Rehabilitacion Succion
Diunggah oleh
Angela Grillo Pizarro0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
30 tayangan11 halamanThis study examined the effects of oral sensory stimulation therapy on 14 infants aged 9 to 210 days old who had sucking abnormalities. The infants lacked at least one oral reflex and had two or more abnormal sucking signs or one abnormal sign and two abnormal reflexes. Therapy was performed three times daily for five days. After therapy, oral reflexes improved and abnormal sucking signs decreased. Milk volumes consumed and sucking rates also increased significantly. The study concluded that oral sensory and motor stimulation can help normalize oral motor functions and feeding in infants with sucking disabilities.
Deskripsi Asli:
Judul Asli
rehabilitacion succion
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniThis study examined the effects of oral sensory stimulation therapy on 14 infants aged 9 to 210 days old who had sucking abnormalities. The infants lacked at least one oral reflex and had two or more abnormal sucking signs or one abnormal sign and two abnormal reflexes. Therapy was performed three times daily for five days. After therapy, oral reflexes improved and abnormal sucking signs decreased. Milk volumes consumed and sucking rates also increased significantly. The study concluded that oral sensory and motor stimulation can help normalize oral motor functions and feeding in infants with sucking disabilities.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
30 tayangan11 halamanRehabilitacion Succion
Diunggah oleh
Angela Grillo PizarroThis study examined the effects of oral sensory stimulation therapy on 14 infants aged 9 to 210 days old who had sucking abnormalities. The infants lacked at least one oral reflex and had two or more abnormal sucking signs or one abnormal sign and two abnormal reflexes. Therapy was performed three times daily for five days. After therapy, oral reflexes improved and abnormal sucking signs decreased. Milk volumes consumed and sucking rates also increased significantly. The study concluded that oral sensory and motor stimulation can help normalize oral motor functions and feeding in infants with sucking disabilities.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 11
Or i g i n a l Ar t i c l e I ndi an J Pedi at r 1999; 66 : 319-329
As s e s s me nt of Sensori al Oral St i mul at i on i n Infants wi t h
Suck Feedi ng Di s abi l i t i es
M. E. R e n d 6 n - M a c f a s 1, L. A. C r u z - P e r e z 2, M. R . M o s c o - P e r a l t a 3, M . M . S a r a i b a - R u s s e l P ,
S. L e v i - T a j f e l d s a n d M . G . M o r a l e s - L 6 p e z 6
~'ZSDepartamc~zto Lactantes - Unidad de Investigaci6n en Epidemiologia Clfnica, and
~'+'+Departamento de Medicina F{sica y Rehabilitaci6n, Hospi t al de Pediatm'a Centro Mddico
Nacional siglo XXI, Inst i t ut o Mexicano del Seguro Socialr Mdxico Distrito Federal
A b s t r a c t : A non- r andomi s ed si ngl e bl i nd st udy was under t aken t o det er mi ne t he cl i ni cal and
physi ol ogi cal c hanges i n suck f eedi ng af t er sensor i al oral st i mul at i on, in f our t een pat i ent s age 9
to 210 days ol d wi t h sucki ng al t erat i ons. Pat i ent s l acked at l east one of t he f i ve oral refl exes, pl us
two or mor e abnor mal sucki ng si ngs or at l east one abnor mal sucki ng si gn, pl us t wo or mor e
abnormal oral r ef l exes.
Oral sensor i al t her apy was per f or med t hr i ce dai l y f or f i ve days. The number of absent oral re-
fl exes, number of abnor mal sucki ng si gns, vol ume of mi l k f or nursi ng and sucki ng rate, wer e reg-
i stered. Di f f er ences of medi ans wer e t est ed usi ng Fr ei dman' s t est and di f f er ent i al of pr opor t i ons
using Cochr an' s Q test.
Af t er t her apy, oral r ef l exes wer e r ec ov er ed (2, 0- 4 vs. 5, 5- 5, p = 0. 0000, medi an r ank of
absence oral r ef l exes) and t he number of abnormal sucki ng si gns decr eased (6,1-9 vs. 1, 0-4; p =
0. 0000). Ther e wer e st at i st i cal l y si gni f i cant i mpr ovement s in pat i ent s who had l ost l aunch up
ni ppl e abi l i ty (p = 0. 005), del ay at t he begi nni ng of sucki ng (p = 0. 0022), dr awi ng of milk from t he
mout h (p = 0. 0001) , c y anos i s (p = 0. 0084) , weani ng (p = 0. 0004) and pr ol onged sucki ng (p =
0.0038). Even i n pat i ent s wi t h moder at e i mprovement , no s t at i s t i c al di f f er ences wer e obser ved in
ni ppl e r oot i ng (p = 0. 09) and c oughi ng (p = 0. 09). No c hanges wer e obs er v ed in pat i ent s who
had cr i ed (p = 0. 31) and spi t t ed (p = 0. 51) dur i ng f eedi ng. At t he end of t her apy, vol umes of
c ons umed mi l k we r e i nc r eas ed at each f eedi ng ( 10 ml, 0- 40 vs. 50 ml, 25- 60; p = 0. 0001) .
Sucki ng rates al so i ncr eased (22 sucks/ mi nut e, 10-35 vs. 40. 5, 35-48; p = 0.0044).
Oral sensor i al and mot or st i mul at i on nor mal i se oral mot or r ef l exes, di mi ni sh t he cl i ni cal
abnormal sucki ng si gns and i ncr ease mi l k vol umes i ngest ed f or nursi ng.
( I n d i a n J P e d l a t r 1 9 9 9 ; 6 6 : 3 1 9 - 3 2 9 )
Key words : S u c k i n g ; Re h a b i l i t a t i o n ; Nur s i ng.
Recent advances in neonat al medi ci ne have
i ncr eased t he n u mb e r of hi gh- r i s k
Re pr i nt r equest s : Mario Enri que Rend6n
Maclas, Uni dad de l nvest i gaci 6n en Epidemi-
ologia Clinica Hospi t al de Pedi at ri a Cent ro
M6dico Nacional siglo XXI, Instituto Mexicano
del Seguro Social, Aveni da Cuauht 6moc #330
colonia Doctores, CP 06720, M6xico Distrito
Federal
n e wb o r n s r e qui r i ng l ong- s t ay hospi t al i sa-
t i on a nd s peci al car e. The n e o n a t e ' s or al -
mo t o r f unct i on a nd abi l i t y to c ons ume ad-
equat e mi l k vol umes ar e s ome f act or s t hat
i nf l uence t he l engt h of st ay at t he neonat al
i nt ensi ve car e uni t ( NI CU) and t he t ype of
f ol l ow- up s er vi ces r e c o mme n d e d at di s-
char ge 1. Ther ef or e, some at t t hor s ha ve sug-
gest ed t hat a f eedi ng p r o g r a mme f or hi gh-
320 M:E. RE NDON- MAd AS ET AL Vol. 66, No. 3, 1999
risk neonat es coul d be effective in avoi di ng
hospi t al compl i cat i ons associ at ed wi t h the
use of t ot al par ent er al nut r i t i on (TPN) or
oral-gastric, nasogast ri c, gast rost omy, and
ent erost omy tubes, if feeding disabilities are
i mproved ~,4.
