Literature Review For Specimen Labeling and Blood Bank
Diunggah oleh
api-236445988Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Literature Review For Specimen Labeling and Blood Bank
Diunggah oleh
api-236445988Hak Cipta:
Format Tersedia
Literature Review for Specimen Labeling and Blood Bank
Laboratory specimens continue to be mislabeled or improperly labeled with many studies and
initiatives throughout the country within hospitals and private laboratories. Working on education of
staff and auditing blood bank specimens I have become familiar with how often these types of events
occur. These events have potential to cause harm to patients, either by treating incorrect lab values,
transfusing incorrect blood, not treating quickly enough waiting for results, or simply longer lengths of
stays and increased costs. Many hospitals have examined their practices to improve labeling processes
and reduce error risk and rates and ultimately improve patient care and safety.
Hill et al. (2010) conducted a cohort post-intervention study to see how electronic ordering and
bar-coded specimens may reduce error rates. The emergency department is notorious for mislabeled
specimens as with the high volume of labs drawn or collected and the chaos of a continuously changing
environment. They reported that with physician order entry and barcode labels can significantly
reduce ED specimen-related errors.
1
They also concluded that many of the specimens continued to be
mislabeled as human contact was necessary with handling and labeling. In this article, they cited that
almost 100,000 people die annually from preventable errors within hospitals. Through all research they
were able to conclude that the electronic system and barcodes had the potential to help errors rates but
the human element continued to be evident.
Synder et al. (2012) completed a meta-analysis to question if barcoding would reduce laboratory
specimen errors that showed similar results. The report accurate identification of patients their
specimens and laboratory test results linked to them is essential in all healthcare settings for providing
effective, safe, timely, efficient, equitable, and patient-centered healthcare.
2
The also stated that most
errors of laboratory specimens are associated with human error and under the control of the
laboratory. They also explained that errors that are reported are probably underreported as some go
unidentified and others simply not reported by staff. The article also notes that most detected errors
do no harm patients since their detection results in the associated erroneous test reports typically not
being released by the laboratory, however errors consequences include incorrect, delayed and/or lack
of treatment which may cause injury, disability, death, longer lengths of stay, higher healthcare costs, as
well as other patient harm and diverted resources. This article emphasizes that error rates are low,
about 0.1 percent, but that number accounts for hundreds of thousands of errors. Through their
review, they established that Barcoding practices demonstrated effectiveness as reducing ID errors for
patient specimen and laboratory testing identification is generalized to most common hospital settings
and patient populations. They reported that limitations including unpublished status and that many of
the studies had missing or undocumented information.
Many studies/articles have also solely focused on blood bank specimen labeling and the
potential for errors with drawn specimens and transfusing uncross-matched blood. ONeill et al. (2009)
describes the strict policies of the blood bank should be used for all laboratories. They state that blood
banks have been able to reduce error rates by 73.5% with low cost education initiative and policy
change.
3
By providing weekly updates and incident feedback they reported a 28% decrease in
mislabeled specimens from their emergency department. This was also accomplished by visually
watching phlebotomists verify patient names information, technique and labeling procedures and
providing immediate feedback and retraining with variances. They concluded that with increased
awareness and stricter policies as adopted by the blood bank for rejection, a decrease in errors had
been noted. They stated that it is unknown if it was solely the stricter policies and education but no
other initiatives had been conducted during the study period.
Tondon et al. (2010) completed a study of errors within the cross match lab and noted that the
most frequent incidents encountered with bedside being the major site of deviation.
4
The describe that
initially there was not strict enforcement of policies for sampling and labeling and a leniency on the
laboratory for acceptance of specimens that were either mislabeled, incorrectly labeled, or partially
labeled. They found that the majority of mislabeled specimens occurred with failure to verify at the
bedside and more than half occurred during the day shift, presumed to relate to volume of patients. At
the conclusion of the study they proposed that a stricter policy be adopted to reject all labs that were
not completely or properly labeled so that clinical staff clearly understands that every specimen will be
rejected if not properly and completely labeled. A recent adoption by our own hospital has mirrored
this policy to hopefully increase awareness and be able to track where deviances occur and by whom.
