1-4 Hemostasis, Surgical Bleeding and Transfusion
Diunggah oleh
Robin Tolentino100%(3)100% menganggap dokumen ini bermanfaat (3 suara)
582 tayangan17 halamanThis document summarizes key aspects of hemostasis, including the four major physiologic events: vascular constriction, platelet plug formation, fibrin formation, and fibrinolysis. It describes the roles of platelets, coagulation factors, fibrin formation and degradation. Specifically, it notes that platelets form a hemostatic plug and contribute to thrombin formation, while the coagulation cascade involves a sequence of enzymatic reactions converting proenzymes to active enzymes to ultimately form a fibrin clot. Fibrinolysis then degrades the fibrin clot through plasmin.
Deskripsi Asli:
Filename: 1-4 Hemostasis, Surgical Bleeding and Transfusion.pdf
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniThis document summarizes key aspects of hemostasis, including the four major physiologic events: vascular constriction, platelet plug formation, fibrin formation, and fibrinolysis. It describes the roles of platelets, coagulation factors, fibrin formation and degradation. Specifically, it notes that platelets form a hemostatic plug and contribute to thrombin formation, while the coagulation cascade involves a sequence of enzymatic reactions converting proenzymes to active enzymes to ultimately form a fibrin clot. Fibrinolysis then degrades the fibrin clot through plasmin.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
100%(3)100% menganggap dokumen ini bermanfaat (3 suara)
582 tayangan17 halaman1-4 Hemostasis, Surgical Bleeding and Transfusion
Diunggah oleh
Robin TolentinoThis document summarizes key aspects of hemostasis, including the four major physiologic events: vascular constriction, platelet plug formation, fibrin formation, and fibrinolysis. It describes the roles of platelets, coagulation factors, fibrin formation and degradation. Specifically, it notes that platelets form a hemostatic plug and contribute to thrombin formation, while the coagulation cascade involves a sequence of enzymatic reactions converting proenzymes to active enzymes to ultimately form a fibrin clot. Fibrinolysis then degrades the fibrin clot through plasmin.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 17
1 of 17
NAMES NG TRANS PEOPLE
Surgery
Hemostasis, Surgical Bleeding, and
Transfusion
DR. Bibera
July 5, 2012 1-4
a complex process whose function is to limit blood loss
from an injured vessel
4 major physiologic events
o vascular constriction
o platelet plug formation
o fibrin formation
o fibrinolysis
Vascular Constriction
is the initial response to vessel injury, more
pronounced in vessels with medial smooth muscles
dependent on local contraction of smooth muscle
subsequently linked to platelet plug formation
potent vasoconstrictors:
o Thromboxane A2 (TXA2) is produced locally at
the site of injury via the release of arachidonic acid
from platelet membranes
o Endothelinsynthesized by injured endothelium
and serotonin (5-hydroxytryptamine) released
during platelet aggregation
o Bradykinin and Fibrinopeptides
the extent of vasoconstriction varies with the degree of
vessel injury
Platelet Function
platelets are anucleate fragments of megakaryocytes,
normal circulating number of platelets ranges between
150,000 and 400,000/ L
up to 30% may be sequestered in the spleen
if not consumed in a clotting reaction, platelets are
normally removed by the spleen and have an average
life span of 7 to 10 days
platelets play an integral role in hemostasis by forming
a hemostatic plug and by contributing to thrombin
formation
injury to the intimal layer in the vascular wall exposes
subendothelial collagen to which platelets adhere,
which requires von Willebrand's factor (vWF)
binds to glycoprotein I/IX/V on the platelet
membrane
after adhesion, platelets initiate a release reaction that
recruits other platelets from the circulating blood to
seal the disrupted vessel. Up to this point, this process
is known as primary hemostasis
platelet aggregation is reversible and is not associated
with secretion
o heparin does not interfere with this reaction
o adenosine diphosphate (ADP) and serotonin are
the principal mediators in platelet aggregation
arachidonic acid released converted by COX to
prostaglandin G2 (PGG2) prostaglandin H2 (PGH2)
converted to TXA2
effects:Arachidonic acid shuttled to adjacent
endothelial cells converted to prostacyclin (PGI2 )
vasodilation and acts to inhibit platelet aggregation
platelet COX is
o irreversibly inhibited by aspirin
o reversibly blocked by NSAIDs
o but is not affected by COX-2 inhibitor
in the second wave of platelet aggregation, a release
reaction occurs in which several substances, including
ADP, Ca2+,serotonin, TXA2, and -granule proteins are
discharged
fibrinogen is a required cofactor, acting as a bridge
for the glycoprotein IIb/IIIa receptor on the activated
platelets
its release causes compaction of the plateletsinto a
plug, a process that is irreversible
thrombospondin, secreted by the granule, stabilizes
fibrinogen binding to the activated platelet surface and
strengthens the platelet-platelet interactions.
platelet factor 4 (PF4), potent heparin antagonist,
and thromboglobulin also are secreted during the
release reaction
the second wave of platelet aggregation is inhibited by
aspirin and NSAIDs, by (cAMP), and by nitric oxide
alterations occur in the phospholipids of the platelet
membrane that allow Ca2+ and clotting factors bind
to the platelet surface enzymatically active
complexes
BIOLOGY OF HOMEOSTASIS
2 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
o the altered lipoprotein surface (sometimes referred
to as platelet factor 3) catalyzes reactions that are
involved in:
- conversion of prothrombin to thrombin by
activated factor X (Xa) in the presence of factor
V and Ca2+
- is also involved in the reaction by which
activated factor IX (IXa), factor VIII, and Ca2+
activate factor X
Coagulation
the coagulation cascade has 2 intersecting pathways:
o Intrinsic pathway
- begins with factor XII and through a cascade of
reactions activates factors XI, IX, and VII in
sequence fibrin clot formation, intrinsic to the
circulating plasma and no surface is required to
initiate the process
o Extrinsic pathway
- requires exposure of tissue factor on the surface
of the injured vessel wall to initiate the cascade
beginning with factor VII
the two arms of the coagulation cascade merge to a
common pathway at factor X
activation sequence of factors II (prothrombin) and I
(fibrinogen)
clot formation occurs after proteolytic conversion of
fibrinogen to fibrin
an elevated activated partial thromboplastin
time(aPTT) abnormal function Intrinsic pathway
an elevated prothrombin time (PT) abnormal
extrinsic pathway
vitamin K deficiency and warfarin use affect factors II,
VII, IX, and X
fibrinogen levels of <50 mg/dL causes prolongation of
the PT and aPTT
primary pathway for coagulation is initiated by
theexposure of subendothelial tissue factor when
vessel surface is injured
propagation of the clotting reaction then ensues with a
sequence of enzymatic reactions, which involves a
proteolytic enzyme
cleavage of a proenzyme and a phospholipid surface
generates the next enzyme in a cascade manner
o each reaction requires a helper protein (i.e.
Factor VIIa binds to tissue factor, and tissue
factor-VIIa complex catalyzes the activation of
factor X to factor Xa)
o the reaction takes place on the phospholipid
surface of activated platelets
o this complex is four orders of magnitude more
active at converting factor X than is factor VIIa
alone and also activates factor IX to factor IXa
o factor Xa, together with factor Va and Ca2+ and
phospholipid, comprises the prothrombinase
complex that converts prothrombin to thrombin
o thrombin has multiple functions in the clotting
process, including conversion of fibrinogen to fibrin
and activation of factors V, VII, VIII, XI,and
XIII, as well as activation of platelets
o factor VIIIa combines with factor IXa to form the
intrinsic factor complex (VIIIa-IXa), which is
responsible for the bulk of the conversion of factor
X to Xa50x more effective at catalyzing factor X
activation than is extrinsic (tissue factor-VIIa)
complex, five to six orders of magnitude more
effective than is factor IXa alone
o the prothrombinase is significantly more effective
at catalyzing its substrate than is factor Xa alone
o once formed, thrombin leaves the membrane
surface converts fibrinogen by two cleavage
steps into fibrin and 2 small peptides termed
fibrinopeptides A and B
o removal of fibrinopeptide A permits end-to-end
polymerization of the fibrin
o cleavage of fibrinopeptide B allows side-to-side
polymerization of the fibrin clot, facilitated by
thrombin-activatable fibrinolysis inhibitor(TAFI)
the coagulation system is exquisitely regulated.
Feedback inhibition on the coagulation cascade
deactivates the enzyme complexes leading to thrombin
formation
exists at upstream, intermediate, and downstream
portions of the coagulation cascade to "turn off"
thrombin formation once the procoagulantsequence is
initially activated
Coagulation Factors Tested
by the PT and the aPTT
PT aPTT
VII XII
X High molecular weight
kininogen
V Prekallikrein
II (prothrombin) XI
Fibrinogen
IX
VIII
X
V
II
Fibrinogen
Based on 3 mechanisms:
o mechanisms of fibrinolysis allow for breakdown of
the fibrin clot and subsequent repair of vessel with
deposition of connective tissue
o tissue factor pathway inhibitor (TFPI) blocks
the extrinsic tissue factorVIIa complex
eliminating this production of factors Xa and IXa
- Antithrombin III effectively neutralizes all of
the procoagulant serine proteases and weakly
inhibits the tissue factorVIIa complex
o mechanism of inhibition of thrombin formation is
the protein C system
- thrombin binds to thrombomodulin and activates
protein C to activated protein C (APC), which
then forms a complex with its cofactor, protein
S, on a phospholipid surface
cleaves factors Va and VIIIa
no longer able to participate in the formation of
tissue factorVIIa or prothrombinasecomplexe
- also activates TAFI, which removes the terminal
lysine on the fibrin molecule clot more
susceptible to lysis by plasmin
3 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
- factor V Leide, gene mutation, that is resistant to
cleavage by APC predisposed to venous
thromboembolic events
degradation of fibrin clot is accomplished by plasmin, a
serine protease derived from the proenzyme
plasminogen
tissue plasminogen activator (tPA) is made by the
endothelium and is the main circulating form of this
family of enzymes
o is selective for fibrin-bound plasminogen so that
endogenous fibrinolytic activity occurs
predominately at the site of clot
o urokinase plasminogen activator (uPA), also
produced by endothelial cells, as well as by
urothelium, is not selective for fibrin-bound
plasminogen
Fibrinolysis
fibrin clot undergoes clot lysis, which permits
restoration of blood flow
fibrinolysis is initiated at the same time as the clotting
mechanismunder the influence of circulating kinases,
tissue activators, and kallikrein
plasmin- main enzyme degrades the fibrin mesh at
various places
plasminogen may be converted by one of several
plasminogen activators, including tPA and uPA
bradykinin, a potent endothelium-dependent
vasodilator cleaved from high molecular weight
kininogen by kallikrein, causes contraction of
nonvascular smooth muscle, increases vascular
permeability, and enhances release of tPA
plasminogen activation may be initiated by activation
of factor XII
the tPA activates plasminogen more efficiently when it
is bound to fibrin, so that plasmin is formed selectively
on the clot
o plasmin is inhibited by 2-antiplasmin, a protein
that is cross-linked to fibrin by factor XIII, which
helps to ensure that clot lysis does not occur too
quickly
o any circulating plasmin also is inhibited by 2-
antiplasmin and circulating tPA or urokinase
clot lysis yields fibrin degradation products, including
E-nodules and D-dimers
o the smaller fragments interfere with normal
platelet aggregation and the larger fragments may
be incorporated into the clot in lieu of normal fibrin
monomers unstable clot.
