Alteration of Serum Inflammatory Cytokines in Active Pulmonarytuberculosis Following Anti-Tuberculosis Drug Therapy
Diunggah oleh
darmariantoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Alteration of Serum Inflammatory Cytokines in Active Pulmonarytuberculosis Following Anti-Tuberculosis Drug Therapy
Diunggah oleh
darmariantoHak Cipta:
Format Tersedia
Molecular Immunology 62 (2014) 159168
Contents lists available at ScienceDirect
Molecular Immunology
j our nal home page: www. el sevi er . com/ l ocat e/ mol i mm
Alteration of serum inammatory cytokines in active pulmonary
tuberculosis following anti-tuberculosis drug therapy
Imran Hussain Chowdhury
a,1
, Albin Mostaque Ahmed
b
, Subhadip Choudhuri
a
,
Aditi Sen
a
, Avijit Hazra
c
, Nishith Kumar Pal
d
, Basudev Bhattacharya
a
, Bojlul Bahar
b,e,
a
Department of Biochemistry, Institute of Postgraduate Medical Education and Research (IPGME&R), 244B, AJC Bose Road, Kolkata 700020, India
b
School of Veterinary Medicine, University College Dublin, Beleld, Dublin 4, Dublin, Ireland
c
Department of Pharmacology, Institute of Postgraduate Medical Education and Research (IPGME&R), 244B, AJC Bose Road, Kolkata 700020, India
d
Department of Microbiology, Institute of Postgraduate Medical Education and Research (IPGME&R), 244B, AJC Bose Road, Kolkata - 700020, India
e
School of Agriculture and Food Science, University College Dublin, Beleld, Dublin 4, Dublin, Ireland
a r t i c l e i n f o
Article history:
Received 20 January 2014
Received in revised form30 May 2014
Accepted 3 June 2014
Available online 12 July 2014
Keywords:
Cytokine
Inammation
Immunity
Mycobacteria
Tuberculosis
a b s t r a c t
Active pulmonary tuberculosis (APTB) is associated with a failure of the host immune system to control the
invading Mycobacterium tuberculosis (Mtb). The objective of this study was to quantify and assess the role
of serum inammatory cytokines in active pulmonary tuberculosis patients following anti-tuberculosis
drug (ATD) therapy.
Blood samples were collected from APTB patients and normal healthy subjects (NHS) (total n = 204) at
baseline and 2, 4 and 6 months post-therapy and the abundance of serum inammatory cytokines were
measured by cytokine specic ELISA.
Compared to NHS, APTB patients at baseline had higher levels of serum pro-inammatory cytokines
IL-12p40 (P < 0.001), IFN- (P < 0.001), TNF- (P < 0.01), IL-1 (P < 0.001) and IL-6 (P <0.001) and anti-
inammatory cytokines IL-10 (P <0.001) and TGF-1 (P < 0.001) while there was no change in the level
of IL-4. In APTB patients, the serum levels of IFN-, TNF-, IL-6 and TGF-1 directly relate to the bacterial
load while the TNF-, IL-1, IL-6 and TGF-1 relate to radiological severity. At baseline, the IL-6 level
in NHS and APTB patients differed most and following ATD therapy, this level rapidly decreased and
stabilized by 4-month in APTB patients.
It is concluded that a subtle reduction in the serum level of IL-6 of the APTB patients following ATD
therapy might play a vital role in immune-protection of the host against Mtb infection and hence the
serum IL-6 level can be a useful marker to diagnose the effectiveness of therapy in the patients.
2014 Elsevier Ltd. All rights reserved.
1. Introduction
Mycobacterium tuberculosis (Mtb) causes life-threatening pul-
monary and extra-pulmonary tuberculosis (TB) in humans (Ellis,
2004). Mechanisms underlying host defense to Mtb infection is
poorly understood (Grange, 1992). In response to infection, the
Abbreviations: APTB, active pulmonary tuberculosis; ATD, anti-tuberculosis
drug; Mtb, Mycobacterium tuberculosis; TB, tuberculosis; IL, interleukin; IFN-,
interferon gamma; TNF-, tumor necrosis factor alfa; Th, T helper; NK, natural
killer; TGF-, transforming growth factor beta; NHS, normal healthy subjects; AFB,
acid-fast bacilli; ZN, ZiehlNeelsen; RNTCP, Revised National Tuberculosis Control
Programme; DC, dendritic cell; TLRs, toll like receptors.
Corresponding author at: School of Agriculture and Food Science, University
College Dublin, Beleld, Dublin 4, Dublin, Ireland. Fax: +353 17166258.
E-mail address: bojlul.bahar@gmail.com(B. Bahar).
1
Present address: Department of Microbiology and Immunology, School of
Medicine, University of Texas Medical Branch, Galveston, Texas, USA.
host immune cells secret a number of cytokine and chemokines
signals (Cooper and Khader, 2008), which play active roles in
initiation and regulation of the immune response at the various
stages of the disease development (Ameglio et al., 2005). Follow-
ing an anti-tuberculosis drug (ATD) therapy, it is likely that the
cytokine mediated cell signaling alters which ultimately lead to the
recovery of the TB infection. Therefore, delineating the relationship
of the major cytokines at various stages of disease progression is
necessary to understand the mechanismof host response to Mtb.
In the Mtb infected hosts, macrophages and primary immune
effector cells [neutrophils, natural killer (NK) cells and dendritic
cells (DC)] serve as the mainreservoir of the organism(Johnsonand
McMurray, 1994). The interaction of infected macrophages with T
lymphocytes is central to protective immunity against Mtb and this
interaction is mediated by a number of inammatory cytokines
produced by both cell types (Munk and Emoto, 1995). The major
cytokines produced by immune cells during the effector phases
of the immune response includes interleukin (IL)-12, interferon
http://dx.doi.org/10.1016/j.molimm.2014.06.002
0161-5890/ 2014 Elsevier Ltd. All rights reserved.
