Vasc Med 2011 Subramaniam 87 95
Diunggah oleh
Uswa MalikHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Vasc Med 2011 Subramaniam 87 95
Diunggah oleh
Uswa MalikHak Cipta:
Format Tersedia
http://vmj.sagepub.
com/
Vascular Medicine
http://vmj.sagepub.com/content/16/2/87
The online version of this article can be found at:
DOI: 10.1177/1358863X11400781
2011 16: 87 originally published online 29 March 2011 Vasc Med
Kai Chew, Tien Y Wong and E. Shyong Tai
Tavintharan Subramaniam, Ei Ei Khaing Nang, Su Chi Lim, Yi Wu, Chin Meng Khoo, Jeannette Lee, Derrick Heng, Suok
Asian population
brachial index and the risk factors of peripheral artery disease in a multi-ethnic Distribution of ankle
Published by:
http://www.sagepublications.com
On behalf of:
Society for Vascular Medicine
can be found at: Vascular Medicine Additional services and information for
http://vmj.sagepub.com/cgi/alerts Email Alerts:
http://vmj.sagepub.com/subscriptions Subscriptions:
http://www.sagepub.com/journalsReprints.nav Reprints:
http://www.sagepub.com/journalsPermissions.nav Permissions:
http://vmj.sagepub.com/content/16/2/87.refs.html Citations:
What is This?
- Mar 29, 2011 OnlineFirst Version of Record
- Apr 20, 2011 Version of Record >>
by guest on June 30, 2014 vmj.sagepub.com Downloaded from by guest on June 30, 2014 vmj.sagepub.com Downloaded from
1
Department of Medicine, Khoo Teck Puat Hospital, Singapore
2
Department of Epidemiology and Public Health, Yong Loo Lin School of
Medicine, National University of Singapore, Singapore
3
Department of Medicine, National University Hospital, Singapore
4
Epidemiology and Disease Control Division, Ministry of Health,
Singapore
5
Centre for Eye Research Australia, University of Melbourne,
Melbourne, Victoria, Australia
6
Singapore Eye Research Institute, Yong Loo Lin School of Medicine,
National University of Singapore, Singapore
Corresponding author:
S Tavintharan
Department of Medicine
Khoo Teck Puat Hospital
90 Yishun Central
Singapore 768828
Singapore
Email: subramaniam.tavintharan@alexandrahealth.com.sg
Vascular Medicine
16(2) 8795
The Author(s) 2011
Reprints and permission: sagepub.
co.uk/journalsPermissions.nav
DOI: 10.1177/1358863X11400781
vmj.sagepub.com
Distribution of anklebrachial index and
the risk factors of peripheral artery disease
in a multi-ethnic Asian population
Tavintharan Subramaniam
1
, Ei Ei Khaing Nang
2
, Su Chi Lim
1
,
Yi Wu
2
, Chin Meng Khoo
3
, Jeannette Lee
2
, Derrick Heng
4
,
Suok Kai Chew
4
, Tien Y Wong
5,6
and E Shyong Tai
2,3
Abstract
Peripheral artery disease (PAD) is a manifestation of systemic atherosclerosis and is associated with increased
cardiovascular morbidity and mortality. We describe the prevalence and risk factors of PAD in a multi-ethnic Asian
population (Chinese, Malays and Indians) in Singapore. The Singapore Prospective Study Program recruited 4132
individuals between 2004 and 2006 in which the anklebrachial index (ABI) was measured using the Smartdop 20EX
bi-directional blood flow detector. PAD was defined as 0.9 and a high ABI > 1.4, with ABI 1.111.20 as reference. The
mean age (SD) of individuals in the study was 49.9 (11.8) years, with 51.8% females. PAD was present in 4.3% of the
population and a high ABI (> 1.4) was rare. Malays and Indians had a higher risk (especially in females). Compared to
those with an ABI between 1.11 and 1.20, those with PAD were more likely to be of Malay and Indian ethnicity, female
sex, with higher systolic blood pressure and pulse pressure, with increased prevalence of diabetes mellitus, hypertension,
albuminuria and renal impairment, and with a past history of stroke. In conclusion, in this large multi-ethnic Asian
population, we document the distribution and risk factor associations for PAD. PAD shows an ethnic distribution similar
to that of coronary artery disease in Singapore, with differences in sex distribution. Apart from traditional vascular risk
factors, pulse pressure, renal impairment and a past history of stroke are important determinants of PAD.
Keywords
anklebrachial index; distribution; peripheral artery disease; risk factors
Introduction
The anklebrachial index (ABI), the ratio of systolic blood
pressure at the ankle to that in the arm, has been shown in stud-
ies to predict cardiovascular diseases (CVD) and mortality.
13
Because the measurement of ABI is non-invasive, relatively
inexpensive and quick, recent guidelines by the American Heart
Association and the American College of Cardiology, among
others, have suggested that measurement of ABI should be
considered for the purposes of cardiovascular risk assessment.
The cut-offs for defining ABI risk, however, have
remained controversial. An ABI lower than 0.9 or 1.0 has
been used for many years to define peripheral artery dis-
ease (PAD) in the legs.
2,4
Studies have shown that low ABI
below these cut-offs, not only predicts poorer walking
endurance,
5
but is also associated with CVD risk factors
and predicts CVD events. More recently, however, it is rec-
ognized that the relationship between ABI and CVD and
mortality may be non-linear. Studies carried out in native
and elderly Americans
6,7
and a meta-analysis of 16 popula-
tion cohort studies,
8
suggests there exists a J or U-shaped
association in which both low and high ABI are associated
with increased cardiovascular morbidity and mortality.
Most previous studies have been conducted in Western
populations, and there are limited data on the distribution of
ABI and the relationship with CVD risk factors in Asian
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
88 Vascular Medicine 16(2)
populations. It has been suggested that the distribution of
ABI varies by race/ethnicity. In the Strong Heart study,
among 4393 American Indians, high ABI was more com-
mon than low ABI.
7
In contrast, in other US and European
white populations,
6,8
high ABI was less common than low
ABI. There are further variations in the distribution of ABI
among white, black, Hispanic and Chinese individuals.
9,10
The aims of this study were to describe the distribution
of ABI in a multi-ethnic Asian population of Chinese,
Malays and Indians (three major racial/ethnic groups in
Asia) in Singapore and to examine the risk factor profiles
associated with PAD in this population.
Methods
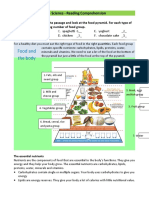
Study design and population
The Singapore Prospective Study Program is a population-
based cross-sectional study of CVD in a multi-ethnic popu-
lation in Singapore, previously described in detail,
1113
and
illustrated in Figure 1. In brief, we invited 10,747
subjects from four previously conducted population-based
cross-sectional surveys carried out in Singapore (1982
1998) to participate in a repeat examination between 2004
and 2007.
1417
Briefly, all studies included a random
sample of individuals from the Singapore population, with
disproportionate sampling stratified by ethnicity to increase
the number in the minority ethnic groups (Malays and
Asian Indians). All subjects were interviewed in their
homes and were subsequently invited to attend a health
examination for additional tests and collection of biological
specimens. In total, 7744 (76.8% response rate) subjects
were interviewed, and 5164 (66.7%) attended the health
examination. During the period 2 April 2005 up to 20
February 2006, owing to limitations in resources, examina-
tion of ABI was carried out only for every alternate
Chinese participant. However, in order to maintain ade-
quate numbers for other ethnic groups, all subjects who
were non-Chinese had ABI measured.