o D-dimers in the circulationmarker of thrombosis
or other conditions in which a significant activation
of the fibrinolytic system is present
Most frequent inherited factor deficiencies
factor VIII deficiency (hemophilia A and von
Willebrand's disease)
factor IX deficiency (hemophilia B or Christmas
disease)
factor XI deficiency
Factor VIII And Factor IX Hemophilia
sex-linked recessive disorders
Severity of both hemophilia A and hemophilia B
depends on the level of factor VIII or factor IX in the
patient's plasma
Disease factor levels:
<1% normal: Severe Disease
1 - 5%: moderately severe disease
5 - 30%: mild disease
MANIFESTATIONS:
Intracranial bleeding, retropharyngeal bleeding, and
bleeding from the tongue or lingual frenulum may be
life-threatening
Moderately severe hemophilia: less spontaneous
bleeding but are likely to bleed severely after trauma
or surgery
Retroperitoneal hematomas
Mild hemophiliacs: do not bleed spontaneously and
have mild bleeding after major trauma or surgery
May not bleed immediately after an injury or minor
surgery but will begin to bleed several hours later
because of normal platelet function
TREATMENT:
Factor VIII (hemo A) or factor IX (hemo B) concentrate
Recombinant factor VIII recommended for HIV and
hepa C virus (HCV)-seronegative
For factor IX replacement :recommended tx are
recombinant or high purity factor IX
Intermediate purity factor IX (prothrombin complex)
concentrates (not use: risk of thrombosis)
1-deamino-D-argininevasopressin (DDAVP,
desmopressin): induces the release of vWF from
endothelial cells, raising the levels of vWF and
associated factor VIII
CONGENITAL FACTOR DEFICIENCIES
4 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Aminocaproic acid (Amicar): inhibitor of fibrinolysis,
useful adjunct to factor VIII or IX or DDAVP especially
for oral and urinary tract bleeding
Patients with high titer inhibitors is not possible to
achieve adequate factor VIII levels with factor VIII
preparations
Alternatives:
Porcine factor VIII
Prothrombin complex concentrates
Recombinant factor VIIa (most effective, given every 2
hrs, expensive)
Von Willebrands Disease
Disorder with low factor VIII
Autosomal dominant disorder
Primary defect: low level of the vWF, a large
glycoprotein with two functions
1. Serve as a carrier for factor VIII
2. Necessary for normal platelet adhesion and
normal aggregation under high shear conditions
Three types:
a) Type I (partial quantitative deficiency)
b) Type II (qualitative defect)
c) Type III (total deficiency)
MANIFESTATIONS:
Menorrhagia is common in women with vWD
Easy bruising and mucosal bleeding (platelet disorder)
TREATMENT:
Intermediate purity factor VIII concentrates (Humate-
P: contains vWF and factor VIII)
DDAVP: raises endogenous vWF levels by release of
the factor from endothelial cells
- EACA (Amicar) is a useful adjunct
In general, type I patients respond well to DDAVP,
type II patients may respond, depending on the
particular defect and type III patients usually do not
respond.
Factor XI Deficiency
Hemophilia C
Prevalent in the Ashkenazi Jewish population
(heterozygote frequency about 1:8)
Mild bleeding disorder, autosomal recessive trait
MANIFESTATIONS:
Spontaneous bleeding is rare, but may occur after
surgery or trauma
TREATMENT:
Fresh-frozen plasma (FFP) infusion
Factor XI concentrates
DDAVP: useful in prevention of surgical bleeding
Deficiencies Of Factors II (Prothrombin), V & X
Rare inherited deficiencies
autosomal recessive traits
Significant bleeding in homozygotes with <1% of
normal activity
Half-life of prothrombin (factor II) is approximately 72
hours
Half-life of factor X is approximately 48 hours
Factor V deficiency may be coinherited with factor VIII
deficiency
TREATMENT:
FFP. Contains 1 unit of activity of each (factors X and
II) per milliliter. However, factor V activity is
decreased because of its inherent instability.
Half-life of factor II is long (approximately 72 hours)
and only 25% of the normal level is needed for
hemostasis, single infusion of FFP is sufficient.
Prothrombin complex concentrates can be used to
treat deficiencies of prothrombin or factor X.
Treatment of bleeding in combined deficiency (factor V
and factor VIII deficiency) requires factor VIII
concentrate and FFP.
Some factor V deficient pt also lacks factor V normally
present in platelets and may need platelet transfusions
as well as FFP
Factor VII Deficiency
Rare disorder
Bleeding is uncommon unless the level is less than 3%
TREATMENT:
FFP or with recombinant factor VIIa
Half-life of recombinant factor VIIa is approximately 2
hours
Half-life of factor VII in FFP is approximately 4 hours
Factor XIII Deficiency
Rare, autosomal recessive trait
MANIFESTATIONS:
Bleeding is delayed because clots form normally but
are susceptible to fibrinolysis
Umbilical stump bleeding
high risk of intracranial bleeding
Spontaneous abortion is usual in women unless they
receive replacement therapy
Half-life of factor XIII is approximately 9 to 14 days
TREATMENT:
Replacement with FFP, cryoprecipitate, or a factor XIII
concentrate
Levels of 1 - 2% : adequate for hemostasis
Inherited Defects
Rare defects
Abnormalities of platelet surface proteins, platelet
granules, and enzyme defects
Major surface protein abnormalities are
thrombasthenia and Bernard-Soulier syndrome
THROMBASTHENIA (GLANZMANN'S DISEASE)
Caused by an absence of functional glycoprotein IIb
IIIa, the receptor for fibrinogen and also a receptor for
vWF
Because platelets must bind fibrinogen or vWF to
expose the ADP receptor so they can bind ADP and
PLATELET FUNCTIONAL DEFECTS
5 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
aggregate, platelets of thrombasthenic patients do not
aggregate
Treatment: platelet transfusions
BERNARD-SOULIER SYNDROME
Caused by a defect in the GP Ib/IX/V receptor for vWF
-necessary for platelet adhesion
Treatment: Platelet transfusion
STORAGE POOL DISEASE
Most common intrinsic platelet defect
May involve loss of dense granules (storage sites for
ADP, ATP, Ca2+, and inorganic phosphate) and
granules
DENSE GRANULE DEFICIENCY
Most prevalent
May be an isolated defect or occur with partial albinism
in the Hermansky-Pudlak syndrome
Bleeding is variable depending on how severe the
granule defect is
Bleeding is primarily caused by the decreased release
of ADP from these platelets
GRAY PLATELET SYNDROME
Isolated defect of the -granules
Bleeding is usually mild
dense and -granules: more severe bleeding disorder
o Treatment:
DDAVP
platelet transfusion: severe bleeding
Other intrinsic platelet defects:
Deficiency of cyclooxygenase
Abnormalities in platelet actin, myosin, cytoskeletal
proteins, and enzymes involved in various aspects of
platelet metabolism
Treatment:
DDAVP- mild bleeding
Platelet transfusion
Quantitative Platelet Defects
Inherited Thrombocytopenia
Rare
Treatment: platelet transfusion, if significant
Platelet Abnormalities
a. Quantitative
Due to failure of production
o as in bone marrow disorders (cuased by leukemia,
myelodysplastic syndrome, severe vitaminB12 or folate
deficiency, chemotherapeutic drug use, radiation
therapy, acute ethanol intoxication, or viral infection)
Shortened survival
Sequestration
b. Qualitative
With indicated treatment, due to symptoms or the
need for an invasive procedure
platelet transfusion is used
Etiology of Platelet Disorders
A. Quantitative disorders
1. Failure of production: related to impairment of
bone marrow function
a. Leukemia
b. Myeloproliferative disorders
c. Vitamin B12 or Folate deficiency
d. Chemotherapy or radiation therapy
e. Acute alcohol intoxication
f. Viral infections
2. Decreased survival
a. Immune-mediated disorders
o Idiopathic thrombocytopenia
o Heparin-induced thrombocytopenia
o Autoimmune disorders or B-cell
malignancies
o Secondary thrombocytopenia
b. Disseminated intravascular coagulation
c. Disorders related to platelet thrombi
o Thrombocytopenic purpura
o Hemolytic uremic syndrome
3. Sequestration
a. Portal hypertension
b. Sarcoid
c. Lymphoma
d. Gaucher's disease
A. Qualitative disorders
1. Massive transfusion
2. Therapeutic administration of platelet inhibitors
3. Disease states
a. Myeloproliferative disorders
b. Monoclonal gammopathies
c. Liver disease
QUANTITATIVE DEFECTS
marrow related diseases (leukemia or myelodysplasia,
vitamin B
12
or folate deficiencies, chemotherapy or
radiation therapy, acute alcohol intoxication, or viral
illnesses ) affects bone marrow production
Shortened platelet survival in immune
thrombocytopenia
o may be idiopathic
o associated with other autoimmune disorders or low-
grade B-cell malignancies disseminated intravascular
coagulation
o secondary to viral infections (HIV infection) or use of
drugs and disorders (thrombotic thrombocytopenic
purpura and hemolytic uremic syndrome)
Secondary immune thrombocytopenia
o very low platelet count
o with petechiae and purpura
o with epistaxis
o initial treatment
corticosteroids
IV gamma globulin
anti-D immunoglobulin in patients who are Rh-
positive
Gamma globulin and anti-D immunoglobulin
rapid onset
Survival of transfused platelets
o Short
ACQUIRED HEMOSTATIC DEFECTS
6 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Primary Immune Thrombocytopenia
known as idiopathic thrombocytopenic
purpura(ITP)
o In children
o acute and short lived
o typically follows a viral illness
In adults
o gradual in onset
o chronic
o no identifiable cause
Circulating platelets: young functional
Bleeding
o less for a given platelet count than when there is
failure of platelet production
Pathophysiology
o involve both impaired platelet production and T cell
mediated platelet destruction
Drug-Induced Immune Thrombocytopenia
Treatment
o Withdrawal of the offending drug
Hastens recovery
o Corticosteroids
o Gamma globulin
o Anti-D immunoglobulin
Management of Idiopathic Thrombocytopenic
Purpura (ITP) in Adults
First Line:
a. Corticosteroids: The majority of patients respond,
but only a few long term.
b. IV immunoglobulin: Indicated with clinical bleeding,
along with platelet transfusion, and when condition is
steroid unresponsive. Response is rapid but transient.
c. Anti-D immunoglobulin: Active only in Rh-positive
patients before splenectomy. Response is transient
Second Line:
a. SPLENECTOMY: Open or laparoscopic. Criteria
include severe thrombocytopenia, high risk of
bleeding, and continued need for steroids.
Treatment failure may be due to retained
accessory splenic tissue.
