First Aid
Diunggah oleh
Jasier SahagunDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
First Aid
Diunggah oleh
Jasier SahagunHak Cipta:
Format Tersedia
ST.
ANDREWS SCHOOL
La Huerta, ParaaqueCity
INTRODUCTION TO FIRST AID
First Aid is the immediate care given to a person who has been injured or suddenly ill. It includes self help and
home care if medical assistance is not available or encouragement, evidence of willingness to help, and promotion of
confidence by demonstration of competence.
ROLES AND RESPONSIBILITIES OF THE FIRST AIDER
1. Bridge that fills the gap between the victim and the physician. It is not intended to compete with, nor
take the place of the services of the physician. It ends when the services of a physician begin.
2. Ensure safety of him/herself and that of bystanders.
3. Gain access to the victim.
4. Determine any threats to patients life.
5. Summon advanced medical care as needed.
6. Provide needed care for the patient.
7. Record all finding and care given to the patient.
OBJECTIVE OF FIRST AID
1. To alleviate suffering.
2. To prevent added/ further injury of danger.
3. To prolong life.
CHARACTERISTICS OF A GOOD FIRST AIDER
GENTLE should not cause pain
RESOURCEFUL should make the best use of things at hand
OBSERVANT should notice all signs
TACTFUL should not alarm the victim
EMPHATIC should be comforting
RESPECTABLE should maintain a professional & caring attitude
HINDRANCES IN GIVING FIRST AID
1. Unfavorable surroundings
2. The presence of crowds
3. Pressure from victim or relatives
TRANSMISSION OF DISEASES AND THE FIRST AIDERS
1. Direct Contact occurs when a person touches an infected persons body fluids
2. Indirect Contact occurs when a person touches objects that have been contaminated by the blood or
another body fluid of an infected person
3. Airborne occurs when a person inhales infected droplets that have become airborne as an infected
person coughs or sneezes.
4. Vector occurs when an animal such as a dog or an insect, such as mosquito, transmits a pathogen into
the body through a bite.
BODY SUBSTANCE ISOLATION (BSI) are precautions taken to isolate or prevent risk of exposure from any other
type of bodily substance.
BASIC PRECAUTIONS AND PRACTICES
1. Personal hygiene maintaining these habits, such as frequent hand washing and proper grooming, are
two important ways to prevent disease transmission regardless of any personal protective equipment
you might use
2. Protective equipment these are equipment and supplies that prevent you from making direct contact
with infected materials.
3. Equipment cleaning and disinfecting this will prevent infection or contamination of equipment and
supplies from spreading.
FIRST AID EQUIPMENT AND SUPPLIES
Basic Equipment
a. Alcohol
b. Povidone Iodine
c. Cotton
d. Gauze pads
e. Tongue depressor
f. Penlight
g. Band aid
h. Gloves
i. Scissors
j. Forceps
k. Triangular bandage
l. Elastic bandage
m. Occlusive dressing
n. Plaster
o. Dressing any sterile cloth material used to cover
the wound
p. Bandage any clean cloth material sterile or not
use to hold the dressing in place
GUIDELINES IN GIVING EMERGENCY CARE
Getting started
1. Planning of Action
2. Gathering of needed materials
3. Remember the initial response:
A Ask for help
I Intervene
D Don no further harm
4. Instruction to helper/s
EMERGENCY ACTION PRINCIPLES
1. Survey the scene
Is the scene safe?
What happened?
How many people are injured?
Are there bystanders who can help?
Identify yourself as a trained first aider
Get CONSENT to give care
2. Do a primary survey of the victim
Check responsiveness (if unresponsive, consent is implied)
Protect spine if necessary
Check ABC, Airway, Breathing, and Circulation
3. Activate Medical Assistance
Depending on the situation
Phone first or phone fast
A bystander should make the telephone call for help
A bystander will be requested to call for a physician
Somebody will be asked to arrange for transfer facility
Information to be remembered
What happened
Location
Number of persons injured
Extent of injury and first aid given
The telephone number from where are you calling
Person who activated medical assistance must be identified and drop the
phone last
4. Do a secondary survey of the victim
Interview the victim (name, what happened, history)
Check for vital signs (pulse rate, respiratory rate, temperature, blood pressure)
Check for skin appearance
Do a Head to Toe examination looking for DCAP BTLS (Deformity, Contusion,
Abrasion, Puncture, Burn, Tenderness, Laceration, Swelling)
SAMPLE (Signs& symptoms, Allergies, Medications, Past medical history, Last oral
taken, Event prior the incident)
SOFT TISSUE INJURIES
Wound is a break in the continuity of a tissue of the body either internal or external.
CLASSIFICATION OF WOUND
1. Closed Wound
Injuries sustained from a blow with a blunt object collision rupturing blood vessels internally without
penetrating the skin. It involves the underlying tissue without a break in the skin or in the mucous
membrane.
