Hiv Aids Review
Diunggah oleh
iri_moise2819Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Hiv Aids Review
Diunggah oleh
iri_moise2819Hak Cipta:
Format Tersedia
HIV & AIDS Review11 (2012) 514
Contents lists available at SciVerse ScienceDirect
HIV & AIDS Review
j our nal homepage: www. el sevi er . com/ l ocat e/ hi var
Review
Highly Active Antiretroviral Therapy for treatment of HIV/AIDS patients: Current
status and future prospects and the Indian scenario
Garima Kumari, Ramendra K. Singh
Nucleic Acids Research Laboratory, Department of Chemistry, University of Allahabad, Allahabad 211 002, India
a r t i c l e i n f o
Article history:
Received 6 September 2011
Accepted 5 February 2012
Available online 3 March 2012
Keywords:
HIV
Drug targets
FDCs
HAART
Viral reservoirs
Indian scenario
a b s t r a c t
As the menace of HIV/AIDS continues to rise, effective drug treatments are required to reach the infected
masses. HAART provides durable control of virus replication, however, it is not devoid of unwanted
side effects, especially in persons undergoing long-term treatment. The current therapy nds its lim-
itations in the emergence of multidrug resistance, transmission of drug-resistant HIV strains, and a
life-long treatment. Moreover, to improve patient adherence and to simplify the treatments, effective
xed dose combinations (FDCs) are needed. The picture of HIV/AIDS in India shows that HIV/AIDS is
declining through the country and perhaps through proper measures HIV can be eradicated. Thus, nd-
ing novel drug targets and new drugs is the need of the hour to treat the infected persons and to reach
HIV reservoirs in the body, like brain, lymph nodes, etc. to achieve the ultimate goal, i.e., the complete
eradication of the dreaded virus HIV, the causative agent for AIDS.
2012 Polish AIDS Research Society. Published by Elsevier Urban & Partner Sp. z.o.o. All rights reserved.
1. Introduction
HIV/AIDS continues tobe a dreadedkiller till date andmore than
33 million people worldwide are currently infected with Human
Immunodeciency Virus (HIV), discoveredabout three decades ago
[1,2] as the causative agent for Acquired Immunodeciency Syn-
drome (AIDS) an immunocompromised condition. Since its rst
disclosure in 1981 (Fig. 1), HIV/AIDS has killed more that 25 mil-
lion people all over the world and stands today as the major threat
to human health. However, as a result of sustained steps, which
also include the impact of HIV prevention efforts, a ray of hope has
emerged as HIVprevalence and incidence have gone down globally
over the decade as per UNAIDS 2010 report, except for, unfortu-
nately, Eastern Europe and Central Asia where a slight increase has
been noticed.
HIVis a retrovirus and possesses RNAas genetic material, which
is covered by a viral coat. Once this virus enters a host cell, it
removes its coat and produces another kind of genetic material
the dsDNA, known as the provirus. This provirus then gets incor-
porated into human DNA, hijacks the host cell apparatus and starts
producing hundreds and hundreds of new virion particles. Since
the whole life cycle of this virus passes inside the host cell, it
becomes really challenging to nd an appropriate treatment. The
This article is dedicated to Prof. David Shugar on his 96th Birth Day
(September 10, 2011).
Corresponding author. Tel.: +91 532 246 1005; fax: +91 532 246 1005.
E-mail address: rksinghsrk@gmail.com(R.K. Singh).
scientic community, however, has found some suitable drugs
against HIV, which target the different stages of its proliferation
and multiplication. Presently, seven groups of anti-HIV drugs tar-
geting different stages of its life cycle are being used: nucleoside
reverse transcriptase inhibitors (NRTIs), nucleotide reverse tran-
scriptase inhibitors (NtRTIs), non-nucleoside reverse transcriptase
inhibitors (NNRTIs), protease inhibitors (PIs), fusioninhibitors (FIs),
co-receptor inhibitors (CRIs) and integrase inhibitors (INIs), and
these drugs have proved their usefulness also in halting the HIV
from reproducing. However, a unique phenomenon was noticed
with HIV. Unlike other viruses, it was found capable of show-
ing different behavior not only from cell to cell but also from
person to person. This was because of mutation in its genetic mate-
rial and as a result, different strains of viruses were developed.
These mutated viruses developed resistance to the drugs being
used.
At this critical junction, a combinationtherapy knownas HAART
(Highly Active Antiretroviral Therapy) was introduced to stop HIV
from reproducing and it has greatly reduced the high morbid-
ity and mortality rate [35]. However, this therapy too cannot
cure AIDS and patients are destined to undergo life-long treat-
ment and use of this therapy has several limitations, like toxicity
[6], development of drug resistance [7] and poor tolerability [8].
The stepping-stones towards the achievement of long-term virus
control are simplication of therapy, improvement of patient
adherence andminimizationof drug resistance. Thus, the challenge
still present before the scientic community all over the world is
to develop novel anti-HIV compounds with new mechanisms of
action, accepted toxicity and resistance prole.
1730-1270/$ see front matter 2012 Polish AIDS Research Society. Published by Elsevier Urban & Partner Sp. z.o.o. All rights reserved.
doi:10.1016/j.hivar.2012.02.003
6 G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514
Fig. 1. Pictorial representation of landmarks in the treatment of HIV.
2. HIV infection: life cycle of HIV and drug targets
During HIV infection the immune system begins to fail, which
leads to various life-threatening opportunistic infections. HIV
infection occurs through transfer of blood, semen, vaginal uids,
pre-ejaculate or breast milk. HIV is present in these body uids
either as free virus particles or within infected immune cells. Thus,
the four major routes of HIV transmission are unsafe sex, con-
taminated needles, breast milk and from a mother to her baby
intrapartum.
2.1. Life cycle of HIV
The life cycle of HIV (Fig. 2) starts with the attachment of the
virus to the host cell membrane and ends with release of the new
virion particles fromthe host cell, which can be summarized in the
following steps:
(i) Binding and fusion: HIVbegins its life cycle by attaching its gly-
coprotein gp120 to CD4
+
T cells followed by CCR5 and CXCR4
co-receptors depending on its tropism. This leads to fusion of
the viral envelope, mediated by gp41, with the cell membrane
and the release of the HIV capsid into the cell. The virus is
now decapsidated releasing the viral RNA into the host cell
cytoplasm.
(ii) Reverse transcription: HIV reverse transcriptase converts its
ssRNA into dsDNA, known as the provirus.
(iii) Integration: The newly formed HIV provirus enters the host
cells nucleus, where an enzyme called HIV integrase, inte-
grates the provirus within the host cells DNA. The provirus
may remain inactive for several years.
(iv) Transcription: The provirus integrated into the host genome
uses a host enzyme called RNA polymerase to create copies of
the HIV genomic material, as well as shorter strands of RNA
called messenger RNA (mRNA).
(v) Translation: The mRNA is used as a blueprint to make long
chains of HIV proteins.
(vi) Assembly and budding: An HIV enzyme called protease cuts
the long chains of HIV proteins into smaller individual func-
tional proteins. The smaller HIV proteins come together with
copies of HIVs RNA genetic material and a new virus particle
is assembled.
(vii) Maturation and release: The newly assembled virus pushes out
from the host cell. During budding, the new virus steals part
of the cells outer envelope. This envelope is studded with
protein/sugar/lipid combinations and constitutes the HIV gly-
coproteins. The newcopies of HIV can nowmove on to infect
other cells.
G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514 7
Fig. 2. Life cycle of HIV showing different stages fromits attachment to the cell membrane to the release of newvirion particles.
2.2. Drug targets
During its proliferation inside the host cell, the virus is exposed
to various types of interventions, which can prove detrimental to
its multiplication and, in turn, its existence. These possible targets
and agents for intervention have been summarized in Table 1.
3. Treatment: current status
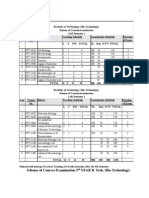
3.1. Landmarks in the development of HAART
The major breakthroughs obtained in the treatment of HIV/AIDS
are shown in Table 2. After the identication of HIV as the etiolog-
ical agent for AIDS [9], collaboration between the National Cancer
Table 1
Possible HIV targets and potential interventions.
Stage of HIV life cycle Potential intervention
Binding to the host cell Antibodies to the virus or cell receptor
Entry to the host cell Drugs blocking fusion
Reverse transcription Reverse transcriptase inhibitors
Integration of DNA into the host
genome
Integrase inhibitors
Expression of viral genes Inhibitors of the tat protein
Production and assembly of viral
components
Myristoylation, glycosylation and
protease inhibitors
Budding of the virus Interferons
Institute, US and Burroughs-Wellcome Company led to the discov-
ery that AZT was able to suppress HIV-1 replication in vitro [10,11].
The approval of rst PI, sanquinavir followed by the rst NNRTI,
nevirapine, brought a revolution in the treatment of HIV/AIDS.