Third Line:
a. Patients for whom firstand second-line therapies
fail are considered to have chronic ITP. The
objective in this subset of patients is to maintain
the platelet count >2030 x 109/L and to
minimize side effects of medications.
b. Rituximab, an anti-CD20 monoclonal antibody:
Acts by eliminating B cells.
c. Alternative medications producing mixed results
and a limited response: Danazol, cyclosporine A,
dapsone, azathioprine, and vinca alkaloids.
Thrombopoietic agents: A new class of drugs for
patients with impaired production of platelets rather than
accelerated destruction of platelets. Second-generation
drugs still in clinical trials include AMG531 and
eltrombopag.
Heparin-Induced Thrombocytopenia (HIT)
form of drug-induced immune thrombocytopenia
immunologic disorder
o antibodies against PF4 affect platelet activation and
endothelial function with resultant thrombocytopenia
and intravascular thrombosis
platelet count
o fall 5 to 7 days after heparin has been started
re-exposure
o decrease in count may occur within 1 to 2 days
should be suspected if the platelet count falls to
<100,000/L or drops by 50% from baseline in a
patient receiving heparinmore common with full-dose
unfractionated heparin (1 to 3%)
occur with prophylactic doses or with low molecular
weight heparins
approximately17% of patients receiving unfractionated
heparin and 8% of those receiving low molecular
weight heparin
o develop antibodies against PF4
with high incidence of thrombosis
may be arterial or venous
absence of thrombocytopenia in these patients
o does not preclude the diagnosis of HIT
Diagnosis of HIT
uses either a serotonin release assay or enzyme-linked
immunosorbent assay (ELISA)
o serotonin release assay
o highly specific but not sensitive
o ELISA has a low specificity
o negative ELISA result
essentially rules out HIT
Initial treatment of HIT
o Goal
to stop heparin
start with alternative anticoagulant
Alternative anticoagulants are primarily thrombin
inhibitors
o Lepirudin
o Argatroban
o Bivalirudin
o In Canada and Europe, danaparoid also is available
Danaparoid
heparinoid that has approximately 20% cross reactivity
with HIT antibodies (vivo < vitro)
Thrombotic Thrombocytopenic Purpura (TTP)
large vWF molecules interact with plateletsactivation
inhibition of metalloproteinase enzyme (ADAMTS13)
characterized by
thrombocytopenia
microangiopathic hemolytic anemia
fever
renal and neurologic signs or symptoms
finding of schistocytes on a peripheral blood smear
aids in the diagnosis
most effective treatment for TTP
o plasmapheresis
RITUXIMAB
Monoclonal antibody against the CD20 protein on B
lymphocytes
Immunomodulatory therapy against acquired TTP
(majority:autoimmune mediated)
Hemolytic Uremic Syndrome (HUS)
often occurs secondary to infection
o Escherichia coli 0157:H7
o other Shiga toxin producing bacteria
metalloproteinase
o normal
usually is associated with some degree of renal failure
7 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
many patients requiring renal replacement therapy
less frequent neurologic symptoms
TTP and HUS developed by patients w/
Autoimmune diseases (SLE)
HIV infection
in association with certain drugs (such as ticlopidine,
mitomycin C, gemcitabin
Associated with immunosuppressive agents (such as
cyclosporine and tacrolimus)
Sequestration
important cause of thrombocytopenia
sequestration of platelets in an enlarged spleen
(related to portal hypertension, sarcoid, lymphoma, or
Gaucher's disease)
In patients with hypersplenism:
they have normal total body platelet mass
larger fraction of the platelets are in the enlarged
spleen
Platelet survival: mildly decreased
Bleeding is less than anticipated from the count
Platelet transfusion does not increase the platelet
count as much as it would in a normal person
o because transfused platelets are similarly
sequestered in the spleen
Splenectomy
do not correct the thrombocytopenia of hypersplenism
caused by portal hypertension
QUALITATIVE PLATELET DEFECTS
Thrombocytopenia
most common abnormality of hemostasis bleeding in
the surgical patient
reduced platelet count due to a variety of disease
processes
marrow usually demonstrates a normal or increased
number of megakaryocytes also occurs in surgical
patients as a result of massive blood loss and
replacement with product deficient in platelets
induced by
o heparin administration (in cardiac and vascular
disorders)
In patients with leukemia or uremia and receiving
cytotoxic therapy
o reduced number of megakaryocytes in the
marrow
In patient for whom an elective operation is being
considered
o management is contingent on the extent
and cause of platelet reduction
o count of >50,000/ L generally requires no
specific therapy
In patients whose thrombocytopenia is refractory to
standard platelet transfusion
o use of human leukocyte antigen (HLA)
compatible platelets coupled with special
processors has proved effective
Platelets
administered preoperatively
o to increase the platelet count in surgical
patients with underlying thrombocytopenia
One unit of platelet concentrate
o with approx. 5.5 x
10
platelets
o increase the circulating platelet count by
approximately 10,000/ L in the average 70-
kg person
Impaired function
o accompanies thrombocytopenia
Decreased effectiveness of platelet transfusion
Fever
Infection
Hepatosplenomegaly
Presence of antiplatelet alloantibodies
o decrease the effectiveness of platelet
transfusions
Impaired ADP-stimulated aggregation
occurs with massive transfusion (>10 units of packed
red blood cells)
Uremia
may be associated with increased bleeding time and
impaired aggregation
can be corrected by hemodialysis or peritoneal dialysis
Defective aggregation and platelet secretion
In patients with
o thrombocythemia
o polycythemia vera
o myelofibrosis
Drugs that interfere with platelet function by design
Aspirin
o through irreversible acetylation of platelet
prostaglandin synthase
Clopidogrel
o Both aspirin and clopidogrel irreversibly inhibit platelet
function, clopidogrel through selective irreversible
inhibition of ADP-induced platelet aggregation
Dipyridamole
Glycoprotein IIB/IIIA Inhibitors
For each drugs (mentioned above)
o a period of approximately 7 days is required
from the time the drug is stopped until an
elective procedure can be performed
Other disorders associated with abnormal platelet
function
Uremia
Myeloproliferative Disorders
o intrinsic to the platelets
o usually improves if the platelet count can be reduced
to normal with chemotherapy
surgery should be delayed until the count has
been decreased
These patients are at risk for both bleeding and
thrombosis
Monoclonal Gammopathies
o result of interaction of the monoclonal protein with
platelets
o treatment with chemotherapy, or occasionally
plasmapheresis
to lower the amount of monoclonal protein
Liver Disease
8 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Administration of desmopressin acetate/ dialysis
o corrects platelet dysfunction in surgical patients
Acquired Hypofibrinogenemia
Disseminated Intravascular Coagulation (DIC)
Characterized by the intravascular activation of
coagulation with the loss of localization arising from
different causes. It can originate from and cause
damage to the microvasculature, , can produce organ
dysfunction
o Additional causes
o Malignancy
o Organ injury (such as severe pancreatitis)
o Liver failure
o Certain vascular abnormalities (such as large
aneurysms)
o Snakebites
o Illicit drugs
o Transfusion reactions
o Transplant rejection
o Sepsis
o Accompanies sepsis and may be associated with
multiple organ failure
o Diagnosis
o inciting cause with associated thrombocytopenia
o prolongation of the PT
o low fibrinogen level
o elevated levels of fibrin markers (fibrin degradation
products, D-dimer, soluble fibrin monomers)
facets of treatment
o relieving the patient's causative primary medical or
surgical problem
o maintaining adequate perfusion
heparin therapy has been proposed
Specific injuries (ofDIC)
o central nervous system injuries with embolization
of brain matter
o fractures with embolization of bone marrow
o amniotic fluid embolization
Excessive Thrombin Generation
leads to microthrombus formationconsumption and
depletion of coagulation factors and platelets classic
picture of diffuse bleeding
Primary Fibrinolysis
caused by acquired hypofibrinogenic state in the
surgical patient
occur in patients after prostate resection when
urokinase is released during surgical manipulation of
the prostate or in patients undergoing extracorporeal
bypass
Fibrinolytic bleeding
o dependent on the concentration of breakdown products
in the circulation
Synthetic amino acid-aminocaproic acid
o interferes with fibrinolysis by inhibiting plasminogen
activation
Myeloproliferative Diseases
Polycythemia - particularly with marked
thrombocytosis
o presents a major surgical risk
Operations are considered only for the most grave
surgical emergencies
Defer operation until medical management has
restored normal blood volume, hematocrit level, and
platelet count
Spontaneous thrombosis
o complication of polycythemia vera
o explained in part by increased blood viscosity
o increased platelet count
o increased tendency toward stasis
Myeloid metaplasia
o frequently represents part of the natural history of
polycythemia vera
o Approximately 50% of patients with myeloid
metaplasia are postpolycythemic
Thrombocytosis
o reduced by the administration of hydroxyurea or
anagrelide
o Elective surgical procedures should be delayed until
the institution of appropriate treatment
o hematocrit level is kept below 48% and platelet count
under 400,000/ L
o In emergency procedure
phlebotomy and blood replacement with lactated
Ringer's solution may be beneficial
Coagulopathy of Liver Disease
Liver
Plays a key role in hemostasis
o responsible for the synthesis of many of the
coagulation factors
Most common coagulation abnormalities associated
with liver dysfunction:
o thrombocytopenia
o impaired humoral coagulation function
manifested as prolongation of the PT
o increase in the International Normalized
Ratio (INR)
Thrombocytopenia in Patients with Liver Disease
typically related to hypersplenism
reduced production of thrombopoietin
immune-mediated destruction of platelets
Immune-mediated thrombocytopenia
o may also occur in cirrhotic patients (w/ hepatitis C and
primary biliary cirrhosis)
Ameliorate thrombocytopenia
o before therapy, the actual need for correction should
be strongly considered
o In general, correction based solely on a low platelet
count should be discouraged
Patients with Hypersplenism
the total body platelet mass is basically normal
abnormally high proportion of the platelets
Less bleeding is seen than would be anticipated from
the platelet count because some of the sequestered
platelets can be released into the circulation
Splenectomy
o less well accepted option is splenectomy or splenic
embolization
reduce hypersplenism
reduced splenic blood flow
reduce portal vein flow with subsequent portal vein
thrombosis
Results are mixed after transjugular intrahepatic
portosystemic shunt (TIPS)
9 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
o treatment of thrombocytopenia should not be the
primary indication for a TIPS procedure
Thrombopoietin
primary stimulus for thrombopoiesis
responsible for some cases of thrombocytopenia in
cirrhotic patients
o should be withheld for invasive procedures and surgery
Platelet transfusions
mainstay of therapy
effect typically lasts only several hours
Administration of Il-11
potential alternative
stimulates proliferation of hematopoietic stem cells and
megakaryocyte progenitors
Most studies using interleukin-11 have been in patients
with cancer
Significant side effects limit its usefulness
Decreased production or increased destruction of
coagulation factors and vitamin K deficiency
contribute to a prolonged PT
increased INR in patients with liver disease
Correction of Coagulopathy
reserved for treatment of active bleeding and
prophylaxis for invasive procedures and surgery
w/ liver disease, treated with FFP
Complete correction is not possible
Fibrinogen level is <100 mg/dL
Administration of cryoprecipitate may be helpful
Cryoprecipitate
o source of factor VIII for the rare patient with a low
factor VIII level
Coagulopathy of Trauma
Causes
o Acidosis
o Hypothermia
o Dilution of coagulation factors
Only patients in shock arrive coagulopathic and that it
is the shock that induces coagulopathy through
systemic activation of anticoagulant and fibrinolytic
pathways
hypoperfusion
o causes activation of thrombomodulin on the surface of
endothelial cells
Circulating thrombin
complexes with thrombomodulin.