Feedi ng is a compl ex mot or activity and
serves as a mar ker of neurol ogi cal mat ura-
tion. Coor di na t e d f eedi ng in i nfant s re-
qui res the sensori al and mot or i nt egrat i on
of suckl i ng, s waUowi ng and br eat hi ng,
wher e several muscl e gr oups part i ci pat e in
an observabl e rhythmic process s.
Sucki ng abnormal i t i es have been classi-
fied into three groups based on their causes.
The first gr oup is t he i mmat ur e sucki ng,
seen in pr et er m i nfant s less t han 34 weeks
post concept i onal age, and has been charac-
terised by a weak, poor and uncoor di nat ed
sucking pat t er n 6 & Some aut hors have sug-
gest ed t hat i nfant s who are subj ect ed to
mi l d or l ow st ress condi t i ons begi n to de-
vel op a mat ur e sucki ng pat t er n appr oxi -
mat el y t wo weeks after t hey reach the 37th
we e k of pos t concept i onal cor r ect ed age
wi t h or wi t hout therapyl,~.L The second
gr oup compr i s es i nfant s wi t h dys f unc-
t i onal sucki ng pat t er ns associ at ed wi t h
structural oral abnormal i t i es requiring sur-
gery 1~ The last gr oup of infants have sev-
eral degrees of di sorgani sat i on a n d / o r dys-
funct i on for sucki ng associ at ed wi t h vari-
ous clinical pat hol ogi es whi ch i nt erfere
wi t h the devel opment of nor mal sucki ng 1.
These i nfant s have a hi st or y of ser i ous
forms of clinical pat hol ogi es requi ri ng pro-
l onged or ot r acheal i nt ubat i on (for over a
week), l ong per i ods of fast i ng, TPN or
orogastric t ube feeding. They are exposed to
noxious oral stimuli that increase the devel -
opment of aberrat i ons on sucki ng pat t erns
a n d / o r st r uct ur al oral abnor mal i t i es as
pal at al gl ove 12,~3. Some of t hem event ual l y
devel op neurol ogi cal disabilities if t hey do
not receive adequat e t her apyt
Vari ous st rat egi es have been i mpl e-
ment ed to i mprove the oral - mot or skills of
neonates wi t h feeding disabilities. Some au-
t hor s appl i ed t he non- nut r i t i ve sucki ng
strategy usi ng a pacifier to accelerate mat u-
ration of the sucking reflex when the infant
was in the fasting periods. This facilitated a
more rapi d transition from non-oral to oral
feeding 14,1s. Other researchers demonst rat ed
that peri oral st i mul at i on wi t h gent l e pres-
sure stimuli to the oral muscul at ure signifi-
cant l y i ncr eased t he rat e of sucks per
mi nut e and the vol ume of milk consumedL
In 1987, Case-Smith appl i ed perioral stimu-
l at i on wi t h r hyt hmi cal pr es s ur e to the in-
fant s' t ongues and s uppor t to the j aw and
t ongue st abi l i t y dur i ng feedi ng, wi t h ves-
tibular stimuli to three high risk pret erm in-
fants wi t h feeding problems. After t wo days
of t her apy infants s howed i mpr ovement in
t hei r t ot al sucki ng scores, but it was ob-
ser ved t hat t he i mpr ove d score t endency
di d not change bet ween the basel i ne to in-
t er vent i on phases, suggest i ng an effect of
maturation.
Nevert hel ess, t here are few st udi es that
assessed t he effect of oral t her apy for im-
pr ovi ng sucki ng f eedi ng disabilities. This
st udy present s the result of our experience
in fourt een infants wi t h a history of serious
illness t hat i nt erfered wi t h the nor mal de-
vel opment of sucking.
M E T H O D S A N D MAT E RI AL S
The s t udy was conduct ed at the Pediatrics
Hos pi t al of t he 21st Cent ury, Nat i onal
Medi cal Centre, Mexican Institute of Social
Security. Pat i ent s wer e seen at t he NI CU
and the Infants Depart ment bet ween March
to October 1997.
Vol. 66, No. 3, 1999 ASSESSMENT OF SENSORIAL ORAL sTIMULATION .IN INFANTS 32~
Cri t eri a for subj ect sel ect i on i ncl uded :
i nfant s wi t h mor e t han f our days of life;
over 35 weeks of postconceptional corrected
aged (gestational age at birth plus postnatal
age); wei ght > 2000 grams; medi cal l y stable
(tolerant to r oom air, vital si gns and bl ood
chemi st ry wi t hi n nor mal limits, and ability
to mai nt ai n nor mot her mi a) ; wi t hout oral,
nasal a n d / o r t r acheo- esophageal mal f or -
mations; not on sedat i ve medi cat i on; infec-
tion-free as referred by culture and a history
of illness requi ri ng medi cal care that inter-
fered wi t h t he nor mal devel opment of the
sucking pattern.
All pat i ent s ha d suckl i ng disabilities
showing absence of at least one of five oral
reflexes, pl us t wo or mor e abnor mal suck-
ing signs, or at least one abnormal sucking
sign plus the absence of t wo or mor e oral re-
flexes. The oral reflexes assessed were suck-
ing reflex, root i ng reflex; biting reflex, gag-
ging reflex and Babkin' s reflex.
The clinical sucki ng si gns i ncl uded (a)
failure to latch on the ni ppl e after st i mul us
of the lips, (b) f ai l ur e to gr asp t he ni ppl e
wi t hout seal i ng lips and maki ng choki ng
sounds, (c) del ay at t he begi nni ng of suck-
ing aft er 20 seconds of oral stimuli, (d) re-
luctance for f eedi ng after few sucks in less
than a mi nut e, (e) poor lip cont r ol wi t h
dr awi ng of mi l k from mout h, (f) coughi ng
dur i ng sucki ng wi t h or wi t hout vomi t i ng,
(g) excessive cryi ng wi t h or wi t hout t urni ng
of t he head, (h) cyanosi s dur i ng sucki ng
(none of the patients had central cyanosis),
(i) spi t t i ng of t he ni ppl es dur i ng t he feed-
ing, and (i) pr ol onged sucking, mani fest ed
by mor e t han 30 mi nut es for bottle-feeding
or more t han 45 mi nut es for nursing.
Pat i ent s who ful fi l l ed t he cri t eri a wer e
evaluated by one of t he medi cal therapists
to confi rm t he sucki ng disabilities and ex-
plore t he oral reflexes. The pat i ent ' s medi -
cal history, sex, gestational age, Apgar at 5
mi nut es, hi st ory of orot racheal intubation,
neonat al sepsis or infection(s), fast i ng
peri od(s), f eedi ng f or mul a( s) offered,
parenteral nutrition, orogastric tube feeding
and syr i nge ni ppl e f eedi ng wer e all re-
corded. In addi t i on, t he age of life, gesta-
tional corrected week, weight, height, diag-
noses, dur at i on of hospi t al st ay and
medications(s) at the beginning of t he Study
wer e consi der ed. Af t er i nf or med consent
f r om parent s t he i nfant s' wer e enrol l ed in
the sl-ud)~
The oral refl exes and f eedi ng sessi ons
were recorded on vi deot ape three times i.e.
before t he begi nni ng of t her apy (baseline
assessment ); aft er 48 hour s and; at 120
hour s (out come eval uat i on) aft er therapy.