The introduction of HAART resulted in marked decrease in plasma
viremia in most patients [12]. Combivir was the rst xed dose reg-
imen consisting of AZT and FTC and it was developed primarily to
improve adherence to treatment, which is a major cause of failure
and emergence of drug resistance. Since then xed-dose combina-
tions (FDCs) have playedanessential role insimplifying some of the
Table 2
Landmarks in the treatment of HIV.
1981 Mortality and Morbidity Weekly Report reports of men treated for
biopsy showed signs of severe immunodeciency.
1983 A newhuman lymphotropic retrovirus (HTLV-III/HIV-1) was
isolated fromthe T-cells of patients
1984 Etiological link of HIV to AIDS was demonstrated
1985 Zidovudine (AZT) was identied as a NRTI
1987 AZT approved for antiretroviral therapy
1995 Sanquinavir (protease inhibitor) approved by FDA
1996 Nevirapine (NNRTI) approved by FDA
1997 Combivir (AZT+3TC) approved as rst xed-dose combination pills
2003 Enfuvirtide (fusion inhibitor) approved by FDA
2006 The rst single pill Atripla (TDF +FTC+EFV) approved by FDA
2007 Maraviroc (CCR5 antaagonist) and raltegravir (integrase inhibitor)
approved by FDA
2009 Long termcontrol of HIV by CCR%-32 stem-cell transplantation
is reported
8 G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514
N
NH
2
O
S
O
HO
N
NH
2
O
S
O
HO
F
N
NH
2
O
S
O
HO
F
Racivir (50:50 mixture of the -enantiomer of emtricitabine)
N
N
N
N
NH
2
NH
2
O
O
HO
N
N
NH
2
O
S
HO
Amdoxovir Elvucitabine
Apricitabine
Fig. 3. NRTIs undergoing phase II or phase III clinical trials.
most frequently used regimens. After the development of AZT, the
Food and Drug Administration (FDA), USA has played an important
role in approving antiretrovirals and in streamlining the regulatory
processes.
The present day combination therapy HAART utilizes seven
classes of drugs that target various stages in the life cycle of HIV.
These drugs are discussed as follows:
3.1.1. Nucleoside reverse transcriptase inhibitors (NRTIs)
The rst approvedanti-HIVdrugfor the treatment of AIDS AZT,
anucleosideanalog, actedbyinhibitingthefunctionof reversetran-
scriptase. Since then, several NRTIs have been approved. In total,
there are seven NRTIs approved for clinical use, viz. zidovudine
(AZT), 1,3-didanosine (ddI), lamivudine (3TC), zalcitabine (ddC),
stavudine (d4T), abacavir (ABC) and emtricitabine (FTC) [1316].
All NRTIs lack 3
-OH group in the sugar moiety and, therefore,
prevent incorporation of the incoming nucleotide. Modications
can be done either in the sugar moiety or base moiety or both sugar
and base moieties.
The NRTIs are phosphorylated by cellular kinases to their
triphosphate derivatives. This triphosphate form is then incorpo-
ratedinto the growing DNAchainby cellular DNApolymerases. The
incorporation of NRTIs into the growing DNAresults in termination
of the elongating DNA chain. Resistance often develops because of
removal of the chain-terminating residue, a kind of repair reaction
occurs, which involves pyrophosphorolysis, a process opposite of
reverse transcription [17,18].
In addition to these seven NRTIs, there are four more NRTIs
undergoing phase II or III clinical trials apricitabine [19], racivir
[20], amdoxovir [21] and elvucitabine [22] (Fig. 3). The studies con-
ducted on these molecules suggest that these are more potent than
the approved NRTIs and have fewer side effects [2326].
3.1.2. Nucleotide reverse transcriptase inhibitors (NtRTIs)
This class of compounds has a phosphonate group that cannot
be cleaved by esterases and need only two phosphorylation steps
to get converted into their active triphosphate forms, which serve
as alternative substrates in the reverse transcription reaction and
cause chain termination as there is no 3
-OH present. The NtRTI
approved currently for treating HIV-infected patients is tenofovir
diisoproxil fumarate [27,28].
This compound is safe and reduces the incidence of lipodys-
trophy. Moreover, it has less side effects and is more efciently
tolerated [29]. Currently, GS-9148 (2
-uoro-2
,3
-didehydro-2
,3
-
dideoxyadenosine) and its derivatives (Fig. 4) are being developed
as NtRTIs as these have shown less renal and mitochondrial toxic-
ities [30].
3.1.3. Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
The NNRTIs bind non-competitively at the allosteric site located
about 10
A away from the active site of reverse transcriptase
[3135]. Currently, four NNRTIs [36,37] are approved for treat-
ment of HIV, viz. nevirapine, efavirenz, delaviridine and etravirine.
The use of rst generation NNRTIs led to the rapid development of
resistance [38]. Thus, second generation NNRTIs were developed.
Six more NNRTIs, rilpivirine [39], calanolide A[40], (R,E)-methyl(2-
carbomyl-5-chloro-1H-indol-3-yl)(3-(2-cyanovinyl-5-methylphe-
nyl)phosphinate) (IDX-899) [41], 1-(5-cyanopyridin-2-yl)-3-
((1S,2S)-2-(6-uoro-2-hydroxy-3-propionyl-phenyl) cyclopropyl)
urea (MIV-150) [42], potassium 4-(2-((5-bromo-4-)(4-cyclo-
propylnaphthalen-1-yl)-4H-1,2,4-triazol-3-yl))-acetamido-3-chl-
orobenzoate (RDEA806) [43] and 4-(2-(11-ethyl-5methyl-6-oxo-
6,11-dihydro-5H-dipyrido[3,2-b:2
,3
-e][1,4]diazepin-8-yl)etho-
xy)-quinoline-1-oxide (BILR 355 BS) [44,45] (Fig. 5) are undergoing
phase II or phase III clinical trials. Besides being more potent and
effective against mutants, these have shown good oral bioavail-
ability. The only anti-HIV natural product undergoing clinical trials
is calanolide A, isolated fromtropical rain forest plant, Calophyllum
lanigerum[46].
3.1.4. Protease inhibitors (PIs)
The protease enzyme is responsible for cleavage of the gag and
gag-pol precursor polyproteins to the structural proteins (p17, p24,
p7, p6, p2 and p1) and (p66/p51) and integrase (p32), thereby
causing maturation of the progeny virions [47]. The HIV protease
is a homodimer that acts catalytically as an asparatic acid pro-
tease, and the active site is located at the interface of the dimer.
Ten protease inhibitors, viz. darunavir (TMC-114) [48], tipranavir
[49], sanquinavir [50], ritonavir [51], indinavir [52], nelnavir [53],
amprenavir [54], lopinavir (ABT-378) [55], fosamprenavir [56] and
atazanavir (ATV) [57] are currently approved by FDA. Except for
tipranavir, all the approved PIs are of peptide nature and have
poor bioavailability. The other side effects are the development of
resistance and toxicity.
3.1.5. Fusion inhibitors (FIs)
The infection of the host cell with HIV involves the interaction
between the virion glycoprotein gp120 on the outer membrane
and the CD4+ receptor on the host cell surface resulting in certain
conformational changes, which lead to the unmasking of a second
gp120-binding site for target chemokines co-receptors CXCR4 and
CCR5. Binding of gp120 to either or both co-receptors leads to the
fusion-active conformation of the viral trans-membrane protein
gp41. A hairpin like structure is formed, which contains a thermo-
dynamicallystablesix-helixbundlethat draws theviral andcellular
membranes closer for fusion [58]. The fusion inhibitor, enfuvirtide
is the only approved fusion inhibitor used for treatment of AIDS
[59].
Studies are going on to nd effective mimics of the transient
gp41intermediate. Tri-functionalized3,2
,2
-terphenyl derivatives
(Fig. 6) are being used and have been found to inhibit HIV-1 medi-
ated cell-to-cell fusion [60].
3.1.6. Co-receptor inhibitors (CRIs)
The chemokine receptors, viz. CCR5 andCXCR4 eventually allow
virus-cell fusion [61]. A large number of CCR5 and CXCR4 antago-
nists have been identied. At present, only maraviroc is approved
for the treatment of HIV infection [62]. Besides this, vicriviroc [63],
TAK-220 [64] and PF-232798 [65] are undergoing phase II and
phase II clinical trials andappear tobe promisingcandidates for fur-
ther development (Fig. 7). The main concern is that these inhibitors
lead to the emergence of resistant HIV-1 strains [66].
G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514 9
N
N
N
N
NH
2
F
O
P
O
HO
HO
N
N
N
N
NH
2
F
O
P
O
O
N
H
O
O
N
N
N
N
NH
2
O P
O
O
O
O
O
O
O
O
O
.
HO
OH
O
O
Fig. 4. Structures of NtRTIs under clinical trials.