induces an anticoagulant state through activation of
protein C
enhances fibrinolysis by deinhibition of tPA through the
consumption of plasminogen activator inhibitor 1
Acquired Coagulation Inhibition
Antiphospholipid Syndrome (APLS)
most common acquired disorder of coagulation
inhibition
lupus anticoagulant and anticardiolipin antibodies are
present
these antibodies are associated with either arterial or
venous thrombosis
APLS is very common in patients with systemic lupus
erythematosus (SLE), and associated with rheumatoid
arthritis and Sjrgens Syndrome
Hallmark is prolonged aPTT in vitro but an increased
risk of thrombosis in vivo
Other Diseases
Paraprotein Disorders
production of abnormal globulin or fibrinogen that
interferes with clotting or platelet function
IgM Waldenstrm's
macroglobulinemia
IgG or IgA multiple myeloma
Cryoglobulin or
cryofibrinogen
liver disease (especially
hepatitis C) or autoimmune
diseases
Treatment:
Chemotherapy -effective in lowering the
paraproteins of macroglobulinemia and
myeloma,
Plasmapheresis- usually removes Cryoglobulins
and cryofibrinogens
Hypersplenism
associated with platelet sequestration and
platelet survival is mildly decreased
total body platelet mass essentially normal, but a
much larger fraction of the platelets than normal
are in the enlarged spleen
Bleeding is less anticipated because
sequestered platelets can be mobilized and enter
the circulation
Platelet transfusion not helpful will end up in
spleen
ACQUIRED HEMOSTATIC DEFECTS
Spontaneous bleeding - complication of
anticoagulant therapy with:
o low molecular weight heparins
o factor Xa inhibitors
To reduce bleeding with continuous infusion of
heparin:
o aPTT must be regulated between 1.5
and 2.5 times the upper limit of normal
Therapeutic anticoagulation is more reliably
achieved with low molecular weight heparin
o laboratory testing is not routinely used to
monitor dosing of these agents
An exaggerated response to oral anticoagulants
may occur if dietary vitamin K is inadequate.
Anticoagulant effect of the warfarin is reduced in
patients receiving barbiturates, contraceptives,
other estrogen-containing compounds,
corticosteroids, ACTH
o Reduced anticoagulant dosage should be
instituted after discontinuance of any of
these drugs.
Medications known to increase the effect of oral
anticoagulants
o Phenylbutazone
o Clofibrate (cholesterol-lowering agent)
o a variety of antibiotics (particularly the
Cephalosporins)
o Anabolic steroids (norethandrolone)
o Amiodarone
o Glucagons
o L-thyroxine
o Quinidine
Onset of hematuria or melena in the patient
receiving anticoagulants should be investigated
may unmask underlying tumors.
o PE reveals other signs of bleeding, such
as ecchymoses, petechiae, or
hematoma
ANTICOAGULATION AND BLEEDING
10 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
CNS and eye surgeries minor bleeding poses a
great problem: anticoagulants should be
discontinued, and, if necessary, reversed
Rebound phenomenon risk of thrombotic
complications is increased when anticoagulation
therapy is discontinued suddenly
When the aPTT is <1.3 times control in a
heparinized patient, or when the INR is<1.5 in a
patient on warfarin, meticulous surgical
technique is mandatory
Certain surgical procedures should not be
performed in the face of anticoagulation;
Procedures requiring blind needle introduction
should be avoided
Management:
Discontinuation of heparin may be
sufficient if the operation can be delayed for
several hours
For more rapid reversal 1 mg of protamine
sulfate for every 100 units of heparin most
recently administered
The reversal of warfarin may take several hours;
more rapid reversal can be accomplished with
fresh-frozen plasma or prothrombin
complex concentrate (Konyne or Proplex)
Parenteral administration of vitamin K
indicated in elective surgical treatment of
patients with biliary obstruction or malabsorption
Excessive Bleeding Associated With
Cardiopulmonary Bypass
Triggering factors:
o excessive fibrinolysis
o abnormal platelet functions
Laboratory evaluation tests may include:
o INR, aPTT, CBC, platelet count,
peripheral blood smear examination and
measurement of fibrin degradation
products
Treatment may include:
o Administration of platelets
o Protamine
o - aminocaproic acid
o aprotinin
o desmopressin acetate
Local Hemostasis
The goal is to prevent or interrupt the flow of
blood from a disrupted vessel that has been incised
or transected.
May be accomplished by:
o interrupting the flow of blood to the
involved area
o direct closure of the blood vessel wall
defect
The techniques are classified as:
1. MECHANICAL
2. THERMAL
3. TOPICAL HEMOSTATIC AGENTS
MECHANICAL PROCEDURES
Digital
Pressure
pressure is applied to an artery
proximal to an area of bleeding to
reduce profuse bleeding
often effective and has the
advantage of being less traumatic
than any hemostatic clamp
cannot be used permanently
Pringle maneuver process by
which a tourniquet is used to
occlude the hepatic artery and
portal vein in the hepatoduodenal
ligament as a method of
controlling bleeding from a
transected cystic artery or the raw
surface of the liver
Hemostatic
Clamps
represents a temporary
mechanical device to stem
bleeding
disadvantage: result in damage to
the intimal wall of a blood vessel
Ligature or
Hemoclip
replaces the hemostat as a
permanent method of effecting
hemostasis of a single disrupted
vessel.
When a small vessel was
transected, a simple ligature is
sufficient. For large arteries with
pulsation and longitudinal motion,
a transfixion suture to prevent
slipping is indicated.
Sutures Required when the bleeding is
from a lateral defect in a large
vessel
represent foreign material, and
selection is based on their
intrinsic characteristics and the
state of the wound
Non-absorbable sutures, such
as silk, polyethylene, and wire
evoke less tissue reaction
Absorbable sutures such as
catgut, polyglycolic (Dexon), and
polyglactin (Vicryl) preferable
for grossly infected wounds
because the nonabsorbable
material can lead to extrusion or
sinus formation
Monofilament wire and
coated sutures have an
advantage over multifilament
material in the presence of
infection because the latter tends
to fragment and permit sinus
formation
Harmonic
Scalpel
an instrument that cuts and
coagulates tissue via vibration
at 55 kHz
A device that converts electrical
energy into mechanical motion
The motion of the blade causes
collagen molecules within the
tissue to become denatured
forming a coagulum
advantageous in performing
thyroidectomy,
hemorrhoidectomy, transsection
of the short gastric veins during
splenectomy, and in transecting
hepatic parenchyma
11 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
THERMAL AGENTS
Heat achieves hemostasis by
denaturation of protein that
results in coagulation of large
areas of tissue
ACTUAL CAUTERYheat is
transmitted from the instrument
by conduction directly to the
tissue
ELECTROCAUTERYheating
occurs by induction from an
alternating current source
DIRECT CURRENT (20- to 100-
mA range) have successfully
controlled diffuse bleeding from a
raw surface; because the protein
moieties and cellular elements of
blood have a negative surface
charge, they are attracted to a
positive pole where a thrombus
is formed
Local Cooling
(decreased
temp)
has been applied to control
bleeding from the eroded mucosa
of the esophagus and stomach.
Direct cooling with iced saline is
effective and acts by increasing
the local intravascular hematocrit
and by causing vasoconstriction
of the arterioles
EXTREME COOLING, i.e.,
cryogenic procedures, have been
applicable in gynecology and as a
method of destroying hepatic
metastases
TOPICAL HEMOSTATIC AGENTS
can be classified based on their mechanism of action
and include physical or mechanical, caustic, biologic,
and physiologic agents
Some agents induce protein coagulation and
precipitation occlusion of small cutaneous vessels
Others take advantage of later stages in the
coagulation cascade activating biologic responses
to bleeding
The ideal topical hemostatic agent:
o With significant hemostatic action
o Has minimal tissue reactivity
o Is nonantigenic
o Biodegrades in vivo
o Provides ease of sterilization
o Low in cost
o Can be tailored to specific needs
Thrombin-
derivative
products
direct the conversion of fibrinogen
to fibrin, aiding in clot formation
takes advantage of natural
physiologic processes avoiding
foreign body or inflammatory
reactions wound bed is not
disturbed
thrombin entry into larger-caliber
vessels can result in systemic
exposure to thrombin with a risk
of disseminated intravascular
clotting or death
Fibrin sealants prepared from cryoprecipitate
(homologous or synthetic)
have the advantage of not
promoting inflammation or tissue
necrosis
particularly helpful in patients who
have received heparin or who
have deficiencies in coagulation
(e.g., hemophilia or von
Willebrand's disease)
Purified gelatin
solution
can be prepared into several
vehicles, including powders,
sponges or foams, and sheets or
films
Hygroscopic - absorbing many
times its weight in water or liquid
effectively metabolized and
degraded by proteinases in the
wound bed over a period of 4 to 6
weeks
provides effective hemostasis for
operative fields with diffuse small-
vessel oozing
Thrombin may be applied to boost
hemostasis
Advantages: relatively
inexpensive, readily available,
pliable, and easy to handle
Disadvantages: implanted gelatin
can serve as a nidus for infection
BACKGROUND
Late 19
th
century social acceptance of
human blood replacement
therapy
1900 Introduction of ABO blood
grouping (Dr. Karl
Landsteiner)
1939 Rh grouping (Dr. Levine &
Dr. Stetson)
Late 1970s Whole blood was
considered the standard
in transfusion
Typing and Cross Matching
serologic compatibility is established routinely for the
recipients' and donors' A, B, O, and Rh groups in
selecting blood for transfusion
cross-matching between the donors' red blood cells
and the recipients' sera (the major cross-match) is
performed
as a rule, Rh-negative recipients should be transfused
only with Rh-negative blood (If the recipient is an
elderly male who has not been transfused previously,
the administration of Rh-positive blood is acceptable if
Rh-negative blood is not available
anti-Rh antibodies form within several weeks of
transfusion
anti-Rh antiserum (RhoGAM) should be given if Rh-
positive products have been given to an Rh-negative
patient
REPLACEMENT THERAPY
TRANSFUSION
12 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Rh-positive blood should not be transfused to Rh-
negative females who are capable of child-bearing
administration of hyperimmune anti-Rh globulin to Rh-
negative women shortly before or after childbirth
largely eliminates Rh disease in subsequent offspring
for patients receiving repeated transfusions, serum
drawn not more than 72 hours before cross-matching
should be used for matching with cells of the donor
(Emergency transfusion can be accomplished with type
O blood)
O-negative and type-specific red blood cells are equally
safe for emergency transfusion
problems are associated with the administration of four
or more units of O-negative blood because there is a
significant increase in the risk of hemolysis
for patients with clinically significant cold agglutinins,
blood should be administered through a blood warmer
(If these antibodies are present in high titer,
hypothermia is contraindicated)
