OBESIDADYESTILODEVIDA
Diunggah oleh
Jorge KlyverDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
OBESIDADYESTILODEVIDA
Diunggah oleh
Jorge KlyverHak Cipta:
Format Tersedia
ISSN: 1524-4539
Copyright 2008 American Heart Association. All rights reserved. Print ISSN: 0009-7322. Online
72514
Circulation is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX
DOI:10.1161/CIRCULATIONAHA.107.759951
2008;117;3062-3069; originally published online Jun 9, 2008; Circulation
Tjnneland, Albert M. Joensen and Kim Overvad
Majken K. Jensen, Stephanie E. Chiuve, Eric B. Rimm, Claus Dethlefsen, Anne
Obesity, Behavioral Lifestyle Factors, and Risk of Acute Coronary Events
http://circ.ahajournals.org/cgi/content/full/117/24/3062
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://www.lww.com/reprints
Reprints: Information about reprints can be found online at
journalpermissions@lww.com
410-528-8550. E-mail:
Fax: Kluwer Health, 351 West Camden Street, Baltimore, MD 21202-2436. Phone: 410-528-4050.
Permissions: Permissions & Rights Desk, Lippincott Williams & Wilkins, a division of Wolters
http://circ.ahajournals.org/subscriptions/
Subscriptions: Information about subscribing to Circulation is online at
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Obesity, Behavioral Lifestyle Factors, and Risk of Acute
Coronary Events
Majken K. Jensen, MSc; Stephanie E. Chiuve, ScD; Eric B. Rimm, ScD; Claus Dethlefsen, PhD;
Anne Tjnneland, PhD; Albert M. Joensen, MD; Kim Overvad, PhD
BackgroundWhether physical activity reduces the impact of obesity on the risk of acute coronary events is much debated.
However, little is known about the role of other potentially modifiable lifestyle factors in combination with obesity.
Methods and ResultsWe followed up 54 783 women and men from the prospective Danish Diet, Cancer and Health
study who were 50 to 64 years at baseline (1993 to 1997) and free of coronary artery disease and cancer. During a
median of 7.7 years, 1127 incident cases of acute coronary syndrome (ACS) occurred. After multivariable adjustments,
each unit of body mass index was associated with a 5% and 7% higher risk of ACS among women and men, respectively
(both P0.0001 for trend). Overweight (body mass index, 25 to 29.9 kg/m
2
) and obesity (body mass index 30 kg/m
2
)
were associated with a higher risk of ACS among the physically active and inactive, in nonsmokers and smokers, and
among those who adhered more or less to a heart-healthy dietary pattern. Obese individuals who were active 1 to 3.5
h/wk had a lower risk than sedentary, obese individuals. In addition, obese nonsmokers had a lower risk than obese
smokers. Adherence to a healthy diet was associated with a lower risk of ACS; however, the relative risk was not
different among obese individuals with the most healthy diet versus obese individuals with a less healthy diet.
ConclusionsObesity confers an elevated risk of ACS in both healthy and less healthy subgroups of lifestyle behaviors.
Adherence to healthy lifestyle behaviors was associated with a lower risk even among obese individuals. (Circulation.
2008;117:3062-3069.)
Key Words: acute coronary syndrome
epidemiology
lifestyle
nutrition
obesity
risk factors
T
he prevalence of overweight and obesity is increasing in
most industrialized countries.
1,2
A high risk of coronary
heart disease is among the well-established adverse health
effects associated with excess weight.
3
Hypertension, hyper-
cholesterolemia, and diabetes are among the clinical condi-
tions that are important mediators of this association.
4,5
Thus,
obesity is an appropriate target for primary prevention efforts
because its modification has the potential to influence several
important clinical conditions along the causal pathway. How-
ever, it is clear that achieving weight loss or preventing
weight gain with aging is difficult for most individuals.
Therefore, investigations of behavioral modifications that
might reduce the impact of obesity on risk of morbidity and
mortality could have potentially great public health impact.
Editorial p 3057
Clinical Perspective p 3069
American and European guidelines for cardiovascular risk
reduction include aims for modifying the following behav-
ioral risk factors: an unhealthy diet, smoking, and a sedentary
lifestyle.
6,7
Thus, although weight loss may be a long-term
goal, these lifestyle factors can be modified over the short
term, and cardiovascular benefits may be gained, even among
the obese. It has been suggested by some,
8,9
but not all,
1013
that physical fitness or activity may alleviate the cardiovas-
cular risk associated with obesity. However, little is known
about the cardiovascular risk associated with obesity in the
context of other behavioral lifestyle factors. In light of the
growing obesity epidemic, we find it of interest to explore
whether obesity is associated with a lower risk in individuals
whose lifestyle is otherwise healthy compared with individ-
uals with less healthy lifestyle behaviors. Therefore, we
report here an analysis of the associations of obesity com-
bined with physical activity, smoking, and a Mediterranean
diet with risk of acute coronary events in a prospective
population-based study of 54 783 middle-aged men and
women.
Received December 14, 2007; accepted April 4, 2008.
From the Department of Clinical Epidemiology, Aarhus University Hospital, Aalborg, Denmark (M.K.J., K.O.); Center for Cardiovascular Research
(M.K.J., C.D., A.M.J., K.O.) and Department of Cardiology (A.M.J., K.O.), Aalborg Hospital, Aarhus University Hospital, Aalborg, Denmark;
Department of Nutrition, Harvard School of Public Health, Boston, Mass (S.E.C., E.B.R.); Department of Epidemiology, Harvard School of Public Health,
Boston, Mass (E.B.R.); Department of Medicine, Channing Laboratory, Brigham and Womens Hospital, Harvard Medical School, Boston, Mass
(E.B.R.); and Institute of Cancer Epidemiology, Danish Cancer Society, Copenhagen, Denmark (A.T.).
Guest Editor for this article was Robert H. Eckel, MD.
Presented at the American Heart Association 47th Annual Conference on Cardiovascular Disease Epidemiology and Prevention in association with the
Council on Nutrition, Physical Activity, and Metabolism, and published in abstract form (Circulation. 2007;115:e214e301).
Correspondence to Majken K. Jensen, Department of Clinical Epidemiology, Aarhus University Hospital, Sdr Skovvej 15, DK-9100 Aalborg,
Denmark. E-mail mkj@dce.au.dk
2008 American Heart Association, Inc.
Circulation is available at http://circ.ahajournals.org DOI: 10.1161/CIRCULATIONAHA.107.759951
3062
Epidemiology
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Methods
Study Population
Between 1993 and 1997, a total of 160 725 persons 50 to 64 years of
age were invited to participate in the Danish prospective Diet,
Cancer and Health study. Eligible participants were born in Denmark
and had no record of cancer in the Danish Cancer Registry. In total,
27 178 men (33.6% of the total number eligible) and 29 875 women
(37.5% of total number eligible) participated. A detailed description
of the cohort has been published.