Signs and symptoms:
Pain and tenderness
Swelling
Discoloration
Hematoma
Uncontrolled restlessness
Thirst
Symptoms of shock
Vomiting or cough up blood
Passage of blood in the urine or feces
Sign of blood along mouth, nose and ear canal
First Aid Management
a. Compression
b. Elevation
2. Open Wound
Injuries sustained from a blow with a sharp object causing the skin to be torn. A break in the skin or in
the mucous membrane.
Classification:
WOUND CAUSES CHARACTERISTICS DANGER
PUNCTURE
Penetrating pointed
instrument such as
nails, ice picks,
daggers, etc.
Deep and narrow,
serious or slight
bleeding
Hemorrhage
Infection
ABRASION
Scrapping or rubbing
against rough
surfaces
Shallow, wide, oozing
of blood, dirty
Infection
LACERATION
Blunt instruments
such as sharpnels,
rocks, broken glasses
Torn with irregular
edges, serious or slight
bleeding
Hemorrhage
Infection
AVULSION
Explosion, Animal
bites, mishandling of
tools, etc.
Tissue forcefully
separated from the
body.
Hemorrhage
Infection
INCISION
Sharp bladed
instruments such as
blades, razors, etc.
Clean cut, deep, severe
bleeding, wound is
clean
Hemorrhage
Infection
First Aid Management
Wound with Severe Bleeding
Control Bleeding
Cover the wound with dressing and secure with a bandage
Care of shock
Consult or refer to physician
Wound with bleeding not severe (home care)
Clean the wound with soap and water
Apply mild antiseptics
Cover wound with dressing and bandage
REMINDERS:
1. All wounds must be thoroughly inspected and covered with a dry dressing to control bleeding and
prevent further contamination.
2. Once bleeding is controlled by compression, the limb should be splinted to further control bleeding,
stabilize the injured part, minimize the victims pain and facilitate the patients transport to the hospital.
3. As with closed soft tissue injuries, the injured art should be elevated to just above the level of the
victims heart to minimize severity.
4. Amputated body parts should be saved, wrapped in a dry gauze, placed in a plastic bag, kept cool and
transported with the patient.
5. Dont induce further bleeding to clean the wound.
6. Dont use absorbent cotton as a dressing.
DANGER SIGNAL OF WOUNDS:
HEMORRHAGE occurs when there is a rupture in one or more blood vessel. Generally, small cuts, only
capillaries are injured. Deeper wounds as in lacerations results in injury of veins and arteries. Bleeding which is
severe enough to endanger life seldom occurs except when arteries or veins are cut or damaged.
INFECTION whenever we suffer a cut, germs are sure to enter the wound, being carried in with the
object that cuts us or being pushed in from our clothes or skin. If the germs grow in the wound and harm us, an
infection of the wound is present.
SHOCK is a depressed condition of many body functions due to failure of enough blood to circulate
throughout the body following serious injury.
First Aid management to Shock:
Proper body position
Proper body heat
Proper transfer
Dislocation is a displacement of a bone end from the joint end. A bone comes out of place at a joint, tearing the
surrounding tissues to some extent.
Fracture is a break or crack in the bone
Kind of Fracture
1. Simple or Closed Fracture bone is broken but there is no connecting wound from the break area to skin.
Signs and Symptoms:
Bleeding
Swelling
Discoloration or deformity
Pain upon moving the area above the injured part
2. Compound or Open Fracture bone is broken and there is an open wound in the skin surface.
Signs and Symptoms:
Presence of signs and symptoms of simple fracture
Wounds through the skin
Bone may or may not protrude
First Aid Management for Fracture
a. PRICEM Protect, Rest, Ice, Compression, Elevation, and Medication
b. Stop bleeding
c. Immobilize the injured area
d. Care for shock
e. Transport properly
f. Referral to physician
Strain are injuries to muscles because of over stretching or tearing. Fibers are stretched and partially torn
First Aid Management:
Apply cold compresses at once
Elevate the limb to reduce swelling and bleeding within the muscle. Rest the pulled muscle for 24 hours.
Get medical help
Sprain stretching or tearing of tissues or ligaments around a joint. A temporary dislocation of joints, especially the
wrist and the ankle
First Aid Management:
Apply cold compresses at once
Remove any clothing or jewelry from around the joint
Elevate affected joint with pillow or clothing
The victims physician may recommend an over the counter analgesic/ anti inflammatory appropriate
for the victims general health
Cramps are usually caused by fatigue or even exertion of the affected muscles that suddenly contract into a tight hard
inset, which incapacitates or greatly inhibit the movement of the muscles.
First Aid Management:
Have the victim stretch out the affected muscle to counteract the cramp
Massage the cramped muscle firmly but gently
Apply heat. Moist heat more effective than dry heat
Get medical help if cramps persist
Splints are devices applied to arms, legs or trunk to immobilize an injured part when a fracture is suspected.
BURNS is an injury involving the skin, including muscles, bones, nerves and blood vessels. This results from heat,
chemicals, electricity or solar or other forms of radiation.
