Periodontal Abscess
Diunggah oleh
periodontics07Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Periodontal Abscess
Diunggah oleh
periodontics07Hak Cipta:
Format Tersedia
CONTENTS
1. Introduction
2. Definitions
3. Classification
4. Prevalence
5. Etiology
!. Clinical features
". Pat#ogenesis
$. %isto&at#ology
'. (icro)iology
1*. Diagnosis+differential diagnosis of &eriodontal a)scess
11. Investigations
12. Treat,ent
13. Co,&lications
14. Conclusion
1
Periodontal -)scess
Periodontal abscess is a frequent condition causing rapid loss of connective tissue.
It is a condition where patient may seek immediate treatment.
Definition. /
Defined as lesion with an expressed periodontal breakdown, occuring during a
limited period of time with easily detectable clinical symptoms !"afstorm et al, 1##$%
with locali&ed accumulation of pus located within gingival wall of periodontal pocket.
!'arran&a et al 1##(%
)ynonym * +ateral abscesses, parietal abscesses.
Classification. /
10 De&ending on location 12illette 3 4an#ous 1'$*5 Carran6a 1''*0
Periodontal abscesses
-ingival abscesses
20 De&ending on course 7 12alego 7 8eal et al 1''5 3 Carran6a 1''*0
.cute abscesses
'hronic abscesses
30 De&ending on nu,)er 1To&oll et al 1''*0
)ingle
/ultiple
Prevalence. /
.mong all emergency dental conditions, periodontal abscesses represent approx
01 of all dental emergences in )pain 1$ in 2). !.hl et al 1#03%. In 24 periodontal
abscess was diagnosed in 3561 of all parts treatment in 1 month !+ewis et al% was third
most prevalent emergency after dentoalveolar abscess !1$5781% periocoronitis !1(5
7
11(1%. Periodontal abscess is more prevalent in periodontitis patients. . periodontal
abscess is more likely to occur in presenting pockets !'arran&a%. 9eeth with abscesses are
usually considered to have hopeless prognosis !:ecker et al 1##$%.
Etiology. /
"ave been either directly associated to periodontitis or to sites without prior
existence of periodontal pockets.
a. Perio a)scesses in &eriodontitis. /
In periodontitis abscesses represent a period of active bone destruction.
;xistence of tortuous pockets with cul5de5sac which eventually becomes isolated
may favour formation of abscesses !'arran&a 1##(%
/arginal closure of pocket may lead to extension of infection into surrounding
PD+ tissue due to pressure of suppuration in closed pocket !<ewman )ims
1#6#%
=ibrin secretion, leading to local accumulation of pus may favour closure of
gingival margin to tooth surface !-alego5=eal et al 1##8%.
'hanges in composition of microflora, bacterial virulence or in host defence
could also make pocket lumen inefficient to drain !4areha et al 1#01%.
.bscesses in periodontitis may occur at various stages.
a. .cute exacerbation of untreated periodontitis !Dello >uso 1#08%.
b. During periodontal treatment !Dello >uso 'arran&a%
c. >efractory periodontitis !=ine 1##$%
d. During periodontal maintenance !'hace +ow 1##?, /c+eod et al
1##1%.
@hen periodontal abscess occurs immediately after scaling or after routine
prophylaxis it is related to dislodging calculus fragment deep into tissue.
!Dello >usso 1#08%
?
/ay also be due to inadequate scaling which will allow calculus to remain in
deepest pocket area, with resolution of inflammation at coronal pocket area which
occludes normal drainage causes abscesses formation !Dello >uso 1#08, 'arran&a
1##(%.
.bscesses immediately after therapy have been reported clinical study of -9>
membrane both resorbable nonresorbable by -arett et al 1##6 reported 1( out
of 0$ !<> barriers% $ out of 07 !>5barriers% showed abscesses or suppuration.