Thyroid and Heart Study
1982 1984
(N = 2034)
National University of
Singapore Heart Study
1993 1995
(N = 982)
National Health
Survey
1992
(N = 3568)
National Health
Survey
1998
(N = 4723)
Total of 10,747 Subjects
Available for the Study
10,080 Subjects Eligible
559 Died
102 Errors in Identity
Card Number
6 Emigrated
7,744 Subjects Contactable
And Completed
Questionnaire
2,306 Subjects Not
Contactable
5,164 Subjects Attended
Health Examination
2,580 Subjects Did Not
Attend Health
Examination
5140 Subjects Had
Blood Samples
24 Subjects Had No
Blood Samples
30 Subjects Refused
5023 Subjects Had
Urine Samples
4132 Subjects Had
Ankle-Brachial
Doppler Readings
Figure 1. Flowchart of study participation.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
Tavintharan S et al. 89
Ethics approval was obtained from two Institutional
Review Boards (National University of Singapore and
Singapore General Hospital) prior to study commence-
ment. Informed consent was obtained from all participants
before the commencement of the study.
Measurement of ABI
Ankle pressures were measured using a standardized Doppler
ultrasonic device (8 MHz; Smartdop 20EX bi-directional
blood flow detector; Hadeco, Japan). Measurements were
carried out after a 5-minute rest in the supine position. The
ABI was calculated as the ratio of the higher of the two sys-
tolic pressures (from posterior tibial and dorsalis pedis) at the
ankle to the average of the right and left brachial artery pres-
sures, unless there was a discrepancy 10 mmHg in blood
pressure values between the two arms. In such cases, the
higher reading was used for ABI. Pressures in each leg were
measured and the ABI was calculated separately for each leg.
Data collection
Data on demographic and lifestyle (alcohol intake, smok-
ing) factors, as well as medical history (including history
of hypertension, diabetes mellitus, hyperlipidemia, dura-
tion of diabetes, and current medications) were collected
using interviewer-administered questionnaires. Smoking
was categorized as never-, ex-, or current-smoker.
For health examination, participants were examined fol-
lowing a 10-hour overnight fast. Venous blood was drawn
and collected in plain and fluoride oxalate tubes and stored
at 4C for a maximum of 4 hours prior to processing.
A random urine specimen was collected. All biochemical
analyses on blood were carried out at the National University
Hospital Referral Laboratory, which is accredited by the
College of American Pathologists. Serum total cholesterol
(TC), triglyceride (TG), high-density lipoprotein cholesterol
(HDL-C) and low-density lipoprotein cholesterol (LDL-C)
levels were measured using an automatized autoanalyzer
(ADVIA 2400; Bayer Diagnostics, Tarrytown, NY, USA).
Glycated hemoglobin A1C (HbA1C) was measured on a Bio-
Rad VARIANT II analyzer (Bio-Rad Laboratories, Hercules,
CA, USA). Plasma glucose was obtained by the enzymatic
method (ADVIA 2400; Bayer Diagnostics) using blood
collected in fluoride oxalate tubes, while high-sensitivity
C-reactive protein (hs-CRP) was measured using immunotur-
bidimetric assay (Roche Integra 400; Roche Diagnostics,
Rotkreuz, Switzerland). Insulin was assayed by microparticle
enzyme immunoassay using the Abbot AXSYM (Abbott
Labora tories, Chicago, IL, USA). Insulin resistance was
assessed by homeostasis model assessment [insulin resis-
tance, HOMA-IR = (fasting insulin fasting glucose)/22.5].
Random urinary spot albumin and creatinine were measured
using commercial assays (Siemens Healthcare Diagnostics,
Inc., USA [Immulite] and Roche Diagnostics GmbH,
Germany) for urinary albumin and creatinine, respectively.
Two readings of blood pressure were taken from parti-
cipants after 5 minutes of resting using an automated
blood pressure monitor (Dinamap Pro100V2; Criticon,
Norderstedt, Germany) by trained observers. A third read-
ing was performed if the difference between two readings
of systolic blood pressure was greater than 10 mmHg or
diastolic blood pressure was greater than 5 mmHg. The
mean values of the closest two readings were calculated.
Definitions
The lower ABI between the two legs was used to define
PAD, taken as an ABI of 0.90.
2
To evaluate the nature of
the association of ABI with CVD risk factors, we catego-
rized ABI into 0.1-unit increments as follows: 0.90,
0.911.0, 1.011.10, 1.111.20, 1.211.30, and 1.311.40.
Only three participants had an ABI above 1.4 and were
excluded from the analysis.
Diabetes was defined as a fasting glucose level 7.0
mmol/l or a known history of diabetes, hypertension as
a systolic blood pressure > 140 mmHg or diastolic blood
pressure > 90 mmHg or a history of hypertension, or
currently taking anti-hypertensive medications. Coronary
artery disease (CAD) was taken as present if the subject
answered yes to the question of whether he/she had a
history of blockage of arteries to the heart, heart attack,
balloon angioplasty of artery to the heart, or heart bypass
operation. Stroke was taken as present if the subject
answered yes to a direct question of whether he/she had
been told by a physician to have had a stroke before. A urine
albumin:creatinine ratio (A/C) of 30 g/mg or above was
taken to indicate the presence of albuminuria. Renal impair-
ment was defined as present if the glomerular filtration rate
(eGFR) (estimated using the 4-variable Modification of
Diet in Renal Disease Study (MDRD) equation) was below
60 ml/min/1.73 m
2
body surface area.
Statistical methods
All statistical analyses were performed using Stata 10 for
Windows (Stata Corporation, College Station, TX, USA).
A total of 4132 subjects were screened for ABI and three
subjects with a high ABI (ABI > 1.4) were excluded from
the analysis. Analysis of variance (ANOVA) was used to
compare continuous variables between the groups. The
distribution of data for fasting glucose, triglycerides, hs-
CRP and HOMA-IR were skewed and log transformation
was done for analysis. The transformed variables were back
transformed before reporting (for clinical relevance) and
expressed in mean (range).
The TukeyKrammer post hoc test and chi-square test
were conducted respectively to assess the mean and propor-
tion difference between the reference group and other ABI
groups. Odds ratios (OR) and 95% confidence intervals
(95% CI) were obtained using the logistic regression model
to determine the association between categories of ABI and
risk factors (e.g. diabetes, hypertension, smoking), using
the ABI 1.111.20 category as the reference group.
Multivariate logistic regression and stepwise multivariate
logistic regression with backward selection were per-
formed, with low ABI as the dependent variable and 13
covariates in the model, to determine independent risk
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
90 Vascular Medicine 16(2)
factors for low ABI. All statistical tests were two-sided
with a level of significance defined as a p-value < 0.05. All
values are given as means (SD) unless stated otherwise.
Results
A total of 4129 subjects were included in the analysis. The
mean age (SD) was 49.9 (11.8) years, with 51.8% females.
There were 59% Chinese, 21.2% Malays and 19.8%
Indians.
The distribution of ABI in each ethnic group is shown in
Figure 2. PAD (defined as ABI 0.9) was present in 4.3%
of the population and very few people had high ABI (> 1.4).
The prevalence of PAD increased with age, and affected
one in 711 of those aged > 60 years (Table 1A). The preva-
lence of PAD also differed by ethnic group and sex. Malays
and Indians had a higher prevalence (and this was espe-
cially pronounced in women (Table 1B).
Table 2 describes the baseline characteristics of the
overall study population and those with PAD. Compared
to the overall population, those with PAD were more likely
to be older, have a higher systolic blood pressure and
pulse pressure, and a higher prevalence of diabetes, hyper-
tension, chronic renal disease, CAD and stroke. As can
be seen in Table 3, these differences were statistically
significant when compared to the reference group (ABI
1.111.20).
