CPP and TCD 2009
Diunggah oleh
ctsakalakisJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CPP and TCD 2009
Diunggah oleh
ctsakalakisHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
Noninvasive Monitoring of Cerebral Perfusion
Pressure in Patients with Acute Liver Failure
Using Transcranial Doppler Ultrasonography
Shushma Aggarwal, David M. Brooks,
2
Yoogoo Kang,
8
Peter K. Linden,
3
and John F. Patzer II
2,4,5,6,7
1
Department of Anesthesiology,
2
Department of Bioengineering,
3
Department of Critical Care Medicine,
4
Department of Surgery,
5
Department of Chemical Engineering,
6
Thomas E. Starzl Transplantation Institute,
and
7
McGowan Institute for Regenerative Medicine, University of Pittsburgh, Pittsburgh, PA; and
8
Jefferson
Medical College, Thomas Jefferson University, Philadelphia, PA
Elevated intracranial pressure (ICP) leads to loss of cerebral perfusion, cerebral herniation, and irreversible brain damage in
patients with acute liver failure (ALF). Conventional techniques for monitoring ICP can be complicated by hemorrhage and
infection. Transcranial doppler ultrasonography (TCD) is a noninvasive device which can continuously measure cerebral blood
ow velocity, producing a velocity-time waveform that indirectly monitors changes in cerebral hemodynamics, including ICP.
The primary goal of this study was to determine whether TCD waveform features could be used to differentiate ALF patients
with respect to ICP or, equally important, cerebral perfusion pressure (CPP) levels. A retrospective study of 16 ALF subjects
with simultaneous TCD, ICP, and CPP measurements yielded a total of 209 coupled ICP-CPP-TCD observations. The TCD
waveforms were digitally scanned and seven points corresponding to a simplied linear waveform were identied. TCD
waveform features including velocity, pulsatility index, resistive index, fraction of the cycle in systole, slopes, and angles
associated with changes in the slope in each region, were calculated from the simplied waveform data. Paired ICP-TCD
observations were divided into three groups (ICP 20 mmHg, n 102; 20 ICP 30 mmHg, n 74; and ICP 30 mmHg,
n 33). Paired CPP-TCD observations were also divided into three groups (CPP 80 mmHg, n 42; 80 CPP 60 mmHg,
n 111; and CPP 60 mmHg, n 56). Stepwise linear discriminant analysis was used to identify TCD waveform features
that discriminate between ICP groups and CPP groups. Four primary features were found to discriminate between ICP groups:
the blood velocity at the start of the Windkessel effect, the slope of the Windkessel upstroke, the angle between the end systolic
downstroke and start diastolic upstroke, and the fraction of time spent in systole. Likewise, 4 features were found to
discriminate between the CPP groups: the slope of the Windkessel upstroke, the slope of the Windkessel downstroke, the
slope of the diastolic downstroke, and the angle between the end systolic downstroke and start diastolic upstroke. The TCD
waveform captures the cerebral hemodynamic state and can be used to predict dynamic changes in ICP or CPP in patients
with ALF. The mean TCD waveforms for corresponding, correctly classied ICP and CPP groups are remarkably similar.
However, this approach to predicting intracranial hypertension and CPP needs to be further rened and developed before
clinical application is feasible. Liver Transpl 14:1048-1057, 2008. 2008 AASLD.
Received November 21, 2007; accepted January 22, 2008.
Abbreviations:
ED
, end diastole angle;
PS
, peak systole angle;
PW
, peak Windkessel angle;
PS
, peak systole angle;
SD
, start diastole
angle;
SW
, start Windkessel angle; ALF, acute liver failure; CBFV, cerebral blood ow velocity; CPP, cerebral perfusion pressure; HR,
heart rate; ICP, intracranial pressure; MAP, mean arterial pressure; PaCO
2
, CO
2
partial pressure; PI, pulsatility index; RI, resistive
index; S
DD
, diastolic downstroke slope; S
DU
, diastolic upstroke slope; S
SD
, systolic downstroke slope; S
SU
, systolic upstroke slope; S
WD
,
Windkessel downstroke slope; S
WU
, Windkessel upstroke slope; SEM, standard error of the mean;
S
, fraction of time spent in systole;
T, core body temperature; TCD, transcranial Doppler ultrasonography; t
ED
, end diastole time; t
PD
, peak diastole time; t
PS
, peak systole
time; t
PW
, peak Windkessel time; t
SD
, systolic downstroke time; t
SS
, start systole time; t
SW
, start Windkessel time; V
ED
, end diastolic
velocity; V
M
, mean velocity over 1 cycle; V
PD
, peak diastole velocity; V
PS
, peak systolic velocity; V
PW
, peak Windkessel velocity; V
SD
, start
diastole velocity; V
SW
, start Windkessel velocity.
Address reprint requests to Shushma Aggarwal, Department of Anesthesiology, University of Pittsburgh Medical Center, Presbyterian C-220, 200
Lothrop Street, Pittsburgh, PA 15213. Telephone: 412-647-3262; FAX: 412-647-6290; E-mail: aggarwals@anes.upmc.edu
DOI 10.1002/lt.21499
Published online in Wiley InterScience (www.interscience.wiley.com).
See Editorial on Page 915
LIVER TRANSPLANTATION 14:1048-1057, 2008
2008 American Association for the Study of Liver Diseases.
Acute liver failure (ALF), the sudden onset of liver fail-
ure with no prior history of liver disease, is a life-threat-
ening condition. Short-term survival without trans-
plant ranges from 17% for cryptogenic liver failure to
nearly 70% in acetaminophen-related liver failure.
1
Ce-
rebral ischemia and herniation caused by cerebral
edema and intracranial hypertension are common
causes of death (38%-81% of cases) in ALF patients.
2-4
Even patients without signs of cerebral swelling in com-
puterized tomography brain scans are at risk for devel-
oping clinically signicant intracranial hypertension
and cerebral ischemia despite aggressive medical care.
5
Autoregulation of cerebral perfusion, which is usually
maintained by cerebral vasoconstriction or dilation in
response to the rate of cerebral metabolism, is impaired
in patients with advanced encephalopathy in ALF.
6
Maintenance of cerebral perfusion is a major goal in
the clinical management of ALF patients. The driving
force for cerebral blood ow is cerebral perfusion pres-
sure (CPP), which is related to the mean arterial pres-
sure (MAP) and intracranial pressure (ICP) by
CPP MAP ICP (1)
Generally, CPP greater than 60 mmHg is considered
sufcient to maintain intact neurological function. CPP
falling below 40 mmHg for more than 2 hours is con-
sidered a contraindication for liver transplantation in
some centers.
