06 Medical Record Guidelines
Diunggah oleh
Lek825Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
06 Medical Record Guidelines
Diunggah oleh
Lek825Hak Cipta:
Format Tersedia
M E D I C A L R E C O R D G U I D E L I N E S
1
August 2008
Medical Record Guidelines Table of Contents
Medical Record Guidelines .....................................................................................................................2
Medical Record Content and Format.....................................................................................................2
Auditing Primary Care Physician Medical Forms...............................................................................4
Accessing Medical Records .....................................................................................................................5
Release of Information to Members .......................................................................................................5
Advance Directives...................................................................................................................................6
Telephonic Medicine ................................................................................................................................7
Patient-Clinician Electronic Mail Policy................................................................................................8
Medical Record Review Tools:
Pediatric and Adolescent Medicine Tool
List of Vaccines for Pediatric and Adolescent-MRR Reporting
Childhood Immunization Tool
Asthma Tool
Congestive Heart Failure Tool
Diabetes Mellitus Flow Sheet
AdultMedicalRecordReviewTool
ListofVaccinesforAdults
AdultPreventiveCareFlowSheet
MaternityMedicalRecordReview
WebResourcesforCommunicableDiseaseReporting
M E D I C A L R E C O R D G U I D E L I N E S
2
August 2008
MEDICAL RECORD GUIDELINES
The medical record is a legal document that contains information about the Plan member,
identifies the patients complaints/symptoms or lack thereof, contains the diagnosis and
basis for the diagnosis, the communication and discussion of treatment options, side effects,
decisions made and treatment rendered. The primary purpose of the record is to document
the course of the members health or illness and treatments and serves as a mode of
communication between physicians and other professionals participating in the care
rendered. The entire medical record of an active member must remain in the primary care
physicians office and must be consistent with all relevant New York State and federal laws,
rules and regulations.
The following guidelines assist the Plan in assuring the appropriate exchange and retention of
member medical data and are used to perform clinical audits in conjunction with ongoing
quality assurance activities. Please see the end of this section for Medical Record Audit Tools
that can help ensure that your medical records adhere to these standards. The tools are also
available at hipusa.com.
Please note that the Plan may request a copy of medical records or visit on site to review your medical records for
internal and regulatory chart audits.
MEDICAL RECORD CONTENT AND FORMAT
There should be a unique medical record for each member. The medical record jacket and all
information contained therein should have, at a minimum, the following information:
Members name.
Members Plan ID number.
Members date of birth.
Members address and phone number.
Members employer name, address and phone number.
Members marital status.
Members benefit plan participation and copayment (if applicable).
Name of the primary care physician (PCP).
Members allergies and/or adverse reactions. (No Known Allergies must also be
appropriately noted in the record.)
M E D I C A L R E C O R D G U I D E L I N E S
3
August 2008
All similar reports should be filed together in chronological or reverse chronological order,
permitting easy retrieval of information (i.e., all progress notes are filed together, all X-ray
reports are filed together, all laboratory reports are filed together, etc.). Reports should be
initialed by the physician to show evidence that they have been read.
All medical records must include, but are not limited to, the following information:
Biographical information.
History and physical.
Diagnostic test results.
Consult reports.
Progress notes.
Medication records.
Problem list.
Allergy documentation.
Telephone/communication log.
Immunization records.
Preventive health screening records.
Inpatient/ER discharge summary reports, if applicable. (The PCP must document
his/her follow up after the members ER visit and/or hospitalization. An office visit,
written correspondence or telephone conversation must be clearly documented in the
members medical record.)
Operative reports, if applicable.
The baseline history and physical is comprehensive and must include a review of:
Subjective and objective complaints/problems.
Family history (including parents, siblings).
Social history (including occupation, education, living situation, risk behaviors).
Significant accidents, surgeries, illnesses and mental health issues.
Complete and comprehensive review of systems, including patients presenting
complaint, as applicable.
For children and adolescents (18 years and younger), the past medical history must
include prenatal care and birth information. (Baseline only.)
Note: Periodic history and physicals should be repeated in accordance with age appropriate
preventive care guidelines. A routine or follow-up office visit consists of a focused review of
systems based upon presenting complaints, active (acute) medical or psychosocial
problems, or management of a chronic, serious or disabling condition.
M E D I C A L R E C O R D G U I D E L I N E S
4
August 2008
Each progress note should be legibly written or typed and contain at least the following
items:
The reason for visit as stated by the member.
The duration of the problem.
Findings on physical examination.
Laboratory and X-ray results, if any.
Diagnosis or assessment of the members condition.
Therapeutic or preventive services prescribed, if any.
Dosage, duration and side effect information regarding any prescription given and
medication allergies and adverse reactions noted prominently (updated at least annually
[preferably during a physical or when a prescription is written]).
Follow-up plan (including self-care training) or that no follow-up is required.
Progress notes must be signed by the author and dated and filed in consistent
chronological (or reverse chronological) order.
All loose reports generated as a result of a request for a test or consultation must be filed
immediately in the medical record with the following identifiers on each document page:
The members name.
The members Plan ID number.
The members date of birth.
It is expected that all test results are reported to the member within a reasonable time after
physician receipt and review. Dating and initialing the report indicates that the physician
reviewed the report. A note should be placed in the progress note indicating who called the
member, when the member was called and the next steps in the treatment plan.
AUDITING PRIMARY CARE PHYSICIAN (PCP) MEDICAL RECORDS
The Quality Review Operations department conducts ongoing audits, based on randomly
selected charts, of a PCPs medical record documentation procedures. The passing score is 90
percent. PCPs are informed of the findings of the results of the audit.
PCPs that do not score at least 90 percent on the initial audit are offered a means of correcting a
deficiency immediately after review. A nurse reviewer will follow-up in one year to re-audit,
and the re-audit consists of at least three records seen by the PCP during the one year
monitoring period. We will also take steps to educate practitioners, including providing record-
M E D I C A L R E C O R D G U I D E L I N E S
5
August 2008
keeping aids, best practices distributed to the practitioner (such as the newsletter) and blinded
records.
ACCESSING MEDICAL RECORDS
The entire medical record of an active member must be maintained in the members PCPs
office. The file area should be secured and located in an area designed to prevent access by
unauthorized persons. The medical record of a member should be available for review and
documentation entry at the time of the members appointment.
Clinicians are responsible for maintaining the original medical records for all members,
including those who have terminated their Plan coverage. All clinicians must observe
applicable state and federal laws, rules and regulations concerning the confidentiality of
medical records.
You are required to supply a copy of your medical records to the Plan when requested for
quality purposes (i.e., medical record audit or quality investigation).
RELEASE OF INFORMATION TO MEMBERS
Members are entitled access to or copies of records concerning their health care. All or part of
the medical record may be released upon written authorization from the member or other
qualified persons in accordance with applicable state and federal law.
Qualified persons are appointed by members or the court to handle specific areas of
concern on the members behalf. Written consent must be on file or the member may give
verbal consent/authorization for release of information. Qualified persons other than the
member who may request access or copies on behalf of the member include, but are not
limited to:
Court-appointed committee for an incompetent.
Parent of a minor.
Court appointed guardian of a minor.
Other legally appointed guardian.
A written request, either in the form of a letter or an authorization form signed by the
patient should include:
Name of the physician from whom the information is requested.
M E D I C A L R E C O R D G U I D E L I N E S
6
August 2008
Name and address of the institution, agency or individual that is to receive the
information.
The members full name, address, date of birth and Plan identification number.
The extent or nature of the information to be released, including dates of treatment.
The date of initiation of authorization.
Signature of the member or qualified person.
Member requests should be honored within 10 days of the date of receipt of the written
authorization.
A member or qualified person may challenge the accuracy of information in the medical record
and may require that a statement describing the challenge be included in the record.
Access to member information may be denied only if the provider determines that access can
reasonably be expected to cause substantial harm to the member or others, or would have a
detrimental effect on the providers professional relationship with the patient or his or her
ability to provide treatment.
The physician may place reasonable limitations on the time, place and frequency of any
inspections of the patient information. Personal notes or observations may be excluded from
any disclosure based on the providers reasonable judgment.
Special authorizations, forms and procedures are required for HIV-related testing (both before
and after the test is performed) and for release of any HIV-related information from the medical
record. The informed consent form and the authorization for release of confidential HIV-
related information must be the New York State Department of Health approved forms or must
be forms that have been approved by the New York State Department of Health. All
authorizations requesting the release of behavioral health records must specify that the
information requested concerns behavioral health treatment.
It is recommended that providers consult legal counsel with specific questions surrounding
records disclosure issues. All Plan providers shall maintain the medical records of members for
six years after the date of service rendered or date the member no longer seeks care from that
provider. In the case of a minor, the records shall be retained for six years after the member
reaches the age of majority.
M E D I C A L R E C O R D G U I D E L I N E S
7
August 2008
ADVANCE DIRECTIVES
Advance directives are written instructions, such as a living will, durable power of attorney for
health care, health care proxy, or do not resuscitate (DNR) request, recognized under state law
and relating to the provision of health care when the individual is incapacitated and unable to
communicate his/her desires.
The Plan wishes to ensure compliance with the requests of any member regarding the type of
care he/she desires should the member become terminally ill or incapacitated and unable to
communicate his/her desires.
Upon enrollment in the Plan, and consistent with relevant federal and state law, each
member receives the following:
New York State Department of Health prepared description of state law entitled
Planning in Advance for Your Medical Treatment, which describes an individuals
rights in New York State with respect to health care decision-making.
New York State Department of Health prepared description of state law entitled
Appointing Your Health Care Agent - New York States Proxy Law, which provides
information and a sample form to be used to appoint a health care agent.
Letter describing the Plans policy implementing the requirements under the law and
regulations.
Plan contracted physicians should discuss advance directives with their patients as appropriate
and include in the medical record a copy of any advance directive document submitted by a
member. The medical record should clearly indicate that an advance directive has been
executed by the member and is included.
TELEPHONIC MEDICINE
The Plan policy is to advise practitioners regarding the practice of telephonic medicine.
Telephonic medicine includes, but is not limited to, diagnosis, treatment, other advice and
instructions given to patients over the phone. The Plan does not pay for telephonic
consultations as a separate billable service.