14
The study was approved by the
Ethical Committees on Human Studies for the Copenhagen and the
Aarhus municipalities (KF 01-116/96).
Measures Obtained by Clinical Examination
Height and weight were measured at 2 study clinics by trained
laboratory technicians and recorded to the nearest half-centimeter
and 100 g, respectively. Body mass index (BMI) was calculated as
weight in kilograms divided by height in meters squared. A single
measurement of blood pressure after 5 minutes of rest also was
obtained, and serum total cholesterol was determined.
Measures Obtained by Self-
Administered Questionnaires
Participants completed a lifestyle questionnaire at the study clinic.
Smoking status was reported as current, former (years since quitting),
never, duration of smoking in years, and the number of cigarettes,
cigars, and cheroots/pipe smoked per day. Current tobacco consumption
was calculated in grams per day by summing the reported numbers per
day using conversion factors of 1 for cigarettes, 4.5 for cigars, and 3 for
cheroots or pipe. Leisure-time physical activity during the past year was
assessed from questions about average number of hours per week spent
on 6 types of activities (walking, gardening, housework, home mainte-
nance, sports, and biking) during summer and winter. Moderate to
vigorous physical activity was defined as average hours per week spent
on sport activities and biking (including as a mean of transport). Length
of education was collected in predefined categories (8, 8 to 10, and
10 years). Participants were asked whether a physician had ever
diagnosed them with hypertension, diabetes, or hypercholesterolemia
and whether they took medication for these conditions. Among women,
we used information on menstruations during the previous year and use
of hormone replacement therapy to define their menopausal status
(premenopausal, perimenopausal, and postmenopausal with and without
use of hormone replacement therapy).
Dietary information was obtained by a detailed, 192-item food-
frequency questionnaire, which the study participants had received by
mail before the visit to the study clinic. A description of the develop-
ment and validation of the food-frequency questionnaire has previously
been published.
15,16
Participants were asked how often they consumed
each food item on average over the past year. There were 12 choices for
frequency of intake, ranging from never or less than once per month
to 8 times or more per day. Total nutrient intake was calculated with
the software program FoodCalc
17
by multiplying the frequency of
consumption of each food by the nutrient content of the specified
portion and then summing the nutrient across all contributing foods. We
used the Mediterranean diet score developed by Trichopoulou et al
18
to
estimate adherence to a heart-healthy diet in this Danish population.
Recently, a modified version of this score, in which monounsaturated
fats are replaced by all unsaturated fats, has been suggested to make its
application more suitable to countries where olive oil is not the main
source of unsaturated fatty acids.
19
To calculate this modified diet score,
sex-specific medians of 8 dietary components were estimated. Partici-
pants received 1 point if their intake was above the median for
vegetables, legumes, fruits and nuts, cereals, fish, and the ratio of
unsaturated to saturated fat. One point also was assigned if the
consumption of meat and dairy products was below the median. The
score ranged from 0 (least healthy) to 8 (most healthy). Although
moderate alcohol intake (defined as 10 to 50 g/d among men and 5 to 25
g/d for women) was included in the original score, we considered it a
separate lifestyle factor.
End Point and Validation
Information on the disease end point was obtained by linkage with
central Danish registries via the unique identification number assigned
to all Danish citizens.
20
We identified participants who were registered
with a first-time discharge diagnosis of acute coronary syndrome (ACS;
unstable angina pectoris and nonfatal and fatal acute myocardial
infarction; International Classification of Diseases [ICD], eighth revi-
sion, codes 410 to 410.99 and 427.27; and ICD-10 codes I20.0, I21.x,
and I46.x) in the Danish National Register of Patients, which covers all
hospital discharge diagnoses since 1977 and all discharge diagnoses
from outpatient clinics since 1995 (until January 1, 2004).
21
Hospital
records of potential cases were retrieved from hospitals and reviewed by
3 reviewers. Cases were classified according to symptoms, signs,
coronary biomarkers, ECGs, and/or autopsy findings in accordance with
the current recommendations of the American Heart Association and the
European Society of Cardiology as described by Luepker et al.
22
A
detailed description of the validation study is in press.
22a
Other valida-
tion studies have indicated that myocardial infarctions are recorded with
a high degree of validity in this register.
23
Furthermore, linkage to the
Cause of Death Register allowed identification of participants with ACS
coded as a primary or secondary cause of death (to January 1, 2004).
Statistical Analysis
The present study included a total of 54 783 participants who were free
of coronary artery disease at baseline and for whom complete informa-
tion on height, weight, and the chosen behavioral factors was available.
We used World Health Organization cutoffs for healthy weight (BMI
25 kg/m
2
), overweight (25.0 to 29.9 kg/m
2
), and obesity (30 kg/m
2
).
For the behavioral factors, participants were categorized into nonsmok-
ers (never/past), light current smokers (1 to 14 g/d), and heavy current
smokers (15 g/d). Categories for moderate to vigorous physical
activity were as follows: 1, 1 to 3.49, and 3.5 h/wk; for the
Mediterranean diet score, they were 0 to 2, 3 to 4, and 5 to 8; and for
alcohol, they were 5, 5 to 25, and 25 g/d for women and 10, 10
to 50, and 50 g/d for men.
The observation time for each participant was the period from
enrollment in the cohort (between December 1993 and May 1997) until
the date of a registered nonfatal or fatal ACS event (n1127), death
resulting from other causes (n2512), emigration (n236), loss to
follow-up (n4), or January 1, 2004, whichever came first. Incidence
rates were calculated by dividing the number of events by the accumu-
lated person-time of follow-up within the groups of BMI. Cox
proportional-hazards regression with age as the underlying time axis
was performed to ensure that the estimation procedure was based on
comparisons of individuals at the same age (STATAversus 9.1 program
software, Stata Corp, College Station, Tex).
24
Multivariable-adjusted
models included smoking, physical activity, Mediterranean diet score,
alcohol, education, and menopausal status among women. Proportional-
hazards assumptions were tested in models including time-by-covariate
interactions, and no violations were detected. Smoothing splines with 5
df were used to assess nonlinear associations of continuous variables.
To determine the combined effects of obesity and the behavioral
factors, the BMI groups were cross-tabulated with each factor. Because
we found no statistically significant sex-based differences, we combined
men and women and allowed for sex-specific baseline hazards. We also
examined the association of BMI and ACS in participants with and
without existing diagnoses of the important clinical intermediates:
hypertension, diabetes, and hypercholesterolemia. Results were similar
when these clinical risk factors were defined according to self-reported
physician diagnoses or by using the clinical measures of blood pressure
and serum cholesterol. Statistical interaction was assessed on the
multiplicative scale by deviance tests based on comparisons of 2 log
likelihood in nested models with and without cross-product terms.