7
ICP is a major determinant of CPP. ICP measurement
by insertion of a monitoring probe into dural space is
the currently accepted method of detecting the pres-
ence of intracranial hypertension in ALF patients.
8
Be-
cause ALF patients uniformly develop coagulopathy
and sepsis, intracranial placement of an ICP sensor is
often complicated by hemorrhage, infection, and
death.
9
Consequently, reliable, noninvasive, continu-
ous monitoring of cerebral perfusion and ICP should be
able to help in assessing cerebral hemodynamics and
viability with minimal complications.
Transcranial Doppler ultrasonography (TCD) is a
noninvasive, continuous monitoring approach that can
measure cerebral blood ow velocity (CBFV) in the ma-
jor intracranial arteries through the intact cranium.
CBFV as measured by TCD is inuenced by the diam-
eter of the intracranial vessels, which, in turn, are af-
fected by the extramural pressure (cerebral swelling)
and intramural pressure (stenosis and vasospasm).
Therefore, changes in CBFV as seen by changes in the
TCDwaveformcan be a reection of changes in cerebral
hemodynamics (CPP, ICP, and CBFV). Several efforts
have been made to extract ICP from TCD waveform
analysis, primarily in head trauma applications in
which rising ICP is also a threat to patient survival.
Proposed correlations of ICP with the pulsatility index
(PI), which is dened as
PI
V
PS
V
ED
V
M
(2)
where V
PS
is the peak systolic velocity, V
ED
is the end
diastolic velocity, and V
M
is the mean velocity over 1
cycle, or the resistive index (RI), which is dened as
RI
V
PS
V
ED
V
PS
(3)
have had mixed results.
10-13
More recently, time series
regression of TCD ow velocity data with arterial blood
pressure has been proposed to compute ICP.
14-17
Other
approaches to estimating ICP from TCD include a bio-
mechanical representation of the brain coupled with
TCD,
18
extrapolation of TCD velocities to zero-ow ve-
locity,
19
and correlation with TCD spectral waveform
properties.
20
Despite the importance of ICP monitoring in ALF,
surprisingly little work has been done with TCD as a
tool for estimating ICP.
21-26
Sidi and Mahla
21
found a
weak correlation between CPP and PI in a case study of
1 ALF patient.
21
Larsen and coworkers have shown that
changes in CBFV can be used to detect changes in
cerebral autoregulation
24,26
and can be predictive of
brain herniation.
22
Because CPP is the difference between the pressures
driving and opposing cerebral perfusion, MAP and ICP,
respectively, we hypothesize that TCD waveform anal-
ysis can be used to detect transitions in CPP or ICP that
signal the need for immediate medical attention in pa-
tients with ALF. Such a diagnostic capability could de-
lay the placement of a traditional ICP monitor until it is
actually required and possibly avoid placement of an
ICP probe entirely if either CPP remains above or ICP
remains below a threshold that mandates medical in-
tervention. Previous clinical experience in head trauma
suggests that ICP rising above about 30 mmHg is a
critical transition.
27
We suggest a corresponding criti-
cal transition of CPP below about 60 mmHg. The aim of
this study is to determine the feasibility of using com-
ponents from the TCD waveform to discriminate the
critical CPP or ICP transition in ALF patients.
PATIENTS AND METHODS
Subject Population
In accordance with a protocol approved by the Univer-
sity of Pittsburgh Institutional Review Board, 16 sub-
jects who (1) were admitted to the Liver Transplant
Intensive Care Unit at the University of Pittsburgh Med-
ical Center (Pittsburgh, PA) with a diagnosis of ALF over
a contiguous 2-year period (to ensure comparable stan-
dards of care), (2) had an epidural ber optic continu-
ous ICP monitor (Ladd Research Laboratories, Burling-
ton, VT) placed as part of routine medical care, and (3)
had readable noninvasive TCD cerebral blood ow
scans were retrospectively identied for inclusion in
this study.
The mean age of the subject population was 38 years
(range: 16-67); 14 females, 2 males. The admission
diagnosis varied and included acetaminophen overdose
(5), viral hepatitis (3), macrodantin (1), postpartum
hepatitis (1), halothane (1), and undetermined (5). All
NONINVASIVE MONITORING WITH TCD IN ALF 1049
subjects were in grade 3 or 4 hepatic coma (grade 3,
coma but responsive to painful stimuli; grade 4, coma
unresponsive to painful stimuli) and were intubated
and mechanically ventilated.
Clinical management was directed toward mainte-
nance of MAP through administration of volume (crys-
talloid, colloid, and packed red blood cells) and vaso-
pressors (dopamine, epinephrine, and norepinephrine)
as needed. ICP sensor placement was by insertion into
the epidural space after gentle stripping of the dura off
the inner table of the skull via a burr hole. If necessary,
fresh frozen plasma and/or platelets were administered
to optimize coagulation as determined by thromboelas-
tography (reaction time 8 minutes and maximum
amplitude 40 mm)
13
prior to ICP sensor placement.
Periodic TCD measurements of CBFV in the middle
cerebral artery were obtained once every 24 hours or
whenever a signicant change in the patients clinical
status or monitored ICP occurred. The TCD measure-
ments were made with a 2-MHz Doppler ultrasound
probe (Transpect, Medasonic, Mountain View, CA),
which was mechanically xed in place by probe holders.
The depth of insonation of the middle cerebral artery
was 45-50 mm. After observation of the TCD signal for 2
minutes for stability, a velocity tracing containing several
consecutive cycles was printed at a speed of 25 mm/s. A
zero velocity baseline was included with each tracing.
The 16 patients yielded a total of 209 coupled CPP-
ICP-TCD observations with associated physiologic sta-
tus measurements, which included electrocardiogram,
systemic blood pressure from an indwelling intra-arte-
rial catheter, arterial blood gas tensions [O
2
partial
pressure, CO
2
partial pressure (PaCO
2
), pH, and base
excess], core body temperature, and coagulation prole
(prothrombin time and/or thromboelastography).
Relationship Between the Cardiac Cycle
Pressure Pulse Waveform and TCD Waveform
Figure 1 schematically depicts the relationship between
the cardiac cycle aortic pressure pulse waveform (solid
line) and the TCD waveform (dotted line). The pressure
pulse and TCD waveforms each consist of 2 phases:
systolic and diastolic. The start of the systolic phase
correlates with the opening of the aortic valve. The sys-
tolic pressure pulse rst rises with myocardial contrac-
tion and volume ejection and then tapers as the volume
ejection tapers. The systolic part of the TCD waveform
exhibits 2 peaks. The rst peak is predominantly re-
lated to myocardial contractility. The second peak
(Windkessel effect) is related to the distensibility (com-
pliance) of the arterial wall and subsequent volume
displacement effect. The dicrotic notch, which marks
the start of the diastolic phase, corresponds to closure
of the aortic valve and is associated with resistance in
the distal vessels.
