Abdominal Pregnancy
Diunggah oleh
Robertus HajaiHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Abdominal Pregnancy
Diunggah oleh
Robertus HajaiHak Cipta:
Format Tersedia
Full-term extrauterine abdominal pregnancy: a case report
Amal A Dahab1, Rahma Aburass1, Wasima Shawkat2, Reem Babgi1, Ola Essa1 andRazaz H Mujallid3
*
*Corresponding author: Razaz H Mujallid rmujallid@gmail.com
Author Affiliations
1
Department of Obstetrics and Gynecology, Maternity and Children Hospital, Jeddah, Saudi Arabia
2
Department of Surgery, Maternity and Children Hospital, Jeddah, Saudi Arabia
3
Department of Anesthesia, Maternity and Children Hospital, Jeddah, Saudi Arabia
For all author emails, please log on.
Journal of Medical Case Reports 2011, 5:531 doi:10.1186/1752-1947-5-531
The electronic version of this article is the complete one and can be found online at:http://www.jmedicalcasereports.com/content/5/1/531
Received: 4 April 2011
Accepted: 31 October 2011
Published: 31 October 2011
2011 Dahab et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License
(http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the
original work is properly cited.
Abstract
Introduction
Extrauterine abdominal pregnancy is extremely rare and is frequently missed during antenatal care. This is a report of a full-term
extrauterine abdominal pregnancy in a primigravida who likely had a ruptured ectopic pregnancy with secondary implantation and
subsequently delivered a healthy baby.
Case presentation
A 23-year-old, Middle Eastern, primigravida presented at 14 weeks gestation with intermittent suprapubic pain and dysuria. An
abdominal ultrasound examination showed a single viable fetus with free fluid in her abdomen. A follow-up examination at term showed
a breech presentation and the possibility of a bicornute uterus with the fetus present in the left horn of her uterus. Our patient underwent
Cesarean delivery under general anesthesia and was found to have a small intact uterus with the fetus lying in her abdomen and
surrounded by an amniotic fluid-filled sac. The baby was extracted uneventfully, but the placenta was implanted in the left broad
ligament and its removal resulted in massive intraoperative bleeding that necessitated blood and blood products transfusion and the
administration of Factor VII to control the bleeding. Both the mother and newborn were discharged home in good condition.
Conclusions
An extrauterine abdominal pregnancy secondary to a ruptured ectopic pregnancy with secondary implantation could be missed during
antenatal care and continue to term with good maternal and fetal outcome. An advanced extrauterine pregnancy should not result in the
automatic termination of the pregnancy.
Introduction
An extrauterine abdominal pregnancy is a very rare form of ectopic pregnancy where implantation occurs within the peritoneal cavity,
outside the Fallopian tube and ovary. It is estimated to occur in 10 out of 100,000 pregnancies in the United States [1]. The diagnosis of
such a condition is frequently missed during antenatal care, despite the routine use of abdominal ultrasonography. However, it is
extremely important to detect an extrauterine abdominal pregnancy because the associated maternal mortality rate is estimated at about
five per 1000 cases, which is approximately seven times higher than the estimated rate for ectopic pregnancy in general, and about 90
times the maternal mortality rate associated with normal delivery in the United States[1]. Survival of the newborn is also affected with a
perinatal mortality rate of 40% to 95% [2]. We report on a successful operative delivery of a healthy baby following a full-term
extrauterine abdominal pregnancy in a primigravida in whom the diagnosis was missed despite repeated ultrasonography during the
antenatal period.
