Treatment of Hypocalcemia
Diunggah oleh
Loreto Pulido Q.Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Treatment of Hypocalcemia
Diunggah oleh
Loreto Pulido Q.Hak Cipta:
Format Tersedia
Official reprint from UpToDate
www.uptodate.com 2014 UpToDate
Author
David Goltzman, MD
Section Editor
Clifford J Rosen, MD
Deputy Editor
Jean E Mulder, MD
Treatment of hypocalcemia
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: May 2014. | This topic last updated: May 08, 2014.
INTRODUCTION Hypocalcemia may be associated with a spectrum of clinical manifestations, ranging from few
if any symptoms if the hypocalcemia is mild and/or chronic, to severe life-threatening symptoms if it is severe
and/or acute. Thus, the management of hypocalcemia depends upon the severity of symptoms. In patients with
acute symptomatic hypocalcemia, intravenous calcium gluconate is the preferred therapy, whereas chronic
hypocalcemia is treated with oral calcium and vitamin D supplements.
The treatment of hypocalcemia will be reviewed here. The etiology, clinical manifestations, and diagnostic approach
to hypocalcemia are reviewed separately. (See "Etiology of hypocalcemia in adults" and "Clinical manifestations of
hypocalcemia" and "Diagnostic approach to hypocalcemia".)
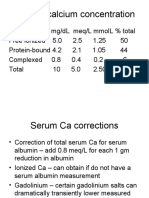
INTERPRETATION OF SERUM CALCIUM Calcium in serum is bound to proteins, principally albumin. As a
result, total serum calcium concentrations in patients with low or high serum albumin levels may not accurately
reflect the physiologically important ionized (or free) calcium concentration. As an example, in patients with
hypoalbuminemia, total serum calcium concentration may be low when serum ionized calcium is normal. The
serum total calcium concentration falls approximately 0.8 mg/dL for every 1 g/dL reduction in the serum albumin
concentration. Thus, in patients with hypoalbuminemia or hyperalbuminemia, the measured serum calcium
concentration should be corrected for the abnormality in albumin (calculator 1) or for standard units (calculator 2).
If there is uncertainty whether the corrected serum calcium is reflective of the ionized calcium, and if a laboratory
known to measure ionized calcium reliably is available, some authorities prefer to measure the ionized calcium
directly. Direct measurement of the ionized calcium concentration could be considered in patients with symptoms
of hypocalcemia in the setting of a normal total calcium concentration. Symptomatic hypocalcemia with normal
total calcium but low ionized calcium can occasionally occur in patients with acute respiratory alkalosis due to
increased binding of calcium to albumin. (See "Relation between total and ionized serum calcium concentrations",
section on 'Acid-base disorders'.)
In patients with asymptomatic hypocalcemia, it is important to verify with repeat measurement (ionized calcium or
total serum calcium corrected for albumin) that there is a true decrease in the calcium concentration.
THERAPEUTIC APPROACH The treatment of hypocalcemia varies with its severity and the underlying cause.
The severity of symptoms (paresthesias, carpopedal spasm, tetany, seizures) and signs (Chvostek's or
Trousseau's signs, bradycardia, impaired cardiac contractility, and prolongation of the QT interval) depends upon
the absolute level of calcium, as well as the rate of decrease. Patients with acute hypocalcemia will be
symptomatic at serum calcium values that would not cause symptoms in patients with chronic hypocalcemia (eg,
hypoparathyroidism). Clinical manifestations also vary with other factors such as the arterial pH and the cause of
hypocalcemia. (See "Clinical manifestations of hypocalcemia".)
There are few studies examining the optimal treatment of hypocalcemia. Most recommendations are based upon
accepted practice or clinical experience [1-3]. We recommend intravenous calcium for symptomatic patients
(carpopedal spasm, tetany, seizures), for patients with a prolonged QT interval, and for asymptomatic patients with
an acute decrease in serum corrected calcium to 7.5 mg/dL (1.9 mmol/L). For those with milder symptoms of
neuromuscular irritability (paresthesias) and corrected calcium concentrations greater than 7.5 mg/dL, oral calcium
supplementation can be initiated. If symptoms do not improve with oral supplementation, we recommend switching
to intravenous calcium.
When vitamin D deficiency or hypoparathyroidism is the cause of hypocalcemia, administration of calcium alone is
usually only transiently effective. Long-term management requires the addition of vitamin D. Recombinant human
parathyroid hormone is approved for the treatment of osteoporosis but is not yet standard care for
hypoparathyroidism because of high cost and the necessity for subcutaneous administration. (See 'Recombinant
human PTH' below.)
Intravenous calcium Intravenous calcium is indicated for acutely symptomatic patients, as can occur when
there is a rapid and progressive reduction in serum calcium (eg, acute hypoparathyroidism following post-radical
neck dissection for head and neck cancer). It is also indicated for asymptomatic hypocalcemia in several other
settings. These include patients with acute decreases in serum calcium to 7.5 mg/dL (1.9 mmol/L) who may
develop serious complications if untreated, and patients with milder degrees of hypocalcemia or with chronic
hypocalcemia (due to hypoparathyroidism) who become unable to take or absorb oral supplements, as may occur
after complex surgical procedures requiring prolonged recuperation.
Intravenous calcium is not warranted as initial therapy for asymptomatic hypocalcemia in patients with impaired
renal function in whom correction of hyperphosphatemia and of low circulating 1,25-dihyroxyvitamin D are usually
the primary goals. (See 'Chronic kidney disease' below.)