A simplied, linear TCD waveform that captures the
changes seen with rising ICP in ALF
28
is depicted in Fig.
2. The linearized waveform is represented by 7 [time (s),
velocity (cm s
1
)] pairs: (1) start systole (start of a new
cycle), (t
SS
, V
ED
); (2) peak systole, (t
PS
, V
PS
); (3) start
Windkessel effect, (t
SW
, V
SW
); (4) peak Windkessel ef-
fect, (t
PW
, V
PW
); (5) start diastole, (t
SD
, V
SD
); (6) peak
diastole, (t
PD
, V
PD
); and (7) end diastole, (t
ED
, V
ED
).
Characteristic features of the waveform, such as the
slope in each linearized segment, angle between linear
segments, mean velocity over a cycle, PI, RI, and frac-
tion of the cycle spent in systole (related to narrowing of
the systolic peak) can be calculated from the (velocity,
time) data. The algebraic equations used to calculate
the characteristic features are provided in the appen-
dix.
Figure 1. Relation between the cardiac output pressure pulse
(solid line; adapted from Bruner
33
) and linearized TCD wave-
form (dashed line) at an equivalent time scale. Both the pres-
sure pulse and the TCD waveform have distinct (A) systolic
upstroke, (B) systolic downstroke, (C) diastolic upstroke, and
(D) diastolic downstroke. (E) In addition, the TCD waveform
has a Windkessel notch during the systolic downstroke.
Figure 2. Schematic of a linearized 7-point TCD waveform
showing Windkessel effect during systolic downstroke. The
seven (velocity, time) points are used with the equations pro-
vided in the appendix to calculate TCD waveform features
including: slope systolic upstroke (S
SU
); slope systolic down-
stroke (S
SD
); slope Windkessel upstroke (S
WU
); slope Windkes-
sel downstroke (S
WD
); slope diastolic upstroke (S
DU
); slope
diastolic downstroke (S
DD
); the angles between adjacent
slopes (); and the fractional time spent in systole (
S
).
1050 AGGARWAL ET AL.
TCD waveforms were digitally scanned. The pixel co-
ordinates corresponding to the waveform origin, veloc-
ity scale, time scale, and 7 (velocity, time) points of the
linearized waveform were visually determined and re-
corded. The pixel values were then converted into ap-
propriate (velocity, time) pairs for use in the analysis.
Statistical Analysis
The 209 observations were classied into 3 ICP groups
based on the following ranges: ICP 20 mmHg (group
1, n 102), 20 mmHg ICP 30 mmHg (group 2, n
74), and ICP 30 mmHg (group 3, n 33). The ICP
groupings were chosen to represent the breakpoints at
which clinical attention to and possible intervention for
rising ICP is warranted
27
: no intervention (ICP 20
mmHg),; close monitoring (20 mmHg ICP 30
mmHg), and probable need for ICP monitor placement
(ICP 30 mmHg). The 209 observations were also in-
dependently classied into 3 CPP groups based on the
following ranges: CPP 80 mmHg (group A, n 42), 80
mmHg CPP 60 mmHg (group B, n 111), and
CPP 60 mmHg (group C, n 56). The CPP groupings
were also chosen to represent breakpoints at which
clinical attention to and possible intervention for falling
CPP might be warranted.
Stepwise linear discriminant analysis (SPSS, Inc.,
Chicago, IL) was used to identify which, if any, TCD
waveform features identied previously and listed in
the appendix discriminate between the 3 ICP groups
and, independently, the 3 CPP groups. Linear discrimi-
nant analysis is a useful tool for determining whether
any known variables distinguish between 2 or more
groups. Computationally, linear discriminant analysis
is similar to analysis of variance or multivariate analy-
sis of variance. The stepwise approach builds the linear
discriminant model variable by variable: at each step,
all variables not currently in the model are evaluated to
determine which contributes most to discrimination
between the groups. That variable is then added to the
model. The process continues until the remaining (ex-
cluded) variables do not signicantly contribute to dis-
crimination between the groups. The F probability for a
waveform feature to enter and be removed from the
discriminant analysis was set at 0.05 and 0.10, respec-
tively.
RESULTS
Means and standard errors of the mean by ICP or CPP
and group are presented in Table 1 for the selected
physiologic variables of ICP, CPP, MAP, core body tem-
perature (C), heart rate (min
1
), and arterial PaCO
2
(mmHg). ICP increases and CPP decreases as ALF
progresses fromgroup 1 to group 3 for either ICP or CPP
groupings. Likewise, MAP declines from group 1 to
group 3 despite the clinical objective of MAP mainte-
nance. The core body temperature remained near nor-
mal for all groupings. The heart rate tended to rise as
ALF progressed. Finally, PaCO
2
declined somewhat as
ALF progressed. This occurred because of an attempt
made to reduce ICP by hyperventilation.
Linear discriminant analysis of the ICP groups iso-
lated 4 waveformfeatures (the blood velocity at the start
APPENDIX: Linearized Seven-Point Transcranial Doppler Ultrasonography Waveform Features Used in the Linear
Discriminant Analysis
Feature Symbol Equation
Mean cycle velocity (cm s
1
) V
M
V
M
0.5
iSS
iPD
V
i1
V
i
t
i1
t
i
/t
ED
t
SS
Pulsatility index PI PI V
PS
V
ED
/V
M
Resistive index RI RI V
PS
V
ED
/V
ED
Fractional time in systole
S
S
t
SD
t
SS
/t
ED
t
SS
Slopes (V/t; cm s
2
)
Systolic upstroke (SU) S
SU
S
SU
V
PS
V
ED
/t
PS
t
SS
Systolic downstroke (SD) S
SD
S
SD
V
SW
V
PS
/t
SW
t
PS
Windkessel upstroke (WU) S
WU
S
WU
V
PW
V
SW
/t
PW
t
SW
Windkessel downstroke (WD) S
WD
S
WD
V
SD
V
PW
/t
SD
t
PW
Diastolic upstroke (DU) S
DU
S
DU
V
PD
V
SD
/t
PD
t
SD
Diastolic downstroke (DD) S
DD
S
DD
V
ED
V
PD
/t
ED
t
PD
Angles ()
Peak systole (PS)
PS
PS
1801 tan
1
S
SD
/100 tan
1
S
SU
/100/
Start Windkessel
SW
SW
1801 tan
1
S
SD
/100 tan
1
S
WU
/100/
Peak Windkessel (PW)
PW
PW
1801 tan
1
S
WD
/100 tan
1
S
WU
/100/
Start diastole (SD)
SD
SD
1801 tan
1
S
WD
/100 tan
1
S
DU
/100/
Peak diastole (PD)
PD
PD
1801 tan
1
S
DD
/100 tan
1
S
DU
/100/
End diastole (ED)
ED
ED
1801 tan
1
S
DD
/100 tan
1
S
SU
/100/
Abbreviations: t
ED
, end diastole time; t
PD
, peak diastole time; t
PS
, peak systole time; t
PW
, peak Windkessel time; t
SD
, systolic
downstroke time; t
SS
, start systole time; t
SW
, start Windkessel time; V
ED
, end diastolic velocity; V
PD
, peak diastole velocity; V
PS
,
peak systolic velocity; V
PW
, peak Windkessel velocity; V
SD
, start diastole velocity; V
SW
, start Windkessel velocity; V, change
in velocity; t, change in time.