Case presentation
A 23-year-old, Middle Eastern primigravida presented to our Emergency Department at 14 weeks gestation with a two-week history of
intermittent suprapubic pain associated with dysuria. On examination, she had a heart rate of 102 beats/min, her blood pressure was
109/71 mmHg, a respiratory rate of 15 breaths/min and temperature of 37.4C. Examination of her cardiac and respiratory systems was
unremarkable. Her abdomen was soft, but with mild suprapubic tenderness. Her laboratory results showed a hemoglobin level of 7.9
g/dL, hematocrit 25.7%, white blood cells 9700 cells/mm
3
, platelets 367 cells/mm
3
, serum urea 14.8 mmol/L and serum creatinine 47
mol/L. Her serum electrolytes, coagulation profile and liver function tests were all within normal limits. Her serum -human chorionic
gonadotropin level was 75,542 IU. A bedside urine analysis showed pus cells and a urine culture subsequently grew Streptococcus
agalactiae, which was sensitive to penicillin and amoxicillin. An ultrasound examination in our Emergency Room showed a single
viable fetus with a crown-rump length corresponding to 13 weeks and five days gestation, the anterior placenta and a normal amount of
liquor. A significant amount of localized fluid in the left side of her abdomen was also noted and was thought to be either ascites or
blood. Our patient received intravenous amoxicillin/clavulanic acid (1 g) and 500 mL of normal saline; her pain subsided, and she was
admitted to the ward for follow-up and further investigation. Iron deficiency anemia was diagnosed based on a negative sickle cell test,
normal hemoglobin electrophoresis, a serum iron level of 32 g/dL, serum ferritin of 89.7 g/dL and a total iron binding capacity of 117
g/dL. Our patient was placed on iron supplements. Four days later, repeat abdominal ultrasound examination suggested the presence of
a bicornute uterus with the fetus in the left horn, and free fluid was noted in her pelvis (Figure 1). Her liver, spleen, kidneys and urinary
bladder appeared normal. A speculum examination indicated the presence of a single cervix. An abdominal fluid tap was offered to our
patient but she declined and she was discharged home on iron supplements and requested to attend outpatient follow-up. At 20 weeks
gestation, our patient's hemoglobin was 9.5 g/dL and a follow-up abdominal ultrasound examination performed by a more experienced
radiologist showed similar findings to the previous examination with a vertical pocket of amniotic fluid that measured 4.2 cm
(Figures 2 and 3). At 40 weeks gestation, a follow-up ultrasound examination showed breech presentation with a highly vascular
placenta. An external cephalic version was offered to our patient but she declined. She was admitted to the hospital for an elective
Cesarean delivery. She opted for general anesthesia which was induced with propofol and suxamethonium chloride, and was maintained
with sevoflurane and an oxygen/air mixture. A Pfannenstiel incision was made and her uterus was found to be intact and small on
entering her abdomen. The fetus was found in her abdomen surrounded by an amniotic membrane filled with liquor. The amniotic
membrane was dissected and incised and the fetus was extracted (see Additional file 1: Movie 1 showing delivery of the baby). The fetal
Apgar scores were 6 and 10 at one and five minutes, respectively. The placenta was attached to the posterior aspect of the left broad
ligament. During its removal, massive bleeding from the placental bed occurred and our patient became hypotensive. She was
aggressively resuscitated with a total of 4000 mL of Ringer's lactate, 7 units of packed red blood cells, 4 units of fresh frozen plasma, 10
units of cryoprecipitate and 2 units of platelets. She continued to bleed and was administered 90 units/kg of intravenous Factor VII,
which controlled her bleeding. Her left ovary and tube were found to be distorted while the right ones were normal. A hemostatic suture
was applied on the distorted tube which was left, together with the ovary, in situ. An abdominal drain was inserted and our patient was
extubated on the table and transferred to our Intensive Care Unit for monitoring. She was discharged to the ward on the following day
and went home with her newborn 10 days after surgery.
Figure 1. Ultrasonography picture at 14 weeks gestation showing a single fetus, corresponding to date in
size, and the possibility of a bicornute uterus.
Figure 2. Ultrasonography picture at 19 weeks showing fetus, amniotic fluid and the possibility of a
bicornute uterus.
Figure 3. Ultrasonography picture at 23 weeks showing fetus, amniotic fluid and normal fetal morphology.
Additional file 1. Cesarean delivery. Movie file showing Cesarean delivery of the baby.
Format: MOV Size: 4MB Download file
Discussion
Extrauterine abdominal pregnancy beyond 20 weeks gestation and with a viable fetus is a rare condition, with an estimated prevalence of
one out of 8099 hospital deliveries [3], and is classified into two types. Primary abdominal pregnancy refers to pregnancy where
implantation of the fertilized ovum occurs directly in the abdominal cavity. In such cases, the Fallopian tubes and ovaries are intact.
There were only 24 cases of primary abdominal pregnancy reported up to 2007[4]. In contrast, secondary abdominal pregnancy accounts
for most cases of advanced extrauterine pregnancy. It occurs following an extrauterine tubal pregnancy that ruptures and gets re-
implanted within the abdomen [5]. Under these circumstances, there is evidence of tubal or ovarian damage.
In this report, the intermittent suprapubic pain that our patient experienced early in her pregnancy, the free fluid seen on ultrasound
examination, and the intraoperative findings of a severely distorted left Fallopian tube and ovary are highly suggestive of a tubal
pregnancy that ruptured and resulted in secondary implantation in the broad ligament. Accordingly, this was most likely a case of
secondary abdominal pregnancy. The diagnosis was unfortunately missed during antenatal care, and the ultrasound examination findings
were repeatedly misinterpreted as an intrauterine pregnancy in a bicornute uterus. A recent report of 163 cases of extrauterine abdominal
pregnancy demonstrated that the diagnosis of this condition is frequently missed, with only about 45% of cases diagnosed during the
antenatal period [3]. The fact that our patient's low hemoglobin was explained by the presence of iron deficiency, her suprapubic pain
was attributed to a urinary tract infection and that the free fluid in her abdomen was thought to be ascites collectively contributed to the
failure to consider the possibility of an extrauterine pregnancy. Had this been discovered at an earlier stage, our patient could have been
admitted to hospital for closer monitoring and her operative delivery would have been performed at an earlier gestational age.
