Cardiovascular + Clinical Scenarios
Diunggah oleh
applesncoreDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cardiovascular + Clinical Scenarios
Diunggah oleh
applesncoreHak Cipta:
Format Tersedia
1
1
BLOOD VESSELS
Dr. Dexter MD FRC Path
Undercover Professor
DEPARTMENT OF PATHOLOGY
SGUSOM GRENADA (W.I.)
2
Anatomy & Histology
Three layers of
arteries
Intima
endothelial cells
Media smooth
muscle cells
Adventitia
connective
tissue
3
ENDOTHELIAL CELL FUNCTIONS
Maintenance of Permeability Barrier
Elaboration of Antithrombotic & Prothrombotic
Molecules
Modulation of Blood Flow and Vascular
Reactivity
Endothelin/NO
Regulation of Inflammation and Immunity
IL-1, IL-6
Regulation of Cell Growth
PDGF/TGF-
Oxidation of Low-Density Lipoprotein
4
Endothelial Dysfunction
Endothelial stimulation rapid, re-
versible; independent of new protein
synthesis.
Endothelial activation - alteration in
gene expression and protein synthesis
5
Characteristics of an activated endothelial cell
A normal arterial wall has anticoagulant properties and low leukocyte adhesivity
6
Complement products
Hypoxia
MHC molecules Viruses
Coagulation proteins Advanced glycosylation
end products
Vasoactive mediators Lipid products
Growth factors Hemodynamic forces
Cytokines / chemokines Bacterial products
Adhesion molecules Cytokines
Induced genes Activators
Endothelial activation
2
7
Vascular Smooth Muscle Cells
Functions
Vasoconstriction and dilation in
response to normal or pharmacological
stimuli
Elaboration of growth factors and
cytokines
Migration to the intima and proliferation
8
Diseases of Blood Vessels
Two principal mechanisms
1. Narrowing or complete obstruction of
the lumen either
progressively (atherosclerosis) or
suddenly (thrombosis)
2. Weakening of the wall of the vessel -
leading to dilatation or rupture.
9
Other Categories
Hypertension
Inflammatory disorders -vasculitis
Congenital Malformations
Neoplasms
10
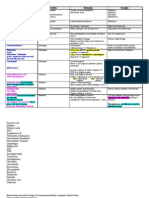
ARTERIOSCLEROSIS
ATHEROSCLEROSIS
LARGE BV
INTIMA
MEDIAL CALCIFIC
SCLEROSIS
MEDIA
ARTERIOLOSCLEROSIS
SMALL VESSEL
FULL THICKNESS
HYPERPLASTIC
HYALINE
11
Atherosclerosis
Derived from Greek word ATHEROS
soft gruel or porridge like
Chronic inflammatory disorder of
intima of large arteries characterized
by formation of fibro fatty plaques
called atheroma.
12
EPIDEMIOLOGY
Five Leading Causes of Death for Males and Females U.S.
3
13
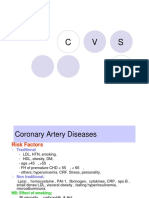
Atherosclerosis Major Risk
Factors
NONMODIFIABLE
Age
Gender
Genetic
predisposition
MODIFIABLE
Hyperlipidemia
Hypertension
Cigarette
smoking
Diabetes mellitus
14
Atherosclerosis
Uncertain, Unquantifiable or Possibly Lesser
Risk Factors
Hyperhomocystinemia
Lipoprotein (a)
Inhibitors of fibrinolysis
Low PA-1 Inhibitor
C-reactive protein
Lack of exercise
Type A personality
Obesity
Trans-unsaturated fat
intake
Postmenopausal
estrogen deficiency
High carbohydrate diet
Chlamydia pneumoniae
15
NON-MODIFIABLE RISK FACTORS
AGE - begins in childhood and progresses with
age
40 -60 yrs five fold increase in incidence of MI
SEX - Males > females
Uncommon in premenopausal women
Postmenopausal Increased incidence
Favorable response to HRT
GENETICS
Familial clustering of other risk factors
Familial hypercholesterolemia
16
MODIFIABLE RISK FACTORS
HYPERLIPIDEMIA
cholesterol most important
Major component associated with risk
LDL bad cholesterol.
inverse relationship between HDL levels
good cholesterol.
17
Evidences linking cholesterol with
Atherosclerosis
Genetic defects in lipoprotein metabolism
Familial hypercholesteremia defect in LDL
receptor hepatic uptake of LDL levels
of LDL
LDL because of abnormal apo E it fails to
bind to LDL receptor
Genetic or acquired diseases like DM &
hypothyroidism premature & severe
A.S.
18
Evidences linking cholesterol with
Atherosclerosis
Atheromas contain cholesterol & cholesterol esters
levels of cholesterol & LDL severity of A.S.
High cholesterol diets produce experimental A.S.
levels of cholesterol by diet/drugs progression
of A.S.
4
19
RISK FACTORS
HYPERTENSION
More importance after age of 45
169/95- 5 fold risk of developing IHD as
compared to 140/90
Anti hypertensive therapy reduces
incidence of A.S. associated diseases
stroke, IHD
20
RISK FACTORS
CIGARETTE SMOKING
Smoking & A.S. Made For Each Other
1/> packs/day for several yearsdeath rate
increases up to 200%
DIABETES MELLITUS
Cholesterol predisposition to AS
100x increased risk of AS induced gangrene
of the lower extremities.
risk of strokes and M.I.
AS in young patients Suspect DM
21
RISK FACTORS
PLASMA HOMOCYSTEINE
Hyper-
Homocystinuria -
Patients have
premature vascular
disease
Can be caused by
low folate & vitamin
B intake
22
RISK FACTORS
LIPOPROTEIN (a)
Altered form of LDL
Potentially atherogenic effects
Lipid accumulation
Endothelial cell modulation
Smooth muscle cell proliferation
Control of neo-vascularization
23
LESSER FACTORS
Stress
Type A personality
Obesity
MULTIPLE RISK FACTORS MAY
HAVE A MULTIPLICATIVE & NOT
ADDITIVE EFFECT
24
LOWER THE BETTER
Blood sugar
Blood pressure
Body weight
LDL
Stress levels
No. of cigarettes
5
25
PATHOGENESIS
RESPONSE TO INJURY HYPOTHESIS
Chronic inflammatory response of the
arterial wall initiated by some form of the
injury to the endothelium.
26
RESPONSE TO INJURY HYPOTHESIS
Role of endothelial cells endothelial injury
Endothelial activation
Increased permeability
Increased adhesion of leukocytes
Increased expression of adhesion molecules
Growth factors
Determinants of endothelial alterations
Hemodynamic factors increased frequency of
lesions at branch points, ostia of vessels
Hypercholesterolemia
27 28
RESPONSE TO INJURY HYPOTHESIS
Role of lipids
Cytotoxic to endothelium
Oxidized (modified) lipids have atherogenic
properties
readily ingested by macrophages foam cells
chemotactic for circulating monocytes
inhibits the motility of macrophages already in the
lesion
stimulates release of growth factors and cytokines
29
RESPONSE TO INJURY HYPOTHESIS
Role of macrophages
Cytokines like IL-1, TN (procoagulant
endothelium)F
Growth factors
Role of smooth muscle proliferation
Conversion of fatty streak into fibrofatty
atheroma
Role of T-cells
Recruitment and activation of monocytes
30
6
31 32
Atherosclerotic plaque
Three principal components
Cells smooth muscle cells,
macrophages, and other leukocytes
Extracellular matrix including collagen,
elastic fibers, and proteoglycans
Intracellular and extracellular lipid
deposits
33
Complicated lesion of
atherosclerosis
Calcification may be patchy or massive.
Focal rupture or gross ulceration, or both,
leading to
thrombus formation
cholesterol emboli or atheroemboli
Hemorrhage .
Superimposed thrombus
Aneurysmal dilatation atrophy of underlying
media
34
Sites of severe
atherosclerosis in
order of frequency
35
Atherosclerosis-Clinical
Manifestations
Coronary heart disease
(CHD)
Acute myocardial
infarction (AMI)
Angina Stable or
Unstable
Chronic ischemic heart
disease leading to
congestive heart
failure(CHF)
Sudden cardiac death
Abdominal aortic
aneurysm (AAA)
Cerebral vascular
disease
Stroke
Transient ischemic
attack (TIA)
Chronic ischemic
encephalopathy
Peripheral vascular
disease
Claudication
Ischemic bowel disease
(mesenteric occlusion)
Gangrene
36
PRECLINICAL
PHASE
7
37
Hypertension
38
Hypertension
Normal < 130 mm Hg systolic & < 85 mm Hg
diastolic)
Hypertension - Sustained increase in blood
pressure
Systolic > 140 mm Hg
Diastolic > 90 mm Hg
Mild + 20; Moderate +40; Severe +80 mm Hg
(systolic)
Malignant hypertension - > 210/120
39
Hypertension
25% of persons in general population are
hypertensive
Leading risk factor MI, DM, Stroke
Silent Killer painless complications
Complications bring to diagnosis but late
Chronic, end organ & vascular damage
40
Regulation of BP:
BP = Cardiac Output x Peripheral Resistance
Endocrine Factors
Renin, Angiotensin, ANP, ADH, Aldosterone.