The vi deo camera was positioned approxi-
mat el y 35 cm besi de t he baby at a 90 de-
grees angle. All vi deot apes were r ecor ded
by the same person, who was previously in-
f or med on angles and timing of recording.
The recordings were done at the same hour
of t he day dur i ng t he f eedi ng session, al-
ways after three hours of fasting, in supine
position, naked or in a diaper. The infants
were fed by their parents or nurses with the
mi l k or f or mul a i ndi cat ed by t hei r physi -
cians. Five mi nut es of vi deot ape recordi ng
was done at t wo intervals. Duri ng the first
mi nut e, t he t her api st st i mul at ed t he pa-
tient' s oral reflexes after which, the' patient
was fed. Total times for feeding were regis-
tered for assessing prol onged feedi ng peri-
ods, and vol umes of mi l k i ngest ed were
meas ur ed (bot t l efed i nfant by r esi dual of
initial vol ume less final volume, breast-fed
infant by difference of weight before and af-
ter nursing). The next vi deot ape recordings
wer e done at 48 and 120 hour s fol l owi ng
t he. same pattern. Each record was labelled
wi t h a code known onl y by one of the re-
322 M.E. RENDON-MACiAS ET AL Vol 66, No. 3, 1999
searcher (MERM).
Interventi on
The strategic activities per f or med by the
t herapi st usi ng hi s / he r fi ngert i ps wer e as
follows :
1. Infant' s head inclined (30 degrees) over
the cradle surface.
2. Root i ng reflex expl ored by light contact
over the lips and cheeks wi t h five fin-
gertips, one to t hree t i mes ( dependi ng
on the infant' s response).
3. A fine ci rcul ar mas s age on t he uppe r
lip and t he ant eri or gum side, for five
minutes.
The mas s age was cont i nued t owa r ds
the l at eral gum si de and i nsi de t he
cheeks for t hree minutes. The massage
was done mor e ext ensi vel y insid~ t he
cheeks (one centimeter cycles).
5. Af t er cheeks are mas s aged t act i l e
st i mul i was appl i ed to t he l ower lip
wi t h little pressure.
Finally, t he t her api st put pr es s ur e on
the sucking poi nt (located in the central
area of t he har d pal at e behi nd the up-
per gum).
7. For infants aged t wo mont hs or more, a
dr op of honey was pl aced on the suck-
ing point at the end of the therapy.
Bet ween feeding peri ods, a pacifier was
kept in their mouths.
.
.
.
Eval uati on
From an ethical st andpoi nt , the pat i ent s
s er ved as t hei r own cont rol s. In or der to
avoi d bi ases on interpretation, all vari abl es
wer e bl i ndl y assessed by t wo occupat i onal
t her apy physi ci ans ( MRMP and MMSR),
who wer e unawar e of the pat i ent ' s clinical
hi st ory and of t hesnt ri od the vi deot ape re-
cording t ook place (before or after interven-
tion). They wat ched the vi deot ape and by
cons ens us assessed t he vari abl es viz.
numbe r of oral ref l exes absent (five con-
sidered), number of cl i ni cal s ucki ng si gns
(nine consi der ed) and s uc ks / mi nut e , t he
latter regi st ered for the number of vertical
mandi bul ar movement s duri ng one mi nut e
for five mi nut es using a digital ret urn chro-
nomet er (Casio model HS, 10W, USA). Each
mandi bul ar movement was regi st ered us-
ing a manual count er ( Count i ng devi ces,
INC, Nort h Branford, CT 06471, USA).
Anal ysi s
Due to the small size of the popul at i on
wi t h abnor mal meas ur ement di st ri but i on,
medi ans, 25-75 quart i l es and ranks wer e
cal cul at ed. For det er mi ni ng the statistical
significant differences duri ng the study, the
medi ans on number of oral reflexes absent,
t he number of clinical sucki ng signs, mi l k
vol ume i ngest ed, and s ucks / mi nut es rate,
t he non- par amet r i cal Fr i edman t est was
used. For eval uat i ng changes in frequency
of clinical sucki ng si gn and vari abl es, a
non-paramet ri cal Q Cochran test was used.
All st at i st i cal anal ysi s was done usi ng
SPSS software.
RESULTS
A total of 29 pat i ent s fulfilled all inclusion
criteria at the begi nni ng of the study. Four-
t een f i ni shed t he s t udy and fi ft een wer e
el i mi nat ed (ei ght wer e di schar ged to an-
ot her hospi t al and di d not compl et e
therapy, six wer e orotracheallv rei nt ubat ed
dur i ng t herapy, and one i nfant di ed 48
hours after t herapy began due to causes not
associ at ed to any of the t herapeut i c proce-
dures).
Table 1 s hows the charact eri st i cs of the
Vol. 66, No. 3, 1999 A S S E S S M E N T O F S E N S O R I A L O R A L S T I M U L A T I O N IN I N F A N T S 323
i
O
i i
Cr~ ~ L
Z
P ~
P ~
o
i
I I
324 M.E. RENDON-MAdAS ET AL Vol. 66, No. 3, 1999
5
w
i 4
1 3
2
E~meUne 48 120
HOURS
Horizontal line = median, square = quartiles
25-75, vertical line = rank.
St a t i s t i c a l d i f f e r e n c e wi t h Friedman's
t e s t p = 0.0000
Suck, root, bite, gag and Babkin reflexes
Fig. 1. Effect of oral mot or and sensorial
t her apy in the presence of oral reflexes
(n = 14)
pa t i e nt s - ni ne mal es a n d f i ve f emal es. Al l
ha d smal l wei ght i ncreases and f eedi ng di f-
fi cul t i es. The y h a d r e q u i r e d an or ogas t r i c
f eedi ng t ube f or a l ong ~ n e aft er pr ol onged
fast i ng, s e c onda r y t o t he use of or ot r acheal
t ubes. Ei ght pa t i e nt s we r e p r e v i o u s l y f ed
us i ng t he s yr i ng ni ppl e t e c hni que wi t h
poor resul t s. Fi ve pat i ent s ( numbe r 3, 5, 9,
11 a n d 14) h a d b e e n f ed t h r o u g h s ucki ng
bef or e t hey be c a me ill. Al t hough, ma n y of
t he m ha d t o be gi ven di f f er ent t ypes of for-
mul ae, onl y t he one t hey we r e t aki ng at t he
begi nni ng of t he s t udy was r egi st er ed. Fi ve
pa t i e nt s (3, 4, 7, 9, 11 pat i ent s ) we r e
br east f ed. Twel ve pat i ent s wer e cons i der ed
t o have abnor mal Sucki ng because t hey had
mo r e t ha n t wo r ef l exes absent , pl us mor e
t ha n t wo cl i ni cal s uc ki ng si gns. In t wo
ot her pat i ent s, one ( pat i ent n u mb e r 4) ha d
six or al r ef l exes absent wi t h onl y one clini-
cal s uc ki ng si gn ( d r a wi n g mi l k) ; t he l ast
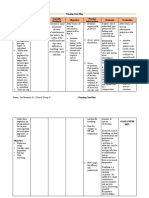
T^BLE 2. Effect of Oral Motor and Sensorial Therapy in the Clinical Suckling Signs
Clinical sign Baseline 48 h 120 h *p
1. Failure to latch on the nipple after lip stimulus 6 3 1 0.09
2. Failure to grasp the nipple without sealing lips 6 1 0 0.005
and making choking sounds
3. Delay at the beginning of sucking after 20 10 5 2 0.0022
seconds of oral stimuli
4. Easily satisfied after few sucks for less than 13 6 3 0.0004
a minute
5. Poor lip control with drawing of milk 12 3 0 0.0001
from mout h
6. Coughing duri ng the suckling with or 4 2 0 0.09
wi t hout vomiting
7. Excessive crying with turning of head or 12 9 10 0.31
crying a lot
8. Cyanosis during suckling 6 7 0 0.0084
9. Spitting the nipples during the feeding 8 8 12 0.51
10. Prolonged suckling 11 9 4 "0.0038
. *Q Cochran test
'Col. 66, No. 3, 1999 ASSESSMENT OF SENSORIAL ORAL STIMULATION IN INFANTS 325
one had ei ght clinical sucki ng si gns and
absence of one sucking reflex.
