Document (3) G
Diunggah oleh
DiskaAstariniDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Document (3) G
Diunggah oleh
DiskaAstariniHak Cipta:
Format Tersedia
Pathophysiology
A number of factors are involved in hair disorders. Genetic factors, diet, endocrine abnormalities,
systemic illnesses, drug intake, and hair shaft abnormalities may cause hair loss. Most alopecia
cases are due to hair cycle changes.Figure 1: Click to Enlarge
Normal Hair Cycling
Understanding the basic facts about normal hair growth is essential for correct interpretation of
hair loss events. The average rate of hair growth for a normal scalp is 0.35 mm a day,3however,
slower growth occurs in elderly people and in patients with chronic illness. Scalp hair grows in an
asynchronous pattern, with approximately 80% of hair follicles in an active growing phase
(anagen) and 10% to 20% in an involuting and resting phase (catagen and telogen). Figure
1 summarizes the hair growth cycle. Telogen hair fibers shed in 3 to 5 months and are responsible
for daily hair shed. Average daily hair loss is 25 to 100 hair fibers.3Alteration of hair growth
cycling manifests clinically as increased shedding of scalp hair. In androgenetic alopecia, the hair
cycle is shorter, and the hair follicle becomes progressively thinner (miniaturization) as a result of
an androgen effect. Telogen effluvium is the result of an increased number of resting follicles,
usually a few weeks after a trigger. Alopecia areata, an autoimmune disease, presents as an anagen
effluvium. Autoimmune inflammation around the hair follicle aborts hair growth. Changes in
chemical or physical structure of the hair shafts result in hair shaft abnormalities
(trichodystrophies). Inherited trichodystrophies are associated with keratinization defects and are
less frequent than acquired ones (from external trauma).Hair stem cells are localized in the
midportion of the follicles, on the middermis.4 If this area remains undisturbed, the follicles
recycle throughout one's life. However, inflammation in this area can destroy the stem cells. In
that case, a cicatricial alopecia is established, and no follicle is able to regrow.5 Examples of
cicatricial alopecia are infectious folliculitis, discoid lupus erythematosus, and lichen
planus (Table 1).
Table 1: Causes of Hair Loss
Noncicatricial alopeciaCicatricial alopeciaAndrogenetic alopeciaTelogen effluviumAlopecia
areataTrichodystrophiesInfectious folliculitisLupus erythematosusLichen planusBack to Top
Signs and Symptoms
Clinical history should include duration of hair loss, family history, affected areas (localized or
diffuse scalp, scalp alone, or other hair-bearing areas), associated nail changes, and hair care
habits (shampooing, bleaching, perming).Figure 3: Click to EnlargeFigure 2: Click to EnlargeThe
way the hair falls out is important to establishing the nature of the problem. One has to determine
whether the hair is falling by the roots (shedding), is thinning, or whether the hair shafts are
fracturing. Each of these complaints is meaningful because each points to a type of hair
disorder (Table 2).The clinical presentation of hair loss caused by androgenetic alopecia, telogen
effluvium, trichodystrophy, or alopecia areata varies from a localized area of thinning on top of the
head in androgenetic alopecia (Figure 2) to a total body hair loss (alopecia areata universalis). The
most common history in patients with alopecia areata is abrupt onset of patchy circular areas of
hair loss(Figure 3). The incidence of progression to a more widespread loss causing alopecia
totalis (total scalp) or alopecia universalis (total body) is about 1%.6
Table 2: Correlation Between Common Complaints and Cause of Hair Loss
ComplaintHair DisorderGradual thinning without sheddingAndrogenetic alopeciaDiffuse
sheddingTelogen effluviumHair breakage or hair that does not growTrichodystrophyShedding
with circular areas of hair lossAlopecia areataCopyright 2002 The Cleveland Clinic
FoundationBack to Top
Diagnosis
The diagnosis of hair disorders is complex, and an evaluation of the clinical presentation, history,
and physical examination is necessary. Laboratory work-up may be helpful. Diagnostic office
techniques include visual examination of all the hair-bearing skin areas as well as examination of
the nails. Inherited keratinization disorders and alopecia areata may be associated with nail
dystrophy. Clinical examination should include scalp condition, pattern of hair loss, and length
and diameter of hair fibers. Additional examinations are hair pulls, clippings, plucks, and
collections (shed hair), light microscopy examination of hair fibers, scrapings of scalp scales for
bacterial and fungal culture, and a scalp punch biopsy (Table 3).