Because undiagnosed illness might bias our results, we compared
the association between BMI and ACS in analyses including cases
that occurred within the first 2 years of follow-up versus analyses
that included cases that occurred after 2 years of follow-up. Further
sensitivity analyses were performed by repeating analyses after the
exclusion of unstable angina from the ACS end point (n62). The
results were similar in these analyses (data not shown).
Jensen et al Obesity, Lifestyle Risk Factors, and ACS 3063
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
The authors had full access to and take full responsibility for the
integrity of the data. All authors have read and agree to the
manuscript as written.
Results
The prevalence and distributions of lifestyle and clinical risk
factors in the study population are shown in Table 1. The median
BMI was 24.8 kg/m
2
for women and 26.1 kg/m
2
for men.
During a median follow-up of 7.7 years, 1127 incident cases
of ACS were registered and verified. The association between
BMI and ACS was strong and graded. Women and men who
were healthy weight (BMI 25 kg/m
2
) had the lowest risk of
ACS, and a higher BMI was associated with an incrementally
higher risk of ACS (Table 2). We did not detect any departures
from a linear association between BMI and ACS when using
smoothing splines. After multivariable adjustments, each unit of
BMI was associated with a 5% and 7% higher risk among
women and men, respectively (both P0.0001 for trend).
Further adjustment for the clinical intermediates attenuated the
associations, although obesity (BMI 30 kg/m
2
) remained
statistically significantly associated with a higher risk of ACS
among both women and men. Although the relative risk associ-
ated with obesity was of smaller magnitude among men than
women, the absolute risk was substantially higher among men
(differences in the unadjusted incidence rates between the
healthy weight and obese individuals, 304 and 112 cases per
100 000 person-years among men and women, respectively).
Smoking, not engaging in moderate to vigorous physical activ-
ity, a low adherence to the Mediterranean diet, and having the
lowest alcohol intake were all associated with a higher risk of
ACS, as were the diagnoses of hypertension, diabetes, and
hypercholesterolemia (Table 3).
Overweight and Obesity Combined With
Behavioral Factors
In Table 4, we show that a higher BMI was associated with a
higher risk of ACS in all 3 groups of physical activity, in
smokers and nonsmokers, in those with a healthy and a less
healthy diet, and among those with and without a moderate
alcohol intake. Overweight (BMI, 25 to 29.9 kg/m
2
) and obesity
(BMI 30 kg/m
2
) were strongly associated with risk of ACS
regardless of smoking status; being a heavy smoker also was
associated with a high risk of ACS in all BMI groups. Compared
with the joint reference group of nonsmokers who were healthy
weight (BMI 25 kg/m
2
), the risk associated with obesity was
lower in nonsmokers (hazard ratio [HR], 2.35, 95% CI, 1.81 to
3.05) than in heavy smokers (HR, 3.74; 95% CI, 2.71 to 5.15).
A low level of physical activity was associated with a
higher risk of ACS in both healthy-weight and overweight
individuals. Among the obese individuals, we did not see a
clear trend for physical activity, but compared with the most
physically active (3.5 h/wk) who were healthy weight, the
HR among obese individuals who were moderately active (1
to 3.5 h/wk) was lower than the HR among the obese who
were physically inactive (1 h/wk) (HR, 1.92, 95% CI, 1.42
to 2.59; and HR, 2.74; 95% CI, 2.04 to 3.68, respectively).
A higher BMI was associated with a higher risk of ACS
across all groups of the Mediterranean diet score and alcohol
intake. In overweight and healthy-weight individuals, greater
adherence to the Mediterranean diet was associated with a
lower risk of ACS, whereas the risk among obese individuals
was not different among those who scored high on this
dietary pattern and those with a less heart-healthy diet.
Only 8% of the participants were in the healthiest group of
all 4 behavioral lifestyle risk factors (physically active 3.5
h/wk, nonsmoking, highest score on the Mediterranean diet
scale, and a light to moderate alcohol intake), and only 47
cases of ACS occurred in this group during follow-up.
Among these participants characterized by an overall healthy
Table 1. Baseline Characteristics of 28 991 Women and
25 792 Men 50 to 64 Years of Age Who Participated in the Diet,
Cancer, and Health Study*
Characteristics Women Men
Anthropometric and
physiological
Age, y 56 (5163) 56 (5163)
BMI, kg/m
2
24.8 (20.831.2) 26.1 (22.531.1)
Postmenopausal, % 85
Use of hormone
replacement therapy, %
48
Behavioral
Current smokers, % 33 40
Physical activity, h/wk 2.5 (0.08.0) 2.0 (0.08.5)
Education 8 y, % 31 34
Mediterranean diet score 4 (26) 4 (26)
Alcohol, g/d 9.3 (1.034.5) 19.4 (3.662.6)
Dietary factors, g/d
Vegetables 167 (68317) 149 (62282)
Fruits 168 (45410) 113 (24320)
Legumes 0.65 (02.83) 0.30 (01.53)
Fish 35 (1570) 42 (1882)
Meat 141 (87219) 208 (135317)
Dairy 305 (81771) 294 (7479)
Cereals 163 (94255) 204 (114312)
Whole-grain cereals 74 (30130) 101 (37171)
Monounsaturated fat 22.8 (14.734.4) 31.6 (20.747.0)
Polyunsaturated fat 11.6 (7.0118.6) 15.0 (9.223.6)
Saturated fat 27.2 (16.642.2) 35.6 (22.553.6)
Energy intake, kcal/d 1935 (13632688) 2373 (17063261)
Clinical
Systolic blood
pressure, mm Hg
136 (112165) 140 (119167)
Diastolic blood
pressure, mm Hg
81 (6894) 84 (7299)
Serum total
cholesterol, mmol/L
6.2 (4.97.8) 5.9 (4.77.4)
Diagnosed hypertension, % 19 17
Diagnosed diabetes, % 1.6 2.8
Diagnosed
hypercholesterolemia, %
11 13
*Continuous characteristics are shown as medians (10th to 90th
percentiles).
Average hours of moderate to vigorous physical activity.
Nonfasting.
3064 Circulation June 17, 2008
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
lifestyle, the HRs for ACS were 1.65 (95% CI, 0.82 to 3.22)
for the overweight and 2.65 (95% CI, 1.12 to 6.27) for the
obese (data not shown).
Overweight and Obesity Combined With Clinical
Risk Factors
We also addressed whether obesity was associated with risk
of ACS among individuals with and without preexisting
diagnoses of the clinical intermediates (hypertension, hyper-
cholesterolemia, and diabetes). BMI was strongly associated
with risk of ACS among participants who did not have these
conditions and among hypercholesterolemic participants.
Among diabetic and hypertensive participants, the associa-
tions between BMI and ACS were not as strong; however,
very few participants were diagnosed with diabetes in this
cohort (3%). The highest risk was consistently observed
among participants who were both obese and diagnosed with
any of the 3 clinical risk factors (Table 5).
