Osteoarthritis Poc
Diunggah oleh
Irene Joy GomezDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Osteoarthritis Poc
Diunggah oleh
Irene Joy GomezHak Cipta:
Format Tersedia
IRENE JOY GOMEZ
4NU01 | GROUP 6
OSTEOARTHRITIS
I. DEFINITION
Osteoarthritis is the most common form of arthritis, affecting millions of people around the
world. Often called wear-and-tear arthritis, osteoarthritis occurs when the protective cartilage
on the ends of your bones wears down over time.
While osteoarthritis can damage any joint in your body, the disorder most commonly affects
joints in your hands, neck, lower back, knees and hips.
Osteoarthritis gradually worsens with time, and no cure exists. But osteoarthritis treatments
can slow the progression of the disease, relieve pain and improve joint function.
II. SIGNS & SYMPTOMS
Osteoarthritis symptoms often develop slowly and worsen over time. Signs and symptoms
of osteoarthritis include:
Pain. Your joint may hurt during or after movement.
Tenderness. Your joint may feel tender when you apply light pressure to it.
Stiffness. Joint stiffness may be most noticeable when you wake up in the morning or after a
period of inactivity.
Loss of flexibility. You may not be able to move your joint through its full range of motion.
Grating sensation. You may hear or feel a grating sensation when you use the joint.
Bone spurs. These extra bits of bone, which feel like hard lumps, may form around the
affected joint.
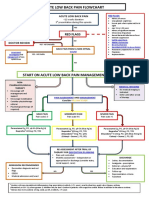
III. PATHOPHYSIOLOGY
Osteoarthritis may be thought as an end result of many factors that, when combined,
predispose the patient to the disease. OA affects the articular cartilage, subchondral bone (the
bony plate that supports the articular cartilage) and synovium. A combination of cartilage
degradation, bone stiffening and reactive inflammation of the synovium occurs. Understand of
OA has been greatly expanded beyond what previously was thought of as simple wear and
tear related to aging. The basic degenerative process in the joint exemplified in OA is presented
in the figure below.
IV. TREATMENT AND MANAGEMENT
There's no known cure for osteoarthritis, but treatments can help to reduce pain and maintain
joint movement.
Medications
Osteoarthritis symptoms can be relieved by a variety of medications, including:
Acetaminophen.Acetaminophen (Tylenol, others) can relieve pain, but it doesn't reduce
inflammation. It has been shown to be effective for people with osteoarthritis who have
mild to moderate pain. Taking more than the recommended dosage of acetaminophen can
cause liver damage.
Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs may reduce inflammation and
relieve pain. Over-the-counter NSAIDs include ibuprofen (Advil, Motrin, others) and
naproxen (Aleve, others). Stronger NSAIDs are available by prescription. NSAIDs can cause
stomach upset, ringing in your ears, cardiovascular problems, bleeding problems, and liver
and kidney damage. Older people have the highest risk of complications.
Mechanical injury
Release of Cytokines
Resulting damage
predispose to further
damage
Stimulation, production,
and release of proteolytic
enzymes,
metalloproteases,
collagenase
Other
Chondrocyte
response
Previous joint damage
Genetic and hormonal
factors
Narcotics. These types of prescription medication typically contain ingredients similar to
codeine and may provide relief from more severe osteoarthritis pain. These stronger
medications carry a risk of dependence, though that risk is thought to be small in people
who have severe pain. Side effects may include nausea, constipation and sleepiness.
Therapy
A combination approach to treatment often works best. Your doctor may suggest:
Physical therapy. A physical therapist can work with you to create an individualized exercise
regimen that will strengthen the muscles around your joint, increase the range of motion in
your joint and reduce your pain.
Occupational therapy. An occupational therapist can help you discover ways to do everyday
tasks or do your job without putting extra stress on your already painful joint. For instance,
a toothbrush with a large grip could make brushing your teeth easier if you have finger
osteoarthritis. A bench in your shower could help relieve the pain of standing if you have
knee osteoarthritis.
Braces or shoe inserts. Consider trying splints, braces, shoe inserts or other medical devices
that can help reduce your pain. These devices can immobilize or support your joint to help
you keep pressure off it.
A chronic pain class. The Arthritis Foundation and some medical centers have classes for
people with osteoarthritis and chronic pain. Ask your doctor about classes in your area or
check with the Arthritis Foundation. These classes teach skills that help you manage your
osteoarthritis pain. And you'll meet other people with osteoarthritis and learn their tips and
tricks for reducing and coping with joint pain.
