1 s2.0 S0272638607013686 Main
Diunggah oleh
RatnaVelugu0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
14 tayangan8 halamanPeriodontal Disease and Other Nontraditional Risk Factors for CKD
Monica A. Fisher, PhD, DDS, MPH,1 George W. Taylor, DMD, DrPH,2 Brent J. Shelton, PhD,3
Kenneth A. Jamerson, MD,2 Mahboob Rahman, MD, MS,1 Akinlolu O. Ojo, MD, PhD,2 and
Ashwini R. Sehgal, MD1
Judul Asli
1-s2.0-S0272638607013686-main
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniPeriodontal Disease and Other Nontraditional Risk Factors for CKD
Monica A. Fisher, PhD, DDS, MPH,1 George W. Taylor, DMD, DrPH,2 Brent J. Shelton, PhD,3
Kenneth A. Jamerson, MD,2 Mahboob Rahman, MD, MS,1 Akinlolu O. Ojo, MD, PhD,2 and
Ashwini R. Sehgal, MD1
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
14 tayangan8 halaman1 s2.0 S0272638607013686 Main
Diunggah oleh
RatnaVeluguPeriodontal Disease and Other Nontraditional Risk Factors for CKD
Monica A. Fisher, PhD, DDS, MPH,1 George W. Taylor, DMD, DrPH,2 Brent J. Shelton, PhD,3
Kenneth A. Jamerson, MD,2 Mahboob Rahman, MD, MS,1 Akinlolu O. Ojo, MD, PhD,2 and
Ashwini R. Sehgal, MD1
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 8
Periodontal Disease and Other Nontraditional Risk Factors for CKD
Monica A. Fisher, PhD, DDS, MPH,
1
George W. Taylor, DMD, DrPH,
2
Brent J. Shelton, PhD,
3
Kenneth A. Jamerson, MD,
2
Mahboob Rahman, MD, MS,
1
Akinlolu O. Ojo, MD, PhD,
2
and
Ashwini R. Sehgal, MD
1
Background: Chronic kidney disease, undiagnosed in a signicant number of adults, is a public
health problem. Given the systemic inammatory response to periodontal disease, we hypothesized
that periodontal disease could be associated with chronic kidney disease.
Study Design: Cross-sectional.
Setting & Participants: We identied 12,947 adults 18 years or older with information for kidney
function and at least one risk factor in the Third National Health and Nutrition Examination Survey.
Predictor: The main predictor was periodontal status. Other nontraditional and traditional risk factors
included socioeconomic status, health status, health behavior, biomarker levels, anthropometric assess-
ment, and health care utilization.
Outcomes & Measurements: Chronic kidney disease was dened using the Kidney Disease
Outcomes Quality Initiative stages 3 and 4 with a moderate to severe decrease in kidney function
(glomerular ltration rate, 15 to 59 mL/min/1.73 m
2
). Univariable and multivariable logistic regression
models assessed the associations between chronic kidney disease and periodontal disease and other
nontraditional risk factors.
Results: Chronic kidney disease prevalence was 3.6%; periodontal disease prevalence was 6.0%;
and edentulism prevalence was 10.5%. Adults with periodontal disease and edentulous adults were
twice as likely to have chronic kidney disease (adjusted odds ratio, 1.60; 95% condence interval, 1.16
to 2.21; adjusted odds ratio, 1.85; 95% condence interval, 1.34 to 2.56, respectively) after simulta-
neously adjusting for other traditional and nontraditional risk factors.
Limitations: Temporal association is unknown.
Conclusions: Periodontal disease and its severe consequence, edentulism, were independently
associated with chronic kidney disease after adjusting for other traditional and nontraditional risk factors.
This model could contribute to identifying individuals at risk of chronic kidney disease and reduce its
burden.
Am J Kidney Dis 51:45-52. 2007 by the National Kidney Foundation, Inc.
INDEX WORDS: Chronic kidney disease; diabetes mellitus; edentulism; glomerular ltration rate;
hypertension; macroalbuminuria; periodontal disease.
C
hronic kidney disease (CKD) is a public
health problem that is undiagnosed in a
signicant number of those affected in the United
States.
1-3
Serious sequelae related to CKD in-
clude end-stage kidney failure, cardiovascular
disease, and premature death, with death and
cardiovascular events more common than pro-
gression to kidney failure.
4-6
The risk of these
serious sequelae increases as glomerular ltra-
tion rate (GFR) decreases to less than 60 mL/min/
1.73 m
2
(1.0 mL/s/1.73 m
2
).
4-6
This level of
moderate to severe decrease in kidney function
corresponds to the National Kidney Foundation-
Kidney Disease Outcomes Quality Initiative
stages 3 and 4 CKD, dened as a GFR of 15 to 59
mL/min/1.73 m
2
(0.25 to 0.98 mL/s/1.73 m
2
).
1
Identication of undiagnosed high-risk indi-
viduals is needed to provide the opportunity for
early detection and intervention to prevent or
delay the onset of end-stage renal disease and
cardiovascular events. Other than one recently
reported prediction model,
7
high-risk subgroups
for CKD typically were identied through a
single traditional risk factor: age older than 60
years,
1,7,8
hypertension,
2,8,9-15
diabetes,
2,7-16
poor
glycemic control,
1,11,12
obesity,
2,12-16
macroalbu-
minuria,
1,3,8,17
smoking,
1,9,12,14-16
C-reactive
protein level,
14,18,19
elevated total choles-
terol level,
1,12,14
low high-density lipoprotein
1
From Case Western Reserve University, Cleveland, OH;
2
University of Michigan, Ann Arbor, MI; and
3
University of
Kentucky, Lexington, KY.