O O
OH
O
O N
N N
Br S
N
H
O
Cl
O
-
K
+
O
O
F
N
H
N
H
O
N
CN
MIV-150 Calanolide A RDEA-806
N
H
Cl
O
NH
2
P
O
O
CN
N
N
N
N
O
O
N
+
O
-
NC
N
H
N
N
N
H
CN
IDX899 BILR 355 BS Rilpivirine
Fig. 5. Structures of NNRTIs undergoing clinical trials.
HO
O
O
OH
O
Fig. 6. Structure of terphenyl derivative.
3.1.7. Integrase inhibitors (INIs)
The enzyme, HIV integrase, catalyzes the integration of the
proviral DNA into the host cell chromosomal DNA. It is a 32kDa
protein comprising of three domains [67]. The key functions of this
enzyme are 3
-end processing and integration [68,69]. The 3
-end
processing takes place after reverse transcription as the cDNA
(or dsDNA) formed, is primed for integration in the cytoplasm
by the trimming of the 3
-ends of the viral DNA by this enzyme.
F
Cl
O
OH
O
HO
O
Fig. 8. Structural formula of integrase inhibitor, elvitegravir, undergoing clinical
trials.
The integrase binds to the viral dsDNA and forms a preintegration
complex. It then cleaves two terminal nucleotides fromeach of the
3
-ends of the DNA. It requires both the integrase and the integrity
of the last 1020 base pairs at both the ends of the viral DNA.
Only one FDA approved HIV-integrase inhibitor, raltegravir is
present and another one, elvitegravir, is under phase III clinical
trials (Fig. 8).
N
O
N
O
Cl
N NH
2
O
N
N
N
O
N
N
O
CF
3
F
H
N
O
N
N
N
N
O
PF-232798 Vicriviroc TAK-220
Fig. 7. Structures of CRIs undergoing clinical trials.
10 G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514
Table 3
Anti-HIV drugs currently undergoing clinical trials.
Drug Manufacturer Class Phase
Elvitegravir Gilead Sciences INIs III
AK-602 Kumamoto University CRIs III
AMD070 AnorMed CRIs II
PF-232798 Pzer CRIs II
Vicriviroc Schering Plough CRIs III
Apricitabine Avexa NRTIs III
Amdoxovir RFS Pharma NRTIs II
Elvucitabine Achillion Pharmaceuticals NRTIs II
Racivir Pharmasset NRTIs II
(+)-Calanolide A Sarawak MediChemPharmaceutics NNRTIs II
IDX899 Idenix Pharma NNRTIs II
RDEA806 Ardea NNRTIs II
Rilpivirine Tibotec NNRTIs II
BILR 355 BS Boehringer Ingelheim NNRTIs II
MIV-150 Medivir, Chiron NNRTIs II
It is doubtless that new anti-HIV drugs are needed with novel
mechanisms of action as these would contribute towards the
broadening of the combinations used in HAART. A number of such
drugs undergoing clinical trials have been summarized in Table 3.
3.2. Combinations of anti-HIV drugs
HAART, the combination therapy, has signicantly decreased
the morbidity and mortality rates in HIV patients [7072]. Cur-
rently, more focus is given on including two or three or even more
drugs targeting the life cycle of HIV. The introduction of HAART in
mid-1990s resulted in increase in the number of tablets to be taken
by the patients, which required an increased drug compliance and
adherence. So efforts are being made to design single formulations
containing more than one drug. Combivir, the rst to be approved,
consists of two NRTIs and is taken as one tablet twice daily. Five
anti-HIV drug combinations are currently being used as shown in
Table4. Theavailabilityof thesedrugcombinations has changedthe
face of anti-HIV drug treatment as a single pill has replaced more
than 10 pills a day. As a result, improvement in adherence to med-
ication is achieved and drug resistance has been lowered, which
has, in turn, improved the quality of life of HIV-positive people.
4. Challenges on the way to successful HAART
The introduction of HAART has achieved tremendous success,
however, still many challenges lay ahead. The main problems faced
currently are the development of resistant strains, toxicity of the
drugs, side effects and lowadherence because of complicated drug
schedule. The challenges before the present treatment can be sum-
marized as:
4.1. Minimizing drug resistance
Suboptimal treatment efcacy and lack of adherence lead to
treatment failure due to the emergence of drug resistance [73].
Thus, the use of potent antiretroviral regimens together with NNR-
TIs and PIs active against drug resistant HIV strains, reduces the
emergence of resistant viral strains. New agents with improved
resistance proles should be explored, for example, the FDCs. The
availabilityof FDCs canhelpimprove the treatment complianceand
reduce further resistance selection.
4.2. Simplication of regimens
To avoid the emergence of resistant strains and suppress viral
replication, it is necessary to achieve a high adherence to HAART
[74]. As soon as the treatment starts, it is necessary to take it for
life but it is quiet a difcult task to maintain [75]. Side effects and
daily life interferences affect adherence to HAART [76,77].
Various strategies are being used to improve adherence, for
example, simplication of drug regimens and newonce-daily xed
dose regimens (FDRs) consisting of tenofovir, FTC, elvitegravir or
GS-9350 or another one consisting of tenofovir DF, FTC and NNRTI
rilpivirine.
4.3. Reduction of side effects
The use of anti-HIV drugs can lead to various toxicities, which,
though not life threatening, can eventually affect the quality of life
and the willingness of the patients to adhere to their regimens. In
some cases, patients may needtochange their initial drugcombina-
tion because of adverse affects. Besides, long-termtoxicities occur
as a result of treatment discontinuation or regimen switching due
to adverse effects. Hence new alternatives with better tolerance
and convenient dose schemes are needed.
Newoptions are nowbeing searched that can alleviate the side
effects and reduce compliance. The growth hormone releasing fac-
tor analogtesamorelinhas shownreductionof adiposetissueinHIV
patients being treated with HAART [78]. Clinical trials are going on
tostudythe effect of uridine, pravastatine andtheir combinationon
the recovery of HAART-associated lipoatrophy. However, minimal
benet has been found in this approach [79].
4.4. Viral reservoirs
These are anatomical sanctuaries of HIV, most often in the brain.
These pose obstacles in the eradication of HIV because most of
anti-HIV drugs fail to cross the BloodBrain-Barrier (BBB). Also the
development of resistant antiretroviral strains canserve as a source
of HIV. In the case of NRTIs, the best drug able to cross the BBB is
AZT and in the case of NNRTIs, nevirapine is the most capable of
crossing the BBB. PIs are not very capable to cross the BBB.
Virtually, almost all anti-HIV drugs are not able to cross the BBB
due to active efux transport [64]. Thus, there is a need for devel-
opment of newanti-HIV drugs, which can effectively cross the BBB
and penetrate the CSF.
5. Future prospects: emerging approaches in the treatment
of HIV infection
Identication and testing of newpotent antiretroviral regimens
are important targets for drug development. The uncertain effects
Table 4
Fixed dose combination pills as approved by FDA.
FDC Components Manufacturer and approval date
Two drug combinations
Combivir AZT (300mg) +3TC (150mg) GlaxoSmithKline; September 27, 1997
Kivexa/Epzicom ABC (600mg) +3TC (300mg) GlaxoSmithKline; August 2, 2004
Truvada TDF (300mg) +FTC (200mg) Gilead Sciences, August 2, 2004
Three drug combinations
Trizivir AZT (300mg) +3TC (150mg) +ABC (300mg) GlaxoSmithKline; November 14, 2000
Atripla TDF (300mg) +RTV (200mg) +efavirenz (600mg) Bristol-Myers Squibb, Gilead Sciences; July 12, 2006
G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514 11
of life-long therapy, requirement of strict adherence and the high
costs of treatment stimulate the exploration of novel approaches
that can potentially be used. Prevention strategies involving
microbicides and antiretroviral prophylaxis, which reduce HIV
transmission rates are being explored extensively [80]. But the best
alternative still would be an efcacious vaccine, the ultimate but
elusive objective for combating the deadly pandemic of AIDS.
5.1. Antiretroviral treatment
The main objective for exploring antiretroviral drugs with new
combinations is to simplify the existing treatment regimens or
to achieve efcacy. NRTIs are the key components of HAART but
these have specic limitations different from other classes of
anti-HIV drugs, like more frequent resistance development and
adverse metabolic effects [81,82]. Probably, with the availability of
new drugs more NRTI-sparing regimen would be explored. It has
been found that NRTI-sparing regimens consisting of novel potent
drugs (for example, raltegravir +etravirine +darunavir/ritonavir)
are attractive options for patients with drug resistance.
One of the newer strategies that have been tested over the years
is maintenance monotherapy. Patients with stable undetectable
viral load while on a combination regimen, may be considered for a
simplied maintenance treatment. Studies have shown that PIs are
more effective for maintenance therapy than NRTIs and NNRTIs.
Moreover, dual combinations of PIs and INIs may be more suit-
able for this therapy [83]. Data fromstudies initially indicated that
delaying the start of therapy, due to adverse effects, resulted in
higher costs and development of resistance. But now it has been
recommended to initiate the treatment at a CD4
+
T cell count of
350 per L or nearby [84]. Recent studies have also shown that
initiating the treatment earlier may prevent or reduce potentially
irreversible immune-systemand end-organ damage.
