First Aid Pharmacology Antimicrobials
Diunggah oleh
Laura Lopez RocaDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
First Aid Pharmacology Antimicrobials
Diunggah oleh
Laura Lopez RocaHak Cipta:
Format Tersedia
Flash cards by Seetal K. Dhaliwal H.
S
Section V
1
Antimicrobial therapy:
Mechanism of Action Drugs
Block cell wall synthesis by inhibition of
peptidoglycan cross-linking
Penicillin, ampicillin, ticarcillin, piperacillin, imipenam,
aztreonam, cephalosporins.
Block peptidoglycan synthesis Bacitracin, vancomycin
Disrupt bacterial cell membrane Polymyxins
Block nucleotides synthesis Sulfonamides, trimethoprim
Block DNA topoisomerase Fluoroquinolones
Block mRNA synthesis Rifampin
Block protein synthesis at 50S ribosomal Chloramphenicol, Macrolides, Clindamycin, Linezolid,
Streptogamins (quinupristin, dalfopristin)
Block protein synthesis at 30S ribosomal Aminoglycosides, Tetracyclines
Bacteriostatic Erythromycin, Clindamycin, Sulfamethoxazole,
Trimethoprim, Tetracyclines, Chloramphenicol.
Bactericidal Vancomycin, Fluoroquinolones, Penicillin,
Aminoglycosides, Cephalosporins, Metronidazole.
ECSTaTiC
bacteriostatics.
Very Finely Proficient
At Cell Murder
2
2
Penicillins:
Penicillin G (IV) and Penicillin V (oral):
Binds PBP, blocks transpeptidase of cell wall cross-linking, activate autolytic enzymes.
Bactericidal for gram postive cocci and rods & gram negative cocci and spirochetes.
-lactamase sensitive. May cause hypersensitivity reactions & Hemolytic anemia.
Methicillin, Nafcillin, Dicloxacillin (penicillinase-resistant penicillins):
Narrow spectrum. -lactamase resistant due to heavier R group.
Used for S. aureus (except MRSA due to altered PBP site); Use Naf for Staph
May cause hypersensitivity reactions; methicillin interstitial nephritis.
Ampicillin, Amoxicillin (aminopenicillins):
Broad spectrum (-lactamase sensitive); Clavulanic acid/Sulbactam (penicillinase inhibitor)
enhances spectrum. AmOxicillin has greater Oral bioavailability than ampicillin.
Used in some gram positive bacteria & gram neg rods H. pylori (amoxicillin), H. influenzae, E.
coli, Listeria monocytogenes (ampicillin), Proteus mirabilis, Salmonella, enterococci & Borrelia
(amoxicillin); Ampicillin/Amoxicillin HHELPS kill enterococci & Borrelia
May cause hypersensitivity reactions, rash or pseudomembranous colitis.
Ticarcillin, carbenicillin, piperacillin (antipseudomonals):
Extended spectrum; TCP takes care of Pseudomonas; Used to kill Pseudomonas spp., and gram
neg rods; -lactamase sensitive use with clavulanic acid. Synergistic with aminoglycosides.
3
3
Cephalosporins:
1
st
generation (cefazolin, cephalexin) PEcK:
Gram positive cocci, Proteus mirabillis, E. coli, Klebsiella pneumoniae.
2
nd
generation (cefoxitin, cefaclor, cefuroxime) HEN PEcKS:
Gram positive cocci, H. influenzae, Enterobacter aerogenes, Neisseria spp., Proteus
mirabillis, E. coli, Klebsiella pneumoniae, Serratia marcescens.
3
rd
generation (ceftriaxone, cefotaxime, ceftazidime):
Serious gram neg infections; meningitis (penetrates BBB); ceftazidine pseudomonas;
ceftriaxone gonorrhea.
:
Activity against organisms.
Toxicity:
Hypersensitivity reactions. Cross hypersensitivity with penicillins (in 5 10%).
nephrotoxicity of aminoglycosides; disulfiram-like reaction with ethanol (in
cephalosporins with a methylthiotetrazole group i.e. cefamandole)
-lactam drugs that inhibit cell wall
synthesis but are less susceptible to
penicillinase. Bactericidal.
4
Aztreonam:
MOA: same as penicillin &
cephalosporins.
Resistant to -lactamase. No cross
allergenicity with penicillins.