Received June 2, 2007. Accepted in revised form Septem-
ber 18, 2007.
This work was done at Case Western Reserve University.
Address correspondence to Monica A. Fisher, PhD, DDS,
MPH, Associate Professor, Case Western Reserve Univer-
sity, 10900 Euclid Ave, Cleveland, OH 44106-4905.E-mail:
monica.sher@case.edu
2007 by the National Kidney Foundation, Inc.
0272-6386/07/5101-0007$34.00/0
doi:10.1053/j.ajkd.2007.09.018
American Journal of Kidney Diseases, Vol 51, No 1 (January), 2008: pp 45-52 45
level,
1,10,12,15
elevated low-density lipoprotein
cholesterol level,
15
race/ethnicity,
1,11,13,14,16
gen-
der,
1,7,9,12,14-16
and income/poverty.
1,13
Recently,
nontraditional risk factors were reported that
may contribute to CKD, such as periodontal
disease,
20-22
education,
13,16
and health care utili-
zation.
13,23
The rationale for considering periodontal dis-
ease as a nontraditional risk factor for CKD
centers around the inammatory response to peri-
odontal disease adding to the chronic systemic
inammatory burden associated with CKD. The
role of chronic inammatory burden in patients
with CKD was reported through the association
between C-reactive protein level and CKD.
19,24
Thus, we speculate that periodontal disease may
contribute to CKD because periodontal disease,
more specically chronic periodontitis, is a
chronic infectious disease caused by gram-
negative bacteria with a persistent host inamma-
tory response. The loss of attachment of the
periodontal ligament and bony support of the
teeth can lead to tooth loss. In adults, periodontal
disease is a major cause of edentulism.
25
The
response to periodontal pathogens leads to a
local tissue-destructive immunoinammatory re-
sponse thought to create a chronic systemic in-
ammatory burden secondary to the systemic
dissemination of periodontal pathogenic bacte-
ria, their products (eg, lipopolysaccharides), and
locally produced inammatory mediators (eg,
interleukin 1, tumor necrosis factor , interleu-
kin 6, prostaglandin E
2
, and thromboxane
B2).
26,27
Furthermore, an acute-phase inamma-
tory response, measured by using elevated C-
reactive protein level, is associated with periodon-
tal disease and edentulism after controlling for
other risk factors for elevated C-reactive protein
level.
28
A similar focus on the systemic inammatory
burden of chronic periodontal disease was hypoth-
esized to contribute to endothelial injury and
atherogenesis.
29
An increasing body of epidemio-
logical evidence supports a signicant associa-
tion between periodontal disease and cardiovas-
cular diseases.
30,31
Additionally, several clinical
studies involving the treatment of patients with
chronic periodontitis reported an improvement
in secondary end points considered important in
cardiovascular disease risk,
27
including a re-
cently reported randomized clinical trial show-
ing a signicant improvement in endothelial func-
tion after periodontal treatment.
29
Chronic inammation is one of the common
risk factors for both atherosclerotic cardiovascu-
lar disease and CKD. Evidence also exists to
support chronic inammation contributing to the
pathogenesis of hypertension and diabetes melli-
tus, both major risk factors for cardiovascular
disease and CKD.
32
Based on the current evi-
dence that periodontal disease is a source of
systemic inammatory burden, it is biologically
plausible to hypothesize that periodontal disease
is a risk factor for CKD.
The use of single risk factors to identify sub-
groups at high risk of CKD is a major limitation
that can be addressed by simultaneously consid-
ering a set of risk factors. Recently, Bang et al
7
proposed a multivariable prediction model for
CKD and also reported that no other multivari-
able method existed to predict CKD. Our study
contributes to helping health care providers iden-
tify patients at high risk of CKD by simulta-
neously considering recognized traditional risk
factors and suspected nontraditional risk factors,
including periodontal disease and one of its im-
portant sequelae, edentulism, in a representative
sample of the US population.
The objective of our study is to investigate the
role of periodontal disease and other nontradi-
tional risk factors in patients with CKD by: (1)
describing and quantifying the relationship be-
tween CKD and periodontal disease, along with
the relationship between CKD and other nontra-
ditional and traditional risk factors, in the Third
National Health and Nutrition Examination Sur-
vey (NHANES III)
33
; and (2) developing a mul-
tivariable model for the association between CKD
and periodontal disease and other nontraditional
risk factors, adjusting for traditional risk factors
to identify risk factors independently associated
with the presence of CKD.
MATERIALS
Study Population
This cross-sectional study was deemed exempt by the
institutional review board, and all investigators complied
with the Data Use Restrictions for the NHANES III public-
use data set collected by the National Center for Health
Statistics, Centers for Disease Control and Prevention.
