DM Hiperestesia 4 PDF
Diunggah oleh
Syahrul Hamidi Nasution0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
101 tayangan6 halamanpdf
Judul Asli
dm hiperestesia 4.pdf
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Inipdf
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
101 tayangan6 halamanDM Hiperestesia 4 PDF
Diunggah oleh
Syahrul Hamidi Nasutionpdf
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 6
http://imr.sagepub.
com/
Research
Journal of International Medical
http://imr.sagepub.com/content/32/5/558
The online version of this article can be found at:
DOI: 10.1177/147323000403200515
2004 32: 558 Journal of International Medical Research
S Takayama, Y Takahashi, M Osawa and Y Iwamoto
Control in Type 2 Diabetes
Acute Painful Neuropathy Restricted to the Abdomen following Rapid Glycaemic
Published by:
http://www.sagepublications.com
can be found at: Journal of International Medical Research Additional services and information for
http://imr.sagepub.com/cgi/alerts Email Alerts:
http://imr.sagepub.com/subscriptions Subscriptions:
http://www.sagepub.com/journalsReprints.nav Reprints:
http://www.sagepub.com/journalsPermissions.nav Permissions:
What is This?
- Oct 1, 2004 Version of Record >>
by guest on June 26, 2014 imr.sagepub.com Downloaded from by guest on June 26, 2014 imr.sagepub.com Downloaded from
The Journal of International Medical Research
2004; 32: 558 562
558
Acute Painful Neuropathy Restricted to
the Abdomen Following Rapid Glycaemic
Control in Type 2 Diabetes
S TAKAYAMA
1
, Y TAKAHASHI
2
, M OSAWA
1
AND Y IWAMOTO
1
1
Diabetes Centre, Tokyo Womens Medical University School of Medicine, Tokyo, Japan;
2
Internal Medicine, Daini Hospital, Tokyo Womens Medical University, Tokyo, Japan
A 46-year-old Japanese man with type 2
diabetes mellitus, whose only diabetic
complication was simple retinopathy,
developed acute painful neuropathy. This
presented as paresthesia and hyper-
esthesia restricted to the abdomen. The
patients haemoglobin A
1c
had dropped
from 12% to 7.5% within 5 months,
following a rapid improvement in
glycaemic control. On investigation, there
were no indications of disease in the intra-
abdominal area. Nerve conduction studies
were consistent with mild sensorimotor
peripheral and autonomic neuropathy.
The patient required medication
(mexiletine, sulpiride and imipramine
hydrochloride) to control the pain.
Four months after presentation, the
symptoms showed a dramatic improve-
ment and the treatment for pain relief was
discontinued without any recurrence of
paresthesia or hyperesthesia in the
patients abdomen. This was a very
unusual case of diabetic post-treatment
painful neuropathy in which the
prominent features were severe pain,
paresthesia and hyperesthesia restricted to
the abdomen.
KEY WORDS: TYPE 2 DIABETES; HYPERESTHESIA; PAIN; PARESTHESIA; NEUROPATHY
Introduction
In patients with diabetes mellitus, painful
sensation and/or paresthesia are sometimes
precipitated by insulin treatment or strict
glycaemic control. The phenomenon is
generally called post-treatment painful
neuropathy, and it is regarded as an entity
of diabetic neuropathy.
1,2
The cause of post-
treatment painful neuropathy and the
reason why an individual might be
predisposed to develop it are unknown; the
prevalence is generally thought to be low.
2
One hypothesis suggests that post-treatment
painful neuropathy results from adequate
diabetic control promoting nerve
regeneration and that the pain may be
related to the ectopic generation of impulses
in regenerating axon sprouts.
3
Post-
treatment painful neuropathy usually
develops several weeks after a rapid
improvement in glycaemic control, and
presents as dramatic and severe pain in the
lower extremities. This usually subsides
within a year.
2
This paper presents a very unusual case of
acute painful neuropathy following a rapid
improvement in glycaemic control in which
the prominent feature was a severe pain
restricted to the abdomen.
by guest on June 26, 2014 imr.sagepub.com Downloaded from
Case report
A Japanese man aged 46 years was
diagnosed with type 2 diabetes in 1999. He
drank alcohol and did not smoke. He was
treated with glimepiride (3 mg/day), vogli-
bose (0.2 mg/day) and buformine (50 mg/day),
but his haemoglobin A
1c
(HbA
1c
) was 9 12%
because he did not control his diet. In April
2003, he adopted a healthier lifestyle by
commencing a strict diet and omitting
alcohol. Subsequently, his HbA
1c
had fallen
from 12% to 7.5% by August 2003, and he
developed pain, paresthesia and hyperesthesia
in his abdomen; these symptoms did not
affect other areas (end of June 2003). In
August 2003, the patient underwent general
clinical examination, an abdominal
ultrasound examination and assessment for
tumour markers (-fetoprotein [AFP],
carcinoembryonic antigen [CEA] and
carbohydrate antigenic determinant 19-9
[CA19-9]), which revealed no intra-
abdominal pathology.