Neural Factors
Sympathetic & Parasympathetic
Blood Volume
Sodium, Mineralocorticoids, ANP
Cardiac Factors
Heart rate & Contractility.
41
Etiologic Classification:
Primary/Essential Hypertension (95%)
Secondary Hypertension (5-10%)
Renal GN, RAS, Renin tumors
Endocrine Cushing, OCP, Thyrotoxicosis
Myxdema, Pheochromocytoma, Acromegaly.
Vascular Coarctation of Aorta, PAN, Aortic
insufficiency.
Neurogenic Psychogenic, Intracranial
pressure, polyneuritis etc.
42
Pathogenesis
Essential - multifactorial.
Increased peripheral resistance (sympathetic tone)
stress, hormonal, neural.
Genetic, familial, life style.
Secondary - Known abnormal control.
Increased blood volume - Sodium retention ADH,
Aldosterone.
Increased sympathetic tone - Adrenal tumors,
sympathetic stimulation.
Increased vasoactive hormones - Cushing's,
Pheochromocytoma,
8
43
GENETIC FACTORS
INCREASED
SYMPATHETIC
ACTIVITY
INCREASED
COP
INCREASED PERIPHERAL
RESISTANCE
HYPERTENSION
INCREASED RENAL
SODIUM RETENTION
INCREASED
BLOOD VOLUME
INCREASED RENIN
ALDOSTERONE ACTIVITY
AUTOREGULATION
ARTERIOLAR NARROWING
EXCESS DIETARY SODIUM
CHRONIC RENAL DISEASE
CUSHING SYNDROME
HYPERALDOSTERONISM
PHEOCHROMOCYTOMA
44
Malignant Hypertension:
Greater than 210/120 BP
May complicate any type of HTN.
Necrotizing arteriolitis.
Rapidly progressive end organ damage.
Renal failure
Left ventricular failure
Hypertensive encephalopathy
45
Hypertension - complications:
Large Blood Vessels
Atherosclerosis and its complications.
Small Blood Vessels
Arteriolosclerosis Hyaline & Hyperplastic
Heart
Left ventricular hypertrophy, Hypertensive
cardiomyopathy IHD, MI.
Kidney
Nephrosclerosis Benign & Malignant.
Eyes:
Hypertensive retinopathy, hemorrhage
Brain:
Haemorrhage, infarction (stroke),
46
Hyaline arteriosclerosis
Homogenous, pink, hyaline thickening of the
walls of the arterioles with loss of underlying
structural details and with narrowing of the
lumen.
Leakage of plasma components across vascular
endothelium and increasing extracellular matrix
production by smooth muscle cells
Chronic hemodynamic stress in hypertension or
metabolic stress in diabetes accentuates en-
dothelial injury
47
Hyperplastic arteriosclerosis
Related to more acute or severe
elevations of blood pressure
Onion-skin, concentric, laminated
thickening of the walls of arterioles with
progressive narrowing of the lumens.
Necrotizing Arteriolitis - deposits of
fibrinoid and acute necrosis of the vessel
wall.
48
VASCULITIS
Inflammation and necrosis of the blood
vessels, including arteries, veins, and
capillaries.
can be classified based on
Type of vessel involved
Etiology
9
49
Type of vessel involved
50
Etiology
Direct infection- Bacterial, Rickettsial, Spirochetal, Fungal
Immunological
Immune complex mediated
(hepatitis B or C virus mediated)
SLE and rheumatoid arthritis
Drug induced
Antineutrophil cytoplasmic antibody (ANCA) mediated
Wegeners granulomatosis
Churg-Strauss syndrome
Direct antibody attack mediated
Goodpasture syndrome (anti-GBM antibodies)
Kawasaki disease (antiendothelial antibodies)
Cell mediated
Allograft organ rejection
Unknown
Giant cell (temporal) arteritis
Takayasu arteritis
Polyarteritis nodosa
51
Anti- Neutrophil Cytoplasmic Antibodies
(ANCA)
Heterogeneous group of auto-antibodies
against enzymes mainly found within the
primary granules in neutrophils and in
lysosomes of monocytes and in endothelial
cells
P- ANCA: microscopic polyangiitis &
Churg-Strauss
C-ANCA: Wegners granulomatosis
52
c-ANCA
c-ANCA Proteinase-3
p-ANCA - Myeloperoxidase
IMMUNOFLUORESCENT STAINING
53
Giant Cell (Temporal) Arteritis
Most common vasculitis
Affects mainly the arteries in the head
Temporal
Vertebral
Ophthalmic can lead to blindness
Pathogenesis unknown
T-cell mediated immunologic reaction
against elastin?
54
Clinical features
Age: 50 and above
Gender: M:F: 1-1
Symptoms, Vague: fever, weight loss,
fatigue, facial pain, headache
Ocular symptoms: diplopia, progressive
hazy vision, loss of vision
10
55
Giant cell arteritis
Diagnosis: Temporal Artery Biopsy
2-3 cm segment
multiple sections
elastic trichrome stain
Treatment: Steroids, Analgesics
Prognosis: Good
Elevated ESR (sed-rate)
Association with polymyalgia rheumatica
56
Takayasu arteritis
Granulomatous vasculitis of
medium and large arteries
with obliteration of lumen
Most commonly affects arch
of aorta with narrowing or
virtual obliteration of the
origins of great vessels
arising in the arch
Can also involve pulmonary,
coronary, and renal arteries.
Etiopathogenesis
Unknown
57
Clinical features
Most common in females < 40 years
Ocular changes: visual disturbances, retinal
hemorrhages, blindness
Progressive diminution of upper limb pulses with
coldness or numbness of fingers - Pulseless
Disease
Low BP in upper limb
Neurologic defects dizziness, focal weakness
or complete hemiparesis
58
Polyarteritis Nodosa (PAN)
Systemic vasculitis
Transmural necrotizing inflammation of
small or medium sized muscular arteries
Typically involves renal and visceral
arteries and spares the pulmonary
circulation.
Arterioles, capillaries, and venules are not
affected
Associated with Hepatitis B antigen (30%)
59
r
e
Remember
No glomerulonephritis
Pathguy..com
Disease of
young adults
Course may be
acute,
subacute, or
chronic and is
frequently
remittent.
30% of
patients have
HBV antigen in
serum
Clinical features
60
Morphology
Gross - Distribution of lesions in descending order of
frequency
Kidney, Heart, Liver, GIT
Lesions have a predilection for branching points and
bifurcations
Histologically
Acute stage - Transmural inflammation, fibrinoid necrosis of the
inner half of the vessel wall.
Later stages - inflammation is replaced by fibrous thickening
of the vessel wall. Risks of thrombus or infarction.
All stages of activity may coexist in different vessels
or even within the same vessel characteristic
feature
11
61
Complications - PAN
Weakening of arterial wall owing to
inflammatory process may cause
aneurysmal dilatation or localized rupture.
Impairment of perfusion causing
ulcerations, infarcts, ischemic atrophy, or
hemorrhages in the areas supplied by
these vessels.
62
Kawasaki syndrome
Arteritis involving the large, medium, and
small arteries (often coronary arteries)
Associated with mucocutaneous lymph
node syndrome
Usually in young children and infants (80%
cases < 4 years)
Epidemic in Japan
Leading cause of acquired heart disease
in children in US (can lead to MI)
63
Kawasaki disease
Pathogenesis Unknown
Autoantibodies against endothelium, smooth
muscle cells, leading to acute vasculitis
Clinical features
Fever
Conjunctival and oral erythema
Edema of the hands and feet
Skin rash often with desquamation
Enlargement of cervical lymph nodes
64
Buerger disease
(Thromboangitis obliterans)
Characterized by segmental, thrombosing, acute
and chronic inflammation of medium sized and
small arteries, characterized by microabcesses
Mainly the tibial and radial arteries and sometimes
secondarily extending to veins and nerves of the
extremities (painful)
Predisposing factors
Cigarette smoking
Hypersensitivity reaction to tobacco direct endothelial
injury
Genetic influence
65
Wegener Granulomatosis
Classic triad
1. Acute necrotizing granulomas of upper and lower respiratory
tract
2. Focal necrotizing or granulomatous vasculitis affecting small to
medium sized vessels, most prominent in lungs, and upper
airways but affecting other sites as well
3. Renal disease in the form of focal or necrotizing, often
crescentic glomerulitis
Limited WG
No renal involvement
Males > females
Average age of onset = 40 years
95% of the patients have c-ANCA
66
Clinical features
Persistent pneumonitis with bilateral
nodular and cavitary infiltrates
Chronic sinusitis
Mucosal ulceration of the nasopharynx
Evidence of renal disease
Untreated patients die within 1 year.
12
67
Morphology
Gross ulcerative
lesions of the nose,
pharynx, palate
Lungs - dispersed
focal necrotizing
granulomas
coalesce to
produce nodules
that may undergo
cavitations.
68
Aneurysms
Localized abnormal dilatation of a blood
vessel caused by a congenital or
acquired weakness in the media.
Aneurysms can be classified based on
Composition of wall
Gross morphology
Etiology
69
Composition of the aneurysmal sac
True
Complete but attenuated vessel wall. The blood
remains within the confines of the circulatory
system.
Atherosclerotic, syphilitic, and congenital
vascular aneurysm
False (pseudoaneurysm)
is an extravascular hematoma that
communicates with the intravascular space.
70
71
Etiology
Atherosclerosis
Syphilis
Mycotic infective.
