Cardiac Excitation
Diunggah oleh
ManuSoodHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cardiac Excitation
Diunggah oleh
ManuSoodHak Cipta:
Format Tersedia
Cardiac Excitation
Cardiac excitation
Cellular contraction depends on action potentials
Cardiac contraction depends on coordinated excitation, which depends on a
pacemaker a conduction systems causing coordinated cellular contraction.
The conduction systems:
o Electrically specialized myocytes including:
Sinoatrial (SA) node
Atrioventricular (AV) node
Bundle of His- right and left bundle branches
Purkinje fibers
o All have inherent excitability, but usually SA node determines rate of heart
The conduction pathway is very sophisticated.
Some special features include:
Substantial atrial to ventricular delay.
This allows the atria to completely
empty their contents into the ventricles.
This is achieved through a delay at the
AV node, as the atria are electrically
isolated from the ventricles apart from
the AV node.
Ventricular contraction begins at the
apex of the heart, progressing from the
apex to the base, and from the
endocardium to the Epicardium. This is
because contraction that squeezes
blood towards the semilunar valves is more efficient that multi-directional squeezes.
The left bundle branch provides electrical conduction to the chordae tendineae of the
mitral valve through a short branch called the anteriosuperior left bundle branch.
Electrical conductivity is also provided to the chordae tendineae of the tricuspid valve
through the moderator band. This allows both atrioventricular valves to close before
ventricular contraction.
Action potentials and relation to cardiac muscle contraction
The cardiac action potential varies in shape in different regions.
Pacemaker cells are the cells within the SA and AV node, whereas non-pacemaker cells are the
atrial and ventricular myocytes, and cells within the Purkinje fibers.
Non-pacemaker cells
In non-pacemaker cells, the cardiac action potential looks as follows:
The phases of this cardiac potential, and the currents responsible for them are shown below:
In the above picture, note that the absolute refractory period lasts from the fast upstroke to
the end of the plateau. The relative refractory period lasts from the end of the plateau to after
repolarization. This ensures a period of relaxation.
The Na
+
activation and inactivation is time- and voltage-related. When inactivated, the H-gate
closes, and is only re-opened after repolarization. Hyperpol can reverse the inactivation of
Na+ channels in Phase 1.
This cardiac action potential causes the muscle fibers to contract and relax according to the
following relationship:
Pacemaker cells
Normally, the SA node in the right atrium is the cardiac
pacemaker. It is a group of specialized muscle cells that have
unstable resting membrane potential
The special thing about this cell is that there is no fast Na
+
channel, and only the slow influx of Ca
2+
allows the SA node to
perform its depolarization function.
The phases of the pacemaker cell are shown below:
On details regarding action potentials in pacemaker
cells:
Slow depolarization is carried out in Phase 4
initially by funny currents, abbreviated to
IF, which are slow, inward Na
+
currents.
When the membrane potential reaches -50
mV, transient or T-type Ca
2+
channels open.
When the membrane potential reaches -40
mV, long-lasting or L-type Ca
2+
channels
open. This continues until the firing
threshold is reached. During this phase, K
+
channels from Phase 3 are inactivated.
Phase 0 depolarization is primarily caused by
increased by Ca
2+
conductance through the L-
type Ca
2+
channels. The other two channels
from Phase 4 close. Because this movement
of Ca
2+
into the cell isnt rapid, the rate of
depolarization is slow.
In Phase 3, K
+
channels open, causing
hyperpolarization. At the same time, L-type
Ca
2+
channels become inactivated.
Autonomic control of the SA node
When parasympathetic fibers are stimulated, the membrane potential is hyperpolarized
and SA node pacemaker activity decreases. Conversely, sympathetic activity depolarizes
the membrane potential and causes increased SA node pacemaker activity.
Electrocardiogram (ECG)
The magnitude of the voltages depends on the mass of tissues involved. Usually ventricles
have a greater mass of tissue than atria. The direction of the voltages is the sum of the
depolarizing and repolarizing waves.
The recorded potential on the ECG depends on:
The size and voltage of each depolarizing element
The distance from the generator
The orientation: maximum when electrodes are parallel to the dipole, but zero when
perpendicular to dipole.
The designation of positive and negative electrodes is arbitrary: generally, positive deflections
are recorded as the depolarization wave reaches the positive electrode.
The ECG only records change transients, not the entire potential of cardiac tissue.
Best depolarization recorded in Lead II, as it is parallel to depolarization wave in heart:
Ventricular repolarization occurs in reverse to depolarization of the heart: it spreads from
epicardial to endocardial regions instead of endocardial to epicardial like in the
depolarization wave. This is why the T wave is observed as a positive deflection, similar to the
QRS complex and P wave.
Note A very good .gif of the relationship between the ECG and conduction through the heart is
here: http://upload.wikimedia.org/wikipedia/commons/0/0b/ECG_Principle_fast.gif
Heart blocks
Partial
1
st
degree AV block:
All the impulses are slower than normal, and an unusually long PR interval.
2
nd
degree AV block:
Conducts some impulses but not others.
o Mobitz type I block (or Wenckebach block):
Gradual prolongation of the PR interval
AV node fails completely
Skips ventricular depolarization
o Mobitz type II block
The P-R interval is constant
Every nth ventricular depolarization is missing
Complete
3
rd
degree AV block:
No impulses are conducted through.
The AV node block electrically severs the atria and ventricles.