160 I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168
gamma (IFN-), andtumor necrosis factor alfa (TNF-) (Boomet al.,
2003). The secretion of TNF- by macrophages, DCs and T lym-
phocytes mainly contribute to a pro-inammatory response (Raja,
2004). Macrophages also secrete IL-12p40, which has been impli-
cated in the pathogenesis of T-cell-mediated response. IL-12p40
causes maturation of antigen-naive T helper (Th) cells into Th type
1 (Th1) cells (Trinchieri, 1994). The IFN- is secreted by Th1 cells as
well as NK cells (Cooper et al., 2011). The IFN- activates alveolar
macrophages to produce a variety of molecules involved in inhibi-
tion of growth and killing of Mtb (Denis, 1991; Conesa-Botella et al.,
2012).
The deleterious effect of excessive pro-inammatory cytokines
is attenuated by secretion of anti-inammatory cytokines
such as IL-10, transforming growth factor beta (TGF-), and
IL-4 (Raja, 2004). However, excessive production of these
anti-inammatory cytokines may completely suppress the pro-
inammatory response resulting in a failure of elimination of Mtb
infection (Sharma and Bose, 2001). Currently, only limited infor-
mation is available to decipher the immune signaling mediated
by inammatory cytokines, which activates inammatory path-
way in the TB patients undergoing ATD therapy. It is necessary
that the levels of different cytokines are ne-tuned and the del-
icate balance between the pro- and anti-inammatory cytokine
signaling is established at various stages of disease progression.
Hence, the objective of this study was to assess the role of inam-
matory cytokines in active pulmonary tuberculosis following ATD
therapy.
2. Material and methods
2.1. Study population
The study population comprised of a total of 204 individuals
with 102 newly diagnosed APTB patients admitted at Bellur ESI TB
hospital or Chest Medicine department of SSKMhospital (Institute
of Post Graduate Medical Education and Research), both located in
Kolkata, India. Atotal of 102 normal healthy subjects (NHS), mostly
students and laboratory personnel living in the same socioecono-
mic environment as the APTB patients and belonging to the same
ethnic group(Bengali descent of West Bengal) were includedinthis
study. All NHS had not taken any medication four weeks prior to
sampling. The ethics committee of the Institute of Post Graduate
Medical Education and Research, Kolkata approved this study and
written informed consent was obtained fromall APTB patients and
NHS prior to sample collection.
2.2. Sampling
Morning sputumsamples were collectedfromthe APTBpatients
on three consecutive days. TB diagnosis was based on (a) clinical
signand symptoms and radiological conrmationof pulmonary TB,
(b) presence of acid-fast bacilli (AFB) in the sputumsmear follow-
ing ZiehlNeelsen (ZN) staining test and (c) conrmation of the
presence of Mtb by multiplex-PCR technique (Chowdhury et al.,
2012). To minimize the possibility of any co-existing bacterial or
viral infection in the APTB patients, smear from the sputum and
blood samples were evaluated and viral serology and HIV testing
were performed. Patients with HIV-seropositive and co-morbid ill-
ness such as diabetes and hepatitis or opportunistic infection such
as Aspergillosis, Cryptococcidiosis or any other clinical manifesta-
tion of infection were excluded in this study. In addition, only those
APTB patients were included who had not administered with any
corticosteroids or immunosuppressive agents in the recent past.
Baseline blood sample (T0) was collected fromthe TB patients after
conrmation of the presence of active pulmonary tuberculosis and
absence of any co-existing bacterial or viral infection. Subsequent
blood samples were collected at the end of 2 (T2), 4 (T4), and 6
(T6) months of ATD therapy as described in the following section.
Single blood sample was collected fromNHS after conrmation of
the absence of any infection by clinical examinations and routine
blood tests.
All APTB patients were placed on ATD regimen. As rst line
therapy, a standard anti-tubercular regimen for all non-resistant
newly diagnosed cases comprised of Isoniazid, Rifampicin, Pyrazi-
namide and Ethambutol (thrice weekly) for two months followed
by Isoniazid and Rifampicin (thrice weekly) for four months. For
relapse patients, the regimen comprised of Isoniazid, Rifampicin,
Pyrazinamide, Ethambutol for three months plus Streptomycin
(all thrice weekly) in initial two months followed by Isoni-
azid, Rifampicin and Ethambutol (thrice weekly) for ve months.
Suspected MDR-TB patients received Kanamycin, Ooxacin (or
Levooxacin), Ethionamide, Cycloserine, Pyrazinamide andEtham-
butol for six months.
On completion of ATDtherapy for 6 months, all patients showed
clinical improvement in terms of resolution of fever and cough and
weight gain. Patients also showed resolution of chest X-ray lesions
(described below) and three consecutive sputumAFB smears were
negative before discharge. These criteria for clinical cure of the
Revised National Tuberculosis Control Programme (RNTCP), India,
were followed uniformly by the attending physicians.
2.3. Evaluation of chest radiograph
All APTB patients had undergone plain postero-anterior and lat-
eral chest radiography. Chest radiographs were evaluated for the
presence and distribution of signs relating to the active pulmonary
tuberculosis that include miliary patterns, cavity, bro-cavity, seg-
mental consolidation, lober consolidation, inltrate and patchy
opacity. To minimize any biasness by the observer, the radiographs
were initially assessed by two independent pulmonary physicians
prior to conducting any laboratory test.
2.4. Microscopy
Prior to the start of ATD therapy, morning sputum samples
were collected on three consecutive days and were investigated for
bacterial load by ZN staining technique. Stratication of the APTB
patients were performed based on the bacilli load as follows: 3+
for 1099 AFB/microscopic eld, 2+ for 19 AFB/microscopic eld,
1+ for 1099 AFB/100 microscopic elds, scanty for 19 AFB/100
microscopic elds or negative sputum smears where no AFB was
detected. Negative sputumwas further conrmed for the presence
of Mtb infection by multiplex-PCR technique described previously
(Chowdhury et al., 2012).
2.5. Cytokines assay
The abundance of serumcytokines was quantied on the blood
samples collected at baseline (T0), 2 (T2), 4 (T4) and 6 (T6) months
post-ATD therapy of APTB patients and at baseline of the NHS. A
panel of eight inammatory marker cytokines including ve pro-
inammatory (IL-12p40, IFN-, TNF-, IL-1 and IL-6) and three
anti-inammatory (IL-10, TGF-1 and IL-4) cytokines were quan-
tied in the serum fraction of the blood. Measurements of all
cytokines were performed by sandwich ELISA method and using
commercially available ELISA kits. The minimum detection limits
of different cytokines arepresentedinTable1. ELISAwas performed
following the suppliers instruction. The standards and samples for
all cytokines weremeasuredinduplicateandtheabsorbancevalues
were analyzed by non-linear regression.