for patients with multiple transfusion and who have
developed alloantibodies, or who have autoimmune
hemolytic anemia with pan-red blood cell antibodies,
typing and cross-matching is often difficult, and
sufficient time should be allotted preoperatively to
accumulate blood that might be required during the
operation
cross-matching should always be performed before the
administration of dextran because it interferes with the
typing procedure
for autologous transfusion, up to 5 units can be
collected for subsequent use during elective
procedures
patients can donate blood if their hemoglobin
concentration exceeds 11 g/dL or if the hematocrit is
greater than 34%
first procurement is performed 40 days before the
planned operation and the last one is performed 3
days before the operation
donations can be scheduled at intervals of 3 to 4 days
recombinant human erythropoietin (rHuEPO)
accelerates generation of red blood cells and allows for
more frequent harvesting of blood
Banked Whole Blood
shelf life extended to 40 5 days
at least 70% of the transfused erythrocytes remain in
the circulation for 24 hours after transfusion and are
viable
rarely indicated and rarely available
changes in the red blood cells that occur during
storage include reduction of intracellular ADP and 2,3-
diphosphoglycerate (2,3-DPG), which alters the curve
of oxygen dissociation from hemoglobin, decreasing
the function of oxygen transport
along with the clotting factors, only factor V and VIII
are stable in banked blood
pH decreases from 7.00 to 6.68, and the lactic acid
level increases from 20 to 150 mg/dL within 21 days
of storage
potassium concentration rises steadily to 32 mEq/dL,
and the ammonia concentration rises from 50 to 680
mg/dL at the end of 21 days
Fresh Whole Blood
blood administered within 24 hours of its donation
rarely indicated
must be administered untested because of the time
required for testing for infectious disease
1 unit of platelet concentrate has more viable platelets
than 1 unit of fresh blood
poor source of platelets and factor VIII
Packed Red Blood Cells and Frozen Red Blood
Cells
product of choice for most clinical situations
concentrated suspensions of red blood cells can be
prepared by removing most of the supernatant plasma
after centrifugation
preparation reduces but does not eliminate reaction
caused by plasma components (also reduces the
amount of sodium, potassium, lactic acid, and citrate
administered)
provides oxygen-carrying capacity
frozen red blood cells are not available for use in
emergencies (used for patients who are known to have
been previously sensitized)
improved red blood cell viability and the ATP and 2,3-
DPG concentrations are maintained
Leukocyte- Reduced and Leukocyte-
Reduced/Washed Red Blood Cells
prepared by filtration
eliminate 99.9% of the WBCs and most of the
platelets (leukocyte-reduced red blood cells), and, if
needed, by additional saline washing (leukocyte-
reduced/washed red blood cells)
leukocyte-reduction prevents almost all febrile,
nonhemolytic transfusion reactions (fever and/or
rigors), alloimmunization to HLA class I antigens, and
platelet transfusion refractoriness and cytomegalovirus
transmission
washed, leukocyte-reduced red blood cells are usually
given only to patients who have had reactions (rash,
urticaria, anaphylaxis) to unwashed red blood cells
Platelet Concentrates
indicated for thrombocytopenia caused by massive
blood loss and replacement with platelet-poor
products; and by inadequate production
also given to patients with qualitative platelet disorders
preparations should be used within 120 hours of
donation
1 unit of platelet concentrate = 50 mL
can transmit infectious diseases and account for
allergic reactions similar to those caused by blood
transfusion
elevate the platelet count to the range of 50,000 to
100,000/microL when treating bleeding caused by
thrombocytopenia or preparing some
thrombocytopenic patients for an operation
leukocyte reduction through filtration prevents HLA
alloimmunization
patients who become alloimmunized through previous
transfusion, or those patients who are refractory from
sensitization through prior pregnancies, HLA-matched
platelets can be used
platelet transfusion thresholds can safely be lowered in
patients without signs of hemostatic deficiency and
who have no history of poor tolerance to low platelet
counts
multiple platelet transfusions predispose to multiorgan
failure and mortality is dose-dependent
shelf life of platelets: 120 hrs from time of donation
Frozen Plasma and Volume Expanders
frozen plasma prepared from freshly donated blood is
the standard source of the vitamin Kdependent
factors (and is the only source of factor V) factor V is
less stable than the vitamin Kdependent factors)
risk of infectious disease is the same whether FFP,
whole blood, or red blood cells is administered
Lactated Ringer's solution or buffered saline solution
administered in amounts 2 to 3 times the estimated
blood loss is effective and associated with fewer
complications
13 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Dextran or a combination of lactated Ringer's solution
and normal serum albumin are preferred for rapid
volume expansion
commercially available dextran should not be
administered more than 1 L/d because of prolonged
bleeding time and consequent hemorrhage
low molecular weight dextran (3040,000 Da)
possesses a higher colloidal pressure than plasma and
effects some reversal of erythrocyte agglutination
Concentrates and Recombinant DNA Technology
antihemophilic concentrates are prepared from plasma
and are available for treatment of factor VIII or factor
IX deficiency
various concentrates are 20 to 30 times as potent as
an equal volume of FFP
concentrated albumin of 25 g can be administered to
provide the equivalent of 500 mL of plasma and has
the advantage of being hepatitis-free
Human Polymerized Hemoglobin (Polyheme)
universally compatible
immediately available
disease-free
oxygen-carrying resuscitative fluid that has been
successfully used in massively bleeding patients when
red blood cells were not transfused
absence of blood-type antigens (no cross-match
needed) and viral infections
long-term stability
disadvantages though are shorter half-life in the
bloodstream and cardiovascular complications
General Indications
Improvement in Oxygen-Carrying Capacity
oxygen-carrying capacity is chiefly a function of RBCs
transfusion should be withheld when anemia can be
treated by specific therapy, such as erythropoietin
acute anemias are more disabling than chronic anemia
because patients with chronic anemia have undergone
an adjustment to the deficiency
moderate drop in the hematocrit level and transfusions
are not indicated to correct the physiologic anemia in
pregnancy if an operation is required
correction of chronic anemia before surgical
intervention is often not necessary
hemoglobin value of less than 10 g/dL or a hematocrit
level less than 30% indicates a need for preoperative
red blood cell transfusion
cardiac output does not increase significantly in
healthy individuals until the hemoglobin value
decreases to approximately 7 g/dL
patients with chronic anemia and a hemoglobin value
of less than 7 g/dL in whom intraoperative bleeding is
not anticipated do not require a transfusion
preoperatively
blood volume can be replaced with dextran solution or
lactated Ringer's solution with a reduction of the
hemoglobin value to levels below 10 g/dL
human polymerized hemoglobin can be used to
increase oxygen-carrying capacity
whole blood substitute, Fluosol-DA, has been proposed
as a solution with increased oxygen-handling capability
Replacement of Clotting Factors
transfusion of platelets and/or proteins contributing to
coagulation may be indicated in specific patients before
or during an operative procedure
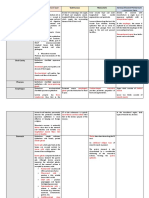
Table for replacement of clotting factors (refer to
the last page)
Specific Indications
Massive Transfusion
entails a single transfusion greater than 2500 mL or
5000 mL transfused over a period of 24 hours
circulatory overload or DIC might occur
dilutional thrombocytopenia, impaired platelet
function, and deficiencies of factors V, VIII, and XI can
also be encountered
routine alkalization is not advisable because this could
have an adverse effect on the hemoglobin dissociation
curve and also is accompanied by an increased sodium
load
Percentage of Original Blood Volume Remaining
in a Patient with a 5-L Blood Volume Transfused
with 500-mL Units
Magnitude of Hemorrhage and Transfusion
Situation 1 Blood
Volume
(10 Units)
2 Blood
Volume
(20 Units)
3 Blood
Volume
(30 Units)
Best 37 14 5
Usual 2530 10 24
Worst 18 3 0.4
"best" situation requires simultaneous and equal
replacement during hemorrhage;
"worst" situation means initial loss of one-half
blood volume not replaced until the hemorrhage
has stopped
citrate toxicity from the use of stored blood may result
in young children, in patients with severe hypotension,
or in patients with liver disease (toxicity is related to
an excessive binding of ionized calcium)
use of stored blood also provides a potassium load, but
there are no effects in the face of normal renal
function
when large volume transfusions are administered, a
heat exchanger should be used because hypothermia
can cause a decrease in cardiac rate and output and
blood pH
use of blood from multiple donors increases the risk of
hemolytic reaction as a consequence of incompatibility
when massive transfusions are administered, the pH,
blood gases, and potassium should be measured
regularly and abnormalities corrected immediately
if diffuse bleeding is noted, coagulation tests and
platelet counts should be measured and deficiencies
corrected
INDICATIONS FOR REPLACEMENT OF
BLOOD AND ITS ELEMENTS
14 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Routine Administration
rate of transfusion depends upon the patient's status
Usually 5 mL/min is administered for the first minute,
after which 10 to 20 mL/min is given
when there is marked oligemia, 500 mL can be given
within 10 minutes and a second 500 mL also can be
given within 10 minutes
approximately 1500 mL/min can be administered
through two 7.5-F catheters
Other Methods
blood can be instilled intraperitoneally or into the
medullary cavity of long bones and the sternum
approximately 90% of red blood cells injected
intraperitoneally enter the circulation, but uptake is not
complete for at least a week
intraoperative autotransfusion is a potentially life-
saving adjunct
roughly 250 mL of blood can be retrieved, washed or
filtered, and returned to the patient over a 5-minute
period
another approach to anticipated intraoperative large
blood losses is hemodilution (at the onset of the
procedure, RBCs are removed while the intravascular
volume is maintained with crystalloid or colloid)
reduced blood viscosity improves the microcirculatory
perfusion
removed blood can then be retransfused during the
operation to replace lost blood
Nonhemolytic Reactions/Febrile Reactions
increase in temperature [>1C (1.8F)]
associated with a transfusion
CAUSE: Preformed cytokines in donated blood
and recipient antibodies reacting with donated
antibodies
PREVENTION:use of leukocyte-reduced and/or
out of date blood products
Acetaminophen/Paracetamol- reduces the
severity of the reaction.
Bacterial contamination of infused blood is rare.