M E D I C A L R E C O R D G U I D E L I N E S
8
August 2008
The Plan expects the highest quality of care, including face-to-face interaction between the
patient and provider. The Plan seeks to assist practitioners in reducing medical errors and
liability risks.
Procedures
Document every phone call in the patients medical record.
Documentation in the record should be based on the same principles of documentation
during face-to-face interaction.
Whenever practical, the practitioner should have the patients medical records available
when telephone interaction is conducted from the practitioners office.
All covering physicians should provide the attending physician office notes of
telephonic interactions with patients, clearly labeled.
Office staff who interact with patients telephonically regarding medical issues including,
but not limited to, appointment reminders, refills and diagnostic reports should
document the telephonic interaction in the medical record.
PATIENT-CLINICIAN ELECTRONIC MAIL POLICY
The Plans policy is to provide clinicians communication guidelines regarding electronic mail
between patients and clinicians. The Plan expects the highest quality of care and privacy
assurance, including face-to-face interaction between the patient and clinician.
The Plan seeks to assist clinician in reducing medical errors and liability risk.
The Plan adapted the American Medical Associations guidelines last updated in December
2004.
For those practitioners who choose to utilize e-mail for selected patient and medical practice
communications, the guidelines listed below must be adopted.
CommunicationGuidelines:
Establishturnaroundtimeformessages.Exercisecautionwhenusingemailforurgent
matters.
Informpatientaboutprivacyissues.
Patientsshouldknowwho,besidesaddressee,processesmessagesduringaddressees
usualbusinesshoursandduringaddresseesvacationorillness.
M E D I C A L R E C O R D G U I D E L I N E S
9
August 2008
Wheneverpossibleandappropriate,physiciansshouldretainelectronicand/orpaper
copiesofemailscommunicationswithpatients.
Establishtypesoftransactions(prescriptionrefill,appointmentscheduling,etc.)and
sensitivityofsubjectmatter(HIV,mentalhealth,etc.)permittedoveremail.
Instructpatientstoputthecategoryoftransactioninthesubjectlineofthemessagefor
filtering:prescription,appointment,medicaladvice,billingquestion.
Requestthatpatientsputtheirnameandpatientidentificationnumberinthebodyofthe
message.
Configureautomaticreplytoacknowledgereceiptofmessages.
Sendanewmessagetoinformpatientofcompletionofrequest.
Requestthatpatientsuseautoreplyfeaturetoacknowledgereadingcliniciansmessage.
Developarchivalandretrievalmechanisms.
Maintainamailinglistofpatients,butdonotsendgroupmailingswhererecipientsare
visibletoeachother.Useblindcopyfeatureinsoftware.
Avoidanger,sarcasm,harshcriticism,andlibelousreferencestothirdpartiesin
messages.
Appendastandardblockoftexttotheendofemailmessagestopatients,which
containsthephysiciansfullname,contactinformation,andremindersaboutsecurity
andtheimportanceofalternativeformsofcommunicationforemergencies.
Explaintopatientsthattheirmessagesshouldbeconcise.
Whenemailmessagesbecometoolengthyorthecorrespondenceisprolonged,notify
patientstocomeintodiscussorcallthem.
Remindpatientswhentheydonotadheretotheguidelines.
Forpatientswhorepeatedlydonotadheretotheguidelines,itisacceptabletoterminate
theemailrelationship.
M E D I C A L R E C O R D G U I D E L I N E S
10
August 2008
MedicolegalandAdministrativeGuidelines:
Developapatientclinicianagreementfortheinformedconsentfortheuseofemail.This
shouldbediscussedwithandsignedbythepatientanddocumentedinthemedicalrecord.
Providepatientswithacopyoftheagreement.Agreementshouldcontainthefollowing:
Termsincommunicationguidelines(statedabove).
Provideinstructionsforwhenandhowtoconverttophonecallsandofficevisits.
Describesecuritymechanismsinplace.
Holdharmlessthehealthcareinstitutionforinformationlossduetotechnicalfailures.
Waiveencryptionrequirement,ifany,atpatientsinsistence.
Describesecuritymechanismsinplaceincluding:
Usingapasswordprotectedscreensaverforalldesktopworkstationsintheoffice,
hospital,andathome.
Neverforwardingpatientidentifiableinformationtoathirdpartywithoutthepatients
expresspermission(inwriting).
Neverusingpatientsemailaddressinamarketingscheme.
Notsharingprofessionalemailaccountswithfamilymembers.
Notusingunencryptedwirelesscommunicationswithpatientidentifiableinformation.
DoublecheckingallTofieldspriortosendingmessages.
Performatleastweeklybackupsofemailontolongtermstorage.Definelongtermas
thetermapplicabletopaperrecords.
Commitpolicydecisionstowritingandelectronicform.
The policies and procedures for e-mail should be communicated to all patients who desire to
communicate electronically.
The policies and procedures for e-mail should be applied to facsimile communications, where
appropriate.
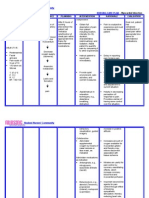
Pediatric and Adolescent Medical Record Review Tool
Primary Care Provider:
Member Name: DOB: Member I.D.#:
Provider Name: Provider I.D. #:
Product: Date of Review: Initials of Reviewer:
The Medical Record contains the following patient information:
1. Patient Identification
Each page within the medical record contains the patients name or ID number on both sides of
the page.
2. Personal Biographical Data
Mark off each data element found in medical record:
DOB
Gender
Address
Home Telephone Number(s)
Parent(s)/Guardian(s) Name(s)
Parent(s)/Guardian(s) Occupation(s)
Parent(s)/Guardian(s) Employer(s)
Parent(s)/Guardian(s) Work Telephone Number(s)
Grade in School/College
Name of School/College
3. All entries in the medical record contain the authors identification.
Author identification may be a handwritten signature, initials, an initials-stamped signature, or a
unique electronic identifier.
4. All entries in the medical record are dated.
5. The medical record is legible to someone other than the writer.
A second surveyor examines any record judged to be illegible.
The Medical Director prior to scoring must review all charts found to be illegible.
Page 1 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
6. Allergies and adverse reactions are prominently noted in the record, or NKA is noted.
Prominently noted refers to: on the front of the chart or inside the front cover of chart or on a
designated problem list or medication page or at the time of each office visit.
Updated at a minimum of annually (preferably during a physical).
7. Medication Record
A medication record/list includes dosages and dates for initial and refill prescriptions.
Discussion of medication side effects and symptoms with the member/parent/guardian and
documented.
8. Significant illnesses and medical conditions are indicated on the problem list.
The medical record contains a problem list that can either be a separate form or listed in the
progress notes.
And
The medical record contains a problem list that can either be a separate form or listed in the
progress notes, which must be updated as appropriate.
And
The problem list should contain all chronic, serious or disabling conditions and/or active (acute)
medical or psychosocial problems.
Or
For those patients without chronic, serious or disabling conditions and/or active (acute) medical
or psychosocial problems, the list should either indicate well visit or no problems/complaints.
[Ref.: Bates, 6
th
Ed.]
Page 2 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
9. The history and physical exam identifies appropriate subjective and objective information
pertinent to the patients presenting complaints.
The baseline history and physical are comprehensive and include a review of:
Baseline History:
Family history, psychosocial, and medical-surgical history must contain at least one qualifier.
Family history - including pertinent medical history of parents and/or sibling(s).
Psychosocial history - including occupation, education, ethnicity, primary language, living situation,
mental health issues/problems, socioeconomic issues/problems, and risk behaviors.
Medical-surgical history - including serious accidents, injuries, operations, illnesses/diseases (acute or
chronic), and mental health/substance abuse issues.
Prenatal care, delivery and birth history.
Baseline Physical:
A comprehensive review of systems with an assessment of presenting complaints (as applicable).
A comprehensive assessment of health and development (physical and psychosocial).
The periodic history and physical are comprehensive and include a review of:
Periodic History and Physicals:
Should be repeated in accordance with age appropriate preventive care guidelines.
Periodic History:
Family history, psychosocial, and medical-surgical history must contain at least one qualifier.
An updated family history.
An updated psychosocial history.
An updated medical-surgical history.
Periodic Physical:
A comprehensive review of systems with an assessment of presenting complaints, as applicable.
An updated assessment of health and development (physical and psychosocial)
[Ref.: Bates 6
th,
Ed.; HIP Preventative Health Care Service Guidelines for 2006]
Page 3 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
10. High-Risk Behaviors and Anticipatory Guidance
There is appropriate notation regarding the inquiry and/or teaching of specific topics and appropriate
notation concerning high-risk behavior inquiry. Based on the childs age, the inquiry(ies) and/or teaching
may be completed with the parent(s)/guardian(s). (If a topic is not applicable, indicate accordingly and
points are given).
Tobacco/Cigarette Query
Alcohol Query
Substance Abuse Query
Safe Sex practices
HIV/STD/Hepatitis Risk Query
Nutrition Guidance
Dental Referral
Injury/Safety Prevention
Violence/Abuse Query/Discussion
Social/Emotional Health/Depression Query
Activity/Exercise Query
Illness Prevention
Sleep Positioning Counseling
And
Is the patient/parent/guardian counseled regarding high-risk behavior(s) or referred to
appropriate treatment.
[Ref.: Bates 6
th
, Ed.; U. S. Preventative Health Task Force; HIP Preventative Health Care Services Guidelines 2006; Bright Futures.]
11. Laboratory and other studies are ordered, as appropriate.
Laboratory and other diagnostic studies are appropriate for the clinical findings and/or diagnoses
stated consistent with Preventive Health Care Guidelines.
[Ref.: Bates 6
th
Ed.; Lippincott Manual of Nursing Practice 6
th
Ed.; A Manual of Laboratory and Diagnostic Tests 5
th
Ed.]
August2008
Page 4 of 8
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
12. Communicable Disease(s) are reported to appropriate regulatory agencies and documented in the
MR. (Reference list of NYS/NYC reportable communicable diseases.
Document Communicable Disease and Regulatory Agency:
______________________________________________________________________________
13. Routine or follow-up visits must include:
A focused review of systems based upon presenting complaints, active (acute) medical or
psychosocial problems, or management of a chronic, serious or disabling condition.
