Anamia Aplasica
Diunggah oleh
Ronydubon10Deskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Anamia Aplasica
Diunggah oleh
Ronydubon10Hak Cipta:
Format Tersedia
Pediatr Blood Cancer 2005;45:770780
REVIEW
Diagnosis and Treatment of Children With Aplastic Anemia
Peter Kurre, MD,
1,2
* F. Leonard Johnson, MD,
1,2
and H. Joachim Deeg, MD
3,4
INTRODUCTION
Aplastic anemia (AA) can occur at any age. In contrast
to adults, however, a signicant proportion of children
present with severe aplastic anemia (SAA) that is neither
acquired nor idiopathic, but rather develops as a con-
sequence of a range of heritable genetic conditions. The
relatively greater incidence of such marrow failure
syndromes underlying childhood SAA leads to distinct
presentations, and requires a comprehensive work-up and
special therapeutic considerations.
While SAA previously was a near uniformly fatal
hematologic disorder, advances in supportive care and the
availability of several therapeutic options have signi-
cantly improved outcome. The treatment of choice for
patients with a human leukocyte antigen (HLA)-identical
sibling is generally a hematopoietic stem cell transplant
(HSCT), with cure rates now approaching 90%. Immu-
nosuppressive treatment (IST) constitutes an alternative
rst-line treatment in patients without a family HSCT
donor. In cases of inadequate response, or recurrence
after failed primary IST, HSCT using alternative donors
should be considered. This approach produces cure rates
of up to 75% of eligible children. Regardless of treatment
method, scrupulous life-long surveillance for the devel-
opment of late complications is required. Ultimately, an
improved understanding of the immunobiology under-
lying the development of marrow failure in acquired
SAA will permit a more narrowly targeted therapeutic
approach. This review summarizes diagnostic consi-
derations, current long-termoutcomes, and complications
of each strategy.
PRESENTATION AND ETIOLOGY
OF PANCYTOPENIA IN CHILDREN
AA, as dened by peripheral blood pancytopenia with
characteristic marrow hypoplasia or aplasia, occurs with
an estimated annual incidence of two per million, and at
higher rates in countries with increased rates of viral
hepatitis [1]. The presentation is directly linked to the
severity of the individual cytopenias and to the underlying
etiology. Specic symptoms related to anemia, infection,
and thrombocytopenia guide initial stabilization and
supportive care. The evaluation of pediatric patients with
SAA requires a potentially extensive diagnostic work-up
to exclude a genetic bone marrowfailure syndrome. Cases
Background. Long-term survival rates among
children diagnosed with severe aplastic anemia
(SAA) are excellent due to the success of
human leukocyte antigen (HLA)-identical related
hematopoietic stem cell transplantation (HSCT),
concurrent advances in immunosuppressive
treatment (IST), and improved supportive care.
The challenge in making treatment recommen-
dations for children with SAA, therefore, is to
balance the apparent chronicity and morbidity
following IST, with the potential up-front toxicity
and complications of HSCT. Methods. This
review provides an update on the diagnosis and
a risk-based treatment algorithmfor children with
acquired SAA. Recent experience using alter-
native donor HSCT and efforts to extend HSCT
eligibility through advances in donor matching,
de-escalation of conditioning regimens, and
potential marrow graft engineering are high-
lighted. We discuss IST response rates, risks of
relapse, and complications including clonal
evolution. Conclusions. While good treatment
options exist for a majority of children diagnosed
with SAA, novel non-transplantation treatments
for unresponsive and relapsed patients without
suitable transplant donors are needed. Further
improvements in outcome will ultimately require
a more complete understanding of the pathophy-
siology of aplastic anemia (AA). Pediatr Blood
Cancer2005;45:770780. 2005Wiley-Liss,Inc.
Key words: aplastic anemia; bone marrow failure; immunosuppressive therapy;
pediatrics; stem cell transplantation
2005 Wiley-Liss, Inc.
DOI 10.1002/pbc.20322
1
Division of Pediatric Hematology/Oncology, Department of
Pediatrics, Oregon Health & Science University, Portland, Oregon
2
OHSU Cancer Institute, Portland, Oregon
3
Fred Hutchinson Cancer Research Center, Seattle, Washington
4
Department of Medicine, University of Washington, Seattle,
Washington
Grant sponsor: NHLBI; Grant numbers: HL 36444, CA 087948.
*Correspondence to: Peter Kurre, Division of Pediatric Hematology/
Oncology, 3181 S.W. Sam Jackson Park Road, CDCRP, Portland, OR
97239-3098. E-mail: kurrepe@ohsu.edu
Received 2 December 2004; Accepted 3 December 2004
of marrow failure arising as a consequence of a heritable
defect require genetic counseling, conscientious patient
education, ancillary diagnostic evaluation for associated
organ manifestations, potential sibling diagnosis, and
family planning. Referral to a specialized center is
recommended. Awide range of etiologies has been linked
to pancytopenia and bone marrow failure in childhood
(Table I). However, causality is frequently difcult to
demonstrate and may not affect the ultimate outcome [2].
DIAGNOSTIC EVALUATION AND
CLASSIFICATION OF SEVERITY
A thorough personal and family history with focus on
potential infectious etiologies and environmental expo-
sures is essential. The diagnostic work-up includes the
evaluation of peripheral blood counts with complete
differential count, reticulocyte count, serum chemistries,
liver enzyme studies, and viral serologies (Table II). Even
in the absence of physical abnormalities, it is imperative to
carry out chromosome breakage studies to exclude DNA
repair disorders presenting with marrow failure, notably
Fanconi anemia (FA). A sizable portion of FA patients
present without obvious physical stigmata, and are
uniquely sensitive to a variety of therapeutic agents used
in the preparative conditioning for HSCT.
Bone marrow studies, including both, an aspirate and a
unilateral trephine biopsy, are obligatory for complete
evaluation. Morphological abnormalities, including pro-
minent dyserythropoiesis and histophagocytosis, eosino-
philia, or prominent lymphoid aggregates are frequently
encountered on biopsies from patients with SAA. Frank
granulocytic or megakaryocytic dyspoiesis is more con-
sistent with a myelodysplastic condition. Additionally,
marrow cytogenetics for karyotyping should be obtained
to identify clonal abnormalities, such as partial or com-
plete loss of chromosome 7. Radiological studies should
be performed based on the clinical index of suspicion and
as part of a further, directed work-up.
A number of investigational tests can be helpful in
distinguishing patients with acquired SAA from those
with other underlying disorders. While not individually
diagnostic of the disorder, they may help in combination
with other tests and can be used as a means of monitoring
treatment response. For example, Sloand and colleagues
reported the increased presence of intracellular interferon
gamma (IFNg) in lymphocytes of patients with SAA,
TABLE I. Differential Diagnosis of Pancytopenia in Children
Diagnoses References
Bone marrow
failure syndromes
SchwachmanDiamond syndrome [3]
Dyskeratosis congenita [4]
Fanconi anemia [5]
Pearson syndrome [6]
Amegakaryocytic thrombocytopenia [7]
Neoplastic/clonal
disorders
Leukemia (lymphoid or myeloid) [8]
Myelodysplasia/myelobrosis [9]
Paroxysmal nocturnal hemoglobinuria
a
[10]
Histiocyte disorders [11]
Infection EBV, CMV, HHV-6 [12]
Hepatitis [13]
HIV [14]
Parvovirus [15]
Environmental
exposure
Toxins [1]
Drugs [16]
Ionizing radiation [1]
Miscellaneous Pregnancy [17]
Osteopetrosis [18]
EBV, Epstein-Barr Virus; CMV, Cytomegalovirus; HHV-6, human
herpes virus 6; HIV, human immunodeciency virus.
a
Overlap exists between paroxysmal nocturnal hemoglobinuria (PNH)
and aplastic anemia (AA) (discussed below).