Common Causes
a. Carelessness with match and cigarette smoking
b. Scald from hot liquid
c. Defective heating, cooking and electrical equipment
d. Immersion in overheated bath water
e. Use of such chemicals, as lye, strong acids and strong detergents
FACTORS TO DETERMINE THE SERIOUSNESS OF THERMAL BURNS
1. The DEPTH. The deeper the burn, the more severe it is. Three depth classifications are used:
a. Superficial (First Degree) mild pain, redness, swelling, no scarring
b. Partial Thickness (Second Degree) severe pain, redness, swelling, blister formation, peeling of the
skin
c. Full Thickness (Third Degree) all layers are involve, not painful
2. The EXTENT to the affected BODY SURFACE AREA. This means estimating how much body surface area the
burns covers.
3. LOCATION of the Burns. Burns on the face, hands feet, and genitals are more severe than the other boy
parts.
4. Victims age and Medical condition. Determine if other injuries or pre-existing medical problems exist or if
the victim is elderly (over 55) or very young (under 5).
TYPES OF BURN INJURIES
1. THERMAL BURNS not all thermal burns are caused by flames. Contact with hot objects, flammable vapor
that ignites and causes a flash or an explosion, and steams or hot liquid are other common causes of burns.
Care for Thermal Burns:
Care for FIRST DEGREE and SECOND DEGREE Burns
Relieve pain by immersing the burned area in cold water or by applying a wet, cold cloth. If
cold water is unavailable, use any cold liquid you drink to reduce the burned skins
temperature.
Cover the burn with a dry, non sticking, sterile dressing or a clean cloth.
Care for THIRD DEGREE Burns
Cover with a dry, non sticking, sterile dressing or a clean cloth
Treat the victim for shock by elevating the legs and giving the victim warm with a lean sheet
or blanket
2. CHEMICAL BURNS chemicals will continue to cause tissue destruction until the chemical agent is removed.
Care for Chemical Burns:
Immediately remove the chemical by flushing with water
Remove the victims contaminated clothing while flushing with water
Flush for 20 minutes or longer. Let the victim wash with a mild soap before a final rinse.
Cover the burned area with a dry dressing or, for large areas, a clean pillowcase
If the chemical is in the eye, flood it for at least 20 minutes, using low pressure
Seek medical attention immediately for all chemical burns.
3. ELECTRICAL BURNS the injury severity from exposure to electrical current depends on the type of current
(direct or altering), the voltage, the area of the body exposed, and the duration of contact.
Care for Electrical Burns:
Unplug, disconnect, or turn off the power. If that is impossible, call the power company or
ask for help
Check the ABCs. Provide Rescue Breathing or Cardiopulmonary Resuscitation if necessary.
If the victim fell, check for spine injury
Treat the victim for shock
Seek medical attention immediately. Electrical injuries are treated in burn center
TRIAGING
- A process used in sorting victims into categories of priority for care and transport based on the severity of
injuries and medical emergencies.
- Categories of PRIORITY of Treatment
1. Casualties requiring minimum treatment
2. Casualties requiring immediate care
3. Casualties whose treatment maybe delayed
4. Expectant treatment for critically injured who are not expected to survive
- Priority Triage
1. FIRST PRIORITY Class I, RED in color difficulty of breathing/severe bleeding
E.g. Respiratory arrest, life threatening injuries, Spine Fracture, Heart Attack
2. SECOND PRIORITY Class II, YELLOW in color burn, bone & joint injury
E.g. Severe burns, Moderate Bleeding, Multiple Fracture, Stable Drug Overdose
3. THIRD PRIORITY Class III, GREEN in color conscious
E.g. Minor bleeding, Minor fracture, soft tissue injuries and other minor injuries
4. FOURTH PRIORITY Class IV, BLACK in color, DECEASED, little chance to survive
Dead victims should not be placed at the collecting station near the injured. A location at a
reasonable distance or a place should be designated as a morgue.
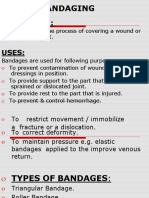
BANDAGING is the art and technique of applying bandages to wounds, fractures and dislocation
Bandage any clean cloth material, sterile or not, used to hold dressing in place.
Uses of Bandage
To control bleeding
Tie splints in place
Immobilize the body part
Supports body parts
Principles of Bandaging
Speed
Careful handling
Accuracy
Neatness
Triangular bandage is useful because it can be folded in a variety of ways to fit almost any part of the body. Usually
made from cloths as bleached muslin 40x40.
GUIDELINES IN USING DRESSING AND BANDAGES
1. Use a dressing that is large enough to extend at least 1 inch beyond the edges of the wound
2. If body tissue or organs are exposed, cover the wound with a dressing that will not stick, such as plastic wrap
or moistened gauze. Then secure the dressing with a bandage or adhesive tapes
3. If the bandage is over a joint, splint and make a bulky dressing so the joint remains immobilized. If there is
no movement of a wound over the joint, there should be improved healing and reduced scarring.
4. A bandage should fit snugly but should not cut off circulation or cause the victim discomfort. If the area
beyond the wound changes color, begin to tingle or feel cold, or if the wound starts to swell, the bandage is
too tight and should be loosened.