Used for gram neg rods Klebsiella
spp., Pseudomonas spp., Seratia spp.
No activity against gram positive or
anaerobes.
For penicillin-allergic patients & those
with renal insufficiency who cannot
tolerate aminoglycosides.
Toxicity:
Usually nontoxic; occasionally GI
upset. No cross sensitivity with
penicillins or cephalosporins.
Imipenem/cilastin, meropenem:
MOA: same as penicillin &
cephalosporins.
Resistant to -lactamase (carbapenem).
Imipenem is broad spectrum:
Administered with ciLASTIN to
inactivation in renal tubules.
Used for gram positive cocci, gram ned
rods, & anaerobes. DOC for
Enterobacter.
The significant side effects limit use to
life threatening infections, or after drugs
have failed. Meropenem, however, has
reduced risk of seizures & is stable to
dihydropeptidase I.
Toxicity:
GI distress, skin rash, & CNS toxicity
(seizures) at high plasma levels.
With Imipenem, the kill is LASTIN with ciLASTIN.
5
Vancomycin:
MOA: inhibits cell wall mucopeptide
formation by binding D-ala D-ala.
Resistance occurs when aa change from
D-ala D-ala to D-ala D-lac.
Used for serious, gram-positive multi-
drug resistant organisms;
S. aureus, C. difficile -
pseudomembranous colitis.
Toxicity:
Nephrotoxicity, Ototoxicity,
Thrombophlebitis, diffuse flushing
red man syndrome (can large
prevent by pretreatment with
antihistamines and slow infusion rate).
Well tolerated in general does NOT
have many problems.
Protein synthesis
inhibitors:
Buy AT 30, CCELL (sell) at 50
30S inhibitors:
Aminoglycosides (bactericidal)
Tetracycline (bacteriostatic)
50S inhibitors:
Chloramphenicol, Clindamycin
(bacteriostatic)
Erythromycin & other macrolides
(bacteriostatic)
Lincomycin (bacteriostatic)
Linezolid (variable)
6
Aminoglycosides:
Gentamicin, Neomycin, Amikacin, Tobramycin, Streptomycin bactericical.
Inhibits formation of initiation complex & cause misreading of mRNA. Require O2
for uptake cannot kill anaerobes Mean GNATS canNOT kill anaerobes
Used for severe gram neg rod infections. Synergistic with -lactam antibiotics.
Neomycin for bowel surgery.
Nephrotoxicity (especially when used with cephalosporins). Ototoxicity (especially
when used with loop diuretics). Terotogen.
Macrolides:
Erythromycin, Azithromycin, Clarithromycin bacteriostatic.
Inhibits protein synthesis by blocking translocation; bind to the 23 rRNA of the
50S ribosomal subunit.
Used for URIs, pneumonias, STDs gram positive cocci, Mycoplasma, Legionella,
Chlamydia, Neisseria.
Prolonged QT interval (especially erythromycin), GI discomfort (most common
cause of noncompliance), acute cholestatic hepatitis, eosinophilia, skin rashes.
Increases serum concentration of theophyllines, oral anticoagulants.
7
7
Tetracyclines:
Tetracycline, doxycycline, democlocycline, minocycline.
Binds 30S & prevents attachment of aminoacyl-tRNA; limited CNS
penetration. Doxycycline is fecally eliminated & is safe in renal failure
patients. Must NOT take with milk, antacids, or iron-containing preparations
because divalent cations inhibit absorption in gut.
Used in Vibrio cholerae, Acne, Chlamydia, Ureaplasma Urealyticum,
Mycoplasma pneumoniae, Tularemia, H. pylori, Borrelia burdorferi (Lyme
disease) & Ricketssia.
Toxicity:
GI distress, dicoloration of teeth & inhibition of bone growth in children,
photosensitivity.
Contraindicated in pregnancy.
VACUUM The BedRoom.
8
Chloramphenicol:
Inhibits 50S
peptidlytransferase.
Used in meningitis (H.
influenzae, N. meningitidis, S.
pneumoniae).
Conservative owing to toxicities.
Toxicity:
Anemia (dose dependent), aplastic
anemia (dose dependent), gray
baby syndrome (in preemies due to
lack of liver UDP-glucuronyl
transferase)
Clindamycin:
Blocks peptide bond
formation at 50S subunit.
Treats anaerobes above the
diaphragm Bacteroides
fragilis, Clostridium
perfringens.