CLINICAL MANIFESTATIONS
o Systemic Signs
- fever and chills
- tachycardia
- hypotension
o GI Symptoms
- abdominal cramps
- vomiting
- diarrhea
o Hemorrhagic Manifestations
- hemoglobinemia
- hemoglobinuria
- disseminated intravascular coagulation
UPON SUSPECTED DIAGNOSIS:
o STOP the transfusion
o Have the donated blood cultured
Emergency treatment
o administration of oxygen
o adrenergic blocking agents
o antibiotics
Allergic Reactions
relatively frequent (~1% of all transfusions)
can occur after the administration of any blood
product
CLINICAL MANIFESTATIONS
o usually mild
o rash
o urticaria
o fever
(alloccurring within 60 to 90 minutes of
transfusion)
o anaphylactic shock - rare
CAUSE
o transfusion of antibodies from hypersensitive
donors
o transfusion of antigens to which the recipient is
hypersensitive
TREATMENT AND PROPHYLAXIS
o antihistamines
o epinephrine or steroids in more serious cases
Respiratory Complications
associated with transfusion-associated
circulatory overloadavoidable complication
occurs with rapid infusion of blood, plasma
expanders, and crystalloids esp. in older patients
with underlying heart disease
Central venous pressure monitoring should be
considered whenever large amounts of fluid are
administered
CLINICAL MANIFESTATION
o rise in venous pressure
o dyspnea
o cough
o rales at the lung bases
TREATMENT
o initiating diuresis
o slowing the rate of blood administration
o minimizing delivery of fluids while blood products
are being transfused
Syndrome of Transfusion-related Acute Lung
Injury (TRALI)
noncardiogenic pulmonary edema related to
transfusion
can occur with the administration of any plasma-
containing blood product
CLINICAL MANIFESTATIONS
o similar to those of circulatory overload
o dyspnea
o hypoxemia
o fever
o rigors
o bilateral pulmonary infiltrates on CXR
o occurs within 1 to 2 hours of transfusion, but
virtually always before 6 hours
CAUSE
o not well established
o thought to be related to anti-HLA or antihuman
neutrophil antigen antibodies in transfused
blood that primes neutrophils in the pulmonary
circulation
RISK FACTORS
o Multiparity of the donor - major risk factor
o Female donors
TREATMENT
o discontinuation of any transfusion
METHODS OF ADMINISTERING BLOOD
COMPLICATIONS OF TRANSFUSION
15 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
o notification of the transfusion service
o provision of pulmonary support
- supplemental oxygen
- mechanical ventilation
Hemolytic Reactions
high index of suspicion is needed to make the
diagnosis
LABORATORY CRITERIA
o hemoglobinuria
o serologic findings that show incompatibility of
the donor and recipient blood
o (+) Coombs' test presence of transfused cells
coated with patient antibody (diagnostic)
GENERAL TREATMENT
o STOP the transfusion immediately
o sample of the recipient's blood drawn and sent
along with the suspect unit to the blood bank
o Monitor Urine output
o Maintain adequate hydration to prevent
precipitation of hemoglobin within the tubules
Acute Hemolytic Reactions
occur with the administration of ABO-
incompatible blood
fatal in up to 6% of cases
CONTRIBUTING FACTORS
o technical or clerical errors in the laboratory
o administration of blood of the wrong blood type
CLINICAL MANIFESTATIONS
o intravascular destruction of red blood cells
o hemoglobinemia
o hemoglobinuria
o pain at the site of transfusion
o facial flushing
o back (flank)
o chest pain
o fever
o respiratory distress
o hypotension
o tachycardia
o for anesthetized patients:
- diffuse bleeding
- hypotension
o DIC
- can be initiated by activation of factor XII
and complement by antibody-antigen
complexescoagulation cascade
o Acute Renal Insufficiency
- results from the toxicity associated with free
hemoglobin in the plasma
- tubular necrosis
- precipitation of hemoglobin within the
tubules
Delayed Hemolytic Reactions
occur 2 to 10 days after transfusion
occur when an individual has a low antibody titer
at the time of transfusion but the titer increases
after transfusion as a result of an anamnestic
response
Reactions to non-ABO antigens involve
immunoglobulin Gmediated clearance by the
reticuloendothelial system.
do not usually require specific intervention
CLINICAL MANIFESTATIONS
o extravascular hemolysis
o mild anemia
o indirect (unconjugated) hyperbilirubinemia
o fever
o recurrent anemia
o Jaundice
o decreased haptoglobin levels
o low-grade hemoglobinemia and hemoglobinuria
o (+) Coombs' test
Transmission of Disease
Diseases that can be transmitted by transfusion:
Malaria
Chagas' disease
Brucellosis
Syphilis (very rarely)
Malaria (most common: Plasmodium malariae)
incubation period: 8 to 100 days
initial manifestations
shaking chills
spiking fever
hepatitis C
HIV-1
Hepatitis B
Prion disorders (e.g., Creutzfeldt-Jakob disease)
Carefully review the patient's clinical history and drug
use, and basic laboratory testing.
Common screening laboratory testing
platelet count
PT or INR
Aptt
normal platelet count :
150,000 to 400,000/ L.
bleeding or thrombotic complications
Platelet counts >1,000,000/L
Increased bleeding complications may be seen with
major surgical procedures when
the platelet count is<100,000/ L
minor surgical procedures when
counts are <50,000/ L
Spontaneous hemorrhage:
o when count falls below 20,000/ L.
PT and aPTT - variations of plasma recalcification
times initiated by the addition of a thromboplastic
agent
PT reagent
o contains thromboplastin and Ca
o when added to plasma, leads to the formation of a
fibrin clot
PT test
o measures the function of factors I, II, V, VII, and X
o Factor VII -shortest half-life of the coagulation
factors, and its synthesis is vitamin K dependent.
o best suited to detection of abnormal coagulation
caused by vitamin K deficiencies and warfarin
therapy
Due to variations in thromboplastin activity, it can be
difficult to accurately assess the degree of
anticoagulation on the basis of PT alone
o determination of the INR is now the method of
choice for reporting PT values.
o International Sensitivity Index (ISI) is unique to
each batch of thromboplastin and is furnished by the
manufacturer tothe hematology laboratory
o Human brain thromboplastin has an ISI of 1, and the
optimal reagent has an ISI between 1.3 and 1.5.
aPTT reagent
o phospholipid substitute, activator, and calcium
TEST OF HEMOSTASIS AND BLOOD
COAGULATION
16 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
o in the presence of plasma leads to fibrin clot
formation
o measures function of factors I, II, and V of the
common pathway and factors VIII, IX, X, and XII
Heparin therapy-monitored by following aPTT values,
with a therapeutic target range of 1.5 to 2.5 times the
control value (approx 50 to 80 seconds)
Low molecular weight heparins are selective factor Xa
inhibitors and may mildly elevate the aPTT, but
therapeutic monitoring is not routinely recommended.
bleeding time -used to evaluate platelet and vascular
dysfunction
o Ivy bleeding time is most commonly
used
determined by placing a
sphygmomanometer on the
upper arm and inflating it to 40
mmHg and then making a 5-mm
stab incision on the flexor surface
of the forearm
Time is measured to cessation of
bleeding
upper limit of normal bleeding
time 7 min
o abnormal bleeding time suggests either
platelet dysfunction (intrinsic or drug
induced), vWD, or certain vascular
defects
replacing the template bleeding time with an in vitro
test
o which blood is sucked through a capillary and the
platelets adhere to the walls of the capillary and
aggregate
o closure time in this system appears to be more
reproducible than the bleeding time
o correlates with bleeding in patients with vWD,
primary platelet function disorders, or other platelet
dysfunction disorders and patients who are taking
aspirin
Additional medications may significantly impair
hemostatic function such as
o antiplatelet agents (clopidogrel and glycoprotein
IIb/IIIa inhibitors)
o anticoagulant agents (hirudin, chondroitin sulfate,
dermatan sulfate)
o thrombolytic agents (streptokinase, tPA)
If abnormal results on any of the coagulation studies
cannot be explained by known medications-
>congenital abnormalities of coagulation or comorbid
disease should be considered
Thromboelastography (TEG)
o monitors hemostasis as a dynamic process rather
than revealing isolated information as in
conventional coagulation screens.
o measures the viscoelastic properties of blood as it is
induced to clot in a lowshear environment
(resembling sluggish venous flow)
o patterns of change in shear elasticity allow the
kinetics of clot formation and growth as well as the
strength and stability of the formed clot to be
determined
o strength and stability data- provide information
about the ability of the clot to perform the work of
hemostasis
o kinetic data- determine the adequacy of quantitative
factors available for clot formation
o sample of celite-activated whole blood is placed
into a prewarmed cuvette ->suspended piston is
then lowered into the cuvette -> rotated through a
4.5-degree arc backwards and forwards
o Normal clot goes through an acceleration and
strengthening phase
o fiber strands that interact with activated platelets
attach to the surface of the cuvette and the
suspended piston
o clot forming in the cuvette transmits its movement
onto the suspended piston
o Weak clot stretches and therefore delays the arc
movement of the piston, which is graphically
expressed as a narrow thromboelastogram
o Strong clot will move the piston simultaneously and
proportionally to the cuvette's movements, creating
a thick thromboelastogram
o strength of a clot is graphically represented over
time as a characteristic cigar-shaped figure
o k- measure of the time from the beginning of clot
formation until the amplitude of the TEG tracing
reaches 20 mm and represents the dynamics of clot
formation
o alpha angle - angle between the line in the middle of
the TEG(r) tracing and the line tangential to the
developing body of the TEG(r) tracing. The alpha angle
represents the acceleration (kinetics) of fibrin buildup
and cross-linking
o MA -maximum amplitude and reflects the strength of
the clot, which is dependent on the number and
function of platelets and the clot's interaction with
fibrin
o MA60 - rate of amplitude reduction 60 minutes after
MA and represents the stability of the clot
Preoperative Evaluation of Hemostasis
Several hematologic disorders may have an impact on
the outcome of surgery.
pre-existing anemia and oral anticoagulation
therapy-common clinical situations faced by the
surgeon
Assessment of bleeding risk should also be considered
in patients with liver or renal dysfunction
When feasible, diagnostic evaluation of the patient
with previously unrecognized anemia should be carried
out before surgery, because certain types of anemia
(particularly sickle cell disease and immune hemolytic
anemias) may have implications for perioperative
management
Hemoglobin levels below 7 or 8 g/dL appear to be
associated with significantly more perioperative
complications than higher levels
Determination of the need for preoperative transfusion
in an individual patient must consider factors other
than the absolute hemoglobin level, including
o presence of cardiopulmonary disease
o type of surgery
o likelihood of surgical blood loss
Many patients have anemia postoperatively secondary
to blood loss and hemodilution and do not necessarily
require transfusion
directed bleeding history- most important component
of the bleeding risk assessment
o provide meaningful clues to the presence
of a bleeding tendency
EVALUATION OF HEMOSTATIC RISK IN THE
SURGICAL PATIENT
17 of 17
Dave.Linelle.Deane.Mhe.Te.Paul
Patients who are reliable historians and who reveal no
suggestion of abnormal bleeding on directed bleeding
history and physical examination are at very low risk
for having an occult bleeding disorder
o Laboratory tests of hemostatic
parameters is not required
When the directed bleeding history is unreliable or
incomplete or when abnormal bleeding is suggested
o formal evaluation of hemostasis should
be performed before surgery
PT, the aPTT, and the platelet
count
Excessive bleeding during or after a surgical procedure
may be the result of
o ineffective hemostasis
o blood transfusion
o undetected hemostatic defect
o consumptive coagulopathy
o fibrinolysis
Excessive bleeding from the operative field
unassociated with bleeding from other sites usually
suggests inadequate mechanical hemostasis
Massive blood transfusion-well-known cause of
thrombocytopenia
Bleeding after massive transfusion can occur due to
o Hypothermia
o dilutional coagulopathy
o platelet dysfunction,
o fibrinolysis
o hypofibrinogenemia
Another cause of hemostatic failure related to the
administration of blood is hemolytic transfusion
reaction
diffuse bleeding -first sign of a transfusion reaction
o release of ADP from hemolyzed red blood cells->
diffuse platelet aggregation->after which the platelet
clumps are removed out of the circulation->bleeding
Transfusion purpura occurs when the donor platelets
are of the uncommon Pl(A1) group
o an uncommon cause of thrombocytopenia and
associated bleeding after transfusion
The platelets sensitize the recipient, who makes
antibody -> antibody then destroys the recipient's own
platelets-> thrombocytopenia and bleeding may
continue for several weeks.
