Birth Rights, PANO
Diunggah oleh
Claudia CarreraDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Birth Rights, PANO
Diunggah oleh
Claudia CarreraHak Cipta:
Format Tersedia
Birth rights
New approaches to safe motherhood
Contents
Executive Summary 1
1 The magnitude of neglect 4
2 Why women die 8
Poverty and ill health 10
Social injustice 13
Undesired fertility 14
3 The Safe Motherhood Initiative 17
The importance of emergency care and skilled attendants 18
4 Struggling services 22
Lessons from success 25
5 The gap between evidence and practice 27
Evidence-based care 27
6 The medicalisation of childbirth 30
7 The social dimensions of childbirth 35
The neglect of womens perspectives 36
8 Human rights: a new paradigm 39
Conclusion 42
Panos: Birth rights 1
M
ore than 525,000 women die every year from complications
of pregnancy and childbirth, exacerbated by existing poor
health and inadequate care.
For each woman who dies, many more suffer damage to their
health. In addition to maternal deaths, each year over 15 million
women experience severe pregnancy-related complications which
lead to long-term illness or disability.
These statistics are one of the most stark indicators of the
widening gap between rich and poor both within and between
countries. For each woman who dies of maternal causes in the
developed world, 99 will die in the developing world. A woman in
Afghanistan or Sierra Leone has a 1 in 7 risk of death during her
reproductive years (lifetime risk see box p6); in Peru it is 1 in 85,
in China 1 in 400 and in Norway 1 in 7,300. The greatest risk of
maternal death is faced by women in sub-Saharan Africa.
The tragedy is that almost every one of these deaths is avoidable.
They are caused by social injustices such as early marriage and
violence, by poverty which leads to malnourishment and anaemia,
by undesired fertility and by lack of access to safe, legal abortion
and adequate maternity services.
When a woman dies in this way, her surviving children are also at
risk each year, maternal health complications contribute to the
deaths of at least 1.5 million infants in the first week of life, and 1.4
million stillborn babies. And the problems rebound on the whole
community, on older siblings, families, neighbours, and friends.
Researchers have identified three major factors that are barriers to
womens access to care: a delay in recognising that there is a problem
and making the decision to seek care; a delay in reaching care, often
due to transport problems; and a delay in receiving adequate
treatment once a woman has arrived at the right health facility.
Even when they do get to a hospital or health clinic, maternity
facilities are frequently under-resourced. In addition, there is a
major gap between scientific evidence about what kinds of care are
best for a woman, and what actually happens in practice. Over the
last decade, a massive international research project known as the
Cochrane Collaboration has shown that many widely adopted
practices such as being required to adopt a supine position and
being strapped down while giving birth, pubic shaving and the
overuse of surgical procedures are not beneficial for women and
Executive Summary
2 Panos: Birth rights
may even be harmful. Evidence has also shown that practices
which can save lives are often underused.
Also during the last decade, a new approach to womens
reproductive health has led to a growing focus on human rights.
The fact that many countries have signed up to conventions on
human rights has opened up new avenues to hold governments
accountable for the neglect of lifesaving and humane obstetric care.
These changes have given fresh impetus to the many initiatives
looking at ways to better ensure womens well-being.
In 1987 the International Safe Motherhood Initiative was
launched in Nairobi. It aimed to halve maternal deaths by the year
2000. Some countries have met with relative success, proving that
reductions are possible within existing resources. But there is no
evidence of significant reductions globally. The latest target is a 75
per cent reduction in deaths from 1990 levels by 2015.
This report argues that the target is achievable. To be successful,
governments would need to implement changes in the laws and
policies that constrain womens choices about when and how often
they bear children. The health sector needs to improve maternity
services to aim to give any woman who needs it access to
comprehensive emergency obstetric services and all women the
assistance at birth of a skilled midwife. Care must be based on
scientific evidence and foster womens well being.
Every person each woman, man, doctor, midwife or politician
has a stake in bringing about these changes.
T
r
y
g
v
e
B
l
s
t
a
d
/
P
a
n
o
s
P
i
c
t
u
r
e
s
Women and children at a clinic in Zambia, where only 20 per cent of women in the
poorest fifth of society receive medical assistance at birth.
Panos: Birth rights 3
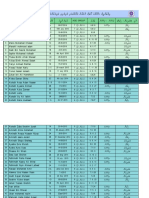
Unsafe motherhood the statistics
525,000 women die each year from maternal causes
For each woman who dies in the North, 99 will die in the South
The greatest risks of maternal death are faced by women in sub-
Saharan Africa
Across regions, lifetime risk of maternal death vary from a low of 1
in 4,000 in Northern Europe to a high of 1 in 16 in sub-Saharan
Africa and 1 in 12 in East and West Africa
In South-east Asia the lifetime risk of death is 1 in 55, in the
Caribbean 1 in 75 and in South America 1 in 140
Maternal health complications contribute to the deaths of at least
1.5 million infants in the first week of life and 1.4 million stillborn
babies.
Each year over 15 million women experience severe pregnancy-
related complications which lead to long-term illness or disability
The biggest direct cause of maternal death is severe bleeding. The
other main causes are infection, unsafe abortion and eclampsia
In Asia, 60 per cent of pregnant women are anaemic, in Africa 52
per cent, in Latin America 39 per cent and in Europe and the US 17
per cent
Girls aged 15 to 19 are twice as likely to die in childbirth as women
in their 20s
More than 50 countries allow marriage at age 16 or younger, and
seven allow marriage as early as age 12
On average, women with seven or more years of education marry
four years later than those with no education
Studies in some countries reported high levels of coercion and force
at first intercourse
Almost one half of maternity services in a study of 49 developing
countries were judged so poorly resourced that they could not carry
out one or more of the lifesaving procedures they were meant to
offer
The World Bank has estimated that the financial cost of basic
maternal and newborn health services is, on average, US$3 per
person per year in developing countries; maternal health services
alone could cost as little as US$2 per person
In 1987 the Safe Motherhood Initiative was launched by the World
Health Organisation and others. It aimed to halve deaths by the year
2000
The current goal of the Safe Motherhood Initiative is to reduce
maternal deaths from 1990 levels by 75 per cent by the year 2015
4 Panos: Birth rights
T
he risk of dying from complications of pregnancy, unsafe
abortion or childbirth remains intractably high in much of the
world. The figures, more than any other health indicator, reveal a
gaping divide in womens well-being between rich and poor
nations and, within countries, between the poorest and the richest.
At least 525,000 women die each year from maternal causes, 99
per cent of them in the South.
1
For every woman who dies, many
more suffer damage to their health. The problems for women also
rebound on their infants many of whom do not survive and on
older siblings, families and communities. Each of these women dies
in the prime of life, when she is most socially and economically
active; at a time when the survival of many family members is
heavily dependent on her.
More than a decade of safe motherhood campaigns have not
altered the stark statistics.
1 The magnitude of neglect
S
e
a
n
S
p
r
a
g
u
e
/
P
a
n
o
s
P
i
c
t
u
r
e
s
A family in Mexico City preventable problems in pregnancy and childbirth have
been the single greatest cause of premature death and disability among women of
reproductive age in the developing world.
Panos: Birth rights 5
A womans lifetime risk of maternal death, by country
Afghanistan 1 in 7 women
Sierra Leone 1 in 7 women
Somalia 1 in 7 women
Angola 1 in 8 women
Yemen 1 in 8 women
Ethiopia 1 in 9 women
Mozambique 1 in 9 women
Mali 1 in 10 women
Nepal 1 in 10 women
Uganda 1 in 10 women
The Gambia 1 in 13 women
Zambia 1 in 14 women
Tanzania 1 in 18 women
Kenya 1 in 20 women
Bangladesh 1 in 21 women
India 1 in 37 women
Pakistan 1 in 38 women
Philippines 1 in 75 women
Peru 1 in 85 women
Brazil 1 in 130 women
Tunisia 1 in 140 women
Thailand 1 in 180 women
Mexico 1 in 220 women
Sri Lanka 1 in 230 women
China 1 in 400 women
Japan 1 in 2900 women
US 1 in 3500 women
UK 1 in 5100 women
Sweden 1 in 6000 women
Norway 1 in 7300 women
Canada 1 in 7700 women
Spain 1 in 9200 women
Hong Kong 1 in 9200 women
Source: The State of the Worlds Mothers 2000, a report by Save the Children, US; Maternal
Health Around the World, wall chart, 1997, Geneva, WHO.
6 Panos: Birth rights
For years preventable problems arising during pregnancy and
childbirth have been the single greatest cause of premature death
and disability among women of reproductive age in the developing
world. Today, the most recent figures available show that among
adult women globally, maternal deaths are second only to deaths
caused by AIDS.
2
The greatest risks of maternal death are faced by women in sub-
Saharan Africa, where one woman in 16 will die from
complications of pregnancy or childbirth. Across regions, lifetime
risks of maternal death vary from a low of 1 in 4,000 in Northern
Europe to a high of 1 in 16 in sub-Saharan Africa and 1 in 12 in
East and West Africa. In South-east Asia the lifetime risk of death is
1 in 55, in the Caribbean 1 in 75, and in South America 1 in 140.
3
Pregnancy-related risk
A maternal death is defined as the death of a woman while
pregnant or within 42 days of termination of pregnancy,
irrespective of the duration and the site of the pregnancy, from
any cause related to or aggravated by the pregnancy or its
management but not from accidental or incidental causes.
4
Three measures are commonly used to measure maternal deaths:
The maternal mortality ratio is the number of maternal deaths
per 100,000 live births.
It indicates the risk of maternal death among pregnant
women and those who have recently delivered and is also
sometimes referred to as the obstetric risk.
The maternal mortality rate is the number of deaths per 100,000
women aged 15 to 49 in a given period.
It reflects both a womans risk of dying from pregnancy-
related causes and her risk of being pregnant at a particular
period in time both are components of risk.
The lifetime risk indicates the probability of death over a
womans reproductive life. It takes into account the fact that
most women have more than one pregnancy in their lifetime
and it is therefore a more realistic assessment of the risk an
individual woman faces because of her reproductive capacity.
A lifetime risk of 1 in 3,000 means that 1 out of every 3,000
women will die and represents a low risk, while 1 in 100
means one per cent of women will die and is a high risk.
Panos: Birth rights 7
Any woman can develop complications, even if she is educated,
healthy and has access to prenatal care, but the poor face the
greatest risks not least because they are least likely to access the
care they need. In most countries the disparity between rich and
poor women in their use of delivery assistance exceeds disparities
in use of modern contraceptives or the immunisation of children.
In Zambia, 90 per cent of women in the richest quintile the
wealthiest fifth of society receive medical assistance, compared to
just 20 per cent in the poorest quintile. In most countries, 70 per
cent of the richest women receive delivery care.
5
When women die, so all too often do their children. Each
year, maternal health complications contribute to the deaths of at
least 1.5 million infants in the first week of life, and 1.4 stillborn
infants.
6
A recent Kenyan study found that when mothers died,
just one third of infants survived the delivery and were alive and
healthy one year later.
7
A study in Bangladesh found that a
mothers death sharply increased the probability that her children,
up to age 10, would die within two years. This was especially true
for daughters.
8
Older children, especially girls, are less likely to
complete their schooling if they dont have a mother as they are
pulled out of education by the necessity of caring for younger
siblings.
In addition to maternal deaths, each year over 50 million women
experience pregnancy-related complications, 15 million of which
lead to long-term illness or disability often because they cannot
access care, because pregnancy has exacerbated already existing
malnourishment or illness, or because the care that they do
manage to access is substandard.
9
Severe anaemia, reproductive
tract infection, pelvic inflammatory disease, infertility, prolapse and
obstetric fistulae (severe damage to the birth canal causing holes
between it and the bladder or rectum) are some of the results.
Without treatment, women with obstetric fistulae often live as
outcasts because of continuous leaking of urine or faeces. Says Dr
Catherine Hamlin, a founder of the Addis Ababa Fistula Hospital in
Ethiopia, Occasionally we get little girls who might be going blind
and we say; Let us get your eyes fixed first and then we will cure
your fistula. But they all say: No, no, cure my fistula first, this is
the worst misery. If I am blind people will talk to me. If I have a
fistula, nobody will talk to me because I smell.
10
Yet most of the deaths, disabilities and ill health are preventable.
8 Panos: Birth rights
W
omen die or become ill during pregnancy and childbirth for
many reasons. In poorer countries multiple disadvantages
combine to put women at risk. Improving womens nutrition,
general health and socio-economic status will reduce the maternal
mortality and morbidity rates. So will access to contraceptives, to
safe, legal abortion services, to tetanus toxoid vaccination, to iron
supplementation and other simple technologies. Appropriate
maternity care during delivery will both prevent emergencies and
save lives.
Worldwide which effectively means in developing countries
because that is where the overwhelming majority of deaths take
place the biggest direct cause of maternal death is severe
bleeding. Indirect causes are the next most common they result
from women being already in very poor health and anaemic or
suffering from conditions such as malaria or HIV while pregnant.
The other main causes are infection, unsafe abortion and
eclampsia. Regionally, these levels may vary.
