Congestive Heart Failure
Diunggah oleh
Merlyn Rivera Pelecin0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
139 tayangan20 halamanNCP, Drug Study
Hak Cipta
© © All Rights Reserved
Format Tersedia
XLSX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniNCP, Drug Study
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai XLSX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
139 tayangan20 halamanCongestive Heart Failure
Diunggah oleh
Merlyn Rivera PelecinNCP, Drug Study
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai XLSX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 20
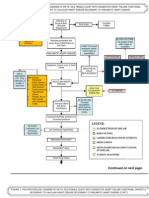
Assessment Diagnosis Goal of Care Intervention
S: Long Term Goal:
After 1 month of
nursing intervention,
the patient will display
hemodynamic stability
(BP, cardiac output,
urinary output and
peripheral pulses
within normal limits)
Independent: Auscultate
apical pulse; assess heart rate,
rhythm
Note heart sounds.
Palpate peripheral pulses.
Monitor BP.
Inspect skin for pallor,
cyanosis.
Monitor urine output, noting
decreasing output and
dark/concentrated urine.
O:
Decreased cardiac
output related to
decreased myocardial
contractility
Short Term Goals:
After 12 hours of
nursing intervention:
-Patient's breath
sounds will be clear to
auscultation
-Patient will have no
signs of dyspnea
-Patient will
demonstrate an
increase in activity
tolerance
Note changes in sensorium,
e.g., lethargy, confusion,
disorientation, anxiety, and
depression.
Encourage rest,
semirecumbent in bed or
chair. Assist with physical
care as indicated.
Provide quiet environment;
explain medical/ nursing
management; help patient
avoid stressful situations;
listen/ respond to expressions
of feelings/ fears.
Provide bedside commode.
Have patient avoid activities
eliciting a vasovagal response,
e.g., straining during
defecation, holding breath
during position changes.
Elevate legs, avoiding
pressure under knee.
Encourage active/ passive
exercises. Increase
ambulation/ activity as
tolerated.
Check for calf tenderness;
diminished pedal pulse;
swelling, local redness, or
pallor of extremity.
Educate patient and caregivers
about the importance of taking
prescribed medications at
prescribed times
Dependent: Administer
supplemental oxygen as
indicated.
Administer medications as
indicated
O:
Decreased cardiac
output related to
decreased myocardial
contractility
Short Term Goals:
After 12 hours of
nursing intervention:
-Patient's breath
sounds will be clear to
auscultation
-Patient will have no
signs of dyspnea
-Patient will
demonstrate an
increase in activity
tolerance
Administer IV solutions,
restricting total amount as
indicated. Avoid saline
solutions.
Monitor/ replace electrolytes.
Educate patient and caregivers
about the importance of taking
prescribed medications at
prescribed times
Assessment Diagnosis Goal of Care Intervention
Long Term Goal: After
1 month of nursing
intervention, the
patient will
demonstrate stabilized
fluid volume with
balanced intake and
output, breath sounds
clear, vital signs within
acceptable range,
stable weight, and
absence of edema.
Independent:
Monitor urine output, noting
amount and color, as well as
time of day when diuresis
occurs.
Monitor/ calculate 24-hour
intake and output (I&O)
balance.
Maintain chair or bedrest in
semi-Fowlers position.
Establish fluid intake schedule
if fluids are medically
restricted, incorporating
beverage preferences when
possible. Give frequent mouth
care/ ice chips as part of fluid
allotment.
O:
Decreased cardiac
output related to
decreased myocardial
contractility
Short Term Goals:
After 12 hours of
nursing intervention:
-Patient's breath
sounds will be clear to
auscultation
-Patient will have no
signs of dyspnea
-Patient will
demonstrate an
increase in activity
tolerance
Fluid volume excess
O: Orthopnea
S3 heart sound
Oliguria Hypertension
abnormal breath
sounds
Short Term Goal: After
12 hours of nursing
intervention, the
patient will display
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization of at
least 3 required dietary
changes
Weigh daily.
Assess for distended neck and
peripheral vessels. Inspect
dependent body areas for
edema with/ without pitting;
note presence of generalized
body edema (anasarca).
Change position frequently.
Elevate feet when sitting.
Inspect skin surface, keep dry,
and provide padding as
indicated.
Auscultate breath sounds,
noting decreased and/or
adventitious sounds, e.g.,
crackles, wheezes. Note
presence of increased
dyspnea, tachypnea,
orthopnea, paroxysmal
nocturnal dyspnea, persistent
cough.