9reatment with systemic antibiotics without subgingival debridement in pats with
advanced periodontitis may cause abscess !"elovuo Pacurio 1#0# 9opoll et
al 1##(%. 9his has been attributed to likely change in composition of subgingival
microbiota leading to super infection !"elovuo et al 1##?%
<ifedipine therapy has also been attributed to abscess formation !4oller :en& et
al 1##7%. . case report should that after initiating therapy 0 abscesses appeared in
8 days. <ifedipine was discontinued drainage was done. 9he abscesses resolved
? weeks later drugs were again started after 7 weeks abscess was detected. <A
clear cut explanation for cause effect relationship is given.
). Periodontal a)scesses in a)sence of &eriodontitis
a. Impaction of foreign body !4areha et al 1#01%, such as orthodontic elastics
!Piniprato et al%, piece of floss !.brams 4opc&yk 1#0?%, popcorn kernel
!>ada et al% dislodged cemental tear !"aney et al 1##7%, corn husk in peri5
implant tissue !Ibbott et al 1##?%, unknown obBects. Periodontal abscesses
caused by foreign body, related with oral hygiene aids have been named oral
hygiene abscesses !-illette Can "ouse 1#0(%
b. Perforation of tooth by endodontic instrument. !'arran&a 1##(, .brams et al
1##7%
c. Infected lateral cysts !4areha et al 1#01%.
$
d. +ocal factors affecting morphology of root may predispose to periodontal
abscess formation.
Presence to cervical cemental tears has been related to rapid progression of
periodontitis abscesses development !"aney et al 1##7, Ishikawa et al% presence of
external root resorption !Dusof -ha&ali 1#0#%, an invaginated tooth !'hen et al% or a
cracked tooth !-oose 1#01% have been suggested as predisposing factors.
3. 8urcation involve,ent. /
.bscesses are frequently found in furcation !'ohen%.In maBority of cases of
abscesses furcation involvement is found !)mith et al 1#03%. In a study by Dang 1#06
most periodontal abscesses occur in molar about #7.81. Periodontal abscesses are
primary reason for molar extraction. =urthermore when loss of abscessed teeth was
compared between furcated non furcated teeth, more furcated teeth were lost than no
furcated teeth. !'arran&a%
4. Dia)etes. /
Predisposition of pats with diabetes to purulent infection makes them prone to
acute periodontal abscesses. )ystemic alteration includes lowered host response, impaired
immunity, decreased leukocyte chemotaxis bactericidal activity. Diabetes also have
vascular changes altered collagen metabolism which may increase susceptibility to
abscess formation. ;nhanced interaction of advanced glysation end products with their
cellular receptor !>.-;% is suggested as one of pathogenic mechanism of accelerated
periodontal disease in diabetes !+alla, "amster et al 1##0%
Pat#ogenesis 3 %isto&at#ology
;ntry of bacteria into pocket wall could be the first event.
Inflammatory cells are then attracted by chemotactic factors released by bacteria
the inflammatory reaction leads to tissue destruction !De @itt et al 1#08%.
9here is subsequent encapsulation of bacterial infection production of pus
!'arran&a 1##(%.
8
%isto&at#ology. /
Intact neutrophils are found surrounding a central area of soft tissue debris destroyed
leukocytes.
+ater stage a pyogenic membrane composed of macrophages neutrophils is organi&ed.
9he rate of destruction in abscesses will depend on growth of bacteria inside the foci
its virulence as well as local p", since acidic environment will favour activity of
lysosomal en&yme !De @itt et al 1#08%.
De @itt et al 1#08 studied biopsy punches from 17 abscesses found from outside to
inside.
a. . normal oral epithelium lamina propria.
b. .n acute inflammatory infiltrate
c. .n intense focus of inflammation !<eutro5+ymhpo% with surrounding '9
destroyed necrotic.
d. . ulcerated destroyed pocket epithelium
e. . central region as a mass of granular acidophilic amorphous debris. In
1 out of # specimen evaluated by ;/, gram negative bacteria were seen
invading the pocket epithelium altered '9
:acteria inside the abscesses were immersed in tissue exudates surrounded by
necrotic tissue.
