Newborn DisordersI
Diunggah oleh
nicewan0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
31 tayangan23 halamannb
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Ininb
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
31 tayangan23 halamanNewborn DisordersI
Diunggah oleh
nicewannb
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 23
Newborn Disorders
Common Abnormal Conditions in the
Neonatal Period
Outline
Sepsis Neonatorum
Respiratory Distress Syndrome
Transient Tachypnea of the Newborn
Meconium Aspiration
Perinatal Asphyxia
Hypoxic Ischemic Encephalopathy
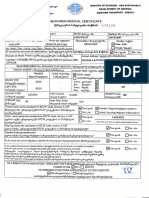
NBS in the Philippines
Neonatal Infectious Disease
Sepsis neonatorum
Early onset versus Late onset
Bacterial, Fungal
Viral - Toxoplasmosis, Rubella, CMV,
Hepatitis,Enteroviruses
Early onset sepsis
90% symptomatic w/in 24 hours of
life
Risk factors : maternal GBS infection, PROM
>18 hours, chorioamnionitis, maternal fever
>38C; prematurity, LBW <2500g
Clinical presentation varied
MC is respiratory distress
EOS : maternal flora
LOS : nosocomial, CA
In preterm infants : MC in LBW
CONS, S. aureus, Entero., Kleb,
etc
Evaluation
Complete PE
Labs : Blood CS, CBC APC, Na, K, CSF, CXR,
APL, etc
Treatment
Broad spectrum antibiotic coverage
Empiric
Definitive
Length of treatment course:
organism, response of patient
7-14 (21 days)
Supportive treatment : mechanical
ventilation, volume and pressor
support
Other medications ie bicarbonate, Pb
Risk Factors for LOS
In Infants <1500 grams :
BW <750 grams
Presence of CVC
Delayed enteral feeds
Prolonged hyperalimentation
Mechanical ventilation
Complications of Prematurity PDA, BPD, NEC
Anaerobic Infections
In the Phil : Neonatal tetanus
Cl. Tetani; WHO est 59,000
deaths due to neonatal tetanus
(2008)
Hypertonia, muscle spasms,
inability to feed, dehydration
Treatment : Tet toxoid 500 U IM
Pen G 100-300,000 U/kg/day 10-
14 days
Supportive care : MV
Requires standard tetanus
immunizations after recovery
Fungal infections
Candidiasis : C. albicans
Oral : Nystatin oral, Gentian violet,
Miconazole
NICU : Fluconazole
Invasive : brain, renal UTZ; eye check
up
Viral and Other Infectious Etiologies
Vertical transmission : Congenital vs
Perinatal infections
Maternal History
Complete PE
Laboratory evaluations
Serology
Imaging modalities
Congenital Toxoplasmosis
4 Recognized patterns
1. Subclinical
2. Neonatal symptomatic disease
3. Delayed onset
4. Sequelae or Relapse in infancy
through adolescence of a previously
undiagnosed infection
Specific symptoms
Neurologic
Ophthalmologic
Organomegaly
Hyperbilirubinemia, persistent conjugated
Thrombocytopenia
Rash
Rare : erythroblastosis fetalis, hydrops,
myocarditis, pneumonitis, nephritis
Diagnosis
Serology : IgM, IgA
PCR
Histology
Isolation of parasite : T. gondii is an
obligate intracellular protozoan. Cats are the only
hosts.