Initially, intravenous calcium (1 to 2 g of calcium gluconate, equivalent to 90 to 180 mg elemental calcium, in 50 mL
of 5 percent dextrose) can be infused over 10 to 20 minutes. The calcium should not be given more rapidly,
because of the risk of serious cardiac dysfunction, including systolic arrest [4]. This dose of calcium gluconate will
raise the serum calcium concentration for only two or three hours; as a result, it should be followed by a slow
infusion of calcium in patients with persistent hypocalcemia.
Either 10 percent calcium gluconate (90 mg of elemental calcium per 10 mL) or 10 percent calcium chloride (270
mg of elemental calcium per 10 mL) can be used to prepare the infusion solution. Calcium gluconate is usually
preferred because it is less likely to cause tissue necrosis if extravasated.
An intravenous solution containing 1 mg/mL of elemental calcium is prepared by adding 11 g of calcium gluconate
(equivalent to 990 mg elemental calcium) to normal saline or 5 percent dextrose water to provide a final volume of
1000 mL. This solution is administered at an initial infusion rate of 50 mL/hour (equivalent to 50 mg/hour). The dose
can be adjusted to maintain the serum calcium concentration at the lower end of the normal range (with the serum
calcium corrected for any abnormalities in serum albumin as noted above). Patients typically require 0.5 to 1.5
mg/kg of elemental calcium per hour.
The infusion should be prepared with the following considerations:
Intravenous calcium should be continued until the patient is receiving an effective regimen of oral calcium and
vitamin D. Calcitriol, in a dose of 0.25 to 0.5 mcg twice daily, is the preferred preparation of vitamin D for patients
with severe acute hypocalcemia because of its rapid onset of action (hours). (See 'Vitamin D and metabolites'
below.)
Concurrent hypomagnesemia Hypomagnesemia is a common cause of hypocalcemia, both by inducing
resistance to parathyroid hormone (PTH) and by diminishing its secretion. (See "Clinical manifestations of
magnesium depletion".)
The calcium should be diluted in dextrose and water or saline because concentrated calcium solutions are
irritating to veins.
The intravenous solution should not contain bicarbonate or phosphate, which can form insoluble calcium salts.
If these anions are needed, another intravenous line (in another limb) should be used.
In patients with hypomagnesemia, hypocalcemia is difficult to correct without first normalizing the serum
magnesium concentration. Thus, if the serum magnesium concentration is low, 2 g (16 mEq) of magnesium sulfate
should be infused as a 10 percent solution over 10 to 20 minutes, followed by 1 gram (8 mEq) in 100 mL of fluid per
hour. Magnesium repletion should be continued as long as the serum magnesium concentration is less than 0.8
mEq/L (1 mg/dL or 0.4 mmol/L). More careful monitoring is required in patients who have impaired renal function
who would be at greater risk of developing hypermagnesemia.
Persistent hypomagnesemia, as occurs in some patients with ongoing gastrointestinal (eg, malabsorption) or renal
losses, requires supplementation with oral magnesium, typically 300 to 400 mg daily divided into three doses. (See
"Causes of hypomagnesemia" and "Evaluation and treatment of hypomagnesemia".)
Oral calcium Oral calcium supplementation is preferred for patients with milder degrees of acute hypocalcemia
(serum corrected calcium concentration of 7.5 to 8.0 mg/dL [1.9 to 2.0 mmol/L] or a serum ionized calcium
concentration above 3.0 to 3.2 mg/dL [0.8 mmol/L]) or for chronic hypocalcemia. Such patients are typically
asymptomatic or at most mildly symptomatic (eg, oral paresthesias). They can be treated initially with 1500 to
2000 mg of elemental calcium given as calcium carbonate or calcium citrate daily, in divided doses. As an
example, calcium carbonate is 40 percent elemental calcium, so that 1250 mg of calcium carbonate contains 500
mg of elemental calcium. The dose of elemental calcium is listed on most supplement labels.
The role of oral calcium as a phosphate binder in patients with chronic kidney disease is presented elsewhere. (See
"Treatment of hyperphosphatemia in chronic kidney disease".)
In addition to calcium, patients with vitamin D deficiency or hypoparathyroidism require vitamin D supplementation,
which often permits a lower dose of calcium supplementation. (See 'Hypoparathyroidism' below and 'Vitamin D
deficiency' below.)
Vitamin D and metabolites Several preparations of vitamin D are available for the treatment of hypocalcemia
due to hypoparathyroidism or vitamin D deficiency. The role of vitamin D therapy in patients with chronic kidney
disease is discussed separately. (See "Management of secondary hyperparathyroidism and mineral metabolism
abnormalities in dialysis patients" and "Management of secondary hyperparathyroidism and mineral metabolism
abnormalities in adult predialysis patients with chronic kidney disease".)
Vitamin D requirements vary considerably from patient to patient and the correct dose in any given patient is
primarily determined by trial and error. Because PTH is required for the renal conversion of calcidiol (25-
hydroxyvitamin D) to the active metabolite calcitriol (1,25-dihydroxyvitamin D), patients with hypoparathyroidism are
preferably treated with calcitriol. The initial dose of calcitriol is typically 0.25 to 0.5 mcg twice daily.
The various preparations differ in onset of action, duration of action, and cost. The major side effects are
hypercalcemia and hypercalciuria, which, if chronic, can cause nephrolithiasis, nephrocalcinosis, and renal failure
[5,6]. Hypercalciuria is the earliest sign of toxicity and can develop in the absence of hypercalcemia; it is most
likely to occur in patients with hypoparathyroidism since parathyroid hormone stimulates renal calcium
reabsorption. However, in patients with vitamin D deficiency, enhanced intestinal absorption of calcium with vitamin
D therapy and the resulting increases in serum calcium may also reduce PTH concentrations, potentially resulting
in hypercalciuria before hypercalcemia occurs. Thus, both serum and urinary calcium should be measured
frequently (two-week intervals) initially and then every six months to one year once a stable dose is achieved.
