DeliveryOptions FS en
Diunggah oleh
gerryajun0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
6 tayangan1 halamanDeliveryOptions FS E
Judul Asli
DeliveryOptions FS En
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniDeliveryOptions FS E
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
6 tayangan1 halamanDeliveryOptions FS en
Diunggah oleh
gerryajunDeliveryOptions FS E
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 1
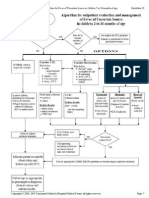
Delivery Options for HIV Positive Pregnant Women
I am HIV positive and pregnant. What
delivery options are available to me when I
give birth?
Depending on your health and treatment status, you may
plan to have either a cesarean (also called c-section) or a
vaginal delivery. The decision of whether to have a
cesarean or a vaginal delivery is something that you
should discuss with your doctor during your pregnancy.
How do I decide which delivery option is
best for my baby and me?
It is important that you discuss your delivery options with
your doctor as early as possible in your pregnancy so that
he or she can help you decide which delivery method is
most appropriate for you.
Cesarean delivery is recommended for an HIV positive
mother when:
her viral load is unknown or is greater than 1,000
copies/mL at 36 weeks of pregnancy
she has not taken any anti-HIV medications or has
only taken AZT (Retrovir or zidovudine) during her
pregnancy
she has not received prenatal care until 36 weeks into
her pregnancy or later
To be most effective in preventing transmission, the
cesarean should be scheduled at 38 weeks or should be
done before the rupture of membranes (also called
water breaking).
Vaginal delivery is recommended for an HIV positive
mother when:
she has been receiving prenatal care throughout her
pregnancy
she has a viral load less than 1,000 copies/mL at 36
weeks, and
Vaginal delivery may also be recommended if a mother
has ruptured membranes and labor is progressing rapidly.
What are the risks involved with these
delivery options?
All deliveries have risks. The risk of mother-to-child
transmission of HIV may be higher for vaginal delivery
than for a scheduled cesarean. For the mother, cesarean
delivery has an increased risk of infection, anesthesia-
related problems, and other risks associated with any type
of surgery. For the infant, cesarean delivery has an
increased risk of infant respiratory distress.
Is there anything else I should know about
labor and delivery?
Intravenous (IV) AZT should be started 3 hours before a
scheduled cesarean delivery and should be continued until
delivery. IV AZT should be given throughout labor and
delivery for a vaginal delivery. It is also important to
minimize the baby's exposure to the mother's blood. This
can be done by avoiding any invasive monitoring and
forceps- or vacuum-assisted delivery.
All babies born to HIV positive mothers should receive
anti-HIV medication to prevent mother-to-child
transmission of HIV. The usual treatment for infants is 6
weeks of AZT; sometimes, additional medications are also
given (see the HIV Positive Women and Their Babies
After Birth Fact Sheet).
For more information:
Contact your doctor or an AIDSinfo Health Information
Specialist at 1 800 448 0440 or http://aidsinfo.nih.gov.
A Service of the U.S. Department of
Health and Human Services
HIV and Pregnancy Delivery Options
Terms Used in This Fact Sheet:
Intravenous (IV): the administration of fluid or medicine into a
vein.
Mother-to-child transmission: the passage of HIV from an HIV
positive mother to her infant. The infant may become infected
while in the womb, during labor and delivery, or through
breastfeeding. Also known as perinatal transmission.
Prenatal: the time before birth.
Rupture of membranes: when the sac containing the unborn
baby bursts or develops a hole. Also known as water breaking.
Reviewed
May 2009
This information is based on the U.S. Public Health Service's Recommendations for Use of Antiretroviral
Drugs in Pregnant HIV-Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV
Transmission in the United States (available at http://aidsinfo.nih.gov).