CT w/o contrast : calcifications
Treatment
Pyrimethamine
Sulfadiazine
Prednisone
Long term ( through 1 year old )
Survival for those not severely afflicted
CMV
DS enveloped DNA virus
Lifelong infection
Herpesvirus family
Abundant cytoplasm with
intranuclear and cytoplasmic
inclusions
Present in all secretions
CMV more common in HIV-1 disease
Congenital early symptomatic :
fulminant
multi-organ involvement, blueberry muffin spots
preterm, IUGR, jaundiced; microcephaly, calcifications
developmental disabilities, hearing loss
neurologic disabilities
Asymptomatic congenital : developmental
disabilities, deafness, dental defects
Perinatal acquired CMV
1. intrapartum exposure in the maternal genital
tract
2. postnatal exposure to infected BM
3. postnatal exposure to infected blood
4. nosocomial via urine or saliva
Preterm infants are at greater risk to develop
acute infection
CMV pneumonitis
Transfusion acquired CMV
4-12 weeks post transfusion
must use CMV seronegative donors
filtered, leucoreduced
Diagnosis
CMV PCR
CMV IgG and IgM
CMV antigen, shell vial
Treatment : Ganciclovir,
Valganciclovir
Read on the other Neonatal
infections :
HIV
Hepatitis
TB
Source : Nelson, Del Mundo
THANK YOU AND GOOD DAY
Anda mungkin juga menyukai
- Foundations For Clinical Mental Health Counseling - 3rd EditionDokumen369 halamanFoundations For Clinical Mental Health Counseling - 3rd EditionJamie Finotti100% (7)
- Week 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20Dokumen32 halamanWeek 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20maha abdallahBelum ada peringkat
- CPT CODING Power PointDokumen24 halamanCPT CODING Power PointJack100% (1)
- Congenital Viral InfectionsDokumen43 halamanCongenital Viral Infectionsannie1970100% (1)
- Neonatal Sepsis 2019.Dokumen6 halamanNeonatal Sepsis 2019.Jean Paúl LópezBelum ada peringkat
- Kırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisDokumen40 halamanKırşehir Ahi Evran Üniversitesi Sağlık Bilimleri Enstitüsü: Neonatal Sepsis & MeningitisAli FalihBelum ada peringkat
- Meningitis in Children 1204809002482509 3Dokumen48 halamanMeningitis in Children 1204809002482509 3Ali FalihBelum ada peringkat
- Torch Infection: Reporter: Zhao Meiling (Alice) Date: April.10.2019Dokumen35 halamanTorch Infection: Reporter: Zhao Meiling (Alice) Date: April.10.2019Hilary WangBelum ada peringkat
- Conduct Effective Quantitative Risk Assessment (QRA) - StepsDokumen14 halamanConduct Effective Quantitative Risk Assessment (QRA) - Stepsamal118Belum ada peringkat
- Neonatal InfectionDokumen18 halamanNeonatal InfectionchinchuBelum ada peringkat
- ROO M General Data Admitt Ing DX Worki NG DX Laboratory Frichmond MedicationsDokumen2 halamanROO M General Data Admitt Ing DX Worki NG DX Laboratory Frichmond MedicationsnicewanBelum ada peringkat
- Gomella - SepsisDokumen15 halamanGomella - SepsisJustine Frances CabalayBelum ada peringkat
- Neonatal InfectionsDokumen19 halamanNeonatal InfectionsA B Siddique RiponBelum ada peringkat
- Neonatal MeningitisDokumen10 halamanNeonatal MeningitisRana KhairunnisaBelum ada peringkat
- Identification and Classification of Neonate With InfectionsDokumen62 halamanIdentification and Classification of Neonate With Infectionsvisuinsvu100% (7)
- Peplu Theory ApplicationDokumen7 halamanPeplu Theory ApplicationVarsha Gurung100% (1)
- Meningitis (Completed)Dokumen26 halamanMeningitis (Completed)seema83% (6)
- San Lazaro Hospital Shifting ExamDokumen6 halamanSan Lazaro Hospital Shifting ExamnicewanBelum ada peringkat
- Neontalinf 150325093401 Conversion Gate01Dokumen86 halamanNeontalinf 150325093401 Conversion Gate01Sanjay Kumar SanjuBelum ada peringkat