On neurological examination, his cranial
nerve, knee jerk reflex and Achilles tendon
reflex were normal. In terms of the sensory
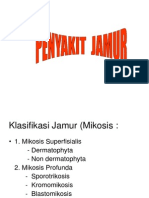
system, Fig. 1 shows that the dermatome
involved in the abnormal sensation
(paresthesia and hyperesthesia) was both
anterior sides of the thoracic (Th) spinal nerves
at levels 8 11. There were no other areas with
559
S Takayama, Y Takahashi, M Osawa et al.
Focal pain in the abdomen following rapid glycaemic control
FIGURE 1: The distribution of thoracic (Th) spinal nerves showing the abnormal
sensation (paresthesia and hyperesthesia) dermatome at levels 8 11 (shaded area)
associated with post-treatment painful neuropathy in a 46-year-old Japanese man
with type 2 diabetes following a rapid improvement in glycaemic control
Th1
Th2
Th3
Th4
Th5
Th6
Th7
Th8
Th9
Th10
Th11
Th12
by guest on June 26, 2014 imr.sagepub.com Downloaded from
abnormal sensation. There were no eruptions
on the skin of his trunk. Nerve conduction
studies were consistent with mild sensorimotor
peripheral neuropathy (motor nerve con-
duction velocity: right ulnar nerve 43.0 m/s,
right peroneal nerve 42.8 m/s; sensory nerve
conduction velocity: right ulnar nerve 48.6 m/s,
right sural nerve 46.5 m/s), and there was a
dysfunction of the autonomic nervous system
(heart rate variation on deep breathing:
9 beats/min). There was an osteophyte at the
Th10 level, but no evidence of spinal cord
compression on magnetic resonance imaging
(MRI) of the thoracic spine. With regard to
other diabetic complications, simple
retinopathy was found, but there was no
evidence of nephropathy.
At the end of August 2003, the patient
commenced treatment with mexiletine
(150 mg/day), sulpiride (150 mg/day) and
imipramine hydrochloride (30 mg/day) for
pain relief. Three weeks after treatment, his
symptoms showed a dramatic improvement,
and these drugs were discontinued at the end
of November 2003. There was no subsequent
recurrence of paresthesia and hyperesthesia
in his abdomen.
Discussion
This is a very unusual case of acute painful
neuropathy following a rapid improvement
in glycaemic control (HbA
1c
reduced from
12% to 7.5% within 5 months); the prominent
features were severe pain, paresthesia and
hyperesthesia restricted to the abdomen. We
speculate that the symptoms in this case
may have been caused by diabetic post-
treatment painful neuropathy.
The aetiology and pathogenesis of post-
treatment painful neuropathy are still
unclear. Previous studies have reported
arterio-venous shunting and proliferating
new vessels in acute painful neuropathy
following rapid glycaemic control.
4,5
Suzuki
et al.
6
reported that all five patients with
diabetic post-treatment painful neuropathy
in their study were identified as having a
mitochondrial tRNA (Leu) mutation at
position 3243. These observations cannot
completely explain the clinical course and
sites of pain sensation associated with post-
treatment painful neuropathy, however.
Greater care should be taken when
commencing strict glycaemic control in
diabetic patients with prolonged hyper-
glycaemia and previous neuropathy.
2,7
In this case, we had to discriminate
between a diagnosis of post-treatment
painful neuropathy or one of truncal
neuropathy. The latter usually presents with
pain and dysesthesia in areas of the chest or
abdomen or both.
8
The pathogenesis of
diabetic truncal neuropathy is also not
known with certainty, although it is widely
thought to be due to an ischaemic change
because it frequently has a sudden onset.
9
Clinically, the differential diagnosis of
diabetic truncal or post-treatment painful
neuropathy is very difficult. This is because
the clinical courses of diabetic truncal and
post-treatment painful neuropathy are very
similar and the symptoms of both often
subside within a year without medication. In
this particular case, it was also difficult to
differentiate between diabetic truncal
neuropathy and post-treatment painful
neuropathy. It is clear that symptoms of each
of these types of diabetic neuropathy are
triggered by a rapid improvement in
glycaemic control.