Table 4 describes the association of risk factors of PAD
according to ethnicity. As seen in the unadjusted model,
risk factor age, sex, BMI, pulse pressure, hypertension, dia-
betes, chronic kidney disease, history of coronary disease
and stroke were associated with PAD in all three major
ethnic groups. We carried out two sets of multivariate anal-
ysis. In the first, we included all potential risk factors in
the model except HOMA-IR. In the second, we used back-
ward stepwise regression to select the most parsimonious
model. The associations for several of the risk factors that
were statistically significant in univariate analyses (age,
hypertension, diabetes mellitus and renal impairment) were
no longer statistically significant following multivariate
analysis, in one or more ethnic groups. Pulse pressure was
identified as a common independent risk factor for PAD in
all ethnic groups. A past history of stroke was also associ-
ated with PAD (except in Malays, where there were no
individuals with stroke amongst those with PAD). Renal
impairment seemed more important in Indians. BMI was
associated with PAD in Chinese and Indians but the direc-
tion of the association was opposite with low BMI associ-
ated with PAD in Chinese but high BMI associated with
PAD in Indians. Interaction between ethnicity and BMI
was noted for PAD (p = 0.003). No other statistically
3.5
5.2
6.2
3.2
25.6
28.3
26.1
30.8
51.2
48.7
49.2
47.1
15.7
15.3
15.8
2.4
1.9
3.1
2.7
0.3 5 . 0 3 . 0 4 . 0
17.0
0.0
10.0
20.0
30.0
40.0
50.0
Chinese Malay Indian Others
P
e
r
c
e
n
t
ABI 0.9 ABI 0.91-1.00 ABI 1.01-1.10 ABI 0.91-1.00 ABI 1.01-1.10 ABI 1.11-1.20 ABI 1.21-1.30 ABI >1.3
Figure 2. Distribution of anklebrachial index (ABI) by ethnicity.
Table 1. (A) Prevalence of PAD by ethnicity, age and sex;
(B) prevalence of PAD by ethnicity and sex
(A)
Ethnicity Sex Age
1839
(n = 772)
4060
(n = 2586)
> 60
(n = 770)
Chinese, n (%) Male 4 (1.77) 11 (1.6) 20 (8.23)
Female 7 (2.4) 28 (3.61) 15 (7.11)
Malay, n (%) Male 1 (1.52) 8 (2.76) 9 (11.54)
Female 5 (6.02) 14 (4.95) 8 (11.27)
Indian, n (%) Male 2 (4.26) 9 (3.52) 8 (8.6)
Female 2 (3.57) 14 (4.83) 10 (13.7)
(B)
a
Sex Ethnicity
Chinese Malay Indian p-value
Overall, n (%) 85 (3.49) 45 (5.15) 46 (5.63) 0.01
Male, n (%) 35 (3.03) 18 (4.14) 19 (4.79) 0.2
Female, n (%) 50 (3.91) 27 (6.18) 27 (6.43) 0.04
a
The sex of one participant was missing.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
Tavintharan S et al. 91
significant interactions were noted for any of the other risk
factors.
Discussion
The results of this population-based study involving a
multi-ethnic Singapore population show that the preva-
lence of PAD was 4.3% in the overall population. The prev-
alence of PAD was higher in Malays and Indians (3.5% in
Chinese, 5.2% in Malays and 5.6% in Indians) and the
ethnic difference was most marked in women. Older age,
female sex, higher systolic blood pressure and pulse pres-
sure, diabetes, hypertension, chronic renal disease, CAD
and stroke are significantly associated with an increased
risk of PAD in all three ethnic groups.
The prevalence of PAD defined (by a low ABI 0.9) in
the overall population was comparable with other studies
which included subjects below 50 years of age.
10,18,19
Our
study shows an ethnic difference in the distribution of ABI.
PAD, compared with Chinese, was more common in Malays
and Indians. Both these latter ethnic groups in Singapore
show an increased propensity to develop myocardial infarc-
tion and our study suggests that this increased risk for CVD
extends to PAD.
20
We found that female sex was associated with an increased
risk of PAD (Table 4) and this association remained statisti-
cally significant after multivariate analysis. This contrasts
with data on the prevalence of myocardial infarction in the
Singapore population.
20
While in myocardial infarction,
compared with females, males had a nearly four times
increased risk, in PAD we found females had a nearly two-
fold higher risk than males. It has been shown that there is a
sex difference in the degree of calcification between coro-
nary artery and peripheral arteries (e.g. thoracic aorta),
21
with
men having greater coronary calcification and women hav-
ing greater calcification of the thoracic aorta. This raises the
possibility that the associations between sex and atheroscle-
rosis may differ between vascular beds, and in part may
explain why, compared with men, women are more likely
to develop PAD but less likely to develop CAD. This sex
difference needs to be further explored in clinical studies.
Our finding in those with PAD is consistent with our
previous work in Malays with diabetes,
22
and is also seen in
Western and Japanese populations in individuals with and
without diabetes.
13,23
The finding that individuals with
PAD were significantly more likely to have pre-existing
atherosclerotic disease, characterized by a history of CAD
or stroke, is important as it suggests that they may have a
number of common risk factors. Our data further supports
this, showing older age, presence of hypertension, diabetes,
albuminuria and renal impairment as important risk factors
for PAD.
In patients with diabetes, hyperglycemia has been postu-
lated as being responsible for the non-enzymatic glycation
of proteins such as elastin and collagen.
24
Hyperinsulinemia
contributes to vascular smooth muscle proliferation, associ-
ated with the pathogenesis of atherosclerosis. Consistent
with this, we found that patients with PAD had significantly
higher fasting blood glucose levels, and higher insulin
resistance assessed by HOMA-IR levels.
In addition to an increased prevalence of hypertension
and higher systolic blood pressure, we noted greater pulse
pressure in those with PAD. In fact, after multivariate ana-
lysis, pulse pressure was the risk factor that was the most
consistently associated with PAD across all three ethnic
groups. Well established as a marker of central arterial
stiffness, elevated pulse pressure is an important determi-
nant of endothelial function and atherosclerotic risk.
25,26
Elevated pulse pressure has been shown prospectively to
be the strongest predictor of atherosclerosis-related aortic
Table 2. Characteristics of the population
Overall
population
PAD (ABI 0.9)
n(%) 4129 176 (4.26)
Age, years 49.9 11.8 56.75 14.2
Female sex, % 51.78 59.09
Ethnicity, %
Chinese
Malay
Indian
Others
59.00
21.14
19.79
0.07
48.30
25.57
26.14
0
BMI, kg/m
2
24.2 4.4 24.54 5.2
Systolic BP, mmHg 132.62 20.9 146.75 25.5
Diastolic BP, mmHg 78.05 10.7 79.11 11.4
Pulse pressure, mmHg 54.57 15.64 67.64 19.9
Fasting glucose, mmol/l 5.05 (4.066.30) 5.37 (4.107.03)
Total cholesterol, mmol/l 5.23 1.0 5.21 1.0
HDL-C, mmol/l 1.39 0.34 1.35 0.34
LDL-C, mmol/l 3.21 0.85 3.22 0.91
Triglycerides, mmol/l 1.20 (0.702.03) 1.25 (0.791.95)
hs-CRP, mg/l 1.32 (0.394.44) 1.45 (0.425.00)
HOMA-IR 1.54 (0.733.25) 1.84 (0.844.01)
eGFR < 60 ml/min/
1.73 m, %
6.55 15.52
Albuminuria, % 13.14 24.85
Hypertension, % 41.65 64.94
Diabetes mellitus, % 12.39 29.55
Coronary artery disease, % 4.10 7.39
Stroke, % 0.92 5.11
Smoking status
No smoker, % 78.65 80.11
Current smoker, % 12.51 13.64
Ex-smoker, % 8.83 6.25
Age group, years
< 40 18.70 12.00
4060 62.65 48.00
> 60 18.65 40.00
PAD, peripheral artery disease; ABI, anklebrachial index; BMI, body
mass index; BP, blood pressure; HDL-C, high-density lipoprotein
cholesterol; LDL-C, low-density lipoprotein cholesterol; hs-CRP,
high-sensitivity C-reactive protein; HOMA-IR, homeostasis model
assessmentinsulin resistance; eGFR, estimated glomerular
filtration rate.
All data presented are as range and mean 1 SD.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
92 Vascular Medicine 16(2)
T
a
b
l
e
3
.