- "Neonatal Infections" Lecture 1: Pediatrics Dr. Sawsan AliDokumen5 halaman"Neonatal Infections" Lecture 1: Pediatrics Dr. Sawsan AliAmmarBelum ada peringkat
- Viral ExanthemDokumen60 halamanViral ExanthemClaire GuanteroBelum ada peringkat
- Neonatal SepsisDokumen51 halamanNeonatal SepsisAngelo Del VentoBelum ada peringkat
- Knust Lect Infectious Disease IDokumen8 halamanKnust Lect Infectious Disease IAnastasiafynnBelum ada peringkat
- 7 Neonatal Diseases & ConditionsDokumen32 halaman7 Neonatal Diseases & ConditionsJohn Wesley OmbogoBelum ada peringkat
- Infection in PregnancyDokumen5 halamanInfection in PregnancyWasem A. JabbarBelum ada peringkat
- Neonatal Sepsis: Definition & IncidenceDokumen8 halamanNeonatal Sepsis: Definition & IncidenceahmedBelum ada peringkat
- Sepsis Neonatal 2016Dokumen102 halamanSepsis Neonatal 2016gcezcurraBelum ada peringkat
- Neonatal Bacterial InfectionDokumen8 halamanNeonatal Bacterial InfectionNuurBelum ada peringkat
- N SepsisDokumen36 halamanN SepsisAbdallah K. RamadanBelum ada peringkat
- Bishaw Assignment NN1of TORCHDokumen67 halamanBishaw Assignment NN1of TORCHRas Siko SafoBelum ada peringkat
- Neonatal Sepsis: Dr. Sunil Kumar Yadav MBBS, MD, DM NeonatologyDokumen64 halamanNeonatal Sepsis: Dr. Sunil Kumar Yadav MBBS, MD, DM NeonatologyKulgaurav RegmiBelum ada peringkat
- Torch Infections LectureDokumen77 halamanTorch Infections LectureL MollyBelum ada peringkat
- TORCH InfectionsDokumen37 halamanTORCH InfectionsEylin Halim Rahardjo100% (1)
- Infections in PregnancyDokumen124 halamanInfections in Pregnancyxzfdf2mwvxBelum ada peringkat
- Pediatric Infectious Diseases. Vaccination ProgramsDokumen44 halamanPediatric Infectious Diseases. Vaccination ProgramsShubhra PaulBelum ada peringkat
- TORCHDokumen42 halamanTORCHKarla RosadoBelum ada peringkat
- MRCPCH Guide InfDokumen19 halamanMRCPCH Guide InfRajiv Kabad100% (1)
- Neonatal Sepsis 1219225703095484 9Dokumen50 halamanNeonatal Sepsis 1219225703095484 9Ali FalihBelum ada peringkat
- Infections of The Fetus and NewbornDokumen55 halamanInfections of The Fetus and Newbornlordoftheweb100% (4)
- Infections of The Central Nervous System: DR John Egbagba FmcpathDokumen46 halamanInfections of The Central Nervous System: DR John Egbagba FmcpathPrincewill SeiyefaBelum ada peringkat
- HIV PediatricsDokumen15 halamanHIV Pediatricshussain AltaherBelum ada peringkat
- Exanthematous Viral DiseasesDokumen64 halamanExanthematous Viral DiseasesHoc Lim SeeBelum ada peringkat
- Patrick Duff, M.D. University of FloridaDokumen57 halamanPatrick Duff, M.D. University of FloridaRajaBelum ada peringkat
- Infectious Deseases in Pregnancy: Margie Reyes-Posadas, M.D. Ob GynDokumen54 halamanInfectious Deseases in Pregnancy: Margie Reyes-Posadas, M.D. Ob GynPrincess Aira Bucag CarbonelBelum ada peringkat
- Bacterial MeningitisDokumen51 halamanBacterial MeningitiscaseinrenninBelum ada peringkat
- Meningitis Beyond The Neonatal AgeDokumen51 halamanMeningitis Beyond The Neonatal AgeBeamlak Getachew WoldeselassieBelum ada peringkat
- Hiv Aids in PediatricsDokumen60 halamanHiv Aids in Pediatricsmy Lord JesusBelum ada peringkat
- Intra-Uterine Infections - Torches, Hiv, Tuberculosis, MalariaDokumen18 halamanIntra-Uterine Infections - Torches, Hiv, Tuberculosis, MalariaNwosu Ogbonna GabrielBelum ada peringkat
- Congenital and Perinatal Infections: Throwing New Light With An Old TORCHDokumen27 halamanCongenital and Perinatal Infections: Throwing New Light With An Old TORCHdr_ashutosh756078Belum ada peringkat
- Neonatal Sepsis & Thermoregulations 2Dokumen40 halamanNeonatal Sepsis & Thermoregulations 2Izzar IzlinBelum ada peringkat
- Infectious DiseasesDokumen140 halamanInfectious DiseasesSamah IzzBelum ada peringkat