Table 3: Examinations for Hair Disorders
Patterns of hair lossLength and diameter of hair fibersScalp skin conditionLight microscopy
examination of hairHair pull, clipping, and pluckHair collectionsScrapings of scales for
cultureScalp punch biopsyA hair clipping for light examination is diagnostic in patients with
trichodystrophies. Trichorrhexis nodosa, a node-like fragile area in the hair shaft, is the most
common finding and can be associated with acquired and inherited hair shaft
abnormalities (Figure 4).Figure 5: Click to EnlargeFigure 4: Click to EnlargeHair collections of
the shed hair can be diagnostic in patients with telogen effluvium. These patients commonly bring
amazingly large hair collections, literally bags of shed hair (Figure 5).Male androgenetic alopecia
is usually genetically predisposed, and no additional investigation is necessary. Female
androgenetic alopecia often appears in women with a strong family history of baldness or a
personal history of hirsutism, acne, or abnormal menses (signs of androgen excess). Genetically
predisposed women may present with androgenetic alopecia in adolescence (puberty),
perimenopause, or postmenopause. Young women have a higher incidence of acquired adrenal
hyperplasia and polycystic ovaries. In general, postmenopausal women have lower levels of
hormones, especially estrogen. However, testosterone levels in postmenopausal women are
relatively high when compared with levels in adolescents. Androgen excess screening for women
with hair loss should include measurements of total testosterone and dehydroepiandrosterone
sulfate.Other laboratory tests, such as a complete blood count, ferritin measurement, and thyroid
screening, may be helpful. Ferritin level should usually be higher than 40 g/L to ensure normal
hair growth. A hair pluck test and a scalp biopsy may be helpful in any hair loss case. Cicatricial
alopecias are difficult to differentiate clinically and often require a scalp biopsy for correct
diagnosis. A 4-mm punch is recommended.Back to Top
Therapy and Outcomes
A great variety of therapies are available for hair loss. The appropriate choice is always based on
the type of hair disorder, age of the patient, and extent of disease. Topical Minoxidil, a promoter of
local hair growth, is widely used in all noncicatricial alopecia.
Androgenetic Alopecia
In men, medical treatment of androgenetic alopecia includes topical minoxidil 2% or 5% (Rogaine
for Women and Rogaine for Men) twice a day and selected antiandrogens. Oral finasteride 1mg
(Propecia), a 5-a-reductase inhibitor, blocks the peripheral conversion of testosterone to
dihydrotestosterone. Serum and tissue (scalp) dihydrotestosterone concentrations are decreased in
men taking finasteride, resulting in a progressive increase in hair count. Additional results can be
achieved with creative hair styles, hair pieces, hair transplantation, and scalp reduction.Women
have more treatment options. Minoxidil 2% and 5% (Rogaine for Women and Rogaine for Men)
can also be used, the 5% being more effective. In addition to antiandrogens, estrogen replacement
therapy can be used.7 These agents include the estrogen-dominant oral contraceptive ethynodiol
diacetate and ethinyl estradiol (Demulen 1/50) or conjugated estrogen (Premarin) given daily or in
conjunction with a progesterone, such as medroxyprogesterone (Provera). Spironolactone
(Aldactone) in doses of 50 to 200 mg has successfully been used as an antiandrogen. If adrenal
suppression is needed for androgen excess, dexamethasone (Decadron) in doses of 0.125 to 0.25
mg may be taken at bedtime for 4 months or longer.
The typical finding of androgenetic alopecia is a total number of follicles within
the usual range, with a decrease in the ratio T:V, where the diagnostic rate is
considered less than or equal to 4:1 (Figure 4).
24-26,28,34
Over time, TC also
increases.
24-26,28,34
Another characteristic of the disease is noticeable variation
between the diameters of the channels and terminal follicular
shafts.
24,25,28,34
Increased size of sebaceous glands is mentioned by some
authors, although this parameter has not been critically
assessed.
34
Inflammation, when present, is predominantly lymphocytic and of
mild intensity, usually around the superficial parts of the
follicle.
25,34
Trichomalacia is not observed. As there is progressive
miniaturization of follicles, the number of follicular fiber tracts also increases,
and the more chronic the disease is, more hyalinized and less vascularized they
become.
T-cell mediated perifollicular inflammation leading to disruption of the normal hair cycle has
been implicated in the pathogenesis of alopecia areata. Unlike cicatricial alopecias (eg, lichen
planopilaris or discoid lupus), the inflammatory process in alopecia areata does not lead to
scarring and destruction of the hair follicle.