Surgical and other procedures
If conservative treatments don't help, you may want to consider procedures such as:
Cortisone shots. Injections of corticosteroid medications may relieve pain in your joint.
During this procedure your doctor numbs the area around your joint, then places a needle
into the space within your joint and injects medication. The number of cortisone shots you
can receive each year is limited, because the medication can worsen joint damage over
time.
Lubrication injections. Injections of hyaluronic acid derivatives (Hyalgan, Synvisc) may offer
pain relief by providing some cushioning in your knee. These agents are similar to a
component normally found in your joint fluid.
Realigning bones. During a surgical procedure called an osteotomy, the surgeon cuts across
the bone either above or below the knee to realign the leg. Osteotomy can reduce knee pain
by shifting your body weight away from the worn-out part of your knee.
Joint replacement. In joint replacement surgery (arthroplasty), your surgeon removes your
damaged joint surfaces and replaces them with plastic and metal devices called prostheses.
The hip and knee joints are the most commonly replaced joints. Surgical risks include
infections and blood clots. Artificial joints can wear out or come loose and may need to
eventually be replaced.
V. DIAGNOSTIC EXAM
During the physical exam, your doctor will closely examine your affected joint, checking for
tenderness, swelling or redness. He or she will also check the joint's range of motion. Your
doctor may also recommend imaging and lab tests.
Imaging tests
Pictures of the affected joint can be obtained during imaging tests. Examples include:
X-rays. Cartilage doesn't show up on X-ray images, but the loss of cartilage is revealed by a
narrowing of the space between the bones in your joint. An X-ray may also show bone spurs
around a joint. Many people have X-ray evidence of osteoarthritis before they experience
any symptoms.
Magnetic resonance imaging (MRI). MRI uses radio waves and a strong magnetic field to
produce detailed images of bone and soft tissues, including cartilage. This can be helpful in
determining what exactly is causing your pain.
Lab tests
Analyzing your blood or joint fluid can help pinpoint the diagnosis.
Blood tests. Blood tests may help rule out other causes of joint pain, such as rheumatoid
arthritis.
Joint fluid analysis. Your doctor may use a needle to draw fluid out of the affected joint.
Examining and testing the fluid from your joint can determine if there's inflammation and if
your pain is caused by gout or an infection.
VI. NURSING CARE
1. Administer anti-inflammatory medication and other drugs as ordered.
2. Provide emotional support and reassurance to help the patient cope with limited
mobility.
3. Encourage the patient to perform as much self-care as his immobility and pain allow.
4. To help promote sleep, adjust pain medications to allow for maximum rest.
5. Help the patient identify techniques and activities that promote rest and relaxation.
6. For joints in hand, provide hot soaks and paraffin dips to relieve pain as ordered.
7. Check crutches, cane, braces, or walker for proper fit.
8. Assess the patients pain patterns.
9. Watch for skin irritation caused by prolonged use of assistive devices.
10. Instruct the patient to plan for adequate rest during the day.
11. Instruct the patient to take medications exactly as prescribed.
Anda mungkin juga menyukai
- Osteoarthritis: Applied Medicine BY: Dr. Kinza IftikharDokumen16 halamanOsteoarthritis: Applied Medicine BY: Dr. Kinza IftikharsabaamjadBelum ada peringkat