A
s
s
o
c
i
a
t
i
o
n
b
e
t
w
e
e
n
r
i
s
k
f
a
c
t
o
r
s
a
n
d
A
B
I
A
B
I
0
.
9
A
B
I
0
.
9
1
1
.
0
0
A
B
I
1
.
0
1
1
.
1
0
A
B
I
1
.
1
1
1
.
2
0
(
R
e
f
e
r
e
n
c
e
)
A
B
I
1
.
2
1
1
.
3
0
A
B
I
>
1
.
3
0
p
-
v
a
l
u
e
n
(
%
)
1
7
6
(
4
.
2
6
)
1
0
9
3
(
2
6
.
4
7
)
2
0
7
3
(
5
0
.
2
1
)
6
7
7
(
1
6
.
4
0
)
1
0
1
(
2
.
4
5
)
9
(
0
.
2
2
)
A
g
e
,
y
e
a
r
s
5
6
.
7
5
1
4
.
2
a
4
9
.
9
2
1
2
.
2
4
9
.
3
6
1
1
.
2
4
9
.
6
2
1
1
.
2
5
1
.
3
1
1
2
.
9
5
4
.
6
9
1
0
.
3
7
<
0
.
0
0
0
1
S
e
x
M
a
l
e
7
2
(
4
0
.
9
)
a
4
3
3
(
3
9
.
6
)
a
1
0
1
5
(
4
9
.
0
)
a
3
9
7
(
5
8
.
6
)
6
6
(
6
5
.
3
)
7
(
7
7
.
8
)
<
0
.
0
0
0
1
F
e
m
a
l
e
1
0
4
(
5
9
.
0
)
a
6
6
0
(
6
0
.
4
)
a
1
0
5
7
(
5
1
.
0
)
a
2
8
0
(
4
1
.
4
)
3
5
(
3
4
.
7
)
2
(
2
2
.
2
)
E
t
h
n
i
c
i
t
y
C
h
i
n
e
s
e
8
5
(
4
8
.
3
)
a
6
2
4
(
5
7
.
1
)
1
2
4
9
(
6
0
.
3
)
4
1
4
(
6
1
.
1
)
6
0
(
6
0
.
0
)
4
(
4
4
.
4
)
0
.
0
8
M
a
l
a
y
4
5
(
2
5
.
6
)
a
2
4
3
(
2
2
.
3
)
4
3
4
(
2
1
.
0
)
1
3
3
(
1
9
.
7
)
1
6
(
1
6
.
0
)
2
(
2
2
.
2
)
I
n
d
i
a
n
4
6
(
2
6
.
1
)
a
2
2
5
(
2
0
.
6
)
3
8
9
(
1
8
.
7
)
1
3
0
(
1
9
.
2
)
2
4
(
2
4
.
0
)
3
(
3
3
.
3
)
B
M
I
,
k
g
/
m
2
2
4
.
5
4
5
.
2
a
2
4
.
1
5
4
.
7
2
4
.
0
8
4
.
2
2
4
.
2
8
4
.
0
2
5
.
8
7
5
.
3
2
5
.
1
2
.
9
9
0
.
0
0
3
W
a
i
s
t
c
i
r
c
u
m
f
e
r
e
n
c
e
,
c
m
8
6
.
3
6
1
2
.
8
a
8
3
.
8
8
1
1
.
7
8
4
.
6
9
1
1
.
7
8
5
.
3
2
1
2
.
0
9
0
.
5
1
1
7
.
6
8
6
.
0
2
2
1
.
9
6
<
0
.
0
0
0
1
S
y
s
t
o
l
i
c
B
P
,
m
m
H
g
1
4
6
.
7
5
2
5
.
5
a
1
3
4
.
6
3
2
1
.
1
a
1
3
1
.
4
6
2
0
.
3
1
2
9
.
6
4
1
9
.
4
1
3
0
.
6
4
2
1
.
0
1
3
0
.
2
2
1
8
.
6
<
0
.
0
0
0
1
D
i
a
s
t
o
l
i
c
B
P
,
m
m
H
g
7
9
.
1
1
1
1
.
4
7
8
.
0
9
1
0
.
3
7
8
.
1
9
1
0
.
9
7
7
.
3
9
1
0
.
5
7
7
.
6
7
1
2
.
1
7
9
.
6
1
1
2
.
1
0
.
4
P
u
l
s
e
p
r
e
s
s
u
r
e
,
m
m
H
g
6
7
.
6
4
1
9
.
9
a
5
6
.
5
5
1
6
.
4
a
5
3
.
2
6
1
4
.
7
5
2
.
2
5
1
4
.
3
5
2
.
9
7
1
4
.
5
5
0
.
6
1
1
0
.
8
<
0
.
0
0
0
1
F
a
s
t
i
n
g
g
l
u
c
o
s
e
,
m
m
o
l
/
l
5
.
3
7
(
4
.
1
0
7
.
0
3
)
a
5
.
1
0
(
4
.
0
1
6
.
4
9
)
5
.
0
5
(
4
.
1
0
6
.
2
3
)
5
.
0
5
(
3
.
9
7
6
.
4
2
)
5
.
0
0
(
4
.
2
2
5
.
9
3
)
4
.
8
9
(
3
.
9
7
6
.
0
1
)
0
.
0
0
7
T
o
t
a
l
c
h
o
l
e
s
t
e
r
o
l
,
m
m
o
l
/
l
5
.
2
1
1
.
0
5
.
2
4
1
.
0
5
.
2
4
0
.
9
5
.
2
1
0
.
9
5
.
3
3
1
.
1
4
.
7
0
.
8
0
.
5
H
b
A
1
c
6
.
3
2
1
.
3
6
.
0
6
1
.
1
6
.
0
2
1
.
1
6
.
0
2
6
.
0
6
.
1
2
0
.
8
6
.
2
6
1
.
1
0
.
0
7
H
D
L
-
C
,
m
m
o
l
/
l
1
.
3
5
0
.
3
4
1
.
4
1
0
.
3
4
1
.
4
0
0
.
3
5
1
.
3
7
0
.
3
3
1
.
3
4
0
.
2
8
1
.
4
4
0
.
2
8
0
.
0
4
L
D
L
-
C
,
m
m
o
l
/
l
3
.
2
2
0
.
9
3
.
2
2
0
.
9
3
.
2
1
0
.
8
3
.
1
9
0
.
9
3
.
3
0
1
.
1
2
.
7
4
0
.
8
0
.
5
T
r
i
g
l
y
c
e
r
i
d
e
s
,
m
m
o
l
/
l
1
.
2
5
(
0
.
7
9
1
.
9
5
)
1
.
1
7
(
0
.
7
0
1
.
9
7
)
1
.
1
9
(
0
.
7
0
2
.
0
1
)
1
.
2
1
(
0
.
7
0
2
.
1
0
)
1
.
3
0
(
0
.
7
7
2
.
1
8
)
1
.
0
5
(
0
.
6
7
1
.
6
5
)
0
.
2
h
s
-
C
R
P
,
m
g
/
l
1
.
4
5
(
0
.
4
2
5
.
0
0
)
1
.
4
5
(
0
.
4
1
5
.
1
0
)
a
1
.
2
6
(
0
.
3
8
4
.
1
4
)
1
.
2
6
(
0
.
4
0
3
.
9
7
)
1
.
7
0
(
0
.
5
3
5
.
4
7
)
1
.
6
4
(
0
.
5
1
5
.
3
2
)
0
.
0
0
9
H
O
M
A
-
I
R
1
.
8
4
(
0
.
8
4
4
.
0
1
)
1
.
6
0
(
0
.
7
3
3
.
4
9
)
1
.
4
9
(
0
.
7
2
3
.
1
0
)
1
.
4
8
(
0
.
7
0
3
.
1
3
)
1
.
6
0
(
0
.
7
8
3
.
2
9
)
1
.
7
3
(
0
.
8
9
3
.
3
7
)
0
.
