for our second primary outcome, time to delivery (a continuous
measure). Specifically, we estimated a
priori that we had 95% power to detect a
2-hour reduction in time to delivery.
R ESULTS
Seven hundred forty-nine women were
screened for eligibility; 84 women (11.2%)
were deemed ineligible by exclusion criteria. Of the 635 eligible nulliparous women,
585 women (92%) consented and were assigned randomly (Figure); 292 women
were assigned to the early amniotomy
group, and 293 women were assigned to
standard treatment. Those who agreed to
participate and those who did not were
similar in terms of baseline characteristics
(age, gestational age, preexisting medical
conditions). The groups were well-balanced with regards to demographics and
maternal medical conditions; the mean
gestational age at induction was similar between the groups (Table 1). The admission
cervical dilation was also similar between
the groups. Likewise, the indications for labor induction were similar between the
groups. The 2 most common indications
for induction were 40-week gestations
and gestational hypertension/preeclampsia. The other category for indication for
induction had a variety of uncommon indications for induction, which included
maternal request/social factors (eg, dis-
Obstetrics
www.AJOG.org
tance from hospital) and oligohydramnios
(Table 2).
Methods for induction were similar
between the early amniotomy and standard treatment groups. Most women received misoprostol; approximately 30%
of the women received a Foley bulb. The
induction method categories are not mutually exclusive, because many women received multiple agents. In fact, 73% of
women in both groups received 1 agent
for induction. As expected, with regards to
timing of amniotomy, the early amniotomy group was ruptured earlier than
the standard treatment group. Twentytwo women who were assigned randomly
to early amniotomy were ruptured after 4
cm of dilation; 13 women who were assigned randomly to standard treatment
were ruptured at 4 cm.
The primary results of this study are
given in Table 3. The average time from
the start of induction to delivery was
shortened by slightly 2 hours in the
early amniotomy group (19.0 vs 21.3
hours, respectively; P .04) compared
with those with standard treatment. This
difference in length of labor occurred
mainly in the first stage of labor, which
was defined as time from random assignment to complete cervical dilation. A
higher proportion of women in the early
amniotomy group were delivered within
24 hours of the initiation of induction
(68% vs 56%, respectively; P .002).
Despite these differences in length of labor and delivery within 24 hours, there
was no difference in the rate of cesarean
deliveries. The rate of chorioamnionitis
was increased numerically in the early
amniotomy group (11.5% v. 8.5%, respectively; P .22), although this difference was not statistically significant.
Likewise, there were 2 cord prolapses in
the early amniotomy group, and none in
the standard treatment group.
Selected neonatal outcomes are shown
in Table 4. There was no increase in the rate
of confirmed or suspected neonatal sepsis
or admission to the special care nursery or
NICU in women who underwent early
amniotomy compared with those who experienced standard care. The infants born
to women with cord prolapse both did
well, with umbilical arterial pH 7.20 and
5-minute Apgar score.
Research
TABLE 1
Baseline characteristics
Early amniotomy
(n 292)
Variable
Standard therapy
(n 293)
P value
Maternal age, y
22.7 5.8
23.3 6.2
.17
African American race, %
72
68
.30
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
Diabetes mellitus, %
3.9
3.5
.81
5.2
.32
..............................................................................................................................................................................................................................................
Chronic hypertension, %
7.2
..............................................................................................................................................................................................................................................
2a
Body mass index, kg/m
28 4.2
28 3.9
.90
GBS, %
29
30
.66
Pitocin, %
93
93
.87
Misoprostol, %
67
69
.70
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
Cervidil, %
6.8
8.4
.45
..............................................................................................................................................................................................................................................
Foley bulb, %
27
30
.43
More than 1 agent, %
73
73
.80
Epidural anesthesia, %
92
94
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
.88
..............................................................................................................................................................................................................................................
a
Admission dilation, cm
1.1 1.03
1.1 0.97
.54
Dilation at rupture of membranes, cm
3.2
7.4
.001
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
a
Station at rupture of membranes
1 1.2
1 1.5
.50
..............................................................................................................................................................................................................................................
a
6.2 3.0
Cervical examinations, n
5.9 3.4
.67
..............................................................................................................................................................................................................................................
a
3323 516
Birthweight, g
3311 566
.78
..............................................................................................................................................................................................................................................
a
39.7 1.4
Gestational age, wk
39.5 1.4
.16
..............................................................................................................................................................................................................................................