Vasculitis (PAN, Kawasakis disease)
Congenital defect in media Marfans
syndrome, Berry aneurysm
Iatrogenic Arteriovenous aneurysms for
chronic renal failure patients for dialysis
72
Atherosclerotic aneurysms
Most common site abdominal aorta
Abdominal aortic aneurysm - diameter is
increased at least 50%.
Most frequent aneurysms, usually
developing after the age of 50 years.
6% after the age of 80 years
13
73
Clinical course
Many aneurysms are asymptomatic.
Abdominal mass
Occlusion of a branch vessel- renal, mesenteric
vertebral vessels.
Embolism from atheroma or mural thrombus.
Impingement on an adjacent structure
compression of ureter or erosion of vertebrae.
Rupture with massive or fatal hemorrhage.
The risk of rupture - about 2% for a small
abdominal aortic aneurysm (<4 cm) to 25-40%
for aneurysms larger than 5 cm.
74
Treatment
Large aneurysms- surgically replaced by
prosthetic grafts.
Timely surgery is critical; operative
mortality is about 5% for unruptured
aneurysms whereas emergency surgery
after rupture carries a mortality rate of
>50%.
75
Syphilitic aneurysms
Seen in the tertiary stage of the syphilis.
Due to obliterative endarteritis of the vasa
vasorum of the aorta - Destruction of the
tunica media
Leading to narrowing of the lumen of these
vessels which causes ischemic injury of
the aortic media followed by inflammation
and scarring.
76
Clinical course
Encroachment on the mediastinal structures by
enlarged heart (Cor bovinum)
Respiratory difficulties.
Difficulty in swallowing.
Persistent cough due to pressure on recurrent laryngeal nerve
Pain caused by erosion of the ribs or vertebrae.
Valvular incompetence (aortic regurgitation) leading to
left ventricular hypertrophy, cardiac ischemia due to
obstruction to coronary ostia.
Rupture of the aneurysm.
Most common cause of death - heart failure due to
aortic regurgitation.
77
Aortic dissection (dissecting
hematoma)
Entry of blood in between and along the
laminar planes of media and its extension
along the length of the vessel.
Often ruptures causing massive
hemorrhage
Not usually associated with marked
dilatation of aorta
78
Etiopathogenesis
Most commonly men 40-60 years of age, in
whom hypertension is almost always present
(>90% of cases of dissection).
Younger patients with abnormality of connective
tissue (Marfans syndrome).
As a complication of
arterial cannulation (e.g. during diagnostic
catheterization or cardiopulmonary bypass)
During pregnancy - unknown reason.
Can result from cystic medial necrosis (loss of
elastic tissue)
14
79
Morphology
Intimal tear - starting point
Occurs most commonly in the ascending aorta,
1 or 2 cm above the aortic ring.
The dissection separates the inner two thirds of
the aorta from the outer third.
The dissection can extend proximally toward the
heart as well as distally along the aorta to
variable distances.
Re-rupture into the lumen of the aorta - double-
barreled aorta.
80
Double-barreled aorta.
81
2 Types
Type A - the more
common (and dangerous)
proximal lesions,
involving either the
ascending portion only or
both ascending and
descending aorta.
Type B distal lesions
not involving the
ascending part and
usually beginning distal to
subclavian artery
Type A Type B
82
Clinical features
Sudden onset of excruciating (tearing)
pain, usually beginning in the anterior
chest, radiating to the back, and moving
downwards as the dissection progresses.
Loss of one or more arterial pulses is
common
83
Complications
Most common cause of death - rupture of the
dissection into any of the three major body
cavities (i.e., pericardial. Pleural, and peritoneal)
Retrograde dissection into the aortic root leading
to disruption of aortic valvular apparatus.
Compression of spinal arteries - Transverse
myelitis.
Cardiac tamponade, aortic insufficiency, and
myocardial infarction can also occur.
84
Mycotic (infectious) aneurysms
result from the weakening of the vessel
wall by a microbial infection.
Common sites of involvement include the
aorta, cerebral vessels, and mesenteric,
renal, and splenic arteries.
15
85
Mycotic (infectious) aneurysms
Mycotic aneurysms may originate
At the site of sticking of a dislodged septic
embolus within a vessel, usually as a
complication of infective endocarditis
As an extension of adjacent suppurative
process like tuberculosis infection or a
bacterial abscess.
By circulating organisms directly infecting the
arterial wall.
86
HEART
SGUSOM GRENADA (W.I.)
87
Weights & Measurements of an
adult heart
- Weight Weight Weight Weight
- 250-300g males
- 200-250g - females)
- Wall thickness
- Right ventricle : 3-5 mm
- Left ventricle : 10-15 mm
- Cardiomegaly Cardiomegaly Cardiomegaly Cardiomegaly increase in cardiac weight or size
- Cardiac hypertrophy increased weight and ventricular
thickness
- Dilation enlarged chamber size
88
Normal Histology
The wall of the heart is composed of three layers
Epicardium
Myocardium
Endocardium
Heart is surrounded and enclosed by visceral and
parietal pericardium, separated by the pericardial
cavity.
Pericardial cavity contains 30-50 ml of fluid
- Acts as a shock absorber
89
VALVES
4 cardiac valves ( Mitral, Tricuspid, Aortic, and
Pulmonary valves)
Maintain unidirectional blood flow
- Scanty blood supply thin enough to be
nourished by diffusion from the hearts blood
Atrioventricular valves
Mitral and Tricuspid
The leaflets of these valves are held in place by the
chordae tendineae, which are contiguous with the
underlying ventricular wall.
Semilunar valves
Aortic and pulmonary valves guard the aorta and
pulmonary arteries respectively.
Three leaflets or cusps
90
BLOOD
SUPPLY
Left Coronary A.
L.A.Descending
Left Circumflex
Right Coronary A.
LCx
LAD
16
91
Blood supply
Functionally
- Right & left coronary arteries are end arteries
- Numerous interconnections collateral
circulation contains little blood in normal hearts
- Collaterals open up when one artery is severely
narrowed
Most blood flow to the myocardium is during
diastole
92
Heart failure
(congestive heart failure)
Is the inability of the heart, working at
normal or elevated filling pressure, to
pump enough blood to meet the metabolic
demands of the body.
93
Etiology
Systolic dysfunction inability to contract properly
MI
Hypertension
Volume overload valvular regurgitation
Cardiomyopathy
Diastolic dysfunction - Inability of the heart chamber
to relax/expand and fill sufficiently during diastole
Massive ventricular hypertrophy
Amyloidosis
Constrictive pericarditis
94
CHF can also be categorized as
Left-sided failure left ventricle is the failing
chamber
Systemic hypertension
Mitral or aortic valve disease
Ischemic heart disease
Cardiomyopathy
Right-sided failure
Left heart failure
Intrinsic disease of lung parenchyma/vasculature
COPD, Pulmonary hypertension
95
Compensatory Mechanisms
- Adrenergic stimulation by endogenous
catecholamines
- Myocardial hypertrophy
- Concentric hypertrophy - hypertension
- Eccentric hypertrophy valvular regurgitation
- Myocardial dilation - Frank Starlings law
increased force of contraction with dilation
96
Compensated heart failure dilated
ventricle is able to maintain cardiac output
to meet the needs of the body
Decompensated heart failure failing
myocardium is no longer able to propel
sufficient blood to meet the needs of the
body, even at rest.
17
97
HEART
FAILURE
DECREASED DECREASED DECREASED DECREASED
CARDIAC OUTPUT CARDIAC OUTPUT CARDIAC OUTPUT CARDIAC OUTPUT
RENAL RENAL RENAL RENAL
HYPOPERFUSION HYPOPERFUSION HYPOPERFUSION HYPOPERFUSION
SODIUM & SODIUM & SODIUM & SODIUM &
WATER RETENTION WATER RETENTION WATER RETENTION WATER RETENTION
RENIN RENIN RENIN RENIN- -- -ANGIOTENSIN SYSTEM ANGIOTENSIN SYSTEM ANGIOTENSIN SYSTEM ANGIOTENSIN SYSTEM
EDEMA
PASSIVE CONGESTION PASSIVE CONGESTION PASSIVE CONGESTION PASSIVE CONGESTION
OF PULMONARY CIRCULATION OF PULMONARY CIRCULATION OF PULMONARY CIRCULATION OF PULMONARY CIRCULATION
PULMONARY ARTERIAL PULMONARY ARTERIAL PULMONARY ARTERIAL PULMONARY ARTERIAL
HYPERTENSION HYPERTENSION HYPERTENSION HYPERTENSION
RIGHT HEART FAILURE
SEVERE & SEVERE & SEVERE & SEVERE &
SUSTAINED SUSTAINED SUSTAINED SUSTAINED
SYSTEMIC VENOUS
CONGESTION
PULMONARY EDEMA PULMONARY EDEMA PULMONARY EDEMA PULMONARY EDEMA
FORWARD FAILURE FORWARD FAILURE FORWARD FAILURE FORWARD FAILURE BACKWARD FAILURE BACKWARD FAILURE BACKWARD FAILURE BACKWARD FAILURE
98
Pathological consequences
of congestive heart failure
99
Clinical features
Left ventricular failure
Dyspnea
Orthopnea
Paroxysmal nocturnal dyspnea
Right ventricular failure
Systemic venous congestion
Distended neck veins
Enlarged tender liver
Soft tissue edema
100
Types of heart disease
Five categories of disease account for
nearly all cardiac mortality
1. Ischemic heart disease (IHD)
2. Hypertensive heart disease (systemic and
pulmonary)
3. Valvular heart disease
4. Non-ischemic (primary) myocardial disease
5. Congenital heart disease
101
ISCHEMIC HEART DISEASE (IHD)
Definition
Generic term for imbalance
between myocardial need for and
supply of oxygenated blood
102
Epidemiology
Leading cause of death for both men and
women in the US and other industrialized
nations
Each year nearly half a million Americans
die of IHD.