Toxicity:
Pseudomembranous colitis (C.
difficile overgrowth), fever,
diarrhea.
9
Sulfonamides:
Sulfamethoxazole (SMX),
sulfisoxazole, sulfadiazine.
PABA antimetabolites inhibit
dihydropteroate synthetase.
Used in gram positive, gram neg,
Nocardia, Chlamydia. Triple Sulfas
or SMX for simple UTI.
Toxicity:
Hypersensitive reactions, hemolysis if
G6PD deficiency, nephrotoxicity
(tubointerstitial nephritis),
photosensitivity, kernicterus, displace
other drugs from albumin (i.e.
warfarin)
Trimethoprim:
Inhibits bacterial dihydrofolate
reductase.
Used with sulfonamides (TMP-
SMX), causing sequential block of
folate synthesis.
Combination used for recurrent
UTIs, Shigella, Salmonella,
Pneumocystis jiroveci pneumonia.
TMP Treats Marrow Poorly
Toxicity:
Megaloblastic anemia,
leukopenia, granulocytopenia.
May alleviate with supplemental
folinic acid.
10
Fluoroquinolones:
Ciprofloxacin, norfloxacin, ofloxacin, sparfloxacin, moxifloxacin, gatifloxacin,
enoxacin & nalidic acid (a quinolone).
Used for gram neg rods of urinary and GI tracts (including Pseudomonas),
Neisseria, & some gram positive organisms.
Toxicity:
GI upset, superinfections, skin rashes, headache, dizziness. Contraindicated in
pregnancy & children damages cartilage. Tendonitis & tendon rupture in adults, leg
cramps & myalgia in kids.
Inhibit DNA gyrase
(topoisimerase II). Must not be
taken with antacids. Bactericidal.
FluoroquinoLONES hurt your BONES
Metronidazol:
Treats Giardia, Entamoeba, Trichomonas, Gardenella vaginalis, Anaerobes
(Bacteriodes, Clostridium). Used with bismuth & amoxicillin (or tetracycline) for
triple therapy of H. Pylori.
Toxicity:
Disulfiram-like reaction with alcohol; headache, metallic taste.
Forms toxic metabolites in bacterial cell that damage DNA.
Bactericidal & antiprotozoal.
GAP METRO
11
Polymixins:
Bind to cell membrane of bacteria & disrupt their osmotic properties. Polymyxins
are cationic, basic proteins that act like detergents.
Used for resistant gram negative infections.
Toxicity:
Neurotoxicity, acute renal tubular necrosis.
Polymyxin B, polymyxin E.
MYXins MIX up membranes.
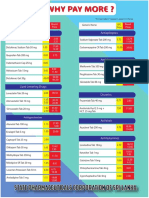
Antimicrobial drugs:
Bacterium Prophylaxis Treatment
M. tuberculosis Isoniazid ifampin, soniazid, yrazinamide,
thambutol ( for treatment)
M. avium-intracellulare Azithromycin Azithromycin, rifampin, ethambutol,
streptomycin
M. leprae NA Dapsone, rifampin, clofazimine
12
Anti-TB drugs
INH-SPIRE (inspire):
Isoniazid (INH), Streptomycin, Pyrazinamide, Rifampin, Ethambutol.
Cycloserine (2
nd
line therapy)
Ethambutol optic neuropathy (red-green color blindness). For other drugs
hepatotoxicity.
Isoniazid (INH): Injures Neurons & Hepatocytes
Synthesis of mycolic acids.
Causes neurotoxicity & hepatotoxicity. Pyridoxine (Vit B
6
) prevents neurotoxicity.
Rifampin:
Inhibits DNA-dependent RNA polymerase.
Delays resistant to dapsone when used for leprosy. Used for meningococcal
prophylaxis & chemoprophylaxis in contacts of children with Haemophilus influenzae
type B.
Minor hepatotoxicity & drug interactions ( CYP450); orange body fluids
(nonhazardous side effect).
Rifampins 4 Rs:
RNA polymerase inhibitor
Revs up microsomal P-450
Red/Orange body fluids
Rapid resistance if used alone
13
Antifungal therapy:
14
Amphotericin B:
Binds ergosterol (unique to fungi); forms membrane pores that allow leakage of
electrolytes.