GBS, Group B streptococcus.
a
Data are given as mean SD.
Macones. Early amniotomy in nulliparous labor induction. Am J Obstet Gynecol 2012.
C OMMENT
Although these differences in duration
of labor and proportion of women delivered within 24 hours may seem to be intermediate outcomes, we would argue
that these are good surrogates for both
maternal and neonatal outcomes. For
example, it has been well-documented
that the length of labor is correlated directly with maternal chorioamnionitis,
postpartum fever, and neonatal infec-
The goal of our study was to assess the
efficacy and safety of early amniotomy in
nulliparous women who undergo labor
induction. The results of this clinical trial
indicate that early amniotomy shortens
labor by approximately 2 hours, increases the proportion of women delivered within 24 hours, but does not impact the rate of cesarean deliveries.
TABLE 2
Indications for induction
Variable
Early
amniotomy, %
Standard, %
P value
40 wk
40
39
.83
Maternal medical indication
13
14
.72
Gestational hypertension/preeclampsia
29
27
.63
.63
12
13
.63
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
Intrauterine growth restriction
..............................................................................................................................................................................................................................................
Other
..............................................................................................................................................................................................................................................
Macones. Early amniotomy in nulliparous labor induction. Am J Obstet Gynecol 2012.
NOVEMBER 2012 American Journal of Obstetrics & Gynecology
403.e3
Research
Obstetrics
www.AJOG.org
TABLE 3
Maternal and labor outcomes
Outcome
Early
amniotomy
(n 292)
Standard
(n 293)
Randomization at delivery, hra
19.0 9.1
21.3 10.1
Delivery at 24 hr, %
68
56
0.72
0.590.89
.002
Cesarean delivery, %
41
40
1.03
0.850.25
.75
Amnioinfusion, %
19
19
1.02
0.731.42
.87
Chorioamnionitis, %
11.5
1.35
0.832.21
.22
Cord prolapsed, %
0.7
Abruption, %
0.4
0.6
0.55
0.056.03
.62
Postpartum hemorrhage, %
8.2
10.1
0.81
0.481.36
.44
Relative
risk
95% CI
P
value
.04
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
8.5
..............................................................................................................................................................................................................................................
.13
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
CI, confidence interval.
a
Data are given as mean SD.
Macones. Early amniotomy in nulliparous labor induction. Am J Obstet Gynecol 2012.
tion.11-13 In addition, a 2-hour difference in labor length has important implications for resource utilization at the
hospital level. For example, a 2-hour difference in time to delivery across many
inductions could lead to a decrease in
staffing of a labor and delivery unit. Last,
there is likely enhanced patient satisfaction with shorter labors as well.
The shorter duration of labor must be
weighed against both maternal and neonatal safety concerns. There were a
greater number of cases of maternal chorioamnionitis in the early amniotomy
group, although this difference was not
statistically significant. For this study,
chorioamnionitis was defined purely on
the basis of fever in labor. Given that fever is an objective measure, we do not
believe that unblinding differentially affected the ascertainment of this outcome. Importantly, this numeric difference in chorioamnionitis did not lead to
an increase in the rate of suspected neo-
natal sepsis or NICU admission, and
there were no serious maternal consequences as a result of chorioamnionitis.
Still, future studies should focus on the
occurrence of chorioamnionitis with
early amniotomy. There were also 2 cord
prolapses in the early amniotomy group
and none in the standard treatment
group. Interestingly, one of the cord prolapses occurred in a patient in the early
amniotomy group who actually was ruptured after 4 cm of dilation. Still, the occurrence of cord prolapse is concerning
and warrants further study.