Unresolved problems from previous office visits are addressed in subsequent visits.
14. Working diagnoses/impressions are consistent with subjective and objective findings.
[Ref.: Bates 6
th
Ed.]
15. Treatment plans are consistent with diagnoses.
The PCP addresses each chief complaint (subjective/objective) and the clinical finding with a
plan of care consistent with standards of care and clinical practice (including further diagnostic
testing, procedures, medication, referrals, etc).
The PCP documents discussion(s) and agreed upon decision (s) with the member/guardian of
potential treatment options that are available to them regarding their health care needs.
[Ref.: Bates 6
th
Ed.]
16. Follow-up Notation
Encounter forms or notes have a notation, when indicated, regarding follow-up care, calls, or visits.
The specific time to return is noted in days, weeks, months, or as needed.
[Ref.: NQA MRR 2006]
17. No-shows or missed appointments should be documented including follow-up efforts to
reschedule appointment.
Page 5 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
18. Follow-up after an ER visit or hospitalization. Date(s) listed for ER and/or
Hospitalizations:_________________________________________________________
An office visit, written correspondence, or telephone follow-up intervention is clearly documented
in the PCP record.
19. Continuity of Care
Indicate whether a specialist consultation:
Name/Specialty: _________________________
Or
If whether a diagnostic study:
Name of Diagnostic Study: ___________________________
If a consultation or diagnostic study is requested, there is a note or report from the consultant in
the record.
The ordering health care provider initials consultation and diagnostic study reports filed in the
chart.
Abnormal consultation and diagnostic study results have an explicit notation of follow-up plans
in the record.
[Ref. : NCQA 2006]
20. The medical record reflects an appropriate utilization of consultants.
Review of Medical Record for Under- or Over- Utilization of Referrals to Consultants.
Evidence of Under Utilization: Yes or No
Definition: Unresolved acute or chronic illness(es) and/or symptoms are being actively treated or
monitored by the PCP without referral(s) to an appropriate specialist/consultant.
Evidence of Over Utilization: Yes or No
Definition: A consistent pattern of referrals to a consultant without PCP formulating a treatment plan based
on assessment of presenting symptoms.
Page 6 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
21. Care rendered is medically appropriate.
(If this standard is not met, the case is immediately referred to the Medical Director for a quality of care review).
Definition: There is evidence that the patient may be placed at inappropriate risk by an inadequate(ly),
incorrect(ly), or inappropriate(ly):
Performed physical examination or assessment.
Performed procedure.
Performed diagnostic studies, including, but not limited to, lost specimens, poor film quality,
misread results, or delayed turnaround time.
Diagnosed the member.
Prescribed, dispensed, or administered medication.
Developed and/or implemented treatment plan.
Other errors, delays or omissions in the delivery of care.
[Ref.: Vytra Health Plans Quality of Care Complaint Policy and Procedure 2003]
22. Immunization
An appropriate immunization history has been made with notation that immunizations are up to
date (See Adult Immunization Schedule).
Immunizations administered after May, 1992 contain lot number and manufacturers name.
(Must have 100% compliance)
[Ref.: CDC; U.S. Preventative Task Force; NYSDOH; HIP Health Plans Preventive Health Service Guidelines for 2006]
23. Advance Directives
Documentation in the Medical Record of all patients (patients/guardians depending on age) at least
45 years and older (if younger, as appropriate) that advance directives have been discussed. If the
patients choice is to make an advance directive, there should be a copy of it in the MR and the
records should be flagged.
Page 7 of 8
August2008
Member Name: Member ID#:
Pediatric and Adolescent Medical Record Review Tool (continued)
24. Preventive Health Guidelines. Indicate: Male Female Age: ___________
There is evidence that preventive screening and services are offered in accordance with the organizations
practice guidelines. (Reference 2006 HIP PHG)
(Refer to high-risk behaviors for additional screening not included in this section.)
Measurements:
Height
Weight
BMI
Head Circumference
Blood Pressure
Sensory Screening
Vision Screening
Hearing Screening
Developmental/Behavioral Milestones by history and appropriate physical examination. If
suspicious, by specific objective developmental testing.
Parenting Skills should be fostered at every visit.
Procedures: General
Lead Testing (NYS Mandated)
H&H
Urinalysis
Hereditary and Metabolic Screening (e.g.: Thyroid, Hemoglobinopathies, PKU, Galactosemia)
Procedures: At Risk
TB Testing
Cholesterol Screening
HIV/STD/Hepatitis
Pelvic Exam (Offered for sexually active females as applicable)
[Ref.: U.S. Preventative Task Force; NYS DOH; HIP Health Plans Preventive Health Service Guidelines for 2006; CDC]
25. Child Abuse
Screening for child abuse is conducted
Suspected child abuse is reported to appropriate regulatory agencies and documented.
End of Pediatric and Adolescent Medical Record Review Tool
Page 8 of 8
***All forms of medical record documentation are acceptable. ***
August2008
LIST OF VACCINES FOR PEDIATRIC AND ADOLESCENT-MRR REPORTING
Member Name: Member ID#:
Name of Vaccine Comments
Administered
Yes/No
Date If
Administered
xx/xx/xxxx
Hepatitis B At birth ALL newborns should receive monovalent Hep B soon
after birth and before hospital discharge.
Following the Birth Dose, the HepB series should be completed
with either monovalent HepB or a combination vaccine containing
HepB.
The2
nd
dose should be admin. at age 1-2 months.
The final dose should be administered at age >=24 months.
It is permissible to admin. 4 doses of HepB.
DPT The 4
th
dose of DtaP may be administered as early as age 12 months,
provided 6 months have elapsed since the 3
rd
dose and the child is
unlikely to return at age 15-18 months. The final dose in the series
should be given at age >=4 years.
HIB Three HIB conjugate vaccines are licensed for infant use.
The final dose in the series should be admin. at age >=12 months.
Inactivated Polio 4 doses.
2 months, 4 months, between 6-18 months and 4-6 years.
MMR The 2
nd
dose of MMR is recommended routinely at age 4-6 years, but
may be admin. during any visit, provided at least 4 weeks have elapsed
since the 1
st
dose and both doses are admin. beginning at or after age
12 months.
Hepatitis A HepA is recommended for all children 1 year of age (ie: 12-23
months).
The 2 doses in the series should be admin. at least 6 months apart.
HepA is also recommended for certain high risk groups.
Meningococcal MCV4 is recommended as a routine vaccination for:
Persons aged 11--12 years,
Adolescents at high school entry (i.e., at approximately age 15
years) if not previously vaccinated with MCV4,
College freshmen living in dormitories.
Other persons at increased risk for meningococcal disease (i.e.,
military recruits and travelers to areas where meningococcal
disease is hyperendemic or epidemic, microbiologists who are
routinely exposed to isolates of Neisseria meningitidis, persons
with anatomic or functional asplenia, and persons with terminal
complement deficiency)
o As of May 2006, there is a supply shortage of this vaccine
and the recommendation is to, until further notice, defer
administration of MCV4 to persons aged 11-12 years.
Page 1 of 2
List of Vaccines for Pediatric and Adolescent-MRR Reporting (continued)
Member Name: Member ID#:
Name of Vaccine Comments Administered
Yes/No
Date If
Administered
xx/xx/xxxx
Varicella The first dose of varicella vaccine is recommended at 12 to 15
months old.
Recommendation from the ACIP to the CDC re: a second dose of
varicella (chickenpox) vaccine for children four to six years old to
further improve protection against the disease.
Pneumococcal 4 doses. Is recommended for all children ages 2-23 months and for
certain children aged 24-59 months. The final dose in the series
should be given at age >=12 months.
Influenza Annually for children aged >=6 months with certain risk factors.
In addition, health children aged 6-23 months and close contacts of
healthy children aged 0-5 months are recommended to receive the
vaccine.
For healthy persons aged 5-49 years, the intranasally admin. Live,
attenuated vaccine is an acceptable alternative to the IM vaccine.
HPV HPV Vaccine is a newly licensed vaccine designed to protect against
human papillomavirus virus (HPV) and is to be routinely given to girls
when they are 11-12 years old. The ACIP recommendation also allows
for vaccination of girls beginning at nine years old as well as
vaccination of girls and women 13-26 years old. According to the
ACIPs recommendation, three doses of the new vaccine should be
routinely given to girls when they are 11 or 12 years old. The advisory
committee, however, noted that the vaccination series can be started as
early as nine years old at the discretion of the physician or health care
provider. The recommendation also includes girls and women 13-26
years old because they will benefit from getting the vaccine. The
vaccine should be administered before onset of sexual activity (i.e.,
before women are exposed to the viruses), but females who are
sexually active should still be vaccinated.
RotoVirus Recommendations of the Advisory Committee on Immunization
Practices (ACIP): In February 2006, a live, oral, human-bovine
reassortant rotavirus vaccine (RotaTeq
) was licensed for use among
U.S. infants. The Advisory Committee on Immunization Practices
recommends routine vaccination of U.S. infants with 3 doses of this
rotavirus vaccine administered orally at ages 2, 4, and 6 months. The
first dose should be administered between ages 6 12 weeks.
Subsequent doses should be administered at 4 10 week intervals, and
all 3 doses should be administered by age 32 weeks. Rotavirus vaccine
can be co-administered with other childhood vaccines. Rotavirus
vaccine is contraindicated for infants with a serious allergic reaction
to any vaccine component or to a previous dose of vaccine.
Page 2 of 2
Medical Record Review for Dr. Medical Group/Network:
Member Name: Member ID#:
Childhood Immunizations Tool
CRITERIA YES NO N/A
1. All immunizations are received within two years of age.
DTP 1 DTP 2 DTP 3 DTP 4
OPV 1 OPV 2 OPV 3
MMR
HIB between 1
st
and 2
nd
birthday HIB 2 HIB 3
Hep between 6 months and 2
nd
birthday Hep 2 Hep 3
VZV
2. There is evidence of a lead test completed by the 25
th
month of birth.
3. There is a contraindication indicated if the child did not receive all
immunizations within the appropriate timeframe.
June2007
Asthma Medical Record Review Tool
Primary Care Provider
Member Name: DOB: Member ID #:
Provider Name: Provider ID#:
Date of Review: Initials of Reviewer:
The Medical Record contains the following patient information:
1. Detailed Medical History Annually
Symptoms (cough, wheezing, shortness of breath, chest tightness, sputum production).