Used for Cryptococcus, Blactomyces, Coccidioides, Aspergillus, Histoplasma,
Candida, Mucor (systemic mycoses). Intrathecally for fungal meningitis; does not
cross BBB.
May cause fever/chills (shake & bake), hypotension, nephrotoxicity,
arrhythymias, anemia, IV phlebitis (amphoterrible). Hydration reduces
nephrotoxicity. Liposomal amphotericin reduces toxicity.
Nystatin:
Binds ergosterol disrupting fungal membranes. Too toxic for systemic use.
Swish and swallow for oral Candidiasis (thrush); topical for diaper rash or
vaginal candidiasis.
15
15
Azoles:
Inhibits fungal sterol (ergosterol) synthesis.
Used for systemic mycoses. Fluconazole for Cryptococcal meningitis in AIDS
(can cross BBB), & candidal infections of all types (i.e. yeast infections).
Ketoconazole for Blastomyces, Coccidioides, Histoplasma, Candida albicans;
hypercortisolisms. Clotrimoxazole & miconazole for topical fungal infections.
Toxicity causes hormone synthesis inhibition (gynecomastia), liver dysfunction
(inhibits CYP450), fever, chills.
Flucytosine:
Inhibits DNA synthesis by conversion to 5-fluorouracil.
Used in systemic fungal infections (candidiasis, cryptococcus) in combination with
amphotericin B.
Causes nausea, vomiting, diarrhea and bone marrow suppresion.
16
16
Terbinafine:
Inhibits fungal enzyme squalene epoxidase.
Used to treat dermatophytoses (especially onychomycosis).
Caspofungin:
Inhibits cell wall synthesis by inhibiting synthesis of -glucan.
Used to treat invasive aspergillosis.
Causes GI upset, flushing.
Griseofulvin:
Interferes with microtubule function; disrupts mitosis. Deposits in keratin-containing
tissues (nails).
Oral treatment of superficial infections; inhibits growth of dermatophytes (tinea,
ringworm).
Teratogenic, carcinogenic, confusion, headaches, CYP450 & warfarin metabolism.
17
17
Antiviral Chemotherapy:
18
Amantadine:
Blocks viral penetration/uncoating (M2 protein); may buffer pH of endosome. Also
causes the release of DA from intact nerve terminals.
Prophylaxis & treatment of Influenza A; Parkinsons disease.
Toxicity ataxia, dizziness, slurred speech.
Mutated M2 protein. 90% of all influenza A strains are resistant to amantadine, so
not used.
Amantadine blocks influenza A & rubellA & causes problems with the cerebellA.
Rimantidine is a derivative with fewer side effects. Does not cross BBB.
Zanamivir, oseltamivir:
Inhibits Influenza neuraminidase, decreasing the release of progeny virus.
Treatment of both Influenza A and B.
19
Acyclovir:
Monophosphorylated by HSV/VZV thymidine kinase. Guanosine analog.
Triphosphate formed by cellular enzymes. Preferentially inhibits viral DNA
polymerase by chain termination.
Used for HSV, VZV, EBV, HSV-induced mucocutaneous & genital lesions as well as
for encephalitis. Prophylaxis in immunocompromised patients. For herpes zoster,
use famciclovir. No effects on latent forms of HSV and VZV.
Generally well tolerated. Resistance develops when lack thymidine kinase.
Ribavirin:
Inhibits synthesis of guanine nucleotides by competitively inhibiting IMP
dehydrogenase.
Used for RSV & chronic Hepatitis C.
Causes hemolytic anemia. Severe teratogen.
20
Ganciclovir:
5-monophosphate formed by a CMV viral kinase of HSV/VZV thymidine kinase.
Guanosine analog. Triphosphate formed by cellular kinases. Preferentially inhibits
viral DNA polymerase.
Used for CMV, especially in immunocompromised patients.
Toxicity leukopenia, neutropenia, thrombocytopenia, renal toxicity. More toxic to
host enzymes than acyclovir.
Resistance develops if mutated CMV DNA polymerase of lack viral kinase.
Foscarnet:
Viral DNA polymerase inhibitor that binds pyrophosphate-bindinig site of the
enzyme. Does not require activation by viral kinase.
Used for CMV retinitis in immunocompromised patients when Ganciclovir fails &
for acyclovir-resistant HSV.
Causes nephrotoxicity.
Resistance develops with mutated DNA polymerase.