This uncommon cause of thrombocytopenia should be
considered if bleeding follows transfusion by 5 or 6
days.
Platelet transfusions are of little help in the
management of this syndrome, because the new donor
platelets usually are subject to the binding of antigen
and damage from the antibody
Corticosteroids may be of some help in reducing the
bleeding tendency.
Posttransfusion purpura is self-limited, and the
passage of several weeks inevitably leads to
subsidence of the problem.
DIC is characterized by systemic activation of the
blood coagulation system-> results in the generation
and deposition of fibrin ->leading to microvascular
thrombi in various organs -> contributing to the
development of multiorgan failure
Consumption and subsequent exhaustion of
coagulation proteins and platelets due to the ongoing
activation of the
coagulation system may induce severe bleeding
complications
Severe hemorrhagic disorders due to
thrombocytopenia have occurred as a result of gram-
negative sepsis
o pathogenesis of endotoxin-induced
thrombocytopemia- related to lability of factor V
Defibrination and hemostatic failure also may occur
with meningococcemia, Clostridium perfringens sepsis,
and staphylococcal sepsis
o Hemolysis appears to be one mechanism in
sepsis leading to defibrination
From omgfacts.com:
Anatidaephobia is the fear that somewhere in the
world, there is a duck watching you.
If you touch your tongue while yawning, it can
stop the yawn.
You're more likely to die on your way to buy a
lottery ticket than you are to actually win the
lottery.
Women speak about 7000 words a day. The
average man averages just over 2000.
'Hippopotomonstrosesquippedaliophobia' is the
fear of long words.
When a person is tickled, the response is actually
a form of panic, as the brain interprets the
tickling sensation as produced by spiders or
other creepy crawlies on your skin - the
uncontrollable laughter is a response to panic.
Those stars and colours you see when you rub
your eyes are called phosphenes.
Yawning is contagious - even thinking about
yawning is enough. After reading this fact, there
is a 50% chance you will yawn.
The total weight of all the ants on Earth is about
the same as the weight of all the humans on
earth.
When you kiss someone for a minute, you both
burn about 2.6 calories.
An elephant can die from a broken heart.
'Dreamt' is the ONLY WORD in the entire English
language that ends in the letters 'mt'.
'Dysania' is the state of finding it hard to get out
of bed in the morning.
One tablespoon of semen has approximately 20
calories. Semen also contains zinc and calcium
which helps prevent tooth decay.
Breathing the air in Mumbai, India for just ONE
DAY, is equivalent to smoking 2.5 packs of
cigarettes.
According to suicide statistics, Monday is the
favored day for self-destruction.
If you walk and talk with someone, eventually
you will synchronize your steps with each other.
Albert Einstein left his first wife for his COUSIN.
A strawberry is not an actual berry, but a banana
is.
Your earlobes line up with your nipples. (Go
try!)
As a punishment for misbehavior, Thai cops have
to wear pink Hello Kitty armbands.
Colgate faced big obstacle marketing toothpaste
in Spanish-speaking countries because Colgate
translates into the command 'go hang yourself.'
In Topeka, Kansas it is illegal to sing the
alphabet on the streets at night. It is also illegal
to install a bathtub, and you may not scream in a
haunted house.
Justin Bieber can solve a Rubik's Cube in less
than 2 minutes.
Humans don't just shrink with age. They shrink
EVERY DAY. (Uh-oh. Deane)
EVALUATION OF EXCESSIVE
INTRAOPERATIVE OR POSTOPERATIVE
BLEEDING
Anda mungkin juga menyukai
- Postoperative Fever - UpToDate PDFDokumen25 halamanPostoperative Fever - UpToDate PDFkatsuiaBelum ada peringkat
- Robbins Ch. 19 The Pancreas Review QuestionsDokumen3 halamanRobbins Ch. 19 The Pancreas Review QuestionsPA2014100% (1)
- Pulmonary PathologyDokumen6 halamanPulmonary PathologyjamesjaanBelum ada peringkat
- Surgery Trans 1 - Systemic Response To InjuryDokumen29 halamanSurgery Trans 1 - Systemic Response To InjuryJoan Caacbay De GuzmanBelum ada peringkat
- Surgical InfectionsDokumen2 halamanSurgical Infectionsjc_sibal13100% (1)
- Bleeding Disorders & Its ManagementDokumen102 halamanBleeding Disorders & Its ManagementnehascribdjoshiBelum ada peringkat
- Metabolic Response To InjuryDokumen55 halamanMetabolic Response To InjuryMuhammad NaveedBelum ada peringkat
- Git PathologyDokumen113 halamanGit PathologyanggitaBelum ada peringkat
- Hemostasis and ThrombosisDokumen23 halamanHemostasis and ThrombosisFiqrotul Umam100% (1)
- FLUID AND ELECTROLYTE MANAGEMENT OF SURGICAL PATIENTSDokumen37 halamanFLUID AND ELECTROLYTE MANAGEMENT OF SURGICAL PATIENTSJie CuetoBelum ada peringkat
- Overview of Central Venous AccessDokumen13 halamanOverview of Central Venous AccessnathanaelandryBelum ada peringkat
- Aetiology, Pathology and Management of Enterocutaneous FistulaDokumen34 halamanAetiology, Pathology and Management of Enterocutaneous Fistularoselinekhadija100% (1)
- Postoperative Assessment, Management and Complications GuideDokumen57 halamanPostoperative Assessment, Management and Complications GuideThon JustineBelum ada peringkat
- Peptic Ulcers GuideDokumen46 halamanPeptic Ulcers GuideEmmanuel MukukaBelum ada peringkat
- Pathology of InfectiousDokumen39 halamanPathology of InfectiousDeEo OnoBelum ada peringkat
- Benign Gynecological LesionsDokumen9 halamanBenign Gynecological LesionsLanceBelum ada peringkat
- Abdominal Trauma Diagnosis and ManagementDokumen9 halamanAbdominal Trauma Diagnosis and ManagementMyrtle Yvonne RagubBelum ada peringkat
- Surgery Systemic Response to InjuryDokumen11 halamanSurgery Systemic Response to InjuryMATTHEW EARL MALUMAYBelum ada peringkat
- Complication of Blood TransfusionDokumen5 halamanComplication of Blood TransfusionChey Ochy ApriliaBelum ada peringkat
- Immune SystemDokumen10 halamanImmune Systemailyn regaladoBelum ada peringkat
- SURGICAL INFECTION PREVENTIONDokumen5 halamanSURGICAL INFECTION PREVENTIONCarl Earvin L. FavoritoBelum ada peringkat
- Cellular Injury, Adaptation and Cell DeathDokumen8 halamanCellular Injury, Adaptation and Cell DeathJessica Febrina Wuisan100% (1)
- Neoplasm Lecture NotesDokumen6 halamanNeoplasm Lecture Notesmiguel gaquitBelum ada peringkat
- Pediatric Surgery Conditions of the Respiratory and Gastrointestinal SystemsDokumen12 halamanPediatric Surgery Conditions of the Respiratory and Gastrointestinal SystemsRenatoCosmeGalvanJunior100% (1)
- Endocrine PathologyDokumen13 halamanEndocrine Pathologysarguss14100% (1)
- Hemostasis, Surgical Bleeding and TransfusionDokumen10 halamanHemostasis, Surgical Bleeding and TransfusionCarl Earvin L. FavoritoBelum ada peringkat
- Surgery 1.1 Fluid and Electrolyte Balance - Azares PDFDokumen7 halamanSurgery 1.1 Fluid and Electrolyte Balance - Azares PDFAceking MarquezBelum ada peringkat
- Nada's GI Path ReviewDokumen44 halamanNada's GI Path ReviewNada Much100% (2)
- Differential Diagnosis of Painful Genital LesionsDokumen7 halamanDifferential Diagnosis of Painful Genital LesionsKyra KhalidBelum ada peringkat
- Dr. Manella Joseph Senior Lecturer/Consultant PathologistDokumen41 halamanDr. Manella Joseph Senior Lecturer/Consultant PathologistNipun Shamika100% (1)
- Pathology of Hematopoietic System 2012-2013 by DR - Mai AliDokumen17 halamanPathology of Hematopoietic System 2012-2013 by DR - Mai AliMuhammad Hilman Abu BakarBelum ada peringkat
- Blood DisordersDokumen21 halamanBlood Disordersapi-448398971Belum ada peringkat
- Pathology - Lab: Pathology of The Blood VesselsDokumen5 halamanPathology - Lab: Pathology of The Blood VesselsRazel PerezBelum ada peringkat
- GI Tract Histology SummaryDokumen5 halamanGI Tract Histology SummaryFluffy_iceBelum ada peringkat
- Surgical Infections Chapter 5 Shcwartz Principles of SurgeryDokumen34 halamanSurgical Infections Chapter 5 Shcwartz Principles of Surgeryanas hindawi100% (4)
- Abdominal Trauma: Fatin Amirah KamaruddinDokumen29 halamanAbdominal Trauma: Fatin Amirah Kamaruddinvirz23Belum ada peringkat
- NeoplasiaDokumen21 halamanNeoplasiabpt2Belum ada peringkat
- Physiologic Monitoring of The Surgical PatientDokumen56 halamanPhysiologic Monitoring of The Surgical PatientSeid Adem100% (2)
- Antibiotic in OmfsDokumen47 halamanAntibiotic in OmfsRajat GuptaBelum ada peringkat
- 3 Surgery - Mediastinum and PleuraDokumen6 halaman3 Surgery - Mediastinum and PleuraCassey Koi FarmBelum ada peringkat
- Refkas CondylomaAccuminataDokumen18 halamanRefkas CondylomaAccuminatamichelle1945Belum ada peringkat
- SURGICAL COMPLICATIONS AND POSTOPERATIVE MANAGEMENTDokumen43 halamanSURGICAL COMPLICATIONS AND POSTOPERATIVE MANAGEMENTshintia novotnaBelum ada peringkat
- Renal colic diagnosis from lab resultsDokumen101 halamanRenal colic diagnosis from lab resultsSaad KhanBelum ada peringkat
- General and Vascular Surgery Princess Margaret Hospital: Dr. D. FarquharsonDokumen16 halamanGeneral and Vascular Surgery Princess Margaret Hospital: Dr. D. FarquharsonacklinsdocBelum ada peringkat