Polyneuropathy affecting the limbs,
usually in a distal or stocking and glove
distribution, has long been recognized in
diabetes mellitus.
10
Usual painful diabetic
neuropathy is just one of a myriad of
secondary conditions that may result from
poor glycaemic control. The sites of symptoms
of usual painful diabetic neuropathy also
560
S Takayama, Y Takahashi, M Osawa et al.
Focal pain in the abdomen following rapid glycaemic control
by guest on June 26, 2014 imr.sagepub.com Downloaded from
References
1 Ellenberg M: Diabetic neuropathy precipitating
after institution of diabetic control. Am J Med Sci
1958; 236: 466 471.
2 Takahashi Y, Takayama S, Ito T, Inoue Y,
Omori Y: Clinical features of eighty-six patients
with post-treatment painful neuropathy. J Jpn
Diab Soc 1998; 41: 165 170.
3 Llewelyn JG, Thomas PK, Fonseca V, King RH,
Dandona P: Acute painful diabetic neuropathy
precipitated by strict glycaemic control. Acta
Neuropathol (Berl) 1986; 72: 157 163.
4 Kihara M, Zollman PJ, Smithson IL, Lagerlund T,
Low PA: Hypoxic effect of exogenous insulin on
normal and diabetic peripheral nerve. Am J
Physiol 1994; 266: E980 E985.
5 Tesfaye S, Malik R, Harris N, Jakubowski JJ,
Mody C, Rennie IG, et al: Arterio-venous
shunting and proliferating new vessels in
acute painful neuropathy of rapid glycaemic
control (insulin neuritis). Diabetologia 1996; 39:
329 335.
6 Suzuki Y, Kadowaki H, Katagiri H, Suematsu M,
Atsumi Y, Hosokawa K, et al: Posttreatment
neuropathy in diabetic subjects with mito-
chondrial tRNA (Leu) mutation. Diabetes Care
1994; 17: 777 778.
7 Wilson JL, Sokol DK, Smith LH, Snook RJ,
Waguespack SG, Kincaid JC: Acute painful
neuropathy (insulin neuritis) in a boy following
rapid glycemic control for type 1 diabetes
mellitus. J Child Neurol 2003; 18: 365 367.
8 Stewart JD: Diabetic truncal neuropathy:
topography of the sensory deficit. Ann Neurol
1989; 25: 233 238.
9 Parry GJ, Floberg J: Diabetic truncal
neuropathy presenting as abdominal hernia.
Neurology 1989; 39: 1488 1490.
10 Ellenberg M: Diabetic neuropathy: clinical
aspects. Metabolism 1976; 25: 1627 1655.
11 Inoue Y, Takahashi Y, Oowada K, Hirata Y:
Clinical features of diabetics with painful post-
treatment neuropathy. Ann Jpn Soc Res Diab
Complicat 1990; 3: 72 78.
561
S Takayama, Y Takahashi, M Osawa et al.
Focal pain in the abdomen following rapid glycaemic control
show a distal or stocking and glove
distribution. The symptom (pain) areas
associated with post-treatment painful
neuropathy not only have a distal
distribution, however, but they may often be
found in other areas. Takahashi et al.
2
reported that the pain sites of post-treatment
painful neuropathy were the lower
extremities, with pain spreading evenly
throughout the body. Patients with post-
treatment painful neuropathy were
significantly thinner than patients without
post-treatment painful neuropathy at the
beginning of diabetic treatment. They also
had a greater impairment of the patella
tendon reflex and motor nerve conduction
velocity in the ulnar and peroneal nerves
and more sensory nerve symptoms.
11
The
present case is very unusual in terms of the
localization of the symptoms of pain.
Painful neuropathy is the transmission of
painful stimuli from the peripheral nerve
fibres (C-fibres) to the higher centres. A
recent study reported that pain from the
abnormal stimulation of C-fibres was caused
by an abnormality of the tetrodotoxin-
resistant sodium channels in post-treatment
painful neuropathy.
12
Alternatively,
abnormal opioid receptors in higher centres
have been shown to influence pain
sensitivity in chronic hyperglycaemia.
13
It is
not known which of these theories is correct,
and we also do not know which peripheral
nerve C-fibres may influence the painful
stimulation associated with post-treatment
painful neuropathy. In this case, there was
an osteophyte at the Th10 level, but there
was no evidence of spinal cord compression
on MRI and the symptoms of pain were not
stimulated by exercise. The osteophyte was
not considered to influence the symptoms,
therefore.