21
HIV therapy:
Protease Inhibitors:
Saquinavir, ritonavir, indinavir, nelfinavir, amprenavir.
Toxicity GI intolerance (nausea, diarrhea), hyperglycemia, lipodystrophy, thromocytopenia
(indinavir).
Reverse transcriptase inhibitors:
Nucleosides (Zidovudine [ZDV/AZT], didanosine [ddI], zalcitabine [ddC], stavudine [d4T],
lamivudine [3TC], abacavir): Have you dined (vudine) with my nuclear (nucleosides) family?
Non-nucleosides (Nevirapine, Efavirenz, Delavirdine): Never Ever Deliver nucleosides.
Toxicity: bone marrow suppression (neutropenia, anemia), peripheral neuropathy, lactic acidosis
(nucleosides), rash (non-nucleosides), megaloblastic anemia (ZDV), pancreatitis (ddI). GM-CSF &
erythropoietin can be used to reduce bone marrow suppression.
Part of HAART. Used when CD4 <500 cells/mm
3
or high viral load. ZDV as prophylaxis during
pregnancy to reduce fetal transmission.
Fusion inhibitors: ENFUVIRTIDE
Binds gp41, inhibits fusion with CD4 cells.
Toxicity: hypersensitivity reactions, reactions at SC injection site, risk bacterial pneumonia.
Used in persistent viral replication infections despite antiretroviral therapy and in combination
with other drugs.
22
22
Interferons:
Glycoproteins from human leukocytes that block various stages of viral RNA & DNA
synthesis. Induce ribonuclease that degrades viral mRNA.
IFN- chronic Hepatis B & C, and Kaposis sarcoma;
IFN- MS;
IFN- NADPH oxidase deficiency.
Toxicity: Neutropenia
Antibiotics to avoid in pregnancy:
Sulfonamides kernicterus
Aminoglycosides ototoxicity
Fluoroquinolones cartilage damage
Erythromycin acute cholestatic hepatitis in moms (and
clarithromycin embryotoxic)
Metronidazole mutagenesis
Tetracycline discolored teeth & inhibition of bone growth
Ribavirin teratogenic
Griseofulvin teratogenic
Chloramphenicol gray baby
SAFE Moms Take
Really Good Care
23
23
Anda mungkin juga menyukai
- AntimicrobialsDokumen1 halamanAntimicrobialsRomaine Barrett100% (1)
- First Aid PharmacoDokumen61 halamanFirst Aid PharmacogirBelum ada peringkat
- Pharmacology - Chapter 29Dokumen5 halamanPharmacology - Chapter 29Ashley-Michelle LewisBelum ada peringkat
- Brenner and Stevens, Pharmacology 3 © 2010Dokumen5 halamanBrenner and Stevens, Pharmacology 3 © 2010PharAwayBelum ada peringkat
- DRUG of CHOICE - InfectiousDokumen1 halamanDRUG of CHOICE - InfectiousJoseph De JoyaBelum ada peringkat
- Medical Topics SpreadsheetDokumen53 halamanMedical Topics SpreadsheetIman AhmedBelum ada peringkat
- Mechanism of Action For Each Class of AntiDokumen146 halamanMechanism of Action For Each Class of AntiReynaldo RiveraBelum ada peringkat
- ChemotherapyDokumen11 halamanChemotherapyNedaAbdullahBelum ada peringkat
- Anti-Viral Drugs AltDokumen42 halamanAnti-Viral Drugs AltSidraBelum ada peringkat
- (Immunology) First Aid For The USMLE Step 1 2020, Thirtieth Edition-1 PDFDokumen29 halaman(Immunology) First Aid For The USMLE Step 1 2020, Thirtieth Edition-1 PDFFabian Peña MolinaBelum ada peringkat
- Antibiotics 9Dokumen11 halamanAntibiotics 9Beth Morales100% (1)
- USMLE 100 Essential DrugsDokumen15 halamanUSMLE 100 Essential DrugsAnnTranBelum ada peringkat
- Lippin NotesDokumen8 halamanLippin Noteswalt65100% (1)
- USMLE Step 1 DrugsDokumen36 halamanUSMLE Step 1 DrugscougardiverBelum ada peringkat
- USMLE STEP 1 CHECKLIST @lifeinwhitecoatDokumen23 halamanUSMLE STEP 1 CHECKLIST @lifeinwhitecoatGlorivy E. Mora Gonzalez100% (3)