It is interesting to note that patients with an extrauterine abdominal pregnancy typically have persistent abdominal and/or gastrointestinal
symptoms during their pregnancy [5]. Our patient, however, did not have any symptoms during her pregnancy other than the intermittent
suprapubic pain that she experienced at the end of her first trimester.
Extrauterine abdominal pregnancy is typically suspected when the baby's parts are easily felt on clinical examination or when the baby's
lie is abnormal [6]. In our current patient, the baby was always in the breech position and the abdominal examination was always
reported as being unremarkable. This could be attributed, at least in part, to the fact that our patient was examined by different physicians
during her antenatal visits and the attending physician only reviewed her records. The amniotic fluid around the baby could have also
contributed to the difficulty in feeling the baby's parts on abdominal examination. Ultrasonography, however, remains the main method
for the diagnosis of extrauterine pregnancy. It usually shows no uterine wall surrounding the fetus, fetal parts that are very close to the
abdominal wall, abnormal lie and/or no amniotic fluid between the placenta and the fetus [6]. Interestingly, amniotic fluid was detected
in all ultrasound examinations in this patient but it was technically difficult to estimate its amount. The impression that the patient had a
bicornute uterus was likely due to the fact that the fetus was lying behind the uterus and the empty uterine cavity was mistaken for the
empty horn. Magnetic resonance imaging and serum -fetoprotein have been used to diagnose abdominal pregnancy [4,7], however,
there was no justification to perform these tests in this patient as the diagnosis was not suspected.
About 21% of babies born after an extrauterine abdominal pregnancy have birth defects, presumably due to compression of the fetus in
the absence of the amniotic fluid buffer. Typical deformities include limb defects, facial and cranial asymmetry, joint abnormalities and
central nervous malformation [8]. In this case, the baby was protected by the surrounding amniotic fluid and sac which could explain the
absence of deformities in the baby.
The massive bleeding that occurred when the placenta was removed was due to the adherence of the placenta to the broad ligament
which, unlike the uterus, does not contract. It has been reported that, unless the placenta can be easily tied off or removed, it may be
preferable to leave it in place and allow for its natural regression [5,6]. However, leaving the placenta in situ has been associated with
increased postoperative morbidity and mortality [9] and is thus not advisable. There have been many reports of advanced extrauterine
pregnancy that ended with a viable fetus and a healthy mother [3]. Since the diagnosis is frequently missed preoperatively [3] and
adverse fetal and maternal outcome does not necessarily occur in association with the continuation of pregnancy, one could argue that
the termination of an advanced extrauterine pregnancy upon antenatal diagnosis might not be warranted. However, these cases should be
followed-up closely when the diagnosis is made to prevent adverse outcomes.
Conclusion
This is a report of an extrauterine abdominal pregnancy that had likely originated in the left Fallopian tube which ruptured and resulted in
secondary implantation in the broad ligament. The pregnancy continued uneventfully to full term and ended successfully with operative
delivery of a healthy baby. The importance of this case report is the fact that an extrauterine abdominal pregnancy could be missed
during antenatal care despite repeated ultrasound examinations. Furthermore, the antenatal diagnosis of advanced extrauterine pregnancy
does not necessarily justify the termination of the pregnancy since good maternal and fetal outcome is not uncommon.
Consent
Written informed consent was obtained from the patient for publication of this case report and the accompanying images and video. A
copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AAD, RB and OE performed the Cesarean delivery and followed up the patient and baby postoperatively until discharge from the
hospital. WS helped during the surgery from a general surgical stand point. RA was the consultant who followed up the patient during
antenatal care and performed the ultrasound examinations. RHM provided the perioperative anesthetic care for the patient and was a
major contributor in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge the help of the operating room and intensive care personnel who assisted in the care of this patient. The authors
also acknowledge the help of Prof. Jamal Alhashemi, King Abdulaziz University, Jeddah, Saudi Arabia for his critical review of the
manuscript.
References
1. Atrash HK, Friede A, Hgue CJR: Abdominal pregnancy in the United States: frequency and mortality.
Obstet Gynecol 1987, 69:333-337. PubMed Abstract
2. Martin JN Jr, Sessums JK, Martin RW, Pryor JA, Morrison JC: Abdominal pregnancy: current concepts of management.
Obstet Gynecol 1988, 71:549-557. PubMed Abstract
3. Nkusu Nunyalulendho D, Einterz EM: Advanced abdominal pregnancy: case report and review of 163 cases reported
since 1946.