The laboratory staff is usually those that discover or identify the mislabeled specimens and are
able to track and check patient results. Salinas et al. (2013) explain many national organizations have
listed improvement of patient identification accuracy as the first of their recommended goals.
5
They
also reported that lab results can influence patient care in up to 70% of cases and thus laboratory
safety is crucial for patient safety. This was a simple study that essential showed that with electronic
order entry there are fewer errors reported, however this emphasizes the fact that human intervention
is still clue despite the advantages of the new technologies and highlights the role of the laboratory
professional to detect errors in order to plan the appropriate barriers. This article reports the study
was limited in that it only studied errors relating to demographic data registration.
Lastly, a publication by the Pennsylvania Patient Safety Authority identified where errors occur
and possible reasons why. They also developed methods to limit those errors by targeting the causes.
They describe contributing factors with the most frequent being: procedures not being followed,
distractions/interruptions, emergency situations, and unplanned workload increased. By far the main
factor was procedures not being followed and interventions for correction included education and re-
education, mandatory competencies, as well as other interventions to address other factors. They
concluded that post interventions they were able to reduce errors by 37% and specimen identification
error analysis combined with interventions to reduce specimen labeling errors can contribute to
improvements in patient safety.
6
A limitation of the study was identified as they were unable to
standardize results between hospitals reviewed.
My initiatives to audit and address blood bank specimen labels with education and re-education
coincide with the above initiatives and suggested interventions to reduce errors. I also presented a
labeling lecture at our yearly skills day to help educated on proper labeling techniques for all specimens.
Our hospital has now undertaken an initiative to be stricter on accepting specimens, much like blood
bank, and to hold those accountable for errors. I believe these more drastic measures are necessary to
increase awareness and attention to preventing errors. The information provided in these studies and
articles supports my attempts at education off staff and prevention of lab specimen related errors.
References:
1. Hill, P. M., Mareiniss, D., Murphy, P., Gardner, H., Hsieh, Y. H., Levy, F., & Kelen, G. D. (2010).
Significant reduction of laboratory specimen labeling errors by implementation of an electronic
ordering system paired with a bar-code specimen labeling process. Annals of Emergency
Medicine, 56(6), 630-636. (LOE 4)
2. Snyder, S. R., Favoretto, A. M., Derzon, J. H., Christenson, R. H., Kahn, S. E., Shaw, C. S., ... &
Liebow, E. B. (2012). Effectiveness of barcoding for reducing patient specimen and laboratory
testing identification errors: a Laboratory Medicine Best Practices systematic review and meta-
analysis. Clinical Biochemistry, 45(13), 988-998. (LOE 1)
3. ONeill, E., Richardson-Weber, L., McCormack, G., Uhl, L., & Haspel, R. L. (2009). Strict adherence
to a blood bank specimen labeling policy by all clinical laboratories significantly reduces the
incidence of wrong blood in tube. American Journal of Clinical Pathology, 132(2), 164-168.
(LOE 7)
4. Tondon, R., Pandey, P., Mickey, K. B. C., & Chaudhary, R. (2010). Errors reported in cross match
laboratory: A prospective data analysis. Transfusion and Apheresis Science, 43(3), 309-314. (LOE
6)