NONINVASIVE MONITORING WITH TCD IN ALF 1051
of the Windkessel effect, the slope of the Windkessel
upstroke, the angle between the end systolic down-
stroke and start diastolic upstroke, and the fraction of
time spent in systole) that could be used to successfully
classify 61% of group 1 (ICP 20 mmHg), 53% of group
2 (20 mmHg ICP 30 mmHg), and 67% of group 3
(ICP 30 mmHg) into the proper groups (see Table 2).
Means and standard errors of the mean of the 4 dis-
criminant waveformfeatures for subjects correctly clas-
sied (true classication) in each group are provided in
Table 1.
Figure 3 depicts TCD waveforms constructed from
the average values of the variables for correctly classi-
ed subjects in each ICP group. As ICP rises fromgroup
1 to group 2, the blood ow velocity increases because
of external compression on the artery reducing the ves-
sel diameter. Consequently, the blood velocity at the
start of the Windkessel effect becomes greater because
of the overall velocity shift upward. The slope associ-
ated with Windkessel upstroke decreases because of
reduced compliance of the arteries. The angle between
the systolic and diastolic phases becomes more acute
as ALF progresses from group 1 to group 3. Finally,
despite contraction of the waveform cycle with respect
to time with progressing disease state, the fraction of
time spent in systole increases.
Linear discriminant analysis of the CPP groups iso-
lated 4 waveform features (the slope of the Windkessel
upstroke, the slope of the Windkessel downstroke, the
TABLE 1. Mean and SEM Values by Group for Selected Physiologic Variables and Discriminating Waveform Features
ICP Groups
Group 1 Group 2 Group 3
Mean SEM Mean SEM Mean SEM
ICP 14.4 0.5 24.2 0.4 37.1 1.3
CPP 75.7 1.7 67.3 2.4 48.7 3.4
MAP 90.2 1.4 91.5 2.2 85.8 2.8
T 37.5 36.5
HR 103.2 3.2 99.1 1.9 112.4 3.7
PaCO
2
30.6 0.7 28.7 1.2 28.6 0.9
Discriminating waveform features
V
SW
55 2 96 5 79 3
S
0.42 0.01 0.46 0.01 0.46 0.01
S
WU
3 27 103 38 618 46
SD
66 2 52 2 35 2
CCP Groups
Group A Group B Group C
Mean SEM Mean SEM Mean SEM
ICP 15.9 1.2 18.7 0.9 28.9 1.8
CPP 90.6 1.3 69.8 0.9 45.9 1.9
MAP 106.5 1.2 88.5 1.0 74.8 1.8
T 37.5 35.3
HR 91.3 3.8 100.4 1.7 110.7 2.6
PaCO
2
31.9 0.8 29.5 1.0 26.3 0.9
Discriminating waveform features
S
SD
293 17 421 20 727 54
S
WU
34 23 10 25 582 39
S
DD
53 2 76 5 84 8
SD
51 1 68 2 39 2
Abbreviations:
SD
, start diastole angle; CPP, cerebral perfusion pressure (mmHg); HR, heart rate (min
1
); ICP, intracranial
pressure (mmHg); MAP, mean arterial pressure (mmHg); PaCO
2
, arterial CO
2
pressure (mmHg); S
DD
, diastolic downstroke
slope; SEM, standard error of the mean; S
SD
, systolic downstroke slope; S
WU
, Windkessel upstroke slope;
S
, fraction of time
spent in systole; T, core body temperature (C); V
SW
, start Windkessel velocity.
TABLE 2. ICP and CPP Group Classication
Percentages, Predicted Versus Actual, from Linear
Discriminant Analysis
Actual ICP group
Predicted ICP Group
1 2 3
1 61 (62) 28 (29) 11 (11)
2 27 (20) 53 (39) 20 (15)
3 18 (6) 15 (5) 67 (22)
Actual CPP group
Predicted CPP Group
A B C
A 76 (32) 19 (8) 5 (2)
B 38 (42) 43 (48) 19 (21)
C 21 (12) 16 (9) 63 (35)
NOTE: n in parentheses.
1052 AGGARWAL ET AL.
slope of the diastolic downstroke, and the angle be-
tween the end systolic downstroke and start diastolic
upstroke) that could be used to successfully classify
76% of group A (CPP 80 mmHg), 43% of group B (80
mmHg CPP 60 mmHg), and 63% of group C (CPP
60 mmHg) into the proper groups (see Table 2). Means
and standard errors of the mean of the 4 discriminant
waveform features for subjects correctly classied in
each group are provided in Table 1.
Figure 4 depicts TCD waveforms constructed from
the average values of the variables for correctly classi-
ed subjects in each CPP group. The Windkessel effect
is dampened and is lost as CPP decreases from group A
to group C. This is reected in the increasingly negative
slopes associated with the Windkessel upstroke and the
Windkessel downstroke. Unlike the ICP groupings, the
angle between the systolic and diastolic phases is more
obtuse for group B than group A and more acute for
group C than both group A and group B. The fourth
discriminating waveform feature in the CPP analysis,
increasingly negative diastolic downstroke slope, is also
evident in Fig. 4.
A time series of TCD scans (middle cerebral artery
blood ow velocity versus time) from a patient with
progressing ALF is shown in Fig. 5A-E. The dark line
above the TCD scan in each frame represents a linear-
ization of the waveform from the scan that was used in
the data analysis. The linearized waveforms in Fig. 5A,B
have a second peak in the systolic phase that reects
the Windkessel effect. As ICP increases and CPP de-
creases (Fig. 5C-E), the Windkessel effect disappears,
and the systolic peak sharpens and narrows.
DISCUSSION
The time series of TCD scans presented in Fig. 5 is a
vignette representing a natural history of the progress-
ing disease states in ALF with respect to cerebral per-
fusion. Figure 5A reects a nearly normal velocity wave-
form with a distinguishable Windkessel notch and
relatively small acceleration at the start of diastole.