Rural Remote Health 2008, 8:1087. PubMed Abstract | Publisher Full Text
4. Krishna D, Damyanti S: Advanced abdominal pregnancy: a diagnostic and management dilemma.
J Gynecol Surg 2007, 23:69-72. Publisher Full Text
5. King M, Bewes PC, Cairns J, Thornton J (Eds): Chapter 8. Abdominal pregnancy
In Primary Surgery. Volume 1: non-trauma
On-line edition available at http://www.meb.uni-bonn.de/dtc/primsurg/docbook/html/x5173.html webcite
6. Kun KY, Wong PY, Ho MW, Tai CM, Ng TK: Abdominal pregnancy presenting as a missed abortion at 16 weeks'
gestation.
Hong Kong Med J 2000, 6:425-427. PubMed Abstract | Publisher Full Text
7. Tromans PM, Coulson R, Lobb MO, Abdulla U: Abdominal pregnancy associated with extremely elevated serum alph-
fetoprotein: case report.
Br J Obstet Gynaecol 1984, 91:296-298. PubMed Abstract | Publisher Full Text
8. Stevens CA: Malformations and deformations in abdominal pregnancy.
Am J Med Genet 1993, 47:1189-1195. PubMed Abstract | Publisher Full Text
9. Rahman MS, Al-Suleiman SA, Rahman J, Al-Sibai MH: Advanced abdominal pregnancy-observation in 10 cases.
Obstet Gynecol 1982, 59:366-372. PubMed Abstract
P Baffoe, C Fofie, and B N Gandau
Author information Copyright and License information
Summary
Go to:
Introduction
Ectopic pregnancy represents about 12% of all pregnancies with 95% occurring in the
fallopian tube. Abdominal pregnancies represent just about 1% of ectopic pregnancies.
1
The
incidence of abdominal pregnancy differs in various publications and ranges between 1:
10000 pregnancies and 1:30,000 pregnancies.
1,2
It was reported for the first time in 1708 as
an autopsy finding and numerous cases have been reported worldwide ever since. In most of
these cases, the diagnosis is made on the basis of the ensuing complications such as
hemorrhage and abdominal pain. Maternal mortality and morbidity are also very high
especially if the condition is not diagnosed and managed appropriately. These pregnancies
generally do not get to 37 weeks (term gestation) and usually the end result is the extraction
of a dead fetus. Another challenge for babies from abdominal pregnancy is the very high
incidence of congenital malformations.
Abdominal pregnancy at term with a healthy viable fetus is therefore an extremely rare
condition and very few of such cases have been published during the last ten years. We
present a case of abdominal pregnancy that resulted in a term live baby without
malformations.
Case Report
A 31- year- old woman, Gravida 3 Para 1, was referred from a District Hospital on 17th June
2008 at 8:00am. Her principal complaint on arrival was severe abdominal pain. She had
irregular menstrual cycles prior to her pregnancy and was not sure of her last date of
menstruation. The patient suffered from severe abdominal pain and vaginal bleeding which
kept her out of work during the first trimester but the second trimester was incident free.
She was, however, again kept out of work during the third trimester with abdominal pain.
Her antenatal card indicated nine visits and a gestational age of 38 weeks at the time of
referral.
On examination, she looked generally stable. She was not pale; vital signs were within
normal parameters. Cardiovascular and respiratory systems did not reveal any
abnormalities. The abdominal examination revealed symphysio-fundal height of 33cm,
transverse lie, foetal heart rate of 136 beats per minute and no uterine contractions.
Vaginal examination revealed posterior located cervix measuring 2cm long without
dilatation. There was no vaginal bleeding. She had five ultrasound scan examination with
the last two within seven days of presentation indicating intrauterine gestation with
transverse lie. The rest of her investigations were normal. The haemoglobin level was
10.9g/dl and blood group was O Rhesus positive. She was booked for emergency caesarean
section on account of transverse lie at term.
At laparotomy the following findings were made: Abdominal pregnancy with a live female
baby weighing 2.3 kilograms and meconium stained liquor. The placenta was extensively
adherent to segments of large bowel, omentum and left cornual region of the uterus
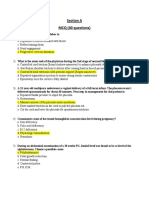
(Figure1).
Figure1
Normal sized uterus and placenta implanted on segment of bowel
The uterus, right tube and both ovaries were normal but the left tube was not identified.
Other abdominal organs were normal.
There was significant bleeding from some detached portions of the placenta, which
prompted removal of the detached placenta tissue to facilitate haemostasis. The rest of the
placenta was left in situ. Haemostasis was secured. Total estimated trans-operative bleeding
was one litre.
A unit of compatible blood was transfused intraoperatively. The patient progressed well and
was discharged on the fifth postoperative day. She was followed up weekly for four weeks.