0
0
2
e
G
F
R
<
6
0
m
l
/
m
i
n
/
1
.
7
3
m
2
,
%
2
7
(
1
5
.
5
)
a
6
9
(
6
.
5
)
1
3
1
(
6
.
4
)
3
3
(
4
.
9
)
6
(
6
.
0
)
0
(
0
)
<
0
.
0
0
0
1
A
l
b
u
m
i
n
u
r
i
a
4
1
(
2
4
.
9
)
a
1
5
5
(
1
4
.
8
)
a
2
3
5
(
1
1
.
7
)
7
4
(
1
1
.
3
)
1
3
(
1
3
.
7
)
1
(
1
1
.
1
)
<
0
.
0
0
0
1
H
y
p
e
r
t
e
n
s
i
o
n
1
1
3
(
6
4
.
9
)
a
4
9
3
(
4
5
.
5
)
a
8
0
3
(
3
9
.
2
)
2
4
4
(
3
6
.
4
)
4
3
(
4
3
.
4
)
4
(
4
4
.
4
)
<
0
.
0
0
0
1
D
i
a
b
e
t
e
s
m
e
l
l
i
t
u
s
5
2
(
2
9
.
6
)
a
1
4
3
(
1
3
.
1
)
2
3
1
(
1
1
.
2
)
7
0
(
1
0
.
4
)
1
1
(
1
1
.
0
)
2
(
2
2
.
2
)
<
0
.
0
0
0
1
C
o
r
o
n
a
r
y
a
r
t
e
r
y
d
i
s
e
a
s
e
1
3
(
7
.
4
)
a
4
4
(
4
.
0
)
7
9
(
3
.
8
)
2
5
(
3
.
7
)
6
(
5
.
9
)
2
(
2
2
.
2
)
a
0
.
0
1
S
t
r
o
k
e
9
(
5
.
1
)
a
1
1
(
1
.
0
)
1
4
(
0
.
7
)
3
(
0
.
4
)
1
(
1
.
0
)
0
(
0
)
S
m
o
k
i
n
g
s
t
a
t
u
s
N
o
s
m
o
k
e
r
1
4
1
(
8
0
.
1
)
8
7
9
(
8
0
.
4
)
a
1
6
3
7
(
8
0
.
0
)
a
5
1
1
(
7
5
.
5
)
7
5
(
7
4
.
2
)
5
(
5
5
.
6
)
0
.
0
0
2
C
u
r
r
e
n
t
s
m
o
k
e
r
2
4
(
1
3
.
6
)
1
3
7
(
1
2
.
5
)
a
2
6
1
(
1
2
.
6
)
a
8
3
(
1
2
.
3
)
9
(
8
.
9
)
2
(
2
2
.
2
)
E
x
-
s
m
o
k
e
r
1
1
(
6
.
3
)
7
7
(
7
.
0
)
a
1
7
5
(
8
.
4
)
a
8
3
(
1
2
.
3
)
1
7
(
1
6
.
8
)
2
(
2
2
.
2
)
A
B
I
,
a
n
k
l
e
b
r
a
c
h
i
a
l
i
n
d
e
x
;
B
M
I
,
b
o
d
y
m
a
s
s
i
n
d
e
x
;
B
P
,
b
l
o
o
d
p
r
e
s
s
u
r
e
;
H
b
A
1
c
,
h
e
m
o
g
l
o
b
i
n
A
1
c
;
H
D
L
-
C
,
h
i
g
h
-
d
e
n
s
i
t
y
l
i
p
o
p
r
o
t
e
i
n
c
h
o
l
e
s
t
e
r
o
l
;
L
D
L
-
C
,
l
o
w
-
d
e
n
s
i
t
y
l
i
p
o
p
r
o
t
e
i
n
c
h
o
l
e
s
t
e
r
o
l
;
h
s
-
C
R
P
,
h
i
g
h
-
s
e
n
s
i
t
i
v
i
t
y
C
-
r
e
a
c
t
i
v
e
p
r
o
t
e
i
n
;
H
O
M
A
-
I
R
,
h
o
m
e
o
s
t
a
s
i
s
m
o
d
e
l
a
s
s
e
s
s
m
e
n
t
i
n
s
u
l
i
n
r
e
s
i
s
t
a
n
c
e
;
e
G
F
R
,
e
s
t
i
m
a
t
e
d
g
l
o
m
e
r
u
l
a
f
i
l
t
r
a
t
i
o
n
r
a
t
e
.
C
o
n
t
i
n
u
o
u
s
v
a
r
i
a
b
l
e
s
a
r
e
e
x
p
r
e
s
s
e
d
i
n
m
e
a
n
S
D
a
n
d
c
a
t
e
g
o
r
i
c
a
l
v
a
r
i
a
b
l
e
s
a
r
e
e
x
p
r
e
s
s
e
d
i
n
n
(
%
)
.
a
M
e
a
n
/
p
r
o
p
o
r
t
i
o
n
d
i
f
f
e
r
e
n
c
e
i
s
s
i
g
n
i
f
i
c
a
n
t
f
r
o
m
t
h
e
r
e
f
e
r
e
n
c
e
g
r
o
u
p
(
A
B
I
1
.
1
1
1
.
2
0
)
.
C
o
n
t
i
n
u
o
u
s
v
a
r
i
a
b
l
e
s
a
r
e
e
x
p
r
e
s
s
e
d
i
n
m
e
a
n
S
D
a
n
d
c
a
t
e
g
o
r
i
c
a
l
v
a
r
i
a
b
l
e
s
a
r
e
e
x
p
r
e
s
s
e
d
i
n
n
(
%
)
.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
Tavintharan S et al. 93
T
a
b
l
e
4
.
A
s
s
o
c
i
a
t
i
o
n
b
e
t
w
e
e
n
r
i
s
k
f
a
c
t
o
r
s
a
n
d
l
o
w
A
B
I
(
A
B
I
0
.
9
)
v
e
r
s
u
s
n
o
r
m
a
l
A
B
I
(
A
B
I
1
.
1
1
1
.
2
0
)
b
y
e
t
h
n
i
c
i
t
y
C
h
i
n
e
s
e
M
a
l
a
y
I
n
d
i
a
n
U
n
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
M
u
l
t
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
S
t
e
p
w
i
s
e
r
e
g
r
e
s
s
i
o
n
U
n
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
M
u
l
t
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
S
t
e
p
w
i
s
e
r
e
g
r
e
s
s
i
o
n
U
n
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
M
u
l
t
i
v
a
r
i
a
t
e
a
n
a
l
y
s
i
s
S
t
e
p
w
i
s
e
r
e
g
r
e
s
s
i
o
n
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
O
R
(
C
I
)
8
5
(
1
7
.
0
3
)
4
5
(
2
5
.
2
8
)
4
6
(
2
6
.
1
4
)
F
e
m
a
l
e
s
e
x
1
.
9
9
*
*
2
.
1
8
*
2
.
0
2
*
*
2
.
1
9
*
2
.
5
2
2
.
0
6
*
3
.
7
1
*
(
1
.
2
4
3
.
2
0
)
(
1
.
1
5
4
.
1
3
)
(
1
.
1
9
3
.
4
3
)
(
1
.
1
0
4
.
3
7
)
(
0
.
8
8
7
.
2
6
)
(
1
.
0
4
4
.
0
9
)
(
1
.
0
9
1
2
.
6
8
)
A
g
e
,
y
e
a
r
s
1
.
0
5
*
*
*
1
.
0
2
1
.
0
3
*
0
.
9
7
1
.
0
6
*
*
*
1
.
0
3
(
1
.
0
3
1
.
0
7
)
(
0
.
9
9
1
.
0
5
)
(
1
.
0
0
1
.
0
6
)
(
0
.
9
3
1
.
0
2
)
(
1
.
0
3
1
.
1
0
)
(
0
.
9
7
1
.
0
8
)
B
M
I
,
k
g
/
m
0
.
9
3
*
0
.