Investigate reports of sudden
extreme dyspnea/ air hunger,
need to sit straight up,
sensation of suffocation,
feelings of panic or impending
doom.
Monitor BP
Fluid volume excess
O: Orthopnea
S3 heart sound
Oliguria Hypertension
abnormal breath
sounds
Short Term Goal: After
12 hours of nursing
intervention, the
patient will display
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization of at
least 3 required dietary
changes
Assess bowel sounds. Note
complaints of anorexia,
nausea, abdominal distension,
constipation.
Provide small, frequent, easily
digestible meals.
Measure abdominal girth, as
indicated.
Encourage verbalization of
feelings regarding limitations.
Maintain fluid/ sodium
restrictions as indicated.
Dependent:
Administer medications as
indicated
Consult with dietitian.
Assessment Diagnosis Goal of Care Intervention
S: Long Term Goal: After
1 month of nursing
intervention, the
patient will be able to
participate in desired
activities and meet
own self-care needs.
Independent: Check
vital signs before and
immediately after activity,
especially if patient is
receiving vasodilators,
diuretics, or beta-blockers.
Document cardiopulmonary
response to activity. Note
tachycardia, dysrhythmias,
dyspnea, diaphoresis, pallor.
Assess for other
precipitators/causes of fatigue,
e.g., treatments, pain,
medications.
Evaluate accelerating activity
intolerance.
Fluid volume excess
O: Orthopnea
S3 heart sound
Oliguria Hypertension
abnormal breath
sounds
Short Term Goal: After
12 hours of nursing
intervention, the
patient will display
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization of at
least 3 required dietary
changes
Activity intolerance
related to poor cardiac
reserve
O:
V/S presence
of dysrhythmias
dyspnea pallor
Short Term Goal: After
12 hours of nursing
intervention, the
patient will achieve
measurable increase in
activity tolerance
evidenced by reduced
fatigue and weakness
and by vital signs
within acceptable
limits during activity.
Provide assistance with self-
care activities as indicated.
Intersperse activity periods
with rest periods.
Collaborative: Implement
graded cardiac
rehabilitation/activity
program.
Assessment Diagnosis Goal of Care Intervention
Long Term Goal: After
1 month of nursing
intervention, the
patient will participate
in treatment regimen
within level of
ability/situation.
Independent:
Auscultate breath sounds,
noting crackles, wheezes.
Instruct patient in effective
coughing, deep breathing.
Encourage frequent position
changes.
Maintain chair/bedrest, with
head of bed elevated 2030
degrees, semi-Fowlers
position. Support arms with
pillows.
Monitor/graph serial ABGs,
pulse oximetry.
Dependent:
Administer supplemental
oxygen as indicated.
Administer medications as
indicated
Assessment Diagnosis Goal of Care Intervention
Activity intolerance
related to poor cardiac
reserve
O:
V/S presence
of dysrhythmias
dyspnea pallor
Short Term Goal: After
12 hours of nursing
intervention, the
patient will achieve
measurable increase in
activity tolerance
evidenced by reduced
fatigue and weakness
and by vital signs
within acceptable
limits during activity.
Risk for impaired gas
exchange related to
fluid shifts into
interstitial
space/alveoli
Short Term Goal:
After 12 hours of
nursing intervention,
the patient will
demonstrate adequate
ventilation and
oxygenation of tissues
evidenced by oximetry
within patients normal
ranges and free of
symptoms of
respiratory distress.
Long Term Goal: After
1 month of nursing
intervention, the
patient will maintain
skin integrity.
Independent: Inspect
skin, noting skeletal
prominences, presence of
edema, areas of altered
circulation/pigmentation, or
obesity/emaciation.
Provide gentle massage
around reddened or blanched
areas.
Encourage frequent position
changes in bed/chair, assist
with active/passive range of
motion (ROM) exercises.
Provide frequent skin care;
minimize contact with
moisture/excretions.
Check fit of shoes/slippers
and change as needed.
Provide alternating
pressure/egg-crate mattress,
sheep skin elbow/heel
protectors.
Risk for impaired skin
integrity related to
decreased tissue
perfusion
Short Term Goal:
After 12 hours of
nursing intervention,
the patient will
demonstrate at least 2
behaviors/ techniques
to prevent skin
breakdown.
Rationale Evaluation
Tachycardia is usually present (even at
rest) to compensate for decreased
ventricular contractility
S1 and S2 may be weak because of
diminished pumping action. Gallop
rhythms are common (S3and S4),
produced as blood flows into
noncompliant/ distended chambers.
Murmurs may reflect valvular
incompetence/ stenosis.