Hypercalciuria and, if present, hypercalcemia usually resolve in a few days after cessation of therapy in patients
treated with calcitriol. In contrast, recovery is slower (as long as two to three weeks because of storage in fat) in
patients treated with vitamin D, but can be accelerated by a short course of glucocorticoid therapy. (See "Treatment
of hypercalcemia".)
Vitamin D Vitamin D deficiency is typically treated with ergocalciferol (vitamin D2) or cholecalciferol (vitamin
D3). Vitamin D is available in several doses for oral administration. In some countries (not in the United States), it is
also available for parenteral administration. (See "Vitamin D deficiency in adults: Definition, clinical manifestations,
and treatment", section on 'Preparations'.)
The major advantage of vitamin D is its low cost, which is approximately 20 percent that of the vitamin D
metabolites. Disadvantages include the necessity for hepatic and renal metabolism and slow onset and long
duration of action. It must be given each day for several weeks before the full effect becomes evident and
hypercalcemia, should it occur, can persist for two to three weeks after it is discontinued.
Calcitriol Calcitriol (1,25-dihydroxyvitamin D, Rocaltrol) is most useful in diseases in which its renal
synthesis is impaired, such as renal failure or hypoparathyroidism. It is the most active metabolite of vitamin D. The
advantages of calcitriol include lack of necessity for endogenous activation, rapid onset of action (hours), and a
biologic half-life of about four to six hours. While hypercalcemia is more common during treatment with calcitriol
than with vitamin D, cessation of treatment is followed by resolution of hypercalcemia in a few days rather than a
few weeks [5,6].
Other vitamin D analogues Vitamin D metabolites can be used to treat hypocalcemia, particularly when
there is abnormal vitamin D metabolism (renal or liver disease). The recommended preparation and dose vary with
the clinical condition. (See "Overview of vitamin D", section on 'Metabolism'.)
DISEASE SPECIFIC APPROACH
Hypoparathyroidism Hypoparathyroidism occurs when there is abnormal parathyroid gland development,
destruction of the parathyroid glands (autoimmune, surgical), altered regulation of parathyroid hormone (PTH)
production, or impaired PTH action. (See "Etiology of hypocalcemia in adults".)
Most patients with hypoparathyroidism require lifelong calcium and vitamin D supplementation. An exception is the
occurrence of transient hypoparathyroidism after thyroidectomy or parathyroidectomy. (See 'Thyroidectomy or
parathyroidectomy' below.)
The goals of therapy in patients with hypoparathyroidism are to relieve symptoms and to raise and maintain the
serum calcium concentration in the low-normal range, eg, 8.0 to 8.5 mg/dL (2.0 to 2.1 mmol/L). Attainment of
higher values is not necessary and is usually limited by the development of hypercalciuria due to the loss of renal
calcium retaining effects of PTH. (See 'Preventing hypercalciuria' below.)
The initial dose of oral calcium should be 1.0 to 1.5 g of elemental calcium daily, in divided doses [8]. Although
calcium carbonate is often used (it is the least expensive), it may be less well-absorbed in older patients and those
who have achlorhydria. These patients might be treated with another preparation, such as calcium citrate. Although
a variety of vitamin D preparations can be used to treat hypoparathyroidism (table 1), calcitriol is often regarded as
the treatment of choice [8,9]. A typical starting dose is 0.25 mcg twice daily, with weekly dose increments to
Alfacalcidol (1-alpha-hydroxyvitamin D3) is a synthetic analog of vitamin D that is converted in the liver to the
active metabolite 1,25-dihydroxyvitamin D. Similar to calcitriol, it has a rapid onset of action and relatively
short half-life. Although it is not available in the United States, it is used in other countries for the treatment of
hypocalcemia associated with hypoparathyroidism [7] and as a treatment adjunct in chronic kidney disease.
(See "Management of secondary hyperparathyroidism and mineral metabolism abnormalities in dialysis
patients" and "Management of secondary hyperparathyroidism and mineral metabolism abnormalities in adult
predialysis patients with chronic kidney disease".)
Dihydrotachysterol is the functional equivalent of 1-hydroxyvitamin D, in that only 25-hydroxylation in the liver
is required to form the active drug. As a result, dihydrotachysterol is effective in patients in whom renal 1-
hydroxylation is impaired, such as those with chronic kidney disease. It has a rapid onset of action and a
relatively short duration of action, so that toxicity resolves in a few days.
Calcidiol (25-hydroxyvitamin D) does not require hepatic 25-hydroxylation, and is therefore most useful in
patients with liver disease. Its action is more rapid and not as prolonged as that of vitamin D, but slower in
onset and more prolonged than that of calcitriol.
achieve a low-normal serum calcium. Many patients require up to 2 mcg daily.
Monitoring of urinary and serum calcium and serum phosphate are required weekly initially, until a stable serum
calcium concentration (at the low end of the normal range) is reached. Thereafter, monitoring at three- to six-month
intervals is sufficient [10].
Preventing hypercalciuria An increase in urinary calcium excretion is a predictable consequence of raising
the serum calcium in patients with hypoparathyroidism [11]. These patients lack the normal stimulatory effect of
PTH on renal tubular calcium reabsorption [12], and therefore excrete more calcium than normal subjects at the
same serum calcium concentration.
Thus, completely correcting hypocalcemia may lead to hypercalciuria, which can produce nephrolithiasis,
nephrocalcinosis, and possible chronic kidney disease [13]. To prevent these complications, urinary calcium
excretion should be measured periodically and the dose of calcium and vitamin D reduced if it is elevated (300 mg
in 24 hours).