- Immunosuppressants - AMBOSS PDFDokumen7 halamanImmunosuppressants - AMBOSS PDFOpio IsaacBelum ada peringkat
- Sketchy WordDokumen9 halamanSketchy WordPäw Yusoph100% (1)
- Anti FungalsDokumen5 halamanAnti FungalskakuBelum ada peringkat
- DR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDokumen1 halamanDR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDr Kumar Ponnusamy100% (1)
- Usmle Step 1 Terms ResumeDokumen16 halamanUsmle Step 1 Terms ResumeJorge Luis LopezBelum ada peringkat
- Exam 1 DiseasesDokumen1 halamanExam 1 DiseasesSolomon Seth SallforsBelum ada peringkat
- SketchyMicro Antibiotics NotesDokumen2 halamanSketchyMicro Antibiotics NotesUsama BilalBelum ada peringkat
- Ahmed Samir - Step 1 Experience - 251Dokumen16 halamanAhmed Samir - Step 1 Experience - 251Mohamed LoaiBelum ada peringkat
- Cancer Drugs Drugs Indication Adverse Effects Interaction and ContraindicationDokumen5 halamanCancer Drugs Drugs Indication Adverse Effects Interaction and ContraindicationOndari gisemba OSINDEBelum ada peringkat
- WWW Cram Com Flashcards Hematology Slides 872178Dokumen8 halamanWWW Cram Com Flashcards Hematology Slides 872178Anonymous t5TDwdBelum ada peringkat
- (8!5!13) Cell Injury OutlineDokumen9 halaman(8!5!13) Cell Injury OutlineBhumiShahBelum ada peringkat
- HematologyDokumen182 halamanHematologyXimena GómezBelum ada peringkat
- Abx FinalDokumen3 halamanAbx Finalyanks1120Belum ada peringkat
- Workbook of BiochemDokumen22 halamanWorkbook of BiochemMedStudent MedStudentBelum ada peringkat
- Sketchy PharmDokumen4 halamanSketchy Pharmsumaiya100% (1)
- New Drugs 2019: New Drug Mechanism of Action UseDokumen6 halamanNew Drugs 2019: New Drug Mechanism of Action Userameez qureshiBelum ada peringkat
- Antibiotics in ActionDokumen1 halamanAntibiotics in Actionjuan esteban MonroyBelum ada peringkat
- Drug AllergyDokumen61 halamanDrug Allergyadysti100% (1)
- For PublicDokumen6 halamanFor PublicMOHAMAD ZAHIN HAFIZ BIN ZULKIPLEBelum ada peringkat
- Glomerulonephritis Cheat Sheet PDFDokumen1 halamanGlomerulonephritis Cheat Sheet PDFAnonymous aA9Ol6239Belum ada peringkat
- Medical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Dokumen377 halamanMedical Boards Step 2 Made Ridiculously Simple (Medicalstudyzone - Com)Benyamin KhalevBelum ada peringkat
- Antibiotic Sensitivity FINAL V4 Sheet1Dokumen1 halamanAntibiotic Sensitivity FINAL V4 Sheet1JHBelum ada peringkat
- NERVOUS MnemonicsDokumen4 halamanNERVOUS MnemonicsHimBelum ada peringkat
- Pharma FinalADokumen33 halamanPharma FinalAvaegmundigBelum ada peringkat
- Quinolones, Folic Acid Antagonist and Urinary Tract Antitb and LeprosyDokumen124 halamanQuinolones, Folic Acid Antagonist and Urinary Tract Antitb and LeprosyrenBelum ada peringkat
- Recalls File Collected PDFDokumen111 halamanRecalls File Collected PDFKC PalattaoBelum ada peringkat
- Pharmayield: Must Know Pharmacology NotesDokumen2 halamanPharmayield: Must Know Pharmacology NotesBianca Desiree VergaraBelum ada peringkat
- Pharm TableDokumen35 halamanPharm TableHannah BaldwinBelum ada peringkat
- HY Endocrine UsmleDokumen22 halamanHY Endocrine UsmleNakhal JararBelum ada peringkat
- Microbiology (Notes From Uworld)Dokumen2 halamanMicrobiology (Notes From Uworld)Nanda MinndinBelum ada peringkat