(icro)iology. /
Periodontal abscesses microflora is composed mainly of periodontal pathogens,
especially P. gingivalis, P. intermedia, =. nucleatum, P. micros :. forsythus.
<ewman )ims 1#6# studied a abscesses found 3?.11 of flora was strict
anaerobes.
9opoll et al reported 8#.81 David "arerra reported $8.11 of anaerobic flora.
Percentage of -ram *ve was 8#.31 rods was 67.71 in <ewman )ims study
where as David "arrera !7(((% reported $$.61 -ram 5ve $$.61 rod in their
study.
3
9otal count of bacteria was approx to 1.?8x1(
3
bacteria in a study by "afstrom et
al.
:lack pigmented bacteria were found as most prevalent group of bacteria P.
gingivalis 8851((1 !9opell et al, .shimoto et al, <ewman )ims et al 1#6#%. P.
intermedia 7851((1 !9opell et al 1##(, <ewman )ims 1#6#%, P. melanogenica
(5771 <ewman )ims 1#6# Can @inkelhoff et al 1#08 and "ererra found 8(1,
37.81 13.61 respectively.
=. nucleatum has shown high prevalence $$.35381 !9opell et al 1##(, "affstorm
et al 1##$% 6(.01 !"arrerra et al 7(((%.
:. forsythus in $6.11 of pats !"arrerra et al% 1$.?1 of patients !.shimoto et al
1##0%
P. micros were found in 6(.31 of pats !"arrerra et al 7(((%. <o other study has
reported so. P. micros is found in patients with periodontitis !>ams et al 1##7%
'. rectus was found in $.71 of patients !"arrerra et al% 0(1 !"afstorm et al
1##$% patients.
P. gingivalis represented the highest percentage when present 1?.31 of total flora
!"arrerra et al 7(((% percentages ranging 1(.$1 to 771 have been reported
!9opell et al 1##(, <ewman )ims 1#6#%.
+ower properties of P. intermedia are reported 0.81 !"arrerra et al 7(((% $.$5
61 by !"affstorm et al 1##$%.
). viridans is most common isolate when aerobic 9ech is used !;pstein 1#66%.
)pirochetes have been found as predominant cell type !mean $(.31 E 1(.#1%
when dark field microscopy was sued !9rope et al 1#00%.
)trains of Peptostreptococcus, ).milleri, :acteroide. capillosus, Cellionela, :.
fragalis ;. corrodens have been isolated !'hen 1#0?%
Disappearances of P. gingivalis from abscessed sites after treatment suggest close
association of these microbes with abscess !"afstrom 1##$%.
Clinical factors./
9wo types clinically i.e. on course of lesion
6
a0 -cute./
.ppears avoid elevation of gingiva along lateral aspect of root.
-ingiva is edematous rod with smooth shining surface.
Pus may be expressed from gingival margin by gentle digital pressure.
)ymptoms may vary from slight discomfort to severe pain swelling. !)mith
Davis 1#03%.
=eeling of pressure in gums is common.
9here is increase mobility, elevation of tooth in socket tenderness to percussion or
mastication.
>egional lymphadenopathy can be detected in some people.
:leeding on probing is present in 331 of cases.
Pockets present are deeper than 3mm in !37.11% cases while $53mm in !?$.$1% cases
!"arrerra 7(((%
>egarding mobility !)mith Devis 1#03% 83.81 to 6#1 !"arrerra et al 7(((% of teeth
showed mobility.