1. Severe bleeding or post partum haemorrhage has a number of causes
a small piece of placenta being retained in the uterus, or the uterus
failing to contract, for example.
2. Indirect causes include anaemia, malaria and heart disease.
3. Infection or sepsis is caused by unclean delivery practices. It can also
arise without being introduced from outside the womans body from
damaged tissue.
2 Why women die
25%
15%
13%
12%
8%
8%
20%
2. Indirect causes
4. Unsafe abortion
5. Eclampsia
6. Obstructed labour
1. Severe bleeding
7. Other direct causes
3. Infection
The causes of maternal death
Source: WHO 1997
Panos: Birth rights 9
4. Unsafe abortion is defined as a procedure for terminating an
unwanted pregnancy either by persons lacking the necessary skills or in an
environment lacking the minimal medical standards, or both.
5. Eclampsia refers to convulsions and coma occurring during
pregnancy, labour or soon after childbirth. Pre-eclampsia a condition in
pregnancy manifested by oedema (fluid retention of the ankles, hands or
face) also kills women. Both can be associated with hypertension (raised
blood pressure).
6. Obstructed labour occurs when the foetus cannot descend through the
birth canal. It is usually caused by malpresentation of the foetus or too
narrow a pelvis as a result of childhood malnutrition.
7. Other direct causes include ectopic pregnancy when the fertilised
egg becomes implanted and begins to develop outside of the uterus, usually
in a fallopian tube. This can occur as a result of damage caused by a
reproductive tract infection; embolism the formation of obstructive blood
clots dangerous to health; and deaths related to the use of anaesthesia.
Measures of blood: the shock of
haemorrhage
In one Indonesian study, 60 per cent of deaths involved serious
haemorrhage. Excessive bleeding is a clear danger sign, requiring
immediate action to prevent the woman losing so much blood
that she lapses into shock, coma, and death. For many family
members the volume of blood produced after a birth is shocking,
causing fear and confusion. To convey the gravity of the
situation, witnesses used the measure of a piece of cloth the
kain sarong used to absorb the blood and staunch the flow.
At 4am she began to experience labour pains her husband
called the traditional birth attendant at 7am [by evening] the
baby was not coming. [The traditional birth attendant] decided
to call the midwife and sent a family member to the house, but
the midwife was absent At 9pm the baby emerged.
The midwife arrived a few minutes later the placenta was
still attached to the roof of the womb. She had not brought her
full kit, but carried only her scissors and sterile string for tying
the umbilical cord, because she did not want to take
responsibility for emergency procedures since a hospital was
nearby as they struggled to remove the placenta, bleeding
continued, and five or six kain were soon filled.
By 9.30pm the placenta was out, but the bleeding continued.
The midwife was beginning to panic and urged the family to
10 Panos: Birth rights
take her to the hospital. They hesitated, replying that they didnt
have the money to pay the costs, but the midwife insisted
They obtained a car at around 10pm and by 11pm were
checking [the woman] into the emergency ward.
The hospital midwife described later that blood was spurting
from the vagina. The [woman] was unconscious and the doctor
realised that she would need blood immediately for an
operation The blood bank was right next to the hospital
there was no fresh blood available it was the middle of the
night so it was impossible to find somebody. At midnight the
[woman] died.
11
Poverty and ill health
In Asia, 60 per cent of pregnant women are anaemic, in Africa 52
per cent, in Latin America 39 per cent and in Europe and the US
17 per cent.
12
Anaemia causes babies to be born prematurely and
with a low birth weight, both of which hugely increase their
chances of dying before they are a year old, and cause serious
maternal illness. Severe anaemia, which affects 5 to 15 per cent of
African women
13
can kill pregnant women by causing heart failure.
The heart of a severely anaemic woman has to pump harder to get
oxygen around the body. A woman may experience palpitations
and dizziness. She will become profoundly tired, pale (especially on
the palms of the hands and inside the eyelids) and breathless.
Eventually her heart will give up. Anaemic women are also much
more vulnerable to the effects of any haemorrhage or infection that
might occur after giving birth.
Food sources of iron are unlikely to meet the increased needs of
pregnant women, therefore iron tablets (usually combined with
folic acid, a vitamin necessary for blood synthesis) should be part of
all prenatal care regimes.
14
However, anaemia control in pregnancy in developing countries
appears to have failed. The overall prevalence of anaemia in
pregnancy does not appear to have changed much in years. There
may be several reasons why: programmes may not have succeeded
in reaching severely anaemic women who are the ones most at
risk, important causes such as malaria, hookworm and Vitamin A
deficiency may not have been adequately addressed, and other
causes such as advanced HIV infection may be increasing.
Panos: Birth rights 11
Malaria and anaemia: a deadly
combination
A recent study in Kilifi, a rural coastal area of Kenya where malaria is
endemic, has shown that giving women the antimalarial sulfadoxine-
pyrimethamine (SP) a couple of times during pregnancy, when
women attend for antenatal care, can reduce severe anaemia in
women having their first child by approaching 40 per cent.
15
Pregnant women with malaria are particularly vulnerable to
anaemia. A woman struggling with mild anaemia who then has an
episode of malaria can find that her anaemia suddenly worsens and
the condition becomes critical. Almost a fifth of severe anaemia in
pregnancy is thought to be due to malaria.
16
Malaria in pregnancy is also a major cause of miscarriage,
premature delivery, low birthweight and newborn death. Forty per
cent of the worlds pregnant women are at risk of malaria infection
during pregnancy.
17
In areas where malaria is endemic, immunity normally develops in
childhood. Adult infection is frequently without symptoms but in
pregnant women, immunity to malaria is altered.
18
In addition, the
placenta can become a home for parasites, undetected by normal
blood tests and without causing fever. The risks are higher for women
in their first pregnancy. In areas where malaria is not endemic,
pregnant women are two to three times more likely to contract the
disease than non-pregnant women, deteriorate faster than non-
pregnant women and are three times more likely to die if they do
develop severe disease. Pregnant women with malaria therefore need
to be treated urgently with effective antimalarials.
In the past, pregnant women were offered weekly prophylactic
chloroquine, but widespread resistance has rendered this useless in
most parts of the world. Insecticide treated bed nets can offer children
substantial protection from malarial infection, but the effectiveness of
bed net use has varied widely in studies with pregnant women.
The treatment regime researched in Kenya targets all pregnant
women because those infected frequently lack symptoms and
infection is difficult to detect with blood tests. It does not involve
continuous chemoprophylaxis which is much harder to stick to, as
the chloroquine regime did. It should not contribute significantly to
the emergence of drug resistance as SP use in pregnant women will
only form a small part of total use. And it is cheap each dose costs 17
US cents.
19
12 Panos: Birth rights
HIV infection and AIDS are an increasingly common cause of
complications of pregnancy, delivery and induced abortion. Many
women are denied the opportunity in their sexual lives to protect
themselves from HIV. For women attempting to become pregnant,
there is almost no likelihood that they can do so. Frequently women
only learn they are HIV-positive from an antenatal HIV test.
Monitoring of tests in such settings shows that increasing numbers of
women attending antenatal clinics are HIV-positive. Where HIV
infection is relatively uncommon, less than one per cent of women
attending antenatal clinics are HIV-positive. The figure rises to over
20 per cent in urban areas in several countries in sub-Saharan Africa,
and as high as 30 to 40 per cent in some studies.
20
Decreased immunity due to HIV infection increases womens
risks of experiencing clinical consequences of malaria, including
anaemia. Several studies have shown that women who are HIV-
positive have delayed wound healing after caesarean sections and
induced abortion. Infections are more common. Women and health
professionals need information about how to support pregnant
women with HIV and improve their health outcomes.
21
Infants are also at risk of contracting HIV from their mothers.
Without preventive treatment, up to 40 per cent of children born
to HIV-positive mothers will be infected about two thirds during
pregnancy and delivery and one third through breastfeeding.
Withholding breastfeeding however, can lead to increased risks of
A
n
n
i
e
B
u
n
g
e
r
o
t
h
/
P
a
n
o
s
P
i
c
t
u
r
e
s
Cecilia, an HIV-positive mother in Peru, kissing her daughter after hearing of her HIV-
negative diagnosis without preventative treatment, up to 40 per cent of children
born to HIV-positive mothers will be infected.
Panos: Birth rights 13
ill health and death for a child if clean water for breastmilk
substitutes is unavailable.
A single dose of the drug Nevirapine given to a woman during
labour and to the newborn baby halves the likelihood of HIV
infection being passed on to the child.
In South Africa a provincial health authority has been sued for
damages on behalf of a six-month-old baby, Tinashe, who contracted
HIV infection at birth. The authority failed to tell the childs 19-year-
old mother, Sibongile, that she was HIV-positive or that drugs could
have prevented her passing the virus on. It appears to be a
deliberate policy of the health authorities to deny HIV-positive
mothers the help and advice they need, said Sibongile.
22
Social injustice
In many countries, practices which inhibit womens chances of
surviving pregnancy and childbirth are enshrined in law and
culture. The result is a chain of disadvantage, ultimately leading
to death.
Early marriage can lead to childbearing before physical
development is complete. Girls aged 15 to 19 are twice as likely to die
in childbirth as women in their 20s,
23
both because they are younger
and their bodies not fully developed and because first births are
more risky. Yet more than 50 countries allow marriage at age 16 or
younger, and seven allow marriage as early as age 12. In many
countries even the youngest brides face immediate pressure to
prove that they are fertile. In sub-Saharan Africa, more than half of
women give birth before age 20. On average, women with seven or
more years of education marry four years later than those with no
education.
24
The pressure to bear children early increases risks of obstructed
labour, resulting in death or severe injury. A young woman who is
malnourished is at greater risk. She may be physically stunted with
a contracted pelvis, smaller even than that normal for her young
years.
Outside marriage too, young women suffer risks of unplanned
pregnancy where contraceptive services are unavailable. Laws that
deny adolescents reproductive health information and services
without parental consent may appear superficially neutral but have a
disproportionately harmful impact on womens health interests.
25
Safe motherhood is not just about surviving pregnancy but about
women having choices. Says Ingar Brueggemann, Director General
of the International Planned Parenthood Federation (IPPF): I do
not think we have a right to speak about safe motherhood only
14 Panos: Birth rights
when a woman survives the birth. To me, it is not a safe
motherhood if I have to see, as I saw recently, a 12-year-old girl
cradling her baby. Is that what we mean by safe motherhood that
this kid survived the birth of her child?
Violence is another risk factor for women associated with both
unplanned pregnancy and adverse obstetric outcomes. Studies in
some countries reported high levels of coercion and force at first
intercourse.
26
Even when pregnant, violence does not necessarily
abate. Surveys in the US and Europe, conducted in a variety of
obstetric or gynaecological settings, revealed that the prevalence of
domestic violence reported by women varied from 0.9 per cent to
46 per cent.
27
Researchers at the University Hospital in Geneva,
Switzerland, have concluded that the prevalence of violence against
pregnant women is high and severely underestimated by their
healthcare providers.
Maternal mortality is a stark reminder of the non-fulfilment of
womens rights and reducing it cannot be separated from broader
structural issues of gender equality. When women are valued,
resources will be made available to ensure their well-being. Says
James Wolfensohn, President of the World Bank: I do not believe
for one minute, that if men were dying in their prime in these
numbers, so little would be being done.
Undesired fertility
A womans health prospects are transformed if she can decide
whether and when she wants to have children, says Margaret
Catley-Carlson, president of the Population Council. Many women
and men rely on traditional methods of birth control such as
withdrawal. They have no access to more reliable methods of
family planning.
In Ghana, 37 per cent of women have an unmet need for family
planning and say they would like to stop having children or space
their next birth, according to national demographic and health
surveys. In Bolivia this figure is 35 per cent, in Tanzania 27 per
cent and in the Philippines 26 per cent. If these women or their
partners had access to contraception and were free to use it
maternal deaths could be reduced by nearly the same amount.
28
The same is true for access to safe, legal abortion. In Romania,
when a restrictive abortion law was implemented in 1966,
maternal mortality rates due to unsafe, illegal abortion increased
more than fivefold. A less restrictive law introduced in 1989 caused
deaths to fall quickly again by the same amount.
29
Panos: Birth rights 15
Access to safe, legal abortion and advice has recently become
harder in many parts of the world as a result of the so called gag
rule which applies to organisations that receive aid funds from the
US for family planning. The rule requires recipients of US funds to
refrain from advocating for changes in abortion laws, or except in
limited circumstances, providing abortion information, counselling
or services, even with their own funds. The law was first
introduced by President Ronald Reagan in 1984 and was in force
intermittently through the 1980s and 1990s. It was reinstated by
George W Bush on his first full day in office.
The impact in many developing countries has been immediate. In
Nepal, a country where 1 in 10 women die from pregnancy-related
causes approximately half from unsafe abortion the Family
Planning Association of Nepal (FPAN) has had to relinquish a
relationship with USAID which had lasted 26 years. Its director
general, Dr Nirmal K Bista, has testified before the United States
Senate Foreign Relations Committee on how the global gag rule
has threatened the lives of poor women in his country. If I were to
accept the restricted US funds I would be prevented from speaking
in my own country to my own government about a healthcare
crisis I know first hand, he said.