Novel viral and host targets are being searched, which include
vif-APOBEC3G, integrase-LEDGF andfactors involvedinHIVassem-
bly and maturation [85]. In persistently lymphopenic patients,
normal T-cell counts can be restored by adjuvant therapies. Simi-
larly, agents like interleukin-T have shown to improve the survival
of T-cells, increasing peripheral CD4
+
T lymphocytes in HIV-
infected patients [86].
Use of more advanced diagnostic technologies will help bring
improvements in the use of antiretrovirals. Interpretation of
genotypic data with new phenotypic assays by using improved
algorithms can streamline drug resistance analyses and make them
more affordable. Also, use of new approaches, such as ultra-deep
sequencing for detection of populations of drug-resistant viruses
andultra-sensitiveviral loadassays for monitoringvirus replication
may achieve more widespread use.
5.2. Prevention and prophylaxis
It is probably the only approach for effectively controlling HIV,
which can ultimately lead to the eradication of this deadly virus.
Main focus is now given on the development of preventive vac-
cines. Efforts are going on for development of vaccines for creating
immunity. Besides this, topical microbicides and oral antiretroviral
prophylaxis are also being explored. Additional ways to reduce HIV
transmission include behavioral changes, medical control of STDs
and male circumcision.
Microbicides can be used to avoid infection through sexual
contact. A large number of topical microbicides have been tested
in clinical trials. Partial protection was achieved by PRO2000, a
non-specic entry/fusion inhibitor. But cellulose sulfate gel, 1%
C31G(SAVVY), carraguardandbuffer-gel products failedtoprevent
HIV transmission. A large number of trials with topically applied
antiretroviral agents, such as tenofovir are going on [87,88].
An effective vaccine that can prevent or cure HIV infection
remains the top priority. Several candidates in this aspect have
been developed but none has qualied so far. The main difcul-
ties for an effective vaccine is that HIV inoculum consists of a
geneticallydiversepopulationof quasispecies andthegenerationof
further diversity over the course of infection, which allows effec-
tive immune escape. Both mucosal and systemic immunity must
be elicited by a vaccine to give protection against transmission of
virus into the bloodstream. Besides, an effective HIV vaccine must
elicit robust humoral and cellular responses. The elite controllers, a
small subset of HIV-positive individuals, have an immune system,
which is able to mount potent antibody and cellular responses. The
capacity of HIV to mutate, allows it to develop new mechanisms
of evading the humoral immune system and shielding the major-
ity of the surface envelop glycoproteins, rapidly mutating exposed
epitopes without signicantly affecting the viral replication.
Several trials with combination treatment are being carried
out to reduce MTCT (Mother-to-Child Transmission) during intra-
partum period. Caesarean can further reduce HIV-1 transmission
during intrapartum period. Replacement feeding is often recom-
mended because HIV can be transmitted through breast-feeding.
Use of antiretrovirals during breast-feeding canalso reduce the risk
of transmission. Focus should be given on initiation of antiretrovi-
ral therapy in pregnant mothers with lowCD4
+
T cell counts at the
time of pregnancy and thereafter. The most effective MTCT therapy
involves a combination of three antiretroviral drugs taken during
pregnancy.
The successful HIV prevention strategies include:
active engagement of civil society and religious leaders in a mul-
tisectoral approach
population-based programs designed to change social norms
increased open communication about sexual activities and
HIV/AIDS
programs to combat stigma and discrimination
STI surveillance and control
interventions targeting key bridge populations populations
that transmit the virus fromhigh-risk to low-risk groups.
6. Indian scenario
The second largest country in the world, India, ranks third in
the number of people living with HIV/AIDS. The total number of
people living with HIV/AIDS (PLHA) in India was estimated at 2.27
million(1.933.04) in2009. Children(<15years) account for 3.5%of
all infections, while 83% are in the age group 1549years. Of all HIV
infections, 39%(0.93 million) are among women. The HIVestimates
20082009 highlight an overall reduction in adult HIV prevalence
and HIV incidence (newinfections) in India. At national level, adult
HIV prevalence has declined from 0.41% in 2000 to 0.29% in 2009,
although variations exist across the states. Thus, it is heteroge-
nous in nature. Over the past decade the estimated number of new
annual HIV infections has declined by more than 50%. This has also
been noticed by the Executive Director, UNAIDS as Indias invest-
ments in the AIDS response are producing results. The reason
behind this success story is Indias evidence-informed and human
rights-based approach towards the HIV epidemic. More detailed
information can be had from Annual Report 20092010 released
by The NACO, Department of AIDS Control, Ministry of Health and
FamilyWelfare, Government of India(http://www.nacoonline.org).
6.1. Routes of transmission
Theinfectionmostlyoccurs throughheterosexual routeof trans-
mission(about 87%). The other routes of transmissionare: parent to
12 G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514
Table 5
Classes of drugs available.
NRTIs NNRTIs PIs Fusion inhibitors
AZT
a
Nevirapine
a
Sanquinavir
a
Enfuvirtide (T-20)
D4T
a
Efavirenz
a
Ritonavir
a
3TC
a
Delavirdine Nelnavir
a
ddI
a
Amprenavir
ddC
a
Indinavir
a
ABC
a
Ritonavir
a
FTC Foseamprenavir
TDF
a
(NtRTI) Atazanavir
a
Tipranavir
a
Available in India.
child transmission (5.4%), injecting drug use (1.6%), men having sex
with men (1.5%) and contaminated blood and blood products (1%).
The high-risk groups can be categorized as: Female Sex Workers
(FSW), Men having Sex with Men (MSM) and Transgenders (TG),
Injecting Drug Users (IDU) and bridge populations (migrants and
truckers).
6.2. Response to the epidemic
The initial response to the HIV/AIDS challenge was the setting
up of an AIDS Task Force by the Indian Council of Medical Research
anda National AIDS Committee. AMediumTermPlanwas launched
in 1990 in four states Tamil Nadu, Maharastra, West Bengal and
Manipur to facilitate targeted campaigns, establishment of surveil-
lance systemand safe blood supply. In 1992 National AIDS Control
Programme (NACP-I) was launched. It was implementedfrom1992
to 1999 with an objective to slow down the spread of HIV infec-
tion so as to reduce morbidity, mortality and impact of HIV. To
strengthen the management capacity, National AIDS Control Board
(NACB), National AIDS Control Organization (NACO) and State AIDS
Control Society (SACS) were also set up. InNovember 1999, the sec-
ond National AIDS Control Programme (NACP-II, 19992007) was
launched to reduce the spread of HIV infection in the country and
to increase Indias capacity to respond to HIV/AIDS on a long-term
basis. The overall aimof the thirdNational AIDS Control Programme
(NACP-III), 20072012, is to halt and reverse the epidemic in India
by 2012.
The main objective of NACP-III is to provide free ART to HIV +ve
persons through 250 ART Centres, to achieve and maintain a high
level of drug adherence and to provide care, support and treatment
by establishment of 350 Community Care Centres. There are 240
fully functional ART Centres.
It is also understood that all the patients in need of ART will
not necessarily be accessing government health set-up and a sig-
nicant number will be getting treatment fromprivate sectors and
Non-Government Organizations (NGOs). Thus, NACO is partnering
with Confederation of Indian Industries (CII), Federation of Indian
Chambers of commerce and Industries (FICCI) and other corporate
sectors for the establishment of ART Centres.
The key goals of the national ART programme are to provide
long-termART to eligible patients, to monitor and report treatment
outcomes on quarterly basis, to attain individual drug adherence
rates of 95% or more, to increase the life span so that at least 50%
of patients on ART are alive 3years after starting the treatment and
to ensure that 50% of patients on ART are engaged in or can return
to their previous employment.
The drugs available currently(Table 5) target the virus bymainly
inhibiting the enzymes reverse transcriptase (RT inhibitors) and
protease (protease inhibitors) and preventing fusion of the virus
with CD4 cells (fusion inhibitors).
According to the NACO guidelines, the national programme fol-
lows the following combinations for rst-line regimens.
Table 6
Regimens and alternatives.
First-line regimen Second-line regimen
NRTI component PI component
Standard regimens AZT+3TC TDF +ABC or LPV
+ NVP ddI +ABC or ATV
AZT+3TC TDF +AZT SQV
+ EFV IND
d4T+3TC+NVP NLF
d4T+3TC+EFV
Special circumstances TDF +3TC ddI/ABC or
+ NVP ddI/AZT
TDF +3TC+EFV
1. d4T (30mg) +3TC (150mg)
2. AZT (300mg) +3TC (150mg)
3. d4T (30mg) +3TC (150mg) +Nevirapine (200mg)
4. AZT (300mg) +3TC (150mg) +Nevirapine (200mg)
5. Efavirenz (600mg)
6. Nevirapine (200mg)
Fixed-dose combinations (FDCs), showninTable 6, are preferred
because of ease in using, improved adherence to treatment and
reduction in chances of development of drug resistance. The PIs
are reserved for second-line treatment. Besides this, the patients
with HIV-2 infection do not respond to nevirapine or efavirenz.