Anda mungkin juga menyukai
- Vulvar Cancer References ListDokumen2 halamanVulvar Cancer References ListgerryajunBelum ada peringkat
- Maternal Mortality Causes ListDokumen2 halamanMaternal Mortality Causes ListgerryajunBelum ada peringkat
- The Isolation of DermatophytesDokumen5 halamanThe Isolation of DermatophytesgerryajunBelum ada peringkat
- Parapneumonic Effusion and EmpyemaDokumen6 halamanParapneumonic Effusion and EmpyemagerryajunBelum ada peringkat
- Patient Conference ReportDokumen8 halamanPatient Conference ReportgerryajunBelum ada peringkat
- Jbs Jan2006Dokumen7 halamanJbs Jan2006gerryajunBelum ada peringkat
- 01 002Dokumen3 halaman01 002gerryajunBelum ada peringkat
- Pleural Effusions 2Dokumen6 halamanPleural Effusions 2gerryajunBelum ada peringkat
- Archive of SID: A First Case of Tinea Imbricata From IranDokumen4 halamanArchive of SID: A First Case of Tinea Imbricata From IrangerryajunBelum ada peringkat
- Microsporum gypseum in an AIDS PatientDokumen4 halamanMicrosporum gypseum in an AIDS PatientgerryajunBelum ada peringkat
- Trends in COPD: Factsheet 2003/1Dokumen2 halamanTrends in COPD: Factsheet 2003/1gerryajunBelum ada peringkat
- O 387Dokumen4 halamanO 387gerryajunBelum ada peringkat
- S 1368980003000880 ADokumen8 halamanS 1368980003000880 AgerryajunBelum ada peringkat
- Sample Statistics: For Use With PressDokumen2 halamanSample Statistics: For Use With PressgerryajunBelum ada peringkat
- Chronic Obstructive Pulmonary DiseaseDokumen2 halamanChronic Obstructive Pulmonary DiseasegerryajunBelum ada peringkat
- COPD - Chronic Bronchitis & Emphysema: How The Lungs Work?Dokumen2 halamanCOPD - Chronic Bronchitis & Emphysema: How The Lungs Work?gerryajunBelum ada peringkat
- COPD ProposalDokumen8 halamanCOPD ProposalgerryajunBelum ada peringkat
- FELINE-Efficacy of Imidacloprid in Controlling Flea Allergy Dermatitis in CatsDokumen3 halamanFELINE-Efficacy of Imidacloprid in Controlling Flea Allergy Dermatitis in Catstaner_soysurenBelum ada peringkat
- Volume 10, Issue 3, December 2009 - A Level of Gastrin Serum and Ulcer Size On Gastric Ulcer Correlated To Helicobacter Pylori Infection PDFDokumen4 halamanVolume 10, Issue 3, December 2009 - A Level of Gastrin Serum and Ulcer Size On Gastric Ulcer Correlated To Helicobacter Pylori Infection PDFgerryajunBelum ada peringkat
- GlaucomaDokumen12 halamanGlaucomagerryajunBelum ada peringkat
- Italian Fever 2Dokumen1 halamanItalian Fever 2gerryajunBelum ada peringkat
- Cit Plain 57424744Dokumen1 halamanCit Plain 57424744gerryajunBelum ada peringkat
- Inguinal HerniaDokumen2 halamanInguinal HerniagerryajunBelum ada peringkat
- O 387Dokumen4 halamanO 387gerryajunBelum ada peringkat
- Inguinal HerniaDokumen2 halamanInguinal HerniagerryajunBelum ada peringkat
- Facts About Chronic Obstructive Pulmonary Disease: What It IsDokumen2 halamanFacts About Chronic Obstructive Pulmonary Disease: What It IsgerryajunBelum ada peringkat
- Peptic UlcerDokumen5 halamanPeptic UlcermerobabuBelum ada peringkat
- Chronic Obstructive Pulmonary DiseaseDokumen2 halamanChronic Obstructive Pulmonary DiseasegerryajunBelum ada peringkat
- 01 002Dokumen3 halaman01 002gerryajunBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- What Is Millenium Development Goal (MDG) ?Dokumen5 halamanWhat Is Millenium Development Goal (MDG) ?memagawaBelum ada peringkat
- CHED Student Logbook for Surgery ProceduresDokumen2 halamanCHED Student Logbook for Surgery ProceduresMarieCrisBelum ada peringkat