Ventricles are driven by their own pacemaker (AV dissociation)
Learning Objectives
Understand the electrical events that underlie the whole heart excitation process.
Understand that the specialized cardiac electrical conduction system and the electrical
properties of cardiac muscle ensure coordinated and ordered contraction that
produces effective pumping
Understand the specialized cardiac conduction pathways and the cell-to-cell
conduction structures
Describe regional differences in action potential configuration and the ionic basis for
the pacemaker potentials
Understand what the ECG is and how it is measured.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Physioex 9.0 Exercise 1 Act 1Dokumen5 halamanPhysioex 9.0 Exercise 1 Act 1Adela LhuzBelum ada peringkat
- Strategies For StartupDokumen16 halamanStrategies For StartupRoshankumar BalasubramanianBelum ada peringkat
- Methods to estimate stakeholder views of sustainabilityDokumen7 halamanMethods to estimate stakeholder views of sustainabilityAlireza FatemiBelum ada peringkat
- Dance Appreciation and CompositionDokumen1 halamanDance Appreciation and CompositionFretz Ael100% (1)
- IELTS Speaking Q&ADokumen17 halamanIELTS Speaking Q&ABDApp Star100% (1)
- Developing the cycle of maslahah based performance management system implementationDokumen27 halamanDeveloping the cycle of maslahah based performance management system implementationM Audito AlfansyahBelum ada peringkat
- Qad Quick StartDokumen534 halamanQad Quick StartMahadev Subramani100% (1)
- Exercise-01: JEE-PhysicsDokumen52 halamanExercise-01: JEE-Physicsjk rBelum ada peringkat
- Revision Worksheet - Matrices and DeterminantsDokumen2 halamanRevision Worksheet - Matrices and DeterminantsAryaBelum ada peringkat
- LEARNING ACTIVITY Sheet Math 7 q3 M 1Dokumen4 halamanLEARNING ACTIVITY Sheet Math 7 q3 M 1Mariel PastoleroBelum ada peringkat
- Srimanta Sankaradeva Universityof Health SciencesDokumen3 halamanSrimanta Sankaradeva Universityof Health SciencesTemple RunBelum ada peringkat
- Marshall Stability Test AnalysisDokumen5 halamanMarshall Stability Test AnalysisZick Zickry50% (2)
- Worksheet 5 Communications and Privacy: Unit 6 CommunicationDokumen3 halamanWorksheet 5 Communications and Privacy: Unit 6 Communicationwh45w45hw54Belum ada peringkat
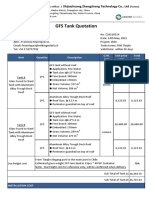
- GFS Tank Quotation C20210514Dokumen4 halamanGFS Tank Quotation C20210514Francisco ManriquezBelum ada peringkat
- GS16 Gas Valve: With On-Board DriverDokumen4 halamanGS16 Gas Valve: With On-Board DriverProcurement PardisanBelum ada peringkat
- Ratio Analysis of PIADokumen16 halamanRatio Analysis of PIAMalik Saad Noman100% (5)
- 202112fuji ViDokumen2 halaman202112fuji ViAnh CaoBelum ada peringkat
- 4 Influencing Factors of Learners Career Choice Parents Choice Vs Personal DescisionDokumen24 halaman4 Influencing Factors of Learners Career Choice Parents Choice Vs Personal Descisionmatteo mamaloBelum ada peringkat
- Damcos Mas2600 Installation UsermanualDokumen26 halamanDamcos Mas2600 Installation Usermanualair1111Belum ada peringkat
- Alternate Tuning Guide: Bill SetharesDokumen96 halamanAlternate Tuning Guide: Bill SetharesPedro de CarvalhoBelum ada peringkat
- Critical Methodology Analysis: 360' Degree Feedback: Its Role in Employee DevelopmentDokumen3 halamanCritical Methodology Analysis: 360' Degree Feedback: Its Role in Employee DevelopmentJatin KaushikBelum ada peringkat
- SolBridge Application 2012Dokumen14 halamanSolBridge Application 2012Corissa WandmacherBelum ada peringkat
- Bad DayDokumen3 halamanBad DayLink YouBelum ada peringkat
- 2021 JHS INSET Template For Modular/Online Learning: Curriculum MapDokumen15 halaman2021 JHS INSET Template For Modular/Online Learning: Curriculum MapDremie WorksBelum ada peringkat
- SBI Sample PaperDokumen283 halamanSBI Sample Paperbeintouch1430% (1)
- Pemaknaan School Well-Being Pada Siswa SMP: Indigenous ResearchDokumen16 halamanPemaknaan School Well-Being Pada Siswa SMP: Indigenous ResearchAri HendriawanBelum ada peringkat
- How To Text A Girl - A Girls Chase Guide (Girls Chase Guides) (PDFDrive) - 31-61Dokumen31 halamanHow To Text A Girl - A Girls Chase Guide (Girls Chase Guides) (PDFDrive) - 31-61Myster HighBelum ada peringkat
- Prlude No BWV in C MinorDokumen3 halamanPrlude No BWV in C MinorFrédéric LemaireBelum ada peringkat
- STS Prelim ExamDokumen2 halamanSTS Prelim ExamMychie Lynne MayugaBelum ada peringkat
- France Winckler Final Rev 1Dokumen14 halamanFrance Winckler Final Rev 1Luciano Junior100% (1)