TABLE II. Evaluation of Patients Presenting With Peripheral
Blood Pancytopenia
Clinical
Vital signs
Allergies
Physical examination
Symptoms
Patient history
Medications
Immunizations
Exposures to environmental toxins
Transfusions
Family history
Constitutional abnormalities
Malignancies
Laboratory
Peripheral blood
Complete blood cell count, reticulocyte counts, smear; MCV
Chemistries, liver function tests, LDH
Vitamin B
12
and Folate levels
Serologies: Hepatitis-A, -B, -C, HIV,EBV, CMV,
HHV-6, Parvovirus
Chromosome breakage studies
ABO-, Rh-Typing, antibody screen
Flow cytometry for CD55/59 (PNH)
ANA, C
3
, CH
50
b-HCG
Bone marrow
Aspirate and biopsy
Flow-cytometry
Cytogenetics
Urine
Urinalysis
Ancillary studies
Hemoglobin-F, small i antigen
X-ray, abdominal ultrasound
EBV, Epstein-Barr virus; CMV, Cytomegalovirus; HHV-6, human
herpes virus 6; HIV, human immunodeciency virus; LDH, lactate
dehydrogenase; PNH, paroxysmal nocturnal hemoglobinuria; ANA,
anti-nuclear antigen; C
3
, CH
50
, complement component and activity;
b-HCG, beta subunit-human chorionic gonadotropin; MCV, mean
corpuscular volume.
Aplastic Anemia in Children 771
and demonstrated a correlation with patients response to
IST [3]. Flow-cytometric assays to detect the presence of
glycosyl phosphatidyl inositol (GPI) linked proteins to
exclude paroxysmal nocturnal hemoglobinuria (PNH) are
routinely performed in AA patients (see below). Abnorm-
alities in telomere length maintenance and telomerase
activity in peripheral blood and bone marrow leukocytes
of patients with SAA have also been described [4].
Telomere shortening and upregulated telomerase enzyme
activity support the concept of stem and progenitor cell
exhaustion following immune destruction with resultant
increased cellular turnover, and suggest a potential role for
telomerase maintenance deciency in the etiology of
SAA. A proposed correlation between telomere short-
ening and clonal evolution in SAA awaits conrmation
[4]. Hematopoietic colony forming assays in SAApatients
show uniformly reduced multilineage colony formation
and suboptimal cytokine responsiveness [5].
Once diagnosed with marrow aplasia, patients are
classied according to severity criteria (Table III) [6,7]. A
correlation exists between the severity and clinical
outcome with non-severe, severe, and very severe AA
carrying a progressively worsening prognosis [6,8,9].
Non-severe or moderately severe cases, while less
frequent, may spontaneously remit, and do not routinely
require therapeutic intervention [10,11]. The natural
history of severe acquired marrow aplasia is one of
inevitable progression to pancytopenia without signicant
chance of spontaneous remission. Once supportive care
has been initiated and the main differential diagnoses have
been ruled out, appropriate front line treatment should
be commenced, as outlined below.
SUPPORTIVE CARE
Vascular Access and Blood Product Transfusion
Placement of a central vascular access device should be
considered for all pediatric patients, given the need for
repeat phlebotomy, frequent blood product transfusions,
and administration of multiple medications. The specic
type of device (e.g., Hickman
, Port-a-Cath
, or other)
should be selected with regard to patient age and planned
therapy.
Patients presenting with anemia and thrombocytopenia
often require prolonged transfusion support in part
depending on the treatment used and the response
obtained. Representative of other studies, Di Bona et al.
reported that 50% of their patients took 3 months from
IST initiation (90% by 1 year) to become independent of
red blood cell and platelet transfusions, albeit not
necessarily with normalization of blood counts in all
cases [12]. All blood products should be leukocyte-
depleted and transfusion guidelines should be restrictive to
minimize allosensitization to red cell and leukocyte
antigens, in particular minor HLA antigens [13,14]. Until
the patients Cytomegalovirus (CMV) serology is avail-
able, all patients should be transfused with blood products
from CMV-seronegative donors. This is particularly
important for potential HSCT recipients, as CMV patient
serostatus may impact transplant outcome. Irradiation and
leukocyte depletion of transfusion products may impair
lymphocyte proliferation and allosensitization to minor
HLA antigens, thereby reducing the risks of graft-versus-
host disease (GVHD) and rejection, respectively [15,16].
Transfusion thresholds depend on the patients status,
clinical condition, existing co-morbidities, and institu-
tional practices. While a platelet count of 20,000/mm
3
has
traditionally been the threshold for platelet transfusions, at
least one study has demonstrated that substantially lower
platelet counts (10,000/mm
3
) and less frequent transfu-
sions are safe and well tolerated, even in the outpatient
setting [17].
Hematopoietic Growth Factors
Growth factors provide supportive care and do not
generally induce disease remission. Granulocyte (G)
and granulocyte macrophage colony stimulating factor
(GM-CSF) used as individual agents occasionally result in
a temporary rise in neutrophil counts [18,19]. More
commonly, growth factors are used in combination with
ISTwhere GM-CSF and G-CSF, alone, or in combination
with erythropoietin, have been shown to promote single
and multilineage responses in up to 80% of patients
[4,20,21]. Few studies have explored the use of inter-
leukins-3 and -6 or stem cell factor (c-kit ligand), but
concerns about a lack of efcacy combined with agent
toxicity have precluded their more widespread use.
Investigations into whether the long-term use of hemato-
poietic growth factors might induce or promote cytoge-
netic abnormalities in SAApatients after ISTare discussed
below. The use of hematopoietic growth factors in patients
with AA has recently been reviewed elsewhere [22].
TABLE III. Diagnostic Criteria for the Classication of AA
Peripheral blood cytopenia
Bone marrow
cellularity
Severe AA Presenting with at least two
of the following
<25%
OR
Granulocytes <500/mm
3
Platelets <20,000/mm
3
Reticulocytes <200/mm
3
25%50% with
<30% hematopoietic
elements
Very severe AA Same as above, except
Granulocytes
<200/mm
3
Non-severe AA Pancytopenia, not fullling
the above criteria
772 Kurre et al.
Infection and Iron Overload
Patients with severe and long-standing leukopenia are
at a signicant risk for developing invasive bacterial and
fungal infections. Infections must be diagnosed promptly
and treated aggressively to minimize long-term organ
damage and avoidchronic persistence in patients who may
receive subsequent or concurrent immunosuppressive or
myeloablative treatment [1].
Iron overload may result fromprolonged red blood cell
transfusion support potentially producing irreversible
multiple organ damage. Most centers will institute
chelation therapy with deferoxamine if the patients serum
ferritin level exceeds 2,000 mg/L [23].
FRONT LINE TREATMENT FOR CHILDREN WITH
HLAIDENTICAL RELATED HEMATOPOIETIC
STEM CELL DONORS
Matched Sibling Stem Cell Transplantation
Based on pre-clinical models of stem cell transplan-
tation, patients with SAA have been treated by HSCT
since the early 1970s using a highly immunosuppressive
cyclophosphamide (CY)-based preparative regimen
[24]. Initial success was limited by graft rejection in up
to 30% of patients receiving such conditioning [25]. This
problem was subsequently found to be due to high rates
of blood product transfusion-related allosensitization
and aggravated by a low stem cell dose [26]. Moreover,
54%of patients conditioned with CYshowed evidence of
mixed donor and host chimerism after transplant,
potentially placing them at risk for late rejection [27].
