Nutrition Review 2.3
Diunggah oleh
ashdmb217Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nutrition Review 2.3
Diunggah oleh
ashdmb217Hak Cipta:
Format Tersedia
1
NUTRITION
7- Diet & Nutrition in Oral Health
1. Four interrelated factors of the oral infectious process:
a. Susceptible host or tooth surface
b. Microorganisms present (Streptococcus mutans, Lactobacillus casein, Streptococcus sanguis)
c. Fermentable carbohydrates (substrate for bacterial metabolism)
d. Timeor duration in the mouth for the bacteria to metabolize carbohydrate
2. Development of caries is a pathologic process of demineralization
a. Plaque bacteria feed on fermentable carbohydrates; Form acid, causes a drop in pH (<5.5)
environment for demineralization; Bacteria destroy the dentin while acid destroy mineralized tissue
3. Factors affecting food cariogenicity:
a. Frequency of consumption of fermentable carbohydrates
i. Any monosaccharides or disaccharides (simple sugars), including: glucose, fructose, maltose,
lactose, and sucrose; Starches can contribute to caries if they are held in the mouth long
b. Length of exposure of teeth to food and beverages
i. Fermentable carbohydrate consumed decline in pH is initiated
within 5-15 minutes and lasts about 20-30 minutes
c. Food form (adherence, exposure time)
d. Sequence of eating foods and combination of foods (buffering effects of certain foods)
e. Nutrient composition of food affects its ability to create an acidic environment
i. Dairy products have calcium and phosphorus that act as buffering and remineralizing agents
ii. Protein foods & fats (butter/oil) are not cariogenic- no fermentable substrate
iii. Relative cariogenicity of a food is not correlated with its carbohydrate (sugar) content
f. Noncarbohydrate sweeteners influence caries in ways
i. Xylitol- anticariogenic- prevents plaque from recognizing an acidogenic food;
Other non-caloric sweeteners such as saccharin, cyclamate, and aspartame are non-cariogenic
4. Periodontal disease and gingivitis result from plaque oral bacteria causing infections
a. The plaque from the gingival sulcus produces toxins that destroy tissue and permit loosening of teeth
b. Factors important for resistance of the gingiva to bacterial invasion are:
i. Oral hygiene
ii. Integrity of the immune system to resist infection
iii. Nutrition: deficiencies in vitamin C, folate and zinc increase the permeability of the
gingival barrier at the gingival sulcus increasing risk of development of periodontal disease
5. Caries and periodontal disease can be prevented and/or arrested with plaque control,
dietary modification, and the use of fluoride
a. Tooth brushing/ mechanical cleaning procedures are the most reliable means of controlling plaque
b. Dietary advice should be based on food records or recalls
i. Diet pattern counts most: Increased freq. of cariogenic food consumption = increased
caries risk; Oral contact time is key; Considered safe: 3 meals, no more than 3 snacks
c. General micronutrient adequacy of the diet (risk for vitamin C, folate & zinc)
d. Fluoride sources should be identified and if needed, provided
e. Patients with salivary glands that are not functioning properly may benefit from an artificial saliva spray
containing calcium, phosphate and fluoride ions; Chewing gum also stimulates salivary flow
6. Fluoride: Mechanisms of Action
a. Tooth Enamel: Reduces Enamel Acid Solubility (Demineralization); Enhances
Remineralization; Alters Enamel Structure: Hydroxyapatite Fluorapatite (less acid soluble)
b. Bacteria: Inhibits Bacterial Growth (Bacteriostatic); Kills Cariogenic Bacteria (Bactericidal)
c. Optimum fluoride concentration in drinking water is between 0.7 to 1.2 ppm
i. Levels > 2.0 ppm increase risk for Dental Fluorosis: enamel hypomineralization; maximum
sensitivity to fluorosis between 11 months to 7 years (when permanent teeth are developing
2
8- Iron
1. Iron Distribution in the Body
a. Hemoglobin (oxygen transport) 69% Ferritin (intracellular storage) 27%
2. Most of the daily iron required is recycled via the reticuloendothelial system
3. Two Dietary Types of Iron
a. Heme iron- Flesh sources (Meat, fish, poultry)
b. Non-heme iron- Plant sources; vitamins & supplements
i. Transport by the divalent cation transporter (DCT1 or DMT1)
ii. Requires solubilization from oxidized 3+ ferric to the reduced ferrous 2+