Even though MAP, ICP, and CPP are almost the same in
Fig. 5B and in Fig. 5A, there is a marked difference in
the shape of the TCD waveform because of the 50%
increase in cerebral blood ow [from 20 (Fig. 5A) to 31
mL/100 g/minute (Fig. 5B)] and cerebral vasodilation
as evidenced by the increased CBFV. As the cerebral
hemodynamics continue to deteriorate (Fig. 5C, ICP
40 mmHg), the TCD waveform shows loss of the Wind-
kessel effect because of dysfunctional elasticity of the
intracranial vessels (vasoparalysis)
24
and increased ex-
tramural pressure from cerebral swelling. Both of these
effects limit expansion of the intracranial arteries dur-
ing the opening of the aortic valve in the cardiac cycle.
However, MAP is still sufcient to drive signicant blood
ow through the narrowed vessels as evidenced by the
high CBFV. Figure 5D depicts the combination of rising
ICP and falling MAP, which results in a sharply dened
systolic ow peak at lower peak velocity as the net
driving force, CPP, drops. In the nal stage of disease
progression, with a net driving force near zero, Fig. 5E
shows a very sharp systolic peak with probable retro-
grade ow during diastole as the extramural pressure
squeezes the arterial vessel closed between cardiac cy-
cle pressure pulses.
The TCD sequence in Fig. 5 indicates that TCD can
provide information about the dynamic state of the in-
Figure 3. Average linearized TCD waveforms calculated from
Group 1 (ICP < 20 mmHg; mean ICP 14 mmHg; range ICP
5-19 mmHg), Group 2 (20 mmHg < ICP < 30 mmHg; mean
ICP 24 mmHg; range ICP 20-29 mmHg), and Group 3
(ICP > 30 mmHg; mean ICP 37 mmHg; ICP range 30-48
mmHg) data correctly classied by linear discriminant analy-
sis. Highlighted signicant classication features found by
the discriminant analysis are: blood velocity at start of the
Windkessel effect (V
SW
); slope of the Windkessel upstroke
(S
WU
); angle between systolic downstroke and diastolic up-
stroke (
SD
). Although not specically identied in order to
maintain clarity, note that the time associated with
SD
, which
is t
S
, decreased (shifts left) with increasing ICP.
Figure 4. Average linearized TCD waveforms calculated from
Group A (CPP > 80 mmHg; mean CPP 91 mmHg; range
CPP 81-110 mmHg), Group B (80 mmHg >CPP >60 mmHg;
mean CPP 70 mmHg; range CPP 61-79 mmHg), and Group
C (CPP < 60 mmHg; mean CPP 46 mmHg; range CPP
16-59 mmHg) data correctly classied by linear discriminant
analysis. Highlighted signicant classication features found
by the discriminant analysis are: slope of the Windkessel up-
stroke (S
WU
); slope of the Windkessel downstroke (S
WD
); slope
of the diastolic downstroke (S
DD
); and the angle between the
end systolic downstroke and the start diastolic upstroke (
SD
).
NONINVASIVE MONITORING WITH TCD IN ALF 1053
Figure 5. Transcranial Doppler waveform recordings from a single patient with progressing acute liver failure. In addition to
sharpening of the systolic peak in the waveform, the waveform changes from one that includes a Windkessel effect (asterisks in
panels Aand B) to one that does not as liver failure progresses. Abbreviations: CPP, cerebral perfusion pressure; ICP, intracranial
pressure; MAP, mean arterial pressure.
1054 AGGARWAL ET AL.
tracranial circulation and perfusion. However, the de-
termination of quantitative relationships between the
various parameters that characterize the state of intra-
cranial hemodynamics with the physiologic status of a
patient is difcult because of the complexity and vari-
ation of the many physiological factors acting at the
same time in the regulation of the cerebral circulation.
For example, unlike peripheral circulation, the magni-
tude of the cranial blood pressure pulse is dependent
on the restricted volume of the intracranial contents as
well as the elasticity and volume of the blood vessels,
and this makes interpretation of the TCD waveform
more complex. Fluctuations in PaCO
2
, MAP, and tem-
perature, which are common in ALF patients, further
complicate interpretation. For example, declining
PaCO
2
with progressing disease state (Table 1) is asso-
ciated with reduced blood vessel elasticity and thus
reduced elastic rebound (Windkessel effect) from the
pressure pulse. Such complex interactions limit the
ability to develop rigorous and quantitative descriptions
for the prediction of intracranial conditions based on
simple measurements.
PI has been the most commonly used parameter for
estimating changes in ICP because of its simplicity of
calculation. Indeed, PI has certain advantages; for ex-
ample, it is not affected by minor changes in the angle of
insonation, and it reects a combination of several
physiological factors, including the resistance in the
distal vessels, elasticity of the vessel wall, and size of
the vessels. However, the shortcomings of PI are that it
is inuenced by multiple factors such as the heart rate,
systemic blood pressure, and arterial oxygen and car-
bon dioxide tension. Consequently, PI alone is insuf-
cient to characterize the overall intracranial hemody-
namic condition.
14,29-32
In particular, PI cannot capture information about
the Windkessel effect. The Windkessel effect arises from
the elastic compliance of arterial vessels. A pressure
wave (forward systole) traveling along an artery causes
(elastic) expansion of the artery against the surround-
ing tissue. The amount of expansion is proportional to
the pressure difference between the interior (arterial)
and exterior (cranial) sides of the vessel. As the pres-
sure pulse recedes (reverse systole), the artery returns
to its original diameter, returning energy to the ow,
which is evidenced as an acceleration in ow velocity.
Increased extramural pressure (for example, cerebral
swelling) or arterial vasoparalysis due to declining CO
2
concentration reduces the ability of the cranial arteries
to expand and contract with the change in pressure
generated by the opening and closing of the cardiac
aortic valve. As a result, rising ICP reduces the arterial
expansion from the pressure pulse and thus reduces
the secondary acceleration associated with the Wind-
kessel effect. Sufciently high ICP prevents arterial ex-
pansion with the systolic pressure wave and leads to
loss of the Windkessel effect.
Rather than use a single lumped parameter index
such as PI (which simply looks at the extrema in ow
velocities), this study indicates that other easily identi-
able and calculable features of the TCD waveform that
noticeably change as both ICP and CPP change can be
advantageously used to infer the state of cerebral per-
fusion with little addition of complexity. The visual,
linearized TCD waveform, as presented in Fig. 2, is
characterized by 7 (time, velocity) pairs from which ad-
ditional parameters such as the mean cycle velocity, PI,
RI, accelerations, and angles can be calculated (see the
appendix). The present work is a retrospective analysis
used to determine whether these features contain use-
able information about ICP and CPP suitable for clinical
decision purposes.