Abdominal ultrasound after six weeks showed normal size uterus and ovaries and the
portion of placenta that was left in situ was not identified. Beta human chorionic
gonadotropin (BhCG) was negative at the same period. All investigations by the
neonatologist and the general paediatrician did not show any abnormality on the baby. The
patient was finally discharged home.
Go to:
Discussions
Advanced abdominal pregnancy is extremely rare. In a review at the Komfo Anokye
Teaching Hospital, Opare-Addo et al reported an incidence of 1:1320 deliveries
3
whilst
Amirtha et al cited 1:25000 deliveries.
4
Most of the cases of abdominal pregnancies are
secondary from aborted or ruptured tubal pregnancy.
4
In this case it was obvious that the
abdominal implantation was secondary to undiagnosed ruptured left tubal ectopic
pregnancy. Clinical diagnosis can be very difficult and ultrasound is very helpful during the
early stages of gestation but can also be disappointing in the later stages.
Other radiological studies such as MRI and CT scan are helpful in the later stages.
5
Teng et
al reported an interesting case in which MRI played a decisive role in the diagnosis
6
,
unfortunately these advanced imaging technologies are not available in most parts of the
third world. Our patient had five ultrasound scan examinations and none of these suggested
the possibility of abdominal pregnancy. In poorly resourced centres, high index of suspicion
is key for prompt diagnosis and timely intervention to prevent life-threatening
complications.
In our opinion, bleeding from placental implantation site is the most life-threatening
complication during laparotomy. The decision to remove the placenta or not can be a
determining factor for the survival or otherwise of the woman and this decision is subject to
the surgeon's expertise and the particular case in question. It is generally recommended to
leave the placenta in situ and make a follow up with human chorionic gonadotropin
levels.
7
In this case there was significant bleeding from some detached portions of the
placenta that prompted removal of these portions to secure haemostasis. The patient was
transfused with one unit of blood during the operation and that was enough. For the
newborn, it is very important to rule out congenital malformations. There are reports of
foetal malformations as high as 40% associated with abdominal pregnancies and only 50%
of these babies survive up to one week post delivery.
8,9
In his extensive review, Stevens found some varying degrees of deformations and
malformations in 21.4% of these infants. In this case that has been presented; no
malformation has been found on the child after ten months.
Go to:
Conclusions
Abdominal pregnancy with resultant healthy newborn is very rare. Diagnosis of the
condition can be difficult especially if the pregnancy is advanced. High level of suspicion,
careful clinical and ultrasound examinations are the routine means of diagnosis though C T
scan and MRI can be useful. Bleeding is the single most important life-threatening
complication for the mother whilst fetal malformation is one of the numerous challenges
that can confront the newborn.
Go to:
Acknowledgement
We wish to acknowledge the kind comments and guidance of Dr R.M.K Adanu on this case
report.
Go to:
References
1. Nwobodo EI. Abdominal pregnancy. A case report. Ann Afr Med. 2004;3(4):195196.
2. Badria L, Amarin Z, Jaradat A, Zahawi H, Gharaibeh A. Full-term viable abdominal
pregnancy. A case report and review. Arch Gynaecol Obstet. 2003;268(4):340
342. [PubMed]
3. Opare-Addo HS, Daganus S. Advanced abdominal pregnancy: a study of 13 consecutive
cases seen in 1993 and 1994 at Komfo Anokye Teaching Hospital, Kumasi, Ghana. Afr J
Reproductive Health.2000;4(1):2839. [PubMed]
4. Amritha B, Sumangali T, Priya B, Deepak S, Rai S. A rare case of term viable secondary
abdominal pregnancy following rupture of a rudimentary horn. A case report. J Med case
reports. 2009;3:38.[PMC free article] [PubMed]
5. Karat LS. Viable Abdominal Pregnancy. J Obstet Gynecol India. 2007;57(2):169170.
6. Cunningham F, Gant N, Leveno K, et al. Williams Obstetrics. 21. Mcgraw-Hill; 2001.
Ectopic Pregnancy; pp. 899902.
7. Jianping Z, Fen L, Qiu S. Full-Term Abdominal Pregnancy. A Case Report and Review of
the Literature. Gynecol Obstet Invest. 2008;65(2):139141. [PubMed]
8. Teng H, Kumar G, Ramli N. A viable secondary intra-abdominal pregnancy resulting
from rupture of uterine scar: role of MRI. Br J Radiol. 2007;80:134136. [PubMed]
9. Kun K, Wong P, Ho M, Tai C. Abdominal pregnancy presenting as a missed abortion at 16
weeks gestation. Hong Kong Med J. 2000;6(4):425427. [PubMed]
10. Stevens CA. Malformations and deformations in abdominal pregnancy. Am J Med
Genet.1993;47(8):11891195. [PubMed]
Abdominal Ectopic Pregnancy
Abdominal pregnancy may account for up to 1.4% of ectopic pregnancies.