- Study of Incidence and Risk Factors For Surgical Site Infection After Cesarean Section at First Referral UnitDokumen3 halamanStudy of Incidence and Risk Factors For Surgical Site Infection After Cesarean Section at First Referral UnitFaozan FikriBelum ada peringkat
- Fundamentals of Caregiving Learner’s GuideDokumen357 halamanFundamentals of Caregiving Learner’s GuideBfp SapangdalagaBelum ada peringkat
- Case Study Fnes 366Dokumen6 halamanCase Study Fnes 366api-347761303Belum ada peringkat
- Balanced Diet ChartDokumen2 halamanBalanced Diet ChartjosephBelum ada peringkat
- Hypothyroidism - StatPearls - NCBI BookshelfDokumen10 halamanHypothyroidism - StatPearls - NCBI BookshelfKarla CordobaBelum ada peringkat
- The same questions apply as aboveDokumen29 halamanThe same questions apply as aboveمحمد عزيز حسن ماضيBelum ada peringkat
- PURELL® Advanced Hand Sanitizer Refresh-Ing Gel: Safety Data SheetDokumen15 halamanPURELL® Advanced Hand Sanitizer Refresh-Ing Gel: Safety Data SheetParth PatelBelum ada peringkat
- Development of Keloid After Surgery & Its TreatmentDokumen2 halamanDevelopment of Keloid After Surgery & Its TreatmentInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- (DR Schuster, Nykolyn) Communication For Nurses H (BookFi)Dokumen215 halaman(DR Schuster, Nykolyn) Communication For Nurses H (BookFi)Ariefatun Nisa100% (1)
- Product B - Edhawa Herbal MedicineDokumen3 halamanProduct B - Edhawa Herbal MedicineJae Tuffie KatneesBelum ada peringkat
- MarijuanaDokumen18 halamanMarijuanaShelby WaltersBelum ada peringkat
- Brain Tumors - KY Cancer RegistryDokumen45 halamanBrain Tumors - KY Cancer RegistryMohammad Galih PratamaBelum ada peringkat
- Pacres SpeechDokumen3 halamanPacres SpeechJohn Emmanuel PacresBelum ada peringkat
- Digital Rectal ExaminationDokumen7 halamanDigital Rectal ExaminationAla'a Emerald AguamBelum ada peringkat
- Grade 6 Health Module 4 FinalDokumen18 halamanGrade 6 Health Module 4 FinalSassa IndominationBelum ada peringkat
- Form Contractor Induction ChecklistDokumen2 halamanForm Contractor Induction ChecklistnikBelum ada peringkat
- Maria Thomas PDFDokumen143 halamanMaria Thomas PDFElizabeth Sinchana100% (2)
- ANM application detailsDokumen3 halamanANM application detailsSOFIKUL HUUSAINBelum ada peringkat
- Post Offer Employment Health Questionnaire SalariedDokumen2 halamanPost Offer Employment Health Questionnaire Salariedtylers0421Belum ada peringkat
- Action Plan On Medical and Nursing: Resource ReqmtsDokumen15 halamanAction Plan On Medical and Nursing: Resource ReqmtsJude Mathew100% (2)
- Chief complaint dental historyDokumen6 halamanChief complaint dental historyralucaBelum ada peringkat
- Pneumonia AnswersDokumen5 halamanPneumonia AnswersColeen Mae CamaristaBelum ada peringkat
- 842 2027 1 SM PDFDokumen11 halaman842 2027 1 SM PDFAngel Franda PutriBelum ada peringkat
- Journal Homepage: - : IntroductionDokumen2 halamanJournal Homepage: - : IntroductionIJAR JOURNALBelum ada peringkat
- Discharge PlanDokumen2 halamanDischarge PlanabraBelum ada peringkat
- Minnesota Multiphasic Personality Inventory TestDokumen26 halamanMinnesota Multiphasic Personality Inventory TestGicu BelicuBelum ada peringkat
- Answer Key CicDokumen3 halamanAnswer Key Cictiburshoc16Belum ada peringkat
- Peace Corps Mefloquine Policy March 2015 Letter To DirectorDokumen7 halamanPeace Corps Mefloquine Policy March 2015 Letter To DirectorAccessible Journal Media: Peace Corps DocumentsBelum ada peringkat