- Osteoarthtritis Symptoms: Older Age. The Risk of Osteoarthritis Increases With AgeDokumen4 halamanOsteoarthtritis Symptoms: Older Age. The Risk of Osteoarthritis Increases With AgeJessica AdhykaBelum ada peringkat
- Osteoarthritis EssayDokumen8 halamanOsteoarthritis EssayMeysha PBelum ada peringkat
- Osteoarthritis - Surgical Therapy, Alternative Medicine and Proper ExerciseDokumen5 halamanOsteoarthritis - Surgical Therapy, Alternative Medicine and Proper ExerciseElsa Novi WulansariBelum ada peringkat
- YOU Don'T Have To Live With Joint Pain: A Patient'S Guide To The Causes and Treatment of Joint PainDokumen18 halamanYOU Don'T Have To Live With Joint Pain: A Patient'S Guide To The Causes and Treatment of Joint PainbaboosabBelum ada peringkat
- OSTEOARTHRITISDokumen42 halamanOSTEOARTHRITISDaisy R. Lim100% (2)
- Osteoarthritis: T Person's of Developing Osteoarthritis. It IncludesDokumen5 halamanOsteoarthritis: T Person's of Developing Osteoarthritis. It IncludesLove Shery SabrosoBelum ada peringkat
- Arthritis Guide: Causes, Symptoms and Treatment OptionsDokumen54 halamanArthritis Guide: Causes, Symptoms and Treatment OptionsPeby M. Ramdhan100% (1)
- Osteoarthritis: Done By: Shameem Faheem Group 6Dokumen32 halamanOsteoarthritis: Done By: Shameem Faheem Group 6Alisha ShamsBelum ada peringkat
- Arthritis of The Knee - OrthoInfo - AAOSDokumen5 halamanArthritis of The Knee - OrthoInfo - AAOSMarcelo KrauseBelum ada peringkat
- Osteoarthritis: CausesDokumen5 halamanOsteoarthritis: CausesYahya i.nBelum ada peringkat
- Cotul Reumatic EnglezaDokumen7 halamanCotul Reumatic EnglezaElena GaneaBelum ada peringkat
- OsteoarthritisDokumen5 halamanOsteoarthritisRobby Dwitria MaulanaBelum ada peringkat
- Arthritis - Diagnosis and Treatment - Mayo ClinicDokumen1 halamanArthritis - Diagnosis and Treatment - Mayo Clinicpoppie0321Belum ada peringkat
- Joint DisordersDokumen39 halamanJoint DisordersangelaBelum ada peringkat
- Osteoarthritis of The Knee - Patient Information and Exercises - PHYSIO 001Dokumen5 halamanOsteoarthritis of The Knee - Patient Information and Exercises - PHYSIO 001Zola Ismu ArjunantoBelum ada peringkat
- Mayumi - How To Cure OsteoarthritisDokumen4 halamanMayumi - How To Cure OsteoarthritisMayumi SariputraBelum ada peringkat
- Aunty ProjectDokumen13 halamanAunty Projectdevansh kumarBelum ada peringkat
- A Review of Arthritis and Its ManagementDokumen19 halamanA Review of Arthritis and Its ManagementPavithra GBelum ada peringkat
- KneeDokumen3 halamanKneedoos1Belum ada peringkat
- Erbil Polytechnic University Erbil Health Technical College Physiotherapy Department Study Year 2020-2021Dokumen13 halamanErbil Polytechnic University Erbil Health Technical College Physiotherapy Department Study Year 2020-2021Muhamad SdeqBelum ada peringkat
- Oa Dedos PieDokumen3 halamanOa Dedos PieWalter PelaezBelum ada peringkat
- Arthritis Joint Pain ReliefDokumen14 halamanArthritis Joint Pain ReliefSam CookBelum ada peringkat
- OsteoarthritisDokumen17 halamanOsteoarthritisNishaThakuriBelum ada peringkat
- OsteoarthritisDokumen4 halamanOsteoarthritisdrnareshBelum ada peringkat
- Arthritis Types and Treatments ExplainedDokumen10 halamanArthritis Types and Treatments ExplainedMuiz SaddozaiBelum ada peringkat
- Degenerative Joint Disease: OsteoarthritisDokumen15 halamanDegenerative Joint Disease: OsteoarthritiseqnaluleBelum ada peringkat
- What Causes Osteoarthritis?Dokumen9 halamanWhat Causes Osteoarthritis?jajabsBelum ada peringkat
- Osteoarthritis Report Details Causes, Symptoms, and TreatmentDokumen6 halamanOsteoarthritis Report Details Causes, Symptoms, and TreatmentJoe Aire SalvediaBelum ada peringkat