Some patients with hypoparathyroidism require a thiazide diuretic (25 to 100 mg daily), with or without dietary
sodium restriction, to decrease urinary calcium excretion [14,15]. A thiazide is typically added when the 24-hour
urinary calcium approaches 250 mg [8]. In patients who develop thiazide-induced hypokalemia, potassium
supplementation is necessary. The mechanism by which both PTH and thiazides enhance distal calcium
reabsorption is reviewed elsewhere. (See "Diuretics and calcium balance".)
Recombinant human PTH The administration of recombinant parathyroid hormone (PTH), which is available
for the treatment of osteoporosis, holds promise as a treatment for hypoparathyroidism [13,16-22]. Subcutaneous
administration of PTH 1-34 and PTH 1-84 have been investigated, as illustrated by the following:
Recombinant human PTH may also improve abnormal skeletal properties in hypoparathyroidism. In a
histomorphometric analysis of paired iliac crest biopsy samples from 30 patients with primary hypoparathyroidism,
PTH treatment of hypoparathyroidism was associated with an increase in the remodeling rate in both trabecular and
cortical compartments with tunneling resorption in the trabecular compartments [20]. These findings suggest that
PTH restores bone metabolism to levels more typical of euparathyroid individuals.
Recombinant human PTH is not yet approved for use in hypoparathyroidism, primarily since the long-term safety of
this dose (relative to its skeletal effects) has not been established, particularly in growing children who may be at
greater risk of osteosarcoma. In addition, recombinant PTH is much more expensive than standard therapy with
calcitriol and calcium. (See "Parathyroid hormone therapy for osteoporosis".)
Thyroidectomy or parathyroidectomy Hypocalcemia is a common problem after total or near-total
thyroidectomy and partial or total parathyroidectomy in patients with primary hyperparathyroidism.
As an example, hypoparathyroidism is the most frequent complication of near-total thyroidectomy. Transient
hypoparathyroidism occurs in up to 20 percent of patients after surgery for thyroid cancer and permanent
hypoparathyroidism occurs in 0.8 to 3.0 percent of patients after total thyroidectomy, particularly when the goiter is
In two randomized trials from the same group, subcutaneous administration of synthetic PTH 1-34 controlled
hypocalcemia with a lower risk of hypercalciuria when compared with calcitriol (all subjects received oral
calcium supplementation) [13,16]. Twice-daily administration of PTH 1-34 provided better metabolic control
and allowed a reduction in total daily PTH dose (46 versus 97 mcg daily) [17]. Similar findings were noted in a
trial comparing once- versus twice-daily PTH administration in 14 children with chronic hypoparathyroidism
(total daily dose 25 versus 58 mcg) [18].
In an open label study of PTH 1-84 (100 mcg every other day) in 30 hypoparathyroid patients, PTH 1-84
significantly reduced supplemental calcium and calcitriol requirements without altering serum and urinary
calcium concentrations [19]. Bone mineral density significantly increased in the lumbar spine (2.9 percent)
and decreased in the distal one-third radius (2.4 percent).
extensive and anatomic landmarks are displaced and obscured. The management of post-thyroidectomy
hypoparathyroidism is reviewed elsewhere. (See "Differentiated thyroid cancer: Surgical treatment", section on
'Hypoparathyroidism' and "Surgery in the treatment of hyperthyroidism: Indications, preoperative preparation, and
postoperative follow-up", section on 'Hypocalcemia'.)
Vitamin D deficient patients undergoing parathyroidectomy are at increased risk for developing postoperative
hypocalcemia and hungry bone syndrome [23]. Hungry bone syndrome most often occurs in hyperparathyroid
patients who developed bone disease preoperatively due to a chronic increase in bone resorption induced by high
levels of PTH (osteitis fibrosa). In these patients, calcium is avidly taken up by the demineralized bone after
surgery, and calcium supplementation is required to maintain a normal serum calcium concentration. Vitamin D
deficient postparathyroidectomy patients may require prolonged, massive calcium and vitamin D therapy due to
hungry bone syndrome. (See "Clinical manifestations of primary hyperparathyroidism", section on 'Classical
manifestations' and "Hungry bone syndrome following parathyroidectomy", section on 'Treatment'.)
Hypoparathyroidism during pregnancy Special care should be taken in the management of women with
hypoparathyroidism during pregnancy and following delivery. There are conflicting data as to whether calcitriol
requirements fall [24-26] or do not fall during pregnancy [27-31]. On the other hand, there is uniform agreement that
calcitriol requirements decrease during lactation [24-26,30,32,33].
Serum concentrations of 1,25-dihyroxyvitamin D (calcitriol) double during a normal pregnancy. However, intact PTH
concentrations remain low-to-normal, suggesting that PTH does not mediate the late partum rise in 1,25-
dihydroxyvitamin D (1,25D) production. The increase in serum 1,25D may be regulated by other pregnancy
hormones, which are normal in hypoparathyroid women, such as PTH-related protein (PTHrP), prolactin, estrogen,
and placental growth hormone [24,32,34].
Thus, serum calcium concentrations should be measured frequently during late pregnancy and lactation in women
with hypoparathyroidism who may have a rise in serum calcium, requiring a decrease in calcitriol dose [24-26,32]. If
the calcitriol dose is not reduced, the combination of elevated serum 1,25D and PTHrP can lead to increases in
intestinal absorption and bone resorption and hypercalcemia [30]. The requirement for calcitriol will return to
antepartum levels with cessation of lactation.
Autosomal dominant hypocalcemia Autosomal dominant hypocalcemia is a rare disorder caused by an
activating mutation in the calcium-sensing receptor (CaSR). Increased activity of this receptor in the renal tubules
results in normal or high urinary calcium excretion despite hypocalcemia; raising the patient's serum calcium
concentrations with vitamin D can result in more hypercalciuria, nephrocalcinosis, and renal insufficiency.