There is still much to learn about post-
treatment painful neuropathy and diabetes,
including which peripheral nerve C-fibres
may influence the painful stimulation.
Received for publication 29 March 2004 Accepted subject to revision 6 April 2004
Revised accepted 9 May 2004
Copyright 2004 Cambridge Medical Publications
by guest on June 26, 2014 imr.sagepub.com Downloaded from
562
S Takayama, Y Takahashi, M Osawa et al.
Focal pain in the abdomen following rapid glycaemic control
12 Hirade M, Yasuda H, Omatsu-Kanbe M,
Kikkawa R, Kitasato H: Tetrodotoxin-resistant
sodium channels of dorsal root ganglion
neurons are readily activated in diabetic rats.
Neuroscience 1999; 90: 933 939.
13 Ohsawa M, Mizoguchi H, Narita M, Kamei J,
Nagase H, Tseng LF: Effects of a mu-opioid
receptor agonist on G-protein activation in
streptozotocin-induced diabetic mice. Eur J
Pharmacol 2000; 28: 55 58.
Address for correspondence
Dr S Takayama
8-1 Kawada-cho, Shinjuku-ku, Tokyo162-8666, Japan.
E-mail: s-taka@ceres.dti.ne.jp
by guest on June 26, 2014 imr.sagepub.com Downloaded from
Anda mungkin juga menyukai
- BETPresentation DiabeticAmyotrophy (08!02!13)Dokumen10 halamanBETPresentation DiabeticAmyotrophy (08!02!13)Nigel SparksBelum ada peringkat
- Patogenesis Neuropatik DiabetikDokumen8 halamanPatogenesis Neuropatik DiabetikStephanie AureliaBelum ada peringkat
- Klair 2014Dokumen3 halamanKlair 2014PabloIgLopezBelum ada peringkat
- Convulsive Seizures With A Therapeutic Dose of Isoniazid: Case ReportDokumen4 halamanConvulsive Seizures With A Therapeutic Dose of Isoniazid: Case ReportSeptira MurtiningsihBelum ada peringkat
- Diabetic Amyotrophy Diagnosis and ManagementDokumen3 halamanDiabetic Amyotrophy Diagnosis and ManagementDavis G. OctaviusBelum ada peringkat
- Iabetic Europathy: DR Saumya H Mittal Neurologist Sharda Hospital & Health CityDokumen39 halamanIabetic Europathy: DR Saumya H Mittal Neurologist Sharda Hospital & Health CityGhea SugihartiBelum ada peringkat
- Hypokalemic Periodic ParalysisDokumen21 halamanHypokalemic Periodic ParalysisVarun VarnBelum ada peringkat
- Diabetic NeuropathyDokumen4 halamanDiabetic NeuropathyAsish GeiorgeBelum ada peringkat
- Essential Tremor - Practice Essentials, Background, EtiologyDokumen6 halamanEssential Tremor - Practice Essentials, Background, EtiologydilaBelum ada peringkat
- Painful Diabetic Neuropathy Treatment and Future AspectsDokumen6 halamanPainful Diabetic Neuropathy Treatment and Future AspectsChikezie OnwukweBelum ada peringkat
- Acute Pandysautonomia 1983Dokumen9 halamanAcute Pandysautonomia 1983iri_balBelum ada peringkat
- Bi Syndrome of The Knee Treated With Acupuncture With Patellofemoral Pain Syndrome As A CaseDokumen4 halamanBi Syndrome of The Knee Treated With Acupuncture With Patellofemoral Pain Syndrome As A CaseInfohoggBelum ada peringkat
- Painful NeuropathiesDokumen6 halamanPainful NeuropathiesAgusBhaktiBelum ada peringkat
- Stiff Person Syndrome and AnesthesiaDokumen15 halamanStiff Person Syndrome and AnesthesiaFarhan AshrafBelum ada peringkat
- Rare Spinal InfectionDokumen3 halamanRare Spinal InfectionAlam MartadipuraBelum ada peringkat
- International Journal of Pharmaceutical Science Invention (IJPSI)Dokumen3 halamanInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsBelum ada peringkat
- Diabetic NeuropathyDokumen10 halamanDiabetic NeuropathyIrma Sari RasyidBelum ada peringkat
- PQ Art 45906-10Dokumen4 halamanPQ Art 45906-10Vinay KumarBelum ada peringkat