May affect any age, but most common in
older individuals
Males > females until the ninth decade
18
103
IHD - syndromes
1. Various forms of angina pectoris (chest pain)
2. Acute myocardial infarction (MI)
3. Sudden cardiac death
4. Chronic ischemic heart disease with congestive
heart failure
Acute coronary syndromes
MI
Unstable angina
Sudden cardiac death
104
ETIOLOGY
Atherosclerosis 90% of cases
Other causes of ischemia
Anemia - hypoxemia
Lowered systemic blood pressure - Shock
Increased cardiac demand hypertrophy,
exercise
Vasculitis (Kawasaki, PAN)
Aortic dissection
105
ETIOPATHOGENESIS
Complex dynamic interaction between
the following factors
1. Fixed coronary obstruction
2. Acute plaque changes
3. Coronary intraluminal thrombosis
4. vasoconstriction
106
Role of Acute Plaque Changes
Disruption of plaque an inability of
plaque to with stand imposed mechanical
stresses
Most often the initiating event
Changes in plaque morphology include
Hemorrhage
Rupture or fissuring
Erosion or ulceration
107
Vulnerable or Unstable Plaque
Characterized by
Moderately stenotic
plaque (50-75%)
Thinner fibrous cap
A core rich in lipid,
macrophages and T-
cells
less evidence of
smooth muscle
proliferation
Markedly eccentric
(not uniform around
the vessel
circumference)
METALLOPROTEINASES
T-cells activate
108
Role of Coronary Artery Thrombosis
Plaque rupture, erosion or ulceration exposure
of thrombogenic lipid and subendothelial
collagen
Platelet aggregation, thrombin generation and
thrombus formation.
If the vessel is completely occluded MI
Incomplete obstruction
Unstable angina or arrhythmias sudden cardiac
death
Embolization to distal branches - micro infarcts
19
109
Role of vasoconstriction
Increases mechanical forces that can contrib-
ute to plaque rupture
Stimulated by
Locally released platelet contents Thromboxane A2
Impaired secretion of EDRF Nitric oxide (NO)
relative to contracting factors (Endothelin)
Increased adrenergic activity
Smoking
110
Four syndromes
Angina pectoris (AP)
Myocardial infarction (MI)
Chronic ischemic heart disease
Sudden cardiac death (SCD)
Consequences
111 112
ANGINA PECTORIS
Intermittent chest pain or discomfort
due to transient, reversible myocar-
dial ischemia, not quite infarction
No elevation in cardiac enzymes
Three types
Typical (stable) angina pectoris
Prinzmetal (variant) angina
Unstable angina pectoris
113
Responds to vasodilators Responds to vasodilators Relieved by rest, vasodilators
Harbinger of subsequent MI
pre-infarction angina
Pain - crushing or squeezing
substernal, may radiate down
the left arm
Induced by disruption of
plaque with superimposed
thrombosis and possibly
vasospasm
Cause and mechanism not
clear
May be due to coronary artery
spasm
Due to critical stenosis -
reduction of coronary
perfusion due to fixed
stenosis
Associated with ST segment
elevation, indicative of
transmural ischemia
Associated with increased
demand -physical activity,
emotional excitement
Pain that occurs with
progressively increasing
frequency and is precipitated
with progressively less effort,
often occurs at rest, and
tends to be of more prolonged
duration.
Occurs at rest, awakens the
patient from sleep
Most common form
UNSTABLE (CRESCENDO) PRINZMETAL VARIANT
ANGINA
(~50-75% occlusion)
ANGINA
STABLE (TYPICAL) ANGINA
(~75% occlusion)
114
MYOCARDIAL INFARCTION
(HEART ATTACK)
Indicates the development of an area of
myocardial necrosis caused by local ischemia
About 1.5 million individuals in the US suffer an
acute MI annually, and approximately one third
of them die.
At least half of them die before they reach the
hospital.
Decreasing incidence since the early 1970s
20
115
Age
Occurs at any age
Incidence increases with increasing
age
Gender
Males 4 5 : 1 ages 45 54
Males 2 : 1 up to age 80
No difference > age 80
Epidemiology
116
MAJOR CONTRIBUTING FACTORS
Hypercholesterolemia
Smoking
Hypertension
Diabetes mellitus
CRP: Good marker for risk of MI
117
Pathogenesis
Coronary artery occlusion 90% of cases
Disruption of plaque 2/3
rd
are < 50% stenotic & 85%
have < 70% stenosis.
Remaining 10% of cases
Vasospasm isolated, intense and relatively
prolonged with or without coronary atherosclerosis
Emboli from the left sided mural thrombus
Unexplained
? Disease of small intramural coronary vessels
? Hematological abnormalities like hemoglobinopathies
118
Myocardial response
Coronary artery
obstruction loss of
critical blood supply to
the myocardium
Induces profound
functional,
biochemical, and
morphological
consequences
> 1 hr Microvascular
injury
20-40 min Irreversible cell
injury
ATP reduced
- To 50% of normal 10 min
- To 10% of normal 40 min
< 2 min Loss of
contractility
Seconds Onset of ATP
depletion
Time Feature
119
C CCO OOR RRO OON NNA AAR RRY YY C CCI IIR RRC CCU UUL LLA AAT TTI IIO OON NN A AAN NND DD T TTH HHE EE L LLO OOC CCA AAT TTI IIO OON NN O OOF FF I IIN NNF FF S SS A AAR RRC CCT TT
120
Progression of
myocardial
necrosis after coronary
artery occlusion
Begins in
subendocardial region
21
121
Morphology
The essential sequence of events in MI is
Coagulation necrosis followed by
Inflammation, resorption of necrotic
myocardium followed by
Formation of granulation tissue and finally
Organization of granulation tissue to form a
collagen rich scar tissue
122
collagen cellularity Firm, grey; scarring complete 2-8 weeks
Active granulation tissue Red-gray depressed border 10-14 days
Early coagulation necrosis Dark Mottling (Occasional) 4-12 hr
LM FEATURES GROSS FEATURES TIME
Dense collagenous scar Scarring complete 2 months +
Well developed phagocytosis
Extensive macrophages
Maximum softening
(no myocytes/no collagen)
7-10 days
Macrophages appear
Breakdown of myofibers
Central softening (Yellow/tan)
Hyperemic border
3-7 days
Heavy neutrophilic infiltrate Mottling (Yellow/tan center) 1-3 days
Early neutrophil infiltrate
Coagulation necrosis,
Contraction bands
Dark Mottling 12-24 hr
Wavy fibers No change 1/2-4 hr
No change No change 0-30 min
123
Contractile dysfunction cardiogenic shock
Arrhythmias
Papillary muscle dysfunction
External rupture of the infarct (3-7 days)
Ventricular free wall
Ventricular septum
Mural thrombi
Ventricular aneurysms (after fibrosis, 2+ months)
Pericarditis
Acute fibrinous or fibro hemorrhagic
Autoimmune Dresslers syndrome
COMPLICATIONS
124
Clinical features
Severe, crushing, substernal chest pain,
which may radiate to neck, jaw, epigastrium,
shoulder, or left arm
Levines sign (clenched fist over chest)
Pain lasts several hours to days and not
significantly relieved by vasodilators
Diaphoresis, dyspnea, rapid weake pulse
Silent MI
elderly patients
underlying Diabetes mellitus/ Hypertension
125
Clinical course
25% sudden death (SCD) vast majority of
deaths occurring before hospitalization
Patients reaching hospital alive
10 20% uncomplicated course
80 90% complicated but not necessarily
fatal course
Complicated course
Cardiac arrhythmias 75 95%
LVF with pulmonary edema 60%
Cardiogenic shock 10%
Rupture of myocardium 4 8 %
126
Diagnosis of MI
Myocardial infarction is diagnosed when
blood levels of sensitive and specific
biomarkers, such as cardiac troponin and
the MB fraction of creatine kinase (CK-
MB), are increased in the clinical setting of
acute ischemia
JACC, vol 36, No. 3, 2000:959-69
22
127
Electrocardiographic abnormalities
ST segment
elevation
Q wave
Inversion of
T wave
128
Cardiac Injury Markers
Creatine Kinase isoenzymes (CK-MB)
Troponins (I and T)
LD (lactate dehydrogenase, LDH)
Myoglobin
129
Troponin I and T
Troponins are most sensitive and specific
Regulate calcium-mediated muscle contraction
Normally not detectable in circulation
Troponin I (TnI) commonly measured clinically
Rise in 2-4 hours
Peak at 48 hours
Persists for 7-10 days
130
Creatine Kinase
CK is a dimer composed of M and B
subunits: MM, MB, BB
CK-MB: most specific for heart, trace
amount in skeletal muscle
Rises within 2-4 hours of MI
Peaks at 24 hours
Disappears by 72 hours
131
Cardiac Injury Markers
Early MI, TnI and CK-MB with similar sensitivity
Troponin is most specific for cardiac injury
Troponin STAYS elevated long after CK is gone
Both elevate sooner in reperfused patients