The addition of myeloablative irradiation decreased the
risk of rejection, but was associated with signicant
long-term effects on growth, neuro-cognitive develop-
ment, pneumonitis, and secondary malignancy in chil-
dren [28]. The introduction of antithymocyte globulin
(ATG) into the preparative regimen and cyclosporine A
(CSP) for GVHD prevention substantially decreased
rejection rates from 32% to 8% [29,30]. As a result,
current conditioning and GVHD prophylaxis strategies,
combined with state-of-the-art supportive care,
produce survival rates after matched sibling transplants
of 85%, or higher in selected series [3133]. On balance
of risk and benet, HSCT is the recommended treatment
for newly diagnosed children with HLA-identical sibling
donors. Given the straightforward logistics, time to
HSCT is typically short for these patients, and no
interim treatment other than ongoing supportive care is
necessary.
Stem Cell Source
Unlike patients treated with HSCT for malignant
disorders, those with SAA derive no benet from a
potential graft-versus-tumor effect associated with
GVHD. Thus, engraftment and minimization of the
rejection risk are the dominant factors to consider
when selecting the optimum source of stem cells. Most
studies to date have used unmanipulated bone marrow
grafts and have aimed at optimizing the cell dose [34].
While larger cell numbers are routinely achieved using
peripheral blood stem cells (PBSC), their use is also
(potentially) associated with higher rates of chronic
GVHD [35]. A recent prospective study by the European
Blood and Marrow Transplant (EBMT) group directly
compared both stem cell sources in SAA patients under-
going HSCT, and reported no apparent additional
advantage with the use of PBSC over marrow grafts
[36]. Cytokine-mobilized PBSC have been used success-
fully in patients who rejected their primary grafts, or in
combination with bone marrow stem cells as a means to
increase inoculum cell numbers [37]. A recent study
explored the use of CD34 selected PBSC in a haploiden-
tical donor setting, illustrating the feasibility and com-
plexity of this approach [38].
Results using cord blood as a stem cell source for SAA
patients have been less favorable due to increased rates of
non-engraftment and regimen toxicity. The use of cord
blood in this disease should be recommended with caution
[39]. Studies in non-AA patients indicate that high
rejection rates and HLA disparities may not be problems
if cord blood units with higher CD34 cell content are used.
Conceivably this strategy can also be applied to patients
with SAA [40].
Late Effects After HSCT
Transient ovarian and testicular dysfunction (with
subsequent recovery) are common after CY-based
HSCT conditioning therapy in SAA patients [41].
Children show normal growth (nal adult height) and
development, as well as thyroid and adrenal function after
conditioning regimens consisting of CYonly. On the other
hand, myeloablative, irradiation-based regimens are
complicated by reduced nal adult height, abnormal
thyroid function, and frequently irreversible gonadal
failure, even in patients who received irradiation sparing
the neuroendocrine axis and focusing on lymphoid
structures [42,43].
GVHD and its sequelae are the major long-term com-
plications after HSCT in SAA patients. A study of 212
patients reported 20-year survival rates among recipients
of HLA-identical sibling grafts without GVHD of 89%,
compared to 69% for patients who developed chronic
GVHD[44]. Most deaths in this study were due to GVHD-
related immunodeciency, infection, or pulmonary mani-
festations resulting from GVHD and its treatment.
The risk of secondary hematologic malignancies or
solid tumors was 14%, 20 years following myeloablative
treatment of 700 patients reviewed in one series. Major
Aplastic Anemia in Children 773
risk factors were the use of irradiation-based conditioning
regimen and the development of chronic GVHD [45].
FRONT LINE TREATMENT OF CHILDREN
DIAGNOSED WITH AA IN THE ABSENCE
OF AN HLA-IDENTICAL SIBLING DONOR
Immunosuppression
Observations of endogenous hematopoietic recovery
after failed HSCT led to the use of IST for the treatment
for SAA patients. Additional compelling evidence came
from improved treatment outcomes of patients receiving
anti-lymphocye globulin (ALG) versus supportive care
only [46,47]. A subsequent larger study by the EBMT
Group reported 61% survival at 5 years from treatment
with ATG [48]. Characteristically, responses to IST are
slow to become manifest, frequently incomplete, and often
followed by disease recurrence. Clinical responses after
IST are commonly graded according to the following
criteria: (Table IV).
The introduction of CSP in combination with ATG/
ALG produced further substantial increases in the
response rate of patients with SAA65% at 6 months in
comparison to 31% after ATG alone [49,50]. Others have
reported overall response rates as high as 75% [9,51,52].
Additionally, median time to response after combination
therapy was signicantly shorter, and the incidence of
treatment failure was signicantly lower among recipients
of a combination of ALGand CSP versus ALGalone [53].
Results are particularly favorable in children with actu-
arial survival exceeding 85%at 8 years in two independent
studies [32,33]. Therefore, combination treatment with
ATG (or ALG), CSP, and G-CSF represents the current
treatment of choice for children without matched sibling
donors [20,33,54,55]. Conceptually, SAA patients treated
with ISTare thought to benet froma functional cure in
up to 50% of those responding to treatment [52].
Accordingly, after IST, a substantial number of patients
will live with a chronic, and at times life-threatening,
disease. Responses may be drug-dependent and the dis-
ease may be prone to recur or show malignant evolution.
Kinetics and Quality of Response to Combination
Immunosuppressive Therapy
Hematopoietic recovery after treatment with ATG and
CSPoccurs by 3 months in 67%of patients and by 1 year in
a total of 78% [9]. Others report trilineage hematologic
responses and transfusion independence in about 82% by
4 months from treatment, using combinations of ATG/
CSP and G-CSF, with actuarial survival exceeding 80%
[20,54]. The update from a large German multi-center
study with 11-year follow-up, comparing treatment with
ALGversus ALGand CSP, shows a more complex picture
[53]. Response rates by 4 months were only 56% overall,
responses were predominantly partial, occurred as late as
3.5 years from diagnosis, and often only after multiple
treatment courses. Combination treatment with ALG and
CSP was shown to produce signicantly shorter median
times to hematopoietic recovery, and was associated with
a reduced incidence of treatment failure, compared with
ALG alone. Use of G-CSF in the context of combination
IST tends to hasten hematologic recovery.
Red blood cell and platelet transfusion independence
was achieved in 50% of patients by 95 days, and in 90%
by 12 months from treatment initiation [12]. In one study
involving 86 pediatric patients, the complete response
rates at 3, 6, and 12 months were 13%, 39%, and 55%with
overall responses (complete plus partial) in 61%, 74%, and
80%of patients, respectively [33]. In rare cases, responses
occurred as late as 18 months fromISTinitiation. Together,
these studies conrm the slow kinetics and incomplete
responses frequently observed in adult patients after IST
[53]. Giving closely spaced additional courses of ATG
based combination immunosuppressive therapy does not
seem to improve response kinetics or overall rates [56].
Recurrence After IST
Recurrence is frequent after IST, occurring in up to 36%
of patients treated with ATG and CSP, without necessarily
predicting for worse survival [9,51,52,57]. Interestingly, the
incidence of recurrence decreased from 30% to 10% after
prolonging the duration of CSP tapering in one study [54].
This observationis supportedbyFuhrer andcolleagues who
reported relapses in 9 of 11 pediatric patients during
cyclosporine tapering, and the subsequent recovery of
responses in 7 of those 9 patients upon restarting CSP [33].