- Two Acupuncture Styles for Painful Diabetic NeuropathyDokumen7 halamanTwo Acupuncture Styles for Painful Diabetic NeuropathyAnonymous PFNzHoBelum ada peringkat
- Seronegative Myasthenia Gravis Presenting With PneumoniaDokumen4 halamanSeronegative Myasthenia Gravis Presenting With PneumoniaJ. Ruben HermannBelum ada peringkat
- Alam2020 Article DiabeticNeuropathyCollectionTrDokumen8 halamanAlam2020 Article DiabeticNeuropathyCollectionTrAkreditasi InternaBelum ada peringkat
- Case Report: Diabetic Myonecrosis: Uncommon Complications in Common DiseasesDokumen3 halamanCase Report: Diabetic Myonecrosis: Uncommon Complications in Common DiseasesRezaBelum ada peringkat
- Status Epilepticus: Current Understanding: D P, M A M C, D GR M C, G, M PDokumen17 halamanStatus Epilepticus: Current Understanding: D P, M A M C, D GR M C, G, M PDMishraBelum ada peringkat
- ACR Fibromyalgia Diagnostic CriteriaDokumen6 halamanACR Fibromyalgia Diagnostic CriteriaMargaretta RambuBelum ada peringkat
- 2018 Article 187Dokumen4 halaman2018 Article 187Mario Francesco GalassoBelum ada peringkat
- Acupuncture For The Treatment of Chronic Painful Peripheral Diabetic Neuropathy: A Long-Term StudyDokumen7 halamanAcupuncture For The Treatment of Chronic Painful Peripheral Diabetic Neuropathy: A Long-Term StudyFernanda GiulianoBelum ada peringkat
- Acute Quadriplegia: An Exercise in Differential Diagnosis: DR - RamDokumen10 halamanAcute Quadriplegia: An Exercise in Differential Diagnosis: DR - Ramram49Belum ada peringkat
- Anaesthetic Considerations in Patients With Transverse MyelitisDokumen3 halamanAnaesthetic Considerations in Patients With Transverse MyelitisIniya RajendranBelum ada peringkat
- The Epilepsy Handbook: Understanding Seizures and Finding Effective TreatmentsDari EverandThe Epilepsy Handbook: Understanding Seizures and Finding Effective TreatmentsBelum ada peringkat
- Dor e FC2Dokumen7 halamanDor e FC2Douglas GarciaBelum ada peringkat
- Two Takayasu Arteritis Patients Successfully Treated With Infliximab: A Potential Disease-Modifying Agent?Dokumen8 halamanTwo Takayasu Arteritis Patients Successfully Treated With Infliximab: A Potential Disease-Modifying Agent?tera95Belum ada peringkat
- Hes 005 Session 12 SasDokumen12 halamanHes 005 Session 12 SasJose Melmar Autida AutenticoBelum ada peringkat
- Hes 005 Session 12 SasDokumen12 halamanHes 005 Session 12 SasBread PartyBelum ada peringkat
- Adrenal Insufficiency: Grand RoundsDokumen8 halamanAdrenal Insufficiency: Grand RoundsindahBelum ada peringkat
- Epilepsy CaseDokumen0 halamanEpilepsy CaseEggy PascualBelum ada peringkat
- Group 5 HFDokumen21 halamanGroup 5 HFJerson Aizpuro SuplementoBelum ada peringkat
- Treatment of Sciatica With Electro PDFDokumen4 halamanTreatment of Sciatica With Electro PDFAngela PagliusoBelum ada peringkat
- Swallow SyncopeDokumen4 halamanSwallow SyncopeKevinSheridanBelum ada peringkat
- Cardiovascular Changes in Patients Presenting With Vertigo: Original Research ArticleDokumen5 halamanCardiovascular Changes in Patients Presenting With Vertigo: Original Research ArticleEnvhy WinaBelum ada peringkat
- Fibromyalgia SyndromeDari EverandFibromyalgia SyndromeJacob N. AblinBelum ada peringkat
- Fatal Star Fruit Intoxication in Patient with Chronic Kidney DiseaseDokumen4 halamanFatal Star Fruit Intoxication in Patient with Chronic Kidney DiseaseMuhammadRizkyRadliyaMaulanaBelum ada peringkat
- Kissing Spine SyndromeDokumen4 halamanKissing Spine SyndromeMarcel Quario OrinaBelum ada peringkat