- Viral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanDokumen46 halamanViral Infections in Pregnant Women: Departemen Mikrobiologi Fak - Kedokteran USU MedanSyarifah FauziahBelum ada peringkat
- Neonatal SepsisDokumen6 halamanNeonatal SepsisSunaina AdhikariBelum ada peringkat
- Viral MeningitisDokumen22 halamanViral MeningitisdariailmasariBelum ada peringkat
- Neonatal Sepsis: Author: Sherrill Roskam RNC MN NNP CNS Updated Presentation: Susan Greenleaf RNC, BSNDokumen46 halamanNeonatal Sepsis: Author: Sherrill Roskam RNC MN NNP CNS Updated Presentation: Susan Greenleaf RNC, BSN'-dooublleaiienn Itouehh IinBelum ada peringkat
- MTS - Fever and Chills in ChildrenDokumen36 halamanMTS - Fever and Chills in ChildrenYayaBelum ada peringkat
- Treating Opportunistic Infection Among HIV-Infected ChildrenDokumen173 halamanTreating Opportunistic Infection Among HIV-Infected ChildrenprasadkakkireniBelum ada peringkat
- NohlpsbfurnDokumen17 halamanNohlpsbfurnTri Setya NBelum ada peringkat
- Inrauterine InfectionsDokumen83 halamanInrauterine Infectionsahmad aminBelum ada peringkat
- Infectia Cu CMVDokumen31 halamanInfectia Cu CMVminerva_stanciuBelum ada peringkat
- Congenital Cytomegalovirus Infection - A Late ManifestationDokumen4 halamanCongenital Cytomegalovirus Infection - A Late ManifestationMinerva StanciuBelum ada peringkat
- IM, CMV and Toxoplasma InfectionsDokumen112 halamanIM, CMV and Toxoplasma Infectionsnada9tarek-2Belum ada peringkat
- Congenital InfectionDokumen15 halamanCongenital Infectionamid sultanBelum ada peringkat
- Herpes ZosterDokumen6 halamanHerpes ZosterRonan suhendraBelum ada peringkat
- Φ PathophysiologyDokumen4 halamanΦ PathophysiologyMariah AshooriyanBelum ada peringkat
- 2 DHF InternaDokumen59 halaman2 DHF Internasaladass 2Belum ada peringkat
- FIGO Ovarian Cancer Staging 1.10.14 2Dokumen2 halamanFIGO Ovarian Cancer Staging 1.10.14 2Elisa Cynthia ArdarickaBelum ada peringkat
- Meds PedsDokumen5 halamanMeds PedsnicewanBelum ada peringkat
- Intro To ImmunologyDokumen7 halamanIntro To ImmunologynicewanBelum ada peringkat
- WHO Dengue Guidelines 2013Dokumen160 halamanWHO Dengue Guidelines 2013Jason MirasolBelum ada peringkat
- Syndromes and DiseasespdfDokumen17 halamanSyndromes and DiseasespdfnicewanBelum ada peringkat
- Ebcpg BileductstonesDokumen12 halamanEbcpg BileductstonesRatih Lestari UtamiBelum ada peringkat
- Infestation SDokumen6 halamanInfestation SnicewanBelum ada peringkat
- Ob ReportDokumen37 halamanOb ReportnicewanBelum ada peringkat
- 5 - 1 Diseases of The IntestineDokumen16 halaman5 - 1 Diseases of The IntestinenicewanBelum ada peringkat
- Laboratory Flow SheetDokumen2 halamanLaboratory Flow SheetnicewanBelum ada peringkat
- Clinical PointsDokumen6 halamanClinical PointsnicewanBelum ada peringkat
- Acls Study Guide September 2011Dokumen18 halamanAcls Study Guide September 2011Zarah Jane Rull NateBelum ada peringkat
- Ten Steps To Successful BreastfeedingDokumen2 halamanTen Steps To Successful BreastfeedingnicewanBelum ada peringkat
- AppendicitisDokumen27 halamanAppendicitisnicewanBelum ada peringkat
- Cutaneous Drug ReactionsDokumen7 halamanCutaneous Drug ReactionsnicewanBelum ada peringkat
- Tetanus CDCDokumen10 halamanTetanus CDCZelfi PrimasariBelum ada peringkat
- Surgery Ortho - TaskDokumen4 halamanSurgery Ortho - TasknicewanBelum ada peringkat
- Pediatric Care GuideDokumen27 halamanPediatric Care GuideFadi AwwadBelum ada peringkat
- 11 13Dokumen4 halaman11 13nicewanBelum ada peringkat
- 5 - 1 Diseases of The IntestineDokumen16 halaman5 - 1 Diseases of The IntestinenicewanBelum ada peringkat
- Malignant Diseases of The CervixDokumen128 halamanMalignant Diseases of The Cervixnicewan0% (1)