5. Salinas, M., Lpez-Garrigs, M., Lillo, R., Gutirrez, M., Lugo, J., & Leiva-Salinas, C. (2013).
Patient identification errors: The detective in the laboratory. Clinical Biochemistry, 46(16), 1767-
1769. (LOE 7)
6. Reducing Errors in Blood Specimen Labeling: A Multihospital Initiative. Pennsylvania Safety
Authority, 8(2), 47-52. (LOE 7)
Anda mungkin juga menyukai
- Effective Difficult Conversations A Step-By-Step GuideDokumen129 halamanEffective Difficult Conversations A Step-By-Step GuidechocobrownieBelum ada peringkat
- Picot PaperDokumen16 halamanPicot Paperapi-24048640167% (3)
- NURS FPX4020 ChiuAmanda Assessment4 1Dokumen14 halamanNURS FPX4020 ChiuAmanda Assessment4 1brinju brianBelum ada peringkat
- JLS JLPT N1-N5Dokumen2 halamanJLS JLPT N1-N5Shienthahayoyohayoha100% (1)
- Personnel Planning and RecruitmentDokumen17 halamanPersonnel Planning and RecruitmentPiper FaustusBelum ada peringkat
- Scavenger Hunt-AnswersDokumen2 halamanScavenger Hunt-Answersapi-236445988Belum ada peringkat
- Ed Staff Meeting MinutesDokumen3 halamanEd Staff Meeting Minutesapi-236445988Belum ada peringkat
- 7 Effective Teaching Strategies For The ClassroomDokumen4 halaman7 Effective Teaching Strategies For The Classroomlea bendijo33% (3)
- References - International Student StudiesDokumen5 halamanReferences - International Student StudiesSTAR ScholarsBelum ada peringkat
- Planning Manual Punjab PDFDokumen115 halamanPlanning Manual Punjab PDFMunir HussainBelum ada peringkat
- Error in Laboratory TestDokumen8 halamanError in Laboratory TestBirupakshya RoutBelum ada peringkat
- Qualitative Article CritiqueDokumen9 halamanQualitative Article CritiqueJohn Smith100% (2)
- Medication ErrorsDokumen8 halamanMedication ErrorsMaricris Ambonan BawagBelum ada peringkat
- Inappropriateness in Laboratory Medicine An Elephant in The RoomDokumen4 halamanInappropriateness in Laboratory Medicine An Elephant in The RoomomaromranBelum ada peringkat
- Clinical Handover and Patient Safety Literature Review Report 2005Dokumen5 halamanClinical Handover and Patient Safety Literature Review Report 2005gw163ckjBelum ada peringkat
- Evidence Paper JpeacottricardosDokumen7 halamanEvidence Paper Jpeacottricardosapi-302415380Belum ada peringkat
- EBP Deliverable Module 2Dokumen6 halamanEBP Deliverable Module 2Marian SmithBelum ada peringkat
- NHS-FPX 4000 Applying Library Research SkillsDokumen7 halamanNHS-FPX 4000 Applying Library Research SkillsIrene WafulaBelum ada peringkat
- ADokumen6 halamanAlawrence otienoBelum ada peringkat
- Theory and Application in Transfusion Medicine at A Tertiary-Care InstitutionDokumen6 halamanTheory and Application in Transfusion Medicine at A Tertiary-Care InstitutionfegariasBelum ada peringkat
- RoilsDokumen4 halamanRoilsapi-568855135Belum ada peringkat
- Radiation Safety PaperDokumen4 halamanRadiation Safety Paperapi-692115810Belum ada peringkat
- Interventions To Decrease Catheter-Related Bloodstream Infections in The ICU: The Keystone Intensive Care Unit ProjectDokumen5 halamanInterventions To Decrease Catheter-Related Bloodstream Infections in The ICU: The Keystone Intensive Care Unit ProjectanggitaBelum ada peringkat
- Quasi-Experimentos Infect DeseaseDokumen8 halamanQuasi-Experimentos Infect DeseaseAlan MoraesBelum ada peringkat