- Dr. Jonaidi T, SPKFR Instalasi Rehabilitasi Medik Rsud Dr. Soedarso, PontianakDokumen29 halamanDr. Jonaidi T, SPKFR Instalasi Rehabilitasi Medik Rsud Dr. Soedarso, PontianakHerlam SyahBelum ada peringkat
- Arthritis PDFDokumen4 halamanArthritis PDFArchana MoreyBelum ada peringkat
- Arthritis AdviceDokumen6 halamanArthritis Adviceapi-309082881Belum ada peringkat
- Osteoarthritis DissertationDokumen8 halamanOsteoarthritis DissertationPaperHelpJackson100% (1)
- Common Causes of Severe Knee PainDokumen8 halamanCommon Causes of Severe Knee PainRatnaPrasadNalamBelum ada peringkat
- ArthritisDokumen2 halamanArthritisannak143Belum ada peringkat
- Arthritis HWDokumen9 halamanArthritis HWraphaelBelum ada peringkat
- Knee Pain: Treating Knee Pain: Preventing Knee Pain: Natural Remedies, Medical Solutions, Along With Exercises And Rehab For Knee Pain ReliefDari EverandKnee Pain: Treating Knee Pain: Preventing Knee Pain: Natural Remedies, Medical Solutions, Along With Exercises And Rehab For Knee Pain ReliefPenilaian: 5 dari 5 bintang5/5 (1)
- Tennis Elbow, Golfer's Elbow, Arthritis GuideDokumen21 halamanTennis Elbow, Golfer's Elbow, Arthritis GuideJalil AhmadBelum ada peringkat
- OsteoarthritisDokumen23 halamanOsteoarthritisGoutham VGouthamBelum ada peringkat
- مقالة عن تغير مفصل الركبةDokumen4 halamanمقالة عن تغير مفصل الركبةDr-Mohammed AdelBelum ada peringkat
- 3 LWG Knee Pain Part 1Dokumen1 halaman3 LWG Knee Pain Part 1Woo Guan LeeBelum ada peringkat
- OsteoarthritisDokumen63 halamanOsteoarthritisDuaa BalochBelum ada peringkat
- Arthritis (Cabansag, Ma. Flor-And-Cabansag, Joyce)Dokumen38 halamanArthritis (Cabansag, Ma. Flor-And-Cabansag, Joyce)Carlojay IniegoBelum ada peringkat
- History and Physical Examination: Rheumatoid ArthritisDokumen12 halamanHistory and Physical Examination: Rheumatoid ArthritisNolar Gamboa AglipayBelum ada peringkat
- Jurnal Tennis ElbowDokumen5 halamanJurnal Tennis ElbowMuhamad Fahrizal RilahiBelum ada peringkat
- Causes and Tips For Coping With Chronic Knee PainDokumen6 halamanCauses and Tips For Coping With Chronic Knee PainRatnaPrasadNalamBelum ada peringkat
- Homeopathy For Joint PainsDokumen3 halamanHomeopathy For Joint PainsstarhomeoBelum ada peringkat
- OESTEOARTHRITIS Joint Pain Sidha Medicine HerbsDokumen5 halamanOESTEOARTHRITIS Joint Pain Sidha Medicine HerbsDURAI RAJBelum ada peringkat
- Oeste o ArthritisDokumen5 halamanOeste o Arthritisdr amitBelum ada peringkat
- Osteoarthritis NotesDokumen11 halamanOsteoarthritis Notesjesmitha2740Belum ada peringkat
- Osteoarthritis ExplanationDokumen6 halamanOsteoarthritis ExplanationmedicembuBelum ada peringkat
- All About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsDari EverandAll About Arthritis- Find Updated Causes, Symptoms, Diagnostic Tests, New Alternative Treatments, Cures and BreakthroughsBelum ada peringkat
- Name Seat #: Class: Assignment On Submitted To: EBP2001051 1 Year Eve (A) Joint DisordersDokumen11 halamanName Seat #: Class: Assignment On Submitted To: EBP2001051 1 Year Eve (A) Joint DisordersAbdul WasayBelum ada peringkat
- Osteoarthritis Symptoms, Causes and TreatmentDokumen6 halamanOsteoarthritis Symptoms, Causes and TreatmentgovindhaBelum ada peringkat
- OsteoarthritisDokumen6 halamanOsteoarthritisgovindhaBelum ada peringkat
- How To Identify and Treat Inner Knee PainDokumen6 halamanHow To Identify and Treat Inner Knee PainRatnaPrasadNalamBelum ada peringkat
- Osteoarthritis New-UpdatedDokumen2 halamanOsteoarthritis New-Updatedshadowfax885Belum ada peringkat
- Your Joint Pain and Treatment Options: Steven L. Drayer M.D. Private Practice-Lansing/Sparrow HospitalDokumen72 halamanYour Joint Pain and Treatment Options: Steven L. Drayer M.D. Private Practice-Lansing/Sparrow Hospitalspinalcord123439Belum ada peringkat