BANDAGING TECHNIQUE
Open phase
1. Heap (topside)
2. Face; back of the head
3. Chest; back of chest
4. Hand; foot
5. Arm sling; underarm sling
Cravat phase
1. Forehead; eye
2. Ear; cheek; jaw
3. Shoulder; hip
4. Arm; leg
5. Elbow; knee (straight; bent)
6. Palm pressure bandage
7. Palm bandage of open hand
8. Shoe on; shoe off
BASIC LIFE SUPPORT AND EMERGENCY RESPONSE
BASIC LIFE SUPPORT
An emergency procedure that consists of recognizing respiratory or cardiac arrest or both and the proper
application of Cardiopulmonary Resuscitation to maintain life until a victim recovers or advanced life support is
available. It is the recognition and immediate treatment of airway obstruction, respiratory arrest, and cardiac arrest.
This includes the ABC of BLS:
A Airway open through
1. Head tilt Chin Lift maneuver
2. Jaw thrust maneuver for victim with suspected neck or back injuries
B Breathing restored Artificial Respiration
C Circulation restored by External Chest Compression
ADVANCED CARDIAC LIFE SUPPORT
The use of special equipment to maintain breathing and circulation for the victim of a cardiac emergency.
PROLONGED LIFE SUPPORT
For post resuscitative and long term resuscitation.
CHAIN OF SURVIVAL
1. The FIRST LINK: EARLY ACCESS
It is the event initiated after the patients collapse until the arrival of Emergency Medical Services
personnel prepared to provide care.
2. The SECOND LINK: EARLY CARDIO PULMONARY RESUCITATION
If started immediately after the victims collapse, the probability of survival approximately doubles when
it is initiated before the arrival of EMS.
3. The THIRD LINK: EARLY DEFIBRILLATION
It is most likely to improve survival. It is the key intervention to increase the chances of survival of
patients with out of hospital cardiac arrest.
4. The FOURTH LINK: EARLY ACLS
If provided by highly trained personnel like paramedics, provision of advanced care outside the hospital
would be possible.
RESPIRATORY ARREST
Stoppage of breathing but circulation and pulse continue for sometimes.
Causes:
Drowning
Suffocation
Poisoning
Drug Overdose
Electrical Shock
Strangulation
Heart Attack/ stroke
Choking
RESCUE BREATHING is a technique of breathing air into a persons lungs to supply him or her with the oxygen needed
to survive.
Ways to ventilate the lungs
a. Mouth Mouth is a quick effective way to provide oxygen and ventilation to the victim.
b. Mouth Nose is recommended when it is impossible to ventilate through the victims mouth, the
mouth cannot be opened (trismus), the mouth is seriously injured, or a tight mouth to mouth seal is
difficult to achieve.
c. Mouth to mouth & nose if the victim is an infant (1 year old), this is the best way in delivering
ventilation by placing your mouth over the infants mouth and nose to create a seal.
d. Mouth to Stoma it is used if the patient has a stoma: a permanent opening that connects the trachea
directly to the front of the neck. These patients breathe only through stoma
e. Mouth to face shield it could provide very low resistance ventilations to a patient by using a thin and
flexible plastic.
f. Mouth to Mask it could deliver ventilation to a patient by using a pocket facemask with a one way
valve to form a seal around the patients nose and mouth.
g. Bag to mask device it could deliver ventilation to a patient by using a hand operated device
consisting of a self inflating bag, one way valve, facemask, and oxygen reservoir.
ASSESSMENT / PROCEDURE IN RESCUE BREATHING
1. Check for consciousness
(Hey, hey, hey, are you okay?)
2. Unresponsive
3. Activate Medical Assistance
4. Prepare for victim transfer to a safe place then position the victim in flat lying (if necessary)
5. Open the airway (head tilt chin lift)
6. Look, Listen and Feel (count for 5 seconds 1001, 1002,. 1005)
7. If breathless
8. Give two (2) full breath
9. Feel the carotid pulse ( count for 5 seconds)
10. Still breathless, but with pulse give RESCUE BREATHING (please refer to the table below)
11. After giving Rescue Breaths for one minute, check again for pulse or do the assessment
12. If the victim is still breathless but with pulse, continue Rescue Breaths If the victim has pulse and is now
breathing, the victim is alive. Place the victim in the recovery position (Lateral Left)
TABLE OF COMPARISON ON RESCUE BREATHING FOR ADULT, CHILD. AND INFANT
ADULT CHILD INFANT
Opening of airway (Head
tilt Chin - Lift)
Maximum tilt of the head Neutral position Neutral position
Location for checking of
pulse
Carotid pulse (side of the neck) Carotid pulse
Brachial pulse (inner
aspect of upper arm)
Method Mouth to mouth or mouth to nose
Mouth to mouth or
mouth to nose
Mouth to mouth and
nose
Breaths
Normal Breath (approx.. 1 second/
breath enough to make the chest
rise)
Normal, regulated breath (1 to 1.5
seconds/breath)
Rate
20 to 24 breaths (breath every 4 to 5
seconds for 2 minutes)
40 breaths (1 breath every 3 seconds for 2
minutes)
Counting for
standardization purpose:
Mnemonic of 1 breathe
every 5/3 seconds
Breath 1, 1002, 1003, 1001
Breath 1, 1002, 1003, 1002
Breath 1, 1002, 1003, 1003
Breath 1, 1002, 1003, 1010 or up to
1024, long breath
Breath 1, 1001
Breath 1, 1002
Breath 1, 1003
Or up to 1040, long breath
FOREIGN BODY AIRWAY OBSTRUCTION MANAGEMENT
Causes:
1. Improper chewing of large pieces of food
2. Excessive intake of alcohol
3. The presence of loose upper and lower dentures
4. For children running while eating
5. For smaller children of hand to mouth stage left unattended
TYPES OF OBSTRUCTION
1. ANATOMICAL when tongue drops back and obstructs the throat. Other causes are acute asthma, croup,
diphtheria, swelling, and cough.