- 6 - Texto - EHR Copy and Paste Can Get Physicians Into TroubleDokumen4 halaman6 - Texto - EHR Copy and Paste Can Get Physicians Into TroubleOmar FimbresBelum ada peringkat
- Continuous Quality Improvements and SafetyDokumen3 halamanContinuous Quality Improvements and Safetyapi-518020510Belum ada peringkat
- Roils PaperDokumen4 halamanRoils Paperapi-633434674Belum ada peringkat
- Adverse Event or Near-Miss Analysis (Nursing) .EditedDokumen10 halamanAdverse Event or Near-Miss Analysis (Nursing) .EditedMaina PeterBelum ada peringkat
- Radiation Oncology Incident Learning System (ROILS) Case StudyDokumen3 halamanRadiation Oncology Incident Learning System (ROILS) Case Studyapi-450246598Belum ada peringkat
- Decongested TherapyDokumen8 halamanDecongested TherapyprathibaBelum ada peringkat
- Bertholf2017 Chapter LaboratoryStructureAndFunctionDokumen23 halamanBertholf2017 Chapter LaboratoryStructureAndFunctionci8084102Belum ada peringkat
- Using Lean Principles To Optimise Inpatient Phlebotomy ServicesDokumen7 halamanUsing Lean Principles To Optimise Inpatient Phlebotomy ServicesMuizzuddin MuizBelum ada peringkat
- Get Homework/Assignment DoneDokumen6 halamanGet Homework/Assignment Donehomeworkping1Belum ada peringkat
- Improving Diagnosis in Health CareDokumen4 halamanImproving Diagnosis in Health CareHLMedit100% (1)
- Sources of Error in Epidemiological StudiesDokumen30 halamanSources of Error in Epidemiological StudiesFebrian FaisalBelum ada peringkat
- Correctly Identification of PatientDokumen9 halamanCorrectly Identification of PatientHezekiah AtindaBelum ada peringkat
- A Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayDokumen7 halamanA Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayRobert MaynardBelum ada peringkat
- Surgical Specimen IdentificationDokumen6 halamanSurgical Specimen IdentificationWanda JuszczukBelum ada peringkat
- Dependency On Laboratory Investigations For Diagnosis by DoctorsDokumen3 halamanDependency On Laboratory Investigations For Diagnosis by DoctorsshahzadBelum ada peringkat
- Clinical Question Final PaperDokumen13 halamanClinical Question Final Paperapi-253509573Belum ada peringkat
- Urine Specimen Collection - How A Multidisciplinary Team Improved Patient Outcomes Using Best Practices - ProQuestDokumen9 halamanUrine Specimen Collection - How A Multidisciplinary Team Improved Patient Outcomes Using Best Practices - ProQuestHelmy HanafiBelum ada peringkat
- A Class Based Approach For Medical Classification of Chest PainDokumen5 halamanA Class Based Approach For Medical Classification of Chest Painsurendiran123Belum ada peringkat
- Evidence-Based Dentistry What's NewDokumen5 halamanEvidence-Based Dentistry What's NewGanisht AzmiBelum ada peringkat
- Quantitative Article Critique and SummaryDokumen8 halamanQuantitative Article Critique and SummaryEmmanuelBelum ada peringkat
- Problem-Based Research PaperDokumen12 halamanProblem-Based Research Paperapi-349372265Belum ada peringkat
- Article - Medical ErrorsDokumen4 halamanArticle - Medical ErrorsDavid S. ChouBelum ada peringkat
- Terms Used in Patient Safety Related To Medication A Literature ReviewDokumen5 halamanTerms Used in Patient Safety Related To Medication A Literature ReviewckkuzaxgfBelum ada peringkat
- 420 Research PaperDokumen12 halaman420 Research Paperapi-372913673Belum ada peringkat