Discussion
In this large prospective study of 54 500 men and women,
BMI was associated with risk of ACS at all levels of classic
behavioral lifestyle risk factors: physical inactivity, smoking,
and an unhealthy diet. The risk of ACS was much lower
among obese nonsmokers than smokers, and a more physi-
cally active lifestyle was associated with a lower risk even in
obese smokers. Although our study suggests that adherence to
a healthy lifestyle reduces the impact of obesity on risk of
ACS, confirmation of a true causal relationship requires an
intervention study with long duration.
Few studies have explored obesity combined with potentially
modifiable behavioral lifestyle factors in relation to coronary
heart disease risk. However, detailed investigations of the
relationship between obesity and physical activity/fitness is an
important exception because their relative importance as predic-
tors of cardiovascular risk remains an area of controversy.
1013,25
Although we had few participants who were both obese and
physically active, our results are generally in line with cohort
studies from Finland,
11
Norway,
13
and the US Nurses Health
Study.
10
These studies all suggest that both obesity and self-
reported physical activity are important independent predictors
of future coronary heart disease. Contrary observations have
been reported from the Aerobics Center Longitudinal Study, in
which body fatness was not associated with a higher risk of
cardiovascular death among those who were physically fit as
measured by a treadmill exercise test.
25
Self-assessed physical
activity and measures of fitness may not fully capture the same
information because physical fitness is not determined solely by
habitual physical activity but also reflects genetics and underly-
ing diseases.
26
We did not have measures of cardiorespiratory
fitness available in our study; however, our findings are compa-
rable to those observed in the Lipids Research Clinics Study, in
which physical fitness also was measured.
12
Our analysis extends the ongoing discussion of the role of
body fatness among those who are physically active or fit by
Table 2. Incidence Rates and HRs With 95% CIs of ACS Among 28 991 Women and 25 792 Men According
to BMI
BMI, kg/m
2
25 2529.9 30 Per 1 kg/m
2
Women
Incidence rate,* cases (n) 87 (101) 139 (106) 199 (62)
Crude HR (95% CI) 1 (Referent) 1.48 (1.131.95) 2.08 (1.522.86) 1.05 (1.021.07)
Multivariable-adjusted HR
(95% CI)
1 (Referent) 1.54 (1.172.03) 2.06 (1.492.86) 1.05 (1.031.07)
Plus clinical factors
(self-reported)
1 (Referent) 1.33 (1.001.76) 1.63 (1.162.29) 1.03 (1.011.06)
Plus clinical factors 1 (Referent) 1.33 (1.001.76) 1.56 (1.112.20) 1.03 (1.011.06)
Men
Incidence rate,* cases (n) 340 (233) 456 (441) 644 (184)
Crude HR (95% CI) 1 (Referent) 1.32 (1.121.54) 1.88 (1.552.28) 1.06 (1.051.08)
Multivariable adjusted HR
(95% CI)
1 (Referent) 1.40 (1.191.64) 1.93 (1.582.35) 1.07 (1.051.08)
Plus clinical factors
(self-reported)
1 (Referent) 1.29 (1.091.52) 1.64 (1.332.02) 1.05 (1.031.07)
Plus clinical factors 1 (Referent) 1.19 (1.011.40) 1.43 (1.151.76) 1.04 (1.021.06)
*Incidence per 100 000 person-years.
Multivariable-adjusted models included physical activity (1, 1 to 3.5, and 3.5 h/wk), smoking (never, past, recent quitters,
currently smoking 1 to 14, 15 to 24, or 24 g/d, and duration of smoking), education (8, 8 to 10, and 10 years), the
Mediterranean diet score (in 3 levels), and alcohol (3 levels). Analyses among women also adjusted for postmenopausal status and
use of hormone replacement therapy (premenopausal, perimenopausal, postmenopausal with no hormone replacement therapy, and
postmenopausal with hormone replacement therapy).
Multivariable model specified above and further adjusted for self-reported physician-diagnosed hypertension, hypercholesterol-
emia, and diabetes (yes/no).
Multivariable model specified above and further adjusted for systolic and diastolic blood pressures (continuous), serum cholesterol
(continuous), and self-reported physician diagnosed of diabetes (yes/no).
Jensen et al Obesity, Lifestyle Risk Factors, and ACS 3065
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
including 2 other well-established behavioral risk factors incor-
porated into international guidelines for cardiovascular disease
reduction. We found that obese individuals had a considerable
lower risk if they were nonsmokers compared with smokers.
Smoking is a modifiable behavioral risk factor that adds sub-
stantially to the cardiovascular risk in all BMI groups of the
population, and advice to quit seems applicable to both normal-
weight and obese individuals. Although we observed that adher-
ence to a Mediterranean style diet was associated with a lower
risk of ACS, this dietary pattern was not strongly associated with
risk among the obese individuals. The scoring systemwe used to
operationalize this dietary pattern relies on strong epidemiolog-
ical evidence for the individual dietary components; in addition,
the score has been validated and shown to strongly predict
morbidity and mortality in several European populations.
18,19
However, we cannot exclude that a different dietary score might
capture a healthy Nordic eating pattern better and that this could
have a stronger association with ACS across all BMI groups. In
addition, we found that BMI was associated with a higher risk
across groups of alcohol intake.
BMI is an easily obtainable measure that remains widely used
as an indicator of overweight and obesity.
11,2729
Although other
adiposity measures such as waist circumference may better
capture the adverse metabolic changes that are likely to mediate
the association between obesity coronary heart disease,
30
we
found a strong and graded association between BMI and ACS. A
strength of our study is the use of directly obtained measures of
height and weight of all participants, which diminishes the
potential bias toward a higher risk of ACS at lower BMI ranges
resulting from possible understated weight in obese individu-
als.
31
Recent weight loss before the baseline examination as a
result of undiagnosed symptoms of cardiovascular illness could
have biased our results toward a higher risk of ACS at lower
levels of BMI. However, we observed a direct association
between BMI and risk when cases that occurred during the first
2 and subsequent years of follow-up were considered.