1. Ferric reductase(ferric/cupric duodenal cytochrome b
reductase, Dcytb) at the brush border reduces Fe+3 to Fe+2
2. If ingested non-heme iron is not reduced, the alkaline environment of the small
intestine will favor formation of ferric hydroxide and this may prevent absorption
4. Dietary components influence bioavailability of non-heme iron
a. Enhance non-heme absorption by improving solubility, reducing ferric iron
or chelating iron to organic (absorbable) compounds that are absorbed
i. Factors Enhancing Iron Absorption: Sugars; Acids; Meat, Ethanol
b. Reduce absorption of non-heme iron by influencing solubility or pH
i. Inhibitors of Iron Absorption
1. Polyphenols (e.g. Tannic acid in tea and red wine); Oxalate
(Grains, fruit, vegetables); Phytates (Legumes, grains, rice,
vegetables); Minerals (Calcium; Zinc; Manganese; Nickel)
c. Efficiency of absorption
i. Transporter mediated pathways- Saturable & regulated by hormones (Hepcidin for Fe)
ii. Parcellular- Not regulated and non-saturable
5. Iron once in the Enterocyte
a. Stored complexed to ferritin or used within cell
b. Exported across the basolateral membrane by ferroportin
i. Iron must be oxidized to 3+ by hephaestin or ceruloplasmin before it
can be bound by transferrin (Copper is required as a cofactor)
ii. Transferrin carries iron in circulation where it can be transported at the
basolateral membrane via transferrin receptors facilitated by HFE
6. Stores of iron within the enterocyte regulate iron transport
a. If iron stores are low, absorption can be up-regulated by increased enzyme
activity at the luminal membrane along with decreased hepcidin production
by the liver more iron transported across intestinal cells into the body
b. When hepcidin increases, stores of iron in the enterocyte increase due to
decrease in both basolateral transport & luminal uptake of non-heme iron
7. Excretion- There is no physiologic mechanism to excrete excess iron. Excretion occurs mostly through
losses such as shed mucosal and skin cells and in secretions and in menstrual losses
8. Excess Intake of Iron
a. Hepcidin and Iron Overload (Hemochromatosis)
i. Defective hepcidin due to hepcidin gene defect
ii. Defective regulation of hepcidin expression by liver by HFE gene defect
iii. Defective ferroportin
b. Pathogenesis of Iron Overload
i. Free iron circulates; ROS species generated by free iron; Insoluble
iron complexes deposited in organs; End organ accumulation of ironTissue damage
c. Bantu iron overload- Genetic predisposition to excess absorption; More diet responsive
3
9. Iron Deficiency
a. Most common nutrient
deficiency world-wide
b. Populations at risk:
Infants/young children,
Adolescents, Menstruating
females, Pregnant women,
Malabsorption syndromes,
Intestinal parasites, Vegetarians,
Athletes, Chronic
gastrointestinal or other losses
c. Symptoms may occur prior
to anemia
i. Results in: Anemia,
Fatigue and lethargy, Cold intolerance, Impaired psychomotor development, intellectual
performance and/or immunity, Adverse pregnancy outcomes, Increased risk lead poisoning
d. Treatment of Iron Deficiency
i. Assess etiology and address abnormal losses; Iron supplements effective;
Can take with low dose vitamin C; Parenteral iron if necessary
9- Water Soluble Vitamins: Vitamin C, Thiamine and Niacin
1. Vitamin C = Ascorbic Acid (active form L-ascorbic acid)
a. Functions as an electron donor (antioxidant)- During oxidation of vitamin C, a
free radical form is produced that is more stable than many other free radicals
b. Ascorbic Acid
i. Synthesized by plants from glucose and fructose
ii. Destroyed by: Oxidation; Heat; Exposure to air or alkaline medium;
Contact with copper and iron oxidizes it to dehydroascorbic acid (DHAA)
iii. Food Sources- Widely distributed in anything that is fresh and rapidly growing
c. Roles include:
i. Collagen synthesis
ii. Carnitine synthesis
iii. Neurotransmitter metabolism
iv. Antioxidant function
v. Regeneration of reduced vitamin E
d. Excreted by kidney as: Ascorbic acid; Can be metabolized to oxalic acid
which may potentiate oxalate nephrolithiasis
e. Supplemental use for decubitus ulcers may enhance wound healing
f. Vitamin C Requirements:
i. Vitamin C Deficiency: Scurvy: prevented by 10 mg/day
1. Weakness and lassitude