2 days of unchanged TnI and CK-MB r/o AMI
132
Intervention
Primary prevention
Thrombolysis
Angioplasty
Coronary bypass graft (CABG)
23
133
Chronic ischemic heart disease
Insidious onset of congestive heart failure
in patients who have past episodes of MI
or anginal attacks
Cardiac decompensation owing to
exhaustion of the compensatory
hypertrophy of non- infarcted viable
myocardium or severe coronary
obstructive disease leading to diffuse
myocardial dysfunction
Dilation of all 4 heart chambers (may
be difficult to distinguish from dilated
cardiomyopathy
134
Sudden Cardiac Death
Unexpected death from cardiac causes
early (usually within 1 hour) after or
without the onset of symptoms
Causes
IHD most common cause
Mitral valve prolapse
Aortic valve stenosis
Dilated or hypertrophic cardiomyopathy
Myocarditis
135
Ultimate mechanism of SCD is a lethal
arrhythmia
Morphology
80-90% of cases critical stenosis of one or
more coronary arteries, high grade stenosis
associated with acute plaque disruption
10-20% - non atherosclerotic in origin
136
Hypertensive heart disease
Presence of left ventricular hypertrophy in
an individual with a history of hypertension
and in whom other causes of hypertrophy
have been excluded
137
Pathogenesis
Stimulus sustained pressure overload
Growth factors
Local mechanical effects
Changes in genes controlling expression of actin, myosin
Hypertrophy
138
Morphology
Concentric hypertrophy of left ventricle
symmetric, circumferential pattern
Long standing cases right ventricular
hypertrophy and dilation
Histologically enlarged myocytes
containing large, hyperchromatic,
rectangular box-car shaped nuclei
24
139
Clinical features
Early stages asymptomatic
Angina pectoris
Signs and symptoms of heart failure with
progression
Cerebrovascular accidents (stroke)
Sudden cardiac death
140
Pulmonary heart Disease
(Cor Pulmonale)
Disease of right sided cardiac chambers
secondary to pulmonary parenchymal or
pulmonary vascular diseases
Excluded from this definition are
Pulmonary hypertension due to left heart
failure
Pulmonary hypertension due to congenital
heart disease
141
Acute cor pulmonale
Pulmonary embolism causing sudden
increase in burden on the right heart
Right ventricle is dilated but no
hypertrophy
Possible cause - Saddle embolus
142
Valvular Heart Disease
Congenital
Acquired
Valvular involvement by disease causes
Stenosis failure of a valve to open completely,
thereby impeding forward flow
Incompetence, regurgitation, or insufficiency failure
of a valve to close completely, thereby allowing
reversed flow
Abnormalities of flow often produce abnormal
heart sounds known as murmurs
143 Myocarditis
Marfan syndrome Dilated cardiomyopathy
Syphilitic aortitis Infective endocarditis
Degenerative aortic dilation
hypertension
Rheumatic heart disease
Rheumatic heart disease Myxomatous degeneration (mitral
valve prolapse
AORTIC REGURGITATION MITRAL REGURGITATION
Calcification of congenitally deformed
valve
Senile calcific aortic stenosis
Rheumatic heart disease Rheumatic heart disease
AORTIC STENOSIS MITRAL STENOSIS
Aortic valve disease Mitral valve disease
144
Rheumatic fever
Acute, immunologically mediated, multisystem
inflammatory disease that follows an episode of
rheumatogenic group A streptococcal
pharyngitis after an interval of few weeks.
Occurs in only about 3% of patients with group A
streptococcal pharyngitis
Mainly a disease of third world countries and
crowded, economically depressed areas of
western world
25
145
Pathogenesis
Exact pathogenesis is not known
Hypersensitivity reaction induced by group A
streptococci
Antibodies directed against the M proteins of
group A streptococci cross react with normal
proteins present in heart, joints, and other
tissues
Evidence in support of this hypothesis
Streptococci are absent from the lesions
Symptoms do not develop until 2-3 weeks after
infection
146
T-cells activated
by streptococcal
antigens
B-cells produce anti-streptococcal
antibodies
Antibodies and T-cells cross react with
Cardiac sarcolemma and valvular glycoproteins
147
Morphology- Acute rheumatic fever
Acute rheumatic carditis inflammatory changes
in all three layers of the heart Pancarditis
Myocarditis - Hallmark is the presence of Aschoff
bodies within connective tissue of the heart.
Endocarditis edematous and thickened valves
with foci of fibrinoid necrosis
Pericarditis fibrinous pericarditis
148
Arthritis chronic inflammatory infiltrate
and edema in the joints and periarticular
soft tissues.
arthritis is self limited and does not cause
chronic deformities
Erythema marginatum maculopapular
rash
Skin nodules contain focal lesions that
are essentially large Aschoff bodies
149
Chronic rheumatic heart disease
Chronic Mitral valvulitis
Conspicuous irregular thickening and calcification of
the leaflets, often with fusion of the commissures
and the chordae tendineae
Chronic aortic valvulitis cusps are thickened, firm,
and adherent to each other valve orifice is reduced to
rigid, triangular channel
150
Clinical features
Acute rheumatic fever
Occurs anywhere from 10 days to 6 weeks
after an episode of group A streptococcal
pharyngitis
Peak incidence 5-15 years
Arthritis migratory, large joints
Carditis pericardial friction rub, weak heart
sounds, congestive heart failure
Stenosis of mitral valve, most common and
characteristic complication
26
151
Clinical features
Chronic rheumatic carditis
Valvulitis - murmurs
Cardiac hypertrophy and dilation
Congestive heart failure
Arrhythmias
Infective endocarditis
152
Diagnosis
Jones criteria
Major manifestations (ACCNE)
Migratory polyarthritis of large joints
Pancarditis
Sydenham chorea involuntary, purposeless, rapid movements
Subcutaneous nodules
Erythema marginatum of skin
Minor manifestations Fever, Arthralgia, and elevated ESR
Presence of either of the 2 major manifestations or 1
major and 2 minor manifestations
+
Evidence of preceding streptococcal infection in the form
of elevated serum ASO titers or positive streptococcal
throat culture
153
Calcific aortic stenosis
Narrowing of the aortic valve lumen as a
result of deposition of calcium in the cusps
and the valve ring.
It can occur in
Elderly patients as a degenerative process.
90% of the patients are > 65 years of age
Congenital bicuspid aortic valve (40-65 years)
Aortic valve scarred as a result of rheumatic
fever (5-15 years)
154
Mitral valve prolapse
One of the most common cardiac disorder
occurring in 3-5% of the general adult
population.
Most cases are discovered between the
ages of 20 and 40 years
More common in females (7x)
May arise as a complication of Marfan
syndrome
155
Morphology
Soft and enlarged mitral valve cusps
ballooning of the valve leaflets into the left
atrium during systole
The chordae tendineae which are often
elongated and fragile, may rupture in
severe cases
The mitral annulus may be dilated
156
Clinical features
Most patients are asymptomatic
Palpitations
Fatigue or atypical chest pain
Mid-systolic click (when valve prolapses)
Severe complications in about 3 % of cases
Mitral regurgitation and congestive heart
failure
Infective endocarditis
Ventricular arrhythmias
27
157
Infective endocarditis
Infection of the cardiac valves or mural
surface of the endocardium resulting in the
formation of adherent, bulky mass of
thrombotic debris and organisms termed
vegetations
158
Classification
Clinical
Acute endocarditis destructive fulminant infection,
frequently of a previously normal heart valve with a
highly virulent organism, that leads to death within
days to weeks of more than 50% of patients despite
antibiotics and surgery.
Sub acute endocarditis organisms of low virulence
cause infection in a previously abnormal heart,
particularly on deformed valves. Most patients
recover with appropriate therapy.
Etiological Bacterial, Fungal, Rickettsial
159
Predisposing factors
Preexisting cardiac abnormality
Mitral valve prolapse most common factor
Chronic rheumatic valvulitis
Degenerative calcific aortic stenosis
Prosthetic heart valves 10-20% of cases
Intravenous drug abuse (Tricuspid valve!)
Transient bacteremia dental procedures,
urinary catheterization, endoscopy.