- Running Head: Sample Errors Analysis 1Dokumen10 halamanRunning Head: Sample Errors Analysis 1api-543686548Belum ada peringkat
- RoilsDokumen3 halamanRoilsapi-530935128Belum ada peringkat
- Medication Error Research PaperDokumen5 halamanMedication Error Research Paperafeaoebid100% (3)
- BronkitisDokumen10 halamanBronkitisTrisandi WiranegaraBelum ada peringkat
- Response ToDokumen7 halamanResponse ToReza AbdarBelum ada peringkat
- 12 Evidence Based Period Ontology Systematic ReviewsDokumen17 halaman12 Evidence Based Period Ontology Systematic ReviewsAparna PandeyBelum ada peringkat
- Radiation Safety Paper Week 2Dokumen4 halamanRadiation Safety Paper Week 2api-313040758Belum ada peringkat
- Final Safety Group Paper490WDokumen17 halamanFinal Safety Group Paper490WLYZETTE TERMANBelum ada peringkat
- Tni PaperDokumen7 halamanTni Paperapi-298609879Belum ada peringkat
- Variables Pre Post AnaliticaDokumen29 halamanVariables Pre Post AnaliticaRandy HuyhuaBelum ada peringkat
- Clinical Application DissertationDokumen4 halamanClinical Application DissertationDoMyPaperForMoneyUK100% (1)
- Role of Registered Nurses in Error Prevention, Discovery and CorrectionDokumen4 halamanRole of Registered Nurses in Error Prevention, Discovery and CorrectionEros CuestaBelum ada peringkat
- Ro-Ils Paper RsDokumen4 halamanRo-Ils Paper Rsapi-379797290Belum ada peringkat
- Tautho-Castillo - Criminal Responsibility For Medication ErrorsDokumen9 halamanTautho-Castillo - Criminal Responsibility For Medication ErrorsAlexis TauthoBelum ada peringkat
- Errors in Clinical Laboratories or Errors in Laboratory Medicine?Dokumen10 halamanErrors in Clinical Laboratories or Errors in Laboratory Medicine?DiegoMaradónBelum ada peringkat
- Week2 Submitter PaperDokumen3 halamanWeek2 Submitter Paperapi-299189797Belum ada peringkat
- Lauren Vandaniker Technology Impact On Nursing PracticeDokumen19 halamanLauren Vandaniker Technology Impact On Nursing PracticeAllysaBelum ada peringkat
- 10 Mertz ClusterRCThandhygieneDokumen8 halaman10 Mertz ClusterRCThandhygieneEddyOmburahBelum ada peringkat
- Unit B Element 2Dokumen6 halamanUnit B Element 2KimAdolfoBelum ada peringkat
- BB Graph 2013Dokumen1 halamanBB Graph 2013api-236445988Belum ada peringkat
- Email To Post Io PolicyDokumen1 halamanEmail To Post Io Policyapi-236445988Belum ada peringkat
- PPPPC June 2014 Take Back TipsDokumen1 halamanPPPPC June 2014 Take Back Tipsapi-236445988Belum ada peringkat
- Charge Nurse Meeting Minutes SampleDokumen2 halamanCharge Nurse Meeting Minutes Sampleapi-236445988Belum ada peringkat
- Summer 2014 NewsletterDokumen5 halamanSummer 2014 Newsletterapi-236445988Belum ada peringkat
- Education Committee Attendance Record 2013-14Dokumen2 halamanEducation Committee Attendance Record 2013-14api-236445988Belum ada peringkat
- Winter 2014 NewsletterDokumen4 halamanWinter 2014 Newsletterapi-236445988Belum ada peringkat
- Spring 2014 NewsletterDokumen5 halamanSpring 2014 Newsletterapi-236445988Belum ada peringkat
- Credential ResumeDokumen2 halamanCredential Resumeapi-236445988Belum ada peringkat
- Request To Defer Admission For International Applicants: ImportantDokumen1 halamanRequest To Defer Admission For International Applicants: Importantharsh rewariBelum ada peringkat