Decreased cardiac output may be
reflected in diminished radial, popliteal,
dorsalis pedis, and posttibial pulses.
Pulses may be fleeting or irregular to
palpation, and pulsus alternans (strong
beat alternating with weak beat) may be
present.
In early, moderate, or chronic HF, BP
may be elevated because of increased
SVR. In advanced HF, the body may no
longer be able to compensate, and
profound/ irreversible hypotension may
occur.
Pallor is indicative of diminished
peripheral perfusion secondary to
inadequate cardiac output,
vasoconstriction, and anemia. Cyanosis
may develop in refractory HF. Dependent
areas are often blue or mottled as venous
congestion increases.
Kidneys respond to reduced cardiac
output by retaining water and sodium.
Urine output is usually decreased during
the day because of fluid shifts into tissues
but may be increased at night because
fluid returns to circulation when patient is
recumbent.
Goal Met: After
12 hours of nursing
intervention: -
Patient's breath sounds
was clear to
auscultation
-Patient had no signs
of dyspnea
-Patient demonstrated
an increase in activity
tolerance
May indicate inadequate cerebral
perfusion secondary to decreased cardiac
output.
Physical rest should be maintained during
acute or refractory HF to improve
efficiency of cardiac contraction and to
decrease myocardial oxygen demand/
consumption and workload.
Psychological rest helps reduce emotional
stress, which can produce
vasoconstriction, elevating BP and
increasing heart rate /work.
Commode use decreases work of getting
to bathroom or struggling to use bedpan.
Vasovagal maneuver causes vagal
stimulation followed by rebound
tachycardia, which further compromises
cardiac function /output.
Decreases venous stasis, and may reduce
incidence of thrombus/embolus
formation.
Reduced cardiac output, venous pooling
/stasis, and enforced bedrest increases
risk of thrombophlebitis.
Patient is often on multiple medications
which can be difficult to manage, thus
increasing the likelihood that medications
can be missed or incorrectly used
Increases available oxygen for myocardial
uptake to combat effects of hypoxia
/ischemia.
A variety of medications may be used to
increase stroke volume, improve
contractility, and reduce congestion.
Goal Met: After
12 hours of nursing
intervention: -
Patient's breath sounds
was clear to
auscultation
-Patient had no signs
of dyspnea
-Patient demonstrated
an increase in activity
tolerance
Because of existing elevated left
ventricular pressure, patient may not
tolerate increased fluid volume (preload).
Patients with HF also excrete less
sodium, which causes fluid retention and
increases myocardial workload.
Fluid shifts and use of diuretics can alter
electrolytes (especially potassium and
chloride), which affect cardiac rhythm
and contractility.
Patient is often on multiple medications
which can be difficult to manage, thus
increasing the likelihood that medications
can be missed or incorrectly used
Rationale Evaluation
Urine output may be scanty and
concentrated (especially during the day)
because of reduced renal perfusion.
Recumbency favors diuresis; therefore,
urine output may be increased at night/
during bedrest.
Diuretic therapy may result in sudden/
excessive fluid loss (circulating
hypovolemia), even though edema
/ascites remains.
Recumbency increases glomerular
filtration and decreases production of
ADH, thereby enhancing diuresis.
Involving patient in therapy regimen may
enhance sense of control and cooperation
with restrictions.
Goal Met: After
12 hours of nursing
intervention: -
Patient's breath sounds
was clear to
auscultation
-Patient had no signs
of dyspnea
-Patient demonstrated
an increase in activity
tolerance
Goal Met: After
12 hours of nursing
intervention, the
patient displayed
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization that
she should avoid salty
and fatty foods and
should limit her fluid
intake
Documents changes in/ resolution of
edema in response to therapy. A gain of 5
lb represents approximately 2 L of fluid.
Conversely, diuretics can result in rapid/
excessive fluid shifts and weight loss.
Excessive fluid retention may be
manifested by venous engorgement and
edema formation. Peripheral edema
begins in feet/ ankles (or dependent areas)
and ascends as failure worsens. Pitting
edema is generally obvious only after
retention of at least 10 lb of fluid.
Increased vascular congestion (associated
with RHF) eventually results in systemic
tissue edema.
Edema formation, slowed circulation,
altered nutritional intake, and prolonged
immobility /bedrest are cumulative
stressors that affect skin integrity and
require close supervision/ preventive
interventions.
Excess fluid volume often leads to
pulmonary congestion. Symptoms of
pulmonary edema may reflect acute left-
sided HF. RHFs respiratory symptoms
(dyspnea, cough, orthopnea) may have
slower onset but are more difficult to
reverse.