Fortunately, most patients with this disorder have few if any symptoms of hypocalcemia and usually require little or
no therapy. When approved, recombinant human parathyroid hormone, which enhances calcium absorption in the
tubules, may be an alternative if therapy is needed. It can raise the serum calcium concentration in this disorder
with a low risk of exacerbating hypercalciuria. Alternatively, calcilytics, a class of drugs in development that inhibit
the CaSR, may provide a useful therapeutic approach in the future. (See "Disorders of the calcium-sensing
receptor: Familial hypocalciuric hypercalcemia and autosomal dominant hypocalcemia", section on 'Autosomal
dominant hypocalcemia'.)
Vitamin D deficiency Nutritional vitamin D deficiency is typically treated with 50,000 international units of
vitamin D2 or D3 weekly for six to eight weeks. (See "Vitamin D deficiency in adults: Definition, clinical
manifestations, and treatment".)
Chronic kidney disease Few patients with chronic kidney disease have symptomatic hypocalcemia. Such
patients are often treated with oral calcium to bind intestinal phosphate and to prevent bone disease rather than
hypocalcemia per se. The addition of an active form of vitamin D is required in some of these patients. These issues
are discussed in detail elsewhere. (See "Treatment of hyperphosphatemia in chronic kidney disease" and
"Management of secondary hyperparathyroidism and mineral metabolism abnormalities in dialysis patients" and
"Management of secondary hyperparathyroidism and mineral metabolism abnormalities in adult predialysis patients
with chronic kidney disease".)
Hypercatabolic state Unless they are symptomatic from hypocalcemia (eg, tetany or cardiac arrhythmia),
patients with acute hypocalcemia and hyperphosphatemia due to a hypercatabolic state such as the tumor lysis
syndrome or massive trauma should not be treated with calcium until the hyperphosphatemia is corrected to
prevent calcium-phosphate precipitation. Hemodialysis is often indicated in such patients who have symptomatic
hypocalcemia. (See "Tumor lysis syndrome: Prevention and treatment", section on 'Treatment of established TLS'.)
Pseudohypoparathyroidism Pseudohypoparathyroidism (PHP) refers to a group of heterogeneous disorders
defined by targeted organ (kidney and, perhaps, bone) unresponsiveness to PTH [35]. It is characterized by
hypocalcemia, hyperphosphatemia, and in contrast to hypoparathyroidism, elevated rather than reduced PTH
concentrations. The clinical manifestations and diagnosis of this disorder are reviewed elsewhere. (See "Etiology of
hypocalcemia in infants and children", section on 'End-organ resistance/pseudohypoparathyroidism'.)
The long-term treatment of hypocalcemia in adults with pseudohypoparathyroidism is similar to the treatment of
hypocalcemia caused by other forms of hypoparathyroidism. However, patients with pseudohypoparathyroidism
infrequently develop hypercalciuria with calcium and vitamin D therapy [35]. Therefore, the goal of treatment with
calcium and vitamin D is to maintain normocalcemia (rather than low-normal serum calcium as for other forms of
hypoparathyroidism). A typical starting dose of calcitriol is 0.25 mcg twice daily. The dose should be increased
weekly to achieve a normal serum calcium. Many patients require up to 2 mcg daily [36]. Approximately 1 to 2 gm
of elemental calcium daily (in divided doses) is recommended.
Patients with pseudohypoparathyroidism may also require screening for other endocrinopathies, particularly
hypothyroidism and hypogonadism.
INFORMATION FOR PATIENTS UpToDate offers two types of patient education materials, The Basics and
Beyond the Basics. The Basics patient education pieces are written in plain language, at the 5 to 6 grade
reading level, and they answer the four or five key questions a patient might have about a given condition. These
articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the
Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the
10 to 12 grade reading level and are best for patients who want in-depth information and are comfortable with
some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these
topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on
patient info and the keyword(s) of interest.)
SUMMARY AND RECOMMENDATIONS
Calcium The treatment of hypocalcemia varies with its severity and the underlying cause.
th th
th th
Basics topics (see "Patient information: Hypoparathyroidism (The Basics)")
Patients with hypocalcemia who are severely symptomatic (carpopedal spasm, tetany, seizures, decreased
cardiac function, or prolonged QT interval) require rapid correction of calcium levels with IV calcium therapy.
We also suggest IV calcium therapy in asymptomatic patients with an acute decrease in serum corrected
calcium to 7.5 mg/dL (1.9 mmol/L) (Grade 2C). (See 'Intravenous calcium' above.)
Intravenous calcium is NOT warranted as initial therapy for asymptomatic hypocalcemia in patients with
impaired renal function in whom correction of hyperphosphatemia and of low circulating 1,25-dihyroxyvitamin D
are usually the primary goals. (See 'Intravenous calcium' above and 'Chronic kidney disease' above.)
For those with milder symptoms of neuromuscular irritability (paresthesias) and corrected serum calcium
concentrations greater than 7.5 mg/dL (1.9 mmol/L), initial treatment with oral calcium supplementation is
sufficient. (See 'Oral calcium' above.) If symptoms do not improve with oral supplementation, intravenous
calcium infusion is required.
Vitamin D When hypoparathyroidism (transient or permanent) or vitamin D deficiency are the cause of
hypocalcemia, administration of intravenous calcium is only transiently effective (as long as the infusion continues),
and oral calcium may not be well absorbed. In these cases, successful management requires the addition of
vitamin D, which often permits a lower dose of calcium supplementation.
Permanent hypoparathyroidism
Use of UpToDate is subject to the Subscription and License Agreement.