160
Pathogenesis
Hemodynamic factors
Abnormal blood flow across a damaged valve
Endothelial injury
Focal deposition of platelets and fibrin
Adherence properties of microorganisms
Fibronectin
Adhesion factors - polysaccharides
161
Causative organisms
Native valve
Most common (50-60%) Streptococcus viridans ; deformed
valves
Staph. aureus (10-20%) previously healthy or deformed valves
HACEK GROUP Haemophilus, Actinobacillus,
Cardiobacterium, Eikenella, Kingella
Prosthetic valve
Staph. Epidermidis
Gram negative bacilli
fungi
Intravenous drug abuse
Staph. Aureus most common
Streptococci
Gram negative bacilli
Fungi
162
Morphology
Mitral and aortic most commonly involved
Tricuspid valve I.V. drug abuse
Acute bacterial endocarditis
Gross
Bulky, friable vegetations that may obstruct the valve
orifice
Rapid destruction of the valves rupture of the
leaflets, chordae tendineae, papillary muscles
Ring abscess abscesses in perivalvular
myocardium
Microscopy
Large number of organisms mixed with fibrin and
blood cells
Minimal inflammatory response
28
163
Subacute endocarditis
Gross
Vegetations are less friable
Associated with less valve destruction
Ring abscesses uncommon
Microscopy
Presence of granulation tissue
Fibrosis, calcification
Chronic inflammatory infiltrate
164
Clinical features
Acute bacterial endocarditis
High grade fever with chills
Features of septicemia
Subacute bacterial endocarditis
Low grade fever; malaise
Weight loss
Changing cardiac murmurs
Splenomegaly
Clubbing of fingers
165
Glomerulonephritis
Immune complex formation Release of bacterial
antigen
CNS emboli and stroke,
myocardial infarction, splenic or
kidney infarcts, mycotic aneurysm
Splinter hemorrhagesnails
Janeway lesions (palms/soles)
Roth spotsretinal hemorrhage
Osler nodessubQ nodules in
pulp of digits
Peripheral emboli
Fragmentation
Congestive heart failure
Heart blocks (1, 2or 3)
Valvular insufficiency
AV conduction
abnormalities
Tissue destruction
Joint, bone, organ disease Seeding of distant sites
Constitutional symptoms Cytokine release
Persistent bacteremia
Host Consequence Complication
Consequence of
Vegetation
166
Diagnosis
Repeated blood cultures for both aerobic
and anaerobic organisms
Treatment
Difficult infection to eradicate avascular
nature of the valves
Antibacterial therapy
167
Nonbacterial thrombotic
Endocarditis
Characterized by the presence of sterile
vegetations
Pathogenesis incompletely understood
Endothelial abnormalities
Hypercoagulable states
Adenocarcinomas (pancreatic & other abdominal)
Usually asymptomatic
Embolization and infective endocarditis
possible complications
168
Libman- Sacks endocarditis
Characterized by presence of sterile
vegetations on the cardiac valves in
patients of SLE
No special predilection for the lines of valve
closure (vegetations on both sides)
Vegetations comprised of fibrin & WBCs
29
169
Myocarditis
Generalized inflammation of the myocar-
dium associated with necrosis and
degeneration of myocytes.
The inflammatory process plays a primary
role in the development of myocardial
injury.
170
Major causes of Myocarditis
Transplant rejection Bacteria c. diphtheriae
Helminthes trichinosis
Protozoa chagas
disease, toxoplasmosis
Drugs sulfonamides Fungi aspergillus,
candida
SLE Rickettsia typhus fever
Giant cell myocarditis Post streptococcal
rheumatic fever
Chlamydia- c. psittaci
Sarcoidosis Post viral Viral coxsackievirus,
CMV, ECHO, HIV
Unknown Immune-
mediated
Infections
171
Viral Myocarditis
Most common cause of myocarditis in US
Coxsackie A and B and other enter-
oviruses account for most cases
Pathogenesis
Direct viral cytotoxicity
Cell mediated immune reactions against
infected myocytes
Diffuse lymphocyte infiltrate with patchy
necrosis
infected myocyte
172
Clinical features
Most cases self limiting disease
Flu like symptoms viral myocarditis
Complications
Acute heart failure giant cell myocarditis
Chronic congestive heart failure viral myocarditis
Arrhythmias ventricular arrhythmias most
dangerous
173
Cardiomyopathy
Primary disease of the myocardium ex-
cluding myocardial diseases caused by
ischemia, hypertension, valvular lesions,
congenital anomalies, or inflammatory
disorders.
Three categories
Dilated cardiomyopathy
Hypertrophic cardiomyopathy
Restrictive cardiomyopathy
174
Dilated Cardiomyopathy
Most common type of cardiomyopathy
(90%)
Characterized by
Progressive cardiac hypertrophy
Dilation (of all 4 chambers)
Contractile (systolic) dysfunction
30
175
Etiopathogenesis
Idiopathic unknown, majority of cases
Genetic mutations 20-30% of cases
Dystrophin gene on X- chromosome
Mitochondrial genes abnormal oxidative phosphorylation
Alcohol direct cytotoxicity
Viral myocarditis
Nutritional disturbances thiamine deficiency,
chronic anemia,
Pregnancy associated - peripartum cardiomyopathy
pregnancy associated hypertension (reversible)
Nutritional disturbances
176
Clinical features
Fundamental defect is ineffective
contraction
Ejection fraction is < 25% (normal 50-
65%)
20-60 year most common
Progressive congestive heart failure
refractory to therapy
Death usually occurs due to progressive
cardiac failure or arrhythmias
177
Hypertrophic cardiomyopathy
Characterized by
Myocardial hypertrophy
Abnormal diastolic filling
Intermittent left ventricular outflow obstruction
in one third of cases
Primarily a diastolic rather than systolic
dysfunction
178
Pathogenesis
Familial autosomal dominant condition
50% of cases.
Occurs due to genetic defect in any of the
following genes
-myosin heavy chain most common
Cardiac troponin T
-tropomyosin
Myosin-binding protein C
179
Clinical features
Exertional dyspnea
Angina or MI
Sudden death due to arrhythmias
(especially in atheletes)
180
Restrictive Cardiomyopathy
(Decreased compliance)
Least common type of cardiomyopathy
Etiology
Endomyocardial fibrosis most common
cause
Lofflers syndrome
Radiation fibrosis
Amyloidosis
Hemochromatosis
Metastatic tumors
Sarcoidosis
31
181
Congenital Heart Disease
Abnormalities of the heart or great vessels
that are present from birth
Most common form of heart disease
among children
1% of live births, higher in premature
infants and stillborns
Incidence increased due to increased
diagnostic sensitivity
182
Etiology and pathogenesis
Only 10% well-defined environmental or genetic
influence
Trisomy 13,15,18,21, and Turner syndrome
Trisomy 21 the most common known genetic cause
Defect in sibling or parent the greatest risk factor
Environmental factors (congenital rubella)
183
Frequency of cardiac
malformations
1% Tricuspid atresia
1% Truncus Arteriosus
4% Transposition of the Great Vessels
5% Tetralogy of Fallot
4% Aortic stenosis
5% Coarctation of the Aorta
8% Pulmonary Stenosis
10% Atrial Septal Defect
7% Patent Ductus Arteriosus
42% Ventricular Septal Defect
% of Congenital
Heart Disease
Malformation
184
Malformation categories
Based on flow of blood
Left-to-right shunt
Right-to-left shunt
Obstruction
Based on cyanosis
Cyanotic from birth
Cyanotic later in life
Not cyanotic
185
Normal
186
Fetal circulation
32
187
Right-to-left Shunt:
Cyanotic heart defects
At birth: The Ts (Tetralogy of Fallot,
Truncus Arteriosus, Tricuspid Atresia,
Total Anomalous Pulmonary Venous
Connection, Transposition of the Great
Vessels)
After birth, when right-sided pressures
increase: Atrial Septal Defect, Ventricular
Septal Defect, Patent Ductus Arteriosus
188
Tetralogy of Fallot
Most common form of cyanotic congenital
heart disease
The four features of tetralogy are
Ventricular septal defect
Pulmonary stenosis
overriding aorta
right ventricular hypertrophy
189 190
Clinical features
Usually present by 6 months
Dyspnea on exertion, cyanosis
Polycythemia cerebral thrombosis
Infective endocarditis
Pulmonary vasculature decreased
Associated with Downs Syndrome
191
Transposition of the Great Arteries
Aorta off RV and
Pulmonary artery off
LV
AV connections
normal
Incompatible with
post natal life, unless
a shunt (VSD or PDA)
is present
192
Truncus Arteriosus
Failure of partitioning of embryologic
truncus into aorta and pulmonary artery
Single great artery gets blood from both
ventricles
Underlying VSD
Blood from both ventricles mixes
Cyanotic
33
193
Truncus Arteriosus
194
Left-to right shunts: The Ds
Atrial Septal Defect
Ventricular Septal Defect
Patent Ductus Arteriosus
195
Remember
Ds are red (acyanotic, left-to-
right shunt) and Ts are blue
(cyanotic, right-to-left shunt).
196
Ostium secundum
Septum primum
Membranous
I.V. septum
Muscular I.V.