I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168 161
Table 1
Cytokine specic ELISA kits, their manufacturers and the minimumdetection limits for different inammatory cytokines.
Cytokine ELISA kits Minimumdetection (pg/ml) Supplier
RayBio
Human IL-12p40 ELISA Kit <10 Raybiotech Inc. Norcross, Goergia, USA
IFN- high sensitivity human ELISA set 2.0 ImmunoTools GmbH, Friesoythe, Germany
TNF alfa high sensitivity human ELISA set 1.4 ImmunoTools GmbH, Friesoythe, Germany
RayBio
Human IL-1 ELISA Kit <0.3 Raybiotech Inc. Norcross, Goergia, USA
RayBio
Human IL-6 ELISA Kit <3.0 Raybiotech Inc. Norcross, Goergia, USA
IL-10 high sensitivity human ELISA set 1.2 ImmunoTools GmbH, Friesoythe, Germany
RayBio Human TGF-1 ELISA Kit <80 Raybiotech Inc. Norcross, Goergia, USA
IL-4 high sensitivity human ELISA set 0.6 ImmunoTools GmbH, Friesoythe, Germany
2.6. Statistical analysis
Data on demographic and clinical characteristics were com-
pared by chi-square (
2
) analysis while the differences in age and
BMI between APTB patients and NHS were evaluated by Students
t test. Differences in each variable between APTB patients and NHS
were evaluated by MannWhitney U-test. Abundances of cytokine
over-time within the APTB group were assessed by Friedman test
followedbyDunns multiple comparison. Relationshipbetweenthe
serum cytokine levels and age and BMI, were evaluated by Spear-
man correlation coefcient while that of binary clinical parameters
were evaluated by Point Biserial correlation.
3. Results
3.1. Demographic and clinical characteristics
Demographic and clinical characteristics of the APTB patients
and NHS (Table 2) indicated that there were no signicant differ-
ences of age and sex existed between the two groups. However,
at baseline, the BMI was signicantly (P<0.001) lower in the APTB
patients compared to the NHS. Following ATD therapy, there was a
conspicuous increase in the BMI during the 6 months monitoring
period (17.8 at baseline vs. 19.1 at 6 month).
3.2. Abundance of serumcytokines at baseline
At baseline, compared to NHS, APTB patients had a signi-
cantly higher level of serumpro-inammatory cytokines IL-12p40
(P<0.001), IFN- (P<0.001), TNF- (P<0.01), IL-1 (P<0.001)
and IL-6 (P<0.001) (Fig. 1). Anti-inammatory cytokines IL-10
(P<0.001) and TGF-1 (P<0.001) were also higher in the APTB
patients while there was no difference in the level of IL-4 in these
two experimental cohorts (Fig. 1).
3.3. Alteration of serumcytokine level following ATD therapy
Following ATD therapy of APTB patients, serum inammatory
cytokines were measured at baseline and 2, 4 and 6 months post-
therapy. In response to ATD therapy, the serum level of all ve
pro-inammatory cytokines signicantly (P<0.001 for all) altered
over the period of 6 months (Fig. 2) and either attained (IFN-, TNF-
andIL-1) or approached(IL-12p40 andIL-6) a value close to that
of NHS. The most interesting and dramatic response of ATDtherapy
was evident in the serumlevel of IL-6 (Fig. 2) that may be a useful
marker to diagnose the effectiveness of therapy in the patients.
In the NHS and APTB patients, the baseline serum IL-6 levels
were 51.373.62pg/ml and 362.113.87pg/ml (mean difference,
310.811.92 standard error of difference, P<0.001), respectively.
Table 2
Demographic and clinical characteristics of active pulmonary tuberculosis patients (APTB, n=102) subjected to rst-line anti-tubercular drug (ATD) treatment and normal
healthy subject (NHS, n=102).
Demographic and clinical characteristics APTB patients NHS P value
Age (yr) 31.340.67 32.230.81 0.38
Men:women 62:40 58:44 0.67
Smoker:non-smoker 38:64 81:21 <0.001
With previous history of tuberculosis 5 1 0.21
With family history of tuberculosis 6 2 0.28
Sign and symptoms:
Productive or unproductive cough 97
Weight loss (no.) 95
Fever (no.) 100
Puried protein derivative response (mm) 14.20.17 10.080.21 0.07
Body mass index (kg/m
2
):
At serumcollection 17.760.11 22.830.16 <0.001
After 2 months of ATD treatment 18.230.11
After 4 months of ATD treatment 18.610.1
After 6 months of ATD treatment 19.060.1
Bacterial Load (individual at serumcollection):
3+ 10
2+ 23
1+ 30
Scanty 32
Negative 7
Status of chest radiographs (Number of individual):
Cavitary tuberculosis 27
Fibrocavitary tuberculosis 4
Inltrate 3
Lober consolidation 17
Segmental consolidation 4
Miliary patterns 5
Patchy opacity 39
162 I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168
Fig. 1. Abundance of serumpro- and anti-inammatory cytokines in the normal healthy subject (NHS, n=102) and active pulmonary tuberculosis (APTB, n=102) patient at
baseline. Mean values (horizontal bar within each group) and error bars (95% condence interval) are shown,
*
except TGF-1 where the Y axis unit is ng/ml.
Following 2 months of ATD-therapy, in APTB patients, the IL-6 lev-
els decreased to 277.210.19pg/ml while after 4 and 6 months of
therapy, the IL-6 levels were 93.185.07 and 86.614.48pg/ml,
respectively.
In order to explore the serum IL-6 levels as a marker to diag-
nose the effectiveness of therapy in individual TB patients, changes
in the IL-6 level over the 6-months follow-up period in randomly
selected (seven) individuals from each of the four major bacterial
loadgroups are presentedinFig. 3. Across the different loadgroups,
individuals response to ATD-therapy remains broadly similar to
that of the overall pattern observed for the APTB patients (n=102)
presented in Fig. 2, that indicated that there was a rapid decrease
in the serum IL-6 levels between 0 to 4-months following ATD-
therapy. Subsequently, the serum level of IL-6 mostly stabilized
in the patients that were apparent for the whole group as well
as the randomly selected individuals representing sub-group with
different severity levels of Mtb infection.