2. Skin and soft tissue (Petechial hemorrhage; Perifollicular
hyperkeratosis; Ecchymosis; Impaired wound healing)
3. Impaired bone growth and bowing; Subperiosteal hemorrhage;
4. Swollen gums that easily bleed; Tooth loss
5. Depression; Confusion, hysteria; Hypochondriasis
g. Vitamin C Excess: UL = 2 g/day (based on diarrhea and bloating)
Sequential Changes in Iron Depletion
4
2. Thiamine (Vitamin B1)
a. Pyrimidine and thiazole groups with methylene bridge; 0 (free form- usually found in plants) to 3 phosphates
b. Sources: Whole & Enriched grains/cereals; Some vegetables and legumes; Meats, Dairy
c. Thiaminases (Fish, shellfish, ferns, microorganisms): Degrade thiamine
d. Antithiaminecompounds (Ferns, teas, betel nuts): Forms oxidized inactive compounds
e. No UL = no toxicity; Body pool=30 days of RDA (50% in muscle); Rapid turnover
f. Co-factor for a limited number of enzymes
i. NADPH biosynthesis- Transketolase in pentose phosphate pathway
ii. Energy metabolism- Dehydrogenases: e.g. Pyruvate dehydrogenase
iii. Nerve function- Synthesis of acetylcholine, glutamate and GABA
g. Thiamine Deficiency
i. Erythrocyte transketolase activity most accurate functional assay
ii. Metabolic Effects: Cellular energy failure; Accumulation of lactate; Reduction in TCA
intermediates; Reduction in high energy phosphate & neurotransmitter synthesis
iii. Beriberi has two overlapping forms
1. Dry- Distal peripheral neuropathy; Diminished reflexes; Calf tenderness
2. Wet- Tachycardia and low peripheral resistance; Edema;
Cardiomegaly and CHF; Peripheral neuropathy
iv. Wernicke-Korsakoff Syndrome suspected that a genetic predisposition may exist
1. Early: W. encephalopathy- Opthalmoplegia; Ataxia; Confusion
2. Later:K. psychosis- Amnesia; Confabulation; Loss of spontaneity/ initiative
h. Risk Factors for Thiamine Deficiency
i. Poor intake OR intake of foods with thiaminases or antithiamines
ii. Alcoholism GI transport out of enterocyte Phosphorylation to diphosphate liver stores with cirrhosis
iii. Maternal thiamine deficiency
iv. Bariatric surgery; Persistent vomiting (Hyperemesis gravidarum); Refeeding syndrome
3. Niacin (Vitamin B3)
a. Sources: Whole grains (bioavailability in grains requires alkali to release
niacin), Meat and fish, Yeast, nuts, Eggs, Milk, Tryptophan (Precursor)
b. Biochemical Roles of Niacin
i. Energy utilization- Oxidation of glucose and fatty acids
ii. Synthesis of- Fatty acids, cholesterol; Steroid hormones and glutamate
iii. Modification of proteins- DNA repair; Cell differentiation and replication
iv. High dose: triglycerides and HDL-C
c. Niacin Toxicity
i. Vasodilatory flushing (partly due to histamine)
ii. GI intolerance; Hepatotoxicity; Hyperuricemia and gout (Niacin competes with
uric acid for excretion); Glucose intolerance and Decreased insulin sensitivity
d. Risk for Niacin Deficiency
i. Diets characterized by the 3 Ms: Maize: untreated with base; Meat: poor
quality and high fat content; Molasses: high CHO diet low in niacin & tryptophan
ii. Hartnups disease; Carcinoid tumors
e. Niacin Deficiency: 4 Ds of Pellagra
i. Dermatitis in sun-exposed areas of the skin (Casals necklace)
ii. Diarrhea due to mucosal atrophy and inflammation
iii. Dementia- Anxiety, depression and insomnia; Delirium and
hallucinations; Neuropathy and muscle weakness
iv. Death
5
10- Water Soluble Vitamins: Folate and Vitamin B12
1. Folate and vitamin B
12
: critical co-enzymes; By inhibiting the MS reaction,
B12 deficiency causes a functional folate deficiency: the methylfolate trap;
Patients with B12 deficiency present with elevated levels of folate
2. Folic acid (B
9
)
a. Folate metabolism supports two critical, and competing
pathways: biological methylation and nucleotide synthesis
i. Is the essential co-factor for the rate-limiting reaction in
DNA synthesis
b. Deficiency risk: Generalized poor diet; Ethanol abuse (Ethanol interferes with folate absorption and
metabolism); Malabsorptive disorders; Drugs interfering with folate absorption/ metabolism
c. Folate status can be assessed by the
concentration in plasma and in RBCs
i. Plasma folate reflects recent intake, decreases 1
st
ii. RBC folate remains relatively stable; decreased
RBC folate occurs in more chronic deficiency
d. Folate Deficiency: manifestations reflect the
vitamins critical functions in rapidly proliferating
