NGT
Diunggah oleh
Roxas CedrickHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
NGT
Diunggah oleh
Roxas CedrickHak Cipta:
Format Tersedia
Nasogastric tubes 1: insertion technique and confirming position.
Indications for nasogastric tube insertion, the procedure for inserting a nasogastric tube
and how to check whether it is in the correct position
Introduction
A nasogastric (NG) tube is a long polyurethane or silicone tube that is passed
through the nasal passages via the oesophagus into the stomach. They are
commonly inserted in surgical practice for various reasons.
According to the National Patient Safety Agency (2005a), 11 deaths and one case of
serious harm occurred over a two-year period because NG feeding tubes had been
misplaced.
Nasogastric tubes are inserted by nurses, junior doctors and sometimes by
anaesthetists in theatre. It is vital that staff inserting them know the correct
insertion technique as well as the procedure for verifying their correct positioning.
This article reviews the indications for NG tubes and the benefits and risks
associated with their use, and explains the correct method of insertion, as well as
how to verify their correct intragastric positioning.
Indications
There are only two main indications for NG tube insertion to empty the upper
gastrointestinal tract or for feeding. Insertion may be for prophylactic or therapeutic
reasons.
Care should be taken in cases where there may be:
Ear, nose and throat abnormalities or infections;
Possible strictures of the oesophagus;
Oesophageal varices;
Anatomical abnormalities (oesophageal diverticulae);
Risk of aspiration.
Gaining consent
Practitioners should give patients a reassuring, detailed explanation of the insertion
procedure, together with the reasons why the tube is necessary. Verbal consent
should then be obtained.
Sizes
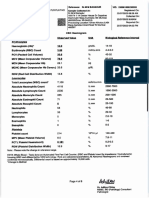
Nasogastric tubes come in various sizes (8, 10, 12, 14, 16 and 18 Fr). Stiff tubes
are easier to insert, and putting them in a refrigerator or filling them with saline
helps to stiffen them. Some fine-bore tubes come with a guide wire to aid
placement. The tube has markings and a radio-opaque marker at the tip to check
its position on X-ray.
Preparation
After washing hands, prepare a trolley including gloves, local anaesthetic jelly or
spray, a 60ml syringe, pH strip, kidney tray, sticky tape and a bag to collect
secretions. Placing a glass of drinking water nearby is useful.
Insertion technique
Tubes are usually inserted by nurses or junior doctors by the bedside or by
anaesthetists in theatre before or during surgery.
External measurement from the tip of the nose to a point halfway between the
xiphoid and the umbilicus distance gives a rough idea of the required length.
The patient should sit up, without any head tilt (chin up). An appropriately sized
tube is chosen and the tip is lubricated by smearing aqua gel or local anaesthetic
gel. Anaesthetic gel is a drug so if it is used it must be prescribed, and precautions
taken such as checking for allergies.
The wider nostril is chosen and the tube slid down along the floor of the nasal
cavity. Patients often gag when the tube reaches the pharynx. Asking them to
swallow their saliva or a small amount of water may help to direct the tube into the
oesophagus. Once in the oesophagus, it may be easy to push it down into the
stomach.
The correct intragastric position is then verified (see below). The tube is fixed to the
nose and forehead using adhesive tapes. The stomach is decompressed by
attaching a 60ml syringe and aspirating its contents. Blocked tubes can be flushed
open with saline or air.
Verifying correct intragastric positioning
The intragastric position of the tube must be confirmed after its initial insertion, and
this must be documented in the patients notes. There are two ways of confirming
the tubes position currently recommended. These are by pH test (Stock et al,
2008; NPSA, 2005a; 2005b) and X-ray. Other methods can be inaccurate and
should not be used.
pH test
The NG tube is aspirated and the contents are checked using pH paper, not litmus
paper (Earley, 2005). The NPSA (2005b) recommended that it is safe to feed
patients (infants, children and adults) if the pH is 5.5 or below. This advice does not
apply to neonates (preterm to 28 days). See the NPSAs (2005b) advice and the
update (2007) for more information.
Note that taking proton pump inhibitors or H
2
receptor antagonists may alter the
pH. Similarly, intake of milk can neutralise the acid.
Chest X-ray
When in doubt, it is best practice to use X-ray to check the tubes location (Stock et
al, 2008). Patients who have swallowing problems, confused patients and those in
ICU should all be given an X-ray to verify the tubes intragastric position. This
involves taking a chest X-ray including the upper half of the abdomen. The tip of
the tube can be seen as a white radio-opaque line and should be below the
diaphragm on the left side.
Syringe test
This test is mentioned here for historic interest only. Also known as the whoosh
test, it has been shown to be an unreliable method of checking tube placement, and
the NPSA (2007; 2005a; 2005b) has said that it must no longer be used.
Confirming position
Correct intragastric positioning should be confirmed:
Immediately after initial placement;
Before each feed;
Following vomiting/coughing and after observing decreased oxygen saturation;
If the tube is accidentally dislodged or the patient complains of discomfort.