NHANES III, 1988-1994, is a complex, multistage, strati-
ed, clustered sample of the civilian noninstitutionalized US
population representative of the US population. NHANES
Fisher et al 46
includes questionnaire, laboratory-assay, and clinical-exami-
nation measures of health outcomes and explanatory vari-
ables. Data used in this study are: (1) responses to questions
regarding age, race/ethnicity, gender, income, education,
smoking, diabetes, and hypertension; (2) laboratory assays
of serum cotinine, glycated hemoglobin, plasma glucose,
serum C-reactive protein, serum creatinine, serum total
cholesterol, serum high-density lipoprotein cholesterol, se-
rum low-density lipoprotein cholesterol, urinary albumin,
and urinary creatinine; and (3) clinical examination data for
systolic and diastolic blood pressure, height, weight, and
periodontal status. We identied 12,947 adults 18 years or
older representing 140.2 million Americans with informa-
tion for kidney function and at least one risk factor, of which
11,955 had information for kidney function and all risk
factors tested in multivariable modeling.
Description of Main Outcome
The main outcome was stages 3 and 4 CKD with moder-
ate to severe decrease in kidney function, dened as GFR of
15 to 59 mL/min/1.73 m
2
(0.25 to 0.98 mL/s/1.73 m
2
).
1
This
denition was reported to be a more precise estimate of
decreased kidney function.
3
Henceforth, we refer to this
denition of stages 3 and 4 CKD simply as CKD. GFR was
estimated by using the 4-variable Modication of Diet in
Renal Disease Study equation: GFR 186.3 (serum
creatinine [mg/dL])
1.154
age
0.203
(0.742 if female)
(1.21 if black). Serum creatinine value was calibrated by
subtracting the value of 0.23 to align the NHANES measures
with creatinine assays in the aforementioned equation.
34
Description of Risk Factors
The principal exposure or predictor for this analysis is
periodontal status based on a clinical examination, and
categorized as no periodontal disease, periodontal disease,
or edentulous. Periodontal disease is dened as one or more
sites with both 4 mm or greater loss of attachment and
bleeding on the same tooth (bleeding as an indicator of
active inammation).
35
Edentulous is dened as having lost
all natural teeth. Other traditional and suspected nontradi-
tional risk factors for CKD included in the analyses are
socioeconomic status (age, race/ethnicity, gender, income,
and education), health status (diabetes mellitus and systemic
hypertension), health behavior and biomarker levels (smok-
ing, macroalbuminuria, C-reactive protein, total cholesterol,
high-density lipoprotein cholesterol, and low-density lipopro-
tein cholesterol), anthropometric assessment (body mass
index), and health care utilization (self-report of an annual
physician visit or hospitalization in the past year).
Lower income is dened as less than $20,000 annual
household income. Diabetes mellitus status is categorized as
no diabetes, diabetes with good control (7% glycated
hemoglobin), and diabetes with poorer control (7% gly-
cated hemoglobin). Diabetes mellitus is dened as fasting
plasma glucose level of 126 mg/dLor greater (7.0 mmol/L)
or 200 mg/dL or greater (11.1 mmol/L) after an oral
glucose tolerance test, or self-reported physician-diagnosed
diabetes. Systemic hypertension is dened as systolic blood
pressure greater than 140 mm Hg or diastolic blood pressure
greater than 90 mm Hg, or being told on two or more
different visits that one had hypertension. Macroalbuminuria
is dened as urinary albumin-creatinine excretion ratio of
300 mg/g or greater. Self-reported smoking status is current,
former, or never, excluding those who reported former or
never smoking but were current smokers based on the gold
standard of serum cotinine levels of 15 ng/mL or greater
(85 nmol/L).
36
Obesity is dened as a body mass index
greater than 27 kg/m
2
. High C-reactive protein level is
dened as greater than 3.0 mg/dL.
Statistical Analyses
Tests of the hypothesis that CKD is associated with
traditional and nontraditional risk factors used univariable
and multivariable logistic regression modeling. Covariates
were selected by using a stepwise regression approach with
P value less than 0.05 as the selection criterion to enter and
remain in the model. This approach simultaneously took into
account the statistically signicant risk factors determined
by means of univariable analyses, with statistical signi-
cance reported as a 95% condence interval (CI). The
independent association between CKD and risk factors,
namely, socioeconomic status, health status, health behavior
and biomarker levels, and health care utilization, was quanti-
ed by calculating the adjusted odds ratio (OR
Adj
). Model t
was assessed by means of the Satterthwaite-adjusted F
statistic test, accounting for the complex study design. Thus,
we compared the nal full model with periodontal disease to
the reduced model with all the same covariates excluding
periodontal status. Analyses were conducted using SAS-
Callable SUDAAN, version 9.0.1 (Research Triangle Insti-
tute, Research Triangle Park, NC)
37
and SAS Systems for
Windows, version 9.1 (SAS Institute Inc, Cary, NC) to
account for complex survey design and sample weights and
to produce national estimates.
RESULTS
Overall Descriptive Summary
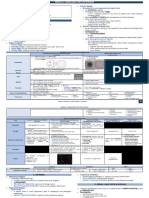
Table 1 presents important characteristics of
the study population and their unadjusted associa-
tion with CKD. Overall, 3.6% of the study popu-
lation had CKD, 6.0% had periodontal disease,
10.5% were edentulous, 23.5% were hyperten-
sive, and 36.4% were obese. The univariable
models reported in Table 1 are similar to the
typical approach that reports a single risk factor
without adjusting for potential confounders. For
example, an adult with the nontraditional risk
factor edentulism was over 10 times more likely
to have CKD (odds ratio [OR
Crude
], 10.38; 95%
CI, 7.87 to 13.70) than an adult without periodon-
tal disease. Likewise, an adult with periodontal
disease was 4 times more likely to have CKD
(OR
Crude
, 3.93; 95% CI, 2.95 to 5.24) than an
adult without periodontal disease.