cells; results in decreased regeneration of tissues
with rapid turnover
i. Megaloblastic (macrocytic) anemia
ii. Megaloblastosis of GI epithelium:
diarrhea and malabsorption
iii. Myelomeningocoele (spina bifida)
e. Folate metabolism: the foundationstone of modern
antibiotics and cancer chemotherapy
i. Methotrexate functions as an inhibitor of dihydrofolate reductase (inhibits DHF THF)
3. Vitamin B12
a. Cofactor for conversion of:
i. Homocysteine to methionine
ii. Methylmalonyl CoA to succinyl CoA
1. Abnormal accumulation of methylmalonic acid is indicator of B12 deficiency
b. Sources: animal foods (plants do not synthesize B12)
c. Absorption- Vitamin B12 in food is bound to protein
i. Low acid states (aging and due to acid-reducing medications) may impair this step
ii. Intrinsic factor (produced in stomach) binds B12 in the intestine and facilitates absorption
d. Vitamin B12 deficiency:
i. Megaloblastic anemia: due to trapping of folate in irreversible rxn to methyl THF
ii. Neuronal death in spinal cord (combined subacute degeneration)
iii. Encephalopathy, myelopathy, peripheral neuropathy, and optic neuropathy
iv. Diarrhea and malabsorption
e. Risk for vitamin B12 deficiency:
i. Vegans and Infants of vegan mothers who rely only on breastfeeding
ii. Conditions resulting in diminished secretion of gastric acid and/or intrinsic
factor: Use of drugs that reduce gastric acid secretion; Atrophic gastritis Reduced
gastric acid; Pernicious anemia loss of intrinsic factor secretion and gastric acid
4. In persons 51 years and older it is recommended that most of the RDA for
vitamin B12 be consumed in the crystalline form, reflecting the increasing
prevalence of atrophic gastritis and difficulty with B12 digestion
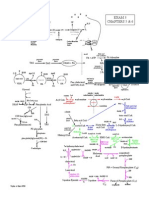
homocysteine
methionine S-AdoMet
SAdoHcy
methyl THF
THF
methylene
THF
DHF
thymidylate
synthesis
methylation
of DNA, RNA,
protein, etc
B12
purine
synthesis
B2
B6
methenyl
THF
formyl
THF
By inhibiting the MS reaction, B12 deficiency causes
a functional folate deficiency: the methylfolate trap
biological methylation nucleotide
synthesis
MS
6
11- Fat Soluble Vitamins
1. General properties
a. Contains only carbon, hydrogen & oxygen; May have precursors or pro-vitamins
b. Absorbed into lymphatic system
c. Daily intake is not critical; Intake in excess of daily needs are stored
d. Deficiency symptoms slow to develop; May be toxic at relatively low concentrations
2. Vitamin A (retinoids)
a. Includes
i. Preformed vitamin A
ii. Provitamin A carotenoids produced by plants & algae
b. Sources:
i. Vitamin A Animal sources- eggs, meat, dairy
ii. Beta-carotene sources- Green, leafy vegetables; intensely colored fruits and vegetables
iii. Raw foods have the lowest bioavailability; cooking helps liberate
c. Digestion and Absorption
i. Retinol absorption is carrier mediated
ii. Carotenoids absorbed passively with digestion of fat
iii. Carotenoids cleaved to retinol in the enterocyte; adequate vitamin A
stores inhibit cleavage
iv. Vitamin A is transported to the liver where it can be stored as retinyl
esters or transported from the liver to other tissues
v. Retinol binding protein facilitates transport in the circulation
d. Biological Roles of Vitamin A
i. Vision
1. Dark adaptation
2. Epithelial tissue
ii. Bone growth
iii. Reproduction
iv. Cell division
v. Cell differentiation
vi. Regulation of the immune system
e. Biological Roles of Carotenoids
i. Provitamin A: -carotene; -carotene; -
cryptoxanthin
ii. Antioxidant that protects cells from free radicals; associated outcomes
such as prevention of macular degeneration
f. Assessment of Vitamin A
i. Risk for deficiency
1. Poor diet
2. Malabsorption
3. Liver disease
ii. Risk for excess
1. Supplements and polar bear liver
2. Renal disease
3. Carotenoids do not lead to vitamin A toxicity
7
3. Vitamin D
a. Forms
i. Vitamin D
2
- Ergocalciferol
1. Sources: Plants, fungi, invertebrates; Supplements and fortified foods
ii. Vitamin D
3
- Cholecalciferol
1. Sources: Skin synthesis; Animal foods; Supplements and fortified foods
b. Advantages to D3; D3 is more effective at
i. Increasing 25-OH vitamin D concentration
1. Obesity is inversely associated with circulating 25-OH
vitamin D concentration
ii. Suppressing PTH
1. Elevated PTH may indicate deficiency of vitamin D
c. Roles of Vitamin D