Fig. 1 s hows t he effect of oral sensori al
t herapy in the recovery of reflexes. At base-
line, the medi an number of normal oral re-
flexes was t wo (range 0 to 4) and at end of
the s t udy all the pat i ent s had recovered all
of reflexes 120 hour s later (Fri edman' s test
X 2 22, p = 0.0000). Cl i ni cal sucki ng si gns
decr eased from a medi an basel i ne amount
of six to one at t he end of . t he s t udy
(Friedman test X 2 24.14, p = 0.0000).
When anal yzi ng the results obtained, de-
monst rabl e i mpr ovement was observed (ta-
ble 2). The maj or effect of t her apy was seen
in the ability of the infants to form a mout h
seal, t hat al l owed for mai nt ai ni ng continu-
ous sucki ng (signs 2, 4 and 5). In some pa-
tients, once t he sucki ng was coor di nat ed,
no choki ng, cyanosi s or coughi ng event s
(signs 2, 6 and 8) occurred dur i ng feeding.
Pat i ent 3 wh o di d not have cyanosi s at
basel i ne pr es ent ed wi t h cyanot i c event at
48 hour s of t her apy associ at ed wi t h nasal
obst r uct i on caused by the mot her ' s breast,
whi l e changi ng f r om bot t l e f eedi ng to
breast -feedi ng. The t i me at whi ch sucki ng
began and sucki ng t i me (si gns 3 and 10)
al so i mpr oved. Two si gns (7 and 9) wer e
not affect ed by t her apy : excessi ve cryi ng
and frequent spitting, present in majority of
the infants.
An increase in relation to the efficacy of
sucking, assessed by the vol ume of ingested
mi l k or f or mul a, was s hown ( Fr ei dman' s
test X 2 18.107, p = 0.0001). Two patients re-
f used the f eed bef or e t her apy and the rest
consumed a medi an vol ume of 10 milliliters
(range : 0 to 40 ml). Aft er 48 hours, the me-
di an vol ume of mi l k i ngest ed i ncreased to
25 milliliters (range 10 to 60 ml) and at 120
hours, all pat i ent s wer e i ngest i ng over 20
ml (fig. 3). The sucking rate for the group in-
8
! 6
i 2
Basel i ne 48 120
HOURS
Hor i z ont al l i ne = medi an, squar e = quar t i l es
25-75, vertical line = rank.
Fr i edman' s test 24.14, p = 0.0000
Fig. 2. Effect of oral motor and sensorial
therapy in the number of clinical suck-
ing signs (14 patients)
70
60
50
40
30
20
10
0
MILLILITERS
Basel i ne 48 120
HOURS
Hori zont al line = medi an, squar e = quart i l es
25-75, vertical line = rank.
Fr i edman' s test 24.14, p = 0.0001
Fig. 3. Effect of oral motor and sensorial
therapy in the milk or formula ingested
(n = 14)
cr eased in a st at i st i cal l y si gni fi cant f or m
( Fr i edman X 2 10.85, p = 0.0044). The fre-
quency of sucki ng per mi nut e rose from a
baseline medi an of 22 to 28.5 (rank 10 to 35)
326 M.E. RENDON-MACIAS ET AL Vol. 66, No. 3, 1999
5o!
40
30
|
20
10
I
I
o
Baseline 48 120
HOURS
Horizontal line = median, square = quartiles
25-75, vertical line = rank.
Friedman's test X2 = 10.85, p = 0.0044
Fig. 4. Effect of the oral motor and sensorial
therapy on the sucking rate (sucks/
minute)
at 48 hours, and finally to 45 (rank 30-48),
at 120 hours after t herapy (fig. 4).
DI SCUSSI ON
Nut r i t i onal sucki ng pl ays a maj or rol e in
the mat urat i on of several physiological sys-
t ems TM and neur obehavi our al devel op-
ment n.17. Nevert hel ess, preval ence of suck-
ing disabilities has increased, as wel l as the
i mpr oved s ur vi val of ne wbor ns at t he
NI CUs. These compl i cat i ons oft en resul t
from ext reme i mmat uri t y that often require
f r equent or l ong- t er m i nt ubat i on, f eedi ng
t hr ough cat het ers and moder at e to severe
br onchopul monar y dyspl asi a, as was seen
in the infant cohort of this study.
Rehabi l i t at i on of sucki ng in pr et er m in-
fants may be achi eved gradual l y and spon-
t aneousl y at 34 weeks of gest at i onal cor-
rect ed age ~.7, but this t ransi t i on from non-
oral to oral feedi ng is mor e difficult when
pat i ent s have dysf unct i onal sucki ng t wo
weeks after birth and after 37 weeks of ges-
tational correct ed age 24. Pat i ent s i ncl uded
in this s t udy had t hese di ffi cul t i es, and
therefore oral t her apy coul d be assessed in
t wo ways. The first was based on the clini-
cal abnormalities of sucking' and the second
was in the i mpr ovement in sucki ng effi-
ciency.
In rel at i on t o clinical aspect s, t he ab-
sence of oral reflexes denot es some degree
of neurological damage. The i mpai rment of
these protective mechani sms that keep air-
ways free of foreign material or help to ex-
pel them, make t hem f undament al for oral
feeding. The application of positive oral tac-
tile st i mul i wi t h t he r emoval of har mf ul
stimuli, i nduced t he r ecover y of oral re-
flexes in the infants of our study. In general,
the r ecover y of reflexes occurred in a very
short peri od of time (48 hours), suggest i ng
that adequat e stimuli are i mport ant factors.
It may also be that the repetitive stimulus of
sensorial oral receptors may help the devel-
opment of reflex pat hways 2.