[54-
56]
Abdominal pregnancies refer to those with extrauterine implantations in
omentum, vital organs, or large vessels. These pregnancies can go undetected
until an advanced gestational age and often result in severe
hemorrhage.
[56]
Rates of maternal mortality have been reported as high as
20%.
[57,58]
Advanced abdominal pregnancy carries a risk of hemorrhage,
disseminated intravascular coagulation, bowel obstruction, and
fistulae.
[59]
Frequently, these pregnancies are encountered with a viable fetus,
which complicates their management.
Implantations have been reported in the pelvic cul-de-sac, broad ligament,
bowel, and pelvic sidewall.
[55,57,60]
The site of implantation and availability of
vascular supply are believed to be factors that may influence the possibility of
fetal survival.
[57]
Risk factors for abdominal pregnancy include tubal damage,
pelvic inflammatory disease, endometriosis, assisted reproductive techniques,
and multiparity.
[60,61]
Abdominal pregnancies are believed to be a result of
secondary implantation from an aborted tubal pregnancy or as a result of intra-
abdominal fertilization of sperm and ovum.
[55,57]
Patients with abdominal pregnancy often present with abdominal pain, nausea,
vomiting, painful fetal movements, and less frequently, vaginal bleeding.
[59]
In
1942, Studdiford outlined his criteria for abdominal pregnancy: (1) normal
bilateral fallopian tubes and ovaries; (2) absence of uteroperitoneal fistula; or
(3) presence of a pregnancy related to the peritoneal surface
exclusively.
[58]
Today, the diagnosis of abdominal pregnancy is often made
using ultrasound and x-ray. The classic ultrasound finding is the absence of
myometrial tissue between the bladder and pregnancy.
[57]
Elevated serum alpha-
fetoprotein has also been associated with abdominal pregnancy.
[62]
Diagnostic
laparoscopy may also be of value when there is a doubt about pregnancy
location.
[63]
In some cases, the diagnosis is not made until
laparotomy.
[58]
Magnetic resonance imaging (MRI) holds promise as a
diagnostic tool.
[64,65]
Our knowledge of abdominal pregnancies comes largely from anecdotal case
reports. Fisch et al
[56]
reported a case of abdominal pregnancy after IVF in a
patient with previous salpingectomy. Omental implantation has been
described.
[57]
Broad ligament pregnancies account for a small number of
abdominal pregnancies.
[66]
Deshpande et al
[67]
reported a broad ligament twin
pregnancy after IVF. The role of possible perforation with an IVF transfer
catheter has been raised. There have also been reports of primary omental
pregnancies.
[58]
Splenic pregnancy has been reported in several cases. Kitade et
al
[68]
reported a first-trimester splenic pregnancy complicated by intra-
abdominal hemorrhage and necessitating splenectomy. Cormio et al
[69]
detailed
a ruptured splenic pregnancy in a patient who presented in hypovolemic shock.
The optimal treatment of abdominal pregnancy is unknown. Abdominal
pregnancies frequently implant in vascular structures such as abdominal organs,
omentum, or pelvic vessels. It has been reported that management of the
placenta correlates well with maternal morbidity. When possible, ligation of
placental blood supply and removal should be attempted to reduce maternal
complications.
[57,59,60]
Alternatively, the umbilical cord may be ligated and
expectant management, arterial embolization, or methotrexate used to facilitate
involution.
[57,64,70]
However, leaving the placenta in situ may lead to further
complications such as infection, secondary hemorrhage, or intestinal
obstruction.
[59,65]
Laparoscopy has been used in the treatment of some early
abdominal pregnancies.
[55,63]
This conservative management should only be
undertaken when the abdominal pregnancy has implanted on a less vascular
surface. Olsen et al
[71]
reported laparoscopic management of a broad ligament
pregnancy without complication. Primary methotrexate has been attempted for
early gestations with minimal success.
[72]
Hemorrhage is the most frequent problem encountered in treating abdominal
pregnancy. Rahaman et al
[65]
used preoperative selective arterial embolization
to help prevent hemorrhage in an advanced abdominal pregnancy that was
removed laparoscopically. However, due to extensive vascular attachments, the
placenta was left in situ and treated with methotrexate. Cardosi et al
[70]
report a
similar experience with selective arterial embolization used as a means of
reducing intraoperative blood loss during removal of a 33-week abdominal fetal
demise. Ginath et al
[73]
reported a ruptured abdominal pregnancy successfully
managed via laparoscopy, although the pregnancy was only 7 weeks gestation.
Furthermore, there are reports of heterotopic abdominal pregnancies treated
with laparoscopy with preservation of the intrauterine gestation.