2. MECHANICAL when foreign objects lodged in the pharynx or airways; fluids accumulate in the back of the
throat.
CLASSIFICATION OF OBSTRUCTION
1. PARTIAL OBSTRUCTION WITH GOOD AIR EXCHANGE partial obstruction and that the victim can still cough and
answer the question are you choking
2. PARTIAL OBSTRUCTION WITH POOR AIR EXCHANGE poor air exchange and increased breathing difficulty a
silent cough, cyanosis or inability to speak or breath.
3. TOTAL OBSTRUCTION the patient becomes unconscious due to complete or total blockage.
ASSESSMENT INDICATING CHOKING
Weak ineffective cough
High pitched noises on inspiration respiratory distress
Inability to speak or breath
Cyanotic
Patient clutches the neck between thumb and fingers (universal distress signal)
HEIMLICH MANEUVER is a technique recommended for relieving foreign body airway obstruction
Abdominal thrust
Chest thrust
CARDIAC ARREST
Circulation ceases and vital organs are deprived of oxygen
Causes:
Coronary heart disease
Dysrhythmia
Respiratory Arrest
Electrocution
Drowning
Choking
Trauma
Idiopathic (Unknown cause)
THREE CONDITIONS OF CARDIAC ARREST
1. Cardiovascular collapse: the heart is still beating but its action is so weak that blood is not being circulated
through the vascular system to the brain and body tissues.
2. Ventricular Fibrillation: occurs when the individual fascicles of the heart beat independently rather than the
coordinated, synchronized manner that produce rhythmic heart beat.
3. Cardiac Standstill: It means that the heart has stopped beating.
CARDIO PULMONARY RESUSCITATION
This is a combination of chest compressions and rescue breathing. This must be combined for effective
resuscitation of the victim of cardiac arrest.
COMPRESSION ONLY CPR
If a person is unwilling or unable to perform mouth to mouth ventilation for an adult victim, chest
compression only CPR should be provided rather than no attempt of CPR being made.
Chest compression only CPR is recommended only in the following circumstances:
1. When a rescuer is unwilling or unable to perform mouth to mouth rescue breathing, or
2. For use in dispatcher assisted CPR instructions where the simplicity of this modified technique allow
untrained bystanders to rapidly intervene.
CRITERIA FOR NOT STARTING CPR
All patients in cardiac arrest receive resuscitation unless:
The patient has a valid DO NOT ATTEMPT RESUSCITATION (DNAR) order.
The patient has signs of irreversible death; rigor mortis, decapitation or dependent lividity.
No physiological benefit can be expected because the vital functions have deteriorated despite maximal
therapy for such conditions as progressive septic or cardiogenic shock.
WHEN TO STOP CPR
S SPONTANEOUS signs of circulation are restored
T TURNED over to medical services or properly trained and authorized personnel
O OPERATOR is already exhausted and cannot continues CPR
P PHYSICIAN assumes responsibility (declares death, take over, etc.
Signs of Life
Movement
Cough/ vomiting
Breathing
TABLE OF COMPARISON ON CARDIOPULMONARY RESUSCITATION FOR ADULT, CHILD. AND INFANT
ADULT CHILD INFANT
Compression Area
Simplified approach center of chest in between
imaginary nipple line
1 finger between the imaginary
nipple line
Depth
Approximately 1.5 to 2
inches
Approximately 1 to 1.5
inches
Approximately .5 to 1 inch
How to compress
Heel of 1 hand, other
hand on top
Heel of 1 hand on top
or heel of 1 hand
2 fingers (middle & ring finger
tips)
Rate Approximately 100/ minute
Compression ventilation
ratio
30:2 (1 or 2 rescuers) 30:2 (1 rescuer; 15:2 for 2 rescuers)
Number of cycles for
approx. 2 minutes
5 cycles (1 or 2 rescuers) 5 cycles (1 rescuer or 2 rescuers at 10 cycles)
Counting for standardization
purposes
1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,1,2,3,4,5,6,7,8,9, and 1, then breathe,
breathe; (up to 5 cycles) then breathe 2x.
