Anesthesia For Patients With Coronary Stents For Non Cardiac ,,, Surgery
Diunggah oleh
Mirabela Colac0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
23 tayangan6 halamanDiscontinuation of antiplatelet therapy soon after Percutaneous Coronary inter!ention+ %ith stenting confers significant mortality during non cardiac surgery. Clopidogrel 1# mg daily should &e gi!en for at least. / months if patients are not at high risk of &leeding.
Deskripsi Asli:
Judul Asli
Anesthesia for Patients With Coronary Stents for Non Cardiac ,,, Surgery
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniDiscontinuation of antiplatelet therapy soon after Percutaneous Coronary inter!ention+ %ith stenting confers significant mortality during non cardiac surgery. Clopidogrel 1# mg daily should &e gi!en for at least. / months if patients are not at high risk of &leeding.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
23 tayangan6 halamanAnesthesia For Patients With Coronary Stents For Non Cardiac ,,, Surgery
Diunggah oleh
Mirabela ColacDiscontinuation of antiplatelet therapy soon after Percutaneous Coronary inter!ention+ %ith stenting confers significant mortality during non cardiac surgery. Clopidogrel 1# mg daily should &e gi!en for at least. / months if patients are not at high risk of &leeding.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 6
ANESTHESIA FOR PATIENTS WITH CORONARY STENTS FOR NON CARDIAC SURGERY
Dr. Mahesh Vakamudi
Professor and Head
Department of Anesthesiology, Critical Care and Pain Medicine
Sri Ramachandra ni!ersity
INTRODUCTION
Appro"imately #$ of patients %ith intracoronary stents %ill undergo non cardiac surgery %ithin the first
year after stenting, and an increasing num&er %ill continue to present for surgery thereafter. As the
success of the stents re'uires long(term antiplatelet therapy, management of patients %ith these
de!ices poses a dilemma to the anesthesiologist. Discontinuation of antiplatelet therapy relati!ely soon
after PC) *percutaneous coronary inter!ention+ %ith stenting confers significant mortality during non
cardiac surgery. As stent endotheliali,ation may not yet &e complete at the time of surgery, a&rupt
discontinuation of antiplatelets com&ined %ith the prothrom&otic state induced &y surgery increases
the risk of acute perioperati!e stent throm&osis *-ig..+ and myocardial infarction. Continuation of
antiplatelet medications may &e associated %ith an increased risk of intraoperati!e &leeding and also
pre!ent administration of regional anesthesia.
As per the /001 -ocused pdate of the ACC2AHA2SCA) /00# 3uideline pdate for Percutaneous
Coronary )nter!ention, all post(PC) stented patients recei!ing a D4S *drug eluting stent+, clopidogrel 1#
mg daily should &e gi!en for at least ./ months if patients are not at high risk of &leeding. -or post(PC)
patients recei!ing a 5MS *&are metal stent+, clopidogrel should &e gi!en for a minimum of . month
and ideally up to ./ months *unless the patient is at increased risk of &leeding6 then it should &e gi!en
for a minimum of / %eeks+. (Level of Evidence: B)
7hey also recommend postponing all electi!e procedures for %hich there is a significant risk of &leeding
until dual(antiplatelet therapy is completed *7a&le .+.
Aspirin is continued throughout the perioperati!e period, e"cept in instances %here surgery is
performed in closed space *intracranial surgery, posterior cham&er of the eye, spinal surgery in the
medullary canal+.
7he su&stitution of non selecti!e 8SA)Ds and 9M:H for dual(antiplatelet therapy is contro!ersial and
there is no scientific e!idence to support their efficacies in pre!enting perioperati!e stent throm&osis.
7he concomitant use of non selecti!e 8SA)Ds and aspirin significantly increases cardiac mor&idity and
mortality in patients %ith coronary artery disease and the incidence may &e e!en higher in patients %ith
coronary stents. Although heparin therapy is often used perioperati!ely for throm&oem&olic
prophyla"is, it does not ha!e antiplatelet properties and is not protecti!e against stent throm&osis.