[56,74]
Abdominal pregnancy is an extremely rare event that may be difficult to
diagnose. The advanced gestational age at which most abdominal pregnancies
are discovered complicates management further. Because of the propensity for
hemorrhage, removal of abdominal pregnancies requires surgical extraction and
discrimination in deciding if placental removal is prudent. There is little
information known about future fertility after abdominal pregnancy.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Plasenta Previa PDFDokumen5 halamanPlasenta Previa PDFRobertus HajaiBelum ada peringkat
- Oxytocin Exposure During Labor Among Women WithDokumen6 halamanOxytocin Exposure During Labor Among Women WithGladys SusantyBelum ada peringkat
- Ipi 328318 DDokumen5 halamanIpi 328318 DRobertus HajaiBelum ada peringkat
- HP Software Time Size LogDokumen1 halamanHP Software Time Size LogRobertus HajaiBelum ada peringkat
- Metformin PDFDokumen2 halamanMetformin PDFRobertus HajaiBelum ada peringkat
- Toxoplasmosis Testing for Pregnant WomenDokumen1 halamanToxoplasmosis Testing for Pregnant WomenherdikoshalatinBelum ada peringkat
- CampbellDokumen5 halamanCampbellRobertus HajaiBelum ada peringkat
- Induction of Labour - NICEDokumen33 halamanInduction of Labour - NICENaeem Khan100% (1)
- The B-Lynch Surgical Technique PDFDokumen4 halamanThe B-Lynch Surgical Technique PDFRobertus HajaiBelum ada peringkat
- 1477 7827 10 26Dokumen8 halaman1477 7827 10 26Robertus HajaiBelum ada peringkat
- HP Software Time Size LogDokumen1 halamanHP Software Time Size LogRobertus HajaiBelum ada peringkat
- HP Device Setup Time Size LogdDokumen1 halamanHP Device Setup Time Size LogdRobertus HajaiBelum ada peringkat
- Syphilis ReverseDokumen1 halamanSyphilis ReverseRobertus HajaiBelum ada peringkat
- SexualDokumen2 halamanSexualRobertus HajaiBelum ada peringkat
- IFRTool LogDokumen7 halamanIFRTool LogRobertus HajaiBelum ada peringkat
- Preterm LaborDokumen11 halamanPreterm LaborTheofilus ArdyBelum ada peringkat
- 2013, Bishop Score and Transvaginal Ultrasound For Preinduction Cervical Assessment, A Randomized Clinical TrialDokumen5 halaman2013, Bishop Score and Transvaginal Ultrasound For Preinduction Cervical Assessment, A Randomized Clinical TrialRobertus HajaiBelum ada peringkat
- Rubella Disease Investigation GuidelineDokumen20 halamanRubella Disease Investigation GuidelineRobertus HajaiBelum ada peringkat
- 02 Bfe 50 F 0748511 Da 7000000Dokumen8 halaman02 Bfe 50 F 0748511 Da 7000000Robertus HajaiBelum ada peringkat
- BR 1Dokumen5 halamanBR 1Robertus HajaiBelum ada peringkat
- Form Mapping A3 A4 7-12-14Dokumen2 halamanForm Mapping A3 A4 7-12-14Robertus HajaiBelum ada peringkat
- Form Mapping A3 A4 3-12-14Dokumen2 halamanForm Mapping A3 A4 3-12-14Robertus HajaiBelum ada peringkat
- EulaDokumen2 halamanEulaKevin CandraBelum ada peringkat
- Form Mapping A3 A4 5-12-14Dokumen2 halamanForm Mapping A3 A4 5-12-14Robertus HajaiBelum ada peringkat
- Bishop Score and Transvaginal Ultrasound For Preinduction Cervical AssessmentDokumen16 halamanBishop Score and Transvaginal Ultrasound For Preinduction Cervical AssessmentRobertus HajaiBelum ada peringkat
- 2Dokumen4 halaman2Robertus HajaiBelum ada peringkat
- Form Mapping A3 A4 TGL 8-10-14Dokumen2 halamanForm Mapping A3 A4 TGL 8-10-14Robertus HajaiBelum ada peringkat
- Clinical Uses of Misoprostol in Obstetrics and Gynaecology: MedicalDokumen4 halamanClinical Uses of Misoprostol in Obstetrics and Gynaecology: MedicalRobertus HajaiBelum ada peringkat
- Overview of Sexual Dysfunction in Women Treated For CancerDokumen5 halamanOverview of Sexual Dysfunction in Women Treated For CancerRobertus HajaiBelum ada peringkat