30
Officials at the Ministry of Health have concluded that legalising
abortion could be a first step towards reducing maternal mortality.
In October this year Nepals lower house passed a bill allowing
abortion upon request within the first 12 weeks and in cases of rape
and incest, or if the lives of the mother or child are in danger.
31
The
new law must also be approved by the upper house and the king.
32
Impact of changes in abortion law in Romania
1
9
6
0
1
9
6
2
1
9
6
4
1
9
6
6
1
9
6
8
1
9
7
0
1
9
7
2
1
9
7
4
1
9
7
6
1
9
7
8
1
9
8
0
1
9
8
2
1
9
8
4
1
9
8
6
1
9
8
8
1
9
9
0
1
9
9
2
1
9
9
4
1
9
9
6
180
160
140
120
100
80
60
40
20
0
M
a
t
e
r
n
a
l
d
e
a
t
h
s
p
e
r
1
0
0
,
0
0
0
l
i
v
e
b
i
r
t
h
s
Maternal deaths per 100,000 live births
Abortion deaths per 100,000 live births
Restrictive law
introduced (1966)
Less restrictive law
introduced (1989)
16 Panos: Birth rights
A coalition of medical experts and womens and development
organisations had long been seeking a change in Nepals harsh laws
which imprison women convicted of attempting to obtain an
abortion. International attention was drawn to the issue four years
ago by the case of Min Min, a 13-year-old girl who was raped and
made pregnant by a relative. Her family managed to secure her an
illegal abortion but she was reported and subsequently jailed her
sentence 20 years. A campaign by FPAN and others led first to the
reduction of her sentence to 12 years and subsequently to her
release after two years of imprisonment. One in five women in jail
in Nepal are there for the same reason. Min Min now works for
FPAN.
In Chile, abortion is illegal in all circumstances, including rape
and incest and where a womans life is in danger. The law
recommends a sentence of three to five years. The current
President, socialist Ricardo Lagos, promised Catholic bishops he
would not alter this during his six-year term which ends in 2006.
The Catholic Church is opposed to abortion and any form of
modern contraception.
33
Chile is nonetheless signatory to the
policy agenda of the United Nations Fourth World Conference on
Women which calls for countries to consider reviewing laws
containing punitive measures against women who have undergone
illegal abortions.
34
USAID does not fund Chilean groups but lawyers and other
experts fear the rule will reinforce the conservative climate and
strengthen the hand of those opposed to womens access to
abortion. Says lawyer Lidia Casas, author of a book about women
imprisoned for abortion in Chile: The suppression of free speech is
very damaging in Southern countries because it is precisely the
avoidance of public discussion that is part and parcel of the strategy
of the conservative forces in maintaining the status quo.
35
In Latin America, deaths from unsafe abortion are relatively high
because of restrictive laws in many countries and account for 21
per cent of all maternal deaths.
Panos: Birth rights 17
I
n 1987, the International Safe Motherhood Initiative placed the
reduction of maternal mortality on the policy map. It was
launched in Nairobi by an inter-agency group of the World Health
Organisation (WHO), the World Bank, the United Nations
Population Fund (UNFPA), the United Nations Childrens Fund
(UNICEF), the International Planned Parenthood Federation (IPPF)
and the Population Council. In May 1999 the International
Confederation of Midwives and the International Federation of
Gynaecology and Obstetrics were added and in December 1999 two
developing country organisations, the Regional Prevention of
Maternal Mortality Network (Africa) and the Safe Motherhood
Network of Nepal also joined the inter-agency group. The
Secretariat is provided by Family Care International in the US.
The initial target was the halving of maternal deaths by 2000.
The current goal is to reduce maternal deaths from 1990 levels by
75 per cent by the year 2015.
In the early years of the Initiative, a lack of consensus about what
strategies were effective in reducing maternal mortality hampered
progress. There had been hopes that much could be done to predict
or prevent emergencies arising during labour by training TBAs
(traditional birth attendants local lay women who help others in
childbirth), assessing whether women were at risk of complications
and providing antenatal care. While these strategies can each
contribute to lowering the risks, experience has shown that they are
not the answer. The keys to success in dealing with complications in
labour are professionally trained front line midwives or other health
professionals with midwifery skills and access in case of a referral
need to a comprehensive emergency facility.
In the lay perception, the distinction between TBAs and
midwives is not always clear but in medical terms there is a clear
distinction. Midwives are trained to recognise, manage and refer
complications. Apart from performing surgery and blood
transfusions, they can carry out lifesaving essential obstetric care.
The training of traditional birth attendants without the support
of basic or comprehensive back-up services could not have been
expected to save womens lives in cases of obstetric emergency.
3 The Safe Motherhood
Initiative
18 Panos: Birth rights
Similarly, large investments in antenatal risk screening also failed to
achieve anticipated reductions in maternal mortality. Detecting
women deemed at risk of obstetric emergency has not proved
easy. While there may be a greater risk of complications in some
groups of women, for example those who have experienced a
complication during an earlier pregnancy, it is difficult to predict
which individual women will develop a life-threatening
complication. A study in Kasongo, Zaire with women who had
already had one child, found that 90 per cent of women who were
identified as at risk for obstructed labour had no problem during
delivery. Of the women who did develop obstructed labour, 71 per
cent had previously had no problems.
36
However, the pattern of resource allocation over the last 15 years
means that in Africa and Asia today, women are more likely to
have an antenatal visit than to deliver their babies with the help of
a skilled attendant.
37
In resource-poor settings, a policy of few rather than many
antenatal visits, and those clearly focussed, is the best use of
resources.
38
Moving towards professionally trained midwives for
front line care backed up by functioning comprehensive emergency
obstetric services is the long-term goal.
The importance of emergency care and skilled
attendants
Emergency obstetric care will always be necessary, however much
womens social status, nutrition and freedom to plan their
pregnancies improve with resulting declines in maternal
P
e
n
n
y
T
w
e
e
d
i
e
/
P
a
n
o
s
P
i
c
t
u
r
e
s
Midwives in Fiji learning about reflexes in a new born baby.
Panos: Birth rights 19
mortality. Where women remain disadvantaged, emergency care
can prevent disadvantage translating into worse health or death.
Basic lifesaving obstetric care can usually be provided by
midwives, or doctors and nurses with midwifery training, and can
be delivered at home, in health centres, maternity facilities or
hospitals. But in many countries, women either have to give birth
at home or in a hospital and there is a lack of intermediate types of
place where women can give birth. Health centres, which are
closest to rural women dont often have beds and are rarely staffed
24 hours a day, says Dr Oona Campbell of the Maternal Health
Programme at the London School of Hygiene and Tropical
Medicine. In some countries too, legal restrictions prevent
midwives from carrying out some obstetric procedures.
Comprehensive lifesaving obstetric care refers to basic care plus
blood transfusions and caesarean sections the latter performed by
obstetricians in hospitals.
Essential Obstetric Care (EOC):
Key Functions
Basic EOC (can be provided by midwives, doctors or nurses with
midwifery training)
Parenteral (intravenous or intramuscular) antibiotics to
prevent or treat infection
Parenteral oxytocics (drugs which make the uterus contract to
stop bleeding)
Parenteral sedatives or anticonvulsants (for eclampsia)
Manual removal of the placenta (in cases of haemorrhage)
Removal of retained products of conception (to prevent
bleeding and infection)
Maternity Care: The Percentage of Women Who:
Africa Asia
80
60
40
20
0
Make at least one antenatal visit Deliver with skilled attendance
p
e
r
c
e
n
t
a
g
e
6
3
4
2
6
5
5
3
Source: Safe Motherhood Initiative
20 Panos: Birth rights
Assisted vaginal delivery (to alleviate prolonged or obstructed
labour)
Comprehensive EOC (includes all the above; can be provided at
hospitals)
Surgery caesarean section (in cases of obstructed labour)
Blood transfusion (in cases of haemorrhage)
Historical lessons from Europe and the US show the importance of
both professionally trained midwives and access to modern
emergency care procedures in reducing the toll of pregnancy-related
ill health and deaths. In Northern Europe Denmark, Norway,
Sweden and the Netherlands maternal mortality declined much
earlier than in the US, the UK and other Western European countries
because of the introduction and professional training of large
numbers of midwives who attended women at home. Between 1870
and 1900, Sweden, the Netherlands, Denmark and Norway achieved
significant reductions in maternal mortality.
Levels then stayed constant for approaching 40 years until the
early 1930s. Then maternal mortality declined and converged in all
industrialised countries and the fall coincided with the use of
antibiotics to fight infection, blood transfusions and better
management of problems caused by abnormally high blood
pressure in pregnancy.
Reductions in maternal mortality 18801950
39
1880 190010
Year
193637 1950
70
60
50
40
30
20
M
a
t
e
r
n
a
l
d
e
a
t
h
s
p
e
r
1
0
,
0
0
0
b
i
r
t
h
s
US
England and Wales
Sweden
Netherlands
Norway
Denmark
Panos: Birth rights 21
The importance of access to emergency obstetric care is also shown
by studies of particular groups in industrialised countries. In the
US, national maternal mortality in the early 1980s stood at just 8
per 100,000 live births. At the same time, maternal deaths among a
religious group called the Faith Assembly, who refused all medical
care, were more than one hundred times greater 872 deaths per
100,000 live births similar to maternal mortality ratios in rural
India.
40
Based on our knowledge about the causes of maternal mortality,
Professor Deborah Maine of the Center for Population and Family
Health of Columbia University in the US, argues that in developing
countries: The absolutely first priority would be to get district
hospitals functioning. These facilities are fairly well distributed
within countries and are supposed to be able to provide
comprehensive emergency obstetric care, including caesarean
section and blood transfusion.
41
However, it is important that comprehensive emergency facilities
are not overwhelmed by normal births. In settings with high
maternal mortality, there is an undoubted need to improve existing
comprehensive based services so that they can cope with life-
threatening maternal emergencies, says Dr Campbell. But
countries also need to strike a balance between this and the longer
term goal of expanding midwifery care so that there is skilled
attendance for all births.
Researchers in developing countries are now attempting to assess
the degree to which professional midwifery care can prevent
emergency complications. Preliminary research suggests that
around 16 per cent to 33 per cent of all maternal deaths may be
avoided through the primary or secondary prevention of four main
complications by skilled attendance at delivery.
42
The primary
prevention role of skilled attendants at births, through effective and
appropriate management of normal labour and delivery, would also
have a significant impact on morbidity. The research suggests that
there is an optimal professional mix for skilled attendance to be
effective in different country and service settings.
Moving towards institutionalising all deliveries would be
profoundly costly. To achieve a balanced system, the partnership
between birth attendants is crucial so that the different skills of
midwives and obstetricians can be appropriately and cost-effectively
deployed according to need.
22 Panos: Birth rights
R
esearchers have conceptualised barriers to womens access to
care in terms of the Three Ds.
A Delay in recognising a problem and making the decision to seek
care
A Delay in reaching care, because of the difficulty of travel for
example
A Delay in receiving adequate treatment once a woman has
arrived at the right health facility
Quite apart from how services themselves are functioning, there
can be many obstacles to a woman with complications arriving at the
door of a health facility in the first place.
The cost of transport, drugs and lodging for family members is
one obstacle. User fees increase the financial hurdles. A study in
Zaria, Nigeria, showed that government attempts to improve health
services by charging users led to a precipitate decline in uptake of
maternity services, accompanied by increasing numbers of deaths.
43
Research in West Africa has found that families of women who
survived serious complications in childbirth spent up to a quarter of
average annual household expenditure on hospital care.
44
Families may not seek to use services because they do not realise
there is a problem with the labour which could be helped by referral.
In some communities even serious problems like heavy bleeding
may not at first be recognised as life-threatening because of local
beliefs that bleeding is cleansing and hence not harmful.
45
4 Struggling services
M
e
l
a
n
i
e
F
r
i
e
n
d
/
P
a
n
o
s
P
i
c
t
u
r
e
s
A bumpy ride in Kosovo for pregnant Zade Topalli, who travelled five kms by pony
and cart to get to hospital.
Panos: Birth rights 23
However, there is evidence that when the seriousness of
complications encountered at home is recognised, help is likely to be
sought. Studies of maternal deaths in two districts of Bangladesh
indicated that women who developed complications during
pregnancy more often received medical help prior to death than
women who developed complications during labour and delivery or
post partum. The studies indicated that the seriousness of
complications encountered during pregnancy and of specific
complications such as hypertensive diseases of pregnancy that lead
to convulsions, was more apparent to women and their families than
the seriousness of prolonged labour or post partum infection.
Analysis of avoidable deaths in countries as diverse as Egypt,
46
Malaysia, Vietnam, Pakistan, Malawi, Tanzania, India, Zimbabwe and
South Africa identified many common patterns. Patient factors
contributing to avoidable deaths included expected logistical problems
such as lack of access to transport. Many however were reported as
patients or relations attitude, patients noncompliance or refusal
to go to hospital. A closer examination of these cases revealed that
failures in the health services delivery system constitute a major
disincentive to use.