Among the anti-inammatory cytokines measured, the tempo-
ral alteration of serum IL-10 and TGF-1 revealed a somewhat
similar pattern (Fig. 2). In this pattern, compared to the baseline
levels, the serum level of these two cytokines remain highly ele-
vated at 2 months post-therapy which is followed by a decline after
4 and 6 months post-therapy. On the other hand, the level of IL-4
had no alteration over time (Fig. 2).
3.4. Serumcytokine and BMI
Correlations of serum cytokine level with the age and BMI of
the subjects were evaluated. In both APTB patients (at baseline and
during post ATD-therapy) and NHS, the inammatory cytokines
evaluated had no correlation with age. While in NHS (at baseline),
the serumcytokine had no correlation with BMI (data not shown),
in the APTB patients at baseline, levels of IL-12p40, IFN-, TNF-
, IL-1, IL-6 and TGF-1 were negatively correlated with BMI
(Fig. 4). Negative relationship of BMI was also evident for IL-12p40,
IFN-, TNF-, IL-1, IL-10 and IL-4 (Fig. 5) and IL-6 and TGF-1
(Fig. 6) after 2 and 4 months of ATD therapy, respectively. Tempo-
ral relationship between the BMI and serum level of IL-6 over the
6-months follow-up period in randomly selected (seven) individ-
uals for each of the four major bacterial load group are presented in
Fig. 7.
The correlation among the different inammatory cytokines in
both NHS and APTB patients were also evaluated. IL-12p40 and IL-
1had a positive relationship in the NHS and in APTB patients after
2, 4 and 6 months of ATD therapy (Fig. 8) while absent in the APTB
at baseline. In the APTB patients at baseline, signicant positive
correlations existed between serum TNF- and IL-10 and TGF1
(data not shown).
3.5. Serumcytokine and disease severity
In the APTB patients, of the inammatory cytokines evaluated,
the serum levels of IFN-, TNF-, IL-6 and TGF-1 had signi-
cant relationship with the bacterial load (Fig. 9), where an increase
in these cytokines were evident with an increase in the bacterial
load. High Mtb loads (3+) was associated with high serum levels
of IFN-, IL-6 and IL-10, moderate load (2+) was associated with
high serum levels of TNF- and IL-4 while a relatively low inten-
sity Mtb load (1+ and scanty) was associated with serum TGF-1.
Serumlevels of TNF-, IL-1, IL-6 and TGF-1 were also related to
radiological severity (Fig. 9). Signicant positive correlations were
evident between the lung cavitations and serumTNF-, IL-1, and
IL-6 and negative correlation existed between patchy opacication
and serumTNF-, IL-6 and TGF-1 levels.
4. Discussion
In a cohort of ethnicity-matched active pulmonary tuberculo-
sis (APTB) patients and healthy subjects of Eastern Indian origin,
serumlevel of eight major inammatory cytokines were measured
andtheir alterationduringa 6-monthperiodfollowingATDtherapy
was assessed. At baseline, the APTB patients had a highly elevated
level of IL-12p40, IFN-, TNF-, IL-1, IL-6, IL-10 and TGF-1. Of
the different inammatory cytokines evaluated, the most inter-
esting and dramatic response of ATD therapy was evident in the
I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168 163
Fig. 2. Abundance of serum pro- (IL-12p40, IFN-, TNF-, IL-1 and IL-6) and anti-inammatory (IL-10, TGF- and IL-4) cytokines in the active pulmonary tuberculosis
(APTB, n=102) patients (o) at baseline and 2, 4 and 6 months after anti-tuberculosis drug (ATD) therapy. Abundance of inammatory cytokines in the normal healthy subjects
at baseline (
O) are also shown. Error bars are shown as standard error of means.
serum level of IL-6 that may be a useful marker to diagnose the
effectiveness of therapy in the patients.
The serum levels of inammatory cytokines IL-12p40, IFN-
, TNF-, IL-1, IL-6, IL-10 and TGF-1 were highly elevated
in the APTB patients at baseline. Upon Mtb infection of host
macrophages, a number of pro-inammatory cytokines including
IL-12p40, IFN-, TNF-, IL-1, IL-6 are secreted in excess (van
Crevel et al., 2002). The fact that the systemic levels of these
cytokines reached/approached to that of healthy subjects follow-
ing therapy, improvement in the BMI, lung cavitations, patchy
opacication and bacterial load, indicated that a recovery phase
was attained after 6-months of therapy. Of the different inam-
matory cytokines evaluated, the most interesting and conspicuous
response of ATD therapy was evident in IL-6. This is because of
the facts, rst, at baseline, the NHS and APTB patients had a high
level of IL-6 expression with little or no overlap between the NHS
(51.373.62pg/ml) and APTB patients (362.113.87pg/ml). Sec-
ond, following ATD-therapy, the IL-6 levels rapidly decreased and
stabilized at 4-month which was also evident in the individual
patients across the different levels of infection severity.
IL-6 is a pleiotropic pro-inammatory cytokine that plays an
important role in interferon signaling and protective Th1 immune
response involve in Mtb infection. An excessive activity of IL-6
inhibits IFN-, a vital signaling molecule required to activate adap-
tive immune response and stimulation of the macrophages to
ultimately kill or conne Mtb, which is critical to immune protec-
tionagainst Mtb(Nagabhushanamet al., 2003). Suchanadverserole
of excessiveIL-6was clearlydemonstratedwhenhost macrophages
withsilencedIL-6 expressionshowedhigher level of interferonand
interferon inducing gene expression leading to reduced Mtb load
(Martinez et al., 2013). In the present study, a subtle reduction in
IL-6 at 02 and 24 months of ATD-therapy was although evident,
no increase in the IFN- level was observed during the correspond-
ing period. IL-6 is associated with some deleterious effect of the
infection as it inhibits the activities of TNF- and IL-1 (van Crevel
et al., 2002). IL-6 also reportedly plays a role in the initiation of
the production of IFN- in the infected lung that plays a major role
in the activation of macrophages to protect against Mtb infection
(Saunders et al., 2000).