i. Calcium- Absorption & Homeostasis
ii. Bone health
iii. Muscle function
d. Vitamin D might Influence DM Risk
i. Mediated by calcium
ii. Modulation of autoimmunity
iii. Increased beta cell insulin secretion
iv. Increased insulin sensitivity
v. Reduced inflammatory cytokines
e. Vitamin D Deficiency
i. Bone
1. Children: Rickets
2. Adults: Osteomalacia; Osteopenia
ii. Myopathy and weakness
iii. Risk factors
1. Infants who are exclusively breastfed
2. Limited sun exposure
3. Greater skin melanin content
4. Age
5. Renal disease
6. Liver disease
7. Drugs
8. Fat malabsorption syndromes (Cystic Fibrosis; Crohns
disease; Celiac disease; Surgical resection of small intestine)
f. Vitamin D Excess
i. Usually from supplements or Rx; Not from UV exposure
ii. Symptoms due to hypercalcemia
1. Nausea and vomiting
2. Elevated serum calcium concentrations
a. Mental status changes; Arrhythmia; Nephrolithiasis;
Calcinosis
g. Assessment of Vitamin D Status
i. Vitamin D status reflected by
1. 25-OH (stable, active form) vitamin D concentration
8
4. Vitamin E
a. Limited food sources
b. Biological Roles
i. Antioxidant (Reduced by vitamin C)
ii. Immune function
iii. DNA repair
c. Is absorbed with micelles and transported to liver
d. Vitamin E Deficiency
i. Deficiency associated with
1. Neuropathy
2. Myopathy
3. Retinopathy
4. RBC hemolysis (RDA is based on the amount needed to
prevent oxidative damage)
ii. Risk factors
1. Premature very low birth weight infants
2. Fat malabsorption
3. Rare genetic disorders (eg. -tocopherol transfer protein
defects)
e. Vitamin E Excess due to supplement use
i. Bleeding
ii. May interfere with vitamin K metabolism
iii. Supplemental doses above 400 IU not routinely recommended
5. Vitamin K
a. Sources: Green leafy vegetables & oils
b. Biological Roles
i. Cofactor for the -carboxylation of Glu to
Gla in proteins involved in
1. Coagulation; Bone mineralization; Regulation
of calcification
c. Vitamin K Deficiency
i. Results in coagulopathy & bleeding
ii. Risk factors
1. Malabsorption
2. Liver disease
3. Poor intake
4. Alcoholism
iii. Babies are born deficient- Must be supplemented at birth to prevent
hemorrhagic disease of the newborn
iv. Warfarin inhibits the vitamin K cycle by acting on the enzymes
required for regeneration of active vitamin A, thus reduces coagulation
and prolongs time to clotting
v. Warfarin use in pregnancy results in embryopathy
Vitamin K Cycle
9
12- Nutrition in Acute Illness
1. Nutrition Goals in Hospitalized Patients= Maintenance of Lean body mass and/or
body weight and Physiologic function
2. The Stress Response- The Metabolic Response to Illness
a. Response proportional to severity of illness
b. Hypermetabolism: increased energy needs proportional to severity of illness
and fever which activates sympathetic nervous system and catecholamines,
inflammatory cytokines, accelerated catabolism and futile cycles
c. Altered protein synthesis and catabolism
i. Accelerated protein catabolism of muscle, albumin and other proteins.
ii. Altered protein synthesis in liver favoring synthesis and secretion of acute phase
proteins and reduction in synthesis negative acute phase proteins (albumin)
1. Albumin is not an indicator of protein nutrition in acute illness setting
iii. Results in protein catabolism, which is measured by urinary nitrogen excretion
d. Hyperglycemia due to inability to suppress gluconeogenesis ( glucagon)
even when blood glucose is normal or elevated and insulin resistance
e. Edema due to hypoalbuminemia, increased capillary leakiness, and water retention
f. Response can occur in well-nourished pt rapidly after severe injury or surgery
i. The dysregulation of protein metabolism along with other elements of the
stress response creates a picture of kwashiorkor even when protein nutrition
hours or days previous was adequate
g. Mostly due to resting expenditure (Range 1.3 to > 2 times normal)
3. Adverse Effects of PEM: Mortality; Prolonged hospitalization; Infection; Impaired wound
healing/ skin integrity; Impaired balance and increased weakness
4. Identifying Protein Energy Malnutrition in Hospitalized Patients
a. Weight and weight change (Influenced by hydration, Scale used)
i. BMI < 18.5 kg/m
2
ii. Involuntary loss of > 10% usual weight over 3-6 months
b. Physical Exam (Muscle wasting; Loss of subcutaneous fat)