8
9
*
0
.
9
1
*
0
.
9
5
0
.
9
5
1
.
0
9
*
1
.
0
8
1
.
1
1
*
(
0
.
8
7
0
.
9
9
)
(
0
.
8
1
0
.
9
7
)
(
0
.
8
4
0
.
9
8
)
(
0
.
8
8
1
.
0
3
)
(
0
.
8
5
1
.
0
6
)
(
1
.
0
2
1
.
1
7
)
(
0
.
9
8
1
.
1
9
)
(
1
.
0
2
1
.
2
0
)
P
u
l
s
e
p
r
e
s
s
u
r
e
,
m
m
H
g
1
.
0
5
*
*
*
1
.
0
4
*
*
*
1
.
0
6
*
*
*
1
.
0
4
*
*
*
1
.
0
5
*
*
*
1
.
0
4
*
*
*
1
.
0
6
*
*
*
1
.
0
3
1
.
0
5
*
*
*
(
1
.
0
4
1
.
0
7
)
(
1
.
0
1
1
.
0
7
)
(
1
.
0
4
1
.
0
7
)
(
1
.
0
2
1
.
0
6
)
(
1
.
0
2
1
.
0
9
)
(
1
.
0
2
1
.
0
6
)
(
1
.
0
4
1
.
0
9
)
(
0
.
9
9
1
.
0
7
)
(
1
.
0
3
1
.
0
8
)
H
O
M
A
-
I
R
1
.
1
3
*
1
.
0
1
1
.
1
5
*
(
1
.
0
2
1
.
2
6
)
(
0
.
8
6
1
.
2
0
)
(
1
.
0
2
1
.
3
0
)
h
s
-
C
R
P
,
m
g
/
l
1
.
0
4
1
.
0
2
0
.
9
6
0
.
8
9
1
.
0
6
*
1
.
0
2
(
0
.
9
7
1
.
1
2
)
(
0
.
9
3
1
.
1
2
)
(
0
.
8
6
1
.
0
7
)
(
0
.
7
7
1
.
0
3
)
(
1
.
0
1
1
.
1
2
)
(
0
.
9
5
1
.
1
1
)
H
D
L
-
C
,
m
m
o
l
/
l
1
.
1
4
0
.
6
8
0
.
9
6
0
.
5
2
1
.
0
0
3
0
.
5
2
(
0
.
5
8
2
.
2
4
)
(
0
.
2
8
1
.
6
3
)
(
0
.
3
0
3
.
0
7
)
(
0
.
1
0
2
.
6
6
)
(
0
.
3
0
3
.
3
2
)
(
0
.
1
0
2
.
6
7
)
L
D
L
-
C
,
m
m
o
l
/
l
1
.
0
3
1
.
1
7
1
.
1
2
1
.
2
1
0
.
7
9
0
.
8
8
(
0
.
7
7
1
.
3
6
)
(
0
.
8
4
1
.
6
3
)
(
0
.
7
9
1
.
5
9
)
(
0
.
8
0
1
.
8
2
)
(
0
.
5
2
1
.
1
9
)
(
0
.
5
0
1
.
5
6
)
H
y
p
e
r
t
e
n
s
i
o
n
3
.
2
4
*
*
*
1
.
1
1
2
.
6
2
*
1
.
4
4
3
.
3
3
*
*
1
.
0
5
(
2
.
0
0
5
.
2
6
)
(
0
.
5
0
2
.
4
4
)
(
1
.
2
6
5
.
4
5
)
(
0
.
4
3
4
.
8
9
)
(
1
.
6
3
6
.
7
9
)
(
0
.
3
6
3
.
1
3
)
D
i
a
b
e
t
e
s
4
.
7
4
*
*
*
1
.
6
4
1
.
8
1
1
.
3
1
3
.
5
0
*
*
1
.
5
9
(
2
.
5
8
8
.
6
8
)
(
0
.
7
2
3
.
7
0
)
(
0
.
7
9
4
.
1
5
)
(
0
.
4
0
4
.
3
3
)
(
1
.
6
4
7
.
4
9
)
(
0
.
5
7
4
.
4
6
)
C
o
r
o
n
a
r
y
a
r
t
e
r
y
d
i
s
e
a
s
e
1
.
4
7
1
.
6
2
6
.
3
9
*
9
.
9
6
1
.
3
5
0
.
7
9
(
0
.
4
0
5
.
4
6
)
(
0
.
3
3
7
.
8
5
)
(
1
.
1
3
3
6
.
1
6
)
(
0
.
6
3
1
5
8
.
4
0
)
(
0
.
4
8
3
.
7
9
)
(
0
.
1
9
7
.
2
8
)
S
t
r
o
k
e
2
0
.
4
0
*
*
1
1
.
9
2
*
1
4
.
1
4
*
N
A
6
.
1
0
*
2
.
1
6
(
2
.
2
5
1
8
4
.
8
4
)
(
1
.
1
7
1
2
1
.
7
6
)
(
1
.
4
3
1
4
0
.
2
0
)
(
1
.
0
8
3
4
.
4
8
)
(
0
.
0
7
6
9
.
6
8
)
R
e
n
a
l
i
m
p
a
i
r
m
e
n
t
2
.
9
9
*
*
*
1
.
2
0
1
.
4
3
0
.
6
2
4
.
1
9
*
*
*
3
.
2
2
*
1
.
0
5
*
*
*
(
1
.
6
9
5
.
2
9
)
(
0
.
5
6
2
.
5
6
)
(
0
.
6
4
3
.
2
0
)
(
0
.
1
9
2
.
0
4
)
(
1
.
9
7
8
.
9
1
)
(
1
.
1
4
9
.
1
1
)
(
1
.
0
3
1
.
0
8
)
S
m
o
k
i
n
g
s
t
a
t
u
s
N
o
s
m
o
k
e
r
R
e
f
e
r
e
n
c
e
R
e
f
e
r
e
n
c
e
R
e
f
e
r
e
n
c
e
C
u
r
r
e
n
t
s
m
o
k
e
r
0
.
6
7
0
.
6
5
1
.
4
3
3
.
3
6
1
.
1
2
3
.
9
8
(
0
.
2
9
1
.
5
4
)
(
0
.
2
1
2
.
0
1
)
(
0
.
6
0
3
.
4
0
)
(
0
.
9
3
1
2
.
1
8
)
(
0
.
4
3
0
.
9
1
)
(
0
.
8
7
1
8
.
2
7
)
E
x
-
s
m
o
k
e
r
0
.
6
1
0
.
9
5
N
A
N
A
1
.
0
2
4
.
6
4
(
0
.
2
5
1
.
4
9
)
(
0
.
3
4
2
.
6
9
)
(
0
.
3
5
3
.
0
7
)
(
0
.
9
3
2
3
.
0
8
)
O
R
,
o
d
d
s
r
a
t
i
o
;
C
I
,
c
o
n
f
i
d
e
n
c
e
i
n
t
e
r
v
a
l
;
B
M
I
,
b
o
d
y
m
a
s
s
i
n
d
e
x
;
H
O
M
A
-
I
R
,
h
o
m
e
o
s
t
a
s
i
s
m
o
d
e
l
a
s
s
e
s
s
m
e
n
t
i
n
s
u
l
i
n
r
e
s
i
s
t
a
n
c
e
;
h
s
-
C
R
P
,
h
i
g
h
-
s
e
n
s
i
t
i
v
i
t
y
C
-
r
e
a
c
t
i
v
e
p
r
o
t
e
i
n
;
H
D
L
-
C
,
h
i
g
h
-
d
e
n
s
i
t
y
l
i
p
o
p
r
o
t
e
i
n
c
h
o
l
e
s
t
e
r
o
l
;
L
D
L
-
C
,
l
o
w
-
d
e
n
s
i
t
y
l
i
p
o
p
r
o
t
e
i
n
c
h
o
l
e
s
t
e
r
o
l
.
*
p
<
0
.