Although there has been work on the
role of amniotomy in spontaneous labor,14 surprisingly, there has been little
previous work on the role of early amniotomy in the context of labor induction. There have been several clinical trials that have compared the combination
of amniotomy and oxytocin with other
methods of induction,15 but no studies
that we are aware of that focus exclu-
TABLE 4
Neonatal outcomes
Outcome
Early
Relative
amniotomy Standard risk
95% CI
P value
5-minute Apgar score
8.6
8.6
Suspected neonatal sepsis, %
9.7
11.1
0.87
0.541.41 .58
.72
Special care nursery admission, % 13.6
15.0
0.90
0.611.35 .63
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
..............................................................................................................................................................................................................................................
CI, confidence interval.
Macones. Early amniotomy in nulliparous labor induction. Am J Obstet Gynecol 2012.
403.e4
American Journal of Obstetrics & Gynecology NOVEMBER 2012
sively on the timing of amniotomy in labor induction. Amniotomy has been
well-studied in the context of those
women in spontaneous labor, which included the active management of labor;
however, the work on active management of labor may not be generalized
necessarily to those women whose labor
is induced.16,17 Fraser et al10 performed a
randomized clinical trial of amniotomy
in nulliparous women in spontaneous
labor. In that study, early amniotomy reduced the occurrence of dystocia (defined as 4 hours of cervical dilation of
0.5 cm/hr) and shortened the first
stage of labor by 136 minutes. The benefit of amniotomy was greatest in women
with 3-cm initial dilation. A recent Cochrane review summarized the available
information on early amniotomy in
spontaneous labor.14 This pooled analysis did not support the notion that early
amniotomy shortened the first stage of
labor or reduced the rate of cesarean deliveries. The authors of this Cochrane review did suggest that additional research
was needed.
Our study has some notable strengths
and limitations. First, our randomization strategy effectively balanced the
study groups with respect to potentially
confounding effects and, more importantly, maximally balanced them on
unmeasured confounders. Second, the
study is relatively large in size compared
with many other studies of labor induction, which allowed us to reach an adequate sample to test our primary hypothesis. Third, we included a diverse
group of patients with various indications for induction and various methods
for induction, lending to the generalizability of the results. Last, our simple
trial design with broad inclusion/exclusion criteria and treating physician decision-making should enhance both generalizability and the translation from
efficacy in a study setting to real world
effectiveness. There are some potential
weaknesses that we believe deserve careful consideration. For practical reasons,
this study was unblinded, which could
have impacted the study results both
with the potential for unequal distribution of cointerventions and the assessment of the secondary outcomes. We
Obstetrics
www.AJOG.org
were reassured that the potential impact
of cointerventions from practitioners
because of group assignment based on
the primary outcomes were likely minimal; there were no differences between
the groups in rates of any of the induction agents that were used alone or in
combination. With regard to the secondary outcomes, it is possible that the
knowledge of treatment assignment may
have influenced our somewhat subjective newborn infant outcomes. We believe that this potential bias, if present,
would have resulted in more neonates in
the early amniotomy group being admitted to the special care nursery, thus inflating the relative risk for NICU admission. The fact that we did not observe a
difference in admissions is reassuring.
Our sample size, although sufficiently
large to test our hypothesis and compared with many studies of labor induction, was limited with respect to the confident assessment of differences in rare
outcomes, such as cord prolapse. Approximately 10% of subjects in the early
amniotomy group were ruptured after 4
cm; likewise, some women were assigned
randomly to standard treatment were
ruptured earlier. This misclassification is
likely random and would therefore likely
bias our results towards the null.
With these strengths and limitations in
mind, this study supports the following
conclusions. First, relative to standard
treatment with later amniotomy, early amniotomy shortens the time to delivery by
2 hours and increases the proportion of
induced nulliparous women who were delivered within 24 hours. Based on these
data, early amniotomy, when deemed
safe by the practitioner, may be a useful
adjunct in nulliparous labor inductions and may be incorporated into induction algorithms.
f
REFERENCES
1. Martin JA, Hamilton BE, Sutton PD, et al.
Births: final data for 2006. Natl Vital Stat Rep
2009;57:1-102.