47
These included failures in health personnel
performance, in availability of health personnel, unavailable or
substandard equipment and facilities. Women encountered vastly
overcrowded facilities without privacy and with poor hygiene, ranging
from dirty linen to non-adherence to aseptic and antiseptic principles
when doing vaginal examinations in crowded wards.
Poor patient management in hospital was identified in several
cases, according to researcher Dr Sundari Ravindran. Delays in
diagnosis and in initiating appropriate treatment were common.
Delays in treatment within health facilities were frequently due to
strict hierarchies in the division of labour among health personnel,
with decision-making responsibility concentrated in a small number
of senior doctors or specialists.
Although it is usually assumed that giving birth in an urban
hospital will always be safest, it is not always as important as the
Impact of user fees on obstetric admissions, Nigeria
Obstetric services Fees for some services Increases in
free (1983) introduced (1985) fees (1988)
Obstetric 7,450 5,437 3,376
admissions
Deliveries 6,535 4,377 2,991
Maternal deaths 2 1 62
24 Panos: Birth rights
quality and professionalism of the care provided. A study compared
four current models of care:
giving birth at home attended by a community member who has
received brief training
giving birth at home attended by a professional
giving birth in a basic essential obstetric care facility attended by a
professional
giving birth in a comprehensive essential obstetric care facility with
the help of professionals
It found unexpected results. In Mexico City, where most women
give birth in large public hospitals, the maternal mortality ratio in 1988
was 114 per 100,000. This hardly differed from safety levels achieved
by non-professional birth attendants in both rural China and some
areas of Brazil.
48
The study revealed from clinical records that 85 per
cent of the Mexican deaths were preventable. Most occurred in four
main hospitals and most were due to mismanagement by physicians.
A study conducted at a university hospital in Nigeria found that
delays by hospital staff in giving appropriate care to women admitted
with complications were more significant in contributing to
unnecessary deaths than any initial delay by women or their families
in seeking emergency care.
49
Poor co-operation between health
service providers and inadequate material resources were identified
by women themselves as constraints to receiving essential obstetric
care in another Nigerian study.
50
In clinics and hospitals in rural and
urban areas of Zimbabwe, a community-based investigation of
maternal deaths found that poor care was an avoidable factor in
nearly 70 per cent of all deaths.
51
A study covering 49 developing countries and encompassing 84 per
cent of the population of the developing world asked local experts to
give their opinion of the effectiveness of the services provided in
health centres and hospitals. Almost one half of the services were
judged so poorly resourced in terms of skills and supplies that they
could not carry out one or more of the lifesaving procedures they
were meant to offer.
52
The capacity of health centres and hospitals to provide lifesaving
services:
At health centres (according to local experts):
38% of staff unable to give antibiotics intravenously to combat
infection
48% of health centres without adequate antibiotic supplies to do so
48% of centres unable to manage post partum haemorrhage
(severe bleeding after birth) the leading cause of maternal death
Panos: Birth rights 25
51% unable to manually remove retained placenta left in the
womb after birth
55% unable to use a partograph chart to plot the progress of labour
and determine if a woman needs to be referred to a more specialist
centre
57% without transport arranged for transfer of a woman with
obstructed labour
76% unable to perform manual vacuum aspiration or electric
suction to remove the products of conception
At hospitals:
33% unable to provide all functions listed above that a health
centre should be able to provide
36% unable to perform emergency caesarean section or operative
delivery
48% unable to perform blood transfusion in cases of severe
haemorrhage
The impact of poorly resourced and poorly run services is felt not
just by women but also by healthworkers, who are severely
demoralised by working in ineffective services. Midwives are
particularly hard hit. Together with other underpaid health
professionals such as nurses, they are leaving the health system in
droves in many areas of the world. Poor pay, poor working conditions,
poor career prospects and lack of status and autonomy are the chief
reasons. Even in Western countries such as the UK, Canada and the
US, the average age of nurses and midwives is increasing because
young people see only poor prospects ahead of them if they join this
work force. The average age of nurses in these countries now stands at
between 43 and 45. The impact of this Western problem is also felt in
poorer countries. During 2000, the UK increased the number of
nurses it recruited from overseas by almost 50 per cent. South Africa
and the Philippines are among the countries which are losing some of
their best and most experienced midwives to the West.
53
To achieve the goals of the International Safe Motherhood Initiative
will require not only greater numbers of staff, but better training and
an improvement in the context in which they work.
Lessons from success
Developing countries that have succeeded in reducing maternal
deaths provide important lessons and show that it is not just a
question of national wealth or poverty. Dramatic reductions in
maternal mortality can be achieved within existing resources. Even
among poor countries with a low gross domestic product (GDP), there
is great variation in death rates.
26 Panos: Birth rights
Lifetime risks, which reveal the compounded effects of multiple
pregnancies, show the greatest variation. Nepal and Gambia have a
similar GDP but much higher lifetime risks of maternal death than
Sri Lanka. 1 in 10 women in Nepal and 1 in 13 in Gambia will die
compared to 1 in 230 in Sri Lanka, where lower fertility and a lower
obstetric risk combine to reduce risk.
54
Sustained political commitment has been a key factor in Sri Lanka
and other countries which have been successful in reducing death
rates despite limited resources, as has a commitment to reduce
inequalities in utilisation of services.
Sri Lanka and Malaysia, which have both reduced maternal deaths
considerably, did so by providing for professional midwives to assist
deliveries. In Sri Lanka by the end of the 1980s most births were
attended by trained staff and more than 75 per cent of births took
place in institutional settings.
55
Increasing skilled attendance at birth
was a key factor in Tunisias success in reducing maternal deaths by
80 per cent in just 23 years.
56
Cuba, China and Costa Rica lowered
maternal death rates by establishing community-based maternal
healthcare systems encompassing antenatal, delivery and post partum
care with a referral system for complications. Cuba also set up
maternity waiting homes near health centres or hospitals so that
women who lived far from a health facility could await delivery close
by. A huge awareness-raising campaign in China about the need for
clean delivery resulted in a massive fall in infection-related deaths.
Haemorrhage remains a problem in sparsely populated rural areas.
57
Even with non-professional attendants, significant reductions in
maternal deaths were made in Fortaleza, North-east Brazil by ensuring
prompt referral to well-run emergency facilities where necessary.
Researchers have captured some of the differences between
countries by developing a Maternal and Neonatal Programme Effort
Index (MNPI). It reveals the importance of strategies such as
reducing rural-urban disparities in use of services for lowering
maternal mortality.
58
The World Bank has estimated that the financial cost of basic
maternal and newborn health services is, on average, US$3 per person
per year in developing countries; maternal health services alone could
cost as little as US$2 per person.
59
These costs are lower than or similar
to those of many other programmes such as measles immunisation.
60
Safe motherhood initiatives have the potential to remove a
massive threat to adult womens health, especially rural womens
health and they are sound investments, offering high social and
economic returns at low cost.
61
Panos: Birth rights 27
A
powerful force for change in maternity facilities has been the
rise of evidence-based care in the health services. Improved
statistical evaluations in the last decade have provided solid
evidence about the risks and benefits of particular healthcare
practices. New scientific evidence about what sort of care for
pregnant women actually works has led to the realisation that
many, perhaps the majority, of women all over the world, are
receiving care that falls short of best practice in some respects.
Evidence-based care can provide new guidance about how to
allocate resources to maximise safety and womens well-being. The
findings do not only apply to women who develop complications of
pregnancy and childbirth, but to all women who give birth. A great
deal of evidence is now available about the sort of care that is
appropriate for women with normal births. For the majority of
women, the research has thrown new light on the meaning of
quality in maternity care.
According to Dr Jos Villar of the World Health Organisation
(WHO), There is a gap between the scientific evidence and the
practice [of] obstetric care.
62
Dr Villars judgement does not
preclude the fact that many health facilities are providing excellent
care with committed staff. But a steady tide of research continues
to reveal that standards of maternity care provided in rich, middle-
income and poor countries too often fall well below what is
desirable, possible and within current budgets. The losers are
women, their newborn infants and their families.
Evidence-based care
The emergence of evidence-based medicine in the early 1990s,
not just in the field of maternal health, has led to a growing
consensus that what matters in healthcare is identifying and using
interventions that have been shown by strong research evidence to
achieve the best outcomes within available resources for everyone.
One of the strongest international research collaborations ever to
exist the Cochrane Collaboration was initiated because of the
insight of a Scottish epidemiologist, Archie Cochrane. In the 1970s
he began to prepare summaries, organised by medical speciality
5 The gap between
evidence and practice
28 Panos: Birth rights
and periodically updated, of the most powerful statistical
assessments of different kinds of care. He documented and ranked
the extent to which different specialities reflected this scientific
evidence in their practice. Obstetrics and gynaecology came last.
63
Based on Cochranes insights, a new research unit was
established in Oxford the National Perinatal Epidemiology Unit
(NPEU). During its first decade, the NPEU carried out some 350
systematic reviews of over 3,000 randomised controlled trials of
interventions in childbirth. These assessed which were beneficial,
which were irrelevant or potentially harmful (and therefore ought
to be abandoned), which appeared promising but required further
evaluation, and which had unknown effects. They identified 99
beneficial forms of care, 61 that should be abandoned in the light
of available evidence, 38 showing promise but requiring further
evaluation and 88 with unknown effects.
64
The findings were published in the now classic publication
Effective Care in Pregnancy and Childbirth,
65
which was subsequently
adapted for a lay audience and used extensively by consumer
groups in the UK and elsewhere.
The NPEUs high quality research in maternity care quickly
gained an international reputation leading to the founding of the
Cochrane Collaboration, an international resource for evidence-
based medicine in all specialities, including maternity care, which
was launched in Oxford in 1993. The evidence base of the
Collaboration is continuously updated. Key findings of relevance to
developing countries in the field of reproductive health, including
maternity care, have been distributed widely by WHO on free
diskettes to health workers in developing countries. In the age of
information technology, the limitations to knowledge that existed
in the past for individual practitioners are on the way to being
overcome.
Armed with the results of the Cochrane Collaboration, research
studies in many settings have found:
an over-application of procedures that should be abandoned on
the basis of the evidence
routine application of procedures that are appropriate only for
non-routine circumstances
an under-application of lifesaving practices
For example, practices such as routine electronic foetal
monitoring, routine ultrasound and routine episiotomy (a surgical
incision to enlarge the vaginal opening), which are all costly and
Panos: Birth rights 29
either unnecessary or harmful for normal births, are widely
practised in many countries. Caesarean sections are often
unavailable when needed to save lives or overused when not
medically indicated, usually in urban settings. Simple and effective
medical interventions are often not used. Even the cost-free but
highly beneficial step of allowing a woman to have a companion in
labour is often restricted.
As well as being used to highlight the enormous variation in
application of procedures of limited usefulness and those that
protect life and health, the findings of the Cochrane Collaboration
have also borne out criticisms made by some womens and
consumers groups of over-medicalised models of childbirth. In
hospitals and health centres around the world, women are still
subjected to a range of medical practices and procedures in the
absence of evidence that they are beneficial and even in the face of
evidence that they are harmful. Many of these practices cause
women unnecessary discomfort and pain. In some cases they may
increase risks of death or lasting damage.
D
r
M
e
f
t
u
n
A
h
m
e
d
/
D
r
i
k
Mother and child, Gozoni Hill, Sherpur, Bangladesh.
30 Panos: Birth rights
M
aternity care in much of the world has been heavily
influenced by hospital-based norms developed in the West.
In much of the West, hospital maternity care became much more
oriented towards intervening medically in normal childbirth during
the 1950s and the legacy remains entrenched.
Susans story
US anthropologist Brigitte Jordan describes her shock when she
studied childbirth practices in the US in the 1970s. Her account
of a young US woman giving birth to her first child highlights
some of the criticisms that have been levelled at highly
medicalised birth practices:
Susan was an unmarried 15-year-old who had managed her
labor admirably The nurse left us pretty much alone and in a
short time Susan and I established a close relationship,
exchanging stories about our very different lives and then with
increasing seriousness, monitoring her experience.
As time went on, Susans contractions became somewhat
painful, but she lasted them out with her deep, joyful conviction
that this was going to bring her baby out, really, so she could see
it, and touch it, and love it. She looked into my eyes during
those contractions and, when they were over, told me she was
glad I was there we laughed.
Finally, she was completely dilated. The nurse rolled in a
gurney [trolley] and transferred her onto it with my help. Susan
was going to the delivery room Bright lights. Gleaming metal.
They transferred her to a narrow table, flat on her back, her legs
grotesquely spread apart, her feet in stirrups. And then I noticed,
to my horror, that they were tying down her hands with leather
straps All of a sudden the situation had changed from the
intimate, exciting atmosphere of the labor room, where we had
worked together to help this wonderful baby be born a
straightforward proposition, easily understandable to a
situation that was out of our hands.
They told her to push. Susan, who had been so courageous
during the long hours of labor, made an effort. Her body strained
6 The medicalisation of
childbirth
Panos: Birth rights 31
and fell back in discouragement. My God, I cant push like this.