May indicate development of
complications (pulmonary edema/
embolus) and differs from
orthopneaparoxysmal nocturnal dyspnea
in that it develops much more rapidly and
requires immediate intervention.
Hypertension suggest fluid volume
excess and may reflect developing/
increasing pulmonary congestion.
Goal Met: After
12 hours of nursing
intervention, the
patient displayed
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization that
she should avoid salty
and fatty foods and
should limit her fluid
intake
Visceral congestion (occurring in
progressive HF) can alter gastric/
intestinal function.
Reduced gastric motility can adversely
affect digestion and absorption. Small,
frequent meals may enhance digestion/
prevent abdominal discomfort.
In progressive RHF, fluid may shift into
the peritoneal space, causing increasing
abdominal girth (ascites).
Expression of feelings/ concerns may
decrease stress/ anxiety, which is an
energy drain that can contribute to
feelings of fatigue.
Reduces total body water/ prevents fluid
reaccumulation.
To help promote wellness.
May be necessary to provide diet
acceptable to patient that meets caloric
needs within sodium restriction.
Rationale Evaluation
Orthostatic hypotension can occur with
activity because of medication effect
(vasodilation), fluid shifts (diuresis), or
compromised cardiac pumping function.
Compromised myocardium/inability to
increase stroke volume during activity
may cause an immediate increase in heart
rate and oxygen demands, thereby
aggravating weakness and fatigue.
Fatigue is a side effect of some
medications (e.g., beta-blockers,
tranquilizers, and sedatives). Pain and
stressful regimens also extract energy and
produce fatigue.
May denote increasing cardiac
decompensation rather than overactivity.
Goal Met: After
12 hours of nursing
intervention, the
patient displayed
understanding of
individual dietary/fluid
restrictions evidenced
by verbalization that
she should avoid salty
and fatty foods and
should limit her fluid
intake
Goal Met: After
12 hours of nursing
intervention, the
patient achieved
measurable increase in
activity tolerance
evidenced by reduced
fatigue and weakness
and by vital signs
within acceptable
limits during activity.
Meets patients personal care needs
without undue myocardial
stress/excessive oxygen demand.
Strengthens and improves cardiac
function under stress, if cardiac
dysfunction is not irreversible. Gradual
increase in activity avoids excessive
myocardial workload and oxygen
consumption.
Rationale Evaluation
Reveals presence of pulmonary
congestion/collection of secretions,
indicating need for further intervention.
Clears airways and facilitates oxygen
delivery.
Helps prevent atelectasis and pneumonia.
Reduces oxygen consumption/demands
and promotes maximal lung inflation.
Hypoxemia can be severe during
pulmonary edema. Compensatory
changes are usually present in chronic
HF.Note: In patients with abnormal
cardiac index, research suggests pulse
oximeter measurements may exceed
actual oxygen saturation by up to 7%.
Increases alveolar oxygen concentration,
which may correct/reduce tissue
hypoxemia.
To help promote wellness.
Rationale Evaluation
Goal Met: After
12 hours of nursing
intervention, the
patient achieved
measurable increase in
activity tolerance
evidenced by reduced
fatigue and weakness
and by vital signs
within acceptable
limits during activity.
Goal Met: After
12 hours of nursing
intervention, the
patient demonstrated
adequate ventilation
and oxygenation of
tissues evidenced by
O2 Sat = 95% and free
of symptoms of
respiratory distress.
Skin is at risk because of impaired
peripheral circulation, physical
immobility, and alterations in nutritional
status.
Short Term Goal:
After 12 hours of
nursing intervention,
the patient
demonstrated 2
behaviors/ techniques
to prevent skin
breakdown like
frequent position
changes in bed and
active range of motion
(ROM) exercises
Improves blood flow, minimizing tissue
hypoxia.Note: Direct massage of
compromised area may cause tissue
injury.
Reduces pressure on tissues, improving
circulation and reducing time any one
area is deprived of full blood flow.
Excessive dryness or moisture damages
skin and hastens breakdown.
Dependent edema may cause shoes to fit
poorly, increasing risk of pressure and
skin breakdown on feet.
Reduces pressure to skin, may improve
circulation.
Drug Name Indications/Contraindications
Cefuroxime 750mg IVTT
Drug Name Indications/Contraindications
Paracetamol 500mg 1 tab q 8h
for fever
Indications: To
relieve mild to moderate pain such
as headache, muscle and joint pain,
and backache. It is also used to
bring down a high temperature.