2. Gelber S, Sciscione A. Mechanical methods
of cervical ripening and induction. Clin Obstet
Gynecol 2006;49:642-57.
3. Rayburn WF. Prostaglandin E2 gel for cervical ripening and induction of labor: a critical
analysis. Am J Obstet Gynecol 1989;160:
529-34.
4. Hofmeyr GJ, Gulmezoglu AM. Vaginal misoprostol for cervical ripening and induction of labour. Cochrane Database of Systematic Reviews 2003;1:CD000941.
5. Wing DA, Jones MM, Rahall A, Goodwin TM,
Paul RH. A comparison of misoprostol and
prostaglandin E2 gel for preinduction cervical
ripening and labor induction. Am J Obstet Gynecol 1995;172:1804-10.
6. Kelly AJ, Kavanagh J, Thomas J. Vaginal
prostaglandin (PGE2 and PGF2a) for induction
of labour at term. Cochrane Database of Systematic Reviews 2003;4:CD003101.
7. Zhang J, Branch DW, Ramirez MM, et al.
Oxytocin regimen for labor augmentation, labor
progression and perinatal outcomes. Obstet
Gynecol 2011;118:249-56.
Research
8. Moore LE, Rayburn WF. Elective induction of
labor. Clin Obstet Gynecol 2006;49:698-704.
9. Luthy DA, Malmgren JA, Zingheim RW. Cesarean delivery after elective induction in nulliparous women: the physician effect. Am J Obstet
Gynecol 2004;191:1511-5.
10. Fraser WD, Marcoux S, Moutquin JM,
Christen A, the Canadian Early Amniotomy
Study Group. Effect of early amniotomy on the
risk of dystocia in nulliparous women. N Engl
J Med 1993;328:1145-9.
11. Seaward PG, Hannah ME, Myhr TL, et al.
International Multicentre Term Prelabor Rupture
of Membranes Study: evaluation of predictors
of clinical chorioamnionitis and postpartum fever in patients with prelabor rupture of membranes at term. Am J Obstet Gynecol 1997;
177:1024-9.
12. Tran SH, Cheng YW, Kaimal AJ, Caughey
AB. Length of rupture of membranes in the setting of premature rupture of membranes at term
and infectious maternal morbidity. Am J Obstet
Gynecol 2008;198:700.e1-5.
13. Herbst A, Kallen K. Time between membrane rupture and delivery and septicemia in
term neonates. Obstet Gynecol 2007;110:
612-8.
14. Smyth RMD, Alldred SK, Markham C. Amniotomy for shortening spontaneous labour.
Cochrane Database of Systematic Reviews
2007;4:CD006167.
15. Howarth G, Botha DJ. Amniotomy plus intravenous oxytocin for induction of labour. Cochrane Database of Systematic Reviews 2001;
3:CD003250.
16. Frigoletto FD, Lieberman E, Lang JM, et al.
A clinical trial of active management of labor.
N Engl J Med 1995;333:745-50.
17. Lopez-Zeno JA, Peaceman AM, Adashek
JA, Socol ML. A controlled trial of a program for
the active management of labor. N Engl J Med
1992;326:450-4.