Pattern of Symptoms (seasonal, episodic, frequency, nocturnal).
Precipitating and /or Aggravating Factors (infections, environmental, smoking, exercise, occupational).
Development of Disease and Treatment (age of onset, present management and response).
Family History (history of asthma, allergy, sinusitis, rhinitis, eczema, or nasal polyps in close relatives).
Social History (daycare, social support, employment, social factors that interfere with adherence).
History of Exacerbations (onset, duration, frequency, severity, usual patterns and management).
Impact of Asthma on Patient and Family (episodes, number of days missed from school/work).
Assessment of Patients and Familys Perceptions of Disease (ability of patient to cope with disease).
Score
2. Physical Examination Every 6 Months
Upper Respiratory Tract (increased nasal secretion, mucosal swelling, and/or nasal polyp).
Chest (sounds of wheezing during normal breathing or prolonged phase of forced exhalation).
Skin (atopic dermatitis, eczema).
Score
3. Spirometry (in patients > 4 years of age) Every 2 Years.
Score
4. Assessment and Monitoring Every 6 Months
Classification of Asthma Severity (intermittent, mild-persistent, moderate-persistent or severe-persistent).
Classification of Asthma Control (well controlled, not well controlled, very poorly controlled).
Score
5. Patient Education Every 6 Months
Taking Medications Correctly (inhaler technique, use of devices).
Identifying and Avoiding Environmental Exposures That Worsen the Patients Asthma (allergens, irritants).
Self-Monitoring (assess level of asthma control, monitor symptoms, recognize early signs and symptoms).
Using a Written Asthma Action Plan (take daily actions to control asthma, adjust medication).
Seeking Medical Care as Appropriate.
Page 1 of 2 Score
August2008
Asthma Medical Record Review Tool (continued)
Member Name: DOB: Member ID #:
6. Control of Environmental Factors and Comorbid Conditions That Affect Asthma Every 6 Months
Allergen and Irritants (tobacco smoke, dust mites, animal dander, cockroach, indoor mold, pollen).
Comorbid Conditions (allergic bronchopulmonary aspergillosis, GERD, obese, obstructive sleep apnea).
Score
7. Medications Every 6 Months
Long-Term Control (corticosteroids, cromolyn sodium, omalizumab, theophylline, LABA).
Quick-Relief (albuterol, levalbuterol, pirbuterol, systemic corticosteroids, anticholinergics).
Score
8. Immunizations Annually
Influenza (safe for administration to children over 6 months of age and adults).
Score
9. Regular Follow-up Contact
To achieve control of asthma, evaluate the patient after 2 to 6 weeks of the visit.
To maintain control of asthma, schedule patient contact at 1- to 6-month intervals.
Score
10. Referrals as Needed
Disease Management Program.
Asthma Specialist.
Score
Page 2 of 2 Total Score
August2008 24
Congestive Heart Failure Tool
Primary Care Practitioner
Member Name: Gender: DOB: Member ID#:
Provider Name: Provider ID#:
Date of Review: Initials of Reviewer:
The Medical Record contains the following patient information:
1. LVF Assessment (annually)
2-dimensional echocardiography or
Radionuclide ventriculography
Score
2. Weight Measurement (each visit)
Score
3. Blood Pressure Measurement (each visit)
Score
4. Assessment of Clinical Signs and Symptoms of Volume Overload (Excess) (each visit)
Dyspnea or Orthopnea
Peripheral Edema or Rales or Hepatomegaly or Ascites or J ugular venous pressure or S3 or S4 gallop
Score
5. Assessment of Activity Level (each visit)
Score
6. Patient Education (each visit)
Smoking cessation
Alcohol
Illicit drug use
Weight monitoring
Diet (sodium restriction)
Physical activity
Medication instruction
Minimizing or avoiding use of NSAIDs
Specific educational or management programs
Prognosis/end-of-life issues
Score
7. Beta-Blocker Therapy for patients with LVEF < 40%
Score
8. Ace Inhibitor or ARB Therapy for patients with recent MI and LVEF < 40%
Score
9. Warfarin Therapy for Patients with Atrial Fibrillation
Page 1 of 2 Score
August 2008
Congestive Heart Failure Tool PCP (continued)
Member Name: DOB: Member ID#:
10. Laboratory Tests (annually)
Complete blood count
Urinalysis
Serum electrolytes (including calcium and magnesium)
Blood urea nitrogen
Blood glucose
Blood lipids
Liver function tests
Thyroid-stimulating hormone
Chest radiograph
12-lead electrocardiogram
Page 2 of 2 Score
Total Score
August 2008
Diabetes Medical Record Review
Primary Care Practitioner
Member Name: Gender: DOB: Member ID#:
Provider Name: Provider ID#:
Date of Review: Initials of Reviewer:
1. Medical History
Eating patterns, nutritional status, and weight history.
Current treatment of diabetes, including medications, meal plan and glucose monitoring.
Exercise history.
DKA frequency, severity and cause.
Hypoglycemic episodes: frequency, severity and cause.
2. Physical Examination
Blood pressure @ every routine diabetic visit.
Annual dilated eye exams.
Thyroid palpation annually.
Skin examination (for acanthosis nigricans and insulin injection sites) annually.
Neurological/foot examination annually.
Inspection.
Palpation of pedal pulses.
3. Laboratory Evaluation
A1C every 3 months for abnormal results, every 6 months for normal results.
Fasting lipid profile, including total LDL and HDL cholesterol and triglycerides (annually).
Liver function tests (annually).
Test for microalbuminuria (annually).
Serum creatinine and calculated glomerular filtration rate (annually).
4. Self-Monitoring of Blood Glucose Annually
Evaluate the patients technique and ability to use data to adjust therapy @ diabetic visit.
5. Obesity Management for BMI>24
Education on nutrition (annually).
Education on physical activity (annually).
Weight (annually).
6. Psychosocial Screening Annually
Should include attitudes about illness, expectations for medical management and outcomes.
Page 1 of 2
August2008
Diabetes Medical Record Review PCP (continued)
Member Name: DOB: Member ID#:
7. Immunization
Influenza Vaccine annually.
Pneumococcal vaccine (per guidelines).
8. High Risk Screening Annual
Advise all patients not to smoke.
Advise all patients on alcohol consumption 1-2 drinks per day.
9. Adherence to Plan
The PCP documents discussions of treatment options and agreed upon decision with member.
10. Assessment of Complications
Referrals if needed.
Ophthalmology.
Nutritionist.
Diabetes educator if not provided by office.
Podiatrist.
Nephrologist.
11. The medical record is legible to someone other than the writer. (Not scored.)
A second surveyor examines any record judged to be illegible.
The Medical Director prior to scoring must review all charts found to be illegible.
12. Care rendered is medically appropriate. (Not scored.)
(If this standard is not met, the case is immediately referred to the Medical Director for a quality of care review.)
Definition: There is evidence that the patient may be placed at inappropriate risk by an inadequate(ly),
incorrect(ly), or inappropriate(ly):
Performed physical examination or assessment.
Performed procedure.
Performed diagnostic studies, including, but not limited to, lost specimens, poor film quality, misread
results, or delayed turnaround time.
Diagnosed the member.
Prescribed, dispensed, or administered medication.
Developed and/or implemented treatment plan.
Other errors, delays or omissions in the delivery of care.
Page 2 of 2
August2008
Adult Medical Record Review Tool -- Primary Care Provider
Member Name: DOB: Member I.D.#:
Provider Name: Provider I.D. #:
Product: Date of Review: Initials of Reviewer:
The Medical Record contains the following patient information:
1. Patient Identification.
Each page within the Medical Record contains the patients name or ID number on both sides of
the page.
2. Personal Biographical Data.
Mark off each data element found in the medical record:
DOB.
Gender.
Address.
Home Telephone Number(s).
Employer.
Occupation.
Work Telephone Number(s).
Marital Status.
Name of Next of Kin/Significant Other/Proxy.
Telephone Number(s) of Next of Kin/Significant Other/Proxy.
3. All entries in the medical record contain the authors identification.
Author identification may be a handwritten signature, initials, an initials-stamped signature, or a
unique electronic identifier.
4. All entries in the medical record are dated.
5. The medical record is legible to someone other than the writer. (No score.)
A second surveyor examines any record judged to be illegible.
The Medical Director prior to scoring must review all charts found to be illegible.
Page 1 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
6. Allergies and Adverse Reactions are prominently noted in the record, or NKA is noted.
Prominently noted refers to: on the front of the chart or inside the front cover of the chart or on
a designated problem list or medication page or at the time of each office visit.
Updated at a minimum of annually (preferably during a physical).
7. Medication Record
A medication record/list includes dosages and dates for initial and refill prescriptions.
Discussion of medication side effects and symptoms are reviewed with the member and
documented.
8. Significant illnesses and medical conditions are indicated on the problem list.
The Medical Record contains a problem list that can either be a separate form or listed in the
progress notes.
And
The Medical Record contains a problem list that can either be a separate form or listed in the
progress notes, which must be updated as appropriate.
And
The problem list should contain all chronic, serious or disabling conditions and/or active (acute)
medical or psychosocial problems.
Or
For those patients without chronic, serious or disabling conditions and/or active (acute) medical
or psychosocial problems, the list should either indicate well visit or no
problems/complaints.
[Ref.: Bates, 6
th
Ed.]
Page 2 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
9. The history and physical exam identifies appropriate subjective and objective information
pertinent to the patients presenting complaints.
The baseline history and physical is comprehensive and includes a review of:
Baseline History:
Family history, psychosocial, and medical-surgical history must contain at least one qualifier.
Family history - including pertinent medical history of parents and/or sibling(s),
Psychosocial history - including occupation, education, ethnicity, primary language, living
situation, mental health issues/problems, socioeconomic issues/problems, risk behaviors,
Medical-Surgical history - including serious accidents, injuries, operations, illnesses/diseases
(acute or chronic), and mental health/substance abuse issues.
Baseline Physical:
A comprehensive review of systems with an assessment of presenting complaints (as
applicable).
A comprehensive assessment of health and development (physical and psychosocial).