Therefore, it has beenrecommendedthat a protease inhibitor based
regimen should be provided for all patients diagnosed with HIV-2.
A large number of research projects on developing effective,
safer and economical microbicides against HIV are ongoing with
nancial assistance from different government organizations, like
Department of Biotechnology (DBT), Indian Council of Medical
Research (ICMR), etc. The authors laboratory is also a contributing
unit under this programme, where several novel NRTIs and NNR-
TIs have been developed on the basis of docking studies of these
molecules with HIV RT, and are being screened for their anti-HIV
activities in India and abroad, as well.
Besides all these, regular campaigns are conducted on mass
media supported by outdoor activities, like music and sports, mid-
media and inter-personal communication on various issues. Red
Ribbon Clubs have been established in colleges and a Red Ribbon
Express Programme covering all the states and 152 halt stations in
the country has beenlaunched to encourage messaging onHIVpre-
vention. A special strategy has also been developed to work closely
with the Tribal Welfare Departments to implement an HIV/AIDS
strategy.
7. Conclusions
The progress made towards the development of anti-HIV drugs
has generated an armory of anti-HIV drugs targeting various stages
of the HIV life cycle. Although the regimens used in HAART have
proventobeeffective, problems of toxicityanddrugresistancehave
limited their use and focus is nowbeing given for the search of new
anti-HIV agents, the next generation drugs.
The major focus of antiretroviral therapy is the same around
the world, however, various factors, like economical, geograph-
ical and political deeply affect the treatment of HIV. Knowledge
of HIV can help prevent this dreaded disease. The counseling and
testing services have received a setback because of fear of knowl-
edge of status as well as sigma and discrimination. As there is an
increase in access to antiretroviral interventions (including MTCT),
it is expected that the opportunities for the testing of HIVwill grow
with newdimensions for a prevention-care continuum.
HIV/AIDS being an exceptional epidemic, demands an excep-
tional response. In spite of several challenges, both scientic and
G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514 13
programmatic, much progress has been achieved in this span of
time. However, it is the need of the hour, as a viable option, to slow
downor halt this pandemic usingantiretroviral treatments, as there
is no protective vaccine or foolproof cure available so far. Thus, the
issues to be focused during the present Highly Active Antiretrovi-
ral Therapy are drug resistance, toxicity, access to viral reservoirs
and, of course, the cost, so that it can be made available to people
in need.
Acknowledgements
Financial assistance for developing this work and JRF to Garima
Kumari from The Department of Biotechnology and Indian Coun-
cil of Medical Research, Government of India, through a research
project grant is sincerely acknowledged.
References
[1] F. Barr-Sinoussi, J.C. Chermann, F. Rey, M.T. Nugeyre, S. Chamaret, J. Gruest, C.
Dauguet, C. Axler-Blin, F. Vzinet-Brun, C. Rouzioux, W. Rozenbaum, L. Montag-
nier, Isolation of a T-lymphotropic retrovirus froma patient at risk for acquired
immune deciency syndrome (AIDS), Science 220 (1983) 868871.
[2] R.C. Gallo, P.S. Sarin, E.P. Gelmann, M. Robert-Guroff, E. Richardson, V.S. Kalya-
naraman, D. Mann, G.D. Sidhu, R.E. Stahl, S. Zolla-Pazner, J. Leibowitch, M.
Popovic, Isolation of human T-cell leukemia virus in acquired immune de-
ciency syndrome (AIDS), Science 220 (1983) 865867.
[3] J.T. King Jr., A.C. Justice, M.S. Roberts, C.C. Chang, J.S. Fusco, Collaboration in HIV
outcomes research U.S. Program Team. Long-term HIV-AIDS survival esti-
mation in the highly active antiretroviral therapy era, Med. Decis. Making 23
(2003) 920.
[4] C.M. Kitchen, S.G. Kitchen, J.A. Dubin, M.S. Gottieb, Initial virological and
immunologic response to highly active antiretroviral therapy predicts long-
termclinical outcome, Clin. Infect. Dis. 33 (2001) 466472.
[5] W.M. Valenti, HAART is a cost-effective and improves outcomes, AIDS Reader
11 (2001) 260262.
[6] A. Carr, Toxicity of antiretroviral therapy and implications for drug develop-
ment, Nat. Rev. Drug Discov. 2 (2003) 624634.
[7] J. Martinez-Picado, M.P. De Pasquale, N. Kartsonis, G.J. Hanna, J. Wong, D. Finzi,
E. Rosenberg, H.F. Gunthard, L. Sutton, A. Savara, C.J. Petropoulos, N. Hellmann,
B.D. Walker, D.D. Richman, R. Siliciano, R.T. DAquila, Antiretroviral resistance
during successful therapy of HIV type 1 infection, Proc. Natl. Acad. Sci. U.S.A.U.
S. A. 97 (2000) 1094810953.
[8] S.J. Little, S. Holte, J.P. Routy, E.S. Daar, M. Markowitz, A.C. Collier, R.A. Koup,
J.W. Mellors, E. Connick, B. Conway, M. Kilby, L. Wang, J.M. Whitcomb, N.S. Hell-
mann, D.D. Richman, Antiretroviral-drug resistance among patients recently
infected with HIV, N. Engl. J. Med. 347 (2002) 385394.
[9] M. Popovic, M.G. Sarngadharan, E. Read, R.C. Gallo, Detection, isolation and
continuous production of cytopathic retroviruses (HTLV-III) frompatients with
AIDS and pre-AIDS, Science 224 (1984) 497500.
[10] S. Broder, The development of antiretroviral therapy and its impact on the
global HIV-1/AIDS pandemic, Antiviral Res. 85 (2010) 118.
[11] H. Mitsuya, K.J. Weinhold, P.A. Furman, St. M.H. Clair, S.N. Lehrman, R.C. Gallo,
D. Bolognesi, D.W. Barry, S. Broder, 3
-Azido-3
-deoxythymidine (BWA509U):
an antiviral agent that inhibits the infectivity and cytopathic effect of human
T-lymphotropic virus type III/lymphadenopathy-associated virus in vitro, Proc.
Natl. Acad. Sci. U.S.A.U. S. A. 82 (1985) 70967100.
[12] C.C. Carpenter, M.A. Fischl, S.M. Hammer, M.S. Hirsch, D.M. Jacobsen, D.A.
Katzenstein, J.S. Montaner, D.D. Richman, M.S. Saag, R.T. Schooley, M.A. Thomp-
son, S. Vella, P.G. Yeni, P.A. Volberding, Antiretroviral therapy for HIV infection
in 1997. Updated recommendations of the International AIDS Society-USA
panel, JAMA 277 (1997) 19621969.
[13] J. Balzarini, G.J. Kang, M. Dalal, P. Herdewijn, E. De Clercq, S. Broder,
D.G. Johns, The anti-HTLV-III (anti-HIV) and cytotoxic activity of 2
,3
-
didehydro-2
,3
-dideoxyribonucleosides: a comparison with their parental
2
,3
-dideoxyribonucleosides, Mol. Pharmacol. 32 (1987) 162167.
[14] S.M. Daluge, S.S. Good, M.B. Faletto, W.H. Miller, St.M.H. Clair, L.R. Boone, M.
Tisdale, N.R. Parry, J.E. Reardon, R.E. Dornsife, D.R. Averett, T.A. Krenitsky,
1592U89, a novel carbocyclic nucleoside analog with potent, selective anti-
human immunodeciency virus activity, Antimicrob. Agents Chemother. 41
(1997) 10821093.
[15] G. Gosselin, R.F. Schinazi, J.P. Sommadossi, C. Mathe, M.C. Bergogne, A.M.
Aubertin, A. Kirn, J.L. Imbach, Antihuman immunodeciency virus activities
of the beta-L enantiomer of 2
,3
-dideoxycytidine and its 5-uoro derivative in
vitro, Antimicrob. Agents Chemother. 38 (1994) 12921297.
[16] R.F. Schinazi, A. McMillan, D. Cannon, R. Mathis, R.M. Lloyd, A. Peck, J.P. Som-
madossi, St M.J. Clair, J. Wilson, P.A. Furman, G. Painter, W.-B. Choi, D.C.
Liotta, Selective inhibition of human immunodeciency viruses by racemates
and enantiomers of cis-5-uoro-1-[2-(hydroxymethyl)-1, 3-oxathiolan-5-
yl]cytosine, Antimicrob. Agents Chemother. 36 (1992) 24232431.
[17] J. Balzarini, Metabolismand mechanismof antiretroviral action of purine and
pyrimidine derivatives, Pharm. World Soc. 16 (1994) 113126.