- Overview of Sexual Dysfunction in Women Treated For CancerDokumen4 halamanOverview of Sexual Dysfunction in Women Treated For CancerRobertus HajaiBelum ada peringkat
- Ectopic PregnancyDokumen6 halamanEctopic PregnancyMarcus Philip GonzalesBelum ada peringkat
- AIPGMEE 2003 Question Paper With AnswerDokumen59 halamanAIPGMEE 2003 Question Paper With AnswerpavaniBelum ada peringkat
- Leslie V FarlandDokumen10 halamanLeslie V FarlandtiaranindyBelum ada peringkat
- Test IIIDokumen26 halamanTest IIISharat ChandraBelum ada peringkat
- Bleeding PregDokumen261 halamanBleeding PregElsya ParamitasariBelum ada peringkat
- MCN Case Study-2pDokumen76 halamanMCN Case Study-2pAngeline ShackletonBelum ada peringkat
- Assessment of The Childbearing Woman: Nursing Health History FormatDokumen12 halamanAssessment of The Childbearing Woman: Nursing Health History FormatJmy CoronadoBelum ada peringkat
- Ectopic PregnancyDokumen4 halamanEctopic PregnancySyahriana AnaBelum ada peringkat
- Ultrasound in Gynecology N ObstetricDokumen9 halamanUltrasound in Gynecology N ObstetricKarthik RajvBelum ada peringkat
- ANTEPARTUM COMPLICATIONS GUIDEDokumen117 halamanANTEPARTUM COMPLICATIONS GUIDEdarren55Belum ada peringkat
- 匀夀䰀䰀䄀䈀唀匀: 匀夀䰀䰀䄀䈀唀匀 䄀 䰀䤀吀夀 䰀䤀匀匀䔀刀Dokumen35 halaman匀夀䰀䰀䄀䈀唀匀: 匀夀䰀䰀䄀䈀唀匀 䄀 䰀䤀吀夀 䰀䤀匀匀䔀刀Zala pratiksha BhagvatsinhBelum ada peringkat
- Kehamilan Ektopik TergangguDokumen2 halamanKehamilan Ektopik TergangguRSIA UMMIBelum ada peringkat
- Health Lesson 1, 2 & 3 Unit 2 (Grade 8)Dokumen15 halamanHealth Lesson 1, 2 & 3 Unit 2 (Grade 8)Cleofe SobiacoBelum ada peringkat
- Yo Vich 2019Dokumen14 halamanYo Vich 2019Julio LeviBelum ada peringkat
- Blocked Fallopian Tubes and Its Management With AyDokumen2 halamanBlocked Fallopian Tubes and Its Management With AywinodhelloBelum ada peringkat
- Diagnostic Laparoscopy: Reason For VisitDokumen4 halamanDiagnostic Laparoscopy: Reason For Visitdrnareshkumar3281Belum ada peringkat
- Maternal and Child Health Programmes: MCH ServicesDokumen10 halamanMaternal and Child Health Programmes: MCH ServicesRosebel LaguraBelum ada peringkat
- Ultrasound of The Early First TrimesterDokumen19 halamanUltrasound of The Early First TrimesterCorvo AtanoBelum ada peringkat
- Cesarean Scar Pregnancies and Their ManagementDokumen7 halamanCesarean Scar Pregnancies and Their ManagementClinton SitanggangBelum ada peringkat
- Complication During PregnancyDokumen43 halamanComplication During PregnancyRizza Domalaon BalangitanBelum ada peringkat
- Group 2B Case Study On Ectopic PregnancyDokumen36 halamanGroup 2B Case Study On Ectopic PregnancyANGEL GADOBelum ada peringkat
- Jay ObDokumen6 halamanJay ObJenxBelum ada peringkat
- Methotrexate for Ectopic Pregnancy is ImmoralDokumen21 halamanMethotrexate for Ectopic Pregnancy is ImmoralelainemenezBelum ada peringkat
- Cghs RatesDokumen25 halamanCghs RatesKi MuBelum ada peringkat
- 3 CH 19 20 High Risk PregnancyDokumen20 halaman3 CH 19 20 High Risk PregnancyabyBelum ada peringkat
- Pelvic Inflammatory DiseaseDokumen5 halamanPelvic Inflammatory DiseaseChona JimenezBelum ada peringkat
- Acute Appendicitis in Adults: Clinical Manifestations and DiagnosisDokumen37 halamanAcute Appendicitis in Adults: Clinical Manifestations and DiagnosisDaniela MuñozBelum ada peringkat
- OBGYN 1st Round 2021 AnsweredDokumen14 halamanOBGYN 1st Round 2021 AnsweredMuhammed Mostafa100% (4)
- Complications of PregnancyDokumen27 halamanComplications of PregnancyPatricia Anne Nicole CuaresmaBelum ada peringkat
- O&G OSCE by MaddyDokumen287 halamanO&G OSCE by MaddyNariska Cooper100% (1)