In Mtb infection, one of the earliest events of activation of
cell-mediated immunity involves the production of IL-12 (Flynn
and Chan, 2001). IL-12 is a pro-inammatory cytokine containing
disulde-linked heterodimer of 40kD (IL-12p40) and 35kD sub-
units. The 40kD subunit is also shared by another inammatory
164 I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168
Fig. 3. Temporal alteration in the serum IL-6 level in seven randomly selected active pulmonary tuberculosis patients following anti-tuberculosis drug (ATD) therapy
representing each of the four major bacterial load group (bacilli load 1099 AFB/microscopic eld for 3+, 19 AFB/microscopic eld for 2+, 1099 AFB/100 microscopic elds
for 1+ and 19 AFB/100 microscopic elds for scanty).
Fig. 4. Relationship between the serumlevels of inammatory cytokines with the body mass index (BMI) of active pulmonary tuberculosis (APTB) at baseline. The inam-
matory cytokines only those (IL-12p40, IFN-, TNF-, Il-1, IL-6 and TGF-1) having a statistically signicant (P<0.05) spearman correlation co-efcient (r) value are shown.
The linear regression curve of best t are shown as solid lines.
I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168 165
Fig. 5. Relationship between the serumlevels of inammatory cytokines with the body mass index (BMI) of active pulmonary tuberculosis patients after 2 months of anti-
tuberculosis drug (ATD) therapy. The inammatory cytokines only those (IL-12p40, IFN-, TNF-, Il-1, IL-10 and IL-4) having a statistically signicant (P<0.05) spearman
correlation co-efcient (r) value are shown. The linear regression curve of best t are shown as solid line.
Fig. 6. Relationship between the serumlevels of inammatory cytokines with the body mass index (BMI) of active pulmonary tuberculosis patients after 4 months of anti-
tuberculosis drug (ATD) therapy. The inammatory cytokines only those (IL-6 and TGF-1) having a statistically signicant (P<0.05) spearman correlation co-efcient (r)
value are shown. The linear regression curve of best t are shown as solid lines.
166 I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168
Fig. 7. Relationship between the BMI and serumIL-6 levels in seven randomly selected patients fromeach of the four different mycobacterial load group (bacilli load 1099
AFB/microscopic eld for 3+, 19 AFB/microscopic eld for 2+, 1099 AFB/100 microscopic elds for 1+ and 19 AFB/100 microscopic elds for scanty).
cytokine, IL-23 and hence the measured IL-12p40 level is a
reection of the activity of IL-12 and IL-23. In Mtb infection,
IL-12p40 level is elevated due to the activation of macrophages
(IL-23) and DCs (IL-12) upon successful interaction of the toll like
receptors (TLRs) present in the phagosome and cell surfaces with
the Mtb associated antigen/s (van Crevel et al., 2002; Zu niga et al.,
2012). The major functions of IL-12p40 include induction of IFN-
production from NK cells and T cells, enhancement of cytotoxity
of NK and cytotoxic T cells, and differentiation of naive T cells
into Th1 effectors, suggesting a key role for IL-12p40 in the devel-
opment of cell-mediated immunity (Aksu et al., 2001). Genetic
mutations in type-1 cytokine (IL-12p40) or type-1 cytokine recep-
tor gene such as IFN-R1, IFN-R2 and IL-12R1 are associated
with severe infections with pathogenic mycobacteria (Aksu et al.,
2001). Casanova (2001) demonstrated that a deciency in receptor
component such as IL-12R and IFN-R are highly susceptibility to
TB infections. These ndings suggested that activation of IL-12p40
and production of IFN- by NK and Th1 cells are essential for
clearance of intracellular Mtb.
In Mtb infection, macrophages, DC and T cells (Flynn and Chan,
2001) secret TNF- which contributes to the formation of granu-
loma and secretion of nitric oxide (NO), two vital mechanisms of
host response to Mtb infection (Flynn and Chan, 2001). In acute
Mtb infection, TNF- is systemically abundant and recovery is
marked by a substantial reduction in the plasma level of this
pro-inammatory cytokine (Hsieh et al., 1999). IL-1 is produced
at the site of Mtb infection where IL-1 stimulates a protective
pro-inammatory response (van Crevel et al., 2002). The intense
pro-inammatory response is associated with tissue damage that
is neutralized by the release of anti-inammatory cytokines (van
Crevel et al., 2002). This was evident in the level of IL-10 and
TGF-1 in the present study. Both IL-10 and TGF-1 suppress
T-cell functions and deactivate macrophages in Mtb infection and
thus tend to nullify the effect of pro-inammatory cytokines.
In the APTB patients, a high serum level of TNF- is likely to
be counter balanced by high levels of IL-10 and TGF-1. This
neutralizing effect of inammatory cytokines can reduce the
adverse effect of inammatory cytokines systemically distributed
in the host and minimizing the tissue damage (van Crevel et al.,
2002).
Presence of co-existing infection such as HIV and/or other
bacterial infection can substantially alter the level of serum
inammatory cytokine as infection can contribute to the pool
of systemically circulating cytokines (Riou et al., 2012). In the
present experiment, the fact that the TB patients were tested for
the presence of any co-existing bacterial and/or viral infection
including HIV and it was unlikely that any new infection success-
fully establish in the host during the period of antibiotic therapy,
the serumcytokine data mostly reect the inammatory response
specic to Mtb infection and subsequent ATD therapy. To our
knowledge, this is one of the large-scale follow up experiment
investigating the alteration in pulmonary tuberculosis patients in
Eastern Indian population over the 6-months periods following
ATD therapy.
I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168 167
Fig. 8. Relationship between the serum levels of IL-12p40 and IL-1 in active pulmonary tuberculosis (APTB) patients at baseline and after 2, 4 and 6 months of anti-
tuberculosis drug (ATD) therapy and NHS at baseline. Spearman correlation co-efcient (r) values and linear regression curve of best t (solid line) are shown.
Fig. 9. Relationship between the most promising serum inammatory cytokines and mycobacterial load (top panelbacilli loads scanty, 1+, 2+ and 3+ correspond to 19
AFB/100 microscopic elds, 1099 AFB/100 microscopic elds, 19 AFB/microscopic eld and 1099 AFB/microscopic eld, respectively) and radiological severity score
(bottom panel1; patchy opacity, 2; inltrate, 3; lober consolidation, 4; segmental consolidation, 5; brocavitary tuberculosis, 6; cavitary tuberculosis and 7; miliary
patterns) in active pulmonary tuberculosis patients (at baseline). Spearman correlation co-efcient (r) values and linear regression curve of best t (solid line) are shown.