Table 3. Incidence Rates and HRs With 95% CIs of ACS Among 28 991 Women and 25 792 Men According to Behavioral Lifestyle
and Clinical Risk Factors
Behavioral Factors
Women Men
Incidence Rate,*
Cases (n)
Crude HR
(95% CI)
Adjusted HR
(95% CI)
Incidence Rate,*
Cases (n)
Crude HR
(95% CI)
Adjusted HR
(95% CI)
Smoking
Not current (never/past) 75 (112) 1 (Referent) 1 (Referent) 306 (361) 1 (Referent) 1 (Referent)
Current, light (114 g/d) 196 (67) 2.47 (1.823.35) 1.76 (1.152.69) 489 (100) 1.58 (1.271.97) 1.34 (1.041.74)
Current, heavy (15 g/d) 232 (90) 3.31 (2.514.37) 2.05 (1.343.13) 719 (397) 2.41 (2.092.78) 1.84 (1.492.28)
Physical activity, h/wk
1 210 (74) 1 (Referent) 1 (Referent) 588 (240) 1 (Referent) 1 (Referent)
13.5 106 (111) 0.54 (0.400.72) 0.67 (0.500.90) 414 (354) 0.72 (0.610.85) 0.88 (0.741.04)
3.5 101 (84) 0.52 (0.380.71) 0.69 (0.500.96) 392 (264) 0.70 (0.590.84) 0.92 (0.771.10)
Per 1 h/wk 0.94 (0.910.98) 0.96 (0.931.00) 0.98 (0.961.00) 1.00 (0.981.01)
Mediterranean diet score
02 161 (63) 1 (Referent) 1 (Referent) 629 (171) 1 (Referent) 1 (Referent)
34 129 (124) 0.79 (0.581.07) 0.94 (0.691.28) 448 (366) 0.71 (0.590.85) 0.81 (0.670.97)
58 93 (82) 0.58 (0.420.80) 0.83 (0.591.17) 378 (321) 0.59 (0.490.71) 0.78 (0.650.95)
Per 1 point 0.88 (0.810.95) 0.95 (0.881.02) 0.89 (0.850.93) 0.95 (0.910.99)
Alcohol, g/d
Women, 5; men 10 176 (122) 1 (Referent) 1 (Referent) 570 (266) 1 (Referent) 1 (Referent)
Women, 525; men, 1050 96 (110) 0.60 (0.460.78) 0.75 (0.570.97) 400 (465) 0.72 (0.610.83) 0.76 (0.660.89)
Women, 25; men 50 95 (37) 0.61 (0.420.88) 0.68 (0.470.99) 412 (127) 0.75 (0.610.93) 0.63 (0.510.78)
Per 10 g/d 0.90 (0.810.98) 0.92 (0.841.00) 0.96 (0.930.99) 0.94 (0.910.96)
Clinical factors
Normotensive 85 (154) 1 (Referent) 1 (Referent) 393 (614) 1 (Referent) 1 (Referent)
Hypertensive 268 (115) 2.85 (2.243.63) 2.69 (2.103.45) 648 (244) 1.56 (1.341.81) 1.50 (1.291.74)
Nondiabetic 116 (245) 1 (Referent) 1 (Referent) 426 (761) 1 (Referent) 1 (Referent)
Diabetic 428 (14) 3.18 (1.865.46) 2.64 (1.524.58) 958 (46) 2.05 (1.522.76) 1.79 (1.332.42)
Normocholesterolemic 96 (156) 1 (Referent) 1 (Referent) 375 (548) 1 (Referent) 1 (Referent)
Hypercholesterolemic 187 (113) 1.71 (1.342.18) 1.52 (1.191.94) 652 (307) 1.71 (1.481.96) 1.60 (1.391.85)
*Incidence per 100 000 person-years.
Adjusted models included BMI, physical activity, smoking status, Mediterranean diet score, alcohol (categories as in the table), and education (8, 8 to 10, and
10 years). Analyses among women also adjusted for postmenopausal status and use of hormone replacement therapy (premenopausal, perimenopausal,
postmenopausal with no hormone replacement therapy, and postmenopausal with hormone replacement therapy).
3066 Circulation June 17, 2008
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Whether obesity exerts independent and direct effects on
coronary atherosclerosis progression and cardiovascular disease
beyond its strong association with established clinical risk
factors remains controversial.
3237
Currently used risk functions
for the prediction of coronary events in the general population do
not include measures of excess body weight because it is
considered to affect risk indirectly through more proximal
physiological and metabolic factors such as blood pressure, lipid
levels, and diabetes.
38
Results from the present study support
other studies that have found that obesity predicts risk of
cardiovascular disease incidence and mortality beyond the es-
tablished clinical conditions.
27,32,35,37,39
Improvements in the
understanding of adipose tissue as a metabolically active tissue
that secretes various adipokines such as leptin, adiponectin,
resistin, interleukin-6, and tumor necrosis factor- suggest that
further knowledge of less conventional risk factors associated
with insulin resistance, inflammation, and thrombosis is needed
to fully elucidate the mechanisms behind the obesity-associated
cardiovascular risk.
40
This prospective study has its major strengths in its size,
minimal loss to follow-up, and use of validated end-point
data. In the validation of all incident cases of ACS that
occurred during 10 years of follow-up, we used the most
recently suggested definition.
22
Exclusion of the subjects who
had confirmed unstable angina pectoris rendered our results
somewhat stronger, supporting the graded gravity of the
subdiagnoses included in this syndrome.
Conclusions
We found that BMI was strongly associated with ACS in
subgroups of important behavioral and clinical risk factors,
suggesting that prevention of obesity is important even in those
who adhere to an otherwise healthy lifestyle or are free of
clinical symptoms. Our results further indicate that behavioral
lifestyle factors contribute to the risk of ACS in an additive
manner, meaning that increasing physical activity level, abstain-
ing from smoking, and consuming a more heart-healthy diet are
likely to result in a lower risk of ACS even in obese individuals.
Table 4. Incidence Rates,* and HRs With 95% CIs of ACS Among 54 783 Women and Men According to
BMI Combined With Behavioral Lifestyle Risk Factors*
Behavioral Factor Healthy Weight Overweight Obese
Smoking
Not current (never/past) 95 (105) 206 (238) 307 (130)
HR (95% CI) 1 (Referent) 1.52 (1.211.92) 2.35 (1.813.05)
Current, light (114 g/d) 227 (68) 390 (76) 444 (23)
HR (95% CI) 1.71 (1.222.39) 2.30 (1.663.18) 2.61 (1.634.19)
Current, heavy (15 g/d) 365 (161) 617 (233) 766 (93)
HR (95% CI) 2.06 (1.542.78) 2.95 (2.243.90) 3.74 (2.715.15)
Physical activity
1 h/wk 295 (85) 451 (142) 553 (87)
HR (95% CI) 1.43 (1.071.93) 1.95 (1.502.54) 2.74 (2.043.68)
13.49 h/wk 185 (155) 287 (231) 304 (79)
HR (95% CI) 1.27 (0.981.64) 1.64 (1.292.09) 1.92 (1.422.59)
3.5 h/wk 132 (94) 286 (174) 446 (80)
HR (95% CI) 1 (Referent) 1.78 (1.362.26) 2.92 (2.163.94)
Mediterranean diet
Score 02 (lowest adherence) 285 (80) 382 (104) 457 (50)
HR (95% CI) 1.58 (1.182.10) 1.74 (1.332.27) 2.29 (1.643.20)
Score 34 174 (136) 340 (250) 395 (104)
HR (95% CI) 1.02 (0.791.30) 1.67 (1.342.09) 2.03 (1.562.66)
Score 58 (highest adherence) 151 (118) 267 (193) 411 (92)
Hazard ratio (95% CI) 1 (Referent) 1.43 (1.131.79) 2.35 (1.793.10)
Alcohol, g/d
Women, 5; men, 10 254 (120) 373 (175) 430 (93)
HR (95% CI) 1.49 (1.181.89) 1.93 (1.562.39) 2.62 (2.023.38)
Women, 525; men, 1050 160 (166) 297 (292) 407 (117)
HR (95% CI) 1 (Referent) 1.50 (1.241.82) 2.17 (1.712.76)
Women, 25; men, 50 145 (48) 291 (80) 388 (36)
HR (95% CI) 0.87 (0.631.19) 1.32 (1.011.73) 1.65 (1.142.37)
Healthy weight, BMI 25 kg/m
2
; overweight, BMI 25 to 29.9 kg/m
2
; and obesity, BMI 30 kg/m
2
.