Septum
197
Ventricular Septal Defect
Most common congenital heart lesion
Associated with Trisomy 21 (DS), 13, 18
Most commonly (90%) membranous
Most VSDs close spontaneously in childhood
Clinical features: Pulmonary hypertension; CHF,
pansystolic murmur,
Shunt reversal leads to cyanosis -
EISENMENGER COMPLEX
198
Atrial Septal Defect
10% of CHD
Age at presentation variable, may be
asymptomatic into adult
Most common congenital cardiac
malformation diagnosed in adults
Pulmonary vascularity increased if significant
left-to-right shunt
34
199
Three types Three types Three types Three types
75% Ostium secundum 75% Ostium secundum 75% Ostium secundum 75% Ostium secundum
15% Ostium primum 15% Ostium primum 15% Ostium primum 15% Ostium primum
10% Sinus venosus 10% Sinus venosus 10% Sinus venosus 10% Sinus venosus
200
Patent Ductus Arteriosus
7% of cardiac malformations
90% isolated anomaly
Females more common than males
Continuous, machinery-like murmur
May need to keep open with prostaglandin
E if associated with other malformations
Shunt may reverse leading to cyanosis
201
PDA Pathology
Connect left pulmonary artery to aortic
arch
Closes with high oxygen tension
Higher incidence in maternal rubella
infection
Associated with polycythemia
202
Patent Ductus Arteriosus
203
Obstructive Congenital Anomalies
Coarctation of the Aorta
Pulmonary Stenosis and Atresia
Aortic Stenosis and Atresia (Hypoplastic
Left Heart Syndrome)
204
Coarctation of the Aorta
Narrowed aortic lumen
Associated with Turners Syndrome
50% cases isolated cardiac anomaly
Remaining cases associated with PDA,
VSD, ASD
Two types
Preductal (infantile)
Postductal (adult)
35
205
PATHOGENESIS
206
Clinical features
Preductal - Presents in infancy as
Congestive heart failure
Selective cyanosis of lower extremities
Femoral pulses are weaker than those of the upper
extremities
Postductal presents in older children and adults
no selective cyanosis is seen
Hypertension of the upper extremities
Blood pressure is low and pulses are weak in lower
extremities
Notching of ribs due to collaterals
Intermittent claudication arterial insufficiency
207
TUMORS OF THE HEART
Primary tumors are rare
Most common are metastatic neoplasms
Clinical presentation
Sudden onset of severe, rapidly progressive
heart failure without apparent cause and/or
arrhythmia
Silent till impair function
208
Cardiac Myxomas
Most common primary tumor
Female preponderance
Age 30 60 years
Often calcify and can, at times, be
seen on X- ray
209
Morphology
Gross lobulated pedunculated mass
Most common location - Left atrium
Histologically multinucleated
stellate cells suspended in an
edematous mucopolysaccharide rich
stroma
210
Clinical features
Most are asymptomatic
Some may fragment and embolize
Ball-valve obstruction of atrioventricular
valve syncopal episodes, sudden death
Associated with diastolic murmur
36
211
Secondary Tumors
Direct extension of lung cancer
Breast
Lymphoma
Malignant melanoma
212
Pericardial diseases
Effusions -
Serous
Congestive heart failure
Hypoalbuminemia
Serosanguineous
Trauma
malignancy
Chylous mediastinal lymphatic obstruction
Hemopericardium cardiac tamponade
Ruptured aortic aneurysm or myocardial infarct
Penetrating traumatic injury
213
Pericarditis
Primary uncommon; usually infectious in
origin; virus most commonly
Secondary acute MI, cardiac surgery,
radiation, rheumatic fever, SLE,
Dresslers Syndrome
Uremia most common systemic disorder
associated with pericarditis
214
Clinical features
Chest pain; worsens on reclining
High-pitched friction rub
Cardiac tamponade
Faint distant heart sounds
Distended neck veins
Declining cardiac output
Shock
215
Morphology
Acute pericarditis fibrinous pericarditis
Chronic pericarditis
Delicate adhesions to dense, fibrotic scars
that obliterate the pericardial space
Extreme cases heart is completely encased
with dense scar tissue; can not expand
constrictive pericarditis
Anda mungkin juga menyukai
- AAFP Family Med Board QuestionsDokumen96 halamanAAFP Family Med Board QuestionsKamil Hanna100% (2)
- Thoracic Radiology For The Small Animal PractitionerDokumen149 halamanThoracic Radiology For The Small Animal PractitionerPaulo Matias Filho100% (10)
- Atherosclerosis and Its Complications-2Dokumen59 halamanAtherosclerosis and Its Complications-2Kelly YeowBelum ada peringkat
- Patofisiologi Jantung: Fika EkayantiDokumen59 halamanPatofisiologi Jantung: Fika EkayantiMaytaravikaHasan100% (1)
- PHAR 233 - Pathophysiology of CVS DisordersDokumen116 halamanPHAR 233 - Pathophysiology of CVS DisordersLina RamojBelum ada peringkat
- Lecture 28 - Pathology of DiabetesDokumen34 halamanLecture 28 - Pathology of Diabetesapi-3703352100% (4)
- Diseases of BLOOD VESSELSDokumen119 halamanDiseases of BLOOD VESSELSmeeeenonBelum ada peringkat
- 12 Blood VesselsDokumen26 halaman12 Blood VesselsBalaji DBelum ada peringkat
- Ch11-Vessels (1) 25Dokumen133 halamanCh11-Vessels (1) 25Anushka SharmaBelum ada peringkat
- Atherosclerosis PresentationDokumen90 halamanAtherosclerosis PresentationAbu SaifBelum ada peringkat
- Gene and CVS DiseasesDokumen61 halamanGene and CVS Diseasesnora almutairiBelum ada peringkat
- AtherosclerosisDokumen9 halamanAtherosclerosisSharmila SeeralanBelum ada peringkat
- Endocrinology - Dr. R. SilverDokumen44 halamanEndocrinology - Dr. R. SilverOmoloye AyooluwaBelum ada peringkat
- Pathological Changes of DM - 2023Dokumen53 halamanPathological Changes of DM - 2023Visura PrabodBelum ada peringkat
- Acute Myeloid LeukemiaDokumen29 halamanAcute Myeloid LeukemiaIsaac MwangiBelum ada peringkat
- Atherosclerosis 2023 CPP LectureDokumen50 halamanAtherosclerosis 2023 CPP LectureKing GeorgeBelum ada peringkat
- Cardiomyopathy: by Addise S. (MD, Asst. Professor of Internal Medicine) August, 2023Dokumen64 halamanCardiomyopathy: by Addise S. (MD, Asst. Professor of Internal Medicine) August, 2023mogesie1995Belum ada peringkat
- Systemic Lupus ErythematosusDokumen75 halamanSystemic Lupus ErythematosusThe AbyssinicansBelum ada peringkat
- K. Patologi Anatomi Endokrin 2Dokumen62 halamanK. Patologi Anatomi Endokrin 2Ade Cahyo Islami100% (1)
- AgeingDokumen27 halamanAgeingDhruti Mysore100% (1)
- 4 CardiomyopathyDokumen54 halaman4 CardiomyopathyDanny DesuBelum ada peringkat
- Disease of Blood VesselsDokumen5 halamanDisease of Blood VesselsKeshant SamarooBelum ada peringkat
- ATHEROSCLEROSISDokumen41 halamanATHEROSCLEROSISDoc On CallBelum ada peringkat
- Hypertension: Arwedi Arwanto Subbagian Ginjal-Hipertensi Bagian Ilmu Penyakit Dalam Rsup Dr. Kariadi FK Undip SemarangDokumen57 halamanHypertension: Arwedi Arwanto Subbagian Ginjal-Hipertensi Bagian Ilmu Penyakit Dalam Rsup Dr. Kariadi FK Undip SemarangRyzaAmirethaSaniBelum ada peringkat
- Cardiovascular Physio Logic ProcessDokumen35 halamanCardiovascular Physio Logic ProcessmatrixtrinityBelum ada peringkat
- Blok Sistem Metabolik & Endokrin (2015)Dokumen107 halamanBlok Sistem Metabolik & Endokrin (2015)Pretty HiaBelum ada peringkat
- Aspek Klinik Penyakit AutoimunDokumen46 halamanAspek Klinik Penyakit AutoimunDjumadi AkbarBelum ada peringkat
- AtherosclerosisDokumen41 halamanAtherosclerosisSachin KumarBelum ada peringkat
- Addison's Disease-Dr. AM IyagbaDokumen34 halamanAddison's Disease-Dr. AM IyagbaDr. Amb. Monday ZaccheausBelum ada peringkat
- EndocrinologyDokumen50 halamanEndocrinologyDonanguyen100% (2)
- Acute Lymphoblastic LeukaemiaDokumen20 halamanAcute Lymphoblastic LeukaemiaPrincewill SeiyefaBelum ada peringkat
- Disorders of The Immune System 3: Richard A. Mcpherson, M.DDokumen45 halamanDisorders of The Immune System 3: Richard A. Mcpherson, M.DrismaarnisBelum ada peringkat
- 7 - Endocrine Disorders 1Dokumen59 halaman7 - Endocrine Disorders 1boboBelum ada peringkat
- s2 Ikd Willy 2016Dokumen16 halamans2 Ikd Willy 2016Muhammad Ali MashuriBelum ada peringkat
- Chapter 43 - Thrombocytopenia and ThrombocytosisDokumen6 halamanChapter 43 - Thrombocytopenia and ThrombocytosisNathaniel SimBelum ada peringkat
- PancreasDokumen46 halamanPancreasgzrgythpyjBelum ada peringkat
- Pathology Lecture SeriesDokumen168 halamanPathology Lecture SeriesButch DumdumBelum ada peringkat
- Ischaemic Heart DiseaseDokumen66 halamanIschaemic Heart DiseaseImtiyazBelum ada peringkat