c. Recent intake; Functional status
5. Who Benefits from Nutrition Support?
a. Pre-operative patients with moderate-to-severe PEM
b. Inpatients with severe alcoholic liver disease
c. Patients undergoing bone marrow transplantation
d. Acutely ill patients with moderate-to-severe malnutrition who will be unable
to meet at least 80% of their needs ad libitum in the next 48 hr
e. An acutely ill patient who is mildly malnourished or well-nourished but is
unlikely to meet >80% of their nutritional needs within the next 7-10 days
6. Nutrition support
a. Enteral nutrition (via the gut)
i. Tubes placed (nose, mouth, stomach, abdominal wall)
ii. Possible benefits of enteral feeding
1. Minimizes complications of parenteral nutrition
iii. Complications of Enteral Feeding
1. Tube placement; Aspiration pneumonia; Diarrhea
iv. Enteral nutrition formulas: Water; Macronutrients; Fiber; Micronutrients; Specialized
formulas (e.g. omega 3 fatty acids)
10
b. Parenteral nutrition (Bypasses the gut: intravenous feeding)
i. Contains: Water; Macronutrients; Electrolytes (minerals); Vitamins and trace elements
ii. Total parenteral nutrition (TPN)
1. High osmolality requires administration in vena cava; Meets energy & protein needs
iii. Peripheral parenteral nutrition (PPN)- Infused through smaller peripheral vein
1. Lower osmolality due to risk of phlebitis; May not meet energy or protein needs
iv. Complications of Parenteral Nutrition
1. Infection; Thrombosis; Hyperglycemia; Hypertriglyceridemia
2. Refeeding syndrome- driven by carbohydrates; Overfeeding
7. Refeeding Syndrome
a. Occurs in patients with PEM or poor intake when
carbohydrate is refed; Usually within hours to 3
days of refeeding
i. The insulin response and subsequent
intracellular transport/ sequestration of
glucose, electrolytes and thiamine can lead
to serious consequences
b. At risk:
i. Recent weight loss, especially if rapid;
Starvation/ Anorexia nervosa; Inadequate
intake > 2 weeks; High output electrolyte
losing disease states (E.g. diarrhea or frequent
vomiting); Alcoholism
c. Prevention of Refeeding Syndrome
i. Replete all electrolytes prior to initiation of
nutrition support; Especially phosphate,
potassium, magnesium
ii. Monitor and replete electrolytes
iii. Thiamine repletion
8. Dont overfeed- This may increase the risk of
hyperglycemia, hypertriglyceridemia, and fat overload
syndrome (a rare problem that is manifested when the reticuloendothelial system is
overloaded with fat, usually due to IV administration)
9. Key Issues in Nutrition in the Elderly
a. Atrophic gastritis leads to decrease in gastric acid
i. Vitamin B12 digestion and reduced intrinsic factor
ii. Reduced mineral absorption
b. Bone loss frailty
i. Reduced vertical height
ii. Reduced skin synthesis of vitamin D
iii. Reduced liver or renal hydroxylation
iv. Reduced intestinal calcium absorption
c. Dental health and tooth loss
i. Sarcopenia
ii. Age related loss of muscle mass
iii. Possibly an inflammatory condition
Refeeding Syndrome
Catani, M. et al. Psychiatr Bull 2007;31:209-211
Clinical presentations of refeeding syndrome
Respiratory failure
Aspiration
Hemolysis
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Room: - Name: - Code Status: - AllergiesDokumen2 halamanRoom: - Name: - Code Status: - Allergiesashdmb217Belum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- HCP FormDokumen8 halamanHCP FormMarkBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Brain 3Dokumen3 halamanBrain 3Nurse Betty100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Room: - Name: - Code Status: - AllergiesDokumen2 halamanRoom: - Name: - Code Status: - Allergiesashdmb217Belum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Starting Out - New in The ICUDokumen30 halamanStarting Out - New in The ICUashdmb217100% (1)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Useful Spanish Words and PhrasesDokumen32 halamanUseful Spanish Words and Phrasesashdmb217Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Student Clinical Report SheetDokumen2 halamanStudent Clinical Report SheetMike100% (4)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Clinical Experience "Tips"Dokumen5 halamanClinical Experience "Tips"ashdmb217Belum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Maxwell Quick Medical Reference PDFDokumen35 halamanMaxwell Quick Medical Reference PDFAnonymous fj68Ms100% (10)