Similarly, Kaltwasser and colleagues found relapses only
after patients (receiving ALG and CSP) had discontinued
CSP [53]. This highlights the existence of a subgroup of
SAApatients treated with ISTwho become long-termCSP-
dependent [12,53]. In the study by Fuhrer and colleagues 6
of 44 patients observed for more than 2 years had CSP-
dependent improvements in hematopoiesis, as did two
patients in the study by Frickhofen and colleagues, who
remained on CSP for 9.7 and 12 years, respectively [53].
One group of investigators suggests that CSP response and
TABLE IV. Response Criteria for Severe Aplastic Anemia (SAA)
Patients After Immunosuppressive Treatment (IST)
Complete
No transfusion support
Hemoglobin normal for age/gender
Absolute neutrophil count >1,500/mm
3
Platelet count >150,000/mm
3
Partial
No transfusion support
Does not meet SAA criteria
None
Meets SAA criteria
774 Kurre et al.
dependence may be more frequent in patients with a HLA-
DR2 (DRB15) haplotype [58]. CSP should be tapered at
small decrements over no less than 6 months.
Re-Treatment
Patients who are unresponsive, or who relapse after an
initial response may benet from repeat treatment with
the identical, or a different, immunosuppressive regimen.
The best chances for successful re-treatment are probably
with a combination IST regimen including ATG/ALG.
Transfusion independent hematopoiesis after one (or
more) repeat treatment cycle of ALG in combination with
CSP given for non-response or relapse was accomplished
in 27 of 43 patients (63%) in one single-center retro-
spective study [59]. The authors noted an increased
incidence of late clonal complications (small numbers
prevented statistical signicance). Responses to repeat
treatment were similar among primary refractory and
relapsed patients, and while survival was 75%for primary
responders, it was 55% for primary non-responders with
subsequent response, and only 29% for primary non-
responders resistant to secondary treatment. Thirteen-year
survival among responders to a second course was 68.5%
versus 80.4% in primary responders. Re-treatment after
non-response to primary combination IST is recom-
mended between 3 and 6 months from the initial course.
ATG is commercially available as a rabbit- (rATG) or
horse-derived (hATG) product. Studies suggest compar-
able efcacy for secondary treatment with rATG/ALG,
showing responses in 22%50% of cases [8,57]. Com-
plete response rates of up to 30% among patients who
failed to respond to hATG and were re-treated with rATG,
or vice versa, have been reported by others [60].
Survival
Mortality among AA patients shows a bimodal distri-
bution with a majority of deaths occuring within the rst
6 months fromdiagnosis due to hemorrhage and infection;
late deaths are the result of complications fromrecurrence,
clonal evolution, and malignancy [52,53]. Response to
treatment, younger age, and less severe cytopenia are
associated with better prognosis [52,53]. Conversely,
clonal evolution during or after ISTand frank malignancy
predict poor outcome [52]. Overall survival in adult
patients after ISTin studies providing long-termfollow-up
of 7 and 11 years was 55% and 58%, respectively [52,53].
Survival of pediatric patients exceeded 80% in three
independent studies, albeit with a median follow-up of
only 4 years, likely underestimating attrition due to late
mortality from clonal disorders [33,55,61].
Long-Term Treatment Complications
The most severe complications in patients who survive
long-termafter ISTare clonal hematopoieticdisorders. It is
currently unclear whether clonal disorders reect the
natural history of SAA, or whether they may in part be
related to IST [12,62,63].
Cytogenetic abnormalities have long been known to be
present in SAA patients at diagnosis, with an incidence as
high as 11% in one study [64]. They may disappear
spontaneously, or after IST, without affecting the response
to IST or survival [6567]. The de novo development of
cytogenetic abnormalities after treatment on the other
hand has been associated with a worse outcome [59,68].
DePlanque et al. noted clonal cytogenetic abnormalities
after treatment in 19 of 209 patients with a median time to
development of 3 years; myelodysplasia (MDS) devel-
oped in 11 of 209 patients at a median of 4.6 years, with
15% actuarial incidence after 7 years. Using a sucrose
hemolysis diagnostic assay, PNH was seen in 13% of
patients by 7 years after treatment [69]. Clonal disease
most often develops within the rst 3 years fromtreatment,
although patients remain at risk thereafter. A more recent
analysis of EBMT data, excluding cases diagnosed within
the rst 12 months of therapy, showed the development of
MDS in 19 of 860 patients, and acute leukemia in
15 additional patients, for a 10-year actuarial incidence of
clonal diseases of 18.8% [63].
A controversial series of articles have linked the use
of G-CSF in combination with IST to the development
of monosomy 7 and MDS in children [70,71]. Analysis of
113 children showed a cumulative incidence of MDS of
13.7%. Non-response to ISTat 6 months, as well as G-CSF
therapy were risk factors predictive for the development of
MDS. However, extended duration of therapy, higher
doses of G-CSF, and enrollment of patients with non-
severe AAmake it difcult to extrapolate the observations.
The provocative hypothesis that prolonged G-CSF use
may promote loss of chromosome 7 (in part or completely)
and result in MDS is not currently supported by data from
other groups, but warrants further laboratory investigation
and prospective clinical analysis. Judicious use of cyto-
kines with adherence to response criteria and dosing
guidelines is recommended. The routine use in non-severe
AA is not recommended.
The simultaneous occurrence of PNH and AA has long
been recognized [66,72], even though only a minority of
10%15%of AA/PNHpatients present with hemolysis or
thrombotic complications (or both) are of classic PNH.
The presence of PNHclones in AApatients, especially in a
minor percentage, is likely underestimated in studies
relying onHamtest for erythrocyte complement activation
and has been re-assessed using a more quantitative ow-
cytometric assay targeting Gs or mononuclear cells
[72,73]. Using this assay, up to 60% of SAA patients in
one study of patients showed GPI abnormalities [74]. The
impact of the presence of these clones on prognosis after
combination IST is controversial, and may portend a
worse outcome [73,75].
Aplastic Anemia in Children 775
TREATMENT OF CHILDREN FAILING TO RESPOND
TO PRIMARY MULTI-AGENT IMMUNOSUPPRESSION
Alternative Donor Stem Cell Transplantation
Pediatric patients failing an initial course of IST
should be considered for HSCT if an allele-level HLA-
matched unrelated stem cell donor is available. Results
after alternative donor transplantation have generally
been less favorable than HLA-identical sibling trans-
plants, with long-term survival of less than 50% irrespec-
tive of the use of mismatched family-, haploidentical-, or
matched-unrelated donors [7678]. Overcoming the HLA
barrier for mismatched grafts and preventing rejection
due to allosensitization after prolonged blood product
transfusion support may require more intense preparative
regimens, with the attendant increased risk of regimen
related mortality [79]. A retrospective analysis on
behalf of the National Marrow Donor Program
(NMDP) conrmed the generally disappointing outcome
after matched unrelated HSCT with 36% overall survival
among 141 patients at a median follow-up of 36 months
from treatment, and identied HLA mismatch as a risk
factor [79]. Based on those ndings, a multi-center
cooperative study was subsequently designed to system-
atically explore the de-escalation of conditioning regimen
intensity, while using more rigorous HLA matching
criteria [80]. Results from this study demonstrated that
regimen related toxicity can be reduced and engraftment
rates maintained by combining CY, ATG, and non-
myeloablative doses (200600 cGy) of total body
irradiation (TBI). In an interim analysis of 50 patients,
outcome was substantially improved compared with
historic controls, and survival rates up to 73% were seen
in patients transplanted within 1 year from diagnosis, and
less than 20 years of age. As reported elsewhere, the
incidence of infectious complications and older age
adversely affected outcome [62,76,81].
Arecent update of this series indicates further outcome
improvement amongyoung patients (<17 years) receiving
bone marrowtransplants frommolecularly HLA-matched
unrelated donors (H. Deeg, unpublished observations).