Cert ai n clinical scales have been con-
st r uct ed for assessi ng clinical sucki ng ab-
normalities and their recovery. Nonetheless,
t he neonat al oral mot or assessment scale
(NOMAS), a clinical assessment tool t hat
descri bes jaw and t ongue funct i on dur i ng
nut ri t i ve sucki ng, has been the most reli-
abl e 18. NOMAS eval uat i on r equi r es close
obser vat i on of the neonat e' s sucki ng pat-
t ern and a cert i fi ed exami ner in
neur odevet opment . Clinical si gns associ-
at ed wi t h sucki ng difficulties wer e eval u-
at ed usi ng vi deot ape records for assuri ng
the consistency on the interpretation of the
i nf or mat i on and mai nt ai ni ng the s t udy' s
blindness; partially using the met hodol ogy
empl oyed by other investigators~"L
In this study, oral t herapy i mpr oved the
abnormal suckling pattern (with coughing,
VOI. 66, No. 3, 1 9 9 9 ASSESSMENT OF SENSORIAL ORAL STIMULATION IN INFANTS 327
cyanosis, choking, etc.) to a normal pattern.
The pri nci pal rehabi l i t at ory effect was seen
in the capaci t y of lip sealing and the possi-
ble r eor gani zat i on of t he sucki ng muscles.
Two signs wer e not modi f i ed after therapy,
cryi ng and ni ppl e spi t t i ng dur i ng feeding.
Cr yi ng dur i ng f eedi ng ma y be associ at ed
wi t h di scomfort s due to internal a n d / o r ex-
ternal factors. The signs ment i oned earlier
are rel at ed to def ence mechani sm to avoi d
choki ng event s dur i ng whi ch t he i nfant
takes a deep breath. Our patients cont i nued
wi t h this be ha vi our i nde pe nde nt of the
therapy, but di d not show cyanosi s or chok-
ing signs. It is pos s i bl e t hat this cr yi ng
coul d be rel at ed to frequent irritable behav-
i our obs er ved in chi l dren hospi t al i zed for
long peri ods of time secondar y to repetitive
harmful external stimuli : noise, light, venal
punct ures, oral or nasal tubes, etc 2~
Ni ppl e spi t t i ng is anot her def ens i ve
mechani s m t o avoi d choki ng 1~ and was
seen in ei ght pat i ent s bef or e begi nni ng
t herapy; later di sappear i ng in four, and at a
r educed f r equency in t he r emai ni ng four.
The r eason wh y this was seen in cases
wi t hout cyanosi s or coughi ng, ma y have
been r el at ed t o bei ng full and to a r api d
endi ng of nursing.
Since t he s econd goal of t he sensori al
st i mul i was to modi f y the sucki ng feedi ng
efficacy, or, in ot her wor ds , to cons ume a
gr eat er vol ume of mi l k wi t hout any
significant effort, bot h the i ngest ed vol ume
of mi l k and sucki ng rat e wer e regi st ered.
Af t er t her apy, t he medi an of i ngest ed
vol ume by sucking doubl ed for all patients.
The opt i mal vol ume r equi r ed for i nfant s
wei ghi ng appr oxi mat el y 3000 g, ill and
mal nour i s hed, was hi gher t han t hat
i ngest ed by t he pat i ent s of this st udy, a
vol ume i nt ended t o s uppl y mi ni mal
nut r i t i onal requi rement s2L Never t hel ess,
oral sucki ng f eedi ng is benefi ci al for the
devel opment of infants 22.
The sucki ng rat e is this gr oup al so in-
creased to a degree enough for maintaining
cont i nuous sucki ng 23.24 and r educed feed-
ing time. Ot her st udi es have demonst r at ed
i ncreases in t he amount of mi l k i ngest ed
and sucki ng rat e by onl y modi f yi ng the
t ype a n d / o r hole size of the ni ppl es 25'2~'. We
wer e unabl e to assess these factors because
of the great vari et y in commerci al ni ppl es
avai l abl e and because fi ve babi es wer e
breastfed. To avoi d possi bl e biases in inter-
pret i ng sucki ng efficacy for t hese ki nds of
st udi es, cont rol of ni ppl e t ypes shoul d be
included.
A fundament al aspect for recovering nor-
mal sucki ng f eedi ng is t he el i mi nat i on of
factors that interfere wi t h normal oral feed-
ing. These conditions were requi red for pa-
tients i ncl uded in this study. Stable condi-
tions per se coul d be beneficial for recover-
ing normal sucking; however , this takes at
least t wo weeks 2,6 and depends on the pa-
t i ent ' s mat ur i t y 6. Our pat i ent s achi eved
their nor mal oral mot or skills in a short er
time, and r ehabi l i t at or y t her apy was per-
formed when they were 37 or more weeks of
gest at i onal correct ed age. Ot her quest i ons
r emai n to be ans wer ed, such as i ncl usi on
criteria, the expendi t ure of time on stimula-
tion, criteria to change or mai nt ai n a
r ehabi l i t at or y pr ogr amme, t her apy inten-
sity, pr edi ct i ve fact ors r egar di ng t her apy
failure and effects of this t herapy for recov-
er y of nor mal f unct i on of di f f er ent organ
systems.
To date, this st udy al l ows us to conclude
t hat sensori al oral s t i mul at or y t her apy
i nduces t he r ecover y of oral pr ot ect i ve
refl exes, i mpr ove me nt of s ympt oms
associated wi t h suction and a more efficient
suction in infants wi t h sucking disabilities.
328 M.E. RENDON-MAC~AS ET AL Voi. 66, No. 3, 1999
Acknowledgement
We would like to thank Dr. Marlene Llopiz for
reviewing the manuscript.
REFERENCES
1. Br aun MA, Pal mer MM. A pi l ot s t udy of
or al mo t o r dys f unc t i on i n "at r i sk" in-
fants. Phys Occup Ther Ped 1985/ 1986; 5 :
13-25.
2. Li pman E, Tr ykowski LE, and Ki rkpat ri ck
BV. Nut r i t i ve s uckl i ng i n hi gh- r i s k
neonat es aft er per i or al st i mul at i on. Phys
Ther 1980; 60 : 299-302.
3. Case- Smi t h J. An ef f i cacy s t udy of occu-
pat i onal t her apy wi t h hi gh-ri sk neonat es.
Am J Occup Ther 1987; 42 : 499-505.
4. Barker S, Jarvi s A, Br eyer M. The t ransi -
t i on f r om non- or al to oral feedi ng in chil-
dren. Am J Occup Ther 1991; 45 : 402-8.
5. Ha nl on MB, Trip JH, Ellis RE, Fl ack FC,
Selley WG and Shoesmi t h HJ. Degl ut i t i on
a pnoe a as i ndi cat or of ma t ur a t i on of
suckl e f eedi ng in bot t l e f ed pr e t e r m in-
fants. Dev Med Child Neurol 1997; 39 : 534-
42.
6. Wolff PH. The serial or gani zat i on of suck-
l i ng in t he y o u n g i nfant . Pediatrics 1968;
42 : 943-53.
7. Gr y b o s k y JD. Suck and s wal l ow i n t he
pr emat ur e infant. Pediatrics 1969; 43 : 96-
102.
8. Cowet t RM, Lipsitt LP, Volr B and Oh W.
Aber r at i ons in suckl i ng behavi our of l ow
bi rt h wei ght infant. Dev Med Child Neurol
1978; 20 : 701-9.