Periodontal Disease and CKD 47
Table 1. Descriptive Summary and Association Between CKD and Periodontal Disease and Other Risk Factors
No CKD CKD OR
Crude
Risk Factors (n 12,330; 96.4%) (n 617; 3.6%) (95% CI)
Socioeconomic status
Age (y)
18-59 (n 9,575; 81.4%) 83.9% 16.3% 1.00
60 (n 3,372; 18.6%) 16.1% 83.7% 26.78 (17.74-40.43)*
Race/ethnicity
Non-Hispanic white (n 5,051; 82.2%) 81.9% 91.3% 5.57 (3.88-8.01)*
Non-Hispanic black (n 3,472; 11.5%) 11.7% 7.4% 3.18 (2.11-4.79)*
Mexican-American (n 3,890; 6.3%) 6.4% 1.3% 1.00
Gender
Female (n 6,922; 52.5%) 52.1% 61.8% 1.49 (1.11-1.99)*
Male (n 6,025; 47.5%) 47.9% 38.2% 1.00
Lower income
Yes (n 6,004; 32.0%) 31.1% 56.7% 2.90 (2.31-3.65)*
No (n 6,725; 68.0%) 68.9% 43.3% 1.00
High school graduate
Yes (n 7,826; 76.6%) 77.5% 53.8% 1.00
No (n 5,040; 23.4%) 22.5% 46.2% 2.95 (2.31-3.78)*
Health status and health behavior
Periodontal status
Edentulous (n 1,610; 10.5%) 9.2% 41.8% 10.38 (7.87-13.70)*
Periodontal disease (n 1,271; 6.0%) 5.8% 11.2% 3.93 (2.95-5.24)*
No periodontal disease (n 10,066; 83.5%) 85.0% 47.0% 1.00
Diabetes
Poor control (n 642; 3.1%) 2.8% 12.1% 5.22 (3.19-8.53)*
Good control (n 512; 3.0%) 2.7% 9.7% 4.32 (2.98-6.27)*
No diabetes (n 11,784; 93.9%) 94.5% 78.2% 1.00
Hypertension
Yes (n 3,659; 23.5%) 21.7% 70.8% 8.73 (6.93-10.99)*
No (n 9,274; 76.5%) 78.3% 29.2% 1.00
Macroalbuminuria
Yes (n 231; 1.0%) 0.7% 8.4% 12.71 (7.92-20.42)*
No (n 12,716; 99.0%) 99.3% 91.6% 1.00
Obesity
Yes (n 5,463; 36.4%) 36.0% 47.4% 1.61 (1.27-2.03)*
No (n 7,460; 63.6%) 64.0% 52.6% 1.00
High C-reactive protein
Yes (n 171; 1.0%) 0.9% 2.8% 3.14 (1.56-6.33)*
No (n 12,767; 99.0%) 99.1% 97.2% 1.00
High cholesterol
Yes (n 2,403; 18.0%) 17.2% 38.9% 3.06 (2.45-3.83)*
No (n 10,505; 82.0%) 82.8% 61.1% 1.00
Low high-density lipoprotein
Yes (n 1,560; 12.9%) 12.6% 20.5% 1.78 (1.34-2.36)*
No (n 11,256; 87.1%) 87.4% 79.5% 1.00
High low-density lipoprotein
Yes (n 948; 16.3%) 15.8% 32.2% 2.53 (1.72-3.70)*
No (n 4,600; 83.7%) 84.2% 67.8% 1.00
Smoking status
Never (n 6,739; 48.2%) 48.3% 44.9% 1.96 (1.40-2.74)*
Former (n 2,753; 22.4%) 21.7% 40.8% 3.95 (2.83-5.53)*
Current (n 3,455; 29.4%) 30.0% 14.3% 1.00
Hospitalized in past year
Yes (n 1,661; 11.3%) 10.8% 23.0% 2.45 (1.89-3.18)*
No (n 11,250; 88.7%) 89.2% 77.0% 1.00
Annual physician visit
Yes (n 10,190; 80.8%) 80.4% 92.2% 2.90 (1.87-4.50)*
No (n 2,656; 19.2%) 19.6% 7.8% 1.00
Note: Unweighted number with weighted percent. Excludes those who reported never or former smoking with serum
cotinine level indicating current smoker. Inclusion criteria were periodontal examination or edentulous.
Abbreviations: CKD, chronic kidney disease; OR
Crude
, unadjusted odds ratio for the association between CKD and the
suspected/recognized risk factors; CI, condence interval.
*P 0.05.
Fisher et al 48
Multivariable Logistic Regression Model
for the Association Between CKD and
Periodontal Disease and Other
Nontraditional Risk Factors
Table 2 presents the most parsimonious model
we estimated for the association between CKD
and periodontal disease and other nontraditional
risk factors, simultaneously adjusting for the
listed risk factors and reporting OR
Adj
and 95%
CI for each risk factor. Adults with periodontal
disease and edentulous adults were approxi-
mately twice as likely to have CKD (OR
Adj
,
1.60; 95% CI, 1.16 to 2.21; OR
Adj
, 1.85; 95% CI,
1.34 to 2.56, respectively) than adults without
periodontal disease after simultaneously adjust-
ing for age, race/ethnicity, gender, income, smok-
ing status, macroalbuminuria, hypertension, total
cholesterol level, high-density lipoprotein choles-
terol level, and hospitalizations, and physician
visits in the past year. It is also noted that older
adults were over 10 times more likely to have
CKD (OR
Adj
, 10.32; 95% CI, 6.97 to 15.27) than
younger adults after simultaneously adjusting for
the other statistically signicant risk factors or
risk indicators.