EMERGENCY RESPONSE
Is a rapid movement of patient from unsafe place to a place of safety.
INDICATIONS FOR EMERGENCY RESCUE
1. Danger of fire or explosion
2. Danger of toxic gases or asphyxia due to lack of oxygen
3. Serious traffic hazards
4. Risk of drowning
5. Danger of electrocution
6. Danger of collapsing walls
METHODS OF RESCUE
1. For immediate rescue without any assistance, drag or pull the victim
2. Most of the one man drags/ carries and other transfer methods can be used as methods of rescue
TRANSFER is moving a patient from one place to another after giving first aid
FACTORS TO BE CONSIDERED IN THE SELETION OR CHOOSING THE TRANSFER METHOD:
Nature and severity of the injury
Size of the victim
Physical capabilities of the first aider
Number of personnel and equipment available
Nature of evacuation route
Distance to be covered
Sex of the victims (last consideration)
POINTERS TO BE OBSERVED DURING TRANSFER
1. Victims airway must be maintained open
2. Hemorrhage is controlled
3. Victim is safely maintained in the correct position
4. Regular check of the victims condition is made
5. Supporting bandages and dressing remain effectively applied
6. The method of transfer is safe, comfortable and as speedy as circumstances permit
7. The patients body is moved as one unit
8. The taller first aiders stay at the head side of the victim
9. First aiders/ bearers must be observed ergonomics in lifting and moving of patient
METHODS OF TRANSFER
1. One man assist/ carries/ drags
Assist to walk
Carry in arms (cradle)
Pack strap
Piggy back
Firemans carry
Blanket drag
Armpit/ shoulder drag
Feet drag
2. Two man assist/ carries
Assist to walk
Four hand seat
Hand as a litter
Carry by extremities
Firemans carry with assistance
3. Three man carries
Bearers along side
Hammock carry
4. Four/six/eight carry
5. Improvised stretcher using two poles with : blanket, empty sack, triangular bandages
6. Commercial stretchers
7. Ambulance
Anda mungkin juga menyukai
- ACLS Provider Manual PDFDokumen63 halamanACLS Provider Manual PDFRiley Escobar100% (1)
- 4 5819047049554822430 PDFDokumen431 halaman4 5819047049554822430 PDFAbog Luis Guillermo Andrade FloresBelum ada peringkat
- 2 - Patient Casualty and HandlingDokumen23 halaman2 - Patient Casualty and HandlingChristmyrian BalabaBelum ada peringkat
- First AidDokumen108 halamanFirst AidKerstine Anne AndradeBelum ada peringkat
- Basic First AidDokumen81 halamanBasic First AidDrVarun Menon100% (1)
- Basic Life SupportDokumen15 halamanBasic Life SupportMizzy Wat EvaBelum ada peringkat
- Medical Emergencies in The Dental PracticeDokumen15 halamanMedical Emergencies in The Dental Practicedaniel187951Belum ada peringkat
- TriageDokumen101 halamanTriageraighnejames19100% (1)
- First Aid HandoutDokumen5 halamanFirst Aid HandoutJohn Timothy KhoBelum ada peringkat
- Head and Neck ExaminationDokumen25 halamanHead and Neck ExaminationDarryl Betts100% (1)
- Administering Oral Medications: Melendez, Anna Carmela PDokumen19 halamanAdministering Oral Medications: Melendez, Anna Carmela PAnna Carmela P. MelendezBelum ada peringkat
- SplintingDokumen57 halamanSplintingNicholeBelum ada peringkat
- Bandaging GNMDokumen46 halamanBandaging GNMjoslinjohn100% (2)
- EpisiorrhaphyDokumen20 halamanEpisiorrhaphyAhmed Ben BellaBelum ada peringkat
- Principles & Practice of First AidDokumen298 halamanPrinciples & Practice of First AidJoshua100% (2)
- Emergency and Disaster Nursing 2012Dokumen218 halamanEmergency and Disaster Nursing 2012Darran Earl Gowing100% (2)
- POSITIONING CLIENTS IN BED ChecklistDokumen2 halamanPOSITIONING CLIENTS IN BED Checklistbevzie datu100% (1)
- RLE 1M Donning and DoffingDokumen48 halamanRLE 1M Donning and DoffingTrisha Apillanes100% (2)
- 1 Intro To First AidDokumen31 halaman1 Intro To First AidRayban AriñoBelum ada peringkat
- Fundamentals of Nursing p.1-37Dokumen38 halamanFundamentals of Nursing p.1-37Wik Wik PantuaBelum ada peringkat
- Bed Making: By: Judy N. Vasquez, M.A.NDokumen43 halamanBed Making: By: Judy N. Vasquez, M.A.NElyka AbellaBelum ada peringkat
- Introduction To First Aid and Basic Life Support CompressedDokumen47 halamanIntroduction To First Aid and Basic Life Support CompressedlunaBelum ada peringkat