9. St evenson RD and Al l ai re JH. The devel -
o p me n t of nor ma l f eedi ng and s wal l ow-
ing. Ped Clin NAmer 1991; 38 : 1439-53.
10. I l l i ngwor t h RS. Sucki ng and s wa l l owi ng
difficulties in i nfancy : di agnost i c pr obl em
Of dys pha gi a . Arch Dis Child 1969; 44 :
655-709.
11. Coul t er M and Coul t er S. Suckl i ng di sor-
der s in i nf ant wi t h neur ol ogi cal disabili-
ties. Clin Perinatol 1989; 1 : 111-33.
12. Vogel S. Or al mot or and f eedi ng pr ob-
l ems in t he t ube fed i nf ant : Suggest ed
t r eat ment st rat egi es for t he occupat i onal
therapist. Occup Ther Health Care 1986; 3 :
63-79.
13. Bl aymor e JA, Fer gus on A, Cho Ch, Oh
W, and Vohr BR. The oral mot or devel op-
ment of l ow we i ght i nf ant s wh o under -
we n t or ot r acheal i nt ubat i on dur i ng t he
neonat al peri od. AJDC 1993; 147 : 858-62.
14. Ber nbaum JC, Pereira GF, Watkins JB and
Peckham GJ. Nonnut r i t i ve s ucki ng dur -
i ng gavage feedi ng enhances gr owt h and
ma t ur a t i on in pr e ma t ur e infants.
Pediatrics 1983; 71 : 4-5.
15. Sehgal SH, Pr akas h O, Gupt a A, Mohan
M and Ana nd NK. Eval uat i on of benefi -
cial effects of nonnut r i t i ve sucki ng in pre-
t erm infants. Indian Ped 1990; 27 : 264-6.
16. Daniels H, Devl i eger H, Mi nami T, Egger-
mont E and Casaer P. I nf ant f eedi ng and
car di or es pi r at or y mat ur at i on. Neuropedi-
atrics 1990; 21 : 9-10.
17. Smot her man WP and Robi nson SR. Milk
as t he pr oxi mal mechani s m for behavi o-
ral change in the newbor n. Acta Paediatr
1994; 397 : 64-70.
18. Mayer - Pal mer M, Cr awl ey K and Blanco
IA. Neonat al or a l - mot or as s es s ment
scale : a reliability study, l Perinatol 1993;
13 : 28-35.
19. Rams ay M, and Gisel EK. Neonat al suck-
l i ng and mat er nal f eedi ng practices. Dev
Med Child Neurol 1996; 38 : 34-47.
20. Glass RP and Wol f LS. A gl obal per spec-
tive on f eedi ng assessment in the neona-
tal i nt ensi ve car e unit. Am ] Occup Ther
1994; 48 : 514-26.
21. Fomon SJ and Bel EF. Energy In : Fomon,
SJ (ed). Nutrition of Normal Infant ISBN,
Mosby. 1995; 102-19.
22. Blass EM. Behavi oural and physi ol ogi cal
cons equences of suckl i ng in rat and hu-
man ne wbor ns . . ~c t a Paediatr 1994; 397
(suppl) : 71-6.
23. Jair L, Sivieri E, Abbasi S and Bhut ani V.
Ener get i c and mechani cs of nut r i t i ve
sucki ng in the pr et er m and term neonate.
J Pediatr 1987; 111 : 894-8.
Vol. 66, No. 3, 1 9 9 9 ASSESSMENT OF SENSORIAL ORAL STIMULATION IN INFANTS 329
24. Mat hew OP. Science of bot t l e feeding. J
Pediatr 1991; 119 : 511-9.
25. Mat hew OP. Det er mi nant s of mi l k flow
t hr ough ni ppl e units. AJDC 1990; 144 :
222-4.
26. Fadavi SH, Punwani IC, Jain L and
Vi dyasagar D. Mechanics and energetics
of nut ri t i ve suckling. A functional com-
pari son of commer ci al l y avai l abl e nip-
pies. J Pediatr 1997; 130 : 740-5.
S HORTER OTI TI S MEDI A TREATMENT
Gi vi ng chi l dren a short -act i ng ant i bi ot i c for fi ve days is an effect i ve t reat ment for
uncompl i cat ed acute otitis medi a (AOM), accordi ng to a met a-anal ysi s of 32 trials. Seven
reviewers independently assessed methodological quality, and studies were included i f:
(a) subjects were between ages 4 weeks and 18 years
(b) a clinical diagnosis of AOM was made, and antimicrobial therapy was not in progress at
di agnosi s;
(c) subjects were assigned randomly to antibiotic treatment of fewer than seven days;
(d) clinical resolution of AOM was assessed.
Trials were grouped by antibiotic used in the short course : (1) short-acting oral antibiotics,
(2) i.m. cefiriaxone sodium and (3) oral azithromycin.
Researchers were interested primarily in whether treatment failed, which included AOM
signs or sympt oms not improving or subjects experiencing relapses or reinfections during 31
days following therapy initiation.
Resul t s i ndi cat ed that a reduct i on in t reat ment from 10 to 5 days of short -act i ng
antibiotics may increase slightly the risk of a child experiencing signs or sympt oms or relapse
or reinfection when the evaluation was done at 8 to 19 days after therapy initiation. However,
this difference no longer was evident at one month following treatment. The risk difference at
30 days following treatment dropped to 2.3 percent; suggests 44 children need to be treated
with a longer course of antibiotics to prevent a single failure following shorter treatment.
Researchers added that a shortened course of short-acting antibiotics has the potential to
save money, improve compliance and decrease antibiotic resistance.