/olars are most commonly involved teeth 3#1 of cases !"arrerra et al 7(((%
)imilar involvement is reported by -ray et al 1##$ slightly lower by )mith Davis
1#03
/c+eod et al showed 381 of affected teeth are multirooted
1(5$(1 pats show regional lymphadenopathy !"arrerra et al 7(((, )mith Davis
1#03%
In a study by "arrerra !7(((%periodontal abscesses were seen $11 associated with
first molar, 7$1 with seemed molar, 161 upper premolars, 61 lower premolars, 61
incisors ?.81 upper third molars.
881 abscesses were found in upper Baw $01 are located on buccal aspect 7$1
distal aspect, 1?.01 on lingual F palatal mesial aspect 371 complained severe pain.
2. C#ronic a)scesses. /
0
-enerally associated with sinus tract. Arifice of fistula may be covered by small
granulation pink mass
2sually asymptomatic although patients can refer mild symptoms !'arran&a
1##(%
.n acute abscess becomes chronic when drainage is established naturally through
sinus tract or sulcus.
Patients may have dull or gnawing pain, slight elevation of tooth desire to bite
tightly of grind.
Diagnosis. /
)hould be made after overall evaluation interpretation of patients chief
complaint, medial F dental history, clinical radiographic examination.
>adiographs pulp test may give additional information relative to etiology of
swelling.
'linically avoid elevation of gingiva along lateral aspect of root !'arran&a 1##(%
)ymptoms range from light to sever discomfort, tenderness of gingiva, swelling
tooth mobility, tooth elevation.
>adiographically may reveal normal appearance F some degree of bone loss
increase width of PD+ space.
Differential Diagnosis. 1-#l et al 1'$!5 4arletta 1'$$0
Periapical abscesses
+ateral periapical cysts
Certical root fracture
;ndo perio abscesses
Post op infection
Asteomyelitis !Parrish et al 1#0#%
-ingival squamous cell carcinoma !9orabineBad >ick 1#0(%
/etastatic carcinoma of pancreatic origin !)elelen et al%
#
;osinophilic granuloma
Treat,ent. /
.cute abscess treatment includes 7 stages. !.mmons 1##3%
/anagement of acute lesion
.ppropriate management of original or residual lesion.
If tooth severely damaged prognosis is bad has to be extracted !)mith Devis
1#0# .mmon 1##3%
Protocol includes !.mmon 1##3 .hl et al 1#03%
a. Drainage through pocket
b. )caling of tooth surface
c. 'ompression debridement of soft tissue wall irrigation with saline.
d. Pat should rinse with when saline examined after 7$5$0 hrs.
e. 1 week later definitive treatment should be given.
Drainage could need external incision or flap topical antiseptic application after
drainage !'arran&a 1##(%.
.ddition of systemic antibiotics is not well defined. )ystemic antibiotic are
advised only when there is clear systemic involvement need for premedication
@hen infection is not well locali&e 'ases in where adequate drainage cannot be
established. )ome authors recommend combination of basic treatment antibiotics
!-aleyo =eal et al%
'ombination of IFD G systemic antibiotics has been considered as successful
!-enco 1##1%
Penicillins are drug of first choice followed by amoxycillin metronida&ale
"afstrom !1##$% suggested conservative treatment top gain as much attachment as
possible. Drainage was done through pocket with saline irrigation tetracycline
was prescribed for 7 weeks !1 gFday%. 9wo conclusions were suggested.
1. Importance of drainage
7. Potential for regeneration
1(
'hronic abscesses can be treated by surgical therapy i.e. gingivectomy flap
procedures. !'arran&a 1##(%. /ainly abscesses associated with vertical bone
defects where resolution of abscesses may only be achieved by surgical operation
!4areha et al 1#01%.
)urgical flaps are proposed in cases of post prophylaxis abscesses to gain good
debridement.
Co,&lication. /
1. Toot# loss. /
)een in cases of advanced to moderate periodontitis !'hace low 1##?, /c+eod
et al 1##6%.