The t of the nal full model with periodontal
status listed in Table 2 is improved compared to
the reduced model with the same risk factors
excluding periodontal status, based on the Satter-
thwaite-adjusted F statistic P value of 0.0005.
This indicates that including periodontal status in
the model provides a statistically signicant con-
tribution to a model that excluded periodontal
status.
DISCUSSION
In our US population-based study, periodontal
disease and edentulism, as well as the nontradi-
tional risk factors that included having an annual
physician visit and being hospitalized in the past
year, were independently associated with CKD
after simultaneously adjusting for the following
traditional risk factors: age, race/ethnicity, gen-
der, smoking status, income, hypertension, mac-
roalbuminuria, total cholesterol level, and high-
density lipoprotein cholesterol level. Our
univariable unadjusted models support the previ-
ous studies that described high-risk subgroups by
using a single risk factor.
1-3,8-23
Additionally, our
study of a sample representative of the US popu-
lation provides a basis to extend the list of
potential nontraditional risk factors to include
periodontal disease status in a multivariable
model for the outcome CKD.
The ndings of this study suggest the impor-
tance of simultaneously taking into account other
risk factors, rather than the typical approach of
identifying high-risk subgroups for CKD based
on a single risk factor. By comparing the OR
Crude
with the OR
Adj
, the need to consider these other
covariates is evident. For example, when age
was the only risk factor considered, older adults
were 27 times more likely to have CKD. How-
ever, when the other risk factors were simulta-
neously taken into account, older adults were 10
times more likely to have CKD. Likewise, when
periodontal status was the only risk factor consid-
ered, adults with edentulism were over 10 times
more likely to have CKD, and adults with peri-
odontal disease were 4 times more likely to have
CKD. However, when the other risk factors were
Table 2. Multivariable Model for the Association
Between CKD and Periodontal Disease and Other
Risk Factors
Risk Factors Final Model OR
Adj
(95% CI)
Age 60 y 10.32 (6.97-15.27)*
Macroalbuminuria 5.13 (2.74-9.63)*
Race/ethnicity
Non-Hispanic white
Non-Hispanic black
3.53 (2.36-5.28)*
2.40 (1.57-3.68)*
Hypertension 2.12 (1.66-2.71)*
Smoking status
Former smoker
Never smoker
1.99 (1.41-2.79)*
1.55 (1.10-2.20)*
Periodontal status
Edentulous
Periodontal disease
1.85 (1.34-2.56)*
1.60 (1.16-2.21)*
Low high-density lipoprotein 1.80 (1.24-2.60)*
Hospitalized in past year 1.68 (1.24-2.27)*
Low income 1.65 (1.29-2.11)*
Annual physician visit 1.65 (1.10-2.50)*
High cholesterol level 1.47 (1.14-1.90)*
Female 1.45 (1.05-2.01)*
Note: The following risk factors were not included in the
nal model because they were not statistically signicant:
education, diabetes status, high C-reactive protein level,
and high low-density lipoprotein cholesterol level. Ex-
cludes those who reported never or former smoking with
serum cotinine level indicating current smoker.
Abbreviations: CKD, chronic kidney disease; OR
Adj
, odds
ratio for the association between CKD, simultaneously
taking into account all the listed potential or recognized risk
factors; CI, condence interval.
*P 0.05.
Periodontal Disease and CKD 49
simultaneously considered, adults with edentu-
lism were almost twice as likely, and adults with
periodontal disease were over 1 times more
likely to have CKD. In addition, when diabetes
status, obesity, C-reactive protein level, and edu-
cation were considered separately, they were
signicant. However, after simultaneously tak-
ing into account the other risk factors, including
periodontal disease status, they were no longer
signicant.
Although African Americans were reported to
be more likely to have CKD than whites,
4,11
this
was not found in our study or in a previous
NHANES III study.
3
This inconsistency may be
partly explained by racial disparity in survival,
such that the prevalence of CKD may be greater
in non-Hispanic whites than non-Hispanic blacks,
whereas the incidence is greater in non-Hispanic
blacks, but they do not survive as long. In addi-
tion, our ndings of greater racial disparities in
unadjusted than adjusted analyses indicate that
results are partly explained by confounding due
to health status, health behaviors, socioeconomic
characteristics, and health care utilization.
An important limitation of this study is its
cross-sectional design, which did not allow for
assessment of temporality. To establish causality,
it is imperative to show that periodontal disease,
as the exposure, precedes the development or
progression of CKD. This cannot be determined
in a cross-sectional study. Another limitation to
consider is that factors that lead to CKD could
also lead to periodontal disease. These are both
chronic conditions that progress in severity. Simi-
lar to the 5 progressive stages of CKD, periodon-
tal disease progresses with increasing loss of
connective tissue attachment and bony support,
often ultimately resulting in tooth loss. Based on
the review of traditional and nontraditional risk
factors for CKD reported herein, and a thorough
recent review of risk factors for periodontal
disease,
38
and more recent publications,
29,30
the
following potential confounders/risk factors are
in common for both diseases and were consid-
ered in our modeling: age, race/ethnicity, gender,
income, education, poorly controlled diabetes,
smoking, obesity, C-reactive protein level, cho-
lesterol level, high-density lipoprotein choles-
terol level, and low-density lipoprotein choles-
terol level. Support for periodontal status having
an independent association with CKD comes in
part from our analytical modeling approach that
involved the simultaneous assessment of poten-
tial confounders/risk factors common to both
periodontal disease and CKD.