Survival among 15 patients who received 200 cGy TBI
was 85% at almost 5 years after HSCT, compared to 65%
among 9 patients who received higher doses of TBI
(Fig. 1). These data further support the feasibility of
conditioning therapy de-escalation as a strategy for
minimizing toxicity (largely pulmonary in this cohort),
while maintaining engraftment in the unrelated stem cell
donor setting.
Similarly, Vassilou and colleagues report encouraging
survival after unrelated HSCT in six patients (median
follow-up 32 months) enrolled in a reduced intensity
protocol using (300 cGy) irradiation combined with CY
and pre-transplant immunodepletion using campath 1-G/
1-H [81].
Other Treatment Modalities
In the absence of a suitable unrelated stem cell donor,
patients may require additional courses of combination
ISTor alternative strategies. Such non-standard treatment
includes androgenic steroids, which have a predomi-
nant effect on erythropoiesis and have led to transient
improvements in hemoglobin levels and transfusion
requirements when given alone or in combination with
ALG [8284]. In spite of responses in 75% of patients,
there was no concurrent improvement in survival [85].
The considerable side effects of androgenic steroids and
availability of more effective multi-agent therapy limit
their overall utility. Anecdotal reports demonstrate that
glucocorticosteroids can induce remission in SAA [86].
However, their serious multi-organ system side effects
preclude long-term use, except for the prevention or
treatment of ATG-induced side effects.
The use of CYas an immunosuppressive agent without
stem cell rescue has recently seen renewed interest and
some controversy. A number of studies have explored its
use in patients with SAA, either as primary, or as salvage
therapy [87,88]. More widespread use, especially in
previously untreated pediatric patients and outside clinical
trials, is limited by short-term toxicity and protracted
response kinetics.
The development of newtherapeutic agents is critically
important to improve response and cure rates for AA
patients unable, or unwilling, to proceed to HSCT. Case
series have reported the use of mycophenolate mofetil in
combination with other immunosuppressive agents in
patients with SAA[89]. Randomized studies investigating
its role in the treatment of newly diagnosed or relapsed
patients are currently underway through the EBMT net-
work and at the National Institutes of Health. The use of
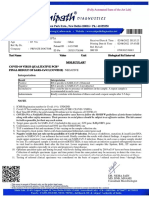
Fig. 1. Overall survival in a subgroup of patients <17 years of age
who received HLA-matched unrelated marrow stem cell grafts
following conditioning therapy as outlined above, including either
single or multiple doses of 200 cGy of TBI.
776 Kurre et al.
additional agents, including anti-IL-2 antibody, sirolimus,
and tacrolimus, has been reviewed elsewhere [89,90].
Splenectomy
A single retrospective analysis describes the use of
splenectomy as adjuvant therapy in patients with SAA.
Rapid and sustained improvement in peripheral blood
hematologic parameters was noted in some patients.
Splenectomy may occasionally be useful in the care of
heavily transfused and allosensitized pediatric patients
refractory to medical treatments and without a stem cell
donor [91].
CONCLUSIONSUPDATING TREATMENT
RECOMMENDATIONS
A risk-based treatment recommendation for pediatric
SAA patients without matched sibling donors should
strive to balance morbidity and long-term complications
from IST with short-term regimen-related toxicities
from pre-transplant conditioning and sequelae of
GVHD after HSCT. The following principal factors
deserve consideration in making such treatment recom-
mendations for patients without matched sibling donors
(Table V).
It is apparent that multiple competing risks for morbi-
dity and mortality, such as infectious complications, iron
overload from transfusion, or clonal evolution, persist
lifelong in patients after IST. This renders SAA a chronic
condition with limited probability of cure. Generally poor
response to further ISTafter primary failure or recurrence,
and escalating risks for infectious or malignant complica-
tions, should lead to prompt donor registry search and
HSCT referral. At the same time, improved HLA typing
technology, reduced intensity conditioning, and novel
GVHD treatment regimens have improved outcome
after unrelated HSCT especially among pediatric re-
cipients. The risk of secondary malignancy and neuro-
developmental side effects may decrease with lower TBI
doses.
Patient eligibility criteria for HLA matched unrelated
HSCT can currently be expanded to include pediatric
patients with SAA, who show inadequate response to
front-line combination ISTand have an available marrow
stem cell donor. HSCT should be undertaken in pediatric
patients with a suitable donor, who are unresponsive to
IST for after an year. With further improvement of results
and availability of unrelated donors matched with the
patient by high resolution HLA typing, HSCT from
unrelated donors may be attractive in the future as the rst-
line approach for selected patients.
ACKNOWLEDGMENT
The authors thank the many colleagues and investi-
gators whose important work could not be cited in this
article due to space constraints. They also thank Janice
Naas for her editorial assistance in preparation of this
manuscript. H. JoachimDeeg was supported by grants HL
36444, CA 087948.
REFERENCES
1. Nathan & Oski. Bone marrow failure syndromes. Hematology of
infancy and childhood. Philadelphia: WD Saunders Group. 1998.
2. Bacigalupo A. Aetiology of severe aplastic anaemia and outcome
after allogeneic bone marrow transplantation or immunosuppres-
sion therapy. Working Party on Severe Aplastic Anaemia of the
European Blood and Marrow Transplantation Group. Eur J
Haematol Suppl 1996;60:1619.
3. Sloand E, Kim S, Maciejewski JP, et al. Intracellular interferon-
gamma in circulating and marrow T cells detected by ow
cytometry and the response to immunosuppressive therapy in
patients with aplastic anemia. Blood 2002;100:11851191.
4. Ball SE, Gibson FM, Rizzo S, et al. Progressive telomere
shortening in aplastic anemia. Blood 1998;91:35823592.
5. Maciejewski JP, Anderson S, Katevas P, et al. Phenotypic and
functional analysis of bone marrowprogenitor cell compartment in
bone marrow failure. Br J Haematol 1994;87:227234.
6. Gluckman E, Devergie A, Poros A, et al. Results of immunosup-
pression in 170 cases of severe aplastic anaemia. Report of the
European Group of Bone Marrow Transplant (EGBMT). Br J
Haematol 1982;51:541550.
7. Camitta BM, Thomas ED, Nathan DG, et al. Severe aplastic
anemia: A prospective study of the effect of early marrow
transplantation on acute mortality. Blood 1976;48:6370.
8. Marsh JC, Hows JM, Bryett KA, et al. Survival after antilympho-
cyte globulin therapy for aplastic anemia depends on disease
severity. Blood 1987;70:10461052.
9. Rosenfeld SJ, Kimball J, Vining D, et al. Intensive immunosuppres-
sion with antithymocyte globulin and cyclosporine as treatment for
severe acquired aplastic anemia. Blood 1995;85:30583065.
10. Howard SC, Naidu PE, Hu XJ, et al. Natural history of moderate
aplastic anemia in children. Pediatr Blood Cancer 2004;43:545.
11. Khatib Z, Wilimas J, Wang W. Outcome of moderate aplastic
anemia in children. Am J Pediatr Hematol Oncol 1994;16:8085.
12. Di Bona E, Rodeghiero F, Bruno B, et al. Rabbit antithymocyte
globulin (r-ATG) plus cyclosporine and granulocyte colony
stimulating factor is an effective treatment for aplastic anaemia
patients unresponsive to a rst course of intensive immunosup-
pressive therapy. Gruppo Italiano Trapianto di Midollo Osseo
(GITMO). Br J Haematol 1999;107:330334.
13. Deeg HJ. Modication of immunogenicity of transfusion products.
Prog Clin Biol Res 1986;211:117127.