Fig.1. Diagram of the pathophysiology of acute perioperative stent thrombosis
A&rupt discontinuation of clopidogrel A&rupt discontinuation of aspirin
Re&ound effect6
Significantly increased inflammatory prothrom&otic state
Signficantly increased platelet adhesion and aggregation
4"cessi!e throm&o"ane A/ acti!ity
Surgical intervention
Increase !rot"ro#$otic an in%la##ator& state
)ncreased cytokines, neuroendocrine, inflammatory mediator release
)ncreased platelet adhesi!eness and persistently high platelet counts
)ncreased release of procoagulant factors
Decreased2)mpaired fi&rinolysis
Prothrom&otic27hrom&otic state %ith incompletely endotheliali,ed stent*s+
Stent throm&osis
Myocardial infarction
Death
;
;
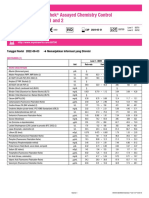
Table 1. Duration of antiplatelet therapy and timing of noncardiac surgery
To summarize treatment options for patients with DES: (1) continue dual-antiplatelet therapy
throughout the perioperative period for patients at low ris of !leeding (") implement #!ridging
therapy$% in which a short acting &' ((!)(((a inhi!itor (tirofi!an or eptifi!atide) or throm!in
inhi!itor% or !oth% is su!stituted for clopidogrel during the perioperative period* or (+)
discontinue clopidogrel preoperatively% restarting it as soon as possi!le postoperatively, &'
((!)(((a inhi!itors have !een favored since this platelet receptor is the pivotal mediator for
platelet aggregation and throm!us formation, They are more potent than the com!ination of
aspirin and a theinopyridine, &' ((!)(((a inhi!itors are recommended as !ridging therapy
primarily (1) in patients who have not completed dual-antiplatelet therapy and (") in patients
whose stent comple-ities and comor!idities significantly increase their ris for developing
catastrophic stent throm!osis and its se.uelae, Tirofi!an and eptifi!atide are administered
parenterally% have half lives / " h% and are eliminated !y renal clearance, 'latelet function returns
to 012 - 312 of normal after the infusion is stopped for 0 4 5 h,
Dilatation 'it"out stenting< / = > %eek of dual(antiplatelet therapy
Surgery postponed for / = > %eek *!ital surgery only+
PCI an ()S< > = ? %eek minimum of dual( antiplatelet therapy
4lecti!e surgery postponed @ ? %eek, &ut not for more than ./ %eek, %hen
restenosis may &egin to occur
PCI an DES< ./ months of dual(antiplatelet therapy
4lecti!e surgery postponed for @ ./ months
)n patients in %hom coronary re!asculari,ation %ith PC) is appropriate for
mitigation of cardiac symptoms and %ho need electi!e non cardiac surgery in the
su&se'uent ./ months, a strategy of &alloon angioplasty or 5MS placement
follo%ed &y > to ? %eeks of dual(antiplatelet therapy is pro&a&ly indicated
Aspirin< 9ifelong therapy, %hiche!er is the re!asculari,ation techni'ue
Fig.2. Algorithm for perioperative management of patients with bare metal stents
7ime of anticipated surgery
A ? %ks after 5MS implantation B ? %ks after 5MS implantation
4lecti!e
rgent
Postpone surgery until
5MS has &een
implanted ? %eeks
Can clopidogrel and aspirin &e
continued in the perioperati!e
periodC
Continue aspirin throughout surgery
if at all possi&le
Des 8o Consider &ridging therapy
Proceed
Can aspirin &e
continuedC
Des 8o
Consider &ridging therapy
Proceed
Fig.3. Algorithm for perioperative management of patients with drug eluting stents
Management of stent throm&osis:
:hen stent throm&osis occurs, it acutely manifests as a S74M) or a sudden malignant dysrhythmia, and
must &e treated %ith immediate reperfusion to a!oid a transmural M) due to the a&rupt interruption of
coronary &lood flo% in a myocardial region that is neither collaterali,ed nor preconditioned &y recurrent
chronic ischemia. 7hrom&olytic therapy *)V or intracoronary+ is significantly less effecti!e than PC) in
treating stent throm&osis and restoring myocardial perfusion. Administration of throm&olytic therapy is
often prohi&iti!e in the perioperati!e period. 7herefore, primary PC) is the definiti!e treatment for
perioperati!e stent throm&osis and restoration of coronary stent patency. Surgical procedures should &e
performed in institutions %here />(h inter!entional cardiology is a!aila&le to pro!ide immediate and
emergent inter!ention. Postoperati!e management should include admission to a higher(acuity unit
%ith continued electrocardiogram monitoring and cardiology sur!eillance.