The periodic history and physicals is/are comprehensive and includes a review of:
Periodic History and Physicals:
Should be repeated in accordance with age appropriate preventive care guidelines
Periodic History must contain
Family history, psychosocial, and medical-surgical history must contain at least one qualifier.
An updated family history,
An updated psychosocial history,
An updated medical-surgical history.
Periodic Physical must contain
A comprehensive review of systems with an assessment of presenting complaints, as applicable.
An updated assessment of health and development (physical and psychosocial).
[Ref.: Bates 6
th,
Ed.; HIP Preventative Health Care Service Guidelines for 2006]
Page 3 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
10. High-Risk Behaviors and Anticipatory Guidance.
There is appropriate notation regarding the inquiry and/or teaching of specific topics and
appropriate notation concerning high-risk behavior inquiry.
Tobacco/Cigarette Query.
Alcohol Query.
Substance Abuse Query.
HIV/STD/Hepatitis Risk Query.
Safe Sex Practices.
Nutrition Guidance.
Injury/Safety Prevention.
Violence/Abuse Query/Discussion.
Social/Emotional Health Query/Depression.
Activity/Exercise Query.
Illness Prevention.
And
Is the patient counseled regarding high-risk behavior(s) or referred to appropriate treatment?
[Ref.: Bates 6
th
, Ed.; U. S. Preventative Health Task Force; HIP Preventative Health Care Service
Guidelines for 2006]
11. Laboratory and other studies are ordered, as appropriate.
Laboratory and other diagnostic studies are appropriate for the clinical findings and/or diagnoses
stated consistent with Preventive Health Care Guidelines.
[Ref.: Bates 6
th
Ed.; Lippincott Manual of Nursing Practice 6
th
Ed.; A Manual of Laboratory and Diagnostic Tests 5
th
Ed.]
12. Communicable Disease(s) are reported to appropriate regulatory agency and documented in the
MR. (Reference list of NYS/NYC reportable communicable diseases).
Document Communicable Disease and Regulatory Agency:
______________________________________________________________________________________________________
Page 4 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
13. Routine or follow-up visits must include:
A focused review of systems based upon presenting complaints, active (acute) medical or
psychosocial problems, or management of a chronic, serious or disabling condition.
Unresolved problems from previous office visits are addressed in subsequent visits.
14. Working diagnoses/impressions are consistent with subjective and objective findings.
[Ref.: Bates 6
th
Ed.]
15. Treatment plans are consistent with diagnoses.
Addresses each chief complaint (subjective/objective) and clinical finding with a plan of care
consistent with standards of care and clinical practice (including, further diagnostic testing,
procedures, medication, referrals, etc)
The PCP documents discussion(s) and agreed upon decision (s) with the member/guardian of
potential treatment options that are available to them regarding their health care needs.
[Ref.: Bates 6
th
Ed.]
16. Follow-up Notation
Encounter forms or notes have a notation, when indicated, regarding follow-up care, calls, or visits.
The specific time of return is noted in days, weeks, months, or as needed.
[Ref.: NCQA MRR 2006]
Page 5 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
17. Follow-up after an ER visit or hospitalization. Date(s) listed for ER and/or hospitalizations:
_______________________________________________________
An office visit, written correspondence, or telephone follow-up intervention is clearly documented
in the PCP record regarding the ER or IP LOS.
18. Continuity of Care
Indicate whether a specialist consultation: Name/Specialty: __________________________
Or
If whether a diagnostic study: Name of Diagnostic Study: ___________________________
If a consultation or diagnostic study is requested, there is a note or report from the consultant
in the record.
The ordering health care provider initials consultation and diagnostic study reports filed in the
chart.
Abnormal consultation and diagnostic study results have an explicit notation of follow-up
plans in the record.
19. Immunization
An appropriate immunization history has been made with notation that immunizations are up
to date (See Adult Immunization Schedule).
Immunizations administered after May, 1992 contain lot number and manufacturers name.
(Must have 100% compliance)
[Ref.: CDC; U.S. Preventative Task Force; NYSDOH; HIP Health Plans Preventive Health Service Guidelines for 2006]
Page 6 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
20. The Medical Record reflects an appropriate utilization of Consultants. (No score.)
Review of Medical Record for Under or Over Utilization of Referrals to Consultants
Evidence of Under Utilization: Yes or No
Definition: Unresolved acute or chronic illness (es) and/or symptoms are being actively treated or
monitored by the PCP without referral(s) to an appropriate specialist/consultant.
Evidence of Over Utilization: Yes or No
Definition: A consistent pattern of referrals to a consultant without PCP formulating a treatment
plan based on assessment of presenting symptoms.
21. Care rendered is medically appropriate. (No score.)
(If this standard is not met, the case is immediately referred to the Medical Director for a quality of
care review).
Definition: There is evidence that the patient may be placed at inappropriate risk by an
inadequate (ly), incorrect (ly), or inappropriate(ly):
Performed physical examination or assessment.
Performed procedure.
Performed diagnostic studies, including, but not limited to, lost specimens, poor film quality,
misread results, or delayed turnaround time.
Diagnosed the member.
Prescribed, dispensed, or administered medication.
Developed and/or implemented treatment plan.
Other errors, delays or omissions in the delivery of care.
[Ref.: Vytra Health Plans Quality of Care Complaint 4/15/2003]
22. Advance Directives (No score.)
Documentation in the Medical Record of all patients at least 45 years and older (if younger as
appropriate) that advance directives have been discussed. If the patient chose is to make an advance
directive, there should be a copy of it in the MR and the records should be flagged.
Page 7 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
23. Preventive Health Guidelines. Indicate:
Male______ Female______ and Age: _______
There is evidence that preventive screening and services are offered in accordance with the organizations practice
guidelines. (Reference 2006 HIP PHG)
(Refer to high-risk behaviors for additional screening not included in this section.)
Measurements
Blood Pressure Once every 2 years.
Pulse/Respirations and Temperature (as appropriate).
Weight.
Height.
BMI.
Procedures/Screening
Cholesterol Starting at 20 years, obtained once every 5 years.
EKG Test to be done for patients at high risk.
Diabetes Screening Starting at age 45 every 3 years.
Abdominal Aortic Screening One-time screening by U/S for men 65-75 smokers.
TB Skin testing for asymptomatic high-risk patients.
Osteoporosis Screening/Testing Age 65 and older, routine screening every 2 years.
Preconception Screening for all women of childbearing age.
RubellaTesting Routine screening for all women of childbearing age at first health visit.
Menopause Screening at physicians discretion.
Vision Screening Annually.
Hearing Screening Starting at 20 years, obtained once every 10 years.
Dental Health Screening Regular check ups.
Chlamydia All sexually active females <26 years, as well as others at risk.
Cancer Screening Examinations
Breast Exam/Mammography Annually for ages 40 and older.
Pap Smear Annually.
Sigmoidoscopy/Fecal Occult Blood/Colonoscopy at 50 both men and women every 5 years.
Prostate Examination/PSA Annually beginning at age 50.
Skin Cancer Routine checkup.
Chemoprevention
Aspirin for Prevention of CHD As PCP advises.
[Ref.: U.S. Preventative Task Force; CDC, HIP Health Plans Preventive Health Service Guidelines for 2006]
Page 8 of 9
August2008
Member Name: Member ID#:
PCP Adult Medical Record Review Tool (continued)
24. No shows or missed appointments.
Missed appointments should be documented.
Follow-up efforts to reschedule appointment.
25. Medical Record Reflects documentation of Care for Older Adults (65 years and greater)
Evidence of Pain Screening (should be preformed at every visit): Yes or No
Can include documentation of either of the following:
Notation of the presence or absence of pain.
Notation of the results of a screening using a standardized tool.
Evidence of a Functional Assessment: Yes or No
Can include documentation of any of the following:
Functional independence.
Loss of independent performance.
Activities of daily living (ADLs).
Social activities.
Instrumental ADLs (IADLs).
The level of assistance needed to accomplish various tasks.
Result of assessment using a standardized functional status assessment tool.
Evidence of Medication Review: Yes or No
Definition: The percentage of older adults who had the presence of a medication list in the medical
record AND a medication review during the measurement year.
Evidence of Advance Care Planning: Yes or No
Definition: Notation of a discussion about preferences for resuscitation, life-sustaining treatment
and end of life care or a patients refusal to discuss advance care planning..
End of PCP Adult Medical Record Review Tool
Page 9 of 9
***All forms of medical record documentation are acceptable***
August2008
List of Vaccines for Adults
Based on 10/05-9/06 Adult Immunization Recommendations, US
List of Vaccines for Adults-MRR Reporting
Name of Vaccine Comments Administered
Yes/No
Date If
Administered
xx/xx/xxxx
Vaccines Needed By All Adults
Hepatitis B Vaccines Adults at Risk
MMR Vaccine Susceptible Adults
Td Vaccine All Adults, Every 10 Years
Vaccines for Travelers Seek NYS DOH/Immigration
Requirements
Varicella Vaccine Susceptible Adults
Vaccines Needed For Those Age 50 and older
Influenza Vaccine (Flu)
Vaccines Needed For Those Age 65 and Older
Pneumococcal Vaccine
Vaccines Needed For Health Care Workers
Hep B
Influenza Vaccine Annually for the Flu
MMR Vaccine
Varicella Vaccine
June2007
Adult Preventive Care Flow Sheet
Patient Name: Medical Record #:
Date of Birth: Sex: M / F Height:
SCREENINGS AND TESTS GUIDELINES ENTER DATE(S) AND RESULT(S)
Smoking Status Every patient at every visit Date / / / / / / / /
(Never/Past/Current) Result
Blood Pressure Every 1 - 2 years Date / / / / / / / /
Result
Body Mass Index* Date / / / / / / / /
Result
Fasting Plasma Glucose 45 y.o. and BMI > 25; Date / / / / / / / /
patients with hypertension or dyslipidemia Result
Cholesterol Every 5 years for: M > 35 y.o. Date / / / / / / / /
F > 45 y.o. Result
HIV Status Ask every patient; offer test if status Date / / / / / / / /
is unknown Result
Depression Screen every patient Date / / / / / / / /
(Use PHQ-2 tool*) Result
Alcohol and Drug Use Screen every patient Date / / / / / / / /
(Use CAGE-AID tool*) Result
Colonoscopy Every 10 years for > 50 y.o. Date / / / / / / / /
Result
Pelvic/Pap Test Every 1 - 3 years Date / / / / / / / /
Result
Mammogram Every 1 - 2 years > 40 y.o. Date / / / / / / / /
Result
IMMUNIZATIONS GUIDELINES ENTER DATE(S) AND VACCINE INFORMATION
Influenza > 50 y.o. and others at high-risk; Date / / / / / / / /
Annually
Pneumococcal > 65 y.o. (high-risk, 1
st
dose at < 65 y.o., Date / / / /
2
nd
dose at 65 y.o. or 5 years from 1
st
dose)
Hepatitis B High-risk groups; 3 or 4 dose series Date / / / / / / / /
Tetanus & Diphtheria Every 10 years Date / / / / / / / /
OTHER IMMUNIZATIONS
Date / / / / / /
Type
Date / / / / / /
Type
HEALTH COUNSELING ENTER DATE(S), TOPIC AND GOALS
Date Topic Patient Self-Management Goals
/ /
/ /
/ /
/ /
/ /
/ /
/ /
Smoking Cessation
Healthy Weight
Physical Activity
Nutrition
Condom Use/
HIV/STD Prevention
Family Planning
Drug Use
Domestic Violence
Injuries (e.g. seatbelts,
falls, etc.)