Drug Name Indications/Contraindications
Contraindications: -
Contraindicated in patients with
allergy to acetaminophen.
-Use cautiously with impaired
hepatic function, chronic
alcoholism, pregnancy, lactation.
Action:
Decreases fever by a
hypothalamic effect leading to
sweating and vasodilation;
Inhibits pyrogen effect on the
hypothalamic-heat-regulating
centers; Inhibits CNS
prostaglandin synthesis with
minimal effects on peripheral
prostaglandin synthesis
Indications: It
is effective for the treatment of
penicillinase-producing Neisseria
gonorrhoea (PPNG). Effectively
treats bone and joint infections,
bronchitis, meningitis, gonorrhea,
otitis media, pharyngitis/tonsillitis,
Contraindications:
Hypersensitivity to
cephalosporins and related
antibiotics; pregnancy
(category B), lactation.
Action: Binds
to one or more of the penicillin-
binding proteins (PBPs) which
inhibits the final
transpeptidation step of
peptidoglycan synthesis in
bacterial cell wall, thus
inhibiting biosynthesis and
arresting cell wall assembly
resulting in bacterial cell death.
Furosemide 80mg IVTT Inidications: Treatment
of edema associated with CHF,
cirrhosis of liver, and kidney
disease, including nephrotic
syndrome. May be used for
management of hypertension, alone
or in combination with other
antihypertensive agents, and for
treatment of hypercalcemia. Has
been used concomitantly with
mannitol for treatment of severe
cerebral edema, particularly in
meningitis.
Drug Name Indications/Contraindications
Salbutamol 1 neb q 6 Indications: To
relieve bronchospasm associated
with acute or chronic asthma,
bronchitis, or other reversible
obstructive airway diseases. Also
used to prevent exercise-induced
bronchospasm.
Action:
Acts relatively selectively at
beta2-adrenergic receptors to
cause bronchodilation and
vasodilation; at higher doses,
beta2 selectivity is lost, and the
drug acts at beta2 receptors to
cause typical sympathomimetic
Contraindications: Contraindicated
with hypersensitivity to albuterol;
tachyarrhythmias, tachycardia
caused by digitalis intoxication;
general anesthesia with halogenated
hydrocarbons or cyclopropane
(these sensitize the myocardium to
catecholamines); unstable
Contraindication: -
Severe sodium and water depletion,
hypersensitivity to sulphonamides
and furosemide, hypokalaemia,
hyponatraemia, precomatose states
associated with liver cirrhosis,
anuria or renal failure.
-Addisons disease.
Action:
Inhibits reabsorption of Na and
chloride mainly in the
medullary portion of the
ascending Loop of Henle.
Excretion of potassium and
ammonia is also increased
while uric acid excretion is
reduced. It increases plasma-
renin levels and secondary
hyperaldosteronism may result.
Furosemide reduces BP in
hypertensives as well as in
normotensives. It also reduces
pulmonary oedema before
diuresis has set in.
Drug Name Indications/Contraindications
Aldazide 1 tab BID Indications:
Essential hypertension, edema and
ascites of CHF, liver cirrhosis,
nephritic syndrome, idiopathic
edema
Action:
Competes with aldosterone for
receptor sites in the distal renal
tubules, increasing sodium
chloride and water excretion
while conserving potassium
and hydrogen ions, may block
the effect of aldosterone on
arteriolar smooth muscle as
well
Contraindications:
Acute renal insufficiency, rapid
deterioration of renal function,
anuria, hyperkalaemia or sensitivity
to thiazides. Lactating mothers
should not receive the combination
as thiazides appear in milk.
Action:
Acts relatively selectively at
beta2-adrenergic receptors to
cause bronchodilation and
vasodilation; at higher doses,
beta2 selectivity is lost, and the
drug acts at beta2 receptors to
cause typical sympathomimetic
Contraindications: Contraindicated
with hypersensitivity to albuterol;
tachyarrhythmias, tachycardia
caused by digitalis intoxication;
general anesthesia with halogenated
hydrocarbons or cyclopropane
(these sensitize the myocardium to
catecholamines); unstable
Side Effects Nursing Responsibilities
CNS: headache, dizziness,lethargy,
paresthesias
Determine history of hypersensitivity
reactions to cephalosporins, penicillins,
and history of allergies, particularly to
drugs, before therapy is initiated.
GI: nausea,vomiting,
diarrhea,anorexia, abdominal pain,
flatulence,
Inspect IV injection site frequently for
signs of phlebitis.
GU: nephrotoxicity Report onset of loose stools or diarrhea.