Topic 826 Version 26.0
To effectively treat hypocalcemia in patients with concurrent magnesium deficiency, hypomagnesemia should
be corrected first. (See 'Concurrent hypomagnesemia' above.)
For the initial management of patients with hypoparathyroidism, we recommend vitamin D supplementation in
addition to calcium (Grade 1A). Calcitriol is the vitamin D metabolite of choice because it does not require
renal activation, it has a rapid onset of action (hours), and a shorter half-life. Other acceptable options include
alfacalcidol, vitamin D (ergocalciferol or cholecalciferol), or dihydrotachysterol (table 1). (See 'Vitamin D and
metabolites' above.)
In individuals with hypocalcemia due to vitamin D deficiency, we recommend vitamin D repletion (Grade 1A).
Nutritional deficiency (25OHD <20 ng/mL [50 nmol/L]) requires initial treatment with 50,000 units of vitamin D2
or D3 orally once per week for six to eight weeks, and then 800 to 1000 international units of vitamin D3 daily
thereafter. (See "Vitamin D deficiency in adults: Definition, clinical manifestations, and treatment".)
In patients with permanent hypoparathyroidism, the goals of therapy are to relieve symptoms, to raise and
maintain the serum calcium concentration in the low-normal range (eg, 8.0 to 8.5 mg/dL [2.0 to 2.1 mmol/L]),
and to avoid hypercalciuria (maintain 24-hour urinary calcium below 300 mg). (See 'Hypoparathyroidism'
above.)
All patients with permanent hypoparathyroidism require adequate calcium intake (1.0 to 1.5 g elemental
calcium daily). (See 'Hypoparathyroidism' above.)
Along with calcium supplementation, we suggest calcitriol rather than recombinant human parathyroid
hormone (PTH) (Grade 2B). The long-term safety of PTH has not been established. In addition, recombinant
PTH is much more expensive than standard therapy with calcitriol. However, in patients with refractory
hypercalciuria, PTH is a reasonable option. (See 'Recombinant human PTH' above.)
The initial treatment of hypercalciuria in patients with hypoparathyroidism is reducing the dose of calcium and
vitamin D. Some patients will require the addition of thiazide diuretics. (See 'Preventing hypercalciuria' above.)
GRAPHICS
Treatment of hypoparathyroidism
Treatment Dosage
Calcium 1.0-1.5 g elemental daily (total diet + supplement) in
divided doses
Adjust dose as needed to control symptoms and maintain
low-normal serum calcium concentration
Vitamin D
Calcitriol 0.5-1.0 micgrograms daily (in divided doses)
Alfacalcidol 0.5-2.0 micrograms daily (in divided doses)
Ergocalciferol (D2) 25,000-100,000 International Units daily
Cholecalciferol (D3)
Dihydrotachysterol 0.2-1.2 mg daily
Thiazide diuretics (if required to
control hypercalciuria)
25-100 mg daily
Data from: Goltzman, D, Cole, DEC. Hypoparathyroidism. In Primer on the Metabolic Bone Diseases and
Disorders of Mineral Metabolism, American Society of Bone and Mineral Research 2006; 6:216.
Graphic 58328 Version 1.0
Anda mungkin juga menyukai
- Hypercalcemia Treatment UptodateDokumen25 halamanHypercalcemia Treatment UptodateNatalia Vasquez MedicoBelum ada peringkat
- How Is Hypokalaemia Treated in Adults?: Medicines Q&AsDokumen6 halamanHow Is Hypokalaemia Treated in Adults?: Medicines Q&AsNotForAbuseBelum ada peringkat
- TreatmentDokumen2 halamanTreatmentJaymark PolicarpioBelum ada peringkat
- HypocalcemiaDokumen12 halamanHypocalcemiaKrinessa May100% (1)
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Treatment - UpToDateDokumen20 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults Treatment - UpToDateSteffBelum ada peringkat
- Managing Hyperkalemia in CKD PatientsDokumen8 halamanManaging Hyperkalemia in CKD PatientsPratik TripathiBelum ada peringkat
- Calcium Gluconate Dosage PlusDokumen8 halamanCalcium Gluconate Dosage PlusJaved ArifBelum ada peringkat
- Treatment and Prevention of Hyperkalemia in Adults - UpToDateDokumen24 halamanTreatment and Prevention of Hyperkalemia in Adults - UpToDateJosé Abraham Amaya DuarteBelum ada peringkat
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentDokumen35 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: TreatmentyorghiLBelum ada peringkat
- Uworld Notes CK PDFDokumen123 halamanUworld Notes CK PDFNik KalairBelum ada peringkat
- Acute Treatment of Hypocalcaemia (Adults)Dokumen2 halamanAcute Treatment of Hypocalcaemia (Adults)Ahed WarwarBelum ada peringkat
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults TreatmentDokumen25 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults TreatmentGabriel MarçalBelum ada peringkat
- Treatment and Prevention of Hyperkalemia in AdultsDokumen34 halamanTreatment and Prevention of Hyperkalemia in Adultsr33realBelum ada peringkat
- Paper Reduction Project Progress Report Doc in White Blue Lines Style - 20240211 - 160421 - ٠٠٠٠Dokumen35 halamanPaper Reduction Project Progress Report Doc in White Blue Lines Style - 20240211 - 160421 - ٠٠٠٠Ryan ReBelum ada peringkat