9ooth with "FA repeated abscesses is considered with other findings, a tooth with
hopeless prognosis !:ecker et al 1#0$%
2. Disse,ination of infection
a. 4actere,ia follo9ing treat,ent of a)scesses
)u&uki Delisle 1#0$ related a case of pulmonary actinomycosis due to
periodontal abscess.
:rain abscess was reported by -allauger et al in case of periodontal abscess
treated by drainage curettage.
9he risk of bacteremia during drainage of an abscess can be reduced if, before
incision a needle aspiration of content of abscess is done !>oberts )heriff 1##(,
=lood et al 1##(%
2ingival a)scess. /
+ocalised, painful, rapidly expanding lesion involving marginal gingiva or
interdental papilla sometimes in a previously disease free area.
2sually an acute inflammatory response to foreign substances forced into gingiva
in its early stages appears as red swelling with smooth, shining surface.
In 7$5$0 hrs the lesion is usually fluctuant pointed, exudate may be expressed.
11
If permitted to progress the lesion gradually ruptures.
)ymptoms include pulpal hypersensitivity.
9reatment includesH
;limination of foreign obBect through careful debridement !.brams 4opc&yle
1#0?%
Drainage through sulcus with a probe or light scaling
>insing with warm saline follow up after 7$5$0 hrs.
Conclusion. /
Periodontal abscess is ?
rd
most frequent dental emergency, representing 651$1 of
all dental emergencies 3561 of all pats seen in clinics
"igher prevalence has been found with
8#1 of untreated pats
1?.81 during active treatment
?61 during maintenance phase
7 main etiologies should be distinguished
1. 9hose related to preexisting periodontal pockets
7. 9hose which do not necessarily need a deepened pocket.
Possible etiologies include
1. ;xacerbation of existing disease
7. Post therapy abscesses
?. >e emergence of cured disease
$. )uper infection
8. Impaction of foreign obBects
3. =actors altering root morphology
/icroflora related with periodontal abscesses is complex dominated by gr5ve
strict anaerobic rods such as P. gingivalis, P. intermedia =. nucleatum
9he periodontal abscess has possibility to spread microbes to other body sites.
17
9ooth with periodontal abscess has worst prognosis has higher chance of being
lost
9hree therapeutic approaches have been discussed
1. Drainage debridement
7. )ystemic antibiotics with or without other treatments
?. Periodontal surgery
:eferences
1. 'arran&aIs clinical periodontology !1(
th
edition%
7. 'onsensus reportH .bscesses of the periodontium .nn. Periodontol pg. 0?, Col. $.
no. 1. Dec. 1###
?. 9reatment of periodontal abscess in .dult Patients Presenting for Dental 'are in
9he Aral "ealth )ervices /inistry Af "ealth /alaysia 7((?
$. 'linical and microbiological characteri&ation of periodontal .bscesses Jaramillo
., J 'lin Periodontol 7((8, ?7H 171?*1710
8. 9he periodontal abscessH a review "errera D, >oldaKn J 'lin Periodontol 7(((,
76H ?66*?03
3. )ystemic anti5infective periodontal therapy5 . systemic review5"affaBee,.nn
periodontology57((?
6. 9he periodontal abscess !I%. 'linical and microbiological findings "errera D,
>oldaKn J 'lin Periodontol 7(((, 76H ?06*?#$
1?