Although pseudomembranous colitis
rarely occurs, this potentially life-
threatening complication should be ruled
out as the cause of diarrhea during and
after antibiotic therapy.
Hematologic: bone marrow
depression
Side Effects Nursing Responsibilities
Check temperatureof patient before
giving the medication. Give the
medication for temperature >37.5 C
Monitor for S&S of: hepatotoxicity, even
with moderate doses, especially in
individuals with poor nutrition.
Ensure patient is not taking other
medications (e.g., cold preparations)
containing acetaminophen without
medical advice; overdosing and chronic
use can cause liver damage and other
toxic effects.
Do not use for fever persisting longer
than 3 d, fever over 39.5 C (103 F), or
recurrent fever.
Side Effects Nursing Responsibilities
Side effects are rare with
paracetamol when it is taken at the
recommended doses. Skin rashes,
blood disorders and acute
inflammation of the pancreas have
occasionally occurred in people
taking the drug on a regular basis
for a long time. One advantage of
paracetamol over aspirin and
NSAIDs is that it doesn't irritate the
stomach or causing it to bleed,
potential Side effects of aspirin and
NSAIDs.
Hypersensitivity: ranging from
rash to fever to anaphylaxis, serum
sickness reaction
Monitor I&O rates and pattern: Especially
important in severely ill patients receiving
high doses. Report any significant
changes.
Observe patients receiving parenteral
drug carefully; closely monitor BP and
vital signs. Sudden death from cardiac
arrest has been reported.
Monitor BP during periods of diuresis and
through period of dosage adjustment.
Observe patient closely during period of
brisk diuresis. Sudden alteration in fluid
and electrolyte balance may precipitate
significant adverse reactions. Report
symptoms to physician.
Lab tests: Obtain frequent blood count,
serum and urine electrolytes, CO2, BUN,
blood sugar, and uric acid values during
first few months of therapy and
periodically thereafter.
Monitor for S&S of hypokalemia.
Monitor I&O ratio and pattern. Report
decrease or unusual increase in output.
Excessive diuresis can result in
dehydration and hypovolemia, circulatory
collapse, and hypotension. Weigh patient
daily under standard conditions.
Side Effects Nursing Responsibilities
Monitor therapeutic effectiveness which
is indicated by significant subjective
improvement in pulmonary function
within 6090 min after drug
administration.
Monitor for: S&S of fine tremor in
fingers, which may interfere with
precision handwork; CNS stimulation
(hyperactivity, excitement, nervousness,
insomnia), tachycardia, GI symptoms.
Report promptly to physician.
Body as a Whole: Hypersensitivity
reaction. CNS: Tremor, anxiety,
nervousness, restlessness,
convulsions, weakness, headache,
hallucinations. CV: Palpitation,
hypertension, hypotension,
bradycardia, reflex tachycardia.
Special Senses: Blurred vision,
dilated pupils. GI: Nausea,
vomiting. Other: Muscle cramps,
hoarseness.
CV: Postural hypotension, dizziness
with excessive diuresis, acute
hypotensive episodes, circulatory
collapse. Metabolic: Hypovolemia,
dehydration, hyponatremia
hypokalemia, hypochloremia
metabolic alkalosis,
hypomagnesemia, hypocalcemia
(tetany), hyperglycemia, glycosuria,
elevated BUN, hyperuricemia. GI:
Nausea, vomiting, oral and gastric
burning, anorexia, diarrhea,
constipation, abdominal cramping,
acute pancreatitis, jaundice.
Urogenital: Allergic interstitial
nephritis, irreversible renal failure,
urinary frequency. Hematologic:
Anemia, leukopenia,
thrombocytopenic purpura; aplastic
anemia, agranulocytosis (rare).
Special Senses: Tinnitus, vertigo,
feeling of fullness in ears, hearing
loss (rarely permanent), blurred
vision. Skin: Pruritus, urticaria,
exfoliative dermatitis, purpura,
photosensitivity, porphyria cutanea
tarde, necrotizing angiitis
(vasculitis). Body as a Whole:
Increased perspiration; paresthesias;
activation of SLE, muscle spasms,
weakness; thrombophlebitis, pain at
IM injection site.
Lab tests: Periodic ABGs, pulmonary
functions, and pulse oximetry.
Side Effects Nursing Responsibilities
Instruct patient to take medication with
meals or milk and avoid excessive
ingestion of food high in potassium or use
of salt substitutes
Diuretic effect may be delayed 2-3 days
and maximum hypertensive may be
delayed 2-3weeks; monitor I and O ratios
and daily weight, BP, serum electrolytes
(K, Na) and renal function
Body as a Whole: Hypersensitivity
reaction. CNS: Tremor, anxiety,
nervousness, restlessness,
convulsions, weakness, headache,
hallucinations. CV: Palpitation,
hypertension, hypotension,
bradycardia, reflex tachycardia.