- Hypokalemic Periodic ParalysisDokumen5 halamanHypokalemic Periodic ParalysisyanamatshahBelum ada peringkat
- Hiperkalemia PDFDokumen26 halamanHiperkalemia PDFJesús Arnoldo Vargas OntiverosBelum ada peringkat
- HyperkalaemiaDokumen6 halamanHyperkalaemiaSSBelum ada peringkat
- ERC Guidelines 2005 Cardiac Arrest in Special CircunstancesDokumen36 halamanERC Guidelines 2005 Cardiac Arrest in Special CircunstancesJoãoBrasil100% (2)
- Groman 2012Dokumen5 halamanGroman 2012EFRAIN CARDENAS MENDOZABelum ada peringkat
- HyperkalaemiaDokumen1 halamanHyperkalaemiaRekaBBelum ada peringkat
- Causes of Hypokalemia in AdultsDokumen23 halamanCauses of Hypokalemia in AdultsOmar Armando Gutiérrez DuránBelum ada peringkat
- Hipopotasemia en AdultosDokumen25 halamanHipopotasemia en AdultosMishu LlerenaBelum ada peringkat
- New Guidelines For Potassium ReplacementDokumen33 halamanNew Guidelines For Potassium ReplacementAnggry MambaitBelum ada peringkat
- Guidelines For The Management Of: Kurdistan Higher Council For Medical SpecialtiesDokumen6 halamanGuidelines For The Management Of: Kurdistan Higher Council For Medical SpecialtiesCik JaaBelum ada peringkat
- Treatment of hypernatremia in adults - UpToDateDokumen34 halamanTreatment of hypernatremia in adults - UpToDateAlexander ZepedaBelum ada peringkat
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: Treatment - UpToDateDokumen23 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults: Treatment - UpToDateAlex KuliaBelum ada peringkat
- HypocalcemiaDokumen34 halamanHypocalcemiaClaudia IrimieBelum ada peringkat
- Jurnal Reading MandiriDokumen5 halamanJurnal Reading MandiriRio PotterBelum ada peringkat
- Approach ConsiderationsDokumen5 halamanApproach ConsiderationsGunawan SetiawanBelum ada peringkat
- Clinical Manifestations and Treatment of Hypokalemia in Adults - UpToDateDokumen22 halamanClinical Manifestations and Treatment of Hypokalemia in Adults - UpToDateNguyễn Trịnh Xuân HợpBelum ada peringkat
- Case 11 DM1 Rev'dDokumen3 halamanCase 11 DM1 Rev'dngBelum ada peringkat
- Clinical Manifestations and Treatment of Hypokalemia in AdultsDokumen25 halamanClinical Manifestations and Treatment of Hypokalemia in Adultsr33realBelum ada peringkat
- Clinical Manifestations and Treatment of Hypokalemia in AdultsDokumen31 halamanClinical Manifestations and Treatment of Hypokalemia in AdultsJansonBelum ada peringkat
- Calcitriol, Calcium Carbonate and Zinc Capsules Calzem CompositionDokumen5 halamanCalcitriol, Calcium Carbonate and Zinc Capsules Calzem CompositionAnjali MongaBelum ada peringkat
- Tratamiento Hipernatremia UptodateDokumen36 halamanTratamiento Hipernatremia UptodateNatalia Vasquez MedicoBelum ada peringkat
- Potassium Disorders by AiyraDokumen25 halamanPotassium Disorders by AiyraAnndrea IlhamBelum ada peringkat
- AntibioticsDokumen13 halamanAntibioticsVjfsyuiBelum ada peringkat
- PLAN1Dokumen3 halamanPLAN1Raya Ibarra LumogdangBelum ada peringkat
- IRIS 2009 Treatment Recommendations SummaryDokumen5 halamanIRIS 2009 Treatment Recommendations SummaryJessicaHernandezBelum ada peringkat
- Hemodialysis Treatment in Patients With Severe Electrolyte DisordersDokumen8 halamanHemodialysis Treatment in Patients With Severe Electrolyte DisordersRESIDENTES MEDICINA INTERNABelum ada peringkat
- Reading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Dokumen15 halamanReading Synthesis # 2: San Roque Extension, Roxas City, Capiz, Philippines 5800Jay VillasotoBelum ada peringkat
- Causes of Hypokalemia in AdultsDokumen18 halamanCauses of Hypokalemia in AdultsTessa AcostaBelum ada peringkat
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- DKADokumen6 halamanDKAtiffarub91% (11)
- HypokalemiaDokumen7 halamanHypokalemiaNader SmadiBelum ada peringkat
- Cetoacidosis MetabolicaDokumen36 halamanCetoacidosis MetabolicaHector ArandaBelum ada peringkat
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults - Treatment - UpToDateDokumen36 halamanDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic State in Adults - Treatment - UpToDateHiKa SaGoBelum ada peringkat
- Electrolyte Disturbance-1Dokumen22 halamanElectrolyte Disturbance-1Doaa Abd El-WahabBelum ada peringkat
- HYPERDokumen4 halamanHYPERhinatakunhinata75Belum ada peringkat
- Electrolyte ImbalanceDokumen76 halamanElectrolyte ImbalanceSarah Racheal Akello100% (2)
- Electrolyte & Acid Base Disturbances in Diabetes MellitusDokumen12 halamanElectrolyte & Acid Base Disturbances in Diabetes MellitusAla SoroceanuBelum ada peringkat
- Diabetic Ketoacidosis:: Evidence Based ReviewDokumen4 halamanDiabetic Ketoacidosis:: Evidence Based ReviewgracedumaBelum ada peringkat