Although we make no claims of causality,
several other features of this study warrant fur-
ther consideration of periodontal disease as a
potential risk factor for CKD. First, we found
that the strength of the unadjusted association for
the nontraditional risk factors edentulism and
periodontal disease is similar to the unadjusted
association between the traditional risk factor
poorly controlled diabetes. Second, the signi-
cant association we found is consistent with
previous studies nding a signicant association
between periodontal disease and renal dis-
ease.
20-22
Third, there is biological plausibility
for chronic periodontal disease as a source of
systemic inammatory burden
28
contributing to
the chronic inammation associated with CKD.
Fourth, our results are consistent with a dose-
response for periodontal status. When we as-
sessed a dose-response ranging fromno periodon-
tal disease to mild to moderate periodontal disease
to severe periodontal disease with 6 mm or
greater loss of attachment,
35
or 80th percentile of
the highest percentage of teeth with periodontal
disease, to edentulous, we found a dose-response
in which the odds of CKD increased as the
severity or extent of periodontal disease in-
creased, similar to that previously reported.
20
Our study has several other strengths. First,
we focused on the simultaneous assessment of
recognized and suspected risk factors for CKD,
nding that some previously recognized factors
were no longer signicant, whereas infrequently
studied nontraditional risk factors, namely peri-
odontal disease and edentulism, remained signi-
cant in the nal multivariable model. Second, the
nal model simultaneously considered 12 risk
factors for CKD rather than looking at only a
single factor at a time. Third, we addressed the
possibility that patients may deny smoking by
incorporating an objective smoking measure (ie,
serum cotinine).
39
Fourth, NHANES III sam-
pling methodology is designed to represent the
US population. Fifth, questionnaire, examina-
tion, and laboratory data were collected in an
unbiased manner such that participants were un-
aware of our study of risk factors for CKD. This
allowed us to investigate multiple recognized
Fisher et al 50
traditional and suspected nontraditional risk fac-
tors. Sixth, data were available for adults who
did not have an annual physician visit, unlike
other studies limited to patients who visited
health care providers.
The next step is to test our model in longitudi-
nal studies. Periodontal therapy may be consid-
ered along with the recommendation to counsel
high-risk individuals to reduce their risk by modi-
fying their behavior, such as smoking-cessation
counseling,
40
diet modication, and exercise,
along with antihypertensive drug therapy.
1,11,41
In summary, our ndings support the conclu-
sion that periodontal disease and edentulism are
potential nontraditional risk factors indepen-
dently associated with CKD in US adults. These
results support the importance of oral health
because adults with periodontally diseased teeth
and adults who lost all their teeth were more
likely to have CKD after controlling for tradi-
tional and nontraditional risk factors. As more
studies of CKD assess the role of periodontal
disease, data will accumulate to support or refute
the inclusion of periodontal therapy in preven-
tive targeted approaches to impede the increas-
ing numbers of individuals with CKD. Addi-
tional research is needed fromprospective studies
to help assess the causal inference and from
intervention studies to assess a decrease in inci-
dence, progression, and complications of CKD.
ACKNOWLEDGEMENTS
Support: This study was supported by grants DE016031-03
and DE016031-04 from the National Institutes of Health.
Financial Disclosure: None.
REFERENCES
1. National Kidney Foundation: K/DOQI Clinical Prac-
tice Guidelines for Chronic Kidney Disease: Evaluation,
classication, and stratication. Am J Kidney Dis 39:S1-
S266, 2002 (suppl 1)
2. Centers for Disease Control and Prevention: Preva-
lence of chronic kidney disease and associated risk factors
United States, 1999-2004. MMWR Morbid Mortal Wkly
Rep 56:161-165, 2007
3. Coresh J, Byrd-Hold D, Astor BC, et al: Chronic
kidney disease awareness, prevalence, and trends among
U.S. adults, 1999 to 2000. J Am Soc Nephrol 16:180-188,
2005
4. Go A, Chertow G, Fan D, McCulloch CE, Hsu Cy:
Chronic kidney disease and the risks of death, cardiovascu-
lar events and hospitalization. N Engl J Med 351:1296-1305,
2004
5. Keith DS, Nichols GA, Guillion CM, Brown JB, Smith
DH: Longitudinal follow-up and outcomes among a popula-
tion with chronic kidney disease in a large managed care
organization. Arch Intern Med 164:659-663, 2004
6. Rahman M, Pressel S, Davis BR, et al: Cardiovascular
outcomes in high-risk hypertensive patients stratied by
baseline glomerular ltration rate. Ann Intern Med 144:172-
180, 2006
7. Bang H, Vupputuri S, Shoham DA, et al: SCreening
for Occult REnal Disease (SCORED): A simple prediction
model for chronic kidney disease. Arch Intern Med 167:
374-381, 2007
8. Stevens LA, Coresh J, Green T, Levey AS: Assessing
kidney functionMeasured and estimated glomerular ltra-
tion rate. N Engl J Med 354:2473-2483, 2006
9. Haroun MK, Jaar BG, Hoffman SC, Comstock GW,
Klag MJ, Coresh J: Risk factors for chronic kidney disease:
A prospective study of 23,534 men and women in Washing-
ton County, Maryland. J Am Soc Nephrol 14:2934-2941,
2003
10. Sarnak MJ, Levy AS, Schoolwerth AC, et al: Kidney
disease as a risk factor for development of cardiovascular
disease: A statement from the American Heart Association
Councils on Kidney in Cardiovascular Disease, High Blood
Pressure Research, Clinical Cardiology, and Epidemiology
and Prevention. Hypertension 42:1050-1065, 2003
11. Jamerson KA: Preventing chronic kidney disease in
special populations. Am J Hypertens 18:S106-S111, 2005
(suppl s)
12. Fox CS, Larson MG, Leip EP, Meigs JB, Wilson
PWF, Levy D: Glycemic status and development of kidney
disease. Diabetes Care 28:2436-2440, 2005
13. Norris KC, Agodoa LY: Unraveling the racial dispari-
ties associated with kidney disease. Kidney Int 68:914-924,
2005
14. Rule AD, Jacobsen SJ, Schwartz GL, et al: Acompari-
son of serumcreatinine-based methods for identifying chronic
kidney disease in hypertensive individuals and their siblings.