- Cerminara 2013Dokumen5 halamanCerminara 2013Roosevelt Santibañez Dla TorreBelum ada peringkat
- Jurding Neuro ShindyDokumen21 halamanJurding Neuro ShindyarifBelum ada peringkat
- Myasthenia Gravis (2016-2017) Lecture NotesDokumen9 halamanMyasthenia Gravis (2016-2017) Lecture NotesJibril AbdulMumin KamfalaBelum ada peringkat
- Fibromyalgia PDFDokumen5 halamanFibromyalgia PDFYalile TurkaBelum ada peringkat
- Electro Neurological Eductor Treatment For Peripheral NeuropathyDokumen36 halamanElectro Neurological Eductor Treatment For Peripheral NeuropathyClaudio Marcelo Naddeo100% (2)
- Thyrotoxic Periodic Paralysis: An Endocrine Cause of ParaparesisDokumen2 halamanThyrotoxic Periodic Paralysis: An Endocrine Cause of ParaparesisRina ErlinaBelum ada peringkat
- Physiotherapy Management: Otago Home Exercise ProgrammeDokumen9 halamanPhysiotherapy Management: Otago Home Exercise ProgrammeanjelikaBelum ada peringkat
- 2014 - Auricular Acupressure Helps Improve Sleep Quality For Severe Insomnia in Maintenance Hemodialysis Patients A Pilot StudyDokumen8 halaman2014 - Auricular Acupressure Helps Improve Sleep Quality For Severe Insomnia in Maintenance Hemodialysis Patients A Pilot StudyJoão PauloBelum ada peringkat
- Pain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Dokumen27 halamanPain Management: Dr. Prabowo Wicaksono Span Bagian/Smf Anestesi FK Unissula/Rsisa 2007Fendy PrasetyoBelum ada peringkat
- 03 Muscle and Neuromuscular Junction Disorders PDFDokumen325 halaman03 Muscle and Neuromuscular Junction Disorders PDFOTTO JESUS VEGA VEGA100% (2)
- General Medicine - 2013 - Shikino - Chest Pain The Only Symptom of Gastric UlcerDokumen3 halamanGeneral Medicine - 2013 - Shikino - Chest Pain The Only Symptom of Gastric UlcerDavid UkaegbuBelum ada peringkat
- Diabetic NeuropathyDokumen21 halamanDiabetic NeuropathyMargaretta RambuBelum ada peringkat
- Acupuncture For Progressive Oropharyngeal DysphagiaDokumen4 halamanAcupuncture For Progressive Oropharyngeal DysphagiaSarapzmBelum ada peringkat
- Treatment of Diabetic Neuropathy - UpToDateDokumen20 halamanTreatment of Diabetic Neuropathy - UpToDateKarina MilaréBelum ada peringkat
- Small Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationDari EverandSmall Fiber Neuropathy and Related Syndromes: Pain and NeurodegenerationSung-Tsang HsiehBelum ada peringkat
- Hypokalaemic Thyrotoxic Periodic Paralysis: Postgraduate ClinicDokumen6 halamanHypokalaemic Thyrotoxic Periodic Paralysis: Postgraduate Clinicrani fajraBelum ada peringkat
- Post-stroke Pain Patient RecoversDokumen6 halamanPost-stroke Pain Patient RecoversRadu StoenescuBelum ada peringkat
- Peripheral Neuropathy Diet: A Beginner's 3-Week Step-by-Step Plan to Managing the Condition Through Diet, With Sample Recipes and a 7-Day Meal PlanDari EverandPeripheral Neuropathy Diet: A Beginner's 3-Week Step-by-Step Plan to Managing the Condition Through Diet, With Sample Recipes and a 7-Day Meal PlanBelum ada peringkat
- Erythro 2Dokumen30 halamanErythro 2Syahrul Hamidi NasutionBelum ada peringkat
- DM Hiperestesia 4 PDFDokumen6 halamanDM Hiperestesia 4 PDFSyahrul Hamidi NasutionBelum ada peringkat
- DM Hiperestesia 4 PDFDokumen6 halamanDM Hiperestesia 4 PDFSyahrul Hamidi NasutionBelum ada peringkat
- KMNDokumen7 halamanKMNSyahrul Hamidi NasutionBelum ada peringkat
- Jamur OkDokumen18 halamanJamur OkSyahrul Hamidi NasutionBelum ada peringkat
- Small Dense LDL in Type 2 Diabetic PatientDokumen7 halamanSmall Dense LDL in Type 2 Diabetic PatientSyahrul Hamidi NasutionBelum ada peringkat