- Shoulder Pain and Common Shoulder ProblemsDokumen14 halamanShoulder Pain and Common Shoulder ProblemsRatnaPrasadNalamBelum ada peringkat
- Osteoarthritis: Natural Drugless Treatments That Really Work!Dari EverandOsteoarthritis: Natural Drugless Treatments That Really Work!Belum ada peringkat
- Hodgkin's Disease Treatment Options by StageDokumen2 halamanHodgkin's Disease Treatment Options by StageIrene Joy GomezBelum ada peringkat
- Everything You Need to Know About BananasDokumen10 halamanEverything You Need to Know About BananasIrene Joy GomezBelum ada peringkat
- Everything You Need to Know About CarrotsDokumen10 halamanEverything You Need to Know About CarrotsIrene Joy GomezBelum ada peringkat
- Case 3Dokumen14 halamanCase 3Irene Joy GomezBelum ada peringkat
- Stab Wound: For Other Uses, SeeDokumen3 halamanStab Wound: For Other Uses, SeeIrene Joy GomezBelum ada peringkat
- Strawberry FactsDokumen8 halamanStrawberry FactsIrene Joy GomezBelum ada peringkat
- Reducible HerniaDokumen1 halamanReducible HerniaIrene Joy GomezBelum ada peringkat
- A. Family Health HistoryDokumen2 halamanA. Family Health HistoryIrene Joy GomezBelum ada peringkat
- Performance Outcome Activities EvaluationDokumen1 halamanPerformance Outcome Activities EvaluationIrene Joy GomezBelum ada peringkat
- Case DDokumen2 halamanCase DIrene Joy GomezBelum ada peringkat
- Case ZDokumen2 halamanCase ZIrene Joy GomezBelum ada peringkat
- Improve Patient Satisfaction and Staff EngagementDokumen2 halamanImprove Patient Satisfaction and Staff EngagementIrene Joy GomezBelum ada peringkat
- Case CDokumen1 halamanCase CIrene Joy GomezBelum ada peringkat
- Case eDokumen2 halamanCase eIrene Joy GomezBelum ada peringkat
- Case BDokumen2 halamanCase BIrene Joy GomezBelum ada peringkat
- AnemiaDokumen6 halamanAnemiaIrene Joy Gomez100% (1)
- Case ADokumen3 halamanCase AIrene Joy GomezBelum ada peringkat
- Study Pinpoints Issues That Leave ED Nurses Vulnerable: Sunday February 9, 2014Dokumen2 halamanStudy Pinpoints Issues That Leave ED Nurses Vulnerable: Sunday February 9, 2014Irene Joy GomezBelum ada peringkat
- Anatomy and PhysiologyDokumen10 halamanAnatomy and PhysiologyIrene Joy GomezBelum ada peringkat
- Study Pinpoints Issues That Leave ED Nurses Vulnerable: Sunday February 9, 2014Dokumen2 halamanStudy Pinpoints Issues That Leave ED Nurses Vulnerable: Sunday February 9, 2014Irene Joy GomezBelum ada peringkat
- AnemiaDokumen6 halamanAnemiaIrene Joy Gomez100% (1)
- Drug Action Contraindication /indication Adverse Effect Nursing ResponsibilityDokumen1 halamanDrug Action Contraindication /indication Adverse Effect Nursing ResponsibilityIrene Joy GomezBelum ada peringkat
- Google GlassDokumen8 halamanGoogle GlassIrene Joy GomezBelum ada peringkat
- AnemiaDokumen6 halamanAnemiaIrene Joy Gomez100% (1)
- RenalDokumen3 halamanRenalIrene Joy GomezBelum ada peringkat
- PPPDokumen2 halamanPPPIrene Joy GomezBelum ada peringkat
- Path o PhysiologyDokumen1 halamanPath o PhysiologyIrene Joy GomezBelum ada peringkat
- Disturbed Thought Process Decreased Attention Span and Difficulty in Concentration Related To Accelerated ThinkingDokumen1 halamanDisturbed Thought Process Decreased Attention Span and Difficulty in Concentration Related To Accelerated ThinkingIrene Joy GomezBelum ada peringkat
- Health TeachingsDokumen8 halamanHealth TeachingsIrene Joy GomezBelum ada peringkat
- Nursing Theory CåonservationDokumen1 halamanNursing Theory CåonservationIrene Joy GomezBelum ada peringkat
- Acute Low Back Pain Flowchart January 2017Dokumen1 halamanAcute Low Back Pain Flowchart January 20171234chocoBelum ada peringkat