*Incidence rates are per 100 000 person-years and are expressed as cases (n). All models included physical activity, smoking,
Mediterranean diet score, alcohol, education (8, 8 to 10, and 10 years), postmenopausal status, and use of hormone replacement
therapy among women (premenopausal, perimenopausal, postmenopausal with no hormone replacement therapy, and postmeno-
pausal with hormone replacement therapy) and were stratified by sex.
Jensen et al Obesity, Lifestyle Risk Factors, and ACS 3067
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Acknowledgment
We would like to thank Professor Thorkild I.A. Srensen for
constructive comments on this manuscript.
Source of Funding
The Diet, Cancer and Health study was funded by the Danish Cancer
Society.
Disclosures
Dr Rimm has funding from Sanofi/Aventis to study the association
between obesity and chronic disease in separate populations. The
remaining authors report no conflicts.
References
1. Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends
in overweight among US children and adolescents, 19992000. JAMA.
2002;288:17281732.
2. Silventoinen K, Sans S, Tolonen H, Monterde D, Kuulasmaa K, Kesteloot
H, Tuomilehto J. Trends in obesity and energy supply in the WHO
MONICA Project. Int J Obes Relat Metab Disord. 2004;28:710718.
3. Obesity: Preventing and Managing the Global Epidemic. Geneva, Swit-
zerland: World Health Organization; 2000. Technical report series.
4. Wilson PW, DAgostino RB, Sullivan L, Parise H, Kannel WB. Over-
weight and obesity as determinants of cardiovascular risk: the Fra-
mingham experience. Arch Intern Med. 2002;162:18671872.
5. Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel
RH. Obesity and cardiovascular disease: pathophysiology, evaluation,
and effect of weight loss: an update of the 1997 American Heart Asso-
ciation Scientific Statement on Obesity and Heart Disease from the
Obesity Committee of the Council on Nutrition, Physical Activity, and
Metabolism. Circulation. 2006;113:898918.
6. Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA,
Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M,
Rudel L, Sacks F, Van HL, Winston M, Wylie-Rosett J. Diet and lifestyle
recommendations revision 2006: a scientific statement from the American
Heart Association Nutrition Committee. Circulation. 2006;114:8296.
7. De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R,
Dallongeville J, Ebrahim S, Faergeman O, Graham I, Mancia G, Cats
VM, Orth-Gomer K, Perk J, Pyorala K, Rodicio JL, Sans S, Sansoy V,
Sechtem U, Silber S, Thomsen T, Wood D. European guidelines on
cardiovascular disease prevention in clinical practice: Third Joint Task
Force of European and Other Societies on Cardiovascular Disease Pre-
vention in Clinical Practice. Atherosclerosis. 2004;173:381391.
8. Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body compo-
sition, and all-cause and cardiovascular disease mortality in men.
Am J Clin Nutr. 1999;69:373380.
9. Wessel TR, Arant CB, Olson MB, Johnson BD, Reis SE, Sharaf BL, Shaw
LJ, Handberg E, Sopko G, Kelsey SF, Pepine CJ, Merz NB. Relationship of
physical fitness vs body mass index with coronary artery disease and car-
diovascular events in women. JAMA. 2004;292:11791187.
10. Li TY, Rana JS, Manson JE, Willett WC, Stampfer MJ, Colditz GA,
Rexrode KM, Hu FB. Obesity as compared with physical activity in
predicting risk of coronary heart disease in women. Circulation. 2006;
113:499506.
11. Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P. Joint
effects of physical activity, body mass index, waist circumference and
waist-to-hip ratio with the risk of cardiovascular disease among
middle-aged Finnish men and women. Eur Heart J. 2004;25:22122219.
12. Stevens J, Cai J, Evenson KR, Thomas R. Fitness and fatness as pre-
dictors of mortality from all causes and from cardiovascular disease in
men and women in the Lipid Research Clinics Study. Am J Epidemiol.
2002;156:832841.
13. Vatten LJ, Nilsen TI, Romundstad PR, Droyvold WB, Holmen J. Adi-
posity and physical activity as predictors of cardiovascular mortality. Eur
J Cardiovasc Prev Rehabil. 2006;13:909915.
14. Tjonneland A, Olsen A, Engholm G, Overvad K. Study design, exposure
variables, and socioeconomic determinants of participation in Diet,
Cancer and Health: a population-based prospective cohort study of 57 053
men and women in Denmark. Scand J Pub Health. 2007;35:432441.
15. Tjonneland A, Overvad K, Haraldsdottir J, Bang S, Ewertz M, Jensen
OM. Validation of a semiquantitative food frequency questionnaire
developed in Denmark. Int J Epidemiol. 1991;20:906912.
16. Tjonneland A, Haraldsdottir J, Overvad K, Stripp C, Ewertz M, Jensen
OM. Influence of individually estimated portion size data on the validity
of a semiquantitative food frequency questionnaire. Int J Epidemiol.
1992;21:770777.
17. FoodCalc. Available at: http://www.ibt.ku.dk/jesper/foodcalc/. Accessed
December 5, 2007.
18. Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a
Mediterranean diet and survival in a Greek population. N Engl J Med.
2003;348:25992608.
19. Trichopoulou A, Orfanos P, Norat T, Bueno-de-Mesquita B, Ocke MC,
Peeters PH, van der Schouw YT, Boeing H, Hoffmann K, Boffetta P,
Table 5. Incidence Rates* and HRs With 95% CIs of ACS Among 54 784 Women and Men
According to BMI Combined With Clinical Risk Factors*
Behavioral Factor Healthy Weight Overweight Obese
Hypertension
Normotensive 156 (250) 286 (392) 321 (126)
HR (95% CI) 1 (Referent) 1.51 (1.291.78) 1.77 (1.422.20)
Hypertensive 349 (84) 431 (155) 587 (120)
HR (95% CI) 2.16 (1.682.76) 2.25 (1.842.75) 3.39 (2.724.23)
Diabetes type 2
Nondiabetic 176 (308) 305 (492) 389 (206)
HR (95% CI) 1 (Referent) 1.42 (1.231.65) 1.94 (1.622.32)
Diabetic 650 (15) 700 (21) 866 (24)
HR (95% CI) 2.57 (1.534.32) 2.47 (1.583.85) 3.50 (2.305.31)
Hypercholesterolemia
Normocholesterolemic 152 (217) 277 (343) 348 (144)
HR (95% CI) 1 (Referent) 1.49 (1.251.77) 1.94 (1.572.41)
Hypercholesterolemic 285 (117) 418 (203) 553 (100)
HR (95% CI) 1.75 (1.402.20) 2.18 (1.802.64) 3.23 (2.544.10)
Healthy weight, BMI 25 kg/m
2
; overweight, BMI 25 to 29.9 kg/m
2
; and obesity, BMI 30 kg/m
2
.