- Duchenne Muscular DystrophyDokumen2 halamanDuchenne Muscular DystrophynicewanBelum ada peringkat
- OrthopaedicsDokumen3 halamanOrthopaedicsnicewanBelum ada peringkat
- MediastinumDokumen8 halamanMediastinumnicewanBelum ada peringkat
- Bones of The Upper LimbDokumen8 halamanBones of The Upper LimbnicewanBelum ada peringkat
- 1Dokumen8 halaman1nicewanBelum ada peringkat
- MediastinumDokumen8 halamanMediastinumnicewanBelum ada peringkat
- 2Dokumen8 halaman2nicewanBelum ada peringkat
- Economics Assignment (AP)Dokumen20 halamanEconomics Assignment (AP)Hemanth YenniBelum ada peringkat
- Abuse and Violence: Working With Our Patients in General Practice (4th Edition)Dokumen152 halamanAbuse and Violence: Working With Our Patients in General Practice (4th Edition)IndahEkaPutriBelum ada peringkat
- Job Safety Analysis: Date/ Jsa No: Jsa Team Members Job: Location: Project/ Client: SupervisorDokumen1 halamanJob Safety Analysis: Date/ Jsa No: Jsa Team Members Job: Location: Project/ Client: SupervisorMuhammad Akbar Al BardawiBelum ada peringkat
- Test I. True or False. Write TRUE If The Statement Is Correct and FALSE If The Statement Is IncorrectDokumen2 halamanTest I. True or False. Write TRUE If The Statement Is Correct and FALSE If The Statement Is IncorrectMariecris Barayuga Duldulao-AbelaBelum ada peringkat
- AbraDokumen4 halamanAbralhhjklllBelum ada peringkat
- Civil Engineering & Its BranchesDokumen37 halamanCivil Engineering & Its BranchesMohammad JavedBelum ada peringkat
- Reflection Paper - Behavioral Problems and TypesDokumen2 halamanReflection Paper - Behavioral Problems and TypesFirdaus AbdullahBelum ada peringkat
- InterbarkadaDokumen8 halamanInterbarkadaJay Vincent DiamanteBelum ada peringkat
- Segmentos Ica 2022 PDFDokumen9 halamanSegmentos Ica 2022 PDFRoberto RodríguezBelum ada peringkat
- UltraCal XS PDFDokumen2 halamanUltraCal XS PDFKarina OjedaBelum ada peringkat
- Shoulder Impingement GuidelinesDokumen3 halamanShoulder Impingement GuidelinesTasha MillerBelum ada peringkat
- Tugas 2Dokumen17 halamanTugas 2NuretikaSalmiaBelum ada peringkat
- VST Electronic Medical RecordsDokumen2 halamanVST Electronic Medical RecordsarunsahayakumarBelum ada peringkat
- Concept of Health EducationDokumen14 halamanConcept of Health EducationYou PanhamorokotBelum ada peringkat
- Chapter 4 and Chapter 5Dokumen58 halamanChapter 4 and Chapter 5Aria DiemBelum ada peringkat
- Jamie's Story 15q21.3-22.2 DeletionDokumen1 halamanJamie's Story 15q21.3-22.2 DeletionNatasha RadcliffeBelum ada peringkat
- Specification Sheet: Product: Salted Anchovy in BarrelsDokumen1 halamanSpecification Sheet: Product: Salted Anchovy in BarrelsPoesía PeruanaBelum ada peringkat
- 07 RPM Chapter Feb 2021 V9 508 Clean FinalDokumen143 halaman07 RPM Chapter Feb 2021 V9 508 Clean FinalShubhamBelum ada peringkat
- Seafarer Medical CertificateDokumen2 halamanSeafarer Medical CertificateKoki ToBelum ada peringkat
- Sonographic Evaluation of The DiaphragmDokumen1 halamanSonographic Evaluation of The DiaphragmAngelo LongoniBelum ada peringkat
- 2 BiotechnologyDokumen5 halaman2 BiotechnologyJannah BuenavistaBelum ada peringkat
- Literature Review On DVTDokumen4 halamanLiterature Review On DVTaflsdefaq100% (1)
- The Intentional Application of Humor With CKD PatientsDokumen8 halamanThe Intentional Application of Humor With CKD PatientsKaryn BuxmanBelum ada peringkat
- Network Hospital Grading Proforma: General InformationDokumen6 halamanNetwork Hospital Grading Proforma: General InformationSanket SahareBelum ada peringkat
- Bulletin 201215 (HTML Edition)Dokumen128 halamanBulletin 201215 (HTML Edition)DonnieBelum ada peringkat