14. Klingemann HG, Self S, Banaji M, et al. Refractoriness to random
donor platelet transfusions in patients with aplastic anaemia: A
TABLE V. Considerations in the Treatment of Children With SAA
Without Sibling Donor
Patient age
Suitable unrelated donor availability
Treatment response quality (complete, CSP-dependence, transfusion
needs)
Treatment response kinetics to IST (keep <1 year)
Complications from pancytopenia (incidence and severity)
Cytogenetic abnormalities (presence, quality, and progression)
CR, complete response; CSP, cyclosporine A; IST, immunosuppressive
treatment.
Aplastic Anemia in Children 777
multivariate analysis of data from 264 cases. Br J Haematol
1987;66:115121.
15. Bean MA, Graham T, Appelbaum FR, et al. Gamma-irradiation of
pretransplant blood transfusions from unrelated donors prevents
sensitization to minor histocompatibility antigens on dog leukocyte
antigen-identical canine marrow grafts. Transplantation 1994;57:
423426.
16. Arranz R, Otero MJ, Ramos R, et al. Clinical results in 50 multiply
transfused patients with severe aplastic anemia treated with bone
marrow transplantation or immunosuppressive therapy. Bone
Marrow Transplant 1994;13:383387.
17. Sagmeister M, Oec L, Gmur J. A restrictive platelet transfusion
policy allowing long-term support of outpatients with severe
aplastic anemia. Blood 1999;93:31243126.
18. Kojima S, Fukuda M, Miyajima Y, et al. Treatment of aplastic
anemia in children with recombinant human granulocyte colony-
stimulating factor. Blood 1991;77:937941.
19. Guinan EC, Lopez KD, Huhn RD, et al. Evaluation of granulocyte
macrophage colony-stimulating factor for treatment of pancyto-
penia in children with fanconi anemia. J Pediatr 1994;124:
144150.
20. Bacigalupo A, Broccia G, Corda G, et al. Antilymphocyte globulin,
cyclosporin, and granulocyte colony-stimulating factor in patients
with acquired severe aplastic anemia (SAA): A pilot study of the
EBMT SAAWorking Party. Blood 1995;85:13481353.
21. Hord JD, Gay JC, Whitlock JA, et al. Long-term granulocyte
macrophage colony-stimulating factor and immunosuppression in
the treatment of acquired severe aplastic anemia. J Pediatr Hematol
Oncol 1995;17:140144.
22. Kumar M, Alter BP. Hematopoietic growth factors for the treatment
of aplastic anemia. Curr Opin Hematol 1998;5:226234.
23. Porter JB. Practical management of iron overload. Br J Haematol
2001;115:239252.
24. Thomas ED, Storb R, Fefer A, et al. Aplastic anaemia treated by
marrow transplantation. Lancet 1972;1:284289.
25. Champlin RE, Horowitz MM, van Bekkum DW, et al. Graft failure
following bone marrow transplantation for severe aplastic anemia:
Risk factors and treatment results. Blood 1989;73:606613.
26. Storb R, Prentice RL, Thomas ED. Marrow transplantation for
treatment of aplastic anemia. An analysis of factors associated with
graft rejection. N Engl J Med 1977;296:6166.
27. Dufour C, Dallorso S, Casarino L, et al. Late graft failure 8 years
after rst bone marrow transplantation for severe acquired aplastic
anemia. Bone Marrow Transplant 1999;23:743745.
28. Cohen A, Duell T, Socie G, et al. Nutritional status and growth after
bone marrow transplantation (BMT) during childhood: EBMT
Late-Effects Working Party retrospective data. European Group for
Blood and Marrow Transplantation. Bone Marrow Transplant
1999;23:10431047.
29. McCann SR, Bacigalupo A, Gluckman E, et al. Graft rejection and
second bone marrow transplants for acquired aplastic anaemia: A
report from the Aplastic Anaemia Working Party of the European
Bone Marrow Transplant Group. Bone Marrow Transplant 1994;
13:233237.
30. Stucki A, Leisenring W, Sandmaier BM, et al. Decreased rejection
and improved survival of rst and second marrow transplants for
severe aplastic anemia (a 26-year retrospective analysis). Blood
1998;92:27422749.
31. Sasaki H, Ikuta K, Okuyama T, et al. The clinical course of acquired
aplastic anemia in childhood; a retrospective study. Int J Hematol
1994;60:239249.
32. Pitcher LA, Hann IM, Evans JP, et al. Improved prognosis for
acquired aplastic anaemia. Arch Dis Child 1999;80:158162.
33. Fuhrer M, Burdach S, Ebell W, et al. Relapse and clonal disease in
children with aplastic anemia (AA) after immunosuppressive
therapy (IST): The SAA 94 experience. German/Austrian
Pediatric Aplastic Anemia Working Group. Klin Padiatr 1998;
210:173179.
34. Niederwieser D, Pepe M, Storb R, et al. Improvement in rejection,
engraftment rate and survival without increase in graft-versus-host
disease by high marrow cell dose in patients transplanted for
aplastic anaemia. Br J Haematol 1988;69:2328.
35. Przepiorka D, Anderlini P, Saliba R, et al. Chronic graft-versus-host
disease after allogeneic blood stem cell transplantation. Blood
2001;98:16951700.
36. Schrezenmeier Hubert CB, Barbara Bruno, Fausto R, et al.
Comparison of allogeneic bone marrow and peripheral blood stem
cell transplantation for aplastic anemia: Collaborative Study of
European Blood and Marrow Transplant Group (EBMT) and
International Bone Marrow Transplant Registry (IBMTR). Blood
Suppl 2003;103:267a.
37. Min CK, Kim DW, Lee JW, et al. Hematopoietic stem cell
transplantation for high-risk adult patients with severe aplastic
anemia; reduction of graft failure by enhancing stem cell dose.
Haematologica 2001;86:303310.
38. Woodard P, Cunningham JM, Benaim E, et al. Effective donor
lymphohematopoietic reconstitution after haploidentical CD34
selected hematopoietic stem cell transplantation in children with
refractory severe aplastic anemia. Bone Marrow Transplant 2004;
33:411418.
39. Gluckman E, Rocha V, Chastang C. European results of unrelated
cord blood transplants. Eurocord group. Bone Marrow Transplant
1998;21:S87S91.
40. Wagner JE, Barker JN, DeFor TE, et al. Transplantation of
unrelated donor umbilical cord blood in 102 patients with mali-
gnant and nonmalignant diseases: Inuence of CD34 cell dose and
HLA disparity on treatment-related mortality and survival. Blood
2002;100:16111618.
41. Sanders JE. The impact of marrowtransplant preparative regimens
on subsequent growth and development. The Seattle Marrow
Transplant Team. Semin Hematol 1991;28:244249.
42. Sanders JE. Endocrine complications of high-dose therapy with
stem cell transplantation. Pediatr Transplant 2004;8:3950.
43. Eapen M, Ramsay NK, Mertens AC, et al. Late outcomes after bone
marrow transplant for aplastic anaemia. Br J Haematol 2000;111:
754760.
44. Deeg HJ, Leisenring W, Nims J. Long-termoutcome and quality of
life after marrow transplantation for severe aplastic anemia. Blood
Suppl 1996;88:643a.
45. Deeg HJ, Socle G, Schoch G, et al. Malignancies after marrow
transplantation for aplastic anemia and fanconi anemia: A joint
Seattle and Paris analysis of results in 700 patients. Blood 1996;
87:386392.
46. Champlin R, Ho W, Gale RP. Antithymocyte globulin treatment in
patients with aplastic anemia: A prospective randomized trial. N
Engl J Med 1983;308:113118.