Special Senses: Blurred vision,
dilated pupils. GI: Nausea,
vomiting. Other: Muscle cramps,
hoarseness.
Gynecomastia, GI symptoms,
lethargy, headache and
thrombocytopenia, leukopenia,
agranulocytosis, cutaneous
eruptions, pruritus, mental
confusion, paresthesia, acute
pancreatitis, jaundice, orthostatic
hypertension, muscle spasm,
weakness, fever, ataxia
Anda mungkin juga menyukai
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Invoice Being Charged Sued If or Violation Has This in Wrongful - RightfulDokumen67 halamanInvoice Being Charged Sued If or Violation Has This in Wrongful - RightfulSteven SchoferBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Open Banking StandardDokumen148 halamanThe Open Banking StandardOpen Data Institute95% (21)
- Aci 306.1Dokumen5 halamanAci 306.1safak kahramanBelum ada peringkat
- Pathophysiology of Congestive Heart FailureDokumen2 halamanPathophysiology of Congestive Heart FailureAnonymous XvwKtnSrMR100% (10)
- Developmental Screening Using The: Philippine Early Childhood Development ChecklistDokumen30 halamanDevelopmental Screening Using The: Philippine Early Childhood Development ChecklistGene BonBonBelum ada peringkat
- Manila Doctors HospitalDokumen7 halamanManila Doctors HospitalMerlyn Rivera PelecinBelum ada peringkat
- Manila Doctors HospitalDokumen7 halamanManila Doctors HospitalMerlyn Rivera PelecinBelum ada peringkat
- Manila Doctors HospitalDokumen7 halamanManila Doctors HospitalMerlyn Rivera PelecinBelum ada peringkat
- CHF Discharge InstructionsDokumen2 halamanCHF Discharge InstructionsMerlyn Rivera PelecinBelum ada peringkat
- Process Safety Management System-PaperDokumen11 halamanProcess Safety Management System-PaperV. Balasubramaniam100% (2)
- Sample Action Research in MathDokumen12 halamanSample Action Research in MathKresta BenignoBelum ada peringkat
- 6 Diabetes Nursing Care PlansDokumen14 halaman6 Diabetes Nursing Care PlansMerlyn Rivera PelecinBelum ada peringkat
- 6 Diabetes Nursing Care PlansDokumen14 halaman6 Diabetes Nursing Care PlansMerlyn Rivera PelecinBelum ada peringkat
- Catch Up Friday 011153Dokumen3 halamanCatch Up Friday 011153Vanessa Pond100% (6)
- Drug Study Paracetamol, Ibuprofen, Cotrimoxazole, AllopurinolDokumen6 halamanDrug Study Paracetamol, Ibuprofen, Cotrimoxazole, Allopurinolpaupaulala89% (9)
- Drug Study Paracetamol, Ibuprofen, Cotrimoxazole, AllopurinolDokumen6 halamanDrug Study Paracetamol, Ibuprofen, Cotrimoxazole, Allopurinolpaupaulala89% (9)
- BC PNP Skills Immigration and Express Entry BC Program Guide PDFDokumen79 halamanBC PNP Skills Immigration and Express Entry BC Program Guide PDFMerlyn Rivera PelecinBelum ada peringkat
- BC PNP Skills Immigration and Express Entry BC Program Guide PDFDokumen79 halamanBC PNP Skills Immigration and Express Entry BC Program Guide PDFMerlyn Rivera PelecinBelum ada peringkat
- EDITED Letter For Direct Solicitations For SchoolsDokumen1 halamanEDITED Letter For Direct Solicitations For SchoolsMerlyn Rivera PelecinBelum ada peringkat
- ReferencesDokumen1 halamanReferencesMerlyn Rivera PelecinBelum ada peringkat
- NTP MoP2004Dokumen131 halamanNTP MoP2004meldestacamentojrBelum ada peringkat
- Case StudyDokumen33 halamanCase StudySarah GatuzBelum ada peringkat
- No RelieSDokumen2 halamanNo RelieSMerlyn Rivera PelecinBelum ada peringkat
- Guidelines For The Narrative Report Revised Ed.Dokumen3 halamanGuidelines For The Narrative Report Revised Ed.Merlyn Rivera PelecinBelum ada peringkat