Am J Hypertens 19:608-614, 2006
15. Parikh NI, Hwang SJ, Larson MG, Meigs JB, Levy
D, Fox CS: Cardiovascular disease risk factors in chronic
kidney disease. Arch Intern Med 166:1884-1891, 2006
16. Vupputri S, Sandler DP: Lifestyle risk factors and
chronic kidney disease. Ann Epidemiol 13:712-720, 2003
17. Cohn JN, Quyyumi AA, Hollenberg NK, Jamerson
KA: Surrogate markers for cardiovascular disease: Func-
tional markers. Circulation 109:31-46, 2004
18. Tonelli M, Sacks F, Pfeffer M, Jhangri GS, Curhan G:
Biomarkers of inammation and progression of chronic
kidney disease. Kidney Int 68:237-245, 2005
19. Stenvinkel P: Newinsights on inammation in chronic
kidney disease-Genetic and non-genetic factors. Nephrol
Ther 2:111-119, 2006
20. Shultis WA, Weil EJ, Looker HC, et al: Effect of
periodontitis on overt nephropathy and end-stage renal dis-
ease in type 2 diabetes. Diabetes Care 30:306-311, 2007
21. Saremi A, Nelson RG, Tulloch-Reid M, et al: Peri-
odontal disease and mortality in type 2 diabetes. Diabetes
Care 28:27-32, 2005
22. Kshirsagar AV, Moss KL, Elter JR, Beck JD, Offen-
bacher S, Falk RJ: Periodontal disease is associated with
renal insufciency in the Atherosclerosis Risk in Communi-
ties (ARIC) Study. Am J Kidney Dis 45:650-657, 2005
Periodontal Disease and CKD 51
23. Feldman HI, Appel LJ, Chertow GM, et al: The
Chronic Renal Insufciency Cohort (CRIC) Study: Design
and method. J Am Soc Nephrol 14:S148-S153, 2003 (suppl
2)
24. Cazzavillan S, Ratanarat R, Segala C, et al: Inamma-
tion and subclinical infection in chronic kidney disease: A
molecular approach. Blood Purif 25:69-76, 2007
25. Phipps KR. Stevens VJ: Relative contribution of
caries and periodontal disease in adult tooth loss for an
HMO dental population. J Public Health Dent 55:250-252,
1995
26. Loos BG: Systemic markers of inammation in peri-
odontitis. J Periodontol 76:2106-2115, 2005
27. Offenbacher S, Beck JD: A perspective on the poten-
tial cardioprotective benets of periodontal therapy. Am
Heart J 149:950-954, 2005
28. Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow
JS: Acute-phase inammatory response to periodontal dis-
ease in the US population. J Dent Res 79:49-57, 2000
29. Tonetti MS, DAiuto F, Nibali L, et al: Treatment of
periodontitis and endothelial function. NEngl J Med 356:911-
920, 2007
30. Demmer RT, Desvarieux M: Periodontal infections
and cardiovascular disease: The heart of the matter. J Am
Dent Assoc 137:S14-S20, 2006 (suppl 2)
31. Beck JD, Offenbacher S: Systemic effects of periodon-
titis: Epidemiology of periodontal disease and cardiovascu-
lar disease. J Periodontol 76:2089-2100, 2005
32. Tonelli M, Pfeffer MA: Kidney disease and cardiovas-
cular risk. Ann Rev Med 58:123-139, 2007
33. National Center for Health Statistics: National Health
and Nutrition Examination Survey III Documentation, Code-
book, and Data Files. Available at: http://www.cdc.gov/nchs/
about/major/nhanes/datalink.htm#NHANESIII. Accessed
August 14, 2007
34. Coresh J, Astor BC, McQuillan G, et al: Calibration
and random variation of the serum creatinine assay as
critical elements of using equations to estimate glomerular
ltration rate. Am J Kidney Dis 39:920-929, 2002
35. Fisher MA, Taylor GW, Tilashalski KR: Smokeless
tobacco and severe active periodontal disease, NHANES III.