As illustrated in Figs. 3 and 4, the average TCD wave-
forms that characterize the state of cerebral perfusion
based on the linear discrimination analysis are remark-
ably similar, regardless of whether ICP or CPP is used
as the grouping variable. The ICP group 1 (Fig. 3) and
CPP group A (Fig. 4) waveforms reect the expectations
of normal cerebral perfusion with a pronounced Wind-
kessel effect. As ICP begins to rise or CPP begins to fall,
the ICP group 2 (Fig. 3) and CPP group B (Fig. 4) wave-
forms both reect an increase in the systolic velocity
and loss in arterial compliance, as reected by the
Windkessel notch angle becoming more obtuse and by
lessening of the Windkessel upstroke slope. Finally, the
waveforms associated with the elevated ICP group 3
(Fig. 3) and low CPP group C (Fig. 4) evidence complete
loss of the Windkessel effect. The similarity in waveform
shapes between ICP and CPP for the various groups is
even more striking when one considers that ICP and
CPP are intimately related by Equation 1 and that clin-
ical management strategy is to maintain constant MAP
through the use of volume and vasopressors.
The value of any classication system has to be eval-
uated in terms of its clinical usefulness. The fact that
the linear discriminant analysis produced remarkably
similar average waveforms regardless of classication
by ICP or CPP indicates that it may be a clinically useful
tool for helping to guide the decision of whether further
invasive monitoring, such as placement of an ICP
probe, is warranted.
Even though the present TCD waveform analysis
could correctly classify subjects into the proper ICP/
CPP group 43%-76% of the time (see Table 2), the re-
sults are encouraging given that this is a retrospective
study used to determine whether further effort in de-
veloping ICP/CPP group predictive capability from TCD
waveform analysis is worth pursuing. Known factors
that limited the ability of the linear discriminant anal-
ysis to correctly classify the linearized TCD waveforms
used in this work into appropriate groups include the
following: (1) the TCD scans that were used were of
variable quality (for example, light to dark contrast and
skewed time and velocity axes); (2) the (velocity, time)
points that characterized an individual, linearized TCD
waveform were visually identied, were somewhat sub-
jective, and could vary between different observers; (3)
stratication into groups arbitrarily converted continu-
ous variables, ICP and CPP, into classication vari-
ables; and (4) the choice of the ICP or CPP cutoff be-
NONINVASIVE MONITORING WITH TCD IN ALF 1055
tween the groups, based on current clinical practice
with respect to medical intervention, was somewhat
arbitrary.
The rst 2 factors can be overcome by real-time fast
Fourier spectral transformation of the TCD waveform.
The resulting spectral information will contain all of the
original waveform information and is not subject to the
problems cited. Given that the objective of this work is
a clinical decision-making tool about the need for inter-
vention rather than accurate prediction of actual ICP,
the second 2 factors represent constraints on classi-
cation performance that should be investigated more
rigorously in a prospective study.
In conclusion, measurement of CBFV by TCD is
useful as a screening tool in the qualitative assess-
ment of vasospasm, stenosis, cerebral blood ow,
ICP, and cerebral embolic episodes. Information ob-
tained by TCD waveform analysis can not only assist
in screening but can also provide quantitative assess-
ment of cerebral hemodynamics. The preliminary re-
sults on the correlation of TCD waveform features
with the state of cerebral perfusion are promising.
Improved predictive capability for ICP and CPP from
TCD is expected from the correlation of the real-time
fast Fourier transform spectrum of the waveform with
ICP and CPP.
REFERENCES
1. Ostapowicz G, Fontana RJ, Schidt FV, Larson A, Davern
TJ, Han SH, et al. Results of a prospective study of acute
liver failure at 17 tertiary care centers in the United States
[see comments; summary for patients appears in Ann In-
tern Med 2002;137:I24]. Ann Intern Med 2002;137:947-
954.
2. Gazzard BG, Portmann B, Murray-Lyon IM, Williams R.
Causes of death in fulminant hepatic failure and relation-
ship to quantitative histological assessment of parenchy-
mal damage. Q J Med 1975;44:615-626.
3. Ware AJ, DAgostino AN, Combes B. Cerebral edema: a
major complication of massive hepatic necrosis. Gastroen-
terology 1971;61:877-884.
4. Ede RJ, Williams RW. Hepatic encephalopathy and cere-
bral edema. Semin Liver Dis 1986;6:107-118.
5. Aggarwal S, Kramer D, Yonas H, Obrist W, Kang Y, Martin
M, Policare R. Cerebral hemodynamic and metabolic
changes in fulminant hepatic failure: a retrospective
study. Hepatology 1994;19:80-87.
6. Riordan SM, Williams R. Fulminant hepatic failure. Clin
Liver Dis 2000;4:25-45.
7. Hoofnagle JH, Carithers RL Jr, Shapiro C, Ascher N. Ful-
minant hepatic failure: summary of a workshop. Hepatol-
ogy 1995;21:240-252.
8. Sass DA, Shakil AO. Fulminant hepatic failure. Gastroen-
terol Clin N Am 2003;32:1195-1211.
9. Blei AT, Olafsson S, Webster S, Levy R. Complications of
intracranial pressure monitoring in fulminant hepatic fail-
ure [see comment]. Lancet 1993;341:157-158.
10. Sidi A, Messinger G, Mahla ME. Transcranial Doppler
monitoring compared with invasive monitoring of intra-
cranial pressure during acute intracranial hypertension.
J Clin Monit Comput 1999;15:185-195.
11. Richards HK, Czosnyka M, Whitehouse H, Pickard JD.
Increase in transcranial Doppler pulsatility index does not
indicate the lower limit of cerebral autoregulation. Acta
Neurochir Suppl 1998;71:229-232.
12. Hanlo PW, Gooskens RH, Nijhuis IJ, Faber JA, Peters RJ,
van Huffelen AC, et al. Value of transcranial Doppler in-
dices in predicting raised ICP in infantile hydrocephalus.
A study with review of the literature. Childs Nerv Syst
1995;11:595-603.
13. Bellner J, Romner B, Reinstrup P, Kristiansson KA, Ry-
ding E, Brandt L. Transcranial Doppler sonography pul-
satility index (PI) reects intracranial pressure (ICP). Surg
Neurol 2004;62:45-51; discussion 51.
14. Schmidt B, Klingelhofer J, Schwarze JJ, Sander D, Wittich
I. Noninvasive prediction of intracranial pressure curves
using transcranial Doppler ultrasonography and blood
pressure curves. Stroke 1997;28:2465-2472.
15. Schmidt EA, Czosnyka M, Gooskens I, Piechnik SK, Matta
BF, Whiteld PC, Pickard JD. Preliminary experience of
the estimation of cerebral perfusion pressure using trans-
cranial Doppler ultrasonography. J Neurol Neurosurg
Psychiatry 2001;70:198-204.