Abst ract ed f r om: Journal Ameri can Medi cal Association, 1998; 2 79 : 1736-42
Anda mungkin juga menyukai
- USMLE 1 Hematology BookDokumen368 halamanUSMLE 1 Hematology BookPRINCEBelum ada peringkat
- Case Study Pleural EffusionDokumen32 halamanCase Study Pleural Effusionwguino100% (1)
- Neonatal Oral MotorDokumen5 halamanNeonatal Oral MotorYessenia DiazBelum ada peringkat
- Stress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.Dokumen94 halamanStress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.sorbariBelum ada peringkat
- Raw Milk FactsDokumen9 halamanRaw Milk FactsRon Loewenstein100% (2)
- Paediatric Dysphagia: How I Inform My Decisions (1) - Penetrating QuestionsDokumen3 halamanPaediatric Dysphagia: How I Inform My Decisions (1) - Penetrating QuestionsSpeech & Language Therapy in PracticeBelum ada peringkat
- Cacophony BurnTheGroundDokumen32 halamanCacophony BurnTheGroundLeo HurtadoBelum ada peringkat
- Essie Hoiball and T.C. Fry - I Live On Fruit (1981)Dokumen40 halamanEssie Hoiball and T.C. Fry - I Live On Fruit (1981)Charles100% (11)
- Varicose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasDokumen8 halamanVaricose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud Ellias100% (2)
- EnuresisDokumen11 halamanEnuresisadrianaBelum ada peringkat
- Growth and DevelopmentDokumen64 halamanGrowth and DevelopmentRahul Dhaker100% (1)
- Yeast Connection (Candida Albicans)Dokumen4 halamanYeast Connection (Candida Albicans)ngranadosg100% (1)
- Science: Modified Strategic Intervention MaterialsDokumen28 halamanScience: Modified Strategic Intervention Materialskotarobrother23Belum ada peringkat
- Pereneal CareDokumen2 halamanPereneal CareindumathiBelum ada peringkat
- Theory ApplicationDokumen38 halamanTheory ApplicationAnusha VergheseBelum ada peringkat
- Natural Science 6 PDFDokumen90 halamanNatural Science 6 PDFBeatriz Garcia67% (3)
- Erasmus 2009, HypersalivationDokumen6 halamanErasmus 2009, HypersalivationSilvanilla PiliBelum ada peringkat
- Oropharyngealdysphagia Inchildren: Mechanism, Source, and ManagementDokumen30 halamanOropharyngealdysphagia Inchildren: Mechanism, Source, and ManagementArif oktavianBelum ada peringkat
- 12 - Media Exposure and Oral Health Outcomes Among AdultsDokumen11 halaman12 - Media Exposure and Oral Health Outcomes Among AdultskochikaghochiBelum ada peringkat
- Association of Breastfeeding Duration, NonnutritiveDokumen5 halamanAssociation of Breastfeeding Duration, NonnutritiveIrma NovitasariBelum ada peringkat
- Ajcn 121061Dokumen9 halamanAjcn 121061MARION JOCELIN MENABelum ada peringkat
- Immunoglobulin A (Iga) NephropathyDokumen25 halamanImmunoglobulin A (Iga) NephropathyErika Joy ImperioBelum ada peringkat
- Breastfeeding, Bottle Feeding, and Non-Nutritive SuckingDokumen3 halamanBreastfeeding, Bottle Feeding, and Non-Nutritive SuckingAulia HardiantiBelum ada peringkat
- Evaluación de La Deglución Con NasofibroscopíaDokumen7 halamanEvaluación de La Deglución Con NasofibroscopíaLoreto Opazo RojasBelum ada peringkat
- Pre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature ArticleDokumen5 halamanPre-Hospital Management of Febrile Seizures in Children Seen at The University College Hospital, Ibadan, Nigeria Feature Articlechaz5727xBelum ada peringkat
- Use of Elastic Bandage Associated With Speech Therapy in The Control of Sialorrhea (Hypersalivation)Dokumen9 halamanUse of Elastic Bandage Associated With Speech Therapy in The Control of Sialorrhea (Hypersalivation)MayzaBelum ada peringkat
- Gingival Disease in Adolescents Related To Puberal Stages and Nutritional StatusDokumen6 halamanGingival Disease in Adolescents Related To Puberal Stages and Nutritional StatusRosa WeilerBelum ada peringkat
- Effects of Gustatory Stimulation On The Behavioral States of Premature NewbornsDokumen7 halamanEffects of Gustatory Stimulation On The Behavioral States of Premature NewbornsLuis RamirezBelum ada peringkat
- Tugas Akhir Blok 11 "Otitis Media": OlehDokumen19 halamanTugas Akhir Blok 11 "Otitis Media": OlehSartika NapitupuluBelum ada peringkat
- Original Article Oral Dryness Among Japanese Youth: Development of A Japanese Questionnaire On Oral Dryness and The Impact of Daily Life On ItDokumen6 halamanOriginal Article Oral Dryness Among Japanese Youth: Development of A Japanese Questionnaire On Oral Dryness and The Impact of Daily Life On ItDanis Diba Sabatillah YaminBelum ada peringkat
- Ileal-Lymphoid-Nodular Hyperplasia, Non-Specific Colitis, and Pervasive Developmental Disorder in ChildrenDokumen11 halamanIleal-Lymphoid-Nodular Hyperplasia, Non-Specific Colitis, and Pervasive Developmental Disorder in ChildrenEmmanuelLeidiBelum ada peringkat
- TB AnakDokumen6 halamanTB AnakHerlin Ajeng NurrahmaBelum ada peringkat
- Routine Amoxicillin For Uncomplicated Severe Acute Malnutrition in ChildrenDokumen10 halamanRoutine Amoxicillin For Uncomplicated Severe Acute Malnutrition in ChildrenMc'onethree BrownBelum ada peringkat
- Early Childhood Caries and Weight Status: A Systematic Review and Meta-AnalysisDokumen11 halamanEarly Childhood Caries and Weight Status: A Systematic Review and Meta-AnalysisRawan AlahehabBelum ada peringkat
- Encopresis and EnuresisDokumen10 halamanEncopresis and EnuresisRoci ArceBelum ada peringkat
- Pediatric Dentistry Aom Pacifier 2001Dokumen5 halamanPediatric Dentistry Aom Pacifier 2001Kobayashi MaruBelum ada peringkat
- Demand For Speech Therapy Intervention in Neonatal Unit of A Teaching Hospital PDFDokumen12 halamanDemand For Speech Therapy Intervention in Neonatal Unit of A Teaching Hospital PDFTatiana Amado GarcíaBelum ada peringkat
- Copia de admin,+587-Article+Text-2097-1-11-20201110Dokumen13 halamanCopia de admin,+587-Article+Text-2097-1-11-20201110aner cristobal alonso alonsoBelum ada peringkat
- Beneficios de Prologar La LM Entre 30 59 Meses para El Correcto Desarrollo OrofacialDokumen6 halamanBeneficios de Prologar La LM Entre 30 59 Meses para El Correcto Desarrollo OrofacialCésar Augusto Gamarra SantamariaBelum ada peringkat
- Clinical-Epidemiological Considerations Regarding Primary Peptic Ulcer in Children - 5 Years Retrospective StudyDokumen10 halamanClinical-Epidemiological Considerations Regarding Primary Peptic Ulcer in Children - 5 Years Retrospective StudySilvia PoamăneagrăBelum ada peringkat
- ChupeteDokumen5 halamanChupeteEve Sepúlveda FerradaBelum ada peringkat
- Constipation: Beyond The Old ParadigmsDokumen18 halamanConstipation: Beyond The Old ParadigmsJhonatan Efraín López CarbajalBelum ada peringkat
- JurnalDokumen9 halamanJurnalNoraine Zainal AbidinBelum ada peringkat