J Dent Res 84:705-710, 2005
36. Pirkle JL, Flegal KM, Bernert JT, Brody DJ, Etzel
RA, Maurer KR: Exposure of the U.S. population to environ-
mental tobacco smoke. JAMA275:1233-1240, 1996
37. Shah B, Barnwell B, Bieler G: SUDAAN Users
Manual, Release 8.0. Research Triangle Park, NC, Research
Triangle Institute, 2001
38. Borrell LN, Papapanou PN: Analytical epidemiology
of periodontitis. J Clin Periodontol 32:S132-S158, 2005
(suppl 6)
39. Fisher MA, Taylor GW, Shelton BJ, Debanne SM:
Sociodemographic characteristics and diabetes predict in-
valid self-reported non-smoking in a population-based study
of U.S. adults. BMC Public Health 7:33, 2007. Available at
http://www.biomedcentral.com/1471-2458/7/33. Accessed
November 13, 2007
40. US Department of Health and Human Services: The
Health Benets of Smoking Cessation: A Report of the
Surgeon General. Rockville, MD, US Department of Health
and Human Services, Centers for Disease Control and Pre-
vention, 1990
41. Rahman M, Pressel S, Davis BR, et al: Renal out-
comes in high-risk hypertensive patients treated with an
angiotensin-converting enzyme inhibitor or a calcium chan-
nel blocker vs a diuretic. Arch Intern Med 165:936-946,
2005
Fisher et al 52
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Journal - Liver Disease Focus On Ascites PDFDokumen2 halamanJournal - Liver Disease Focus On Ascites PDFTriLightBelum ada peringkat
- Pediatrics MnemonicsDokumen11 halamanPediatrics MnemonicsIndrajit Rana95% (21)
- MCI FMGE Previous Year Solved Question Paper 2003 PDFDokumen30 halamanMCI FMGE Previous Year Solved Question Paper 2003 PDFrekha meenaBelum ada peringkat
- Sample Paper ASAT X PDFDokumen17 halamanSample Paper ASAT X PDFanurag680% (1)
- 15 Virusne Infekcije U Trudnoci - PrevedenoDokumen7 halaman15 Virusne Infekcije U Trudnoci - PrevedenoVelibor StankovićBelum ada peringkat
- Microbiology Course FileDokumen41 halamanMicrobiology Course FileRavi IndraBelum ada peringkat
- Week-12 VirologyDokumen8 halamanWeek-12 VirologyAlex LiganBelum ada peringkat
- Bovi-Shield Gold FP 5 VL5Dokumen2 halamanBovi-Shield Gold FP 5 VL5טורו קוראזוןBelum ada peringkat
- Hair CareDokumen8 halamanHair CareNeelofur Ibran Ali100% (4)
- Managing Infectious Health Hazards and Diseases in The Construction Industry - SlidesDokumen126 halamanManaging Infectious Health Hazards and Diseases in The Construction Industry - SlidesHuzaifa SafdarBelum ada peringkat
- Pgi May 2012 Ebook PDFDokumen50 halamanPgi May 2012 Ebook PDFloviBelum ada peringkat
- Mnemonic For PharmaDokumen4 halamanMnemonic For PharmaFershell SiaoBelum ada peringkat
- Physical Therapy ReviewDokumen4 halamanPhysical Therapy Reviewpearl042008100% (1)
- Hla IgDokumen48 halamanHla Igprakas44Belum ada peringkat
- Enterobacter Spp.Dokumen32 halamanEnterobacter Spp.ntnquynhpro100% (1)
- 35-1404729796 JurnalDokumen3 halaman35-1404729796 JurnalNancy ZhangBelum ada peringkat
- NematodesDokumen10 halamanNematodesNicolette Go100% (1)
- Canine - Leptospirosis Marge PoughDokumen1 halamanCanine - Leptospirosis Marge Poughw00fBelum ada peringkat
- ChromID CPS Brochure Final-1Dokumen2 halamanChromID CPS Brochure Final-1horia96Belum ada peringkat
- Hand HygieneDokumen3 halamanHand Hygieneashlyn0203Belum ada peringkat
- The Order OnygenalesDokumen24 halamanThe Order Onygenalesnevin100% (1)
- Obstetrics Evidence-Based Algorithms, 2016Dokumen351 halamanObstetrics Evidence-Based Algorithms, 2016stase anak80% (5)
- Viral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDokumen14 halamanViral Infections of The Gastrointestinal Tract and Viral Infections of The Genitourinary SystemDARLENE CLAIRE ANDEZABelum ada peringkat
- Evaluation of Antimicrobial Activity of ZITRITIDEDokumen16 halamanEvaluation of Antimicrobial Activity of ZITRITIDEednisoBelum ada peringkat
- ImmunoSeroLab M4Dokumen3 halamanImmunoSeroLab M4ela kikayBelum ada peringkat
- The Vaccination Controversy The Rise, Reign and Fall of Compulsory Vaccination For SmallpoxDokumen273 halamanThe Vaccination Controversy The Rise, Reign and Fall of Compulsory Vaccination For Smallpoxjamie_clark_2100% (2)
- Lane J 1953 - Neotropical Culicidae Vol IDokumen550 halamanLane J 1953 - Neotropical Culicidae Vol IDavid Schiemann100% (3)
- ROTAVIRUSDokumen13 halamanROTAVIRUSAsma HossainBelum ada peringkat
- Public Health Surveillance-BHWDokumen73 halamanPublic Health Surveillance-BHWPaul Angelo E. CalivaBelum ada peringkat
- Respiratory ReflectionDokumen2 halamanRespiratory ReflectionJennalyn Padua SevillaBelum ada peringkat