NOVEMBER 2012 American Journal of Obstetrics & Gynecology
403.e5
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Birth Class 11Dokumen5 halamanBirth Class 11anushkaparashar85Belum ada peringkat
- 10 1016@j Jaim 2018 08 006Dokumen7 halaman10 1016@j Jaim 2018 08 006Ega AihenaBelum ada peringkat
- Using in Children and Adolescents: BenzodiazepinesDokumen4 halamanUsing in Children and Adolescents: BenzodiazepinesEunike KaramoyBelum ada peringkat
- OPPro Psychometric PropertiesDokumen3 halamanOPPro Psychometric PropertiesShaniceBelum ada peringkat
- In-Patient: Benefit ScheduleDokumen2 halamanIn-Patient: Benefit Scheduledinda testBelum ada peringkat
- PTS I Bhs Inggris XIIDokumen7 halamanPTS I Bhs Inggris XIIVriska Budi pratiwiBelum ada peringkat
- V6 - Health CS VC Collectors 22.08.2023Dokumen92 halamanV6 - Health CS VC Collectors 22.08.2023MdnowfalBelum ada peringkat
- Turtura ResumeDokumen1 halamanTurtura ResumeaturturaBelum ada peringkat
- Is RH Factor Is Behind The Moderate Life Expectancy of Uttarakhandtribals A Brief Review 2332 0915 1000191Dokumen7 halamanIs RH Factor Is Behind The Moderate Life Expectancy of Uttarakhandtribals A Brief Review 2332 0915 1000191Mainak ChakrabortyBelum ada peringkat
- Pemilihan Kerjaya Menurut Teori HollandDokumen2 halamanPemilihan Kerjaya Menurut Teori HollandKHAIRUNISABelum ada peringkat
- Redacted Letter To Winn Correctional Center, June 10, 2021Dokumen5 halamanRedacted Letter To Winn Correctional Center, June 10, 2021Katie CrolleyBelum ada peringkat
- Nursing SeatmatrixDokumen8 halamanNursing SeatmatrixKanza KaleemBelum ada peringkat
- F3 Exam PaperDokumen20 halamanF3 Exam PaperAgnes Hui En WongBelum ada peringkat
- Natural ChildhoodDokumen28 halamanNatural Childhoodapi-205697600100% (1)
- Reinforcement Theory of MotivationDokumen10 halamanReinforcement Theory of Motivationimdad ullahBelum ada peringkat
- Tired 2. Motivated 3. Excited 4. Scared 5. Angry 6. Happy 7. Disappointed 8. Bored 9. Delighted 10.sadDokumen11 halamanTired 2. Motivated 3. Excited 4. Scared 5. Angry 6. Happy 7. Disappointed 8. Bored 9. Delighted 10.sadAnita Zarza BandaBelum ada peringkat
- TETRINDokumen2 halamanTETRINDr.2020Belum ada peringkat
- 200 PSM Questions Solved by DR AshwaniDokumen16 halaman200 PSM Questions Solved by DR AshwaniShaaron Sky SonaBelum ada peringkat
- Adherence To Medication. N Engl J Med: New England Journal of Medicine September 2005Dokumen12 halamanAdherence To Medication. N Engl J Med: New England Journal of Medicine September 2005Fernanda GilBelum ada peringkat
- Boykin & Schoenhofer's Theory of Nursing As CaringDokumen1 halamanBoykin & Schoenhofer's Theory of Nursing As CaringErickson CabassaBelum ada peringkat
- SOP For EHSSRM SystemDokumen17 halamanSOP For EHSSRM SystemMd Rafat ArefinBelum ada peringkat
- Apr W1,2Dokumen6 halamanApr W1,2Toànn ThiệnnBelum ada peringkat
- US V RodgersDokumen12 halamanUS V RodgersMelissa BoughtonBelum ada peringkat
- Asr 1Dokumen40 halamanAsr 1nadia viBelum ada peringkat
- Birla Institute of Technology & Science, Pilani Work Integrated Learning Programmes DigitalDokumen10 halamanBirla Institute of Technology & Science, Pilani Work Integrated Learning Programmes DigitalAAKBelum ada peringkat
- Cainta Catholic College Cainta, Rizal Senior High SchoolDokumen54 halamanCainta Catholic College Cainta, Rizal Senior High SchoolandyBelum ada peringkat
- Gurdjieff S Sexual Beliefs and PDokumen11 halamanGurdjieff S Sexual Beliefs and PDimitar Yotovski0% (1)
- Literature Review: Terapi Relaksasi Otot Progresif Terhadap Penurunan Tekanan Darah Pada Pasien HipertensiDokumen8 halamanLiterature Review: Terapi Relaksasi Otot Progresif Terhadap Penurunan Tekanan Darah Pada Pasien Hipertensinadia hanifaBelum ada peringkat
- INFOKIT Future ForestDokumen6 halamanINFOKIT Future ForestPOPBelum ada peringkat
- Organizing Is Good For Mental HealthDokumen2 halamanOrganizing Is Good For Mental Healthamos wabwileBelum ada peringkat