- Cuidado É FundamentalDokumen7 halamanCuidado É FundamentalAlessandra FonsecaBelum ada peringkat
- Behavioral Analysis of Children's Response To Induction of AnesthesiaDokumen7 halamanBehavioral Analysis of Children's Response To Induction of AnesthesiaSuci MaghfirahBelum ada peringkat
- Efficacy of A New Hypotonic Oral Rehydration Solution Containing Zinc and Prebiotics in The Treatment of Childhood Acute Diarrhea: A Randomized Controlled TrialDokumen6 halamanEfficacy of A New Hypotonic Oral Rehydration Solution Containing Zinc and Prebiotics in The Treatment of Childhood Acute Diarrhea: A Randomized Controlled TrialOlpinBelum ada peringkat
- Maternal Risk Factors Associated With The Development of Cleft Lip and Cleft Palate in Mexico: A Case-Control StudyDokumen7 halamanMaternal Risk Factors Associated With The Development of Cleft Lip and Cleft Palate in Mexico: A Case-Control StudyFauzi NoviaBelum ada peringkat
- Anomalias Dento Maxilares y Factores Asociados en Ninos Con Paralisis CerebralDokumen9 halamanAnomalias Dento Maxilares y Factores Asociados en Ninos Con Paralisis CerebralyoselinfrancoBelum ada peringkat
- Ficha Bibliografica de Parasitosis IntestinalDokumen44 halamanFicha Bibliografica de Parasitosis Intestinalconsultorio la cardeneraBelum ada peringkat
- Maternal Malnutrition, Environmental Exposure During Pregnancy and The Risk of Non-Syndromic Orofacial CleftsDokumen6 halamanMaternal Malnutrition, Environmental Exposure During Pregnancy and The Risk of Non-Syndromic Orofacial CleftsFlórian JeffersonBelum ada peringkat
- ETO NA TALAGA - Tapos Na Ang Lahat !!!Dokumen32 halamanETO NA TALAGA - Tapos Na Ang Lahat !!!Keenen Engel Bonifacio Pascua100% (1)
- AfrJPaediatrSurg5265-5010858 012330 PDFDokumen6 halamanAfrJPaediatrSurg5265-5010858 012330 PDFSandi ApriadiBelum ada peringkat
- A Proposal For A'new Method of Evaluation - of The Newborn Infant PDFDokumen8 halamanA Proposal For A'new Method of Evaluation - of The Newborn Infant PDFcbac1990Belum ada peringkat
- Anak KonstipasiDokumen6 halamanAnak KonstipasiAzwar ArigaBelum ada peringkat
- Report On OME - EditedDokumen8 halamanReport On OME - Editedoreo 925Belum ada peringkat
- Nej M 200104193441601Dokumen9 halamanNej M 200104193441601Tri Rahma Yani YawatiBelum ada peringkat
- JOHOE - Volume 5 - Issue 1 - Pages 13-16Dokumen4 halamanJOHOE - Volume 5 - Issue 1 - Pages 13-16Tô ThuỷBelum ada peringkat
- Rumination Syndrome in Children and Adolescents: Diagnosis, Treatment, and PrognosisDokumen7 halamanRumination Syndrome in Children and Adolescents: Diagnosis, Treatment, and PrognosisryselBelum ada peringkat
- Lyceum of The Philippines UniversityBatangas College of NursingDokumen83 halamanLyceum of The Philippines UniversityBatangas College of NursingmarkzamBelum ada peringkat
- Anomalías Dento Maxilares y Factores Asociados en Niños Con Parálos Cerebral PDFDokumen9 halamanAnomalías Dento Maxilares y Factores Asociados en Niños Con Parálos Cerebral PDFAnonymous yTnAACeGBelum ada peringkat
- Little 2019 THPQ SP2 Cites Ver PDFDokumen5 halamanLittle 2019 THPQ SP2 Cites Ver PDFcLAUDIABelum ada peringkat
- Intervencion Temprana SuccionDokumen13 halamanIntervencion Temprana Succionjulianamd87Belum ada peringkat
- Neonatal JaundiceDokumen5 halamanNeonatal JaundiceKartik KumarasamyBelum ada peringkat
- Vasconcelos 2017Dokumen7 halamanVasconcelos 2017Putri Atthariq IlmiBelum ada peringkat
- PrognosisDokumen7 halamanPrognosispenyimpanankoas8Belum ada peringkat
- Pacifier-Sucking Habit Duration and Frequency On Occlusal and Myofunctional Alterations in Preschool ChildrenDokumen7 halamanPacifier-Sucking Habit Duration and Frequency On Occlusal and Myofunctional Alterations in Preschool ChildrenEva Sala RenauBelum ada peringkat
- Association Between Oral Contraceptive Use and Interleukin-6 Levels and Periodontal HealthDokumen8 halamanAssociation Between Oral Contraceptive Use and Interleukin-6 Levels and Periodontal Healthmy srBelum ada peringkat
- Habib y 1995Dokumen4 halamanHabib y 1995adeBelum ada peringkat
- Consideraciones Clin en Pediatricos en La Ev Clinica VS Evaluacion Insturmental de La DeglucionDokumen8 halamanConsideraciones Clin en Pediatricos en La Ev Clinica VS Evaluacion Insturmental de La DeglucionAngélica GarcíaBelum ada peringkat
- Application of HBMDokumen15 halamanApplication of HBMSashwat TanayBelum ada peringkat
- Pediatric Dysphagia: Challenges and ControversiesDari EverandPediatric Dysphagia: Challenges and ControversiesJulina OngkasuwanBelum ada peringkat
- Nursing Care PlanDokumen13 halamanNursing Care PlanJan DamesBelum ada peringkat
- People vs. BonoanDokumen6 halamanPeople vs. BonoannellafayericoBelum ada peringkat
- New Renalcare CatalogDokumen16 halamanNew Renalcare CatalogKaushik Hanskumar ShahBelum ada peringkat
- Colic in Horse: A Presentation OnDokumen32 halamanColic in Horse: A Presentation OnMuhammad Saif KhanBelum ada peringkat
- Multiple Dengue Virus Types Harbored by Individual MosquitoesDokumen7 halamanMultiple Dengue Virus Types Harbored by Individual MosquitoesYL Slalu BahagieaBelum ada peringkat
- Hallie Berger Resume 11-2Dokumen2 halamanHallie Berger Resume 11-2api-281008760Belum ada peringkat
- Splice PDFDokumen5 halamanSplice PDFpedroBelum ada peringkat
- Sub - PG Dissertation Title Registration With KNR UHS, WarangalDokumen7 halamanSub - PG Dissertation Title Registration With KNR UHS, WarangalPradeep VunnamBelum ada peringkat
- Scid 5 CVDokumen26 halamanScid 5 CVZubair Mahmood KamalBelum ada peringkat
- Acute Cardiac EKG Interpretation - Basics Part 1 - ScriptDokumen2 halamanAcute Cardiac EKG Interpretation - Basics Part 1 - ScriptDarby GravinoBelum ada peringkat
- XII Chemistry CH#11 Notes (Sir Nasim Zulfiqar)Dokumen9 halamanXII Chemistry CH#11 Notes (Sir Nasim Zulfiqar)salmanBelum ada peringkat
- Ob Osce.04 CTG ReadingDokumen6 halamanOb Osce.04 CTG ReadingDasha VeeBelum ada peringkat
- Pros and Cons EuthanasiaDokumen3 halamanPros and Cons EuthanasiaMirantika Audina100% (1)
- New Microsoft Word DocumentDokumen3 halamanNew Microsoft Word Documentnew one10% (1)
- Mci Mbbs SyllabusDokumen110 halamanMci Mbbs Syllabusmetabolicmedicine100% (1)
- UntitledDokumen44 halamanUntitled제올Belum ada peringkat
- Endodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentDokumen28 halamanEndodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentardeleanoanaBelum ada peringkat
- Burdens of Family Caregiving at The End of LifeDokumen6 halamanBurdens of Family Caregiving at The End of LifeNurul ShahirahBelum ada peringkat
- Silkworm in NepalDokumen11 halamanSilkworm in NepalRitesh Raj Shrestha50% (4)