[18] Z. Hao, D.A. Cooney, D. Farquhar, C.F. Perno, K. Zhang, R. Masood, Y. Wilson, N.R.
Hartman, J. Balzarini, D.G. Johns, DNA chain termination activity and selective
inhibition of human immunodeciency virus reverse transcriptase by 2
,3
-
dideoxyuridine-5
-triphosphate, Mol. Pharmacol. 37 (1990) 157163.
[19] J.M. De Muys, H. Gourdeau, N. Nguyen-Ba, D.L. Taylor, P.S. Ahmed, T. Mansour,
C. Locas, N. Richard, M.A. Wainberg, R.F. Rando, Anti-humanimmunodeciency
virus type 1 activity, intracellular metabolism, andpharmacokinetic evaluation
of 2
-deoxy-3
-oxa-4
-thiocytidine, Antimicrob. Agents Chemother. 43 (1999)
18351844.
[20] R.F. Schinazi, A. McMillan, D. Cannon, R. Mathis, R.M. Lloyd, A. Peck, J.P.
Sommadossi, St.M. Clair, J. Wilson, P.A. Furman, G. Painter, W.-B. Choi, D.C.
Liotta, Selective inhibition of human immunodeciency viruses by racemates
and enantiomers of cis-5-uoro-1-[2-(hydroxymethyl)-1, 3-oxathiolan-5-
yl]cytosine, Antimicrob. Agents Chemother. 36 (1992) 24232431.
[21] H.O. Kim, R.F. Schinazi, K. Shanmuganathan, L.S. Jeong, J.W. Beach, S. Nampalli,
D.L. Cannon, C.K. Chu, L--(2S, 4S)- and L--(2S,4R)-Dioxolanyl nucleosides as
potential anti-HIV agents: asymmetric synthesis and structureactivity rela-
tionships, J. Med. Chem. 36 (1993) 519528.
[22] T.S. Lin, M.Z. Luo, M.C. Liu, S.B. Pai, G.E. Dutschman, Y.C. Cheng, Antiviral activity
of -L()-2
,3
-dideoxy-5-uoro-cytidine (L()ddC) against hepatitis B virus
and human immunodeciency virus type 1 in vitro, Biochem. Pharmacol. 47
(1994) 171174.
[23] R.C. Bethell, Y.S. Lie, N.T. Parkin, In vitro activity of SPD754, a new deoxyc-
itidine nucleoside reverse transcriptase inhibitor (NRTI), against 215 HIV-1
isolates resistant to other NRTIs, Antiviral, Chem. Chemother. 16 (2005)
295302.
[24] Z. Gu, B. Allard, J.M. de Muys, J. Lippens, R.F. Rando, N. Nguyen-Ba, C. Ren, P.
McKenna, D.L. Taylor, R.C. Bethell, In vitro antiretroviral activity and in vitro
toxicity prole of SPD754, a new deoxycytidine nucleoside reverse tran-
scriptase inhibitor for treatment of human immunodeciency virus infection,
Antimicrob. Agents Chemother. 50 (2006) 625631.
[25] P. Cahn, I. Cassetti, R. Wood, P. Phanuphak, L. Shiveley, R.C. Bethell, J.
Sawyer, Efcacy and tolerability of 10-day monotherapy with apricitabine in
antiretroviral-nave, HIV-infected patients, AIDS 20 (2006) 12611268.
[26] S. Cox, S. Moore, J. Southby, A. Alsumbe, Safety prole of apricitabine, a novel
NRTI, during 24-week dosing in experienced HIV-1 infected patients, in: XVII
International AIDS Conference, Mexico City, Mexico, August 38, 2008, abstract
no. TUAB0106.
[27] I. Cassetti, J.V.R. Madruga, J.M.A.H. Suleiman, A. Etzel, L.J. Zhong, A.K. Cheng, J.
Enejosa, The safetyandefcacyof tenofovir DF incombinationwithlamivudine
and efavirenz through 6 years in antiretroviral-nave HIV-1-infected patients,
HIV Clin. Trials 8 (2007) 164172.
[28] J.E. Gallant, S. Straszewski, A.L. Pozniak, E. DeJesus, J.M.A.H. Suleiman, M.D.
Miller, D.F. Coakley, B. Lu, J.J. Toole, A.K. Cheng, Efcacy and safety of tenofovir
DF vs stavudine in combination therapy in antiretroviral-nave patients. A 3-
year randomized trial, JAMA 292 (2004) 191201.
[29] J.R. Arribas, A.L. Pozniak, J.E. Gallant, E. Dejesus, B. Gazzard, R.E. Campo,
S.S. Chen, D. McColl, C.B. Holmes, J. Enejosa, J.J. Toole, A.K. Cheng, Tenofovir
disoproxil fumarate, emtricitabine, and efavirenz compared with zidovu-
dine/lamivudineandefavirenzintreatment-navepatients: 144-weekanalysis,
J. Acquir. Dec. Syndr. 47 (2008) 7478.
[30] T. Cihlar, A. Ray, D. Boojamra, L. Zhang, H. Hui, D. Grant, K. White, M. Desai, N.
Parkin, R. Mackman, GS9148: a novel nucleotide active against HIV-1 variants
with drug resistance mutations in reverse transcriptase, in: 13th Conference
on Retroviruses and Opportunistic Infections, Denver, CO, February 58, 2006,
abstract no. 45.
[31] E. De Clercq, Non-nucleoside reverse transcriptase inhibitors (NNRTIs): past,
present and future, Chem. Biodivers. 1 (2004) 4464.
[32] M. Baba, H. Tanaka, E. DeClercq, R. Pauwels, J. Balzarini, D. Schols, H. Nakashima,
C.-F. Perno, R.T. Walker, T. Miyasaka, Highly specic inhibition of human
immunodeciency virus type 1 by a novel 6-substituted acyclouridine deriva-
tive, Biochem. Biophys. Res. Commun. 165 (1989) 13751381.
[33] V.J. Merluzzi, K.D. Hargrave, M. Labadia, K. Grozinger, M. Skoog, J.C. Wu, C.K.
Shih, K. Eckner, S. Hattox, J. Adams, A.S. Rosenthal, R. Faanes, R.J. Eckner, R.A.
Koup, J.L. Sullvian, Inhibition of HIV-1 replication by a nonnucleoside reverse
transcriptase inhibitor, Science 250 (1990) 14111413.
[34] R. Pauwels, New non-nucleoside reverse transcriptase inhibitors (NNRTIs) in
development for the treatment of HIV infections, Curr. Opin. Pharmacol. 4
(2004) 437446.
[35] R. Pauwels, K. Andries, J. Desmyter, D. Schols, M.J. Kukla, H.J. Breslin, A. Raey-
maeckers, J. Van Gelder, R. Woestenborghs, J. Heykants, K. Schellekens, M.A.C.
Janssen, E. De Clercq, P.A. Janssen, Potent and selective inhibition of HIV-1
replication in vitro by a novel series of TIBO derivatives, Nature 343 (1990)
470474.
[36] K. Andries, M.-p. de Bethune, M.J. Kukla, H. Azijn, P.J. Lewi, P.A.J. Janssen,
R. Pauwels, R165335-TMC125, a novel nonnucleoside reverse transcriptase
inhibitor (NNRTI) with nanomolar activity against NNRTI resistant HIV strains,
in: 40th Interscience Conference on Antimicrobial Agents and Chemotherapy,
Toronto, Canada, September 1720, 2000, abstract no. 1840.
[37] T.J. Dueweke, S.M. Poppe, D.L. Romero, S.M. Swaney, A.G. So, K.M. Downer,
I.W. Althaus, F. Reusser, M. Busso, L. Resnick, D. Mayers, J. Lane, P.A. Aristoff,
R.C. Thomas, W.G. Tarpley, U-90152, a potent inhibitor of human immunod-
eciency virus type 1 replication, Antimicrob. Agents Chemother. 37 (1993)
11271131.
14 G. Kumari, R.K. Singh / HIV & AIDS Review 11 (2012) 514
[38] R.A. Domaoal, L.M. Demeter, Structural and biochemical effects of human
immunodeciency virus mutants resistant to non-nucleoside reverse tran-
scriptase inhibitors, Int. J. Biochem. Cell Biol. 36 (2004) 17351751.
[39] P.A. Janssen, P.J. Lewi, E. Arnold, F. Daeyaert, M. De Jonge, J. Heeres, L. Koy-
mans, M. Vinkers, J. Guillemont, E. Pasquier, M. Kukla, D. Ludovici, K. Andries,
M.P. De Bethune, et al., In search of a novel anti-HIV drug: multidisciplinary
coordination in the discovery of 4-[4-[[4-[(1E)-2, 6-dimethylphenyl]amino]-2-
pyrimidinyl]amino]benzonitrile (R278474, rilpivirine), J. Med. Chem. 48(2005)
19011909.