0
5
,
*
*
p
<
0
.
0
1
,
*
*
*
p
<
0
.
0
0
0
1
.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
94 Vascular Medicine 16(2)
calcifications,
27
and is an independent predictor of PAD in
type 2 diabetes mellitus,
28
likely having a key role in initi-
ating and sustaining chronic inflammation associated with
atherogenesis.
Impaired renal function and albuminuria are associated
with atherosclerosis and cardiovascular events.
29
Patients
with PAD in our study had significantly reduced renal func-
tion and an increased prevalence of albuminuria. Although
the mechanisms for this association are not fully elucidated,
it is well known that both PAD and renal impairment share
a number of common risk factors. Concomitant atheroscle-
rosis involving renal arteries in patients with PAD, together
with metabolic changes resulting from decreased renal
function, could potentially contribute to the association
between renal impairment, albuminuria and PAD.
While current smoking is associated with an increased
risk of PAD in a number of studies,
6,7
in middle-aged and
elderly Koreans, the prevalence of smoking was more com-
mon in those with low and high ABI.
30
In our study, cigarette
smoking was not associated with an increased risk of PAD.
One possibility is that our finding is due to chance. The pro-
portion of smokers is small (12.5%) and the confidence
intervals for the effect estimates are wide. Another possibil-
ity is that the number of cigarettes consumed by smokers in
Singapore may be relatively low compared to other popula-
tions and, thus, we were not able to detect the effect. With
very strong legislation on tobacco taxation and prohibition in
public places, there is a falling trend of tobacco consumption
and currently Singapores smoking rate is among the lowest
of the developed countries.
31
Given these limitations, and the
known health benefits of smoking cessation, we still recom-
mend that all smokers consider efforts to cease smoking.
The strength of our study includes the large number of
subjects studied and these individuals are representative of a
multi-ethnic South Asian population. Subjects were system-
atically sampled to establish a random sample representative
of the general population. Interviewers and ABI operators
were trained and data were collected using standard, repro-
ducible protocols. To reduce bias, ABI operators were also
blinded from questionnaire data.
A few limitations in our study need to be mentioned. In
spite of stratified sampling to increase the recruitment of a
minority population (Malays and South Indians), the number
studied is still relatively small (876 Malays and 818 Indians).
Hence, this minority ethnicity may be under-represented in
our study population. Additionally, the cross-sectional nature
of our study precludes conclusions regarding the temporal
nature of the observations.
In conclusion, in this large, multi-ethnic, Asian population,
we document distribution and risk factor associations for PAD.
PAD affects 4.3% of the population, and is most common in
Indians, followed by Malays and Chinese. Apart from tradi-
tional vascular risk factors, pulse pressure, renal impairment
and past history of stroke are important determinants of PAD.
Acknowledgements
Our most sincere thanks go to the participants of this study because
without their support this study would not have been possible.
Guarantor statement: The guarantor, ST, accepts full responsi-
bility for the work and/or the conduct of the study, had access to
the data, and controlled the decision to publish.
All authors contributed to the intellectual development of this
paper.
Conflict of interest
There are no conflicts of interest related to this manuscript.
Funding
This work was supported by grants from the Biomedical Research
Council (grant number: 03/1/27/18/216) and the National Medical
Research Council (grant number: 0863/2004), Republic of
Singapore.
The funding agencies had no role in the research presented in
the paper and the researchers were fully independent in pursuing
this research.
References
1. Newman AB, Shemanski L, Manolio TA, et al. Anklearm
index as a predictor of cardiovascular disease and mortality
in the Cardiovascular Health Study. The Cardiovascular
Health Study Group. Arterioscler Thromb Vasc Biol 1999; 19:
538545.
2. Murabito JM, Evans JC, Larson MG, Nieto K, Levy D,
Wilson PW; Framingham Study. The anklebrachial index in
the elderly and risk of stroke, coronary disease, and death: the
Framingham Study. Arch Intern Med 2003; 163: 19391942.
3. Hooi JD, Kester AD, Stoffers HE, Rinkens PE, Knottnerus
JA, van Ree JW. Asymptomatic peripheral arterial occlusive
disease predicted cardiovascular morbidity and mortality in a
7-year follow-up study. J Clin Epidemiol 2004; 57: 294300.
4. Stoffers J, Kester A, Kaiser V, Rinkens P, Kitslaar P,
Knottnerus A. The diagnostic value of the measurement of the
anklebrachial systolic pressure index in primary health care.
J Clin Epidemiol 1996; 49: 14011405.
5. McDermott MM, Ferrucci L, Guralnik JM, et al. The ankle
brachial index is associated with the magnitude of impaired
walking endurance among men and women with peripheral
arterial disease. Vasc Med 2010; 15: 251257.
6. OHare AM, Katz R, Shlipak MG, Cushman M, Newman AB.
Mortality and cardiovascular risk across the anklearm index
spectrum. Circulation 2006; 113: 388393.
7. Resnick HE, Lindsay RS, McDermott MM, et al. Relationship
of high and low ankle brachial index to all-cause and cardio-
vascular disease mortality: the Strong Heart Study. Circulation
2004; 109: 733739.
8. Ankle Brachial Index Collaboration, Fowkes FG, Murray
GD, Butcher I, et al. Ankle brachial index combined with
Framingham Risk Score to predict cardiovascular events and
mortality: a meta-analysis. JAMA 2008; 300: 197208.
9. Resnick HE, Foster GL. Prevalence of elevated ankle
brachial index in the United States 1999 to 2002. Am J Med
2005; 18: 676679.
10. McDermott MM, Liu K, Criqui MH, et al. Anklebrachial index
and subclinical cardiac and carotid disease. The Multi-Ethnic
Study of Atherosclerosis. Am J Epidemiol 2005; 162: 3341.
11. Nang EE, Khoo CM, Tai ES, et al. Is there a clear threshold
for fasting plasma glucose that differentiates between those
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
Tavintharan S et al. 95
with and without neuropathy and chronic kidney disease?:
The Singapore Prospective Study Program. Am J Epidemiol
2009; 169: 14541462.
12. Wu Y, Tai ES, Heng D, Tan CE, Low LP, Lee J. Risk factors
associated with hypertension awareness, treatment, and con-
trol in a multi-ethnic Asian population. J Hypertens 2009; 27:
190197.
13. Sabanayagam C, Lim SC, Wong TY, Lee J, Shankar A, Tai
ES. Ethnic disparities in prevalence and impact of risk factors
of chronic kidney disease. Nephrol Dial Transplant 2010; 25:
25642570.
14. Hughes K, Yeo PP, Lun KC, et al. Cardiovascular diseases in
Chinese, Malays, and Indians in Singapore. II. Differences in
risk factor levels. J Epidemiol Community Health 1990; 44:
2935.
15. Tan CE, Emmanuel SC, Tan BY, Jacob E. Prevalence of dia-
betes and ethnic differences in cardiovascular risk factors. The
1992 Singapore National Health Survey. Diabetes Care 1999;
22: 241247.
16. Hughes K, Aw TC, Kuperan P, Choo M. Central obesity,
insulin resistance, syndrome X, lipoprotein(a), and cardio-
vascular risk in Indians, Malays, and Chinese in Singapore.
J Epidemiol Community Health 1997; 51: 394399.
17. Tan CE, Tai ES, Tan CS, et al. APOE polymorphism and lipid
profile in three ethnic groups in the Singapore population.
Atherosclerosis 2003; 170: 253260.
18. Premalatha G, Shanthirani S, Deepa R, Markovitz J, Mohan
V. Prevalence and risk factors of peripheral vascular disease
in a selected South Indian population: the Chennai Urban
Population Study. Diabetes Care 2000; 23: 12951300.
19. Criqui MH, Vargas V, Denenberg JO, et al. Ethnicity and
peripheral arterial disease: the San Diego Population Study.
Circulation 2005; 112: 27032707.