Folate
Calcium Supplement
Polypharmacy
High-Risk Travel
Varicella: Non-immune, 2 doses
Rubella: Non-pregnant women of childbearing age & healthcare workers, 1 dose
High-risk travel: Recommendations by country: www.cdc.gov/travel
P
a
t
i
e
n
t
s
*See back for BMI chart, PHQ-2, and CAGE-AID
Adapted from the U.S. Preventive Services Task Force, the Centers for Disease Control and Prevention, the National Institutes of Health, and the American Diabetes Association.
/ /
BMI= x703
(Height in inches) x (Height in inches)
(Weight in Pounds)
( )
The New York City Department of Health and Mental Hygiene
ADDITIONAL SCREENINGS ENTER DATE(S) AND RESULT(S)
AND TESTS
STD Screen (if sexually active) Hearing HCT
Vision Skin Thyroid Function
Glaucoma (high-risk: Q 2 years, others: Q 3 - 4 years) Oral Cavity Rubella Titer ( of child-bearing age)
Cognitive and Functional Impairment Urinalysis Prostate/Testicular Cancer
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
Date / / / / Date / / / /
Result Result
BODY MASS INDEX (BMI) FOR ADULTS
4'10" 91 96 100 105 110 115 119 124 129 134 138 143 148 153 158 162 167 172 177 181 186 191 196 201 205 210 215
4'11" 94 99 104 109 114 119 124 128 133 138 143 148 153 158 163 168 173 178 183 188 193 198 203 208 212 217 222
5' 97 102 107 112 118 123 128 133 138 143 148 153 158 163 168 174 179 184 189 194 199 204 209 215 220 225 230
5'1" 106 111 116 122 127 132 137 143 148 153 158 164 169 174 180 185 190 195 201 206 211 217 222 227 232 238
5'2" 109 115 120 126 131 136 142 147 153 158 164 169 175 180 186 191 196 202 207 213 218 224 229 235 240 246
5'3" 113 118 124 130 135 141 146 152 158 163 169 175 180 186 191 197 203 208 214 220 225 231 237 242 248 254
5'4" 116 122 128 134 140 145 151 157 163 169 174 180 186 192 197 204 209 215 221 227 232 238 244 250 256 262
5'5" 120 126 132 138 144 150 156 162 168 174 180 186 192 198 204 210 216 222 228 234 240 246 252 258 264 270
5'6" 124 130 136 142 148 155 161 167 173 179 186 192 198 204 210 216 223 229 235 241 247 253 260 266 272 278
5'7" 127 134 140 146 153 159 166 172 178 185 191 198 204 211 217 223 230 236 242 249 255 261 268 274 280 287
5'8" 131 138 144 151 158 164 171 177 184 190 197 203 210 216 223 230 236 243 249 256 262 269 276 282 289 295
5'9" 135 142 149 155 162 169 176 182 189 196 203 209 216 223 230 236 243 250 257 263 270 277 284 291 297 304
5'10" 139 146 153 160 167 174 181 188 195 202 209 216 222 229 236 243 250 257 264 271 278 285 292 299 306 313
5'11" 143 150 157 165 172 179 186 193 200 208 215 222 229 236 243 250 257 265 272 279 286 293 301 308 315 322
6' 147 154 162 169 177 184 191 199 206 213 221 228 235 242 250 258 265 272 279 287 294 302 309 316 324 331
6'1" 151 159 166 174 182 189 197 204 212 219 227 235 242 250 257 265 272 280 288 295 302 310 318 325 333 340
6'2" 155 163 171 179 186 194 202 210 218 225 233 241 249 256 264 272 280 287 295 303 311 319 326 334 342 350
6'3" 160 168 176 184 192 200 208 216 224 232 240 248 256 264 272 279 287 295 303 311 319 327 335 343 351 359
6'4" 164 172 180 189 197 205 213 221 230 238 246 254 263 271 279 287 295 304 312 320 328 336 344 353 361 369
Locate height and weight range. The number at the top of the column is the BMI. Maximum healthy weight is defined as BMI < 25.
BODY MASS INDEX (BMI) FOR ADULTS
BMI 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 39 40 41 34 35 36 37
Weight in Pounds
Healthy Weight Overweight Obese Extremely Obese
42 43 44 45 38
156
100
104
107
110
114
118
121
125
132
128
136
140
144
148
152
BMI is a general measure and healthy limits may vary for some groups.
To calculate exact BMI: weight in pounds height in inches squared X 703.
Source: National Heart, Lung and Blood Institute (www.nhlbi.nih.gov/guidelines/obesity/bmi_tbl.htm).
BMI is a general measure and healthy limits may vary for some groups.
Source: National Heart, Lung and Blood Institute (www.nhlbi.nih.gov/guidelines/obesity/bmi_tbl.htm).
Over the past 2 weeks, have you often been bothered by:
1. Little interest or pleasure in doing things? Yes No
2. Feeling down, depressed, or hopeless? Yes No
If the patient responded yes to either question, follow-up using the
PHQ-9, a nine-item, self-administered questionnaire.*
*www.depression-primarycare.org/images/pdf/phq_9_quest.pdf
DEPRESSION SCREENING TOOL: Patient Health Questionnaire (PHQ-2)
1. Have you felt you ought to Cut down on your drinking or drug use? Yes No
2. Have people Annoyed you by criticizing your drinking or drug use? Yes No
3. Have you felt bad or Guilty about your drinking or drug use? Yes No
4. Have you ever had a drink or used drugs first thing in the morning Yes No
to steady your nerves or to get rid of a hangover (Eye-opener)?
Yes to 1 or 2 questions = possible problem
Yes to 3 or 4 questions = probable dependence
ALCOHOL AND DRUG USE SCREENING TOOL: CAGE-AID Questionnaire
Locate height and weight range.
The number at the top of the
column is the BMI. Maximum
healthy weight is defined as
BMI < 25.
H
P
D
1
X
2
5
7
1
1
-
1
2
.
0
5
August2008
Maternity Medical Record Review
Obstetrical Practitioner
Member Name: Member DOB: Member ID#:
Provider Name: Provider Office Location: Provider ID#:
Initials of Reviewer: Date of Review: Product:
PCAP Site: Y/N Name:
Prenatal Care Section of Maternity Medical Record Review
1. Patient Identification
Each page within the record contains the patients name or ID number on both sides of the
page.
2. Personal biographical data
Mark off each data element found in the medical record:
DOB.
Address.
Home Telephone Number.
Occupation. Indi
e Number.
cate Occupation:______________________________
Work Telephon
Marital Status.
Name of Next of Kin/Significant Other/Proxy.
Telephone Number(s) of Next of Kin/Significant Other/Proxy.
Primary Language. Indicate Primary Language:_______________________
Education. Indicate Level of Education:________________________
Eligibility Determination.
3. All entries in the medical record contain the authors identification.
a handwritten signature, an initials-stamped signature, or a
unique electronic identifier.
Author identification may be
4. All entries are dated.
5.
Prior to scoring, the Medical Direc w all charts found to be illegible.
The record is legible to someone other than the writer.
A second surveyor examines any record judged to be illegible.
tor must revie
Page 1 of 13
August2008
Member Name
: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
6. Allergies and adverse reactions are prominently noted in the record, or NKA is noted.
Prominently noted refers to: on the front of the chart or inside the front cover of the chart or
on a designated problem list or medication page or at the time of each office visit.
Updated at a minimum of annually (preferably during a physical).
7. one of the options.):
First prenatal visit within the first trimester
When prenatal care was first rendered (Choose
.
First prenatal visit within 42 days of Plan enrollment.
Or
First trimester visit within 3 weeks of a pregnancy diagnosis
Or
via (+) HCG or ultrasound.
Second trimester visit within 2 weeks of a pregnancy diagnosis
Or
via (+) HCG or ultrasound.
it within 1 week of a pregnancy diagnosis v
Or
Third trimester vis ia (+) HCG or ultrasound.
[Ref. DOH Access and Availability]
8. Criteria for determining early prenatal care (Circle criteria that applies.):
ision Rule 1 Dec
o dwife, or family practitioner or other primary care
atal care was initiated.
Any prenatal visit to an OB practitioner, a mi
practitioner with documentation of when pren
Ma
o Any visit to an OB/GYN, family practitioner or other primary care practitioner with either an US
or a principal diagnosis of pregnancy.
Or
rker Event
Page 2 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
Or
Decision Rule 2
o Any visit to an OB practitioner, or midwife WITH evidence of any of the following
screening tests:
OB Panel.
TORCH antibody panel (Cytomegalovirus, Herpes simplex, Rubella, Toxoplasma,
Rubella).
Rubella antibody/titer with Rh incompatibility (ABO/Rh blood typing).
Ultrasound (echography) of a pregnant uterus.
Pregnancy-related diagnosis code.
ICD=9-CM diagnosis for prenatal care.