- SymbolsDokumen1 halamanSymbolsashdmb217Belum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Adventitious Breath SoundsDokumen1 halamanAdventitious Breath Soundsashdmb217Belum ada peringkat
- Critical Care PhysiologyDokumen287 halamanCritical Care Physiologyashdmb217100% (7)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Nurse Brain Sheet Telemetry Unit SBARDokumen1 halamanNurse Brain Sheet Telemetry Unit SBARashdmb217Belum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Nursing Management of The Perioperative PatientDokumen16 halamanNursing Management of The Perioperative Patientashdmb217Belum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Medical TerminologyDokumen13 halamanMedical Terminologyashdmb217Belum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Information Regarding Family History DocumentDokumen9 halamanInformation Regarding Family History Documentashdmb217Belum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Histology Exam 2 Review.1Dokumen18 halamanHistology Exam 2 Review.1ashdmb217Belum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Iron regulation and water-soluble vitamin functionsDokumen3 halamanIron regulation and water-soluble vitamin functionsashdmb217Belum ada peringkat
- Histology Exam 3 ReviewDokumen7 halamanHistology Exam 3 Reviewashdmb217Belum ada peringkat
- Histology Exam IV Review Part 2Dokumen26 halamanHistology Exam IV Review Part 2ashdmb217Belum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- AbbreviationsDokumen5 halamanAbbreviationsashdmb217Belum ada peringkat
- Nutrition Review1.2Dokumen12 halamanNutrition Review1.2ashdmb217Belum ada peringkat
- Histology Exam IV Review Part 1Dokumen36 halamanHistology Exam IV Review Part 1ashdmb217Belum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Exam 3 PathwaysDokumen1 halamanExam 3 Pathwaysashdmb217Belum ada peringkat
- Exam IV ReviewDokumen39 halamanExam IV Reviewashdmb217Belum ada peringkat
- Exam 4 PathwaysDokumen1 halamanExam 4 Pathwaysashdmb217Belum ada peringkat
- Exam 1 Study Guide.2Dokumen52 halamanExam 1 Study Guide.2ashdmb217Belum ada peringkat
- Biochem Exam 2 Review.2Dokumen31 halamanBiochem Exam 2 Review.2ashdmb217Belum ada peringkat
- Biochem Exam III Review.2Dokumen24 halamanBiochem Exam III Review.2ashdmb217Belum ada peringkat
- Social Taboos and Superstitions in Food Consumption During Pre and Post Natal Period of Tribal Women in Rayagada DistrictDokumen3 halamanSocial Taboos and Superstitions in Food Consumption During Pre and Post Natal Period of Tribal Women in Rayagada DistrictRashmi MishraBelum ada peringkat
- Remembering Abram Hoffer SsDokumen104 halamanRemembering Abram Hoffer SsSchool Vegetable Gardening100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Lipid Lowering AgentsDokumen2 halamanLipid Lowering Agentsapi-623203696Belum ada peringkat
- Biochemistry - Nutrition - Module 5 60 Random Questions For MCQ TestDokumen4 halamanBiochemistry - Nutrition - Module 5 60 Random Questions For MCQ Testkirki pBelum ada peringkat
- Tiens Product Guide PDFDokumen36 halamanTiens Product Guide PDFKweku Robertson100% (1)
- Hyperlipidemia Guide: Causes, Symptoms and TreatmentDokumen17 halamanHyperlipidemia Guide: Causes, Symptoms and Treatmentbent alfay7a2Belum ada peringkat
- Turmeric Nutrition FactsDokumen40 halamanTurmeric Nutrition FactsUdhaya KumarBelum ada peringkat
- Adrenochrome Hypothesis and PsychiatryDokumen14 halamanAdrenochrome Hypothesis and PsychiatryErik KammlerBelum ada peringkat
- Successful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3Dokumen5 halamanSuccessful Treatment of Schizophrenia Requires Optimal Daily Doses of Vitamin b3Joop WezenbeekBelum ada peringkat
- Nutrition Plays An Important Role in Improving The Growth and Development of SilkwormDokumen25 halamanNutrition Plays An Important Role in Improving The Growth and Development of SilkwormNarasimha Murthy0% (1)