*Incidence rates are per 100 000 person-years and are expressed as cases (n). All models included physical
activity, smoking, Mediterranean diet score, alcohol, education (8, 8 to 10, and 10 years), postmenopausal status,
and use of hormone replacement therapy among women (premenopausal, perimenopausal, and postmenopausal with
no hormone replacement therapy, and postmenopausal with hormone replacement therapy) and were stratified by sex.
3068 Circulation June 17, 2008
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Nagel G, Masala G, Krogh V, Panico S, Tumino R, Vineis P, Bamia C,
Naska A, Benetou V, Ferrari P, Slimani N, Pera G, Martinez-Garcia C,
Navarro C, Rodriguez-Barranco M, Dorronsoro M, Spencer EA, Key TJ,
Bingham S, Khaw KT, Kesse E, Clavel-Chapelon F, Boutron-Ruault MC,
Berglund G, Wirfalt E, Hallmans G, Johansson I, Tjonneland A, Olsen A,
Overvad K, Hundborg HH, Riboli E, Trichopoulos D. Modified Medi-
terranean diet and survival: EPIC: Elderly Prospective Cohort Study.
BMJ. 2005;330:991997.
20. Pedersen CB, Goetzche H, Moeller J, Mortensen PB. The Danish Civil
Registration System: a cohort of eight million persons. Dan Med Bull.
2006;53:441449.
21. Andersen TF, Madsen M, Jorgensen J, Mellemkjoer L, Olsen JH. The
Danish National Hospital Register: a valuable source of data for modern
health sciences. Dan Med Bull. 1999;46:263268.
22. Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D,
Goldberg RJ, Hand MM, Jaffe AS, Julian DG, Levy D, Manolio T,
Mendis S, Mensah G, Pajak A, Prineas RJ, Reddy KS, Roger VL,
Rosamond WD, Shahar E, Sharrett AR, Sorlie P, Tunstall-Pedoe H. Case
definitions for acute coronary heart disease in epidemiology and clinical
research studies: a statement from the AHA Council on Epidemiology
and Prevention; AHA Statistics Committee; World Heart Federation
Council on Epidemiology and Prevention; the European Society of Car-
diology Working Group on Epidemiology and Prevention; Centers for
Disease Control and Prevention; and the National Heart, Lung, and Blood
Institute. Circulation. 2003;108:25432549.
22a. Joensen AM, Jensen MK, Overvad K, Dethlefsen C, Schmidt EB, Ras-
mussen LH, Tjonneland A, Johnsen SP. Predictive values of acute
coronary syndrome discharge diagnoses differ in the Danish National
Patient Registry. J Clin Epidemiol. In press.
23. Madsen M, Davidsen M, Rasmussen S, Abildstrom SZ, Osler M. The
validity of the diagnosis of acute myocardial infarction in routine sta-
tistics: a comparison of mortality and hospital discharge data with the
Danish MONICA registry. J Clin Epidemiol. 2003;56:124130.
24. Cox DR. Regression models and life-tables [with discussion]. J Royal
Stat Soc (B). 1972;34:187220.
25. Wei M, Kampert JB, Barlow CE, Nichaman MZ, Gibbons LW, Paffen-
barger RS Jr, Blair SN. Relationship between low cardiorespiratory
fitness and mortality in normal-weight, overweight, and obese men.
JAMA. 1999;282:15471553.
26. Rico-Sanz J, Rankinen T, Rice T, Leon AS, Skinner JS, Wilmore JH, Rao
DC, Bouchard C. Quantitative trait loci for maximal exercise capacity
phenotypes and their responses to training in the HERITAGE Family
Study. Physiol Genomics. 2004;16:256260.
27. Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson
RR, Speizer FE, Hennekens CH. A prospective study of obesity and
risk of coronary heart disease in women. N Engl J Med. 1990;322:
882889.
28. Jonsson S, Hedblad B, Engstrom G, Nilsson P, Berglund G, Janzon L.
Influence of obesity on cardiovascular risk: twenty-three-year follow-up
of 22,025 men from an urban Swedish population. Int J Obes Relat Metab
Disord. 2002;26:10461053.
29. Rexrode KM, Buring JE, Manson JE. Abdominal and total adiposity and
risk of coronary heart disease in men. Int J Obes Relat Metab Disord.
2001;25:10471056.
30. Molarius A, Seidell JC. Selection of anthropometric indicators for clas-
sification of abdominal fatness: a critical review. Int J Obes Relat Metab
Disord. 1998;22:719727.
31. Niedhammer I, Bugel I, Bonenfant S, Goldberg M, Leclerc A. Validity of
self-reported weight and height in the French GAZEL cohort. Int J Obes
Relat Metab Disord. 2000;24:11111118.
32. Yan LL, Daviglus ML, Liu K, Stamler J, Wang R, Pirzada A, Garside DB,
Dyer AR, Van HL, Liao Y, Fries JF, Greenland P. Midlife body mass index
and hospitalization and mortality in older age. JAMA. 2006;295:190198.
33. Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease.
J Clin Endocrinol Metab. 2004;89:25952600.
34. Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ,
Rogers WJ, Reis SE. Clinical importance of obesity versus the metabolic
syndrome in cardiovascular risk in women: a report from the Womens
Ischemia Syndrome Evaluation (WISE) study. Circulation. 2004;109:
706713.
35. Cassidy AE, Bielak LF, Zhou Y, Sheedy PF, Turner ST, Breen JF, Araoz
PA, Kullo IJ, Lin X, Peyser PA. Progression of subclinical coronary
atherosclerosis: does obesity make a difference? Circulation. 2005;111:
18771882.
36. Kannel WB, Wilson PW, Nam BH, DAgostino RB. Risk stratification of
obesity as a coronary risk factor. Am J Cardiol. 2002;90:697701.
37. Bogers RP, Bemelmans WJ, Hoogenveen RT, Boshuizen HC, Woodward
M, Knekt P, van Dam RM, Hu FB, Visscher TL, Menotti A, Thorpe RJ Jr,
Jamrozik K, Calling S, Strand BH, Shipley MJ. Association of overweight
with increased risk of coronary heart disease partly independent of blood
pressure and cholesterol levels: a meta-analysis of 21 cohort studies including
more than 300 000 persons. Arch Intern Med. 2007;167:17201728.