- FAQ - denosumab-induced hypocalcemia in CKD and dialysisDokumen9 halamanFAQ - denosumab-induced hypocalcemia in CKD and dialysisraea.dobsonBelum ada peringkat
- Hypocalcemia & HypercalcemiaDokumen21 halamanHypocalcemia & HypercalcemiaRomMy WiEn MicKhoBelum ada peringkat
- Hypokalemia - Practice Essentials, Pathophysiology, EtiologyDokumen15 halamanHypokalemia - Practice Essentials, Pathophysiology, EtiologymirzeroBelum ada peringkat
- Management of Potassium Disorders 17706 ArticleDokumen4 halamanManagement of Potassium Disorders 17706 ArticlealeBelum ada peringkat
- Abnormalities of Electrolytes: Hypokalemia, Hyperkalemia, Hypocalcemia, and MoreDokumen84 halamanAbnormalities of Electrolytes: Hypokalemia, Hyperkalemia, Hypocalcemia, and MoreMalueth AnguiBelum ada peringkat
- Laboratory FindingsDokumen22 halamanLaboratory FindingseffiniasiregarBelum ada peringkat
- Exp: 1 Day (RT)Dokumen4 halamanExp: 1 Day (RT)Mohd FirdausBelum ada peringkat
- Hypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandHypercalcemia, (High Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Schaefer 2010Dokumen12 halamanSchaefer 2010Rohan BhagatBelum ada peringkat
- PDFDokumen2 halamanPDFAnonymous 80XHV2IIq0% (1)
- Pelatihan Dry NeedleDokumen101 halamanPelatihan Dry NeedleAri SudarsonoBelum ada peringkat
- Case Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022Dokumen6 halamanCase Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022SALAH YOUNISBelum ada peringkat
- Role of OT in Rett SyndromeDokumen2 halamanRole of OT in Rett SyndromeDanielle Stella N'LucaBelum ada peringkat
- 3594 New Delhi Hospitals Jan 17thDokumen18 halaman3594 New Delhi Hospitals Jan 17thrajaasr79Belum ada peringkat
- 80.9 Breathing Filters, HMEs and HMEFs Information SheetDokumen12 halaman80.9 Breathing Filters, HMEs and HMEFs Information Sheethosp PeBelum ada peringkat
- Oxytocin Hormone Benefits and Side Effects by Ray SahelianDokumen5 halamanOxytocin Hormone Benefits and Side Effects by Ray SahelianCondor7tBelum ada peringkat
- Gastroenterology: Case Discussion: Pharmacological PerspectiveDokumen21 halamanGastroenterology: Case Discussion: Pharmacological PerspectivePanini PatankarBelum ada peringkat
- Caring for Dementia PatientsDokumen4 halamanCaring for Dementia PatientsDerick RanaBelum ada peringkat
- The Hypnosis Treatment Option: Proven Solutions For Pain, Insomnia, Stress, Obesity, and Other Common Health ProblemsDokumen54 halamanThe Hypnosis Treatment Option: Proven Solutions For Pain, Insomnia, Stress, Obesity, and Other Common Health ProblemsCopper Ridge Press100% (5)
- ماتريال المراكز والوحدات كاملة-3Dokumen33 halamanماتريال المراكز والوحدات كاملة-3Sanaa SbdelghanyBelum ada peringkat
- An Introduction To Basic Medical English Terminology 1Dokumen346 halamanAn Introduction To Basic Medical English Terminology 1bbbanyi100% (2)
- Qsar by Hansch Analysis: Faculty of Pharmaceutical Sciences, Maharshi Dayanand University, RohtakDokumen5 halamanQsar by Hansch Analysis: Faculty of Pharmaceutical Sciences, Maharshi Dayanand University, RohtakastrimentariBelum ada peringkat
- 12 SP English Core CbseDokumen11 halaman12 SP English Core Cbseviplove100% (1)
- Case StudyDokumen6 halamanCase StudySarah McKayBelum ada peringkat
- Australian Ironman Magazine July 2016 PDFDokumen140 halamanAustralian Ironman Magazine July 2016 PDFgeorgeBelum ada peringkat
- CMS Phy Fee SCH RVU 11-1-11Dokumen1.235 halamanCMS Phy Fee SCH RVU 11-1-11Robert KowalickBelum ada peringkat
- Delirium ToolkitDokumen16 halamanDelirium ToolkitSusana De MatosBelum ada peringkat
- Persuasive - GR 11-27 AugustDokumen1 halamanPersuasive - GR 11-27 AugustShourya PanwarBelum ada peringkat
- Etiology of Epilepsy PDFDokumen2 halamanEtiology of Epilepsy PDFKellieBelum ada peringkat
- Coffea - The Best Homeopathic Medicine For Insomnia: Insomnia Treatment in HomeopathyDokumen4 halamanCoffea - The Best Homeopathic Medicine For Insomnia: Insomnia Treatment in HomeopathysharmadxBelum ada peringkat
- Chemotherapy DrugsDokumen43 halamanChemotherapy Drugsbrigette_lagat100% (2)
- DrugsDokumen61 halamanDrugsPrabir SahaBelum ada peringkat
- NCP Post CSDokumen5 halamanNCP Post CSPeachy Marie AncaBelum ada peringkat
- Nasopharyngeal Angiofibroma Treatment OptionsDokumen51 halamanNasopharyngeal Angiofibroma Treatment OptionsAbhishek ShahBelum ada peringkat
- Types of Wounds: Abrasions, Incisions, Lacerations & PuncturesDokumen19 halamanTypes of Wounds: Abrasions, Incisions, Lacerations & PuncturesVj TolentinoBelum ada peringkat
- Code Blue Management SOPDokumen25 halamanCode Blue Management SOPenumula kumar100% (4)
- Hybrid Compounds As Direct Multitarget Ligands: A ReviewDokumen36 halamanHybrid Compounds As Direct Multitarget Ligands: A ReviewJames TerryBelum ada peringkat
- 2011 - Quick Reference Insulin TherapyDokumen90 halaman2011 - Quick Reference Insulin TherapyEzzaty Kazmin100% (1)