Disruption of the hair cycle Hair follicles in normal skin cycle through periods of active hair
growth (anagen), follicular involution (catagen), and follicular rest (telogen) (picture below). In
alopecia areata, perifollicular inflammation is associated with dystrophic changes in anagen
follicles and stimulates premature transition of anagen follicles to the nonproliferative catagen
and telogen phases.
Autoimmunity The association of alopecia areata with autoimmune diseases such as
thyroiditis and vitiligo suggest an autoimmune etiology for this disorder. Theories for the
mechanism of autoimmunity have included the following:
Collapse of the immune-privileged status of hair follicles leads to a cell-mediated immune
response that targets follicular antigens.
Immune privilege does not extend to the catagen phase, and inflammatory cells that present
during follicular regression inappropriately trigger an immune response against follicular
antigens.
Although a cell-mediated immune response is thought to be primarily responsible for hair loss in
alopecia areata, hair follicle autoantibodies are frequently present in sera from affected
individuals. Whether these antibodies have a pathogenic role is uncertain.
Genetics Genetic background influences risk for the development of alopecia areata. In a
study of 206 patients with alopecia areata, 20 percent had a first degree relative with the
disease. The importance of genetics is also supported by studies reporting high concordance
rates among identical twins. In one study involving 19 sets of monozygotic twins, both twins
were affected in 42 percent of twin sets. In contrast, among 31 pairs of dizygotic twins, only 10
percent shared the disease.
The genetic predisposition for alopecia areata is thought to be polygenic in nature, and the
results of a genome-wide association study suggest that genes involved in the regulation of the
innate and adaptive immune systems participate in the pathogenesis of this disease. In the
study, genomic regions containing the CTLA4, IL-2/IL-21, IL-2RA, and Eos genes, all of which
are involved in regulating the activation or proliferation of regulatory T cells, were identified as
susceptibility loci for alopecia areata. A strong association also was detected in a region
containing genes encoding ULBPs, molecules involved in the stimulation of natural killer, natural
killer T, gamma delta T, and CD8+ lymphocytes.
In addition to these findings, the genome-wide association study confirmed previously reported
associations of alopecia areata with human leukocyte antigen (HLA) genes. The HLA-DQB1*03
allele, among others, may be an important marker for susceptibility to the disease. Several
susceptibility loci that have been associated with other autoimmune diseases (eg, CTLA4,
IL-2/IL-21, IL-2RA) also were identified, indicating that alopecia areata may share a common
pathway with other autoimmune diseases.
Other A variety of factors, such as infections, drugs, and vaccinations, have been implicated
in triggering episodes of alopecia areata. Some patients report severe stress, especially
emotional stress, as a precipitating event, although many patients have no such history. Remote
events, such as childhood trauma, have also been associated with the development of alopecia
areata in adults
Anda mungkin juga menyukai
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Normal Puerperium & Lactation Dr. Renu SinghDokumen29 halamanNormal Puerperium & Lactation Dr. Renu SinghDiskaAstariniBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Chapter 2 Maternal Anatomy WilliamsDokumen60 halamanChapter 2 Maternal Anatomy WilliamsDiskaAstariniBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Presentation 1Dokumen2 halamanPresentation 1DiskaAstariniBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Leukocoria 2016Dokumen35 halamanLeukocoria 2016DiskaAstarini100% (1)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Relative Afferent Pupillary DefectDokumen11 halamanRelative Afferent Pupillary DefectDiskaAstariniBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Lisa Payne - Group Leader: Sharron Beasley Venessa Escobar Kristy Fendley Brenda Jackson Vanessa Martin Natasha VillarsDokumen19 halamanLisa Payne - Group Leader: Sharron Beasley Venessa Escobar Kristy Fendley Brenda Jackson Vanessa Martin Natasha VillarsDiskaAstariniBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Case Report: Viona I11109064Dokumen41 halamanCase Report: Viona I11109064DiskaAstariniBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- My Dissa PresentDokumen39 halamanMy Dissa PresentDiskaAstariniBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Leukocoria 2016fixDokumen37 halamanLeukocoria 2016fixDiskaAstariniBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Red Eye With Normal VisionDokumen58 halamanRed Eye With Normal VisionDiskaAstariniBelum ada peringkat