16. Schmidt B, Czosnyka M, Klingelhofer J. Clinical applica-
tions of a non-invasive ICP monitoring method [published
correction appears in Eur J Ultrasound 2003;16:265]. Eur
J Ultrasound 2002;16:37-45.
17. Schmidt B, Czosnyka M, Raabe A, Yahya H, Schwarze JJ,
Sackerer D, et al. Adaptive noninvasive assessment of
intracranial pressure and cerebral autoregulation. Stroke
2003;34:84-89.
18. Ursino M, Ter Minassian A, Lodi CA, Beydon L. Cerebral
hemodynamics during arterial and CO pressure changes:
in vivo prediction by a mathematical model. Am J Physiol
Heart Circ Physiol 2000;279:H2439H2455.
19. Buhre W, Heinzel FR, Grund S, Sonntag H, Weyland A.
Extrapolation to zero-ow pressure in cerebral arteries to
estimate intracranial pressure. Br J Anaesth 2003;90:
291-295.
20. Miao J, Benkeser PJ, Nichols FT. A computer-based sta-
tistical pattern recognition for Doppler spectral waveforms
of intracranial blood ow. Comput Biol Med 1996;26:53-
63.
21. Sidi A, Mahla ME. Noninvasive monitoring of cerebral per-
fusion by transcranial Doppler during fulminant hepatic
failure and liver transplantation. Anesth Analg 1995;80:
194-200.
22. Larsen FS, Pott F, Hansen BA, Ejlersen E, Knudsen GM,
Clemmesen JD, Secher NH. Transcranial Doppler sonog-
raphy may predict brain death in patients with fulminant
hepatic failure. Transplant Proc 1995;27:3510-3511.
23. Larsen FS, Hansen BA, Ejlersen E, Secher NH, Clem-
mesen JO, Tygstrup N, Knudsen GM. Cerebral blood
ow, oxygen metabolism and transcranial Doppler
sonography during high-volume plasmapheresis in ful-
minant hepatic failure. Eur J Gastroenterol Hepatol
1996;8:261-265.
24. Larsen FS, Strauss G, Moller K, Hansen BA. Regional
cerebral blood ow autoregulation in patients with fulmi-
nant hepatic failure. Liver Transpl 2000;6:795-800.
25. Larsen FS, Strauss G, Knudsen GM, Herzog TM, Hansen
BA, Secher NH. Cerebral perfusion, cardiac output, and
arterial pressure in patients with fulminant hepatic fail-
ure. Crit Care Med 2000;28:996-1000.
26. Strauss GI, Moller K, Holm S, Sperling B, Knudsen GM,
Larsen FS. Transcranial Doppler sonography and internal
jugular bulb saturation during hyperventilation in pa-
tients with fulminant hepatic failure. Liver Transpl 2001;
7:352-358.
27. Miller JD, Becker DP, Ward JD, Sullivan HG, Adams WE,
Rosner MJ. Signicance of intracranial hypertension in
severe head injury. J Neurosurg 1977;47:503-516.
1056 AGGARWAL ET AL.
28. Otis SM. Pitfalls in transcranial Doppler diagnosis. In:
Babikian VL, Wechsler LR, Eds. Transcranial Doppler Ul-
trasonography. St. Louis, MO: Mosby; 1993:39-50.
29. Chan KH, Miller JD, Dearden NM, Andrews PJ, Midgley S.
The effect of changes in cerebral perfusion pressure upon
middle cerebral artery blood ow velocity and jugular bulb
venous oxygen saturation after severe brain injury [see
comment]. J Neurosurg 1992;77:55-61.
30. Chan KH, Dearden NM, Miller JD, Andrews PJ, Midgley S.
Multimodality monitoring as a guide to treatment of intra-
cranial hypertension after severe brain injury. Neurosur-
gery 1993;32:547-552; discussion 552-543.
31. Ursino M, Giulioni M, Lodi CA. Relationships among ce-
rebral perfusion pressure, autoregulation, and transcra-
nial Doppler waveform: a modeling study. J Neurosurg
1998;89:255-266.
32. Newell DW. Transcranial Doppler measurements. New
Horiz 1995;3:423-430.
33. Bruner J. Handbook of Blood Pressure Monitoring. Little-
ton, MA: PSG Publishing; 1978.
NONINVASIVE MONITORING WITH TCD IN ALF 1057
Anda mungkin juga menyukai
- STR 0000000000000418Dokumen13 halamanSTR 0000000000000418Nelson Da VegaBelum ada peringkat
- Wa0002.Dokumen36 halamanWa0002.Alfonso GrajalesBelum ada peringkat
- Outcomes Following Tracheostomy 2023Dokumen10 halamanOutcomes Following Tracheostomy 2023ctsakalakisBelum ada peringkat
- ESC Guidelines Acute Coronary SyndromesDokumen107 halamanESC Guidelines Acute Coronary SyndromesSergio Mora CanelaBelum ada peringkat
- Perioperative Management of Anticoagulant andDokumen14 halamanPerioperative Management of Anticoagulant andIlija Kosić100% (2)
- ANCA - Associated Vasculitis 2022Dokumen18 halamanANCA - Associated Vasculitis 2022ctsakalakisBelum ada peringkat
- Cir 0000000000001168Dokumen111 halamanCir 0000000000001168sakomeBelum ada peringkat
- Pulmonary Hypertension 2023Dokumen24 halamanPulmonary Hypertension 2023ctsakalakisBelum ada peringkat
- ESICM Guidelines On ARDS 2023Dokumen33 halamanESICM Guidelines On ARDS 2023ctsakalakisBelum ada peringkat
- 2023 Therapeutic Plasma ExchangeDokumen18 halaman2023 Therapeutic Plasma ExchangeJesus PlanellesBelum ada peringkat
- ACLF Guidelines 2023Dokumen31 halamanACLF Guidelines 2023ctsakalakisBelum ada peringkat
- Kidney Stone 2023Dokumen18 halamanKidney Stone 2023ctsakalakisBelum ada peringkat
- Autoimmune Encephalitis With Antibodies 2023Dokumen14 halamanAutoimmune Encephalitis With Antibodies 2023ctsakalakisBelum ada peringkat
- 2023 Therapeutic Plasma ExchangeDokumen18 halaman2023 Therapeutic Plasma ExchangeJesus PlanellesBelum ada peringkat
- CBM guidelines for chronic painDokumen19 halamanCBM guidelines for chronic painToni TesfayBelum ada peringkat
- Aspiration Pneumonia Recommendations 2023Dokumen19 halamanAspiration Pneumonia Recommendations 2023ctsakalakisBelum ada peringkat