- Step 1 DrugsDokumen46 halamanStep 1 DrugsZebram ZeeBelum ada peringkat
- +++++great Review Path Notes & Pics+++++Dokumen430 halaman+++++great Review Path Notes & Pics+++++patriciacafBelum ada peringkat
- Hematology & Oncology FirecrackerDokumen91 halamanHematology & Oncology FirecrackerMiri PravdaBelum ada peringkat
- Chart Antibacterial Drugs PDFDokumen1 halamanChart Antibacterial Drugs PDFMunaf AlsumaryBelum ada peringkat
- Viruses NonlivingDokumen6 halamanViruses NonlivingKirat SinghBelum ada peringkat
- AntibioticsDokumen2 halamanAntibioticsPGI Custodio, Ed KristianBelum ada peringkat
- Antibiotic GuideDokumen6 halamanAntibiotic GuideAnnTran100% (1)
- Sketchy Pharm RuntimesDokumen5 halamanSketchy Pharm RuntimesBerkay ArslanBelum ada peringkat
- Bacteria PDFDokumen13 halamanBacteria PDFJohn Christopher LucesBelum ada peringkat
- USMLE Flashcards: Microbiology and Immunology - Side by SideDokumen196 halamanUSMLE Flashcards: Microbiology and Immunology - Side by SideMedSchoolStuff0% (1)
- Zanki (Complete) + R/medicalschoolanki Microbiology ErrataDokumen70 halamanZanki (Complete) + R/medicalschoolanki Microbiology ErrataedBelum ada peringkat
- EKG ExamplesDokumen9 halamanEKG ExamplesMayer Rosenberg99% (235)
- Next Step in Management 2014 - CCS Step3 PreviewDokumen72 halamanNext Step in Management 2014 - CCS Step3 PreviewLaura Lopez RocaBelum ada peringkat
- Psych NotesDokumen3 halamanPsych NotesLaura Lopez RocaBelum ada peringkat
- Cardio Step 3 Review MTB3Dokumen6 halamanCardio Step 3 Review MTB3Laura Lopez RocaBelum ada peringkat
- Obgyn Notes Uwise QbankDokumen11 halamanObgyn Notes Uwise QbankLaura Lopez Roca0% (1)
- Medical AbbreviationsDokumen4 halamanMedical AbbreviationsNelly PaniaguaBelum ada peringkat
- Case Presentation Uterine MyomaDokumen22 halamanCase Presentation Uterine MyomaLaura Lopez RocaBelum ada peringkat
- Neuro Images Step1Dokumen46 halamanNeuro Images Step1Laura Lopez Roca100% (2)
- Neuro Images Step1Dokumen44 halamanNeuro Images Step1Laura Lopez Roca83% (6)
- Obgyn UWISE Notes (And Master The Boards)Dokumen8 halamanObgyn UWISE Notes (And Master The Boards)Laura Lopez Roca100% (5)
- Anato Head and Neck MnemonicsDokumen10 halamanAnato Head and Neck MnemonicsLaura Lopez RocaBelum ada peringkat
- NBME Forms (Images, Photos)Dokumen120 halamanNBME Forms (Images, Photos)Laura Lopez Roca100% (7)
- Anato Head and Neck MnemonicsDokumen10 halamanAnato Head and Neck MnemonicsLaura Lopez RocaBelum ada peringkat
- Second Aid - USMLE MnemonicsDokumen21 halamanSecond Aid - USMLE MnemonicsKgerbBelum ada peringkat
- Pharmacology - 4 Inflamatory and RelatedDokumen25 halamanPharmacology - 4 Inflamatory and RelatedLaura Lopez RocaBelum ada peringkat
- Medicine Price List MPL Acute and Chronic November 2020Dokumen123 halamanMedicine Price List MPL Acute and Chronic November 2020karar hussainBelum ada peringkat
- Introduction To Health Psychology 2022Dokumen721 halamanIntroduction To Health Psychology 2022Brain Smith100% (4)
- Strengthening The Quality Agenda in Health Care in Low-And Middle-Income Countries: Questions To ConsiderDokumen5 halamanStrengthening The Quality Agenda in Health Care in Low-And Middle-Income Countries: Questions To ConsiderJose RamirezBelum ada peringkat
- Medicines & Supplies: FebruaryDokumen85 halamanMedicines & Supplies: FebruaryPharmacy DeamhiBelum ada peringkat