Regional anesthesia *RA+<
8eura"ial &lockade attenuates the hypercoagula&le perioperati!e state &y &lunting the sympathetic
response. Systemic a&sorption of local anesthetics pro!ides antiplatelet effects &y &locking 7"A/ and
decreasing platelet aggregation. 7hese &enefits of regional anesthesia are ad!antageous in patients %ith
intracoronary stents. ASRA recommendations ha!e to &e follo%ed to decide %hen RA can &e
administered in patients on antiplatelets.
7he role of perioperati!e platelet transfusions in patients on dual(antiplatelet therapy %hen RA is
considered cannot &e Eustified. 4" !i!o studies ha!e sho%n that transfused platelets may not &e
inhi&ited &y the presence of ade'uate serum le!els of antiplatelet drugs. Moreo!er, the throm&ogenic
surfaces of stents may attract and acti!ate donor platelets to a e!en greater e"tent than endogenous
platelets, further increasing the risk of stent throm&osis, M) and death.
CF8C9S)F8
7he management of patients %ith coronary artery stents during the perioperati!e period is an important
safety issue. Communication &et%een the patientGs cardiologist, surgeon and anesthesiologist is
essential to minimi,e the risk of catastrophic stent throm&osis.
Anda mungkin juga menyukai
- 2009 Esc GuidelinesperioperativecardiaccareDokumen44 halaman2009 Esc GuidelinesperioperativecardiaccareAgnese ValentiniBelum ada peringkat
- ESPEN GuidelineDokumen37 halamanESPEN GuidelineAuliangi TamayoBelum ada peringkat
- 100 BLWrecipesDokumen52 halaman100 BLWrecipeslona2010100% (1)
- Managing Coagulopathy ICUDokumen38 halamanManaging Coagulopathy ICUMirabela Colac100% (1)
- 00.QUICK GUIDE TO Cardiopulmonary Care 3rd PDFDokumen246 halaman00.QUICK GUIDE TO Cardiopulmonary Care 3rd PDFMirabela ColacBelum ada peringkat
- Ventilator Final Version 180215Dokumen64 halamanVentilator Final Version 180215Mirabela ColacBelum ada peringkat
- Ultrasound Guidance - PollardDokumen72 halamanUltrasound Guidance - Pollardmasquebolso100% (3)
- HSRP 04 153Dokumen15 halamanHSRP 04 153Mirabela ColacBelum ada peringkat
- ARDSnet Ventilation Protocol SummaryDokumen2 halamanARDSnet Ventilation Protocol SummaryvbfisioBelum ada peringkat
- Anesthesia GuideDokumen84 halamanAnesthesia GuideRaisa Paz RamosBelum ada peringkat
- 05 OA - 033-0911 - Koh Liang Khai DarrenDokumen7 halaman05 OA - 033-0911 - Koh Liang Khai DarrenMirabela ColacBelum ada peringkat
- Ten Things To Know - Stroke Guidelinesv1Dokumen1 halamanTen Things To Know - Stroke Guidelinesv1Mirabela ColacBelum ada peringkat
- 168 Antibiotics in Critical Care - An IntroductionDokumen6 halaman168 Antibiotics in Critical Care - An IntroductionMirabela ColacBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- MS Case PresDokumen33 halamanMS Case PresShaine_Thompso_6877Belum ada peringkat
- Jcpe 12206 PDFDokumen17 halamanJcpe 12206 PDFrozh rasulBelum ada peringkat
- How To Whistle Loud 14 Steps (With Pictures) - WikiHowDokumen4 halamanHow To Whistle Loud 14 Steps (With Pictures) - WikiHowVeselin VasilevBelum ada peringkat
- ENT Radiology ADokumen64 halamanENT Radiology AMitulsinh M RavaljiBelum ada peringkat