- Bandaging (Handouts)Dokumen55 halamanBandaging (Handouts)Cik AmoiBelum ada peringkat
- Bandaging 140511011904 Phpapp02Dokumen46 halamanBandaging 140511011904 Phpapp02Kristela Mae ColomaBelum ada peringkat
- First AidDokumen37 halamanFirst AidPearl Delay100% (1)
- Bed MakingDokumen73 halamanBed MakingivernjayBelum ada peringkat
- FIRST AID Is An Immediate Care Given To A Person Who Has Been Injured or Suddenly Taken IllDokumen6 halamanFIRST AID Is An Immediate Care Given To A Person Who Has Been Injured or Suddenly Taken IllLeigh Yah86% (7)
- NCM 103: Skills Laboratory: LiftingDokumen74 halamanNCM 103: Skills Laboratory: LiftingLanzen DragneelBelum ada peringkat
- IeetDokumen63 halamanIeetfaraaz94Belum ada peringkat
- BLS-Participants-Workbook Updated 021218 V4Dokumen18 halamanBLS-Participants-Workbook Updated 021218 V4Elith Baclea-anBelum ada peringkat
- Wound DressingDokumen9 halamanWound Dressingapi-3722051100% (2)
- BSN 3 ProceduresDokumen128 halamanBSN 3 Procedureslourd nabBelum ada peringkat
- Community Health Nursing: Related Learning ExperienceDokumen13 halamanCommunity Health Nursing: Related Learning ExperienceKissy BesarioBelum ada peringkat
- Communicable Disease NursingDokumen50 halamanCommunicable Disease NursingGreggy Ventura100% (1)
- Bed MakingDokumen24 halamanBed Makingeha_9213423Belum ada peringkat
- First Aid Notes 2019Dokumen84 halamanFirst Aid Notes 2019Fredrick WedderburnBelum ada peringkat
- 2 Changing A Dry Sterile DressingDokumen3 halaman2 Changing A Dry Sterile DressingAnn Jalover PerezBelum ada peringkat
- Levels of PreventionDokumen30 halamanLevels of Preventionethics wixBelum ada peringkat
- Definition of BandagingDokumen18 halamanDefinition of Bandagingvkshamini91604250% (2)
- EN719DT Rescue Diver Knowledge Review Answer Key v101 PDFDokumen18 halamanEN719DT Rescue Diver Knowledge Review Answer Key v101 PDFmax minBelum ada peringkat
- First Aid and Water SurvivalDokumen7 halamanFirst Aid and Water SurvivalJoel BarotellaBelum ada peringkat
- Bandaging and SplintingDokumen2 halamanBandaging and Splintinglovemaeus6797Belum ada peringkat
- Knot-Tying and BandagingDokumen8 halamanKnot-Tying and Bandagingipo_dam4441Belum ada peringkat
- Carrying and Victim: TransportingDokumen28 halamanCarrying and Victim: TransportingAliya Nicole AranetaBelum ada peringkat
- Bed Making and Bed Linen StockDokumen19 halamanBed Making and Bed Linen StockDinda RamosBelum ada peringkat
- Perioperative Nursing Module 1Dokumen169 halamanPerioperative Nursing Module 1fleur harrisonBelum ada peringkat
- Patient Positioning: Complete Guide For MidwivesDokumen12 halamanPatient Positioning: Complete Guide For MidwivesRohlen BaguioBelum ada peringkat
- HA-RLE-WS # 5 Assessing General Status and Vital SignsDokumen5 halamanHA-RLE-WS # 5 Assessing General Status and Vital SignsAshley Blaise JoreBelum ada peringkat
- Emergency Rescue and TransferDokumen12 halamanEmergency Rescue and TransferColeen Ann Bagasol100% (1)
- Dressing and BandageDokumen11 halamanDressing and Bandageaidan valin100% (2)
- Module 4 Emergency Preparedness and Response ManagementDokumen18 halamanModule 4 Emergency Preparedness and Response ManagementMa. AlbinaBelum ada peringkat
- Bedpan or A Urinal: What You Need To Know: What Are Bedpans and Urinals?Dokumen8 halamanBedpan or A Urinal: What You Need To Know: What Are Bedpans and Urinals?Shereen AlobinayBelum ada peringkat
- Positioning Checklist Revised Mar 3Dokumen3 halamanPositioning Checklist Revised Mar 3Justine Matthew Gavile CoronicaBelum ada peringkat
- Procedure For Giving Perineal Care To The Male ClientDokumen3 halamanProcedure For Giving Perineal Care To The Male ClientParado Cabañal SkylieghBelum ada peringkat
- ESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Dokumen4 halamanESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Hannah Angelu CabadingBelum ada peringkat
- Ambulating A PatientDokumen5 halamanAmbulating A PatientSushmaBelum ada peringkat
- Skill Performance Evaluation - Measuring Intake and OutputDokumen2 halamanSkill Performance Evaluation - Measuring Intake and OutputLemuel Que100% (1)
- Perineal CareDokumen12 halamanPerineal CareSheing Estores-aroso100% (1)