- ENGLISH A1 01 Greet People and Introduce YourselfDokumen15 halamanENGLISH A1 01 Greet People and Introduce YourselfNayaraBelum ada peringkat
- ICEUBI2019-BookofAbstracts FinalDokumen203 halamanICEUBI2019-BookofAbstracts FinalZe OmBelum ada peringkat
- A Study On Measuring of E-Shopping at Flipkart: Chapter-1Dokumen49 halamanA Study On Measuring of E-Shopping at Flipkart: Chapter-1MohanBelum ada peringkat
- Gonzalez SanmamedDokumen14 halamanGonzalez SanmamedGuadalupe TenagliaBelum ada peringkat
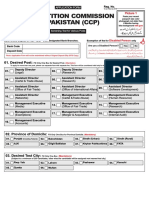
- Competition Commission of Pakistan (CCP) : S T NS T NDokumen4 halamanCompetition Commission of Pakistan (CCP) : S T NS T NMuhammad TuriBelum ada peringkat
- Babcock University Bookshop An Babcock University BookshopDokumen11 halamanBabcock University Bookshop An Babcock University BookshopAdeniyi M. AdelekeBelum ada peringkat
- Daily Lesson Plan: Learning Objectives: by The End of The Lesson Learners Will Be Able ToDokumen3 halamanDaily Lesson Plan: Learning Objectives: by The End of The Lesson Learners Will Be Able ToDaima HussainBelum ada peringkat
- Suchita Srivastava & Anr Vs Chandigarh Administration On 28 August 2009Dokumen11 halamanSuchita Srivastava & Anr Vs Chandigarh Administration On 28 August 2009Disability Rights AllianceBelum ada peringkat
- The Historical Development of Guidance and Counseling: September 2020Dokumen17 halamanThe Historical Development of Guidance and Counseling: September 2020Martin Kit Juinio GuzmanBelum ada peringkat
- Ps Mar2016 ItmDokumen1 halamanPs Mar2016 ItmJessie LimBelum ada peringkat
- Identity and MulticulturalismDokumen57 halamanIdentity and MulticulturalismbastajelenaBelum ada peringkat
- Amsterdam University College: Application Guidelines 2021-2022Dokumen16 halamanAmsterdam University College: Application Guidelines 2021-2022Vinod TanwaniBelum ada peringkat
- Implementasi Program Literasi Dalam Meningkatkan Minat Baca Siswa Madrasah Ibtidaiyah Negeri 4 Jakarta SelatanDokumen38 halamanImplementasi Program Literasi Dalam Meningkatkan Minat Baca Siswa Madrasah Ibtidaiyah Negeri 4 Jakarta SelatanDea ApriliyantiBelum ada peringkat
- Evidence Law Reading ListDokumen9 halamanEvidence Law Reading ListaronyuBelum ada peringkat
- Editorial Board 2023 International Journal of PharmaceuticsDokumen1 halamanEditorial Board 2023 International Journal of PharmaceuticsAndrade GuiBelum ada peringkat
- Media Information Literacy: Final ExaminationDokumen3 halamanMedia Information Literacy: Final ExaminationRodessa Marie Canillas LptBelum ada peringkat
- 10 Global Trends in ICT and EducationDokumen3 halaman10 Global Trends in ICT and Educationmel m. ortiz0% (1)
- Regional Ecology Center (REC) GuidelinesDokumen48 halamanRegional Ecology Center (REC) GuidelinesKarlou BorjaBelum ada peringkat
- Textile Conservation in Museums: Learning ObjectivesDokumen12 halamanTextile Conservation in Museums: Learning ObjectivesdhhfdkhBelum ada peringkat
- Syllabus Usi 101 1Dokumen10 halamanSyllabus Usi 101 1api-444977588Belum ada peringkat
- PE Assessment Plan 1-2Dokumen1 halamanPE Assessment Plan 1-2Rhuvy RamosBelum ada peringkat
- CMV RulesDokumen174 halamanCMV Rulessunithascribd100% (1)
- A Description of A CelebrationDokumen3 halamanA Description of A CelebrationzhannaBelum ada peringkat