Or
Decision Rule 3
o Any visit to a family practitioner or other primary care practitioner** with a pregnancy
related ICD-9_CM diagnosis code And one of the following:
OB Panel.
TORCH antibody panel.
Rubella antibody/titer with Rh incompatibility (ABO/Rh blood typing).
Ultrasound (echography) of a pregnant uterus.
Or
Decision Rule 4
o Any visit to a family practitioner or other primary care practitioner with diagnosis-based
evidence of prenatal care in the form of a documented LMP or EDD WITH either a
complete obstetrical history or risk assessment and counseling/education.
** When using a visit to a family practitioner or other primary care practitioner, it is necessary to
determine that prenatal care was rendered and that the member was not merely diagnosed as
pregnant and referred to another practitioner for prenatal care.
[Ref. HEDIS Technical Specifications]
9. A standardized prenatal tool must be initiated at the first prenatal visit.
Identify Tool used: ___________________________________________________________
Page 3 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Matenity Medical Record Review (continued)
10. Use of an appropriate antepartum record including supplements that are consistent with
ACOG Antepartum Record (Appendix A).
The Baseline History and Physical Exam identifies appropriate subjective and objective
information and includes a review of:
Pregnancy history and/or risks must include (ref: ACOG Past Pregnancies):
Gravida and para .
D (Rh) status.
Type of delivery.
e at delivery. Gestational ag
Anesthesia.
Length of labor.
Birth outcome/risks.
Maternal complications.
Sex/weight of child.
sychosocial History must include (ref: ACOG Medical History & ACOG Medical-Surgical and P
Personal Health History):
Serious accidents.
Operations.
Infections.
Illnesses.
Substance abuse.
Mental health.
Screening for depression.
Gynecological conditions.
Infertility.
Stress.
Living situation.
Socioeconomic evaluation.
Date Initial Risk Assessment Performed:_________________________No Score
Page 4 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
Genetic Screening and Counseling must include (ref: ACOG Genetic Screening/Teratology
Counseling):
A review of familial history of birth defects, deformities, mental retardation, or inherited
diseases (e.g., muscular dystrophy, hemophilia, cystic fibrosis).
aternal (> M 35yo) / paternal (>50yo) age at time of delivery.
Ethnicity.
ling must include (ref: PCAP 85.40): Nutritional screening and counse
Dietary intake
Hydration
Prenatal vitamins
Weight loss/gain
Elimination
F d oo /shelter resources
WIC referral
o Was a referral for Nutritional counseling and enrollment in the Supplemental Food and
Nutrition Program for Women, Infants, and Children (WIC) done? Yes/No
o If Yes, provide date (month/year)___________________________
k b t include an appropriate notation concerning Ris ehaviors/exposures mus
40): (ref: ACOG Psychosocial Screening, PCAP 85.
Tobacco.
Alcohol.
Chemical dependency.
HIV/STD/Hepatitis/HPV risks.
Domestic violence.
Safe sex practices.
Sexual abuse.
Safety risks/environmental/occupational hazards.
HIV pre-test recommendation & counseling.
HIV post-test counseling (if applicable).
rtum Record-Form B): Physical Exam must include (ref: Appendix A: ACOG Antepa
A comprehensive review of systems.
A focused gynecologic and obstetrical examination.
An assessment of presenting comp laints, if any.
EDD confirmation.
18-20 week EDD update.
Page 5 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
11. Ongoing/Follow-up Prenatal Care Visits
These visits shall be for the purpose of providing ongoing prenatal care and shall include the
following components:
General Visit Frequency Guide (Uncomplicated Pregnancy):
(Appendix A: ACOG Antepartum Record-Form C)
Every 4 weeks until 28 weeks gestation.
Every 2-3 weeks until 36 weeks gestation.
Every week thereafter.
NOTE: Women with medical or obstetrical problems may require closer surveillance; the appropriate
int ems. ervals between visits are determined by the nature and severity of the probl
___________________________________________________________________________________
prenatal visit must include Obstetrical Screening - Each ongoing
pe orm C, ACOG Supplemental-Form F): (Ap ndix A: ACOG Antepartum Record-F
Weeks gestation.
Fundal height.
Presentation.
Fetal heart rate.
Fetal movement.
Preterm labor signs and symptoms.
Cervical exam.
Blood pressure.
Weight.
Urine albumin/glucose.
Problems/comments.
_____ ____________ _____________________________________________
Diagnostic Testing - Trimester appr (ref: ACOG Antepartum opriate are to be performed
Record Form D) (NYS DOH recommended lab tests, include, but are not limited to the
following in the Laboratory Testing Prenatal table on the following page):
Page 6 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
The Table with the Diagnostic Tests is on this page in order to keep all testing requirements together.
(Circle each element found in the MR.)
Laboratory Testing Prenatal
Early Prenatal Visits 8-18 weeks 20-28 weeks 32-36 weeks
Initial labs
All initial labs are
required.
Optional labs
Documentation
should indicate
N/A or
Refused.
Optional labs
Documentation should
indicate N/A or
Refused.
Documentation
should indicate
N/A or Refused.
No Score
Documentation
should indicate
N/A or Refused.
HIV testing/counsel
No Score
ABO/Rh (D) Blood
Typing
Sickle Cell Screening
as applicable
US as clinically indicated H&H H&H
RBC Antibody Screen PPD as indicated Alpha-fetoprotein (AFP) D (Rh) US
Obstetric Panel (H&H;
Diff; WBC; Platelet
Count)
Genetic (Form B)
Amniocentesis/
CVS
Rhogram
(28 weeks)
VDRL
Cervical-Vaginal (PAP) Karatype
Glucose Challenge
(28 weeks)
Repeat chlamydia,
gonorrhea and syphilis
screen during 3
rd
trimester, as clinically
indicated.
HIV Testing
Group B Strep culture
at 35-37 weeks,
according to
CDC guidelines
VDRL (Syphilis)
(Mandated by PHL)
Urinalysis and Urine
C&S as clinically
indicated
Urinalysis testing for
sugar and albumin
(at each visit)
Urine Culture
Rubella Antibody Titre
(May be part of a
TORCH Panel)
Hepatitis B
(Mandated by PHL)
Gonorrhea/chlamydia
Serum Lead Level, as
indicated.
If >10ug/dl report to
DOH
TORCH: Four infections
must be present for this
component:
Cytomegalovirus; Herpes
simplex; Rubella (can be
done separately;
Toxoplasmosis
Page 7 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
Risk Designation - Diagnoses/impression is consistent with objective and subjective
findings. Affirmative risks are identified in any of the following areas:
(Ref: ACOG Antepartum Record):
Past pregnancy maternal risks.
Past pregnancy birth outcome risks.
Past medical history risk.
Genetic risks.
Psychosocial risks.
Risk behaviors/exposures.
Nutritional risk.
Abnormal maternal physical exam/diagnostic results.
Abnormal fetal exam/diagnostic results.
Knowledge deficit/learning/adherence barriers.
u Foc sed Assessment - each routine or follow-up obstetrical visit must include:
A focused history and review of systems based upon presenting complaints, risk factors,
active (acute) medical or psychosocial problems, and/or management of chronic, serious,
or disabling conditions, or should indicate no problems or complaints.
s, and/or care plans from previous office visits are Unresolved problems, risk factor
addressed in subsequent visits.
12. Significant illnesses and medical conditions are indicated on the problem list.
contains a problem list that can either The medical record be a separate form or listed in
the progress notes.
And
The medical record contains a problem list that can either be a separate form or listed in
the progress notes, which must be updated as appropriate.
And
The problem list should contain all ch c, roni serious or disabling conditions and/or active
(acute) medical or psychosocial problems.
Or
For those patients without chronic, serious or disabling conditions and/or active (acute)
medical or psychosocial problems, the list should either indicate well visit or no
problems/complaints.
[R B ef.: ates, 6
th
Ed.]
13. Medication Record
A medication record/list includes dosages and dates for initial and refill prescriptions.
medication side eff toms are reviewed with the member and Discussion of ects and symp
documented.
Page 8 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
14. Immunization
An appropriate immunization history has been made with notation that immunizations are
up-to-date.
Immunizations administered after May, 1992 contain lot number and manufacturers
name. (Must have 100% compliance)
[Ref.: CDC; U.S. Preventative Task Force; NYSDOH; HIP Health Plans Preventive Health Service Guidelines for 2006]
15. Communicable Disease(s) are reported to appropriate regulatory agency and documented
in the MR. (Reference list of NYS/NYC reportable communicable diseases)
Document Communicable Disease and Regulatory Agency:
____________________________________________________________________________
16. Treatment plans are clearly documented in the record and reflect:
A clear link to risk factors.
Individualization.
Routinely updated at each visit.
J oint implementation by the pregnant woman, her family (when mutually agreeable) and
the health care team.
N ed ate services, including but not limited to: eed referrals and coordination of all appropri
a. Diagnostic testing and counseling.
b. Inpatient.
c. Specialty physician care.
d. Transfer of high risk patient from mid-level to obstetrician.
e. Genetic services.
f. Dental care.
g. Home care.
h. Pharmaceutical.
i. Transportation.
j. Nutritional.
k. Alcohol and chemical dependency.
l. Psychosocial.
m. DSS.
n. WIC.
o. HIV specialist.
p. Other: Indicate Other:___________________________________________
No Score in this section
Page 9 of 13
August2008
Member Name: Member ID#:
Prenatal Care Section of Maternity Medical Record Review (continued)
17. tments should be documented including follow-up efforts to No-shows or missed appoin
reschedule appointment.
18. Follow-up Notation
re, calls, or Encounter forms or notes have a notation, when indicated, regarding follow-up ca
visits. The specific time of return is noted in days, weeks, months, or as needed.
[ ef.: NCQA MRR 2006] R
19. Follow-up after an ER visit or hospitalization
Date(s) listed for ER and/or hospitalization(s):___________________________________
________________________________________________________________________
or telephone follow-up intervention is clearly An office visit, written correspondence
documented in the obstetrical record.
20. Continuity of Care
Indicate whether a specialist consultation:
Name/Specialty: ________________________________________________
Or
If whether a diagnostic study:
Name of Diagnostic Study: _______________________________________
Or
Prenatal home visitation:
Name of Home Care Agency:______________________________________
ed, there is a note or report from If a consultation or diagnostic study or home care is request
the consultant, facility or home care agency in the record.
ciplinary input is clearly documented by a consultants note/report in Appropriate multidis
the chart.