20. Mak KH, Chia KS, Kark JD, et al. Ethnic differences in acute
myocardial infarction in Singapore. Eur Heart J 2003; 24:
151160.
21. Nasir K, Roguin A, Sarwar A, Rumberger JA, Blumenthal
RS. Gender differences in coronary arteries and thoracic
aorta calcification. Arterioscler Thromb Vasc Biol 2007; 27:
12201222.
22. Tavintharan S, Ning Cheung, Su Chi Lim, et al. Prevalence and
risk factors for peripheral artery disease in an Asian population
with diabetes mellitus. Diab Vasc Dis Res 2009; 6: 8086.
23. Gregg EW, Sorlie P, Paulose-Ram R, et al. Prevalence of lower
extremity disease in the U.S. adult population >=40 years of
age with and without diabetes: 19992000 National Health
and Nutrition Examination Survey. Diabetes Care 2004; 27:
15911597.
24. Brownlee M, Vlassara H, Cerami A. Nonenzymatic glyco-
sylation and the pathogenesis of diabetic complications. Ann
Intern Med 1984; 101: 527537.
25. Glynn RJ, LItalien GJ, Sesso HD, Jackson EA, Buring JE.
Development of predictive models for long-term cardiovascu-
lar risk associated with systolic and diastolic blood pressure.
Hypertension 2002; 39: 105110.
26. Beigel R, Dvir D, Arbel Y, Shechter A, Feinberg MS, Shechter
M. Pulse pressure is a predictor of vascular endothelial func-
tion in middle-aged subjects with no apparent heart disease.
Vasc Med 2010; 15: 299305.
27. Miwa Y, Tsushima M, Arima H, Kawano Y, Sasaguri T. Pulse
pressure is an independent predictor for the progression of
aortic wall calcification in patients with controlled hyperlipid-
emia. Hypertension 2004; 43: 536540.
28. Tseng CH. Pulse pressure as a risk factor for peripheral vas-
cular disease in type 2 diabetic patients. Clin Exp Hypertens
2004; 25: 475485.
29. Mann JFE, Gerstein HC, Pogue J, Bosch J, Yusuf S (for
the HOPE Investigators). Renal insufficiency as a predictor
of cardiovascular outcomes and the impact of ramipril: the
HOPE randomized trial. Ann Intern Med 2001; 134: 629636.
30. Kweon SS, Shin MH, Park KS, et al. Distribution of the
anklebrachial index and associated cardiovascular risk fac-
tors in a population of middle-aged and elderly Koreans.
J Korean Med Sci 2005; 20: 373378.
31. Lim TK. Singapore and the tobacco pandemic. Ann Acad Med
Singapore 2008; 37: 363364.
by guest on June 30, 2014 vmj.sagepub.com Downloaded from
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Circulation Research 2001 Davidge 650 60Dokumen12 halamanCirculation Research 2001 Davidge 650 60Uswa MalikBelum ada peringkat
- Arterioscler Thromb Vasc Biol 2011 Ricciotti 986 1000Dokumen16 halamanArterioscler Thromb Vasc Biol 2011 Ricciotti 986 1000Uswa MalikBelum ada peringkat
- Vasc Med 2011 Subramaniam 87 95Dokumen10 halamanVasc Med 2011 Subramaniam 87 95Uswa MalikBelum ada peringkat
- Slide RehabDokumen18 halamanSlide RehabUswa MalikBelum ada peringkat
- Circ Cardiovasc Qual Outcomes 2009 Ray 155 63Dokumen10 halamanCirc Cardiovasc Qual Outcomes 2009 Ray 155 63Uswa MalikBelum ada peringkat
- Circ Cardiovasc Imaging 2013Dokumen27 halamanCirc Cardiovasc Imaging 2013Uswa MalikBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- DMSCO Log Book Vol.13 1936Dokumen49 halamanDMSCO Log Book Vol.13 1936Des Moines University Archives and Rare Book RoomBelum ada peringkat
- Risk For Fluid ImbalanceDokumen8 halamanRisk For Fluid Imbalanceapi-277522722100% (1)
- Final VeganDokumen11 halamanFinal Veganapi-314696134Belum ada peringkat
- Subjective Global Assessment Form: Medical HistoryDokumen2 halamanSubjective Global Assessment Form: Medical Historynadia susiyanaBelum ada peringkat
- Sample Meal PlanningDokumen6 halamanSample Meal PlanningSherrie Mae RoncalBelum ada peringkat
- WINGS Corporation's Growth into a Market LeaderDokumen9 halamanWINGS Corporation's Growth into a Market LeaderERna Permana PrasodjoBelum ada peringkat
- ReportDokumen17 halamanReportBùi Văn PhúBelum ada peringkat
- writing task 2Dokumen2 halamanwriting task 2Bảo Nhi HoàngBelum ada peringkat
- Food Chemistry (Cheese) FullDokumen11 halamanFood Chemistry (Cheese) FullAlia CameliaBelum ada peringkat
- الملكيDokumen123 halamanالملكيGl HasnBelum ada peringkat
- Brochure Physical ActivityDokumen2 halamanBrochure Physical Activityapi-340126515Belum ada peringkat
- HLTH 1322 Assign 7 Vitamins & SuperTracker - Andrea AlvarezDokumen3 halamanHLTH 1322 Assign 7 Vitamins & SuperTracker - Andrea AlvarezAndrea Galeazzi RosilloBelum ada peringkat
- Effects of Sugar Consumption on Human Behavior and PerformanceDokumen13 halamanEffects of Sugar Consumption on Human Behavior and PerformanceAndi BayerlBelum ada peringkat
- Argumentative Research PaperDokumen6 halamanArgumentative Research Paperjlewi113Belum ada peringkat
- 6-Egg Public HealthDokumen48 halaman6-Egg Public Healthhamad hamadBelum ada peringkat
- CaffeineDokumen31 halamanCaffeinemaheshbabuhereBelum ada peringkat
- Lucca 1994Dokumen8 halamanLucca 1994dhea giftBelum ada peringkat
- Seminar HipoglikemiaDokumen19 halamanSeminar HipoglikemiaRidyah Ning TyasBelum ada peringkat
- Variety of Herbal TeasDokumen5 halamanVariety of Herbal Teassuzyana jamesBelum ada peringkat
- Nutrition and Keeping FitDokumen4 halamanNutrition and Keeping FiteltisiBelum ada peringkat
- The Most Important Topics of Our Time PDFDokumen24 halamanThe Most Important Topics of Our Time PDFeric weaver100% (1)
- Beed 9 Reviewer: I. Family What Is A Family?Dokumen8 halamanBeed 9 Reviewer: I. Family What Is A Family?DaeBelum ada peringkat
- Clinical NutritionDokumen175 halamanClinical NutritionCristianaParvanBelum ada peringkat
- Balanced DietDokumen40 halamanBalanced DietAkshatha ShivBelum ada peringkat
- Aloe Vera Gel as an Anti-Blood CoagulantDokumen8 halamanAloe Vera Gel as an Anti-Blood CoagulantDanica Bondoc50% (2)
- Bualaw Also Know Binatog As Is A Common Street Food Found in The PhillpipinesDokumen2 halamanBualaw Also Know Binatog As Is A Common Street Food Found in The PhillpipinesFerimard Brian BorjaBelum ada peringkat
- 10 Things You Need To Know About Premixes: by DSM Nutritional ProductsDokumen2 halaman10 Things You Need To Know About Premixes: by DSM Nutritional ProductsanaBelum ada peringkat
- Why Is The Keto Diet Good For YouDokumen6 halamanWhy Is The Keto Diet Good For YouNema cringBelum ada peringkat
- Food Pyramid Word WorksheetDokumen2 halamanFood Pyramid Word WorksheetAnabelBelum ada peringkat
- Growth Performance of Catfish Fed Diet Containing Live MaggotDokumen16 halamanGrowth Performance of Catfish Fed Diet Containing Live MaggotIorhee saviourBelum ada peringkat