- Adult Motor Neurone DiseaseDokumen3 halamanAdult Motor Neurone DiseaseSyahrul Hamidi NasutionBelum ada peringkat
- Blood Cells UDokumen58 halamanBlood Cells USyahrul Hamidi NasutionBelum ada peringkat
- Predictor of Coronary Artery DiseasesDokumen7 halamanPredictor of Coronary Artery DiseasesSyahrul Hamidi NasutionBelum ada peringkat
- Dermatosa Vesiko BulosaDokumen14 halamanDermatosa Vesiko BulosaSyahrul Hamidi NasutionBelum ada peringkat
- Useful Marker Ofmetabolic SyndromeDokumen6 halamanUseful Marker Ofmetabolic SyndromeSyahrul Hamidi NasutionBelum ada peringkat
- SumberDokumen1 halamanSumberSyahrul Hamidi NasutionBelum ada peringkat
- Small Dense LDL in Type 2 Diabetic PatientDokumen7 halamanSmall Dense LDL in Type 2 Diabetic PatientSyahrul Hamidi NasutionBelum ada peringkat
- 595 - 610 Chimponda TDokumen16 halaman595 - 610 Chimponda TSyahrul Hamidi NasutionBelum ada peringkat
- AFHS0901 0040lkDokumen6 halamanAFHS0901 0040lkSyahrul Hamidi NasutionBelum ada peringkat
- Ghana study finds over half of TB patients malnourished at start of treatmentDokumen7 halamanGhana study finds over half of TB patients malnourished at start of treatmentSyahrul Hamidi NasutionBelum ada peringkat
- Nutrition, Diabetes and Tuberculosis in The Epidemiological TransitionDokumen7 halamanNutrition, Diabetes and Tuberculosis in The Epidemiological TransitionSyahrul Hamidi NasutionBelum ada peringkat
- Plasma MicrornaDokumen16 halamanPlasma MicrornaSyahrul Hamidi NasutionBelum ada peringkat
- Journal Pone 0029671Dokumen11 halamanJournal Pone 0029671Syahrul Hamidi NasutionBelum ada peringkat
- Fgene 02 00104Dokumen22 halamanFgene 02 00104Syahrul Hamidi NasutionBelum ada peringkat
- DAFTAR PUSTAKA - DocxlmDokumen2 halamanDAFTAR PUSTAKA - DocxlmSyahrul Hamidi NasutionBelum ada peringkat
- Serum MicrornaDokumen9 halamanSerum MicrornaSyahrul Hamidi NasutionBelum ada peringkat
- Serum MicroRNADokumen6 halamanSerum MicroRNASyahrul Hamidi NasutionBelum ada peringkat
- Relationship Between Computed Tomography Findings and Nutritional Status in Elderly Patients With Pulmonary TuberculosisDokumen6 halamanRelationship Between Computed Tomography Findings and Nutritional Status in Elderly Patients With Pulmonary TuberculosisSyahrul Hamidi NasutionBelum ada peringkat
- AJTCAM0701 0079jkjlkDokumen6 halamanAJTCAM0701 0079jkjlkSyahrul Hamidi NasutionBelum ada peringkat
- American Cancer SocietyDokumen66 halamanAmerican Cancer SocietySyahrul Hamidi NasutionBelum ada peringkat
- American Cancer SocietyDokumen66 halamanAmerican Cancer SocietySyahrul Hamidi NasutionBelum ada peringkat
- HPV and CA CerviksDokumen8 halamanHPV and CA CerviksSyahrul Hamidi NasutionBelum ada peringkat
- NIH Stroke ScaleDokumen8 halamanNIH Stroke Scalesridhar100% (2)
- Souvenir Program - APSAVD 2018Dokumen36 halamanSouvenir Program - APSAVD 2018Tiel NoembreuxBelum ada peringkat
- 17 Homeopathic Remedies for High CholesterolDokumen12 halaman17 Homeopathic Remedies for High CholesterolTora Kazi100% (1)
- Health Grade 11 LSDokumen4 halamanHealth Grade 11 LSMohammad AhmadBelum ada peringkat
- Food and Nutrition: Paper 6065/01 TheoryDokumen7 halamanFood and Nutrition: Paper 6065/01 Theorymstudy123456Belum ada peringkat
- Unit 1 Concepts of Physical FitnessDokumen116 halamanUnit 1 Concepts of Physical FitnessnanaBelum ada peringkat
- PT Free Course PreviewDokumen25 halamanPT Free Course Previewmathu0% (1)