Anda mungkin juga menyukai
- Bleeding Disorder & Periodontitis: Department of PeriodonticsDokumen35 halamanBleeding Disorder & Periodontitis: Department of Periodonticsperiodontics07Belum ada peringkat
- Classification and Types of Periodontal PocketsDokumen48 halamanClassification and Types of Periodontal Pocketsperiodontics07Belum ada peringkat
- Periodontal PocketDokumen31 halamanPeriodontal Pocketperiodontics07Belum ada peringkat
- IncisionDokumen32 halamanIncisionperiodontics07Belum ada peringkat
- Classification and Types of Periodontal PocketsDokumen48 halamanClassification and Types of Periodontal Pocketsperiodontics07Belum ada peringkat
- NupDokumen37 halamanNupperiodontics07Belum ada peringkat
- Root Surface ConditioningDokumen88 halamanRoot Surface Conditioningperiodontics07Belum ada peringkat
- Mechanical Induction of New Bone Formation Through Distraction OsteogenesisDokumen26 halamanMechanical Induction of New Bone Formation Through Distraction OsteogenesissprapurBelum ada peringkat
- Cement UmDokumen2 halamanCement Umperiodontics07Belum ada peringkat
- TFODokumen30 halamanTFOperiodontics07Belum ada peringkat
- LDDDokumen82 halamanLDDperiodontics07Belum ada peringkat
- CementumDokumen139 halamanCementumpraveenmdasBelum ada peringkat
- GTRDokumen2 halamanGTRperiodontics07Belum ada peringkat
- LDDDokumen82 halamanLDDperiodontics07Belum ada peringkat
- Classification of Periodontal Diseases: DR Prateek ShresthaDokumen28 halamanClassification of Periodontal Diseases: DR Prateek ShresthaHimalayawandererBelum ada peringkat
- Surgical Periodontal TherapyDokumen37 halamanSurgical Periodontal Therapyperiodontics07Belum ada peringkat
- Periodontal Pockets DefinedDokumen23 halamanPeriodontal Pockets Definedperiodontics07Belum ada peringkat
- Alveolar RidgeDokumen8 halamanAlveolar Ridgeperiodontics07Belum ada peringkat
- Dental PlaqueDokumen2 halamanDental Plaqueperiodontics07Belum ada peringkat
- Dental PlaqueDokumen2 halamanDental Plaqueperiodontics07Belum ada peringkat
- Gingival RessionDokumen12 halamanGingival Ressionperiodontics07Belum ada peringkat
- Dental stains: Causes, types and treatmentDokumen30 halamanDental stains: Causes, types and treatmentArtur Radvanszki100% (1)
- T ConsentDokumen1 halamanT Consentperiodontics07Belum ada peringkat
- Dentin HypersensitivityDokumen147 halamanDentin Hypersensitivityperiodontics07Belum ada peringkat
- PlaqueDokumen75 halamanPlaqueperiodontics07Belum ada peringkat
- To All The Great Teachers & Those Who Aspire To BeDokumen18 halamanTo All The Great Teachers & Those Who Aspire To Beperiodontics07Belum ada peringkat
- Pmn's and Its AbnormalitiesDokumen65 halamanPmn's and Its Abnormalitiesperiodontics07Belum ada peringkat
- Journal ClubDokumen41 halamanJournal Clubperiodontics07Belum ada peringkat
- Ridge DDokumen10 halamanRidge Dperiodontics07Belum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- CIPHIDokumen256 halamanCIPHIसदानंद देशपांडेBelum ada peringkat
- Ban Biblio NumberedDokumen23 halamanBan Biblio NumberedYayangAsanggaBelum ada peringkat
- Latihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2Dokumen9 halamanLatihan Un Bahasa Inggris 2018: The Following Text Is For Questions 1 and 2AWDBelum ada peringkat
- Botany Vol-2 - EMDokumen232 halamanBotany Vol-2 - EMVandanaBelum ada peringkat
- Managing The Myths of Health Care PDFDokumen5 halamanManaging The Myths of Health Care PDFkaremBelum ada peringkat
- Correlation of Sound and Colour - Paul Foster CaseDokumen30 halamanCorrelation of Sound and Colour - Paul Foster Casesrk777100% (7)