Never insert the guide wire while the nasogastric tube is in the patient.
Advantages
There are several advantages associated with the use of NG tubes. They will
decompress the stomach by releasing air and liquid contents. This is important for
patients with ileus, intestinal and gastric outlet obstruction. These conditions can
cause vomiting, and patients are at risk of aspirating their stomach contents, which
can lead to potentially lethal pneumonitis.
Nasogastric tubes may also be useful for feeding patients who have dysphagia, for
example after experiencing a stroke, and also for those being who have undergone
a tracheostomy.
Nasojejunal tubes are longer versions of NG tubes. They are inserted under
endoscopic guidance to lie further in the jejunum and may be useful in feeding
patients with pancreatitis.
Part 2 of this unit, to be published next week, looks at complications and guidance on using
nasogastric tubes.
For the Portfolio Pages corresponding to this unit see the document above
Portfolio Pages contain activities that correspond to the learning objectives in the unit. They are
presented in a convenient format for you to print out or work through on screen and can be filed in
your professional portfolio as evidence of your learning and professional development.
Anda mungkin juga menyukai
- A Gas Sds CyclopentaneDokumen7 halamanA Gas Sds CyclopentaneRoxas CedrickBelum ada peringkat
- MOH NGT ProcedureDokumen56 halamanMOH NGT ProcedureMheanne Romano100% (2)
- R & D R & D: Rebecca Lynn Jones David James West Rebecca Lynn Jones David James WestDokumen1 halamanR & D R & D: Rebecca Lynn Jones David James West Rebecca Lynn Jones David James WestRoxas CedrickBelum ada peringkat
- NGTDokumen4 halamanNGTRoxas CedrickBelum ada peringkat
- House BlessingDokumen3 halamanHouse BlessingRoxas CedrickBelum ada peringkat
- 6th Central Pay Commission Salary CalculatorDokumen15 halaman6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 7 27 14sambuhayDokumen8 halaman7 27 14sambuhayRoxas CedrickBelum ada peringkat
- Poor HygieneDokumen2 halamanPoor HygieneRoxas CedrickBelum ada peringkat
- House BlessingDokumen1 halamanHouse BlessingRoxas CedrickBelum ada peringkat
- Acls Course HandoutsDokumen8 halamanAcls Course HandoutsRoxas CedrickBelum ada peringkat
- R - Rescue: R.A.C.E. Method For Fire ResponseDokumen2 halamanR - Rescue: R.A.C.E. Method For Fire ResponsecedieboyBelum ada peringkat
- SSS RS - 5Dokumen1 halamanSSS RS - 5Anid AzertsedBelum ada peringkat
- RecieptDokumen1 halamanRecieptRoxas CedrickBelum ada peringkat
- Twenty-Fourth Sunday in Ordinary TimeDokumen5 halamanTwenty-Fourth Sunday in Ordinary TimeJoe RoxBelum ada peringkat
- Certificate of Residency: BarangayDokumen1 halamanCertificate of Residency: BarangayRoxas CedrickBelum ada peringkat
- Genitounrinary SystemDokumen22 halamanGenitounrinary SystemRoxas CedrickBelum ada peringkat
- Bioterrorism HandoutsDokumen13 halamanBioterrorism HandoutsRoxas CedrickBelum ada peringkat
- Novena To Our Lady of Peace and Good VoyageDokumen4 halamanNovena To Our Lady of Peace and Good VoyageJoe RoxBelum ada peringkat
- Anatomy and Physiology Nurseslabs GUTDokumen5 halamanAnatomy and Physiology Nurseslabs GUTRoxas CedrickBelum ada peringkat
- Breast CancerDokumen20 halamanBreast CancerRoxas CedrickBelum ada peringkat
- NGTDokumen4 halamanNGTRoxas CedrickBelum ada peringkat
- NELEC1 ProjectDokumen14 halamanNELEC1 ProjectRoxas CedrickBelum ada peringkat
- Assignment OneDokumen5 halamanAssignment OneRoxas CedrickBelum ada peringkat
- Patient Transfer To StretcherDokumen3 halamanPatient Transfer To StretcherRoxas CedrickBelum ada peringkat
- Drug Study: Drug Actions Contraindications Side Effects Nursing ConsideartionsDokumen1 halamanDrug Study: Drug Actions Contraindications Side Effects Nursing ConsideartionsRoxas CedrickBelum ada peringkat
- Assistance To PWDsDokumen27 halamanAssistance To PWDsRod MagatBelum ada peringkat
- Drug Study: Drug Actions Contraindications Side Effects Nursing ConsideartionsDokumen1 halamanDrug Study: Drug Actions Contraindications Side Effects Nursing ConsideartionsRoxas Cedrick100% (1)