168 I.H. Chowdhury et al. / Molecular Immunology 62 (2014) 159168
At the end of the longitudinal follow-up period of 6 months, all
patients showed clinical improvement as diagnosed on the basis
of resolution of fever and cough and chest X-ray lesions, sus-
tained weight gain and absence of any bacteria in the sputum.
In TB patients, BMI is usually related to the severity of disease
and hence a correlation between the bacterial score and BMI
can be expected. In the present experiment, the observed cor-
relations of the levels of inammatory cytokines with cachexia
(low BMI) and severity of infection (as reected by bacteriological
and radiological data) are indications of negative energy balance
in the TB patients. Such a negative energy balance is a char-
acteristic of chronic systemic inammatory diseases caused by
bacterial infection including TB (Schaible and Kaufmann, 2007)
and sepsis (Medzhitov, 2013). The leptin, a key hormone involved
in energy balance, is proposed to be an important link between
the metabolic energy status and chronic inammatory status in
TB patients (Keicho et al., 2012). However, serum level of lep-
tin was not measured in the present study, hence the role of
this hormone in the context of the correlations of inamma-
tory cytokine levels and BMI and infection severity cannot be
ascertained. A negative correlation was evident between the BMI
and serum levels of IL-6 and TGF-1 at 4 months post-therapy.
However, this correlation was lost after 6 months post-therapy.
Similarly, relationships were also evident between the lung cavi-
tations, patchy opacication and bacterial load with the levels of
serum IL-6 levels. Based on this, whether the serum levels of this
inammatory cytokine particularly IL-6 can serve, as a marker to
reect the status of Mtb infection within the host needs further
research.
5. Conclusion
In a cohort of ethnically matched TB patients of Eastern Indian
origin, the systemic level of inammatory cytokines IL-12p40,
IFN-, TNF-, IL-10, IL-6, IL-10 and TGF-1 were highly elevated
compared to the healthy subjects. Following an anti-tuberculosis
therapeutic intervention, of the different inammatory cytokines
evaluated, the most interesting and dramatic response of therapy
was evident in the serumlevel of IL-6 that may be further explored
as predictive of response to therapy particularly to determine the
clinical status of Mtb infection and disease progression in patients.
Acknowledgements
This work was supported by Indian Council of Medical Research,
Govt. of India (5/8/5/6/2009-ECD-1). We also acknowledge patients
and normal healthy subjects for voluntarily participating in this
study.
References
Ellis, S.M., 2004. The spectrum of tuberculosis and non-tuberculous mycobacterial
infection. Eur. Radiol. 14, E34E42.
Grange, J.M., 1992. The mystery of the mycobacterial persister. Tubercle Lung Dis.
73, 249251.
Cooper, A.M., Khader, S.A., 2008. The role of cytokines in the initiation, expansion,
and control of cellular immunity to tuberculosis. Immunol Rev. 226, 191204.
Ameglio, F., Casarini, M., Capoluongo, E., Mattia, P., Puglisi, G., Giosue, S., 2005. Post-
treatment changes of sixcytokines inactivepulmonarytuberculosis: differences
between patients with stable or increased brosis. Int. J. Tuberc. Lung Dis. 9,
98104.
Johnson, B.J., McMurray, D.N., 1994. Cytokine gene expression by cultures of human
lymphocytes with autologous Mycobacteriumtuberculosisinfected monocytes.
Infect. Immun. 62, 14441450.
Munk, M.E., Emoto, M., 1995. Functions of T-cell subsets and cytokines in mycobac-
terial infections. Eur. Respir. J. Suppl. 20, 668675.
Boom, W.H., Canaday, D.H., Fulton, S.A., Gehring, A.J., Rojas, R.E., Torres, M., 2003.
Human immunity to M. tuberculosis: T cell subsets and antigen processing.
Tuberculosis (Edinb.) 83, 98106.
Raja, A., 2004. Immunology of tuberculosis. Indian J. Med. Res. 120, 213232.
Trinchieri, G., 1994. Interleukin-12: a cytokine produced by antigen-presenting cells
with immunoregulatory functions in the generation of T-helper cells type 1 and
cytotoxic lymphocytes. Blood 84, 40084027.
Cooper, A.M., Mayer-Barber, K.D., Sher, A., 2011. Roleof innatecytokines inmycobac-
terial infection. Mucosal Immunol. 4, 252260.
Denis, M., 1991. Killing of Mycobacterium tuberculosis within human monocytes:
activation by cytokines and calcitriol. Clin. Exp. Immunol. 84, 200206.
Conesa-Botella, A., Meintjes, G., Coussens, A.K., van der Plas, H., Goliath, R., Schutz,
C., Moreno-Reyes, R., Mehta, M., Martineau, A.R., Wilkinson, R.J., Colebun-
ders, R., Wilkinson, K.A., 2012. Corticosteroid therapy, vitamin D status, and
inammatory cytokine prole in the HIV tuberculosis immune reconstitution
inammatory syndrome. Clin. Infect. Dis. 55, 10041011.
Sharma, S., Bose, M., 2001. Role of cytokines in immune response to pulmonary
tuberculosis. Asian Pac. J. Allergy Immunol. 19, 213219.
Chowdhury, I.H., Sen, A., Bahar, B., Hazra, A., Chakraborty, U., Choudhuri, S., Goswami,
A., Pal, N.K., Bhattacharya, B., 2012. A molecular approach to identication and
proling of rst-line drug resistant mycobacteria from sputum of pulmonary
tuberculosis patients. J. Clin. Microbiol. 50, 20822084.
vanCrevel, R., Ottenhoff, T.H., vander Meer, J.W., 2002. Innate immunity toMycobac-
teriumtuberculosis. Clin. Microbiol. Rev. 15, 294309.
Nagabhushanam, V., Solache, A., Ting, L.M., Escaron, C.J., Zhang, J.Y., Ernst, J.D., 2003.
Innate inhibition of adaptive immunity: Mycobacteriumtuberculosis-induced IL-
6 inhibits macrophage responses to IFN-gamma. J. Immunol. 171, 47504757.