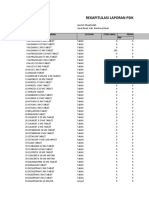
- Rekapitulasi Laporan Psikotropika Bandung BaratDokumen8 halamanRekapitulasi Laporan Psikotropika Bandung BaratFajarRachmadiBelum ada peringkat
- Swami Paramarthananda's Talks on Self-KnowledgeDokumen332 halamanSwami Paramarthananda's Talks on Self-Knowledgemuralipmd100% (1)
- Estevan Jimenez Patient Clinical Report ForDokumen7 halamanEstevan Jimenez Patient Clinical Report ForIsrael MelloBelum ada peringkat
- Male Stress Urinary Incontinence: Giulio Del Popolo Donatella Pistolesi Vincenzo Li MarziDokumen189 halamanMale Stress Urinary Incontinence: Giulio Del Popolo Donatella Pistolesi Vincenzo Li MarziVeronika AtaBelum ada peringkat
- Errata: Shadow of The Demon LordDokumen3 halamanErrata: Shadow of The Demon LordKaio CorsatoBelum ada peringkat
- Alconfactsheet CenturionDokumen3 halamanAlconfactsheet Centurionsudhakar.mrBelum ada peringkat
- Gold Foil: Safety Data SheetDokumen4 halamanGold Foil: Safety Data SheetSyawatulshuhada SyawalBelum ada peringkat
- CPHQ Review Course Nov 28-29 2012Dokumen195 halamanCPHQ Review Course Nov 28-29 2012Khaskheli Nusrat100% (2)
- The Clinical Toxicology of Sulfur Mustard: Review ArticleDokumen18 halamanThe Clinical Toxicology of Sulfur Mustard: Review ArticleGiany GausBelum ada peringkat
- 129 Accommodative EsotropiaDokumen6 halaman129 Accommodative EsotropiakarenafiafiBelum ada peringkat
- BONE Level 2-BDokumen60 halamanBONE Level 2-Bjefri banjarnahorBelum ada peringkat
- Maharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListDokumen30 halamanMaharashtra Government PGM Admissions 2015-2016 Round 2 Selection ListAbhinav BhardwajBelum ada peringkat
- 1 Gram Positive Bacterial InfectionDokumen87 halaman1 Gram Positive Bacterial InfectionCoy NuñezBelum ada peringkat
- Pain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalDokumen50 halamanPain Management in The Emergency: Dr. Prathiba Prasad Emergency Physician Masafi HospitalPrathiba PrassaddBelum ada peringkat
- Sirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureDokumen3 halamanSirenomelia: A Case Report of A Rare Congenital Anamaly and Review of LiteratureInt Journal of Recent Surgical and Medical SciBelum ada peringkat
- Final Project LevofloxacinDokumen102 halamanFinal Project LevofloxacinJalwaz TihamiBelum ada peringkat
- Research Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Dokumen4 halamanResearch Background: (Budget 2016: Chapter 5 - An Inclusive and Fair Canada, 2021)Talha NaseemBelum ada peringkat
- Activity Intolerance Care Plan For CFDokumen8 halamanActivity Intolerance Care Plan For CFapi-314197645Belum ada peringkat
- Turmeric Benefits: Health Benefits of Turmeric - Are There Any Side Effects of Turmeric?Dokumen5 halamanTurmeric Benefits: Health Benefits of Turmeric - Are There Any Side Effects of Turmeric?Angelyn Taberna NatividadBelum ada peringkat
- C 5 Dosage Form DesignDokumen20 halamanC 5 Dosage Form DesignrajeebBelum ada peringkat
- Cranial Base Dan Emergency CaseDokumen34 halamanCranial Base Dan Emergency Caserahmad wahyuBelum ada peringkat
- Nurdiana. R PD-B/ 0810713031: Module TaskDokumen10 halamanNurdiana. R PD-B/ 0810713031: Module TaskNurdiana RahmadaniBelum ada peringkat
- CBD Sirosis, Hematemesis MelenaDokumen29 halamanCBD Sirosis, Hematemesis Melenadyah farahBelum ada peringkat
- Bioactive Compounds in Phytomedicine BookDokumen228 halamanBioactive Compounds in Phytomedicine BookAnil KumarBelum ada peringkat