- Final Report SampleDokumen42 halamanFinal Report SampleVenkata VihariBelum ada peringkat
- Eng PDFDokumen302 halamanEng PDFAnonymous YdFUaW6fBBelum ada peringkat
- Formularium Obat Viva Generik Kebraon: AntibiotikDokumen8 halamanFormularium Obat Viva Generik Kebraon: AntibiotikLahar SatryaBelum ada peringkat
- ED Produk KF - KF (Nama Apotek)Dokumen19 halamanED Produk KF - KF (Nama Apotek)Eko FebryandiBelum ada peringkat
- Ebook PDF We The People Full Twelfth Edition 12th Edition PDFDokumen41 halamanEbook PDF We The People Full Twelfth Edition 12th Edition PDFdale.brinkman835100% (36)
- HPN DM RegistryDokumen9 halamanHPN DM RegistryBorbe ClauBelum ada peringkat
- WHOPIR - PT SANBE13 17february2017Dokumen17 halamanWHOPIR - PT SANBE13 17february2017Shoaib BiradarBelum ada peringkat
- Managing Epidemics Interactive 1 260 11Dokumen1 halamanManaging Epidemics Interactive 1 260 11Pankaj GautamBelum ada peringkat
- Doze AntibioticeDokumen6 halamanDoze AntibioticeMocanu Cristina-Viorica100% (1)
- Fortified Drops Chart A4 Modified 1pdfpdf 2Dokumen1 halamanFortified Drops Chart A4 Modified 1pdfpdf 2Rubén SepúlvedaBelum ada peringkat
- Health: Quarter 1 - Module 1: Community and Environmental HealthDokumen24 halamanHealth: Quarter 1 - Module 1: Community and Environmental Healthma kathrine cecille macapagal100% (1)
- Who Pen 2020Dokumen85 halamanWho Pen 2020Faye PalmaresBelum ada peringkat
- MEDICAMENTEDokumen13 halamanMEDICAMENTELily Ozunu100% (1)
- Price ComparisonDokumen2 halamanPrice ComparisonSurin AthukoralaBelum ada peringkat
- Leprosy Summary of MedsDokumen1 halamanLeprosy Summary of MedsNikki LegaspiBelum ada peringkat
- Reflection Paper Write A Short Reflection On The Topic. "How Does Global Migration Benefit The Philippines? Will Your Answer Be The Same On Account of The New Development On COVID-19 Pandemic?Dokumen4 halamanReflection Paper Write A Short Reflection On The Topic. "How Does Global Migration Benefit The Philippines? Will Your Answer Be The Same On Account of The New Development On COVID-19 Pandemic?bjihuhBelum ada peringkat
- WHO Systems Thinking 9789241563895 - EngDokumen112 halamanWHO Systems Thinking 9789241563895 - EngCraig Dalton100% (1)
- Thank You!: MUN Manifesto! We Hope You Will Find This A Helpful andDokumen55 halamanThank You!: MUN Manifesto! We Hope You Will Find This A Helpful andAbdulahi MaxamedBelum ada peringkat
- Visitor Health Declaration FormDokumen1 halamanVisitor Health Declaration FormHung Kwan1 KeungBelum ada peringkat
- Pharma LE5Dokumen35 halamanPharma LE5MOHANTA, deviprasadBelum ada peringkat
- Faktur AM-4-1-2-1-1-1-1Dokumen242 halamanFaktur AM-4-1-2-1-1-1-1ZaenuriBelum ada peringkat
- Pharm II Exam 1 - Abx I HintsDokumen3 halamanPharm II Exam 1 - Abx I HintsNhung NguyenBelum ada peringkat
- 5 New Code of Ethics For Nurses August 2008Dokumen11 halaman5 New Code of Ethics For Nurses August 2008Lucinda JaneBelum ada peringkat
- WHOCC - List of DDDs Combined Products 2013Dokumen7 halamanWHOCC - List of DDDs Combined Products 2013blancaBelum ada peringkat
- W.H.O. Murdered Africa by Dr. William Campbell DouglasDokumen20 halamanW.H.O. Murdered Africa by Dr. William Campbell DouglasJohn Burns100% (4)
- Genericsking Trading Inc Ampules Vials 1 WholesaleDokumen12 halamanGenericsking Trading Inc Ampules Vials 1 Wholesaleapi-276695824Belum ada peringkat