Martinez, A.N., Mehra, S., Kaushal, D., 2013. Role of interleukin 6 in innate immunity
to Mycobacteriumtuberculosis infection. J. Infect. Dis. 207, 12531261.
Saunders, B.M., Frank, A.A., Orme, I.M., Cooper, A.M., 2000. Interleukin-6 induces
early gamma interferon production in the infected lung but is not required for
generation of specic immunity to Mycobacteriumtuberculosis infection. Infect.
Immun. 68, 33223326.
Flynn, J.L., Chan, J., 2001. Immunology of tuberculosis. Annu. Rev. Immunol. 19,
93129.
Zu niga, J., Torres-Garca, D., Santos-Mendoza, T., Rodriguez-Reyna, T.S., Granados,
J., Yunis, E.J., 2012. Cellular and humoral mechanisms involved in the control of
tuberculosis. Clin. Dev. Immunol. 2012, 193923.
Aksu, G., Tirpan, C., Cavus o glu, C., Soydan, S., Altare, F., Casanova, J.L., Kutukculer,
N., 2001. Mycobacterium fortuitum-chelonae complex infection in a child with
complete interleukin-12 receptor beta 1 deciency. Pediatr. Infect. Dis. J. 20,
551553.
Casanova, J.L., 2001. Mendelian susceptibility to mycobacterial infection in man.
Swiss Med. Wkly. 131, 445454.
Hsieh, S.M., Hung, C.C., Chen, M.Y., Sheng, W.H., Chang, S.C., 1999. Dynamics of
plasma cytokine levels inpatients withadvancedHIVinfectionandactive tuber-
culosis: implications for early recognition of patients with poor response to
anti-tuberculosis treatment. AIDS 13, 935941.
Riou, C., Perez Peixoto, B., Roberts, L., Ronacher, K., Walzl, G., Manca, C., Rustomjee,
R., Mthiyane, T., Fallows, D., Gray, C.M., Kaplan, G., 2012. Effect of standardtuber-
culosis treatment on plasma cytokine levels in patients with active pulmonary
tuberculosis. PLoS One 7, e36886.
Schaible, U.E., Kaufmann, S.H., 2007. Malnutrition and infection: complex mecha-
nisms and global impacts. PLoS Med. 4, e115.
Medzhitov, R., 2013. Septic shock: on the importance of being tolerant. Immunity
39, 799800.
Keicho, N., Matsushita, I., Tanaka, T., Shimbo, T., Hang, N.T., Sakurada, S., Kobayashi,
N., Hijikata, M., Thuong, P.H., Lien, L.T., 2012. Circulating levels of adiponectin,
leptin, fetuin-Aand retinol-binding protein in patients with tuberculosis: mark-
ers of metabolismand inammation. PLoS One 7, e38703.
Anda mungkin juga menyukai
- Simulation of Pulmonary Breathing PDFDokumen4 halamanSimulation of Pulmonary Breathing PDFdarmariantoBelum ada peringkat
- Jurnal Kekerapan Esofagitis-Dr - AgusDokumen15 halamanJurnal Kekerapan Esofagitis-Dr - AgusJamaluddin Ahmad100% (1)
- TB ImmunotherapyDokumen25 halamanTB ImmunotherapydarmariantoBelum ada peringkat
- A Study of Sputum Conversion in New Smear Positive Pulmonary Tuberculosis Cases at The Monthly Intervals of 1st, 2nd & 3rd Month Under Directly Observed Treatment, Short Course (Dots) RegimenDokumen11 halamanA Study of Sputum Conversion in New Smear Positive Pulmonary Tuberculosis Cases at The Monthly Intervals of 1st, 2nd & 3rd Month Under Directly Observed Treatment, Short Course (Dots) RegimendarmariantoBelum ada peringkat
- Aetiological Agents in Occupational AsthmaDokumen26 halamanAetiological Agents in Occupational AsthmadarmariantoBelum ada peringkat
- Cancer Care Ontario's Symptom Management Guide-To-Practice Loss of AppetiteDokumen31 halamanCancer Care Ontario's Symptom Management Guide-To-Practice Loss of AppetitedarmariantoBelum ada peringkat
- Cytokine Polymorphisms, Their Influence and LevelsDokumen14 halamanCytokine Polymorphisms, Their Influence and LevelsdarmariantoBelum ada peringkat
- Comorbidities of AsthmaDokumen6 halamanComorbidities of AsthmadarmariantoBelum ada peringkat
- Irritant Induced Asthma and Reactive Airways Dysfunction Syndrome Rads 2155 6121.1000174Dokumen7 halamanIrritant Induced Asthma and Reactive Airways Dysfunction Syndrome Rads 2155 6121.1000174darmariantoBelum ada peringkat
- Glucocorticoid Effects On The Immune SystemDokumen92 halamanGlucocorticoid Effects On The Immune SystemdarmariantoBelum ada peringkat
- CDC Tuberculosis - What The Physician Should KnowDokumen320 halamanCDC Tuberculosis - What The Physician Should KnowbillyBelum ada peringkat
- Diaphragmatic Dysfunction and Respiratory Illness (Review) - PulmCCMDokumen4 halamanDiaphragmatic Dysfunction and Respiratory Illness (Review) - PulmCCMdarmariantoBelum ada peringkat
- Anatomy of The Thorax (CT)Dokumen7 halamanAnatomy of The Thorax (CT)darmariantoBelum ada peringkat
- LungIndia TB and NutrtionDokumen8 halamanLungIndia TB and NutrtiondarmariantoBelum ada peringkat
- Cepheid OnDemand Report Vol 4 Issue 1 Spring 2011Dokumen12 halamanCepheid OnDemand Report Vol 4 Issue 1 Spring 2011darmariantoBelum ada peringkat
- An Unexpected Consequence of ElectronicDokumen4 halamanAn Unexpected Consequence of ElectronicdarmariantoBelum ada peringkat
- Physiotherapy in Intensive Care An Updated Systematic ReviewDokumen23 halamanPhysiotherapy in Intensive Care An Updated Systematic ReviewdarmariantoBelum ada peringkat
- Revisión DressDokumen10 halamanRevisión Dressvintage20Belum ada peringkat