- 7 NOV 2023 Inborn Errors of Lipid MetabolismDokumen66 halaman7 NOV 2023 Inborn Errors of Lipid Metabolismwaleedemad649Belum ada peringkat
- LeukemiasDokumen31 halamanLeukemiasIsaac MwangiBelum ada peringkat
- Gangguan Darah & Sistem Reproduksi: Dr. Akhmad JufanDokumen49 halamanGangguan Darah & Sistem Reproduksi: Dr. Akhmad JufanSintia EPBelum ada peringkat
- Blood Vessel Diseases LEVEL IIDokumen33 halamanBlood Vessel Diseases LEVEL IIDavid Ogechi AtandiBelum ada peringkat
- Acute Myeloblastic Leukaemia: BY DR Halima Talba Consultant Haematologist Department of Haematology and BtsDokumen44 halamanAcute Myeloblastic Leukaemia: BY DR Halima Talba Consultant Haematologist Department of Haematology and BtsMuhammad Modu BulamaBelum ada peringkat
- DM in ElderlyDokumen34 halamanDM in ElderlyMariaa EndahhBelum ada peringkat
- Cardiovascular DiseaseDokumen7 halamanCardiovascular Diseaseمروه الغابريBelum ada peringkat
- AtherosclerosisDokumen51 halamanAtherosclerosisWilliam Wong100% (1)
- 14cardiovascular Diseases (CVD)Dokumen18 halaman14cardiovascular Diseases (CVD)fatima.noor0747Belum ada peringkat
- Clinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreDokumen74 halamanClinical Medicine Hypertension: DR - Muhammad Nauman Senior Lecturer (DOVS) University of The LahoreNoman MunirBelum ada peringkat
- Metabolic Syndrome & Cardiovascular Disease Relationships: A World Wide Pandemic DR Yuliana Rahmah, SPPDDokumen33 halamanMetabolic Syndrome & Cardiovascular Disease Relationships: A World Wide Pandemic DR Yuliana Rahmah, SPPDAhmad Jaelani Jayadi SiajengBelum ada peringkat
- Preventionandcontrolofchronicdiseases 140121035128 Phpapp01Dokumen77 halamanPreventionandcontrolofchronicdiseases 140121035128 Phpapp01SaadBelum ada peringkat
- Cardiomyopathies: Budi Yuli Setianto Department of Cardiology Faculty of Medicine Gadjah Mada University YogyakartaDokumen43 halamanCardiomyopathies: Budi Yuli Setianto Department of Cardiology Faculty of Medicine Gadjah Mada University YogyakartaadnajaniBelum ada peringkat
- Cagayan State University College of Medicine and Surgery SY: 2009-2010Dokumen41 halamanCagayan State University College of Medicine and Surgery SY: 2009-2010ahmad usmanBelum ada peringkat
- CVS 1 PDFDokumen24 halamanCVS 1 PDFafaq alismailiBelum ada peringkat
- Autoimmune Polyglandular SyndromesDokumen76 halamanAutoimmune Polyglandular SyndromesSenoAriBelum ada peringkat
- Haematological Malignancies: Dr. Maruf Bin Habib Associate Professor of Medicine UamcDokumen54 halamanHaematological Malignancies: Dr. Maruf Bin Habib Associate Professor of Medicine UamcSaifSeddikiBelum ada peringkat
- The Endocrine Systyem NDokumen93 halamanThe Endocrine Systyem NMuh YaminBelum ada peringkat
- Leukamia and Transfusion MedicineDokumen26 halamanLeukamia and Transfusion MedicineSamuel kuriaBelum ada peringkat
- ThrombophiliaDokumen46 halamanThrombophiliaNabelle MarieBelum ada peringkat
- Pathology of Endocrine System: Dr. Nesreen Bataineh MD, FrcpathDokumen20 halamanPathology of Endocrine System: Dr. Nesreen Bataineh MD, FrcpathQutaybah JahmanyBelum ada peringkat
- Acute Myeloid LeukemiaDokumen10 halamanAcute Myeloid LeukemiaMinakshi MawariBelum ada peringkat
- Renal Pathology: Kidney and The Urinary Collecting SystemDokumen37 halamanRenal Pathology: Kidney and The Urinary Collecting Systemapplesncore100% (1)
- Pediatric PathologyDokumen27 halamanPediatric PathologyapplesncoreBelum ada peringkat
- Gastrointestinal Tract (Partial Edit)Dokumen47 halamanGastrointestinal Tract (Partial Edit)applesncoreBelum ada peringkat
- CardiopathophysiologyDokumen63 halamanCardiopathophysiologyapplesncoreBelum ada peringkat
- CardiopathophysiologyDokumen63 halamanCardiopathophysiologyapplesncoreBelum ada peringkat
- Pathology of The Lung Objectives: Define and Use in Proper Context The Following TermsDokumen45 halamanPathology of The Lung Objectives: Define and Use in Proper Context The Following TermsapplesncoreBelum ada peringkat
- Hematopoietic SystemDokumen39 halamanHematopoietic SystemapplesncoreBelum ada peringkat
- Neoplasia Path NotesDokumen13 halamanNeoplasia Path NotesapplesncoreBelum ada peringkat
- ImmunopathologyDokumen21 halamanImmunopathologyapplesncoreBelum ada peringkat
- Pathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2Dokumen25 halamanPathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2applesncoreBelum ada peringkat
- Fluid and Hemodynamic DisordersDokumen19 halamanFluid and Hemodynamic DisordersapplesncoreBelum ada peringkat
- Gluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)Dokumen3 halamanGluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)applesncoreBelum ada peringkat
- Teaching Internal Medicine Pearls On The WardsDokumen212 halamanTeaching Internal Medicine Pearls On The WardsAnonymous ZeqcLl100% (10)
- Cardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With CardiacDokumen10 halamanCardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With Cardiacmerin sunilBelum ada peringkat
- Fitz Cardiology Paces NotesDokumen26 halamanFitz Cardiology Paces NotesMuhammad BilalBelum ada peringkat
- Pearls in CardiologyDokumen65 halamanPearls in CardiologyAmber MerrittBelum ada peringkat
- (Mahesh Chandra) Objective Cardiology PDFDokumen609 halaman(Mahesh Chandra) Objective Cardiology PDFfajarBelum ada peringkat
- All MRCP Theory Notes For DR Abeer in One PDFDokumen3.151 halamanAll MRCP Theory Notes For DR Abeer in One PDFRumana Ali100% (2)
- 118a - CardiomyopathyDokumen10 halaman118a - CardiomyopathyJoanna TaylanBelum ada peringkat
- Cos105000 H-P-Cosmos Instructions For Use 150 50 LC HPC Master Rev 1.02Dokumen102 halamanCos105000 H-P-Cosmos Instructions For Use 150 50 LC HPC Master Rev 1.02empiricaorasureBelum ada peringkat
- International Journal of Medical StudentsDokumen132 halamanInternational Journal of Medical StudentsDan BoicuBelum ada peringkat
- CardiomyopathiesDokumen13 halamanCardiomyopathiesNinna Isabel VictorioBelum ada peringkat
- Soal Cardio VascularDokumen27 halamanSoal Cardio VascularJonathan FebiantoBelum ada peringkat
- 病理國考複習 PDFDokumen61 halaman病理國考複習 PDFAnonymous ZUQcbcBelum ada peringkat
- Cardiology - MRCP NotesDokumen5 halamanCardiology - MRCP NotesShazina Kohli100% (1)
- 2021 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyDokumen107 halaman2021 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyLourdes FrancoBelum ada peringkat
- Stress-Induced (Takotsubo) CardiomyopathyDokumen13 halamanStress-Induced (Takotsubo) CardiomyopathyAdrian GeambasuBelum ada peringkat
- Drug Name Mode of Action Indications Contraindications Side Effects/ Advserse Effects (Specify) Nursing InterventionsDokumen4 halamanDrug Name Mode of Action Indications Contraindications Side Effects/ Advserse Effects (Specify) Nursing InterventionsKaterina Petrova100% (1)
- Cardiology An Integrated Approach Human Organ Systems Dec 29 2017 - 007179154X - Mcgraw Hill 1St Edition Elmoselhi Full ChapterDokumen52 halamanCardiology An Integrated Approach Human Organ Systems Dec 29 2017 - 007179154X - Mcgraw Hill 1St Edition Elmoselhi Full Chapterdouglas.zimmer226100% (17)
- Anaesthesia For Cardiac DiseaseDokumen26 halamanAnaesthesia For Cardiac DiseasePrabhu KumarBelum ada peringkat
- Cardiomyopathy SeminarDokumen17 halamanCardiomyopathy SeminarJyoti SinghBelum ada peringkat
- Packrat 14 - 2009Dokumen86 halamanPackrat 14 - 2009EmersonMoreno80% (5)
- What Is CardiomyopathyDokumen8 halamanWhat Is CardiomyopathysakuraleeshaoranBelum ada peringkat
- Cardiomegaly in CatsDokumen2 halamanCardiomegaly in CatspilipBelum ada peringkat
- OBGYN Quick Notes Full - pdf-1162990791Dokumen104 halamanOBGYN Quick Notes Full - pdf-1162990791Delphine Sistawata Akwo100% (3)
- Aortic StenosisDokumen8 halamanAortic Stenosisdr.moni.co.ukBelum ada peringkat
- Board Desember 2015 Fix Answer - BALIDokumen67 halamanBoard Desember 2015 Fix Answer - BALIrahageng wida kusuma100% (1)
- Cardiomyopathy and HeartDokumen20 halamanCardiomyopathy and HeartDewi AnggrainiBelum ada peringkat
- 03.cleveland Clinic of Pediatrics - Selected Questions PDFDokumen17 halaman03.cleveland Clinic of Pediatrics - Selected Questions PDFLakshaya SinghBelum ada peringkat