How can I push like this? she wailed. She was already
transformed by the ties, by her position, by the green-clad
bodies surrounding her, into an object strapped onto a table
They told her to push again. Her eyes were searching for me
She looked at me imploringly. Gitti, please untie my hands.
They ended up stimulating her labour and pulling the baby
out with forceps... I went home and swore that my daughters
would not have to go through that.
66
Jordan also studied birth practices in the Yucatan in Mexico, in the
Netherlands and in Sweden. In the Yucatan, women are given
physical and emotional support, often from their husband who
stands behind his wife to allow her to pull on his neck with her arms
while delivering. A doctor can be brought in case of difficulties but
hospital-based care for real emergencies is not there and women still
face a risk of dying. In the Netherlands and Sweden, Jordan saw
other models for childbirth. In the Netherlands midwife-supported
homebirths with very little medication were backed up by the
possibility of referral to hospital if necessary. In Sweden, births took
place in hospitals with a birth team including the mother, a midwife
and her assistant and a non-specialist attendant of the womans
choosing her husband, friend, mother or someone else. The
woman and her attendant conducted much of her labour in privacy
using a call button to ring for assistance. Women and their infants
fared better under the Dutch and Swedish than the US systems.
In what position do you feel most comfortable during labour?
Extracts from a Brazilian poster by Projeto Luz
32 Panos: Birth rights
Jordan concluded that there is massive cultural variation in
behaviour towards birthing women.
Practices which were once routine in the West and are now
being discredited have been widely exported to developing
countries, who frequently lack the means to update their
knowledge.
A study of procedures used during 303 vaginal deliveries in
Shanghai, China between April and May 1999
67
found that several
practices that should be eliminated on the basis of current scientific
evidence were in fact widespread. Practices which are harmful if
overused were nonetheless overused.
Percentage of labours in which practice was applied:
Practices that should be eliminated
Pubic shaving 73%
Enemas 8%
Rectal examination 70%
Supine position 99%
(lying on the back during delivery instead of adopting a position of choice; a
more upright position can open the pelvis more)
Practices that should not be used routinely
Electronic foetal monitoring 62%
Episiotomy 82%
Lebanon
A national sample of 39 hospitals in Lebanon found that:
Very little information was given to women before birth or
during birth about what to expect in delivery
For many women ultrasound was a routine prenatal test at
each visit to the obstetricians clinic, despite the limited
benefits and high costs
Women routinely had their pubic hair shaved while they were
in active labour
Women were routinely given an enema
Many women were required to change into a hospital gown
rather than wear their own night clothes
Women were routinely given an episiotomy, often without
their permission being sought
More than half of the women in 31 of the 39 hospitals were
automatically attached to an IV drip with labour-inducing
drug, which increases the severity of contractions
Panos: Birth rights 33
Most hospitals forbad women to drink anything during labour,
allowing only sips of water or wetting of lips
In the first stage of labour (cervical dilation), 10 out of 39
hospitals did not allow women to have a companion. In the
second stage of labour (delivery), 26 of the 39 hospitals refused
access to a companion
In the first stage of labour, women were allowed to move
around with some degree of freedom in 32 hospitals, but just
15 encouraged them to adopt whatever position was
comfortable. 11 hospitals confined movement to the bed and
restricted women to supine position. In the second stage of
labour, no hospitals allowed women to choose their own
position for delivery. All required the supine position
In 23 of the 39 hospitals women were tied down during
delivery in eight hospitals both arms and legs were tied
Many hospitals used problematic forms of pain relief, such as
intramuscular Haolperidol and Diazepam
Most women had to wait several hours before having the
chance to hold their baby.
Most hospitals did not initiate breastfeeding within one hour of
birth or give breastfeeding assistance and few had rooming in
(allowing the mother and baby to be together in the same room)
Most hospitals did not provide women with family planning
methods and a few did not discuss contraceptive methods at all
Every one of these practices contradicts World Health Organisation/
Cochrane guidelines for the care of women in labour and newborns.
68
Unnecessary interference in womens labours also becomes
entrenched where vested interests in particular forms of care
develop, particularly where these generate financial profits.
Caesarean section can earn doctors considerable fees in private
practice. Even government provision can be skewed by the greater
financial reimbursement given for these than for normal vaginal
deliveries. In many areas of Brazil caesareans have been more
lucrative: hospitals and doctors made more money when billing the
Social Security Medical Service (INAMPS) because sections mean
longer hospitalisation and medicalisation than vaginal births.
69
Caesarean section rates are increasing in many countries. The
national rate in Brazil is 36 per cent, in the UK 21.5 per cent,
70
in
Thailand 28 per cent.
71
Rates as high as 30 per cent have been
reported in some hospitals in China
72
and India.
73
A level of 45 per
cent was reported from affluent populations in Chennai, India.
74
34 Panos: Birth rights
WHO guidelines stress that levels of just 5 per cent to 15 per cent are
advisable in medical terms.
The cost for the Mexican nation of its excess sections that
proportion which are not medically called for has been estimated
to be at least US$12,204,704.
75
In the UK, Caroline Flint, an
independent midwife and former President of the Royal College of
Midwives calculates that the National Health Service could save
68.7 million if the caesarean section rate was brought down to
WHO recommended levels.
76
In addition to the epidemic of caesarean sections, there are signs
of a worldwide epidemic of other obstetrical interventions,
according to US Professor Pierre Bueckens.
77
High episiotomy rates
have been reported in many countries of Latin America and Africa.
Hospitals in Argentina have reported rates of 91 per cent
78
and in
Nigeria up to 87 per cent
79
among women having their first babies.
An editorial in the British Medical Journal has stressed the need to
decrease episiotomy rates in developing countries.
80
While episiotomies cost less than caesarean sections, their
widespread use when unnecessary represents a substantial waste of
resources. In Argentina each episiotomy, including suturing and
anaesthetic, costs a little over US$6. Evidence suggests that
reducing the episiotomy rate from 80 per cent to 30 per cent would
significantly benefit womens health.
81
In the Netherlands system of low-tech care, resources are used
differently. 31.5 per cent of births in 1992 took place at home.
Unless considered high risk, Dutch women can choose to give birth
at home or in hospital, assisted by independent midwives or
general practitioners. Those with high-risk pregnancies give birth in
hospital under the supervision of obstetricians. Women who are
not high risk cannot request a caesarean and all women who give
birth at home are offered a home help to cook, clean, and help
with older children as required for a period of 10 days following
the birth.
82
Panos: Birth rights 35
T
he inevitable corollary of the over-use of unnecessary medical
practices is a reduction in the amount of control women have
over giving birth. Adequate maternity care needs to allow for
partnership between women, their lay and professional carers.
Giving birth takes several hours. During this time, women show
considerable variation in how they wish to conduct the physiological
process of birth, adopting different positions at different times during
labour, resting, finding ways of dealing with contractions.
Birth is not only a biological event. Anthropological research
shows that there are no known societies where birth is treated by
the people involved as a merely physiological function.
83
It is a rich
personal event where the quality of relationships between a
woman giving birth and those with her can define the experience.
Researchers studying quality of care in a variety of healthcare
settings have stressed the importance of interpersonal, rather than
simply technical, care.
84
Yet in many maternity care settings, women have little control or
companionship. The results of a lack of choice are dissatisfaction,
anger, guilt, disappointment. A study in four European and US
cities found widespread restrictions placed on women. In another
study in St Petersburg, Russia, nearly half the women interviewed
in 11 hospitals wanted their partners to be with them during
labour, but partners are not allowed in most hospitals. Nearly 75
per cent of hospitals allowed no bedside visiting after birth. Some
hospitals allowed visiting only in the foyer. Forty-two per cent of
women could only see visitors through the windows of the
building.
Having social support during labour has, in the absence of
emergencies, been shown by Cochrane Collaboration research
evidence to have a huge impact on the outcome of normal birth for
both woman and infant. Social support means paying attention to a
womans wishes, feelings of well-being, need for information and
her choices.
Social support during labour has been shown to:
reduce the incidence of medical interventions such as drugs to
control pain; forceps delivery; caesarean section
6 The social dimensions of
childbirth
36 Panos: Birth rights
shorten the length of labour
increase a womans satisfaction with birth and increase levels of
well-being measured in the first six weeks after childbirth
speed her physical recovery after childbirth
facilitate breastfeeding and strengthen the early mother-infant
relationship.
85, 86, 87, 88, 89
Encouraging social support for pregnant women remains
contrary to documented practice in several countries.
We feel very abandoned the first things they take away from
us are our documents, our belongings, our husbands, our mothers,
says Dr Simone Diniz, a doctor working with the Brazilian Feminist
Network for Health and Reproductive Rights (RedeSade),
describing the experience of Brazilian women.
90
Women in Mexico
A study in Mexico found that women offered support from a
doula a trained companion for first time mothers expressed
themselves more easily, asked questions and received more
information about their care. They were more aware of their
progress and how they dealt with pain: I felt calm, I was
relaxed, I took deep breaths, I pushed hard, they said. They
were also more able express complaints, for example about the
ways in which vaginal examinations were conducted: Why are
they so rough?, Why dont they wait until the contraction is
over [before examining]?
Women receiving standard care which in this system meant
having no companion felt they had little active part in the
birth and that the moment of delivery was just the last in a
series of interventions. They received less information about
particular procedures. For example, a woman who received an
episiotomy reflected, It seems that they cut me, and then when
I had to go to the bathroom, it burnt me a lot and I said, Whats
happening to me? But it was because they cut me. Others
spoke of their desire to be accompanied. I would have liked my
mother or my husband to be there, to have some support, to feel
someones affection, to feel I was important to someone
91
The neglect of womens perspectives
Safety of both herself and her baby is the primary concern of
every pregnant woman, her family and care providers. Satisfaction
Panos: Birth rights 37
with the birth process is readily sacrificed by most women in the
interests of perceived safety. Yet it need not be. When satisfaction
with the quality of care offered in the health sector is too low the
result is under- and late-utilisation of services, increasing the risks
of death or serious injury to mother and child. An unnecessary
barrier to womens access to care is created.
In the Lebanon study, 84 per cent of women giving birth in
hospitals cited safety as the primary reason for their choice. The
concern for safety overrode the desire to have a female birth
attendant and, in rural areas, problems of distance to the facility.
Women accorded complete trust to their physicians and rarely
questioned routinely applied procedures even though they reported
finding them intimidating or that they caused discomfort or pain.
As in other studies, women accepted hospital rules, though in
limited ways tried to subvert some of them and increase their room
for manoeuvre. They reported delaying the time at which they
referred themselves to a medical facility. If they had had a hospital
birth before, some chose to shave themselves at home in order to
avoid what they regard as an unpleasant aspect of the hospital
procedures.They preferred to leave the hospital within 24 hours of
giving birth.
92
In Finland, women and men who planned a home birth reported
concealing their desire from prenatal care staff in order not to be
labelled as a risk parent. They felt that deviating from the normal
expectation that birth would take place in hospital would expose them
to censure and a less supportive approach during antenatal care.
93
In many countries of the West, highly medicalised models of
childbirth have undergone significant reform, often as a result of
leadership from concerned doctors and midwives and organisations
representing women and their families the consumers of care.
Family-centred care in Ukraine,
Moldova and Russia
The Newly Independent States (NIS) of the former Soviet Union
have struggled with the Soviet legacy since their transition to
open societies, particularly in the realm of health care..The
conditions in the maternity clinic are impossible. There is no hot
water, nothing to the point that when I had given birth, and I
asked them to put the baby on my stomach, they said to me,
Then how will you wash yourself? and didnt give it to me,
said one woman in Vladivostok.
38 Panos: Birth rights
Focus group discussions in hospitals found several
discrepancies between the views of staff and women and their
families. Most medical staff objected to the participation of the
husband and relatives. Husbands felt differently. It should be
like this you come to your wife, you pay the money and stay
there as long as you want. But they wouldnt let us; they limit
the time to 20 minutes. What if I dont even manage to talk
enough to my wife in 20 minutes?
The Family Centered Maternity Care (FCMC) approach is a
new concept in the NIS. FCMC focuses primarily on meeting the
informational, social, emotional and physical needs of pregnant
women and their families during pregnancy, childbirth and post
partum. The approach emphasises education and preparation for
childbirth so that a woman and her family can assume more
active roles.
FCMC decreases costs, with savings ranging from just over
US$7 to just over US$16 per birth. Who benefits from the cost
savings? Given the difficult economic situation, many medical
supplies, including drugs, are paid for directly by a patient.
Because medical supplies and other equivalent variable costs
represent the majority of cost savings due to an FCMC approach,
the woman and her family are the primary beneficiaries.
94
As developing countries expand their maternity services,
appropriate frameworks for quality, woman-centred care need to be
in place. Says researcher Dr Sundari Ravindran: If quality of care
means to meet womens needs, then community awareness on one
side and accountability to the community on the other are required
from the time that facilities are set up.
95
Developing countries need to question the prevailing models of
provision for maternity care, from the dual perspective of current
scientific knowledge and a commitment to womens empowerment
and human rights.