47. Camitta BM, Storb R, Thomas ED. Aplastic anemia (second of two
parts): Pathogenesis, diagnosis, treatment, and prognosis. N Engl J
Med 1982;306:712718.
48. Bessho M, Hirashima K, Asano S, et al. Treatment of the anemia of
aplastic anemia patients with recombinant human erythropoietin in
combination with granulocyte colony-stimulating factor: A multi-
center randomized controlled study. Multicenter Study Group. Eur
J Haematol 1997;58:265272.
49. Frickhofen N, Kaltwasser JP. Immunosuppressive treatment of
aplastic anemia: A prospective, randomized multicenter trial
evaluating antilymphocyte globulin (ALG) versus ALG and
cyclosporin A. Blut 1988;56:191192.
50. Frickhofen N, Kaltwasser JP, Schrezenmeier H, et al. Treatment of
aplastic anemia with antilymphocyte globulin and methylpredni-
778 Kurre et al.
solone with or without cyclosporine. The German Aplastic Anemia
Study Group. N Engl J Med 1991;324:12971304.
51. Frickhofen N, Rosenfeld SJ. Immunosuppressive treatment of
aplastic anemia with antithymocyte globulin and cyclosporine.
Semin Hematol 2000;37:5668.
52. Rosenfeld S, Follmann D, Nunez O, et al. Antithymocyte globulin
and cyclosporine for severe aplastic anemia: Association between
hematologic response and long-term outcome. Jama 2003;289:
11301135.
53. Frickhofen N, Heimpel H, Kaltwasser JP, et al. Antithymocyte
globulin with or without cyclosporin A: 11-year follow-up of a
randomized trial comparing treatments of aplastic anemia. Blood
2003;101:12361242.
54. Bacigalupo A, Brand R, Oneto R, et al. Treatment of acquired
severe aplastic anemia: Bone marrow transplantation compared
with immunosuppressive therapyThe European Group for Blood
and Marrow Transplantation experience. Semin Hematol 2000;37:
6980.
55. Kojima S, Horibe K, Inaba J, et al. Long-term outcome of acquired
aplastic anaemia in children: Comparison between immunosup-
pressive therapy and bone marrow transplantation. Br J Haematol
2000;111:321328.
56. Matloub YH, Smith C, Bostrom B, et al. One course versus two
courses of antithymocyte globulin for the treatment of severe
aplastic anemia in children. J Pediatr Hematol Oncol 1997;19:
110114.
57. Schrezenmeier H, Marin P, Raghavachar A, et al. Relapse of
aplastic anaemia after immunosuppressive treatment: A report
from the European Bone Marrow Transplantation Group SAA
Working Party. Br J Haematol 1993;85:371377.
58. Nakao S, Takamatsu H, Chuhjo T, et al. Identication of a specic
HLA class II haplotype strongly associated with susceptibility to
cyclosporine-dependent aplastic anemia. Blood 1994;84:42574261.
59. Tichelli A, Gratwohl A, Nissen C, et al. Late clonal complications
in severe aplastic anemia. Leuk Lymphoma 1994;12:167175.
60. Stein RS, Means RT Jr, Krantz SB, et al. Treatment of aplastic
anemia with an investigational antilymphocyte serum prepared in
rabbits. Am J Med Sci 1994;308:338343.
61. Goldenberg NA, Graham DK, Liang X, et al. Successful treatment
of severe aplastic anemia in children using standardized immuno-
suppressive therapy with antithymocyte globulin and cyclosporine
A. Pediatr Blood Cancer 2004;43:718722.
62. Schrezenmeier H, Hinterberger W, Hows J, et al. Second
immunosuppressive tratment of patients with aplastic anemia not
responding to rst course of immunosuppression (IS) a report from
the Working party on severe Aplastic Anemia of the EBMT. Bone
Marrow Transplantation Suppl 1995;15:65a.
63. Socie G, Henry-Amar M, Bacigalupo A, et al. Malignant tumors
occurring after treatment of aplastic anemia. European Bone
Marrow Transplantation-Severe Aplastic Anaemia Working Party.
N Engl J Med 1993;329:11521157.
64. Appelbaum FR, Barrall J, Storb R, et al. Clonal cytogenetic
abnormalities in patients with otherwise typical aplastic anemia.
Exp Hematol 1987;15:11341139.
65. Mikhailova N, Sessarego M, Fugazza G, et al. Cytogenetic
abnormalities in patients with severe aplastic anemia. Haematolo-
gica 1996;81:418422.
66. Socie G, Rosenfeld S, Frickhofen N, et al. Late clonal diseases of
treated aplastic anemia. Semin Hematol 2000;37:91101.
67. Ohga S, Ohara A, Hibi S, et al. Treatment responses of childhood
aplastic anaemia with chromosomal aberrations at diagnosis. Br J
Haematol 2002;118:313319.
68. Maciejewski JP, Risitano A, Sloand EM, et al. Distinct clinical
outcomes for cytogenetic abnormalities evolving from aplastic
anemia. Blood 2002;99:31293135.
69. de Planque MM, Kluin-Nelemans HC, van Krieken HJ, et al.
Evolution of acquired severe aplastic anaemia to myelodysplasia
and subsequent leukaemia in adults. Br J Haematol 1988;70:
5562.
70. Kaito K, Kobayashi M, Katayama T, et al. Long-term administra-
tion of G-CSF for aplastic anaemia is closely related to the early
evolution of monosomy 7 MDS in adults. Br J Haematol 1998;
103:297303.
71. Kojima S, Tsuchida M, Matsuyama T. Myelodysplasia and
leukemia after treatment of aplastic anemia with G-CSF. N Engl
J Med 1992;326:12941295.
72. van der Schoot CE, Huizinga TW, vant Veer-Korthof ET, et al.
Deciency of glycosyl-phosphatidylinositol-linked membrane
glycoproteins of leukocytes in paroxysmal nocturnal hemoglobi-
nuria, description of a new diagnostic cytouorometric assay.
Blood 1990;76:18531859.
73. Maciejewski JP, Rivera C, Kook H, et al. Relationship between
bone marrow failure syndromes and the presence of glycopho-
sphatidyl inositol-anchored protein-decient clones. Br J Haematol
2001;115:10151022.
74. Mukhina GL, Buckley JT, Barber JP, et al. Multilineage
glycosylphosphatidylinositol anchor-decient haematopoiesis in
untreated aplastic anaemia. Br J Haematol 2001;115:476482.
75. Wang H, Chuhjo T, Yasue S, et al. Clinical signicance of a
minor population of paroxysmal nocturnal hemoglobinuria-
type cells in bone marrow failure syndrome. Blood 2002;100:
38973902.
76. Margolis D, Camitta B, Pietryga D, et al. Unrelated donor bone
marrow transplantation to treat severe aplastic anaemia in children
and young adults. Br J Haematol 1996;94:6572.
77. Henslee-Downey PJ, Abhyankar SH, Parrish RS, et al. Use of
partially mismatched related donors extends access to allogeneic
marrow transplant. Blood 1997;89:38643872.
78. Bacigalupo A, Hows J, Gordon-Smith EC, et al. Bone marrow
transplantation for severe aplastic anemia from donors other than
HLA identical siblings: A report of the BMT Working Party. Bone
Marrow Transplant 1988;3:531535.
79. Deeg HJ, Anasetti C, Petersdorf E, et al. Cyclophosphamide plus
ATG conditioning is insufcient for sustained hematopoietic
reconstitution in patients with severe aplastic anemia transplanted
with marrow from HLA-A, B, DRB matched unrelated donors.