- Free Printable at Home Brain Breaks and Active CalmingDokumen12 halamanFree Printable at Home Brain Breaks and Active Calmingapi-505036826Belum ada peringkat
- Passive to Active Voice ConversionDokumen3 halamanPassive to Active Voice ConversionQhaisya Binasanjaya67% (3)
- Location and External Anatomy of The KidneysDokumen15 halamanLocation and External Anatomy of The KidneysKyla Malapit GarvidaBelum ada peringkat
- Lecture 3 - Monod KineticsDokumen19 halamanLecture 3 - Monod KineticsZeny Naranjo0% (1)
- The Stages of Mitosis and Meiosis Cell DivisionDokumen50 halamanThe Stages of Mitosis and Meiosis Cell DivisionRosana Beatrix GualbertoBelum ada peringkat
- Human Body System WorksheetDokumen2 halamanHuman Body System WorksheetRPh Krishna Chandra JagritBelum ada peringkat
- jm800328v PDFDokumen9 halamanjm800328v PDFVINODBelum ada peringkat
- Full Lab ReportDokumen5 halamanFull Lab ReportchampmorganBelum ada peringkat
- Answer Guide For O Level Biology (5090/3) - Paper 3 Practical Test June 2001Dokumen3 halamanAnswer Guide For O Level Biology (5090/3) - Paper 3 Practical Test June 2001MSHBelum ada peringkat
- Cell Division MCQ Questions & AnswersDokumen17 halamanCell Division MCQ Questions & Answersmurali.prionsgm100% (1)
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiDokumen2 halamanLyphochek Assayed Chemistry Control Levels 1 and 2: Tanggal Revisi 2022-06-03 Menunjukkan Informasi Yang DirevisiFahmiBelum ada peringkat
- 9700 w01 Ms 2Dokumen4 halaman9700 w01 Ms 2Sathya Seelan0% (1)
- Photosynthesis WorksheetDokumen3 halamanPhotosynthesis WorksheetByambazaya E100% (2)
- Mod 7 PoisoningDokumen12 halamanMod 7 Poisoningrez198767% (3)
- Imaging Modalities For Lung DiseasesDokumen14 halamanImaging Modalities For Lung DiseasesYnaffit Alteza Untal100% (1)
- Pre-Dental Jaw Relationship ReportDokumen10 halamanPre-Dental Jaw Relationship ReportFidz LiankoBelum ada peringkat
- Passion and Deceit Part VI PDFDokumen20 halamanPassion and Deceit Part VI PDFno2meBelum ada peringkat
- Clinic VisitDokumen5 halamanClinic VisitEka YunusBelum ada peringkat
- 15 Healing Miracles EX735 SCENAR Book StoriesDokumen11 halaman15 Healing Miracles EX735 SCENAR Book StoriesBacean Aurel Ioan100% (5)
- Shanks 1996Dokumen5 halamanShanks 1996Sarly FebrianaBelum ada peringkat
- THYMUS PPT Final 7marDokumen15 halamanTHYMUS PPT Final 7marRajesh UgalmugleBelum ada peringkat
- O Treinamento Físico Atenua A Cardiomiopatia Cirrótica (TRADUZIR)Dokumen11 halamanO Treinamento Físico Atenua A Cardiomiopatia Cirrótica (TRADUZIR)Igor Ferrari StreitBelum ada peringkat
- Potato Poisoning: Understanding Solanine ToxicityDokumen13 halamanPotato Poisoning: Understanding Solanine ToxicityDaz Jones100% (2)
- A Simplified Technique For Determining The Occlusal Plane in Full Denture ConstructionDokumen4 halamanA Simplified Technique For Determining The Occlusal Plane in Full Denture ConstructionAlejandro García ArmentaBelum ada peringkat
- Memory SkillsDokumen70 halamanMemory SkillsAsiri Samanatha Elegoda100% (1)
- Cardiology MCQDokumen12 halamanCardiology MCQAhmed MahanaBelum ada peringkat