Panos: Birth rights 39
D
uring the last decade, womens reproductive health, and the
factors which determine it throughout the life cycle, have
increasingly been viewed and monitored through the lens of
human rights. Three major United Nations Conferences in the last
decade the International Conference on Population and
Development (ICPD), the Fourth World Conference on Women and
the World Conference on Human Rights have led to a significant
change in the policy climate. Each placed the well-being of
individuals and couples at the heart of planning.
ICPD defined reproductive health as a state of complete, physical,
mental and social well-being and not merely the absence of disease
or infirmity, in all matters relating to the reproductive system and to
its functions.
96
The international policy agenda which emerged
from the conference and was endorsed by 179 nations, placed a
strong emphasis on womens empowerment and stressed that its
definition of reproductive rights was based on human rights that
were already recognised in national laws, international human rights
documents and other consensus documents. Thus it moved the goal
posts from the limited approach of preventing or eradicating disease
or dysfunction, to the more comprehensive one of total well-being.
The rights agenda thus moves us from a negative preventive stance
to an affirmative one, say Indian researchers Professor Gita Sen and
Dr Srilatha Batliwala.
97
In the field of safe motherhood, both the magnitude of needless
death and disability and the quality of care that some women
receive are increasingly scrutinised in the light of countries
obligations under legally binding regional and international human
rights treaties to which they are signatory.
Most countries of the world have signed up to a range of
international human rights instruments such as the Universal
Declaration of Human Rights (UDHR). Specific rights protected in
these treaties can be applied to different factors contributing to
maternal mortality and well being.
Several human-rights treaties, including the Convention on the
Elimination of all forms of Discrimination against Women (the
Womens Convention) make specific mention of state obligations
relating to the prevention of maternal mortality and provision of
7 Human rights: a new
paradigm
40 Panos: Birth rights
appropriate services for pregnant women. On this basis, the
Committee on the Elimination of all forms of Discrimination against
Women, the body which is charged with monitoring implementation
of the Womens Convention, has reminded a number of countries of
the need for further action. The Human Rights Committee (HRC),
which monitors implementation of the UDHR, specified in 2000
through its General Comment 28 on Equality of rights between men
and women, that when reporting on the right to life, protected by
article 6 of the UDHR, States Parties are now required to provide data
on pregnancy and childbirth-related deaths of women.
98
Guidelines for monitoring the availability and use of obstetric
services, which can assist treaty-monitoring bodies, have been
developed by UNICEF and other UN partners.
99
They spell out six
questions to be asked:
Are there enough health facilities providing lifesaving care for
women with obstetric complications?
Are these facilities equally distributed across the population?
Are pregnant women using these facilities?
Are pregnant women with obstetric complications using these
facilities?
Are the facilities providing enough lifesaving surgery to meet the
needs of the population?
Is the quality of these services adequate?
The failure to address preventable maternal disability and death
represents one of the greatest social injustices of our time, argue
Professors Rebecca Cook and Bernard Dickens, co-authors of a
WHO study on advancing safe motherhood through human rights.
A human rights approach shows that womens reproductive
health risks are not mere misfortunes and unavoidable natural
disadvantages of pregnancy but, rather, injustices that societies are
able and obligated to remedy, they add.
100
Midwife Sister Anne Thompson, who has worked for 25 years in
developing countries, argues: If hundreds of thousands of men were
suffering and dying every year, alone and in fear and agony, or if
millions upon millions of men were being injured and disabled and
humiliated, [some] sustaining massive and untreated injuries and
wounds to their genitalia, leaving them in constant pain, infertile and
incontinent, and in dread of having sex, then we would all have heard
about this issue long ago, and something would have been done.
101
Whether or not a society commits resources to appropriate
services is itself a measure of womens status.
102
Panos: Birth rights 41
In the field of reproductive health, several womens health
organisations, academics and legal bodies have begun to use human-
rights treaties at a national level to improve access to and quality of
services for women.
The Colombian non-governmental organisation Profamilia, which
provides family planning and sexual health information, has prepared
material explaining womens rights and how they can be used under
the Womens Convention, to which Colombia is signatory. In 1991
when the constitution of Colombia was being revised, womens
groups used the material to convince the government to include
family planning as a right protected by the Constitution.
The Peruvian Movimiento Amplio de Mujeres (Comprehensive
Womens Movement), have used human-rights treaties to declare
new standards for accountability in service provision. In the case of
family-planning services, the womens movement has paid
considerable attention to coercion, lack of informed consent and
other issues of quality of care.
A recent human rights mission examining violence against women
in Peruvian public health facilities, including maternity wards, found
that the care women receive violated their human rights.
Peru
Women in maternity facilities described being shouted at and verbally
abused in terms that reflected a view of giving birth as a form of
punishment for having sex: The nurses and technicians yelled at me,
Who forced you to have kids? What were you expecting? You should
have thought about it before you did it. If you open your legs to your
husband, get ready to give birth.
Abuse of women giving birth was physical: A nurse who was
helping me [as I gave birth], told me that I should help, [that] I should
push. At that moment I couldnt. I cried out. The nurse slapped me. I
felt ashamed
In cases in which women were poor, the fee system severely
affected their right to access care, even in an emergency. In some
cases it was used as a lever for bribery When a pregnant woman
arrives at the emergency obstetric ward, she should count on paying
50 per cent of the total costs plus a small bonus.
103
Similar findings were documented by researchers in Benin,
West Africa. Those satisfied with the care they received considered
themselves lucky to land a kind midwife. The research
concluded that the inclusion of womens voices in the objective
of safe motherhood programmes is necessary to better serve
womens needs.
104
42 Panos: Birth rights
I
t is possible to achieve the goal of reducing maternal mortality by
75 per cent by the year 2015. And it must be made a reality.
Not simply because these are women in the prime of their lives
Not simply because a maternal death is one of the most terrible
ways to die But above all because almost every maternal death is
an event that could have been avoided, and should never have
been allowed to happen, says Dr Mahmoud Fathalla, President of
the International College of Obstetricians and Gynaecologists.
The strategies that will work include strengthening professional
frontline midwifery care and comprehensive obstetric facilities for
emergencies and making services accountable; enlisting
sympathetic obstetricians and midwives to lead change within their
professions, and supporting womens, consumers and professional
groups to lobby for change. Women, their families and
communities should be provided with the information they need to
prepare for pregnancy and birth.
In parallel to changes within the health sector, governments also
need to implement changes in laws and policies which constrain
womens choices about when and how often they will bear children.
Internationally the focus of the Safe Motherhood Initiative has
been to ensure women have a low risk of death and severe
complications from pregnancy and childbirth. As services expand, it
is crucial that service providers and women remember that the vast
majority of pregnancies and births are normal. Ensuring high
standards of care for these women too should not be squeezed off
the agenda. Often this means avoiding overuse of medical
technologies and encouraging partnership between women, their
families and healthcare professionals.
The influence of the international consensus on reproductive
health agreed at ICPD, with its emphasis on womens
empowerment, will increasingly be felt in maternity care.
An approach focused on empowerment leads to a powerful
merging of the rights and health agendas, says Professors Sen and
Batiwala, because empowered women who are aware of their
sexual and reproductive rights are in a stronger position to
determine how they are able to access health and how they are
treated by health services.
To achieve this kind of change requires making women, their
communities, care providers and governments aware of what is
Conclusion
Panos: Birth rights 43
possible on the basis of current evidence and finance and what
additional finance or reallocation of resources is needed to ensure
womens safety and well-being.
Says Peter Adamson, editor of UNICEFs Progress of Nations report,
the strategies that work have been identified and the resources
will follow if priority lights the way. What is needed now is a much
noisier demand for action to force this issue into public
consciousness and on to the political agenda.
105
Training poster from the South African Better Births Initiative.
44 Panos: Birth rights
Notes
1
Hill K, AbouZahr C and Wardlaw T, Estimates of Maternal Mortality for
1995 Bulletin of the World Health Organisation, Geneva, 2001
2
Global Burden of Disease (GBD) 2000, Version 1 Estimates, World Health
Organisation.
www3.who.int/whosis/menu.cfm?path=whosis,burden,burden_gbd2000&langu
age=english
3
AbouZhar C, Maternal Mortality Overview, Health Dimensions of Sex and
Reproduction. Murray C J L and Lopez A D, Harvard University Press, 1998,
pp111164
4
International Statistical Classification of Diseases, Injuries and Causes of Death
Tenth Revision (ICD-10)
5
Kunst A E and Houweling T, A global picture of poor-rich differences in
the utilisation of delivery care in De Brouwere V and Van Lerberghe W, (eds),
Safe Motherhood Strategies: a Review of the Evidence, Studies in Health Services
Organisation & Policy, 17, 2001
6
Tinker A, Safe Motherhood as an Economic and Social Investment.
Presentation at Safe Motherhood Technical Consultation in Sri Lanka, 1823
October 1997, cited in Safe Motherhood Fact Sheet: Maternal Health: A Vital
Social and Economic Investment
www.safemotherhood.org/facts_and_figures/good_maternal_health.htm
7
Boerma J T, Mati J K G, Identifying maternal mortality through
networking: results from coastal Kenya Studies in Family Planning, 20, 1989,
pp245253
Kenya Maternal Mortality Baseline Survey Population, Studies and Research
Institute, University of Nairobi, Kenya, 1996 cited in Murray C J L and Lopez A D,
Health Dimensions of Sex and Reproduction
8
Safe Motherhood Fact Sheet: The Safe Motherhood Initiative
www.safemotherhood.org/facts_and_figures/initiative.html
9
Tsui A O, Wasserheit J and Haaga J G, (eds), Reproductive Health in
Developing Countries: Expanding Dimensions, Building Solutions National Research
Council, National Academy Press, Washington DC, 1997
10
Gudeta T, The Silent Shame: Obstetric Fistula in Ethiopia in Mirsky J and
Radlett M, (eds), Private Decisions, Public Debate: Women, Reproduction and
Population The Panos Institute, London, 1994
11
Iskandar M B, Utomo B, Hull T, Dharmaputra N G, Azwar Y, Unravelling
the mysteries of maternal death in West Java: Reexamining the Witnesses Center for
Health Research, Research Institute University of Indonesia, 1996
12
The Prevalence of Anaemia in Women: A Tabulation of Available Information
WHO, 1992, WHO/MCM/MSM/92.9
13
Shulman C, Malaria and Anaemia in Pregnancy; Importance, Detection and
Prevention Amsterdam, Thela Thesis 2001
14
McGuire J, Hidden Hunger III: Winning One Battle Against Anaemia, HRO
Dissemination Notes, The World Bank, 1994
www.worldbank.org/html/extdr/hnp/hddflash/hcnote/hrn020.html
15
Shulman C, Malaria in pregnancy: its relevance to safe-motherhood
programmes Annals of Tropical Medicine and Parasitology, 93, 1999 Supp 1,
S59S66
16
Brabin B J, Hakimi M, et al, An analysis of anaemia and pregnancy-
related mortality Journal of Nutrition, 131, 2000 (Suppl) 604S615S
17
Shulman C, Dorman E K, Importance and Prevention of Malaria in Pregnancy
forthcoming 2001
Panos: Birth rights 45
18
Shulman C, Dorman E K, Malaria in Pregnancy Africa Health, September
2000
19
Shulman C E, et al, Intermittent sulphadoxine-pyrimethamine to prevent
severe anaemia secondary to malaria in pregnancy: a randomised placebo-
controlled trial The Lancet, 353, 1999, pp632636
20
Berer M, HIV/AIDS, Pregnancy and Maternal Mortality and Morbidity:
Implications for Care in Berer M and Sundari Ravindran T K, (eds), Safe
Motherhood Initiatives: Critical Issues, Reproductive Health Matters, Special Edition
1999
21
Fact Sheets on HIV/AIDS for nurses and midwives, World Health
Organization 2000. www3.who.int/whosis/factsheets_hiv_nurses/index.html
22
HIV baby sues Pretoria for not protecting her Chris McGreal,
The Guardian, October 2001
23
Too Old for Toys, Too Young for Motherhood UNICEF, New York, 1994
24
Safe Motherhood Fact Sheet: Adolescent Sexuality and Childbearing
www.safemotherhood.org/facts_and_figures/adolescent_sexuality.htm
25
Cook R J and Dickens B M, Advancing Safe Motherhood Through Human
Rights, WHO, 2001, Geneva, WHO/RHR/01.5
26
Heise L, Ellsberg M, Gottemoeller M, Ending Violence Against Women
Population Reports Series I, 1999, 11:918
27
Irion O, Boulvain M, Straccia A-T, Bonnet J, Emotional, physical and
sexual violence against women before or during pregnancy British Journal of
Obstetrics and Gynaecology, 107, 2000, pp13061308
28
Womens Lives and Experiences: A Decade of Research Findings from the
Demographic Health Surveys Program Macro International, Calverton, MD, 1994
29
Investing in Health World Development Report 1993, World Bank, New
York, Oxford University Press
30
Global gag rule threatens lives of Nepali women, Press release, IPPF, July
19, 2001
31
Personal communication, Ramyata Limbu
32
More Rights for Nepali Women The Guardian, October 10, 2001
33
Frasca T, US wrongs and womens rights Panos Features, April 2001, The
Panos Institute, London
34
Paragraph 106k, Platform for Action, Fourth World Conference on
Women, 1995
35
As 33 above
36
Maine D, Safe Motherhood Programs: Options & Issues Center for Population
and Family Health, Columbia University, New York, undated
37
www.safemotherhood.org/facts_and_figures
38
Villar J, et al, WHO antenatal care randomised trial for the evaluation of a
new model of routine antenatal care The Lancet, 2001, 357, 155164
39
Van Lerberge W and De Brouwere V, Of blind alleys and things that have
worked: historys lessons on reducing maternal mortality in De Brouwere V and
Van Lerberge W, as note 5
40
Kaunitz A M, Spense C, Danielson T S, Rochat R W, Grimes D A, 1984,
Perinatal and maternal mortality in a religious group avoiding obstetric care
American Journal of Obstetrics and Gynaecology 150 (7), 1999, pp826831
41
Maine D, Whats So Special about Maternal Mortality? In Berer M and
Sundari Ravindran T K, (eds), Safe Motherhood Initiatives: Critical Issues, Special
Issue, Reproductive Health Matters 1999
42
Graham W J, Bell J S, Bullough C H W, Can skilled attendance at delivery
reduce maternal mortality in developing countries? In Van Lerverghe W and De
Brouwere V, as note 5 above
46 Panos: Birth rights
43
Good Quality Maternal Health Services.