38. Wilson PW, DAgostino RB, Levy D, Belanger AM, Silbershatz H,
Kannel WB. Prediction of coronary heart disease using risk factor cate-
gories. Circulation. 1998;97:18371847.
39. Dyer AR, Stamler J, Garside DB, Greenland P. Long-term consequences of
body mass index for cardiovascular mortality: the Chicago Heart Association
Detection Project in Industry study. Ann Epidemiol. 2004;14:101108.
40. Van Gaal LF, Mertens IL, De Block CE. Mechanisms linking obesity
with cardiovascular disease. Nature. 2006;444:875880.
CLINICAL PERSPECTIVE
Obesity is an important modifiable risk factor for coronary heart disease. However, it is clear that achieving weight loss
or preventing weight gain with aging is difficult for most individuals. Whether the high cardiovascular risk associated with
obesity is alleviated by physical activity remains controversial; furthermore, little is known about the cardiovascular risk
associated with obesity in the context of other behavioral lifestyle factors. In our investigation of the associations of obesity
in combination with potentially modifiable behavioral lifestyle factors among 54 783 middle-aged men and women, we
found that obesity was strongly associated with the risk of acute coronary syndrome among the physically active and
inactive, in nonsmokers and smokers, among those who adhered to a more or less heart-healthy dietary pattern, and in
participants with and without a moderate alcohol intake. Body mass index also was associated with acute coronary
syndrome in subgroups of important clinical risk factors, suggesting that prevention of obesity is important even in those
who adhere to an otherwise healthy lifestyle or who are free of clinical symptoms. Our results further indicated that
increasing physical activity level, abstaining from smoking, consuming a more heart-healthy diet, and having a moderate
alcohol intake likely result in a lower risk of acute coronary syndrome even in obese individuals.
Jensen et al Obesity, Lifestyle Risk Factors, and ACS 3069
at BRISTOL ROYAL INFIRMARY on July 4, 2008 circ.ahajournals.org Downloaded from
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Influence of Complication Events On The Empowerment Selfcare of Diabetes Mellitus PatientsDokumen5 halamanThe Influence of Complication Events On The Empowerment Selfcare of Diabetes Mellitus PatientsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Orchitis: Dr. Egi Edward Manuputty, Sp.UDokumen26 halamanOrchitis: Dr. Egi Edward Manuputty, Sp.Uvanadiel4Belum ada peringkat
- Who Pneu Im Pgi ProtocolDokumen2 halamanWho Pneu Im Pgi ProtocolRoxanneGailBigcasGoleroBelum ada peringkat
- Body Dysmorphic Disorder: SymptomsDokumen7 halamanBody Dysmorphic Disorder: SymptomsamiraBelum ada peringkat
- Management of Nursing PersonnelDokumen3 halamanManagement of Nursing PersonnelsomyachughBelum ada peringkat
- WaterleafDokumen2 halamanWaterleafGILBERTBelum ada peringkat
- Dieta DiverticulosisDokumen8 halamanDieta DiverticulosisvicenteBelum ada peringkat
- MCQs ThyroidtDokumen14 halamanMCQs ThyroidtAhmed Attia100% (5)
- Al HijamahTherapyDokumen6 halamanAl HijamahTherapyNarendra DadhichBelum ada peringkat
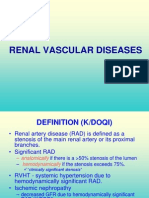
- Curs 02 Renal Vascular DiseasesDokumen56 halamanCurs 02 Renal Vascular DiseasesMadalina SercaianuBelum ada peringkat
- Diuretics How They Work Cautions and ContraindicationsDokumen5 halamanDiuretics How They Work Cautions and ContraindicationsCatalina Paz DiazBelum ada peringkat
- Menopause Related Symptoms and Their Correlates: A Community Based Cross Sectional Study in Kollam District, KeralaDokumen129 halamanMenopause Related Symptoms and Their Correlates: A Community Based Cross Sectional Study in Kollam District, Keraladhaya georgeBelum ada peringkat
- Nursing CS Acute-Kidney-Injury 04Dokumen1 halamanNursing CS Acute-Kidney-Injury 04Mahdia akterBelum ada peringkat
- Community-Acquired Pneumonia in Adults - Rapid Evidence ReviewDokumen6 halamanCommunity-Acquired Pneumonia in Adults - Rapid Evidence ReviewpachomdBelum ada peringkat
- Prevent Platelet Plugs.: Never IMDokumen1 halamanPrevent Platelet Plugs.: Never IMdekspeerBelum ada peringkat
- Acute Iron Poisoning - PharmacologyDokumen10 halamanAcute Iron Poisoning - PharmacologyAmmaarah IsaacsBelum ada peringkat
- ASS - History Taking and Physical ExaminationDokumen142 halamanASS - History Taking and Physical ExaminationTrixDelaCruz100% (3)
- Case Study (Typhoid Fever)Dokumen2 halamanCase Study (Typhoid Fever)lance rowyBelum ada peringkat
- Medicinal Plants HistoryDokumen21 halamanMedicinal Plants HistorybpypathalaBelum ada peringkat
- Sample Family Care Study (N107)Dokumen51 halamanSample Family Care Study (N107)Dan Dan Soi T97% (31)
- Cue and Clue Problem List and Initial Diagnosis PlanningDokumen3 halamanCue and Clue Problem List and Initial Diagnosis PlanningWilujeng AnggrainiBelum ada peringkat
- Hyper+&+Hypothyroid+ +patho,+s S+causes+Dokumen1 halamanHyper+&+Hypothyroid+ +patho,+s S+causes+Bianca WelchBelum ada peringkat
- Career Point:, CP Tower, IPIA, Road No.1, Kota (Raj.), PH: 0744-3040000 Immunity and DiseaseDokumen25 halamanCareer Point:, CP Tower, IPIA, Road No.1, Kota (Raj.), PH: 0744-3040000 Immunity and DiseaseSonika AlohiyaBelum ada peringkat
- Bipolar DisordersDokumen63 halamanBipolar DisorderselvinegunawanBelum ada peringkat
- Acute and Chronic InflammationDokumen36 halamanAcute and Chronic Inflammationibnbasheer89% (18)
- PD - Examination of The EyeDokumen8 halamanPD - Examination of The EyeJohn TecsonBelum ada peringkat
- Body LiceDokumen2 halamanBody LiceCeline BrantegemBelum ada peringkat
- Path 122 Week STUDENT 5 & 6 Respiratory DisordersDokumen107 halamanPath 122 Week STUDENT 5 & 6 Respiratory DisordersGwendolaine PicaBelum ada peringkat
- Cardiomyopathy Dilated CardiomyopathyDokumen5 halamanCardiomyopathy Dilated Cardiomyopathym3d1k100% (1)
- Index Case Presentation: TuberculosisDokumen14 halamanIndex Case Presentation: Tuberculosisnandini singhBelum ada peringkat