- ΕΘΝΙΚΟ ΣΥΝΤΑΓΟΛΟΓΙΟ 2007Dokumen739 halamanΕΘΝΙΚΟ ΣΥΝΤΑΓΟΛΟΓΙΟ 2007Aleksandros VasiliBelum ada peringkat
- Aspiration Pneumonia Recommendations 2023Dokumen19 halamanAspiration Pneumonia Recommendations 2023ctsakalakisBelum ada peringkat
- CBM guidelines for chronic painDokumen19 halamanCBM guidelines for chronic painToni TesfayBelum ada peringkat
- Autoimmune Encephalitis With Antibodies 2023Dokumen14 halamanAutoimmune Encephalitis With Antibodies 2023ctsakalakisBelum ada peringkat
- ACLF Guidelines 2023Dokumen31 halamanACLF Guidelines 2023ctsakalakisBelum ada peringkat
- Baclofen Overdose Mimicking Brain Death 2012Dokumen4 halamanBaclofen Overdose Mimicking Brain Death 2012ctsakalakisBelum ada peringkat
- BossDokumen2 halamanBossapi-3763038Belum ada peringkat
- Hepatocellular Carcinoma 2009Dokumen58 halamanHepatocellular Carcinoma 2009ctsakalakisBelum ada peringkat
- Brain Death Confirmation 2010Dokumen7 halamanBrain Death Confirmation 2010ctsakalakisBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Newly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManDokumen4 halamanNewly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManIJELS Research JournalBelum ada peringkat
- Film set safety rules for COVIDDokumen12 halamanFilm set safety rules for COVIDTanveer HossainBelum ada peringkat
- Cambridge IGCSE: 0450/11 Business StudiesDokumen12 halamanCambridge IGCSE: 0450/11 Business StudiesGodfreyFrankMwakalingaBelum ada peringkat
- A Strategic Management PaperDokumen7 halamanA Strategic Management PaperKarll Brendon SalubreBelum ada peringkat
- Analog Communication Interview Questions and AnswersDokumen34 halamanAnalog Communication Interview Questions and AnswerssarveshBelum ada peringkat
- 4PW16741-1 B EKBT - Bufftertank - Installation Manuals - EnglishDokumen6 halaman4PW16741-1 B EKBT - Bufftertank - Installation Manuals - EnglishBernard GaterBelum ada peringkat
- Unit 5 Vocabulary Basic 1 Match 1-10 With A-J To Make Innovations and InventionsDokumen6 halamanUnit 5 Vocabulary Basic 1 Match 1-10 With A-J To Make Innovations and InventionsCristina Garcia50% (2)
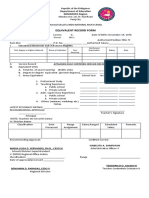
- Equivalent Record Form: Department of Education MIMAROPA RegionDokumen1 halamanEquivalent Record Form: Department of Education MIMAROPA RegionEnerita AllegoBelum ada peringkat
- Tiger Tales: From Colonial MalayaDokumen16 halamanTiger Tales: From Colonial MalayamatarsBelum ada peringkat
- Important instructions on judicial procedure from Narada SmritiDokumen6 halamanImportant instructions on judicial procedure from Narada SmritirohitBelum ada peringkat
- Law of The Limiting FactorsDokumen4 halamanLaw of The Limiting FactorsBiswajit DarbarBelum ada peringkat
- 3.5 Lonaphala S A3.99 PiyaDokumen9 halaman3.5 Lonaphala S A3.99 PiyaPiya_TanBelum ada peringkat
- User Manual: C43J890DK C43J892DK C49J890DK C49J892DKDokumen58 halamanUser Manual: C43J890DK C43J892DK C49J890DK C49J892DKGeorge FiruțăBelum ada peringkat
- Vikash Kumar: 1. Aunico India May 2018Dokumen4 halamanVikash Kumar: 1. Aunico India May 2018Rama Krishna PandaBelum ada peringkat
- Strategicmanagement Finalpaper 2ndtrisem 1819Dokumen25 halamanStrategicmanagement Finalpaper 2ndtrisem 1819Alyanna Parafina Uy100% (1)
- TG KPWKPDokumen8 halamanTG KPWKPDanmar CamilotBelum ada peringkat
- MarasiNews Issue 12Dokumen47 halamanMarasiNews Issue 12Sunil Kumar P GBelum ada peringkat
- Specification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VDokumen2 halamanSpecification: F.V/Tim e 3min 5min 8min 10MIN 15MIN 20MIN 30MIN 60MIN 90MIN 1.60V 1.67V 1.70V 1.75V 1.80V 1.85VJavierBelum ada peringkat
- The Seasons of Life by Jim RohnDokumen111 halamanThe Seasons of Life by Jim RohnChristine Mwaura97% (29)
- 236b3 Esquema Electrico Mini Cargador CatDokumen29 halaman236b3 Esquema Electrico Mini Cargador Cathenry laviera100% (2)
- Implementing a JITD system to reduce bullwhip effect and inventory costsDokumen7 halamanImplementing a JITD system to reduce bullwhip effect and inventory costsRaman GuptaBelum ada peringkat
- Plano Electrico 785CDokumen2 halamanPlano Electrico 785CLuis MartínezBelum ada peringkat
- Openstack Deployment Ops Guide PDFDokumen197 halamanOpenstack Deployment Ops Guide PDFBinank PatelBelum ada peringkat
- JNTUA Mechanical Engineering (R09) Syllabus BookDokumen147 halamanJNTUA Mechanical Engineering (R09) Syllabus Bookslv_prasaad0% (1)
- Delhi Police ResultDokumen26 halamanDelhi Police ResultExam Aspirant100% (1)
- Genigraphics Poster Template 36x48aDokumen1 halamanGenigraphics Poster Template 36x48aMenrie Elle ArabosBelum ada peringkat
- Catalogue PDFDokumen4 halamanCatalogue PDFShivam GuptaBelum ada peringkat
- ATLAS CYLINDER LUBRICATOR MANUALDokumen36 halamanATLAS CYLINDER LUBRICATOR MANUALKaleb Z king webBelum ada peringkat
- Rustia V Cfi BatangasDokumen2 halamanRustia V Cfi BatangasAllen GrajoBelum ada peringkat
- Land Equivalent Ratio, Growth, Yield and Yield Components Response of Mono-Cropped vs. Inter-Cropped Common Bean and Maize With and Without Compost ApplicationDokumen10 halamanLand Equivalent Ratio, Growth, Yield and Yield Components Response of Mono-Cropped vs. Inter-Cropped Common Bean and Maize With and Without Compost ApplicationsardinetaBelum ada peringkat