www.safemotherhood.org/facts_and_figures/maternal_health.htm
44
Acquah C, Borghi J, Ekanmian G, Hanson K, Near-miss audit: economic
analysis Presentation at Near-Miss audit workshop, London School of Hygiene
and Tropical Medicine, 37 September 2001
45
Personal communication with Dr Oona Campbell
46
National Maternal Mortality Study: Egypt 19921993 Preliminary report of
findings and conclusions, Cairo: Child Survival Project, July 1994. Egypt Ministry
of Health 1994. National Maternal Mortality Study: Egypt 2000 Egypt Ministry of
Health and Population, Cairo, John Snow, Inc, June 2001
47
Sundari Ravindran T K, The Untold Story: How The Health Care Systems
In Developing Countries Contribute To Maternal Mortality International Journal
of Health Services, 22, 1992, 3, pp513528
48
Koblinsky M A, Campbell O, Heichelheim J, Organizing delivery care:
what works for safe motherhood? Bulletin of the World Health Organisation, 77, 5,
1999, pp399406
49
Okonofua F E, Abejide A, Makanjuola R A, Ile-Ife, Nigeria: A study of risk
factors Studies in Family Planning, 25, 5, 1992, pp279291
50
Okafor C B, Rizzuto R R, Womens and health-care providers views of
maternal practices in rural Nigeria Studies in Family Planning, 25, 6, 1994,
pp353361
51
Fawcus S, Mbizvo M, Lindmark G, Nystrm, A community-based
investigation of avoidable factors for maternal mortality in Zimbabwe Studies in
Family Planning, 27, 6, 1996, pp319327
52
Bulatoa R A and Ross J A, Rating Maternal and Neonatal Health Programs
in Developing Countries MEASURE Evaluation Project, The Futures Group
International, 2000
53
Press Release: Nursing and Midwifery Services Facing Crisis, Experts Say,
WHO, 20 December 2000
54
AbouZahr C, 1998, as note 3
55
AbouZahr C, 1998, as note 3
56
Press Release, Saving Lives: Skilled Attendance at Childbirth Governments unite
to save womens lives. Secretariat, Inter-Agency Group for Safe Motherhood, 13
November 2000
57
Zhang L and Ding H, 1986, Analysis of cause and rate of maternal death
in 21 provinces, municipalities and autonomous regions Chinese Journal of
Obstetrics and Gynaecology, 1986, 21(4)
58
Ross J A, Campbell O M R, Bulatao R, The Maternal and Neonatal
Programme Effort Index (MNPI) Tropical Medicine and International Health 2001,
6(10), 787798
59
Mother-baby Package Costing Spreadsheet [unpublished]. WHO, Geneva,
1997. Cited in Safe Motherhood Fact Sheet: Maternal Health: A Vital Social and
Economic Investment
60
Starrs A, The Safe Motherhood Action Agenda: Priorities for the Next Decade. New
York: Inter-Agency Group for Safe Motherhood and Family Care International,
1997
61
Safe Motherhood and the World Bank: Lessons from 10 years of experience The
World Bank, 1999
62
Dr Jos Villar, obstetrician and group leader, maternal and perinatal health
research, WHO, presentation to the International Conference on the
Humanization of Childbirth, 24 November 2000, Fortaleza, Brazil
63
Oakley A, Experiments in Knowing: Gender and Method in the Social Sciences
Polity Press, Cambridge, 2000
Panos: Birth rights 47
64
Johnson K C, Randomized Controlled Trials as Authoritative Knowledge:
Keeping an Ally from Becoming a Threat to North American Midwifery Practice
in Davis-Floyd R E, and Sargent C F, Childbirth and Authoritative Knowledge: Cross-
Cultural Perspectives University of California Press, 1997, pp350361
65
Chalmers I, Enkin M, Keirse M J N C, (eds), Effective Care in Pregnancy and
Childbirth Oxford University Press 1989
66
Jordan B, Birth in Four Cultures: A Crosscultural Investigation of Childbirth in
Yucatan, Holland, Sweden and the United States Waveland Press, Inc, Illinois, 1993
67
Xu Q, Smith H, Li Z, et al, 2000, unpublished, cited by Villar (note 62)
68
Kabakian-Khasholian T, et al, Womens experiences of maternity care:
satisfaction or passivity? Social Science and Medicine. 51, 2000 pp10313. Khayat R
and Campbell O, Hospital policies and practices for normal childbirth in
Lebanon Health Policy and Planning. 15(3), 2000, pp2708
69
Eustquio Gomes Choice or Authorised Crime? An epidemic of caesareans
and sterilisations in Brazil in Private Decisions, Public Debate: Women, Reproduction
and Population, Mirsky J, Radlett M, (eds), The Panos Institute, London, 1994,
pp6980
70
Guardian/www.rcog.org.uk
71
Van Lerverghe W and De Brouwere V, Of blind alleys and things that
have worked: historys lessons on reducing maternal mortality in Van
Lerverghe W and De Brouwere V, (eds), Safe Motherhood Strategies: a Review of the
Evidence, Studies in Health Services Organisation & Policy, 2001, 17, pp195227
72
Wu W, Caesarean delivery in Shantou, China: A retrospective analysis of 1922
women Birth 2000, 27, pp8690
73
Thankappan K R, Caesarean section deliveries on the rise in Kerala The
National Medical Journal of India 1999, 12, p297
74
Pai M, Sundaram P, Radhakrishnan K K, Thomas K, Muliyil J P, A high
rate of Caesarean sections in an affluent section of Chennai: Is it cause for
concern? The National Medical Journal of India 1999, 12, pp156158
75
Gonzales-Perez G J, et al, Caesarean sections in Mexico: are there too
many? Health Policy and Planning 16 (1), 2001, pp6267
76
Boseley, S and Chrisafis A, 2001, Hospital Births costing millions The
Guardian, September 29, 2001
77
Bueckens P, 2001, Over-medicalisation of Maternal Care in Developing
Countries in De Brouwere and Van Lerberghe W, (eds), Safe Motherhood
Strategies: a Review of the Evidence, Studies in Health Services Organisation &
Policy, 17, pp195227
78
Argentine Episiotomy Trial Collaborative Group, Routine versus selective
episiotomy: a randomised controlled trial Lancet 1993, 342, pp15171518
79
Otoide V O, Ogvonmwan S M, Okonofua F E, Episiotomy in Nigeria
International Journal of Gynecology and Obstetrics 2000, 68, pp1317
80
Maduma-Butshe A, Dyall A, Garner P, Routine episiotomy in developing
countries; time to change a harmful practice British Medical Journal, 1998, 316,
pp11791180
81
Argentine Episiotomy Trial Collaborative Group, as note 78 above
82
Wiegers T A, van der Zee J, Kerssens J J, Keirse M J N C, Home Birth or
Short-Stay Hospital Birth in a Low Risk Population in the Netherlands Social
Science and Medicine, 46, 11, 1998, pp15051511
83
Jordan B as note 66
84
Donabendian A, The Quality of Care: How Can It Be Assessed? Journal of
the American Medical Association, 1988, 260(12), pp1743-1748
85
Hodnett E D, Support from caregivers in childbirth in: Enkin M W, Keirse,
M J N C, Renfrew M J, Neilson J P, (eds), Pregnancy and Childbirth Module of the
Cochrane Database of Systematic Reviews. London, BMJ Publishing Group, 1995
48 Panos: Birth rights
86
Oakley A, Hickey D, Rajan L, Rigby A, Social support in pregnancy: does
it have long term effects? Journal of Reproductive and Infant Psychology, 141, 1996,
pp722
87
Klaus M, Kennell J, Robertson S, Sosa R, Effects of social support during
parturition on maternal and infant morbidity British Medical Journal, 293, 1986,
pp5857
88
Hofmeyer G J and Nikodem V Ch, et al, Companionship to modify the
clinical birth environment: effects on progress and perceptions of labour and
breastfeeding British Journal of Obstetrics and Gynaecology, 98, 1991, pp756764
89
Klaus M, et al, Maternal Assistance and Support in Labor: Father, Nurse,
Midwife, or Doula? Clinical Consultations in Obstetrics and Gynaecology, 4, (4),
1992, pp17
90
Diniz S, presentation to the ICHC, 24 November 2000
91
Campero, et al, Alone, I wouldnt have known what to do A qualitative
study on social support during labor and delivery in Mexico. Social Science and
Medicine, 1998, 47(3), 395403
92
As note 68
93
Viisainen K, 2000, The moral dangers of home birth: parents perceptions
of risks in home birth in Finland Sociology of Health and Illness, 22, 6, 2000,
pp792814
94
MotherCare Matters, 7(2), Arlington, John Snow, Inc, 1998
95
Sundari Ravindran T K and Berer M, Preventing Maternal Mortality:
Evidence, Resources, Leadership, Action in Berer M and Sundari Ravindran T K,
(eds), Safe Motherhood Initiatives: Critical Issues, Reproductive Health Matters,
Special Edition 1999
96
Para 7.2, Chapter VII: Reproductive Rights and Reproductive Health,
Programme of Action, International Conference on Population and
Development, 1994
97
Sen G and Batliwal S, Empowering Women for Reproductive Rights in
Presser H B and Sen G, (eds), Womens Empowerment and Demographic Processes:
Moving Beyond Cairo, International Studies in Demography, Oxford: Oxford
University Press, 2000
98
Cook R J and Dickens B M as note 25 above
99
Maine D as note 41 above
100
Cook R J and Dickens B M as note 25 above
101
Adamson P, A failure of imagination, The Progress of Nations, 1996
102
Freedman L, Maine D, Womens Mortality: A Legacy of Neglect in
Koblinksky M, Timyan J, Gay J, (eds), The Health of Women: A Global Perspective
Westview Press, Boulder, Colorado, 1993
103
Silence and Complicity: Violence Against Women in Peruvian Public Health
Facilities Latin American and Caribbean Committee for the Defense of
Womens Rights (CLADEM) and the Center for Reproductive Law and Policy
(CRLP), 1999
104
Grossmann-Kendall F, Filippi V, De Koninck M and Kanhonou L, Giving
Birth in Maternity Hospitals in Benin: Testimonies of Women Reproductive Health
Matters, 2001, 9(17)
105
Adamson P, A failure of imagination, The Progress of Nations, 1996
Anda mungkin juga menyukai
- Retirement SpeechDokumen11 halamanRetirement SpeechRayan Castro100% (1)
- The Tragedy of Karbala by Dr. Israr AhmedDokumen13 halamanThe Tragedy of Karbala by Dr. Israr AhmedMehboob Hassan100% (2)
- DLF New Town Gurgaon Soicety Handbook RulesDokumen38 halamanDLF New Town Gurgaon Soicety Handbook RulesShakespeareWallaBelum ada peringkat
- On MCH and Maternal Health in BangladeshDokumen46 halamanOn MCH and Maternal Health in BangladeshTanni ChowdhuryBelum ada peringkat
- PAPER 2 RevisedDokumen36 halamanPAPER 2 RevisedMâyúř PäťîĺBelum ada peringkat
- You Are The Light of The WorldDokumen2 halamanYou Are The Light of The WorldKathleen Lantry100% (1)
- Abortion in The PhilippinesDokumen24 halamanAbortion in The PhilippinesJeff Ray DobluisBelum ada peringkat
- Maternal HealthDokumen43 halamanMaternal HealthAsfand KhanBelum ada peringkat
- The Department of Education On Academic DishonestyDokumen3 halamanThe Department of Education On Academic DishonestyNathaniel VenusBelum ada peringkat
- Tafelberg Short: The Politics of Pregnancy: From 'population control' to women in controlDari EverandTafelberg Short: The Politics of Pregnancy: From 'population control' to women in controlBelum ada peringkat