- Inventory of Culture and DST Methods - July 31 2011 - FinalDokumen15 halamanInventory of Culture and DST Methods - July 31 2011 - FinaldarmariantoBelum ada peringkat
- Body weight changes in tuberculosis patients during chemotherapyDokumen8 halamanBody weight changes in tuberculosis patients during chemotherapyNiar MarhaliBelum ada peringkat
- Relationship Between Body Mass Index and Asthma Severity in AdultsDokumen6 halamanRelationship Between Body Mass Index and Asthma Severity in AdultsdarmariantoBelum ada peringkat
- Molecular Origin Lung CancerDokumen14 halamanMolecular Origin Lung CancerdarmariantoBelum ada peringkat
- Manual Hyperinflation (MHI)Dokumen7 halamanManual Hyperinflation (MHI)darmariantoBelum ada peringkat
- Updating The International Standards For Tuberculosis CareDokumen9 halamanUpdating The International Standards For Tuberculosis CaredarmariantoBelum ada peringkat
- Cytokine Polymorphisms, Their Influence and LevelsDokumen14 halamanCytokine Polymorphisms, Their Influence and LevelsdarmariantoBelum ada peringkat
- Article Tuberculosis Among Diabetic PatientDokumen14 halamanArticle Tuberculosis Among Diabetic PatientdarmariantoBelum ada peringkat
- Prognostic Values of Serum IP-10 and IL-17 inDokumen10 halamanPrognostic Values of Serum IP-10 and IL-17 indarmariantoBelum ada peringkat
- ISTC 3rdedDokumen92 halamanISTC 3rdedmichaelqurtisBelum ada peringkat
- Perbandingan Validasi APACHE II Dan SOFA ScoreDokumen10 halamanPerbandingan Validasi APACHE II Dan SOFA ScoredarmariantoBelum ada peringkat
- Sopori 2002 PDFDokumen7 halamanSopori 2002 PDFVasilScherbaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Division Celular Mitosis y MeiosisDokumen5 halamanDivision Celular Mitosis y MeiosisGiovanna Macías100% (1)
- Unit 4 ObesityDokumen40 halamanUnit 4 Obesityapi-306481199Belum ada peringkat
- 001 Run Less Run Faster - Marathon Training With The FIRST MethodDokumen2 halaman001 Run Less Run Faster - Marathon Training With The FIRST MethodEduardo Medina0% (2)
- NKC Fast Facts - Poop Chart - 5 2017 PDFDokumen1 halamanNKC Fast Facts - Poop Chart - 5 2017 PDFFaniaBelum ada peringkat
- Burn OutDokumen8 halamanBurn OutAtiqahAzizanBelum ada peringkat
- Essencial Phrasal VerbsDokumen4 halamanEssencial Phrasal VerbsalvereBelum ada peringkat
- Understanding the Physiology of Oxygen DeliveryDokumen6 halamanUnderstanding the Physiology of Oxygen DeliveryBharath NarasimhaBelum ada peringkat
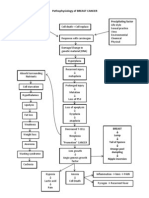
- Pathophysiology of BREAST CANCERDokumen1 halamanPathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- 06 - Cell Nucleus and ChromosomesDokumen57 halaman06 - Cell Nucleus and Chromosomessabina maharaniBelum ada peringkat
- Laryngeal ObstructionDokumen59 halamanLaryngeal ObstructionpravinBelum ada peringkat
- Trimestral Exam First GradeDokumen3 halamanTrimestral Exam First Gradeemmanuel espinozaBelum ada peringkat
- IGCSE Biology 2015 Paper 21Dokumen20 halamanIGCSE Biology 2015 Paper 21VeronicaAndrianBelum ada peringkat
- Topic Test Oxfordaqa Int Gcse Biology 9201 BioenergeticsDokumen29 halamanTopic Test Oxfordaqa Int Gcse Biology 9201 BioenergeticsNovanolo Christovori ZebuaBelum ada peringkat
- Cardiology Teaching PackageDokumen13 halamanCardiology Teaching Packagesarah morleyBelum ada peringkat
- Chapter 1 - INTRODUCTION TO ANATOMY AND PHYSIOLOGY PDFDokumen121 halamanChapter 1 - INTRODUCTION TO ANATOMY AND PHYSIOLOGY PDFKorina Marawis67% (3)
- Antiarrhythmic Drugs-Test-1-QuestionsDokumen7 halamanAntiarrhythmic Drugs-Test-1-QuestionsDrishya Bioplannet100% (2)
- Cell Membrane Structure and FunctionDokumen18 halamanCell Membrane Structure and Functionkevin_ramos007Belum ada peringkat
- Physiology of The Liver: Corresponding AuthorDokumen12 halamanPhysiology of The Liver: Corresponding AuthorMansour HazaBelum ada peringkat
- UQU SLE CORRECTED FILE by DR Samina FidaDokumen537 halamanUQU SLE CORRECTED FILE by DR Samina Fidaasma .sassi100% (1)
- mx400 PDFDokumen534 halamanmx400 PDFalissonandraBelum ada peringkat
- Q and A DactylosDokumen56 halamanQ and A DactylosJUNN REE MONTILLA100% (2)
- Types of Plant HormonesDokumen6 halamanTypes of Plant HormonesKarren ReyesBelum ada peringkat
- PKa LectureDokumen26 halamanPKa LectureShelley JonesBelum ada peringkat
- Insulin Regulation of Gluconeogenesis 2018Dokumen25 halamanInsulin Regulation of Gluconeogenesis 2018Владимир ДружининBelum ada peringkat
- Infinity Urea Liquid Reagent ENDokumen2 halamanInfinity Urea Liquid Reagent ENKouame FrancisBelum ada peringkat
- CK-MB production method reportDokumen1 halamanCK-MB production method reportOkura JoshuaBelum ada peringkat
- Neuroscience Pathways Fall 2012Dokumen46 halamanNeuroscience Pathways Fall 2012Yezin ShamoonBelum ada peringkat
- New European Guidelines Address Hyponatremia ManagementDokumen5 halamanNew European Guidelines Address Hyponatremia ManagementGherciuChirilaLarisaBelum ada peringkat
- Neurology SyllabusDokumen42 halamanNeurology SyllabusCHALAPATHI ENJAPURIBelum ada peringkat
- Regenesis 1Dokumen14 halamanRegenesis 1White Light100% (3)