[40] M.T. Flavin, J.D. Rizzo, A. Khilevich, A. Kucherenko, A.K. Shwinkman, V. Vilay-
chack, L. Lin, W. Chen, E.M. Greenwood, T. Pengsuparp, J.M. Pezzuto, S.H.
Hughes, T.M. Flavin, W.A. Boulanger, R.L. Shone, Z.Q. Xu, Synthesis, chro-
matographic resolution, and anti-human immunodeciency virus activity of
(+)-calanolide A and its enantiomers, J. Med. Chem. 39 (1996) 13031313.
[41] D.D. Richman, C.B. Dousson, R. Storer, A. Moussa, J. Randall, E. Bridges, M. Liuzzi,
J. Jakubik, M. Seifer, D. Standring, IDX12899 and IDX12989, novel NNRTI with
potent anti-HIV activity, enhanced barrier to resistance and favorable phar-
macokinetic prole, in: 14th Conference on Retroviruses and Opportunistic
Infections, Los Angeles, February 2528, 2007, CA abstract 489.
[42] H. Zhang, B. Oberg, D. Bottiger, D. Phillips, J.F. Romeo, M. Thom, L. Vrang, MIV-
150 in a vaginal microbicide with superior anti-HIV activities, in: Presented
at the XV International AIDS Conference, Bangkok, Thailand, July 1216, 2004,
abstract no. TuPeB4667.
[43] J.-L. Girardet, Y.-H. Koh, M. De La Rosa, E. Gunic, Z. Zhang, R. Hamatake, L.
Yeh, The discovery of RDEA806, a potent new HIV NNRTI in phase 1 clinical
trials, in: 47th Annual Interscience Conference on Antimicrobial Agents and
Chemotherapy, Chicago, IL, September 1720, 2007, abstract no. 3285.
[44] P. Bonneau, P. Robinson, J. Duan, L. Doyon, B. Simoneau, C. Yoakim, M. Gar-
neau, M. Bos, M. Cordingley, B. Brenner, B. Spira, M. Wainberg, F. Huang, K.
Drda, C. Ballow, D. Mayers, Antiviral characterization and human experience
withBILR355BS, anovel next-generationnon-nucleosidereversetranscriptase
inhibitor with a broad anti HIV-1 prole, in: 12th Conference on Retroviruses
and Opportunistic Infections, Boston, MA, February 2225, 2005, abstract no.
558.
[45] Z.K. Sweeney, K. Klumpp, Improving non-nucleoside reverse transcriptase
inhibitors for rst-line treatment of HIV infection: the development pipeline
and recent clinical data, Curr. Opin. Drug Discov. Devel. 11 (2008) 458470.
[46] Y. Kashman, K.R. Gustafson, R.W. Fuller, J.H. Cardellina, J.B. McMohan, M.J. Cur-
rens, R.W. Buckheit, S.H. Hughes, G.M. Cragg, M.R. Boyd, HIV inhibitory natural
products. Part 7. The calanolides, a novel HIV-inhibitory class of coumarin
derivative from the tropical rain forest tree, Calophyllum lanigerum, J. Med.
Chem. 35 (1992) 27352743.
[47] E. De Clercq, New approaches towards anti-HIV chemotherapy, J. Med. Chem.
48 (2005) 12971313.
[48] J.M. Molina, A. Hill, Darunavir (TMC114): anewHIV-1proteaseinhibitor, Expert
Opin. Pharmacother. 8 (2007) 19511964.
[49] Z. Temesgen, F. Cainelli, S. Vento, Tipranavir, Drugs Today 41 (2005) 711720.
[50] K. Bragman, Sanquinavir, Adv. Exp. Med. Biol. 394 (1996) 305317.
[51] A.P. Lea, D. Faulds, Ritonavir, Drugs 52 (1996) 541546.
[52] G.L. Plosker, S. Noble, Indinavir: a review of its use in the management of HIV
infection, Drugs 58 (1999) 11651203.
[53] P. Tebas, W.G. Powderly, Nelnvir mesylate, Expert Opin. Pharmacother. 1
(2000) 14291440.
[54] J.C. Adkins, D. Faulds, Amprenavir, Drugs 55 (1998) 837842.
[55] E.M. Mangum, K.K. Graham, Lopinavir-ritonavir: a new protease inhibitor,
Pharmacotherapy 21 (2001) 13521363.
[56] S. Becker, L. Thornton, Fosamprenavir: advancing HIV protease inhibitor treat-
ment options, Expert Opin. Pharmacother. 5 (2004) 19952005.
[57] J.J. Orrick, C.R. Steinhart, Atazanavir, Ann. Pharmacother. 38 (2004) 16641674.
[58] T. Matthews, M. Salgo, M. Greenberg, J. Chung, R. DeMasi, D. Bolognesi, Enfuvir-
tide: the rst therapy to inhibit the entry of HIV-1 into host CD4 lymphocytes,
Nat. Rev. Drug Discov. 3 (2004) 215225.
[59] C. Wild, T. Greenwell, T. Matthews, A synthetic peptide from HIV-1 gp41is a
potent inhibitor of virus-mediatedcell-cell fusion, AIDS Res. Hum. Retroviruses
9 (1993) 10511053.
[60] J.T. Ernst, O. Kutzki, A.K. Debnath, S. Jiang, H. Lu, A.D. Hamilton, Design of a
protein surface antagonist based on alpha-helix mimicry: inhibition of gp41
assembly and viral fusion, Angew. Chem. Int. Ed. 41 (2002) 278281.
[61] E.A. Berger, R.W. Doms, E.M. Fenyo, B.T. Korber, D.R. Littman, J.P. Moore, Q.J.
Sattentau, H. Schuitemaker, J. Sodroski, R.A. Weiss, Anewclassicationfor HIV-
1, Nature 392 (1998) 240.
[62] P. Dorr, M. Westby, S. Dobbs, P. Grifn, B. Irvine, M. Macartney, J. Mori, G. Rick-
ett, C. Smith-Burchnell, C. Napier, R. Webster, D. Armour, D. Price, B. Stammen,
A. Wood, M. Perros, Maraviroc (UK-427, 857), a potent, orally bioavailable and
selective small-molecule inhibitor of chemokines receptor CCR5 with broad-
spectrum anti-human immunodeciency virus type 1 activity, Antimicrob.
Agents Chemother. 49 (2005) 47214732.
[63] J.M. Strizki, C. Tremblay, S. Xu, L. Wojcik, N. Wanger, W. Gonsiorek, R.W. Hip-
kin, C.C. Chou, C. Pugliese-Sivo, Y. Xiao, J.R. Tagat, K. Cox, T. Priestley, S. Sorota,
W. Huang, M. Hirsch, G.R. Reyes, B.M. Baroudy, Discovery and characteriza-
tion of vicriviroc (SCH 417690), a CCR5 antagonist with potent activity against
human immunodeciency virus type 1, Antimicrob. Agents Chemother. 49
(2005) 49114919.
[64] K. Takashima, H. Miyake, N. Kanzaki, Y. Tagawa, X. Wang, Y. Sugihara, Y. Iizawz,
M. Baba, Highly potent inhibition of human immunodeciency virus type 1
replicationby TAK-220, anorally bioavailable small-molecule CCR5 antagonist,
Antimicrob. Agents Chemother. 49 (2005) 34743482.
[65] P. Dorr, M. Westby, L. McFadyen, J. Mori, J. Davis, F. Perruccio, R. Jones, P. Stuppe,
D. Middleton, PF-232798, a second generation Pzer oral CCR5 antagonist, in:
15th Conference on Retroviruses and Opportunistic Infections, Boston, MA,
February 36, 2008, abstract no. 737.
[66] V. Idemyor, Human immunodeciency virus (HIV) entry inhibitors (CCR5 spe-
cic blockers) in development: are they the next novel therapies? HIV Clin.
Trials 6 (2005) 272277.
[67] Y. Pommier, A.A. Johnson, C. Marchand, Integrase inhibitors to treat HIV/AIDS,
Nat. Rev. Drug Discov. 4 (2005) 236248.
[68] R. Craigie, HIV integrase, a brief overview from chemistry to therapeutics, J.
Biol. Chem. 276 (2001) 2321323216.
[69] V. Summa, A. Petrocchi, F. Bonelli, B. Crescenzi, M. Donghi, M. Ferrara, F. Fiore,
C. Gardelli, O.G. Paz, D.J. Hazuda, P. Jones, O. Kinzel, R. Laufer, E. Monteagudo,
E. Muraglia, E. Nizi, F. Orvieto, P. Pace, G. Pescatore, R. Scarpelli, K. Stillmock,
M.V. Witmer, M. Rowley, Discovery of raltegravir, a potent, selective orally
bioavailable HIV-integrase inhibitor for the treatment of HIV-AIDS infection, J.
Med. Chem. 51 (2008) 58435855.
[70] A.S. Fauci, The AIDS epidemic. Considerations for the 21st century, N. Engl. J.
Med. 341 (1999) 10461050.