- 4813 Kit Mother Child Health FinalDokumen3 halaman4813 Kit Mother Child Health FinalRahmania Eka SagitaBelum ada peringkat
- Safe Motherhood: Programme of Action 1994-2004Dokumen3 halamanSafe Motherhood: Programme of Action 1994-2004Rahmania Eka SagitaBelum ada peringkat
- Maternal Mortality: Key FactsDokumen4 halamanMaternal Mortality: Key FactsMasniahBelum ada peringkat
- World Health OrganizationDokumen10 halamanWorld Health OrganizationErlaNuraniBelum ada peringkat
- Who MMRDokumen6 halamanWho MMRviannikkkyBelum ada peringkat
- Family Planning Saves Lives BackgrounderDokumen6 halamanFamily Planning Saves Lives Backgrounderwaqas724Belum ada peringkat
- Yosano Akiko, "Labour Pains," Japan, 1878-1942Dokumen30 halamanYosano Akiko, "Labour Pains," Japan, 1878-1942Vedant TapadiaBelum ada peringkat
- Oral CommDokumen2 halamanOral CommAngelika IngosanBelum ada peringkat
- Abortion RightsDokumen2 halamanAbortion RightsIsleen CleofasBelum ada peringkat
- Maternal Health: Overuse and Under Use of Caesarean Section CoexistDokumen10 halamanMaternal Health: Overuse and Under Use of Caesarean Section CoexistMuhammad HashamBelum ada peringkat
- MANILA, Philippines - It's A Breezy Afternoon in A Cold January, But It's Humid As Usual in This BlockDokumen6 halamanMANILA, Philippines - It's A Breezy Afternoon in A Cold January, But It's Humid As Usual in This BlockErl D. MelitanteBelum ada peringkat
- Abortion Facts and FiguresDokumen5 halamanAbortion Facts and FiguresHershey LeeBelum ada peringkat
- The Social Determinants of Maternal Death and Disability: Rich Mother, Poor MotherDokumen7 halamanThe Social Determinants of Maternal Death and Disability: Rich Mother, Poor MotherHermin DalleBelum ada peringkat
- Unintended Pregnancy and Unsafe Abortion in The PhilippinesDokumen3 halamanUnintended Pregnancy and Unsafe Abortion in The PhilippinesChristian BalbonBelum ada peringkat
- INTRODUCTION Grop 1 Presentation 222Dokumen12 halamanINTRODUCTION Grop 1 Presentation 222Usama Musa DanwaraiBelum ada peringkat
- Abortion, Social Inequity, and Women's Health: Obstetrician-Gynecologists As Agents of ChangeDokumen7 halamanAbortion, Social Inequity, and Women's Health: Obstetrician-Gynecologists As Agents of ChangeSamsul 91Belum ada peringkat
- Maternal Mortality: Where Do Maternal Deaths Occur?Dokumen7 halamanMaternal Mortality: Where Do Maternal Deaths Occur?Pintu KumarBelum ada peringkat
- Meron Second Draft Proposal. 1 Before Docx 2Dokumen27 halamanMeron Second Draft Proposal. 1 Before Docx 2Meron AhmedBelum ada peringkat
- RH Part 3, Socio-EconomicsDokumen18 halamanRH Part 3, Socio-EconomicsDonnaManlangitBelum ada peringkat
- En SRH Fact Sheet LifeandDeathDokumen5 halamanEn SRH Fact Sheet LifeandDeathbirolidiaBelum ada peringkat
- Abortion - Constructive SpeechDokumen4 halamanAbortion - Constructive SpeechRydl Pnp100% (1)
- Unsafe Abortion: The Preventable Pandemic: Sexual and Reproductive Health 4Dokumen13 halamanUnsafe Abortion: The Preventable Pandemic: Sexual and Reproductive Health 4EdyWibowoBelum ada peringkat
- Senior Project Paper 1Dokumen23 halamanSenior Project Paper 1api-455004232Belum ada peringkat
- WHO RHR 19.20 Eng PDFDokumen4 halamanWHO RHR 19.20 Eng PDFElsa SembiringBelum ada peringkat
- Key Facts: Scope of The ProblemDokumen2 halamanKey Facts: Scope of The ProblemKarl Wooden CarnateBelum ada peringkat
- Maternal Health in NigeriaDokumen8 halamanMaternal Health in NigeriaprofangieBelum ada peringkat
- English Bilogy RH BillDokumen2 halamanEnglish Bilogy RH BillAgatha FrancheskaBelum ada peringkat
- Maternal Mortality PDFDokumen101 halamanMaternal Mortality PDFCamille Joy BaliliBelum ada peringkat
- Topic Deaths From Childbirth: Dosen Pengampu: Dr. Masrul, M.PDDokumen12 halamanTopic Deaths From Childbirth: Dosen Pengampu: Dr. Masrul, M.PDNuretikaSalmiaBelum ada peringkat
- Search For The Situation of Unsafe Abortion in Pakistan With Special Emphasis On PunjabDokumen4 halamanSearch For The Situation of Unsafe Abortion in Pakistan With Special Emphasis On PunjabMahnoor AwaisBelum ada peringkat
- Philippines: At-A-Glance: PhilippinesDokumen8 halamanPhilippines: At-A-Glance: PhilippinesGari LazaroBelum ada peringkat
- Safe MotherhoodDokumen16 halamanSafe MotherhoodOswald DachagaBelum ada peringkat
- Final Proposal ExampleDokumen7 halamanFinal Proposal ExampleRichel SuarezBelum ada peringkat
- Adolescent PregnancyDokumen24 halamanAdolescent PregnancyKyler DarkBelum ada peringkat
- Excerpts From An Unpublished Thesis: WWW - Usaid.govDokumen4 halamanExcerpts From An Unpublished Thesis: WWW - Usaid.govJaylen CayBelum ada peringkat
- Maternal Mortality and The Safe Motherhood Programme in Nigeria: Implication For Reproductive HealthDokumen12 halamanMaternal Mortality and The Safe Motherhood Programme in Nigeria: Implication For Reproductive HealthArie Risdiana Asmita'Belum ada peringkat
- HereDokumen6 halamanHereapi-395468231Belum ada peringkat
- Stillbirths: The Invisible Public Health Problem: Embargo: Hold For Release Until 6:30 P.M. EST, April 13Dokumen8 halamanStillbirths: The Invisible Public Health Problem: Embargo: Hold For Release Until 6:30 P.M. EST, April 13Akhmad Fadhiel NoorBelum ada peringkat
- FB Induced Abortion PDFDokumen2 halamanFB Induced Abortion PDFrockyr09Belum ada peringkat
- Midterm Examination in Purposive Communication: Name: Philipp Louie G. Cabarrubias Year/Section: BSMT-1 GolfDokumen4 halamanMidterm Examination in Purposive Communication: Name: Philipp Louie G. Cabarrubias Year/Section: BSMT-1 GolfYoj EscarioBelum ada peringkat
- Demographics Abortion PhilippinesDokumen3 halamanDemographics Abortion PhilippinesspringdingBelum ada peringkat
- Population GrowthDokumen6 halamanPopulation Growthcryptow361Belum ada peringkat
- MY - PROJECT (1) Mai Kwai BroDokumen39 halamanMY - PROJECT (1) Mai Kwai BroAlameen kokoBelum ada peringkat
- 14.future of Health Psy. Part 3Dokumen15 halaman14.future of Health Psy. Part 3noorBelum ada peringkat
- Document 1Dokumen3 halamanDocument 1api-458293384Belum ada peringkat
- WHO RHR 14.08 EngDokumen4 halamanWHO RHR 14.08 EngAkebu LubasiBelum ada peringkat
- Woman's Health (Violence, Menopause, Brest Cancer, and Reproductive Health) Physical Examination and History TakingDokumen41 halamanWoman's Health (Violence, Menopause, Brest Cancer, and Reproductive Health) Physical Examination and History TakingAnonymous hviAPOrJBelum ada peringkat
- Chapter1 1Dokumen8 halamanChapter1 1Sydrix Rulona DapitillaBelum ada peringkat
- Adolescent Pregnancy: Many Adolescent Girls Between 15 and 19 Get PregnantDokumen3 halamanAdolescent Pregnancy: Many Adolescent Girls Between 15 and 19 Get PregnantladyanjaniBelum ada peringkat
- Unintended Pregnancy and Unsafe Abortion in The Philippines - Context and C172750Dokumen12 halamanUnintended Pregnancy and Unsafe Abortion in The Philippines - Context and C172750Khrisha faith TayoBelum ada peringkat
- Focus On AdolescentsDokumen2 halamanFocus On AdolescentsWiljohn de la CruzBelum ada peringkat
- Sexual and Reproductive Health - WikipediaDokumen6 halamanSexual and Reproductive Health - WikipediaBikash ChinharaBelum ada peringkat
- Minister Pledges To Reduce High Maternal and Newborn MortalityDokumen5 halamanMinister Pledges To Reduce High Maternal and Newborn MortalityTrophie NilemoaBelum ada peringkat
- Teenage Pregnancy in The PhilippinesDokumen7 halamanTeenage Pregnancy in The PhilippinesJanine Marie CaprichosaBelum ada peringkat
- (OPINION) It's Time For The Philippines To Decriminalize Abortion By: Clara Rita PadillaDokumen3 halaman(OPINION) It's Time For The Philippines To Decriminalize Abortion By: Clara Rita PadillaLevi BautistaBelum ada peringkat
- PDFDokumen24 halamanPDFGoldi RaghavBelum ada peringkat
- Eicher HR PoliciesDokumen23 halamanEicher HR PoliciesNakul100% (2)
- Contract of Lease - Torres My FarmDokumen2 halamanContract of Lease - Torres My FarmAngeles Sabandal SalinasBelum ada peringkat
- EIB Pan-European Guarantee Fund - Methodological NoteDokumen6 halamanEIB Pan-European Guarantee Fund - Methodological NoteJimmy SisaBelum ada peringkat
- Report of Apple Success PDFDokumen2 halamanReport of Apple Success PDFPTRBelum ada peringkat
- Basic Accounting Equation Exercises 2Dokumen2 halamanBasic Accounting Equation Exercises 2Ace Joseph TabaderoBelum ada peringkat
- Variable Costing Case Part A SolutionDokumen3 halamanVariable Costing Case Part A SolutionG, BBelum ada peringkat
- Organizational Behavior: Chapter 6: Understanding Work TeamDokumen6 halamanOrganizational Behavior: Chapter 6: Understanding Work TeamCatherineBelum ada peringkat
- Sarala Bastian ProfileDokumen2 halamanSarala Bastian ProfileVinoth KumarBelum ada peringkat
- Lean Supply Chains: Chapter FourteenDokumen29 halamanLean Supply Chains: Chapter FourteenKshitij SharmaBelum ada peringkat
- 2016 GMC Individuals Round 1 ResultsDokumen2 halaman2016 GMC Individuals Round 1 Resultsjmjr30Belum ada peringkat
- Budo Hard Style WushuDokumen29 halamanBudo Hard Style Wushusabaraceifador0% (1)
- An Assessment On The Impact of Indutrialization On Economic Growth in Nigeria PDFDokumen49 halamanAn Assessment On The Impact of Indutrialization On Economic Growth in Nigeria PDFSebastian GroveBelum ada peringkat
- ADPO Syllabus - 10Dokumen2 halamanADPO Syllabus - 10pranjal.singhBelum ada peringkat
- Open Quruan 2023 ListDokumen6 halamanOpen Quruan 2023 ListMohamed LaamirBelum ada peringkat
- MAKAUT CIVIL Syllabus SEM 8Dokumen9 halamanMAKAUT CIVIL Syllabus SEM 8u9830120786Belum ada peringkat
- Student Guidelines The School PoliciesDokumen5 halamanStudent Guidelines The School PoliciesMaritessBelum ada peringkat
- Au L 53229 Introduction To Persuasive Text Powerpoint - Ver - 1Dokumen13 halamanAu L 53229 Introduction To Persuasive Text Powerpoint - Ver - 1Gacha Path:3Belum ada peringkat
- Census 2011 PDFDokumen2 halamanCensus 2011 PDFvishaliBelum ada peringkat
- 4-Cortina-Conill - 2016-Ethics of VulnerabilityDokumen21 halaman4-Cortina-Conill - 2016-Ethics of VulnerabilityJuan ApcarianBelum ada peringkat
- Pentesting ReportDokumen14 halamanPentesting Reportazeryouness6787Belum ada peringkat
- Pineapples Export's To Copenhagen, DenmarkDokumen13 halamanPineapples Export's To Copenhagen, DenmarkMuhammad SyafiqBelum ada peringkat
- (MX) Public Figures, Private LivesDokumen3 halaman(MX) Public Figures, Private LivesbestatemanBelum ada peringkat
- Vayigash BookletDokumen35 halamanVayigash BookletSalvador Orihuela ReyesBelum ada peringkat
- Unit Test 11 PDFDokumen1 halamanUnit Test 11 PDFYOBelum ada peringkat