- Jurnal Reading IpdDokumen12 halamanJurnal Reading IpdDiskaAstariniBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Radiology of The Respiratory SystemDokumen184 halamanRadiology of The Respiratory SystemDiskaAstariniBelum ada peringkat
- Introduction To Psychology: States of ConsciousnessDokumen27 halamanIntroduction To Psychology: States of ConsciousnessCharlie Ken Cruz-GrazaBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Christenhusz 2011 Et Al Phytotaxa19 Gymnosperms 55 70Dokumen16 halamanChristenhusz 2011 Et Al Phytotaxa19 Gymnosperms 55 70Aldo BarelaBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Normal CT ChestDokumen81 halamanNormal CT ChestRahmat SyahiliBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Puberphonia 11Dokumen19 halamanPuberphonia 11jaguar1979100% (2)
- Rapid Sterility Testing Using PallchekDokumen29 halamanRapid Sterility Testing Using Pallchekvkumar6883Belum ada peringkat
- Module 2Dokumen14 halamanModule 2Muskaan BindalBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- 1000 Extremely Golden Points For Exam by Dr. Asif Ali KhanDokumen35 halaman1000 Extremely Golden Points For Exam by Dr. Asif Ali KhanSadiq Achakzai100% (2)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Muscular System NotesDokumen40 halamanMuscular System NotesWindhy Dzakiyyah Aurora100% (1)
- PathophysiologyDokumen9 halamanPathophysiologypaul andrew laranjo asuncionBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Solomon y Corbit - 1978 - An Opponent-Process Theory of MotivationDokumen14 halamanSolomon y Corbit - 1978 - An Opponent-Process Theory of Motivationmario_garcés_4Belum ada peringkat
- 3-Kingdom AnimaliaDokumen16 halaman3-Kingdom AnimaliaEhmz XavièrBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Renal New Growth - NCM 103 - or CaseDokumen19 halamanRenal New Growth - NCM 103 - or CasePat EnriquezBelum ada peringkat
- Amino AcidsDokumen18 halamanAmino AcidsShreesh MohanBelum ada peringkat
- PB 840 - Brochure PDFDokumen4 halamanPB 840 - Brochure PDFPriyankaBelum ada peringkat
- The Resveratrol StoryDokumen7 halamanThe Resveratrol StoryCliusBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- ArticlesDokumen4 halamanArticleschris7982Belum ada peringkat
- Red Flags For The MRCGPDokumen3 halamanRed Flags For The MRCGPUsm LeeBelum ada peringkat
- Stages of SleepDokumen16 halamanStages of SleepMelanie100% (1)
- Azithromycin 500mg Tab (Zithromax)Dokumen6 halamanAzithromycin 500mg Tab (Zithromax)Mayownski TejeroBelum ada peringkat
- VisibleBody Knee Flexion EbookDokumen13 halamanVisibleBody Knee Flexion EbookdophuBelum ada peringkat
- Binaural Frequency List GuideDokumen30 halamanBinaural Frequency List GuideChristopher Parker100% (7)
- What Is Cardiomyopathy?Dokumen11 halamanWhat Is Cardiomyopathy?ImmanuelBelum ada peringkat
- TrainingPlanGuideforAerobicBasePlan PDFDokumen2 halamanTrainingPlanGuideforAerobicBasePlan PDFAlex HeslopBelum ada peringkat
- Automated Counters3Dokumen14 halamanAutomated Counters3Jacky SharmaBelum ada peringkat
- IB Diploma Biology Topic 1 Cell Biology Answers To Practice ProblemsDokumen1 halamanIB Diploma Biology Topic 1 Cell Biology Answers To Practice ProblemsMahebul MazidBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Reactive The Trauma Active Brain WorksheetDokumen5 halamanReactive The Trauma Active Brain Worksheetkadbury1900Belum ada peringkat
- Features of The Muscular SystemDokumen34 halamanFeatures of The Muscular SystemQuỳnh NhưBelum ada peringkat
- Yoga and High Blood Pressure Hypertension 2 AVonCammererDokumen9 halamanYoga and High Blood Pressure Hypertension 2 AVonCammererAndrea Van RankinBelum ada peringkat
- General Principles of Exercise For Health and Fitness: © 2014 Pearson Education, IncDokumen24 halamanGeneral Principles of Exercise For Health and Fitness: © 2014 Pearson Education, IncmichelleBelum ada peringkat
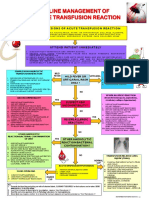
- Transfusion Reaction PDFDokumen1 halamanTransfusion Reaction PDFKah Man GohBelum ada peringkat