Blood 1994;83:34173418.
80. Deeg HJ, Amylon ID, Harris RE, et al. Marrow transplants from
unrelated donors for patients with aplastic anemia: Minimum
effective dose of total body irradiation. Biol Blood Marrow
Transplant 2001;7:208215.
81. Vassiliou GS, Webb DK, Pamphilon D, et al. Improved outcome of
alternative donor bone marrow transplantation in children with
severe aplastic anaemia using a conditioning regimen containing
low-dose total body irradiation, cyclophosphamide and Campath.
Br J Haematol 2001;114:701705.
82. Kaltwasser JP, Dix U, Schalk KP, et al. Effect of androgens on the
response to antithymocyte globulin in patients with aplastic
anaemia. Eur J Haematol 1988;40:111118.
83. Bacigalupo A, Chaple M, Hows J, et al. Treatment of aplastic
anaemia (AA) with antilymphocyte globulin (ALG) and methyl-
prednisolone (MPred) with or without androgens: A randomized
trial from the EBMT SAA working party. Br J Haematol 1993;
83:145151.
84. Shahidi NT, Diamond LK. Testosterone-induced remission in
aplastic anemia of both acquired and congenital types. Further
observations in 24 cases. N Engl J Med 1961;264:953967.
85. Champlin RE, Ho WG, Feig SA, et al. Do androgens enhance the
response to antithymocyte globulin in patients with aplastic
anemia? Aprospective randomized trial. Blood 1985;66:184188.
Aplastic Anemia in Children 779
86. Bacigalupo A, van Lint MT, Frassoni F, et al. High dose bolus
methylprednisolone for the treatment of acute graft versus host
disease. Blut 1983;46:125132.
87. Tisdale JF, Dunn DE, Geller N, et al. High-dose cyclophosphamide
in severe aplastic anaemia: A randomised trial. Lancet 2000;356:
15541559.
88. Brodsky RA, Chen AR, Brodsky I, et al. High-dose cyclopho-
sphamide as salvage therapy for severe aplastic anemia. Exp
Hematol 2004;32:435440.
89. Tisdale JF, Dunn DE, Maciejewski J. Cyclophosphamide and other
new agents for the treatment of severe aplastic anemia. Semin
Hematol 2000;37:102109.
90. Maciejewski JP, Sloand EM, Nunez O, et al. Recombinant humanized
anti-IL-2 receptor antibody (daclizumab) produces responses in
patients with moderate aplastic anemia. Blood2003; 102:35843586.
91. Speck B, Tichelli A, Widmer E, et al. Splenectomy as an adjuvant
measure in the treatment of severe aplastic anaemia. Br J Haematol
1996;92:818824.
780 Kurre et al.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1091)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Sickle Cell AnemiaDokumen13 halamanSickle Cell AnemiaDr. Ashish JawarkarBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Bimanual Vaginal Examination - OSCE Guide - Geeky MedicsDokumen6 halamanBimanual Vaginal Examination - OSCE Guide - Geeky MedicsJahangir AlamBelum ada peringkat
- Nursing Bullets - Psychiatric NursingDokumen13 halamanNursing Bullets - Psychiatric NursingDr. Jayesh PatidarBelum ada peringkat
- Measles PDFDokumen3 halamanMeasles PDFdrpranandhaBelum ada peringkat
- Child Guidance ClinicDokumen22 halamanChild Guidance ClinicBinal Joshi67% (3)
- Bonica - Management of Pain 3rd Ed PDFDokumen1.484 halamanBonica - Management of Pain 3rd Ed PDFȘtefania Raluca Mănescu100% (1)
- Small For Gestational AgeDokumen14 halamanSmall For Gestational AgeMaria Delia Salvado100% (2)
- Treatment of Malar Mounds With Hyaluronic Acid Fillers - An Anatomical ApproachDokumen5 halamanTreatment of Malar Mounds With Hyaluronic Acid Fillers - An Anatomical ApproachArcelino FariasBelum ada peringkat
- Diabetic KetoacidosisDokumen41 halamanDiabetic KetoacidosisllaychinBelum ada peringkat
- Conservative Treatment of Early Postoperative Small Bowel Obstruction With Obliterative PeritonitisDokumen10 halamanConservative Treatment of Early Postoperative Small Bowel Obstruction With Obliterative Peritonitisalemago90Belum ada peringkat
- DARUNDAY - NCM 117 Asynchronous ActivityDokumen17 halamanDARUNDAY - NCM 117 Asynchronous ActivityEzra Miguel DarundayBelum ada peringkat
- Case-1 20230826 104209 0000Dokumen14 halamanCase-1 20230826 104209 0000paulzkieyyBelum ada peringkat
- Neuropathic Diabetic Foot Ulcers: Clinical PracticeDokumen8 halamanNeuropathic Diabetic Foot Ulcers: Clinical PracticeEgyFairuzPratiwiBelum ada peringkat
- ImmerciDokumen14 halamanImmercitextilessathishBelum ada peringkat
- Afework MelesseDokumen260 halamanAfework MelesseBefekadu BerhanuBelum ada peringkat
- Complex Torch Si SarcinaDokumen23 halamanComplex Torch Si SarcinamoldoveanuBelum ada peringkat
- Vasospasm: Endothelial Cell InjuryDokumen4 halamanVasospasm: Endothelial Cell InjuryPuja ArgaBelum ada peringkat
- Differential Diagnosis of Thoracic, Lumbar & Sacrum SpineDokumen59 halamanDifferential Diagnosis of Thoracic, Lumbar & Sacrum Spinekashmala afzalBelum ada peringkat
- Cushing - AddisonDokumen27 halamanCushing - AddisonMelissa-Andreea Ardeleanu Carvajal OsorioBelum ada peringkat
- Hubungan Self-Efficacy Dengan Tingkat Kepatuhan Minum Obat Pada Penderita HipertensiDokumen13 halamanHubungan Self-Efficacy Dengan Tingkat Kepatuhan Minum Obat Pada Penderita HipertensiArista jawamaraBelum ada peringkat
- College of Health Sciences: Kabacan, Cotabato PhilippinesDokumen2 halamanCollege of Health Sciences: Kabacan, Cotabato PhilippinesKervy JuntillaBelum ada peringkat
- Advancesinlocal Anesthesiain Dentistry: Orrett E. Ogle,, Ghazal MahjoubiDokumen19 halamanAdvancesinlocal Anesthesiain Dentistry: Orrett E. Ogle,, Ghazal Mahjoubicarlos gilbertoBelum ada peringkat
- ThyrotoxicosisDokumen16 halamanThyrotoxicosisFiorella Peña MoraBelum ada peringkat
- Post-ACLS Megacode Flashcards - QuizletDokumen9 halamanPost-ACLS Megacode Flashcards - QuizletMaya LaPradeBelum ada peringkat
- Madhav GuptaDokumen1 halamanMadhav GuptaLABBelum ada peringkat
- Kode ICD 10Dokumen4 halamanKode ICD 10Laela SariBelum ada peringkat
- Blinding in Clinical Trials: Patients' AcademyDokumen12 halamanBlinding in Clinical Trials: Patients' AcademyaravindBelum ada peringkat
- 25. London Cancer Guidelines for Administration of Systematic Anti-Cancer Therapy-محولDokumen106 halaman25. London Cancer Guidelines for Administration of Systematic Anti-Cancer Therapy-محولAnsam MohBelum ada peringkat
- DiclofenacDokumen3 halamanDiclofenacapi-37979410% (1)
- CABG Discharge Planning 1Dokumen16 halamanCABG Discharge Planning 1pipporudyBelum ada peringkat