- Shampooing Hair in Bed Procedure ChecklistDokumen2 halamanShampooing Hair in Bed Procedure ChecklistMarku LeeBelum ada peringkat
- Perception & Coordination NCM 104Dokumen162 halamanPerception & Coordination NCM 104bianqueeBelum ada peringkat
- PS FREL 5 LiftingAndMovingPatientsPowerPointDokumen18 halamanPS FREL 5 LiftingAndMovingPatientsPowerPointVirjhon MachsunBelum ada peringkat
- HSU 100-1 Choking and Other Conditions - Lecture 4Dokumen84 halamanHSU 100-1 Choking and Other Conditions - Lecture 4Nixi MbuthiaBelum ada peringkat
- Chicken Pox: By: Ari & JennDokumen12 halamanChicken Pox: By: Ari & JennEzekiel ArtetaBelum ada peringkat
- Module First AidDokumen12 halamanModule First AidHermie JosephBelum ada peringkat
- Module First AidDokumen18 halamanModule First AidThrina DubbBelum ada peringkat
- First Aid: Prepared by David R. Legarto III R.N., R.MDokumen93 halamanFirst Aid: Prepared by David R. Legarto III R.N., R.MdaveBelum ada peringkat
- Survival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)Dari EverandSurvival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)Belum ada peringkat
- Basic Life Support Program - Andhra Medical CollegeDokumen6 halamanBasic Life Support Program - Andhra Medical CollegeRajasekhar BandiBelum ada peringkat
- CHILDDokumen29 halamanCHILDFirdaus BaharuddinBelum ada peringkat
- Symbiosis Institute of Health Sciences (Sihs)Dokumen23 halamanSymbiosis Institute of Health Sciences (Sihs)Anshuman KhaitanBelum ada peringkat
- Medical EmergenciesDokumen3 halamanMedical Emergencieskiranvarma2uBelum ada peringkat
- Cardiovascular CareDokumen4 halamanCardiovascular Carenoble786Belum ada peringkat
- Advanced Cardiac Life Support Overview and Protocol - ACLS AHADokumen47 halamanAdvanced Cardiac Life Support Overview and Protocol - ACLS AHAEunice PalloganBelum ada peringkat
- Swimming and Aquatics Module 1Dokumen33 halamanSwimming and Aquatics Module 1Jezza PolicarpioBelum ada peringkat
- BLS 2Dokumen1 halamanBLS 2Moxie MacadoBelum ada peringkat
- Basic Life SupportDokumen54 halamanBasic Life SupportAdrianBelum ada peringkat
- Kauvery Hospital:: Kauvery Medical Centre-2002 - KMC Speciality Hospital Has Named As Kauvery Hospital. 2004Dokumen21 halamanKauvery Hospital:: Kauvery Medical Centre-2002 - KMC Speciality Hospital Has Named As Kauvery Hospital. 2004Sashi Kumar0% (1)
- Entry Level Nurse Resume Sample - Windsor OriginalDokumen2 halamanEntry Level Nurse Resume Sample - Windsor OriginalTejinder BhattiBelum ada peringkat
- CV For EportfolioDokumen5 halamanCV For Eportfolioapi-301128538Belum ada peringkat
- Emergency Management of Anaphylactic Shock in Dental Practice - A ReviewDokumen10 halamanEmergency Management of Anaphylactic Shock in Dental Practice - A ReviewKaram SarhanBelum ada peringkat
- Bab I.First Aid: PPSDM MigasDokumen31 halamanBab I.First Aid: PPSDM MigasacidafdolaBelum ada peringkat
- Perverted Indian WifeDokumen3 halamanPerverted Indian WifeDebolina DeyBelum ada peringkat
- History of CPR Research PaperDokumen8 halamanHistory of CPR Research Paperphqfgyvkg100% (1)
- DR Kshitij ResumeDokumen3 halamanDR Kshitij ResumeBarney StinsonBelum ada peringkat
- MT TRAINING CNA Class & AHA Classes - HCP BLS & CPR & FirstAid Online & On-SiteDokumen4 halamanMT TRAINING CNA Class & AHA Classes - HCP BLS & CPR & FirstAid Online & On-Siteheartandhandstraining_com100% (2)
- Pha CPR Bls Acls Manual 2012 Edited (08 25 2012)Dokumen30 halamanPha CPR Bls Acls Manual 2012 Edited (08 25 2012)Gene Alfonso BanawaBelum ada peringkat
- Disusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.BDokumen26 halamanDisusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.Bsangid yahyaBelum ada peringkat
- Course Exercise - PALS Precourse Self-Assessment and Precourse WorkDokumen3 halamanCourse Exercise - PALS Precourse Self-Assessment and Precourse WorkPRICIBelum ada peringkat
- 21-0409 - CASA Permit - RedactedDokumen23 halaman21-0409 - CASA Permit - RedactedKristen Faith SchneiderBelum ada peringkat
- Pra & Intra Hospital Cardiac Arrest Management-MAHESA Agustus 2021Dokumen65 halamanPra & Intra Hospital Cardiac Arrest Management-MAHESA Agustus 2021Menggy 31Belum ada peringkat