- 2019-Kubelka-Munk Double Constant Theory of Digital Rotor Spun Color Blended YarnDokumen6 halaman2019-Kubelka-Munk Double Constant Theory of Digital Rotor Spun Color Blended YarnyuBelum ada peringkat
- FS 3 Technology in The Learning EnvironmentDokumen24 halamanFS 3 Technology in The Learning EnvironmentJayson Gelera CabrigasBelum ada peringkat
- [Advances in Neurosurgery 2] O. Stochdorph (Auth.), W. Klug, M. Brock, M. Klinger, O. Spoerri (Eds.) - Meningiomas Diagnostic and Therapeutic Problems Multiple Sclerosis Misdiagnosis Forensic Problems in NeurosurgDokumen461 halaman[Advances in Neurosurgery 2] O. Stochdorph (Auth.), W. Klug, M. Brock, M. Klinger, O. Spoerri (Eds.) - Meningiomas Diagnostic and Therapeutic Problems Multiple Sclerosis Misdiagnosis Forensic Problems in Neurosurgbayu_gendeng666Belum ada peringkat
- Salary Survey (Hong Kong) - 2022Dokumen7 halamanSalary Survey (Hong Kong) - 2022Nathan SmithBelum ada peringkat
- Operation ManualDokumen83 halamanOperation ManualAn Son100% (1)
- Advanced Features and Troubleshooting ManualDokumen138 halamanAdvanced Features and Troubleshooting ManualHugo Manuel Sánchez MartínezBelum ada peringkat
- XETEC 4g300 / 4g600Dokumen6 halamanXETEC 4g300 / 4g600Harun ARIKBelum ada peringkat
- BonBonB What Map ReviewsDokumen396 halamanBonBonB What Map Reviewstoyi kamiBelum ada peringkat
- Corporate Governance Committees in India: Key Reports and RecommendationsDokumen39 halamanCorporate Governance Committees in India: Key Reports and Recommendationskush mandaliaBelum ada peringkat
- Civil Engineering Softwares and Their ImplementationsDokumen13 halamanCivil Engineering Softwares and Their ImplementationsADITYABelum ada peringkat
- The dangers of electrostatic phenomenaDokumen14 halamanThe dangers of electrostatic phenomenaYaminBelum ada peringkat
- Al-Qawlul Mufeed: Backbiting and Its Impact On SocietyDokumen2 halamanAl-Qawlul Mufeed: Backbiting and Its Impact On SocietyMountainofknowledgeBelum ada peringkat
- General and Local AnesthesiaDokumen1 halamanGeneral and Local Anesthesiaahmedhelper300Belum ada peringkat
- BTechSyllabus EC PDFDokumen140 halamanBTechSyllabus EC PDFHHBelum ada peringkat
- Assessment of Blast Furnace Behaviour Through Softening-Melting TestDokumen10 halamanAssessment of Blast Furnace Behaviour Through Softening-Melting TestvidhyasagarBelum ada peringkat
- RPT Mathematics Year 5Dokumen24 halamanRPT Mathematics Year 5Anonymous wirViz1tyoBelum ada peringkat
- Stanford MSE FlowchartDokumen1 halamanStanford MSE FlowchartJoseyBelum ada peringkat
- Unit 1 Lesson 2 PDFDokumen20 halamanUnit 1 Lesson 2 PDFKristyll ArguellesBelum ada peringkat
- Guidelines For Submitting An Article To Gesta: General InformationDokumen1 halamanGuidelines For Submitting An Article To Gesta: General InformationneddyteddyBelum ada peringkat
- EngM6 TB WebDokumen161 halamanEngM6 TB WebNong BillBelum ada peringkat
- Quantum Dot PDFDokumen22 halamanQuantum Dot PDFALI ASHRAFBelum ada peringkat
- 2021062476 (1)Dokumen8 halaman2021062476 (1)Naidu SairajBelum ada peringkat
- 1 HeterogenitasDokumen46 halaman1 HeterogenitasRani JuliariniBelum ada peringkat





























































![[Advances in Neurosurgery 2] O. Stochdorph (Auth.), W. Klug, M. Brock, M. Klinger, O. Spoerri (Eds.) - Meningiomas Diagnostic and Therapeutic Problems Multiple Sclerosis Misdiagnosis Forensic Problems in Neurosurg](https://imgv2-1-f.scribdassets.com/img/document/375359245/149x198/fae4c10859/1522685798?v=1)



