[71] S.H. Michaels, R. Clark, P. Kissinger, Declining morbidity and mortality among
patients with advanced human immunodeciency virus infection, N. Engl. J.
Med. 339 (1998) 405406.
[72] P.P. Sendi, H.C. Bucher, B.A. Craig, M. Puger, Estimating AIDS-free survival in a
severely immunosuppressed asymptomatic HIV-infected population in the era
of antiretroviral triple combination therapy. Swiss HIV Cohort Study, J. Acquir.
Immune Dec. Syndr. Hum. Retrovirol. 20 (1999) 376381.
[73] L. Menendez-Arias, Molecular basis of Human Immunodeciency Virus drug
resistance: an update, Antiviral Res. 85 (2010) 210231.
[74] L. Osterberg, T. Blaschke, Adherence to medication, N. Engl. J. Med. 353 (2005)
487497.
[75] M.A. Chesney, M. Morin, L. Sherr, Adherence to HIV combination therapy, Soc.
Sci. Med. 50 (2000) 15991605.
[76] S. Mehta, R.D. Moore, N.M. Graham, Potential factors affecting adherence with
HIV therapy, AIDS 11 (1997) 16651670.
[77] N.H. Miller, Compliance with treatment regimens in chronic asymptomatic
diseases, Am. J. Med. 102 (1997) 4349.
[78] J. Falutz, S. Allas, K. Blot, D. Potvin, D. Kotler, M. Somero, D. Berger, S. Brown,
G. Richmond, J. Fessel, R. Turner, S. Grinspoon, Metabolic effects of a growth
hormone-releasing factor in patients with HIV, N. Engl. J. Med. 357 (2007)
23592370.
[79] A. Calmy, B. Hirschel, D.A. Cooper, A. Carr, A new era of antiretroviral drug
toxicity, Antivir. Ther. 14 (2009) 165179.
[80] J. Fox, S. Fidler, Sexual transmission of HIV, Antivirol Res. 85 (2010)
276285.
[81] R.H. Haubrich, S.A. Riddler, A.G. DiRienzo, L. Komarow, W.G. Powderly, K. Kling-
man, K.W. Garren, D.L. Butcher, J.F. Rooney, D.W. Haas, J.W. Mellors, D.V. Havlir,
Metabolic outcomes in a randomized trial of nucleoside, nonnucleoside and
protease inhibitor-sparing regimens for initial HIV treatment, AIDS 23 (2009)
11091118.
[82] S.A Riddler, R. Haubrich, A.G. DiRienzo, L. Peeples, W.G. Powderly, K.L. Kling-
man, K.W. Garren, T. George, J.F. Rooney, B. Brizz, U.G. Lalloo, R.L. Murphy, S.
Swindells, D. Havlir, J.W. Mellors, Class-sparing regimens for initial treatment
of HIV-1 infection, N. Engl. J. Med. 358 (2008) 20952106.
[83] J.E. McKinnon, J.W. Mellors, S. Swindells, Simplication strategies to reduce
antiretroviral drug exposure: progress and prospects, Antivir. Ther. 14 (2009)
112.
[84] A.R. Zolopa, The evolution of HIVtreatment guidelines: current state-of-the art
of ART, Antiviral Res. 85 (2010) 241244.
[85] W.C. Greene, Z. Debyser, Y. Ikeda, E.O. Freed, E. Stephens, W. Yonemoto, R.W.
Buckheit, J.A. Este, T. Cihlar, Novel targets for HIV therapy, Antiviral Res. 80
(2008) 251265.
[86] Y. Levy, C. Lacabaratz, L. Weiss, J.P. Viard, C. Goujard, J.D. Lelievre, F. Boue,
J.M. Molina, C. Rouzioux, V. Avettand-Fenoel, T. Croughs, S. Beq, R. Thiebaut,
G. Chene, M. Morre, J.F. Delfraissy, Enhanced T cell recovery in HIV-1-infected
adults through IL-7 treatment, J. Clin. Invest. 119 (2009) 9971007.
[87] R.W. Buckheit, K.M. Watson, K. Moorrow, A.S. Ham, Development of topical
microbicides to prevent the sexual transmissionof HIV, Antiviral Res. 85 (2010)
142158.
[88] C.J. Elias, L.L. Heise, Challenges for the development of female-controlled vagi-
nal microbicides, AIDS 8 (1994) 110.
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Instant Notes in Medicinal ChemistryDokumen289 halamanInstant Notes in Medicinal ChemistryRini Wulandari100% (2)
- LC Bright BrochureDokumen1 halamanLC Bright Brochureapi-528907705Belum ada peringkat
- Almonds 101 - Nutrition Facts and Health BenefitsDokumen12 halamanAlmonds 101 - Nutrition Facts and Health BenefitsThảo BùiBelum ada peringkat
- CATS & DOGS Nutrition PDFDokumen71 halamanCATS & DOGS Nutrition PDFErald Renz LaurenteBelum ada peringkat
- Bio Set 1 (Answer Key)Dokumen5 halamanBio Set 1 (Answer Key)sajan161106Belum ada peringkat
- Crop Protection 1 Syllabus in The New NormalDokumen14 halamanCrop Protection 1 Syllabus in The New NormalJESRYL PAULITE100% (3)
- Conspectus of The Bulgarian Vascular Flora. Third EditionDokumen454 halamanConspectus of The Bulgarian Vascular Flora. Third EditionBoris AssyovBelum ada peringkat
- B. Tech. Biotech Syllabus MDUDokumen51 halamanB. Tech. Biotech Syllabus MDUVineet50% (4)
- Indian Journals Indexed in Web of Science 14 2019 PDFDokumen5 halamanIndian Journals Indexed in Web of Science 14 2019 PDFRAMAKRISHNA VBelum ada peringkat
- Class 8 - Science - Microorganisms - 6 (Question Bank 1)Dokumen2 halamanClass 8 - Science - Microorganisms - 6 (Question Bank 1)DASHIKA HANDA 13159-12Belum ada peringkat
- Part 1: Math Classroom Environment Strongly Disagree Disagree Agree Strongly AgreeDokumen8 halamanPart 1: Math Classroom Environment Strongly Disagree Disagree Agree Strongly AgreeCy Dollete-SuarezBelum ada peringkat
- Cell WallDokumen4 halamanCell WallSamia KhandkerBelum ada peringkat
- Annotated BibliographyDokumen5 halamanAnnotated Bibliographyapi-272734509Belum ada peringkat
- 1651048027class 7 (Science Notes CH 2 Nutrition in Animals)Dokumen4 halaman1651048027class 7 (Science Notes CH 2 Nutrition in Animals)VijayaLakshmi KuchimanchiBelum ada peringkat
- Axonal Degeneration: Nerve RegenerationDokumen1 halamanAxonal Degeneration: Nerve RegenerationYogi drBelum ada peringkat
- Daftar Pustaka PDFDokumen10 halamanDaftar Pustaka PDFgunawanmulyana12Belum ada peringkat
- MergedDokumen427 halamanMergedNishit kumar100% (1)
- Origami Protein HandoutDokumen4 halamanOrigami Protein HandoutRaajeswaran BaskaranBelum ada peringkat
- Cnvert 1-Halaman-392-397Dokumen6 halamanCnvert 1-Halaman-392-397atma cansBelum ada peringkat
- Environment VS SocietyDokumen9 halamanEnvironment VS SocietyPriyanka PalBelum ada peringkat
- Soni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyDokumen1 halamanSoni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyVishalBelum ada peringkat
- Sex Linked Genes &Dokumen9 halamanSex Linked Genes &Ristner Tacay BalucanagBelum ada peringkat
- Human Papilloma VirusDokumen3 halamanHuman Papilloma Virusxwendnla russiaBelum ada peringkat
- Lecture - Week 3 (Natural Immunity & Complement System)Dokumen5 halamanLecture - Week 3 (Natural Immunity & Complement System)rennel ybarolaBelum ada peringkat
- Clinical MycologyDokumen534 halamanClinical MycologyAlhamra MustafaBelum ada peringkat
- Pathogenesis of Type 1 Diabetes MellitusDokumen12 halamanPathogenesis of Type 1 Diabetes MellitusJIEHASMARTBelum ada peringkat
- 2012 Dse Bio 1 MS 1Dokumen6 halaman2012 Dse Bio 1 MS 1peakBelum ada peringkat
- The Phylum Annelida: A Short IntroductionDokumen3 halamanThe Phylum Annelida: A Short IntroductionTI Journals PublishingBelum ada peringkat
- Reading Comprehension - Life Science StoriesDokumen60 halamanReading Comprehension - Life Science StoriesAndreaBelum ada peringkat
- Phenetic Approaches To Classification: Academy of Natural Sciences, Philadelphia, Pennsylvania 19103Dokumen8 halamanPhenetic Approaches To Classification: Academy of Natural Sciences, Philadelphia, Pennsylvania 19103Trang PhamBelum ada peringkat