- AbramHoffer Orthomolecular Psychiatry What Would Abram Hoffer Do 29.2Dokumen13 halamanAbramHoffer Orthomolecular Psychiatry What Would Abram Hoffer Do 29.2Ebook PDF100% (1)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Niacine (Vitamin B3) PDFDokumen12 halamanNiacine (Vitamin B3) PDFGuranda SilvianBelum ada peringkat
- Nutrition Quiz Tests Food Group KnowledgeDokumen11 halamanNutrition Quiz Tests Food Group KnowledgePearl Aude100% (9)
- Bitterness Compounds in Coffee Brew Measured by Analytical Instruments and Taste Sensing SystemDokumen34 halamanBitterness Compounds in Coffee Brew Measured by Analytical Instruments and Taste Sensing SystemSolisBelum ada peringkat
- Vitamin B ComplexDokumen32 halamanVitamin B ComplexAlain J. GagnonBelum ada peringkat
- International Society of Sports Nutrition Position Stand Energy Drinks and Energy ShotsDokumen73 halamanInternational Society of Sports Nutrition Position Stand Energy Drinks and Energy ShotsCarlos RamírezBelum ada peringkat
- Enzyme Catalysis-Chapter 7 (Part 1)Dokumen22 halamanEnzyme Catalysis-Chapter 7 (Part 1)OmSilence2651Belum ada peringkat
- Nutrient Requirements of Indian Major Carp: Protein and Amino AcidsDokumen4 halamanNutrient Requirements of Indian Major Carp: Protein and Amino AcidsBadrul HassanBelum ada peringkat
- MSc Home Economics Food & Nutrition MCQsDokumen153 halamanMSc Home Economics Food & Nutrition MCQsSaba ChaudhryBelum ada peringkat
- Sources of Different Vitamins and Diseases Caused by Their DeficiencyDokumen2 halamanSources of Different Vitamins and Diseases Caused by Their DeficiencyPrashant SuryawanshiBelum ada peringkat
- Milk Calcium Dietary Supplement 600 MG 100 Soft GelsDokumen3 halamanMilk Calcium Dietary Supplement 600 MG 100 Soft Gelssindi setiyadiBelum ada peringkat
- Chemical Compositions of Ipomea Aquatica Green Kangkong PDFDokumen7 halamanChemical Compositions of Ipomea Aquatica Green Kangkong PDFPaul DizonBelum ada peringkat
- 27 - Najla - Tugas Individu PSGDokumen7 halaman27 - Najla - Tugas Individu PSGDIII - Gizi - NajlaBelum ada peringkat
- Burning Feet SyndromeDokumen4 halamanBurning Feet SyndromeSellappan MuthusamyBelum ada peringkat
- Biology Form 4 Chapter 6 - VitaminsDokumen3 halamanBiology Form 4 Chapter 6 - VitaminsSim Zong Xern0% (1)
- Water-soluble Vitamins CompilationDokumen5 halamanWater-soluble Vitamins CompilationJustin AncogBelum ada peringkat
- University of The Philippines ManilaDokumen11 halamanUniversity of The Philippines ManilaAngeli Jean Koreen CorpuzBelum ada peringkat
- Food Chemistry Lecture on VitaminsDokumen50 halamanFood Chemistry Lecture on VitaminsQamber pkBelum ada peringkat
- Niacinamide and The SkinDokumen6 halamanNiacinamide and The SkinLesti LubisBelum ada peringkat
- Fortified Rice Kernel Manufacturing Industry: (Capacity: 200kgs Per Hour)Dokumen57 halamanFortified Rice Kernel Manufacturing Industry: (Capacity: 200kgs Per Hour)charsaubees420Belum ada peringkat
- The Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossDari EverandThe Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossPenilaian: 4 dari 5 bintang4/5 (22)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisDari EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisPenilaian: 3 dari 5 bintang3/5 (2)
- Forever Strong: A New, Science-Based Strategy for Aging WellDari EverandForever Strong: A New, Science-Based Strategy for Aging WellBelum ada peringkat
- Power Souping: 3-Day Detox, 3-Week Weight-Loss PlanDari EverandPower Souping: 3-Day Detox, 3-Week Weight-Loss PlanPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthDari EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthBelum ada peringkat
- The Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthDari EverandThe Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthPenilaian: 5 dari 5 bintang5/5 (37)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyDari EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyPenilaian: 5 dari 5 bintang5/5 (1)
- Happy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainDari EverandHappy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainPenilaian: 3.5 dari 5 bintang3.5/5 (6)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeDari EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifePenilaian: 5 dari 5 bintang5/5 (1)