The ordering health care provider initials consultation and diagnostic study reports filed in
the chart.
Abnormal consultation and diagnostic study results have an explicit notation of follow-up
plans in the recrord.
Page 10 of 13
August2008
M b em er Name: Member ID#
Prenatal Care Section of Maternity Medical Record Review (continued)
21. Care rendered is medically appropriate.
(If this standard is not met, the case is immediately referred to the Medical Director for a quality of care
review).
Definition: There is evidence that the patient may be placed at inappropriate risk by an
inadequate(ly), incorrect(ly), or inappropriately:
Performed physical examination or assessment.
Performed procedure.
Performed diagnostic studies, including, but not limited to, lost specimens, poor film quality, misread
results, or delayed turn around time.
Diagnosed member.
Prescribed, dispensed, or administered medication.
Developed and/or implemented treatment plan.
Other errors, delays or omissions in the delivery of care.
22.
uca
omplications.
ality in pregnancy.
oisoning).
.
eeding except where contraindicated, i.e. HIV).
eck all that apply.) (May be provided in group or individual setting based on
omans needs.)
Classes.
Home visits.
s.
Prin
No Score in this section.
R P cord Form E)
Pregnancy education and counseling:
Ed tion should include:
Risk-factor, as appropriate.
Rights and responsibilities of pregnant woman.
Signs of pregnancy c
Physical activity, exercise, and sexu
Avoidance of harmful substances (Lead P
Occupational risks.
Orientation to facility procedures
Newborn HIV testing.
Signs of pre-term labor.
Signs of labor.
Relaxation techniques in labor.
Labor and delivery procedures.
a/analgesia. OB anesthesi
Parenting skills.
Newborn screening.
Family planning.
Infant feeding options (encourage breastf
Dental care.
directive (as appropriate). Advance
Educational Methods: (Ch
assessment of pregnant w
Office teaching.
Video
ted materials.
( ef.: CAP and ACOG Antepartum Re
Page 11 of 13
August2008
Member Name: Member ID#
Postpartum Visit Section of Maternity Medical Record Review Tool:
23. Demographic Information
Date of delivery: ________/________/________
Inf ts bir an th weight (if documented in medical record): ______________
Gestational age at birth: ____________________
Type of delivery:
Vaginal.
C/S.
Vaginal delivery after C/S (VBAC).
24. Use of appropriate postpartum record outlining indicated components of care.
25. e p rs within 21 to 56 days Th ostpartum visit occu after the delivery date.
26. e p Th ostpartum visit includes:
(Ref. PCAP Article 85.40)
Physical assessment.
o B/P, weight, pelvic exam, abdominal exam, breast exam.
Nutritional status.
Substance use assessment.
Education on postpartum changes.
Psychosocial status.
Family adjustments.
Personal health habits.
Family planning/preconception counseling.
Newborn health status and care.
Sexual activity.
Nutrition.
Laboratory testing, as clinically indicated.
Prevention of HIV/STD/Hepatitis.
Page 12 of 13
August2008
Member Name: Member ID#
Postpartum Visit Section of Maternity Medical Record Review Tool:
27. ild made as appropriate. Referrals for community resources for mother and ch
(Not Applicable receives points, no deductions.)
Nutritional counseling.
Social worker/DSS/WIC.
PCP/specialty physicians.
Behavioral health services.
Postpartum home visit.
Infant health/care.
Expand eligibility (depending on type of product).
28. The postpartum visit addresses Depression.
Signs and symptoms.
Risk factors.
Referrals if applicable.
Resources.
29. The p during and after delivery. ostpartum visit addresses continuity of care
pecialty consult for diabetes S
Date_________________________________
Provider information____________________
Specialty consult for depression
Date_________________________________
Provider information____________________
End of Maternity Medical Record Review Tool
Page 13 of 13
***All forms of medical record documentation are acceptable. ***
M E D I C A L R E C O R D G U I D E L I N E S
June2007
Web resources for Communicable Disease Reporting
NYSDOHCommunicableDiseaseReportingRequirements
http://www.health.state.ny.us/nysdoh/cdc/cdcrept.pdf
NYSDOHmaterials
http://www.health.state.ny.us/nysdoh/cdc/main.htm
NYCDOHandMHWebsiteforCommunicableDiseaseReporting
http://home2.nyc.gov/html/doh/downloads/pdf/wnv/wnvserologyform.pdf
NYCDOHandMHUniversalReportingForm
http://home2.nyc.gov/html/doh/downloads/pdf/hcp/urf0803.pdf
NewYorkCountyResources
http://www.nysacho.org/Directory/directory.html
NYCDOH and MH Health Care Providers Report of Communicable Diseases and Suspected
Outbreaks to the DOHMH
http://home2.nyc.gov/html/doh/html/hcp/hcpreporting.shtml
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- 625 List AlphabeticalDokumen4 halaman625 List AlphabeticalMux Muxic100% (1)
- Physician To Population Ratios Physician Supply StandardsDokumen5 halamanPhysician To Population Ratios Physician Supply StandardsjackeldescargadorBelum ada peringkat
- Treatment of Oropharyngeal Dysphagia CarolMcKee (1) DPNS StudyDokumen23 halamanTreatment of Oropharyngeal Dysphagia CarolMcKee (1) DPNS Studyconstantineelia100% (1)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- TestDaF Broschuere EnglischDokumen12 halamanTestDaF Broschuere EnglischLek825Belum ada peringkat
- Testdaf-Levels Subtest Level Descriptions: WWW - Testdaf.De 1 © G.A.S.T., 07/2012Dokumen2 halamanTestdaf-Levels Subtest Level Descriptions: WWW - Testdaf.De 1 © G.A.S.T., 07/2012Lek825Belum ada peringkat
- Definition of Systems Approach ICSUDokumen2 halamanDefinition of Systems Approach ICSULek825Belum ada peringkat
- Course Handbook - MRes Clinical Research CRDM PathwayDokumen45 halamanCourse Handbook - MRes Clinical Research CRDM PathwayLek825Belum ada peringkat
- MTA Frequency ScheduleDokumen2 halamanMTA Frequency ScheduleLek825Belum ada peringkat
- High Lateral Tension AbdominoplastyDokumen14 halamanHigh Lateral Tension AbdominoplastyAhmad Arbi AninditoBelum ada peringkat
- Gay Issue A Century AgoDokumen4 halamanGay Issue A Century AgoElla Jane EngoBelum ada peringkat
- Bahasa Inggris"diagnosa Keperawatan Dan Masalah Keperawatan "Dokumen9 halamanBahasa Inggris"diagnosa Keperawatan Dan Masalah Keperawatan "Nur Azizah WijayantiBelum ada peringkat
- MSDS Pupuk Haracoat PDFDokumen4 halamanMSDS Pupuk Haracoat PDFAnonymous UQVygYg3lfBelum ada peringkat
- Part 1 - Bernal Safety - Intro and Emergencies - Powerpoint - 29mar21Dokumen34 halamanPart 1 - Bernal Safety - Intro and Emergencies - Powerpoint - 29mar21John TorrezBelum ada peringkat
- Choking and AspirationDokumen23 halamanChoking and AspirationAgni MubarokBelum ada peringkat
- Rekap Umr 2019-4Dokumen52 halamanRekap Umr 2019-4Derri HafaBelum ada peringkat
- 101 Storie ZenDokumen16 halaman101 Storie ZendbrandBelum ada peringkat
- Top 10 Highest Paying Medical SpecialtiesDokumen1 halamanTop 10 Highest Paying Medical SpecialtiesGresjana RamajBelum ada peringkat
- Big RPLDokumen1 halamanBig RPLRahayu LestariBelum ada peringkat
- WarfarinDokumen2 halamanWarfarinWAHYU NOFANDARI HERDIYANTIBelum ada peringkat
- Storage ConditionDokumen4 halamanStorage Conditioneshwar_1953Belum ada peringkat
- FREMEC FormsDokumen1 halamanFREMEC FormsAviation MedicineBelum ada peringkat
- 2002 Solution-Focused Brief TherapyDokumen9 halaman2002 Solution-Focused Brief Therapymgnpni100% (1)
- Lose Weight With Reiki PDFDokumen19 halamanLose Weight With Reiki PDFAfua Oshun100% (3)
- Nursing Care Plan Myocardia InfarctionDokumen3 halamanNursing Care Plan Myocardia Infarctionaldrin1920Belum ada peringkat
- TableDokumen6 halamanTablemanuBelum ada peringkat
- Design Manual IndexDokumen4 halamanDesign Manual Indexellee6222100% (1)
- 2019 Fall RNSG 2263 Clinical Mental Health CIDDokumen102 halaman2019 Fall RNSG 2263 Clinical Mental Health CIDadam50% (2)
- Raw Materials & Purification - NitrogenDokumen9 halamanRaw Materials & Purification - Nitrogensexyrusty0% (1)
- Sales Account Manager Biotechnology in Boston MA Resume Cynthia SmithDokumen2 halamanSales Account Manager Biotechnology in Boston MA Resume Cynthia SmithCynthiaSmith2Belum ada peringkat
- Human Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40Dokumen4 halamanHuman Biology Laboratory 4: Body Tissues and Organization List The 4 Tissue Types and Give A General Function: Pg. 40bugyourselfBelum ada peringkat
- Guterbock Hittite MedicineDokumen6 halamanGuterbock Hittite MedicineTarek AliBelum ada peringkat
- Cesarean Surgical Techniques - GLOWMDokumen36 halamanCesarean Surgical Techniques - GLOWMOana BalintBelum ada peringkat
- Methicillin-Resistant Staphylococcus Aureus PDFDokumen23 halamanMethicillin-Resistant Staphylococcus Aureus PDFGerardo N. Pabón Gallino100% (1)
- Asymptomatic HyperuricemiaDokumen46 halamanAsymptomatic HyperuricemiaDivya Shree100% (1)
- The Science of NutritionalDokumen738 halamanThe Science of NutritionalMonching Adecer100% (1)
- The Right Choice: Smith&nephewDokumen4 halamanThe Right Choice: Smith&nephewapi-19808945Belum ada peringkat