- FdarDokumen1 halamanFdarRoxas Cedrick100% (1)
- Breast CancerDokumen20 halamanBreast CancerRoxas CedrickBelum ada peringkat
- Office of The Punong BarangayDokumen1 halamanOffice of The Punong BarangayRoxas CedrickBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Dula-Tungkulin o Gampanin NG ProduksyonDokumen12 halamanDula-Tungkulin o Gampanin NG ProduksyonBernadette DuranBelum ada peringkat
- Bedwetting in ChildrenDokumen41 halamanBedwetting in ChildrenAnkit ManglaBelum ada peringkat
- Aldrine Ilustricimo VS Nyk Fil Sjip Management IncDokumen11 halamanAldrine Ilustricimo VS Nyk Fil Sjip Management Inckristel jane caldozaBelum ada peringkat
- Sample Questionnaire For Understanding The Self: For Private Use OnlyDokumen6 halamanSample Questionnaire For Understanding The Self: For Private Use Onlyirene ilustrisimo100% (1)
- Amazing Facts About Our BrainDokumen4 halamanAmazing Facts About Our BrainUmarul FarooqueBelum ada peringkat
- Week 1 - NCMA 219 LecDokumen27 halamanWeek 1 - NCMA 219 LecDAVE BARIBEBelum ada peringkat
- DASH Questionnaire Disability Arm Shoulder HandDokumen3 halamanDASH Questionnaire Disability Arm Shoulder HandChristopherLawrenceBelum ada peringkat
- MBF90324234Dokumen407 halamanMBF90324234Emad Mergan100% (1)
- Breast Imaging Review - A Quick Guide To Essential Diagnoses (2nd Edition) PDFDokumen264 halamanBreast Imaging Review - A Quick Guide To Essential Diagnoses (2nd Edition) PDFGregorio Parra100% (2)
- Pigeons: Animal SciencesDokumen15 halamanPigeons: Animal SciencesSafi Ul RehmanBelum ada peringkat
- Abnormal Psychology Final Practice QuestionsDokumen16 halamanAbnormal Psychology Final Practice QuestionsJames WilkesBelum ada peringkat
- Sino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBDokumen2 halamanSino-Nasal Outcome Test (SNOT-22) Questionnaire: Patient's Name Date DOBIchsanJuliansyahBelum ada peringkat
- 12 Psychology - Meeting Life Challenges - Notes & Video LinkDokumen11 halaman12 Psychology - Meeting Life Challenges - Notes & Video LinkRamesh TalukdarBelum ada peringkat
- Subjective: Diarrhea Related To Watery Short Term: IndependentDokumen4 halamanSubjective: Diarrhea Related To Watery Short Term: IndependentEmma Lyn SantosBelum ada peringkat
- ResearchDokumen28 halamanResearchReylon PachesBelum ada peringkat
- Criminal SociologyDokumen53 halamanCriminal SociologyJackielyn cabayaoBelum ada peringkat
- GENERAL RISK ASSESSMENT Mechatronics LaboratoryDokumen2 halamanGENERAL RISK ASSESSMENT Mechatronics LaboratoryJason TravisBelum ada peringkat
- BM Procedure and ProcessingDokumen28 halamanBM Procedure and ProcessingNidhi JaisBelum ada peringkat
- Music Therapy in Nursing HomesDokumen7 halamanMusic Therapy in Nursing Homesapi-300510538Belum ada peringkat
- State Consumer Disputes Redressal Commission, Punjab, ChandigarhDokumen50 halamanState Consumer Disputes Redressal Commission, Punjab, ChandigarhKandlagunta Gayathri PraharshithaBelum ada peringkat
- Preterm Prelabour Rupture of MembranesDokumen12 halamanPreterm Prelabour Rupture of MembranesSeptiany Indahsari DjanBelum ada peringkat
- Maxime Gorky and KingstonDokumen433 halamanMaxime Gorky and KingstonBasil FletcherBelum ada peringkat
- Bentonite MSDSDokumen10 halamanBentonite MSDSkhai ruleBelum ada peringkat
- NUR091 - Session 8Dokumen6 halamanNUR091 - Session 8aquinoemjay27Belum ada peringkat
- Protokol KemoterapiDokumen147 halamanProtokol KemoterapiDala VW100% (1)
- Adobe Scan Jul 28, 2023Dokumen6 halamanAdobe Scan Jul 28, 2023Krishna ChaurasiyaBelum ada peringkat
- Carbon Monoxide PoisoningDokumen31 halamanCarbon Monoxide PoisoningDheerajBelum ada peringkat
- 13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsDokumen36 halaman13) Technical Guideline On Irritation, Sensitization and Hemolysis Study For Chemical DrugsAzam DanishBelum ada peringkat
- Mapeh: Music - Arts - Physical Education - HealthDokumen23 halamanMapeh: Music - Arts - Physical Education - HealthExtremelydarkness100% (1)
- Cytogenetics - Prelim TransesDokumen15 halamanCytogenetics - Prelim TransesLOUISSE ANNE MONIQUE L. CAYLOBelum ada peringkat