- Association of Third Trimester Body Mass Index and Pregnancy Weight Gain in Obese Pregnant Women To Umbilical Artery Atherosclerotic Markers and Fetal OutcomesDokumen7 halamanAssociation of Third Trimester Body Mass Index and Pregnancy Weight Gain in Obese Pregnant Women To Umbilical Artery Atherosclerotic Markers and Fetal OutcomesMahida El shafiBelum ada peringkat
- Content PDFDokumen63 halamanContent PDFJayvincent JuanBelum ada peringkat
- Mobilizzazione LipidicaDokumen21 halamanMobilizzazione LipidicaLuca PellaBelum ada peringkat
- Dental Hygiene Board Exam Sample QuestionsDokumen3 halamanDental Hygiene Board Exam Sample Questionsgeislernet100% (5)
- Lordosis: Mark Anthony O.BernabeDokumen11 halamanLordosis: Mark Anthony O.BernabeJayson King Legaspi CruzBelum ada peringkat
- Accelerating Non-Communicable Disease Prevention and Control in The PhilippinesDokumen10 halamanAccelerating Non-Communicable Disease Prevention and Control in The PhilippinesRex RevelarBelum ada peringkat
- Biochemical and Molecular Mechanisms of Diabetic RetinopathyDokumen9 halamanBiochemical and Molecular Mechanisms of Diabetic RetinopathyNor Ubudiah SetiBelum ada peringkat
- Health and Physical Education Mod 1-2Dokumen20 halamanHealth and Physical Education Mod 1-2Ethel Jane RemoBelum ada peringkat
- 5 Ways of Healthy Living: Teliti Poster Di Bawah Dan Jawab Soalan-Soalan Yang BerikutDokumen2 halaman5 Ways of Healthy Living: Teliti Poster Di Bawah Dan Jawab Soalan-Soalan Yang BerikutMichael EllisBelum ada peringkat
- Chrononutrition in The Management of DiabetesDokumen11 halamanChrononutrition in The Management of DiabetesEva Mayte GuadarramaBelum ada peringkat
- Cholesterol Special Report - by Dr. MercolaDokumen17 halamanCholesterol Special Report - by Dr. Mercola4webusers administrator100% (3)
- 10 Rules of Progressive OverloadDokumen7 halaman10 Rules of Progressive Overloadambuenaflor100% (1)
- Athletic AdvantageDokumen14 halamanAthletic AdvantagealibababuaBelum ada peringkat
- Assignment in MSHR 507: Trends On Nutrition: A Paradigm Shif (Part I) & A Research Study (Part II)Dokumen61 halamanAssignment in MSHR 507: Trends On Nutrition: A Paradigm Shif (Part I) & A Research Study (Part II)Yiv IvesBelum ada peringkat
- EWSeasonalDesserts Web 2Dokumen15 halamanEWSeasonalDesserts Web 2imeir29Belum ada peringkat
- Body Mass Index As A Measure of Body Fatness Age and Sexspecific Prediction FormulasDokumen10 halamanBody Mass Index As A Measure of Body Fatness Age and Sexspecific Prediction Formulasdiego soltoBelum ada peringkat
- Expert system diagnoses diabetesDokumen123 halamanExpert system diagnoses diabetesIdhaRufaida100% (1)
- Endurance and Strength Training For Soccer PlayersDokumen16 halamanEndurance and Strength Training For Soccer PlayersMirko GraneseBelum ada peringkat
- NHIS DataDokumen80 halamanNHIS DataJin SiclonBelum ada peringkat
- Length-For-Age GIRLS: Birth To 6 Months (Percentiles)Dokumen15 halamanLength-For-Age GIRLS: Birth To 6 Months (Percentiles)Ceryle EriadyBelum ada peringkat
- Report-3 Organic LabDokumen12 halamanReport-3 Organic LabOmar SamirBelum ada peringkat
- Basic Biometrics StudentDokumen71 halamanBasic Biometrics StudentKatie100% (1)
- Standardization, Development and Organoleptic Evaluation of Nutri Bar Supplemented With Barley (Hordeum Vulgare)Dokumen5 halamanStandardization, Development and Organoleptic Evaluation of Nutri Bar Supplemented With Barley (Hordeum Vulgare)Abu Sufiyan FarooquiBelum ada peringkat
- Isa PH Project Chapter One To ThreeDokumen40 halamanIsa PH Project Chapter One To ThreeErhueh Kester AghoghoBelum ada peringkat