- Sutures and Ligatures-1Dokumen4 halamanSutures and Ligatures-1Pranjali ParkheBelum ada peringkat
- Endocrine and Metabolic EmergenciesDokumen320 halamanEndocrine and Metabolic EmergenciesReem Ben Omran100% (1)
- 14 Patho Head and Neck PathologyDokumen10 halaman14 Patho Head and Neck PathologyMartin TanBelum ada peringkat
- Abdominal Compartment Syndrome: By: Adel Ghuloom, MD Lubna Kamaldien, MDDokumen42 halamanAbdominal Compartment Syndrome: By: Adel Ghuloom, MD Lubna Kamaldien, MDnanang anacardia Subagyo100% (1)
- Surgery Fluids & Electrolytes-1Dokumen9 halamanSurgery Fluids & Electrolytes-1Aimie DagaleaBelum ada peringkat
- Clotting Pathway GuideDokumen13 halamanClotting Pathway Guideardy420100% (1)
- Surgical Site InfectionDokumen14 halamanSurgical Site InfectionSri AsmawatiBelum ada peringkat
- Chapter Summary - PANCREAS Final (Schwartz) PDFDokumen19 halamanChapter Summary - PANCREAS Final (Schwartz) PDFMiguel Cuevas DolotBelum ada peringkat
- Neoplasia Patho - 1Dokumen53 halamanNeoplasia Patho - 1Alishba MushtaqBelum ada peringkat
- Surgical InfectionDokumen9 halamanSurgical InfectionJL DeomampoBelum ada peringkat
- Understanding Toxic Epidermal NecrolysisDokumen13 halamanUnderstanding Toxic Epidermal NecrolysisHend AbdallaBelum ada peringkat
- Intra Abdominal 2009Dokumen8 halamanIntra Abdominal 2009Shinta Dwi Septiani Putri WibowoBelum ada peringkat
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Pleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsDari EverandPleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsBelum ada peringkat
- Introduction To Blood CoagulationDokumen22 halamanIntroduction To Blood Coagulationemman_abzBelum ada peringkat
- Hemostasis, Hemorrhagic Disorders and ThrombosisDokumen114 halamanHemostasis, Hemorrhagic Disorders and ThrombosisZeeBelum ada peringkat
- Creamy Carbonara RecipeDokumen1 halamanCreamy Carbonara RecipeRobin TolentinoBelum ada peringkat
- Annex B-1 RR 11-2018 Sworn Statement of Declaration of Gross Sales and ReceiptsDokumen1 halamanAnnex B-1 RR 11-2018 Sworn Statement of Declaration of Gross Sales and ReceiptsEliza Corpuz Gadon89% (19)
- Immunization Routine Table3 PDFDokumen9 halamanImmunization Routine Table3 PDFOwaisBelum ada peringkat
- Basic Manual For Free Range Chicken Production (Meat Type) : Emerson E. SiscarDokumen14 halamanBasic Manual For Free Range Chicken Production (Meat Type) : Emerson E. SiscarRobin TolentinoBelum ada peringkat
- Heritage Chicken Breeds (Pure Breeds)Dokumen3 halamanHeritage Chicken Breeds (Pure Breeds)Robin Tolentino100% (3)
- Radio JournalDokumen40 halamanRadio JournalRobin TolentinoBelum ada peringkat
- Cassia Fistula Golden-Shower: Fact Sheet ST-127Dokumen3 halamanCassia Fistula Golden-Shower: Fact Sheet ST-127Robin TolentinoBelum ada peringkat
- Medicine IM Platinum-1Dokumen357 halamanMedicine IM Platinum-1Bom Tna67% (3)
- How to plant and care for Amaltas treesDokumen1 halamanHow to plant and care for Amaltas treesRobin TolentinoBelum ada peringkat
- Liver Anatomy and Physiology MedicineDokumen73 halamanLiver Anatomy and Physiology MedicineRobin TolentinoBelum ada peringkat
- Questionnaires For CONDUCTOR'S LICENSE EXAM APPLICANTS EDITEDDokumen4 halamanQuestionnaires For CONDUCTOR'S LICENSE EXAM APPLICANTS EDITEDJohn MagayanoBelum ada peringkat
- The Jayjay Song Ronda CatongaDokumen6 halamanThe Jayjay Song Ronda CatongaRobin TolentinoBelum ada peringkat
- Temporal and Infratemporal FossaeDokumen29 halamanTemporal and Infratemporal FossaeRobin Tolentino100% (1)
- Physics Andits Laws in AnaesthesiaDokumen111 halamanPhysics Andits Laws in AnaesthesiaRobin TolentinoBelum ada peringkat
- Gen Anesthesia Medicine PhysiologgyDokumen82 halamanGen Anesthesia Medicine PhysiologgyRobin TolentinoBelum ada peringkat
- The Face and ScalpDokumen31 halamanThe Face and ScalpRobin TolentinoBelum ada peringkat
- The Choral Works of Robert Delgado - SATB ScoreDokumen48 halamanThe Choral Works of Robert Delgado - SATB ScoreRobin Tolentino88% (16)
- Anatomic Structures: St. Paul University PhilippinesDokumen6 halamanAnatomic Structures: St. Paul University PhilippinesRobin TolentinoBelum ada peringkat
- Alcohol by Dr. SibbalucaDokumen4 halamanAlcohol by Dr. SibbalucaRobin TolentinoBelum ada peringkat
- Anatomy and Physiology Quiz ReviewDokumen9 halamanAnatomy and Physiology Quiz ReviewRobin Tolentino100% (1)
- Anatomy of The EYEDokumen115 halamanAnatomy of The EYERobin TolentinoBelum ada peringkat
- Biochemistry of CarbohydratesDokumen7 halamanBiochemistry of CarbohydratesRobin TolentinoBelum ada peringkat
- Antihypertensives Summary Katzung PharmacologyDokumen8 halamanAntihypertensives Summary Katzung PharmacologyRobin TolentinoBelum ada peringkat
- 3 Shoulder Joint - Chapter Summary - Anatomy of The Shoulder Joint by Snell Medicine LectureDokumen76 halaman3 Shoulder Joint - Chapter Summary - Anatomy of The Shoulder Joint by Snell Medicine LectureRobin TolentinoBelum ada peringkat
- Ikaw (Zamora)Dokumen5 halamanIkaw (Zamora)Robin Tolentino100% (5)
- Phlebotomy Unit 6 Study GuideDokumen3 halamanPhlebotomy Unit 6 Study GuidemilBelum ada peringkat
- MCQ ON Acute Posthemorrhagic AnemiaDokumen22 halamanMCQ ON Acute Posthemorrhagic AnemiaSampath KumarBelum ada peringkat
- Organ Systems InteractionsDokumen6 halamanOrgan Systems InteractionsHart OlpendaBelum ada peringkat
- Knowledge of Blood Transfusion Practice Among NursesDokumen37 halamanKnowledge of Blood Transfusion Practice Among NursesCallumBelum ada peringkat
- Rbcs Modifie 2Dokumen6 halamanRbcs Modifie 2Habib UllahBelum ada peringkat
- Module 1 Plant and Animal Organ Systems and Their Functions Part 2 PDFDokumen57 halamanModule 1 Plant and Animal Organ Systems and Their Functions Part 2 PDFMoto FlashBelum ada peringkat
- RognidanDokumen18 halamanRognidanchowdegowda100% (1)
- Pulse Variations MYP4 Biology Criterion B and CDokumen4 halamanPulse Variations MYP4 Biology Criterion B and ColivinamacBelum ada peringkat
- Grade 9 Science Packet Covers Respiratory and Circulatory SystemsDokumen107 halamanGrade 9 Science Packet Covers Respiratory and Circulatory SystemsFhranscea KimBelum ada peringkat
- Analysis of Polyethylene-Glycol-Polylactide Nano-Dimension Artificial Red Blood Cells in Maintaining Systemic Hemoglobin Levels and Prevention of Methemoglobin FormationDokumen19 halamanAnalysis of Polyethylene-Glycol-Polylactide Nano-Dimension Artificial Red Blood Cells in Maintaining Systemic Hemoglobin Levels and Prevention of Methemoglobin FormationIstván PortörőBelum ada peringkat
- Sharir Kriya SyllabusDokumen14 halamanSharir Kriya SyllabusShahrukh QadriBelum ada peringkat
- Hemolytic Disease of NewbornDokumen14 halamanHemolytic Disease of NewbornAradhanaRamchandaniBelum ada peringkat
- Rescue Plan Working at HeightDokumen11 halamanRescue Plan Working at Heightadeoye AdeyemiBelum ada peringkat
- Consumptive CoagulopathyDokumen20 halamanConsumptive Coagulopathyilvan yanuarBelum ada peringkat
- Bible of Bee Venom TherapyDokumen0 halamanBible of Bee Venom TherapypaulxeBelum ada peringkat
- The Gates of HellDokumen458 halamanThe Gates of Hellmailinglistenator761100% (8)
- Thrombolytics-1Dokumen3 halamanThrombolytics-1Shayan ShayanBelum ada peringkat
- Hematology, Immunology & OncologyDokumen10 halamanHematology, Immunology & Oncologyjennaaahhh67% (3)
- What Documents Do You Need After A Blood Transfusion?: BT Checklist 1Dokumen5 halamanWhat Documents Do You Need After A Blood Transfusion?: BT Checklist 1Edelweiss Marie CayetanoBelum ada peringkat
- Ascp StudyDokumen18 halamanAscp StudyJamaica EstorninosBelum ada peringkat
- The Structures of The Human Body and Its FunctionsDokumen4 halamanThe Structures of The Human Body and Its FunctionsLESSON TIMEBelum ada peringkat
- Bepe 115 Module 1Dokumen41 halamanBepe 115 Module 1rosanalicudineeeBelum ada peringkat
- Order of DrawDokumen1 halamanOrder of Drawighiunghius100% (1)
- Automated Blood Coagulation Analyzer CA-500: Basic Data Sheet - (Fibrinogen)Dokumen9 halamanAutomated Blood Coagulation Analyzer CA-500: Basic Data Sheet - (Fibrinogen)Aahsan Iqbal احسن اقبالBelum ada peringkat
- Blood BankingDokumen118 halamanBlood BankingRay Jr Jr100% (2)
- Dehp in PVC Medical FDADokumen119 halamanDehp in PVC Medical FDAkalebasveggieBelum ada peringkat
- Disseminated Intravascular Coagulation Is A Condition in Which Small Blood Clots DevelopDokumen4 halamanDisseminated Intravascular Coagulation Is A Condition in Which Small Blood Clots DevelopRiaz JiwaBelum ada peringkat
- Physiological Changes During Pregnancy: Presented By: Ms. Vruti PatelDokumen44 halamanPhysiological Changes During Pregnancy: Presented By: Ms. Vruti PatelSANJEEV KUMARBelum ada peringkat
- The Human Body: A Concise Look at Brain Power and Blood FlowDokumen2 halamanThe Human Body: A Concise Look at Brain Power and Blood FlowSergioBelum ada peringkat
- Typhoid Test ReportDokumen4 halamanTyphoid Test ReportDEEPAK DubeyBelum ada peringkat