- Moving Away From Knee Osteoarthritis - Harvard HealthDokumen1 halamanMoving Away From Knee Osteoarthritis - Harvard HealthOctavio LópezBelum ada peringkat
- MY MD Patent Synthetic Cannabinoid Compounds For Treatment of Epilepsy, Substance Addiction and Alzheimer's DiseaseDokumen14 halamanMY MD Patent Synthetic Cannabinoid Compounds For Treatment of Epilepsy, Substance Addiction and Alzheimer's DiseaseCharles GrossBelum ada peringkat
- Pharma For StudentsDokumen23 halamanPharma For StudentsDominic Reambonanza0% (1)
- LansaprozolDokumen178 halamanLansaprozolapi-2519793100% (2)
- 2138531.PA0013 - 088 - 001..000001cataflam 25mg and 50mg REG PIL PF12-51 For IMB Website.140213 PDFDokumen8 halaman2138531.PA0013 - 088 - 001..000001cataflam 25mg and 50mg REG PIL PF12-51 For IMB Website.140213 PDFMALAHIM RAUFBelum ada peringkat
- Is COVID-19 A Bioweapon? A Special Interview With Dr. Richard M. FlemingDokumen24 halamanIs COVID-19 A Bioweapon? A Special Interview With Dr. Richard M. FlemingTdale100% (1)
- A Fi Sau NuDokumen7 halamanA Fi Sau NumicleanBelum ada peringkat
- Nonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinDokumen13 halamanNonsteroidal Antiinflammatorydrugsfor Acuteandchronicpain: Timothy J. Atkinson,, Jeffrey FudinMaBe MejíaBelum ada peringkat
- NSAIDSDokumen7 halamanNSAIDSDjev David DazaBelum ada peringkat
- Understanding Cancer Pain 2021Dokumen68 halamanUnderstanding Cancer Pain 2021AnestilBelum ada peringkat
- How RA Affects Joints and Other Parts of the BodyDokumen10 halamanHow RA Affects Joints and Other Parts of the Bodysen_subhasis_58Belum ada peringkat
- Sindrome MiofacialDokumen13 halamanSindrome MiofacialAngie Paola RodriguezBelum ada peringkat
- Drug CardsDokumen38 halamanDrug CardsJason D Wilkins92% (25)
- What Inpatient Treatments Do We Have For Acute Intractable MigraineDokumen3 halamanWhat Inpatient Treatments Do We Have For Acute Intractable Migrainetsiko111Belum ada peringkat
- Final ProjectDokumen33 halamanFinal ProjectShowmiya NBelum ada peringkat
- Treating and Preventing Ear Infections in ChildrenDokumen4 halamanTreating and Preventing Ear Infections in ChildrenbehrangBelum ada peringkat
- Livng With CirrhosisDokumen16 halamanLivng With CirrhosisN. Hansraj100% (1)
- USPI - Med Guide - Feldene - Piroxicam - CapsulesDokumen15 halamanUSPI - Med Guide - Feldene - Piroxicam - CapsulesDini FarhatunnabilahBelum ada peringkat
- NSAIDsDokumen34 halamanNSAIDsAliImadAlKhasaki75% (4)
- Various Drugs Used in Paediatric DentistryDokumen56 halamanVarious Drugs Used in Paediatric DentistryPo PowBelum ada peringkat
- OTC Bulletin PDFDokumen24 halamanOTC Bulletin PDFLungu DianaBelum ada peringkat
- MSM Information BookletDokumen36 halamanMSM Information Bookletzimko100% (3)
- NUR149 Syphilis Case StudyDokumen30 halamanNUR149 Syphilis Case StudyVenia Mae SarayanBelum ada peringkat
- Safety Comparison of NSAIDsDokumen16 halamanSafety Comparison of NSAIDsSuraj SubediBelum ada peringkat
- Acetylsalicilic Acid 100mg (Aspirin Cardio, Micropirin, Cartia, Tevapirin, Godamed)Dokumen8 halamanAcetylsalicilic Acid 100mg (Aspirin Cardio, Micropirin, Cartia, Tevapirin, Godamed)asdwasdBelum ada peringkat
- Anti Inflamasi Dan ANALGETIK (Anti Nociceptive)Dokumen30 halamanAnti Inflamasi Dan ANALGETIK (Anti Nociceptive)SEPTIANA SAPUTRIBelum ada peringkat
- Engineering Ethics Case StudyDokumen5 halamanEngineering Ethics Case Studyijaz aliBelum ada peringkat
- 5 6066812399917203502 PDFDokumen8 halaman5 6066812399917203502 PDFAnindya Nandini IndriasariBelum ada peringkat
- ProbDokumen5 halamanProbMa Christina Miravalles SergioBelum ada peringkat